Caring for Patients With Cardiac Disorders Learning Outcomes
- Slides: 73
Caring for Patients With Cardiac Disorders
Learning Outcomes 1. Compare and contrast the causes, pathophysiology, effects, and manifestations of common cardiac disorders. 2. Safely administer drugs commonly prescribed for patients with heart disease. 3. Provide individualized and evidence-based nursing care for patients undergoing invasive procedures or surgery of the heart. 4. Use clinical judgment and the nursing process to conduct focused assessments, contribute to care planning, and provide individualized nursing care for patients with disorders of the heart.
Learning Outcomes 5. Provide and reinforce appropriate teaching for patients with heart disorders and their families, taking patient values, expressed needs, and preferences into consideration. 6. Use electronic resources for planning and documenting nursing care for patients with heart disorders.
Disorders of Cardiac Function
Heart Failure • Inability of heart to function as pump • Results from any condition that causes: • Impaired contractions • Increased workload of the heart • Leading causes • Hypertension • CHD with myocardial ischemia and MI
Pathophysiology • Cardiac output drops • Compensatory mechanisms activated • Sympathetic nervous system stimulated • Arteries and veins constrict • Venous return increases to the heart • Increase in preload
Pathophysiology • Renin–angiotensin–aldosterone system activated • Salt and water retention • Heart chambers dilate • Ventricular hypertrophy • Reduced cardiac reserve • Classified as left-sided or right-sided
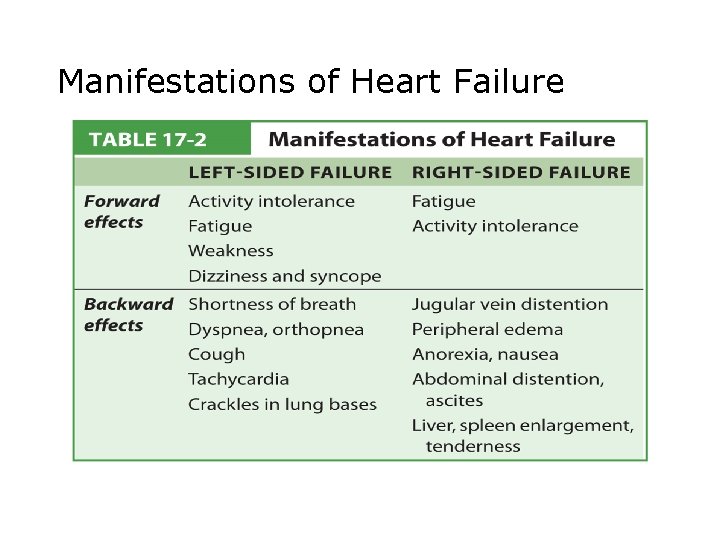
Pathophysiology • Left-sided heart failure • Manifestations • • • Pulmonary congestion Reduced cardiac output Fatigue, activity intolerance Dyspnea on exertion (DOE) Orthopnea • Acute pulmonary edema
Pathophysiology • Right-sided heart failure • Manifestations • • • Fatigue Activity intolerance Jugular vein distention (JVD) Peripheral edema Anorexia, nausea Abdominal distention
Pathophysiology • Right-sided heart failure • Manifestations • Ascites • Liver/spleen enlarged and tender • Biventricular failure • Paroxysmal nocturnal dyspnea (PND) • Acute and chronic failure • Multisystemic effects
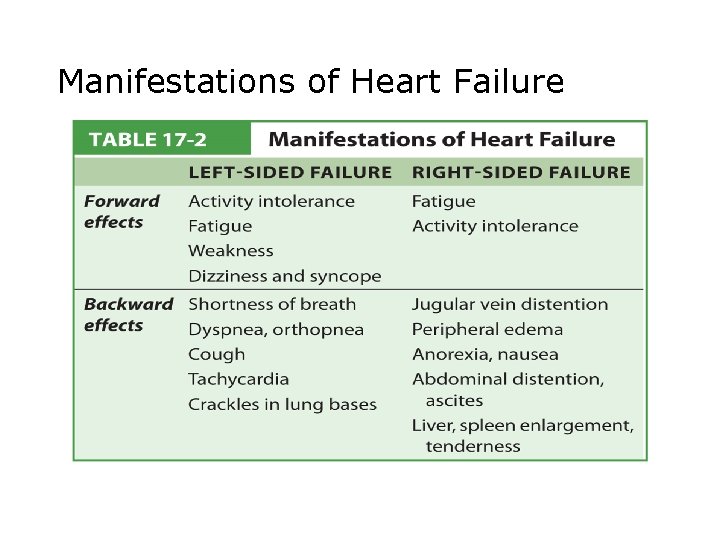
Manifestations of Heart Failure
Collaborative Care • Diagnostic tests • Cardiac hormones, atrial natriuretic factor, and brain natriuretic peptide • Serum electrolytes • Chest x-ray • Echocardiogram • ECG
