How to Help Patients with Chronic Myofascial Pain








- Slides: 76
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head and Neck Region 神經內科 洪國華
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head and Neck Region • Some diseases are not curable, but all patient could be given help
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head and Neck Region • Acute pain – A biologically useful symptom • Chronic pain (>3 months) – Patient continue to cope, work, love and embrace life, even with pain • Chronic pain syndrome – A disease in itself
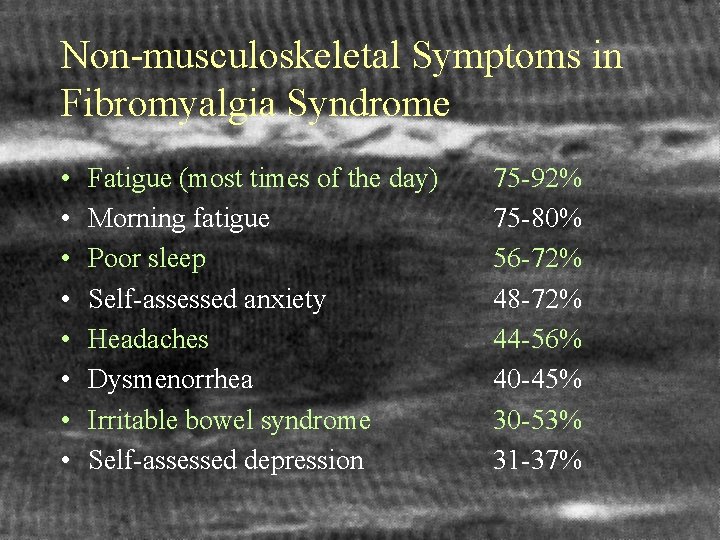
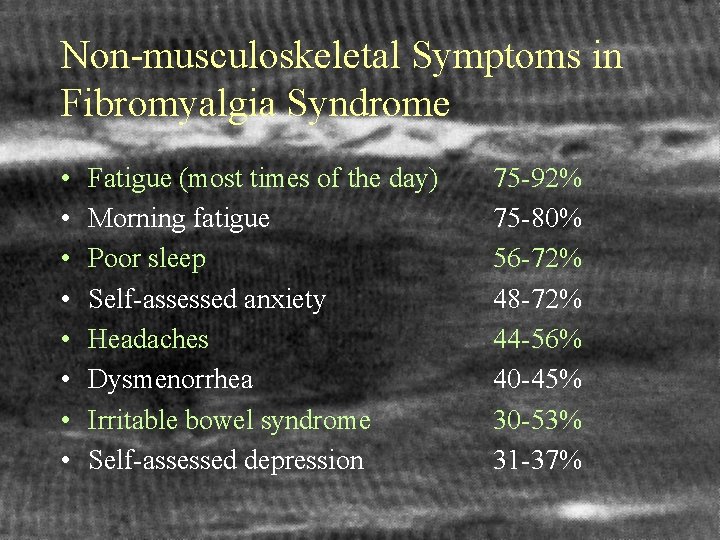
Non-musculoskeletal Symptoms in Fibromyalgia Syndrome • • Fatigue (most times of the day) Morning fatigue Poor sleep Self-assessed anxiety Headaches Dysmenorrhea Irritable bowel syndrome Self-assessed depression 75 -92% 75 -80% 56 -72% 48 -72% 44 -56% 40 -45% 30 -53% 31 -37%
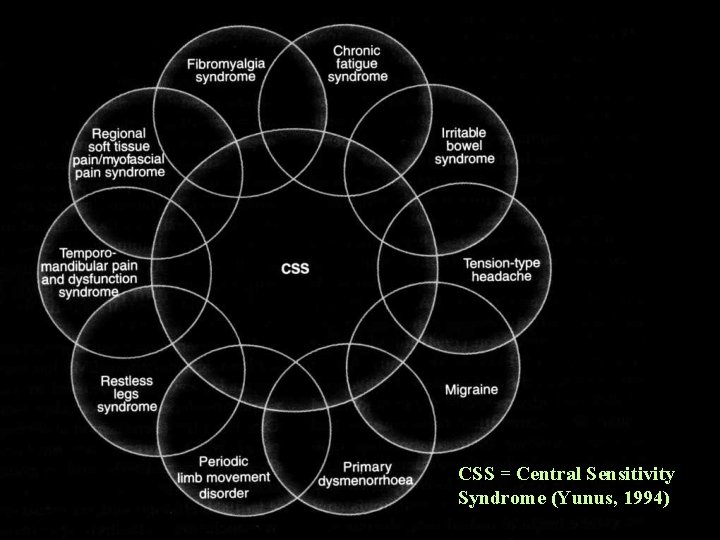
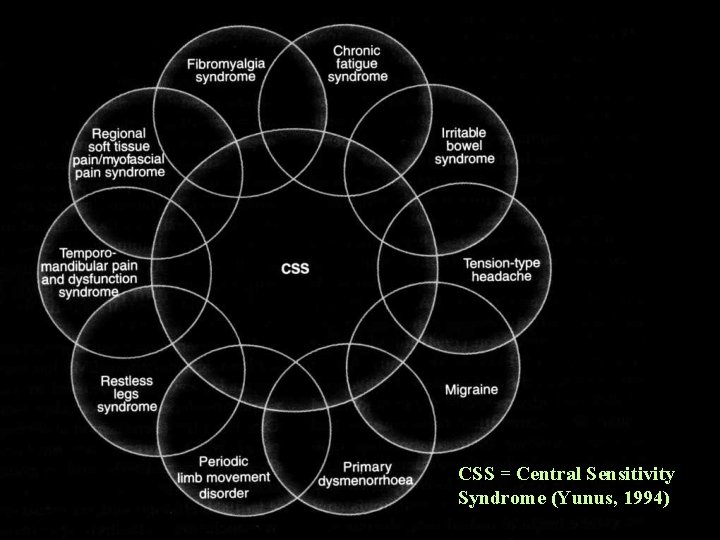
CSS = Central Sensitivity Syndrome (Yunus, 1994)
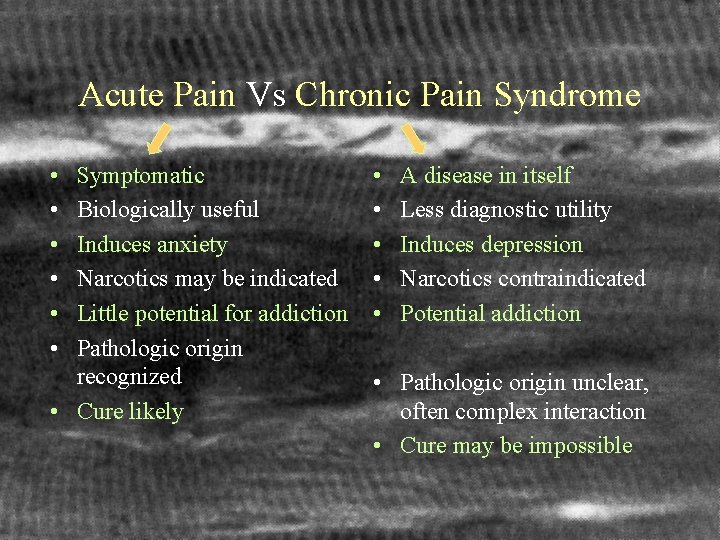
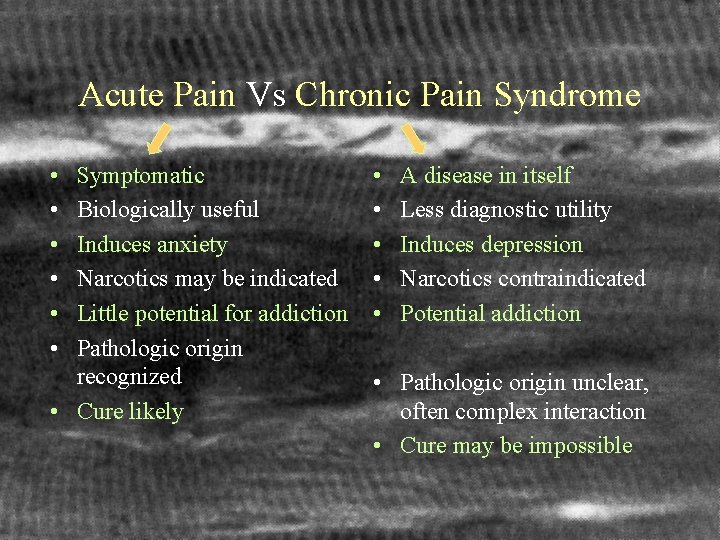
Acute Pain Vs Chronic Pain Syndrome • • • Symptomatic Biologically useful Induces anxiety Narcotics may be indicated Little potential for addiction Pathologic origin recognized • Cure likely • • • A disease in itself Less diagnostic utility Induces depression Narcotics contraindicated Potential addiction • Pathologic origin unclear, often complex interaction • Cure may be impossible
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head and Neck Region • Skeletal muscle – the largest organ of our body • Muscle Pain – One of the major sources of pain that may be overlooked
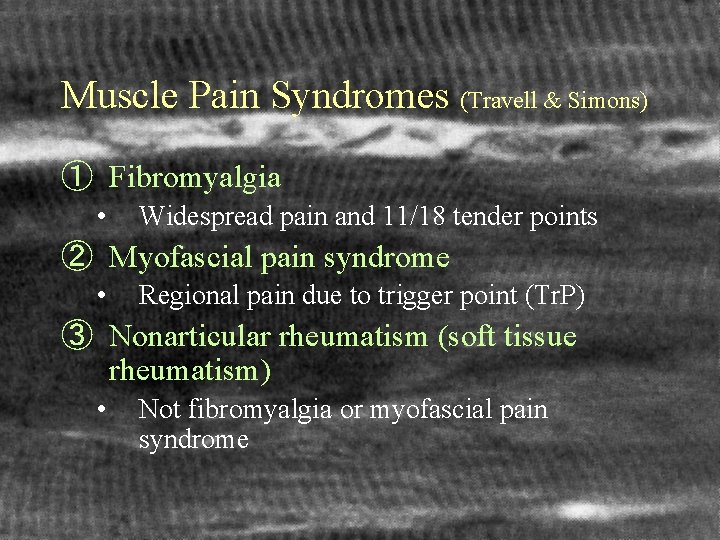
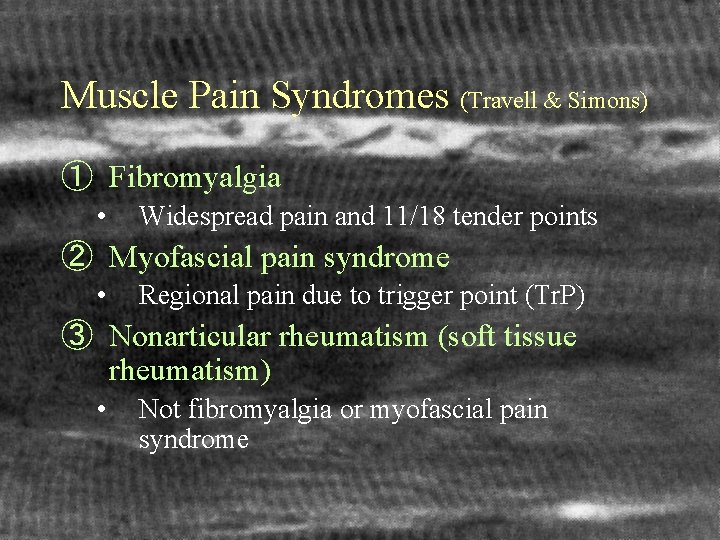
Muscle Pain Syndromes (Travell & Simons) ① Fibromyalgia • Widespread pain and 11/18 tender points ② Myofascial pain syndrome • Regional pain due to trigger point (Tr. P) ③ Nonarticular rheumatism (soft tissue rheumatism) • Not fibromyalgia or myofascial pain syndrome
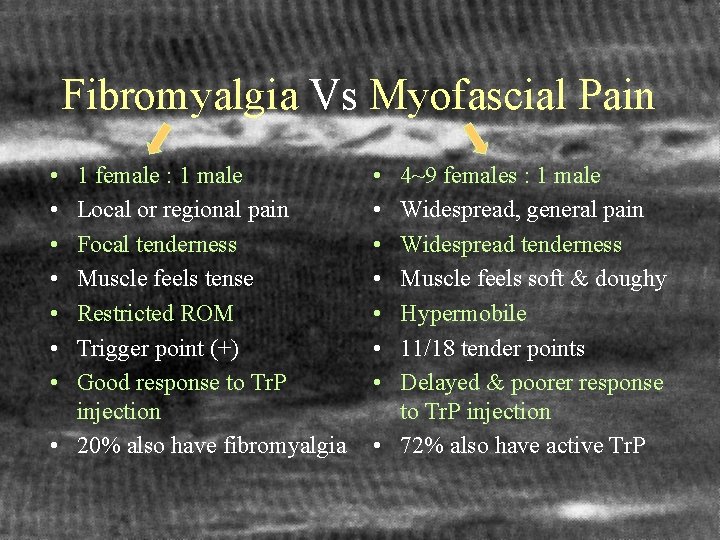
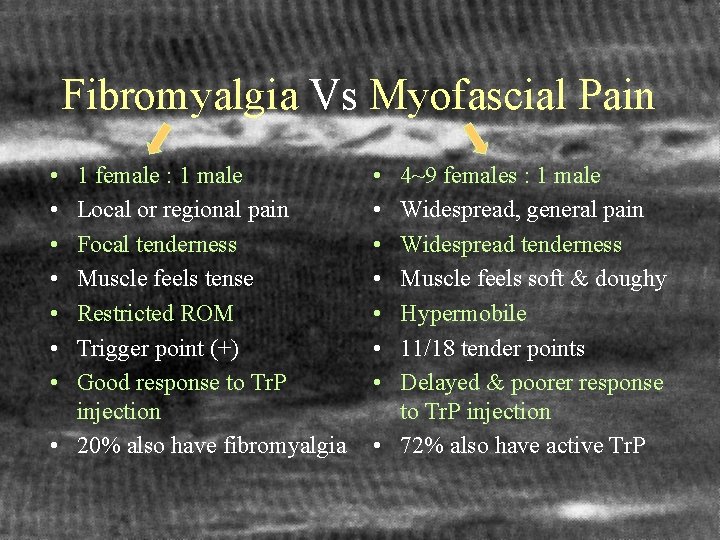
