Infections of the Central Nervous System Stephen M











- Slides: 75
Infections of the Central Nervous System Stephen M. Kralovic, MD, MPH Professor of Medicine Division of Infectious Diseases, University of Cincinnati Hospital Epidemiologist, Cincinnati VA Medical Center February 3, 2018
Case 1 • HISTORY – 43 year old previously healthy white male – Intermittent fevers – Headache – Speech difficulties – Left arm and leg weakness – This has all occurred over a 5 -6 week period
Case 1 continued • PHYSICAL EXAM – – – Mildly obese No neck stiffness ( no Brudzhinski’s sign) Gingival retraction but no dental abscesses No skin lesions No lung or cardiac abnormalities 4/5 left arm and forearm (distal and proximal) weakness with 4+/5 left thigh weakness • LABS – Peripheral CBC w/ WBC 16, 200 (75% segs)
Case 1 continued • What do you think at this point? • Does the history give you any clues? • Do the physical exam findings suggest anything to you?
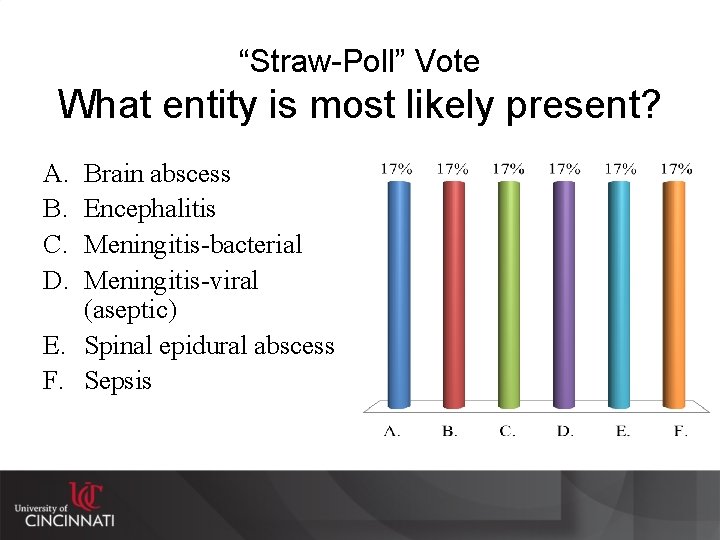
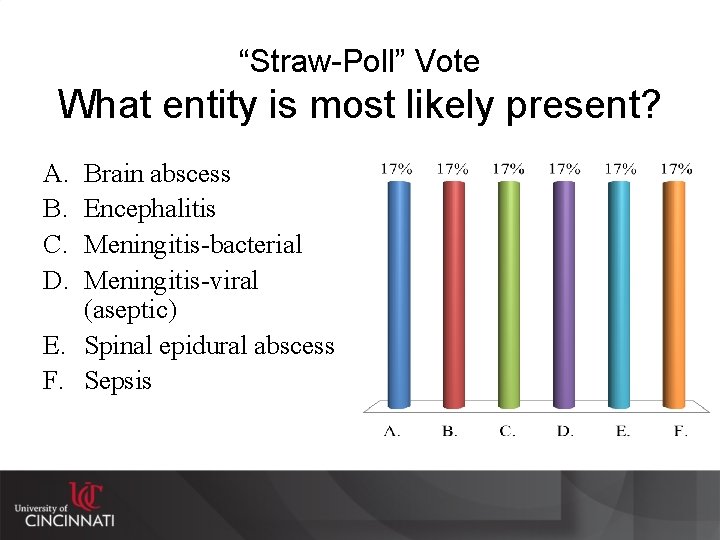
“Straw-Poll” Vote What entity is most likely present? A. B. C. D. Brain abscess Encephalitis Meningitis-bacterial Meningitis-viral (aseptic) E. Spinal epidural abscess F. Sepsis
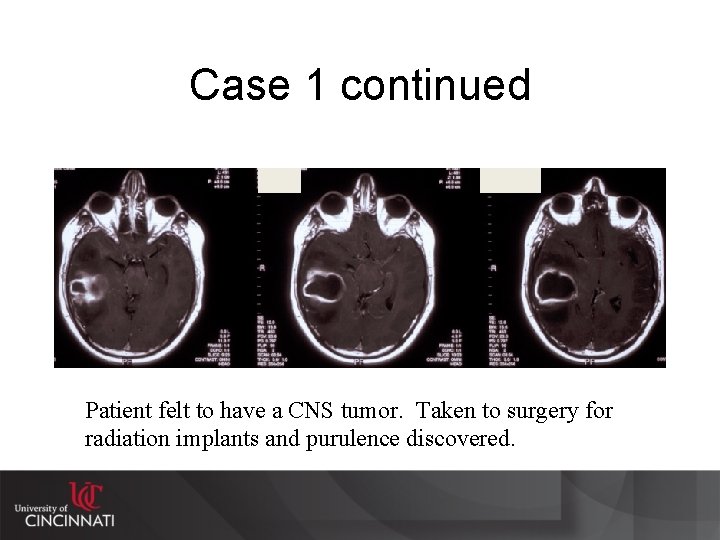
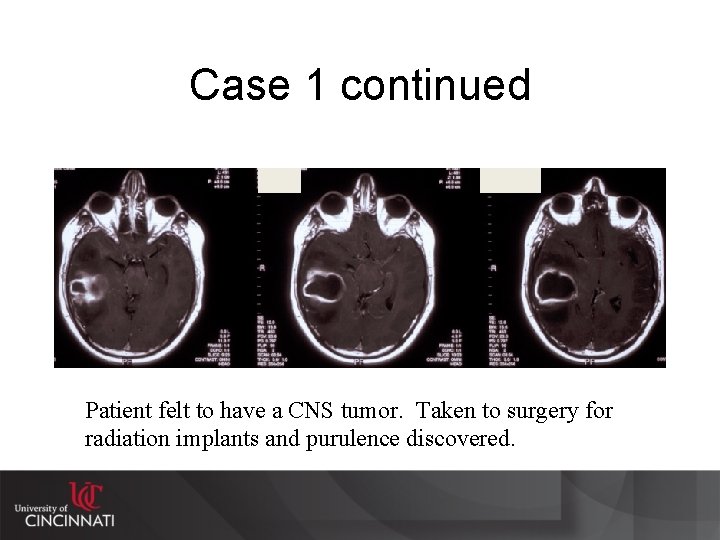
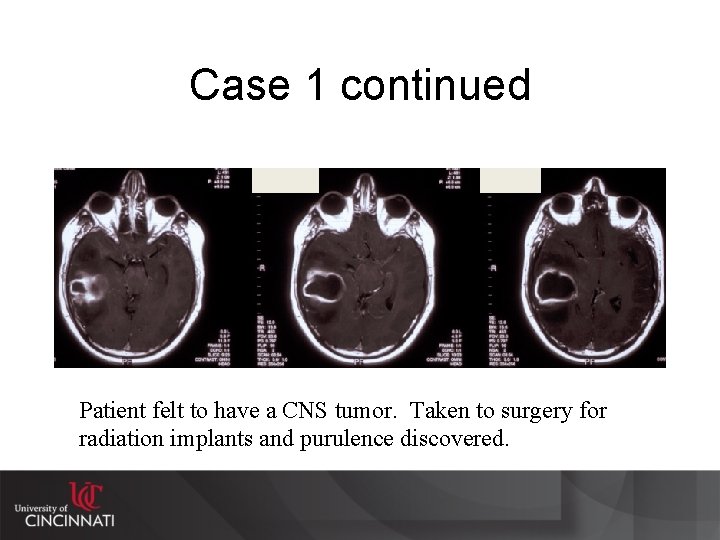
Case 1 continued Patient felt to have a CNS tumor. Taken to surgery for radiation implants and purulence discovered.
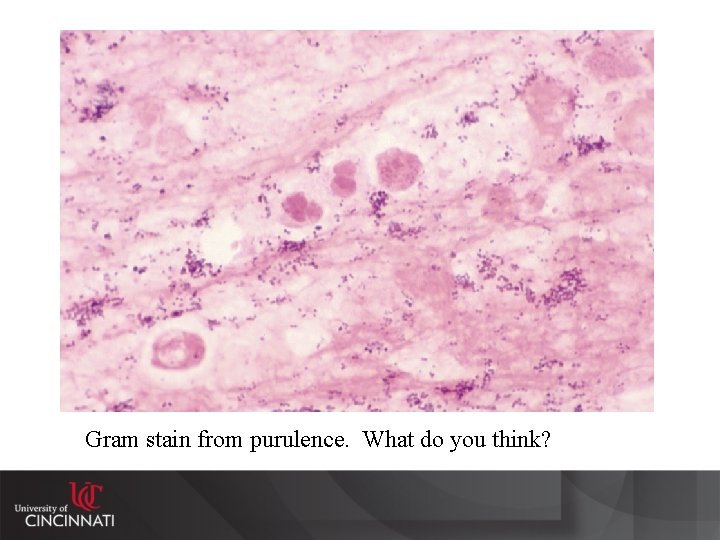
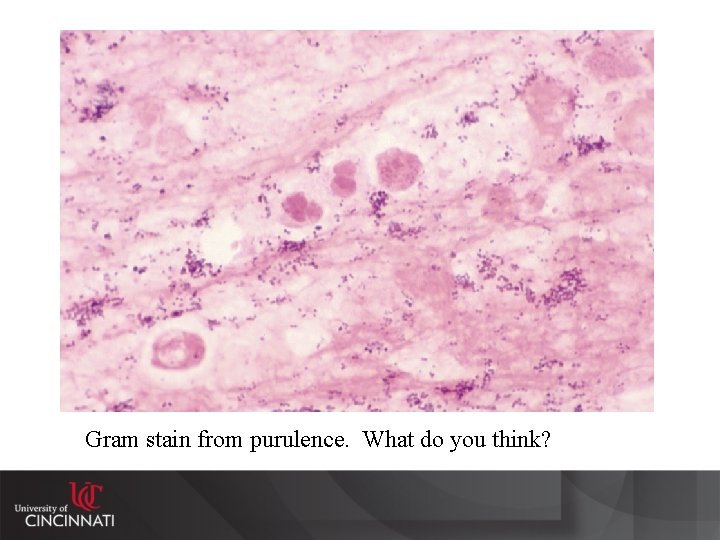
Gram stain from purulence. What do you think?