Collaborative Care • Hemodynamic monitoring • Assess cardiovascular function • Multilumen catheter inserted through central vein in right side of the heart • Pulmonary artery used to measure central venous pressure, pulmonary artery pressures, and cardiac output • Arterial blood pressure measured using a peripheral arterial line
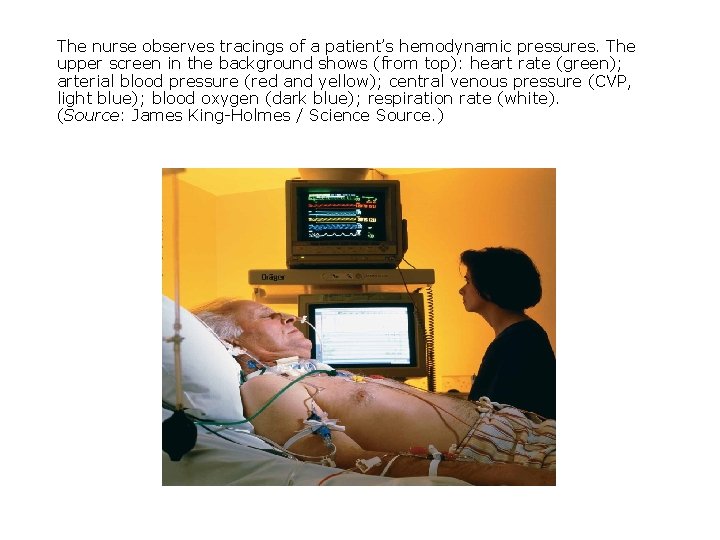
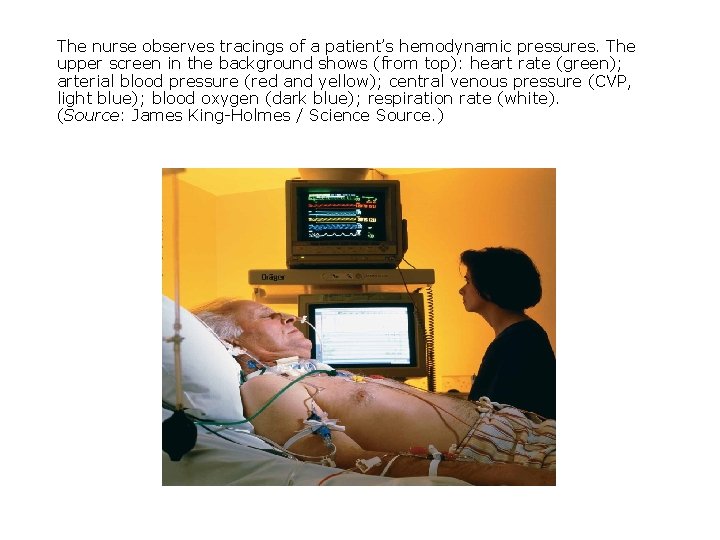
The nurse observes tracings of a patient’s hemodynamic pressures. The upper screen in the background shows (from top): heart rate (green); arterial blood pressure (red and yellow); central venous pressure (CVP, light blue); blood oxygen (dark blue); respiration rate (white). (Source: James King-Holmes / Science Source. )
Collaborative Care • Medications • • • ACE inhibitors ARBs (angiotensin II receptor blockers) Diuretics Inotropic medications Vasodilators
Collaborative Care • Medications • Morphine sulfate • Pulmonary edema treatment • Digitalis • Positive inotropic effect on heart • Narrow therapeutic index • Easy digitalis toxicity
Collaborative Care • Diet and activity • Low-sodium diet • Bed rest during acute phase • Activity gradually increased • Implanted devices • Implantable cardiac defibrillator (ICD) • Biventricular pacemaker
Collaborative Care • Surgery • Heart transplant • Infection and rejection main concerns • Immunosuppressive drugs • Dynamic cardiomyoplasty • Skeletal muscle graft around heart to support myocardium • No real success
Nursing Care • Prioritizing nursing care • Oxygen demand • Reduce workload of heart • Health promotion • Measures to prevent CHD • Assessing • Frequent, careful assessment
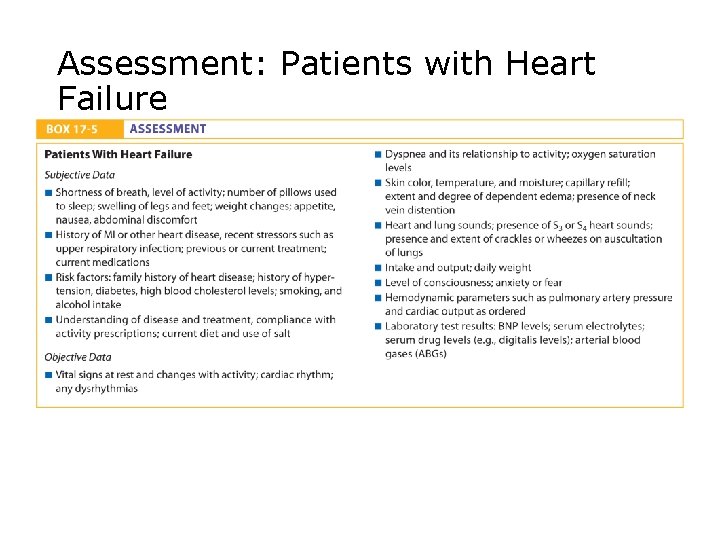
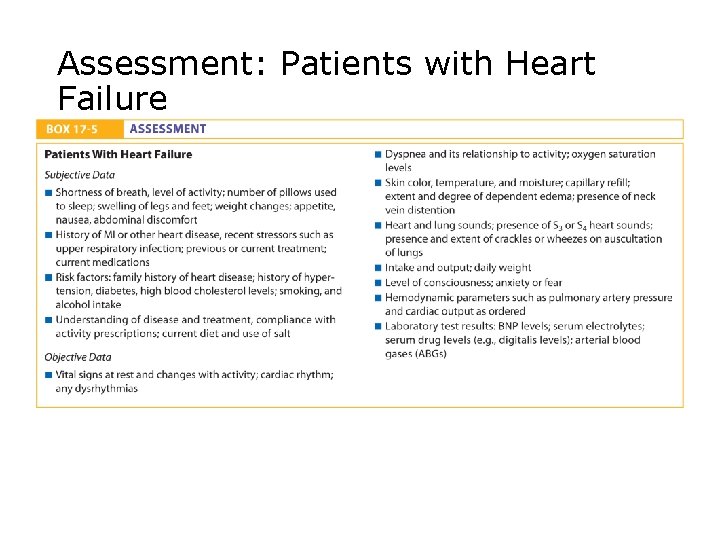
Assessment: Patients with Heart Failure
Nursing Care • Identifying potential complications • Acute pulmonary edema • Liver, kidney failure • Mental status changes • Diagnosing, planning, and implementing • Decreased cardiac output • Heart and breath sounds • Mental status
Nursing Care • Diagnosing, planning, and implementing • Decreased cardiac output • • • Urinary output (UOP) Oxygen Medications Rest Quiet
Nursing Care • Diagnosing, planning, and implementing • Excess fluid volume • • • Panic I&O Daily weights Fowler's position Diuretics/medications Fluid restriction
