Drugs used in Parkinsons disease Parkinsons disease Parkinsonism

- Slides: 45
Drugs used in Parkinson’s disease
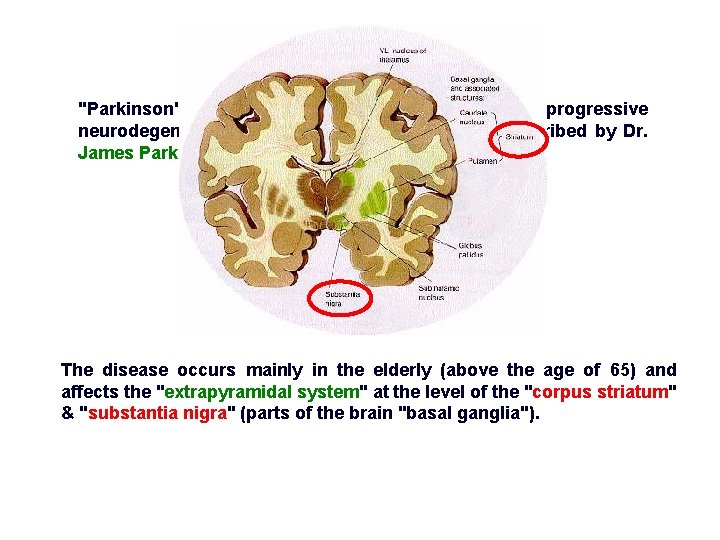
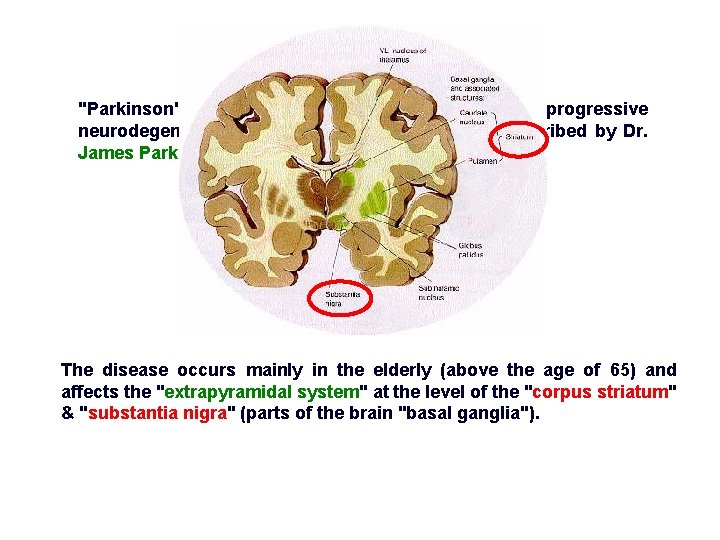
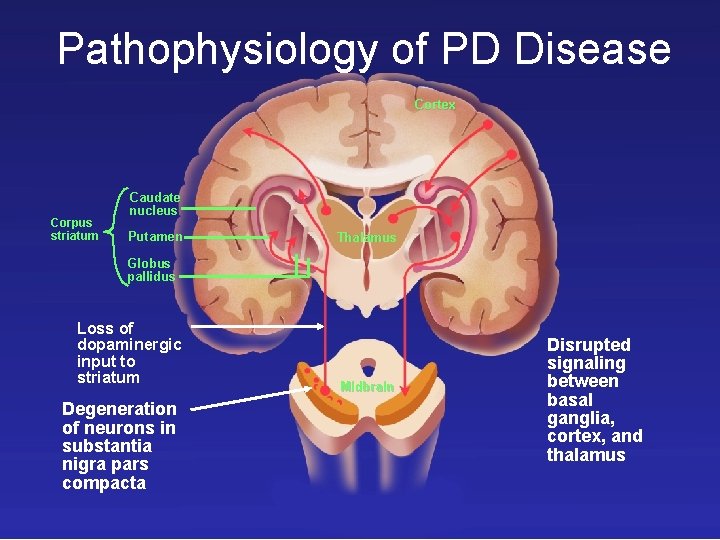
"Parkinson's disease" (Parkinsonism, PD) is a progressive neurodegenerative brain disorder that was first described by Dr. James Parkinson in 1817. The disease occurs mainly in the elderly (above the age of 65) and affects the "extrapyramidal system" at the level of the "corpus striatum" & "substantia nigra" (parts of the brain "basal ganglia").
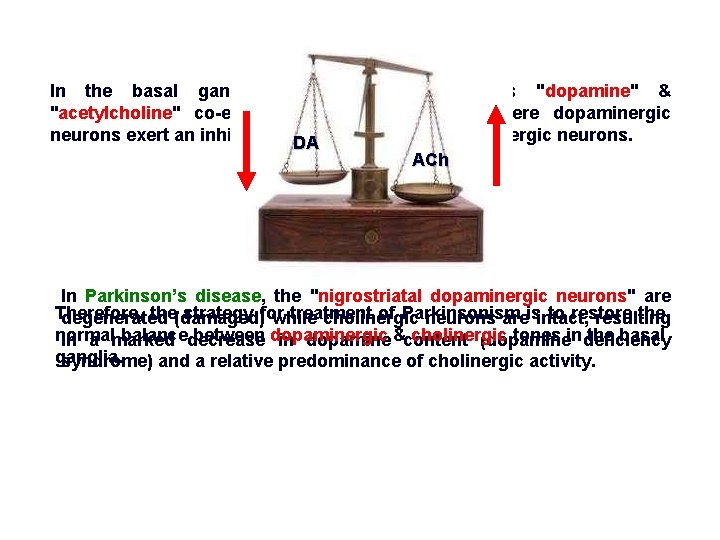
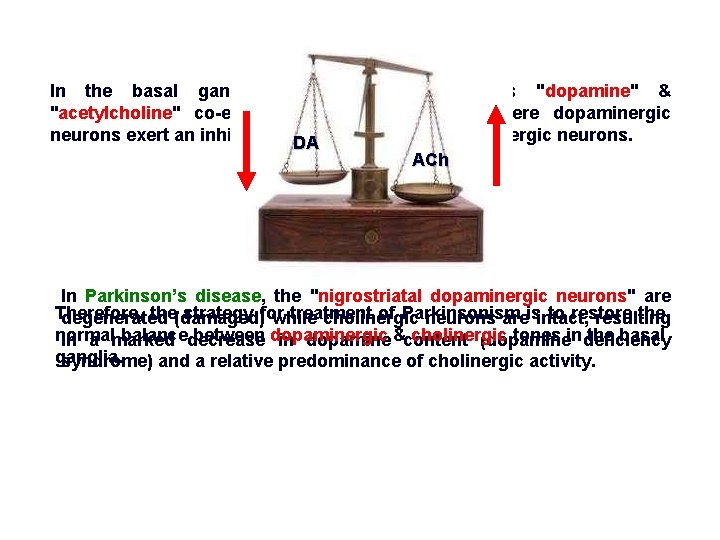
In the basal ganglia, the 2 neurotransmitters "dopamine" & "acetylcholine" co-exist in a normal balance, where dopaminergic neurons exert an inhibitory effect DA on excitatory cholinergic neurons. ACh In Parkinson’s disease, the "nigrostriatal dopaminergic neurons" are Therefore, the(damaged) strategy for treatment of Parkinsonism to restore the degenerated while cholinergic neurons areisintact, resulting normal balancedecrease between dopaminergic cholinergic tones in deficiency the basal in a marked in dopamine &content (dopamine ganglia. syndrome) and a relative predominance of cholinergic activity.