Fibromyalgia Vs Myofascial Pain • • 1 female : 1 male Local or regional pain Focal tenderness Muscle feels tense Restricted ROM Trigger point (+) Good response to Tr. P injection • 20% also have fibromyalgia • • 4~9 females : 1 male Widespread, general pain Widespread tenderness Muscle feels soft & doughy Hypermobile 11/18 tender points Delayed & poorer response to Tr. P injection • 72% also have active Tr. P
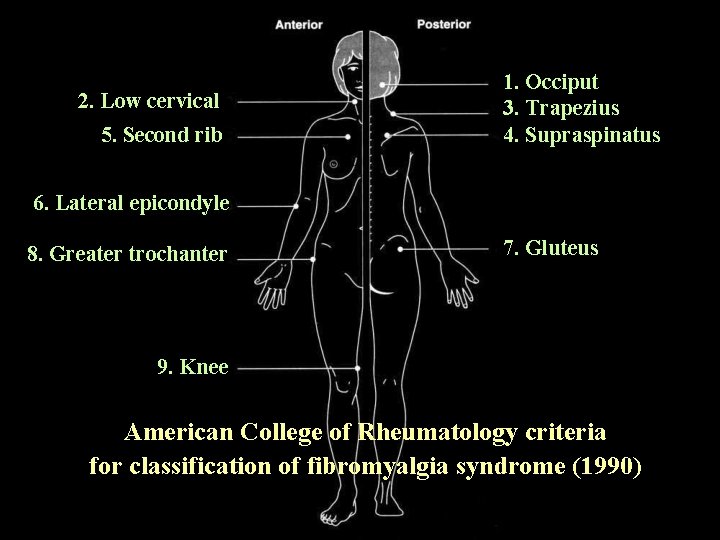
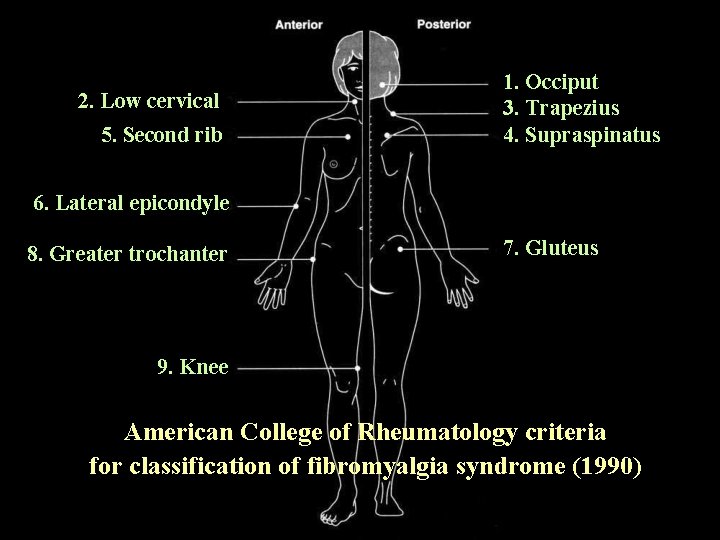
2. Low cervical 5. Second rib 1. Occiput 3. Trapezius 4. Supraspinatus 6. Lateral epicondyle 8. Greater trochanter 7. Gluteus 9. Knee American College of Rheumatology criteria for classification of fibromyalgia syndrome (1990)
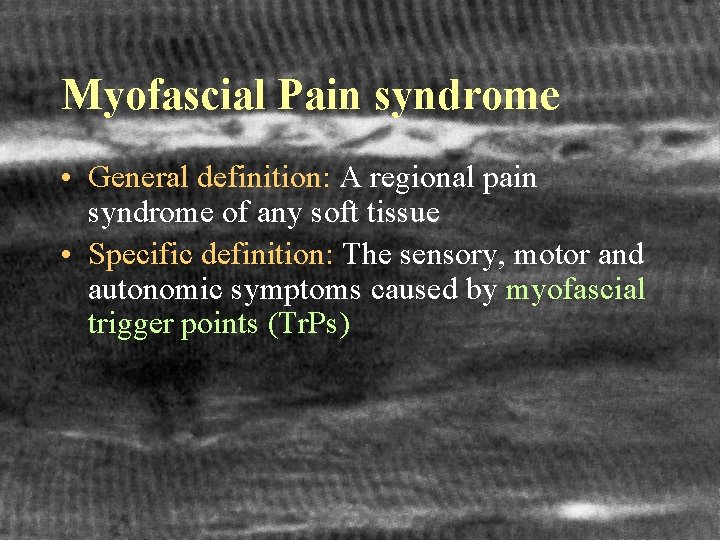
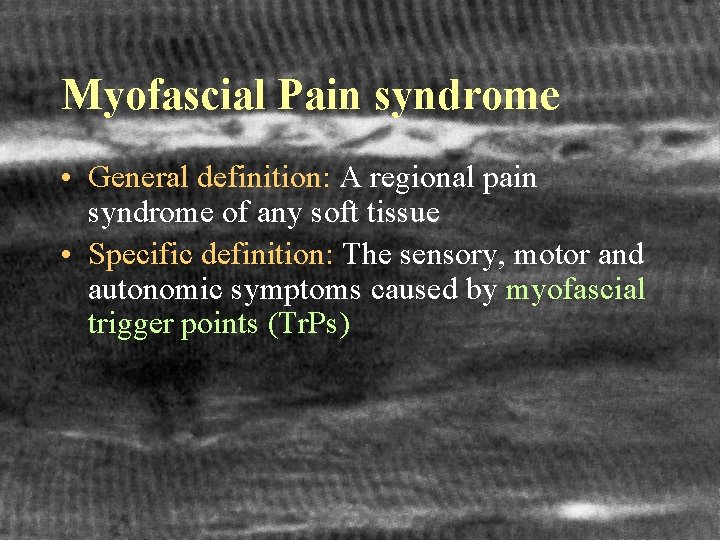
Myofascial Pain syndrome • General definition: A regional pain syndrome of any soft tissue • Specific definition: The sensory, motor and autonomic symptoms caused by myofascial trigger points (Tr. Ps)
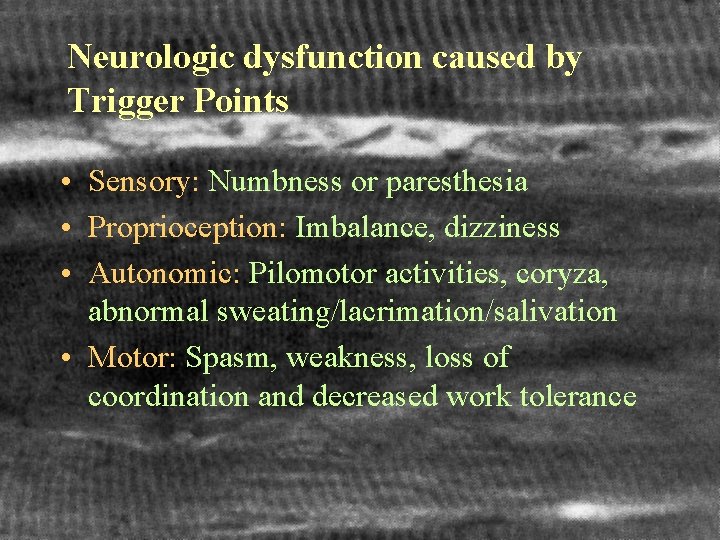
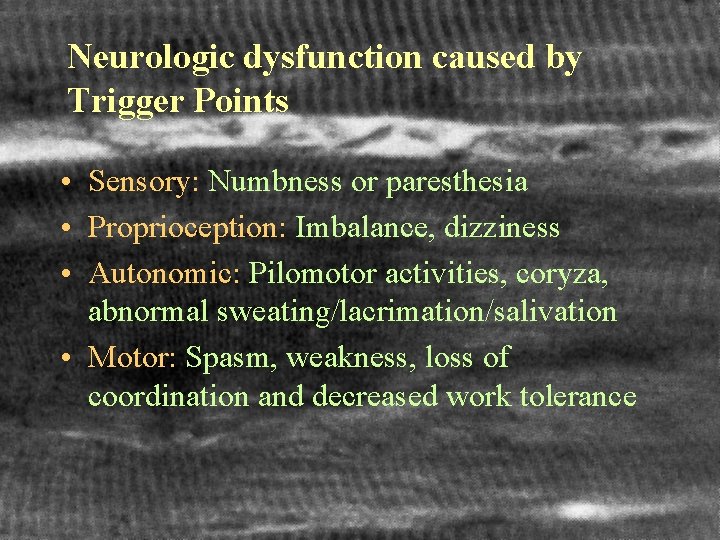
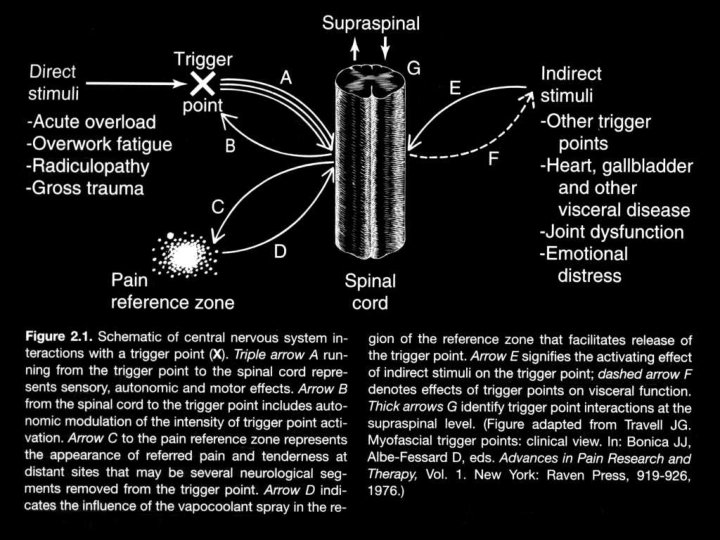
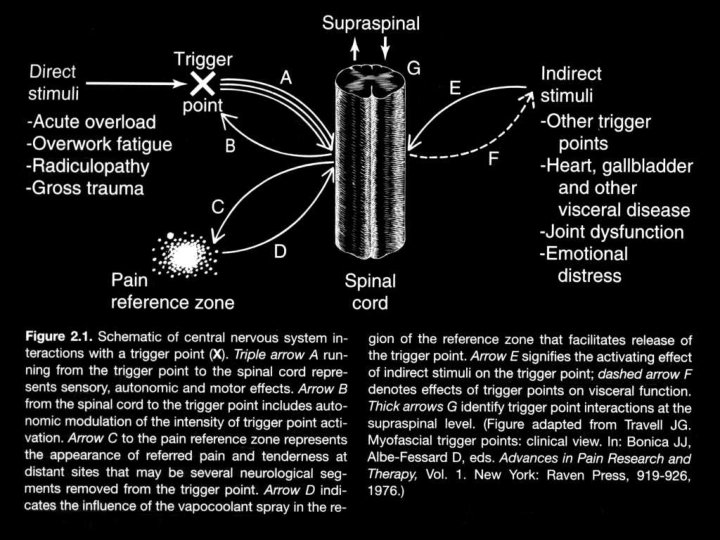
Neurologic dysfunction caused by Trigger Points • Sensory: Numbness or paresthesia • Proprioception: Imbalance, dizziness • Autonomic: Pilomotor activities, coryza, abnormal sweating/lacrimation/salivation • Motor: Spasm, weakness, loss of coordination and decreased work tolerance
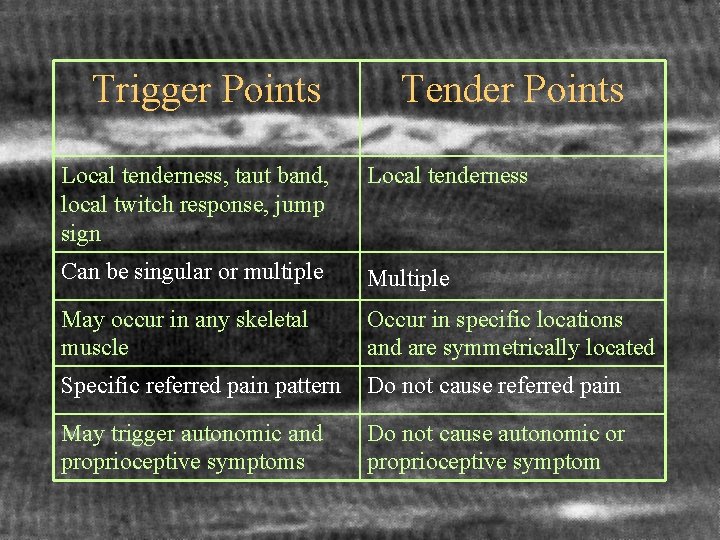
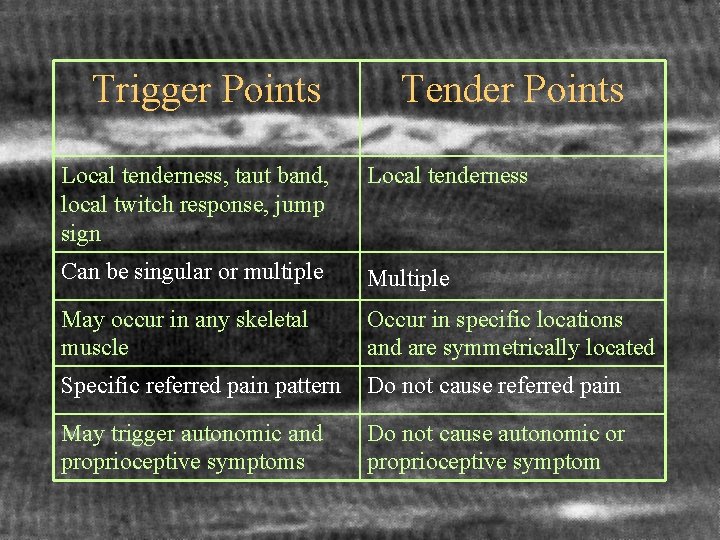
Trigger Points Tender Points Local tenderness, taut band, local twitch response, jump sign Local tenderness Can be singular or multiple May occur in any skeletal muscle Occur in specific locations and are symmetrically located Specific referred pain pattern Do not cause referred pain May trigger autonomic and proprioceptive symptoms Do not cause autonomic or proprioceptive symptom
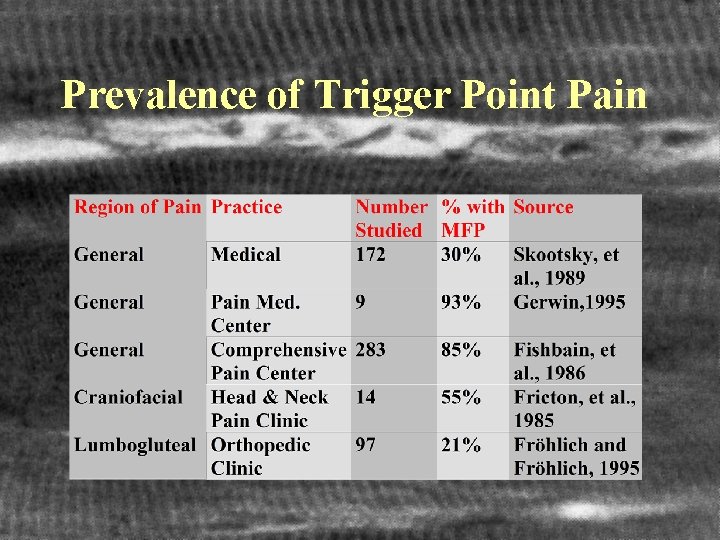
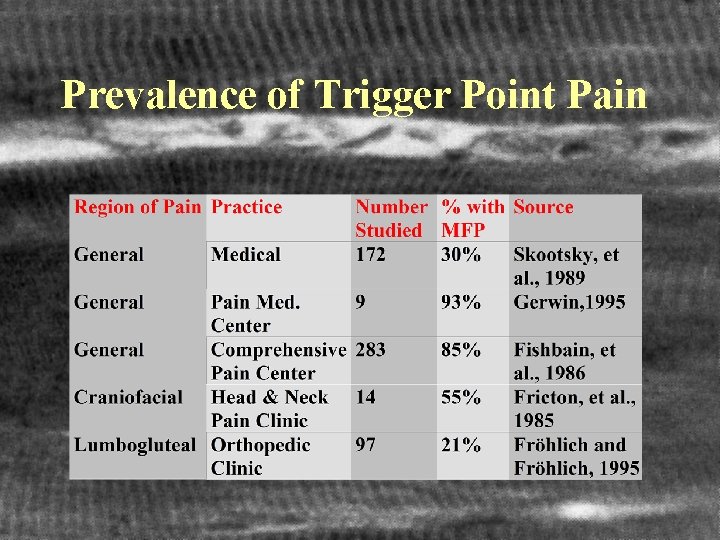
Prevalence of Trigger Point Pain
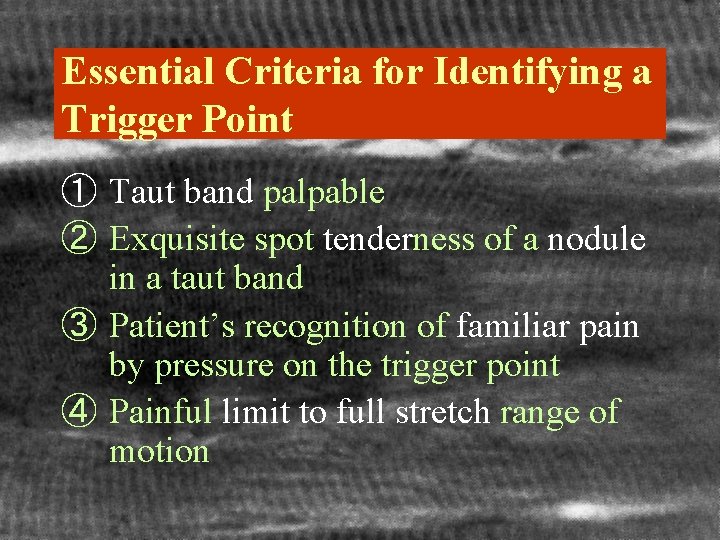
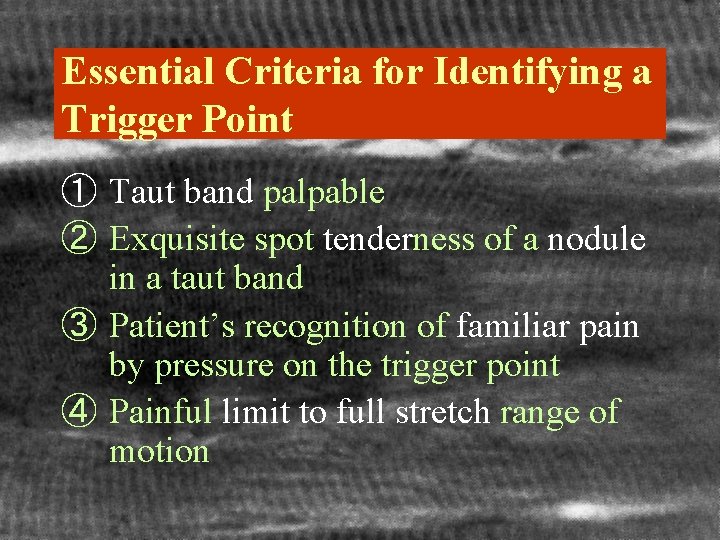
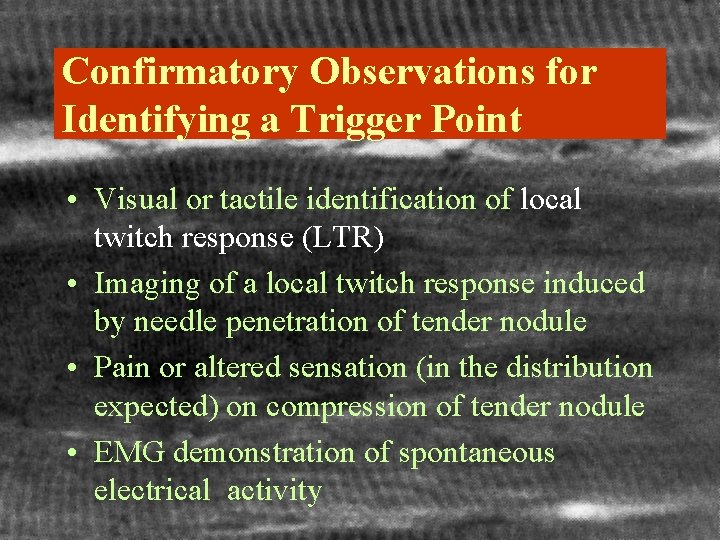
Essential Criteria for Identifying a Trigger Point ① Taut band palpable ② Exquisite spot tenderness of a nodule in a taut band ③ Patient’s recognition of familiar pain by pressure on the trigger point ④ Painful limit to full stretch range of motion
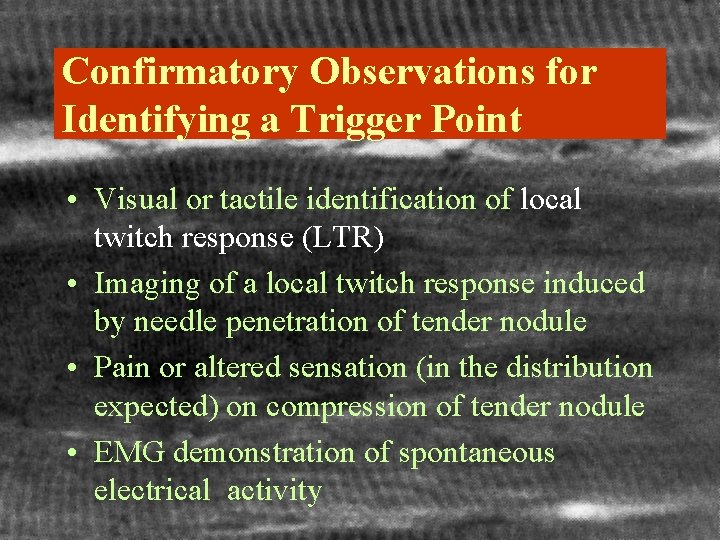
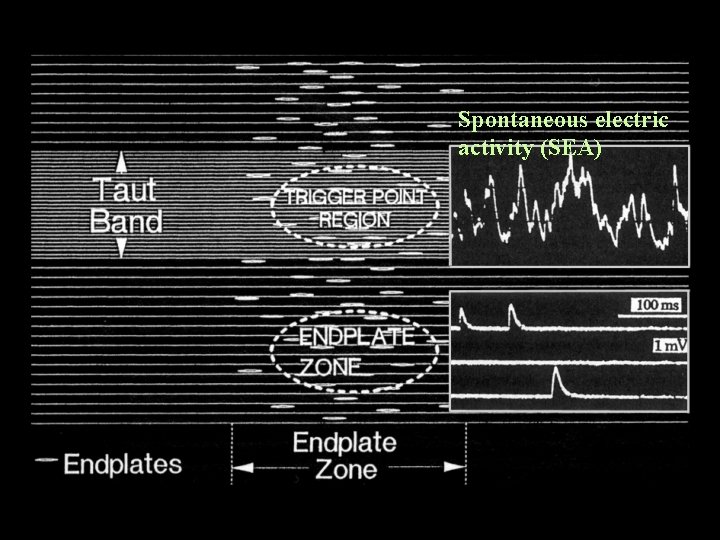
