Epidemiology of Periodontal Diseases Epidemiology derived from Greek





- Slides: 62
Epidemiology of Periodontal Diseases
Epidemiology, derived from Greek word epi, meaning "upon, among", demos, meaning "people, logos, meaning "study, n
What is Epidemiology? n n The study of the distribution and determinants of health-related states in populations, and the application of this study to control health problems Basic Science of Public Health
n n Public Health deals with health of Community group or population Clinical practice deals with health of an individual.
Epidemiology Definition implies 1. 2. 3. Determining amount & distribution of disease Investigation of causes of disease Applying this knowledge for control of disease
n n The final purpose of Epidemiology is to apply the knowledge gained through studies to Promote Health Protect Health Restore Health
Distribution of diseases n n n Distribution of diseases/periodontal diseases in populations is not random Some members or subgroups of the population are more susceptible Physical, biologic, behavioral, cultural and social factors
Epidemiology in periodontics should provide information about: 1. Prevalence & severity 2. Risk factors 3. Effectiveness of preventive & therapeutic measures
Classification of Periodontal Diseases n n Numerous Classifications existed in the past World workshop in periodontics 1989 AAP classification 1999
Periodontal Diagnosis n n n Great importance Distinguishing between “Normal” & “Abnormal” is based on thresholds Thresholds are derived from epidemiological studies
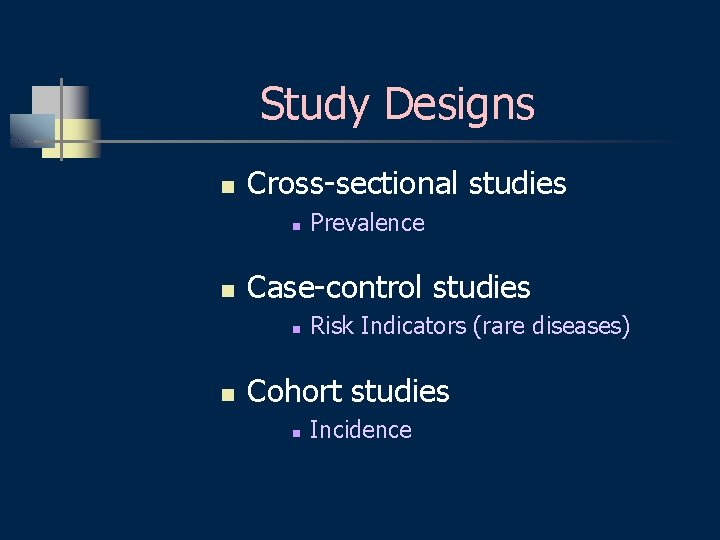
Study Designs n Cross-sectional studies n n Case-control studies n n Prevalence Risk Indicators (rare diseases) Cohort studies n Incidence
Definitions n n n Prevalence Incidence Sensitivity Specificity Positive predictive value Negative predictive value
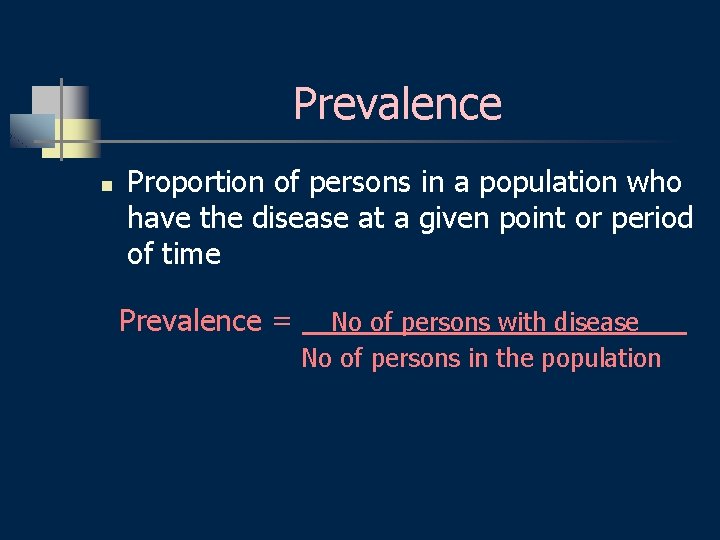
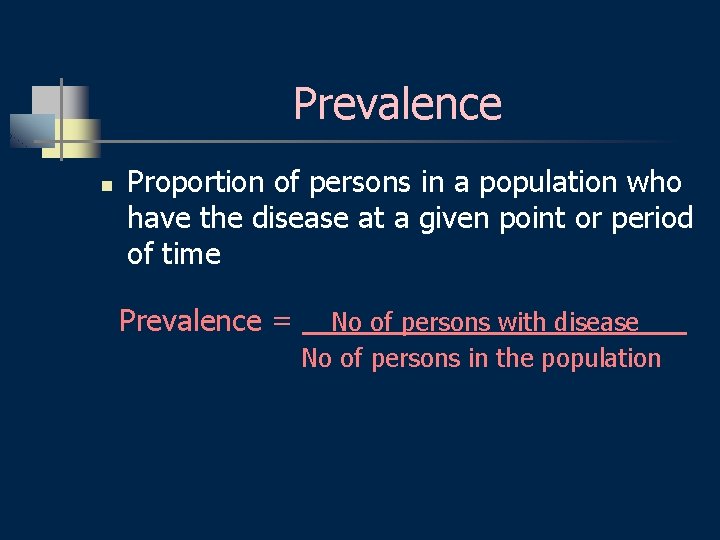
Prevalence n Proportion of persons in a population who have the disease at a given point or period of time Prevalence = No of persons with disease No of persons in the population
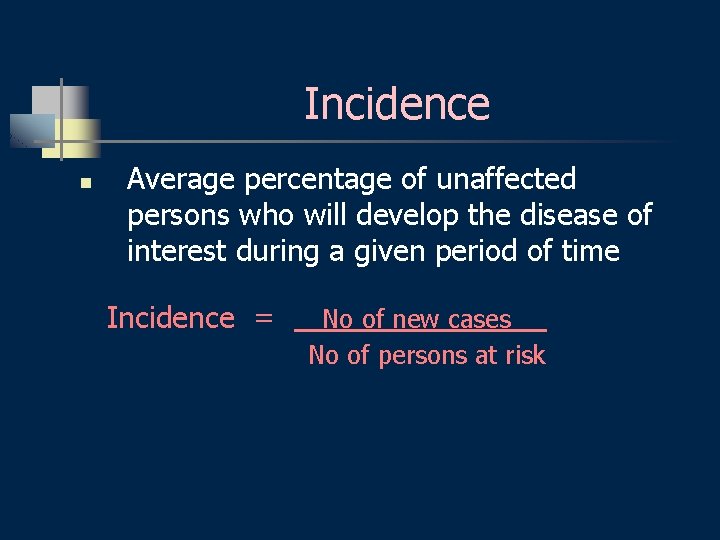
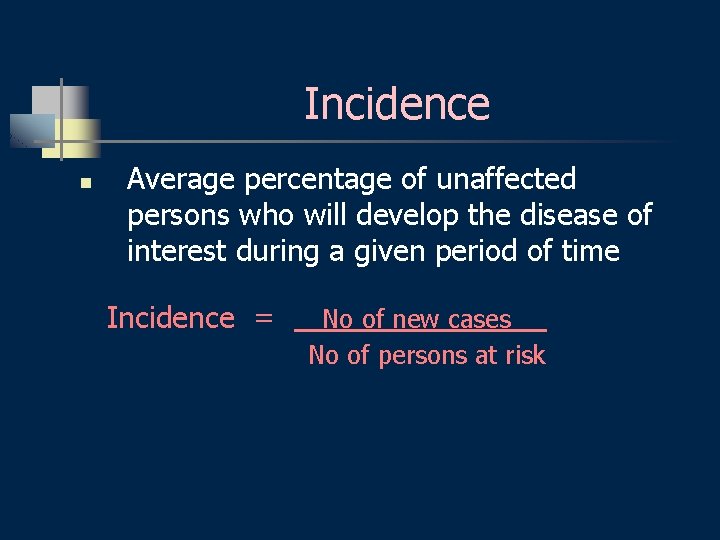
Incidence n Average percentage of unaffected persons who will develop the disease of interest during a given period of time Incidence = No of new cases No of persons at risk
n Incidence of periodontal diseases in a strict sense is almost impossible at the present level of knowledge.