Case 2 • HISTORY – 70 year old woman – Hypertension, hyperlipidemia, h/o MI 10 years ago – Presents for confusion and erratic behavior over the last couple of days – Low grade fever according to her spouse – Agitated—which is unusual for this woman
Case 2 continued • PHYSICAL EXAMINATION – T=101. 2 o. F, HR=68, RR=16, BP=128/72 – Alert and oriented to self (A+Ox 1) – Nothing else specific on physical examination – No focal neurological deficits • LABS – Peripheral CBC (WBC=7, 500 w/61% segs)
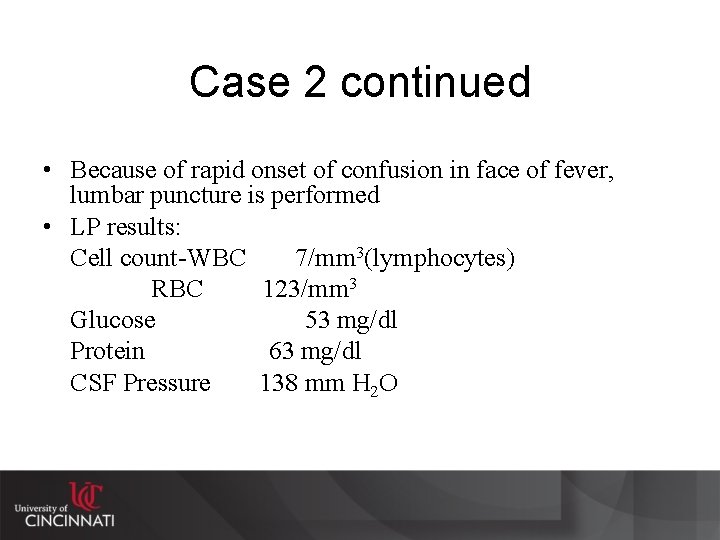
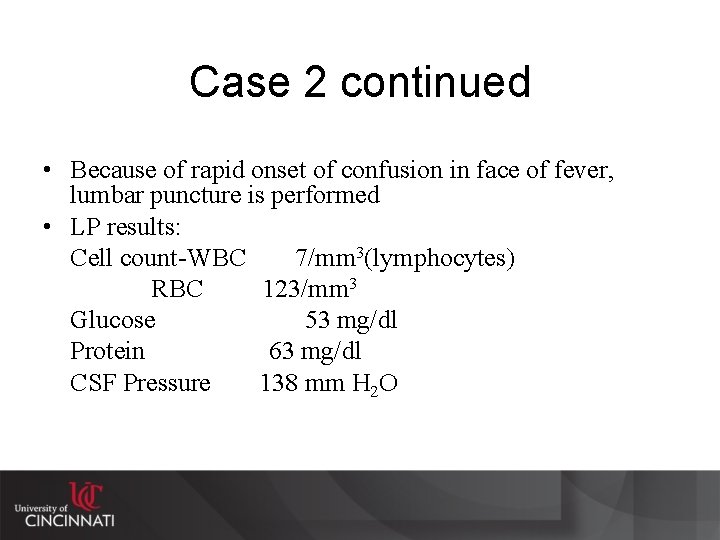
Case 2 continued • Because of rapid onset of confusion in face of fever, lumbar puncture is performed • LP results: Cell count-WBC 7/mm 3(lymphocytes) RBC 123/mm 3 Glucose 53 mg/dl Protein 63 mg/dl CSF Pressure 138 mm H 2 O
“Straw-Poll” Vote What entity is most likely present? A. B. C. D. Brain abscess Encephalitis Meningitis-bacterial Meningitis-viral (aseptic) E. Spinal epidural abscess F. Sepsis
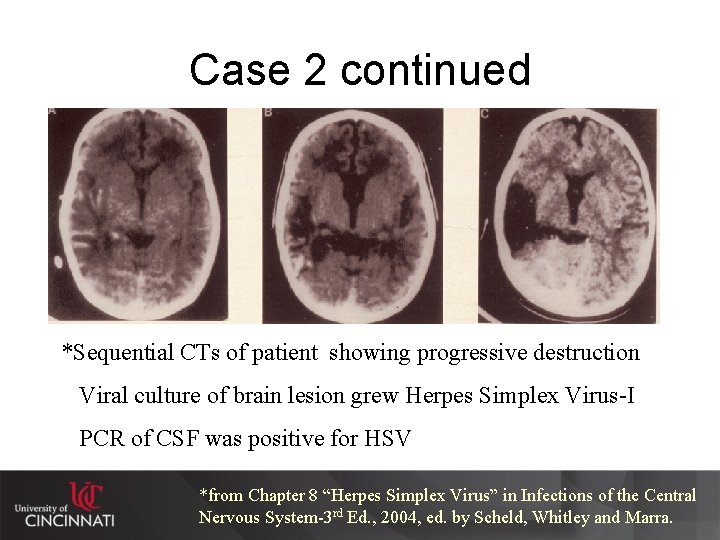
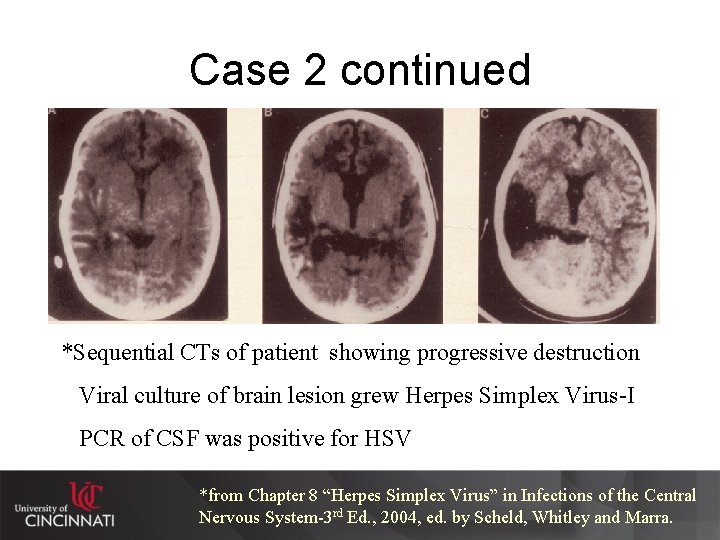
Case 2 continued *Sequential CTs of patient showing progressive destruction Viral culture of brain lesion grew Herpes Simplex Virus-I PCR of CSF was positive for HSV *from Chapter 8 “Herpes Simplex Virus” in Infections of the Central Nervous System-3 rd Ed. , 2004, ed. by Scheld, Whitley and Marra.
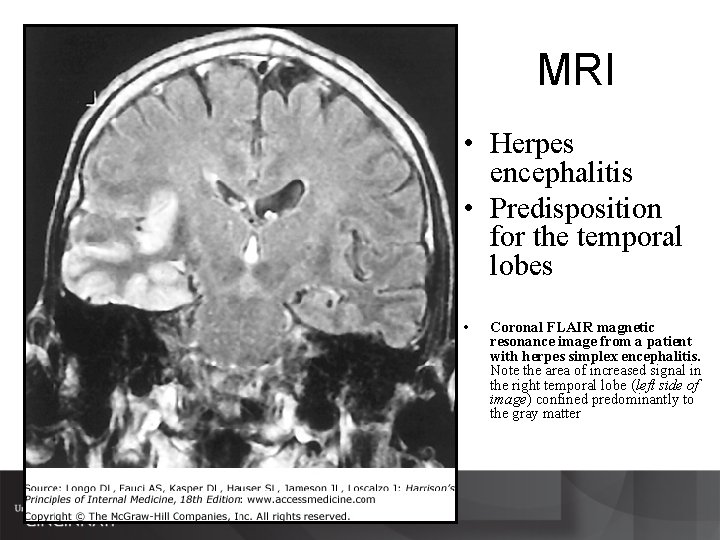
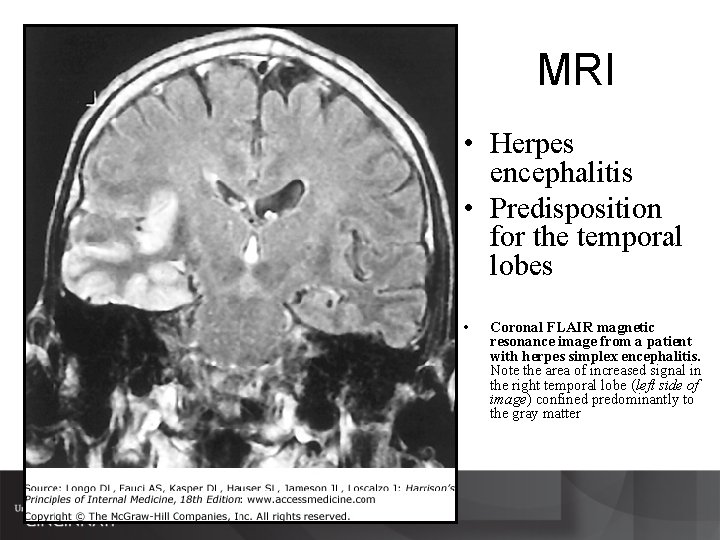
MRI • Herpes encephalitis • Predisposition for the temporal lobes • Coronal FLAIR magnetic resonance image from a patient with herpes simplex encephalitis. Note the area of increased signal in the right temporal lobe (left side of image) confined predominantly to the gray matter
Importance of History and Physical Examination • Give important clues as to whether infection is present or not • May give clues as the where or how infection was acquired – Trauma – Exposure • May give clues as to current location of infectious process • May give clues as to immune status of patient and risk for unusual (as well as usual) infections • Time of onset may give clues as to type of infection
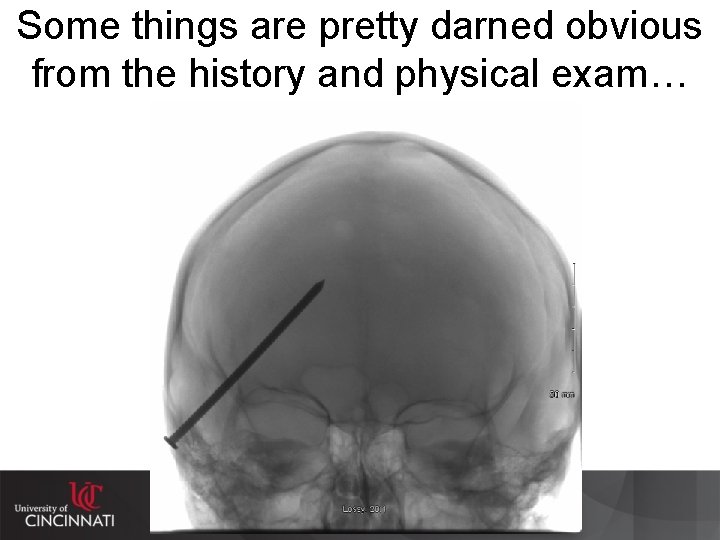
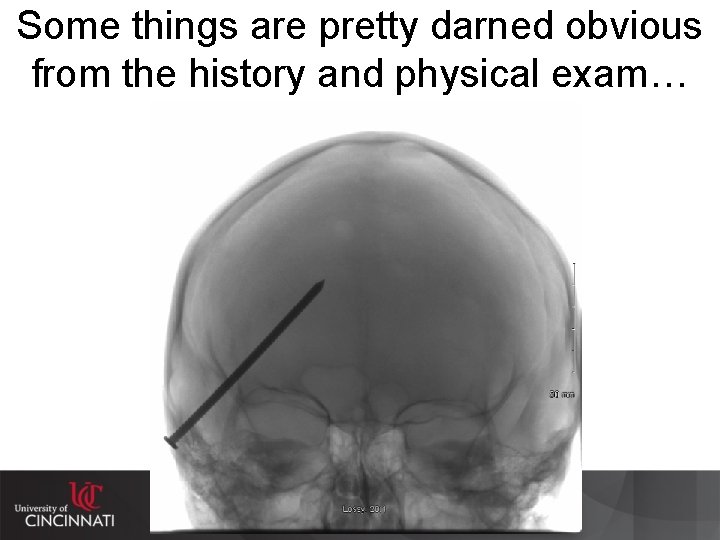
Some things are pretty darned obvious from the history and physical exam…
Some cardinal manifestations SUGGESTING CNS infection Fever Headache Alteration of mental status Focal neurological signs • These are obtained from History and Physical Examination • Remember these are not specific for infection, but general for CNS pathology
Clinical Syndromes of CNS Infections • Acute vs. Chronic – Meningitis vs. Encephalitis vs. Myelitis • Symptoms • Space-occupying lesions • Other – Toxin mediated – Post-infectious syndromes – Prions (“slow viruses”) » Adapted from Chapter 1 in Infections of the Central Nervous System-3 rd Ed. , Lippincott, Williams, and Wilkins 2004, edited by Scheld, Whitley and Marra
Acute vs. Chronic • Acute--rapid or sudden onset – Usually hours to a couple of days – Clinical presentation may be quite dramatic or fulminate (e. g. “looks deathly ill”) • Chronic--slower more progressive onset – Usually several days to weeks to months or longer – Clinical presentation may not be as dramatic or fulminate • Subacute--somewhere between acute and chronic

Encephalitis vs. Meningitis • En • ceph • a • li • tis-- n. Pathology, Inflammation of the brain (a. k. a. “Brain fever”) • Men • in • gi • tis--n. Pathology, Inflammation of any or all of the meninges of the brain and the spinal cord, usually caused by a bacterial infection – The American Heritage Dictionary of the English Language: New College Edition, Houghton Mifflin Company, 1976

