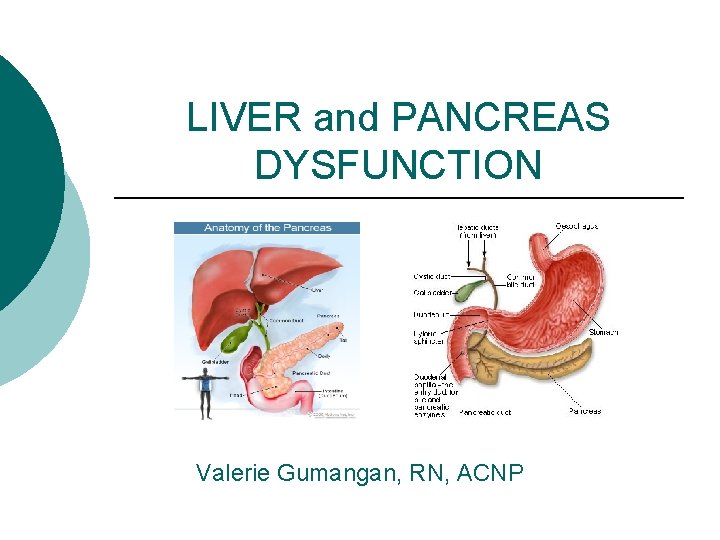
LIVER and PANCREAS DYSFUNCTION Valerie Gumangan RN ACNP
- Slides: 74
LIVER and PANCREAS DYSFUNCTION Valerie Gumangan, RN, ACNP
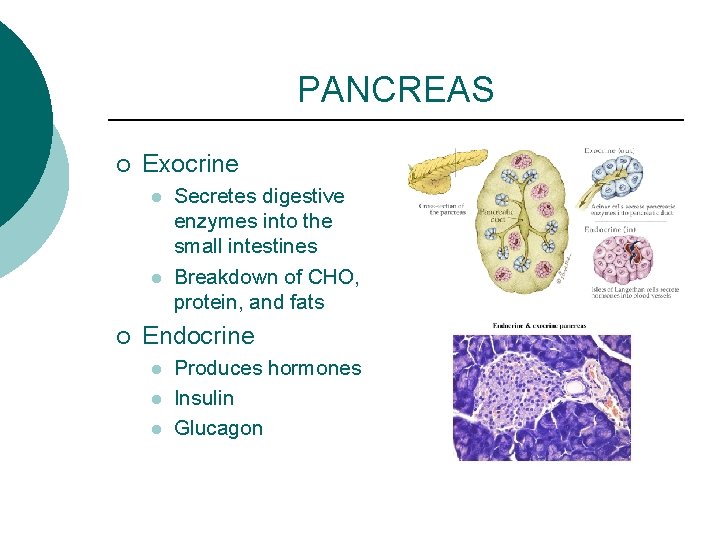
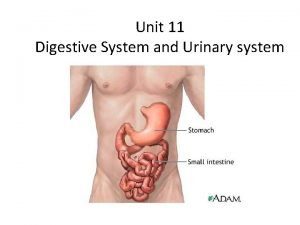
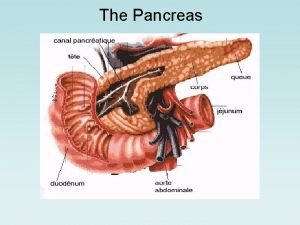
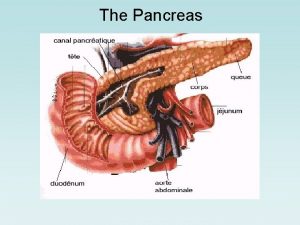
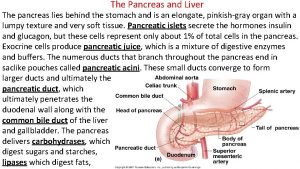
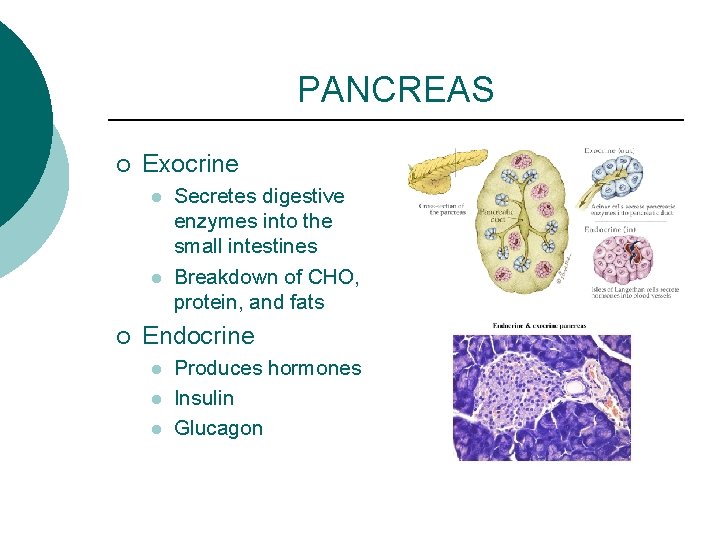
PANCREAS ¡ Exocrine l l ¡ Secretes digestive enzymes into the small intestines Breakdown of CHO, protein, and fats Endocrine l l l Produces hormones Insulin Glucagon
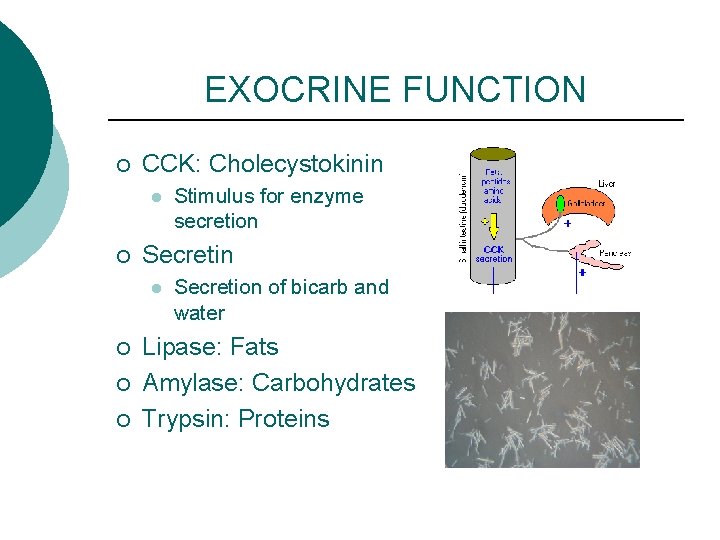
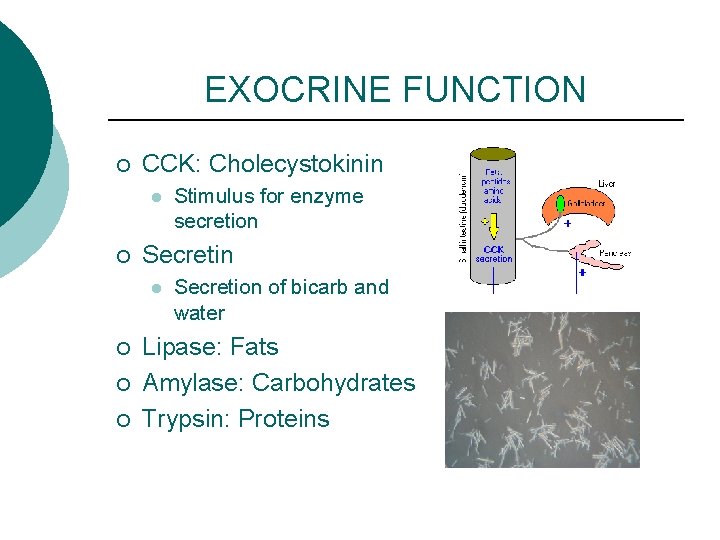
EXOCRINE FUNCTION ¡ CCK: Cholecystokinin l ¡ Secretin l ¡ ¡ ¡ Stimulus for enzyme secretion Secretion of bicarb and water Lipase: Fats Amylase: Carbohydrates Trypsin: Proteins
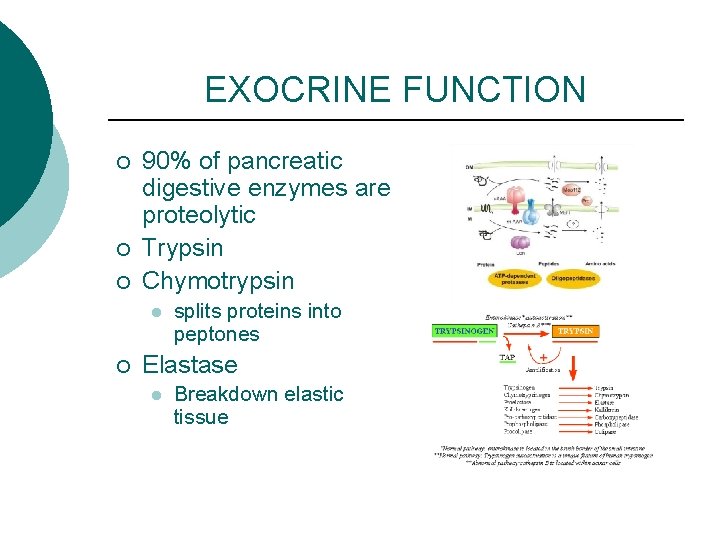
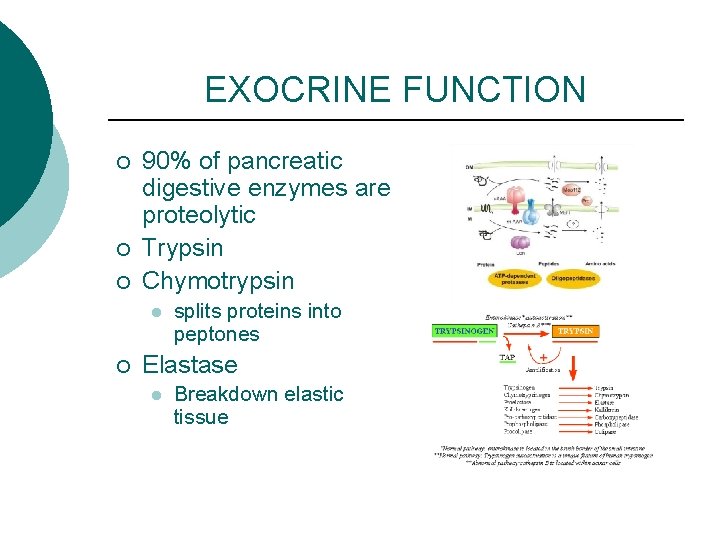
EXOCRINE FUNCTION ¡ ¡ ¡ 90% of pancreatic digestive enzymes are proteolytic Trypsin Chymotrypsin l ¡ splits proteins into peptones Elastase l Breakdown elastic tissue
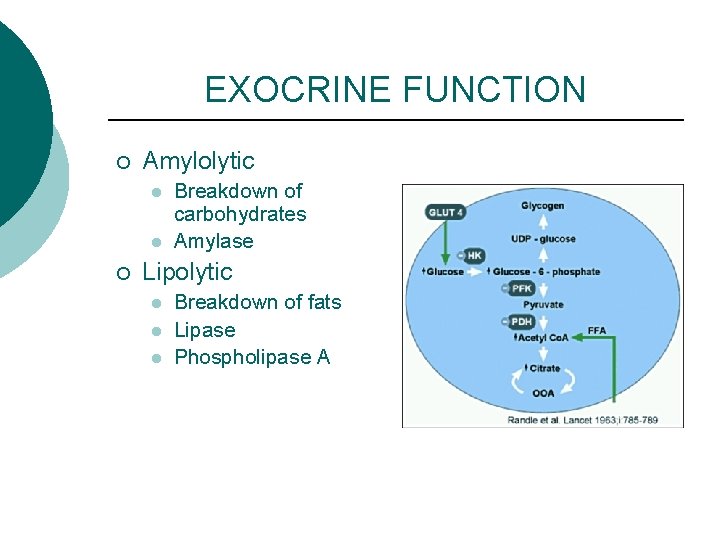
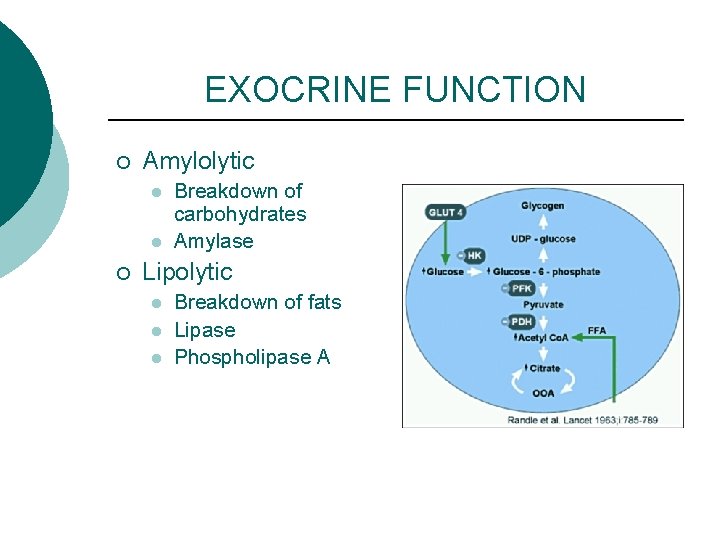
EXOCRINE FUNCTION ¡ Amylolytic l l ¡ Breakdown of carbohydrates Amylase Lipolytic l l l Breakdown of fats Lipase Phospholipase A
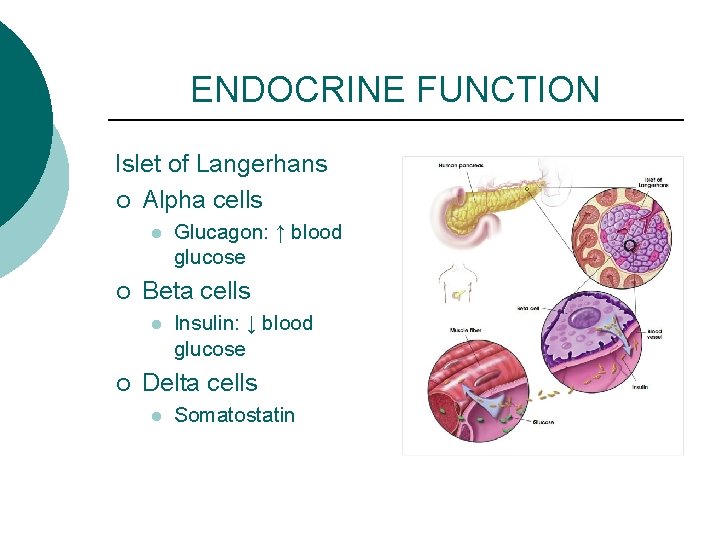
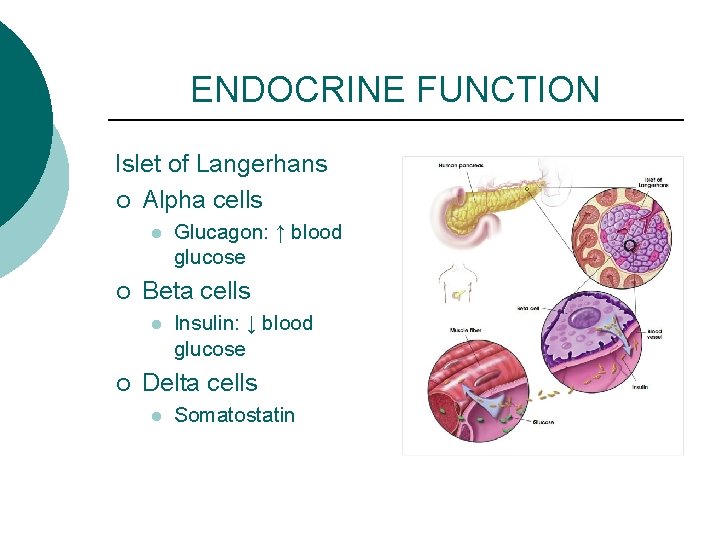
ENDOCRINE FUNCTION Islet of Langerhans ¡ Alpha cells l ¡ Beta cells l ¡ Glucagon: ↑ blood glucose Insulin: ↓ blood glucose Delta cells l Somatostatin
PANCREATITIS ¡ ¡ ¡ Inflammation of the pancreas Autodigestion of the pancreas by pancreatic enzymes Cellular destruction and organ damage
ACUTE PANCREATITS ¡ Acute l l l Mild or Nonhemorrhagic Severe or Hemorrhagic Fulminant
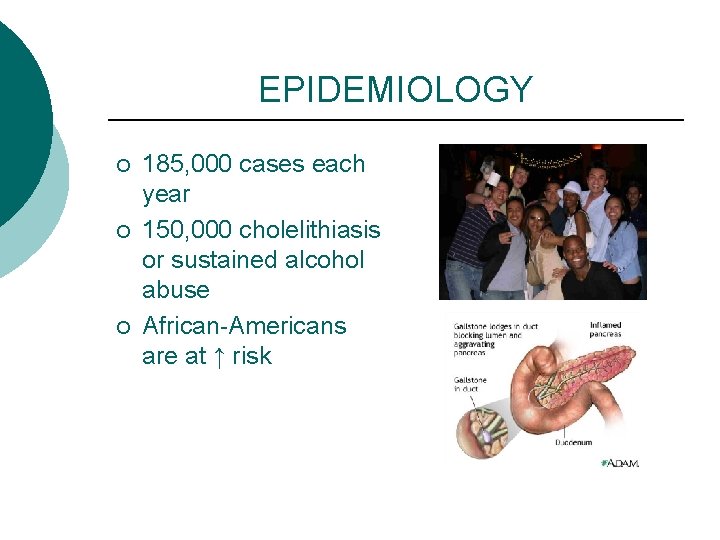
EPIDEMIOLOGY ¡ ¡ ¡ 185, 000 cases each year 150, 000 cholelithiasis or sustained alcohol abuse African-Americans are at ↑ risk
CAUSES ¡ ¡ ¡ ¡ Alcohol consumption Gallstones Pancreatic obstruction Drugs and toxins Hyperlipidemia Family history Trauma and iatrogenic factors