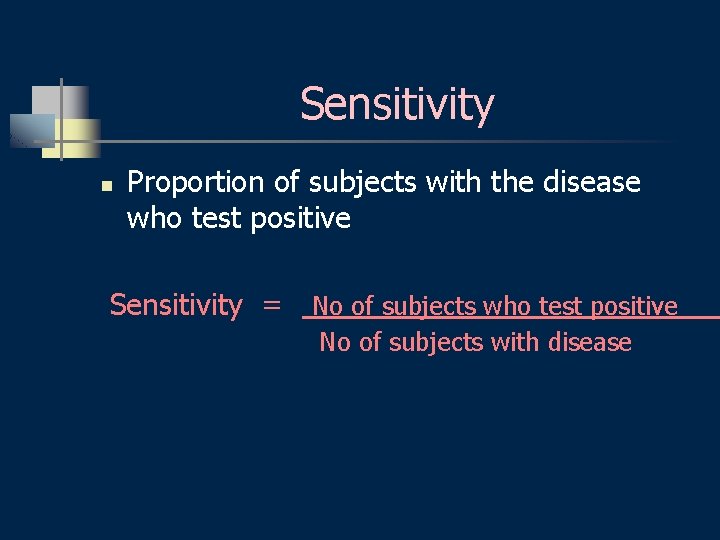
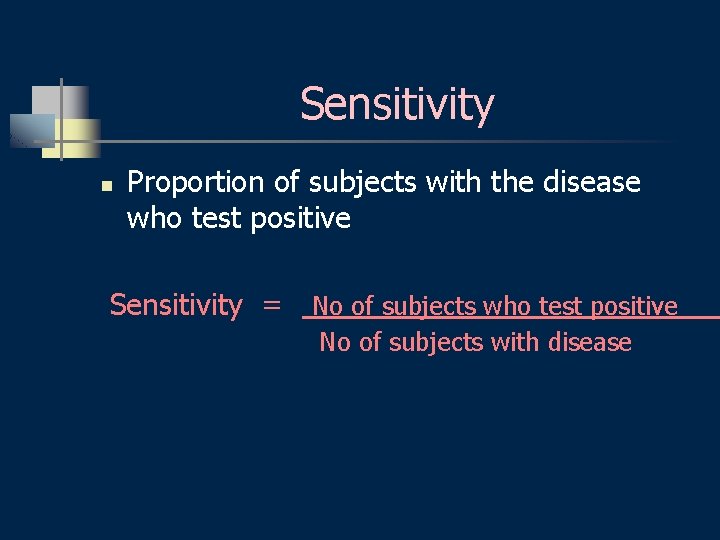
Sensitivity n Proportion of subjects with the disease who test positive Sensitivity = No of subjects who test positive No of subjects with disease
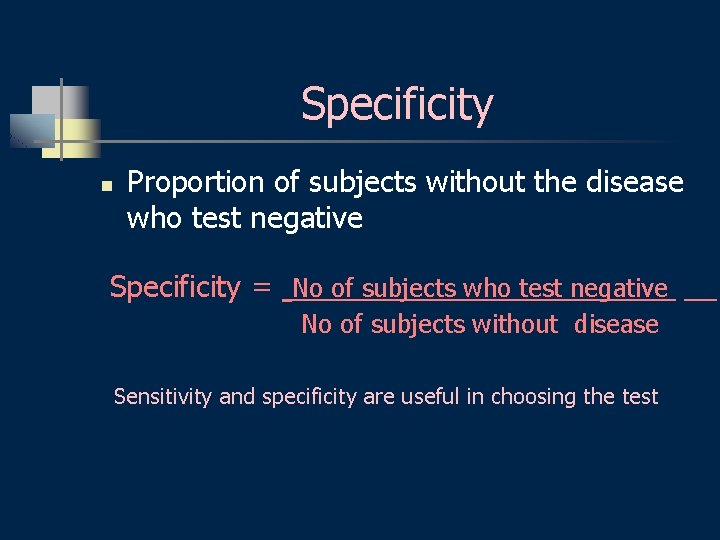
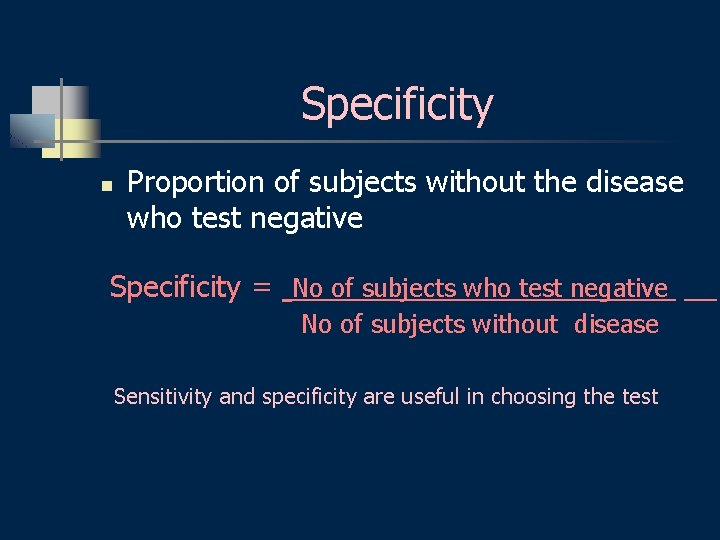
Specificity n Proportion of subjects without the disease who test negative Specificity = No of subjects who test negative No of subjects without disease Sensitivity and specificity are useful in choosing the test
Predictive Value n Once the result of a test is ready: what are the chances that it is right or wrong? Predictive value
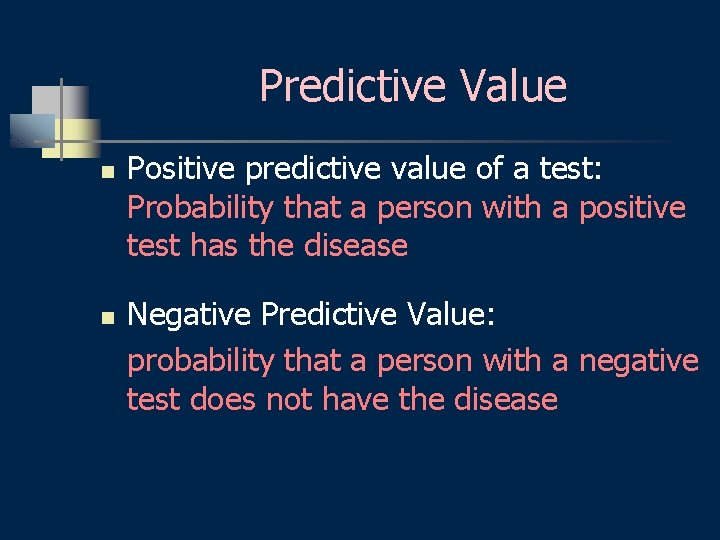
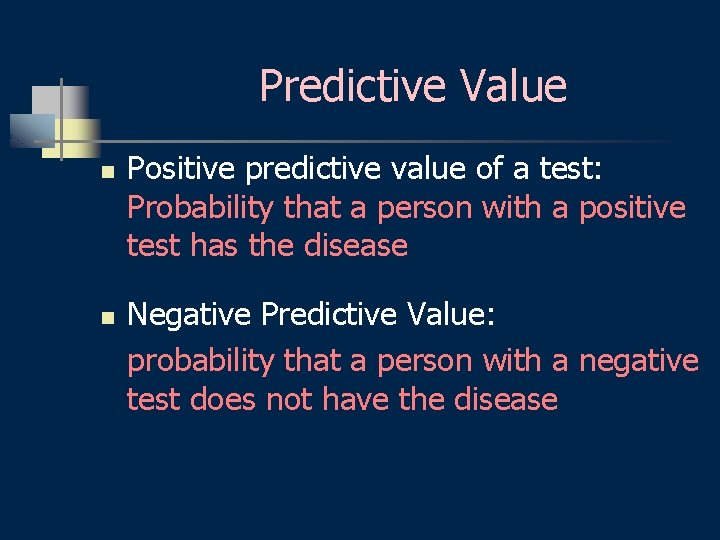
Predictive Value n n Positive predictive value of a test: Probability that a person with a positive test has the disease Negative Predictive Value: probability that a person with a negative test does not have the disease
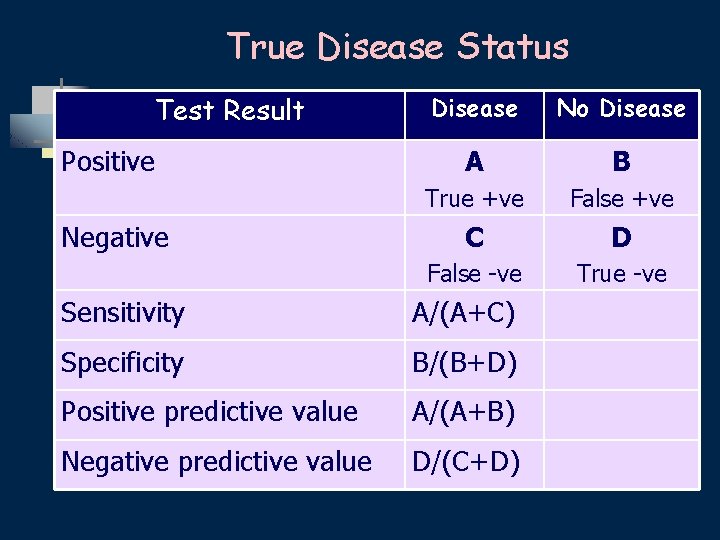
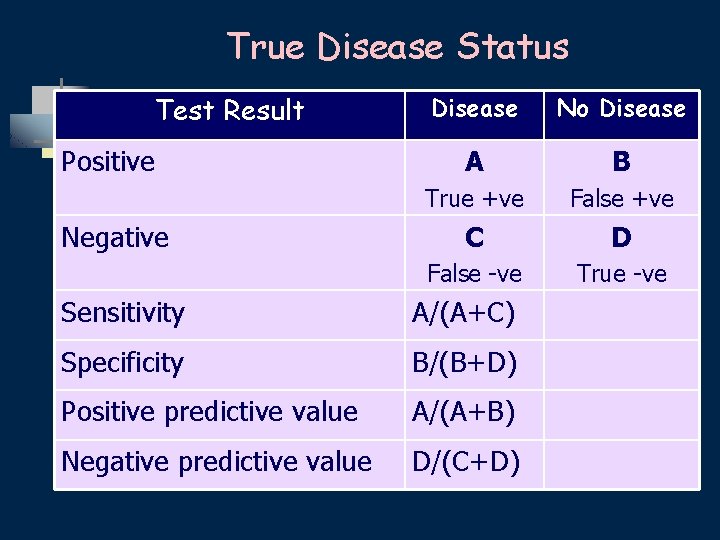