Confirmatory Observations for Identifying a Trigger Point • Visual or tactile identification of local twitch response (LTR) • Imaging of a local twitch response induced by needle penetration of tender nodule • Pain or altered sensation (in the distribution expected) on compression of tender nodule • EMG demonstration of spontaneous electrical activity
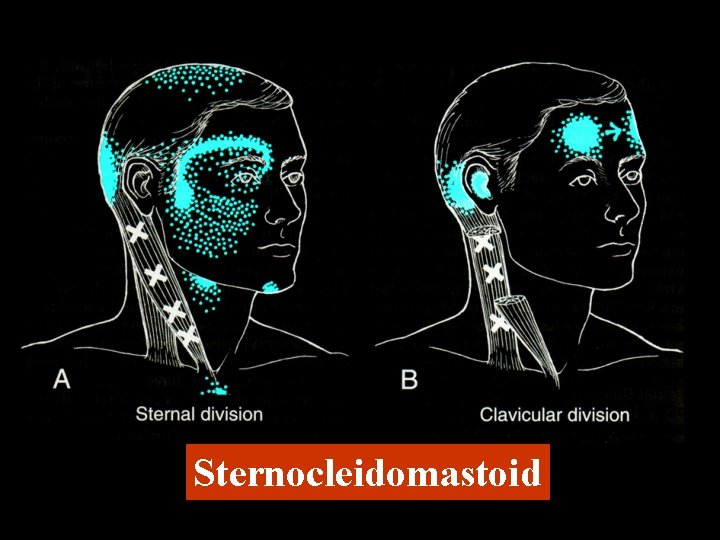
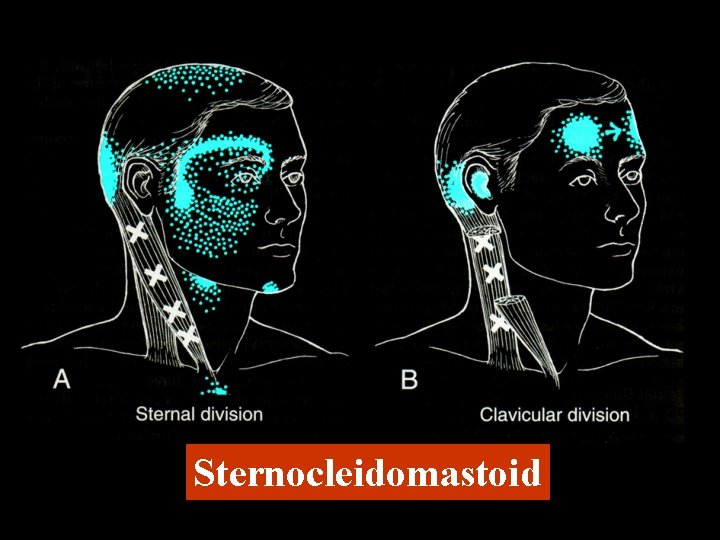
Sternocleidomastoid
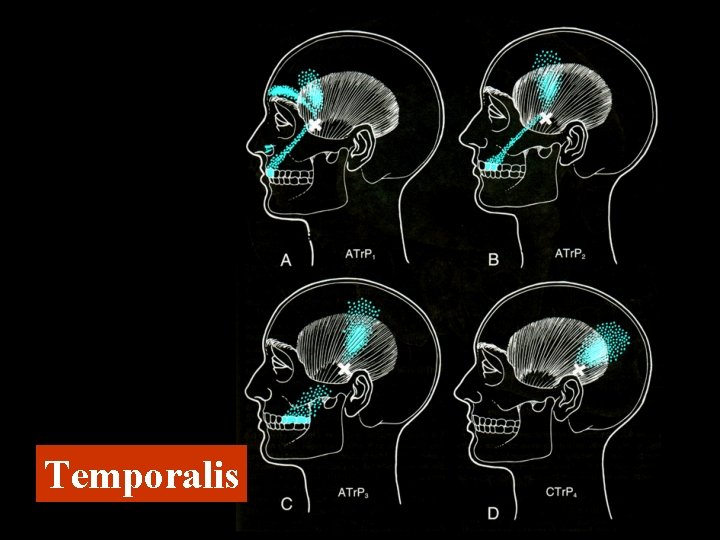
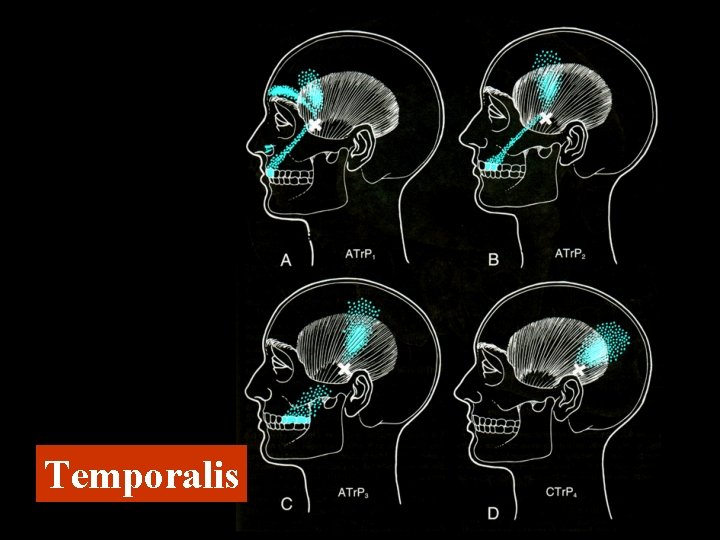
Temporalis
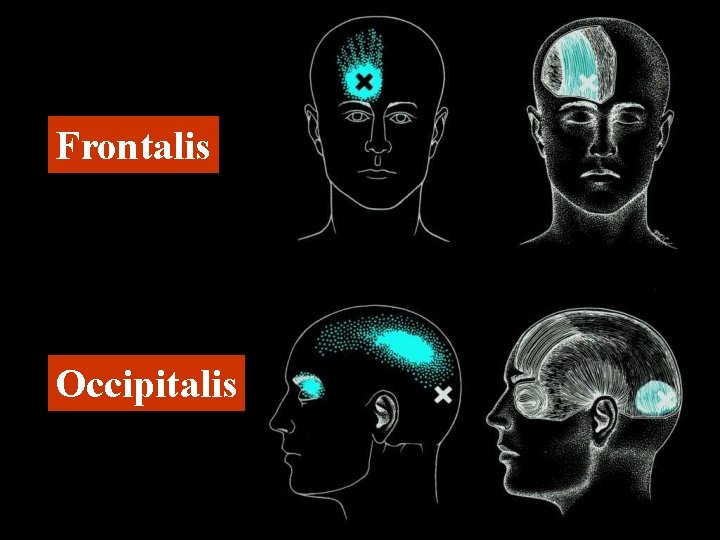
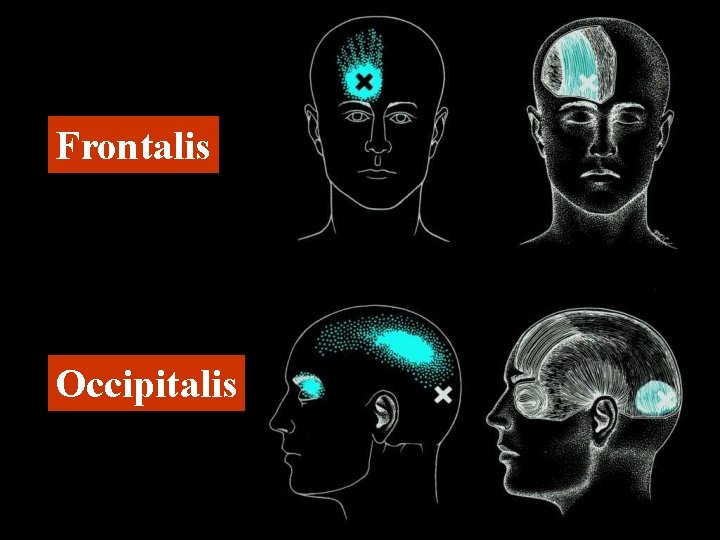
Frontalis Occipitalis
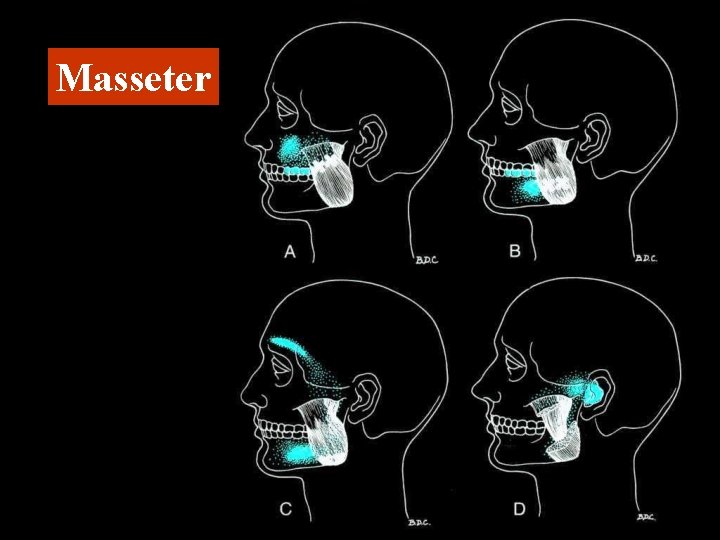
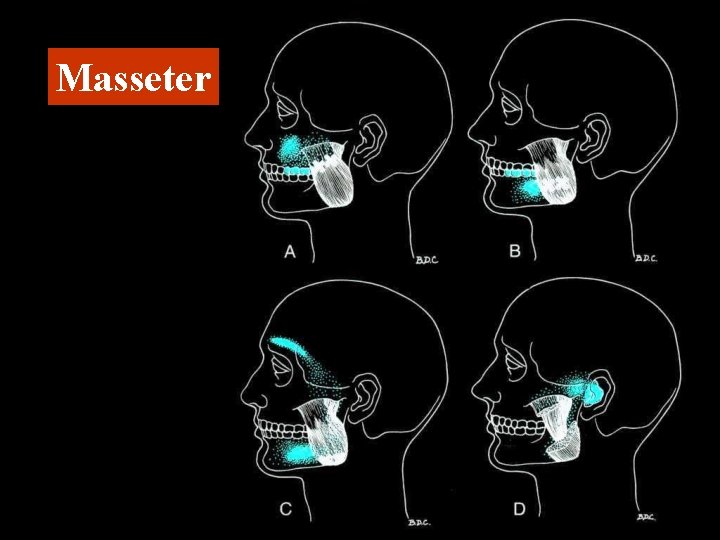
Masseter
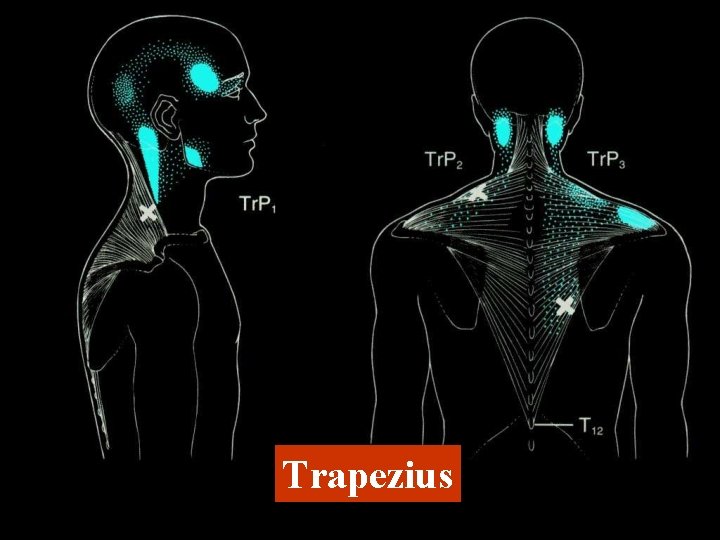
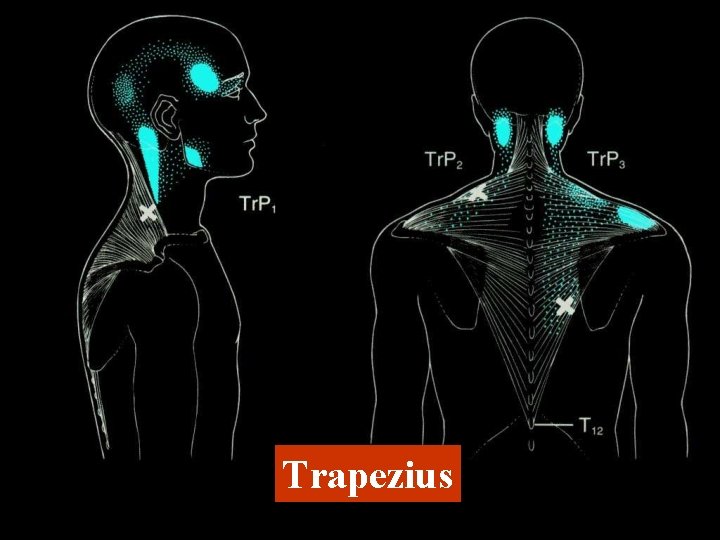
Trapezius
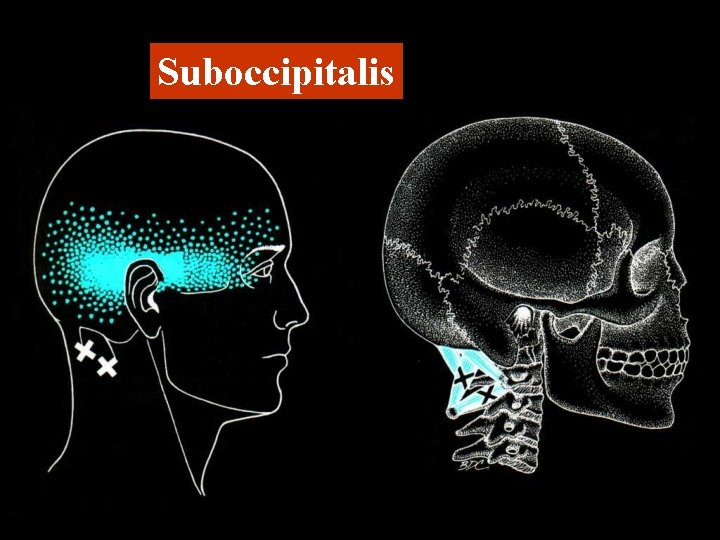
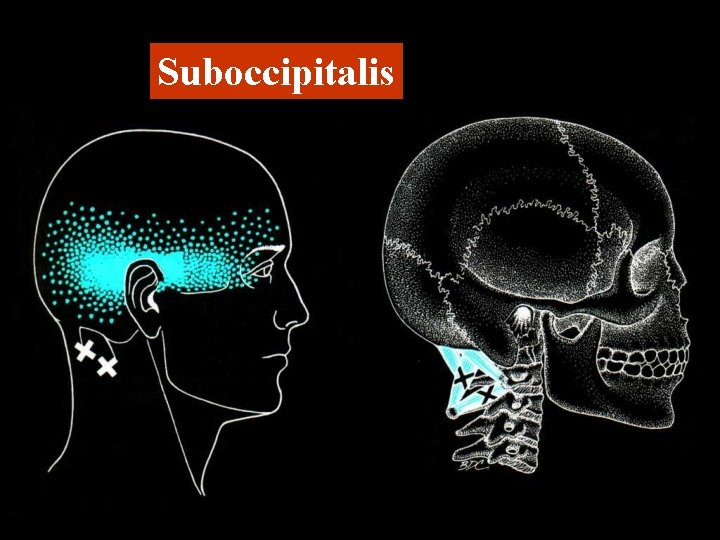
Suboccipitalis
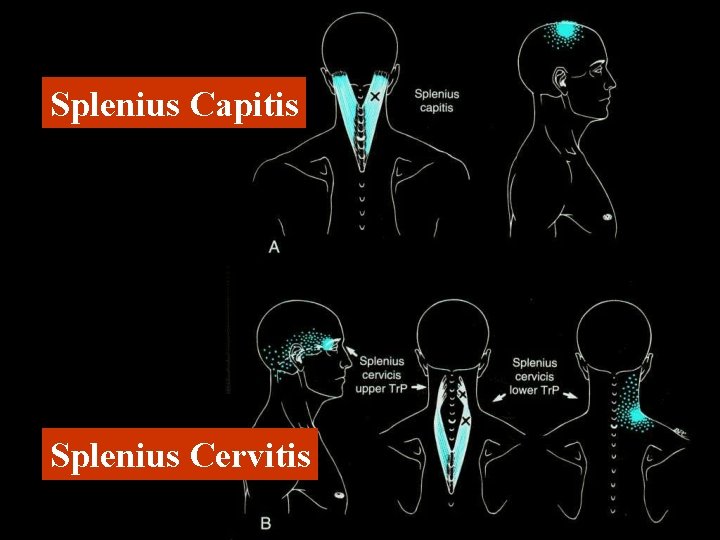
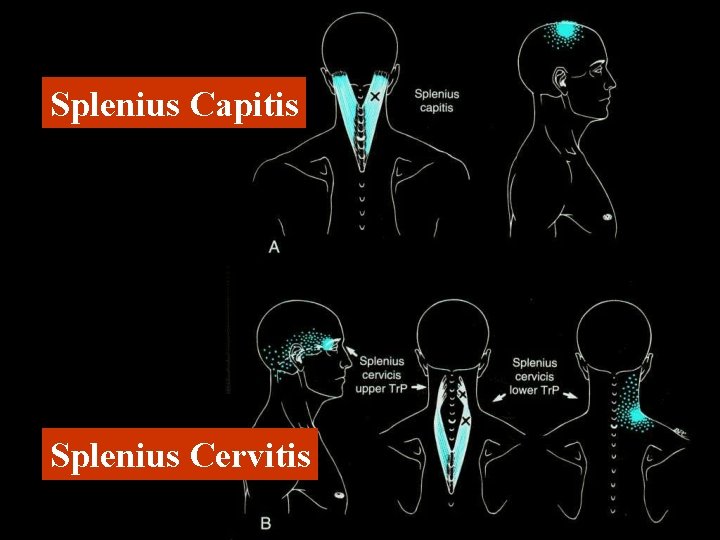
Splenius Capitis Splenius Cervitis
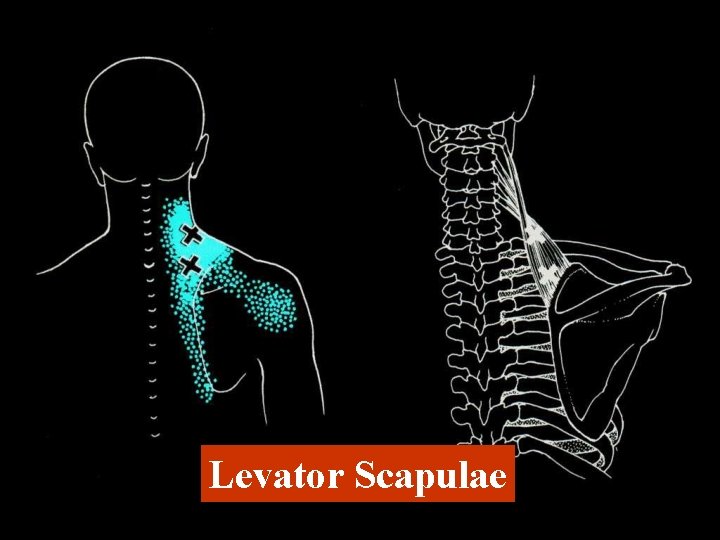
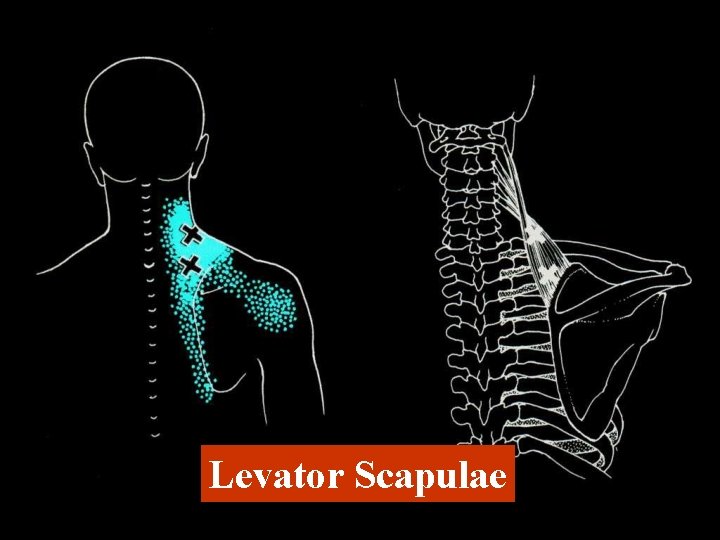
Levator Scapulae



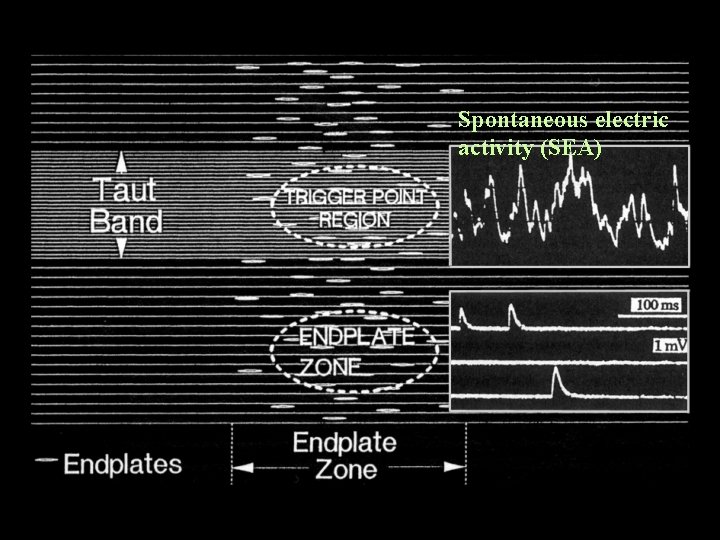
Spontaneous electric activity (SEA)


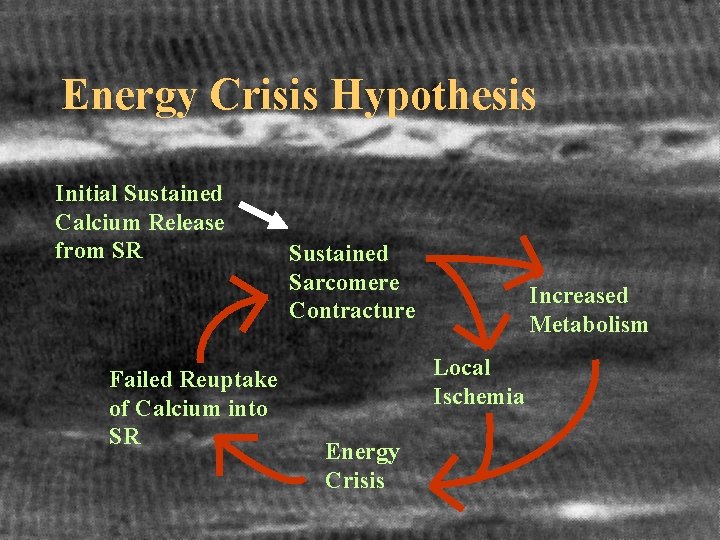
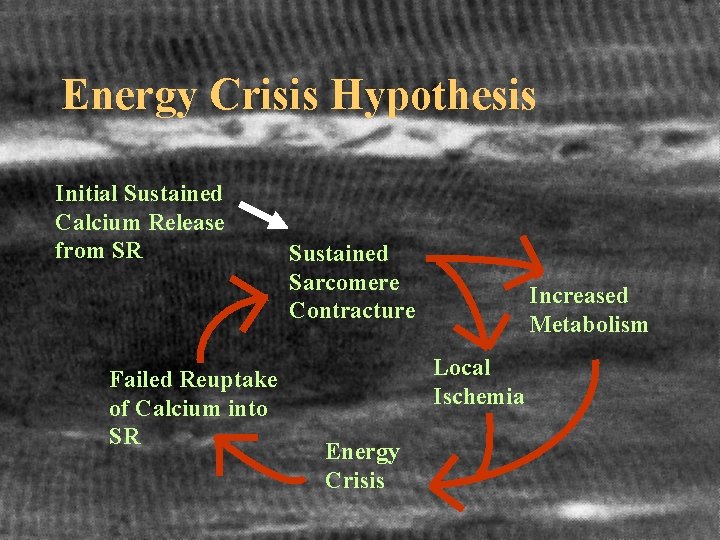
Energy Crisis Hypothesis Initial Sustained Calcium Release from SR Failed Reuptake of Calcium into SR Sustained Sarcomere Contracture Increased Metabolism Local Ischemia Energy Crisis

Acute Vs Chronic Myofascial Tr. P Pain • Acute single muscle syndrome often revert spontaneously to pain-free latent Tr. P , but are subject to reactivation • Acute myofascial Tr. P pain syndromes with perpetuating factors sets the stage of development of secondary and satellite Tr. Ps if not properly treated
Categories of Trigger Points • Active Tr. Ps produce a familiar symptom when the Tr. P is digitally compressed • Latent Tr. Ps produce characteristics of a Tr. P but no spontaneous pain • An active key Tr. P in one muscle can induce an active satellite Tr. P in another muscle
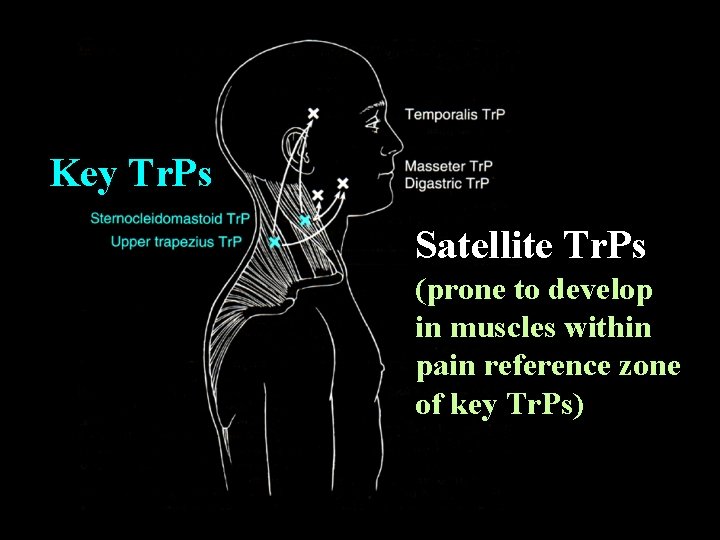
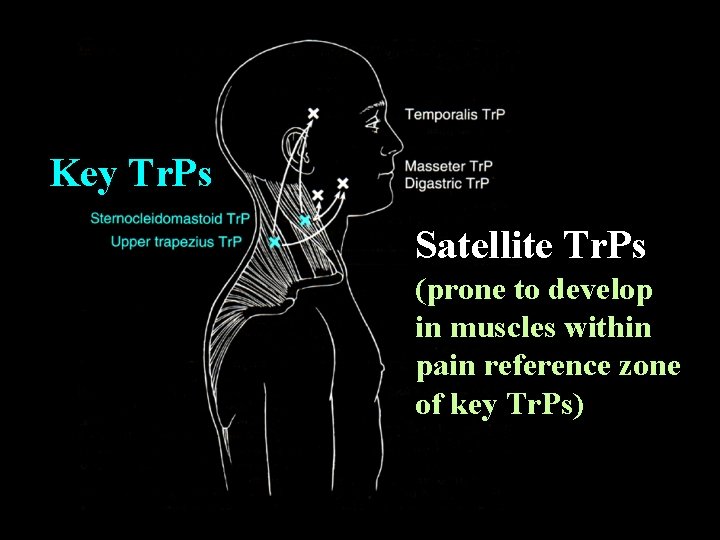
Key Tr. Ps Satellite Tr. Ps (prone to develop in muscles within pain reference zone of key Tr. Ps)