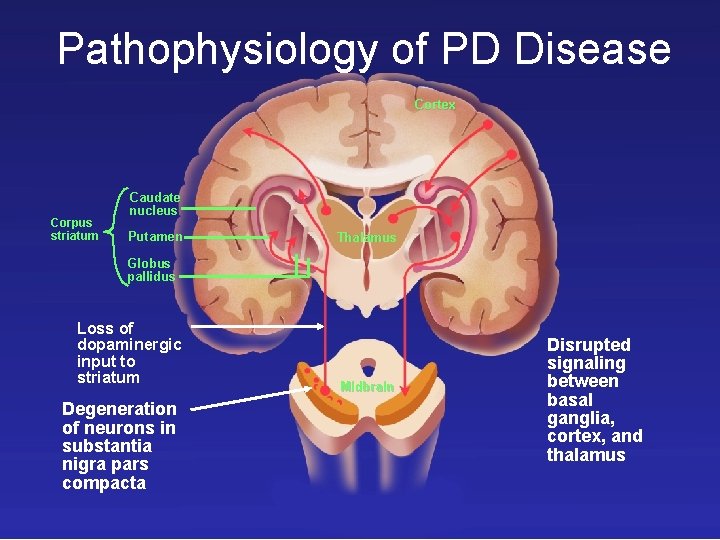
Pathophysiology of PD Disease Cortex Corpus striatum Caudate nucleus Putamen Thalamus Globus pallidus Loss of dopaminergic input to striatum Degeneration of neurons in substantia nigra pars compacta Midbrain Disrupted signaling between basal ganglia, cortex, and thalamus
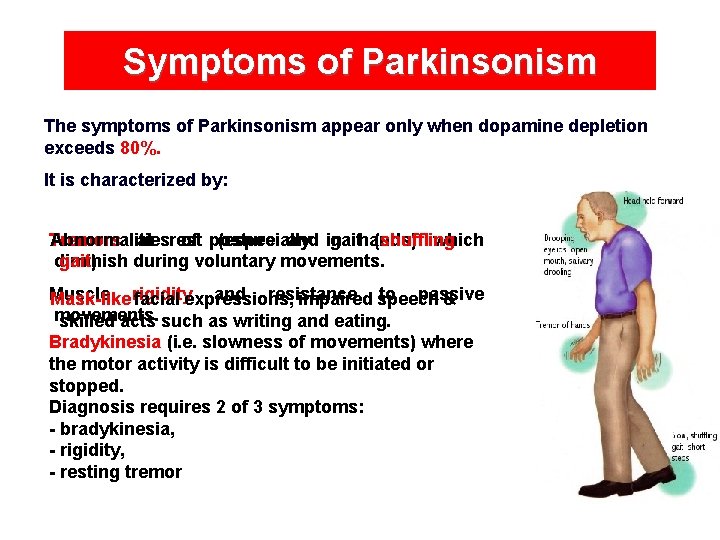
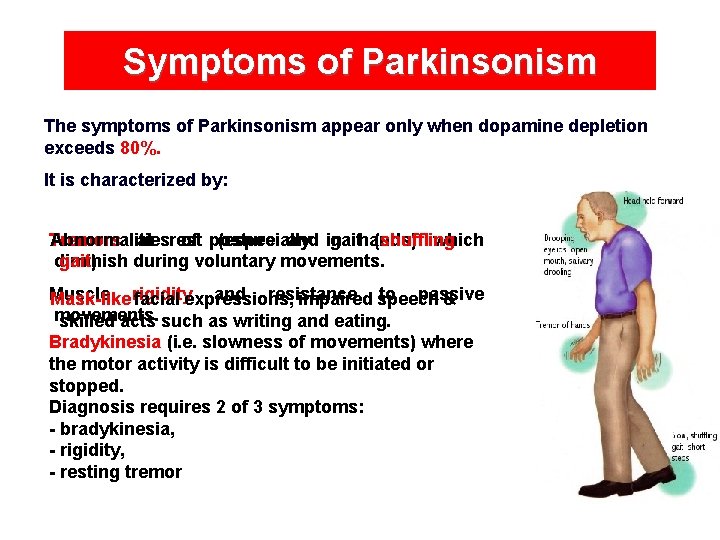
Symptoms of Parkinsonism The symptoms of Parkinsonism appear only when dopamine depletion exceeds 80%. It is characterized by: Abnormalities of posture and in gaithands) (shuffling Tremors at rest (especially which gait). diminish during voluntary movements. Muscle and resistance to passive Mask-like rigidity facial expressions, impaired speech & movements. skilled acts such as writing and eating. Bradykinesia (i. e. slowness of movements) where the motor activity is difficult to be initiated or stopped. Diagnosis requires 2 of 3 symptoms: - bradykinesia, - rigidity, - resting tremor
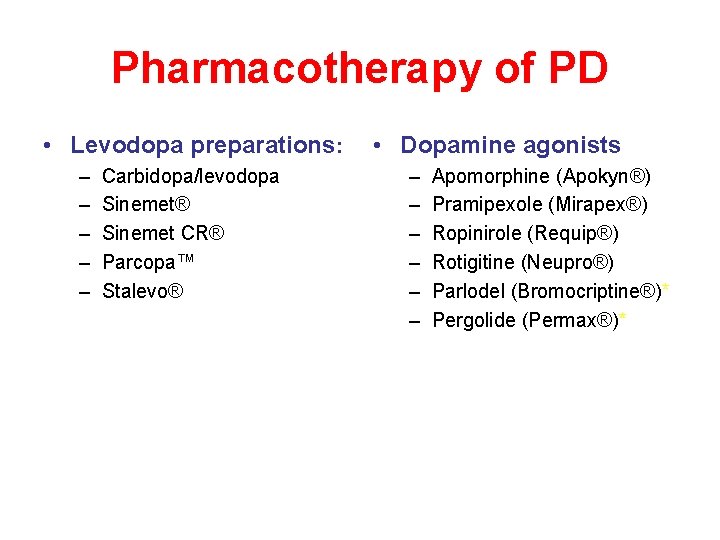
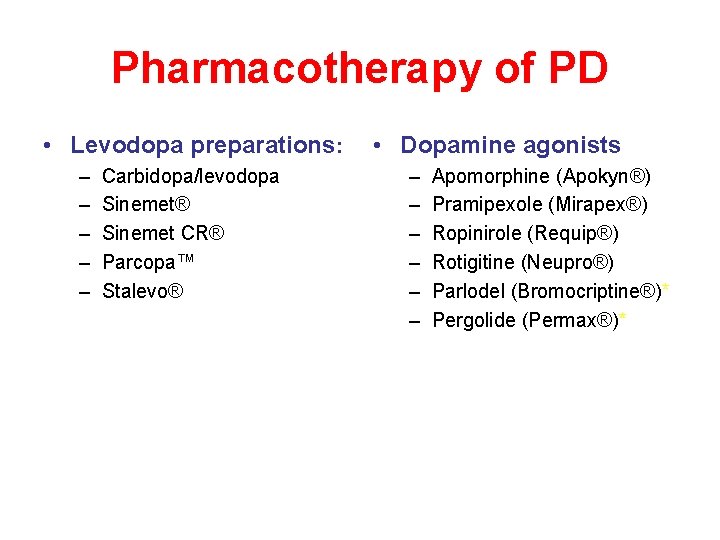
Pharmacotherapy of PD • Levodopa preparations: – – – Carbidopa/levodopa Sinemet® Sinemet CR® Parcopa™ Stalevo® • Dopamine agonists – – – Apomorphine (Apokyn®) Pramipexole (Mirapex®) Ropinirole (Requip®) Rotigitine (Neupro®) Parlodel (Bromocriptine®)* Pergolide (Permax®)*
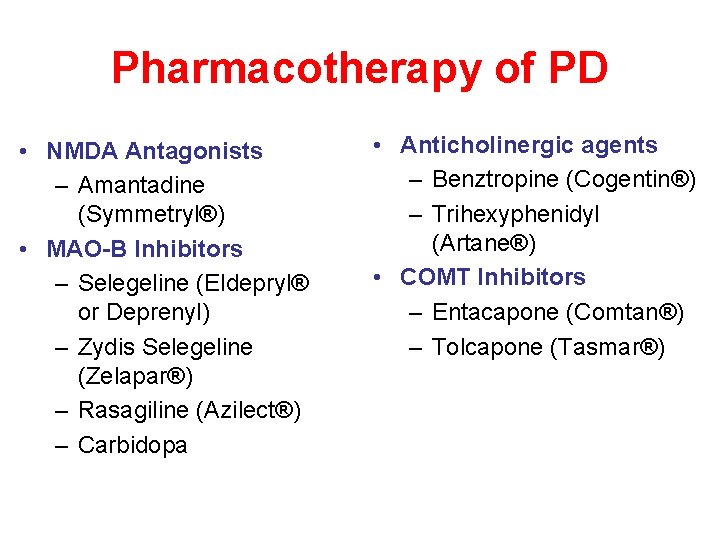
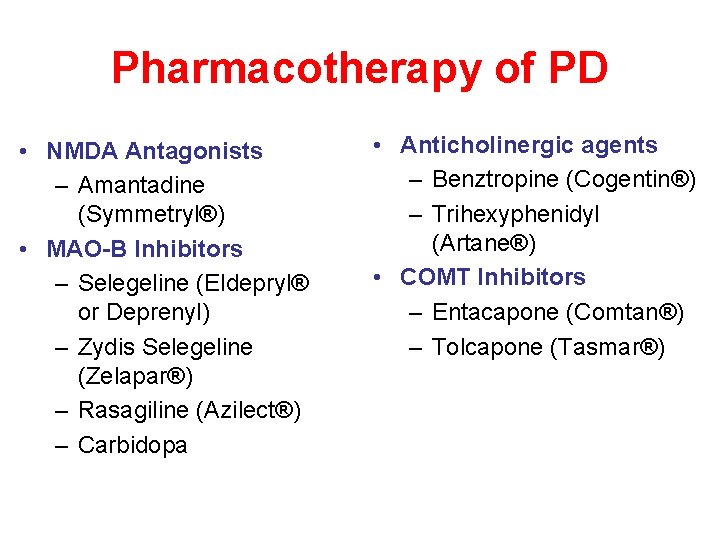