Nursing Care • Diagnosing, planning, and implementing • Activity intolerance • • • VS Rest periods Assist with care Progressive activity plan Small, frequent meals
Nursing Care • Documenting • Note any changes • Note patient's response to treatment • Continuity of care • Chronic, progressive nature • Lifestyle changes • Exercise parameters • Referrals to home health agencies
Inflammatory Cardiac Disorders
Rheumatic Fever and Rheumatic Heart Disease • Pathophysiology • Streptococcal bacteria • Carditis • Valves swollen and red • Scarring of valves • In RHD, scarring leads to valve stenosis and regurgitation.
Rheumatic Fever and Rheumatic Heart Disease • Manifestations • • Fever Migratory joint pain and inflammation Rash on trunk or extremities Chest pain/discomfort Tachycardia SOB Heart sound changes Muscle spasms
Rheumatic Fever and Rheumatic Heart Disease • Collaborative care • Laboratory testing • WBC, ESR elevated • C-reactive protein • Rapid antigen test for group A Streptococcus • Antistreptolysin-O titer • Cardiac enzymes • Echocardiogram
Rheumatic Fever and Rheumatic Heart Disease • Collaborative care • Treat primary infection, manifestations • Prevent complications and recurrences • Antibiotics • Medications • • Antibiotics Aspirin Ibuprofen Steroids
Nursing Care • Prioritizing nursing care • Supportive care • Health promotion • Prompt treatment of streptococcal throat infections • Assessing • Recent sore throat or "strep throat" • Chest pain • SOB
Nursing Care • Assessing • • • Fatigue Weakness Fever Joint pain Rash • Identifying potential complications • Decreasing activity tolerance or change in heart sounds
Nursing Care • Diagnosing, planning, and implementing • Acute pain • Report increased chest pain • Administer medications as prescribed • Warm, moist compresses prn
Nursing Care • Diagnosing, planning, and implementing • Activity intolerance • Reduce stress on the heart • Diversional activities • Monitor activity intolerance
Nursing Care • Evaluating • Degree of pain • VS • Response to activity • Documenting • Any symptoms, changes • Continuity of care • Importance of antibiotics
Infective Endocarditis • Inflammation of endocardium • Usually affects patients with underlying heart disease • Acute • Staphylococcus aureus • Subacute • Streptococcus viridans
Pathophysiology • Bacteria enter body and settle in mitral valve. • Normal valve closure prevented • Regurgitation of blood • Heart murmurs • Onset can be sudden or gradual.