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head & Neck Region 1. To encourage patients to take an active role in the management 2. To ameliorate pain 3. To understand aggravating factors of myofascial Tr. P pain 4. To understand alleviating factors of myofascial Tr. P pain Go to Help (2)
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head & Neck Region 5. 6. 7. 8. To achieve physical fitness To improve sleep quality To express emotions To eliminate or modify possible perpetuating factors Jump into Conclusion
1. To encourage patients to take an active role in the management • Two Assumptions for Recurring Symptoms a. The patient is doing something (albeit unconsciously) to perpetuate the symptoms b. The patient is not doing something (albeit unconsciously) that would alleviate the symptoms Back to Help(1)
2. To Ameliorate Pain a. Medications b. Tr. P injections c. Nonpharmacologic interventions – – – Stretching exercise with phased respiration Moist heat or cold packing Trigger Point Pressure Release Massage Other physical therapy
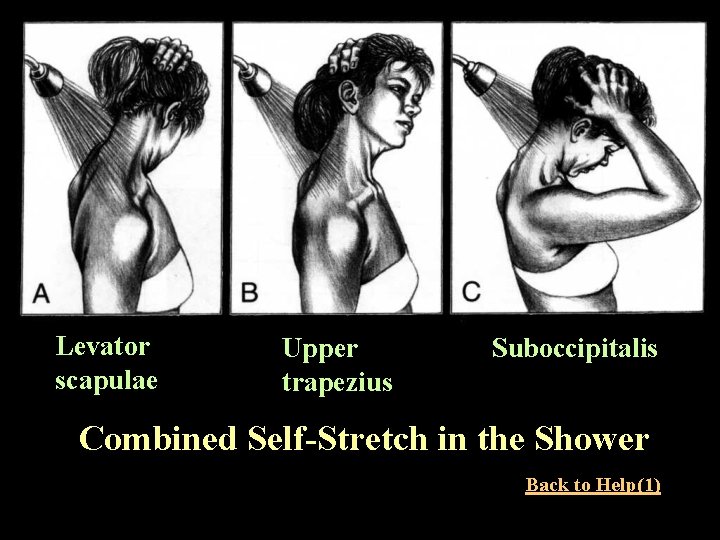
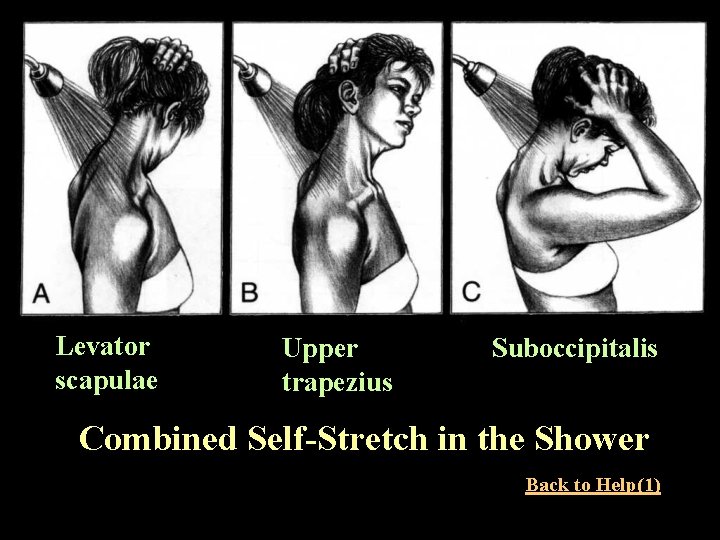
Levator scapulae Upper trapezius Suboccipitalis Combined Self-Stretch in the Shower Back to Help(1)
3. To Understand the Aggravating Factors of Myofascial Tr. P pain • • Sustained/repeated contraction of involved muscle Passive stretching muscle Pressure on Tr. P Placing involved muscle in shortened position for prolonged period • Cold, damp weather, viral infections, & periods of marked nervous tension • Exposure to cold draft, esp. when muscle is fatigue Back to Help(1)
4. To Understand the Alleviating Factors of Myofascial Tr. P pain • Specific myofascial therapy • Slow, steady passive stretching of involved muscles, particularly under a warm shower • Moist heat is applied over Tr. P • Short periods of light activity with movement • Short period of rest Back to Help(1)
5. To Achieve Physical Fitness • • Gradual increase of physical activities Increased sense of control Relaxation and antidepressant effect Following aerobic exercise, increase in βendorphin-like products, prolactin and growth hormone Go to Help (2)
6. To Improve Sleep Quality • • • Restless leg syndrome & periodic limb movements during sleep could be treated with dopaminergic drugs or clonazepam Tricyclic antidepressant and trazodone may be of help in both insomnia and pain management Treat rhinitis or asthma if exists Go to Help (2)