True Disease Status Test Result Positive Negative Disease No Disease A B True +ve False +ve C D False -ve True -ve Sensitivity A/(A+C) Specificity B/(B+D) Positive predictive value A/(A+B) Negative predictive value D/(C+D)
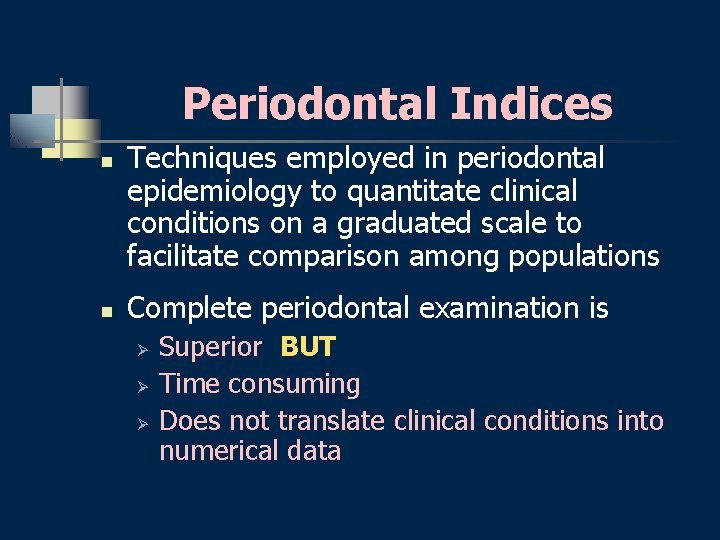
Periodontal Indices n n Techniques employed in periodontal epidemiology to quantitate clinical conditions on a graduated scale to facilitate comparison among populations Complete periodontal examination is Ø Ø Ø Superior BUT Time consuming Does not translate clinical conditions into numerical data
Ideal Index n n Simple & quick to use Accurate Reproducible Quantitative
Indices n n n Gingival health/bleeding Plaque Calculus Attachment loss Radiographic bone loss Treatment needs
Periodontal Indices n Indices measuring the degree of gingival inflammation Example: Gingival index (GI; Löe & Silness; 1967) Modified Gingival Index (Lobene et al, 1986)
Periodontal Indices n Indices used to measure periodontal destruction Example: Periodontal Index (PI, Russel; 1956) Periodontal Disease Index ( Ramfjord, 1959)
Periodontal Indices n Indices used to measure plaque accumulation Example: Plaque Index (Silness & Löe, 1964)
Periodontal Indices n Indices used to measure calculus Example: Calculus component of the PDI
Periodontal Indices n Indices used to assess treatment needs Example: Community Periodontal Index Of Treatment Needs (CPITN) Ainamo et al, 1977
Prevalence of Periodontal Diseases National Health & Nutrition Examination Survey n NHANES I (1971 -1974) NHANES III (1988 -1994) NIDR (1985 -1986) n Difficult to compare results n n
Prevalence of Periodontal Diseases Geographic distribution n More than 70% of adults have some degree of gingivitis or periodontitis n Gingivitis and calculus are more prevalent and severe in developing countries
Gingivitis n n n At the population level Found in early childhood Prevalence & severity in adolescence Prevalence of gingivitis in USA among population aged 13 and older= 54%
Gingival Bleeding NHANES III n Highest among 13 -17 yr old (63%) n Declined through 35 - to 44 -yr-old group n Increased in 45 - to 54 - yr old group
Gingivitis In Adults n n n First national survey in US (1962): 85% of men & 79% of women had gingivitis ? ? Gingivitis has declined in developed countries? ?
