Spinal Surgery Neurosurgery Leads the Way or has







- Slides: 48
Spinal Surgery: Neurosurgery Leads the Way or has Lost its Way Volker K. H. Sonntag, M. D. Barrow Neurological Institute Phoenix, Arizona

Trends, Major Medical Complications, and Charges Associated with Surgery for Lumbar Spinal Stenosis in Older Adults Deyo RA JAMA, April 7, 2010 – Vol 303, No. 13 “Conclusions: Among Medicare recipients, between 2002 and 2007, the frequency of complex fusion procedures for spinal stenosis increased while the frequency of decompression surgery and simple fusions decreased. In 2007, compared with decompression, simple fusion and complex fusion were associated with increased risk of major complications, 30 -day mortality, and resource use. ”
Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 Method: Used Part A Claims for 2002 -2007 3 categories: § decompression § Simple fusion: anterior or posterior fusion, 1 or 2 levels § Complex fusion: 360° or any fusion > 2 levels Results: Surgical procedure declined (1. 4%) § Complex fusions up 15 x
Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 Definitions: Decompression: Any combination of discectomy and laminectomy without fusion Simple Fusion: Single surgical approach (anterior fusion, posterior fusion, transverse fusion) involving 1 or 2 disc levels Complex Fusion: 360° spine fusions by single incision, any combination of anterior with either transverse process or posterior fusion, or any fusions of more than 2 disc levels.
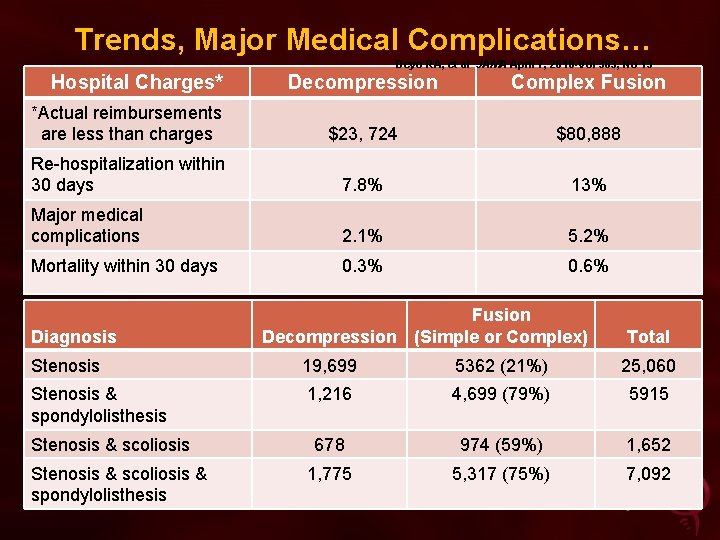
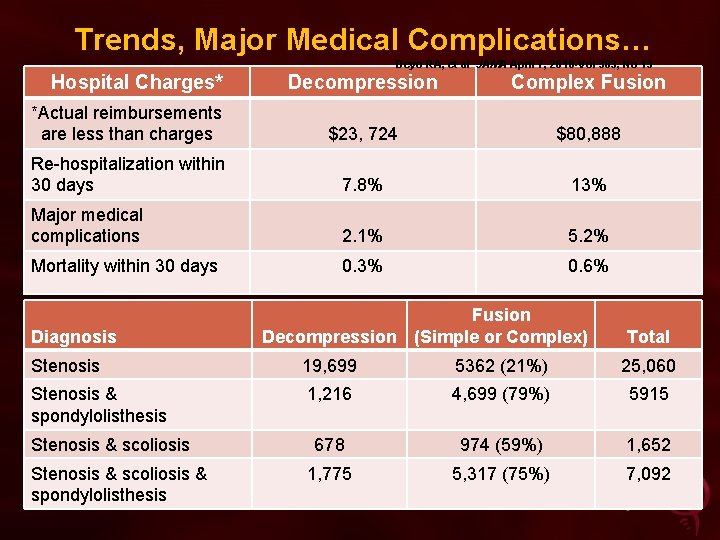
Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 Hospital Charges* Decompression Complex Fusion *Actual reimbursements are less than charges $23, 724 $80, 888 Re-hospitalization within 30 days 7. 8% 13% Major medical complications 2. 1% 5. 2% Mortality within 30 days 0. 3% 0. 6% Diagnosis Fusion Decompression (Simple or Complex) Total Stenosis 19, 699 5362 (21%) 25, 060 Stenosis & spondylolisthesis 1, 216 4, 699 (79%) 5915 678 974 (59%) 1, 652 1, 775 5, 317 (75%) 7, 092 Stenosis & scoliosis & spondylolisthesis
Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 Only 21% of patients that had stenosis only, had a fusion vs. 59%-79% that had stenosis and a secondary diagnosis
Possible reason for fusion in the 21%: Instability intra-op Pre-op flexion/extension films: instability Intra-op: both facets violated Severe back pain
Simple to Complex surgery changed in ICD Coding Method Ø ICD codes identifying the number of levels fused were not available until October 2003* Ø Multi-level single-approach surgeries in 2002 -2003 would have been “simple” Ø These same surgeries were considered “complex” in 2003 -2004 *http: /www. irpsys. com/fedregs/icdchg 09. htm
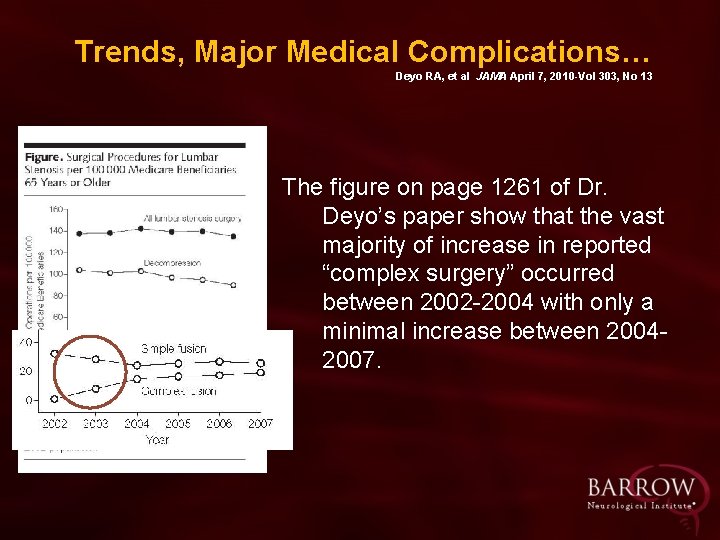
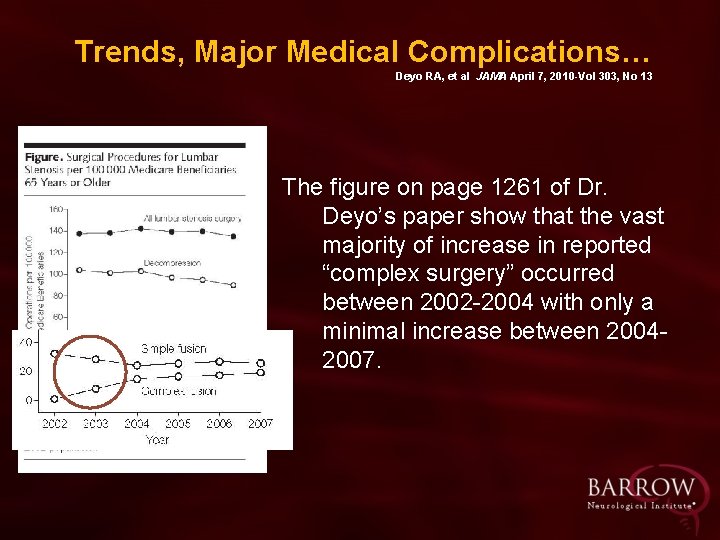
Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 The figure on page 1261 of Dr. Deyo’s paper show that the vast majority of increase in reported “complex surgery” occurred between 2002 -2004 with only a minimal increase between 20042007.
This change in coding methodology could account for a substantial proportion of the increase in “complex fusion. ”
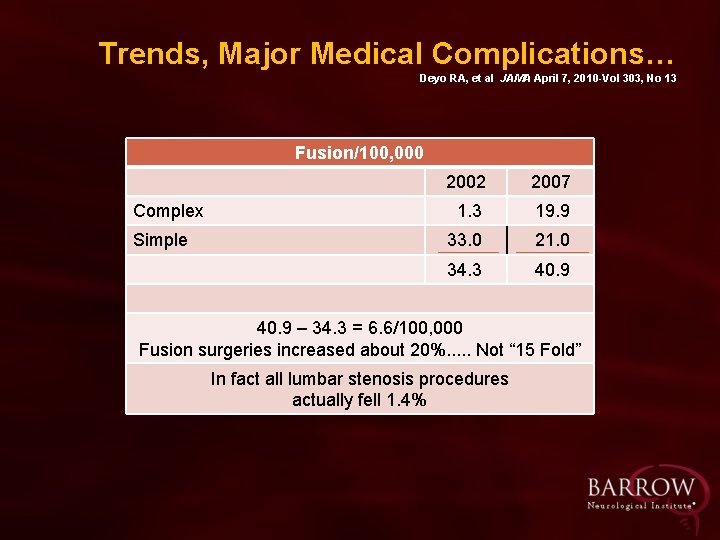
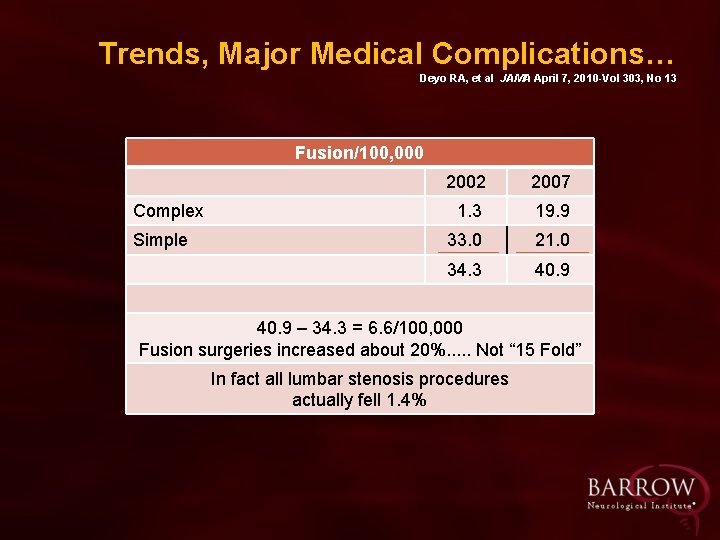
Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 Fusion/100, 000 Complex Simple 2002 2007 1. 3 19. 9 33. 0 21. 0 34. 3 40. 9 – 34. 3 = 6. 6/100, 000 Fusion surgeries increased about 20%. . . Not “ 15 Fold” In fact all lumbar stenosis procedures actually fell 1. 4%

Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 pg 1264 Ø “However, there also limitations. ” Ø “Diagnosis and procedures may be miscoded. ” Ø “Surgeons use varying definition of spine instability and ICD-9 diagnosis codes may not represent this concept well. ”
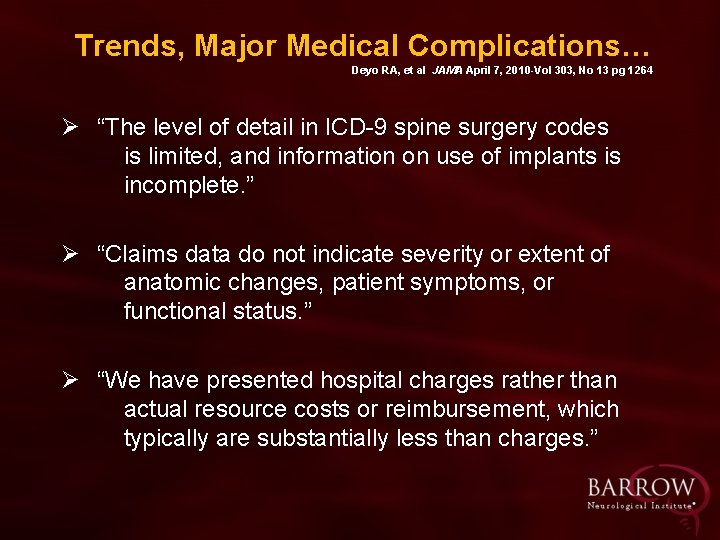
Trends, Major Medical Complications… Deyo RA, et al JAMA April 7, 2010 -Vol 303, No 13 pg 1264 Ø “The level of detail in ICD-9 spine surgery codes is limited, and information on use of implants is incomplete. ” Ø “Claims data do not indicate severity or extent of anatomic changes, patient symptoms, or functional status. ” Ø “We have presented hospital charges rather than actual resource costs or reimbursement, which typically are substantially less than charges. ”
“The only way to address the appropriateness of this trend of doing more “complex fusions” is to present data including clinical variables used for technique selection and outcome measures describing the effectiveness of the procedure. ” Letter to JAMA concerning the Deyo paper, not published, Daniel K. Resnick, et al
“A clear understanding of patient selection criteria, outcomes achieved, and risk stratification needs to be present or over-interpretation of such data is potentially misleading. ” Letter to JAMA concerning the Deyo paper, not published, Daniel K. Resnick, et al
Lumbar HNP Good data (RCT/Observational) that lumbar HNP treated surgically after failed conservative treatment is effective Ø Peul WC, et al NEJM 365: 2245 -2256, 2007 Ø Atlas SJ, Deyo RA, et al Spine 21: 1777 -1786, 1996 Deyo RA Ø Ø Ø Atlas SJ, et al, Spine 26: 11791187 2001 Atlas SJ, et al, Spine 30: 927935, 2005 Weinstein JN, et al, (SPORT) Spine 33: 2789 -2800, 2008 (EBM: RCT/Observational)