7. To Express Emotions • Relaxation via recreation is vital to decrease stress and maintain health • Through art, pet, dance, horticulture, communication, etc Go to Help (2)
8. To eliminate or modify possible perpetuating factors a. b. c. d. e. f. g. Short upper arms Postural stress Nutritional Inadequacies Metabolic & endocrine factors Psychological factors Temporomandibular joint disorders Comorbid illnesses Go to Help (2)
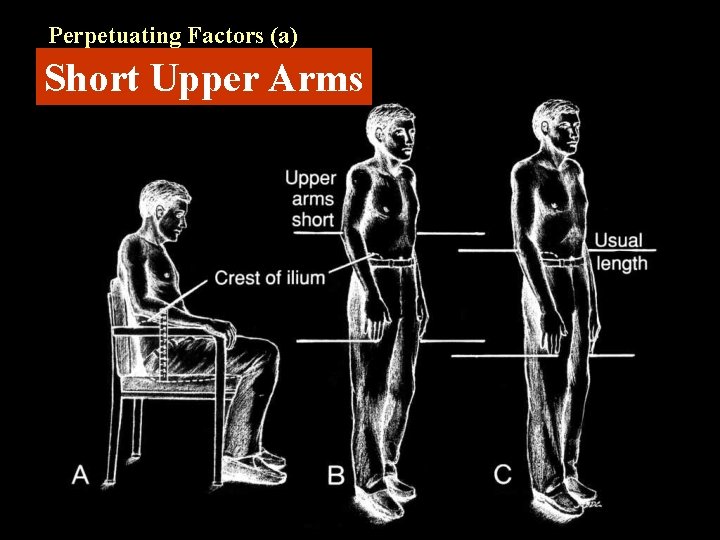
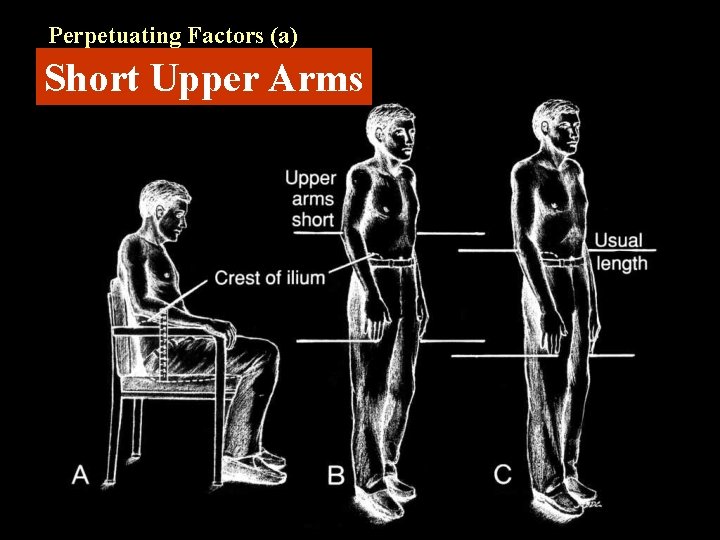
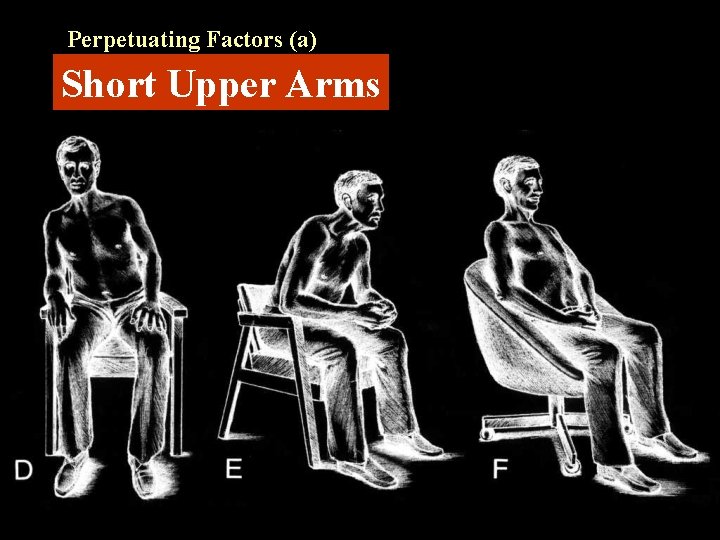
Perpetuating Factors (a) Short Upper Arms
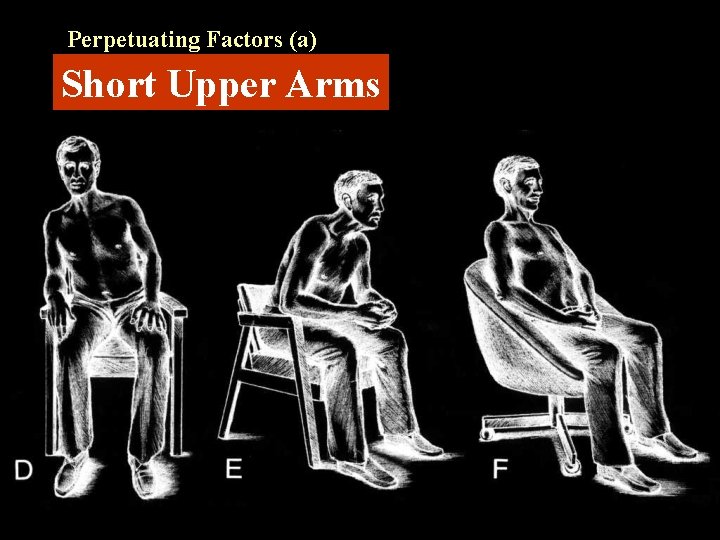
Perpetuating Factors (a) Short Upper Arms
Back to Perpetuating Factors
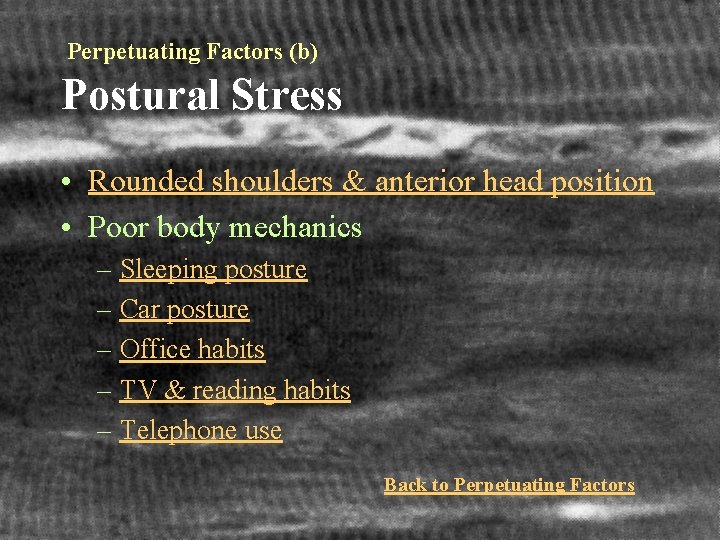
Perpetuating Factors (b) Postural Stress • Rounded shoulders & anterior head position • Poor body mechanics – Sleeping posture – Car posture – Office habits – TV & reading habits – Telephone use Back to Perpetuating Factors
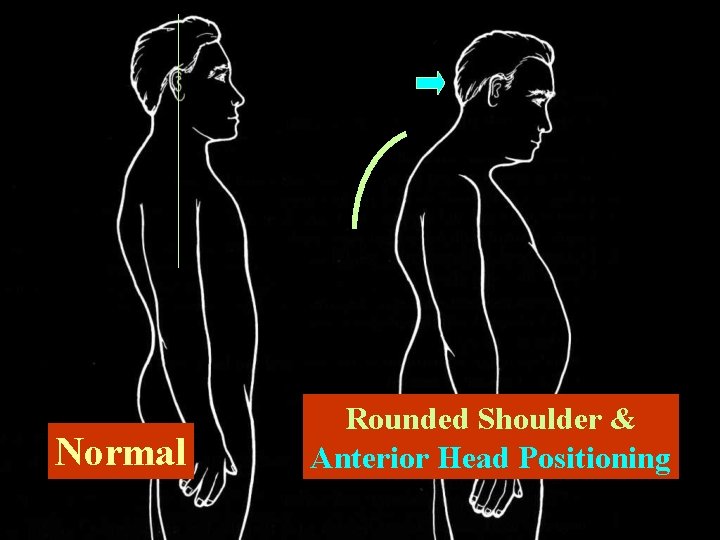
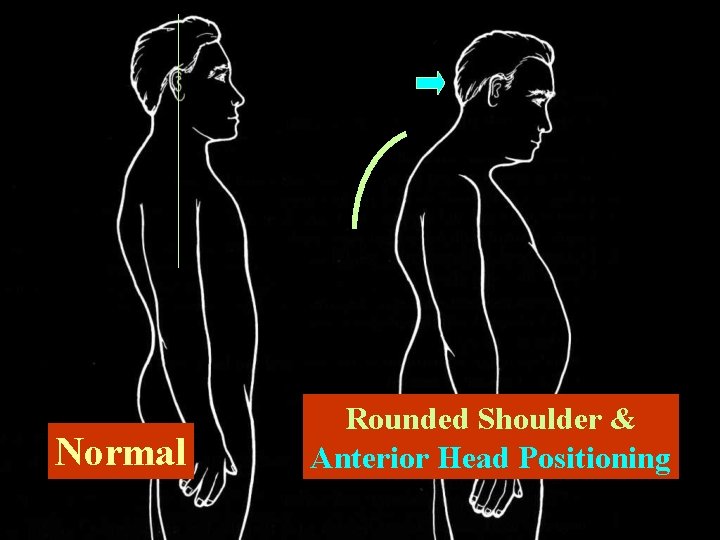
Normal Rounded Shoulder & Anterior Head Positioning
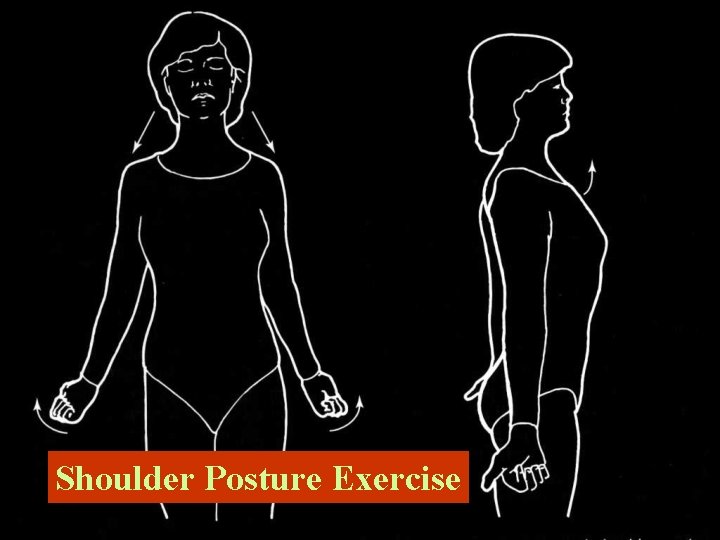
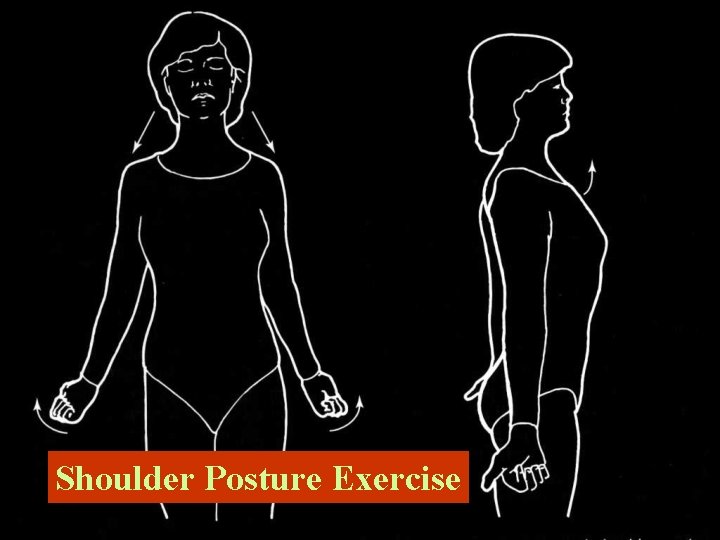
Shoulder Posture Exercise
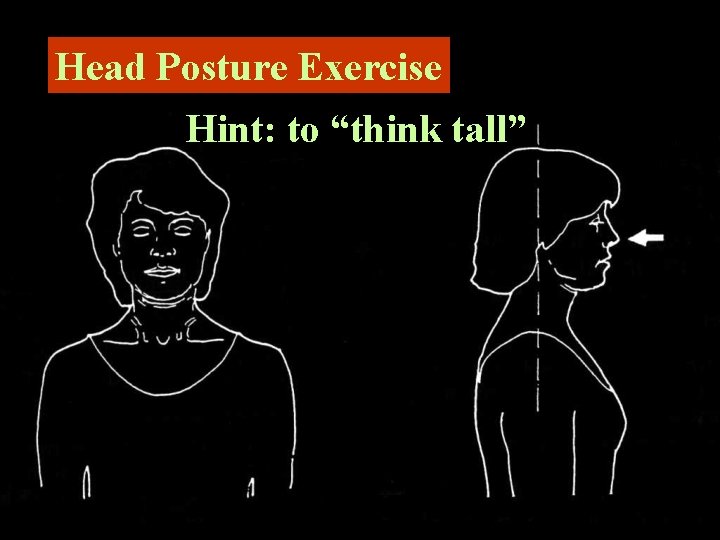
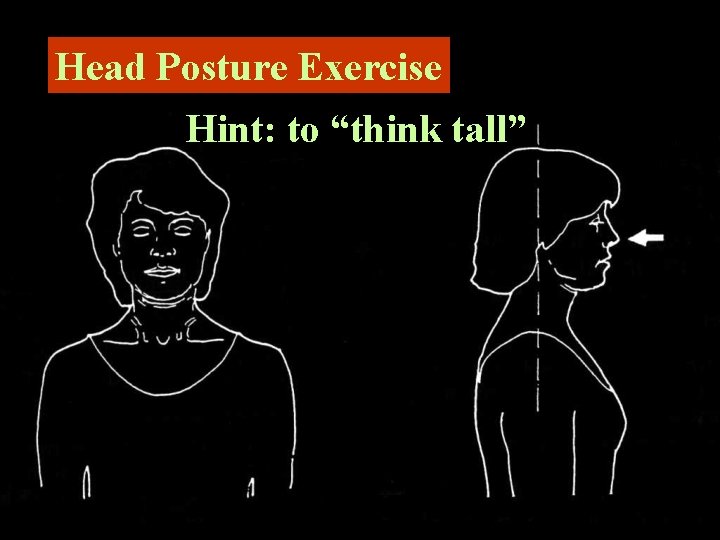
Head Posture Exercise Hint: to “think tall”

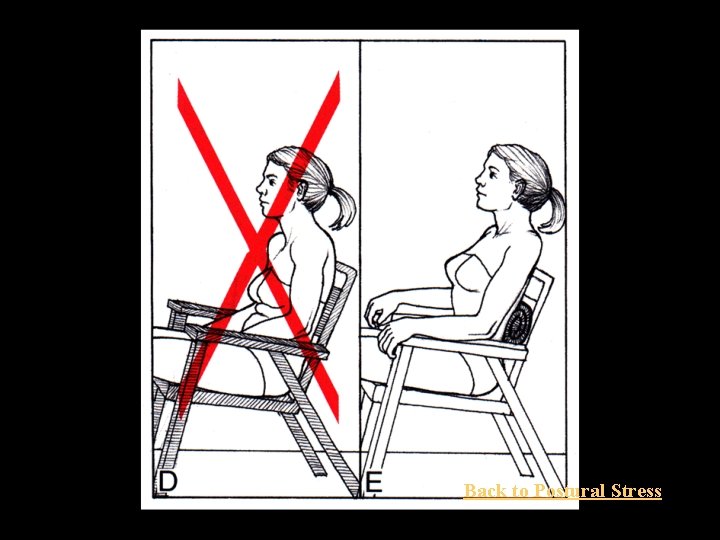
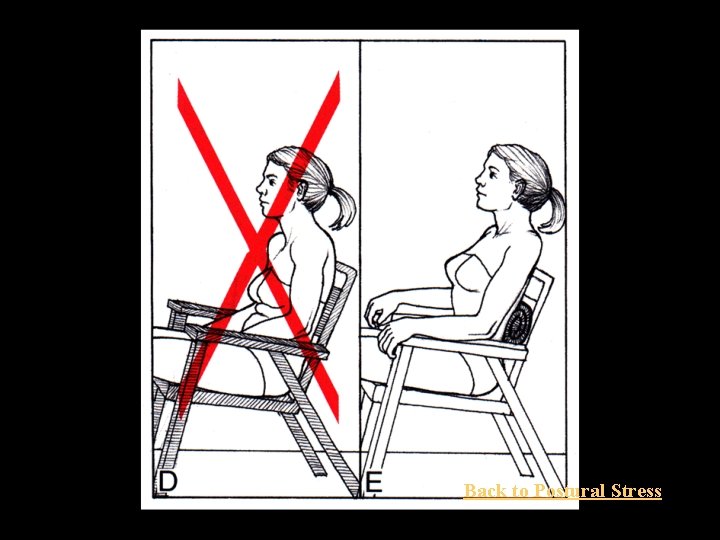
Back to Postural Stress
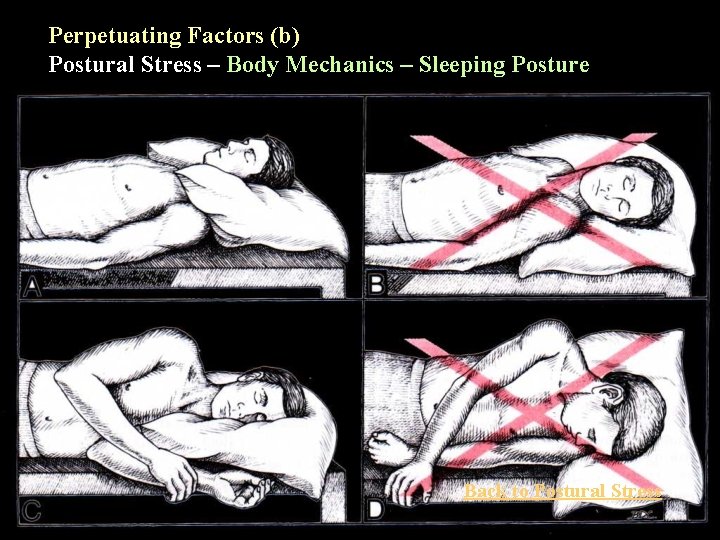
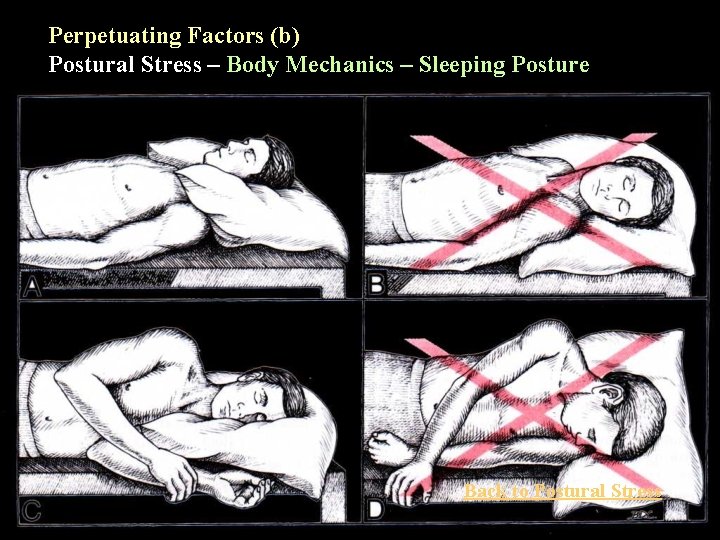
Perpetuating Factors (b) Postural Stress – Body Mechanics – Sleeping Posture Back to Postural Stress
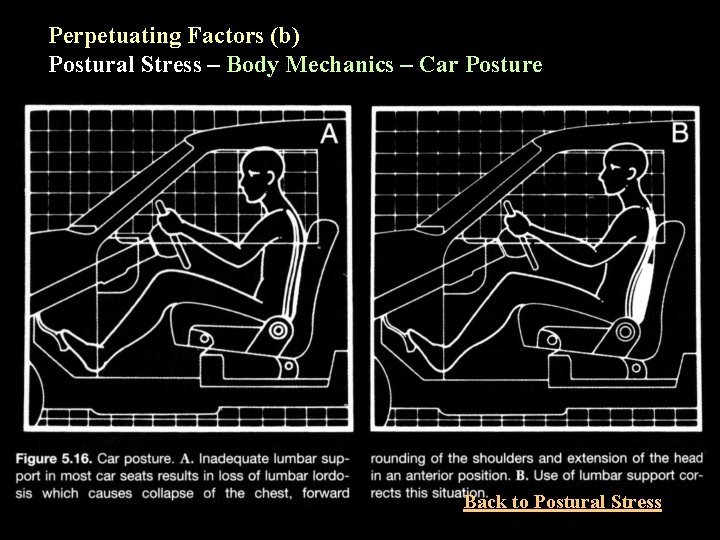
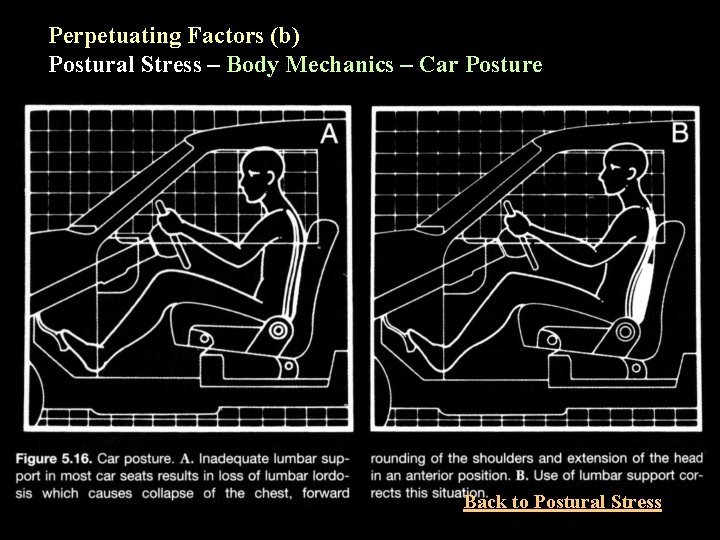
Perpetuating Factors (b) Postural Stress – Body Mechanics – Car Posture Back to Postural Stress
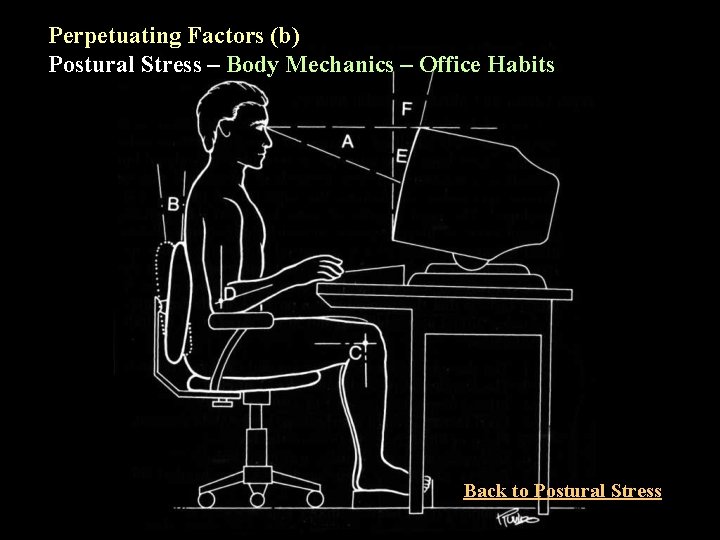
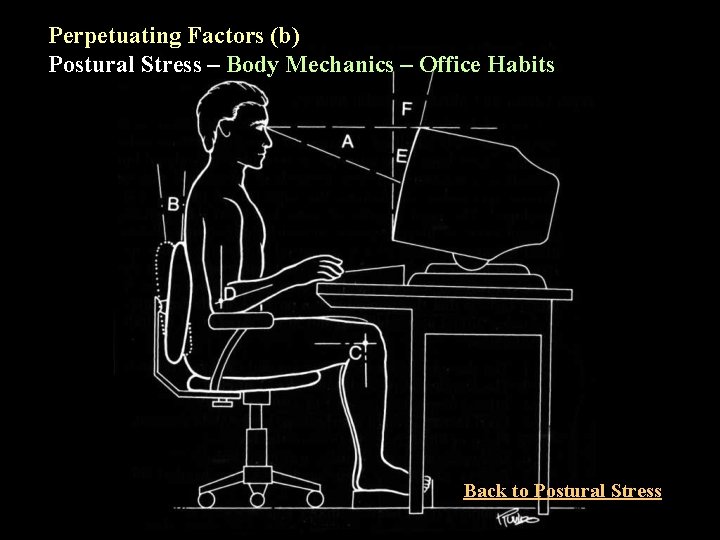
Perpetuating Factors (b) Postural Stress – Body Mechanics – Office Habits Back to Postural Stress
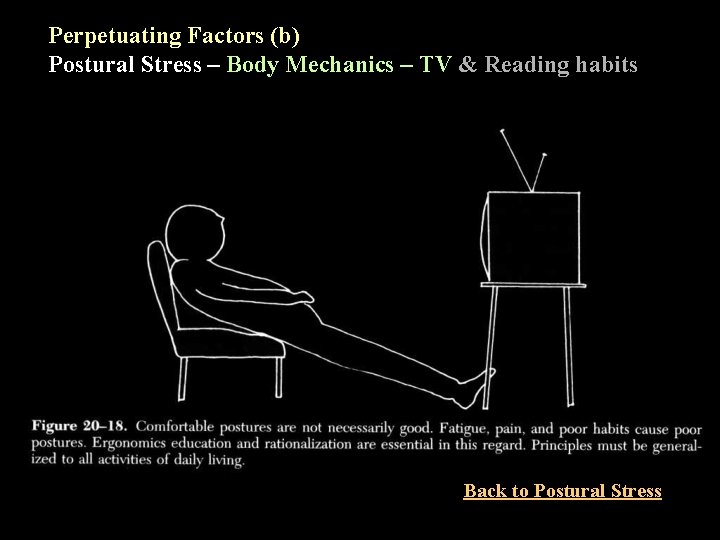
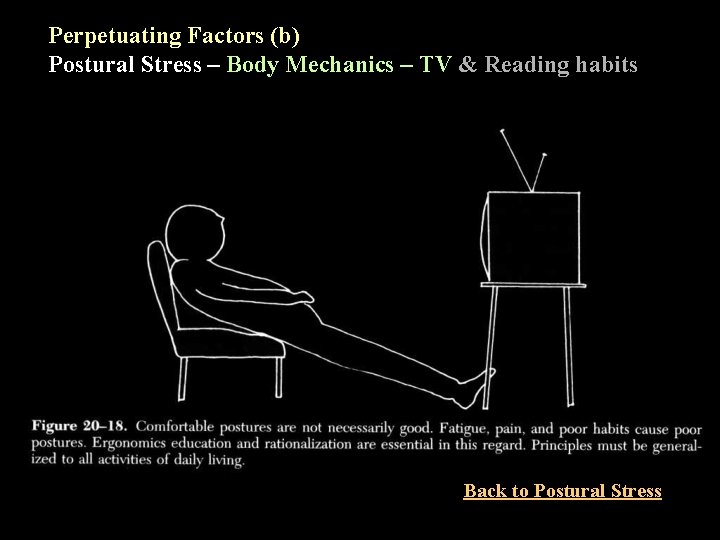
Perpetuating Factors (b) Postural Stress – Body Mechanics – TV & Reading habits Back to Postural Stress