SIGNS and SYMPTOMS ¡ Severe abdominal pain l l ¡ ¡ ¡ Epigastrium radiating to midback Not relieved by vomiting Fever, malaise Nausea, vomiting Rigid and distended Rebound tenderness Absent or diminished bowel sounds
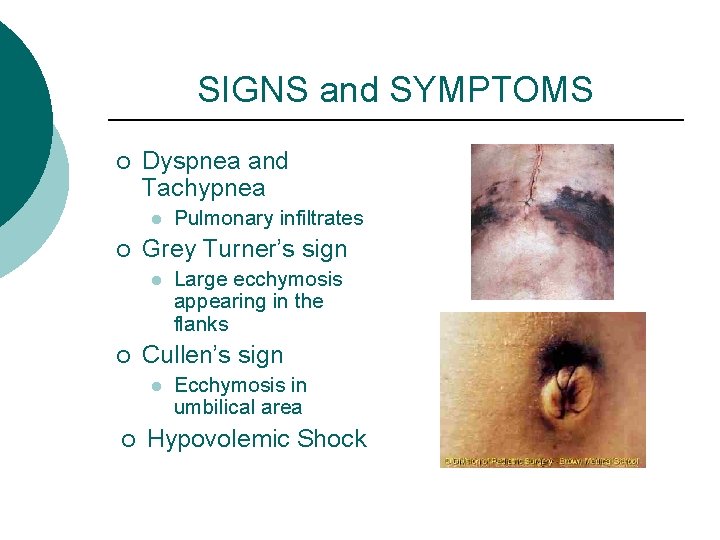
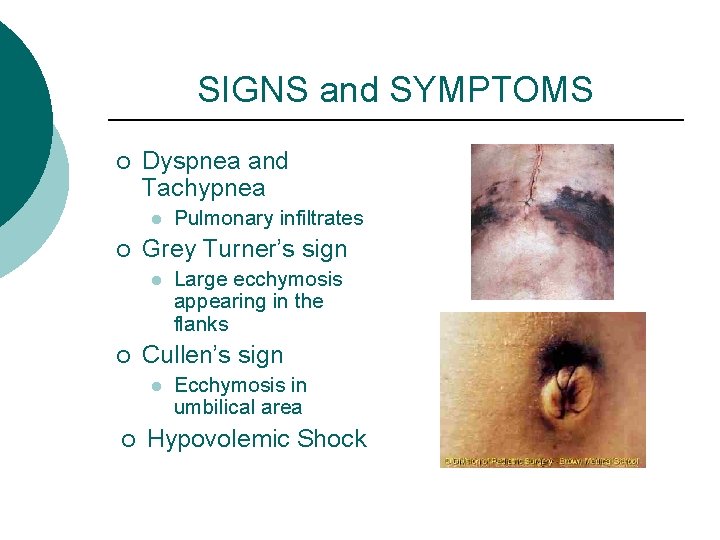
SIGNS and SYMPTOMS ¡ Dyspnea and Tachypnea l ¡ Grey Turner’s sign l ¡ Large ecchymosis appearing in the flanks Cullen’s sign l ¡ Pulmonary infiltrates Ecchymosis in umbilical area Hypovolemic Shock
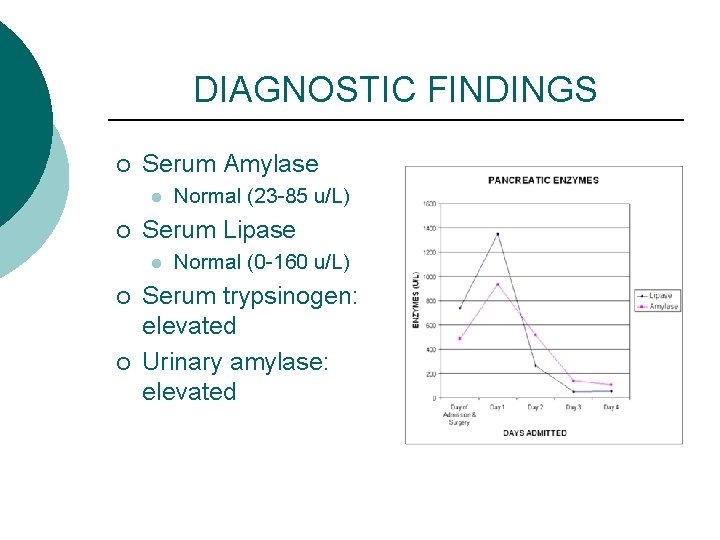
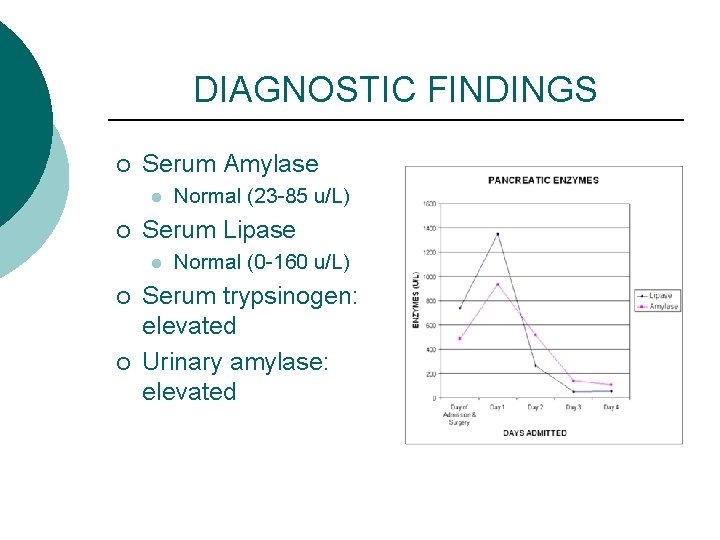
DIAGNOSTIC FINDINGS ¡ Serum Amylase l ¡ Serum Lipase l ¡ ¡ Normal (23 -85 u/L) Normal (0 -160 u/L) Serum trypsinogen: elevated Urinary amylase: elevated
DIAGNOSTIC FINDINGS ¡ ¡ Hematocrit: initially elevated then later decreased WBC: elevated C-reactive protein: elevated Liver function tests: elevated
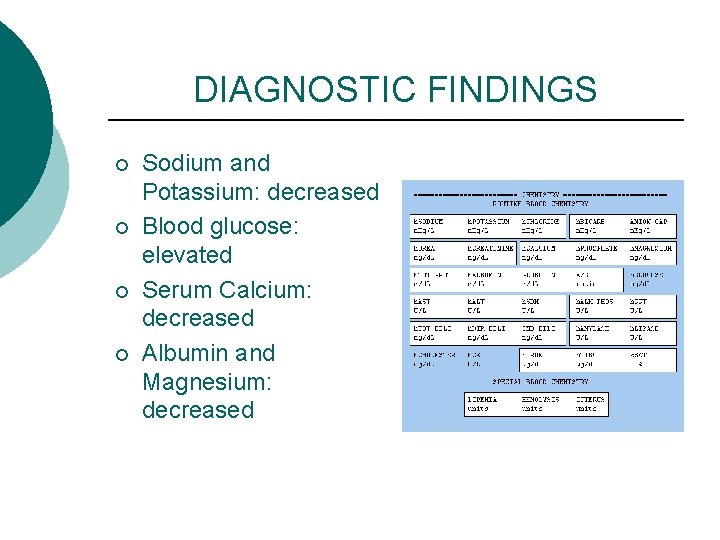
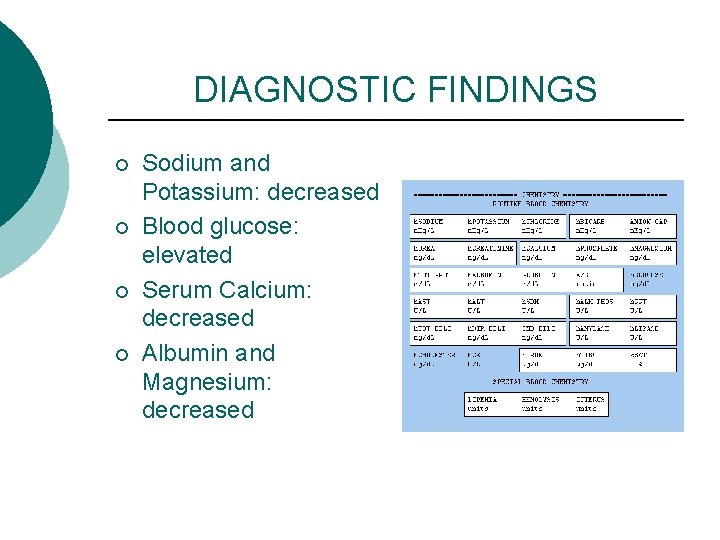
DIAGNOSTIC FINDINGS ¡ ¡ Sodium and Potassium: decreased Blood glucose: elevated Serum Calcium: decreased Albumin and Magnesium: decreased
DIAGNOSTIC FINDINGS ¡ ¡ ¡ Abdominal and Chest X-ray CT scan, Ultrasound, MRI Endoscopic Retrograde Cholangiopancreatography (ERCP) Aspiration biopsy Stool studies: steatorrhea
COMPLICATIONS ¡ Hypovolemic shock l l 3 rd spacing Hemorrhage Vomiting Decreased protein intake
COMPLICATIONS ¡ Pulmonary complications l l Atelectasis Acute lung injury Pleural effusion ARDS
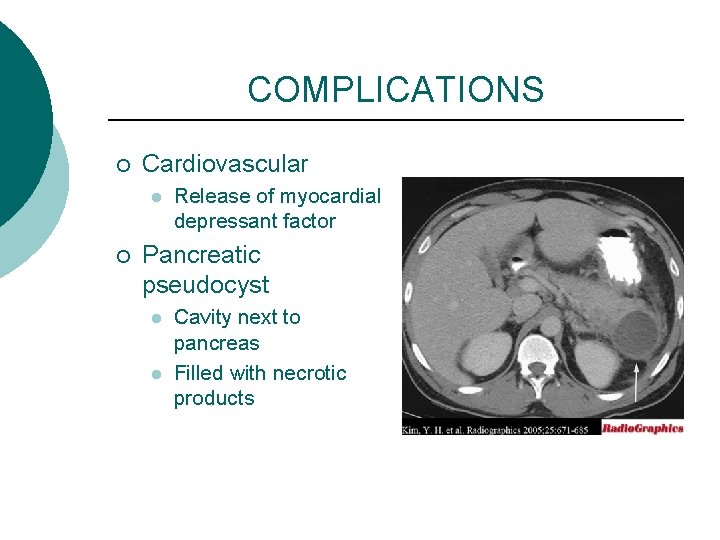
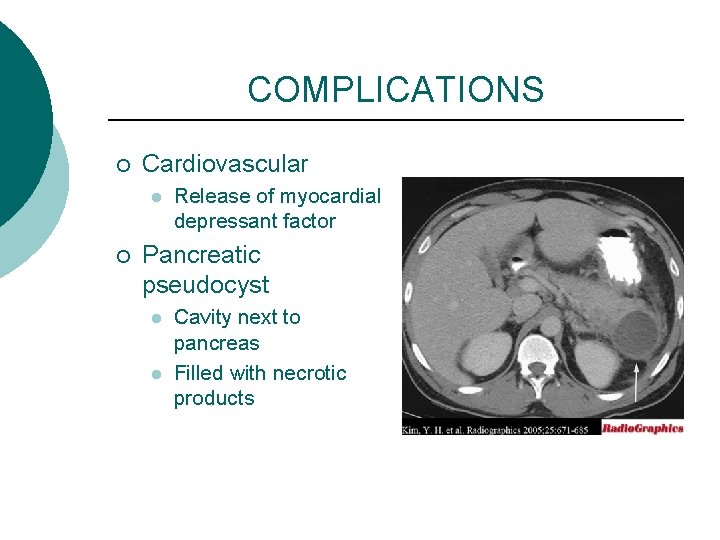
COMPLICATIONS ¡ Cardiovascular l ¡ Release of myocardial depressant factor Pancreatic pseudocyst l l Cavity next to pancreas Filled with necrotic products
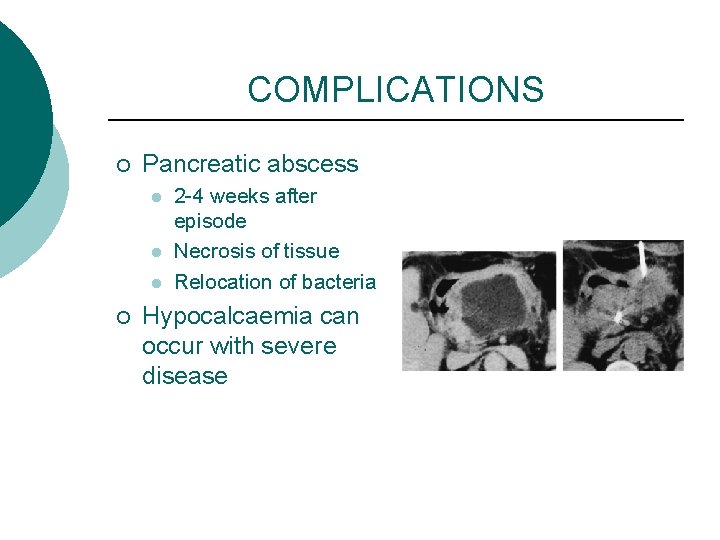
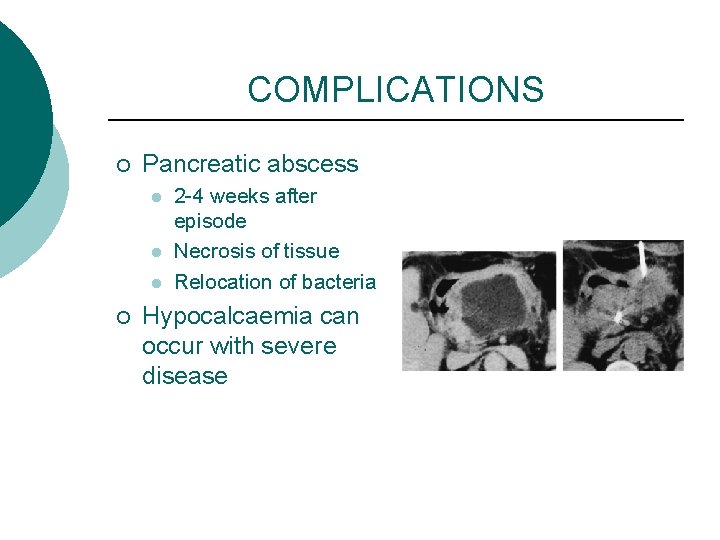
COMPLICATIONS ¡ Pancreatic abscess l l l ¡ 2 -4 weeks after episode Necrosis of tissue Relocation of bacteria Hypocalcaemia can occur with severe disease
COMPLICATIONS ¡ Fluid and electrolytes l l l Vomiting NG suction Redistribution of fluids
TREATMENT ¡ Pain Management l l l ¡ IV opioid analgesics Dilaudid IV PCA Demerol and Morphine IV GI rest l l Decrease stimulation of pancreas Nasogastric tube insertion