Manifestations and Complications • Elevated temperature • Flu-like • Cough • SOB • Joint pain • Petechiae • Splinter hemorrhages • Heart failure or stroke
Collaborative Care • No definitive tests • Prevention • Teach risks of IV drug use • Preventative antibiotics if indicated • Medications • Antibiotics • Surgery • Replace damaged valves
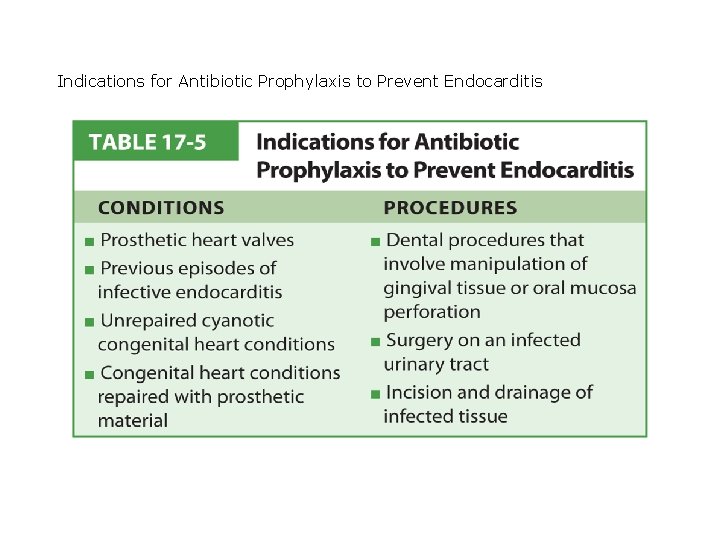
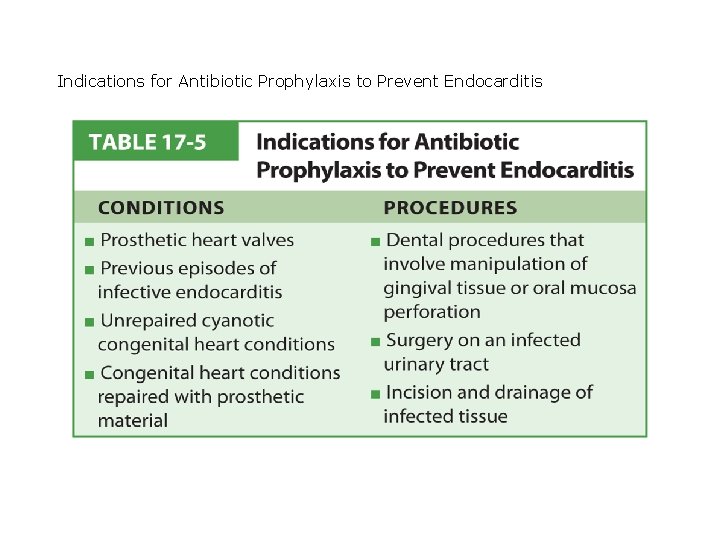
Indications for Antibiotic Prophylaxis to Prevent Endocarditis
Nursing Care • Prioritizing nursing care • Treat infection process. • Maintain heart function. • Health promotion • Teach prevention. • Advise patients at high risk to avoid body piercing.
Nursing Care • Assessing • • • Risk factors Recent surgery or dental work IV drug use Current S/S VS Heart and breath sounds
Nursing Care • Diagnosing, planning, and implementing • Hyperthermia • Risk for ineffective tissue perfusion • Review of system • Managing nursing care • Vital signs, I&O, and hygiene
Nursing Care • Evaluating • Reduction in symptoms • Documenting • Subjective, objective assessments • Continuity of care • Education and support through course • Importance of reporting unusual manifestations
Myocarditis • Inflammatory disorder of heart • Causes include: • • • Infection Immunity Radiation Poisons Drugs Burns
Myocarditis • Manifestations • Asymptomatic or fever, fatigue, malaise, dyspnea • Heart failure manifestations • Nursing care • Decrease myocardial work • Explain all procedures, tests to decrease anxiety
Pericarditis • Pathophysiology • Damaged pericardial tissue • Fluid and exudates in pericardial space • Manifestations • Chest pain, sharp • Pericardial friction rub • Fever
Pericarditis • Complications • Pericardial effusion • Abnormal collection of fluid between pericardial layers • Cardiac tamponade • Fatal if untreated • Paradoxical pulse