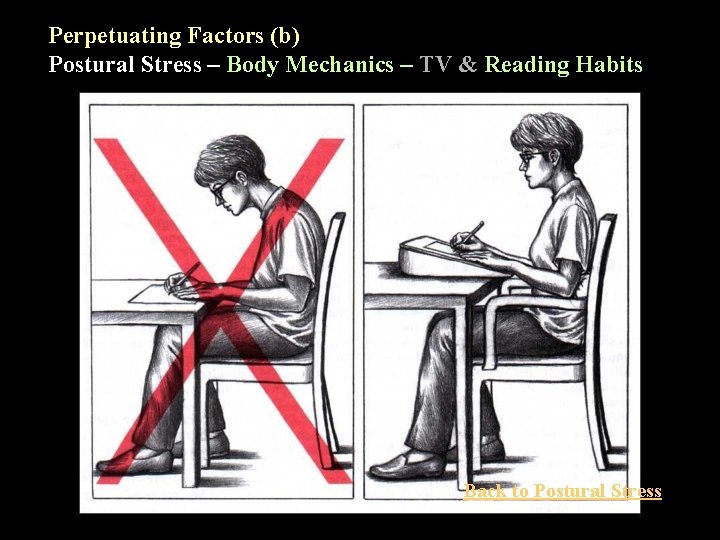
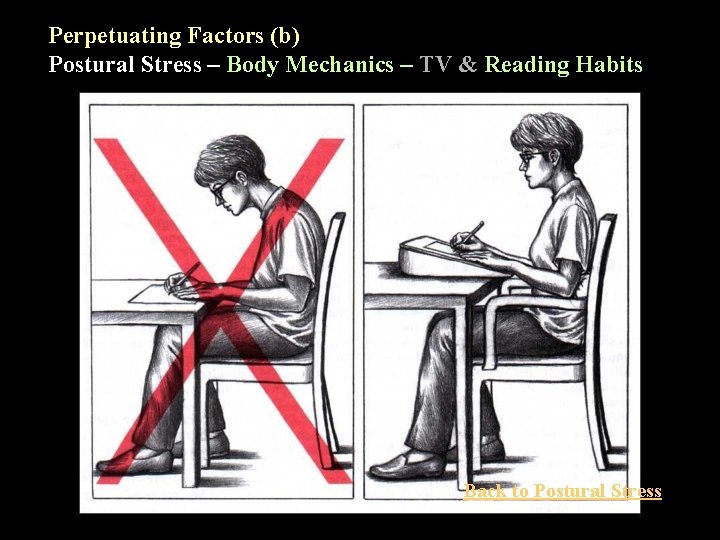
Perpetuating Factors (b) Postural Stress – Body Mechanics – TV & Reading Habits Back to Postural Stress
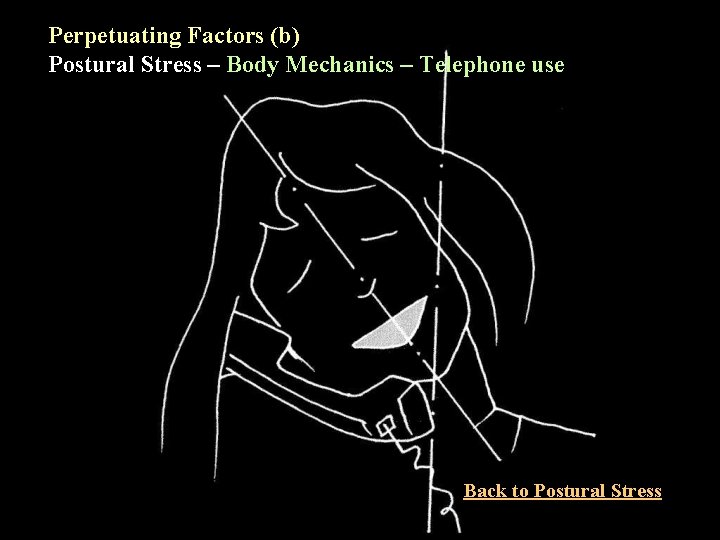
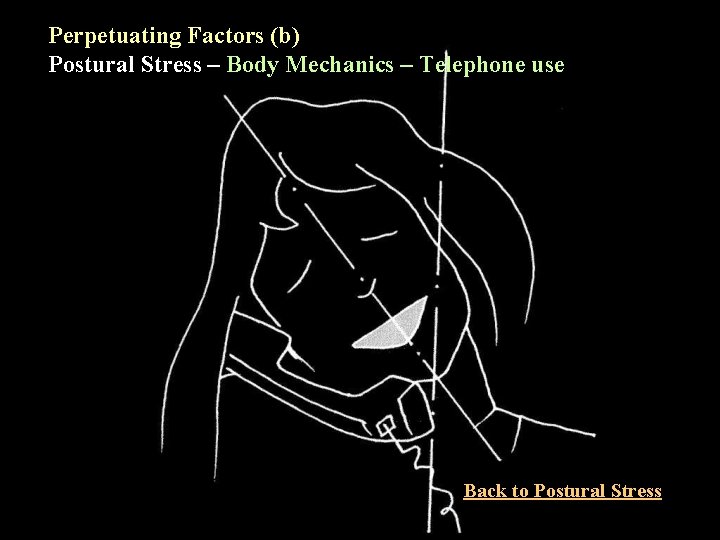
Perpetuating Factors (b) Postural Stress – Body Mechanics – Telephone use Back to Postural Stress
Perpetuating Factors (c) Nutritional Inadequacies • Patients with chronic myofascial pain has high prevalence of vitamin deficiencies • The five vitamins of special importance to myofascial pain syndromes are vitamins B 1, B 6, B 12, folic acid, and vitamin C • Iron, calcium, potassium, and magnesium, are needed for normal muscle function Back to Perpetuating Factors
Perpetuating Factors (d) Metabolic & Endocrine Factors • Myofascial Tr. Ps are aggravated or perpetuated in patients who have hypothyroidism, gouty diathesis, or hypoglycemic attacks Back to Perpetuating Factors
Perpetuating Factors (e) Psychological Factors • Physician must be careful not to assume that the psychological factors are primary – Hopelessness (Be careful with labels) – Depression – Anxiety & Tension – “Good Sport” Syndrome Back to Perpetuating Factors
Perpetuating Factors (f) Temporomandibular Joint Disorders • Screen for the followings – Joint capsule tenderness – Joint sounds – Mandibular range of motion • Common in patients with bruxism, habit of chewing betel nut, or evidence of notable occlusal wear Back to Perpetuating Factors
Perpetuating Factors (f) Comorbid Illnesses • Chronic infection & infestations – Viral Disease – Bacterial Infection (abscessed tooth, sinusitis, chronic UTI) – Infestations • Allergic rhinitis • Nerve impingement Back to Perpetuating Factors

Misconception (1) • Myofascial pain syndromes are self -limiting and will cure themselves.
Misconception (2) • The pain cannot be as severe as the patient says and must be largely psychogenic.
Misconception (3) • Simply treating the Tr. P should be sufficient
Misconception (4) • Relief of pain by treatment of skeletal muscles for myofascial Tr. Ps rules out serious visceral disease.
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head & Neck Region 1. To encourage patients to take an active role in the management 2. To ameliorate pain 3. To understand aggravating factors of myofascial Tr. P pain 4. To understand alleviating factors of myofascial Tr. P pain