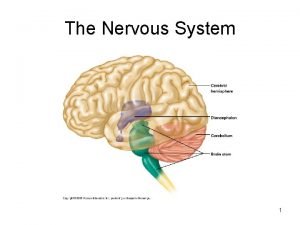
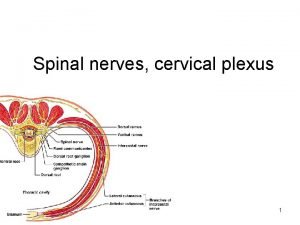
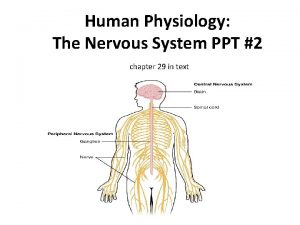
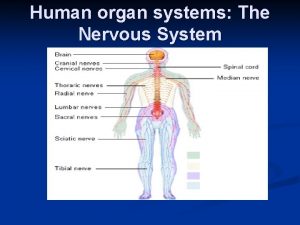
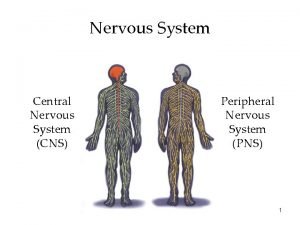
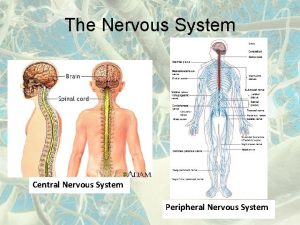
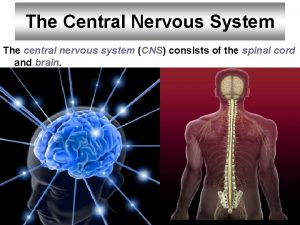
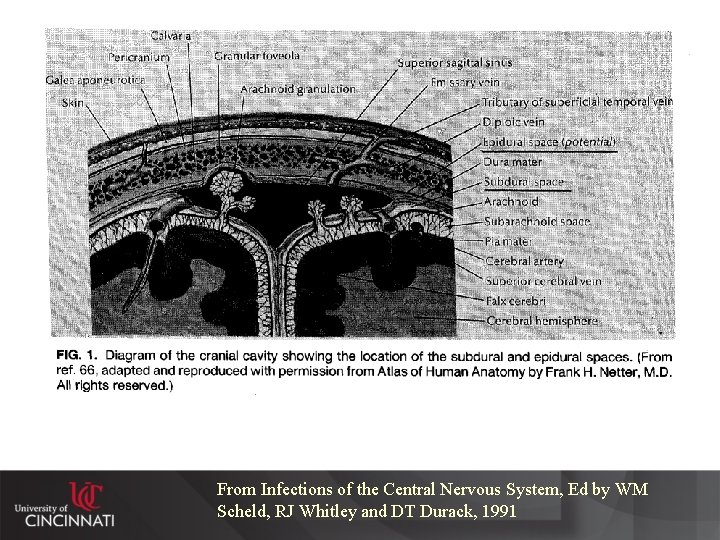
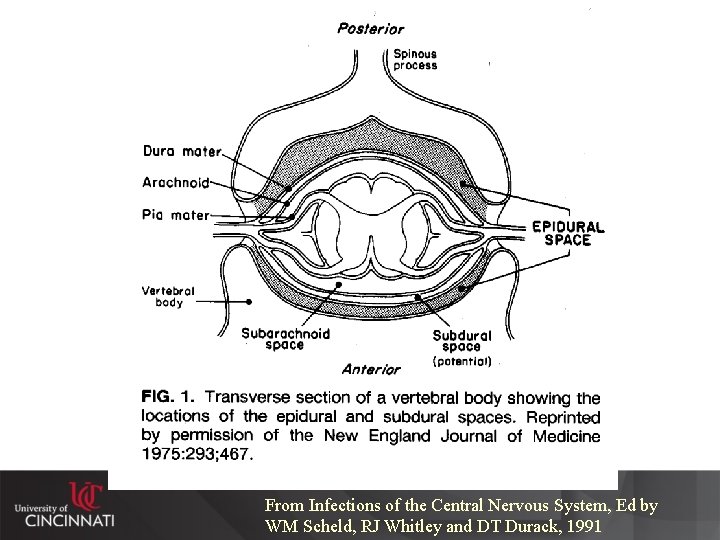
Know anatomic relationships • This is true for all neurological pathology • Remember CNS is enclosed both: – Anatomically – Physiologically (blood-brain barrier) • Immunologically • The immunological isolation may determine how infectious processes present
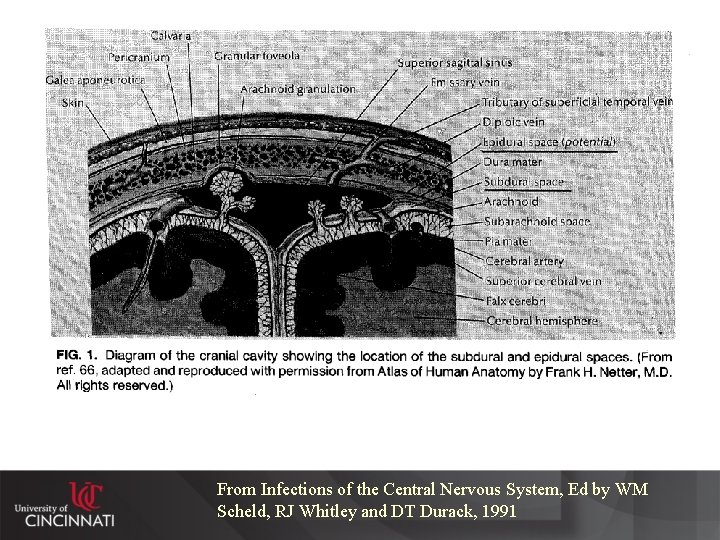
From Infections of the Central Nervous System, Ed by WM Scheld, RJ Whitley and DT Durack, 1991
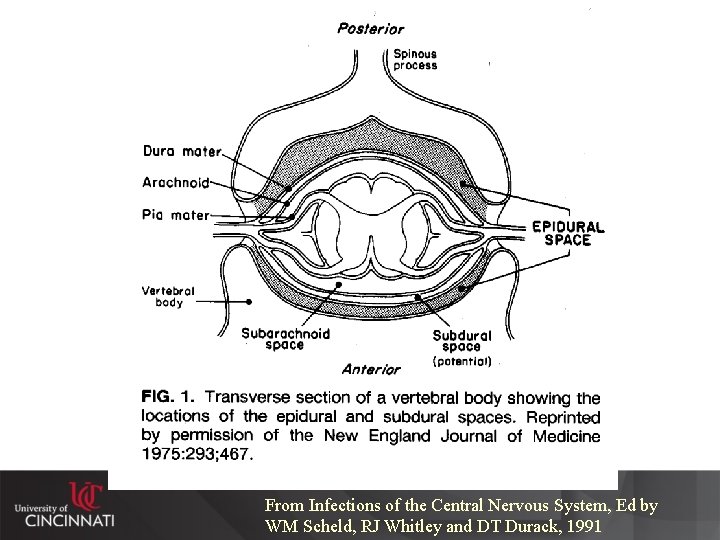
From Infections of the Central Nervous System, Ed by WM Scheld, RJ Whitley and DT Durack, 1991
Keep in mind that what affects the brain can also affect the spinal cord Brain • Meningitis • Encephalitis • Space-occupying lesions (e. g. , brain abscess, subdural abscess) • Toxin-mediated syndromes • Post-infectious syndromes Spinal Cord • Arachnoiditis • Transverse myelitis • Space-occupying lesions (e. g. , spinal epidural abscess) • Toxin-mediated syndromes • Post-infectious syndromes

Space occupying lesions • Clinical signs and symptoms will depend on anatomic location • Because of limited space in CNS focal findings on neurological examination may indicate the anatomic location of these lesions – e. g. • frontal lobe-personality, • motor cortex-upper motor neuron muscular weakness or focal seizure, • spinal canal-lower motor neuron weakness with sensory deficits • Brain abscess, spinal epidural abscess, neurocysticercosis
Toxin-mediated Syndromes • Infections occurring in locations other than CNS • Infecting organisms releases toxin into the host • Toxin has effect at site different than where infection is located • Examples: – Tetanus--stimulates nerves – Botulism--interrupts neural transmissions
Postinfectious Syndromes • Usually begins as another infection (many times sub-clinical or not considered to be noteworthy) • Infection may not be in CNS, but at distant site • Presumed to be immunologically-mediated • Examples: – Guillain-Barre – Post-infectious encephalomyelitis – ADEM (acute demyelinating encephalomyelitis)
Prions (“slow viruses”) • Considered to be unconventional infections • Truly chronic (years to decades in many cases) • Usually no fevers • High mortality • Examples: – Kuru, Creutzfeldt-Jakob disease (CJD), progressive multifocal leukoencephalitis (PML), “new-variant” Creutzfeldt-Jakob disease (nv. CJD) (a. k. a. variant CJD)
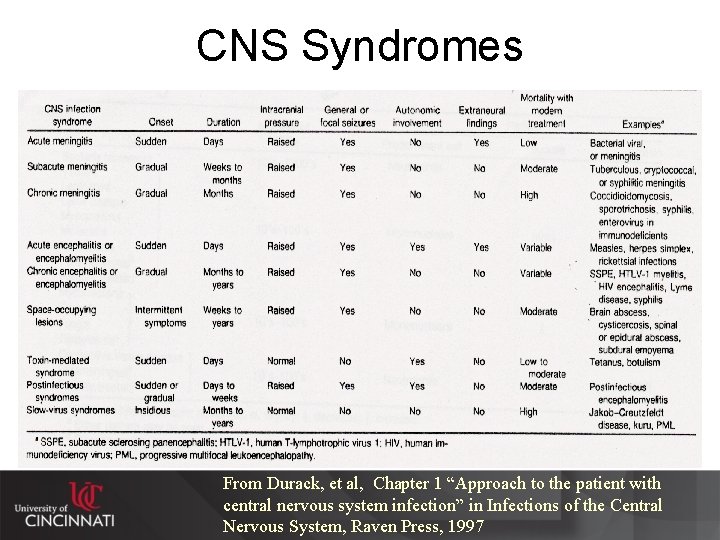
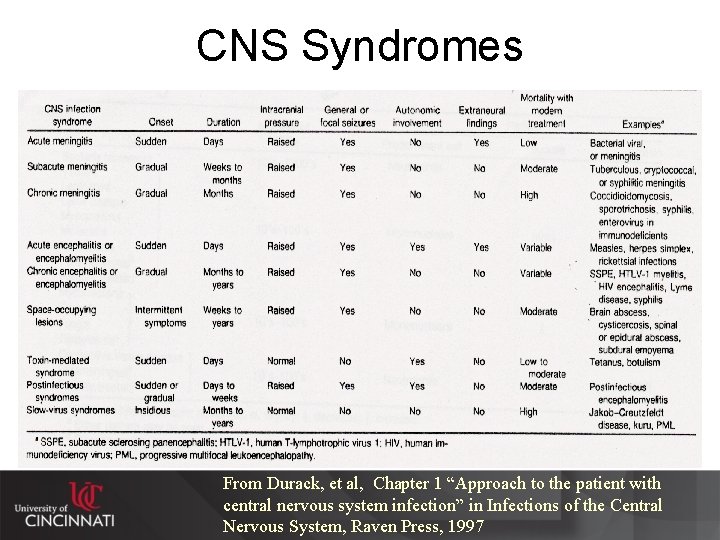
CNS Syndromes From Durack, et al, Chapter 1 “Approach to the patient with central nervous system infection” in Infections of the Central Nervous System, Raven Press, 1997
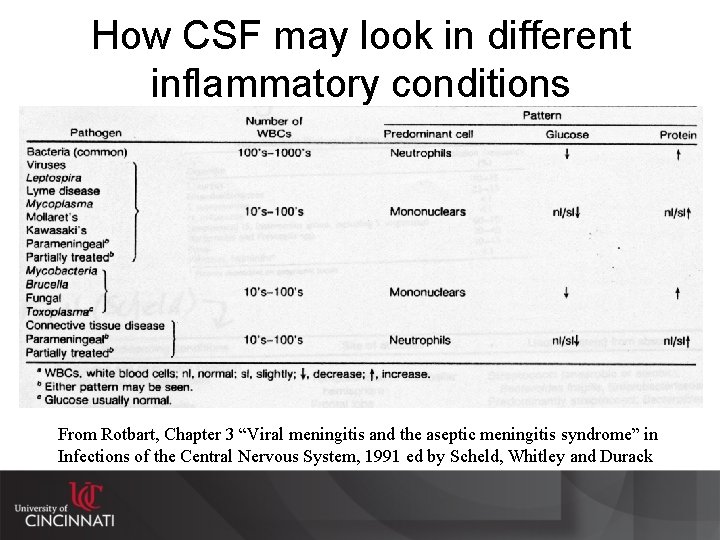
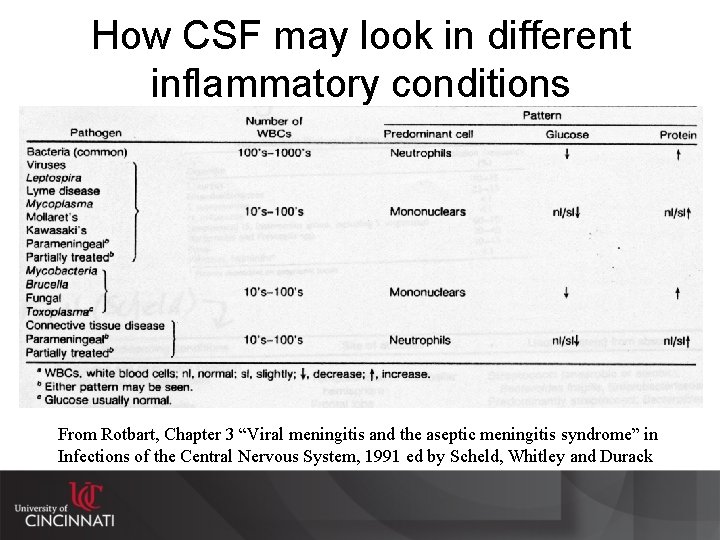
How CSF may look in different inflammatory conditions From Rotbart, Chapter 3 “Viral meningitis and the aseptic meningitis syndrome” in Infections of the Central Nervous System, 1991 ed by Scheld, Whitley and Durack
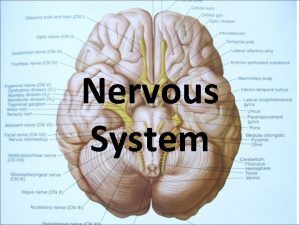
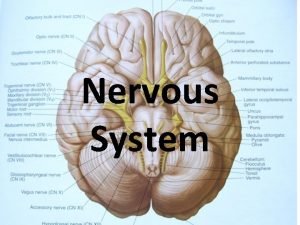
Meningitis • This is the CNS infection entity that causes the most sensation – Especially acute, bacterial meningitis • When meninges inflamed, anything passing through them is at risk for involvement – Blood vessels feeding the cerebral cortex – Nerves exiting the brain (i. e. cranial nerves, especially those at the base of the brainstem)
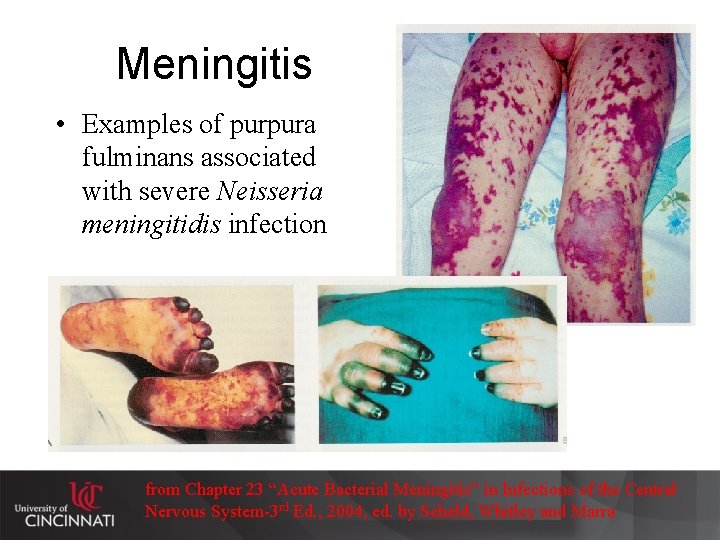
