Valvular Heart Disease Tulika Jain MD Resident Teaching




















- Slides: 98
Valvular Heart Disease Tulika Jain, MD Resident Teaching Conference December 5, 2008 © Continuing Medical Implementation …. . . bridging the care gap
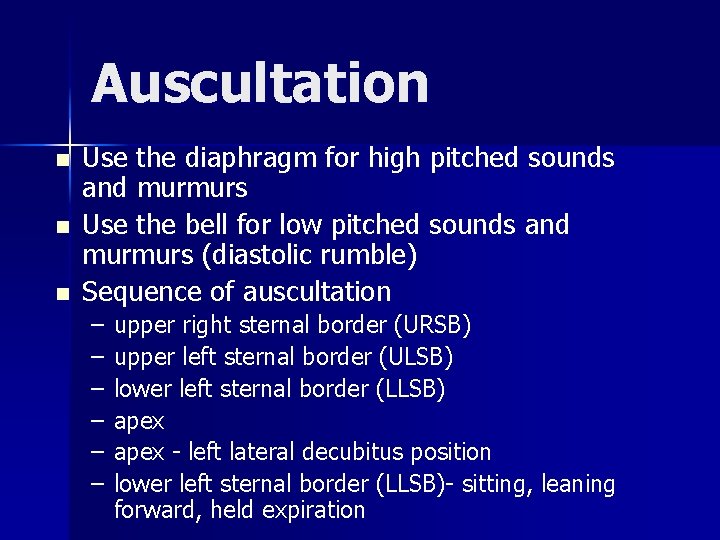
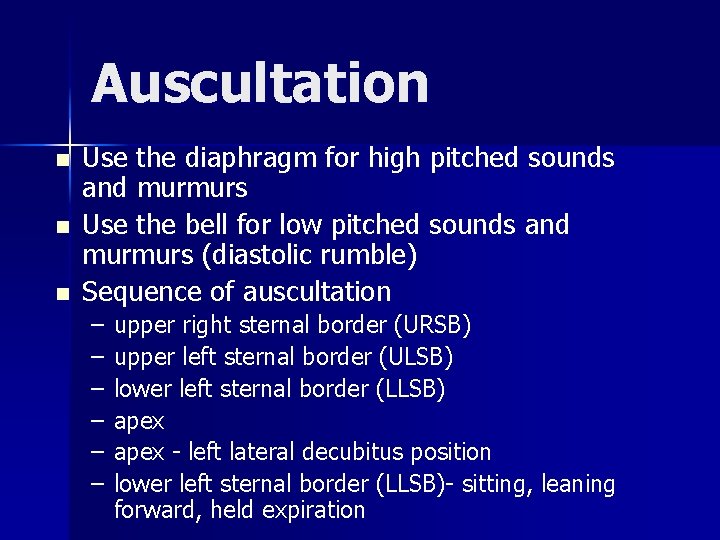
Auscultation n Use the diaphragm for high pitched sounds and murmurs Use the bell for low pitched sounds and murmurs (diastolic rumble) Sequence of auscultation – – – upper right sternal border (URSB) upper left sternal border (ULSB) lower left sternal border (LLSB) apex - left lateral decubitus position lower left sternal border (LLSB)- sitting, leaning forward, held expiration
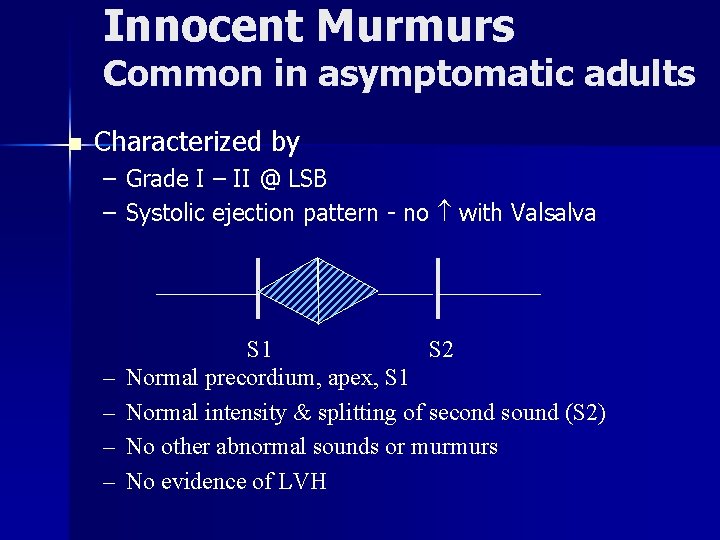
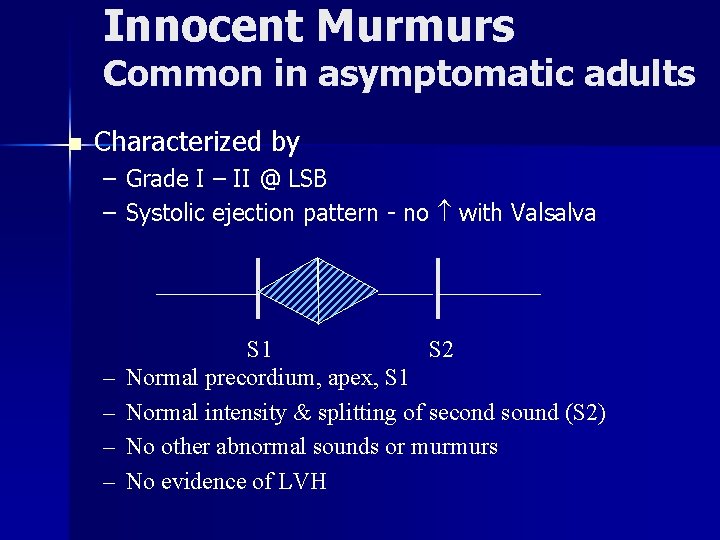
Innocent Murmurs Common in asymptomatic adults n Characterized by – Grade I – II @ LSB – Systolic ejection pattern - no with Valsalva – – S 1 S 2 Normal precordium, apex, S 1 Normal intensity & splitting of second sound (S 2) No other abnormal sounds or murmurs No evidence of LVH

Characteristic of the NOT Innocent Murmur Diastolic murmur n Loud murmur - grade III or above n Regurgitant murmur n Murmurs associated with a click n Murmurs associated with other signs or symptoms e. g. cyanosis n Abnormal 2 nd heart sound – fixed split, paradoxical split or single n
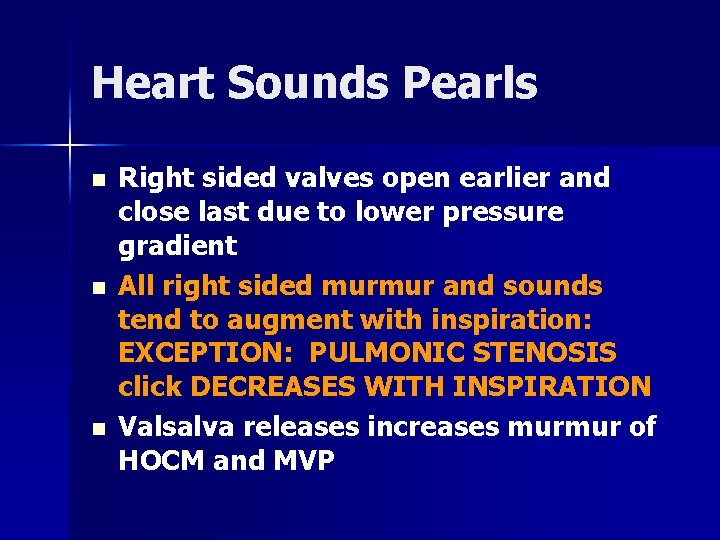
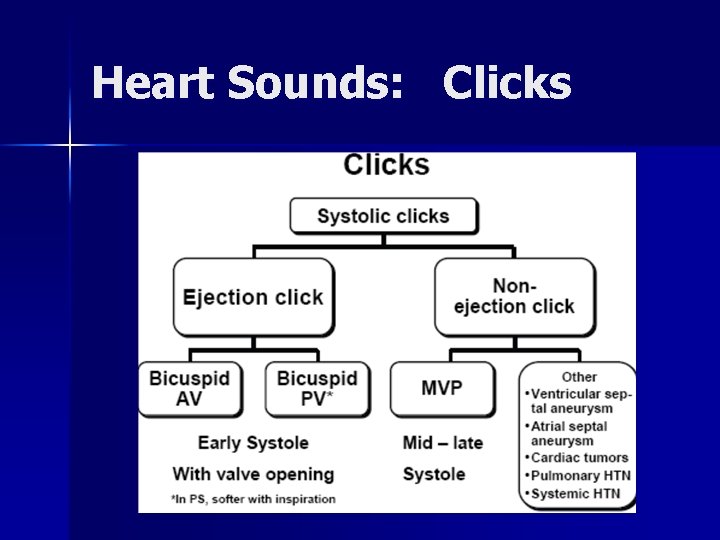
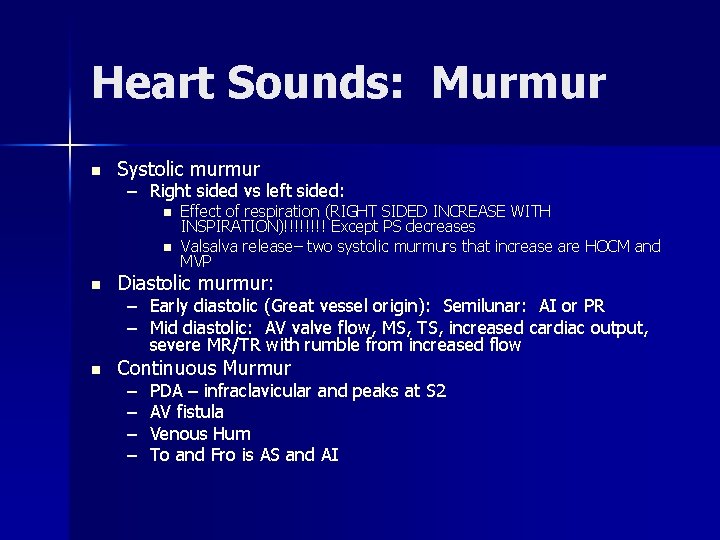
Heart Sounds Pearls n n n Right sided valves open earlier and close last due to lower pressure gradient All right sided murmur and sounds tend to augment with inspiration: EXCEPTION: PULMONIC STENOSIS click DECREASES WITH INSPIRATION Valsalva releases increases murmur of HOCM and MVP
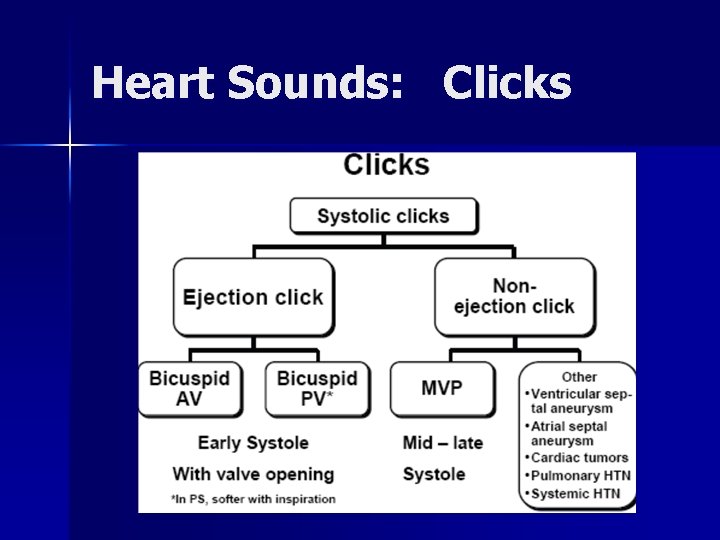
Heart Sounds: Clicks
Valve Disorders Etiology n Symptoms n Physical Exam n Testing n Severity n Indications for Surgery n
Common Clinical Scenarios n Younger people – Functional murmur vs MVP vs bicuspid AV n Older people – Aortic sclerosis vs aortic stenosis
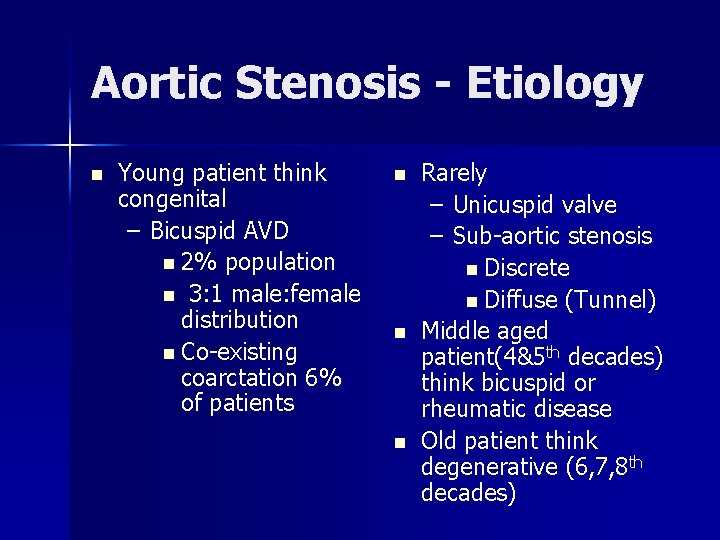
Aortic Stenosis - Etiology n Young patient think congenital – Bicuspid AVD n 2% population n 3: 1 male: female distribution n Co-existing coarctation 6% of patients n n n Rarely – Unicuspid valve – Sub-aortic stenosis n Discrete n Diffuse (Tunnel) Middle aged patient(4&5 th decades) think bicuspid or rheumatic disease Old patient think degenerative (6, 7, 8 th decades)
Aortic Stenosis: Etiology Valvular n Subvalvular n Supravalvular n

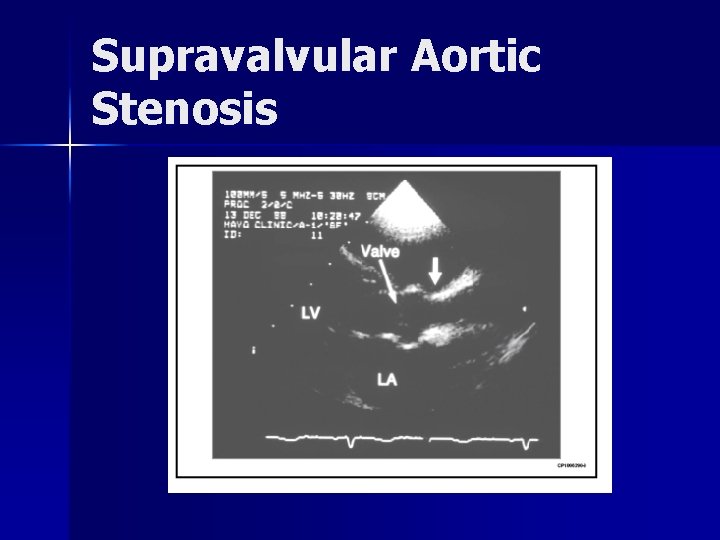
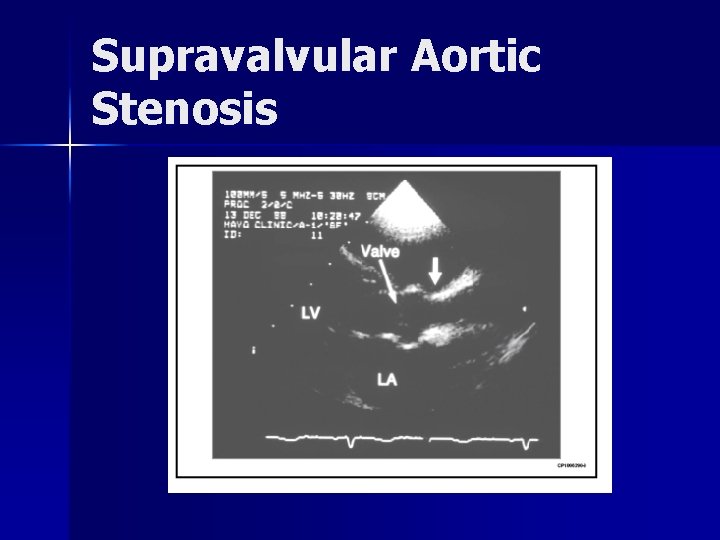
Supravalvular Aortic Stenosis
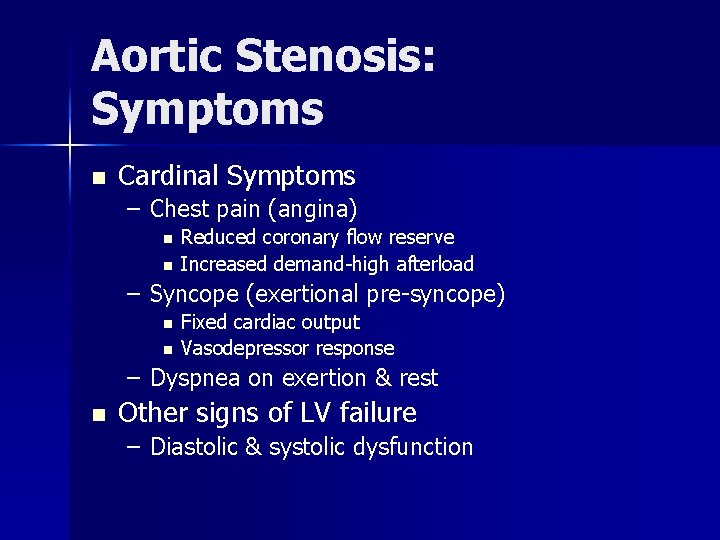
Aortic Stenosis: Symptoms n Cardinal Symptoms – Chest pain (angina) n n Reduced coronary flow reserve Increased demand-high afterload – Syncope (exertional pre-syncope) n n Fixed cardiac output Vasodepressor response – Dyspnea on exertion & rest n Other signs of LV failure – Diastolic & systolic dysfunction
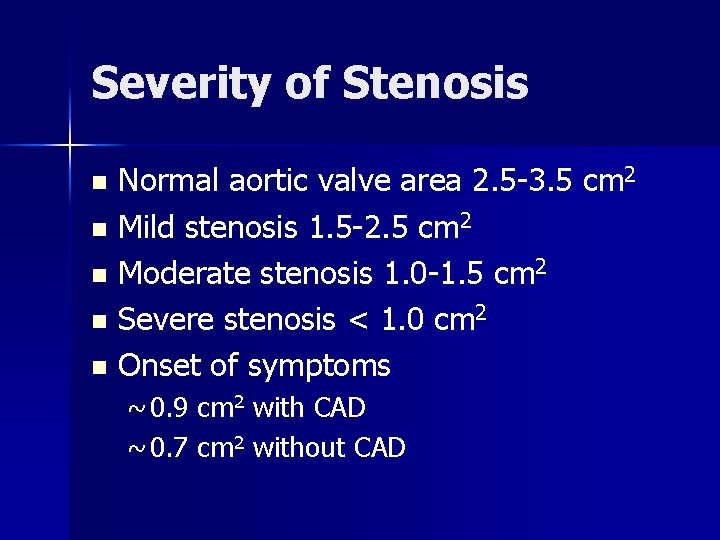
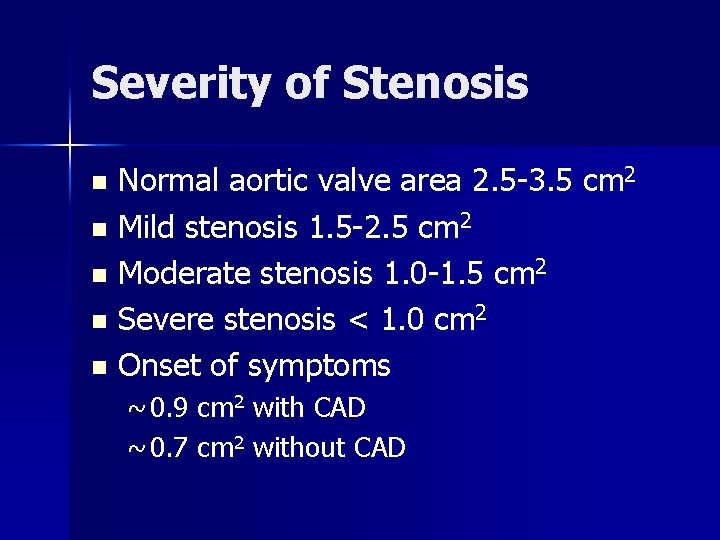
Severity of Stenosis Normal aortic valve area 2. 5 -3. 5 cm 2 n Mild stenosis 1. 5 -2. 5 cm 2 n Moderate stenosis 1. 0 -1. 5 cm 2 n Severe stenosis < 1. 0 cm 2 n Onset of symptoms n ~ 0. 9 cm 2 with CAD ~ 0. 7 cm 2 without CAD