Pharmacotherapy of PD • NMDA Antagonists – Amantadine (Symmetryl®) • MAO-B Inhibitors – Selegeline (Eldepryl® or Deprenyl) – Zydis Selegeline (Zelapar®) – Rasagiline (Azilect®) – Carbidopa • Anticholinergic agents – Benztropine (Cogentin®) – Trihexyphenidyl (Artane®) • COMT Inhibitors – Entacapone (Comtan®) – Tolcapone (Tasmar®)
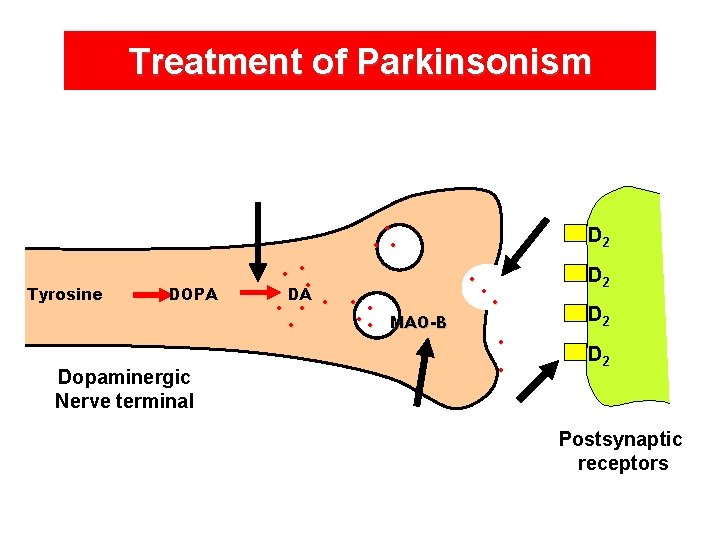
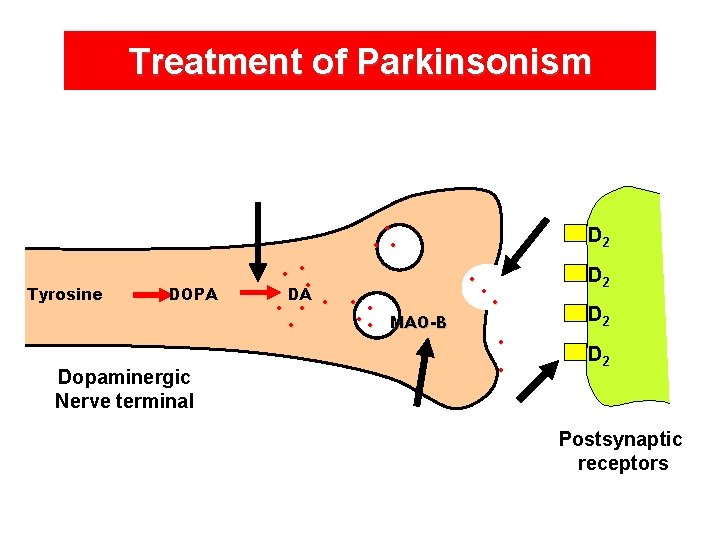
Treatment of Parkinsonism • • • Tyrosine DOPA Dopaminergic Nerve terminal • • • DA • • • MAO-B • • • D 2 Postsynaptic receptors
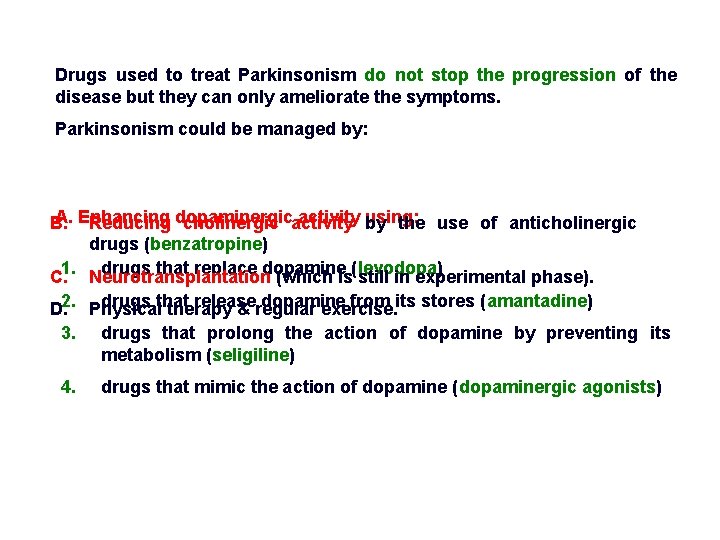
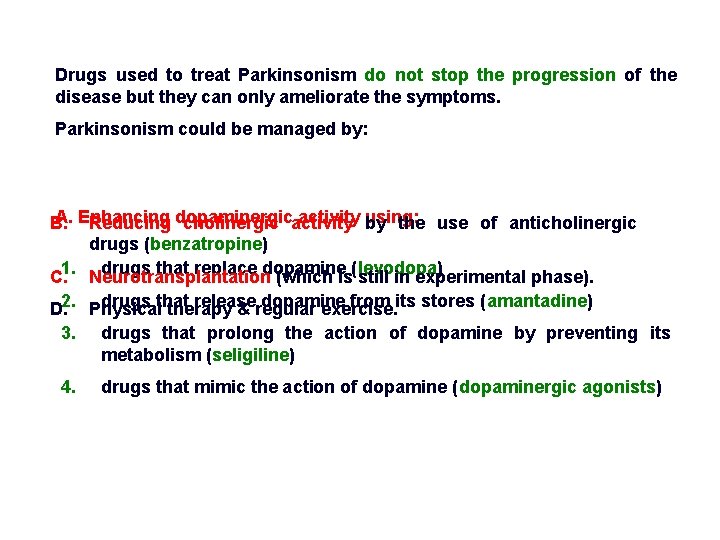
Drugs used to treat Parkinsonism do not stop the progression of the disease but they can only ameliorate the symptoms. Parkinsonism could be managed by: A. Enhancing activity using: B. Reducing dopaminergic cholinergic activity by the use of anticholinergic drugs (benzatropine) drugs that replace dopamine C. 1. Neurotransplantation (which is(levodopa) still in experimental phase). drugs that release dopamine from its stores (amantadine) D. 2. Physical therapy & regular exercise. 3. drugs that prolong the action of dopamine by preventing its metabolism (seligiline) 4. drugs that mimic the action of dopamine (dopaminergic agonists)
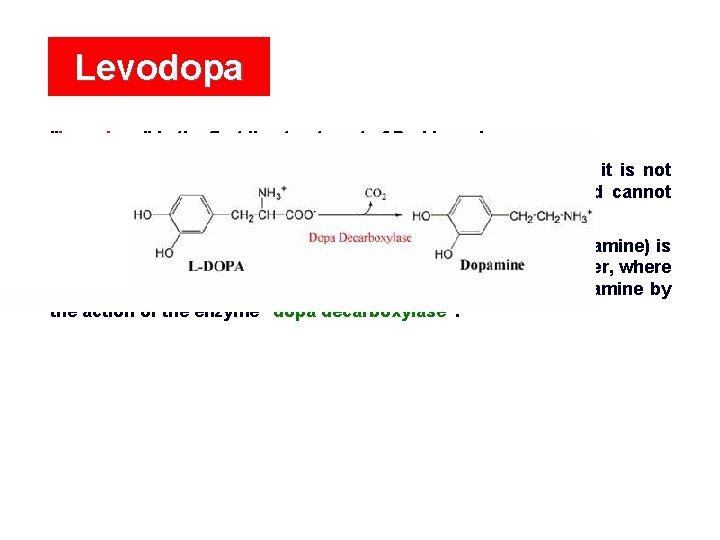
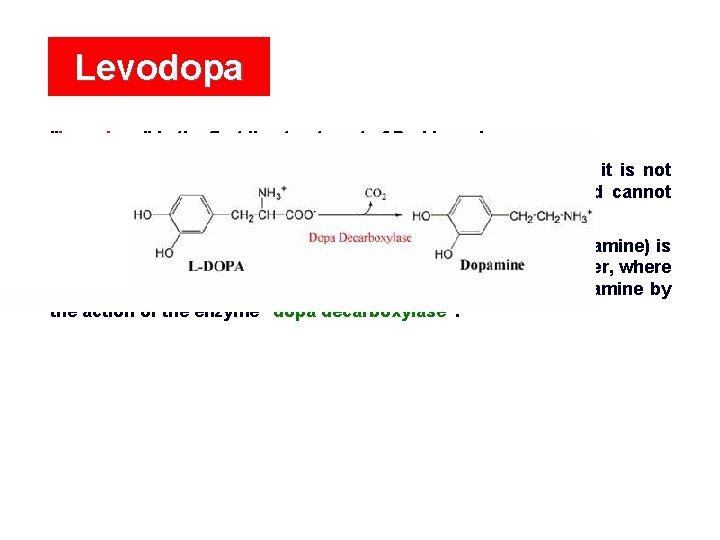
Levodopa "Levodopa" is the first line treatment of Parkinsonism. Dopamine itself has no therapeutic effect in Parkinsonism as it is not lipid soluble and therefore is not absorbed from the GIT and cannot cross the blood brain