Prevalence of Chronic Periodontitis n Depends on: n n n Population & Threshold definition NHANES III: > 1 mm prevalence=99% : > 3 mm AL in at least one site of the mouth= 53% : > 7 mm =7%
Prevalence of Aggressive Periodontitis n n Differs with populations In the US: 0. 13%, 0. 53% and 1% prevalence has been reported
Confusion n Confusion in interpreting data from older studies, due to differences in measurement Severity of periodontitis according to AAP CAL (PAL; LPA)
Incidence of Periodontitis n Longitudinal study of periodontitis on 480 tea workers in Sri Lanka (Löe et al 1986) n Revealed natural history of disease n Parallel Study in Norway
Results n n n 8% rapid progression 81% moderate progression 11% no progression beyond gingivitis GR progresses on all surfaces In Norway; upper SES: GR buccally Reason for CAL in both groups
RISK
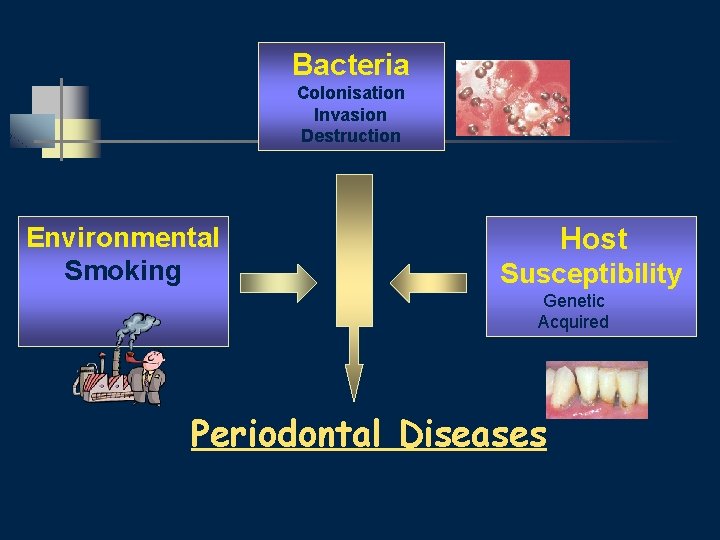
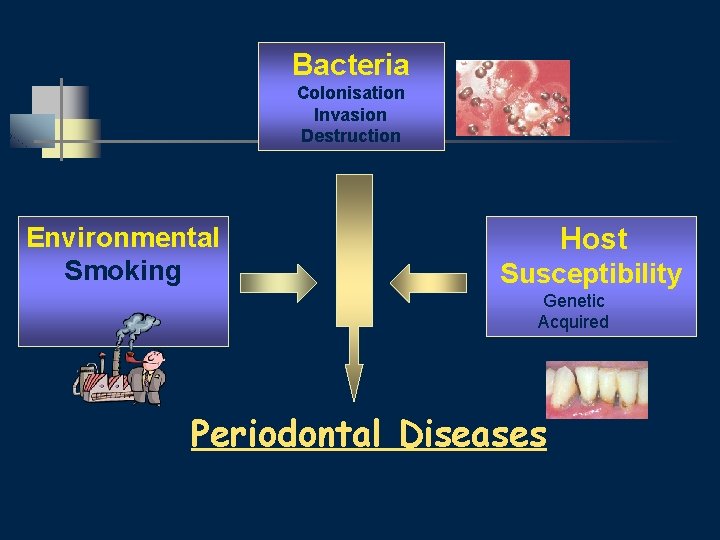
Bacteria Colonisation Invasion Destruction Environmental Smoking Host Susceptibility Genetic Acquired Periodontal Diseases

Aetiology n n n Risk Factors Susceptibility factors Severity factors

Risk Identified in terms of: n Risk Factors n Risk Indicators n Risk predictors (Pihlstrom, 2001)
Risk factors n n 1. 2. 3. 4. Identified through Longitudnal studies Examples Tobacco Smoking Diabetes Pathogenic Bacteria Microbial tooth deposits
Risk Determinants n n n 1. 2. 3. 4. 5. Also called Background Characteristics Cannot be modified Examples Genetic factors Age Gender Socioeconomic status Stress
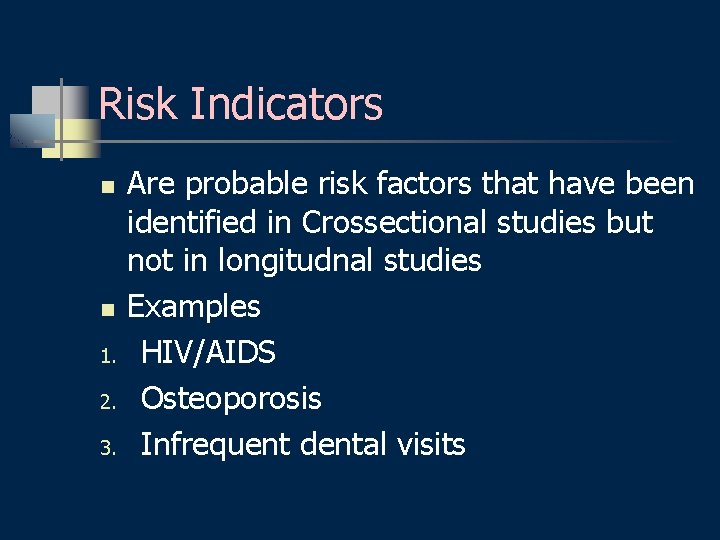
Risk Indicators n n 1. 2. 3. Are probable risk factors that have been identified in Crossectional studies but not in longitudnal studies Examples HIV/AIDS Osteoporosis Infrequent dental visits
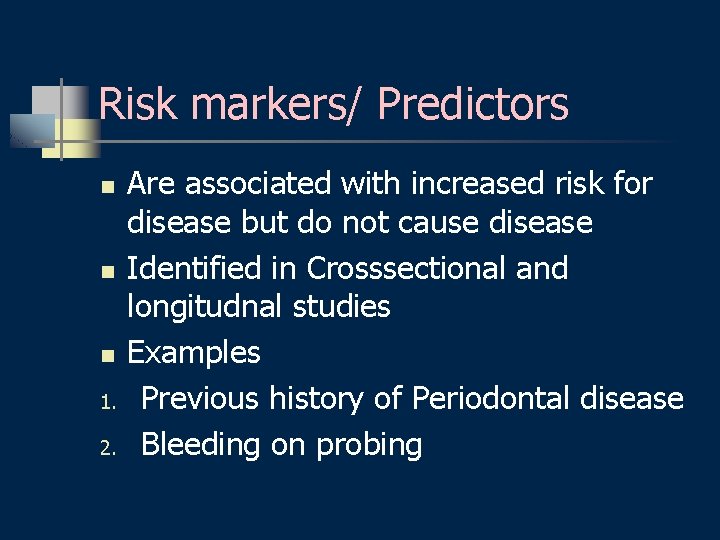
Risk markers/ Predictors n n n 1. 2. Are associated with increased risk for disease but do not cause disease Identified in Crosssectional and longitudnal studies Examples Previous history of Periodontal disease Bleeding on probing

Gender & Race n n n Men have poorer periodontal health than women, in terms of LPA, pockets and subgingival calculus Women have better oral hygiene No established differences in susceptibility to chronic periodontitis
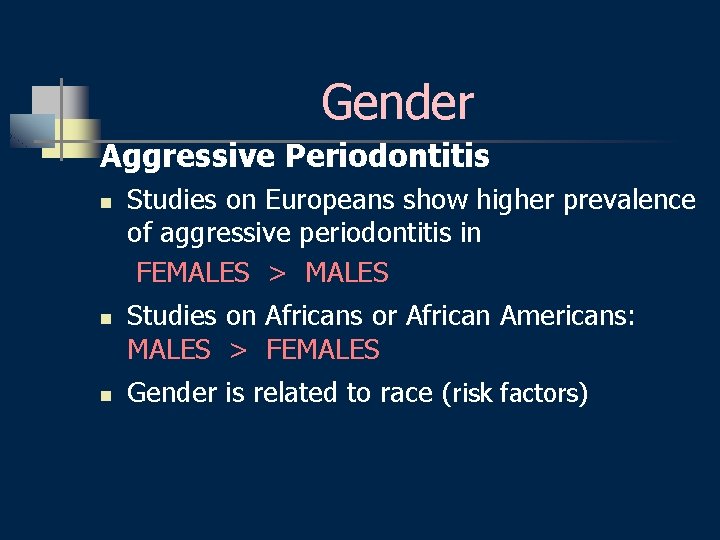
Gender Aggressive Periodontitis n n n Studies on Europeans show higher prevalence of aggressive periodontitis in FEMALES > MALES Studies on Africans or African Americans: MALES > FEMALES Gender is related to race (risk factors)
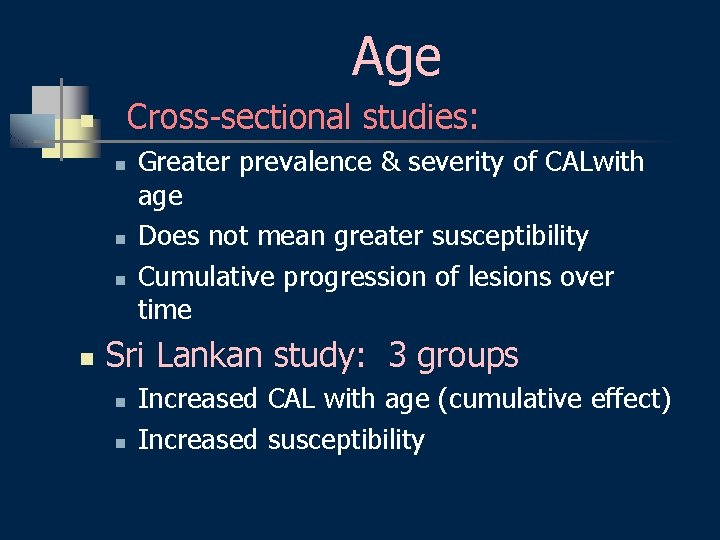
