Heart murmurs Dynamic Auscultation Dr Nithin P G
![How is a murmur produced? [Re >4000 turbulent flow] L = linear dimension (internal How is a murmur produced? [Re >4000 turbulent flow] L = linear dimension (internal](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-6.jpg)


![MS • Low n rough rumbling [sound of distant thunder] MDM • Localized to MS • Low n rough rumbling [sound of distant thunder] MDM • Localized to](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-53.jpg)
![Other diastolic murmurs • Cabot– Locke Murmur- [Diastolic Flow murmur] – The Cabot–Locke murmur Other diastolic murmurs • Cabot– Locke Murmur- [Diastolic Flow murmur] – The Cabot–Locke murmur](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-60.jpg)
![Position A. Lt Lateral Decubitus LV impulse [apical sounds, murmurs better heard] Act of Position A. Lt Lateral Decubitus LV impulse [apical sounds, murmurs better heard] Act of](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-73.jpg)


- Slides: 89
Heart murmurs & Dynamic Auscultation Dr Nithin P G
Outlay of Seminar • Definition • What to look for/ how to describe a murmur • Classification of murmurs • Types of murmurs • Dynamic Auscultation
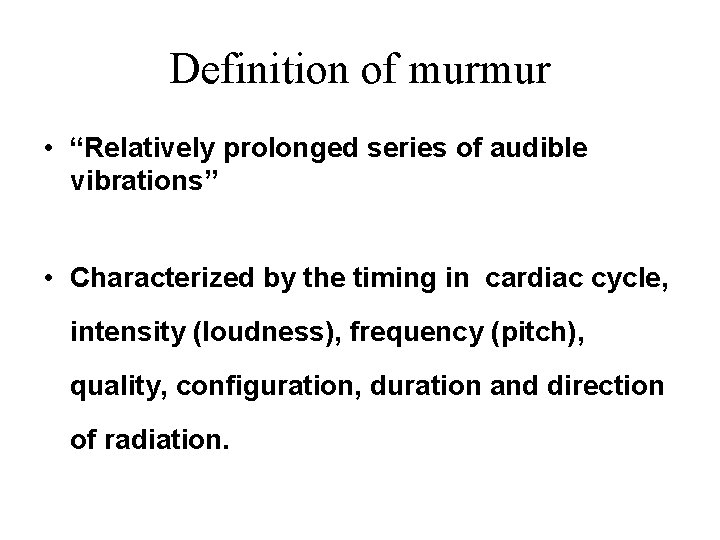
Definition of murmur • “Relatively prolonged series of audible vibrations” • Characterized by the timing in cardiac cycle, intensity (loudness), frequency (pitch), quality, configuration, duration and direction of radiation.
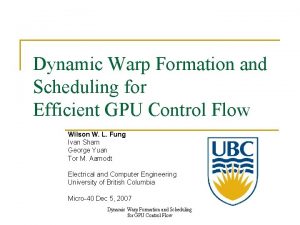
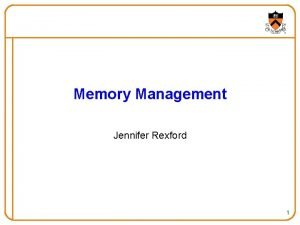
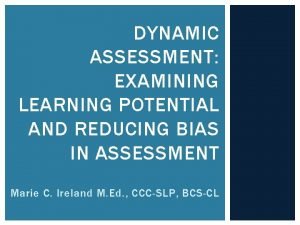
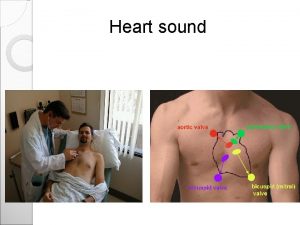
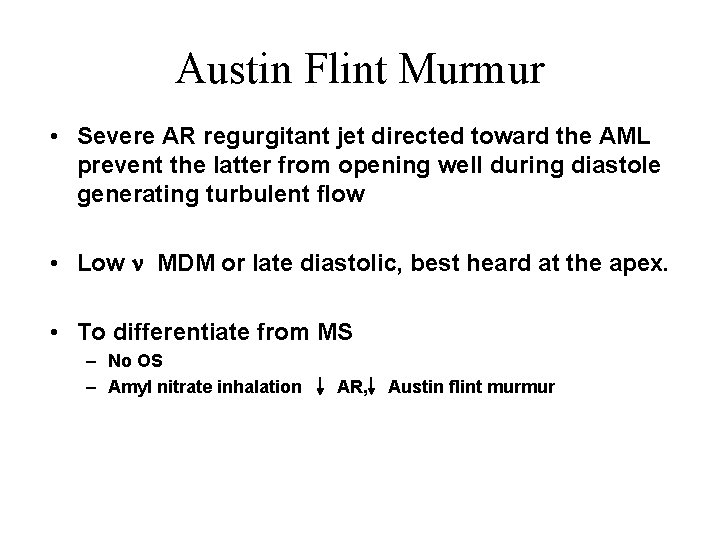
How is a murmur produced and heard?
How is a murmur produced? Sound is produced by vibration Turbulence generated in the blood column vibrations set up in the vessel wall & cardiac structures murmurs
![How is a murmur produced Re 4000 turbulent flow L linear dimension internal How is a murmur produced? [Re >4000 turbulent flow] L = linear dimension (internal](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-6.jpg)
How is a murmur produced? [Re >4000 turbulent flow] L = linear dimension (internal diameter In pipes) Q = V 1*A 1= V 2*A 2 V = mean fluid velocity Q = P/R Q = volumetric flow rate A = pipe cross-sectional area m = dynamic viscosity of the fluid Re => Turbulence => n = kinematic viscosity [m/ r] murmur r = density of the fluid
Auscultation of murmur Other factors affecting auscultation of murmur • Distance from chest wall, position of patient • Underlying soft tissue, lung, fluid • Quality of apparatus
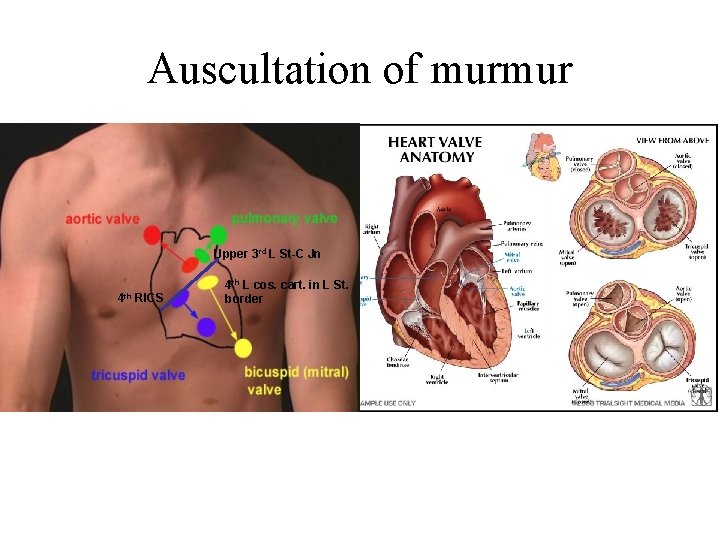
Auscultation of murmur Upper 3 rd L St-C Jn 4 th RICS 4 th L cos. cart. in L St. border
How to describe a murmur?
Description of a Murmur • Position in the cardiac cycle • Site of murmur [max. intensity] • Intensity • Quality & Pitch • Conduction • Dynamic changes
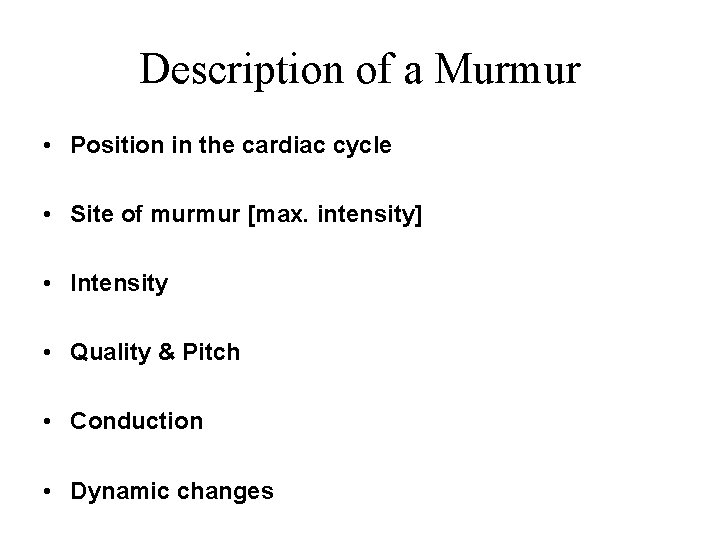
Position in the cardiac cycle • Systolic murmur • Diastolic murmur • Continuous murmur early systolic mid systolic late systolic pan/holo systolic early diastolic mid diastolic pre systolic
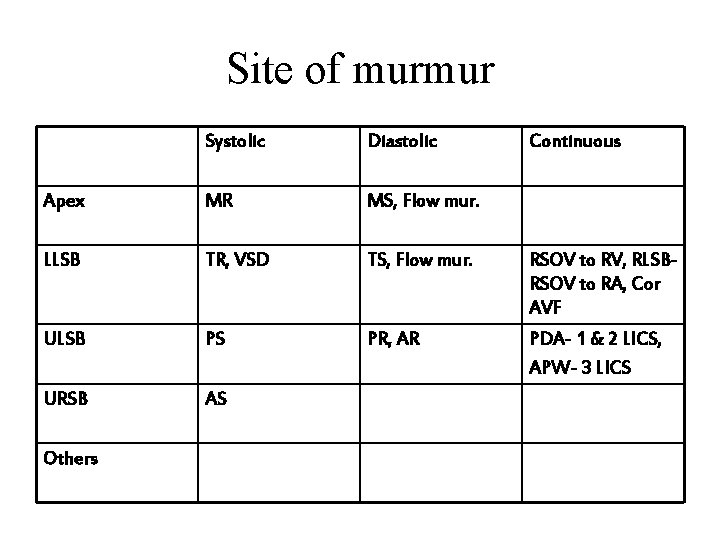
Site of murmur Systolic Diastolic Apex MR MS, Flow mur. LLSB TR, VSD TS, Flow mur. RSOV to RV, RLSBRSOV to RA, Cor AVF ULSB PS PR, AR PDA- 1 & 2 LICS, APW- 3 LICS URSB AS Others Continuous
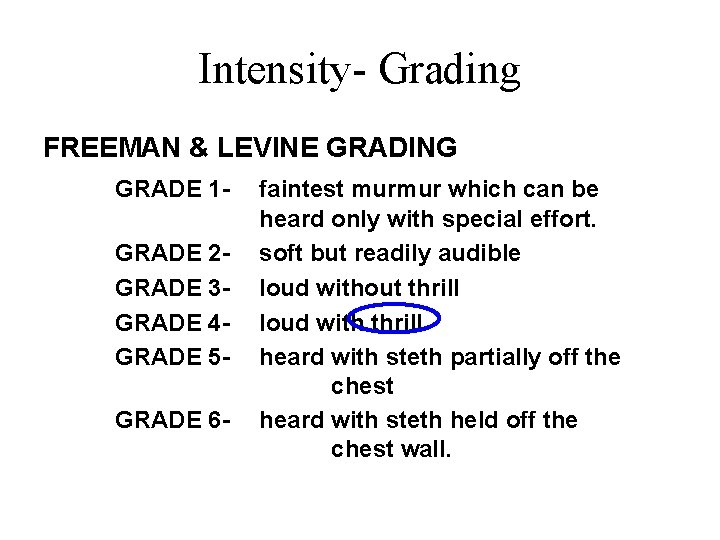
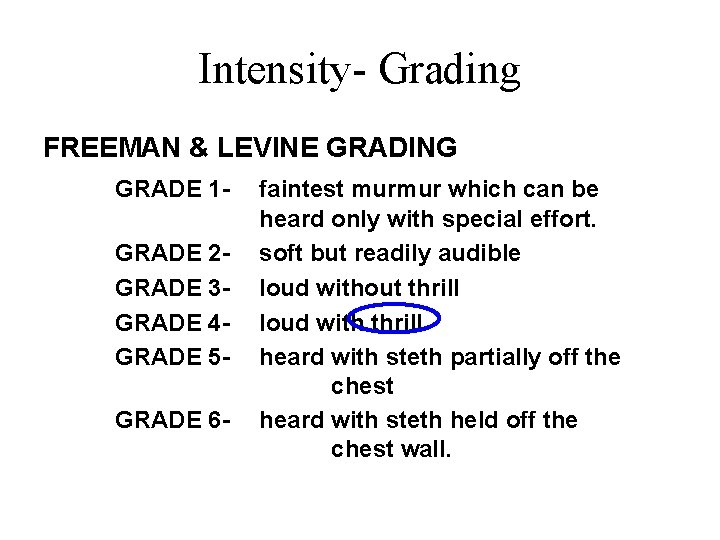
Intensity- Grading FREEMAN & LEVINE GRADING GRADE 1 GRADE 2 GRADE 3 GRADE 4 GRADE 5 GRADE 6 - faintest murmur which can be heard only with special effort. soft but readily audible loud without thrill loud with thrill heard with steth partially off the chest heard with steth held off the chest wall.
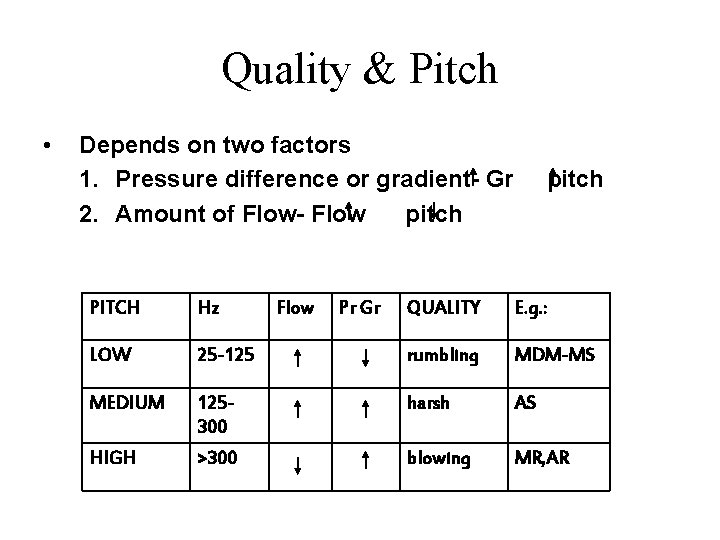
Quality & Pitch • Depends on two factors 1. Pressure difference or gradient- Gr 2. Amount of Flow- Flow pitch PITCH Hz LOW Flow Pr Gr pitch QUALITY E. g. : 25 -125 rumbling MDM-MS MEDIUM 125300 harsh AS HIGH >300 blowing MR, AR
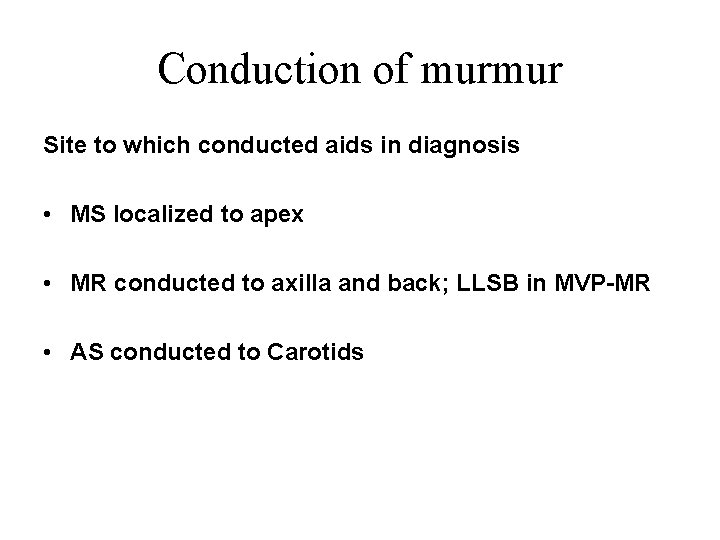
Conduction of murmur Site to which conducted aids in diagnosis • MS localized to apex • MR conducted to axilla and back; LLSB in MVP-MR • AS conducted to Carotids
Classification & types of murmurs
Classification & types of murmurs • Systolic murmur • Diastolic murmur • Continuous murmur early systolic mid systolic late systolic pan/holo systolic early diastolic mid diastolic pre systolic
Systolic Murmurs