TREATMENT ¡ ¡ Fluid and Electrolyte replacement Cessation of alcohol consumption Nutrition: enteral versus parenteral Surgery if there is biliary obstruction
TREATMENT ¡ Respiratory l l Oxygen Monitor oxygen saturation Arterial blood gas Ventilator support
TREATMENT ¡ Fluid volume deficit l l l IV fluids Plasma expanders Vasopressors Blood replacement Strict intake and output
TREATMENT ¡ Fluid and electrolyte imbalance l l ¡ LR or IV maintenance fluid containing K+ Calcium gluconate Hypocalcemia l l Chvostek’s sign Trousseau’s sign
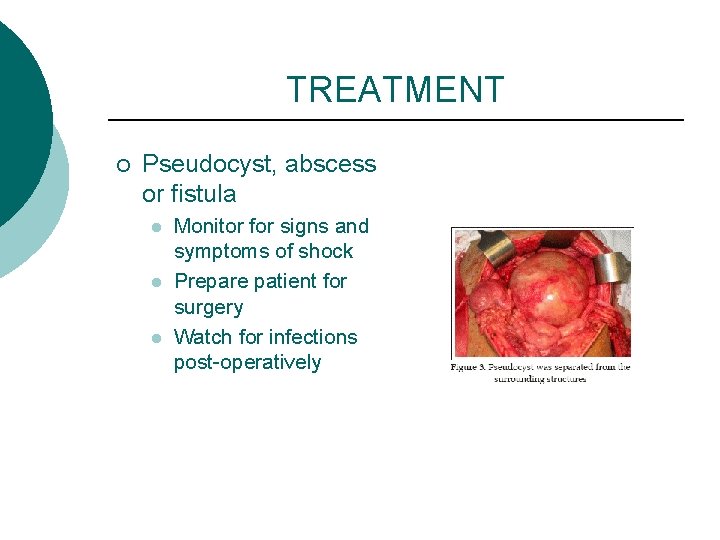
TREATMENT ¡ Pseudocyst, abscess or fistula l l l Monitor for signs and symptoms of shock Prepare patient for surgery Watch for infections post-operatively
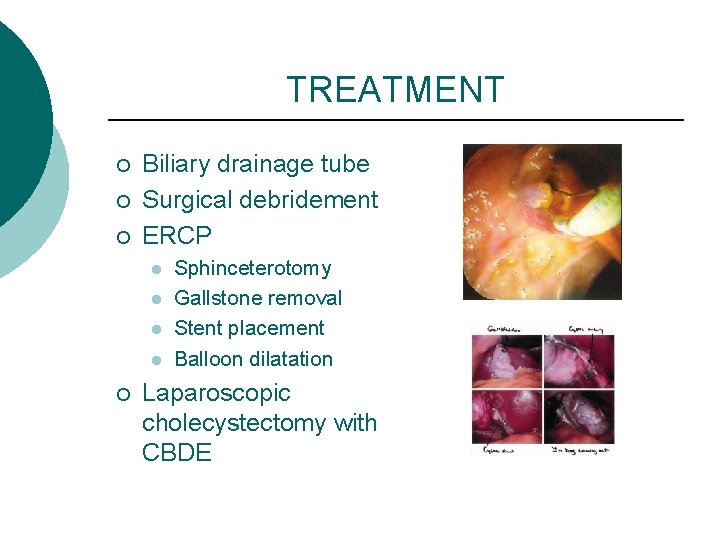
TREATMENT ¡ ¡ ¡ Biliary drainage tube Surgical debridement ERCP l l ¡ Sphinceterotomy Gallstone removal Stent placement Balloon dilatation Laparoscopic cholecystectomy with CBDE
MEDICATIONS ¡ Viokase l ¡ Pancrease l ¡ Replace pancreatic enzymes Glucagon l Treat hypoglycemia
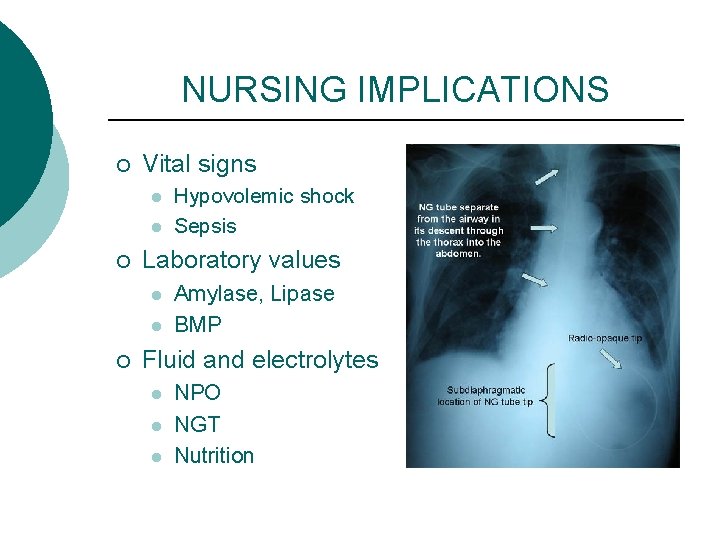
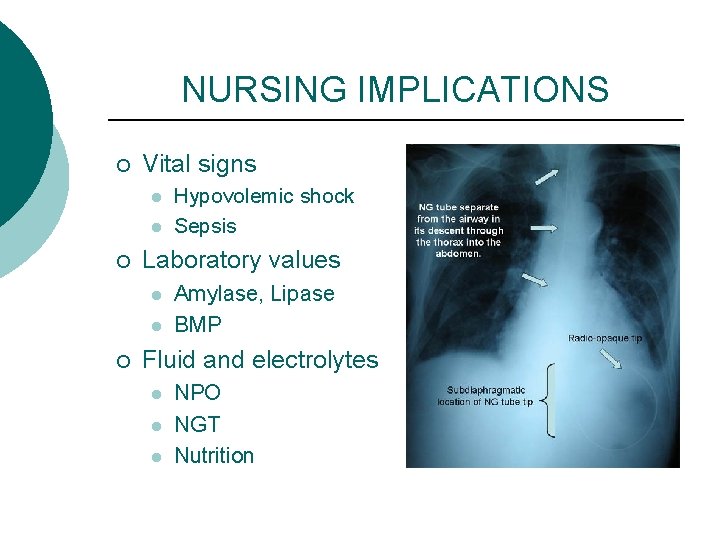
NURSING IMPLICATIONS ¡ Vital signs l l ¡ Laboratory values l l ¡ Hypovolemic shock Sepsis Amylase, Lipase BMP Fluid and electrolytes l l l NPO NGT Nutrition
NURSING IMPLICATIONS ¡ ¡ Administer pain medication Monitor blood glucose Monitor intake and output Daily weight
CHRONIC PANCREATITIS ¡ ¡ Persistent inflammation of the pancreas Scarring and calcification of the pancreatic ducts
CAUSES ¡ ¡ 70% is caused by alcohol abuse 20% is caused by obstruction, trauma, metabolic disturbances
SIGNS & SYMPTOMS ¡ 80% of pancreatic destruction causes l l l Malabsorption resulting in nutritional deficits Diarrhea and steatorrhea Impaired glucose regulation
DIAGNOSTIC FINDINGS ¡ ¡ ¡ LFT, CMP, CBC, ESR Stool studies Abdominal CT scan l ¡ Abdominal US l ¡ Images organ, detect inflammation Detect inflammation and calcifications ERCP l looks for stones
TREATMENT ¡ ¡ GI rest Pain control No Alcohol Daily weight
TREATMENT ¡ ¡ ¡ Low fat, protein, and high carbohydrate diet Oral pancreatic enzymes Monitor blood glucose