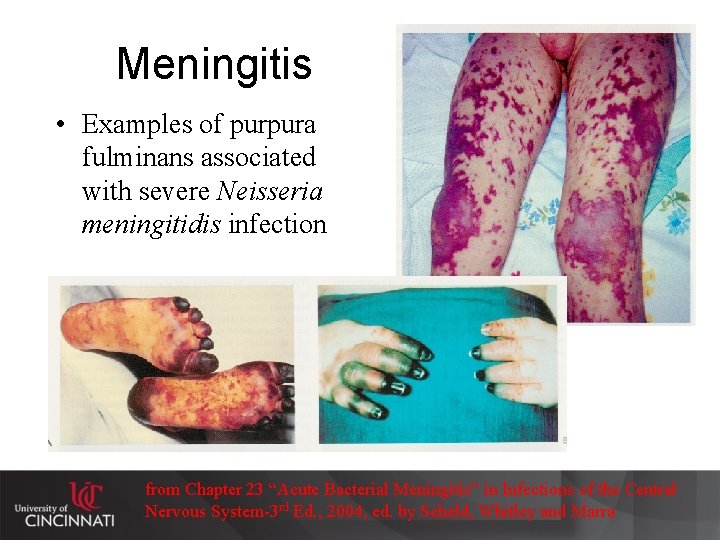
Meningitis • Examples of purpura fulminans associated with severe Neisseria meningitidis infection from Chapter 23 “Acute Bacterial Meningitis” in Infections of the Central Nervous System-3 rd Ed. , 2004, ed. by Scheld, Whitley and Marra
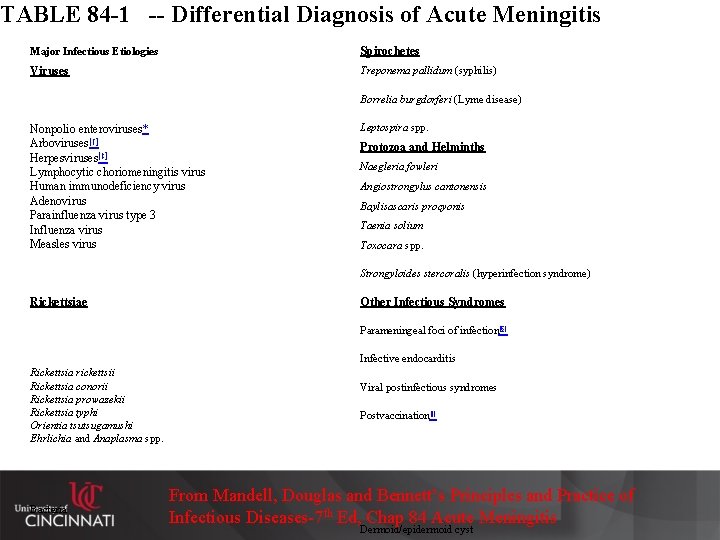
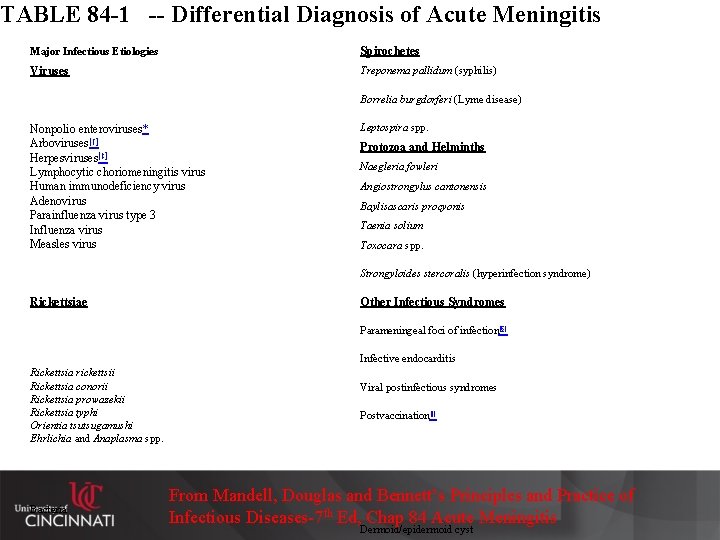
TABLE 84 -1 -- Differential Diagnosis of Acute Meningitis Major Infectious Etiologies Spirochetes Viruses Treponema pallidum (syphilis) Borrelia burgdorferi (Lyme disease) Nonpolio enteroviruses* Arboviruses[†] Herpesviruses[‡] Lymphocytic choriomeningitis virus Human immunodeficiency virus Adenovirus Parainfluenza virus type 3 Influenza virus Measles virus Leptospira spp. Protozoa and Helminths Naegleria fowleri Angiostrongylus cantonensis Baylisascaris procyonis Taenia solium Toxocara spp. Strongyloides stercoralis (hyperinfection syndrome) Rickettsiae Other Infectious Syndromes Parameningeal foci of infection[§] Infective endocarditis Rickettsia rickettsii Rickettsia conorii Rickettsia prowazekii Rickettsia typhi Orientia tsutsugamushi Ehrlichia and Anaplasma spp. Bacteria Viral postinfectious syndromes Postvaccination[|] From Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases-7 th Ed, Chap 84 Acute Meningitis Dermoid/epidermoid cyst

Noninfectious Etiologies and Diseases of Unknown Etiology Bacteria Haemophilus influenzae Neisseria meningitidis Streptococcus pneumoniae Listeria monocytogenes Escherichia coli Streptococcus agalactiae Propionibacterium acnes Staphylococcus aureus Staphylococcus epidermidis Enterococcus spp. Klebsiella pneumoniae Pseudomonas aeruginosa Salmonella spp. Acinetobacter spp. Viridans streptococci Streptococcus bovis Fusobacterium necrophorum Stenotrophomonas maltophilia Streptococcus pyogenes Streptococcus suis Pasteurella multocida Capnocytophaga canimorsus Nocardia spp. Mycobacterium tuberculosis Intracranial Tumors and Cysts Craniopharyngioma Dermoid/epidermoid cyst Teratoma Medications Antimicrobial agents[¶] Nonsteroidal anti-inflammatory agents** Muromonab-CD 3 (OKT 3) Azathioprine Cytosine arabinoside (high dose) Carbamazepine[††] Immune globulin Ranitidine Phenazopyridine Systemic Illnesses Systemic lupus erythematosus Vogt-Koyanagi-Harada syndrome Procedure-related Postneurosurgery Spinal anesthesia Intrathecal injections[‡‡] Chymopapain injection Miscellaneous Seizures Migraine or migraine-like syndromes Mollaret's meningitis From Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases-7 th Ed, Chap 84 Acute Meningitis
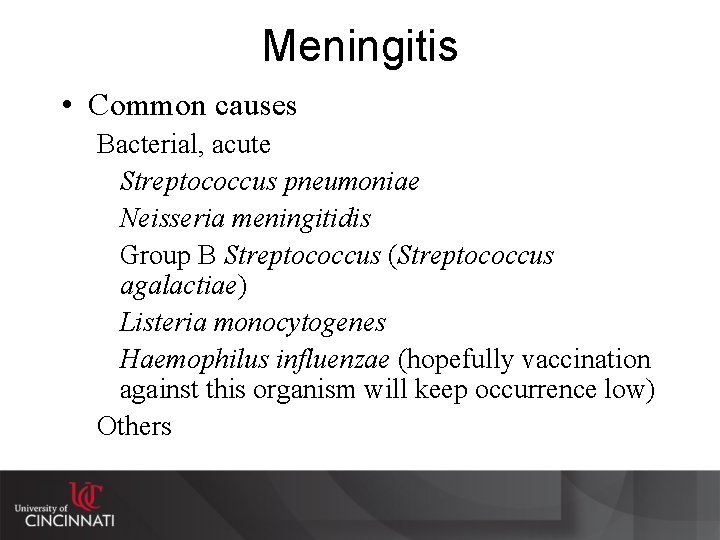
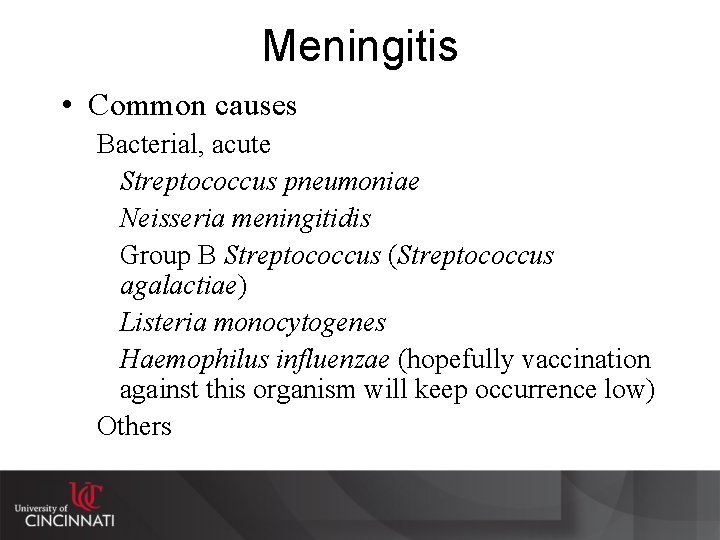
Meningitis • Common causes Bacterial, acute Streptococcus pneumoniae Neisseria meningitidis Group B Streptococcus (Streptococcus agalactiae) Listeria monocytogenes Haemophilus influenzae (hopefully vaccination against this organism will keep occurrence low) Others
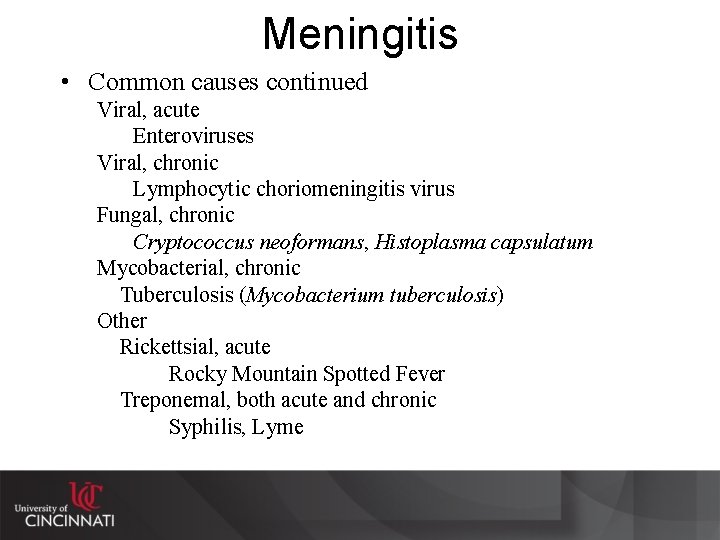
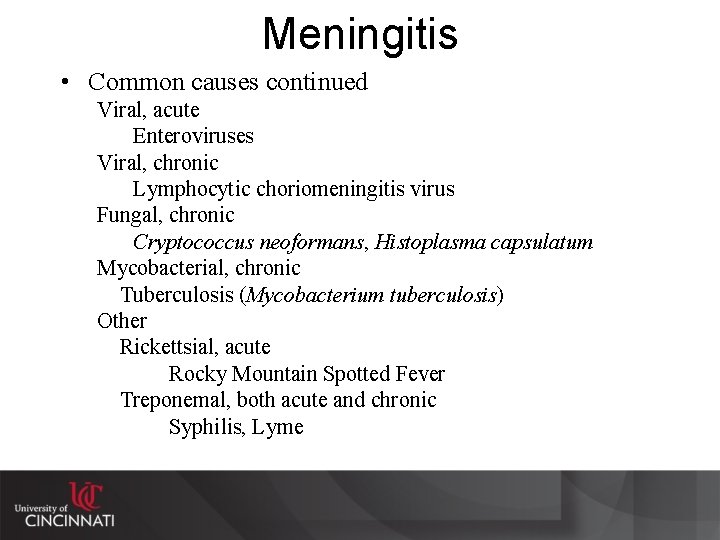
Meningitis • Common causes continued Viral, acute Enteroviruses Viral, chronic Lymphocytic choriomeningitis virus Fungal, chronic Cryptococcus neoformans, Histoplasma capsulatum Mycobacterial, chronic Tuberculosis (Mycobacterium tuberculosis) Other Rickettsial, acute Rocky Mountain Spotted Fever Treponemal, both acute and chronic Syphilis, Lyme

Meningitis—U. S. Epidemiology 1 Schuchat, et al, N Engl J Med 1997; 337: 970 -6. ) Note the distribution in the age groups. Keep in mind that the numbers within these groups are not equal, so the rate of disease by age group is not proportional to the number of cases. Note also that Escherichia coli is not included in the analysis.