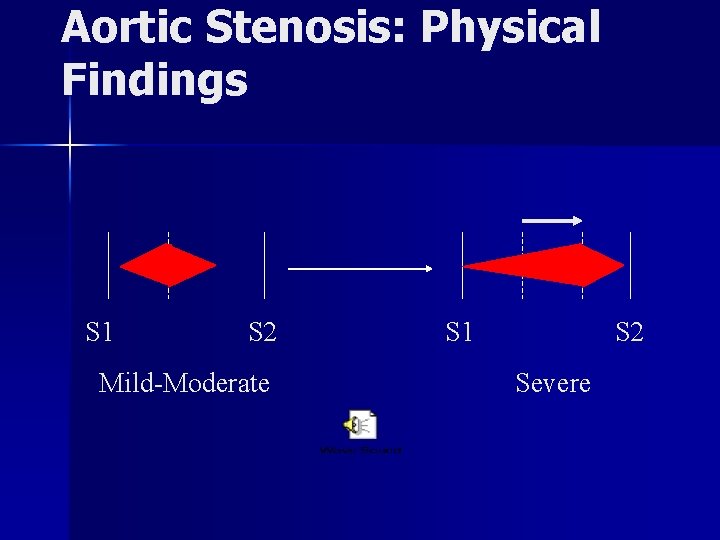
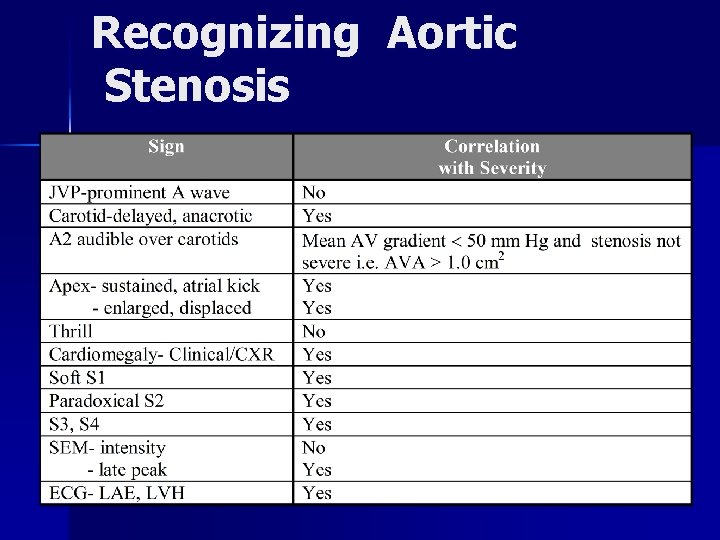
Aortic Stenosis: Physical Findings n n n n Intensity DOES NOT predict severity Presence of thrill DOES NOT predict severity “Diamond” shaped, systolic crescendodecrescendo Decreased, delay & prolongation of pulse amplitude: “pulsus parvus and tardus” Paradoxical S 2 S 4 (with left ventricular hypertrophy) S 3 (with left ventricular failure)
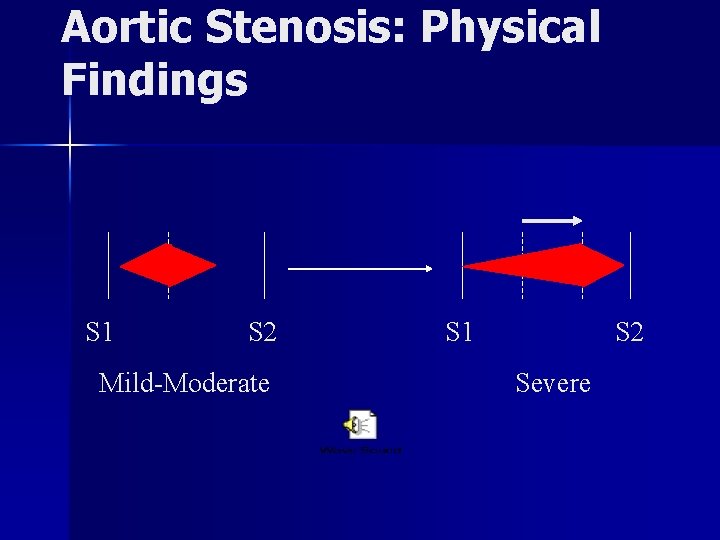
Aortic Stenosis: Physical Findings S 1 S 2 Mild-Moderate S 1 S 2 Severe
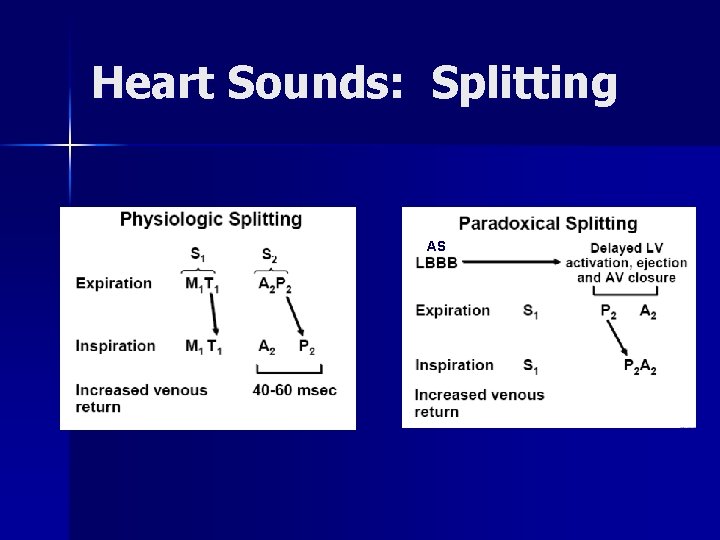
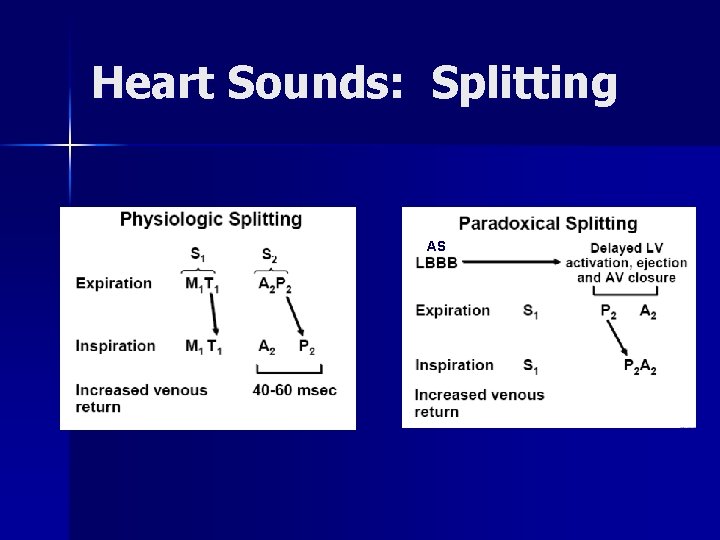
Heart Sounds: Splitting AS

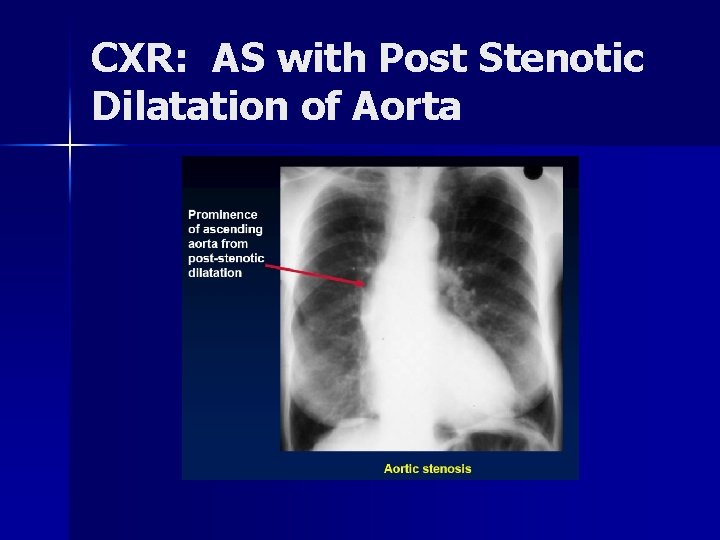
Aortic Stenosis : Lab EKG: LVH n CXR: Intially have concentric LVH so unremarkable; Critical AS may show post stenotic dilation of the aorta, hypertrophy, congestion n
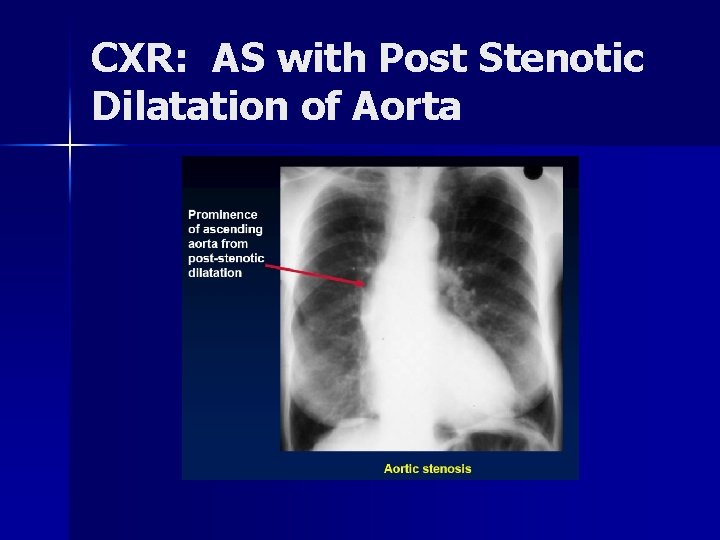
CXR: AS with Post Stenotic Dilatation of Aorta

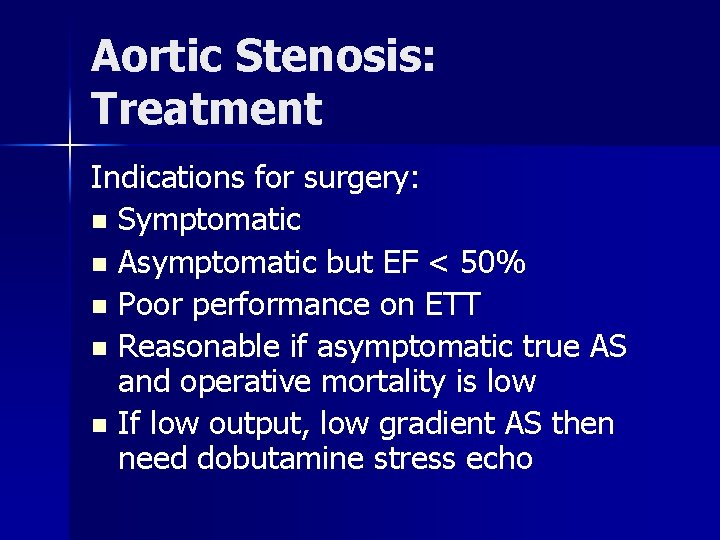
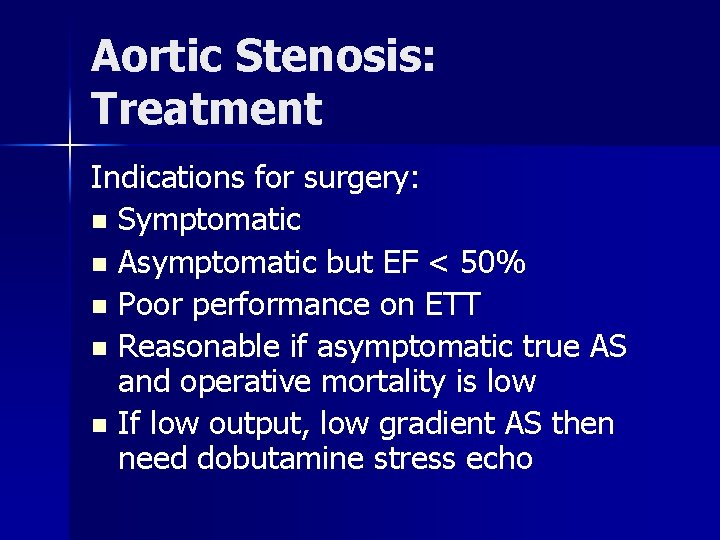
Aortic Stenosis: Treatment Indications for surgery: n Symptomatic n Asymptomatic but EF < 50% n Poor performance on ETT n Reasonable if asymptomatic true AS and operative mortality is low n If low output, low gradient AS then need dobutamine stress echo
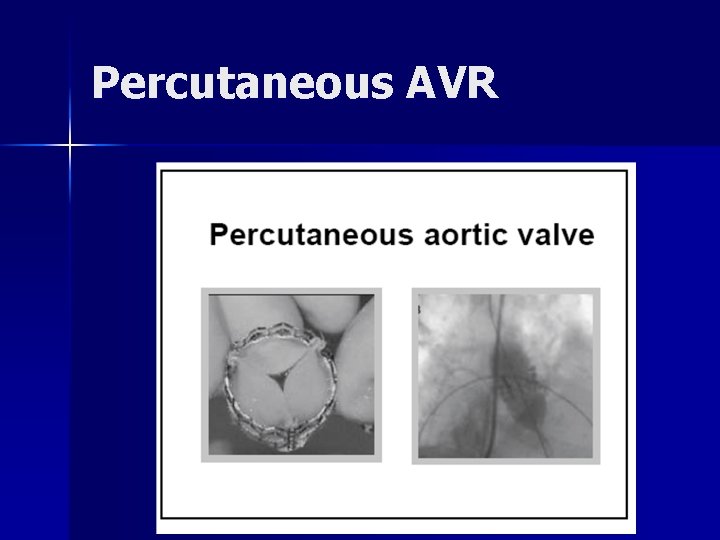
Aortic Stenosis: Treatment Aortic stenosis is a surgical disease n Treatment is valve replacement n Aortic valve balloon valvuloplasty rarely done due to stroke risk and other complications n Current trials using catheter based aortic valve replacement n