TREATMENT ¡ ¡ ¡ Replacement of fat soluble vitamins Octreotide (Sandostatin) Celiac plexus block
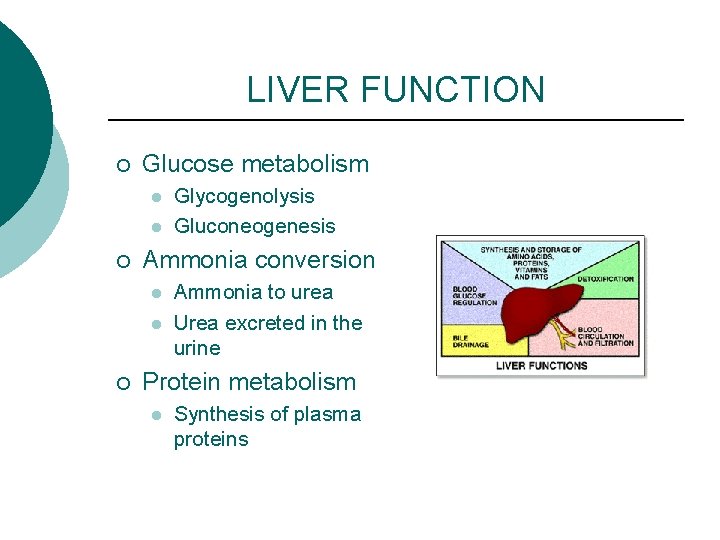
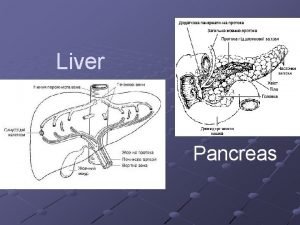
LIVER FUNCTION ¡ Glucose metabolism l l ¡ Ammonia conversion l l ¡ Glycogenolysis Gluconeogenesis Ammonia to urea Urea excreted in the urine Protein metabolism l Synthesis of plasma proteins
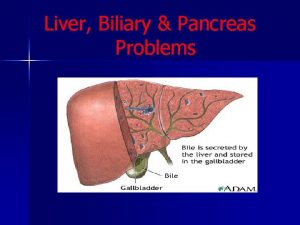
LIVER FUNCTION ¡ Fat metabolism l ¡ Vitamin and iron storage l ¡ ¡ ¡ Fatty acids broken down for energy Vitamin A, B, D, and Bcomplex vitamins Bile formation Bilirubin excretion Drug metabolism
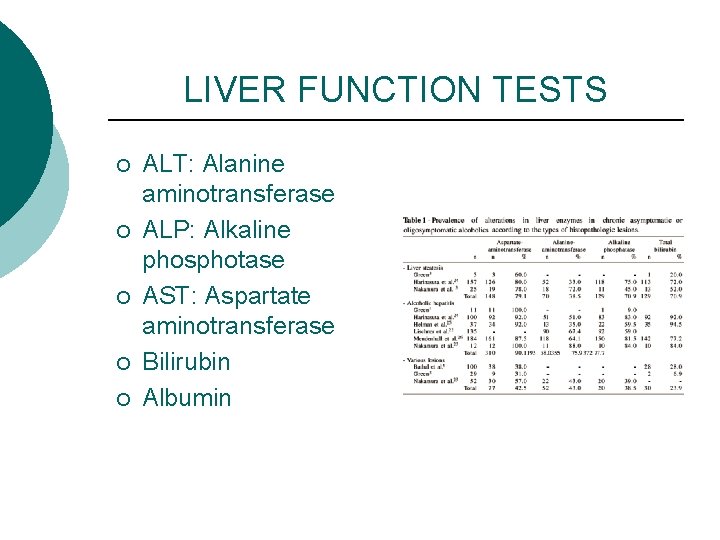
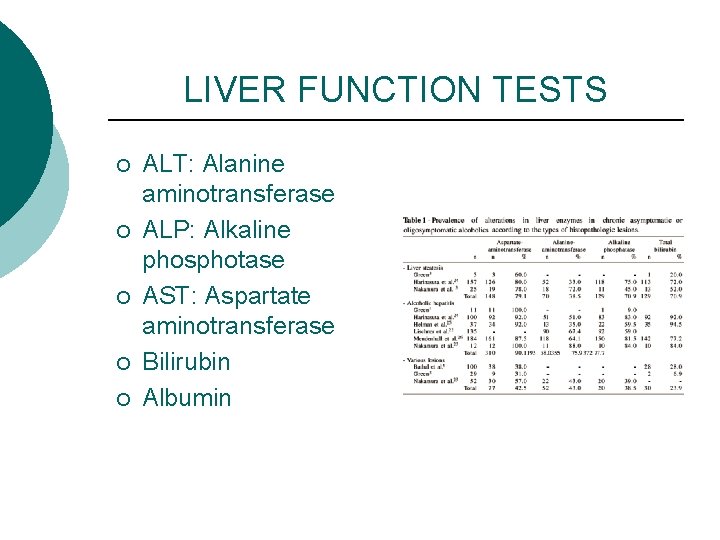
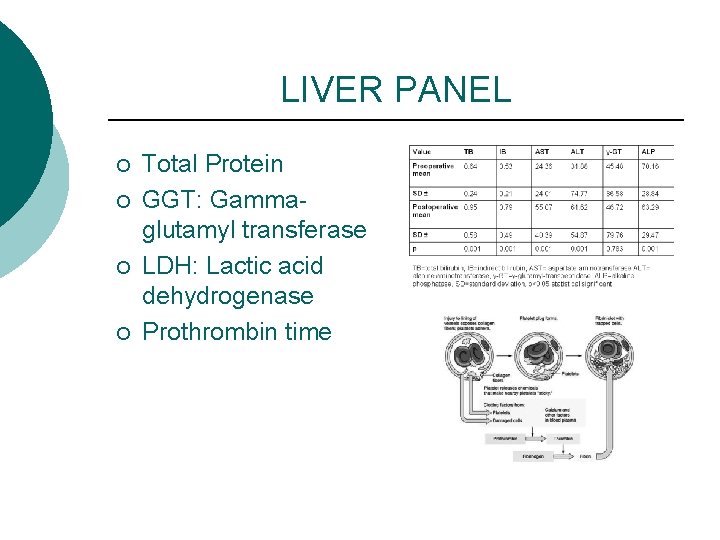
LIVER FUNCTION TESTS ¡ ¡ ¡ ALT: Alanine aminotransferase ALP: Alkaline phosphotase AST: Aspartate aminotransferase Bilirubin Albumin
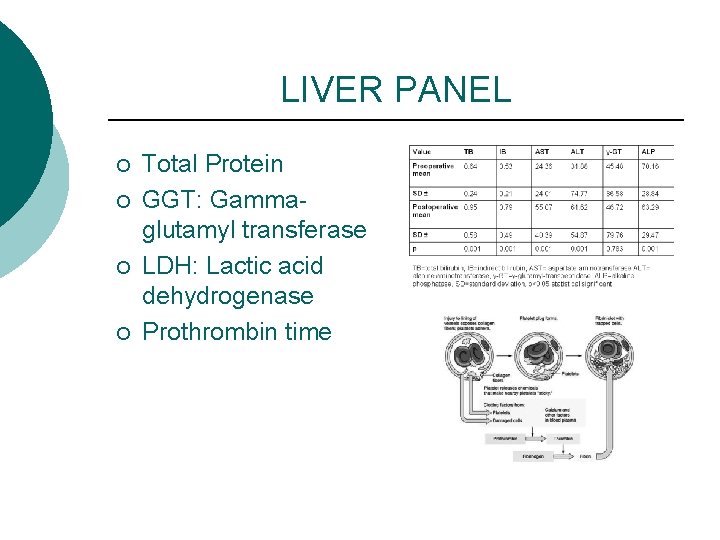
LIVER PANEL ¡ ¡ Total Protein GGT: Gammaglutamyl transferase LDH: Lactic acid dehydrogenase Prothrombin time
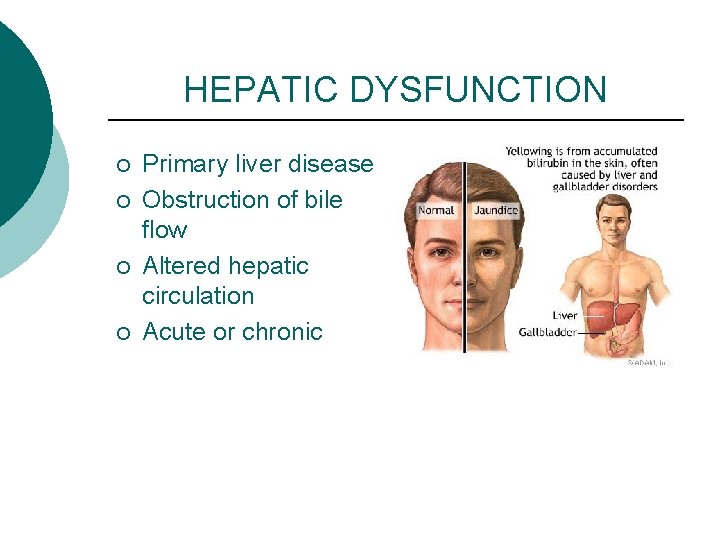
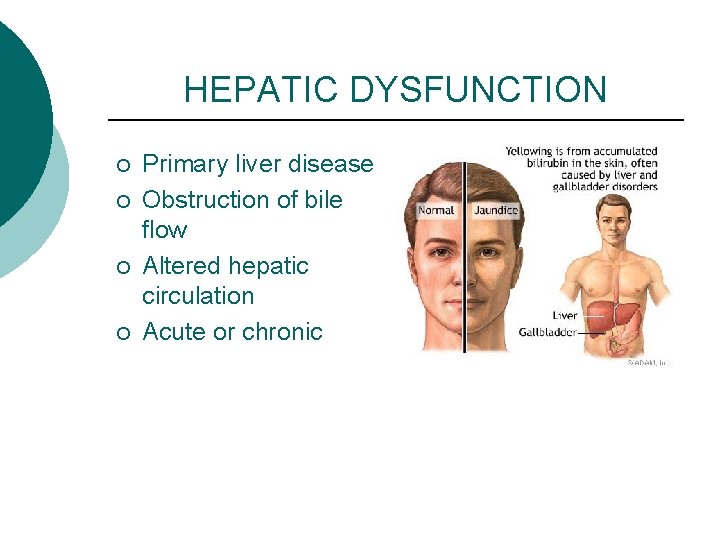
HEPATIC DYSFUNCTION ¡ ¡ Primary liver disease Obstruction of bile flow Altered hepatic circulation Acute or chronic
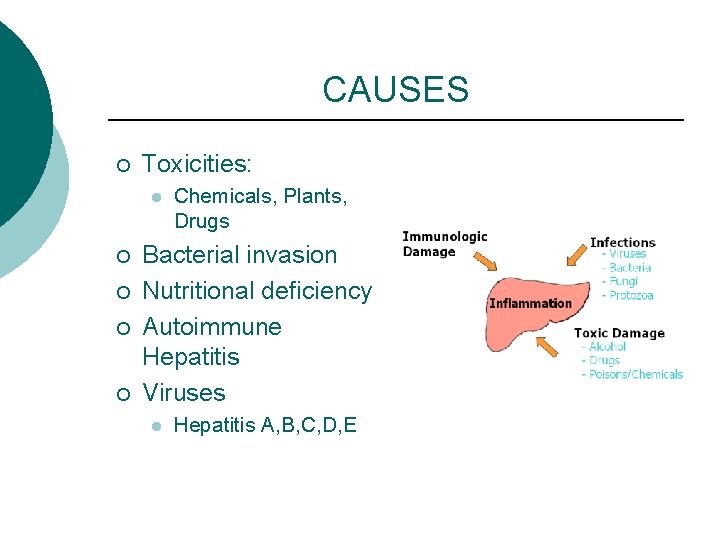
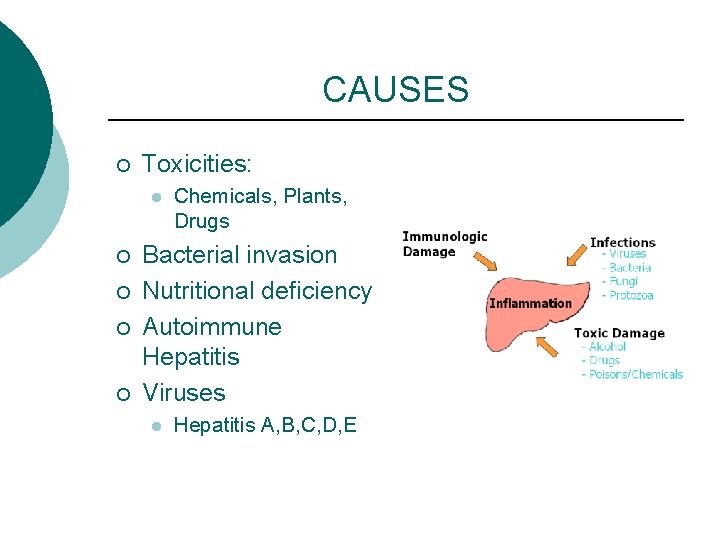
CAUSES ¡ Toxicities: l ¡ ¡ Chemicals, Plants, Drugs Bacterial invasion Nutritional deficiency Autoimmune Hepatitis Viruses l Hepatitis A, B, C, D, E
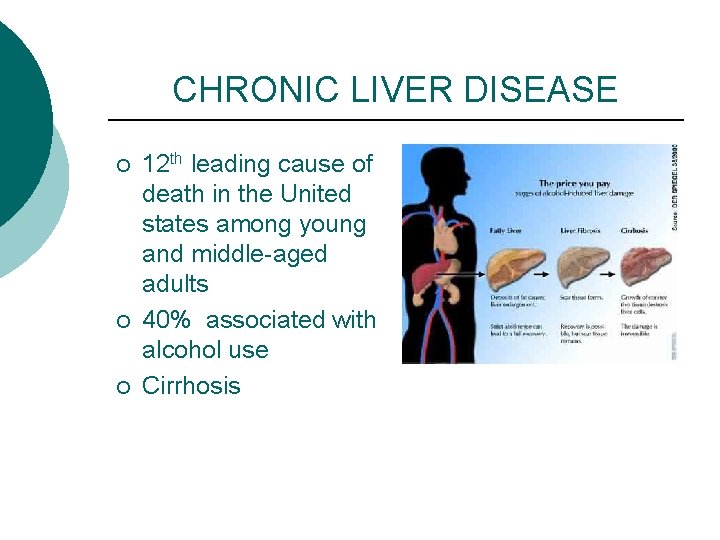
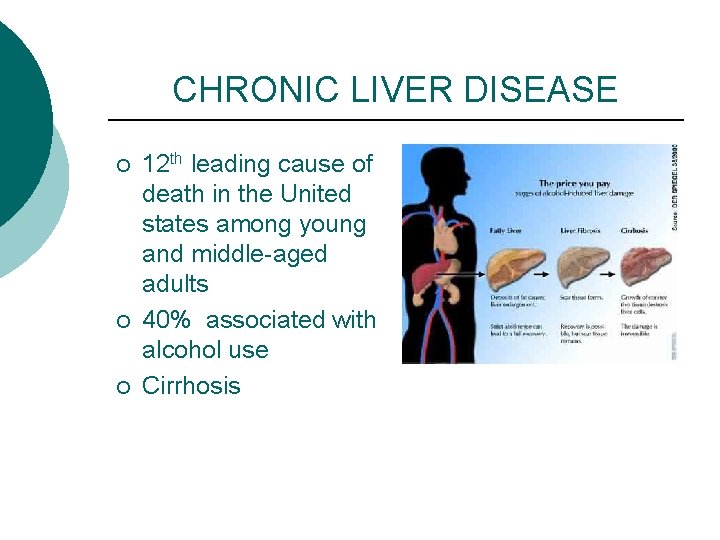
CHRONIC LIVER DISEASE ¡ ¡ ¡ 12 th leading cause of death in the United states among young and middle-aged adults 40% associated with alcohol use Cirrhosis
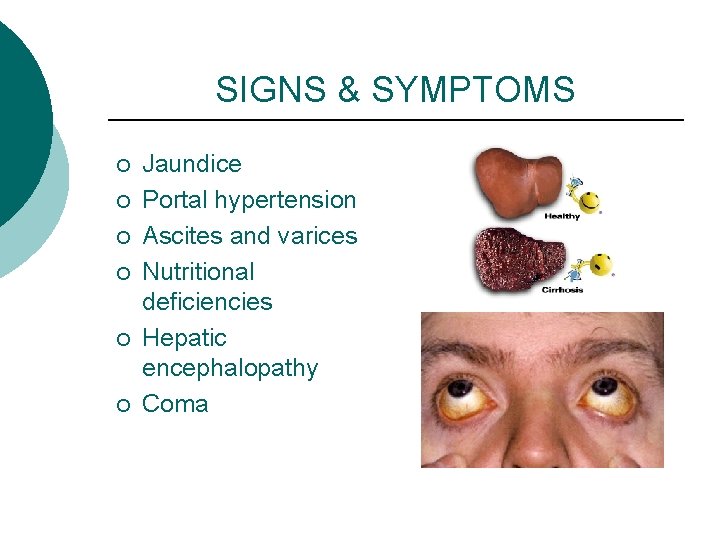
SIGNS & SYMPTOMS ¡ ¡ ¡ Jaundice Portal hypertension Ascites and varices Nutritional deficiencies Hepatic encephalopathy Coma
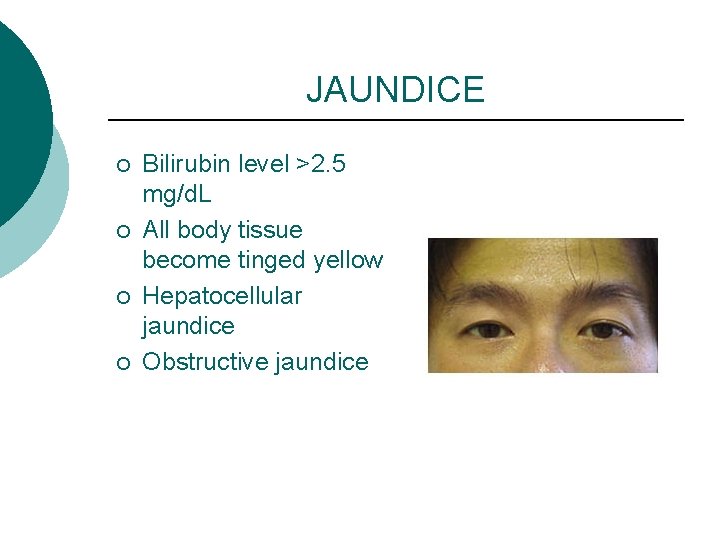
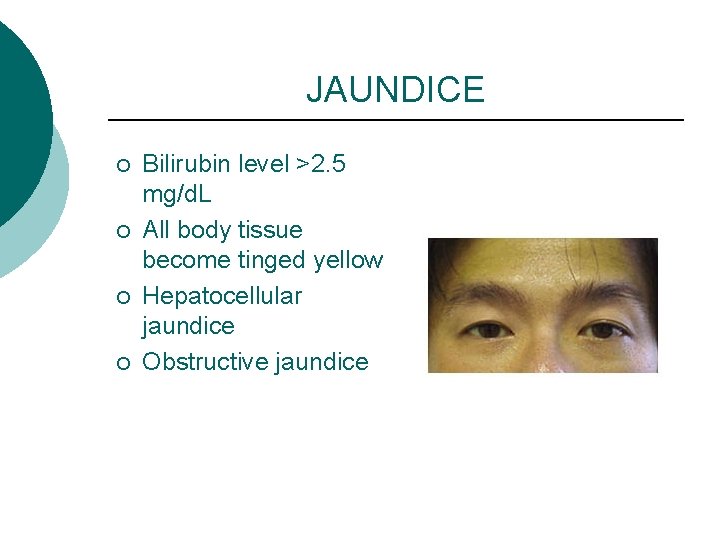
JAUNDICE ¡ ¡ Bilirubin level >2. 5 mg/d. L All body tissue become tinged yellow Hepatocellular jaundice Obstructive jaundice
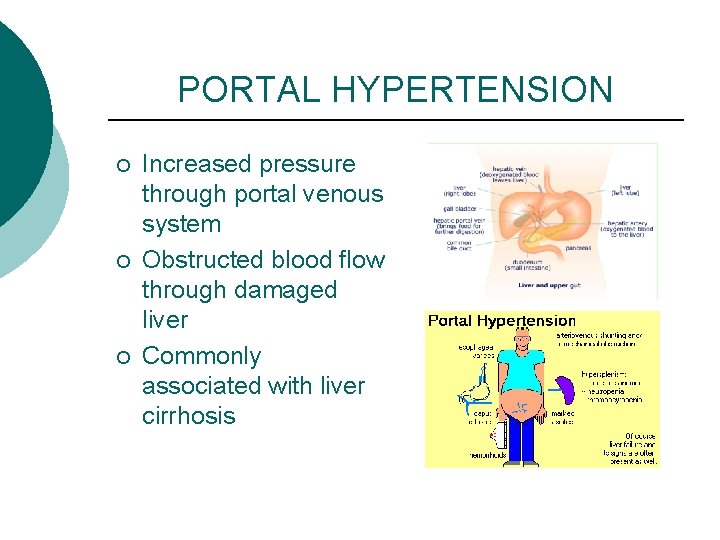
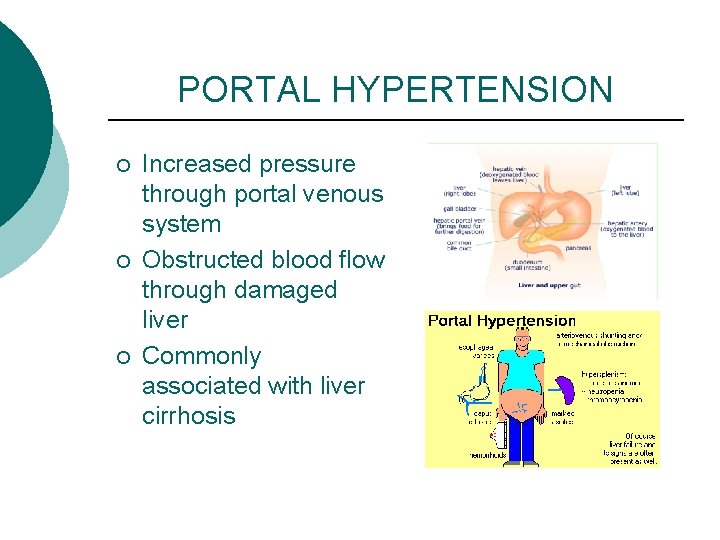