Midsystolic murmur • • Most common murmur heard in everyday practice. Starts at an interval after S 1 and ends before S 2. It could be PATHOLOGICAL INNOCENT/PHYSIOLOGICAL 5 settings 1. 2. 3. 4. Ventricular outflow obstruction Dilation of aorta and pulmonary trunk Accelerated systolic flow into aorta or pulmonary trunk Innocent midsystolic murmur( including those due to morphological changes of valve with no obstruction) 5. Some forms of MR
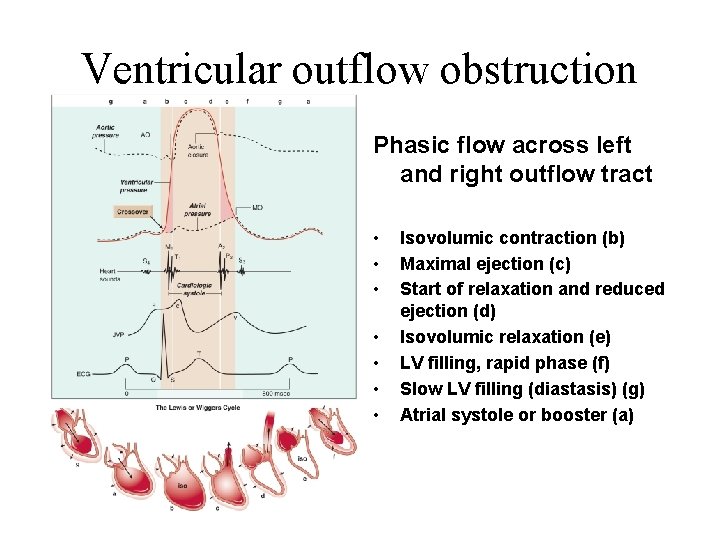
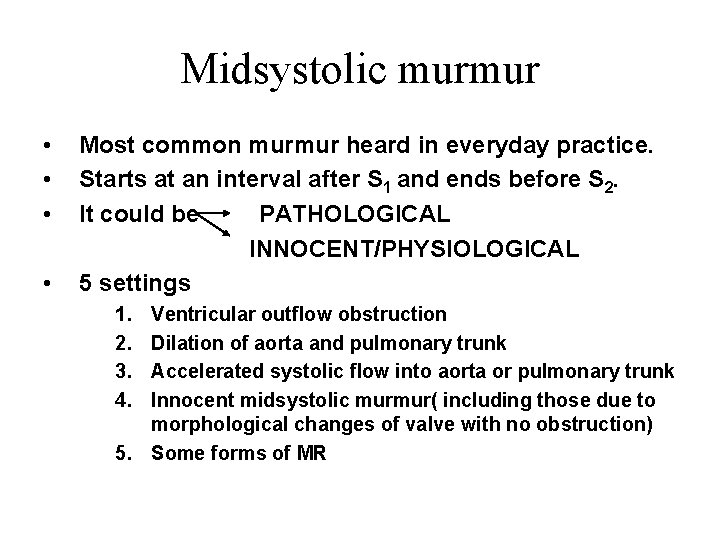
Ventricular outflow obstruction Phasic flow across left and right outflow tract • • Isovolumic contraction (b) Maximal ejection (c) Start of relaxation and reduced ejection (d) Isovolumic relaxation (e) LV filling, rapid phase (f) Slow LV filling (diastasis) (g) Atrial systole or booster (a)
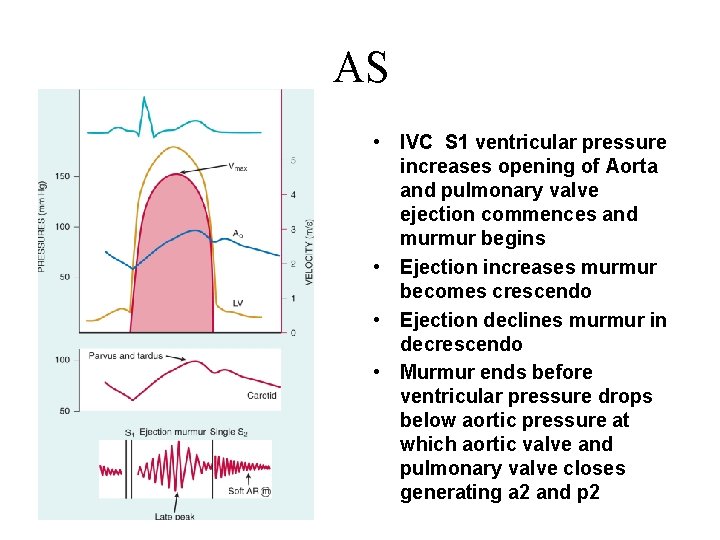
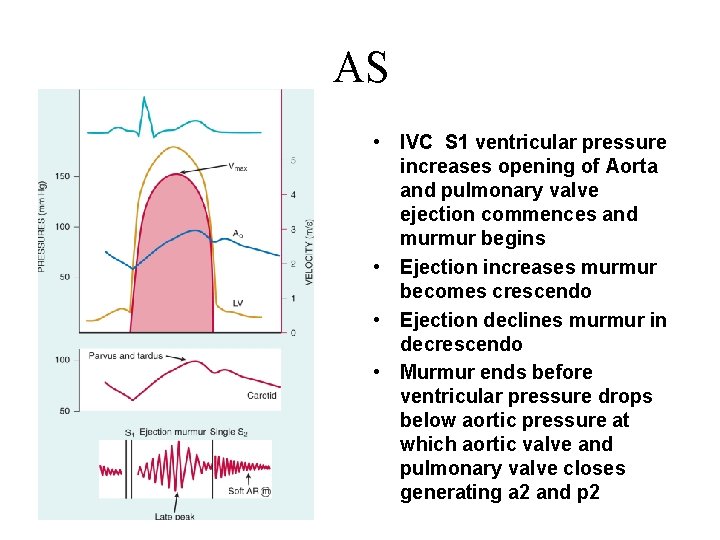
AS • IVC S 1 ventricular pressure increases opening of Aorta and pulmonary valve ejection commences and murmur begins • Ejection increases murmur becomes crescendo • Ejection declines murmur in decrescendo • Murmur ends before ventricular pressure drops below aortic pressure at which aortic valve and pulmonary valve closes generating a 2 and p 2
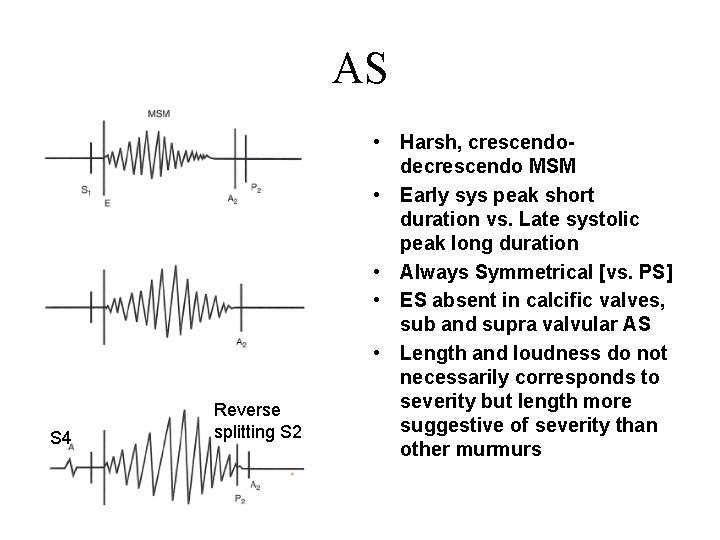
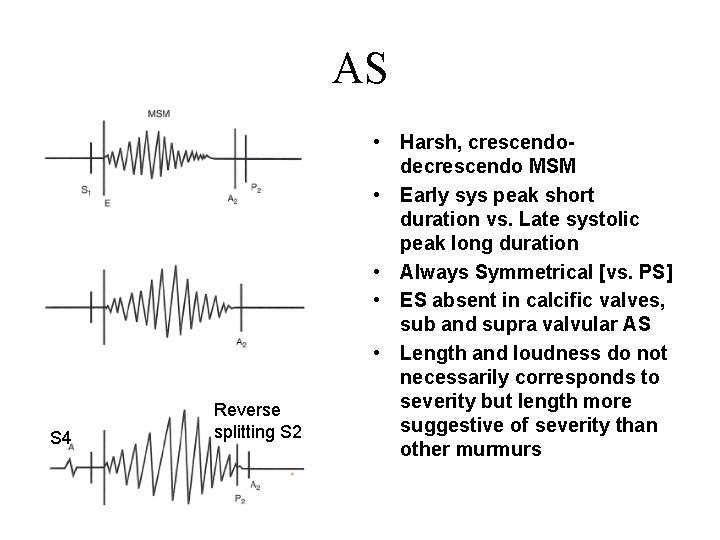
AS S 4 Reverse splitting S 2 • Harsh, crescendodecrescendo MSM • Early sys peak short duration vs. Late systolic peak long duration • Always Symmetrical [vs. PS] • ES absent in calcific valves, sub and supra valvular AS • Length and loudness do not necessarily corresponds to severity but length more suggestive of severity than other murmurs
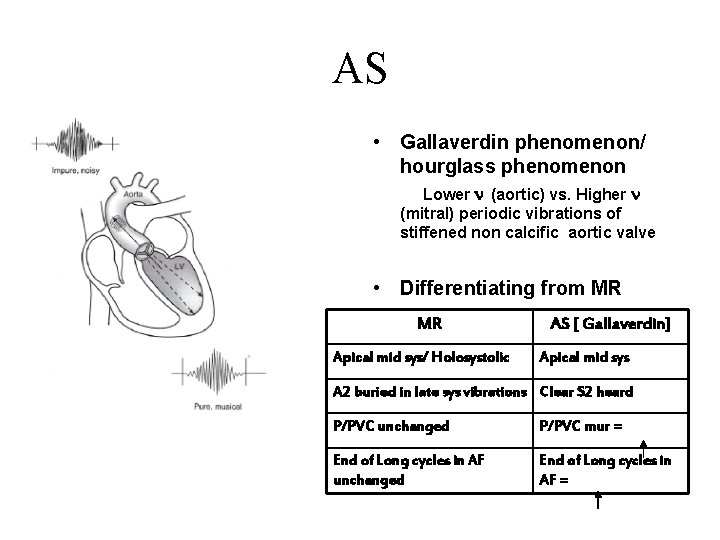
AS • Gallaverdin phenomenon/ hourglass phenomenon Lower n (aortic) vs. Higher n (mitral) periodic vibrations of stiffened non calcific aortic valve • Differentiating from MR MR Apical mid sys/ Holosystolic AS [ Gallaverdin] Apical mid sys A 2 buried in late sys vibrations Clear S 2 heard P/PVC unchanged P/PVC mur = End of Long cycles in AF unchanged End of Long cycles in AF =
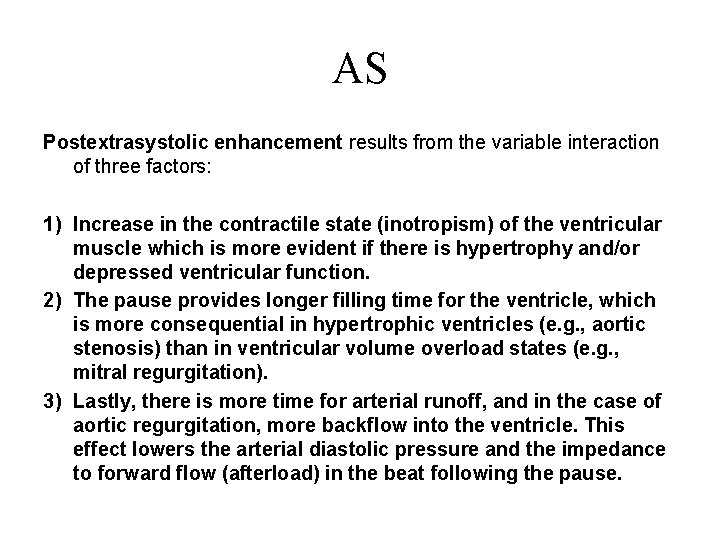
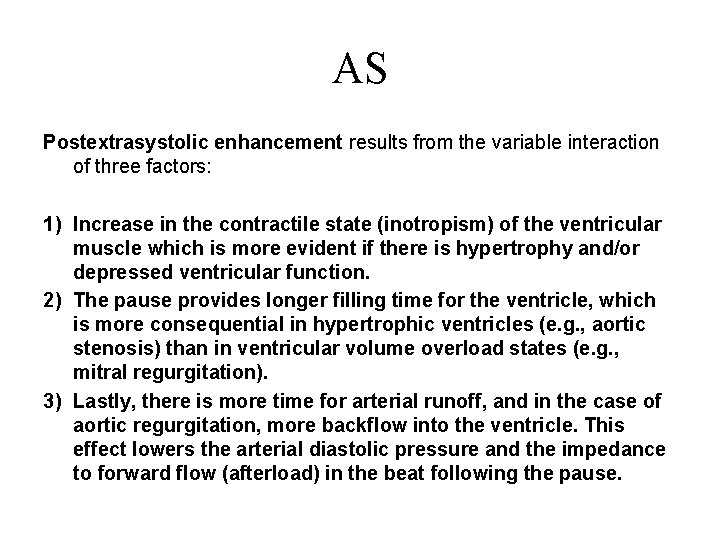
AS Postextrasystolic enhancement results from the variable interaction of three factors: 1) Increase in the contractile state (inotropism) of the ventricular muscle which is more evident if there is hypertrophy and/or depressed ventricular function. 2) The pause provides longer filling time for the ventricle, which is more consequential in hypertrophic ventricles (e. g. , aortic stenosis) than in ventricular volume overload states (e. g. , mitral regurgitation). 3) Lastly, there is more time for arterial runoff, and in the case of aortic regurgitation, more backflow into the ventricle. This effect lowers the arterial diastolic pressure and the impedance to forward flow (afterload) in the beat following the pause.
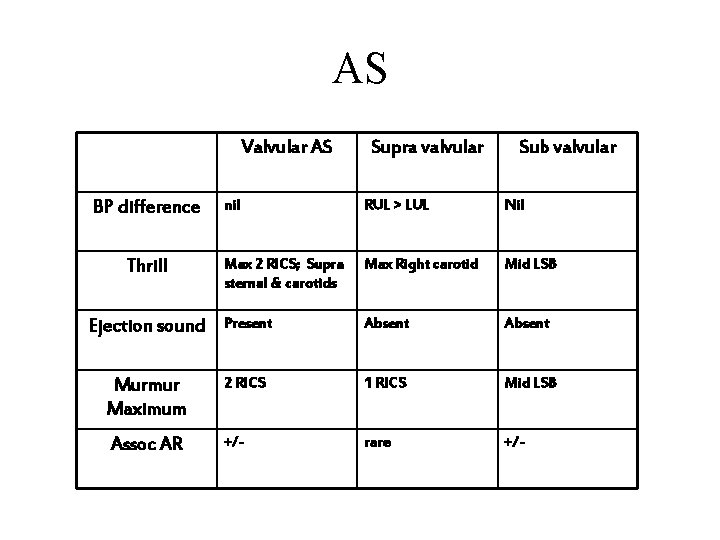
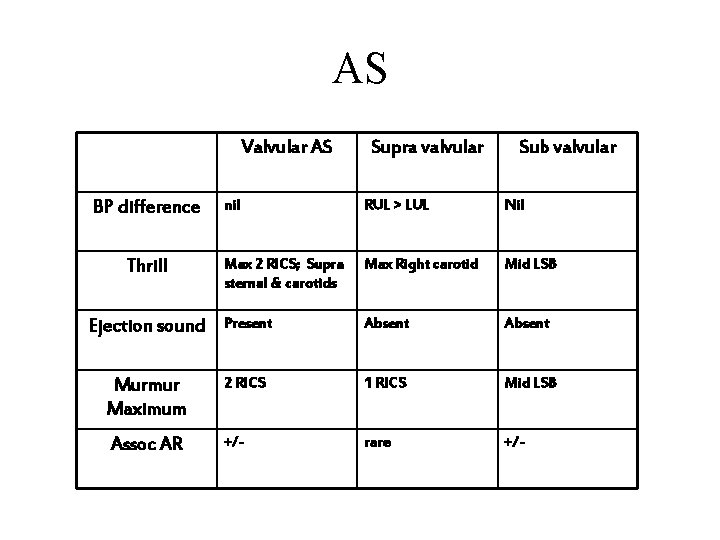
AS Valvular AS Supra valvular Sub valvular nil RUL > LUL Nil Max 2 RICS; Supra sternal & carotids Max Right carotid Mid LSB Ejection sound Present Absent Murmur Maximum 2 RICS 1 RICS Mid LSB Assoc AR +/- rare +/- BP difference Thrill
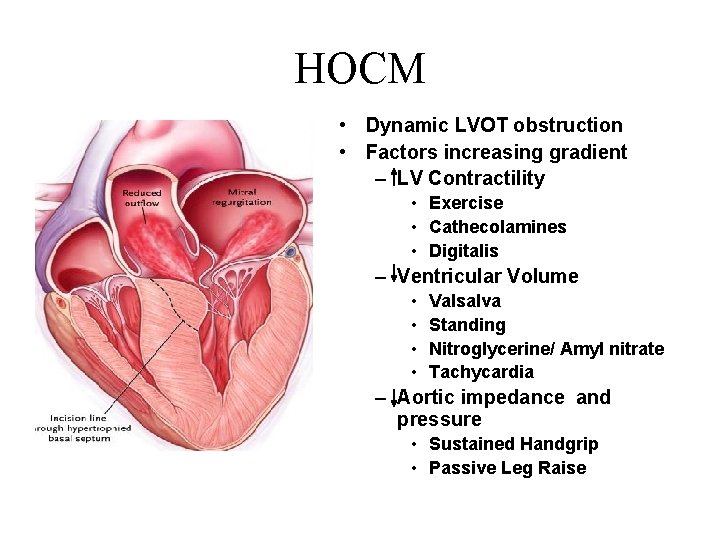
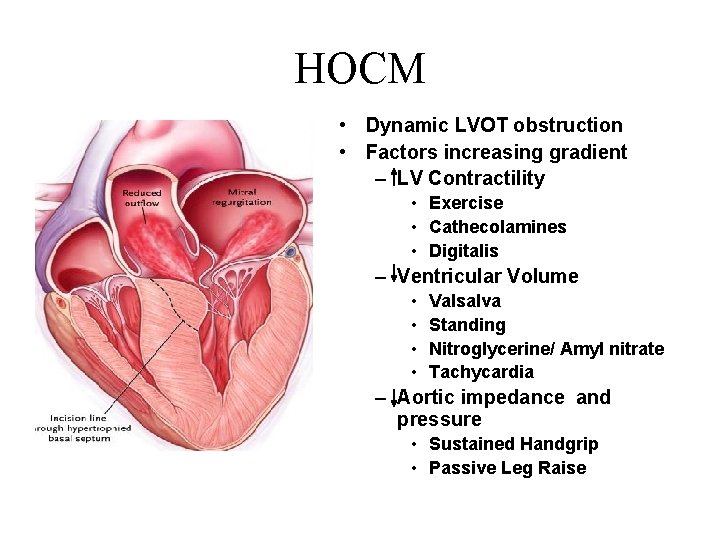
HOCM • Dynamic LVOT obstruction • Factors increasing gradient – LV Contractility • Exercise • Cathecolamines • Digitalis – Ventricular Volume • • Valsalva Standing Nitroglycerine/ Amyl nitrate Tachycardia – Aortic impedance and pressure • Sustained Handgrip • Passive Leg Raise
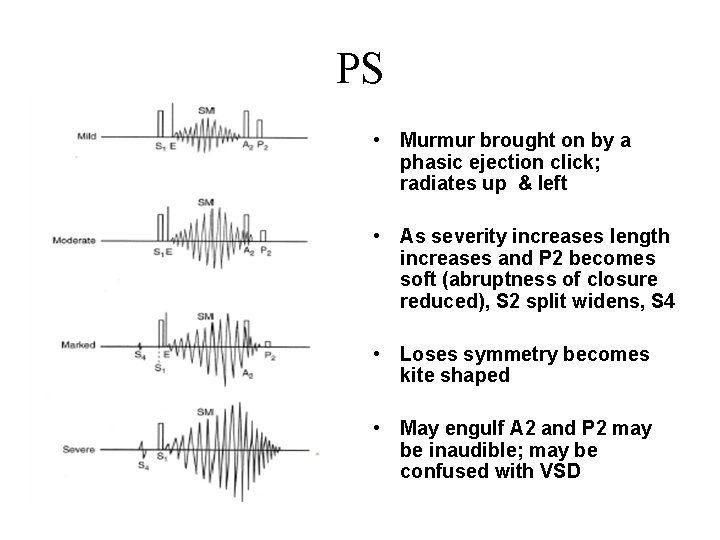
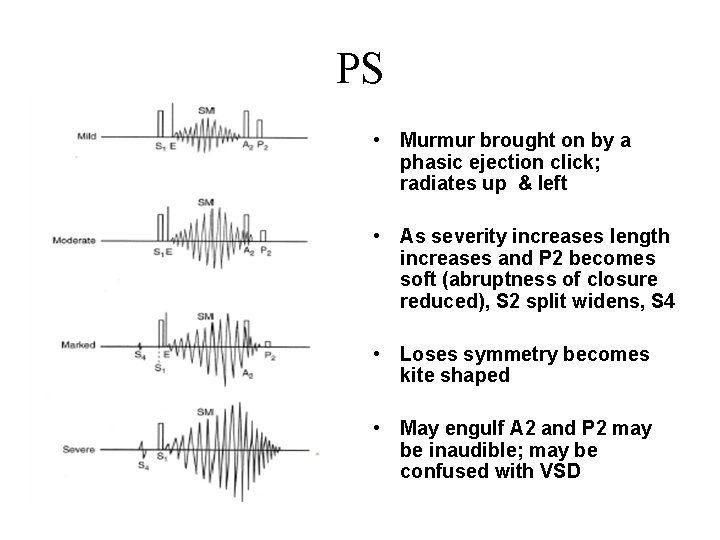
PS • Murmur brought on by a phasic ejection click; radiates up & left • As severity increases length increases and P 2 becomes soft (abruptness of closure reduced), S 2 split widens, S 4 • Loses symmetry becomes kite shaped • May engulf A 2 and P 2 may be inaudible; may be confused with VSD
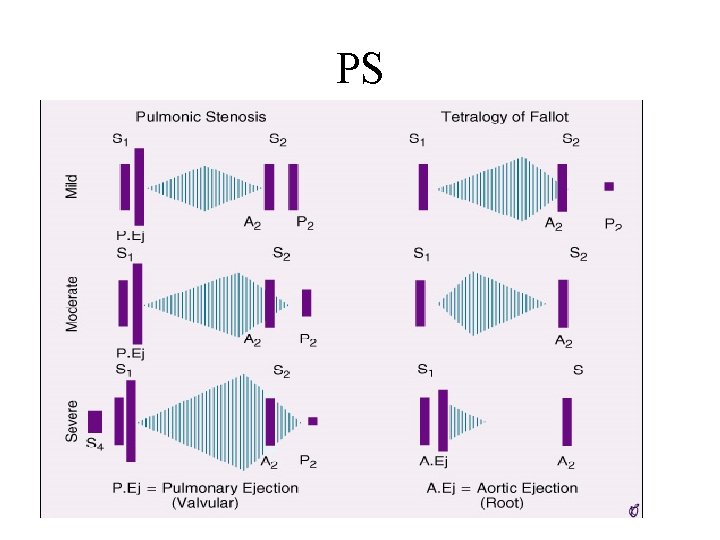
PS
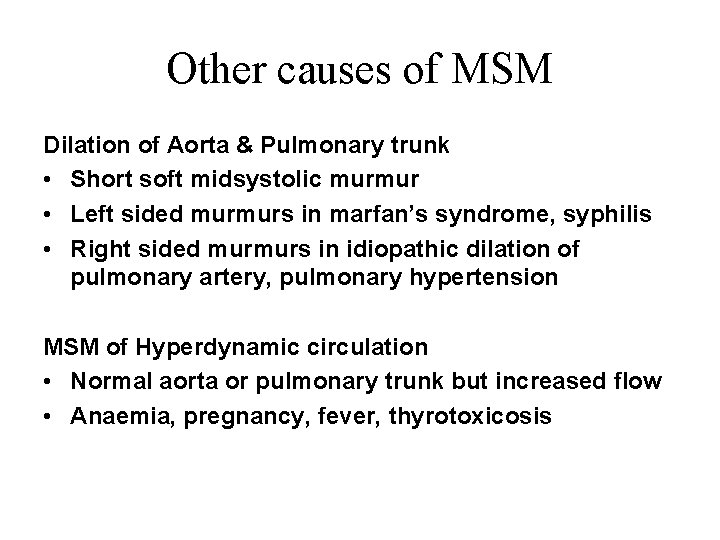
Other causes of MSM Dilation of Aorta & Pulmonary trunk • Short soft midsystolic murmur • Left sided murmurs in marfan’s syndrome, syphilis • Right sided murmurs in idiopathic dilation of pulmonary artery, pulmonary hypertension MSM of Hyperdynamic circulation • Normal aorta or pulmonary trunk but increased flow • Anaemia, pregnancy, fever, thyrotoxicosis
Other causes of MSM OS-ASD • Rapid flow across pulmonary valve to dilated pulmonary trunk Pure AR • Due to Accelerated LV ejection
Physiological causes Innocent systolic murmur • Still’s murmur • Pulmonary mid systolic murmur • Peripheral pulmonary systolic murmur • Supraclavicular or brachiocephalic systolic murmur • Aortic sclerosis • Systolic mammary soufflé
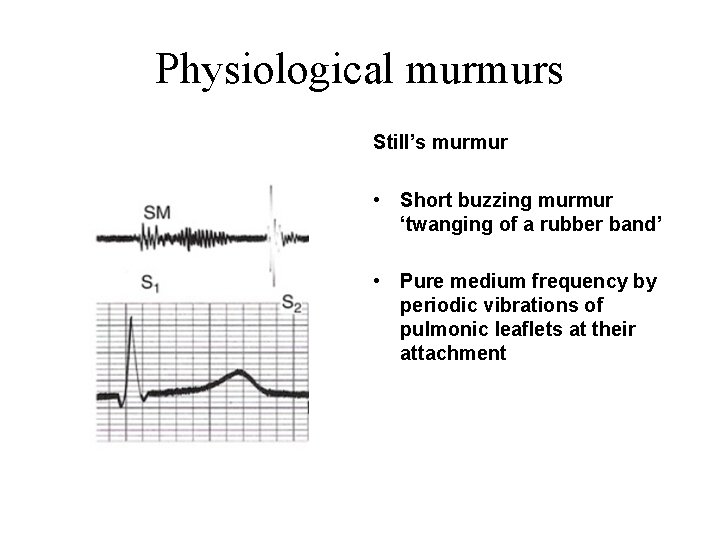