Lumbar Stenosis Good data (RCT/Observational) that lumbar stenosis treated surgically after failed conservative treatment is effective Ø Malmivaara A, et al (Finnish) Spine 32: 1 -6, 2007 Ø Atlas SJ, et al (Maine) Spine 30: 936 -943, 2005 Ø Weinstein JN (SPORT) NEJM 358: 794 -810 2008 Ø Anna NA, et al (SPORT – Costeffectiveness) Ann. Internal Med 149: 843 -853 2008 Ø Atlas SJ, Deyo RA, et al (Maine) Spine 21: 1787 -1795, 1996 Deyo RA (EBM: RCT/Observational)

DEGENERATIVE SPONDYLOLISTHESIS
Fusion +/- Laminectomy Good data (RCT/observational) that lumbar degenerative spondylolisthesis with or without stenosis treated surgically (fusion+/- laminectomy), after failed conservative treatment is effective Ø Weinstein J, et al, NEJM 2007 JBJS 2009 (SPORT) Ø Martin CR, et al, Spine 2007 Ø Herkowitz HN, Kurz LT JMJS 1991 Ø Kornblum , et al, Spine 29, 2004 Ø Tosteson AN, et al, Ann Internal Medicine: 149, 2008

AXIAL LOW BACK PAIN
Axial Low Back Pain Mixed data (RCT/observational) that axial LBP treated surgically with fusion (after conservative treatment) is better then conservative treatment only +/- Brox JI, et al, Spine 2003: Both groups improved significantly and equally +/- Fairbank J, et al, BMI 2005: Improvement in ODI only with surgery (barely statistically significant) +/- Brox JI, et al, Pain 2006 (Norway): Surgery vs. conservative = No difference
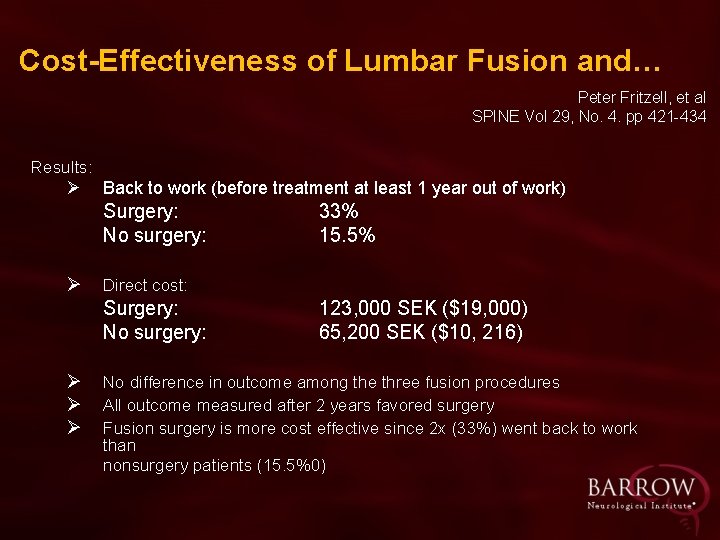
Axial Low Back Pain Mixed data (RCT/observational) that axial LBP treated surgically with fusion (after conservative treatment) is better then conservative treatment only. + Fritzell P, et al, Spine 29, 2004 (Sweden): Surgery group did better. The fusion surgery cost $19, 000 vs. nonsurgery $10, 216, but 33% of the fusion patients went back to work vs only 15. 5% of the non-surgery patients. Authors conclude the fusion surgery is more cost effective. +/- Fritzell P, et al, Spine 2001: Fusion may lead to a better outcome.