PORTAL HYPERTENSION ¡ ¡ ¡ Increased pressure through portal venous system Obstructed blood flow through damaged liver Commonly associated with liver cirrhosis
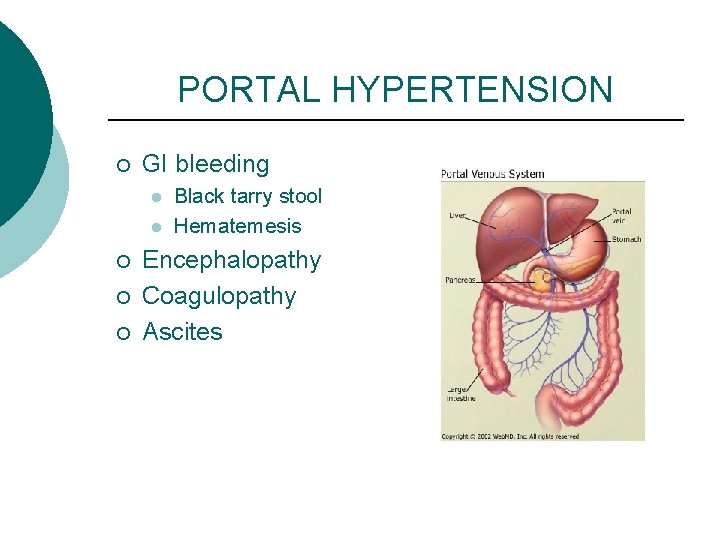
PORTAL HYPERTENSION ¡ GI bleeding l l ¡ ¡ ¡ Black tarry stool Hematemesis Encephalopathy Coagulopathy Ascites
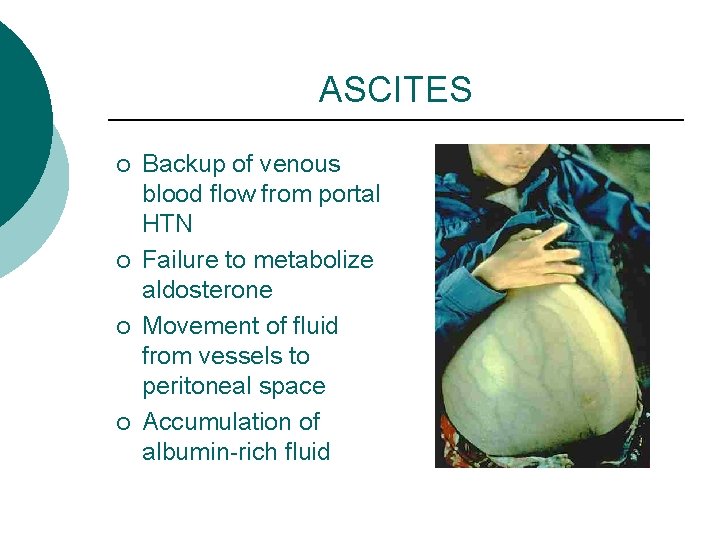
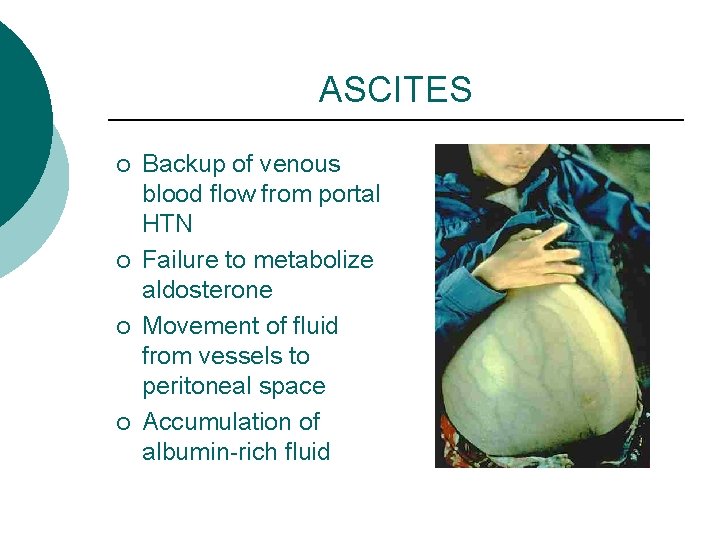
ASCITES ¡ ¡ Backup of venous blood flow from portal HTN Failure to metabolize aldosterone Movement of fluid from vessels to peritoneal space Accumulation of albumin-rich fluid
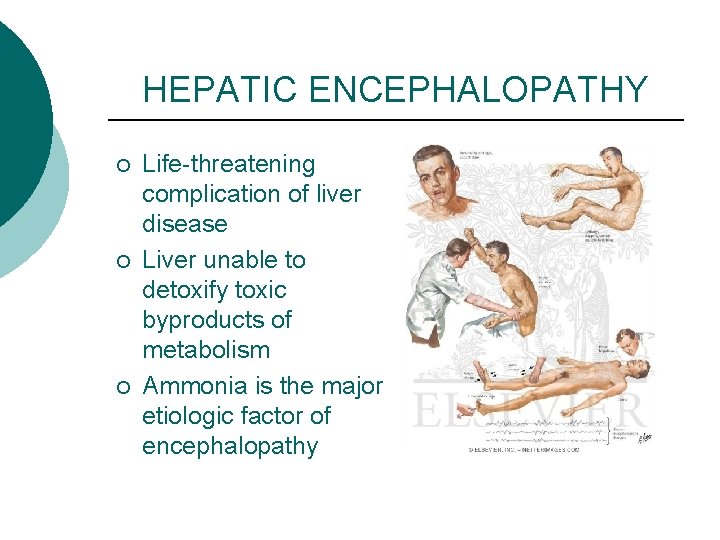
HEPATIC ENCEPHALOPATHY ¡ ¡ ¡ Life-threatening complication of liver disease Liver unable to detoxify toxic byproducts of metabolism Ammonia is the major etiologic factor of encephalopathy
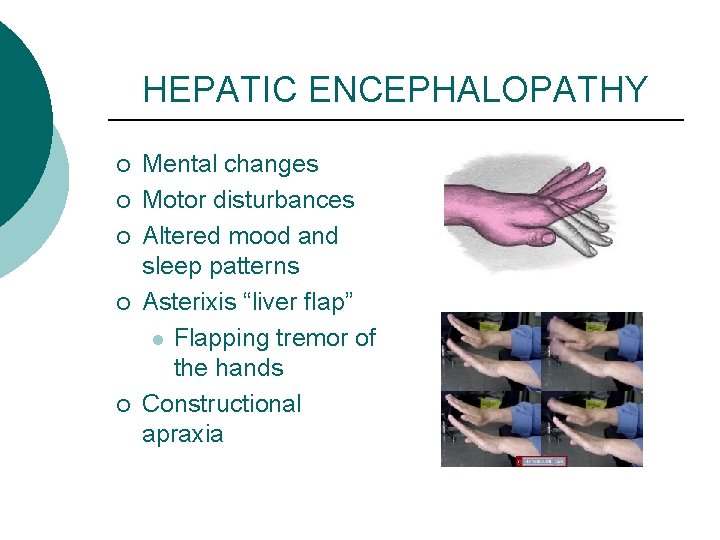
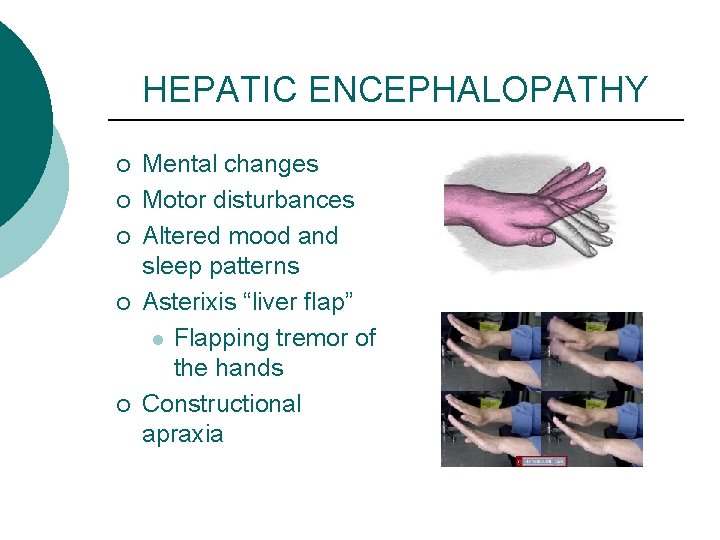
HEPATIC ENCEPHALOPATHY ¡ ¡ ¡ Mental changes Motor disturbances Altered mood and sleep patterns Asterixis “liver flap” l Flapping tremor of the hands Constructional apraxia
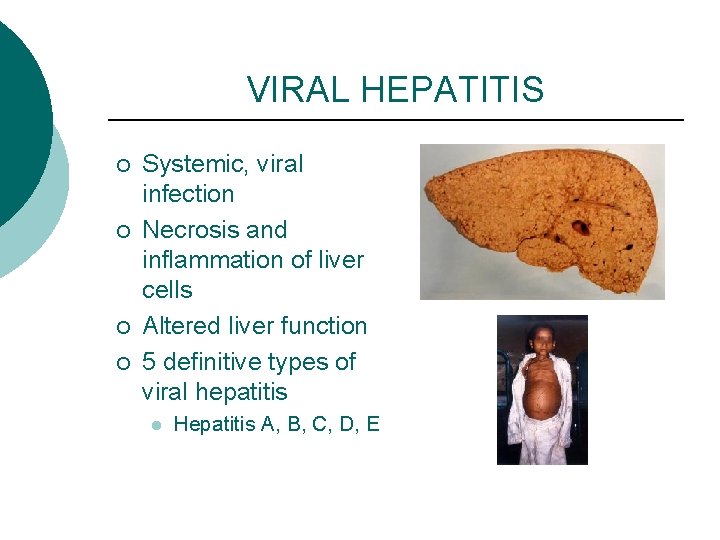
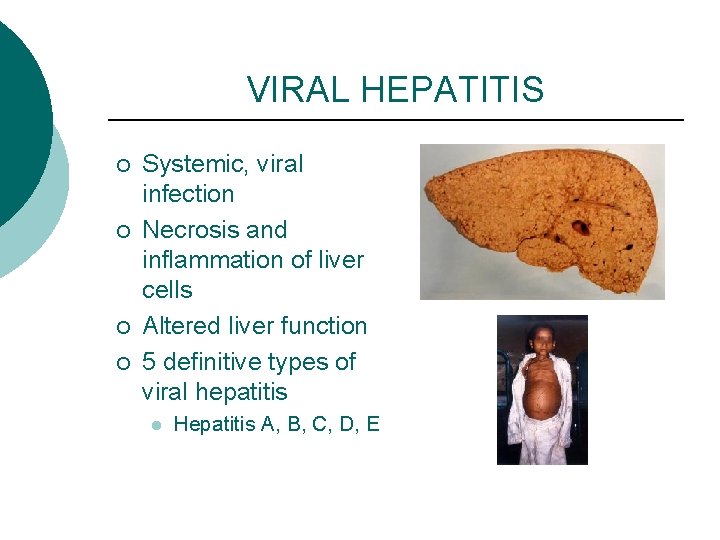
VIRAL HEPATITIS ¡ ¡ Systemic, viral infection Necrosis and inflammation of liver cells Altered liver function 5 definitive types of viral hepatitis l Hepatitis A, B, C, D, E
HEPATITIS A ¡ ¡ Hepatitis A Virus Fecal-oral transmission l l l ¡ Poor sanitation Person-person contact Water and food borne Incubation l 15 -50 days
SIGNS and SYMPTOMS Hepatitis A Phases ¡ Preicteric l l l Flu-like symptoms Fatigue Loss of appetite Nausea Cough Joint pain
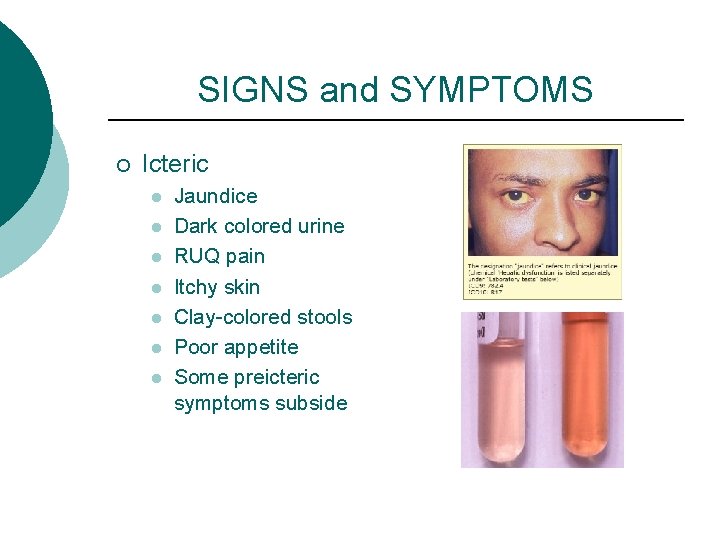
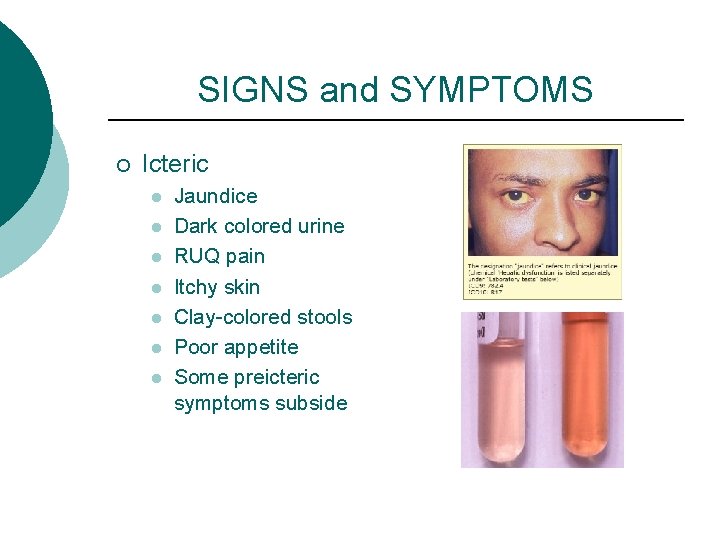
SIGNS and SYMPTOMS ¡ Icteric l l l l Jaundice Dark colored urine RUQ pain Itchy skin Clay-colored stools Poor appetite Some preicteric symptoms subside
SIGNS and SYMPTOMS ¡ Post icteric phase l l Things start to return to normal Fatigue can remain
HEPATITIS A ¡ ¡ ¡ Mild with recovery No carrier state Doesn’t usually lead to chronic state
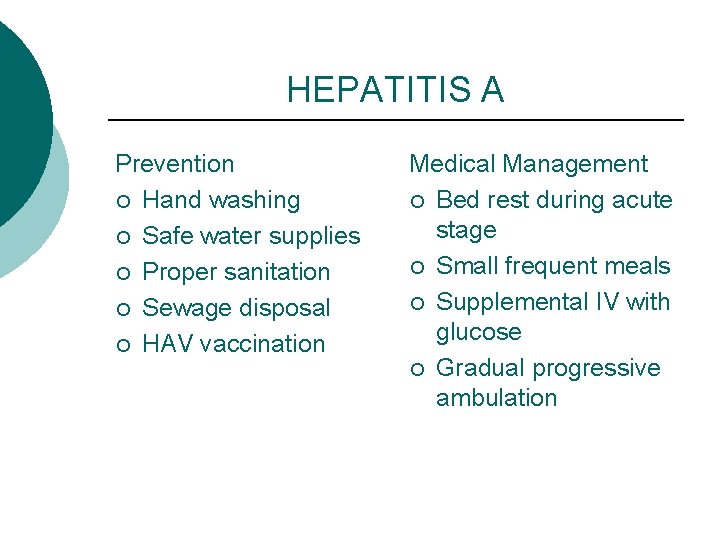
