Drug treatment of Parkinsons disease Parkinsons Disease Parkinsons

- Slides: 10

Drug treatment of Parkinson’s disease
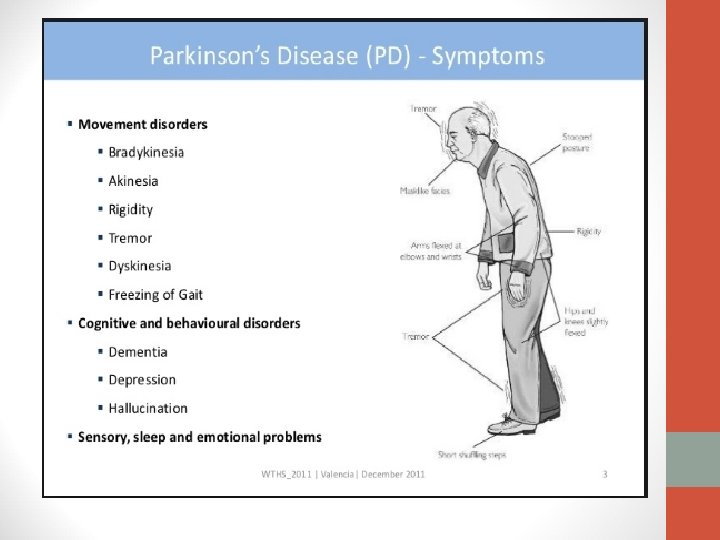
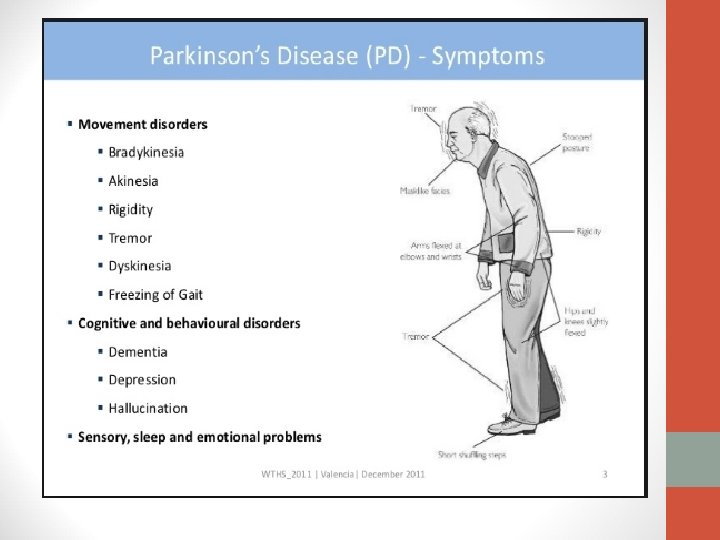
Parkinson’s Disease • Parkinson’s disease (PD) is a progressive degenerative disorder, mostly affecting older people, first described by James Parkinson in 1817. • It is an extrapyramidal motor disorder characterized by rigidity, tremor and hypokinesia with secondary manifestations like defective posture and gait, mask-like face; and sometimes dementia. • If untreated the symptoms progress over several years to end-stage disease in which the patient is rigid, unable to move, unable to breathe properly; succumbs mostly to chest infections/embolism. • The disease is characterized by progressive loss/deficiency of dopaminereleasing neurons in the brain (specifically in the substantia nigra). This results in deficiency of dopamine (DA) in the striatum which controls muscle tone and coordinates movements. • An imbalance between dopaminergic (inhibitory) and cholinergic (excitatory) system in the striatum occurs giving rise to the motor defect. • Though the cholinergic system is not primarily affected, its suppression (by anticholinergics) tends to restore balance
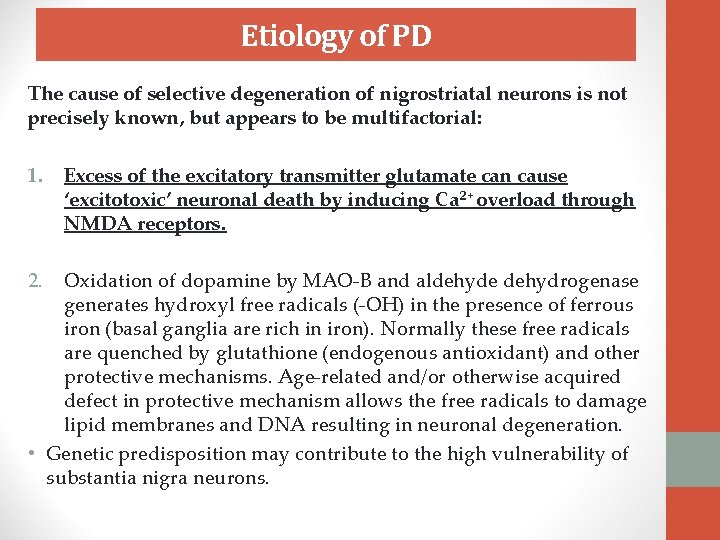
Etiology of PD The cause of selective degeneration of nigrostriatal neurons is not precisely known, but appears to be multifactorial: 1. 2. Excess of the excitatory transmitter glutamate can cause ‘excitotoxic’ neuronal death by inducing Ca 2+ overload through NMDA receptors. Oxidation of dopamine by MAO-B and aldehyde dehydrogenase generates hydroxyl free radicals (-OH) in the presence of ferrous iron (basal ganglia are rich in iron). Normally these free radicals are quenched by glutathione (endogenous antioxidant) and other protective mechanisms. Age-related and/or otherwise acquired defect in protective mechanism allows the free radicals to damage lipid membranes and DNA resulting in neuronal degeneration. • Genetic predisposition may contribute to the high vulnerability of substantia nigra neurons.