Utilization of Spinal Fusion for Isolated Lumbar Degenerative Disc Disease and Long-term Development of Associated Spinal Pathologies: A Population-based Study Mc. Girt M. et al AANS/CNS Section on Disorders of the Spine and Peripheral Nerves Annual Meeting, Phoenix, AZ, March 2011 Ø The Market. Scan® Commercial Claims and Encounters and The Medicare Supplemental and Coordination of Benefits databases, 2003 -2008, were queried to identify all patients with new diagnosis of isolated lumbar DDD utilizing ICD-9 -CM codes Ø Kaplan-Meier survivorship analysis was used to assess the five year cumulative incidents of surgical intervention and new diagnoses of associated spinal pathologies
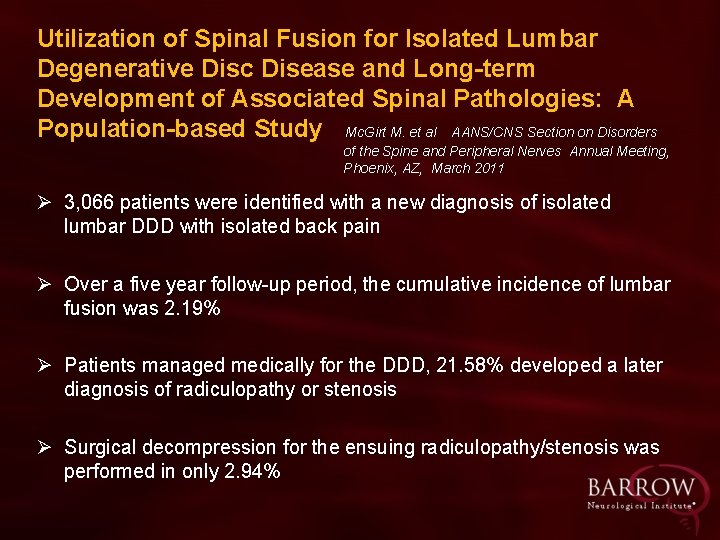
Utilization of Spinal Fusion for Isolated Lumbar Degenerative Disc Disease and Long-term Development of Associated Spinal Pathologies: A Population-based Study Mc. Girt M. et al AANS/CNS Section on Disorders of the Spine and Peripheral Nerves Annual Meeting, Phoenix, AZ, March 2011 Ø 3, 066 patients were identified with a new diagnosis of isolated lumbar DDD with isolated back pain Ø Over a five year follow-up period, the cumulative incidence of lumbar fusion was 2. 19% Ø Patients managed medically for the DDD, 21. 58% developed a later diagnosis of radiculopathy or stenosis Ø Surgical decompression for the ensuing radiculopathy/stenosis was performed in only 2. 94%