Aortic Regurgitation: Etiology n n Any conditions resulting in incompetent aortic leaflets Congenital n – Rheumatic heart disease – Dilated aorta (e. g. hypertension. . ) – Degenerative – Connective tissue disorders – Bicuspid valve n Aortopathy – Cystic medial necrosis – Collagen disorders (e. g. Marfan’s) – Ehler-Danlos – Osteogenesis imperfecta – Pseudoxanthoma elasticum Acquired n E. g. ankylosing spondylitis, rheumatoid arthritis, Reiter’s syndrome, Giant-cell arteritis ) – Syphilis (chronic aortitis) n Acute AI: aortic dissection, infective
Aortic Regurgitation: Symptoms n n Dyspnea, orthopnea, PND With extreme reductions in diastolic pressures (e. g. < 40) may see angina
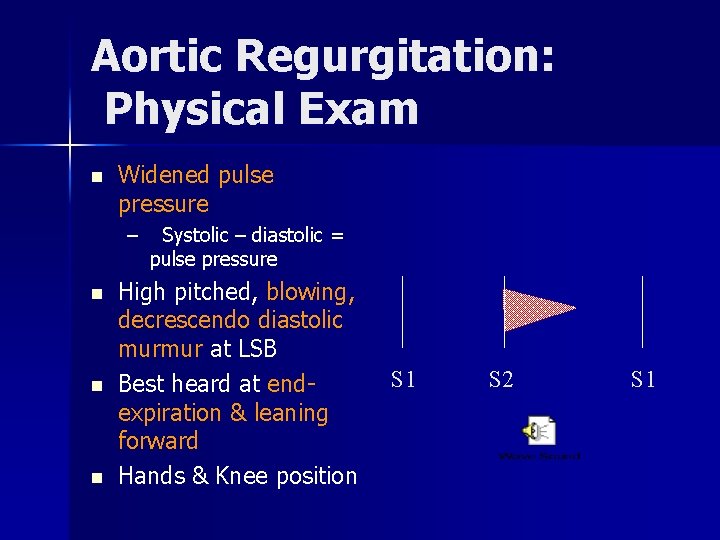
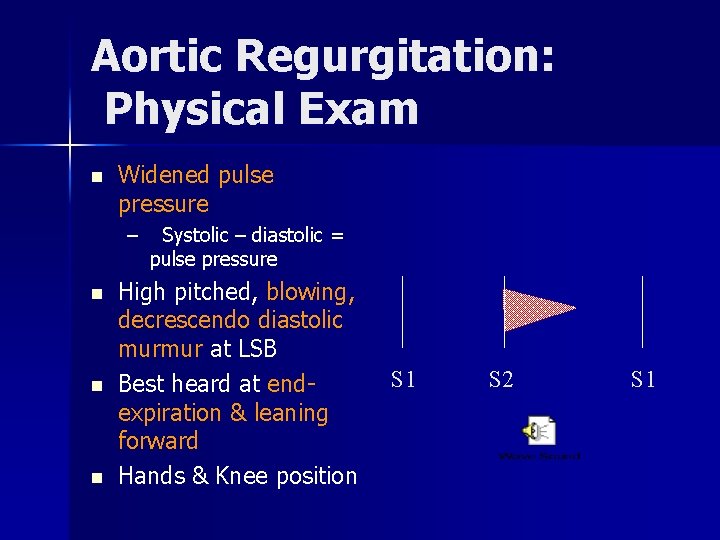
Aortic Regurgitation: Physical Exam n Widened pulse pressure – n n n Systolic – diastolic = pulse pressure High pitched, blowing, decrescendo diastolic murmur at LSB Best heard at endexpiration & leaning forward Hands & Knee position S 1 S 2 S 1
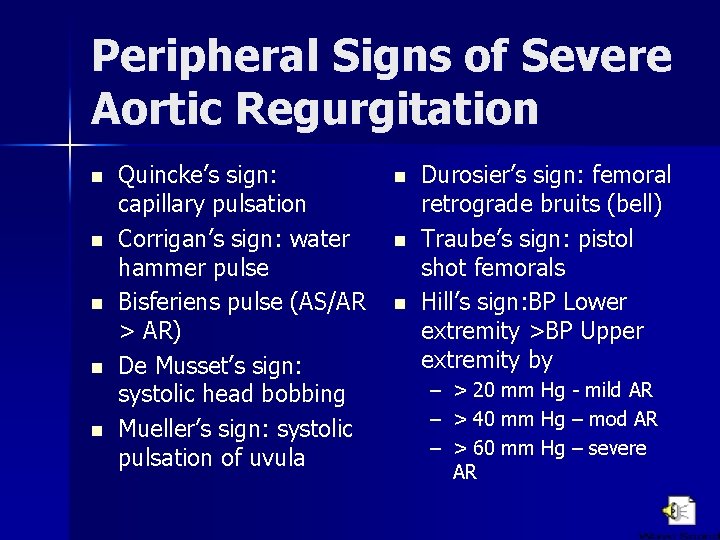
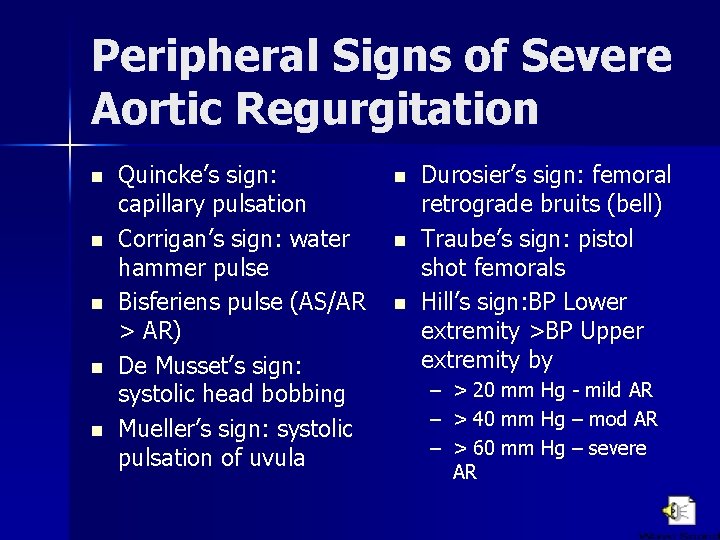
Peripheral Signs of Severe Aortic Regurgitation n n Quincke’s sign: capillary pulsation Corrigan’s sign: water hammer pulse Bisferiens pulse (AS/AR > AR) De Musset’s sign: systolic head bobbing Mueller’s sign: systolic pulsation of uvula n n n Durosier’s sign: femoral retrograde bruits (bell) Traube’s sign: pistol shot femorals Hill’s sign: BP Lower extremity >BP Upper extremity by – > 20 mm Hg - mild AR – > 40 mm Hg – mod AR – > 60 mm Hg – severe AR
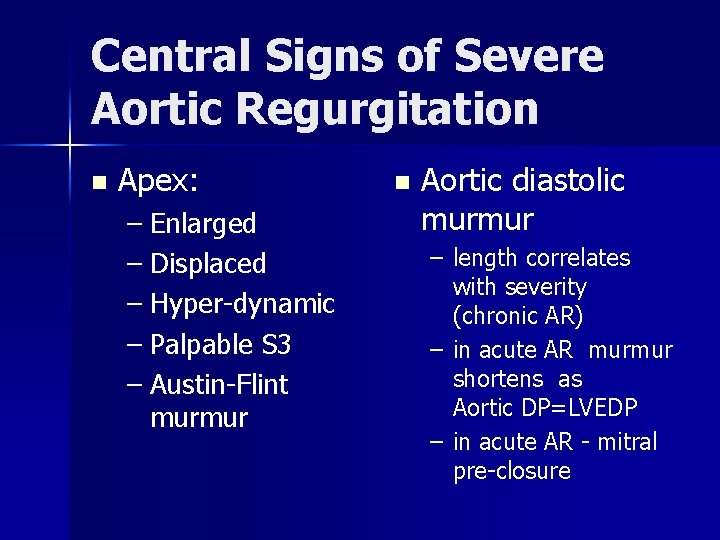
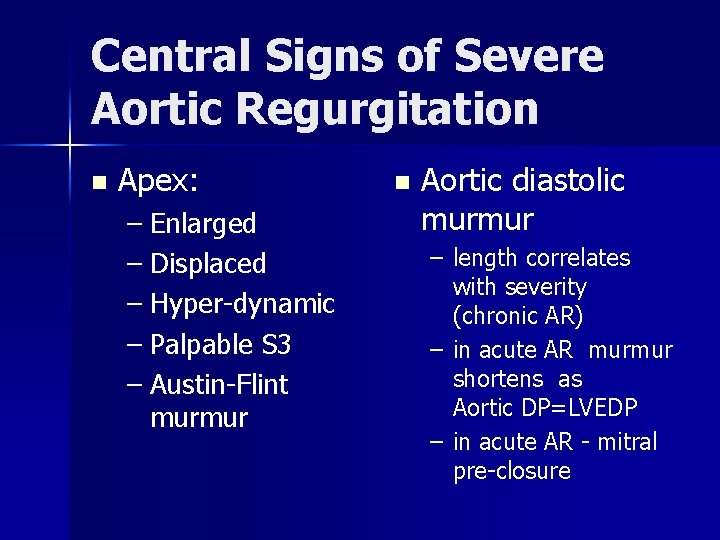
Central Signs of Severe Aortic Regurgitation n Apex: – Enlarged – Displaced – Hyper-dynamic – Palpable S 3 – Austin-Flint murmur n Aortic diastolic murmur – length correlates with severity (chronic AR) – in acute AR murmur shortens as Aortic DP=LVEDP – in acute AR - mitral pre-closure
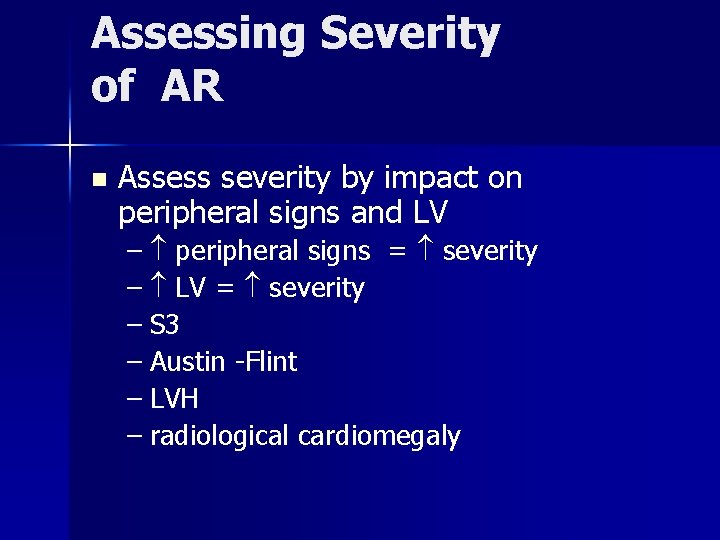
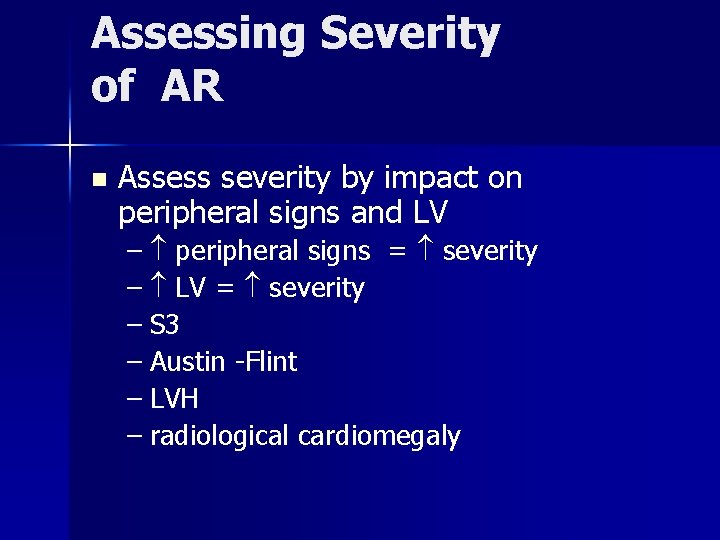
Assessing Severity of AR n Assess severity by impact on peripheral signs and LV – peripheral signs = severity – LV = severity – S 3 – Austin -Flint – LVH – radiological cardiomegaly
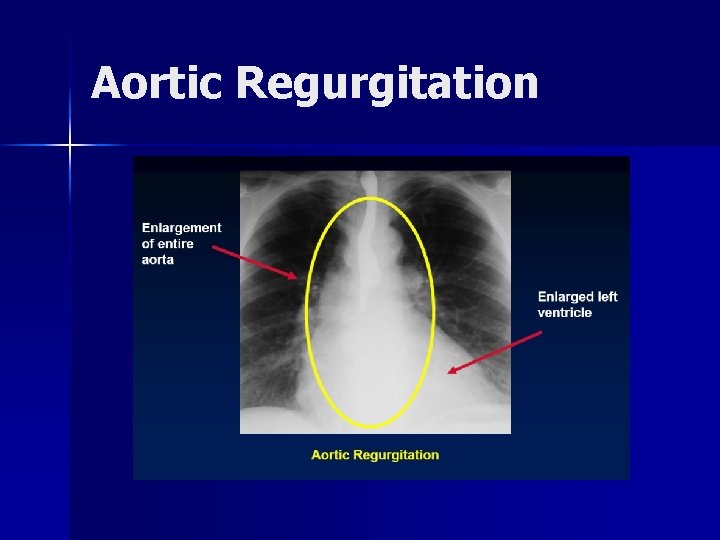
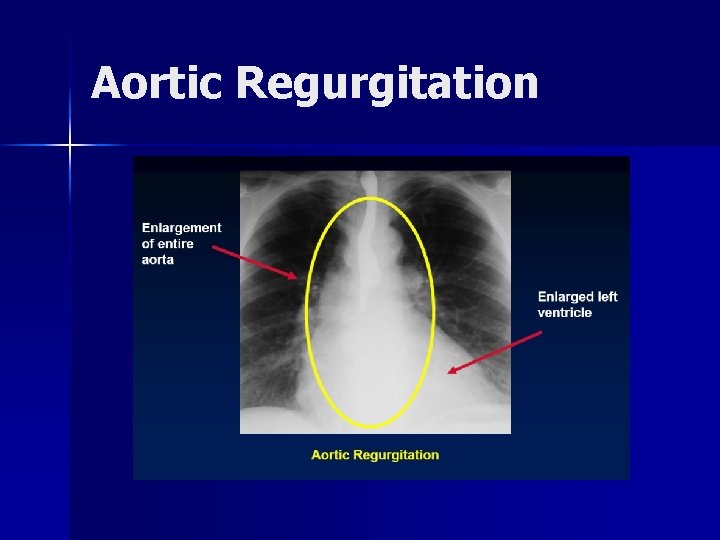
Aortic Regurgitation
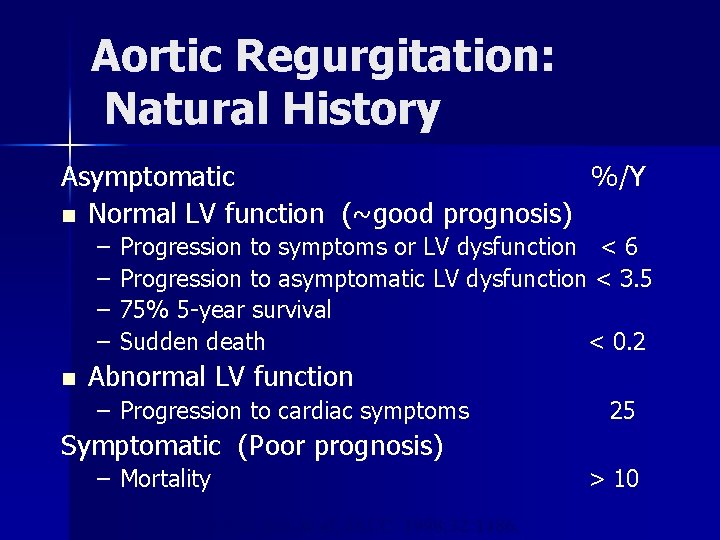
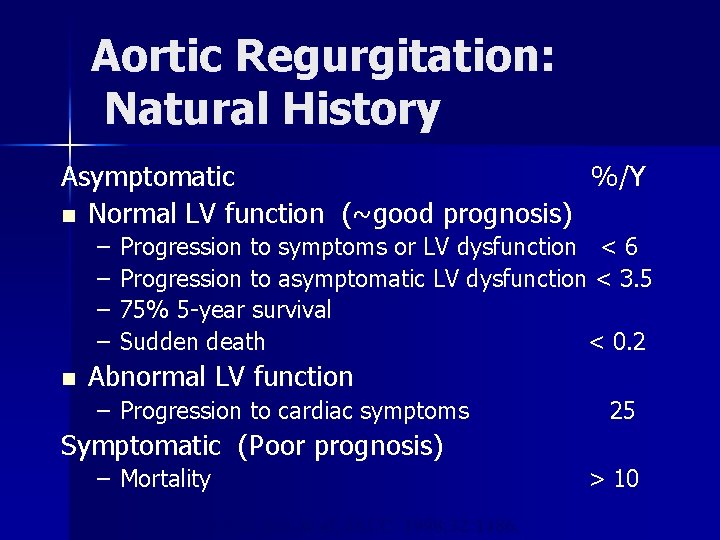
Aortic Regurgitation: Natural History Asymptomatic %/Y n Normal LV function (~good prognosis) – – n Progression to symptoms or LV dysfunction < 6 Progression to asymptomatic LV dysfunction < 3. 5 75% 5 -year survival Sudden death < 0. 2 Abnormal LV function – Progression to cardiac symptoms 25 Symptomatic (Poor prognosis) – Mortality Bonow RO, et al, JACC. 1998; 32: 1486. > 10
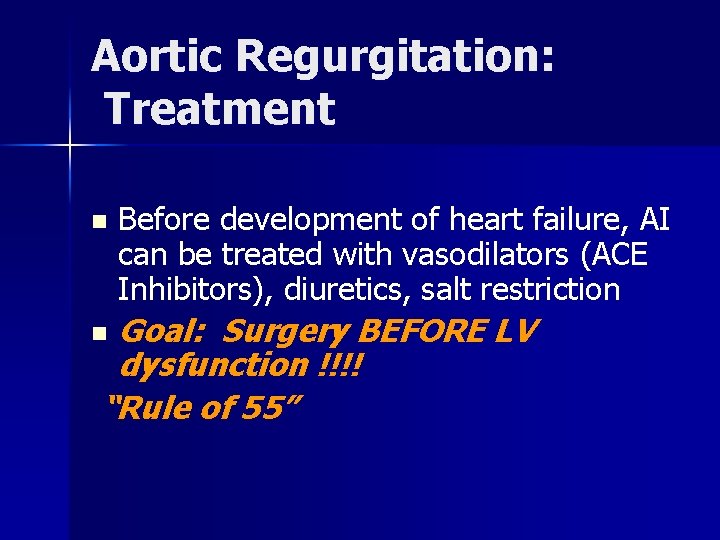
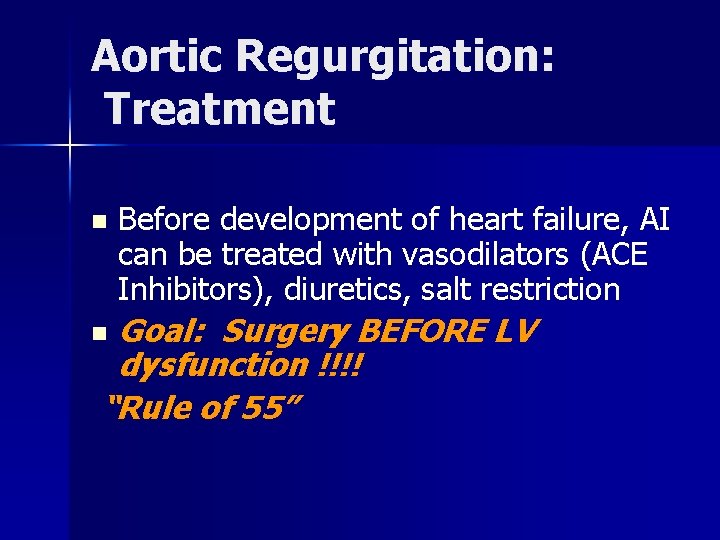
Aortic Regurgitation: Treatment n Before development of heart failure, AI can be treated with vasodilators (ACE Inhibitors), diuretics, salt restriction Goal: Surgery BEFORE LV dysfunction !!!! “Rule of 55” n
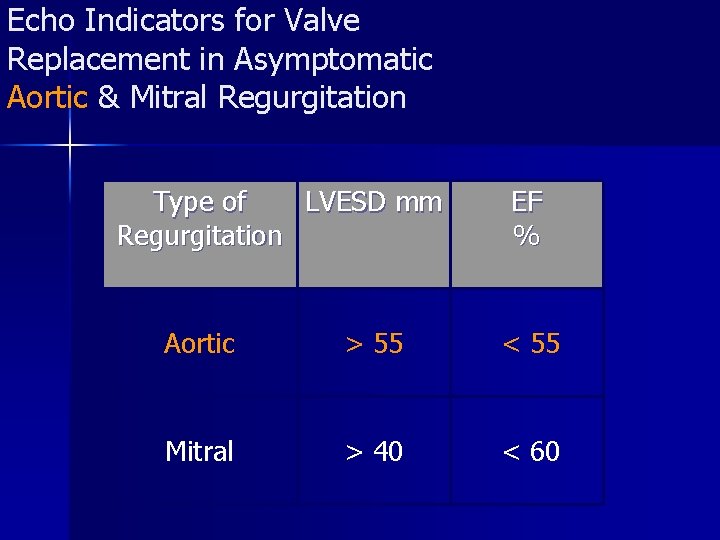
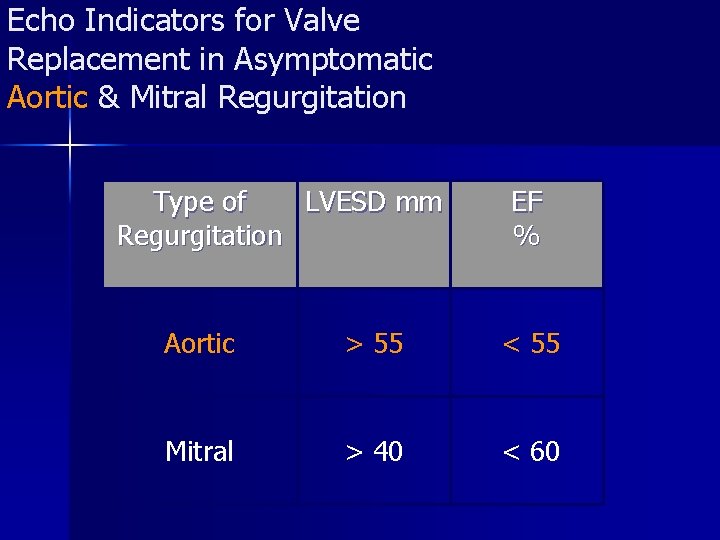
Echo Indicators for Valve Replacement in Asymptomatic Aortic & Mitral Regurgitation Type of LVESD mm Regurgitation EF % Aortic > 55 < 55 Mitral > 40 < 60
A 75 year old woman with Recent orthopnea/PND n n n Chronic dyspnea Class 2/4 Fatigue Recent orthopnea/PND Nocturnal palpitation Pedal edema