barrier. However, "levodopa" (which is the immediate precursor of dopamine) is well absorbed from the GIT and can cross the blood brain barrier, where it is taken up by dopaminergic neurons and converted to dopamine by the action of the enzyme "dopa decarboxylase".
In patients with early Parkinsonism, the number of residual dopaminergic neurons in the substantia nigra (about 20% of normal) is still enough to convert levodopa to dopamine. However, when the disease progresses, a fewer number of neurons are capable to take up levodopa and convert it to dopamine resulting in a “declined effectiveness” of levodopa. This indicates that the effect of levodopa depends on the presence of "functional dopaminergic neurons".
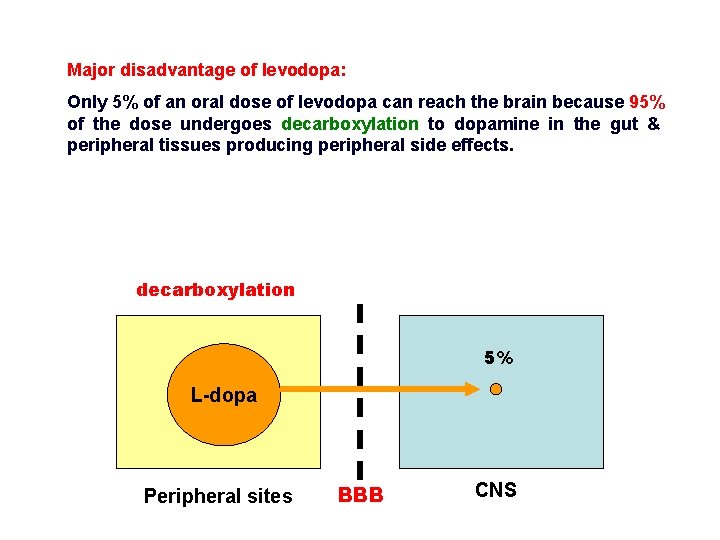
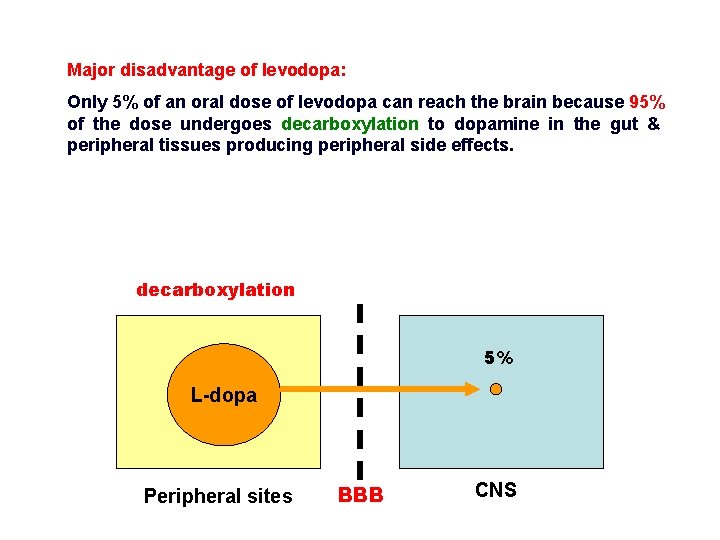
Major disadvantage of levodopa: Only 5% of an oral dose of levodopa can reach the brain because 95% of the dose undergoes decarboxylation to dopamine in the gut & peripheral tissues producing peripheral side effects. decarboxylation 5% L-dopa Peripheral sites BBB CNS
This problem was solved by the concomitant administration of levodopa with an inhibitor of dopa decarboxylase that does not cross the BBB (peripheral dopa decarboxylase inhibitor). Example of peripheral dopa decarboxylase inhibitors: carbidopa or benzerazide. Carbidopa or benzerazide inhibit the peripheral decarboxylation of levodopa allowing it to reach its desired site of action (i. e. the nigrostriatal system) in a greater proportion.