Age Cross-sectional studies: n n n Greater prevalence & severity of CALwith age Does not mean greater susceptibility Cumulative progression of lesions over time Sri Lankan study: 3 groups n n Increased CAL with age (cumulative effect) Increased susceptibility
Age Conclusion n n Susceptibility determines age of onset (CAL or attachment loss) increases with age in the group susceptible to aggressive periodontitis
Socioeconomic Status (SES) n Gingivitis & poor OH Low SES n Subgingival calculus Low SES n n Relationship between periodontitis & SES is less direct Higher prevalence of attachment & alveolar bone loss with lower SES
Oral Hygiene Classic studies n n n Plaque (Löe et al, 1965) Gingivitis Plaque & calculus correlate poorly with severe periodontitis Quantity of plaque correlates poorly with periodontitis Sensitive aetiologic factor in susceptible individuals
Local Factors n n Example: overhangs Epidemiologically: Of minor importance in aetiology of periodontal diseases
Nutrition Insufficient studies n Vitamin C deficiency n Vitamin B 6 & B 12 deficiency n Iron deficiency n
Smoking n NHANES I: 1971 -1975 n Smoking Periodontal Disease clear association Independent of Oral. Hygiene , age & other factors
Smoking n n Higher prevalence of periodontitis among smokers Smoking suppresses vascular reaction to plaque Twice as many smokers require dentures after age 50 93%-97% of patients with refractory sites are smokers
Smoking is a major Risk Factor for Periodontitis
Systemic Diseases n Diabetes Mellitus n HIV infection n CVS diseases
Diabetes Mellitus n n n Known risk factor for periodontitis Periodontitis: classic complication of DM Both types I ( IDDM) & and II (NIDDM) IDDM patients: more gingivitis & pockets IDDM: poorer glycemic control greater LPA and bone loss

Diabetes Mellitus n n Periodontitis progresses more rapidly in poorly controlled diabetics Studies on Gila River community in Arizona : n n n NIDDM: Greater CAL, bone & tooth loss Risk for periodontitis in NIDDM: 2. 81 Risk for alveolar bone loss in NIDDM: 3. 43
HIV Infection n n Not many controlled studies Controversial results High risk for CAL, bone & tooth loss Alarming signs: NUG, NUP (not statistically)

n THANKS
 Greek word for polygon
Greek word for polygon Greek word for physics
Greek word for physics Photography comes from the greek words photos and graphos
Photography comes from the greek words photos and graphos Educational technology is derived from a greek word
Educational technology is derived from a greek word The word trigonometry is derived from
The word trigonometry is derived from Geometry greek word
Geometry greek word Indikasi enap
Indikasi enap Dental case
Dental case Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Modified widman flap
Modified widman flap Plicae digestive system