Pericarditis • Collaborative care • • Self-limiting and will resolve Ecocardiography, CT, MRI Acetominophen, NSAIDs Pericardiocentesis • Large (16 - to 18 -gauge) needle inserted into pericardial sac to remove fluid • May be done as an emergency procedure for cardiac tamponade
Nursing Care • Prioritizing nursing care • Acute pain • Pain scale • NSAIDs • Calm/quiet environment • Ineffective breathing pattern • Respiratory rate • Incentive spirometer • Oxygen
Nursing Care • Risk for decreased cardiac output • VS • Heart sounds • Prepare for pericardiocentesis as necessary
Nursing Care • Continuity of care • • Stay on medications Medication teaching Fluid intake Activity restrictions
Disorders of Cardiac Structure
Valvular Heart Disease • Rheumatic heart disease most common cause • Endocarditis • After MI • Congenital heart defects • Changes in structures with normal aging
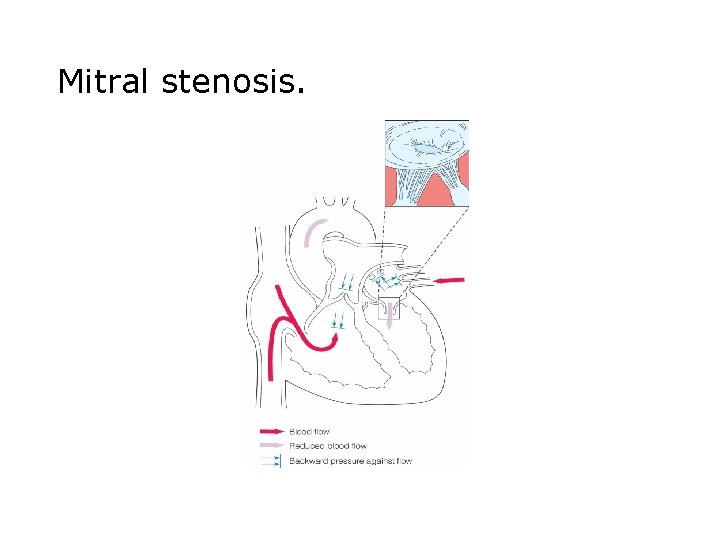
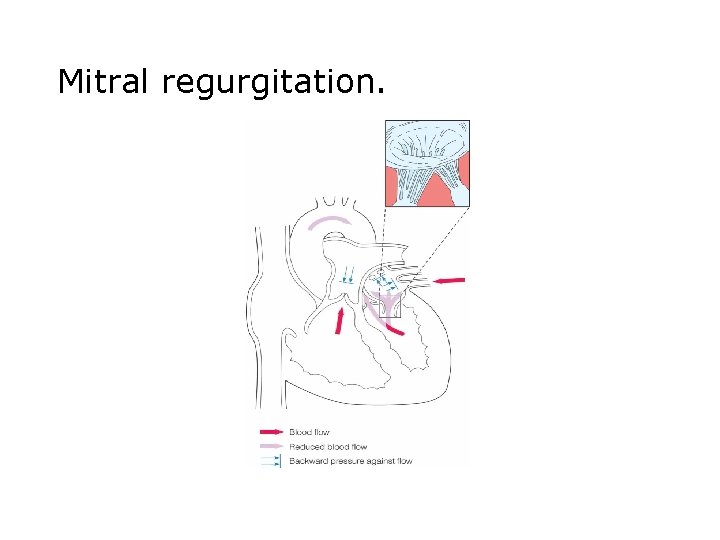
Pathophysiology and Manifestations • Mitral stenosis • Valve leaflets fuse. • Dyspnea on exertion (DOE) • Palpable thrill • Mitral regurgitation • Valves do not close. • "Cooing" or "seagull-like"
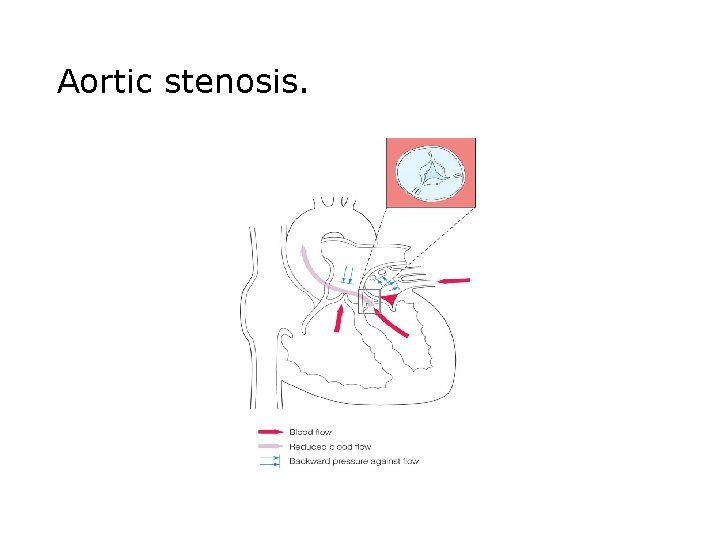
Pathophysiology and Manifestations • Mitral valve prolapse • Unknown cause but may relate to inherited collagen defect • Young women aged 14– 30 • Aortic stenosis • Idiopathic, congenital, or RHD • Left ventricle hypertrophies. • At risk for sudden cardiac death
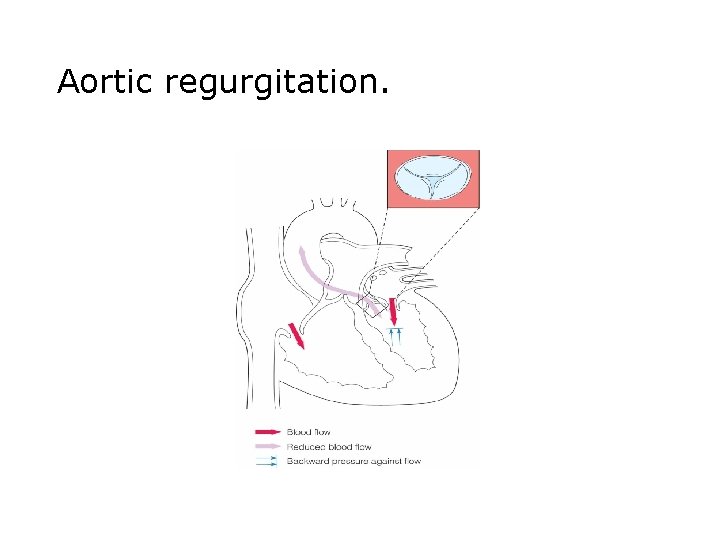
Pathophysiology and Manifestations • Aortic regurgitation • Aortic valve fails to close completely. • Mild-to-moderate • Palpitations when lying flat • Angina
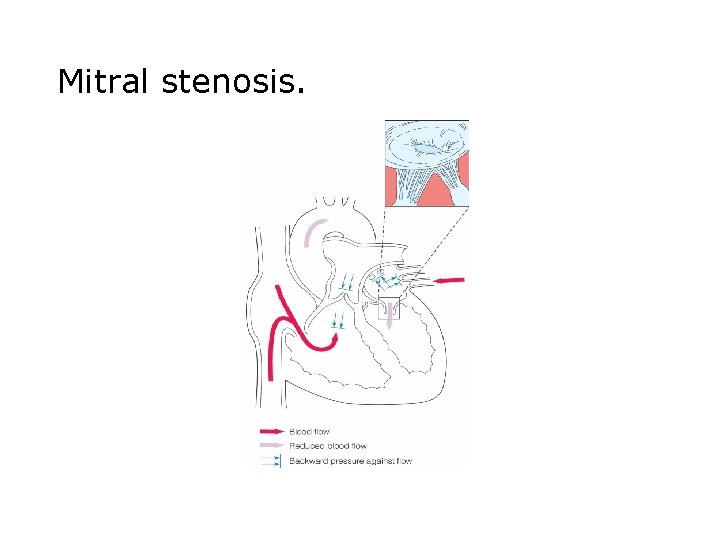
Mitral stenosis.