SINEMET (CARBIDOPA-LEVODOPA) DESCRIPTION SINEMET* (Carbidopa-Levodopa) is a combination of carbidopa and levodopa for the treatment of Parkinson's disease and syndrome.
Combing levodopa with the peripheral dopa decarboxylase inhibitors "carbidopa" or "benzerazide" has the following advantages: 3. 1. 2. If. The levodopa dose of is levodopa administered can be alone reduced (i. e. bywithout about 75%. carbidopa), it can interact with pyridoxine (vitamin B 6) in multivitamin preparations The peripheral side effects of levodopa are greatly reduced. which enhances its peripheral metabolism (dopa decarboxylase is a pyridoxine-dependent enzyme). On the other hand, if levodopa is combined with carbidopa, pyridoxine cannot reduce therapeutic effectiveness of levodopa since the peripheral decarboxylation of levodopa is already inhibited with carbidopa.
Pharmacological actions of levodopa: • Levodopa restores "dopamine" content in the basal ganglia. • Dopamine then acts on dopaminergic D 2 receptors in the nigrostriatal pathway to ameliorate the symptoms of Parkinsonism and improve the overall functional ability of Parkinsonian patients. • Dopamine can also act on the limbic system, tuberohypophyseal system and CTZ producing side effects.
Side effects of levodopa: On-Off" effect: 4. 1. "Tachycardia 2. "Dyskinesia" resulting and induction from dopamine of abnormal action voluntary on themovements. heart. This effect results from fluctuations of the level of levodopa in the 3. plasma 5. Psychological "Nausea & vomiting" levodopa to t½ stimulation mayhours). lead of to dopamine an over receptors activity of because ofeffects: its verydue short (1 -2 dopamine in the chemoreceptor in the limbic trigger system zone leading (CTZ) to "schizophrenia-like in the medulla Thesyndrome". "off" effect can be very sudden so that patients stop while walking oblongata. or are unable to rise from a chair in which they have sat down a few moments earlier. 6. normally This Endocrine effect iseffects: counteracted inhibition by the ofco-administration prolactin secretion of "food" due toand the peripheral of is DAcounteracted (but on thenot tuberohypophyseal central) system. ofantagonists (e. g. an Thiseffect by thedopaminergic combination levodopa with domperidone) levodopa. inhibitor of COMTwith (e. g. entacapone) to inhibit the degradation of dopamine.
Drug interactions of levodopa: 1. 3. "Pyridoxine" (vitamin ) increases peripheral break downand of "Antipsychotic drugs"B 6 block centralthe dopaminergic receptors levodopa andparkinsonism-like reduces its effectiveness. can induce syndrome themselves. 2. Concomitant administration of levodopa with "MAO inhibitors" leads Therefore they are contraindicated during Parkinsonism or levodopa totherapy hypertensive crisis due to increased catecholamines since they can reverse the benefits of levodopa. (dopamine is a substrate for MAO and is also converted to noradrenaline).
Dopamine Agonists • • • Pramipexole (Mirapex®) Ropinirole (Requip®) Rotigitine (Neupro™) Apomorphine (Apokyn®) (cabergoline, lisuride)
Dopamine Agonists • May be used as initial therapy for patients with mild disease or as “add on” therapy for patients with more severe disease • May delay need for levodopa therapy in early patients • Later stage patients may be able to decrease levodopa dosing if DA added • Neuroprotective effect?
Dopamine Agonists • Directly stimulate dopamine receptors • No metabolic conversion required • Longer half-life than levodopa (exception: apomorphine) • May delay onset of dykinesias or motor fluctuations
Dopamine agonists • Advantages over levodopa: no need for biotransformation; no competition with other substances across intestine • Absorption rate decreased in when patient has full stomach • Side effects: hallucinations, peripheral edema, somnolence, compulsive behavior • Ergot alkaloid DA no longer used
Apomorphine • Structurally similar to dopamine • First synthesized in 1869 from acidic treatment of morphine (but retains no opiate properties) • Requires parenteral delivery
Apomorphine • Indications – Acute, intermittent treatment of hypomobility, off episodes (“end-of-dose wearing off” and unpredictable “on/off” episodes) associated with advanced PD – As an adjunct to other medications • Contraindicated – In patients who have demonstrated hypersensitivity to the drug or its ingredients, such as its preservative metabisulfite
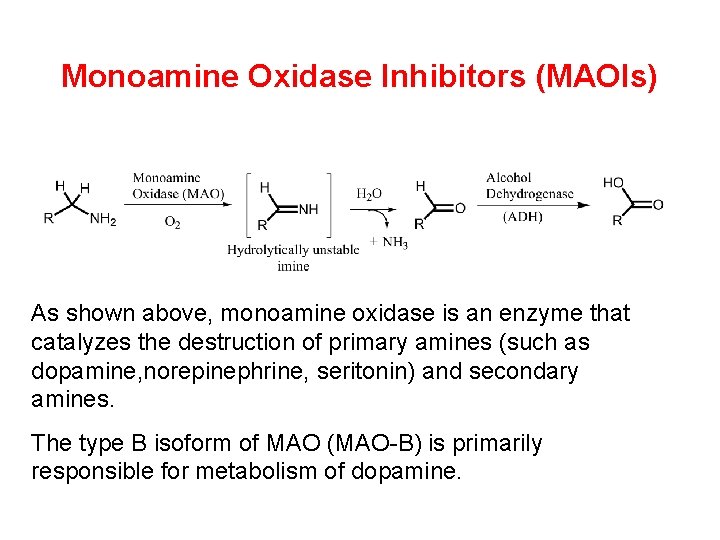
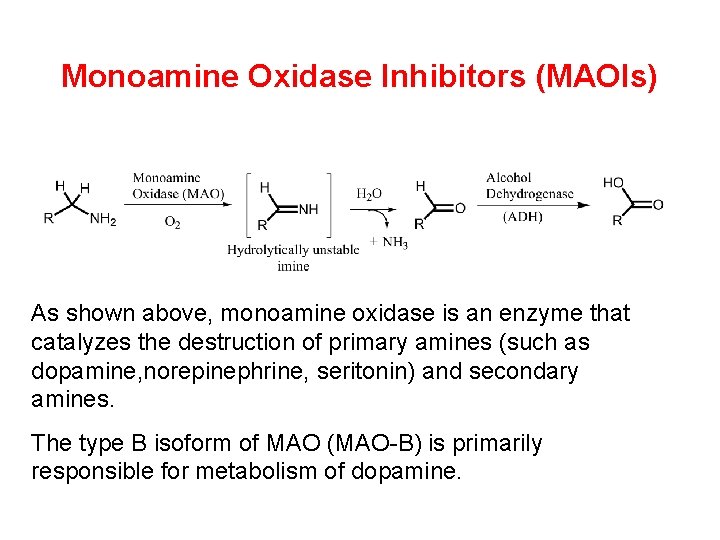
Monoamine Oxidase Inhibitors (MAOIs) As shown above, monoamine oxidase is an enzyme that catalyzes the destruction of primary amines (such as dopamine, norepinephrine, seritonin) and secondary amines. The type B isoform of MAO (MAO-B) is primarily responsible for metabolism of dopamine.