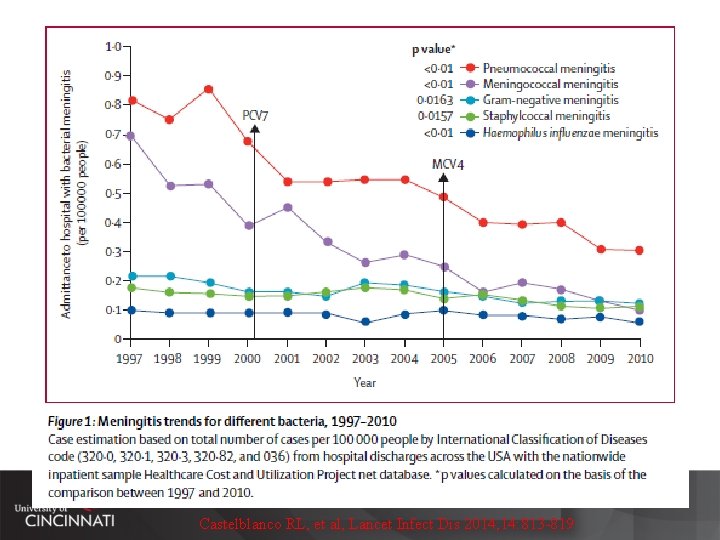
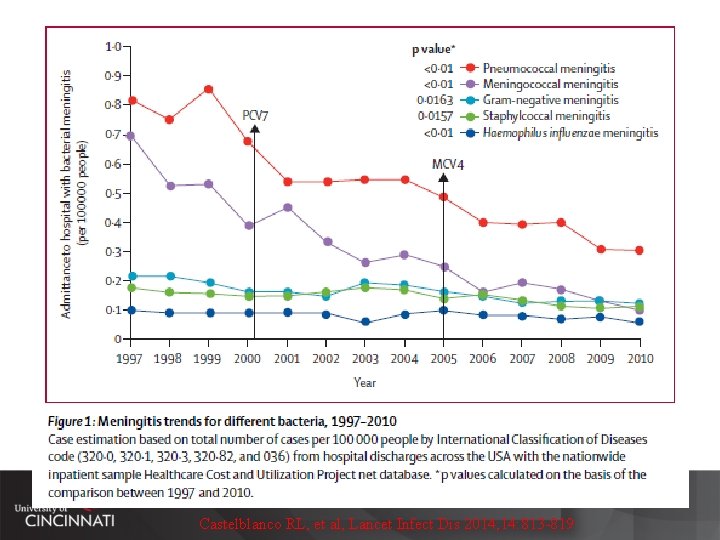
Castelblanco RL, et al, Lancet Infect Dis 2014; 14: 813 -819
Management Meningitis--IDSA http: //www. idsociety. org/uploaded. Files/IDSA/Guidelines. Patient_Care/PDF_Library/Bacterial%20 Meningitis(1). pdf
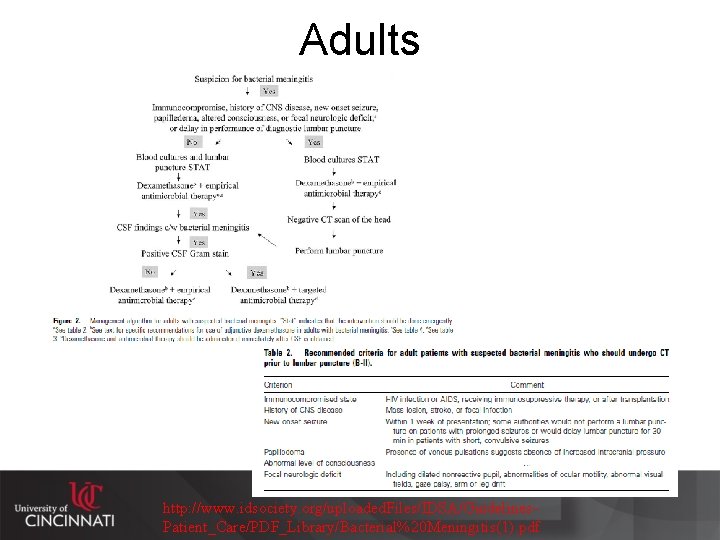
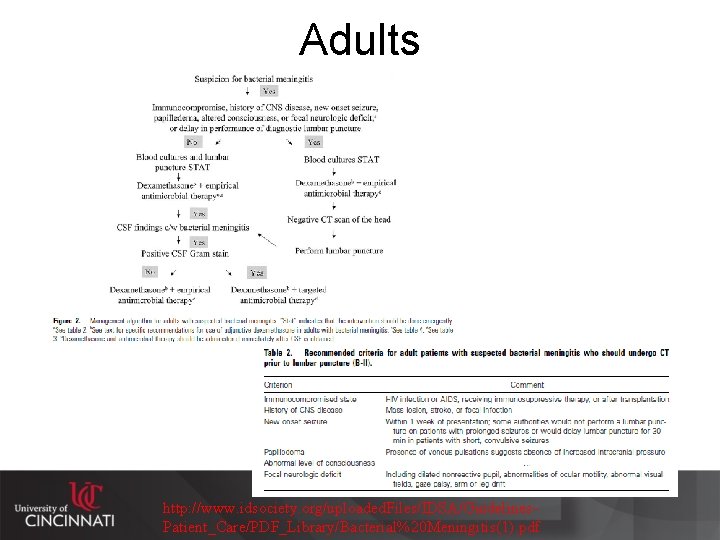
Adults http: //www. idsociety. org/uploaded. Files/IDSA/Guidelines. Patient_Care/PDF_Library/Bacterial%20 Meningitis(1). pdf

Meningitis--Treatment • Empiric treatment based on rapid diagnostics (basic CSF picture and gram stain) and host characteristics • Knowing resistance patterns of common organisms in your geographic area is important (e. g. penicillin resistance in S. pneumoniae) • Getting a medication that crosses blood-brain barrier is important (easy when meninges are inflamed, but less so when not inflamed)
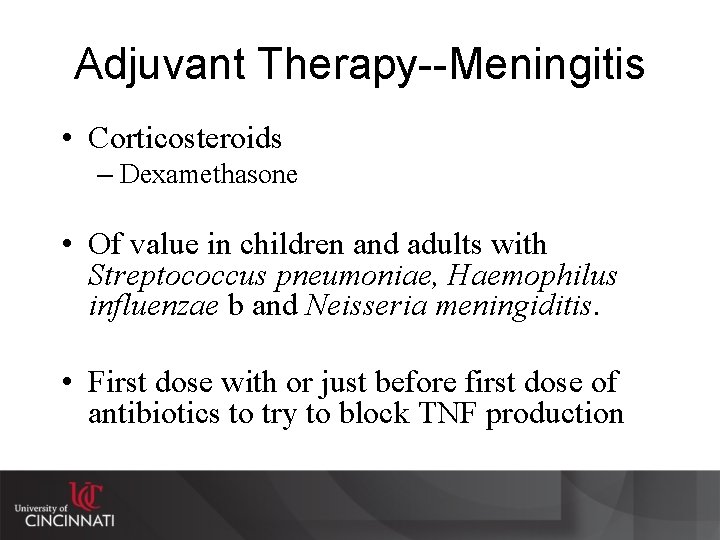
Adjuvant Therapy--Meningitis • Corticosteroids – Dexamethasone • Of value in children and adults with Streptococcus pneumoniae, Haemophilus influenzae b and Neisseria meningiditis. • First dose with or just before first dose of antibiotics to try to block TNF production
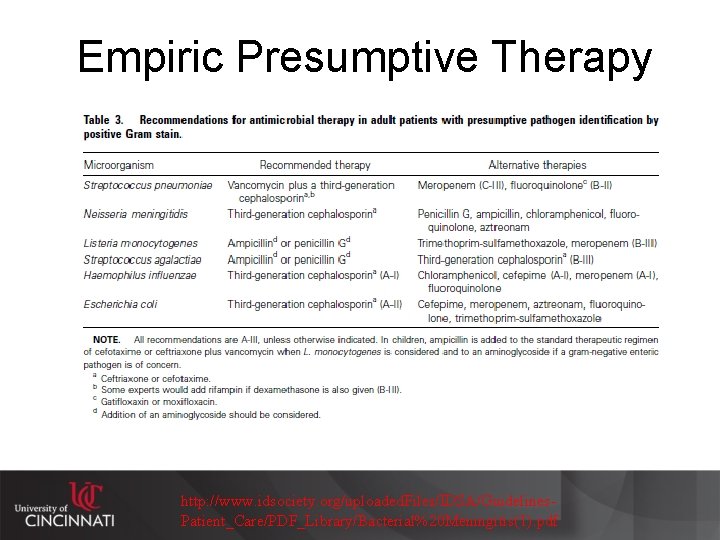
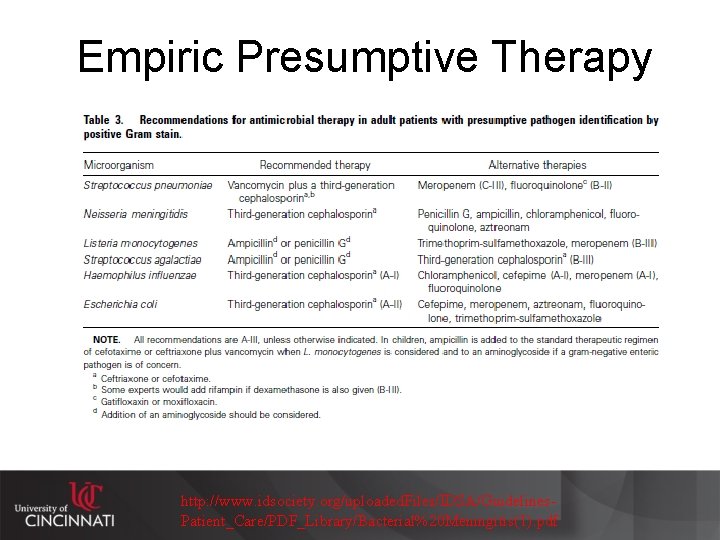
Empiric Presumptive Therapy http: //www. idsociety. org/uploaded. Files/IDSA/Guidelines. Patient_Care/PDF_Library/Bacterial%20 Meningitis(1). pdf
Case 3 • 25 year old white male • 5 -day history of headache – nausea, vomiting, photophobia and phonophobia, anorexia, fevers, chills and myalgias • HIV-infected (diagnosed ~5 years ago) – CD 4 count 450+ cells/mm 3, HIV viral = quantitation below level of detection • Diabetes x 7 years • Meds--efavirenz, zidovudine/lamivudine, rosiglitazone, esomeprazole, citalopram
Case 3 continued • PE – T=98. 2 o. F, HR-79, RR-18, BP-122/77 – unremarkable otherwise • Labs – WBC 10, 400 (normal differential), serum glucose 107 • CSF findings – – No opening pressure recorded 262 WBC (97% lymphocytes) glucose = 62 protein = 62
Case 3 continued • • Viral culture of CSF no growth Viral culture of rectal swab ordered--grew enterovirus Gram stain without organisms seen Bacterial culture no growth Cr. Ag = negative HSV PCR = negative ARBOviral serologies (acute) = non-diagnostic West Nile PCR of both CSF and blood = negative

Aseptic meningitis (“viral meningitis”) • 85 -95% of cases where causative agent identified are enterovirues • Enteroviruses – small ss +sense RNA viruses (picornaviruses) in a naked icosahedral capsid spread by the fecal-oral route and have a Summer-Fall seasonality in temperate climates – Include—polioviruses, coxsackieviruses, echoviruses, parechoviruses, and others simply designated enteroviruses – Treatment is supportive care
Encephalitis • CNS entity that causes a more global dysfunction (i. e. less likely to have focal neurological deficits, but can depending upon location) • Many times associated with viruses, but bacteria and other organisms may contribute to this • Herpes simplex encephalitis is not the most common; however, it causes serious morbidity and mortality. It is an important clinical entity in that it is one of the few viral encephalitides that can be effectively treated. Therefore, it is important to consider in a differential diagnosis.