Plicae digestive system Perimylolysis
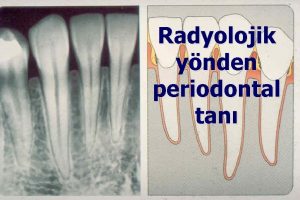
Perimylolysis Diagnosis of periodontal disease
Diagnosis of periodontal disease Glickman's concept
Glickman's concept Periodontal radyoloji
Periodontal radyoloji Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Class v facial composite charting
Class v facial composite charting Bolsa periodontal falsa y verdadera
Bolsa periodontal falsa y verdadera Rationale of periodontal treatment
Rationale of periodontal treatment Infrabony pocket
Infrabony pocket Periodonto de protección
Periodonto de protección Periapical granuloma
Periapical granuloma Plak boyayıcı ajan
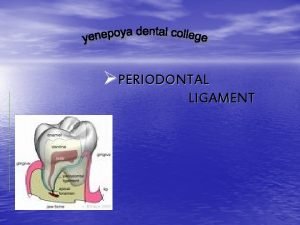
Plak boyayıcı ajan Periodontal ligament injection definition
Periodontal ligament injection definition Non-infective
Non-infective Notching of the crestal lamina dura
Notching of the crestal lamina dura Russell periodontal index
Russell periodontal index Periodontal healing
Periodontal healing Periodontal ligament meaning
Periodontal ligament meaning Peridonal
Peridonal Modified widman flap
Modified widman flap Periapical
Periapical Periodontium definition
Periodontium definition Periodontal disease
Periodontal disease Akut streptokokal gingivitis
Akut streptokokal gingivitis Murat alikan
Murat alikan Periodontal tendonitis
Periodontal tendonitis Fases de la enfermedad periodontal
Fases de la enfermedad periodontal Principles of periodontal surgery
Principles of periodontal surgery Gracey curette classification
Gracey curette classification Sement dokusu
Sement dokusu Periodonto de insercion
Periodonto de insercion Ligamento periodontal
Ligamento periodontal Periodontal abscess
Periodontal abscess Gingival description
Gingival description Kista lateral periodontal
Kista lateral periodontal Técnica de retroceso step back
Técnica de retroceso step back What is the greek miracle in greek mythology
What is the greek miracle in greek mythology Attack rate calculation
Attack rate calculation How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Distribution in epidemiology
Distribution in epidemiology Gate frame epidemiology
Gate frame epidemiology Spurious association
Spurious association Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Attack rate epidemiology formula
Attack rate epidemiology formula Logistic regression epidemiology
Logistic regression epidemiology John snow epidemiology
John snow epidemiology Epi
Epi Gordon epidemiology
Gordon epidemiology Defination of epidemiology
Defination of epidemiology Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Epidemiology definition
Epidemiology definition Epidemiology definition
Epidemiology definition