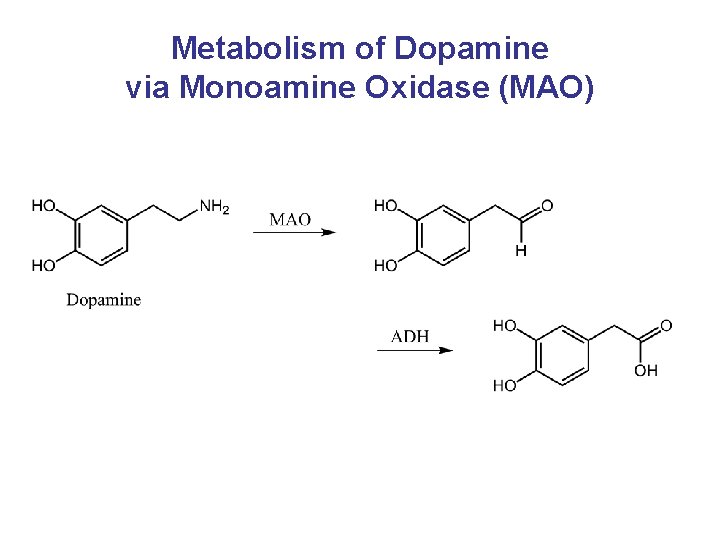
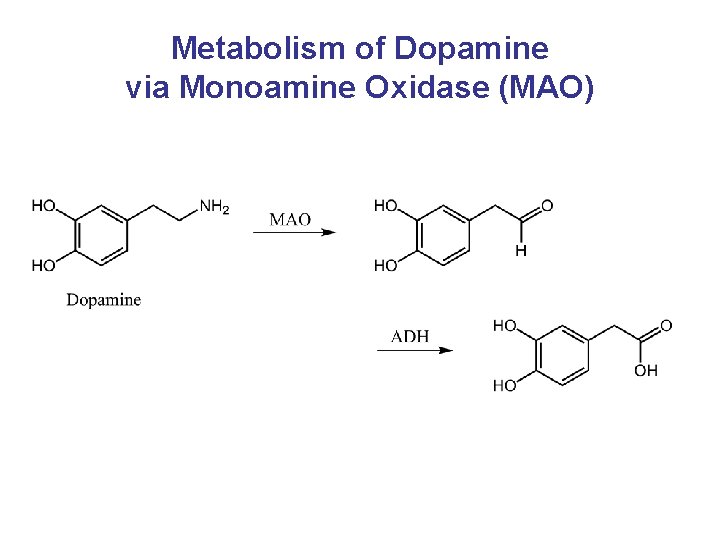
Metabolism of Dopamine via Monoamine Oxidase (MAO)
MAO Inhibitors - General • MAO-B breaks down dopamine within the CNS • Inhibition of MAO-B increases dopamine levels and function • Because of increase in dopamine activity within CNS, potential for increased dopamine side effects
Inhibitor of MAO-B • Selegiline (l-deprenyl, Eldepryl® or Anipryl® veterinary) is a drug used for the treatment of early-stage Parkinson's disease and senile dementia. • In normal clinical doses it is a selective irreversible MAO-B inhibitor.
• In late stage Parkinson’s Disease, Selegiline is usually added to levodopa to prolong and enhance its effect
MAO Inhibitors • Selegeline – At low doses, remains selective for MAO-B – At doses >10 mg, becomes non-selective – Active amphetamine-like metabolite
MAO Inhibitors • Rasagaline – Precise mechanism of action is unknown – thought to contribute to increased dopamine levels within CNS due to inhibition of MAO – Althought to be MAO-B selective, packaged with non-selective dietary and drug restrictions
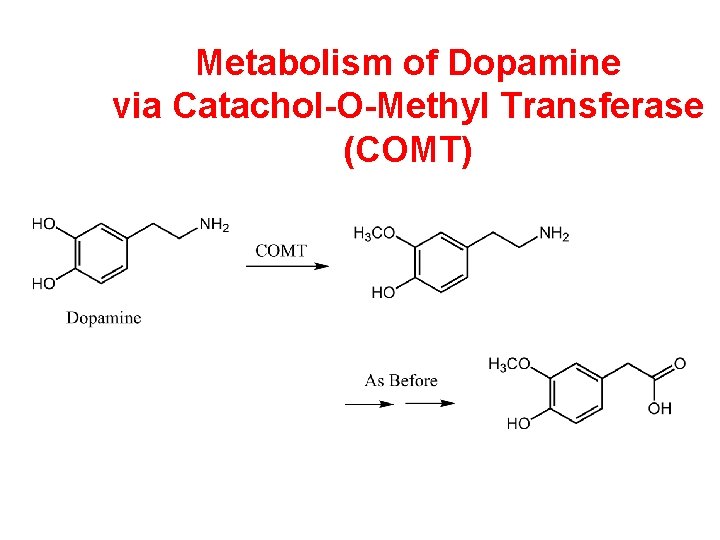
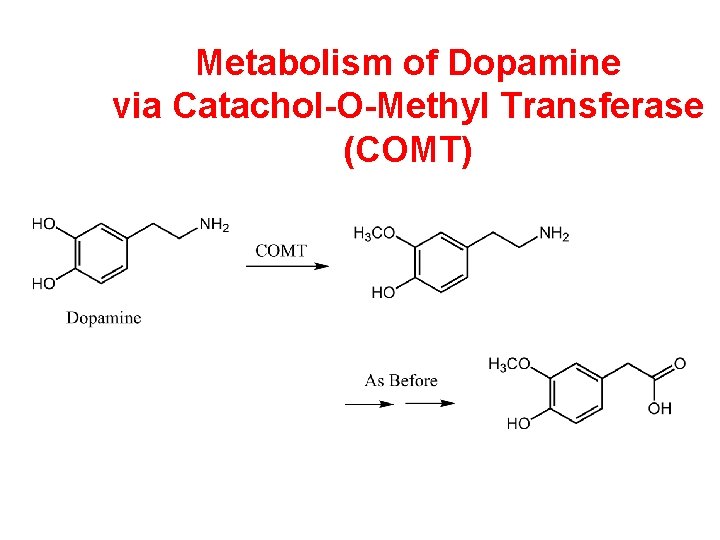
Metabolism of Dopamine via Catachol-O-Methyl Transferase (COMT)
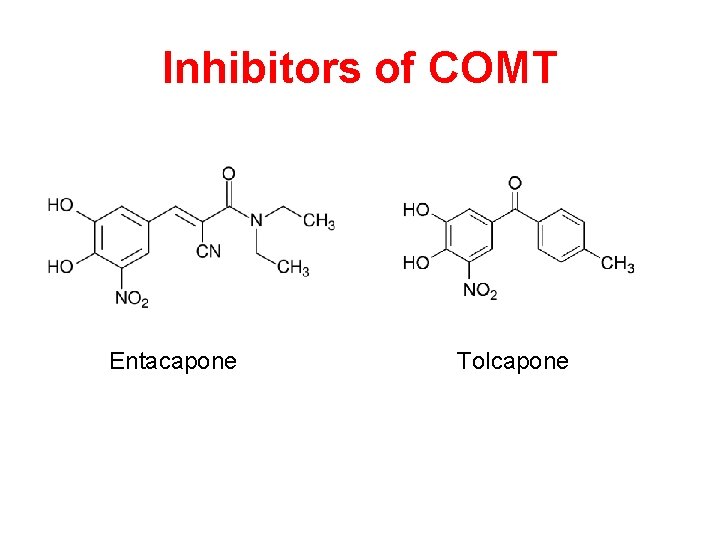
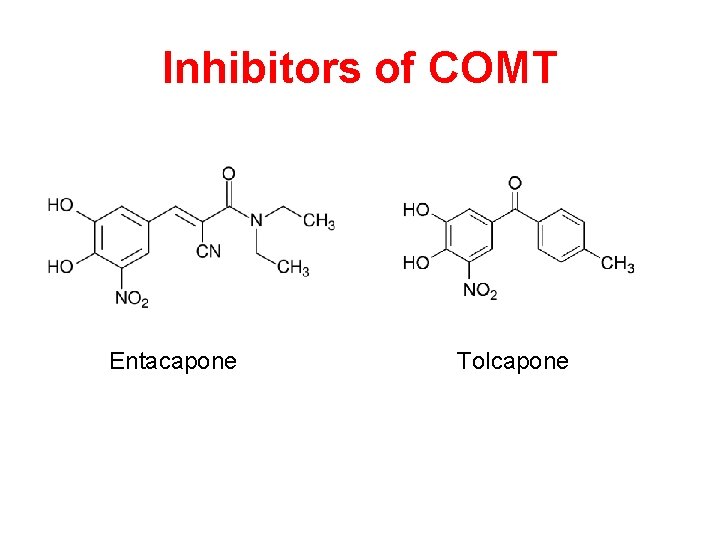
Inhibitors of COMT Entacapone Tolcapone
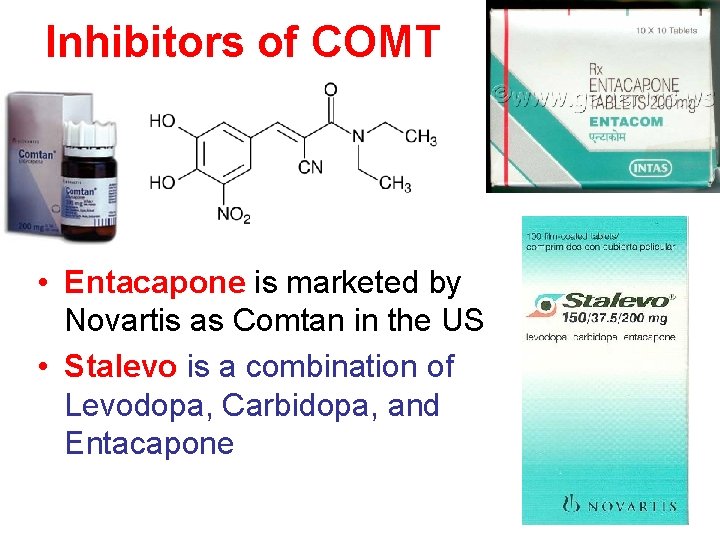
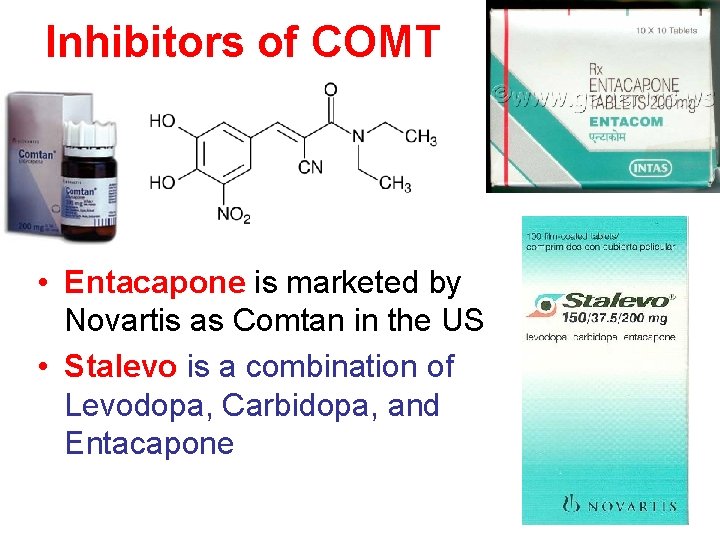
Inhibitors of COMT • Entacapone is marketed by Novartis as Comtan in the US • Stalevo is a combination of Levodopa, Carbidopa, and Entacapone
COMT Inhibitors • In presence of a decarboxylase inhibitor (carbidopa), COMT is major metabolizing enzyme of levodopa • Effect of medication thought to be due to increased/sustained plasma levels of levodopa • Entacapone and Tolcapone