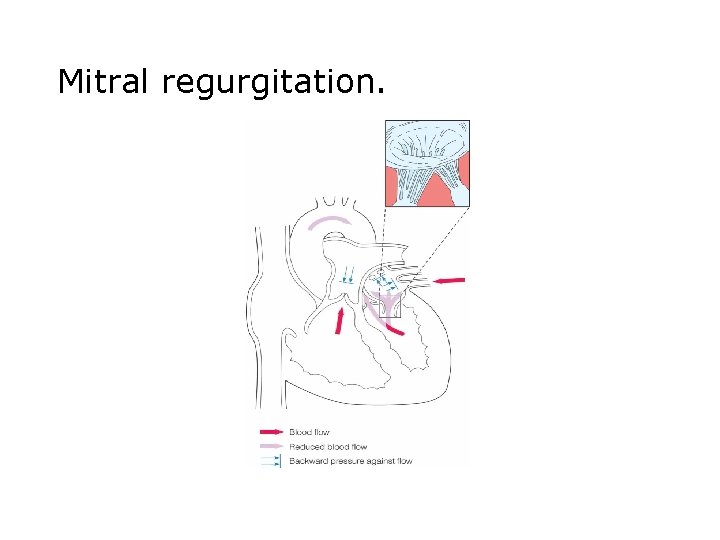
Mitral regurgitation.
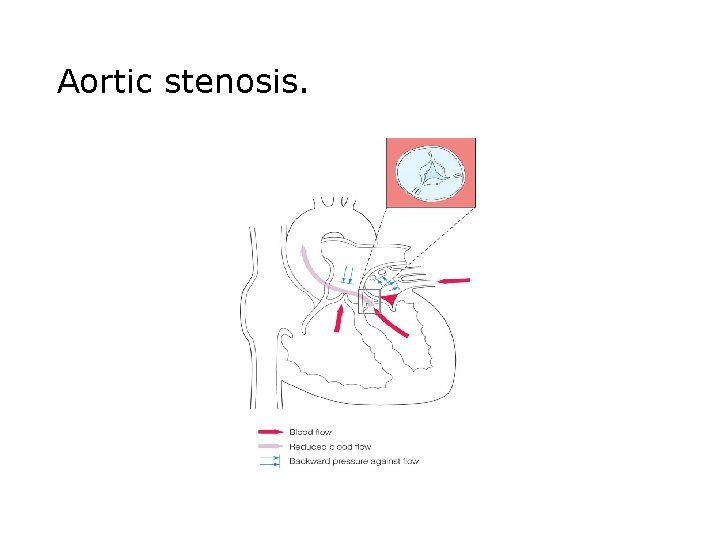
Aortic stenosis.
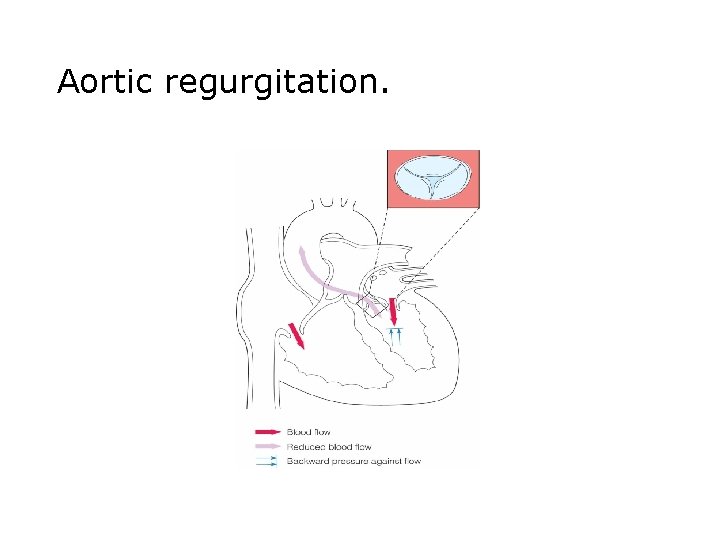
Aortic regurgitation.