Physiological murmurs Still’s murmur • Short buzzing murmur ‘twanging of a rubber band’ • Pure medium frequency by periodic vibrations of pulmonic leaflets at their attachment
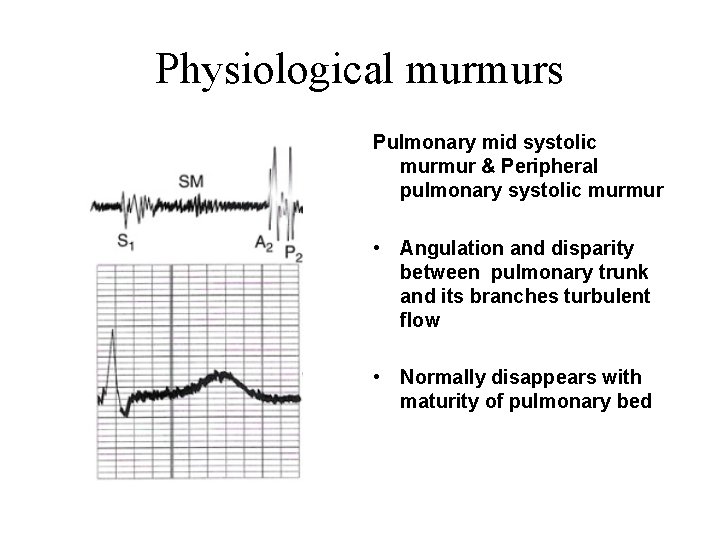
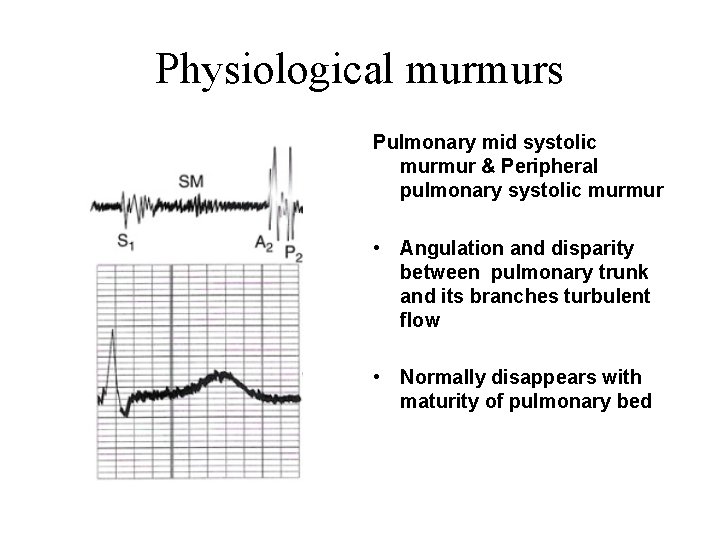
Physiological murmurs Pulmonary mid systolic murmur & Peripheral pulmonary systolic murmur • Angulation and disparity between pulmonary trunk and its branches turbulent flow • Normally disappears with maturity of pulmonary bed
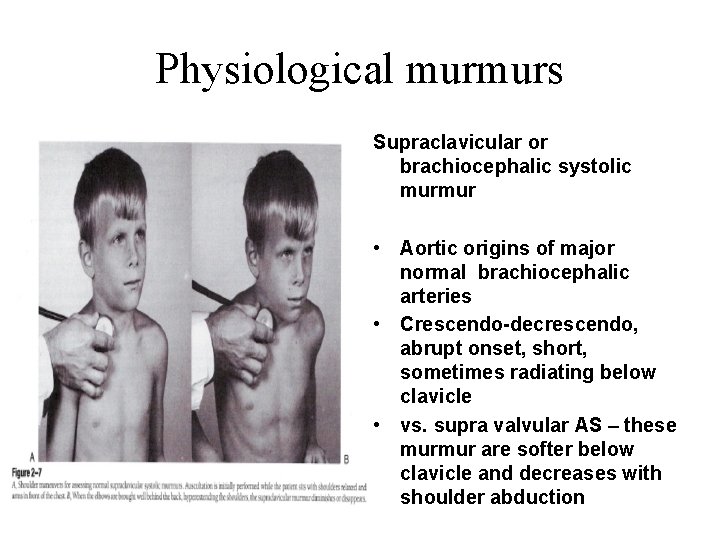
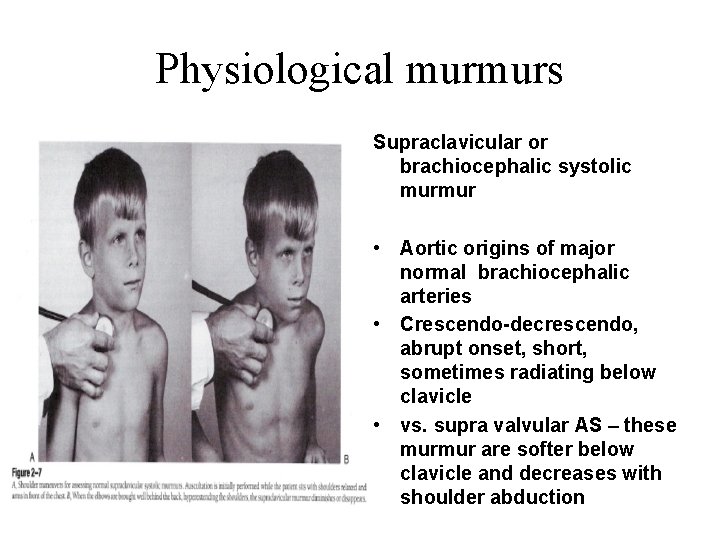
Physiological murmurs Supraclavicular or brachiocephalic systolic murmur • Aortic origins of major normal brachiocephalic arteries • Crescendo-decrescendo, abrupt onset, short, sometimes radiating below clavicle • vs. supra valvular AS – these murmur are softer below clavicle and decreases with shoulder abduction
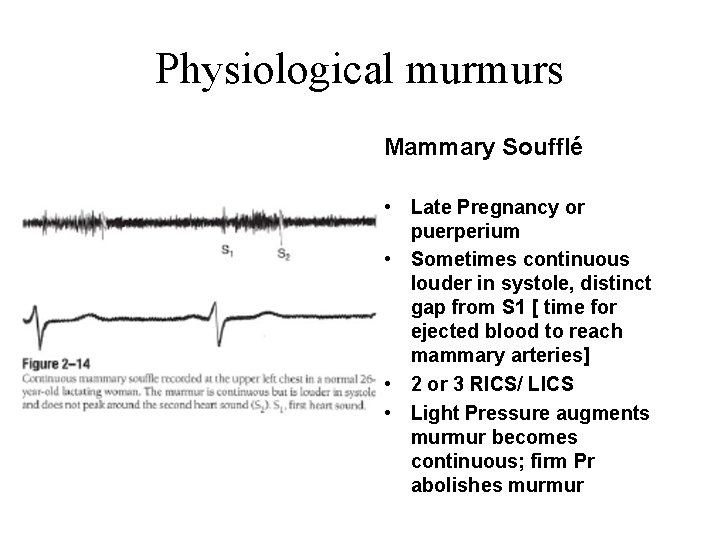
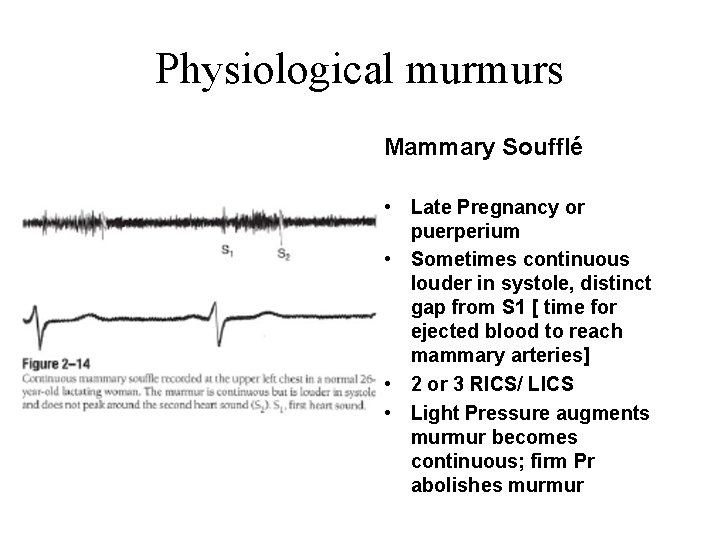
Physiological murmurs Mammary Soufflé • Late Pregnancy or puerperium • Sometimes continuous louder in systole, distinct gap from S 1 [ time for ejected blood to reach mammary arteries] • 2 or 3 RICS/ LICS • Light Pressure augments murmur becomes continuous; firm Pr abolishes murmur
Pan Systolic/ Holo Systolic Murmur Flow from a chamber or vessel whose pressure or resistance throughout systole is higher than pressure or resistance of the chamber receiving the flow • • • Mitral Regurgitation Tricuspid Regurgitation Ventricular Septal Defect Aorto Pulmonary Window Patent Ductus Arteriosus with PAH
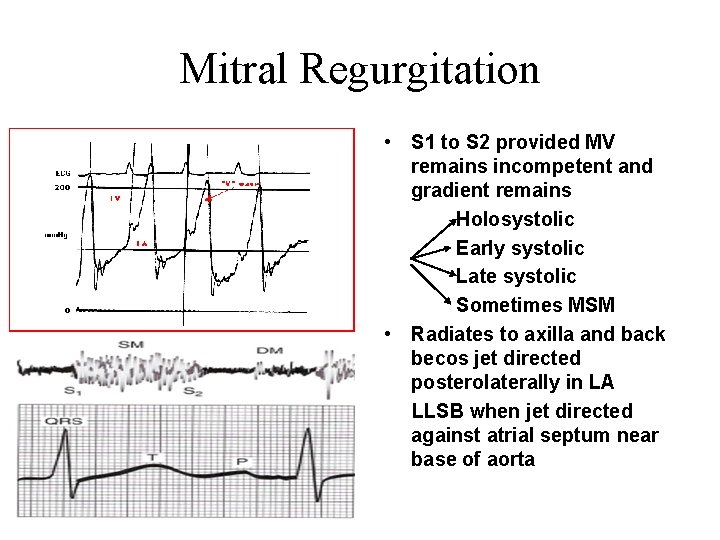
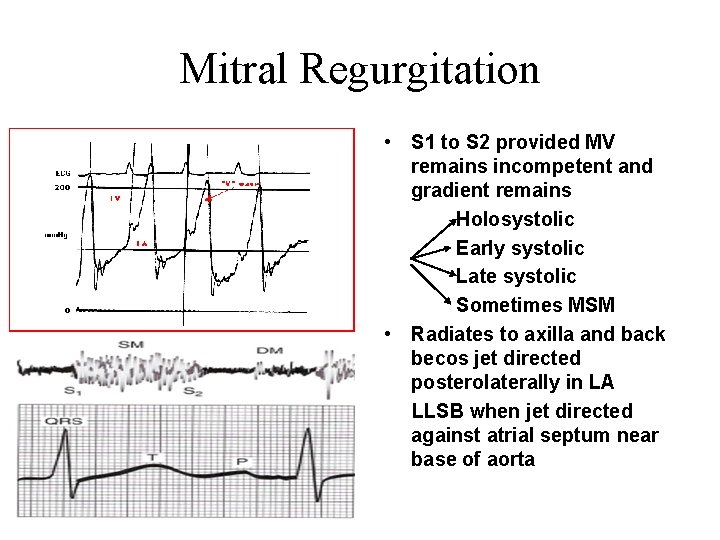
Mitral Regurgitation • S 1 to S 2 provided MV remains incompetent and gradient remains Holosystolic Early systolic Late systolic Sometimes MSM • Radiates to axilla and back becos jet directed posterolaterally in LA LLSB when jet directed against atrial septum near base of aorta
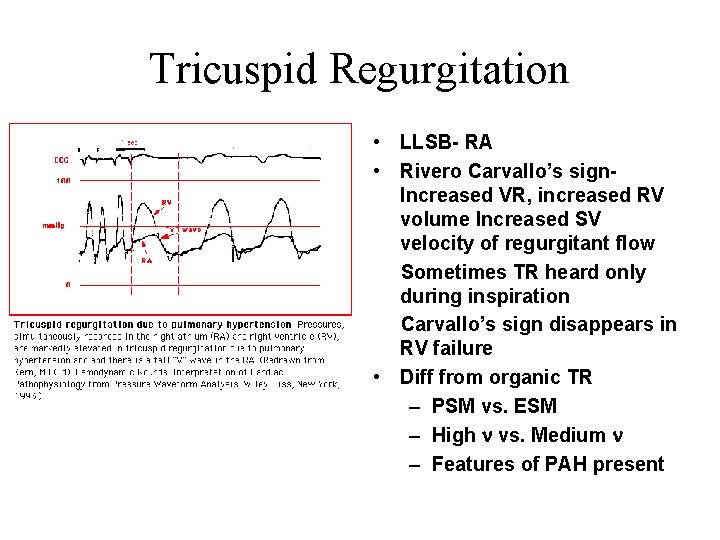
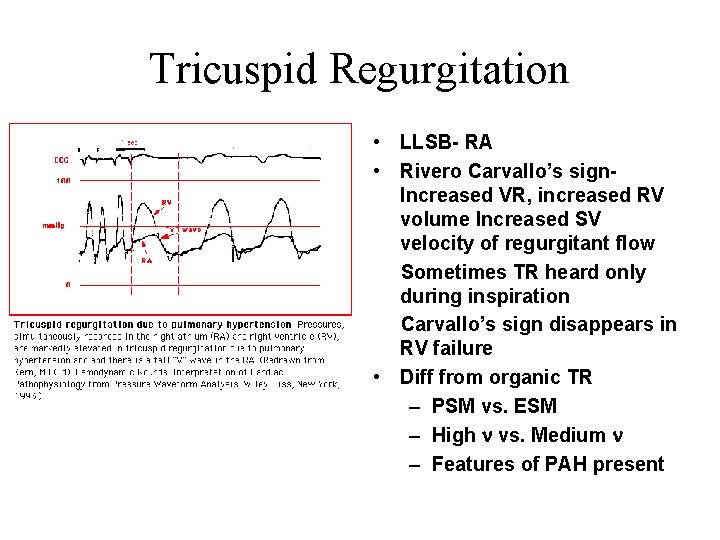
Tricuspid Regurgitation • LLSB- RA • Rivero Carvallo’s sign. Increased VR, increased RV volume Increased SV velocity of regurgitant flow Sometimes TR heard only during inspiration Carvallo’s sign disappears in RV failure • Diff from organic TR – PSM vs. ESM – High n vs. Medium n – Features of PAH present
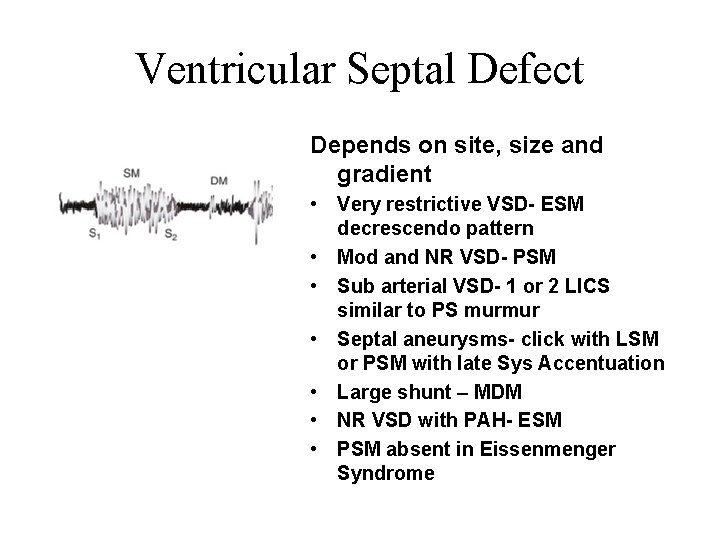
Ventricular Septal Defect Depends on site, size and gradient • Very restrictive VSD- ESM decrescendo pattern • Mod and NR VSD- PSM • Sub arterial VSD- 1 or 2 LICS similar to PS murmur • Septal aneurysms- click with LSM or PSM with late Sys Accentuation • Large shunt – MDM • NR VSD with PAH- ESM • PSM absent in Eissenmenger Syndrome
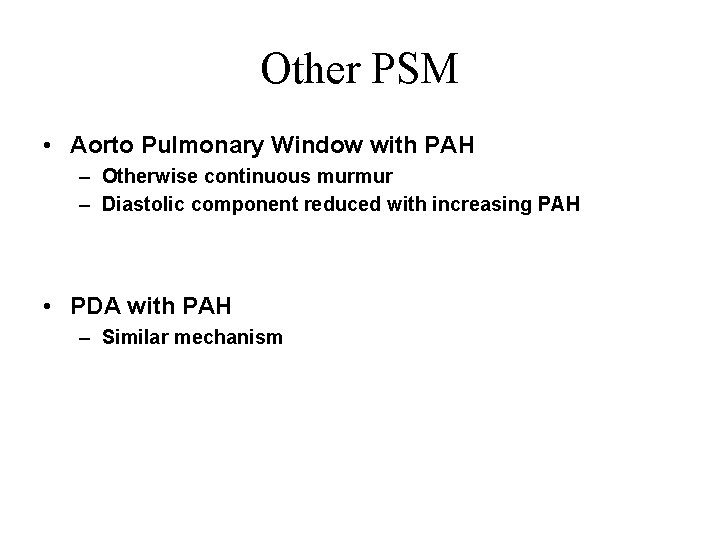
Other PSM • Aorto Pulmonary Window with PAH – Otherwise continuous murmur – Diastolic component reduced with increasing PAH • PDA with PAH – Similar mechanism
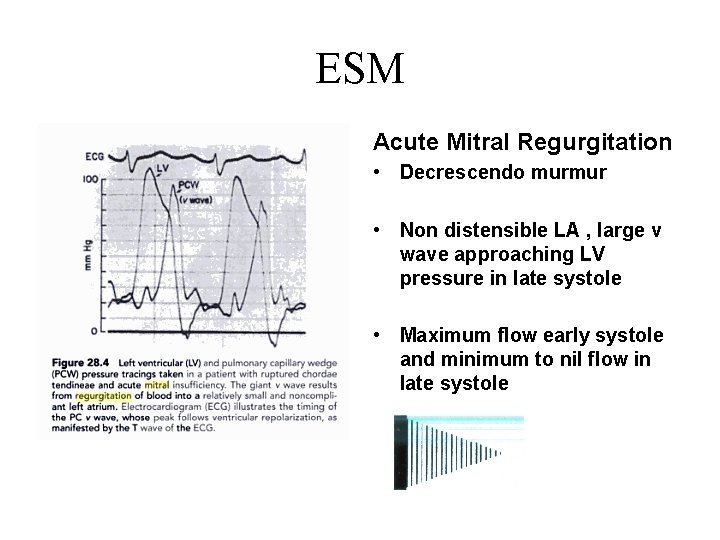
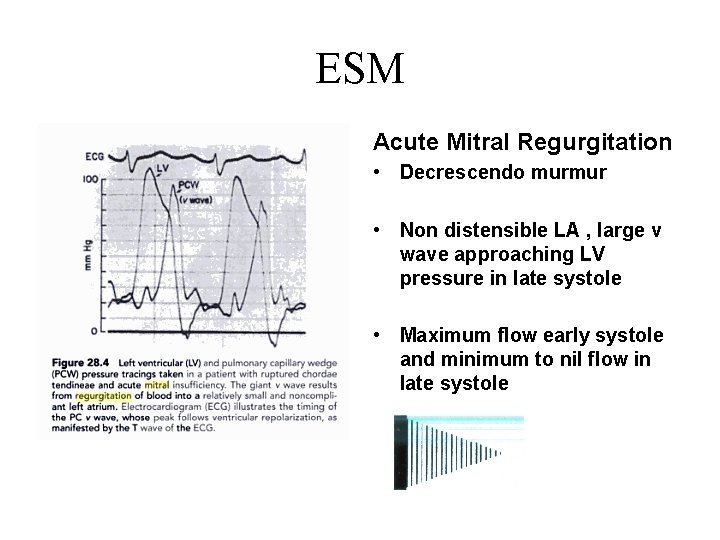
ESM Acute Mitral Regurgitation • Decrescendo murmur • Non distensible LA , large v wave approaching LV pressure in late systole • Maximum flow early systole and minimum to nil flow in late systole
Other ESM • Normal pressure TR, Organic TR Tall RA v waves reach the level of normal RV pressure in late systole, so lower rate of regurgitant flow Moderate to low frequency as compared to high frequency in high pressure TR • VSD with PVR or small muscular VSD -Equalization of pressures in cases of PAH -Small VSD closes in late systole
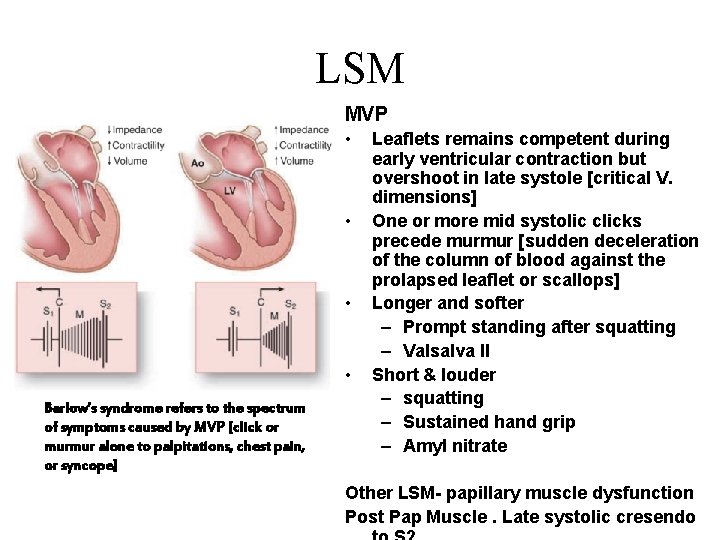
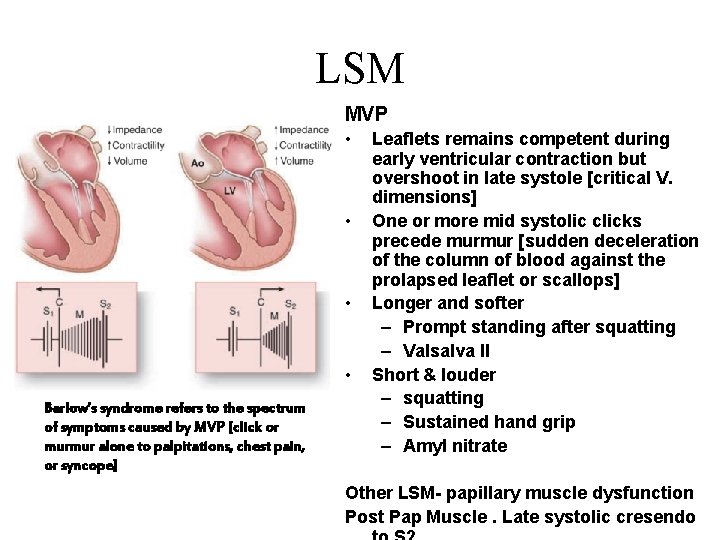
LSM MVP • • Barlow’s syndrome refers to the spectrum of symptoms caused by MVP [click or murmur alone to palpitations, chest pain, or syncope] Leaflets remains competent during early ventricular contraction but overshoot in late systole [critical V. dimensions] One or more mid systolic clicks precede murmur [sudden deceleration of the column of blood against the prolapsed leaflet or scallops] Longer and softer – Prompt standing after squatting – Valsalva II Short & louder – squatting – Sustained hand grip – Amyl nitrate Other LSM- papillary muscle dysfunction Post Pap Muscle. Late systolic cresendo
Diastolic Murmurs

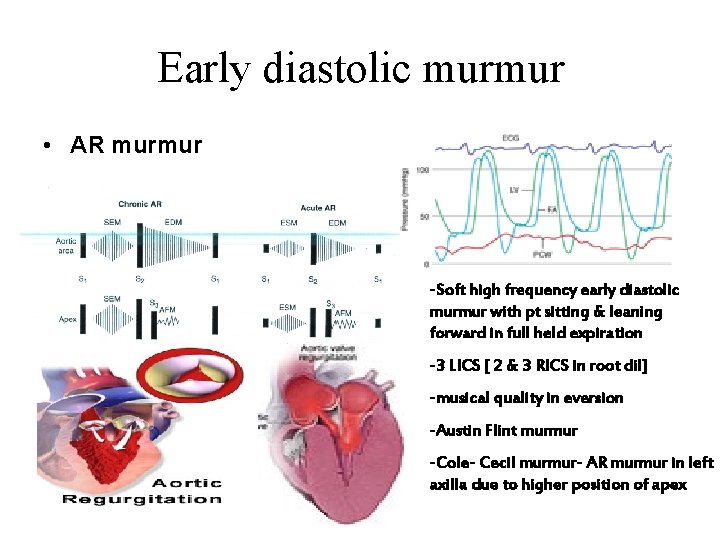
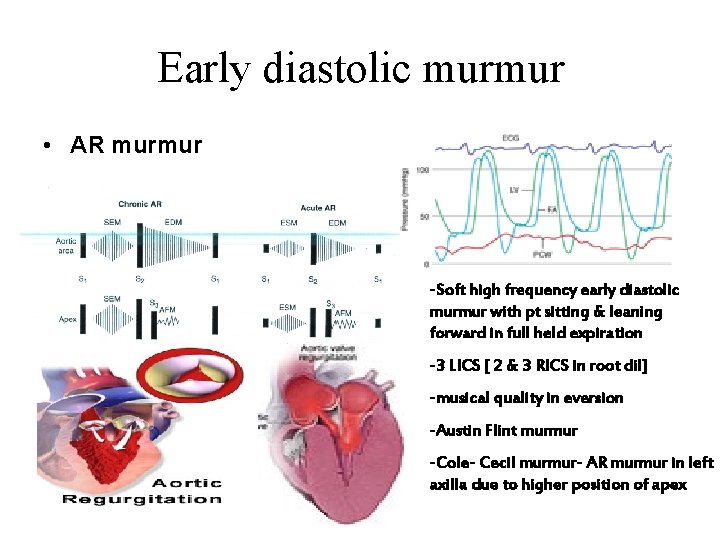
Early diastolic murmur • AR murmur -Soft high frequency early diastolic murmur with pt sitting & leaning forward in full held expiration -3 LICS [ 2 & 3 RICS in root dil] -musical quality in eversion -Austin Flint murmur -Cole- Cecil murmur- AR murmur in left axilla due to higher position of apex
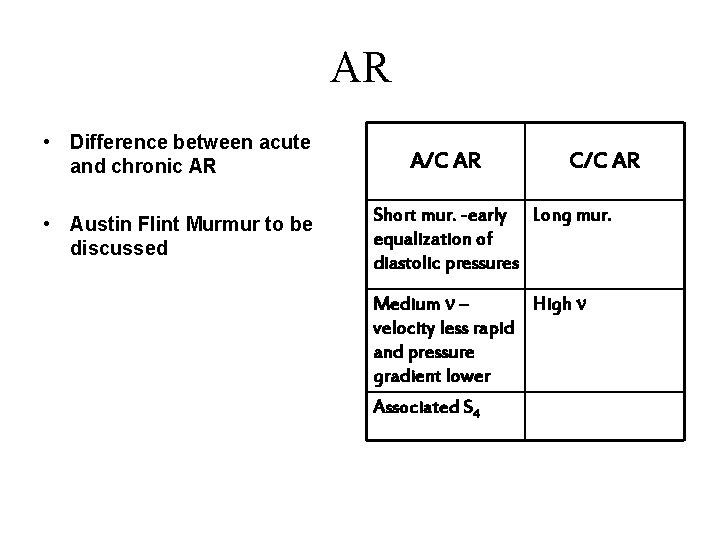