Utilization of Spinal Fusion for Isolated Lumbar Degenerative Disc Disease and Long-term Development of Associated Spinal Pathologies: A Population-based Study Mc. Girt M. et al AANS/CNS Section on Disorders of the Spine and Peripheral Nerves Annual Meeting, Phoenix, AZ, March 2011 CONCLUSION: “In the US, fusion procedures for lumbar DDD (for axial low back pain) are performed in a small minority of patients and that medically-managed patients should be monitored for progressive lumbar degeneration”
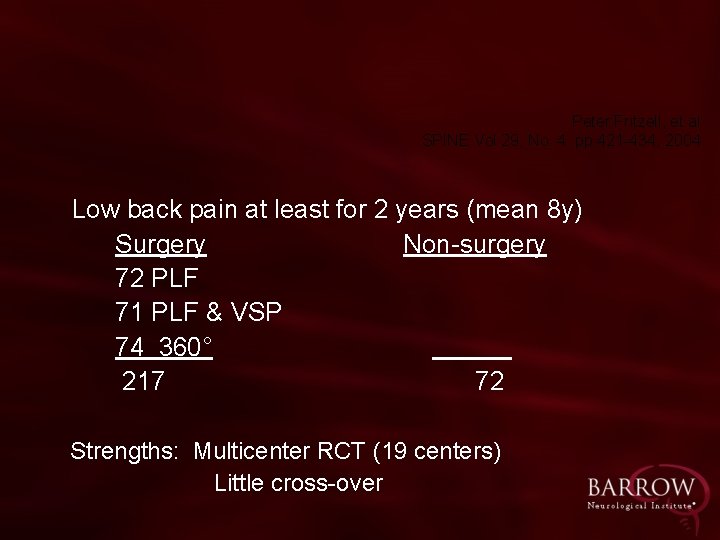
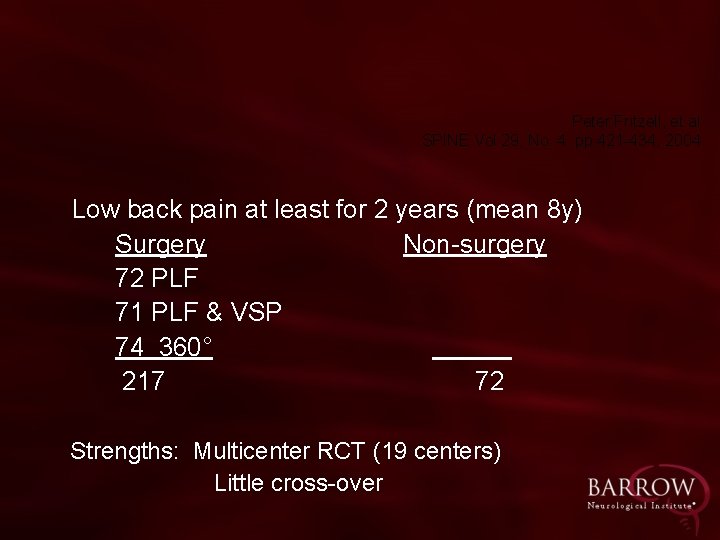
Peter Fritzell, et al SPINE Vol 29, No. 4. pp 421 -434, 2004 Low back pain at least for 2 years (mean 8 y) Surgery Non-surgery 72 PLF 71 PLF & VSP 74 360° 217 72 Strengths: Multicenter RCT (19 centers) Little cross-over
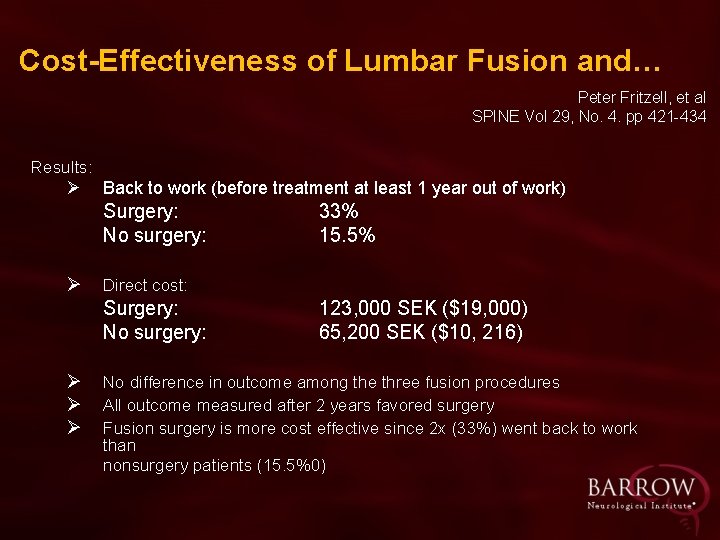
Cost-Effectiveness of Lumbar Fusion and… Peter Fritzell, et al SPINE Vol 29, No. 4. pp 421 -434 Results: Ø Back to work (before treatment at least 1 year out of work) Surgery: No surgery: Ø Direct cost: Surgery: No surgery: Ø Ø Ø 33% 15. 5% 123, 000 SEK ($19, 000) 65, 200 SEK ($10, 216) No difference in outcome among the three fusion procedures All outcome measured after 2 years favored surgery Fusion surgery is more cost effective since 2 x (33%) went back to work than nonsurgery patients (15. 5%0)
Quality of Life in the Elderly and Fusion Surgery “Because older patients are more susceptible to surgical complications, the implication of fusion may be particularly important in this group. ” Deyo RA, et al, ” Lumbar Spine Fusion”, page 1464, Spine 18, 1993
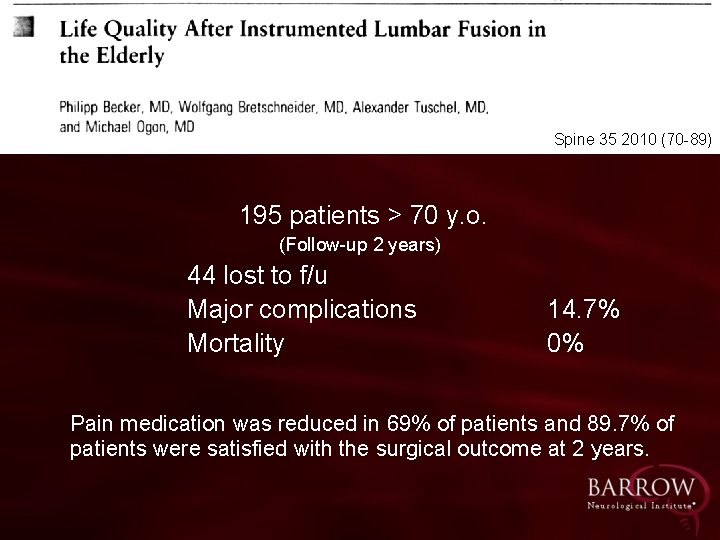
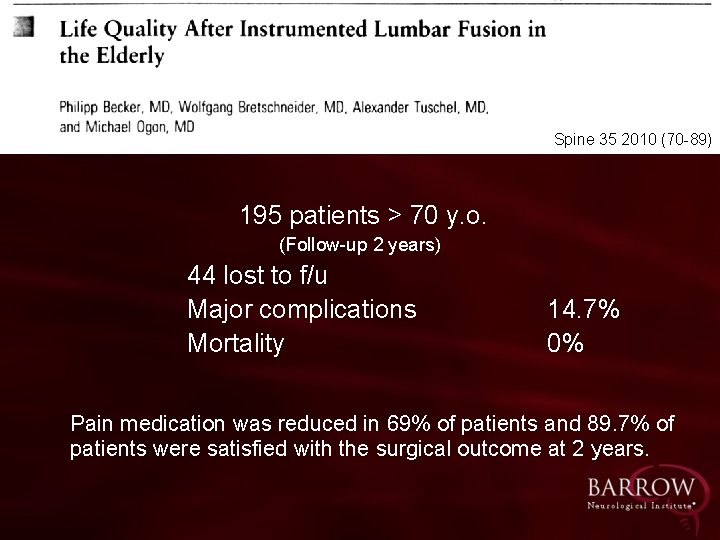
Spine 35 2010 (70 -89) 195 patients > 70 y. o. (Follow-up 2 years) 44 lost to f/u Major complications Mortality 14. 7% 0% Pain medication was reduced in 69% of patients and 89. 7% of patients were satisfied with the surgical outcome at 2 years.