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head & Neck Region 5. 6. 7. 8. To achieve physical fitness To improve sleep quality To express emotions To eliminate or modify possible perpetuating factors
8. To eliminate or modify possible perpetuating factors a. b. c. d. e. f. g. Short upper arms Postural stress Nutritional Inadequacies Metabolic & endocrine factors Psychological factors Temporomandibular joint disorders Comorbid illnesses
Each Physician is a Drug • With each encounter, a physician’s actions can – produce side effects – exhibit a duration of action – induce toxicity – be given in an overdose – be given in an underdose – or most of all … produce a placebo effect.
How to Help Patients with Chronic Myofascial Pain Syndrome of the Head and Neck Region • Some diseases are not curable, but all patient could be given help
 Myofascial release salisbury
Myofascial release salisbury Indication and contraindication of mobilization
Indication and contraindication of mobilization Eds
Eds Chronic pain definition
Chronic pain definition Chronic pain comorbidities
Chronic pain comorbidities Santa fe pain and spine
Santa fe pain and spine Some patients shout in pain while ______ an injection.
Some patients shout in pain while ______ an injection. Lewis mad pain and martian pain
Lewis mad pain and martian pain Symptoms before period
Symptoms before period Pms vs pregnancy
Pms vs pregnancy Help us help you
Help us help you Easy asl sentences
Easy asl sentences Spagetti poem
Spagetti poem Im being oppressed
Im being oppressed Help help chapter 1
Help help chapter 1 Self help and community help is the motto of
Self help and community help is the motto of Chronic sinusitis
Chronic sinusitis Chronic myeloid leukemia
Chronic myeloid leukemia Stigmata of chronic liver disease
Stigmata of chronic liver disease Site:slidetodoc.com
Site:slidetodoc.com Improving chronic illness care model
Improving chronic illness care model Chronic meningitis
Chronic meningitis Chronic rejection
Chronic rejection Nephrology near atwater
Nephrology near atwater Chronic unease safety
Chronic unease safety Chronic dacryocystitis
Chronic dacryocystitis Cardinal signs of inflammation