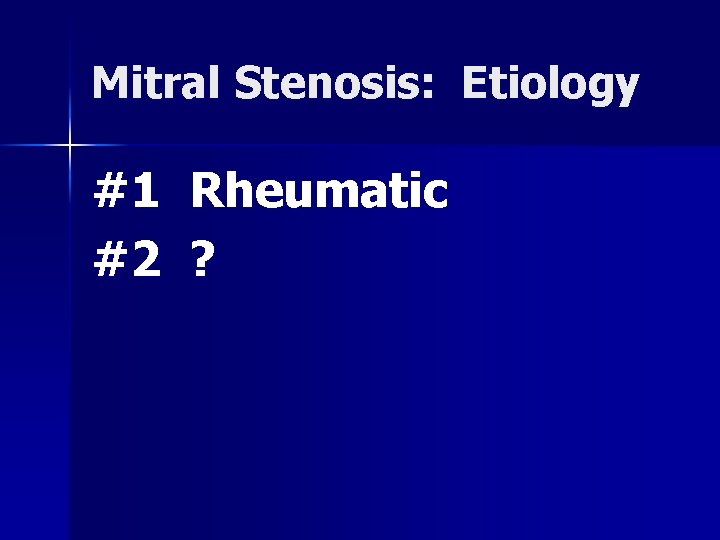
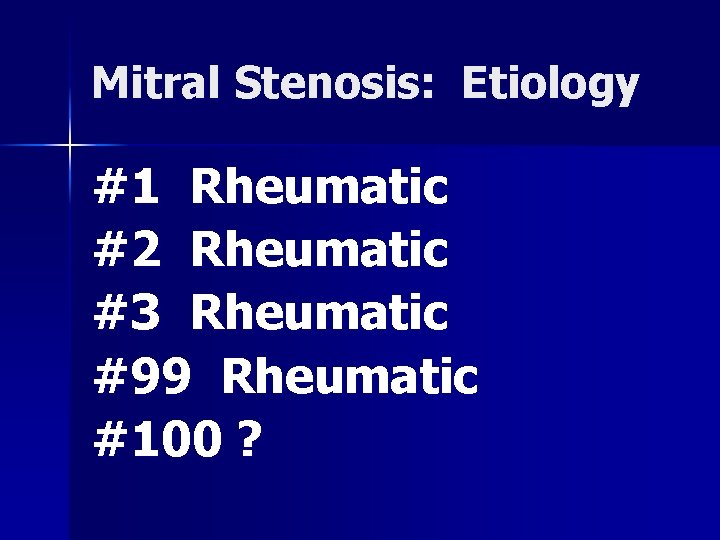
Mitral Stenosis: Etiology #1 Rheumatic
Mitral Stenosis: Etiology #1 Rheumatic #2 ?
Mitral Stenosis: Etiology #1 Rheumatic #2 Rheumatic
Mitral Stenosis: Etiology #1 #2 #3 Rheumatic
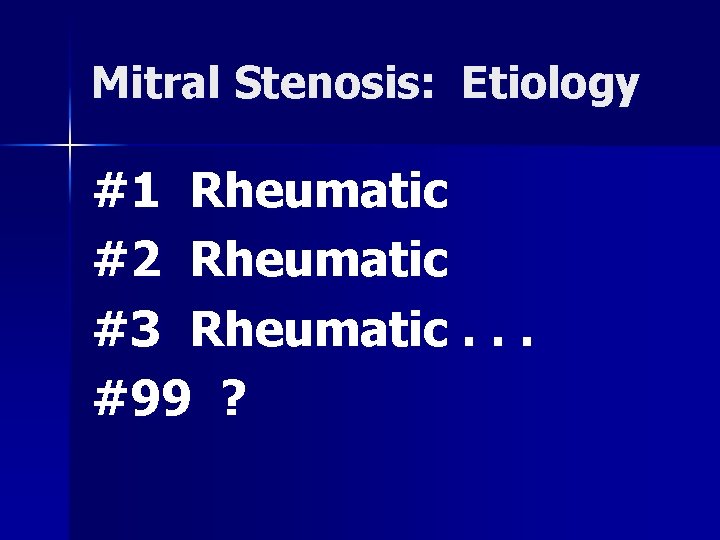
Mitral Stenosis: Etiology #1 Rheumatic #2 Rheumatic #3 Rheumatic. . . #99 ?
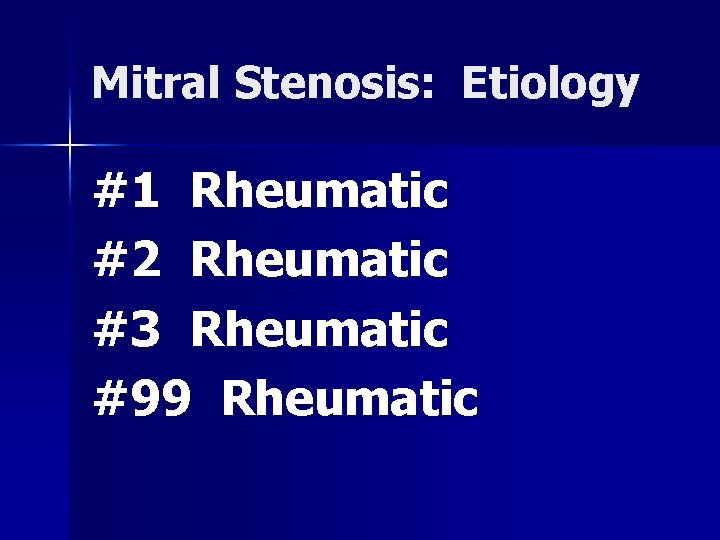
Mitral Stenosis: Etiology #1 Rheumatic #2 Rheumatic #3 Rheumatic #99 Rheumatic
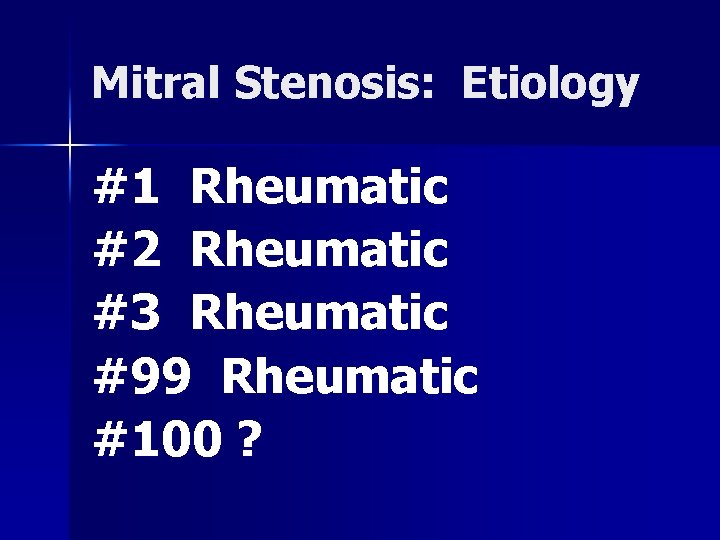
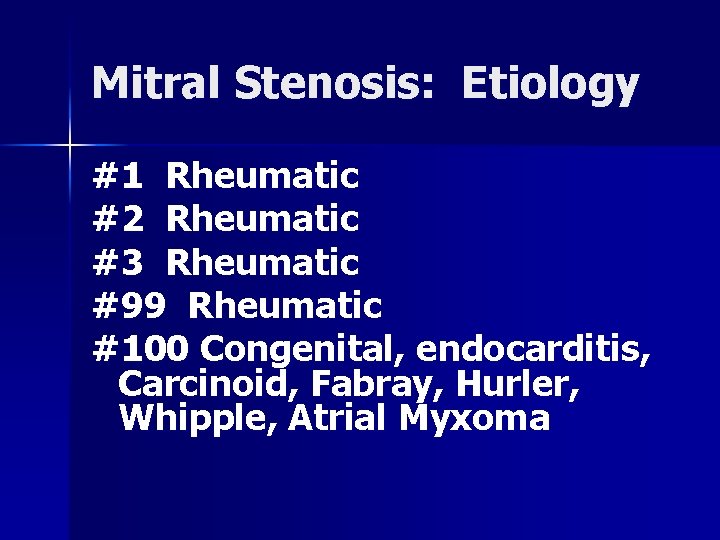
Mitral Stenosis: Etiology #1 Rheumatic #2 Rheumatic #3 Rheumatic #99 Rheumatic #100 ?
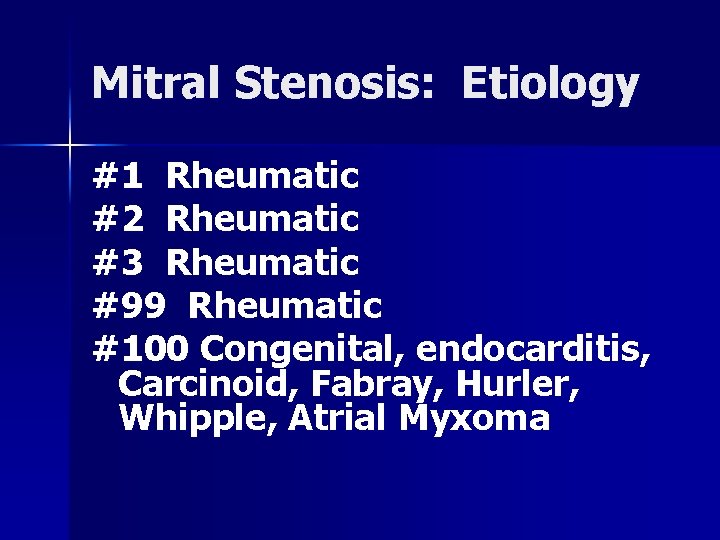
Mitral Stenosis: Etiology #1 Rheumatic #2 Rheumatic #3 Rheumatic #99 Rheumatic #100 Congenital, endocarditis, Carcinoid, Fabray, Hurler, Whipple, Atrial Myxoma
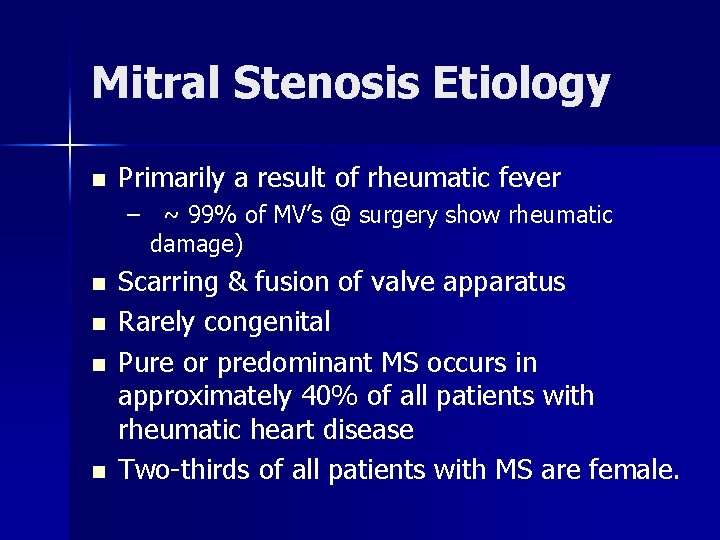
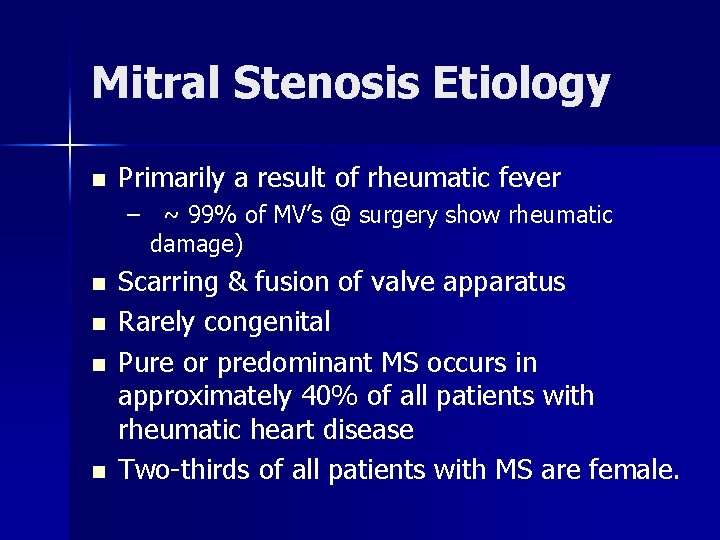
Mitral Stenosis Etiology n Primarily a result of rheumatic fever – ~ 99% of MV’s @ surgery show rheumatic damage) n n Scarring & fusion of valve apparatus Rarely congenital Pure or predominant MS occurs in approximately 40% of all patients with rheumatic heart disease Two-thirds of all patients with MS are female.
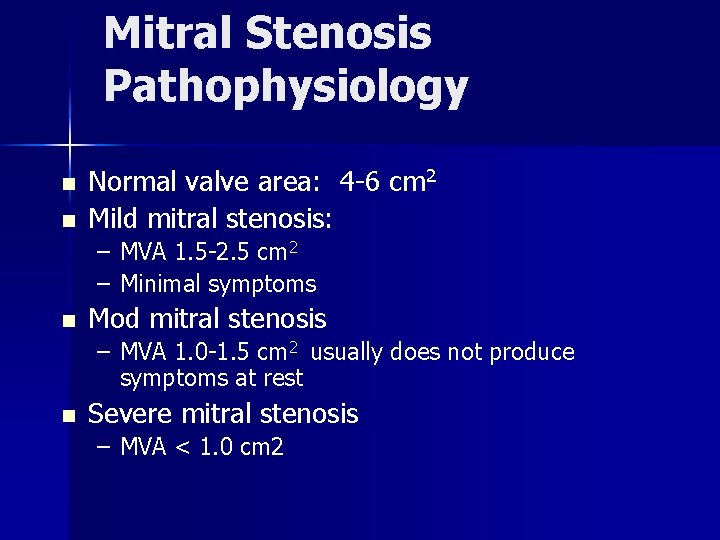
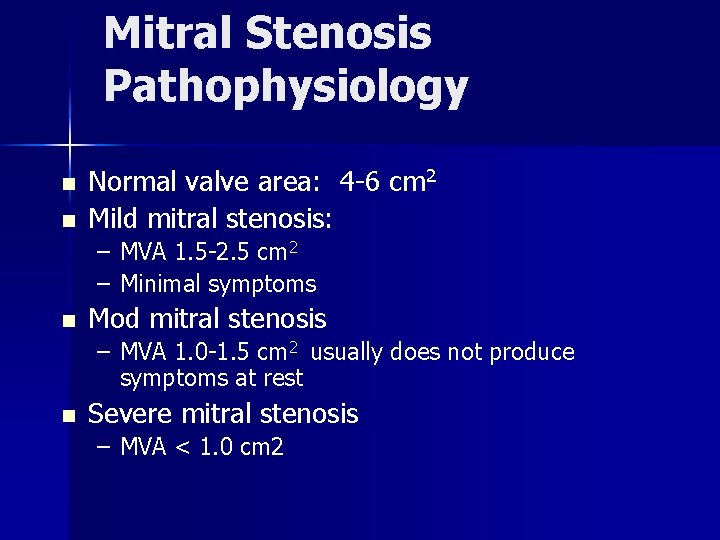
Mitral Stenosis Pathophysiology n n Normal valve area: 4 -6 cm 2 Mild mitral stenosis: – MVA 1. 5 -2. 5 cm 2 – Minimal symptoms n Mod mitral stenosis – MVA 1. 0 -1. 5 cm 2 usually does not produce symptoms at rest n Severe mitral stenosis – MVA < 1. 0 cm 2

Mitral Valve Stenosis Pathophysiology Right Heart Failure: Hepatic Congestion JVD Tricuspid Regurgitation RA Enlargement RV Pressure Overload RVH RV Failure Pulmonary HTN Pulmonary Congestion LA Enlargement Atrial Fib LA Thrombi LA Pressure LV Filling
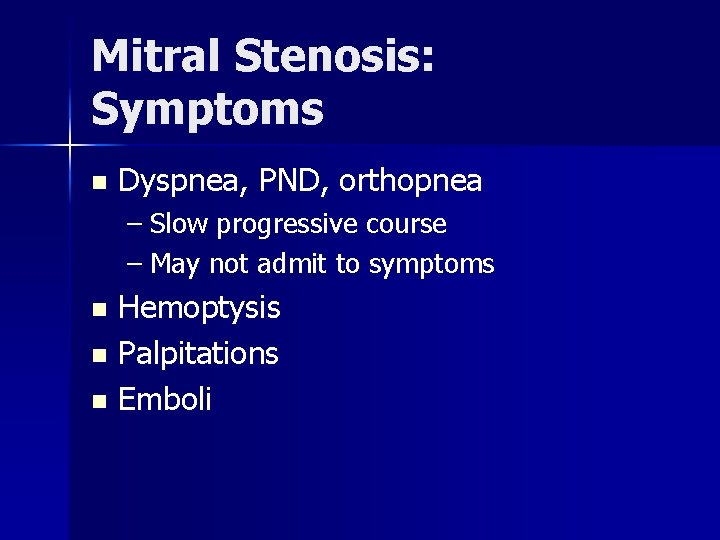
Mitral Stenosis: Symptoms n Dyspnea, PND, orthopnea – Slow progressive course – May not admit to symptoms Hemoptysis n Palpitations n Emboli n
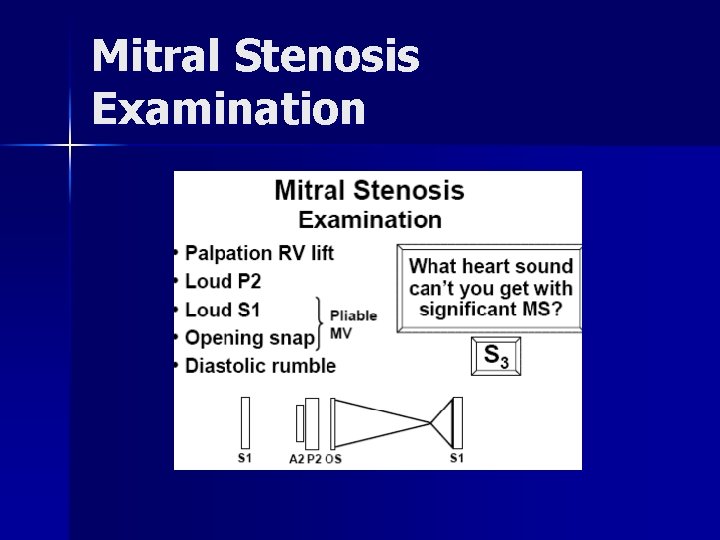
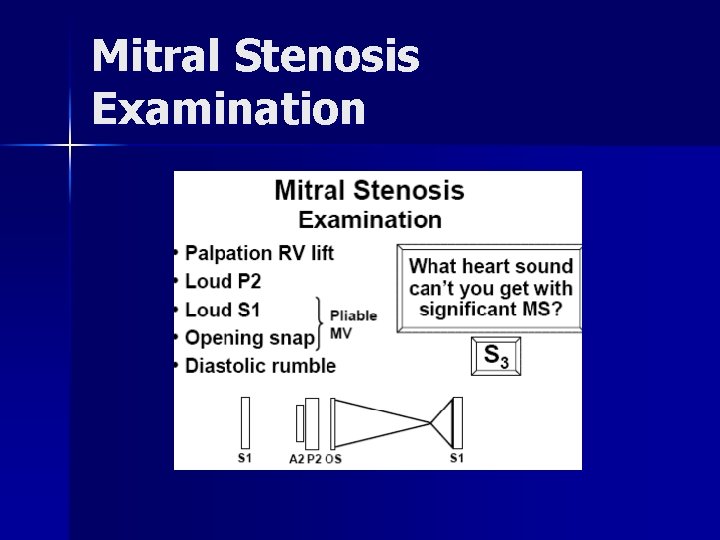
Mitral Stenosis Examination
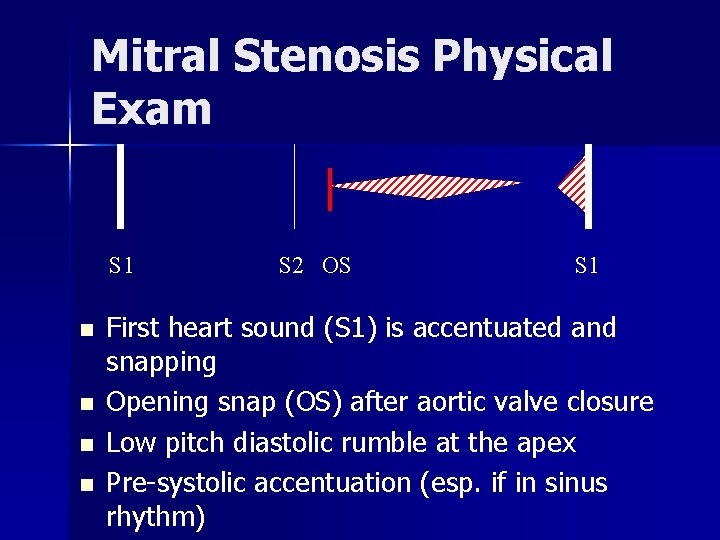
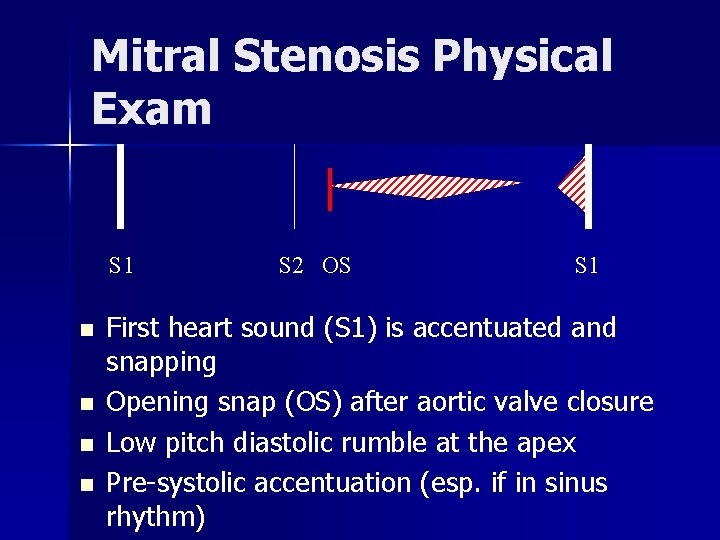
Mitral Stenosis Physical Exam S 1 n n S 2 OS S 1 First heart sound (S 1) is accentuated and snapping Opening snap (OS) after aortic valve closure Low pitch diastolic rumble at the apex Pre-systolic accentuation (esp. if in sinus rhythm)
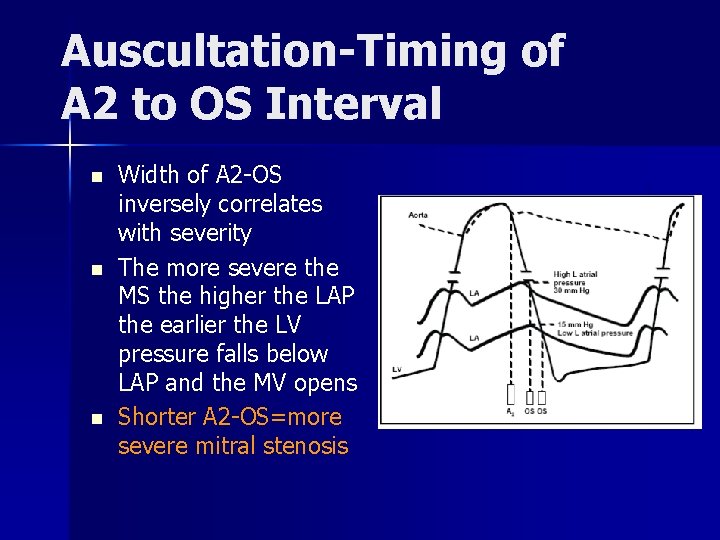
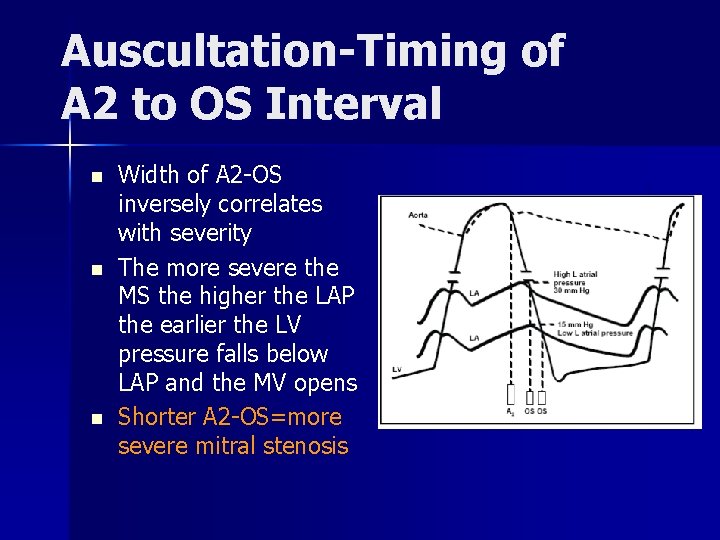
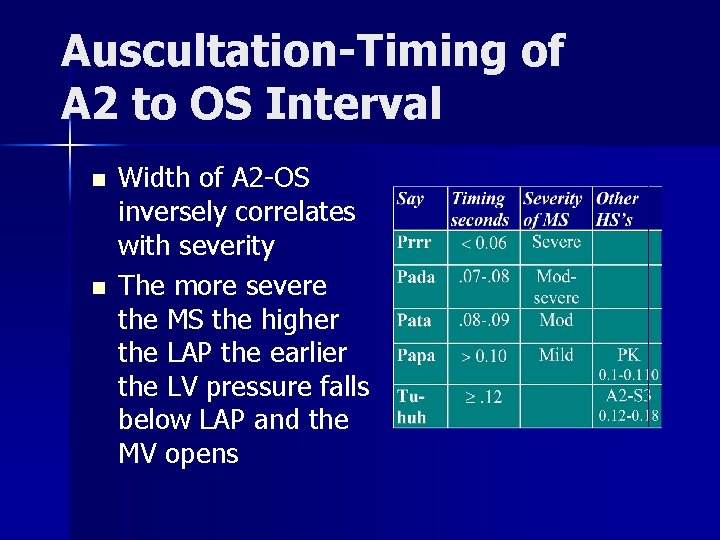
Auscultation-Timing of A 2 to OS Interval n n n Width of A 2 -OS inversely correlates with severity The more severe the MS the higher the LAP the earlier the LV pressure falls below LAP and the MV opens Shorter A 2 -OS=more severe mitral stenosis
Mitral Stenosis: ECG LAE n With pulm HTN: RAD, RVH n AFIB n