COMT Inhibitors • General precautions: should not be given with non-selective MAO inhibitors • May decrease metabolism of epinephrine, isoproterenol, norepinephrine, dobutamine, alpha-methyldopa • Will potentiate side effects of levodopa • Tolcapone: Black box warning; liver monitoring required
Amantadine • Antiviral agent; anti-PD effect found accidentally • Effective for tremor, rigidity and dyskinesias • Actual mechanism of action poorly understood: – perhaps facilitates release of dopamine from striatal neurons, inhibits presynaptic reuptake of catacholamines, or creates an NMDA receptor blockade. Does have weak DA properties • Decreases glutamatergic output from STN (may account for anti-dyskinetic effect)
Amantadine • T 1/2 is 2 -4 hours • Medication is excreted mostly unchanged in the urine • Side effects may include hypotension, hallucinations, sedation, dry mouth • Rare side effect unique to amantadine is livido reticularis – patchy discoloration of the skin (although unsightly, harmless to patient; resolves with discontinuation of med)

Livido reticularis
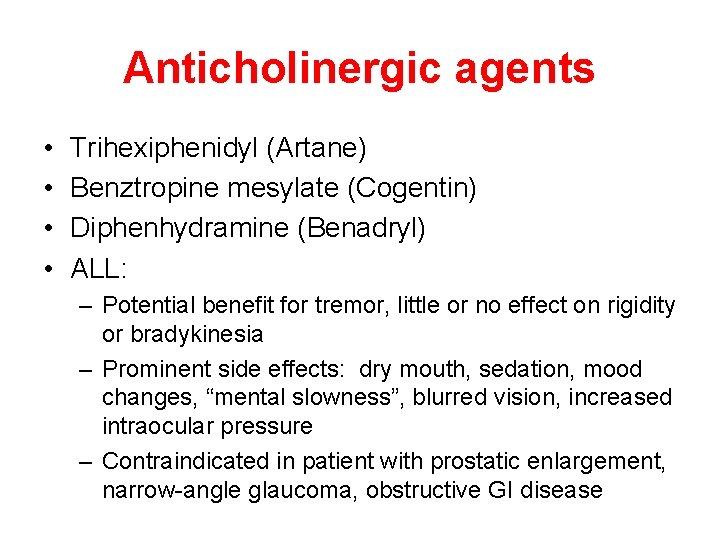
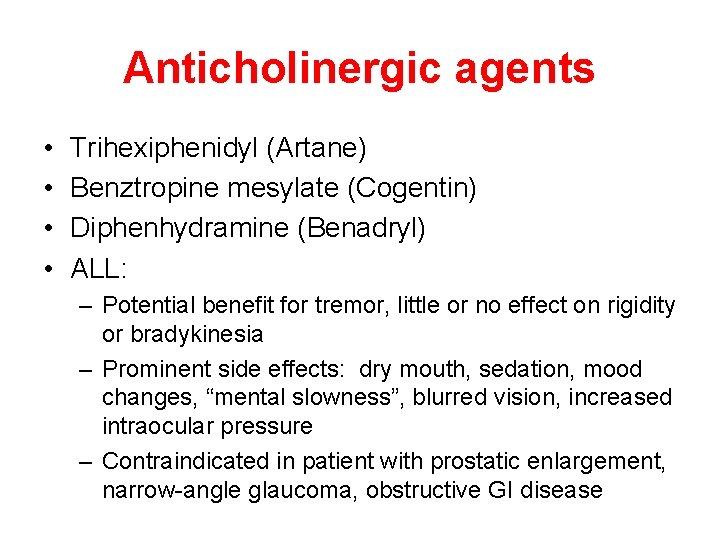
Anticholinergic agents • • Trihexiphenidyl (Artane) Benztropine mesylate (Cogentin) Diphenhydramine (Benadryl) ALL: – Potential benefit for tremor, little or no effect on rigidity or bradykinesia – Prominent side effects: dry mouth, sedation, mood changes, “mental slowness”, blurred vision, increased intraocular pressure – Contraindicated in patient with prostatic enlargement, narrow-angle glaucoma, obstructive GI disease
Anticholinergic drugs are less effective than levodopa and can diminish mainly the tremors and to a lesser extent the rigidity and bradykinesia. Therefore, they are used as supplemental treatment with levodopa. Anticholinergic drugs are used "instead of levodopa" in: 2. 3. 1. Parkinsonianpatientswho receiving cannotcentral benefit tolerate from dopaminergic levodopa because antagonists because of of its non-functional side (antipsychotic effects or contraindications. dopaminergic drugs) which can neurons. nullify the effect of levodopa.