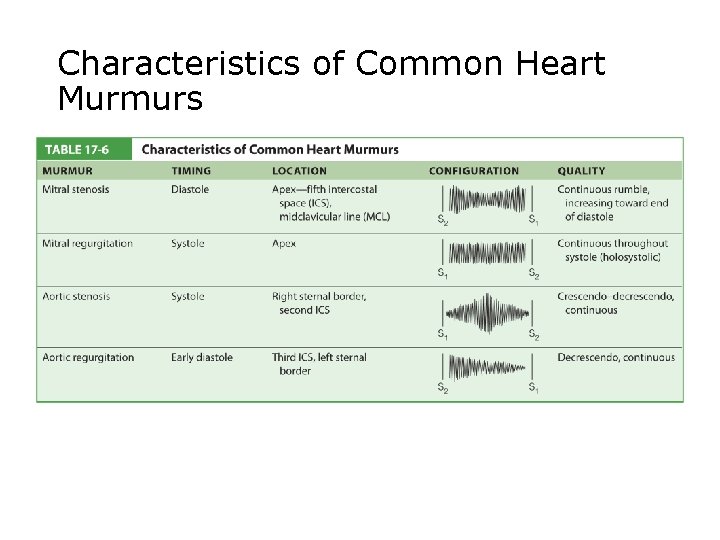
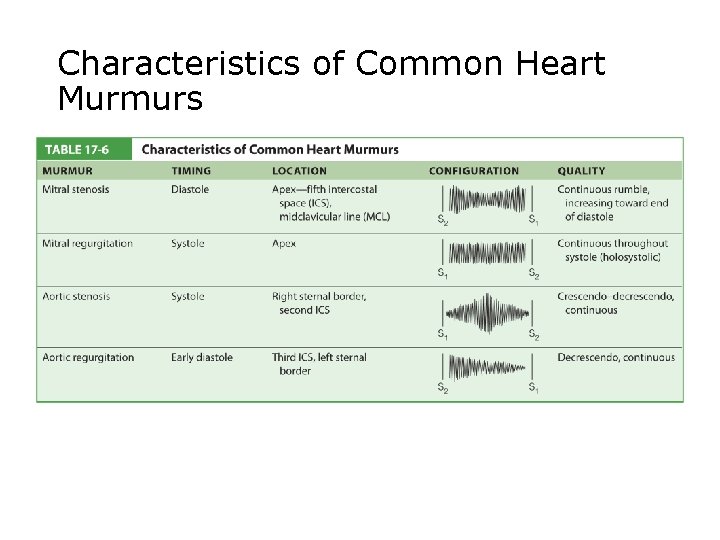
Characteristics of Common Heart Murmurs
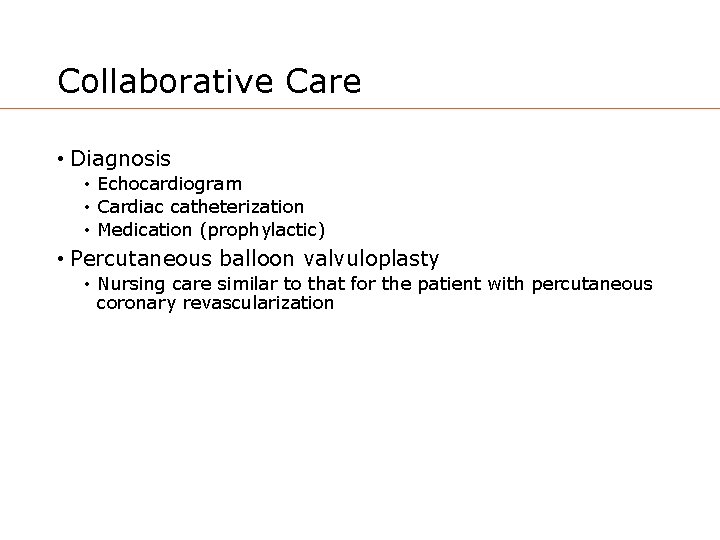
Collaborative Care • Diagnosis • Echocardiogram • Cardiac catheterization • Medication (prophylactic) • Percutaneous balloon valvuloplasty • Nursing care similar to that for the patient with percutaneous coronary revascularization
Collaborative Care • Surgery • Valvuloplasty • Resection • Valve replacement
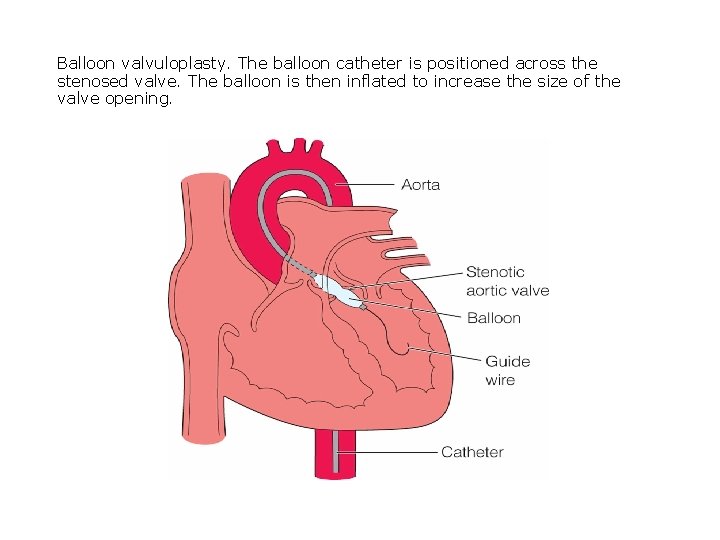
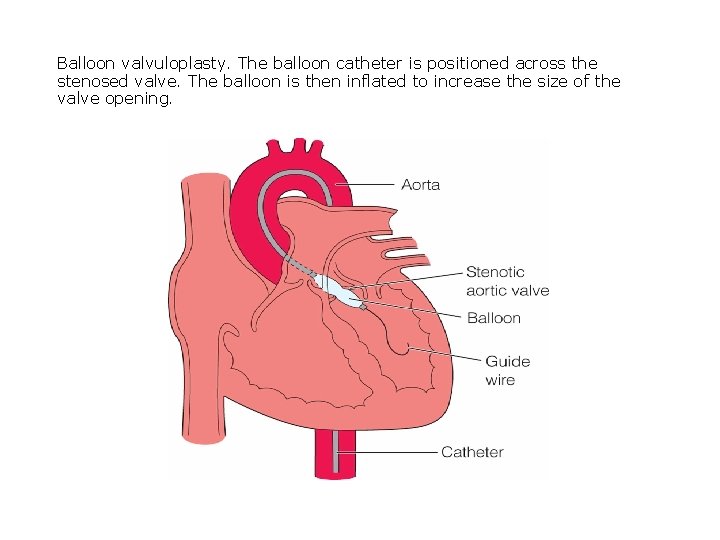
Balloon valvuloplasty. The balloon catheter is positioned across the stenosed valve. The balloon is then inflated to increase the size of the valve opening.