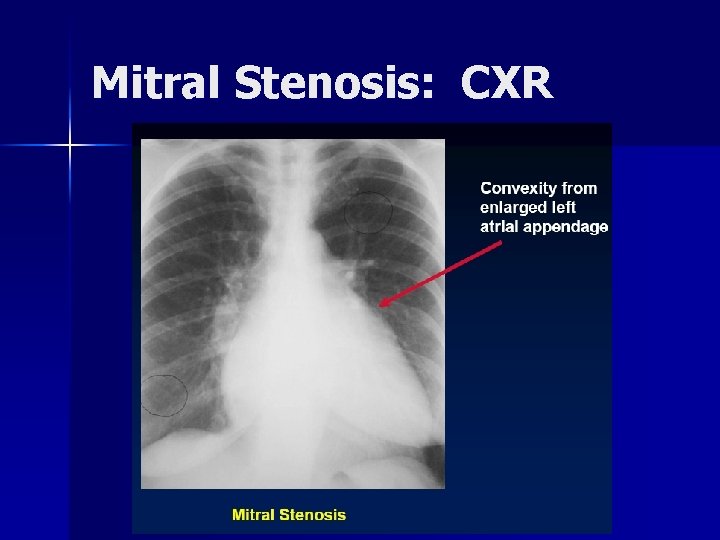
Mitral Stenosis: CXR
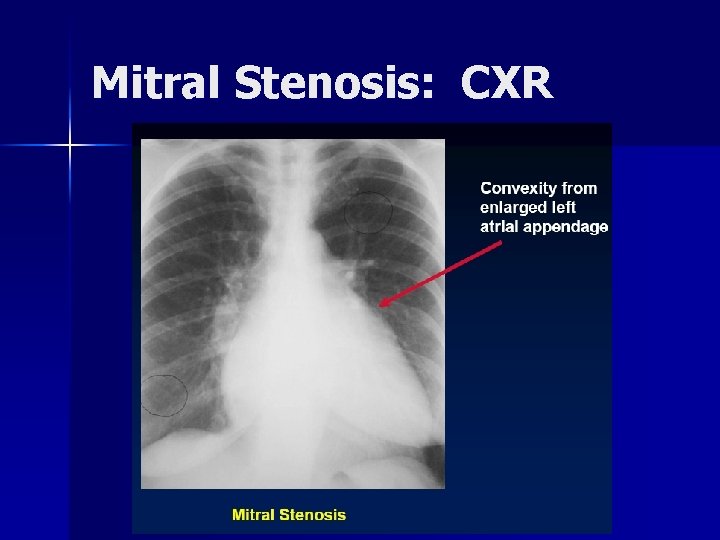
Mitral Stenosis: CXR
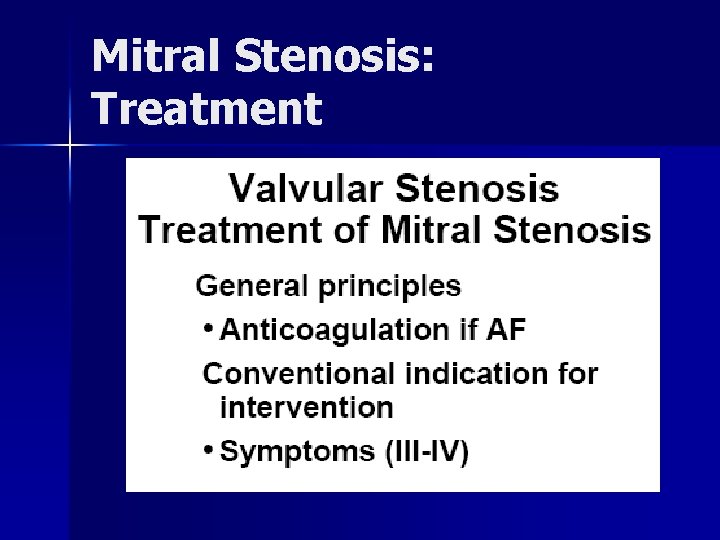
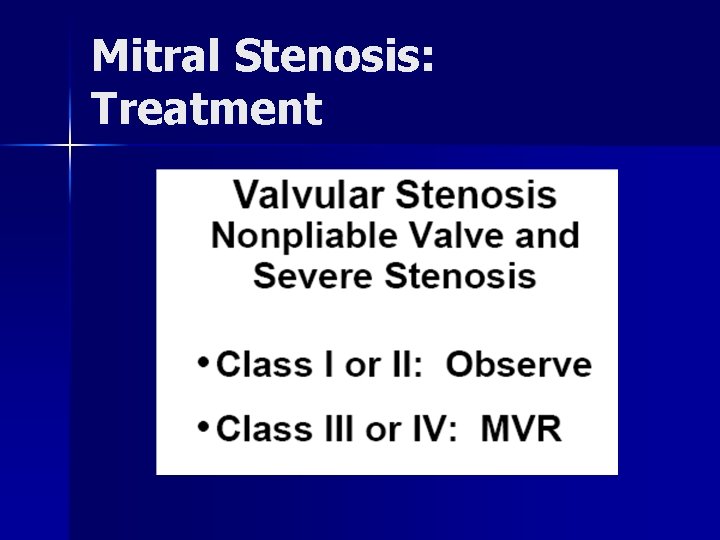
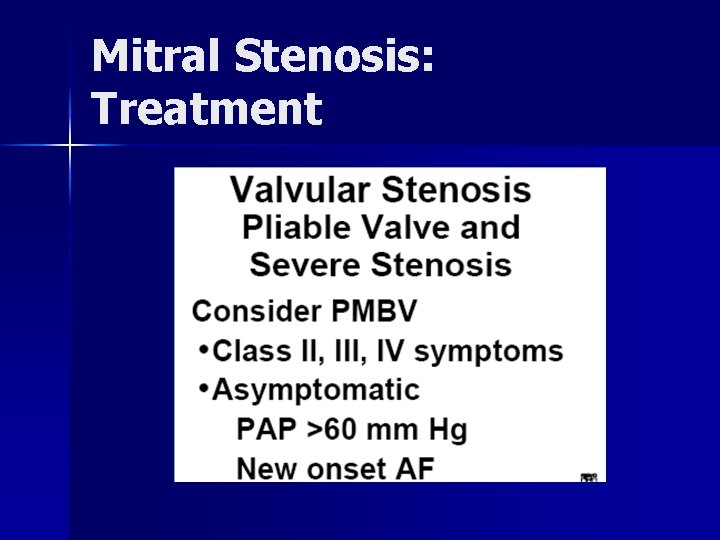
Mitral Stenosis: Treatment
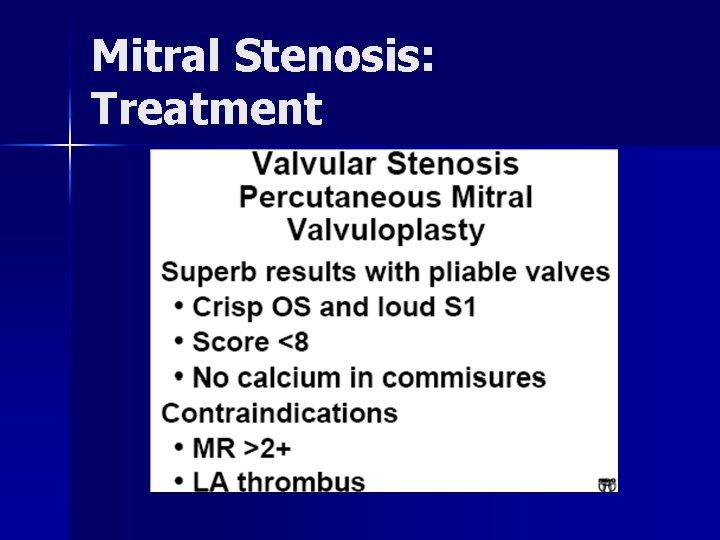
Mitral Stenosis: Treatment
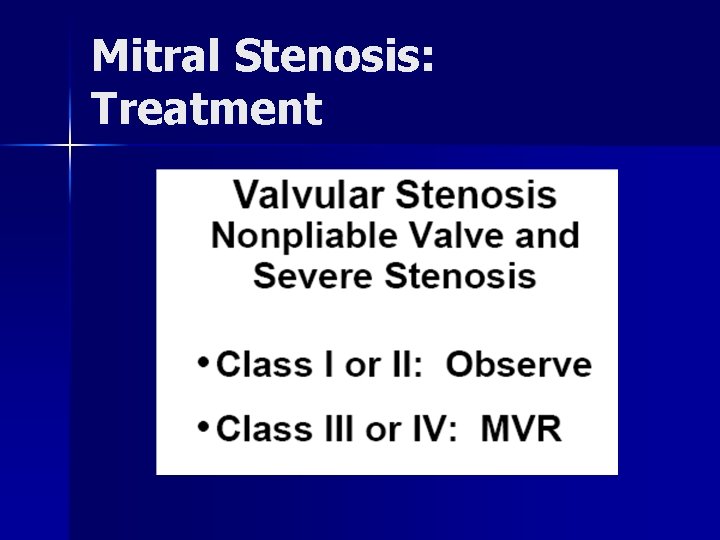
Mitral Stenosis: Treatment
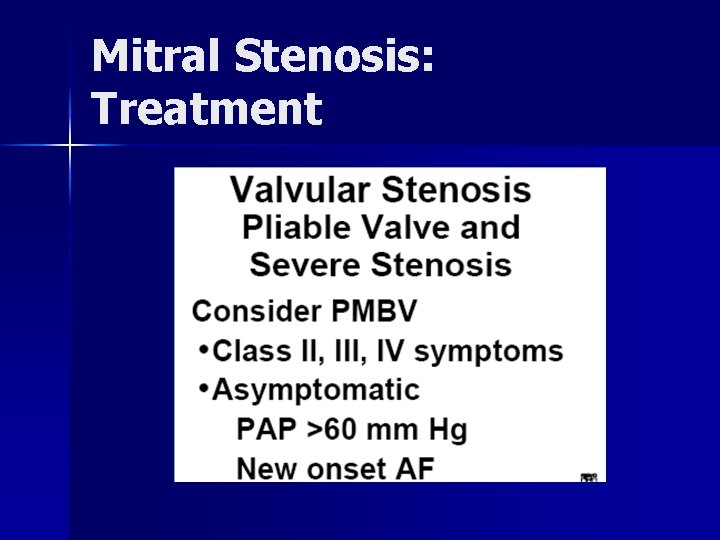
Mitral Stenosis: Treatment
An 80 year old woman with increasing dyspnea n n n Longstanding heart murmur Increasing dyspnea & fatigue Recent ER visit Dx CHF
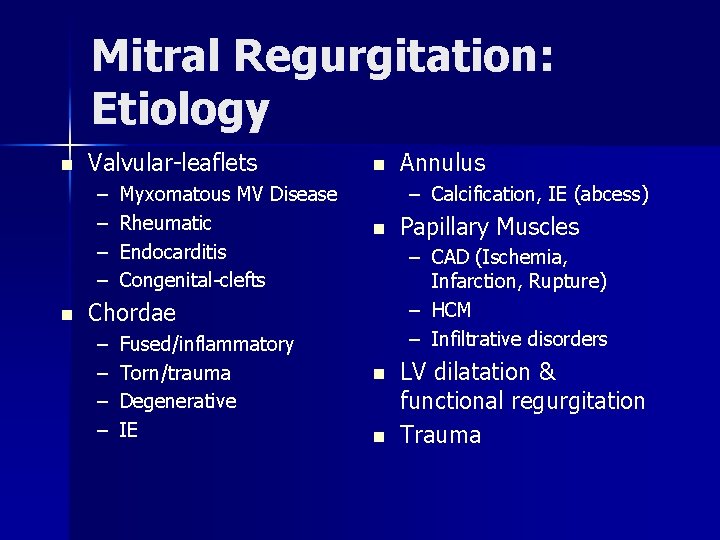
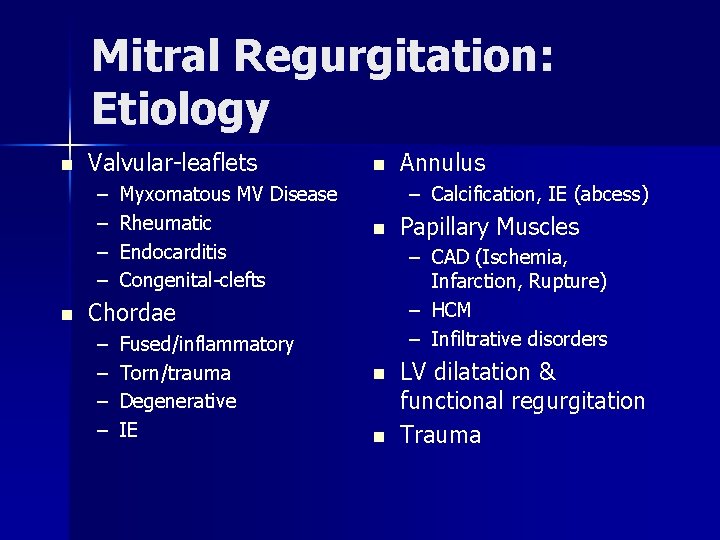
Mitral Regurgitation: Etiology n Valvular-leaflets – – n Myxomatous MV Disease Rheumatic Endocarditis Congenital-clefts n – Calcification, IE (abcess) n Fused/inflammatory Torn/trauma Degenerative IE Papillary Muscles – CAD (Ischemia, Infarction, Rupture) – HCM – Infiltrative disorders Chordae – – Annulus n n LV dilatation & functional regurgitation Trauma
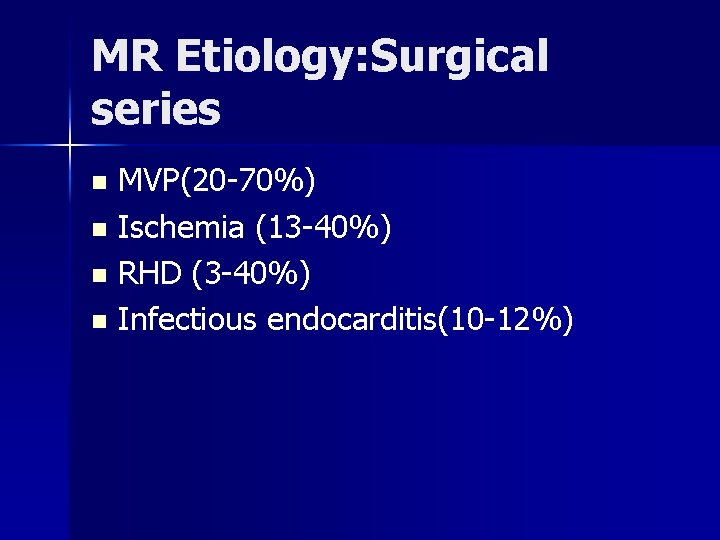
MR Etiology: Surgical series MVP(20 -70%) n Ischemia (13 -40%) n RHD (3 -40%) n Infectious endocarditis(10 -12%) n
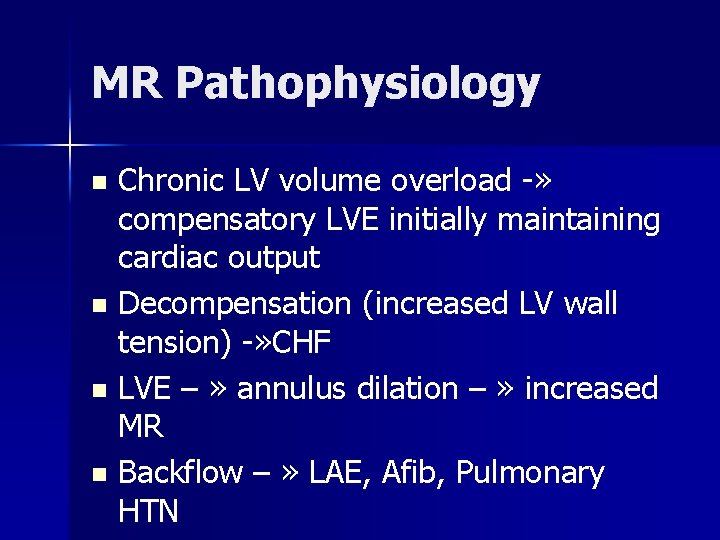
MR Pathophysiology Chronic LV volume overload -» compensatory LVE initially maintaining cardiac output n Decompensation (increased LV wall tension) -» CHF n LVE – » annulus dilation – » increased MR n Backflow – » LAE, Afib, Pulmonary HTN n
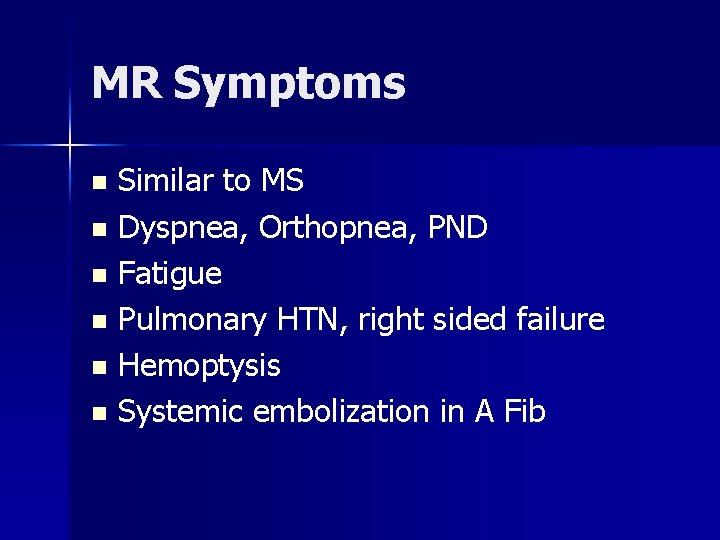
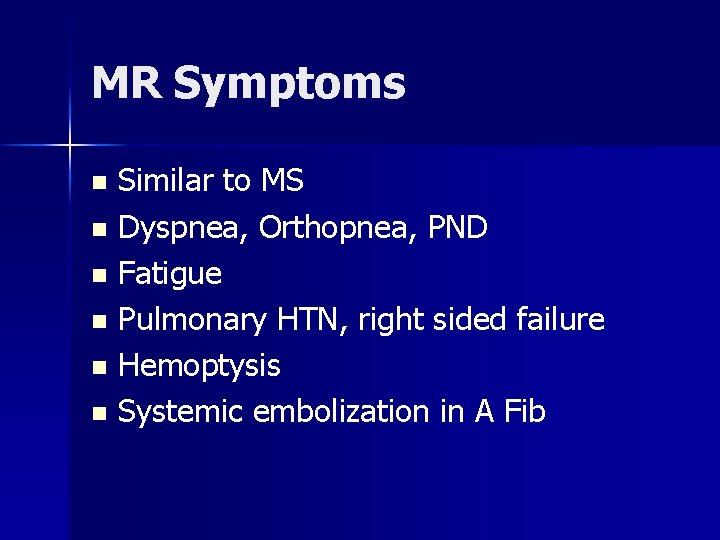
MR Symptoms Similar to MS n Dyspnea, Orthopnea, PND n Fatigue n Pulmonary HTN, right sided failure n Hemoptysis n Systemic embolization in A Fib n
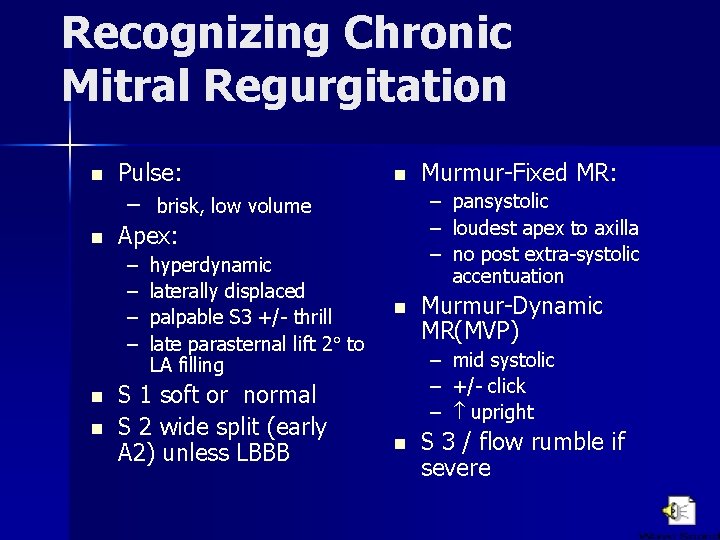
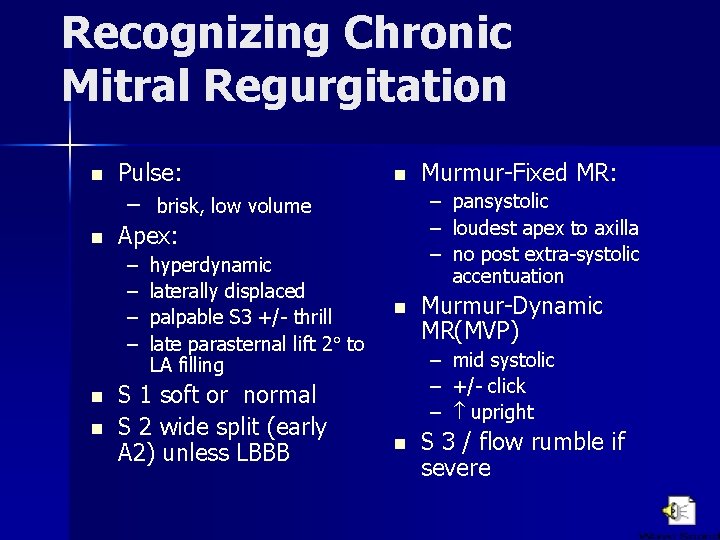