The Burden of Encephalitis • Roughly 20, 000+ cases annually – 50% etiology known (about half are infectious) – ~6% with a fatal outcome • Cost ~2 Billion dollars annually (2010 dollars) – Direct hospitalization only – No physician charges, no cost for subsequent rehabilitation • Seasonal peaks—late Summer/early Fall Vora, NM, et al, Neurology 2014; 85(5): 443 -451
Treatment of Herpes Encephalitis • Supportive care • Antiviral agents with activity: – High-dose acyclovir or related agents Activated by viral thymidine kinase to become a competitive inhibitor of viral DNA polymerase by blocking deoxyguanosine uptake
Encephalitis—Epidemiology in US • ARBOviruses have some geographic propensity—St. Louis, California, Eastern Equine • West Nile encephalitis recently introduced into the US is causing some concern • Rabies predominantly from non-domestic animals—bats, skunks, coyotes, raccoons
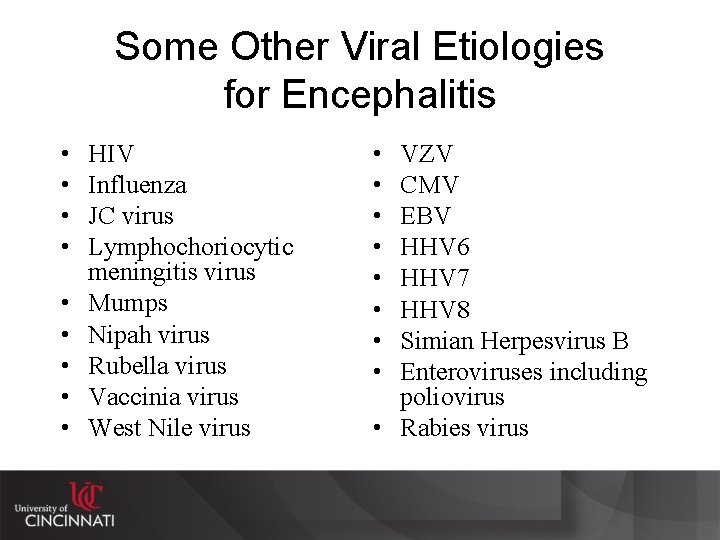
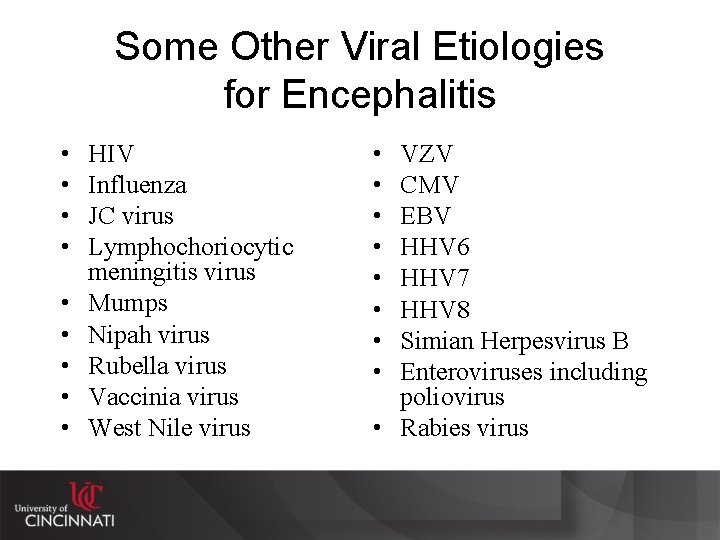
Some Other Viral Etiologies for Encephalitis • • • HIV Influenza JC virus Lymphochoriocytic meningitis virus Mumps Nipah virus Rubella virus Vaccinia virus West Nile virus • • VZV CMV EBV HHV 6 HHV 7 HHV 8 Simian Herpesvirus B Enteroviruses including poliovirus • Rabies virus
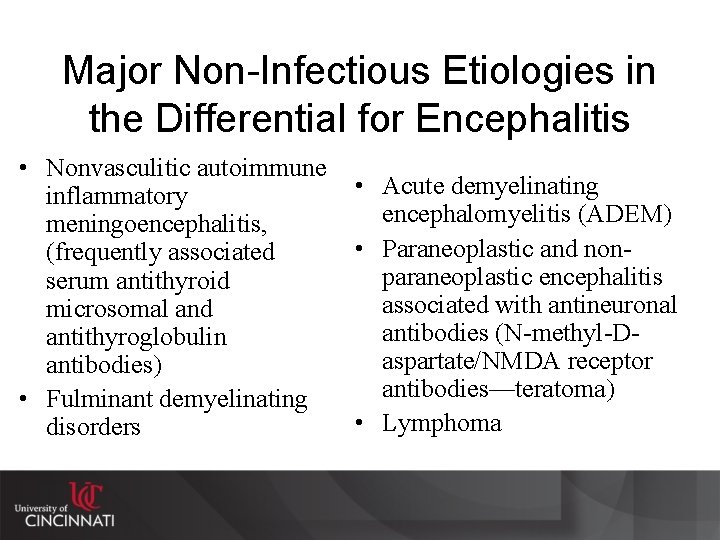
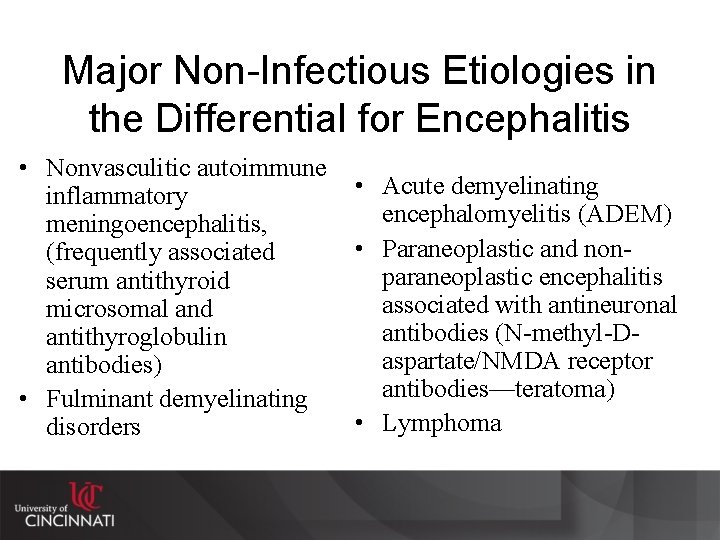
Major Non-Infectious Etiologies in the Differential for Encephalitis • Nonvasculitic autoimmune • Acute demyelinating inflammatory encephalomyelitis (ADEM) meningoencephalitis, • Paraneoplastic and non(frequently associated paraneoplastic encephalitis serum antithyroid associated with antineuronal microsomal and antibodies (N-methyl-Dantithyroglobulin aspartate/NMDA receptor antibodies) antibodies—teratoma) • Fulminant demyelinating • Lymphoma disorders
Management Encephalitis—IDSA http: //www. idsociety. org/uploaded. Files/IDSA/Guidelines. Patient_Care/PDF_Library/Encephalitis. pdf
Adults Diagnosing Encephalitis • Algorithms are complex and contextual • Each situation is somewhat different • Remember, currently can only truly treat Herpes, and noninfectious Venketesan, et al, Clinical Infectious Diseases 2013; 57(8): 1114– 28 Children
Brain abscess • Due to spread from a contiguous site (sinuses, dental infections or traumatic injury) • Due to distant disease: Heart: Endocarditis and other valve abnormalities Lungs/respiratory: Bronchiectasis, lung abscess Compromised host status: HIV, immunosuppresion, malignancy
Epidemiology of Brain Abscesses • Dependent on predisposing conditions • Usually not of viral etiology • Streptococci, staphylococci, Bacteroides spp. , and Prevotella spp. , Haemophilus spp. , enterobacteriaceae and oral anaerobes commonly from contiguous sites. • Viridans streptococci, Stapylococcus aureus, and microaerophilic streptococci commonly from heart sites • Nocardia spp. , Actinomyces spp. , Fusobacterium sp. , and streptococci commonly from respiratory sites • Fungi and mycobacterial organisms become more common in immunocompromise, as does Nocardia spp. , and enterobacteriaceae. • Protozoa and helminths (neurocysticercosis) not common in US, but common elsewhere in the world
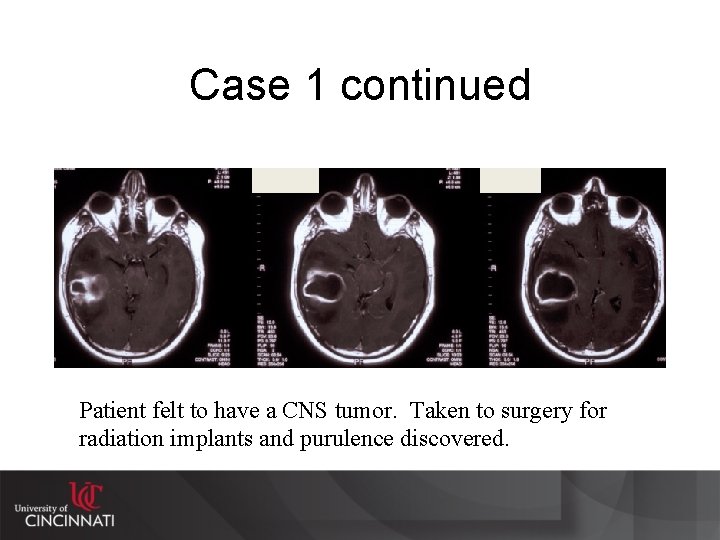
Case 1 continued Patient felt to have a CNS tumor. Taken to surgery for radiation implants and purulence discovered.
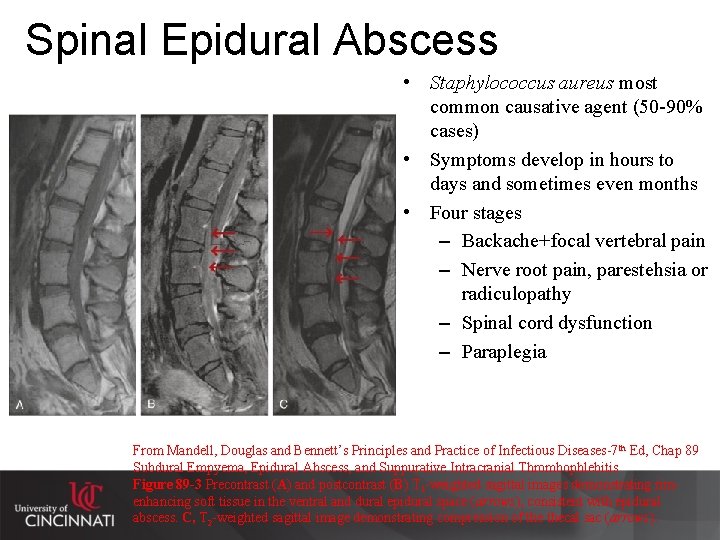
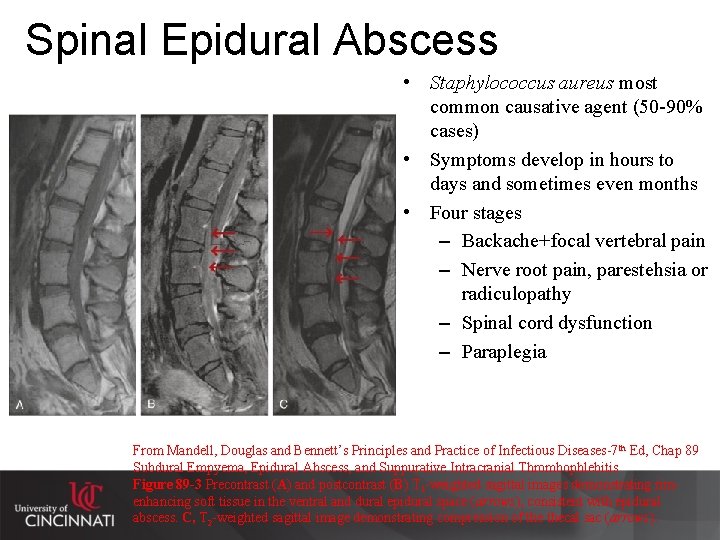
Spinal Epidural Abscess • Staphylococcus aureus most common causative agent (50 -90% cases) • Symptoms develop in hours to days and sometimes even months • Four stages – Backache+focal vertebral pain – Nerve root pain, parestehsia or radiculopathy – Spinal cord dysfunction – Paraplegia From Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases-7 th Ed, Chap 89 Subdural Empyema, Epidural Abscess, and Suppurative Intracranial Thrombophlebitis Figure 89 -3 Precontrast (A) and postcontrast (B) T 1 -weighted sagittal images demonstrating rimenhancing soft tissue in the ventral and dural epidural space (arrows), consistent with epidural abscess. C, T 2 -weighted sagittal image demonstrating compression of thecal sac (arrows).