AR • Difference between acute and chronic AR • Austin Flint Murmur to be discussed A/C AR C/C AR Short mur. -early Long mur. equalization of diastolic pressures Medium n – High n velocity less rapid and pressure gradient lower Associated S 4
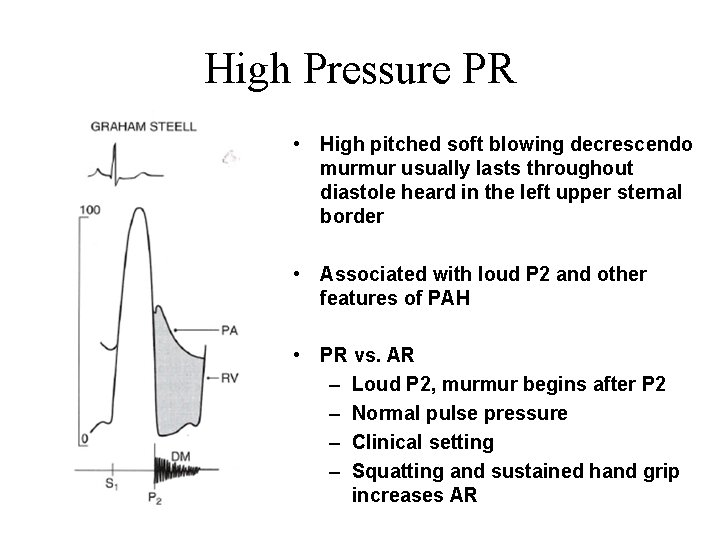
High Pressure PR • High pitched soft blowing decrescendo murmur usually lasts throughout diastole heard in the left upper sternal border • Associated with loud P 2 and other features of PAH • PR vs. AR – Loud P 2, murmur begins after P 2 – Normal pulse pressure – Clinical setting – Squatting and sustained hand grip increases AR
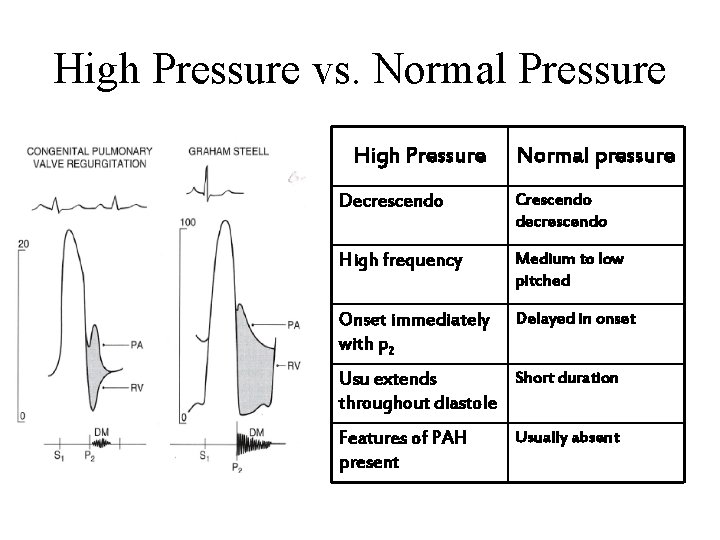
High Pressure vs. Normal Pressure High Pressure Normal pressure Decrescendo Crescendo decrescendo High frequency Medium to low pitched Onset immediately with p 2 Delayed in onset Short duration Usu extends throughout diastole Features of PAH present Usually absent
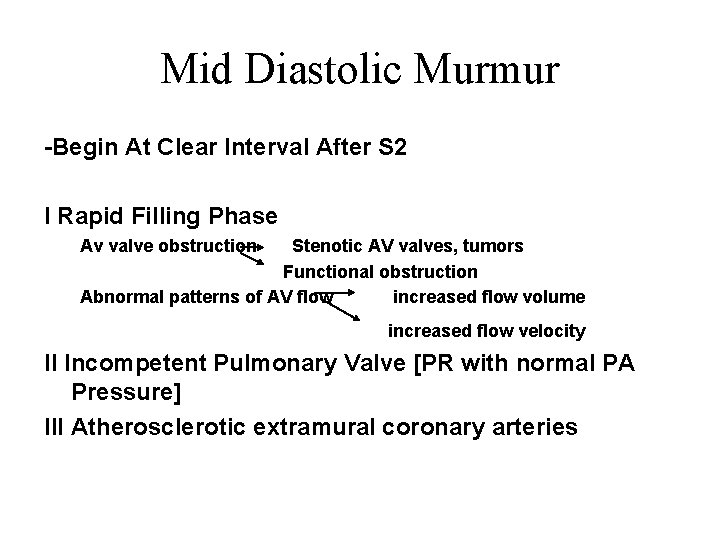
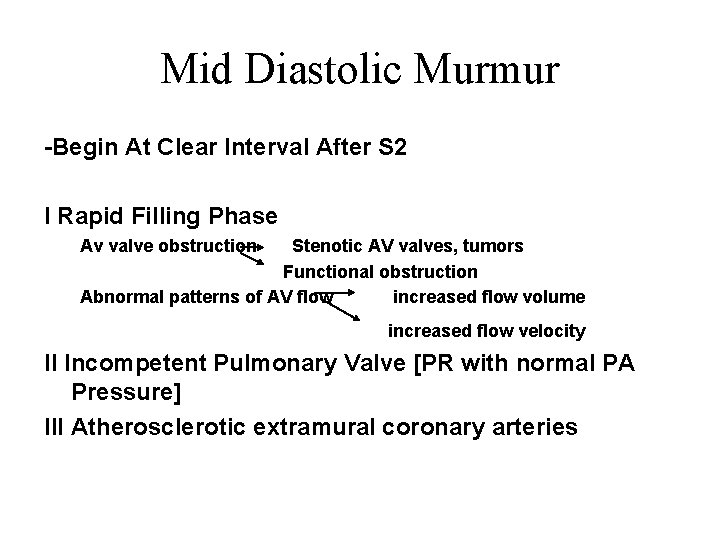
Mid Diastolic Murmur -Begin At Clear Interval After S 2 I Rapid Filling Phase Av valve obstruction Stenotic AV valves, tumors Functional obstruction Abnormal patterns of AV flow increased flow volume increased flow velocity II Incompetent Pulmonary Valve [PR with normal PA Pressure] III Atherosclerotic extramural coronary arteries
Mid Diastolic Murmur RV LV - TS - TR - MS - ASD - Carey-Comb's - Austin Flint murmur - VSD - PDA - MR OTHERS -Atrial Myxoma
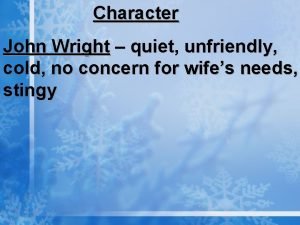
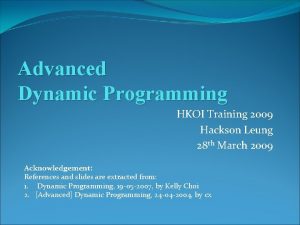
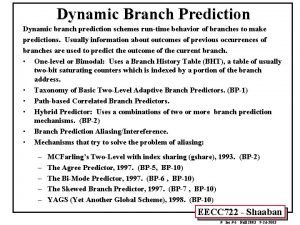
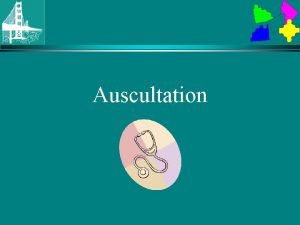
![MS Low n rough rumbling sound of distant thunder MDM Localized to MS • Low n rough rumbling [sound of distant thunder] MDM • Localized to](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-53.jpg)
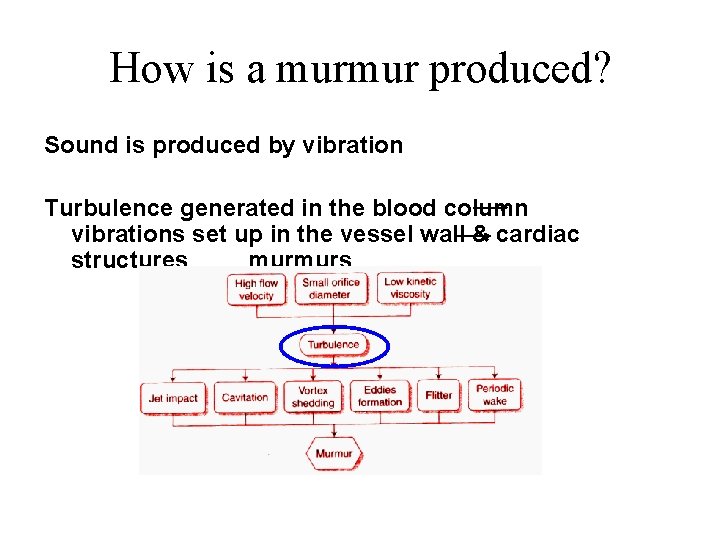
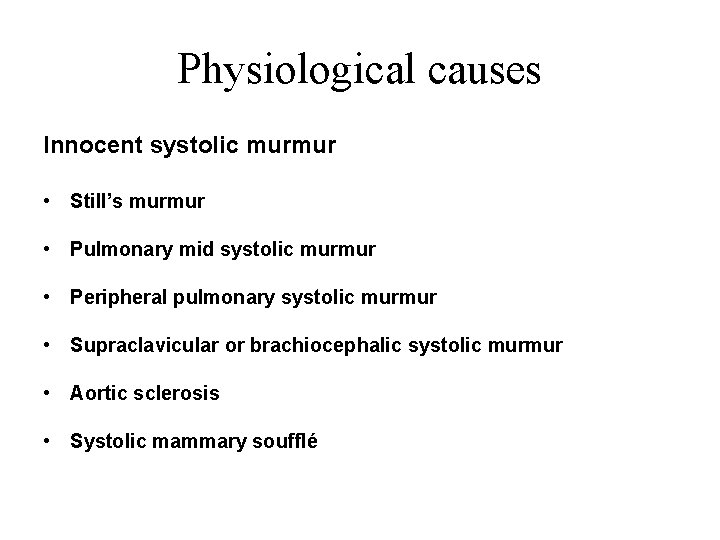
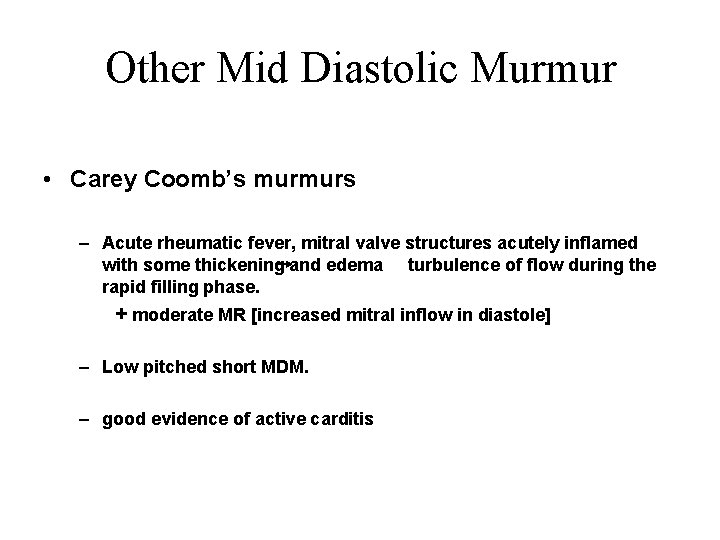
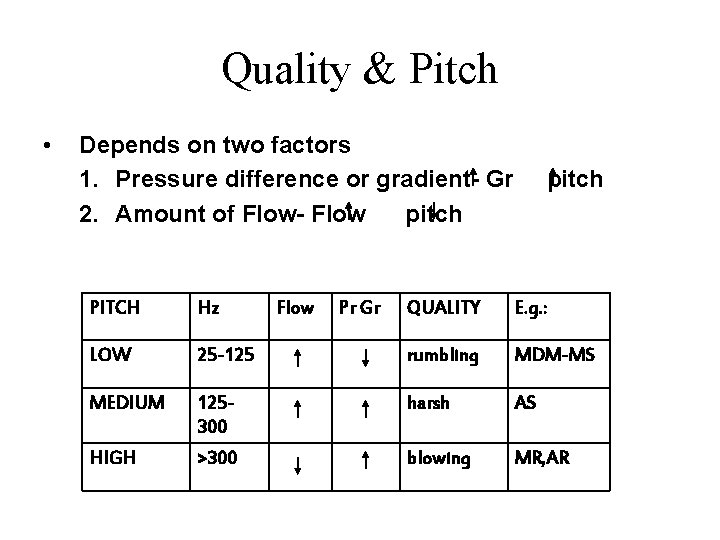
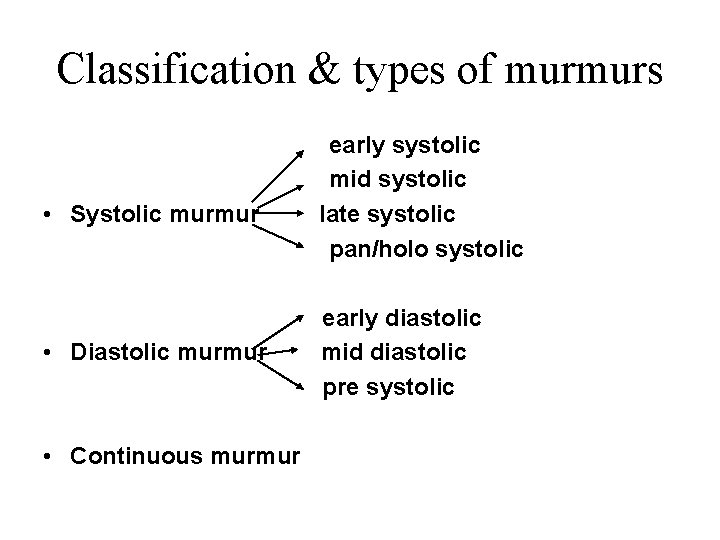
MS • Low n rough rumbling [sound of distant thunder] MDM • Localized to apex, better heard in left lateral position with bell • Length a severity • Long murmurs up to S 1 even in long cycles of AF- severe MS • Late diastolic or Pre systolic accentuation usually seen in pliable valves and in NSR [ sometimes in AF]
TS • Similar to MS • Murmur usually seen associated with AF • Diff. from MS – Increases during inspiration [Augmentation of RV volume, RV Diastolic Pr. , Flow rate and gradient across valve] – LLSB
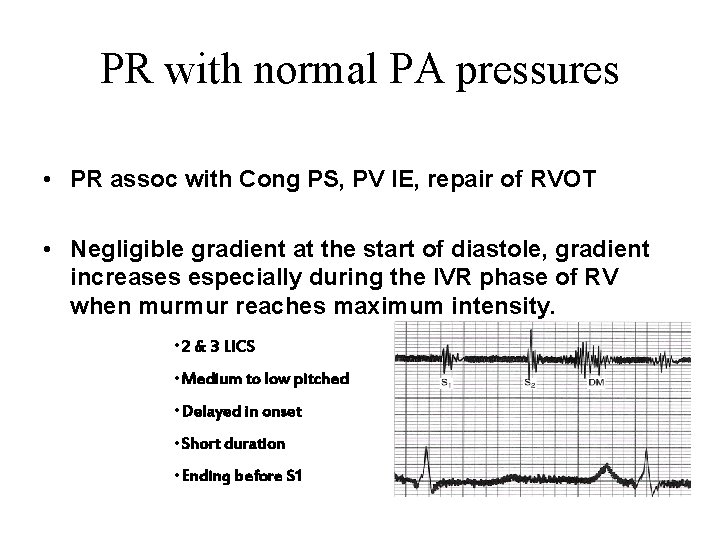
PR with normal PA pressures • PR assoc with Cong PS, PV IE, repair of RVOT • Negligible gradient at the start of diastole, gradient increases especially during the IVR phase of RV when murmur reaches maximum intensity. • 2 & 3 LICS • Medium to low pitched • Delayed in onset • Short duration • Ending before S 1
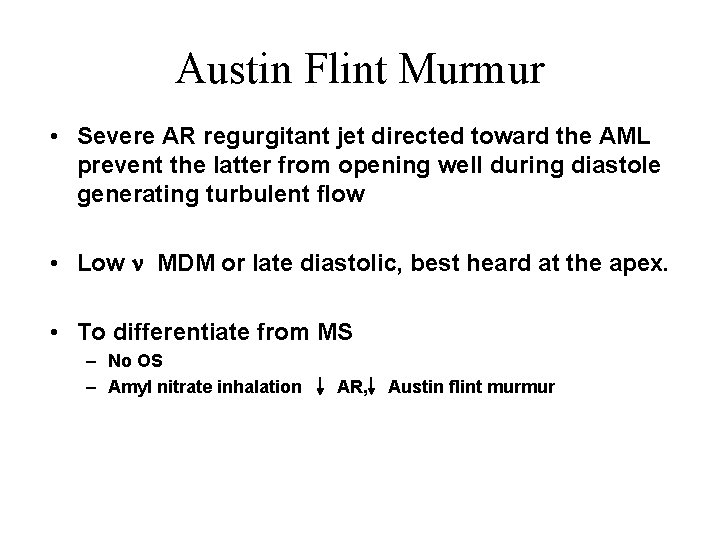
Austin Flint Murmur • Severe AR regurgitant jet directed toward the AML prevent the latter from opening well during diastole generating turbulent flow • Low n MDM or late diastolic, best heard at the apex. • To differentiate from MS – No OS – Amyl nitrate inhalation AR, Austin flint murmur
Other Mid Diastolic Murmur • Carey Coomb’s murmurs – Acute rheumatic fever, mitral valve structures acutely inflamed with some thickening and edema turbulence of flow during the rapid filling phase. + moderate MR [increased mitral inflow in diastole] – Low pitched short MDM. – good evidence of active carditis
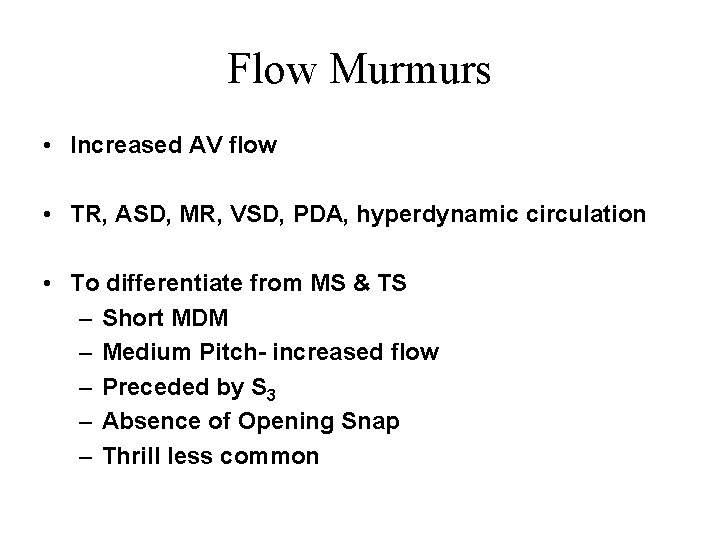
Flow Murmurs • Increased AV flow • TR, ASD, MR, VSD, PDA, hyperdynamic circulation • To differentiate from MS & TS – Short MDM – Medium Pitch- increased flow – Preceded by S 3 – Absence of Opening Snap – Thrill less common
Late Diastolic/ Pre-systolic Murmurs MS • Higher frequency than MDM • Sometimes only PSA heard- mild MS • Generally absent in calcified valves and most of AF [ may be present during short cycle lengths in AF] • Cause– Increased flow during atrial contraction in late systole – Increased dp/dt of LV contraction increases turbulence [ esp. in AF short cycles]
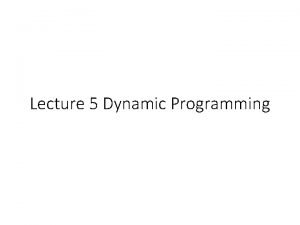
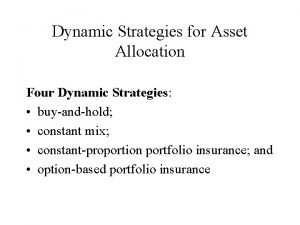
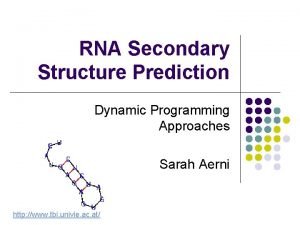
![Other diastolic murmurs Cabot Locke Murmur Diastolic Flow murmur The CabotLocke murmur Other diastolic murmurs • Cabot– Locke Murmur- [Diastolic Flow murmur] – The Cabot–Locke murmur](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-60.jpg)
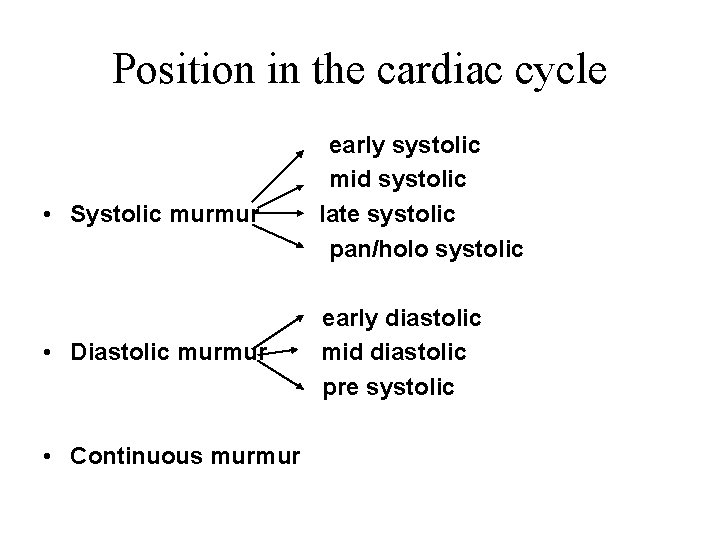
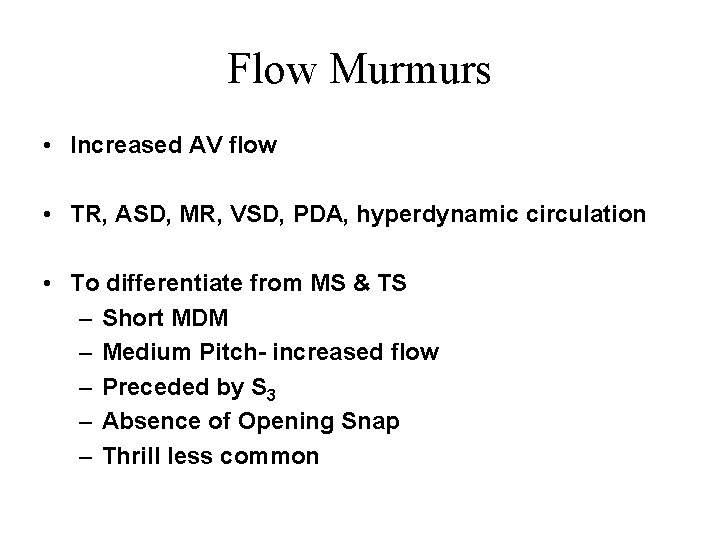
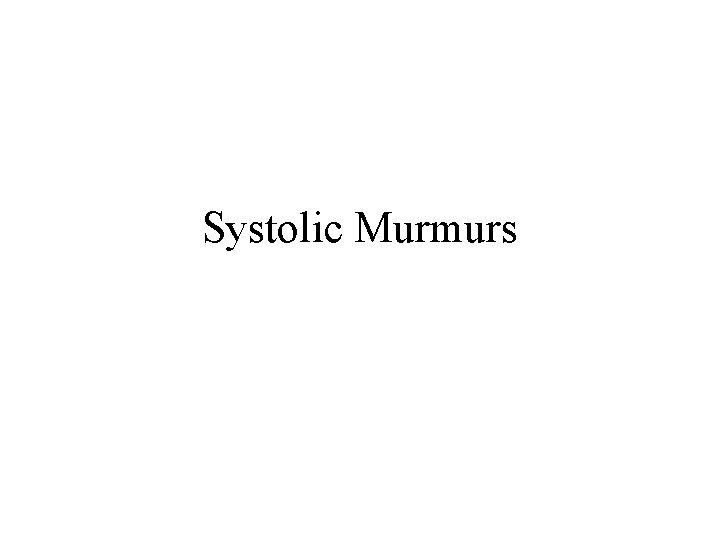
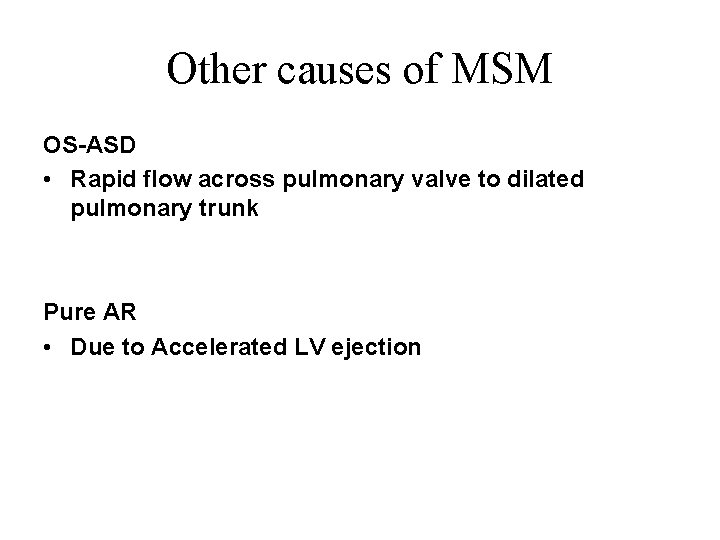
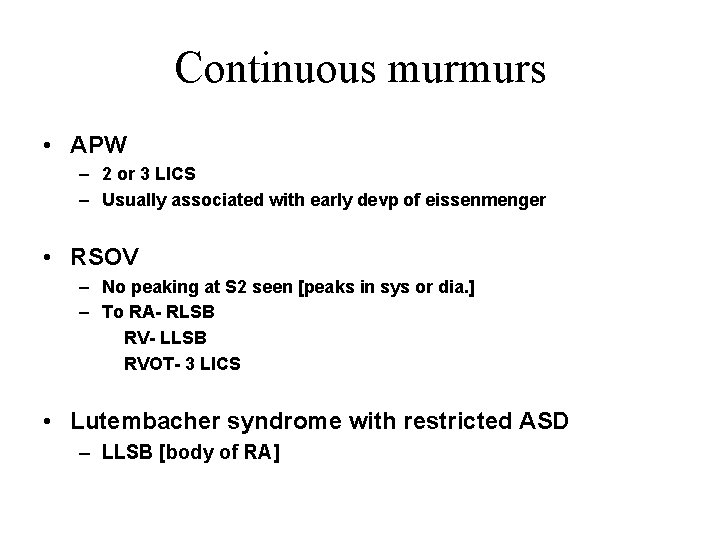