Recognizing Chronic Mitral Regurgitation n n Pulse: – brisk, low volume Apex: – – n n hyperdynamic laterally displaced palpable S 3 +/- thrill late parasternal lift 2 to LA filling S 1 soft or normal S 2 wide split (early A 2) unless LBBB n Murmur-Fixed MR: – pansystolic – loudest apex to axilla – no post extra-systolic accentuation n Murmur-Dynamic MR(MVP) – – – n mid systolic +/- click upright S 3 / flow rumble if severe
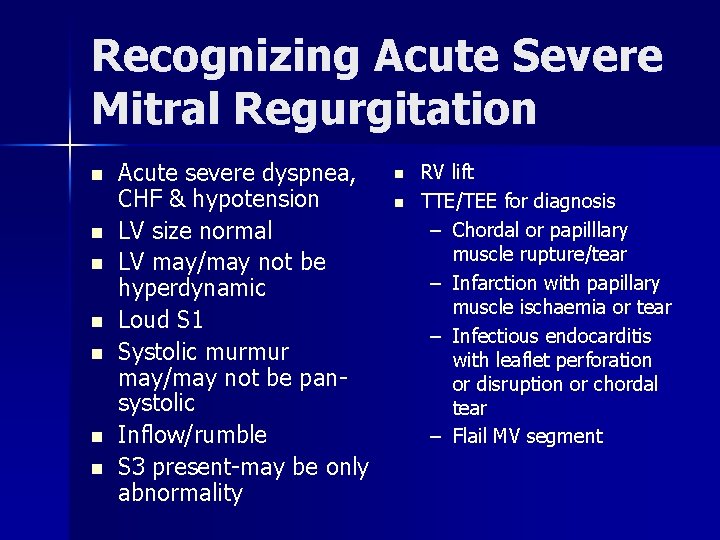
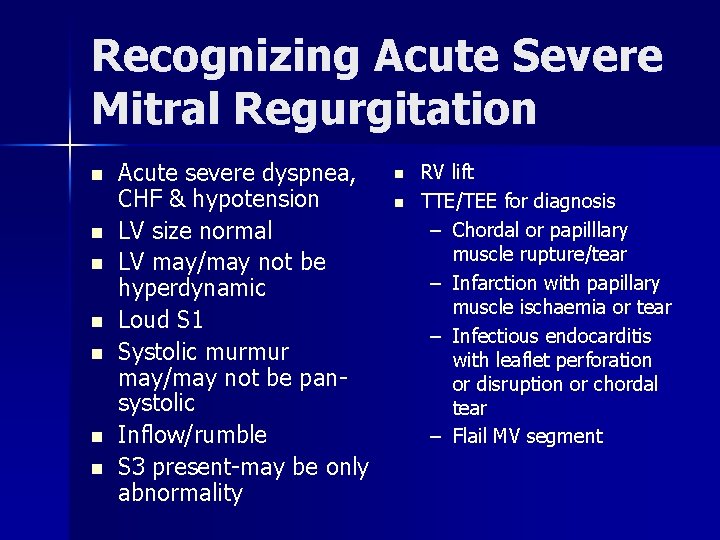
Recognizing Acute Severe Mitral Regurgitation n n n Acute severe dyspnea, CHF & hypotension LV size normal LV may/may not be hyperdynamic Loud S 1 Systolic murmur may/may not be pansystolic Inflow/rumble S 3 present-may be only abnormality n n RV lift TTE/TEE for diagnosis – Chordal or papilllary muscle rupture/tear – Infarction with papillary muscle ischaemia or tear – Infectious endocarditis with leaflet perforation or disruption or chordal tear – Flail MV segment
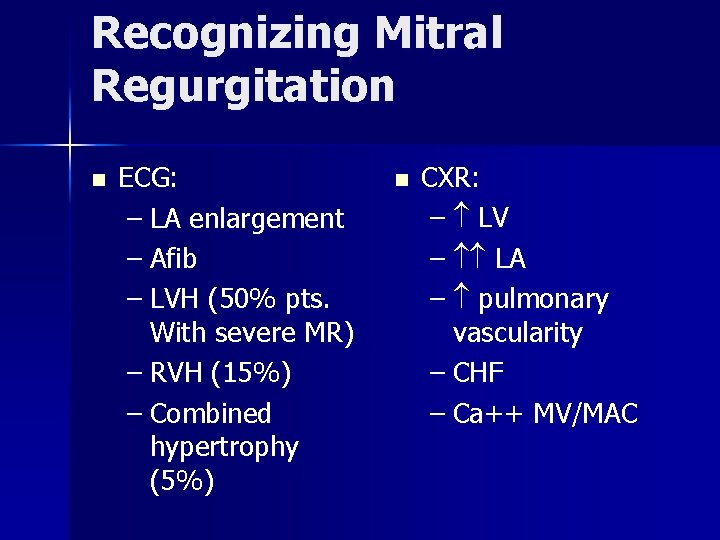
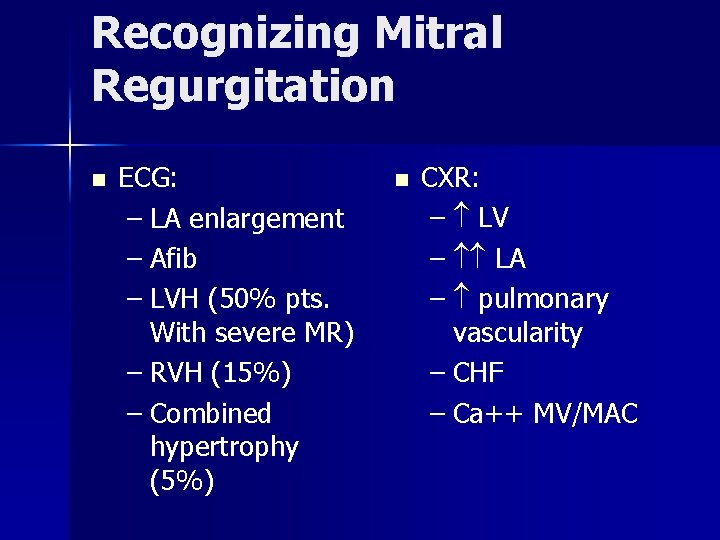
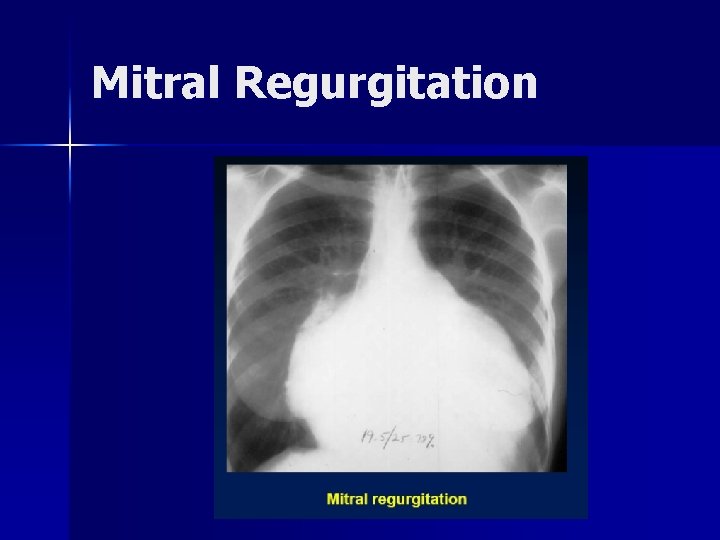
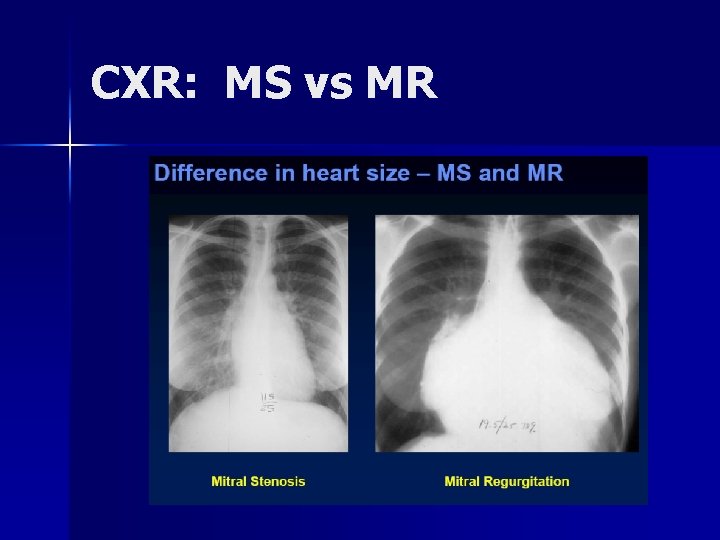
Recognizing Mitral Regurgitation n ECG: – LA enlargement – Afib – LVH (50% pts. With severe MR) – RVH (15%) – Combined hypertrophy (5%) n CXR: – LV – LA – pulmonary vascularity – CHF – Ca++ MV/MAC
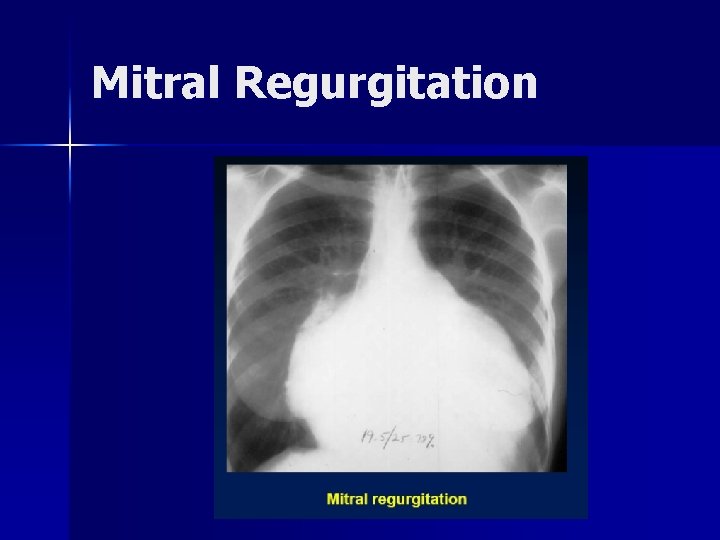
Mitral Regurgitation
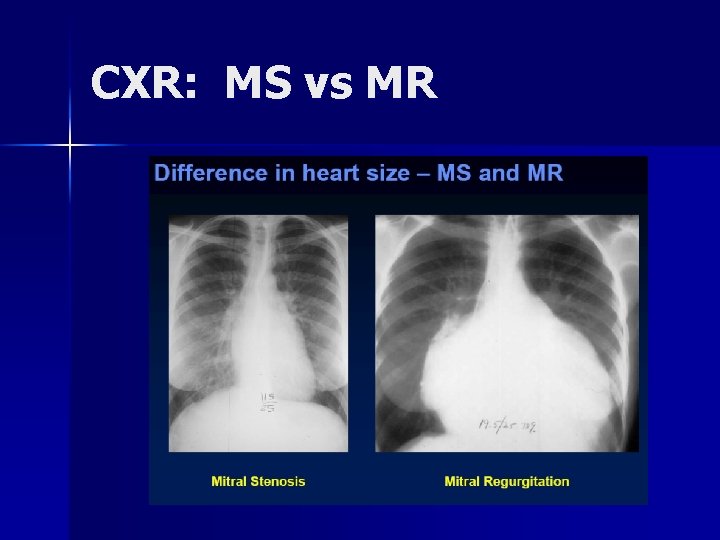
CXR: MS vs MR
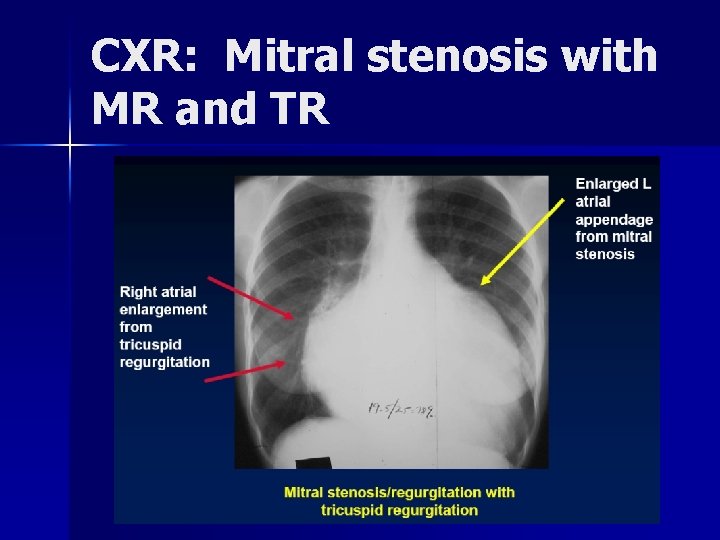
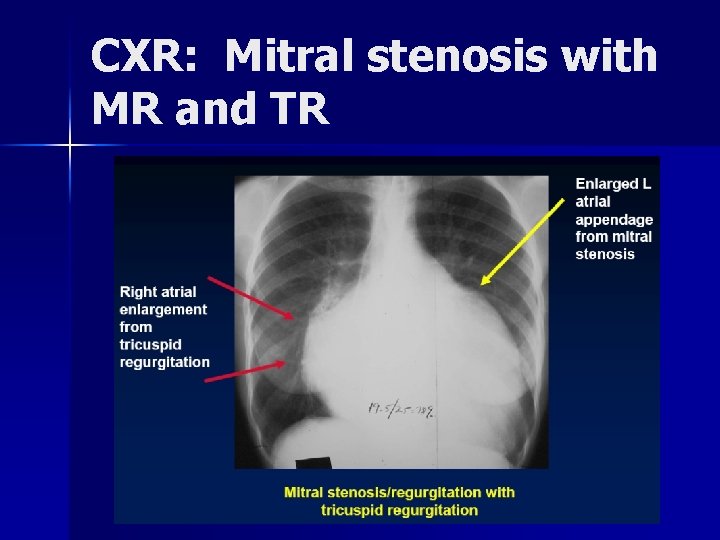
CXR: Mitral stenosis with MR and TR
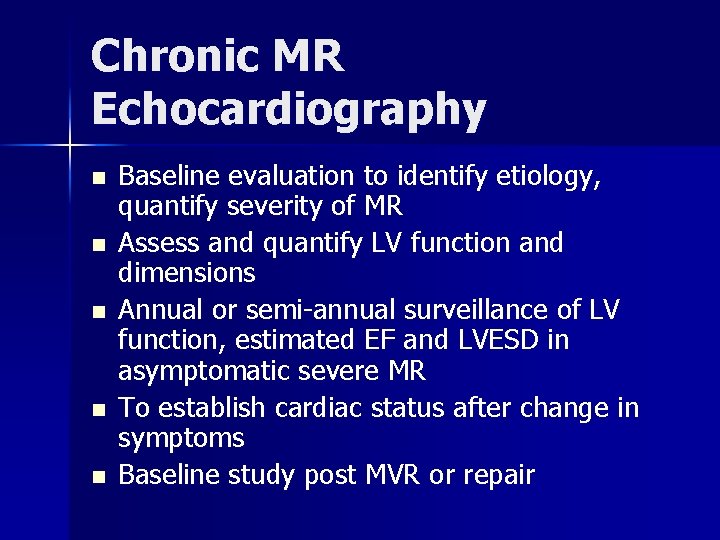
Chronic MR Echocardiography n n n Baseline evaluation to identify etiology, quantify severity of MR Assess and quantify LV function and dimensions Annual or semi-annual surveillance of LV function, estimated EF and LVESD in asymptomatic severe MR To establish cardiac status after change in symptoms Baseline study post MVR or repair