Life Quality After Instrumented Lumbar Fusion in the Elderly Becker P, et al Spine 35 2010 (70 -89) “The existing studies show that the assessment of success after spinal fusion surgery in the geriatric patient has been based on the peri-operative complication rate with little attention directed toward improvement in perception of pain and the need for pain medication. ”
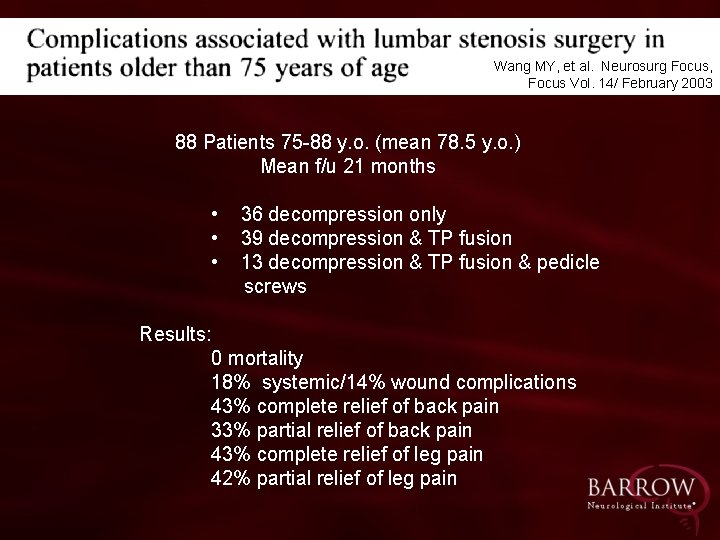
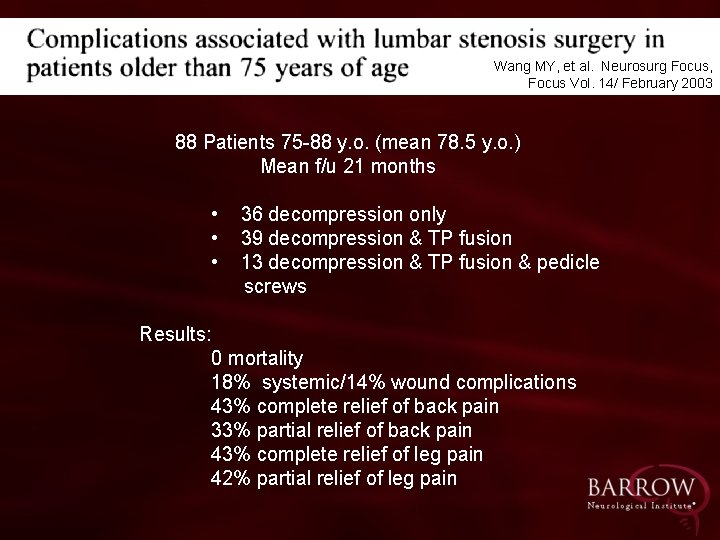
Wang MY, et al. Neurosurg Focus, Focus Vol. 14/ February 2003 88 Patients 75 -88 y. o. (mean 78. 5 y. o. ) Mean f/u 21 months • • • 36 decompression only 39 decompression & TP fusion 13 decompression & TP fusion & pedicle screws Results: 0 mortality 18% systemic/14% wound complications 43% complete relief of back pain 33% partial relief of back pain 43% complete relief of leg pain 42% partial relief of leg pain
Complications Associated with Lumbar Wang MY, et al. Neurosurgery Stenosis Surgery……. Focus Vol. 14/ February 2003 Length of operative time (p=0. 003) and comorbidity index score (p=0. 088) were statistically associated with risk of complication, however patients older than 75 yo with lumbar stenosis have a similar success rate as younger patients
Treatment of more complex spine cases is now possible in the elderly, treating patients that before had no option, after failed conservative treatment : Ø Population has increased, especially in the >65 year old and therefore increasing the chance to develop symptomatic degenerative spine Ø Less invasive technique (MISS) Ø Better surgical technique Ø Better imaging Ø Advancement in anesthesia and supportive care
Treatment of more complex spine cases is now possible in the elderly, treating patients that before had no option, after failed conservative treatment: Ø Ø Improvement in diagnosis Advanced instrumentation Increased spine fellowships Advanced biomechanics
Treatment of more complex spine cases is now possible in the elderly, treating patients that before had no option, after failed conservative treatment: Ø 65 y. o. or older population is a healthier population than 10 years ago and can undergo surgical instrumentation. Ø 65 y. o. or older do have greater demands to be active than 10 years ago.