Other diastolic murmurs • Cabot– Locke Murmur- [Diastolic Flow murmur] – The Cabot–Locke murmur is a diastolic murmur that sounds similar to aortic insufficiency but does not have a decrescendo; it is heard best at the left sternal border. [High flow thru coronary vessels, LMCA, LAD] – The murmur resolves with treatment of anaemia. • Dock’s murmur – diastolic crescendo-decrescendo, with late accentuation, [consistent with blood flow through the coronary] in a sharply localized area, 4 cm left of the sternum in the 3 LICS, detectable only when the patient was sitting upright. – Due to stenosis of LAD
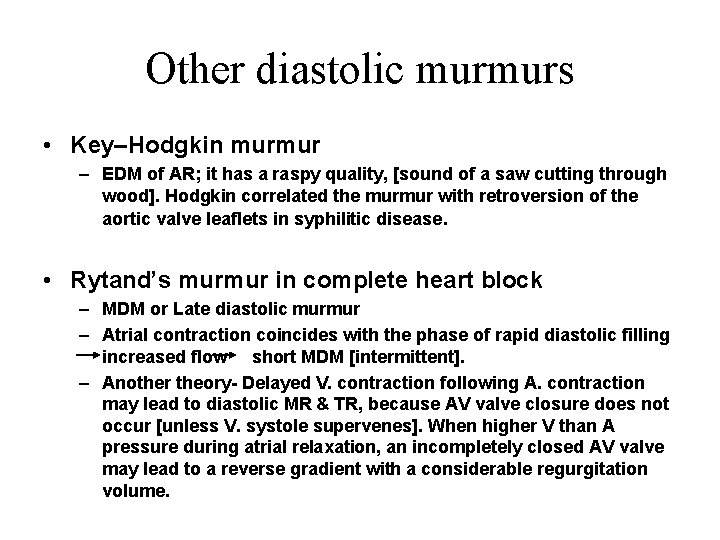
Other diastolic murmurs • Key–Hodgkin murmur – EDM of AR; it has a raspy quality, [sound of a saw cutting through wood]. Hodgkin correlated the murmur with retroversion of the aortic valve leaflets in syphilitic disease. • Rytand’s murmur in complete heart block – MDM or Late diastolic murmur – Atrial contraction coincides with the phase of rapid diastolic filling increased flow short MDM [intermittent]. – Another theory- Delayed V. contraction following A. contraction may lead to diastolic MR & TR, because AV valve closure does not occur [unless V. systole supervenes]. When higher V than A pressure during atrial relaxation, an incompletely closed AV valve may lead to a reverse gradient with a considerable regurgitation volume.
Continuous murmur
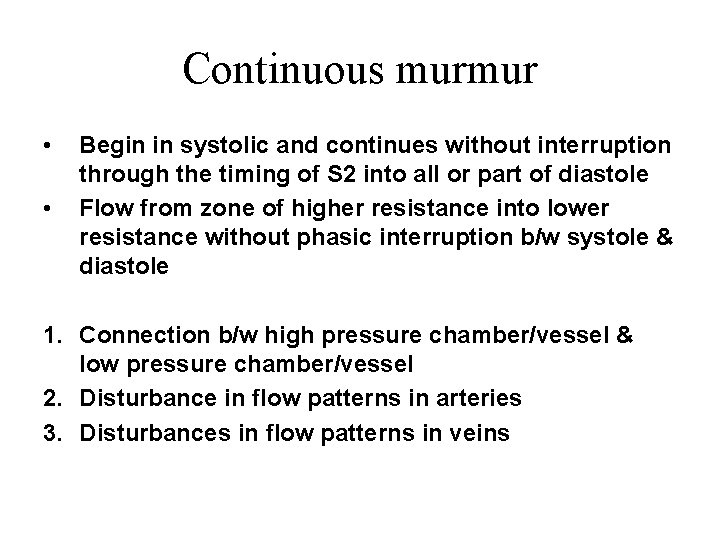
Continuous murmur • • Begin in systolic and continues without interruption through the timing of S 2 into all or part of diastole Flow from zone of higher resistance into lower resistance without phasic interruption b/w systole & diastole 1. Connection b/w high pressure chamber/vessel & low pressure chamber/vessel 2. Disturbance in flow patterns in arteries 3. Disturbances in flow patterns in veins
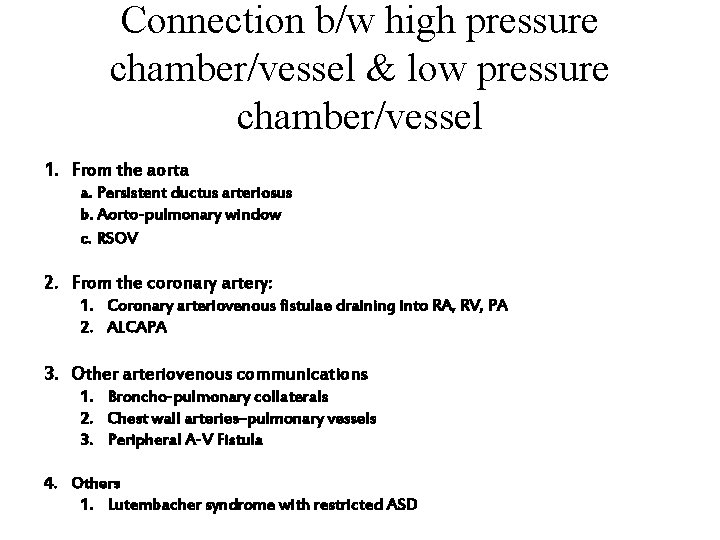
Connection b/w high pressure chamber/vessel & low pressure chamber/vessel 1. From the aorta a. Persistent ductus arteriosus b. Aorto-pulmonary window c. RSOV 2. From the coronary artery: 1. Coronary arteriovenous fistulae draining into RA, RV, PA 2. ALCAPA 3. Other arteriovenous communications 1. Broncho-pulmonary collaterals 2. Chest wall arteries–pulmonary vessels 3. Peripheral A-V Fistula 4. Others 1. Lutembacher syndrome with restricted ASD
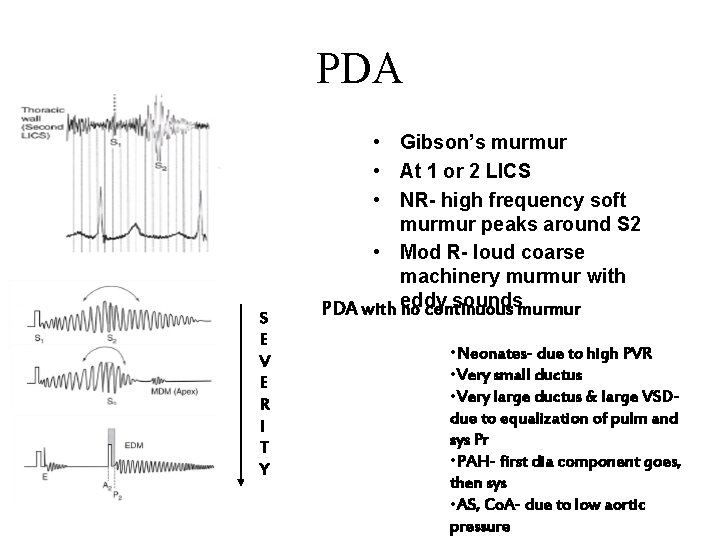
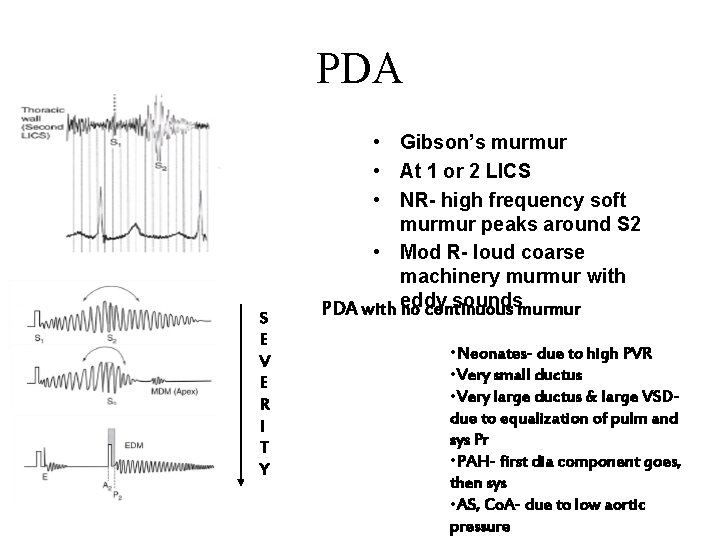
PDA S E V E R I T Y • Gibson’s murmur • At 1 or 2 LICS • NR- high frequency soft murmur peaks around S 2 • Mod R- loud coarse machinery murmur with soundsmurmur PDA with eddy no continuous • Neonates- due to high PVR • Very small ductus • Very large ductus & large VSDdue to equalization of pulm and sys Pr • PAH- first dia component goes, then sys • AS, Co. A- due to low aortic pressure
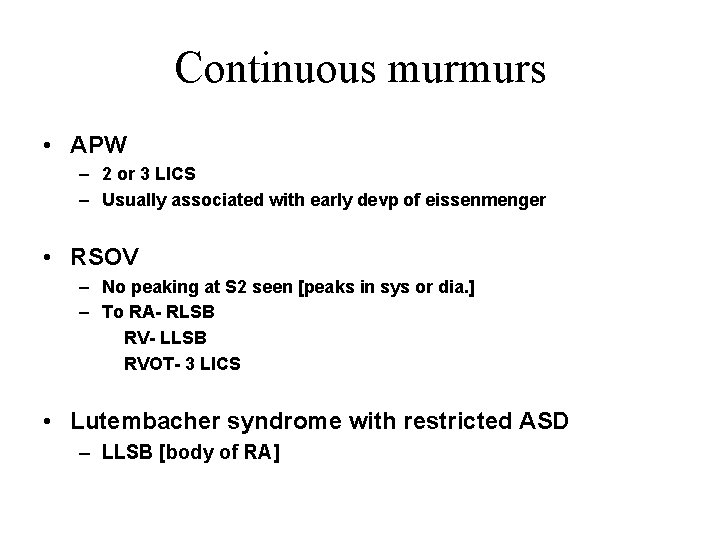
Continuous murmurs • APW – 2 or 3 LICS – Usually associated with early devp of eissenmenger • RSOV – No peaking at S 2 seen [peaks in sys or dia. ] – To RA- RLSB RV- LLSB RVOT- 3 LICS • Lutembacher syndrome with restricted ASD – LLSB [body of RA]
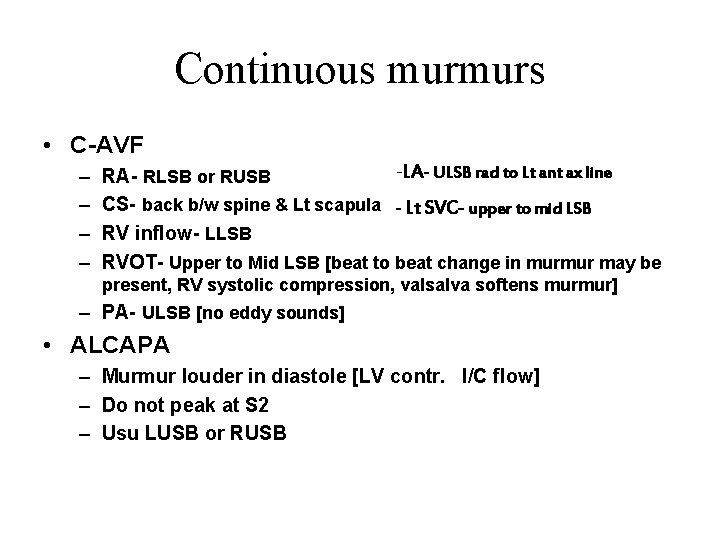
Continuous murmurs • C-AVF – – -LA- ULSB rad to Lt ant ax line RA- RLSB or RUSB CS- back b/w spine & Lt scapula - Lt SVC- upper to mid LSB RV inflow- LLSB RVOT- Upper to Mid LSB [beat to beat change in murmur may be present, RV systolic compression, valsalva softens murmur] – PA- ULSB [no eddy sounds] • ALCAPA – Murmur louder in diastole [LV contr. I/C flow] – Do not peak at S 2 – Usu LUSB or RUSB
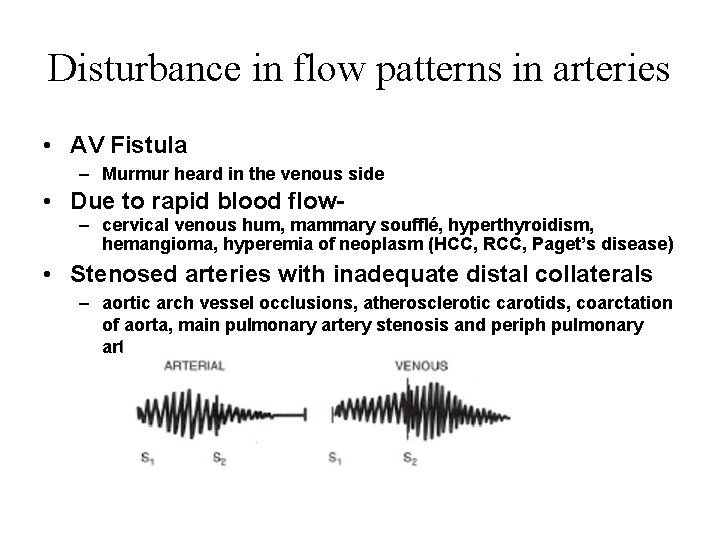
Disturbance in flow patterns in arteries • AV Fistula – Murmur heard in the venous side • Due to rapid blood flow– cervical venous hum, mammary soufflé, hyperthyroidism, hemangioma, hyperemia of neoplasm (HCC, RCC, Paget’s disease) • Stenosed arteries with inadequate distal collaterals – aortic arch vessel occlusions, atherosclerotic carotids, coarctation of aorta, main pulmonary artery stenosis and periph pulmonary artery stenosis
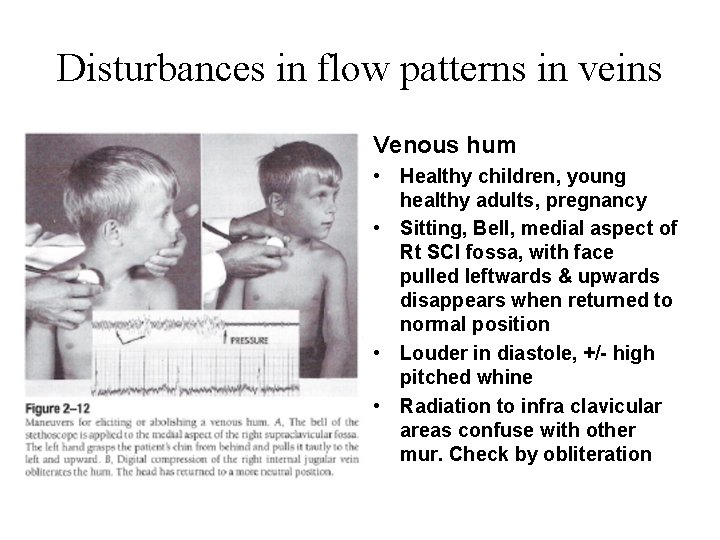
Disturbances in flow patterns in veins Venous hum • Healthy children, young healthy adults, pregnancy • Sitting, Bell, medial aspect of Rt SCl fossa, with face pulled leftwards & upwards disappears when returned to normal position • Louder in diastole, +/- high pitched whine • Radiation to infra clavicular areas confuse with other mur. Check by obliteration
Dynamic Auscultation
Dynamic Auscultation It refers to the technique of altering circulatory dynamics by a variety of physiological and pharmacological maneuvers and determining the effects of these maneuvers on heart sounds and murmurs.