Echo Indicators for Valve Replacement in Asymptomatic Aortic & Mitral Regurgitation Type of LVESD mm Regurgitation EF % Aortic > 55 < 55 Mitral > 40 < 60
Mitral Valve Prolapse: Epidemiology n n n Affects 5 -10% of population Most common cause of isolated severe MR Females >> males; Ages of 14 and 30 years Strong hereditary component (? autosomal dominant) 2º to failure of apposition/coaptation of the anterior and posterior mitral valve leaflets. Results form diverse pathologic conditions, but cause is unknown in a majority of pts

Mitral Valve Prolapse: Symptoms Majority are asymptomatic for entire life n Palpitations n Chest pain (atypical). n – Often substernal, prolonged, poorly related to exertion, and rarely resembles typical angina n Syncope
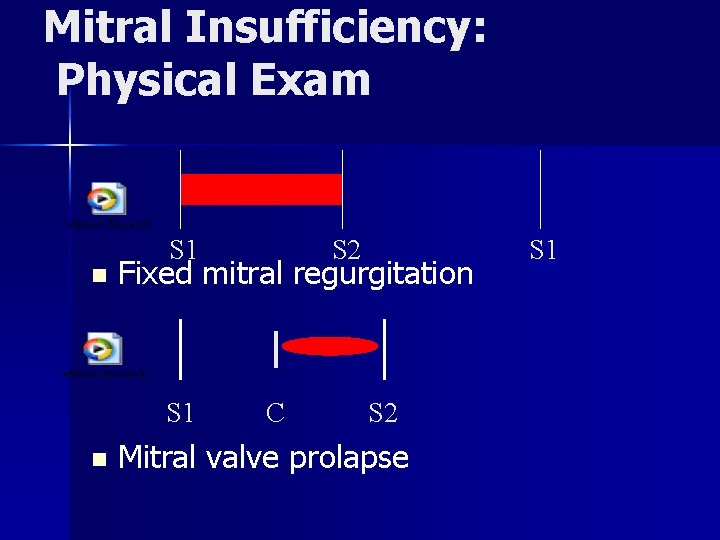
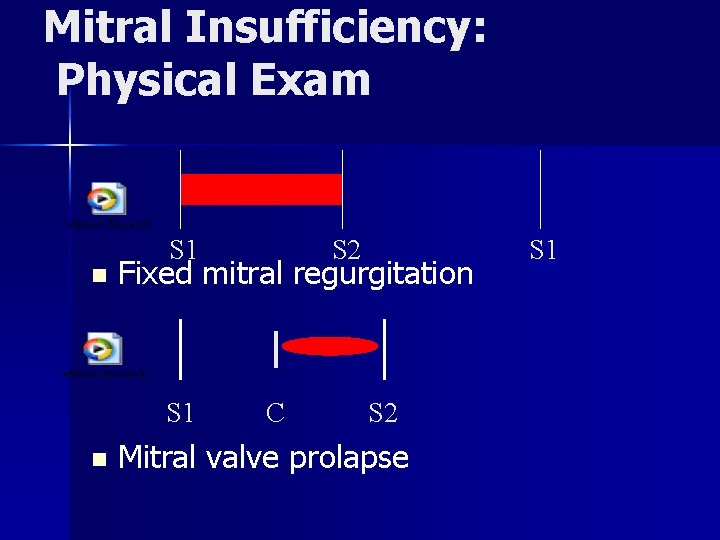
Mitral Insufficiency: Physical Exam n S 1 Fixed mitral regurgitation S 1 n S 2 C S 2 Mitral valve prolapse S 1
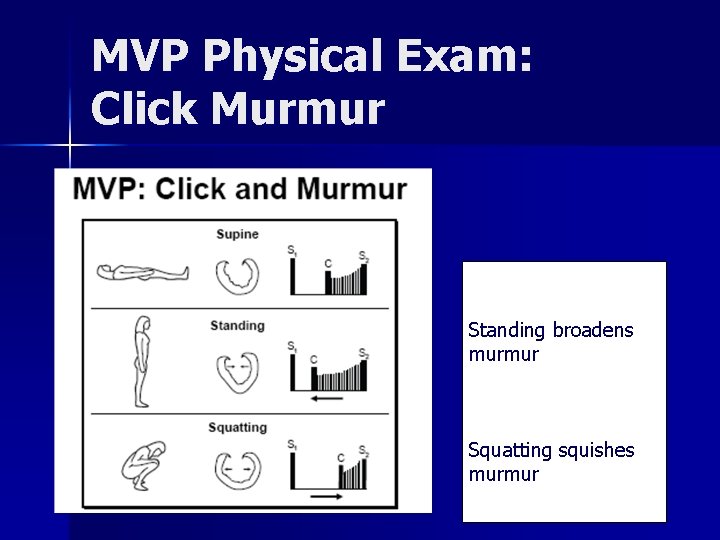
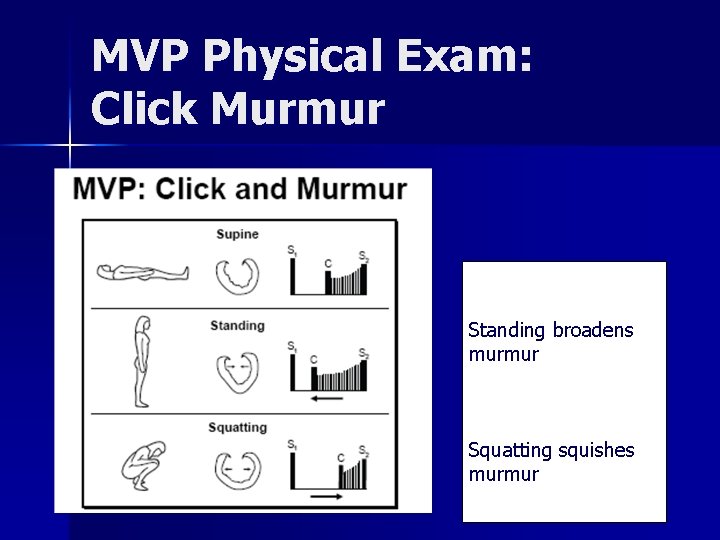
MVP Physical Exam: Click Murmur Standing broadens murmur Squatting squishes murmur
Mitral Valve Prolapse: Complications Arrhythmias (Usually PVC, PSVT>>VT) n Transient cerebral ischemic (embolic – rare) n Infective endocarditis (if assoc w/ MR) n Sudden death (rare) n
MVP Treatment Watch for mitral regurgitation n As with MR, surgery when LVESD>40 mm or EF <60%. n
Thanks! © Continuing Medical Implementation …. . . bridging the care gap

PS


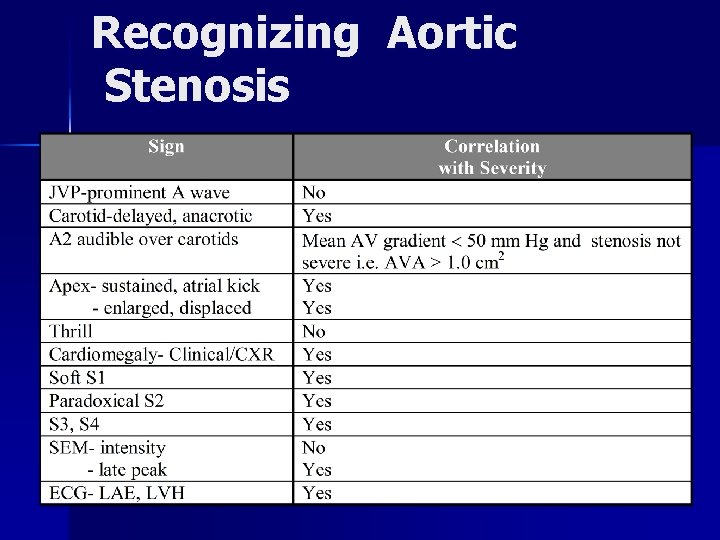
Recognizing Aortic Stenosis

Echo Indicators for Valve Replacement in Asymptomatic Aortic & Mitral Regurgitation Type of LVESD mm Regurgitation EF FS % Aortic > 55 < 0. 27 Mitral > 45 < 60 < 0. 32
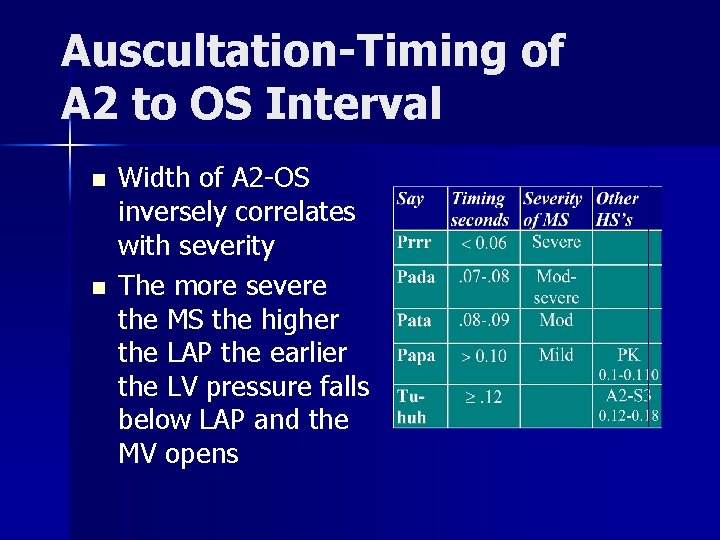
Auscultation-Timing of A 2 to OS Interval n n Width of A 2 -OS inversely correlates with severity The more severe the MS the higher the LAP the earlier the LV pressure falls below LAP and the MV opens

Echo Indicators for Valve Replacement in Asymptomatic Aortic & Mitral Regurgitation Type of LVESD mm Regurgitatio n EF FS % Aortic > 55 < 0. 27 Mitral > 45 < 60 < 0. 32

Recognizing Mitral Stenosis Palpation: n n n Small volume pulse n Tapping apex-palpable S 1 n +/- palpable opening snap (OS) n RV lift n Palpable S 2 ECG: n Auscultation: LAE, AFIB, RVH, RAD Loud S 1 - as loud as S 2 in aortic area A 2 to OS interval inversely proportional to severity Diastolic rumble: length proportional to severity In severe MS with low flow- S 1, OS & rumble may be inaudible

Mitral Stenosis: Symptoms
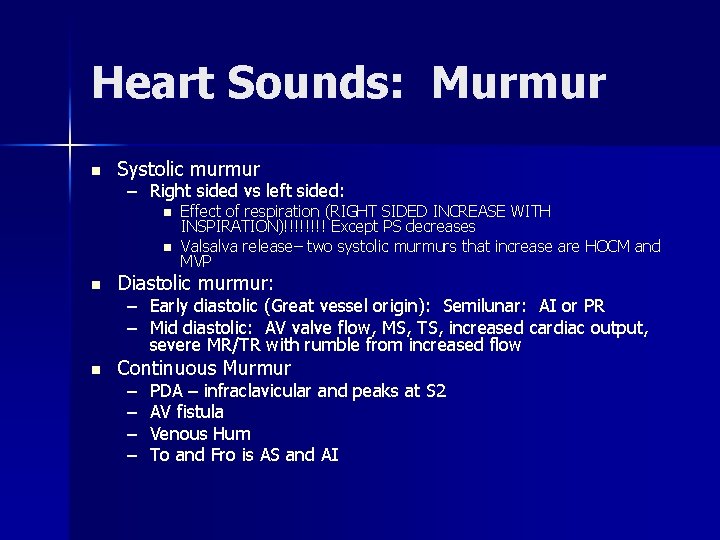
Heart Sounds: Murmur n Systolic murmur – Right sided vs left sided: n n Effect of respiration (RIGHT SIDED INCREASE WITH INSPIRATION)!!!! Except PS decreases Valsalva release– two systolic murmurs that increase are HOCM and MVP n Diastolic murmur: n Continuous Murmur – Early diastolic (Great vessel origin): Semilunar: AI or PR – Mid diastolic: AV valve flow, MS, TS, increased cardiac output, severe MR/TR with rumble from increased flow – – PDA – infraclavicular and peaks at S 2 AV fistula Venous Hum To and Fro is AS and AI
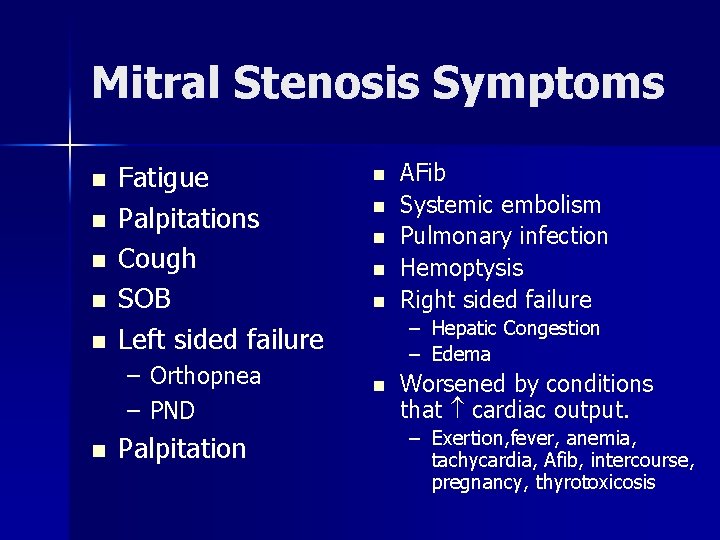
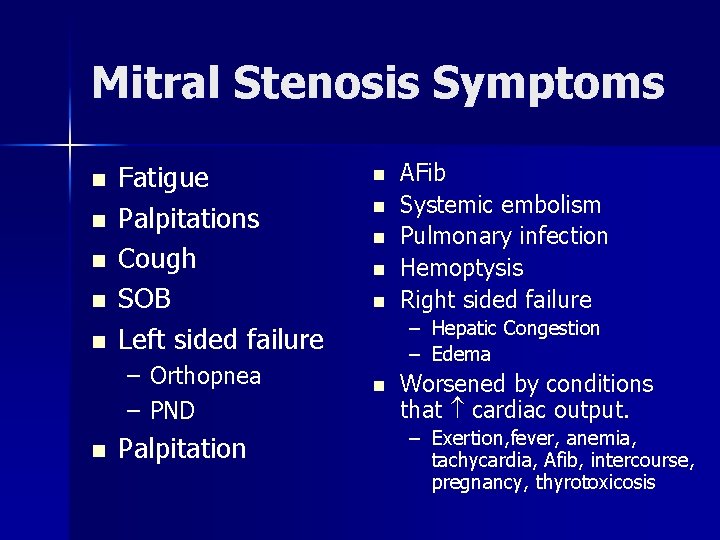
Mitral Stenosis Symptoms n n n Fatigue Palpitations Cough SOB Left sided failure – Orthopnea – PND n Palpitation n n AFib Systemic embolism Pulmonary infection Hemoptysis Right sided failure – Hepatic Congestion – Edema n Worsened by conditions that cardiac output. – Exertion, fever, anemia, tachycardia, Afib, intercourse, pregnancy, thyrotoxicosis
Aortic Regurgitation: Symptoms n n Dyspnea, orthopnea, PND With extreme reductions in diastolic pressures (e. g. < 40) may see angina
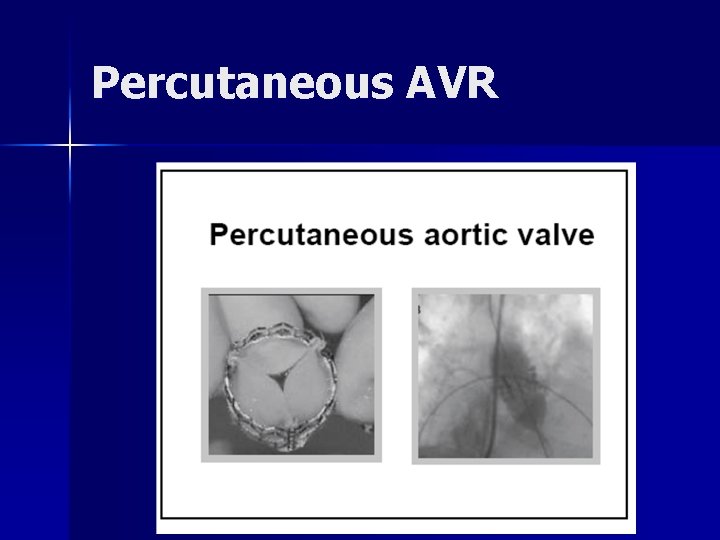
Percutaneous AVR
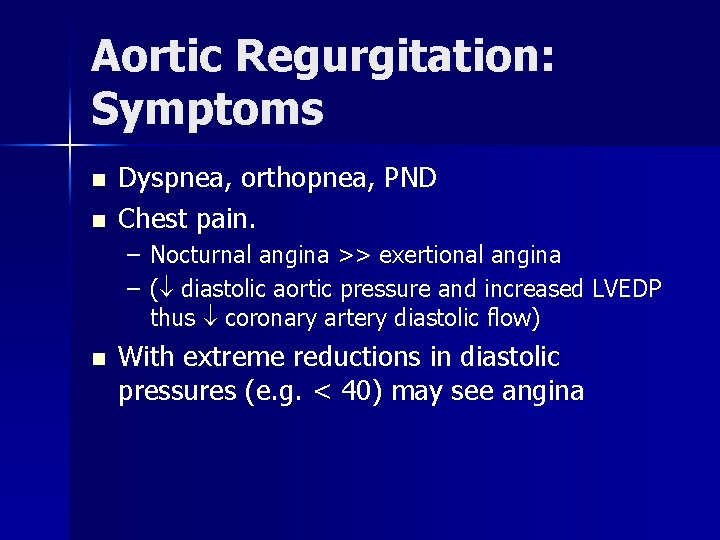
Aortic Regurgitation: Symptoms n n Dyspnea, orthopnea, PND Chest pain. – Nocturnal angina >> exertional angina – ( diastolic aortic pressure and increased LVEDP thus coronary artery diastolic flow) n With extreme reductions in diastolic pressures (e. g. < 40) may see angina
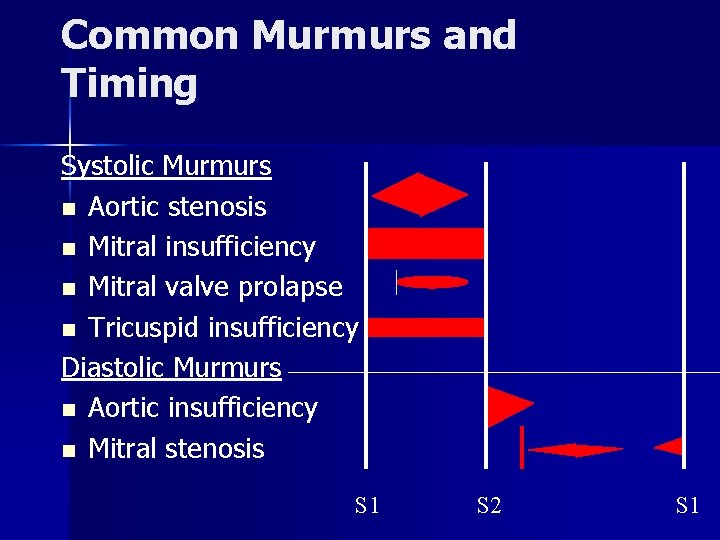
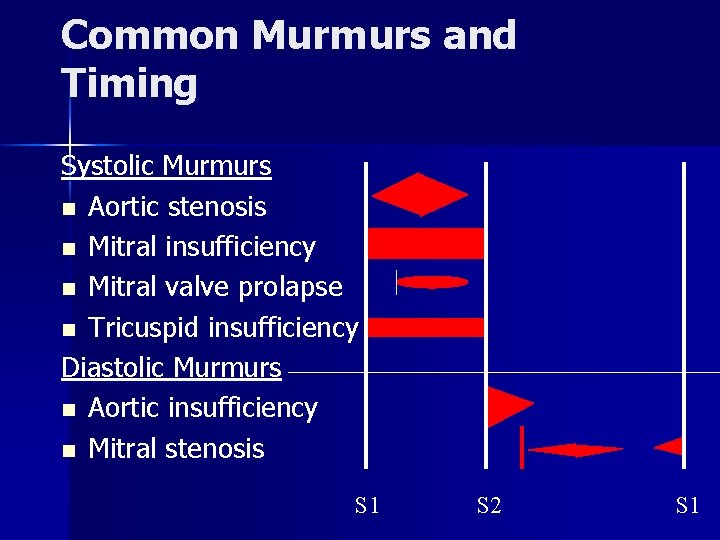
Common Murmurs and Timing Systolic Murmurs n Aortic stenosis n Mitral insufficiency n Mitral valve prolapse n Tricuspid insufficiency Diastolic Murmurs n Aortic insufficiency n Mitral stenosis S 1 S 2 S 1