3. A synthetic toxin N-methyl-4 -phenyl tetrahydropyridine (MPTP), which occurred as a contaminant of some illicit drugs, produces nigrostriatal degeneration and manifestations similar to PD by impairing energy metabolism in dopaminergic neurons. It has been proposed that MPTP-like chemicals may be present in the environment, small quantities of which accelerate age related or otherwise predisposed neuronal degeneration of parkinsonism, but there is no proof. 3. Drug-induced temporary parkinsonism due to neuroleptics, metoclopramide (dopaminergic blockers) and reserpine (Dopamine depleter). 4. A theory has it that PD could be caused by a virus, and another is that it’s caused by cerebral hypoxia (atherosclerosis in the brain) Treatment strategy v. Boost CNS dopaminergic activity
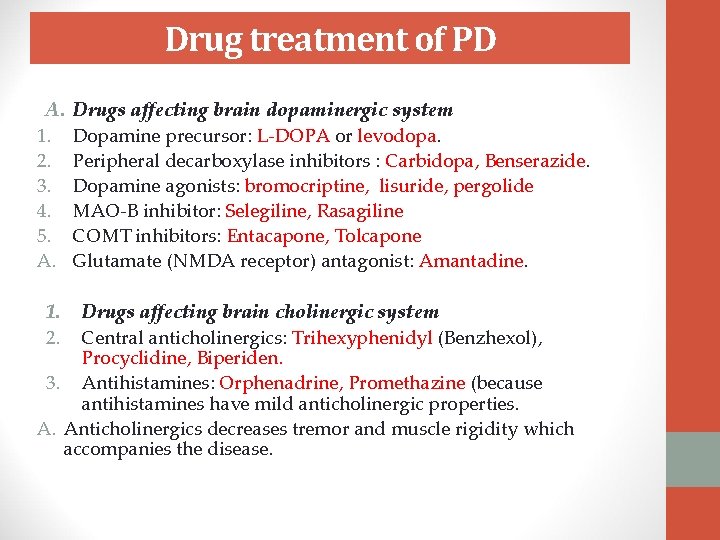
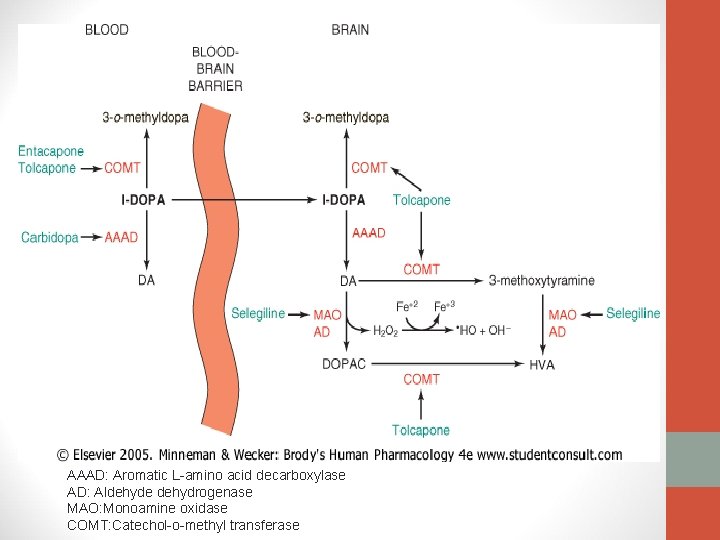
Drug treatment of PD A. 1. 2. 3. 4. 5. A. Drugs affecting brain dopaminergic system 1. 2. Drugs affecting brain cholinergic system Dopamine precursor: L-DOPA or levodopa. Peripheral decarboxylase inhibitors : Carbidopa, Benserazide. Dopamine agonists: bromocriptine, lisuride, pergolide MAO-B inhibitor: Selegiline, Rasagiline COMT inhibitors: Entacapone, Tolcapone Glutamate (NMDA receptor) antagonist: Amantadine. Central anticholinergics: Trihexyphenidyl (Benzhexol), Procyclidine, Biperiden. 3. Antihistamines: Orphenadrine, Promethazine (because antihistamines have mild anticholinergic properties. A. Anticholinergics decreases tremor and muscle rigidity which accompanies the disease.