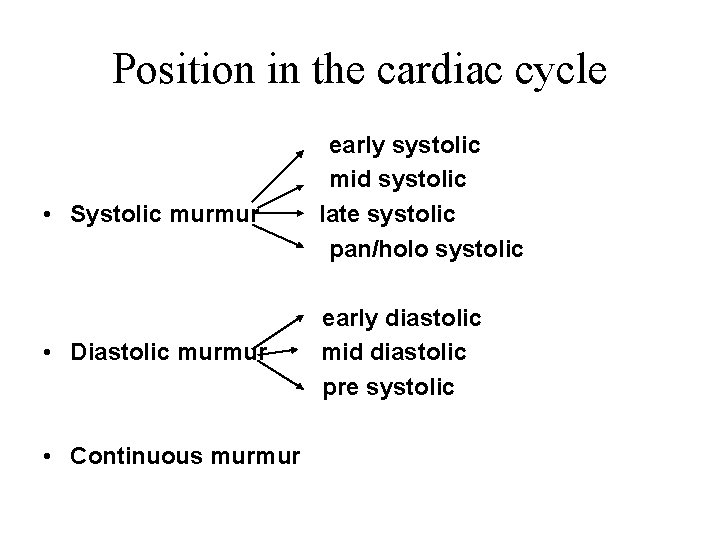
Intervention • Position • Physical maneuvers • Pharmacological
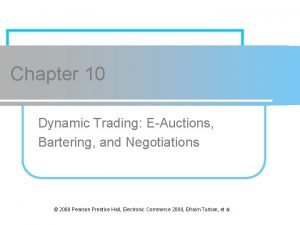
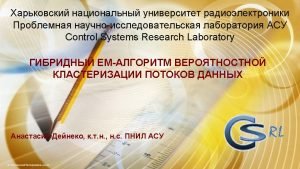
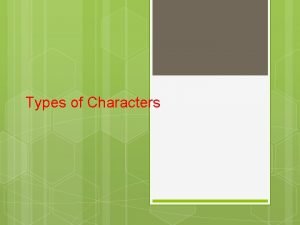
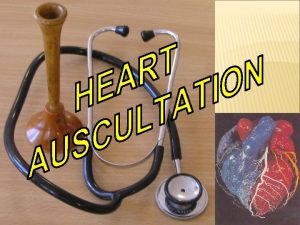
![Position A Lt Lateral Decubitus LV impulse apical sounds murmurs better heard Act of Position A. Lt Lateral Decubitus LV impulse [apical sounds, murmurs better heard] Act of](https://slidetodoc.com/presentation_image_h2/c9489504df04427585303d0242cad60f/image-73.jpg)
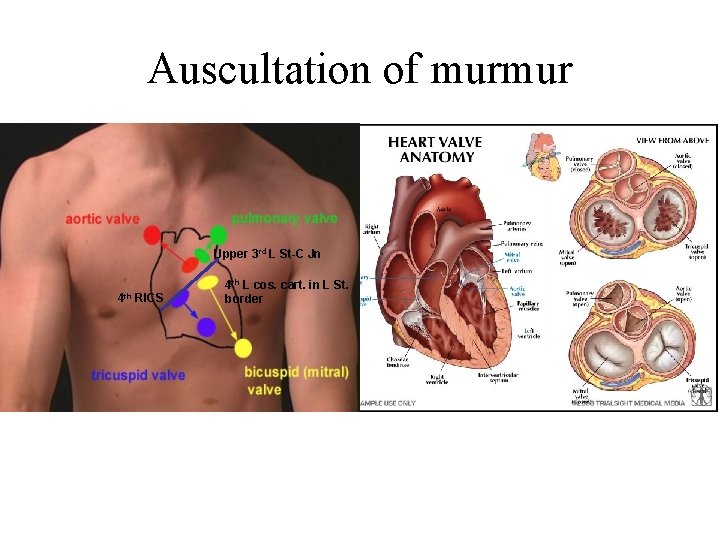
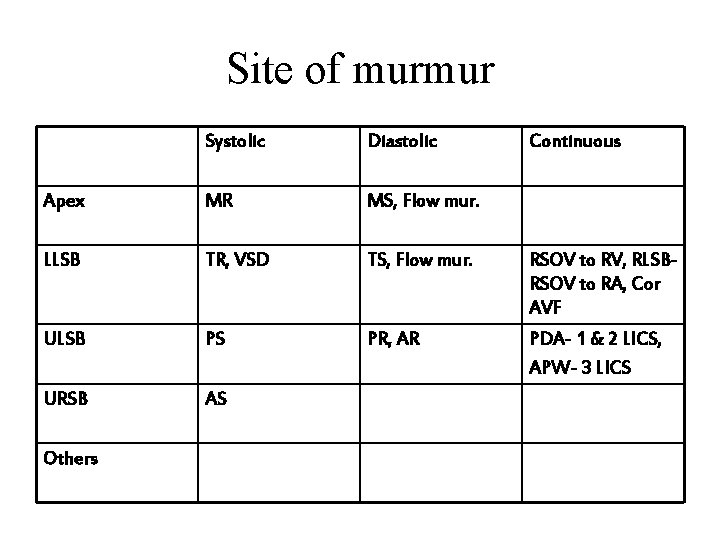
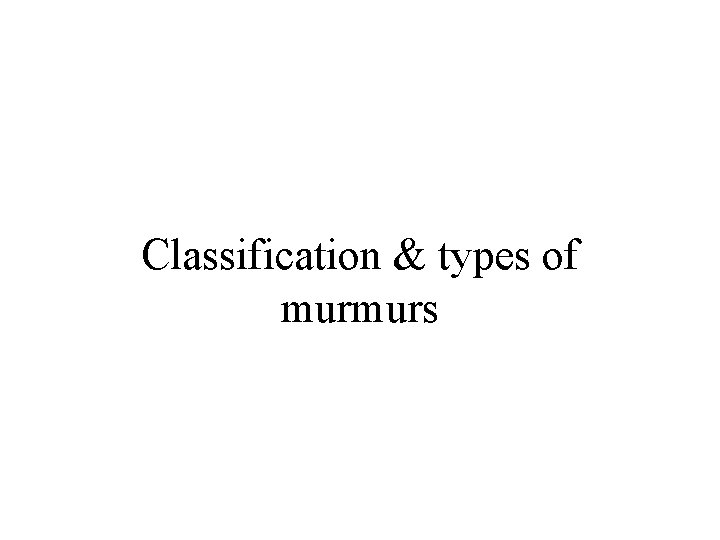
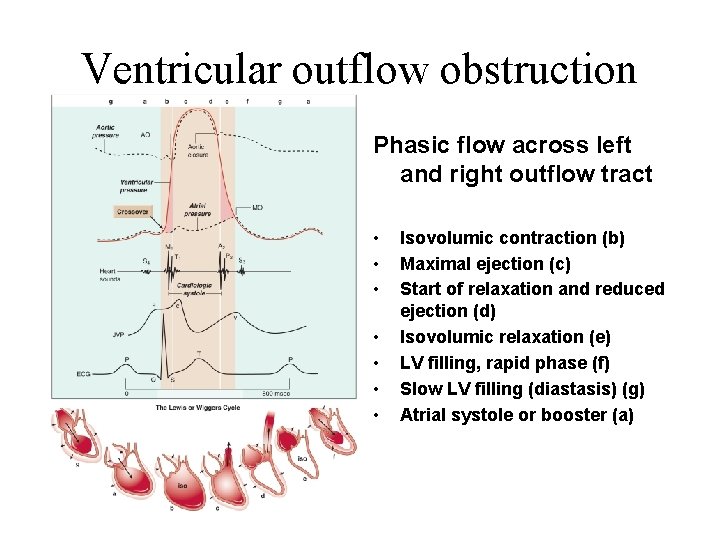
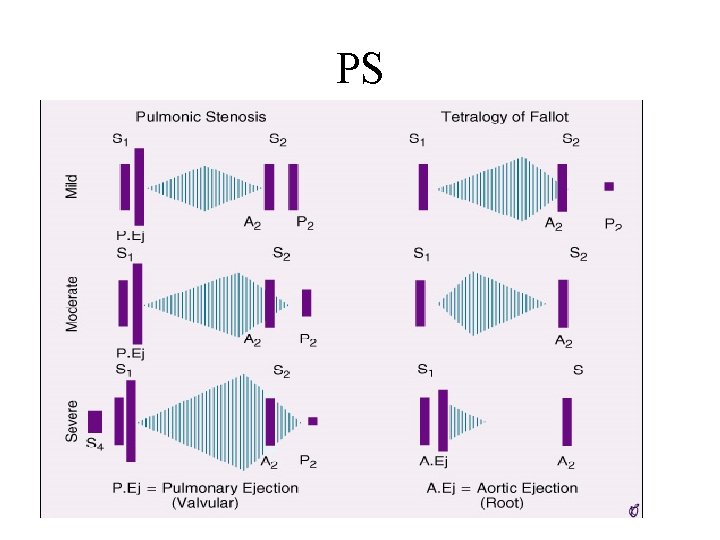
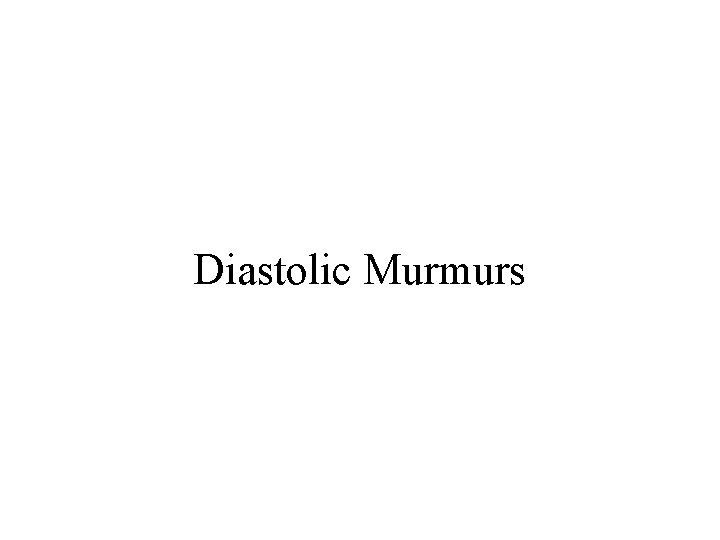
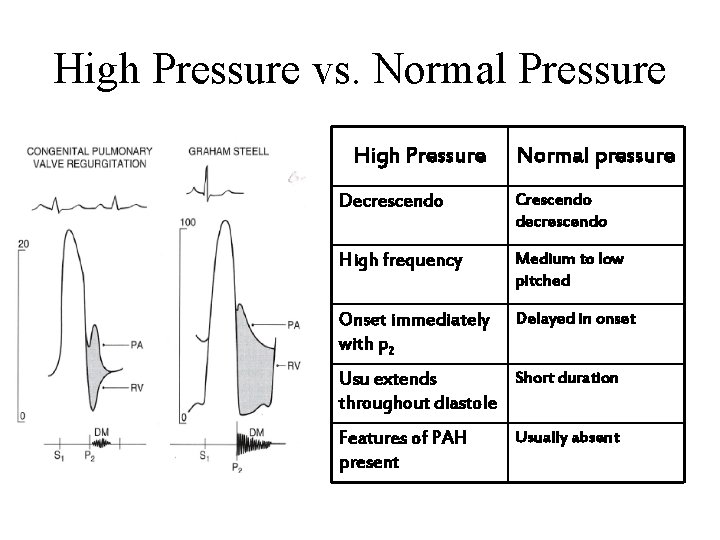
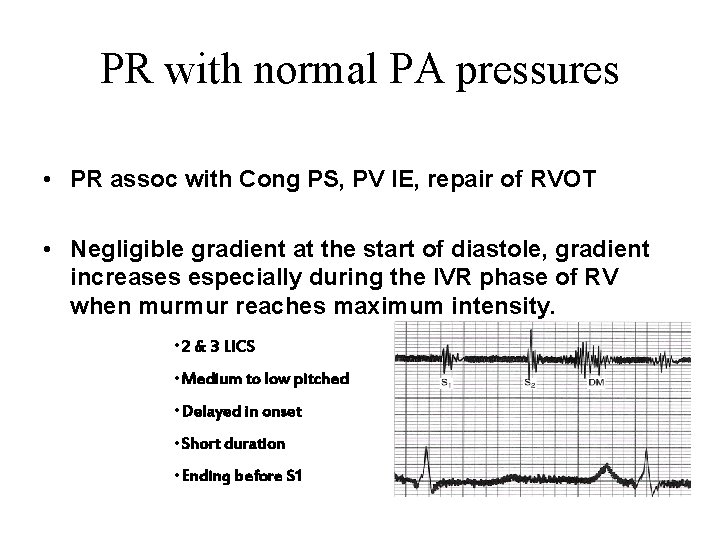
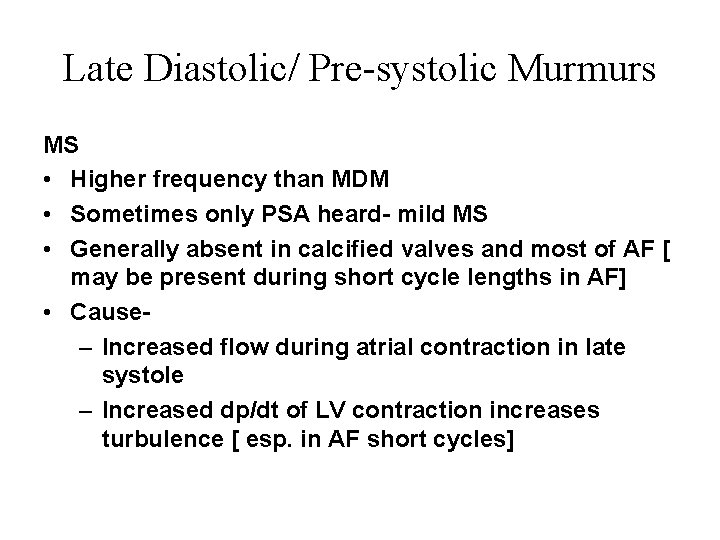
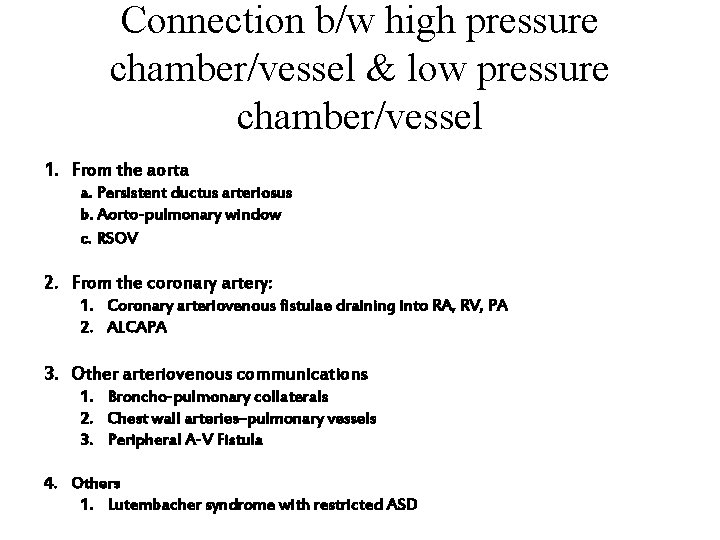
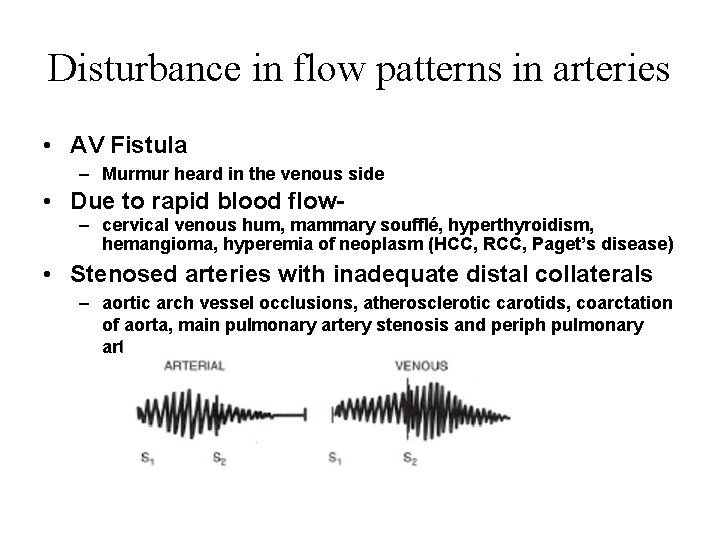
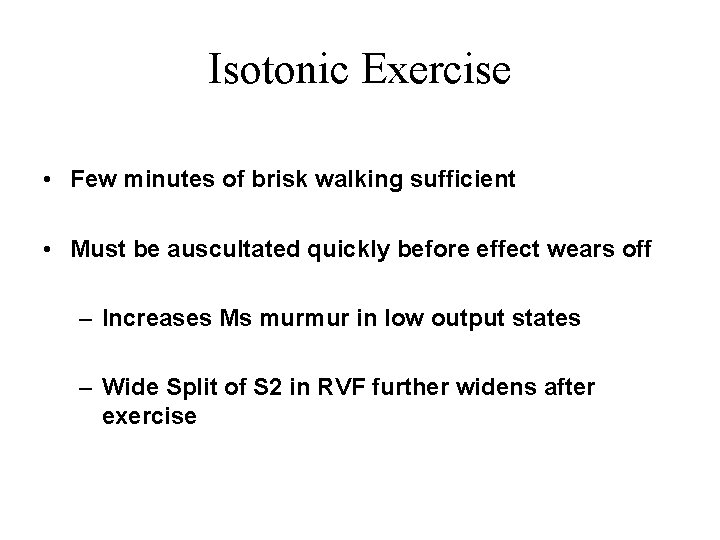
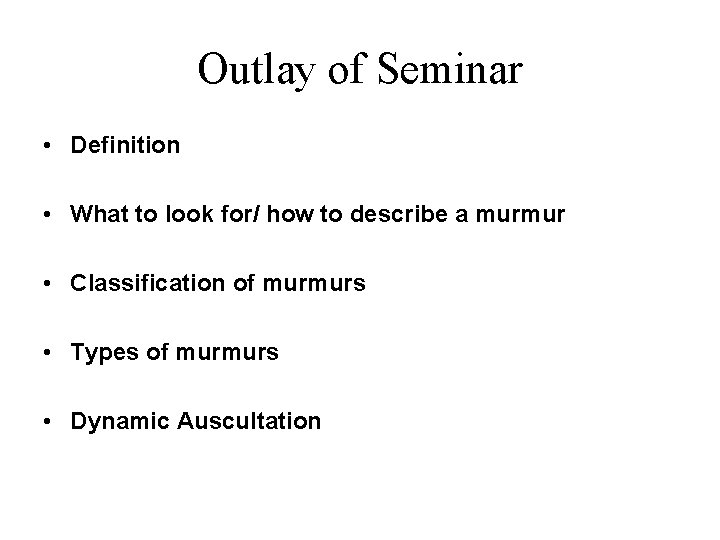
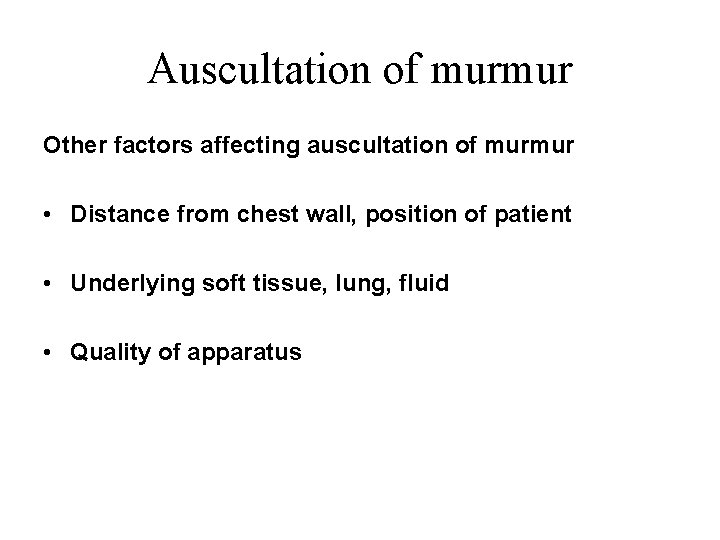
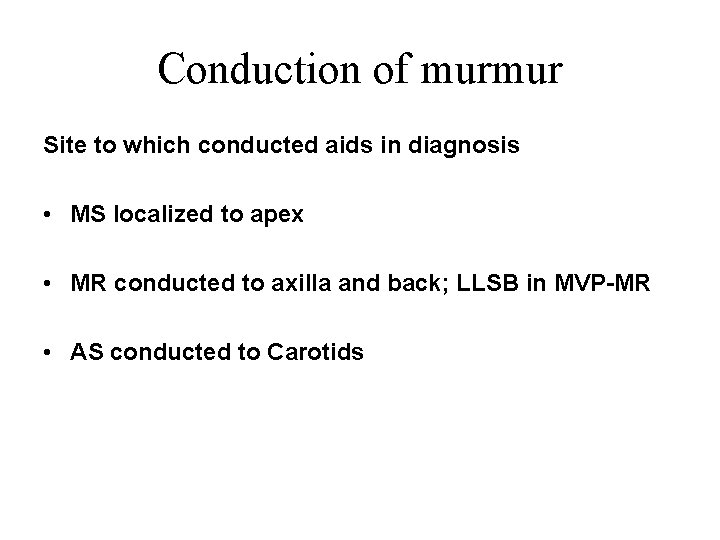
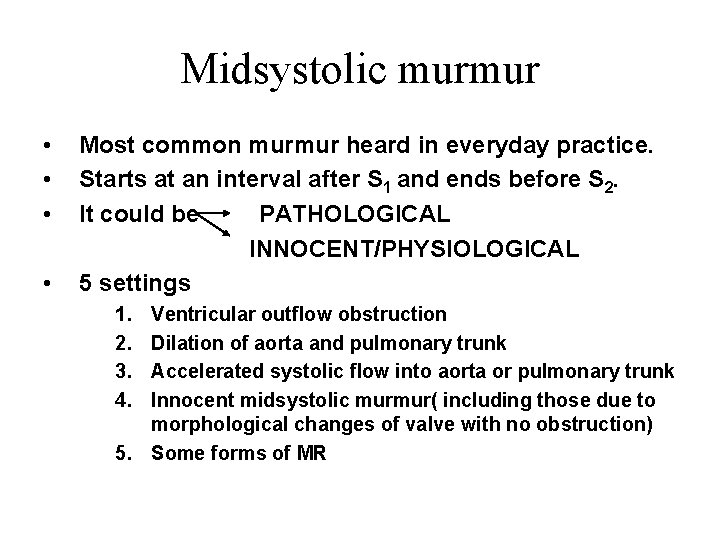
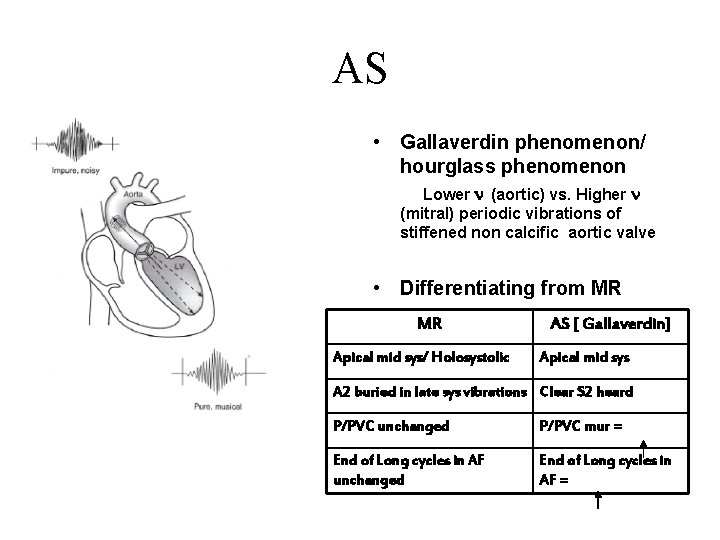
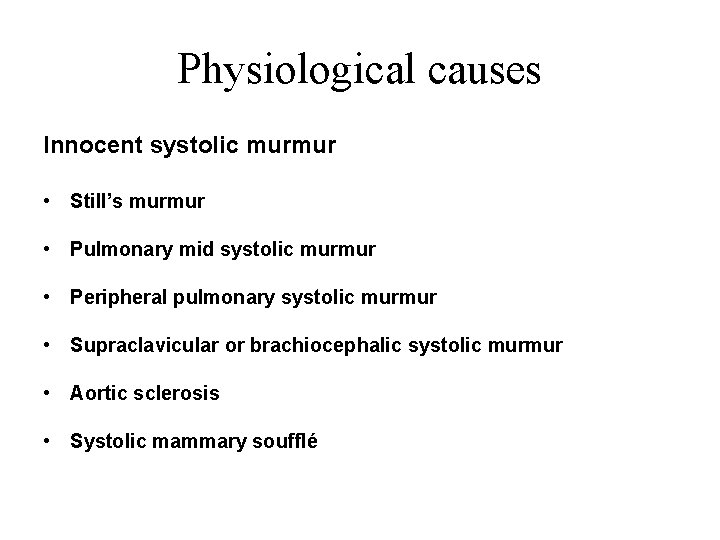
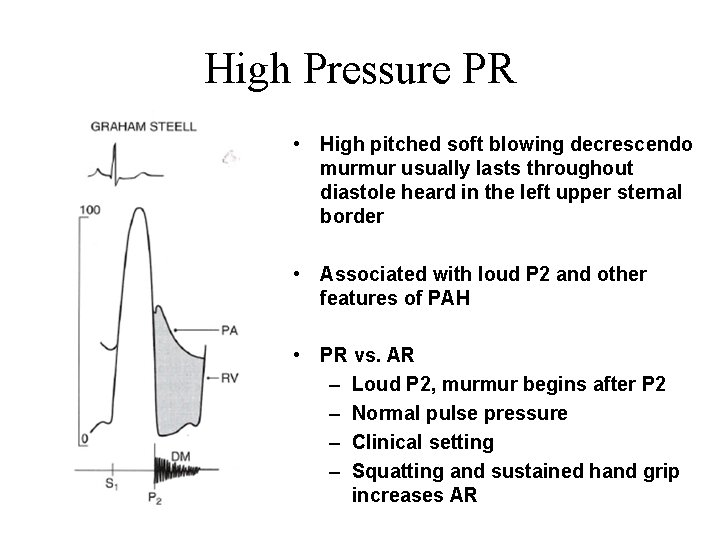
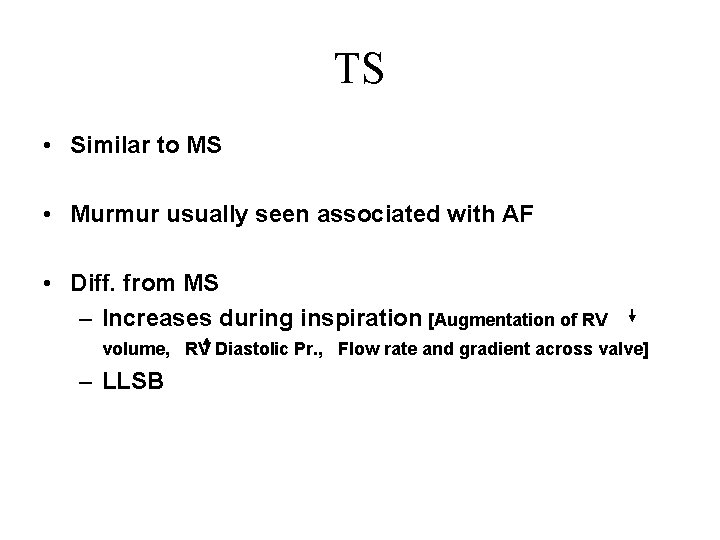
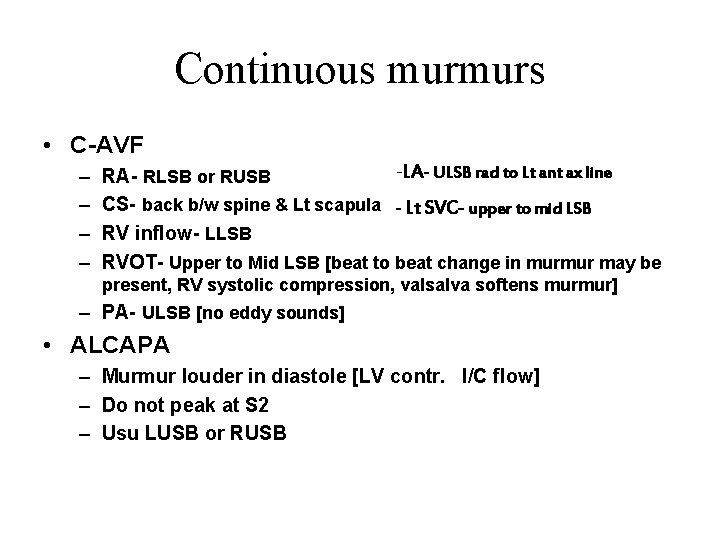
Position A. Lt Lateral Decubitus LV impulse [apical sounds, murmurs better heard] Act of turning increases HR[ MDM & PSA of MS ], induces PVC [AS murmur vs. MR murmur (n/c)] B. Sitting leaning forward full held expiration AR & PR EDM C. Sitting with legs dangling Further reduces venous return If S 2 fails to fuse on sitting D. Elbow Knee Position Pericardial friction rub
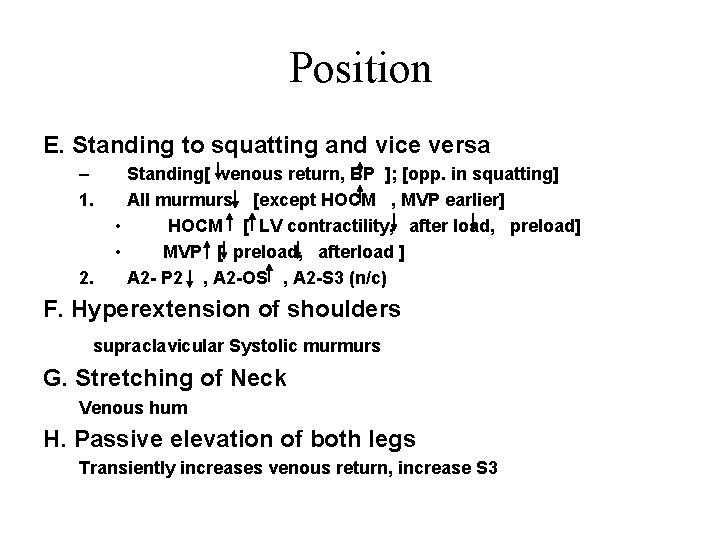
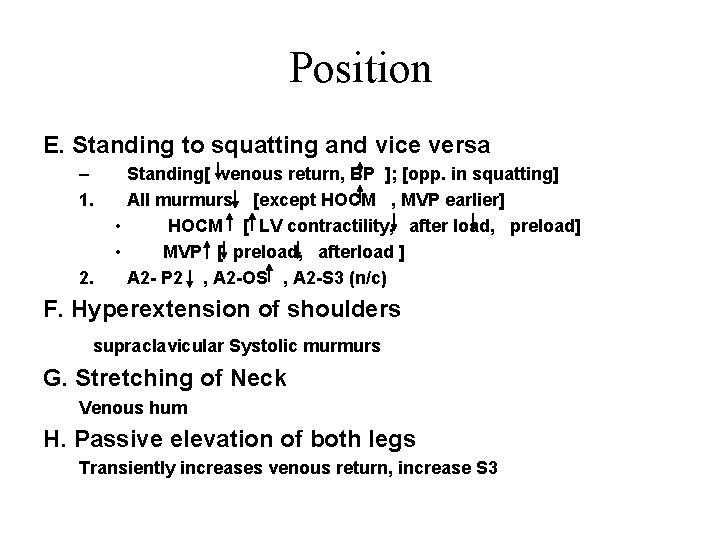
Position E. Standing to squatting and vice versa – 1. 2. Standing[ venous return, BP ]; [opp. in squatting] All murmurs [except HOCM , MVP earlier] • HOCM [ LV contractility, after load, preload] • MVP [ preload, afterload ] A 2 - P 2 , A 2 -OS , A 2 -S 3 (n/c) F. Hyperextension of shoulders supraclavicular Systolic murmurs G. Stretching of Neck Venous hum H. Passive elevation of both legs Transiently increases venous return, increase S 3
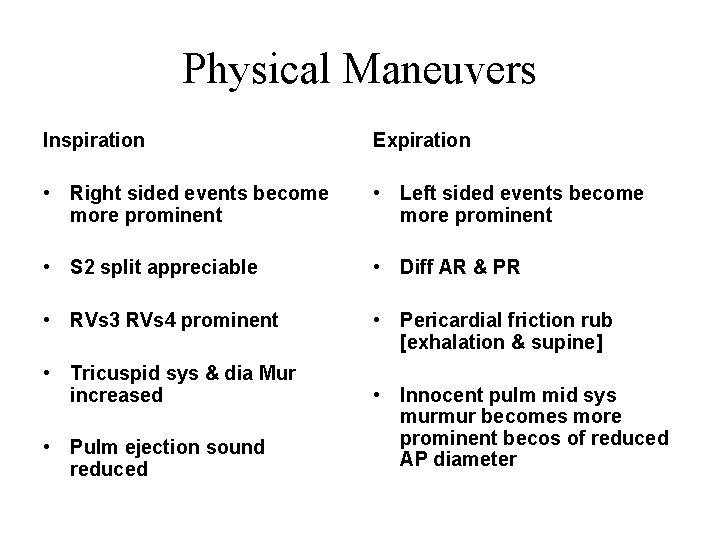
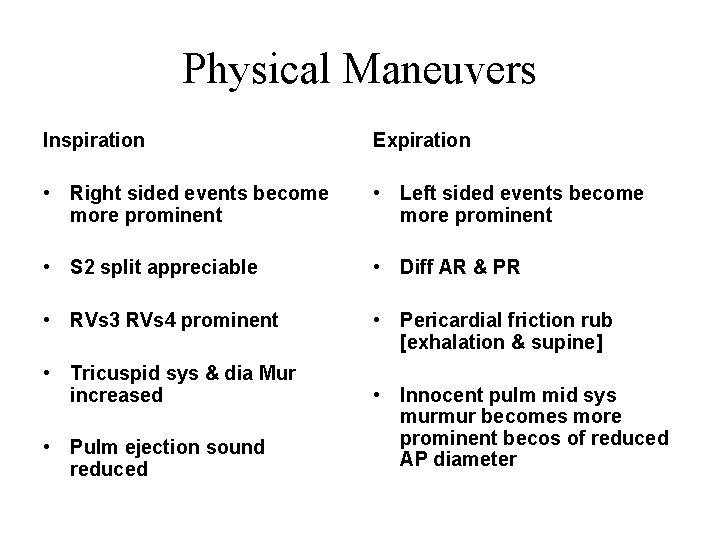
Physical Maneuvers Inspiration Expiration • Right sided events become more prominent • Left sided events become more prominent • S 2 split appreciable • Diff AR & PR • RVs 3 RVs 4 prominent • Pericardial friction rub [exhalation & supine] • Tricuspid sys & dia Mur increased • Pulm ejection sound reduced • Innocent pulm mid sys murmur becomes more prominent becos of reduced AP diameter
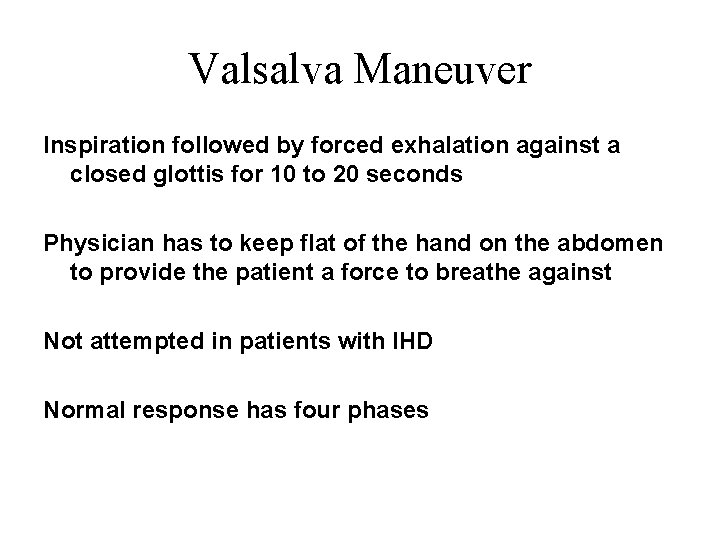
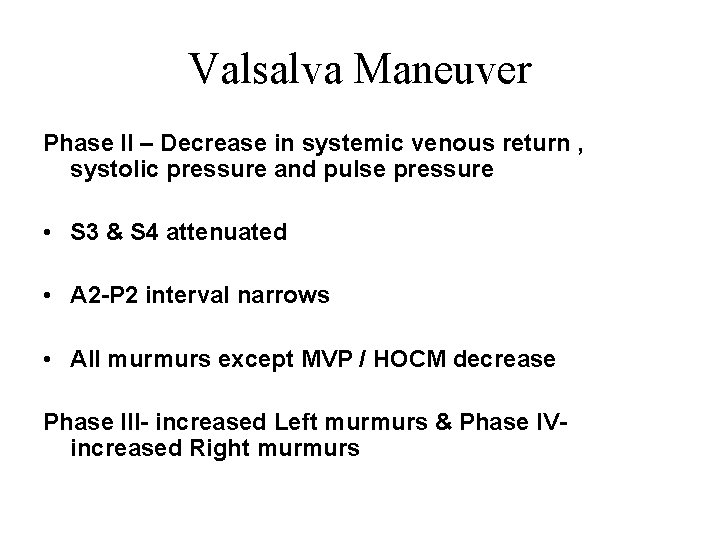
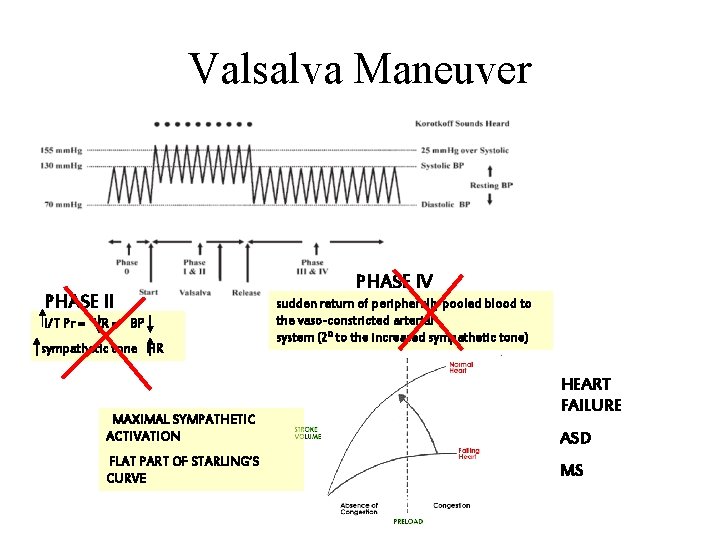
Valsalva Maneuver Inspiration followed by forced exhalation against a closed glottis for 10 to 20 seconds Physician has to keep flat of the hand on the abdomen to provide the patient a force to breathe against Not attempted in patients with IHD Normal response has four phases
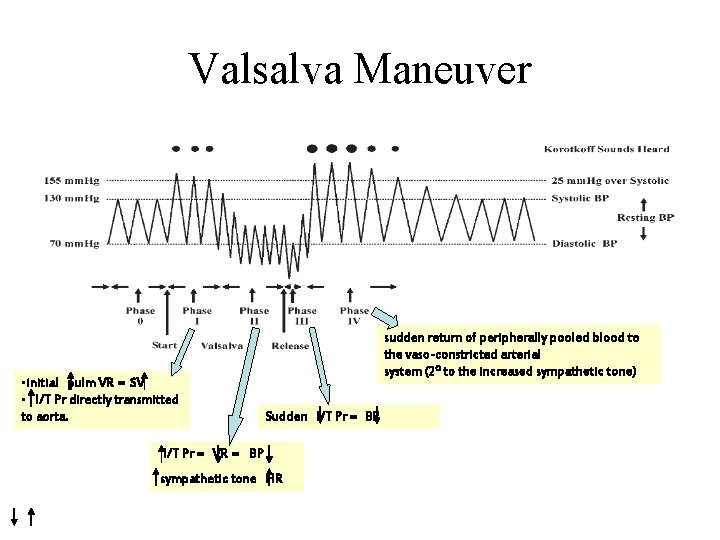
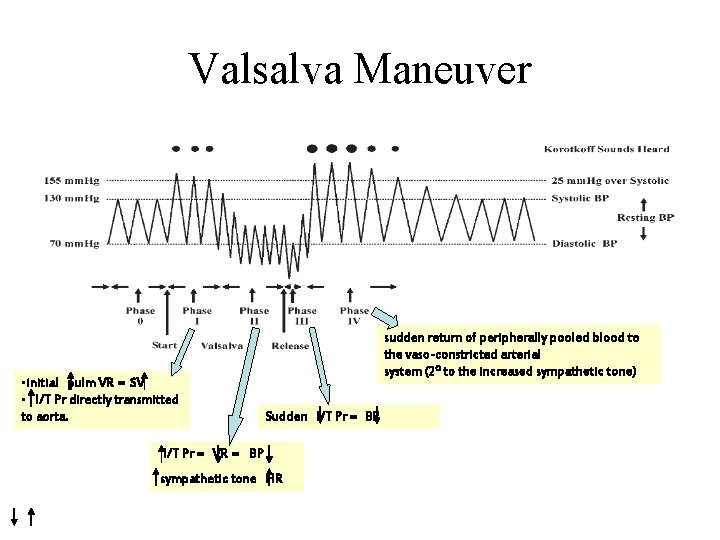
Valsalva Maneuver • initial pulm VR = SV • I/T Pr directly transmitted to aorta. sudden return of peripherally pooled blood to the vaso-constricted arterial system (20 to the increased sympathetic tone) Sudden I/T Pr = BP I/T Pr = VR = BP sympathetic tone HR
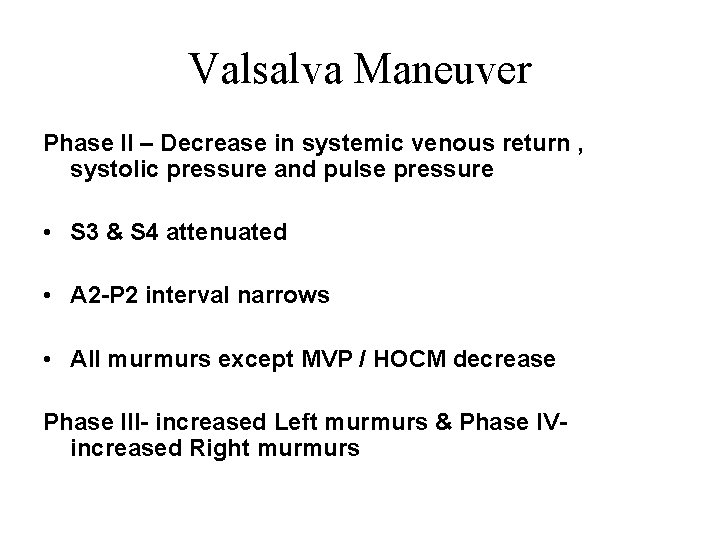
Valsalva Maneuver Phase II – Decrease in systemic venous return , systolic pressure and pulse pressure • S 3 & S 4 attenuated • A 2 -P 2 interval narrows • All murmurs except MVP / HOCM decrease Phase III- increased Left murmurs & Phase IVincreased Right murmurs
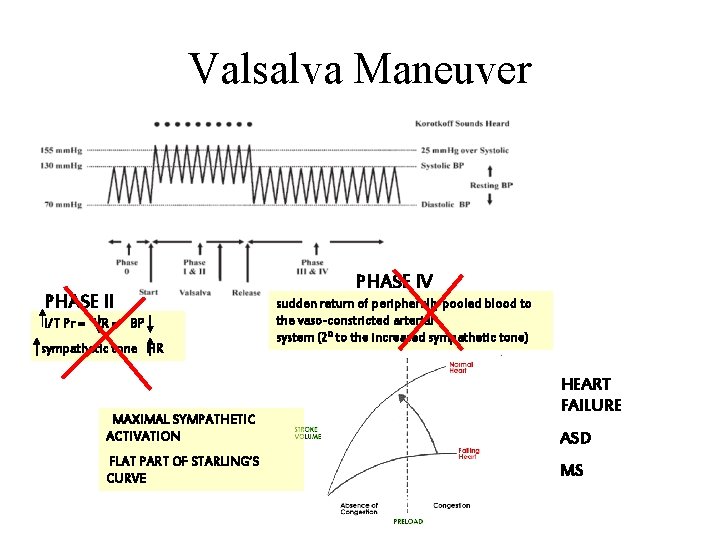