HEPATITIS A Prevention ¡ Hand washing ¡ Safe water supplies ¡ Proper sanitation ¡ Sewage disposal ¡ HAV vaccination Medical Management ¡ Bed rest during acute stage ¡ Small frequent meals ¡ Supplemental IV with glucose ¡ Gradual progressive ambulation
HEPATITIS B ¡ ¡ ¡ Hepatitis B Virus Parenteral transmission Intimate contact with carriers Perinatal: mother to baby Occupational hazard to health care workers
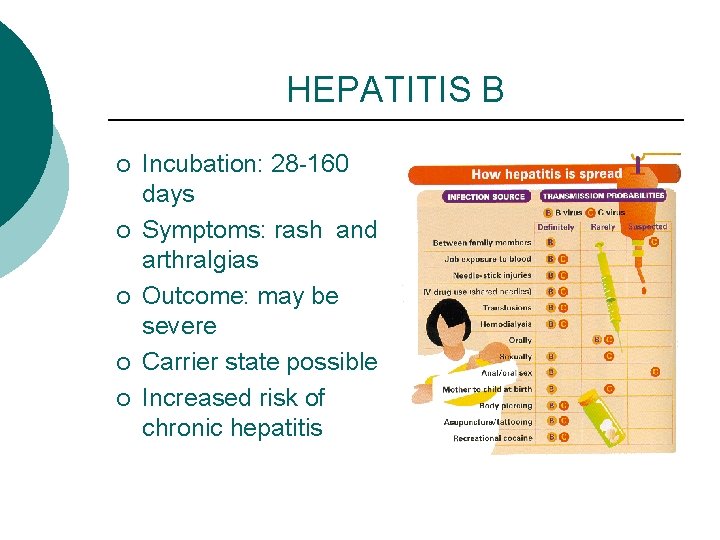
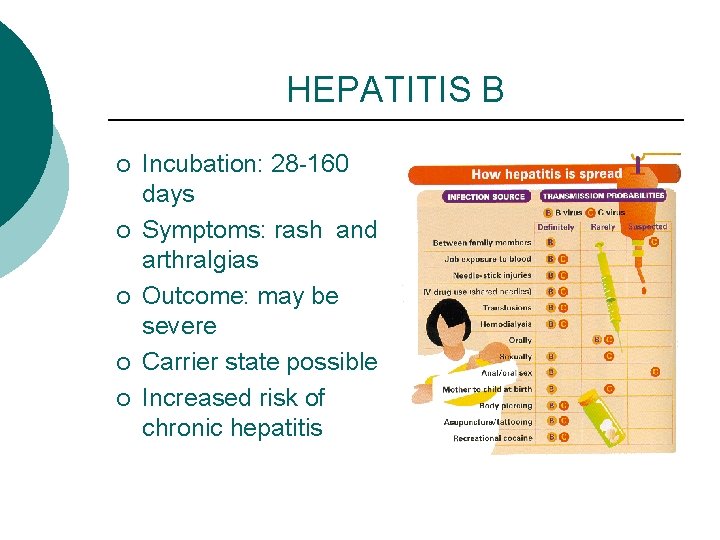
HEPATITIS B ¡ ¡ ¡ Incubation: 28 -160 days Symptoms: rash and arthralgias Outcome: may be severe Carrier state possible Increased risk of chronic hepatitis
HEPATITIS B Prevention ¡ Hand washing ¡ Wear gloves when handling body fluids ¡ safe sex ¡ HBV vaccination ¡ Hepatitis B Immunoglobulin Medical management ¡ Alpha-interferon ¡ Lamivudine (Epivir) and adefovir (Hepsera) ¡ Bed rest until s/s subside ¡ Restrict activities ¡ Adequate nutrition
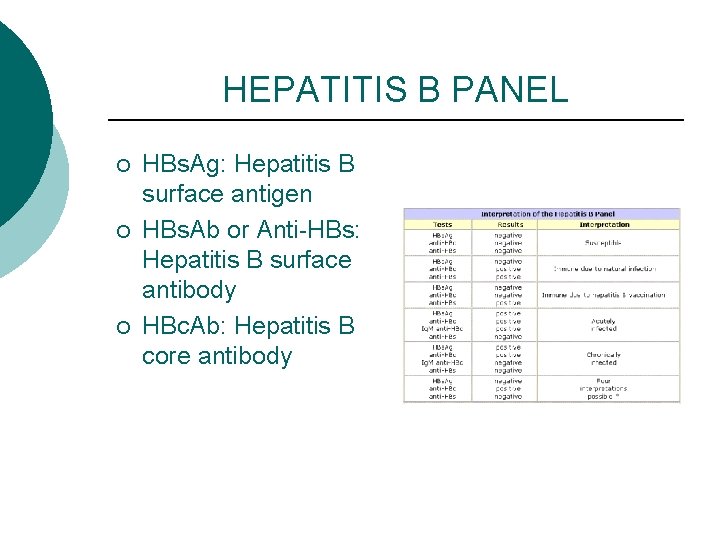
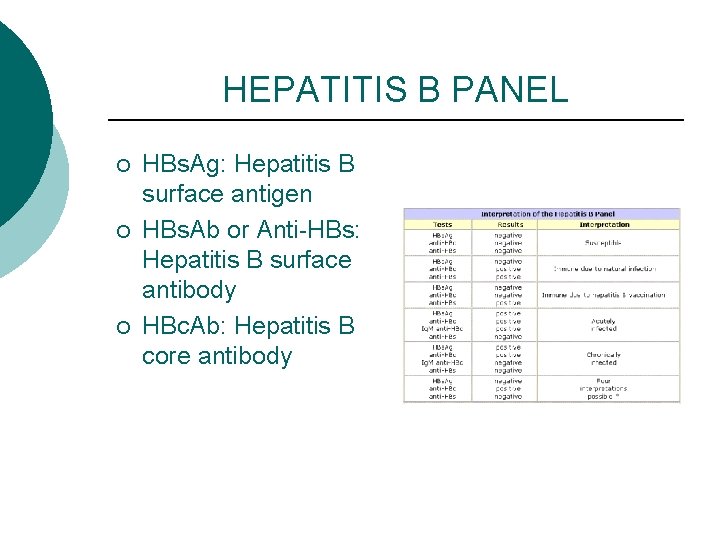
HEPATITIS B PANEL ¡ ¡ ¡ HBs. Ag: Hepatitis B surface antigen HBs. Ab or Anti-HBs: Hepatitis B surface antibody HBc. Ab: Hepatitis B core antibody
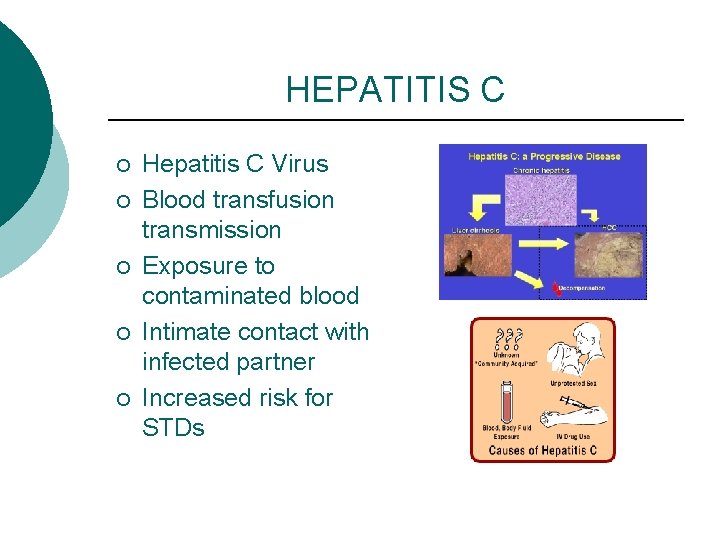
HEPATITIS C ¡ ¡ ¡ Hepatitis C Virus Blood transfusion transmission Exposure to contaminated blood Intimate contact with infected partner Increased risk for STDs
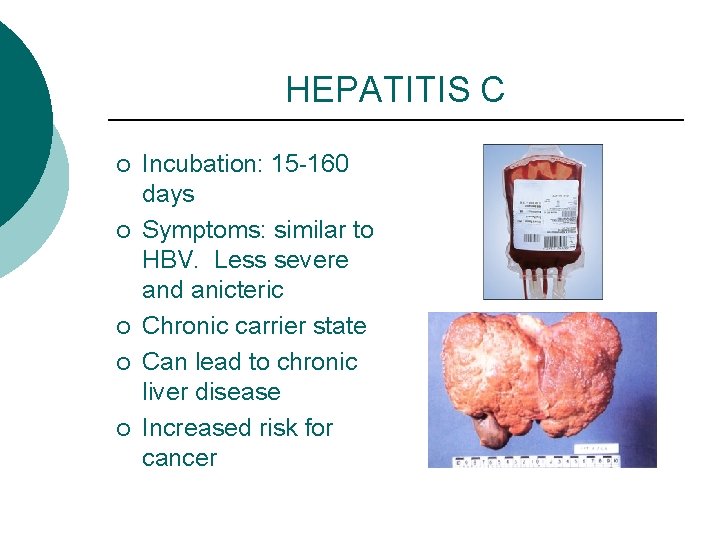
HEPATITIS C ¡ ¡ ¡ Incubation: 15 -160 days Symptoms: similar to HBV. Less severe and anicteric Chronic carrier state Can lead to chronic liver disease Increased risk for cancer
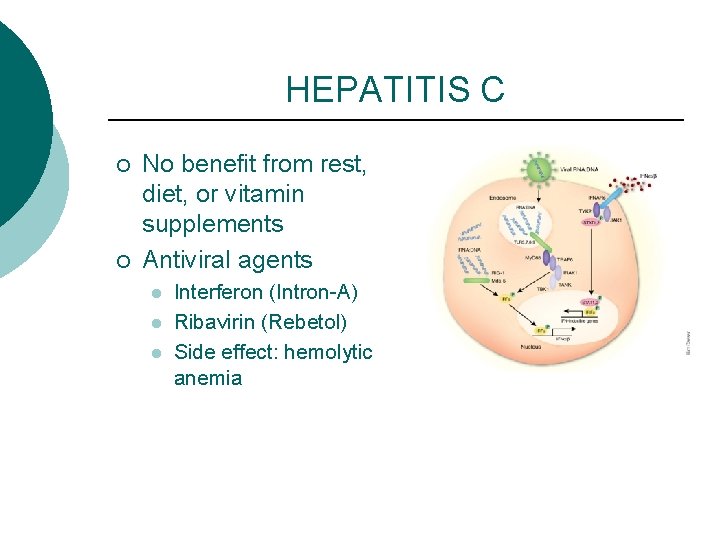
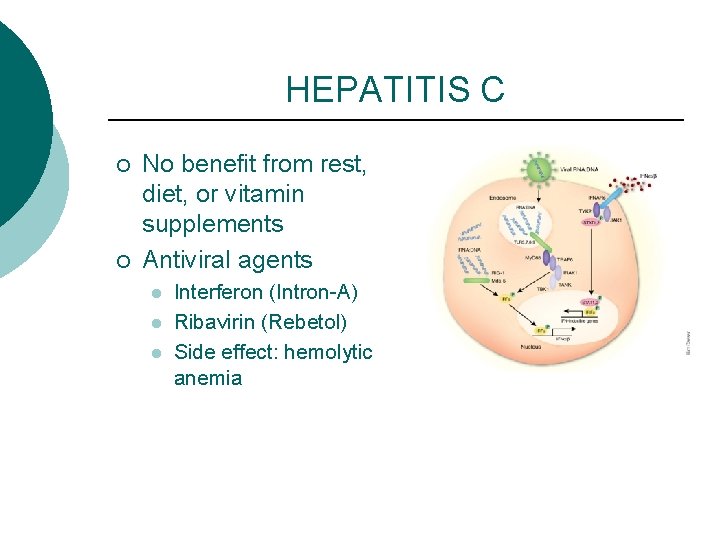
HEPATITIS C ¡ ¡ No benefit from rest, diet, or vitamin supplements Antiviral agents l l l Interferon (Intron-A) Ribavirin (Rebetol) Side effect: hemolytic anemia
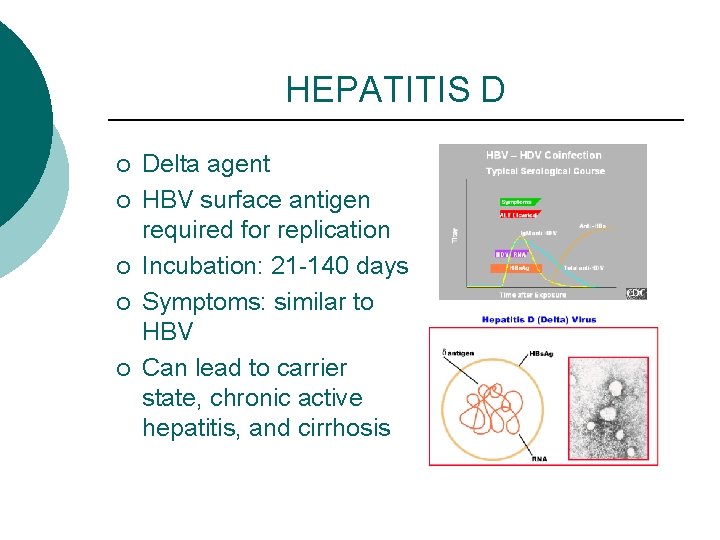
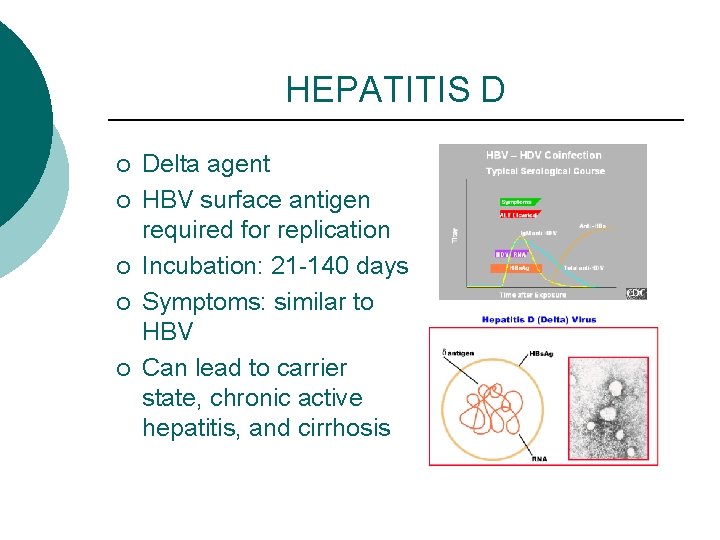
HEPATITIS D ¡ ¡ ¡ Delta agent HBV surface antigen required for replication Incubation: 21 -140 days Symptoms: similar to HBV Can lead to carrier state, chronic active hepatitis, and cirrhosis
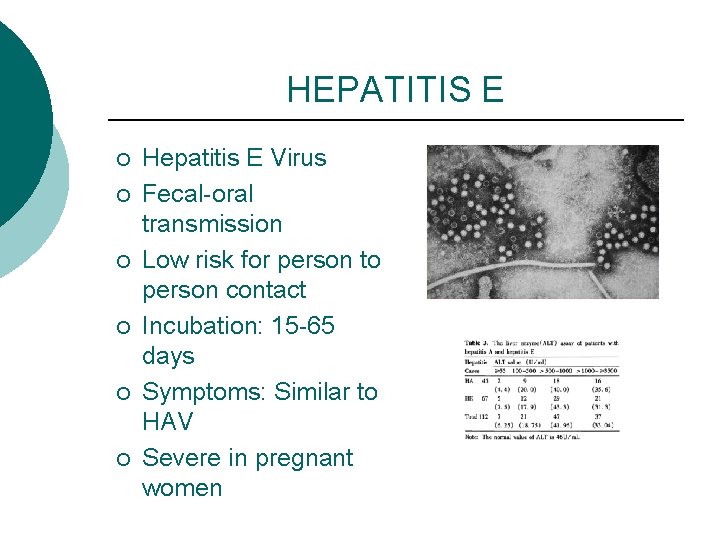