Assessing Severity of Chronic Mitral Regurgitation Measure the Impact on the LV: n Apical displacement and size n Palpable S 3 n Longer/louder MR murmer (chronic MR) n S 3 intensity/ length of diastolic flow rumble n Wider split S 2 (earlier A 2) unless HPT narrows the split
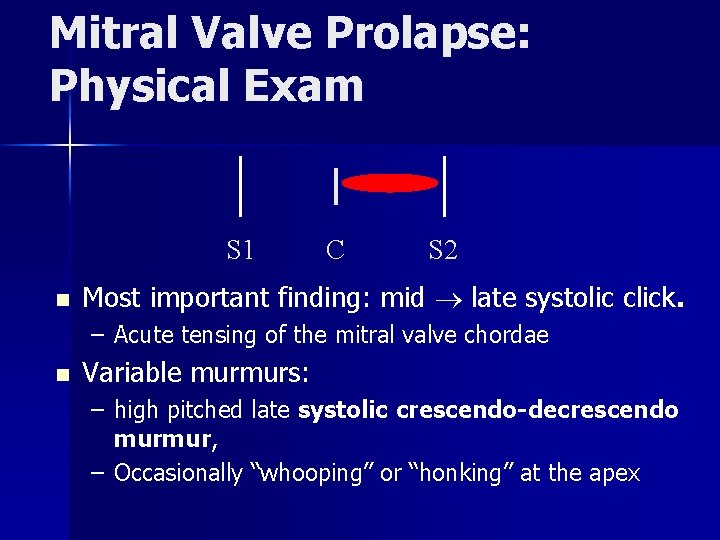
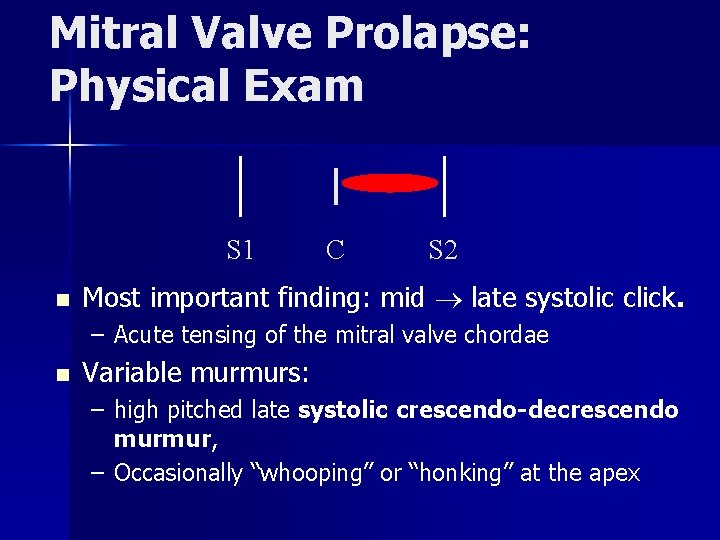
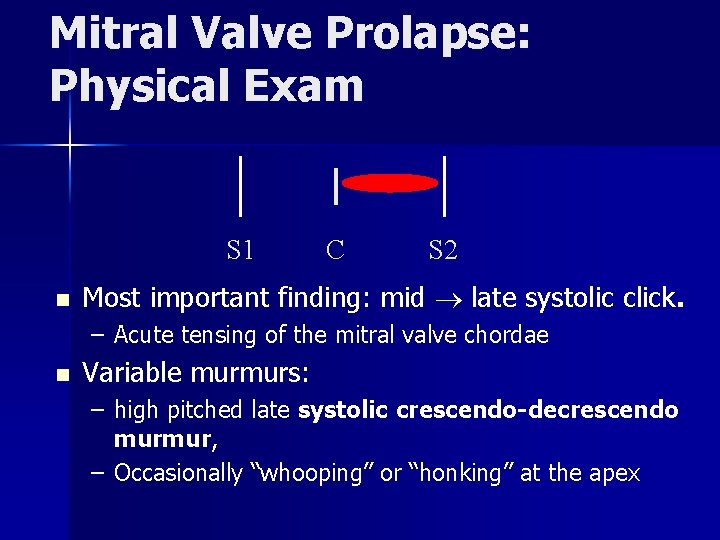
Mitral Valve Prolapse: Physical Exam S 1 n C S 2 Most important finding: mid late systolic click. – Acute tensing of the mitral valve chordae n Variable murmurs: – high pitched late systolic crescendo-decrescendo murmur, – Occasionally “whooping” or “honking” at the apex
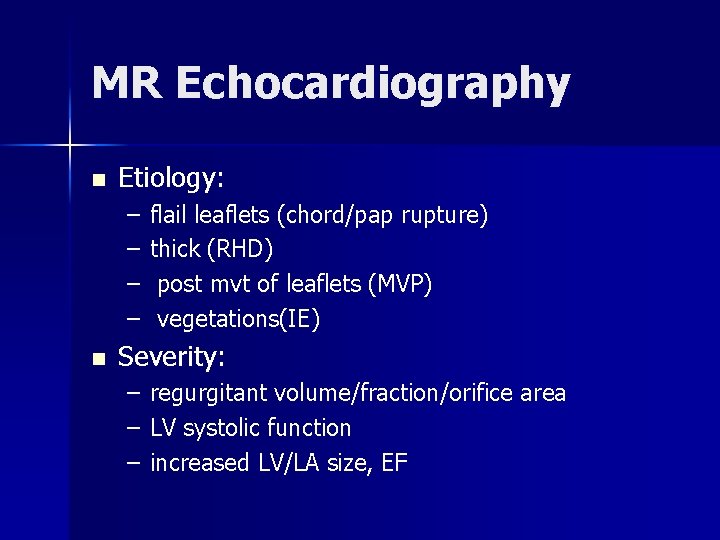
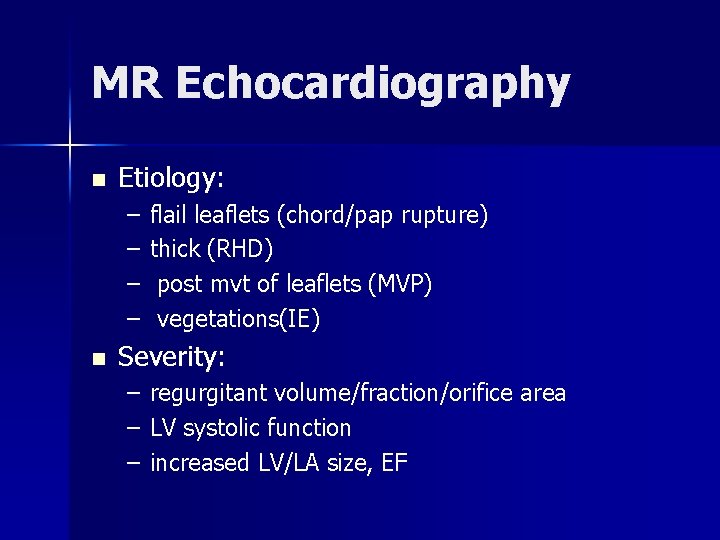
MR Echocardiography n Etiology: – – n flail leaflets (chord/pap rupture) thick (RHD) post mvt of leaflets (MVP) vegetations(IE) Severity: – – – regurgitant volume/fraction/orifice area LV systolic function increased LV/LA size, EF
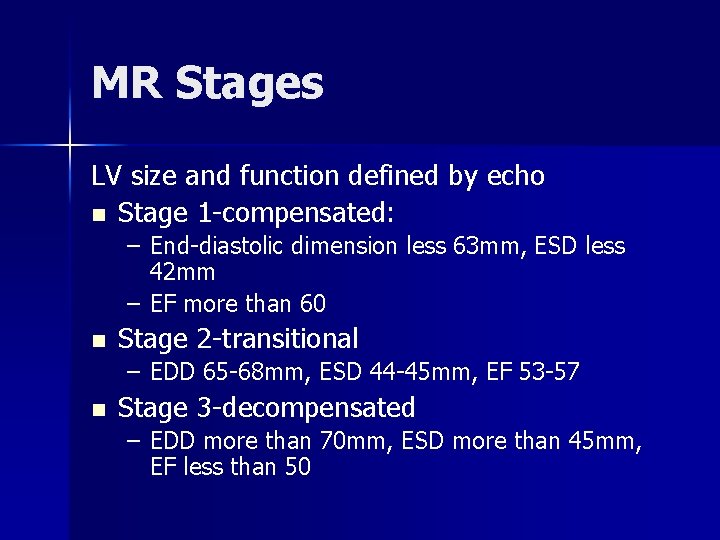
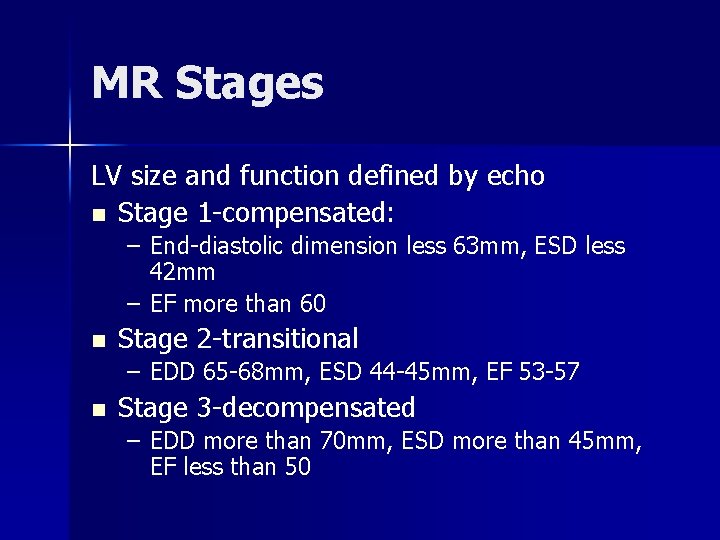
MR Stages LV size and function defined by echo n Stage 1 -compensated: – End-diastolic dimension less 63 mm, ESD less 42 mm – EF more than 60 n Stage 2 -transitional – EDD 65 -68 mm, ESD 44 -45 mm, EF 53 -57 n Stage 3 -decompensated – EDD more than 70 mm, ESD more than 45 mm, EF less than 50
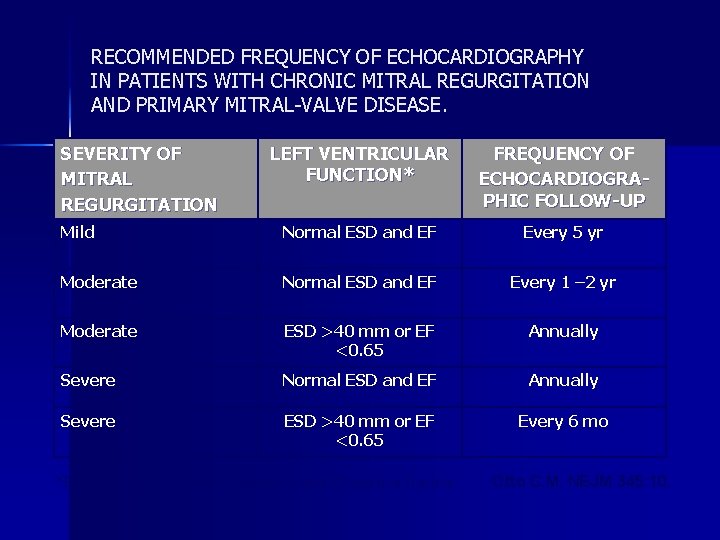
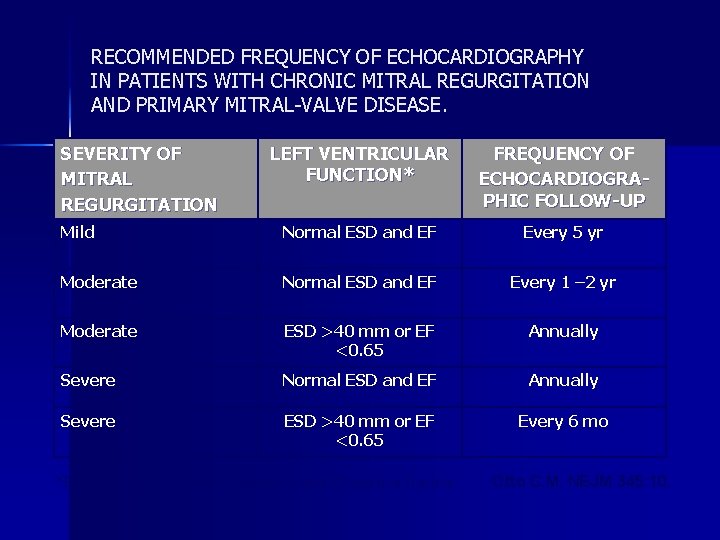
RECOMMENDED FREQUENCY OF ECHOCARDIOGRAPHY IN PATIENTS WITH CHRONIC MITRAL REGURGITATION AND PRIMARY MITRAL-VALVE DISEASE. SEVERITY OF MITRAL REGURGITATION LEFT VENTRICULAR FUNCTION* FREQUENCY OF ECHOCARDIOGRAPHIC FOLLOW-UP Mild Normal ESD and EF Every 5 yr Moderate Normal ESD and EF Every 1 – 2 yr Moderate ESD >40 mm or EF <0. 65 Annually Severe Normal ESD and EF Annually Severe ESD >40 mm or EF <0. 65 Every 6 mo *ESD denotes end-systolic dimension and EF ejection fraction. Otto C. M. NEJM 345: 10.
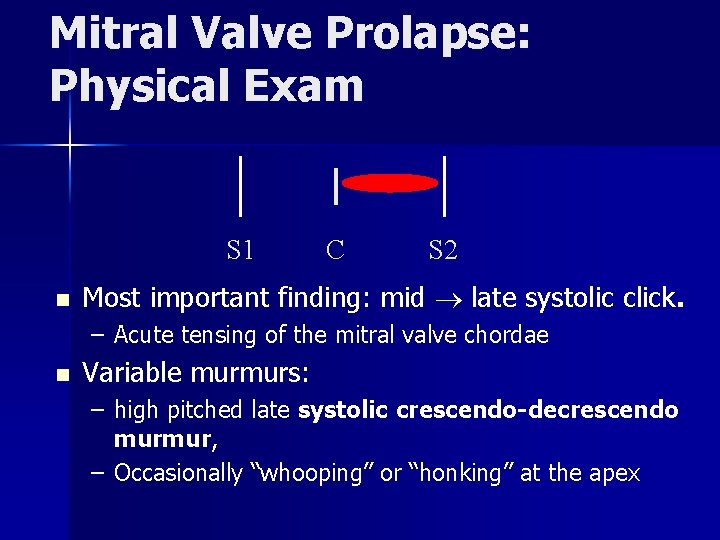
Mitral Valve Prolapse: Physical Exam S 1 n C S 2 Most important finding: mid late systolic click. – Acute tensing of the mitral valve chordae n Variable murmurs: – high pitched late systolic crescendo-decrescendo murmur, – Occasionally “whooping” or “honking” at the apex
 Site:slidetodoc.com
Site:slidetodoc.com Lvvo heart
Lvvo heart Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Upper lobe blood diversion
Upper lobe blood diversion Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Dopamine uses
Dopamine uses Causes of valvular heart disease
Causes of valvular heart disease Mitral regurgitation symptoms
Mitral regurgitation symptoms Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Tulika jain md
Tulika jain md Dr tulika jain
Dr tulika jain Tulika mitra
Tulika mitra Traslape valvular
Traslape valvular Bharathi viswanathan
Bharathi viswanathan Classification of antianginal drugs
Classification of antianginal drugs Fish mouth buttonhole stenosis
Fish mouth buttonhole stenosis Feline
Feline Aortic heart disease
Aortic heart disease Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Footbal player wordle
Footbal player wordle Heart disease
Heart disease Rheumatic heart disease
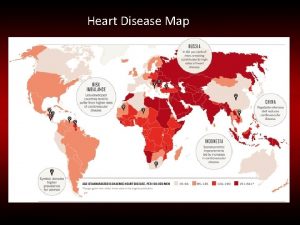
Rheumatic heart disease Heart disease data
Heart disease data Nyha class 분류
Nyha class 분류 Beau's lines autoimmune disease
Beau's lines autoimmune disease Tetralogy of fallot murmur
Tetralogy of fallot murmur Coronary heart disease
Coronary heart disease Rheumatic heart disease causes
Rheumatic heart disease causes Ie
Ie Pico question examples heart disease
Pico question examples heart disease Modern treatment of heart disease
Modern treatment of heart disease Heart disease and stroke are the world's biggest killers
Heart disease and stroke are the world's biggest killers Congenital heart disease pda
Congenital heart disease pda Knee chest position
Knee chest position Superadded changes in coronary atherosclerosis
Superadded changes in coronary atherosclerosis Terrible t's cyanotic heart disease
Terrible t's cyanotic heart disease Cyanotic vs acyanotic
Cyanotic vs acyanotic Chronic rheumatic heart disease
Chronic rheumatic heart disease Transamerica estate planning foreign nationals
Transamerica estate planning foreign nationals Yelena bogdan md
Yelena bogdan md Employment of non-resident aliens in the philippines
Employment of non-resident aliens in the philippines Taxable income formula
Taxable income formula Resident subnet
Resident subnet When ambulating a resident should be wearing
When ambulating a resident should be wearing Resident set management
Resident set management Resident and family engagement
Resident and family engagement Acgme survey questions
Acgme survey questions Telephone 911
Telephone 911 Divine intervention episode 143
Divine intervention episode 143 Attending vs resident
Attending vs resident Resident assessment instrument definition
Resident assessment instrument definition Partially resident textures
Partially resident textures Resident retention
Resident retention Ota core curriculum
Ota core curriculum Conflict resolution customer service
Conflict resolution customer service Resident lifecycle
Resident lifecycle Examples of misappropriation of resident property
Examples of misappropriation of resident property Tarrytown chief resident conference
Tarrytown chief resident conference Resident and family engagement
Resident and family engagement Acgme resident survey
Acgme resident survey The working set strategy
The working set strategy Define resident flora
Define resident flora Describe the care team and the chain of command
Describe the care team and the chain of command If a resident with ad shows violent behavior the na should
If a resident with ad shows violent behavior the na should Difference between microteaching and traditional teaching
Difference between microteaching and traditional teaching Seamless mpls vs unified mpls
Seamless mpls vs unified mpls Ashish jain microsoft
Ashish jain microsoft Jainendra k. jain
Jainendra k. jain Cherry hill jain sangh
Cherry hill jain sangh Jain agam literature
Jain agam literature Pankaj jain iitk
Pankaj jain iitk Prateek jain
Prateek jain Lunawat
Lunawat Nus myedu
Nus myedu Importance of jainism
Importance of jainism Jain
Jain Preet jain
Preet jain Jain way of life
Jain way of life Eric jain
Eric jain Raina jain dartmouth
Raina jain dartmouth Anu jain
Anu jain Temple
Temple Melena management
Melena management 1 yojan in jainism
1 yojan in jainism Jain society of central florida
Jain society of central florida Jsne
Jsne Prateek jain msr
Prateek jain msr Jain bcn
Jain bcn Jain portal
Jain portal Vinod jain ca
Vinod jain ca Jain temple boston
Jain temple boston Jain way of life
Jain way of life Vaibhav.14v
Vaibhav.14v Eakta jain
Eakta jain Dr salil jain
Dr salil jain Reti di calcolatori corradi
Reti di calcolatori corradi Vidya jain case
Vidya jain case Jain
Jain Partial rebreather mask indications
Partial rebreather mask indications