Valsalva Maneuver PHASE II I/T Pr = VR = BP sympathetic tone HR MAXIMAL SYMPATHETIC ACTIVATION FLAT PART OF STARLING’S CURVE PHASE IV sudden return of peripherally pooled blood to the vaso-constricted arterial system (20 to the increased sympathetic tone) HEART FAILURE ASD MS
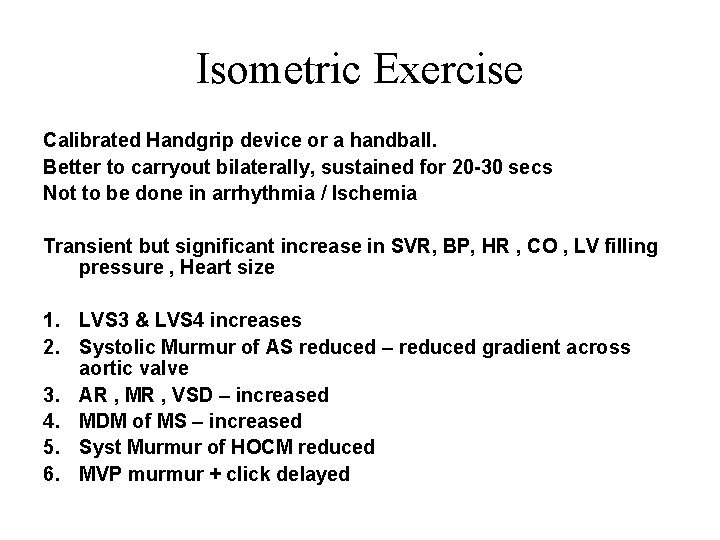
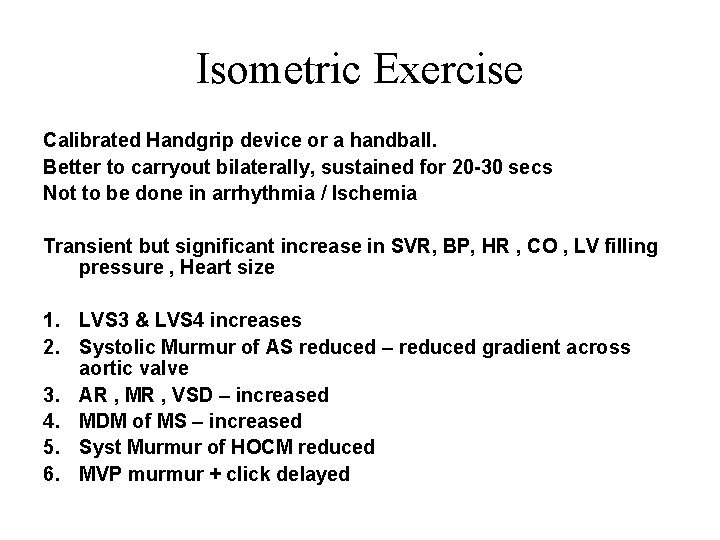
Isometric Exercise Calibrated Handgrip device or a handball. Better to carryout bilaterally, sustained for 20 -30 secs Not to be done in arrhythmia / Ischemia Transient but significant increase in SVR, BP, HR , CO , LV filling pressure , Heart size 1. LVS 3 & LVS 4 increases 2. Systolic Murmur of AS reduced – reduced gradient across aortic valve 3. AR , MR , VSD – increased 4. MDM of MS – increased 5. Syst Murmur of HOCM reduced 6. MVP murmur + click delayed
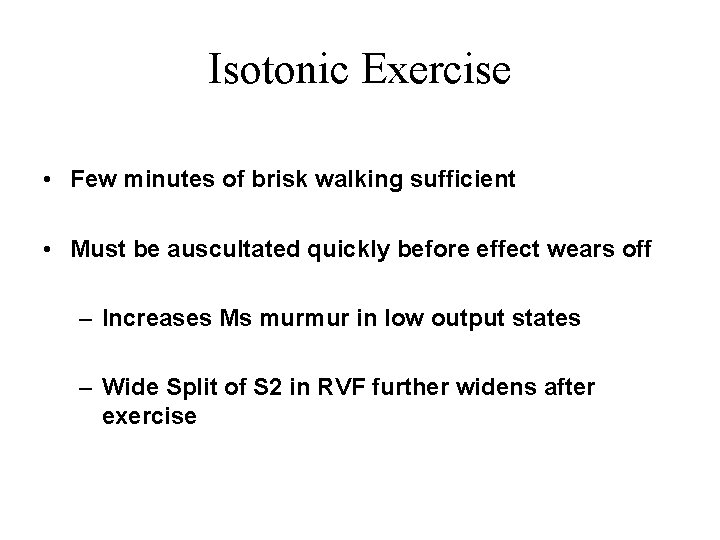
Isotonic Exercise • Few minutes of brisk walking sufficient • Must be auscultated quickly before effect wears off – Increases Ms murmur in low output states – Wide Split of S 2 in RVF further widens after exercise
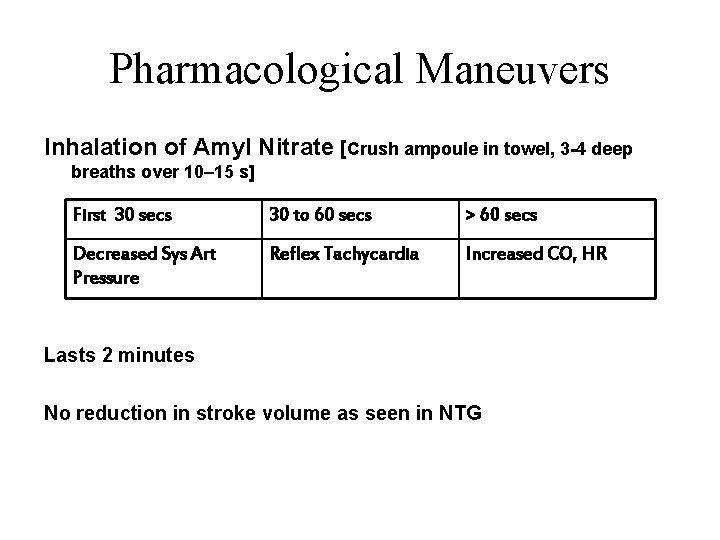
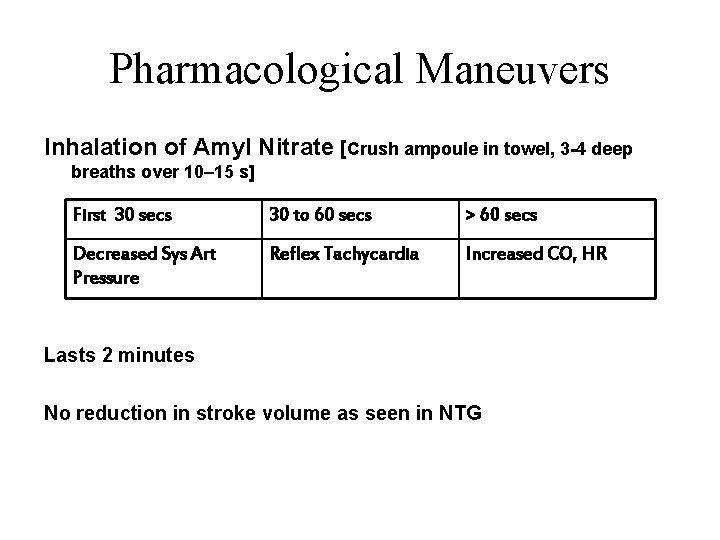
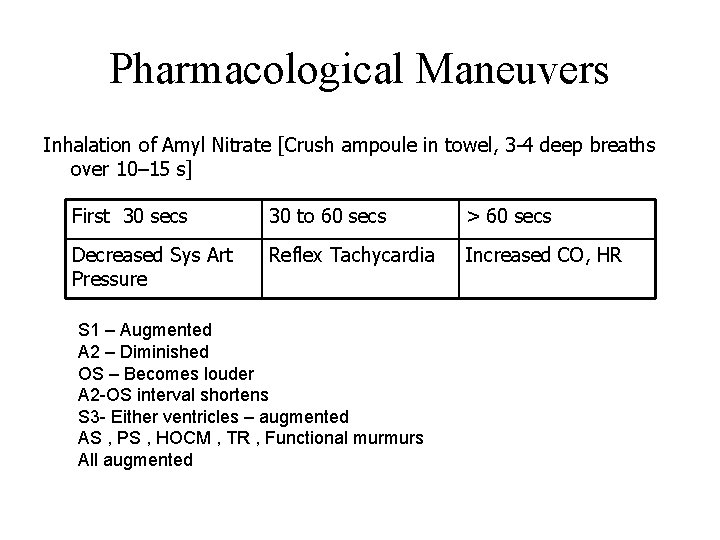
Pharmacological Maneuvers Inhalation of Amyl Nitrate [Crush ampoule in towel, 3 -4 deep breaths over 10– 15 s] First 30 secs 30 to 60 secs > 60 secs Decreased Sys Art Pressure Reflex Tachycardia Increased CO, HR Lasts 2 minutes No reduction in stroke volume as seen in NTG
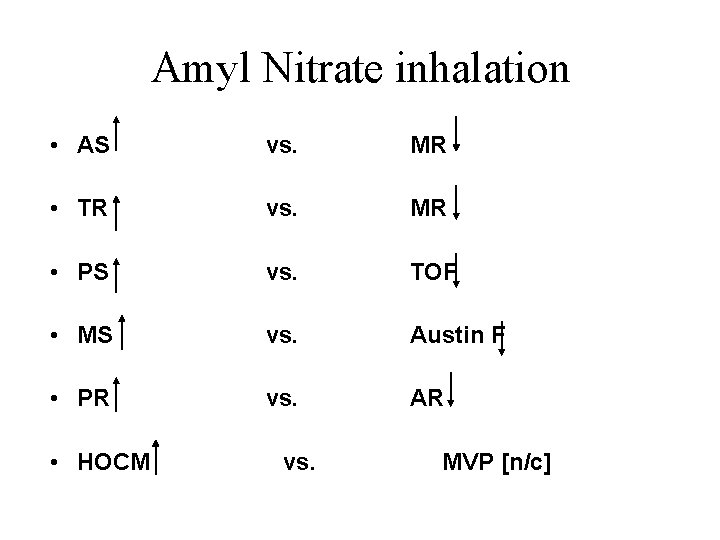
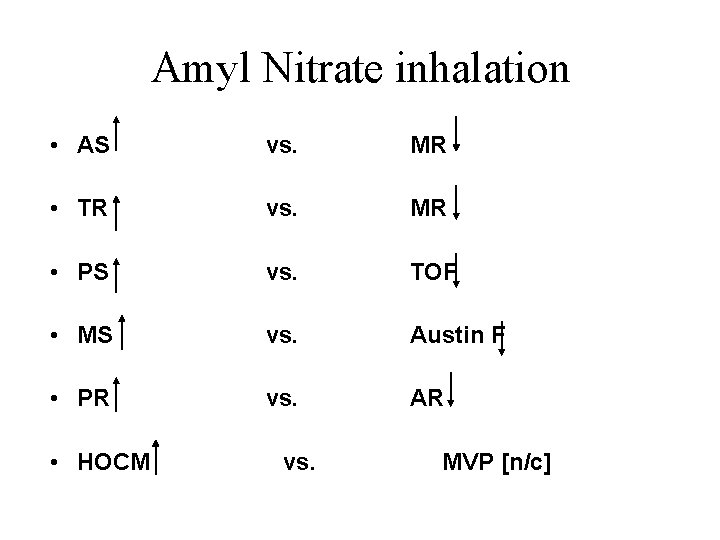
Amyl Nitrate inhalation • AS vs. MR • TR vs. MR • PS vs. TOF • MS vs. Austin F • PR vs. AR • HOCM vs. MVP [n/c]
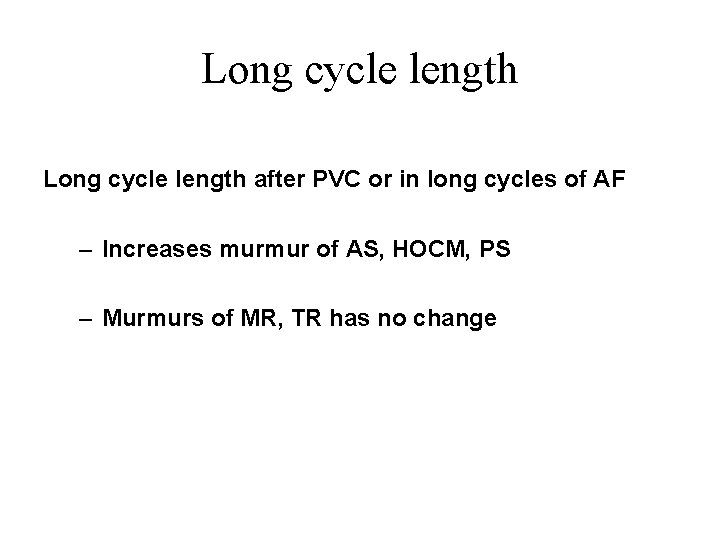
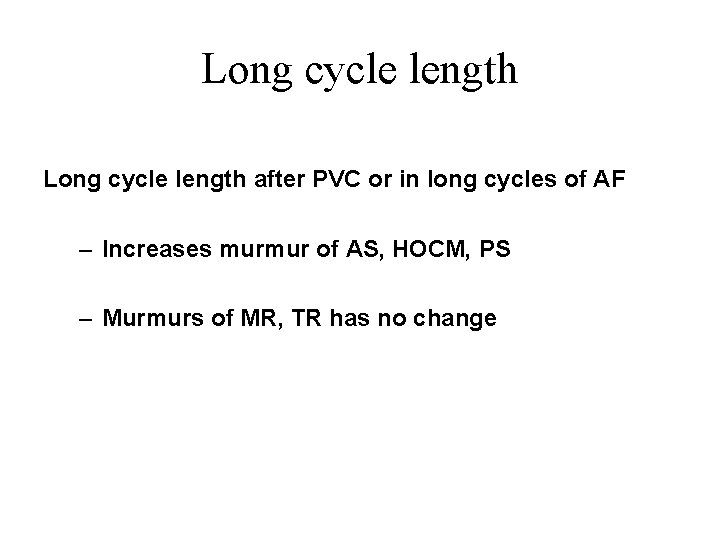
Long cycle length after PVC or in long cycles of AF – Increases murmur of AS, HOCM, PS – Murmurs of MR, TR has no change

Thank you

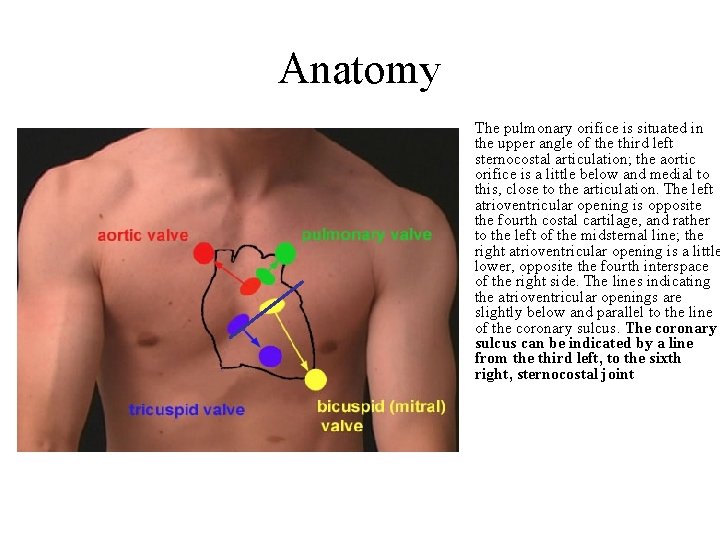
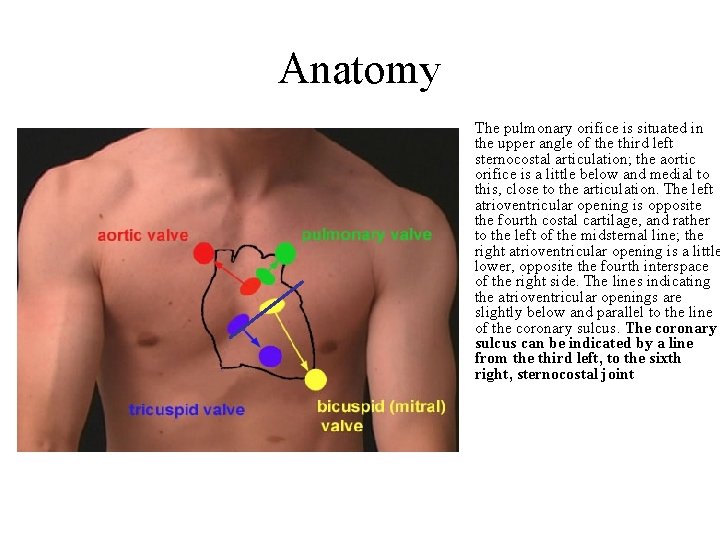
Anatomy The pulmonary orifice is situated in the upper angle of the third left sternocostal articulation; the aortic orifice is a little below and medial to this, close to the articulation. The left atrioventricular opening is opposite the fourth costal cartilage, and rather to the left of the midsternal line; the right atrioventricular opening is a little lower, opposite the fourth interspace of the right side. The lines indicating the atrioventricular openings are slightly below and parallel to the line of the coronary sulcus. The coronary sulcus can be indicated by a line from the third left, to the sixth right, sternocostal joint
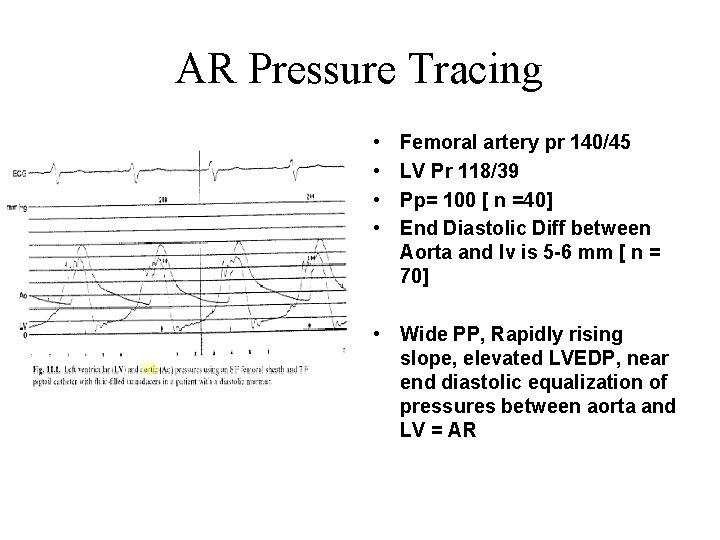
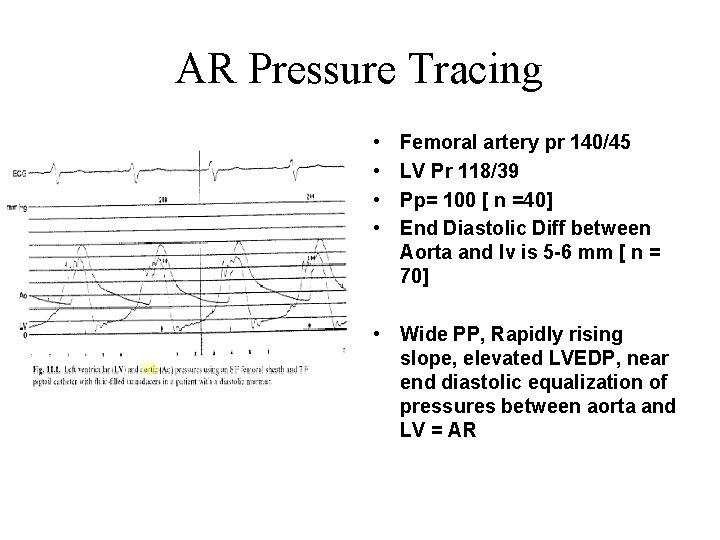
AR Pressure Tracing • • Femoral artery pr 140/45 LV Pr 118/39 Pp= 100 [ n =40] End Diastolic Diff between Aorta and lv is 5 -6 mm [ n = 70] • Wide PP, Rapidly rising slope, elevated LVEDP, near end diastolic equalization of pressures between aorta and LV = AR
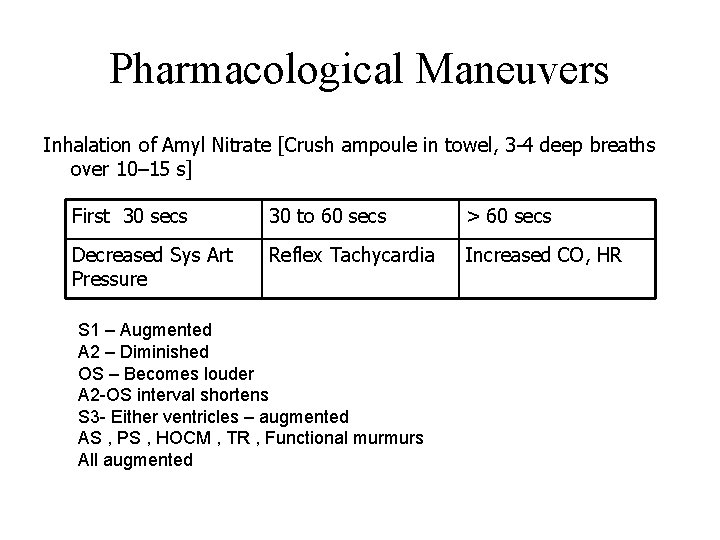
Pharmacological Maneuvers Inhalation of Amyl Nitrate [Crush ampoule in towel, 3 -4 deep breaths over 10– 15 s] First 30 secs 30 to 60 secs > 60 secs Decreased Sys Art Pressure Reflex Tachycardia Increased CO, HR S 1 – Augmented A 2 – Diminished OS – Becomes louder A 2 -OS interval shortens S 3 - Either ventricles – augmented AS , PS , HOCM , TR , Functional murmurs All augmented
 Cardiac output and heart rate
Cardiac output and heart rate Heart murmurs
Heart murmurs Tetralogy of fallot heart sounds
Tetralogy of fallot heart sounds Heart murmurs
Heart murmurs Prinivil
Prinivil Heart murmurs
Heart murmurs Dynamic auscultation
Dynamic auscultation Austin flint murmur
Austin flint murmur Heart sounds
Heart sounds Auscultate heart sounds
Auscultate heart sounds Thrill murmur grade
Thrill murmur grade Auscultation of heart sounds
Auscultation of heart sounds Giant gravitational wave murmurs universe
Giant gravitational wave murmurs universe Tulika jain