Case 4 • A 35 year old Mexican man is brought to the emergency department following an apparent seizure. According to family members, the patient has no history of seizures and has been in generally good health. He came to the United States two years ago. • On physical examination the patient is lethargic and oriented only to person. Temperature is 37. 8 C (100. 0 F). Pulse rate is 72 per minute, and blood pressure is 140/90 mm Hg. There is no rash or lymph node enlargement. The neck is supple; the chest is clear. Cardiac and abdominal examinations are normal. No neurological abnormalities are noted. Reflexes are 2+ and symmetrical. The Babinski sign is absent
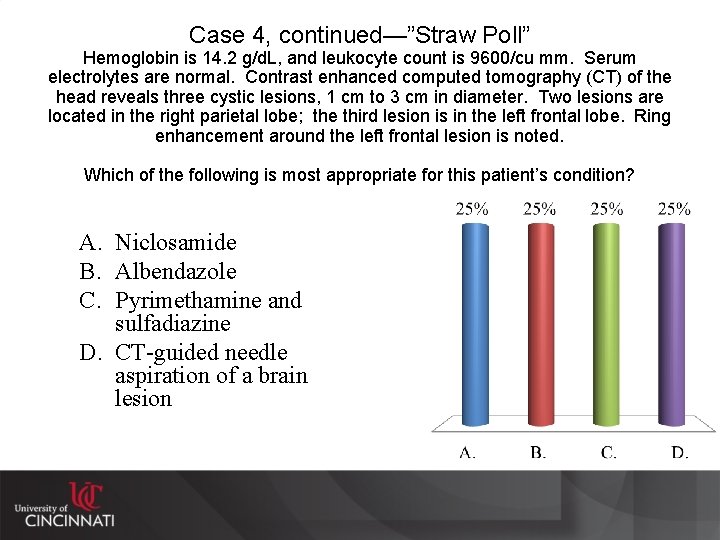
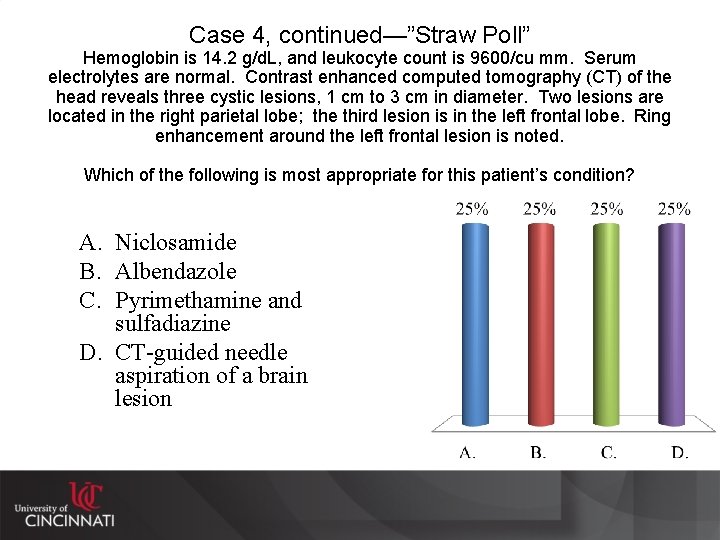
Case 4, continued—”Straw Poll” Hemoglobin is 14. 2 g/d. L, and leukocyte count is 9600/cu mm. Serum electrolytes are normal. Contrast enhanced computed tomography (CT) of the head reveals three cystic lesions, 1 cm to 3 cm in diameter. Two lesions are located in the right parietal lobe; the third lesion is in the left frontal lobe. Ring enhancement around the left frontal lesion is noted. Which of the following is most appropriate for this patient’s condition? A. Niclosamide B. Albendazole C. Pyrimethamine and sulfadiazine D. CT-guided needle aspiration of a brain lesion
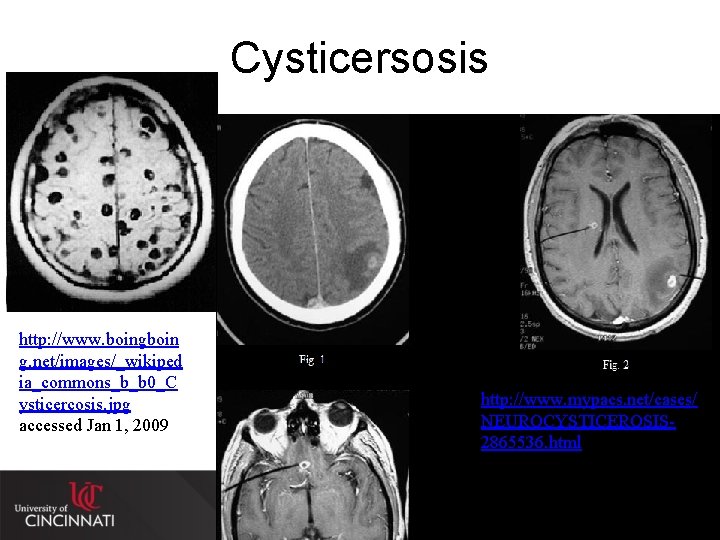
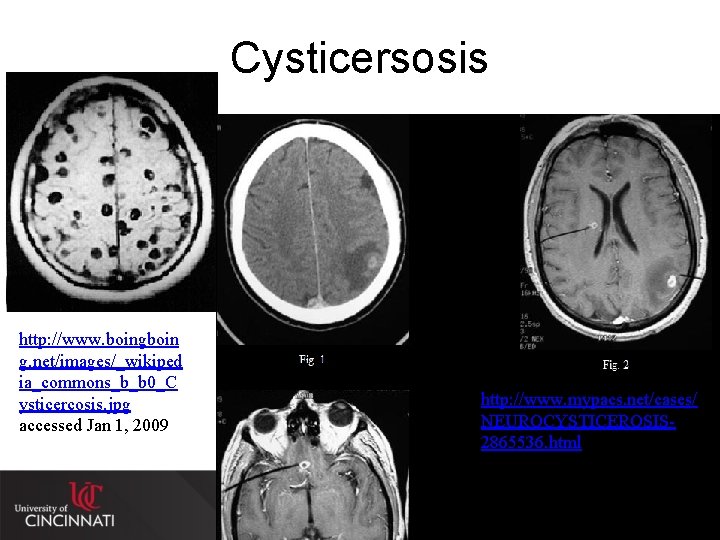
Cysticersosis http: //www. boingboin g. net/images/_wikiped ia_commons_b_b 0_C ysticercosis. jpg accessed Jan 1, 2009 http: //www. mypacs. net/cases/ NEUROCYSTICEROSIS 2865536. html accessed Jan 1, 2009
Tapeworms • Treatment – Parenchymal or degenerations cysts • Antiinflammatories (dexamethasone)and antiparasitics (albendazole) x 30 days • May need antiseizure medication also – Niclosamide for T. solium (but no longer available) so praziquantel x 1 dose (particularly if larval forms seen – Surgical removal—eye, brain

Chickenpox and Shingles From Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases-7 th Ed, Chap 137 Varicella. Zoster Virus
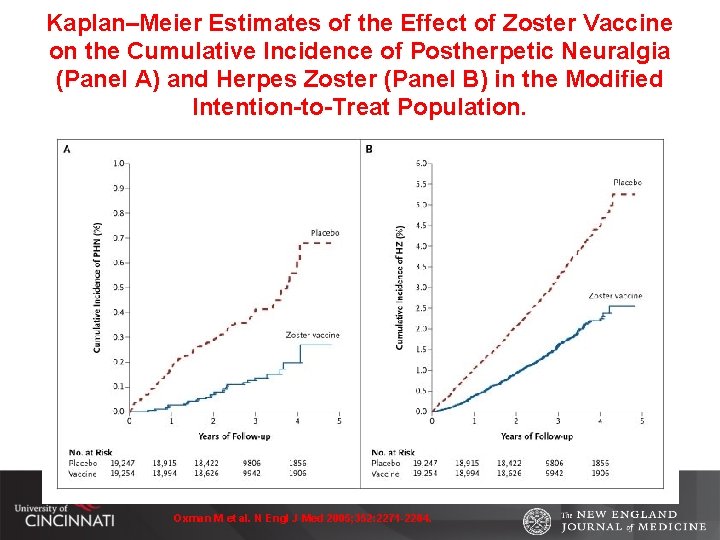
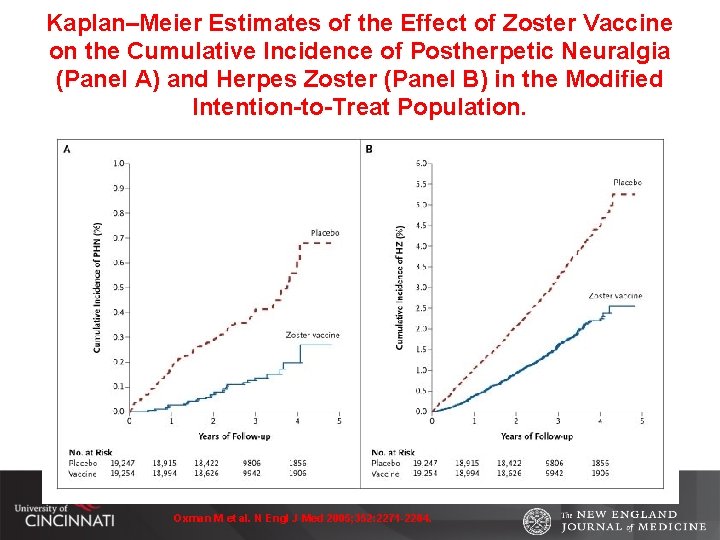
Kaplan–Meier Estimates of the Effect of Zoster Vaccine on the Cumulative Incidence of Postherpetic Neuralgia (Panel A) and Herpes Zoster (Panel B) in the Modified Intention-to-Treat Population. Oxman M et al. N Engl J Med 2005; 352: 2271 -2284.
Prevention • Disrupt transmission – ARBOviruses—decrease vectors encountering hosts – Fecal-oral/waterborne—pasteurization, treatment of water with oxidants (chlorine) – Social distancing – Prophylaxis • Promote host immunological resistance – Vaccinations • Pneumococcal, meningococcal, Haemophilus influenzae B (HIB), poliomyelitis, measles, chicken pox/shingles, influenza, Bacille-Calmette-Guerin (BCG) vaccines
Case 5 • Patient is a 25 year old male with recent history of sinusitis treated with amoxicillin/clavulanate (Augmentin). Presents with an 18 -24 hours onset or nausea, vomiting and intense headache. Brought to the ED due to recent lethargy with these symptoms.
Case 5, continued Physical Exam: T-101. 8 o. F, HR-112; RR-20; BP-120/60 HEENT Anicteric sclerae; EOMI; PERRL Nares-mild hyperemia and bilateral mucosa fullness Throat-no swelling, exudate or erythema noted No enlarged or tender adenopathy Heart Regular, rapid rate with murmurs, rubs or ballops Lungs Clear to auscultation bilaterally with good air movement Abd soft, nontender, nondistended with BSx 4 Ext No gross lesions noted Neuro Lethargic; oriented to person, place and partially to time CN II-XII grossly intact No obvious focal deficits
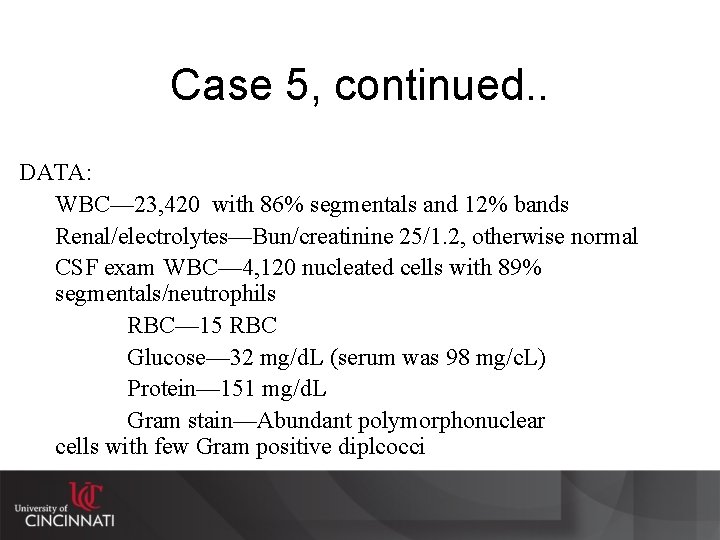
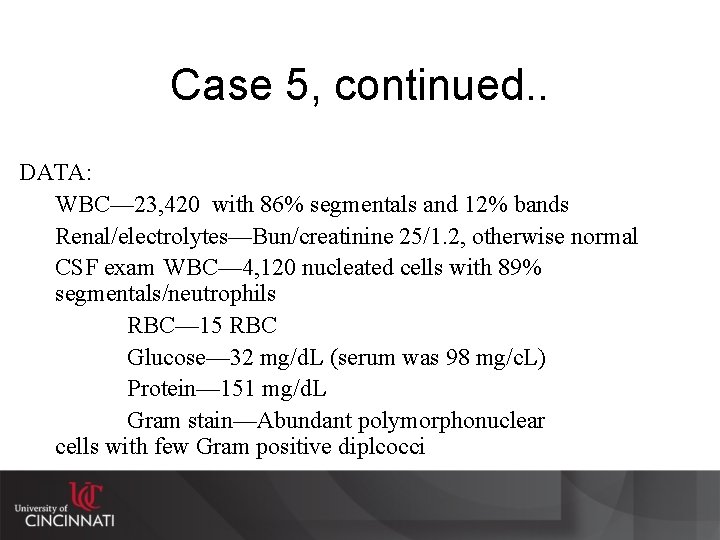
Case 5, continued. . DATA: WBC— 23, 420 with 86% segmentals and 12% bands Renal/electrolytes—Bun/creatinine 25/1. 2, otherwise normal CSF exam WBC— 4, 120 nucleated cells with 89% segmentals/neutrophils RBC— 15 RBC Glucose— 32 mg/d. L (serum was 98 mg/c. L) Protein— 151 mg/d. L Gram stain—Abundant polymorphonuclear cells with few Gram positive diplcocci
Case 5 “Straw-Poll” Vote Which of the following would be the most appropriate choice for empiric therapy? A. B. C. D. Vancomycin alone Penicillin alone Cefepime alone Cetriaxone and vancomycin E. Ampicillin, acyclovir and cefepime

Adjunct Question to Case 5 “Straw-Poll” Vote When are adjunctive corticosteroids indicated for this patient? A. Corticosteroid adjunctive therapy is not indicated for this patient (it should be reserved for pediatric cases). B. Immediately before empiric antibiotic therapy is given. C. Once the diagnosis of Streptococcus pneumoniae is confirmed to prevent sequelae.