HEPATITIS E ¡ ¡ ¡ Hepatitis E Virus Fecal-oral transmission Low risk for person to person contact Incubation: 15 -65 days Symptoms: Similar to HAV Severe in pregnant women
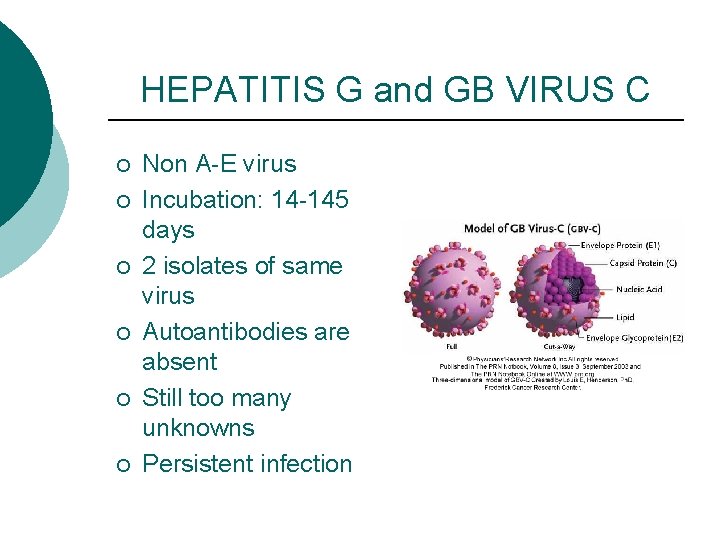
HEPATITIS G and GB VIRUS C ¡ ¡ ¡ Non A-E virus Incubation: 14 -145 days 2 isolates of same virus Autoantibodies are absent Still too many unknowns Persistent infection
TOXIC HEPATITIS ¡ ¡ Resembles viral hepatitis Exposure to toxic chemicals l l ¡ Medications Botanicals Remove causative agent
TOXIC HEPATITIS ¡ ¡ ¡ Anorexia, nausea, vomiting Jaundice Hepatomegaly No effective antidotes Delay in treatment can result in increased severity
DRUG INDUCED HEPATITIS ¡ ¡ ¡ Most common cause of acute liver failure 50% of all cases in the U. S. Acetaminophen has been identified as the leading cause of acute liver failure
DRUG INDUCED HEPATITIS ¡ ¡ Onset is abrupt Early symptoms l ¡ Late symptoms l ¡ Fever, chills, rash, arthralgia, pruritus, anorexia Jaundice, dark urine, enlarged and tender liver Treatment l Short course of high-dose corticosteroids
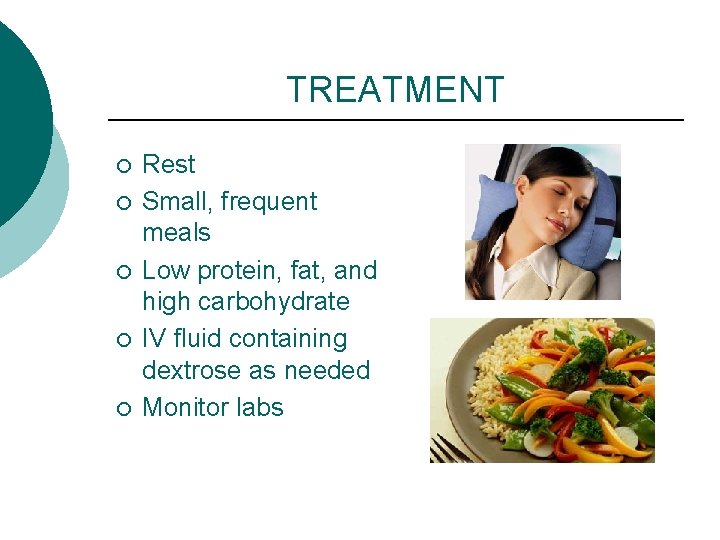
TREATMENT ¡ ¡ ¡ Rest Small, frequent meals Low protein, fat, and high carbohydrate IV fluid containing dextrose as needed Monitor labs
 Acnp gestionale
Acnp gestionale Q
Q Liver and pancreas function
Liver and pancreas function Function of duodenum
Function of duodenum Pancreasitis
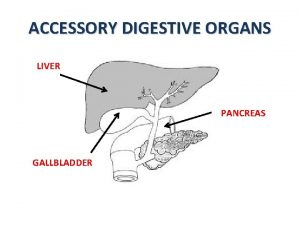
Pancreasitis Structure of liver gallbladder and pancreas
Structure of liver gallbladder and pancreas Creative commons
Creative commons Phases of 1st stage of labour
Phases of 1st stage of labour Orgasmic dysfunction
Orgasmic dysfunction Rib raising omt
Rib raising omt Sam byron
Sam byron Dr arshad ejazi
Dr arshad ejazi Rib somatic dysfunction
Rib somatic dysfunction True labour pain
True labour pain Conjunction dysfunction meaning
Conjunction dysfunction meaning What causes ataxia
What causes ataxia Spinocerebellar ataxia type 3 symptoms
Spinocerebellar ataxia type 3 symptoms Robert k merton structural functionalism
Robert k merton structural functionalism Ivrt echo
Ivrt echo Urt
Urt Nulliparous
Nulliparous Judy ritchie
Judy ritchie Impaired mentation