Tulika jain Gravitational wave detectors hear murmurs from
Gravitational wave detectors hear murmurs from Holosystolic murmur
Holosystolic murmur Giant wave detectors murmurs universe
Giant wave detectors murmurs universe Parasternal heave
Parasternal heave Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Foyer cardiaque
Foyer cardiaque Auscultatory triangle of the back
Auscultatory triangle of the back Boundaries of kronig isthmus
Boundaries of kronig isthmus Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Psoas sign
Psoas sign Conncets
Conncets Focused gi assessment
Focused gi assessment Costovertebral angle
Costovertebral angle Auscultation
Auscultation 5 heart sounds landmarks
5 heart sounds landmarks Splenomegaly physical exam
Splenomegaly physical exam Apical pulse location
Apical pulse location Lingula auscultation
Lingula auscultation Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Foyer auscultation cardiaque
Foyer auscultation cardiaque 5 point auscultation
5 point auscultation Apical heart sounds
Apical heart sounds Protract retract
Protract retract Transferered
Transferered Sheep heart diagram
Sheep heart diagram Stars dogs plowhorses and puzzles
Stars dogs plowhorses and puzzles Third heart sound
Third heart sound Static assessment vs dynamic assessment
Static assessment vs dynamic assessment Dynamic programming vs divide and conquer
Dynamic programming vs divide and conquer Maximo service management
Maximo service management Dynamic unit testing
Dynamic unit testing A state of dynamic balance
A state of dynamic balance Dynamic scattering type lcd
Dynamic scattering type lcd Chapter 3 the dynamic earth
Chapter 3 the dynamic earth Distal extension base
Distal extension base Dynamic fulfillers inc
Dynamic fulfillers inc Dynamic environment of international trade
Dynamic environment of international trade Warp divergence
Warp divergence John wright character analysis
John wright character analysis Knapsack dynamic programming pseudocode
Knapsack dynamic programming pseudocode Dynamic trading and auctioneers
Dynamic trading and auctioneers Dynamic memory management
Dynamic memory management Xxx
Xxx Dynamic programming bottom up
Dynamic programming bottom up Dynamic strategies for asset allocation
Dynamic strategies for asset allocation Dynamic data mining
Dynamic data mining Pearl dynamic assessment
Pearl dynamic assessment Helix swarf conveyor
Helix swarf conveyor Small dynamic business search from the ccr home page
Small dynamic business search from the ccr home page Dynamic branch prediction
Dynamic branch prediction Pseudoknot structure
Pseudoknot structure Static character
Static character Curriculum development models
Curriculum development models Quagga linux
Quagga linux Dynamic firewalls
Dynamic firewalls Binomial coefficient using dynamic programming
Binomial coefficient using dynamic programming Dwp dynamic purchasing system
Dwp dynamic purchasing system Assignment problem dynamic programming
Assignment problem dynamic programming Relocatable dynamic partitions
Relocatable dynamic partitions Motive arousal in consumer behaviour
Motive arousal in consumer behaviour Difference between static and dynamic characters
Difference between static and dynamic characters Dynamic data structure
Dynamic data structure Dynamic multiprocessor systems.
Dynamic multiprocessor systems. Recursive thought
Recursive thought Dynamic time warping
Dynamic time warping Dynamic white box testing
Dynamic white box testing Spongy bone structure
Spongy bone structure A python function definition begins with
A python function definition begins with Exact indexing of dynamic time warping
Exact indexing of dynamic time warping Dynamic programming
Dynamic programming Dantzig
Dantzig Dad curve equation
Dad curve equation Dynamic irony
Dynamic irony Utep mph
Utep mph Amadeus dynamic travel documents
Amadeus dynamic travel documents