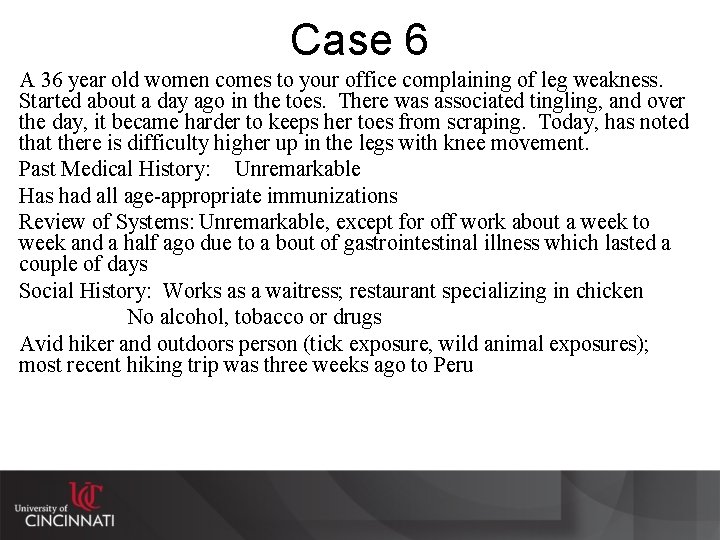
Case 6 A 36 year old women comes to your office complaining of leg weakness. Started about a day ago in the toes. There was associated tingling, and over the day, it became harder to keeps her toes from scraping. Today, has noted that there is difficulty higher up in the legs with knee movement. Past Medical History: Unremarkable Has had all age-appropriate immunizations Review of Systems: Unremarkable, except for off work about a week to week and a half ago due to a bout of gastrointestinal illness which lasted a couple of days Social History: Works as a waitress; restaurant specializing in chicken No alcohol, tobacco or drugs Avid hiker and outdoors person (tick exposure, wild animal exposures); most recent hiking trip was three weeks ago to Peru

Case 6, continued Physical Exam T-98. 6 o. F, HR-72; RR-14; BP-132/74 HEENT-Anicteric; EOMI; PERRL Throat-without swelling, exudate or erythema No enlarged or tender nodes Heart Regular rate without murmurs Lung Clear to auscultation bilaterally Abd soft and unremarkable Neuro Bilateral lower extremity weakness—symmetrical -Toe extensors and flexors 3+/5 bilaterally -Quads and hamstrings 4+/5 bilaterally -CN II-XI gross intact Sensory—normal -Bilateral Achilles and patellar reflexs are absent

Case 6 “Straw-Poll” Vote What is the most likely diagnosis? A. Rabies B. Zika virus infection C. Guillain-Barre Syndrome D. Tick borne paralysis E. Poliomyelitis
Bibliography • • Harrison’s Principles of Internal Medicine— 18 th Edition 2012, pages 3410 -3447 (Chapters 120, 381 -383) – Harrison’s Principles of Internal Medicine— 14 th Edition 1998, pages 749 -754, 2419 -2451 (Chapters 120, 377 -379) Infections of the Central Nervous System— 4 rd Edition, 2014. Ed. by WM Scheld, RT Whiley, CM Marra (this is a detailed and comprehensive text on the topic of nearly 1, 000 pages) – 3 rd Edition (2004), 2 nd Edition (1997) and 1 st Edition (1991) also hav some good images and tables. , Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases— 8 th Edition, 2015. Chapters 89 -94, pages 1091 -1193) J Attia, et al. Does this Adult Patient have Acute Meningitis? J Am Med Assoc 1999; 282: 175 -181. (Nice review of associated clinical signs and symptoms, and their sensitivity in helping to diagnose acute meningitis) Schuchat A, et al, N Engl J Med 1997; 337: 970 -6. Castelblanco RL, et al, Lancet Infect Dis 2014; 14: 813 -819 IDSA Clinical Practice Guidelines—Meningitis, 2004 http: //www. idsociety. org/uploaded. Files/IDSA/Guidelines. Patient_Care/PDF_Library/Bacterial%20 Meningitis(1). pdf IDSA Clinical Practice Guidelines—Encephalitis, 2008 http: //www. idsociety. org/uploaded. Files/IDSA/Guidelines. Patient_Care/PDF_Library/Encephalitis. pdf
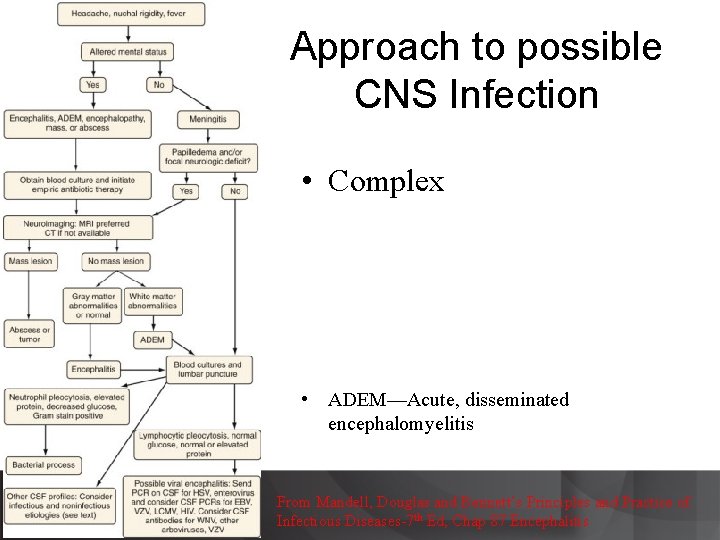
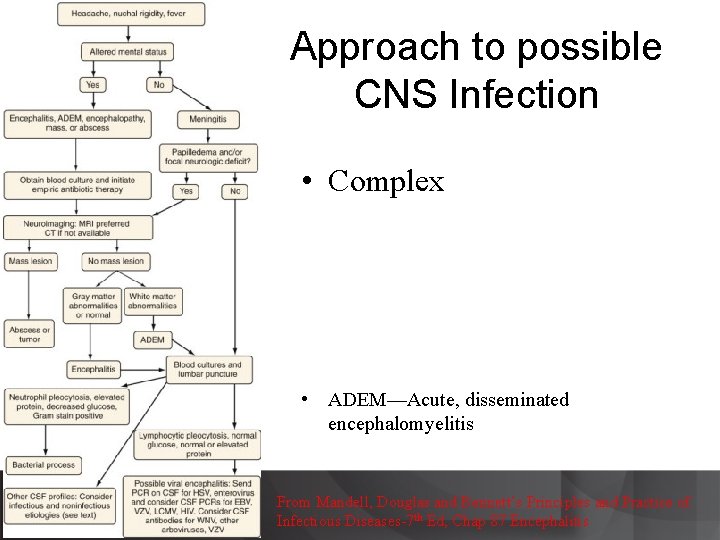
Approach to possible CNS Infection • Complex • ADEM—Acute, disseminated encephalomyelitis From Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases-7 th Ed, Chap 87 Encephalitis
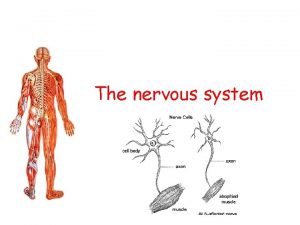
 Neuron process
Neuron process Sensory input and motor output
Sensory input and motor output Processes of neuron
Processes of neuron Central and peripheral nervous system
Central and peripheral nervous system Central nervous system amusement park
Central nervous system amusement park The central nervous system
The central nervous system Nervous system vocabulary
Nervous system vocabulary Hydra neurons
Hydra neurons Bser aer
Bser aer Part of nervous system
Part of nervous system Central nervous system for kids
Central nervous system for kids Nervous system and digestive system
Nervous system and digestive system Endocrine system vs nervous system
Endocrine system vs nervous system General mechanism of hormone action
General mechanism of hormone action Endocrine system and nervous system
Endocrine system and nervous system Opportunistic infections
Opportunistic infections Methotrexate yeast infection
Methotrexate yeast infection Opportunistic infections
Opportunistic infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Johnson and johnson botnet infections
Johnson and johnson botnet infections Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Neurosiphyllis
Neurosiphyllis Eye infections
Eye infections Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Genital infections
Genital infections Salmonella life cycle
Salmonella life cycle Acute gingival infections
Acute gingival infections Central nervous sysytem
Central nervous sysytem Chemical messengers of the nervous system
Chemical messengers of the nervous system Segmentation of platyhelminthes
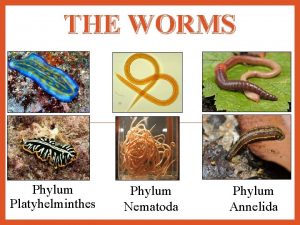
Segmentation of platyhelminthes The nervous system is made up of
The nervous system is made up of What are the three basic functions of the nervous system
What are the three basic functions of the nervous system Nervous system learning objectives
Nervous system learning objectives Componentes componentes
Componentes componentes Stimulus in nervous system
Stimulus in nervous system Nervous system objectives
Nervous system objectives Craniosacral region
Craniosacral region Sympathetic nervous system def
Sympathetic nervous system def 31 nerves
31 nerves Sns somatic nervous system
Sns somatic nervous system Brain scienstructable
Brain scienstructable Somatic vs autonomic nervous system
Somatic vs autonomic nervous system Nematoda
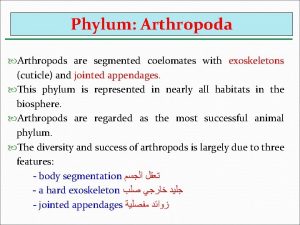
Nematoda Phylum arthropoda marine
Phylum arthropoda marine Jointed foot phylum
Jointed foot phylum Are arthropods coelomates
Are arthropods coelomates Parasympathatic nervous system
Parasympathatic nervous system Nervous system of coelenterata
Nervous system of coelenterata Autonomic nervous system consists of
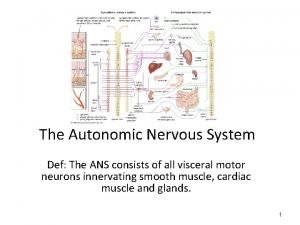
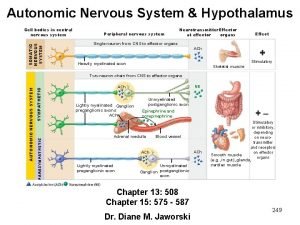
Autonomic nervous system consists of Differences between nervous system and endocrine
Differences between nervous system and endocrine Section 35-1 human body systems answer key
Section 35-1 human body systems answer key Ans
Ans L
L Basic unit of nervous system
Basic unit of nervous system Homeostasis positive feedback examples
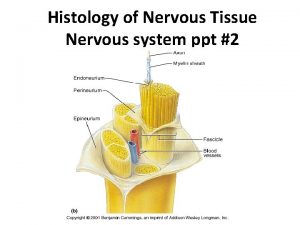
Homeostasis positive feedback examples Nervous system histology ppt
Nervous system histology ppt Gray matter in the brain
Gray matter in the brain Comparison of endocrine and nervous system
Comparison of endocrine and nervous system 8 divisions of the nervous system
8 divisions of the nervous system How to take care of your nervous system
How to take care of your nervous system Nervous system effector cells
Nervous system effector cells Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Exocrine glands are ductless
Exocrine glands are ductless Beta-blockers for overactive sympathetic nervous system
Beta-blockers for overactive sympathetic nervous system Hypothalamus
Hypothalamus Autonomic
Autonomic Excretory system of silkworm
Excretory system of silkworm Section 35-3 divisions of the nervous system
Section 35-3 divisions of the nervous system What is the building block of the nervous system
What is the building block of the nervous system Structure of nervous system graphic organizer
Structure of nervous system graphic organizer Medunerve
Medunerve Planaria nervous system
Planaria nervous system