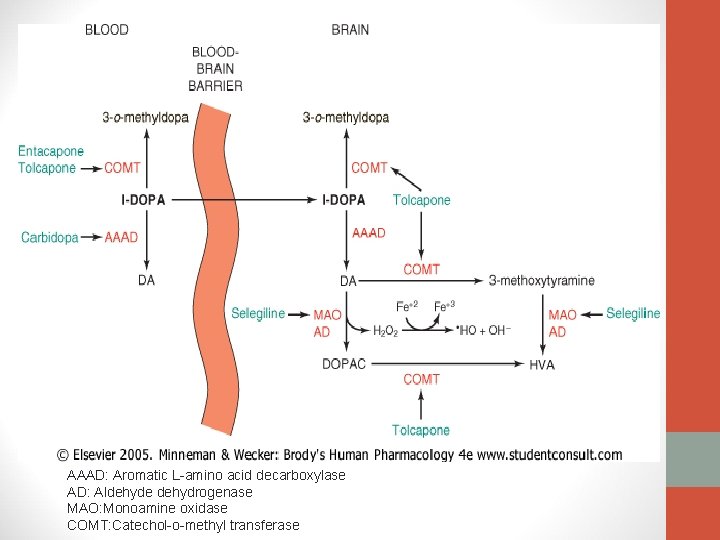
AAAD: Aromatic L-amino acid decarboxylase AD: Aldehyde dehydrogenase MAO: Monoamine oxidase COMT: Catechol-o-methyl transferase
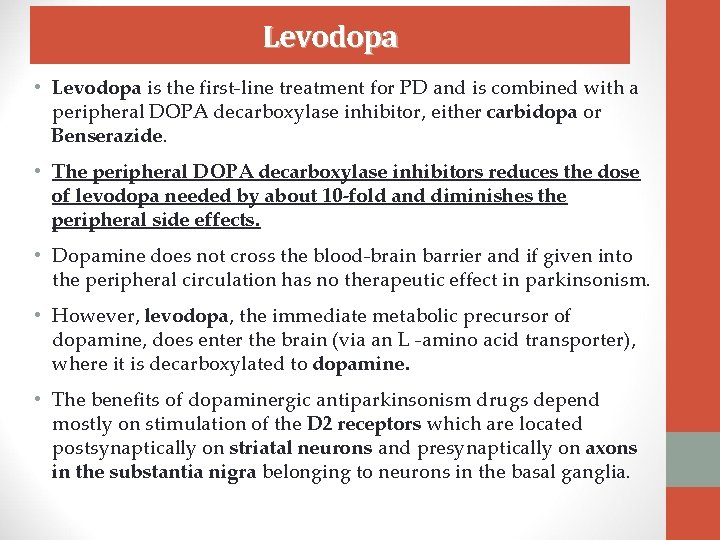
Levodopa • Levodopa is the first-line treatment for PD and is combined with a peripheral DOPA decarboxylase inhibitor, either carbidopa or Benserazide. • The peripheral DOPA decarboxylase inhibitors reduces the dose of levodopa needed by about 10 -fold and diminishes the peripheral side effects. • Dopamine does not cross the blood-brain barrier and if given into the peripheral circulation has no therapeutic effect in parkinsonism. • However, levodopa, the immediate metabolic precursor of dopamine, does enter the brain (via an L -amino acid transporter), where it is decarboxylated to dopamine. • The benefits of dopaminergic antiparkinsonism drugs depend mostly on stimulation of the D 2 receptors which are located postsynaptically on striatal neurons and presynaptically on axons in the substantia nigra belonging to neurons in the basal ganglia.