Impaired mentation Nzrsi
Nzrsi North dakota null hypothesis brain inventory
North dakota null hypothesis brain inventory Afnameprotocol machine
Afnameprotocol machine Valérie altuzarra
Valérie altuzarra Valerie nyberg
Valerie nyberg Swift og franzen
Swift og franzen Automatic thoughts examples
Automatic thoughts examples Valerie lavat
Valerie lavat Valerie brossier
Valerie brossier Valerie buitron
Valerie buitron Machine learning actuary
Machine learning actuary Valerie du preez
Valerie du preez Valerie blair
Valerie blair Valérie langevin
Valérie langevin Valerie marneffe
Valerie marneffe Valerie stevenson
Valerie stevenson Valerie schmutz
Valerie schmutz Organelle case study answer key
Organelle case study answer key Valerie ding parents
Valerie ding parents Valerie namer
Valerie namer Dysphonetic
Dysphonetic Valerie flournoy
Valerie flournoy Ice hockey
Ice hockey Beniahan
Beniahan Valerie collier
Valerie collier Valerie iseminger
Valerie iseminger Valerie schulz
Valerie schulz Valerie dominguez facebook
Valerie dominguez facebook Peter martinazzi
Peter martinazzi Valerie huhn
Valerie huhn Valerie blair
Valerie blair Valerie booth drexel
Valerie booth drexel Valérie seyssiecq
Valérie seyssiecq Changer l'eau des fleurs valérie perrin
Changer l'eau des fleurs valérie perrin Huck finn chapter 24 summary
Huck finn chapter 24 summary Mirjam vili
Mirjam vili Valerie fauvel
Valerie fauvel Valerie ding
Valerie ding Valerie buitron
Valerie buitron Anatomy and physiology of diabetes
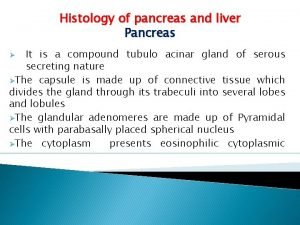
Anatomy and physiology of diabetes Pancreas histology slide
Pancreas histology slide Pineal and pancreas glands
Pineal and pancreas glands Gastric glands
Gastric glands Criterios de ranson biliar
Criterios de ranson biliar Tmpi de rama secundaria
Tmpi de rama secundaria Vascolarizzazione pancreas
Vascolarizzazione pancreas El proceso de digestion
El proceso de digestion Lame rétro porte
Lame rétro porte Pancreas anatomia microscopica
Pancreas anatomia microscopica Right triangular ligament
Right triangular ligament Système porte schéma
Système porte schéma Astenia nervosa
Astenia nervosa