Side effects of anticholinergic drugs: • Dry mouth • Blurred vision • Constipation • Urine retention • Glaucoma
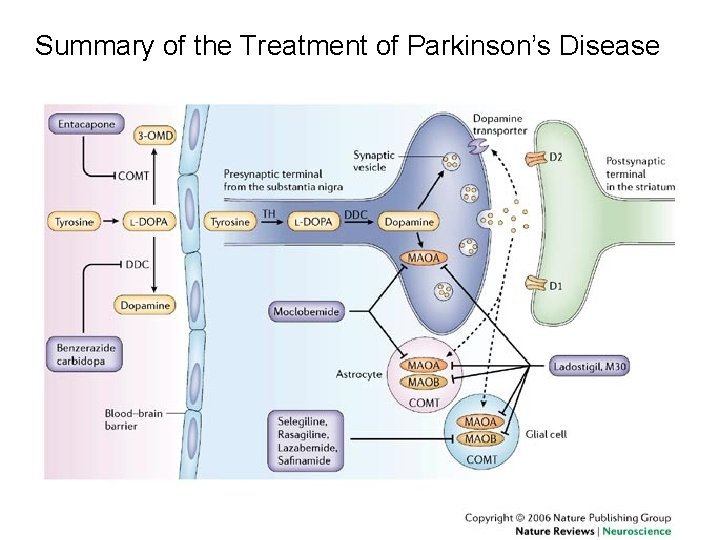
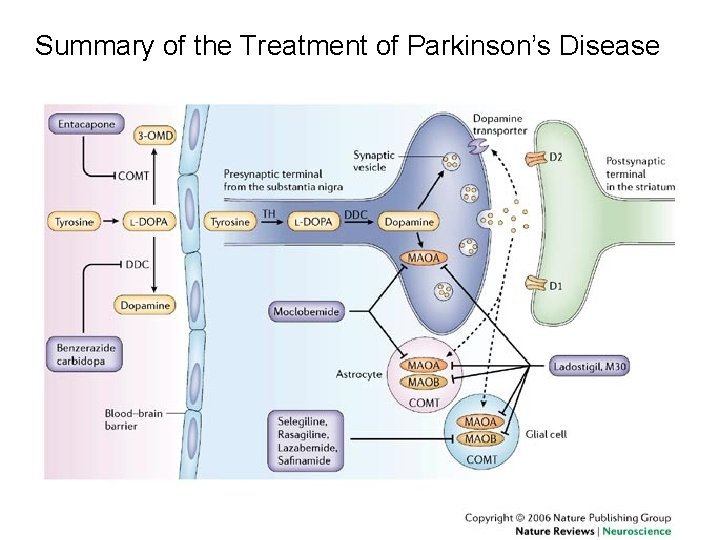
Summary of the Treatment of Parkinson’s Disease
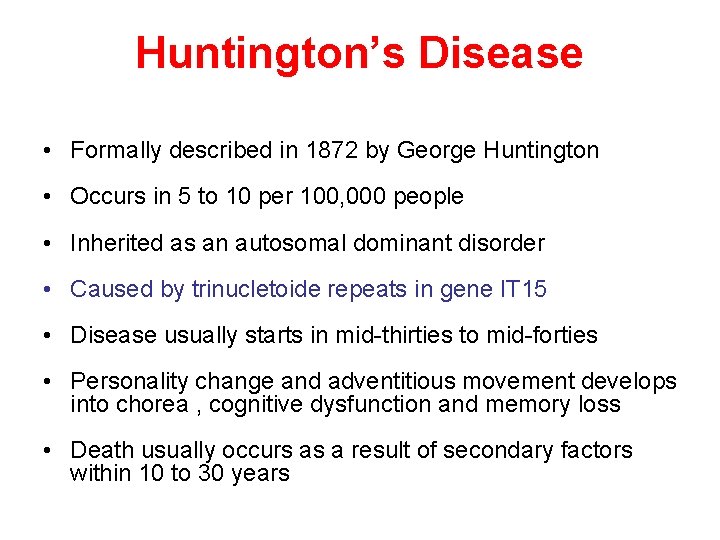
Huntington’s Disease • Formally described in 1872 by George Huntington • Occurs in 5 to 10 per 100, 000 people • Inherited as an autosomal dominant disorder • Caused by trinucletoide repeats in gene IT 15 • Disease usually starts in mid-thirties to mid-forties • Personality change and adventitious movement develops into chorea , cognitive dysfunction and memory loss • Death usually occurs as a result of secondary factors within 10 to 30 years
 Parkinsonism
Parkinsonism Parkinsons disease hereditory
Parkinsons disease hereditory Tasha big feet
Tasha big feet Amantadin
Amantadin Behcet wiki
Behcet wiki Parkinsons plus
Parkinsons plus Rectosigmoid junction
Rectosigmoid junction Disease modifying antirheumatic drugs
Disease modifying antirheumatic drugs Emergency drugs used in delivery room
Emergency drugs used in delivery room Drugs used in pregnancy
Drugs used in pregnancy Communicable disease and non communicable disease
Communicable disease and non communicable disease In a premix burner used in fes the fuel used is
In a premix burner used in fes the fuel used is In a premix burner used in fes the fuel used is
In a premix burner used in fes the fuel used is Antidiabetic drugs classification
Antidiabetic drugs classification Belladonna alkaloids drugs
Belladonna alkaloids drugs Pharmacy gta 5
Pharmacy gta 5 Atropine mechanism of action
Atropine mechanism of action Drugs that alter moods thoughts and sense perceptions
Drugs that alter moods thoughts and sense perceptions Chapter 19 vocabulary glencoe health
Chapter 19 vocabulary glencoe health Intraperitoneal route advantages and disadvantages
Intraperitoneal route advantages and disadvantages Complete floor stock system
Complete floor stock system Reconstitution of powdered drugs
Reconstitution of powdered drugs Sar of sympathomimetic agents
Sar of sympathomimetic agents 9 rational use of drugs
9 rational use of drugs Narrow therapeutic index drugs
Narrow therapeutic index drugs Psychoactive drugs chart
Psychoactive drugs chart Na k atpase pump
Na k atpase pump Mechanism of action of thrombolytic agents
Mechanism of action of thrombolytic agents First pass hepatic metabolism
First pass hepatic metabolism Costco pharmacy huntington
Costco pharmacy huntington Anticholinergic drugs mechanism of action
Anticholinergic drugs mechanism of action Section 35-1 human body systems answer key
Section 35-1 human body systems answer key Daffodil lower classifications
Daffodil lower classifications Ion pair transport of drugs
Ion pair transport of drugs Antianginal drugs
Antianginal drugs Anthelmintic drugs
Anthelmintic drugs Chapter 7 alcohol other drugs and driving
Chapter 7 alcohol other drugs and driving Antipsychotic drugs classification
Antipsychotic drugs classification Glucouronide
Glucouronide Module 25 psychoactive drugs
Module 25 psychoactive drugs Mechanism of action of parasympathomimetic drugs
Mechanism of action of parasympathomimetic drugs Thyroid hormone synthesis mnemonic
Thyroid hormone synthesis mnemonic Hypertension drugs
Hypertension drugs Etanecept
Etanecept Reconstitution of powdered drugs
Reconstitution of powdered drugs Digitalis use
Digitalis use