Nursing Care • Prioritizing nursing care • Decreased cardiac output • • • VS Hemodynamic measures Cardiac output every 8 hours I&O Daily weights Fluid restriction
Nursing Care • Prioritizing nursing care • Decreased cardiac output • Elevate HOB • Oxygen • Medications • Activity intolerance • VS • Gradually increase activity • Assist as needed
Nursing Care • Managing nursing care • As appropriate • Continuity of care • • • Prevent rheumatic fever Explain all tests and procedures Diet Medications Rest Evaluate for edema
Cardiomyopathy • Group of disorders that affect filling and output • Often lead to heart failure • Cause often unknown • Categorized by effects on heart • Dilated • Hypertrophic • Restrictive
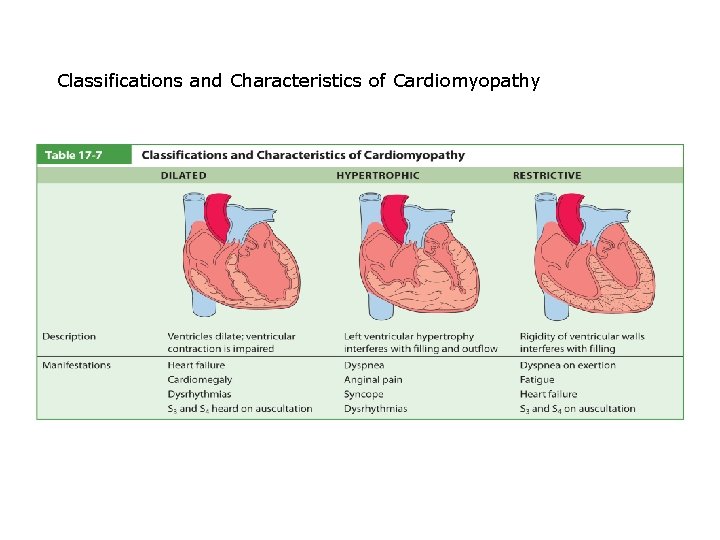
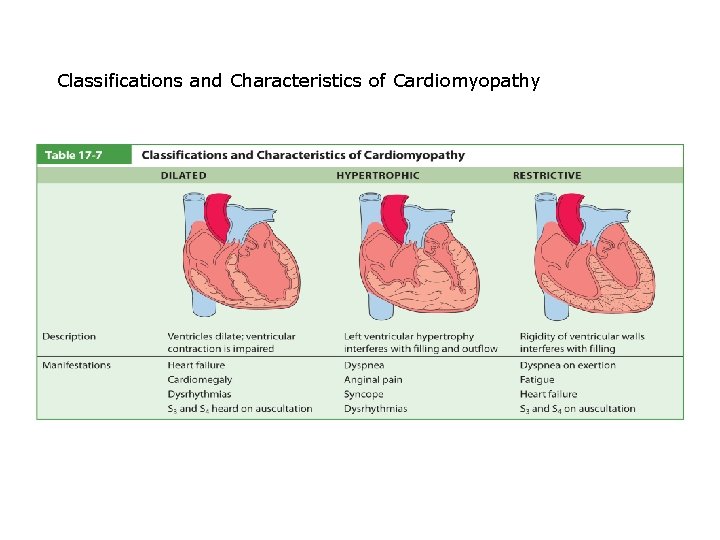
Classifications and Characteristics of Cardiomyopathy
Cardiomyopathy • Medical management • Positive inotropic agents • Digoxin • Sympathomimetic agents • Dopamine • Notify health care provider of abdominal pain, rash, or burning.
Cardiomyopathy • Medical management • ACE inhibitors • Vasotec, Prinivil • Change position slowly. • Report bruising or weight gain. • Diuretics • Abdominal pain, jaundice • Electrolyte imbalances • Blood pressure changes
Cardiomyopathy • Treatment • • Minimize heart failure Treat dysrhythmias Prevent sudden cardiac death Surgery • Cardiac transplant for dilated form • Resection for hypertrophic form • Focus on self-care measures and education.