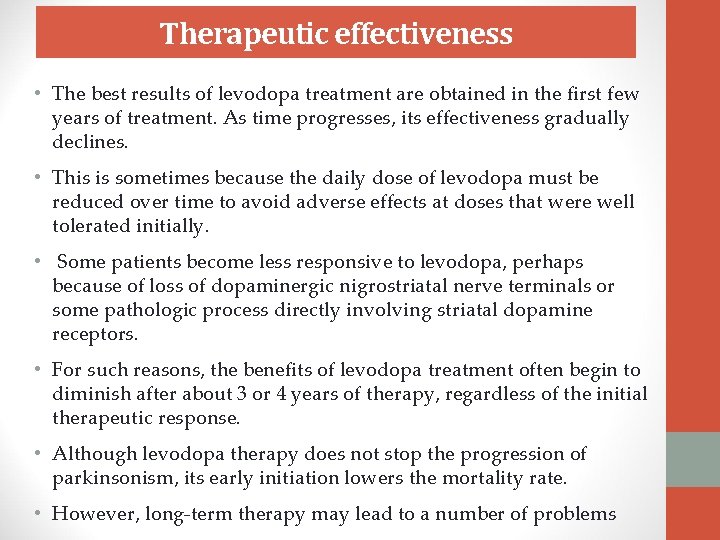
Therapeutic effectiveness • The best results of levodopa treatment are obtained in the first few years of treatment. As time progresses, its effectiveness gradually declines. • This is sometimes because the daily dose of levodopa must be reduced over time to avoid adverse effects at doses that were well tolerated initially. • Some patients become less responsive to levodopa, perhaps because of loss of dopaminergic nigrostriatal nerve terminals or some pathologic process directly involving striatal dopamine receptors. • For such reasons, the benefits of levodopa treatment often begin to diminish after about 3 or 4 years of therapy, regardless of the initial therapeutic response. • Although levodopa therapy does not stop the progression of parkinsonism, its early initiation lowers the mortality rate. • However, long-term therapy may lead to a number of problems
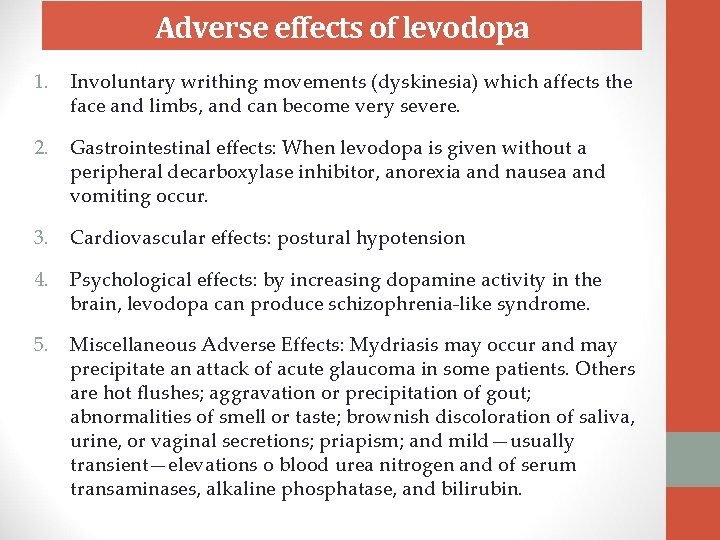
Adverse effects of levodopa 1. Involuntary writhing movements (dyskinesia) which affects the face and limbs, and can become very severe. 2. Gastrointestinal effects: When levodopa is given without a peripheral decarboxylase inhibitor, anorexia and nausea and vomiting occur. 3. Cardiovascular effects: postural hypotension 4. Psychological effects: by increasing dopamine activity in the brain, levodopa can produce schizophrenia-like syndrome. 5. Miscellaneous Adverse Effects: Mydriasis may occur and may precipitate an attack of acute glaucoma in some patients. Others are hot flushes; aggravation or precipitation of gout; abnormalities of smell or taste; brownish discoloration of saliva, urine, or vaginal secretions; priapism; and mild—usually transient—elevations o blood urea nitrogen and of serum transaminases, alkaline phosphatase, and bilirubin.
 Basal ganglia
Basal ganglia Tasha big feet
Tasha big feet Deliberate adulteration definition
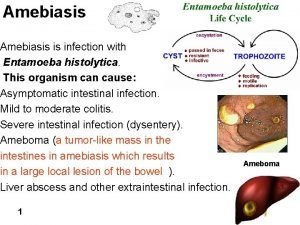
Deliberate adulteration definition Drug of choice for the treatment of extraluminal amebiasis
Drug of choice for the treatment of extraluminal amebiasis Cdtcc
Cdtcc Principles effective addiction treatment
Principles effective addiction treatment Neurosurgery
Neurosurgery Drug of choice for the treatment of extraluminal amebiasis
Drug of choice for the treatment of extraluminal amebiasis Katharine hepburn parkinsons
Katharine hepburn parkinsons Behcet disease wikipedia
Behcet disease wikipedia Shy drager syndrome
Shy drager syndrome