Cardinal signs of inflammation Chronic rejection
Chronic rejection Antianginal drugs classification
Antianginal drugs classification Chronic rejection
Chronic rejection Chronic care model definition
Chronic care model definition Chronic disease
Chronic disease Chronic respiratory alkalosis
Chronic respiratory alkalosis The meek customer
The meek customer Cld chronic liver disease
Cld chronic liver disease Wagner chronic care model 1998
Wagner chronic care model 1998 Gastritis
Gastritis Multiple chronic conditions chartbook
Multiple chronic conditions chartbook Hepatitis causes
Hepatitis causes Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Morphological patterns of acute inflammation
Morphological patterns of acute inflammation Myalgic encephalomyelitis
Myalgic encephalomyelitis Chronic rejection
Chronic rejection Chronic hepatitis
Chronic hepatitis Dacryocystectomy steps
Dacryocystectomy steps Developed by ed
Developed by ed Chronic inducible urticaria
Chronic inducible urticaria Treatment of cml
Treatment of cml Chronic medication service
Chronic medication service Chronic care solutions
Chronic care solutions Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Chronic meningitis
Chronic meningitis Chronic rejection
Chronic rejection Hetrotropia
Hetrotropia Icd 10 code for seasonal allergies unspecified
Icd 10 code for seasonal allergies unspecified Chronic meningitis
Chronic meningitis Lll leukemia
Lll leukemia Pathophysiology of cholelithiasis ppt
Pathophysiology of cholelithiasis ppt Pathology
Pathology Chronic care
Chronic care Kate lorig stanford
Kate lorig stanford Chronic rejection
Chronic rejection Kronfeld mountain pass theory
Kronfeld mountain pass theory Acg pancreatitis
Acg pancreatitis Chronic inflammation
Chronic inflammation Angioectasia icd 10
Angioectasia icd 10 Chronic myeloid leukemia
Chronic myeloid leukemia Causes of secretory diarrhea
Causes of secretory diarrhea Nursing diagnosis for pancreatitis
Nursing diagnosis for pancreatitis Carlee oakley
Carlee oakley Chronic misbehavior
Chronic misbehavior Periradicular disease definition
Periradicular disease definition Acute subacute chronic
Acute subacute chronic Respiratory acinus
Respiratory acinus Stigmata of chronic liver disease
Stigmata of chronic liver disease Patho
Patho Iceberg phenomenon
Iceberg phenomenon