The Stethoscope (Laennec 1816) Despite its benefits many doctors opposed the stethoscope: Reiser, SJ Technological Medicine: The Changing World of Doctors and Patients Pages 6 -10 § Diversity of sounds from different parts of the body § Large learning curve § Unwillingness of doctors to become students again § Relying too much on instruments
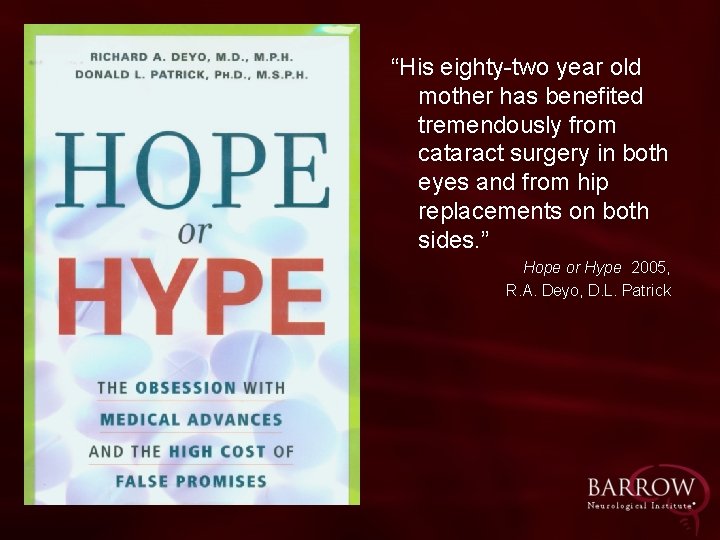
“His eighty-two year old mother has benefited tremendously from cataract surgery in both eyes and from hip replacements on both sides. ” Hope or Hype 2005, R. A. Deyo, D. L. Patrick
“Spinal fusion surgery is undoubtedly effective for some conditions in some patients. ” “Its efficacy for most common indications, such as degenerative disk disease, remains unclear. ” NEJM Feb 2004
“There is growing evidence to support the use of decompression surgery, but other questions about surgical efficacy and safety abound. Aside from co-existing spondylolisthesis and scoliosis, what are the indications for fusion in treating stenosis? (2010)
JAMA, December 8, 2010 – Vol 304, No. 22 “Medicine needs to be scientifically based, but physicians need to be engaged through their passion and emotions. ”
Could it be possible that the neurosurgeon recommends/does the bigger operation because: Ø Ø Ø it is necessary / it is possible has the best chance of helping the patient is based on best evidence that he/she has
Neurosurgery is leading the way: Ø Judicious use of instrumentation Ø Continue to advance the field of spine, including development of better instrumentation/image guidance/MISS Ø As the >65 y. o. population increases, spinal surgery with/without instrumentation should be offered after failed conservative treatment after considering all alternatives
Neurosurgery is leading the way: Ø As in all of medicine, a few have lost the way (financially driven? ) Ø Spine surgery including lumbar fusion can be done safely in the elderly Ø Quality of life is improved with surgical intervention for lumbar stenosis, HNP , spondylolisthesis, with fusion when indicated
Neurosurgery is leading the way: Ø ICD code changes in 2003 contributes to the perceived increase in complex fusion Ø Fusion for axial low back pain is controversial Ø Passion + Emotions + Good Judgment + Science lead the well trained (residency +/-fellowship) neurosurgeon to the appropriate procedure THANK YOU FOR YOUR ATTENTION!

New promotional material for book sales

 Pathologic q wave criteria
Pathologic q wave criteria Figure 13-2 spinal nerves
Figure 13-2 spinal nerves Lateral pectoral nerve
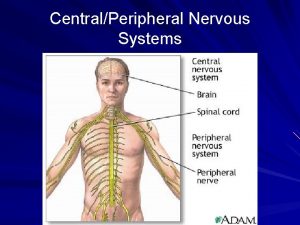
Lateral pectoral nerve Spinal cord and spinal nerves exercise 15
Spinal cord and spinal nerves exercise 15 Spinal cord labelled
Spinal cord labelled Amy lee plastic surgery
Amy lee plastic surgery Norse referral login
Norse referral login The walton centre for neurology and neurosurgery
The walton centre for neurology and neurosurgery Neurosurgery
Neurosurgery Penn state neurosurgery faculty
Penn state neurosurgery faculty Neurosurgery
Neurosurgery Alan cohen neurosurgery
Alan cohen neurosurgery Chapter 7 section 2 britain leads the way worksheet answers
Chapter 7 section 2 britain leads the way worksheet answers All the way my savior leads me fanny crosby
All the way my savior leads me fanny crosby All the way my savior leads me
All the way my savior leads me Walk this way talk this way
Walk this way talk this way Threaded binary tree in data structure
Threaded binary tree in data structure Pertanyaan tentang anova
Pertanyaan tentang anova Beda one way anova dan two way anova
Beda one way anova dan two way anova The old way and the new way
The old way and the new way How to do a two way frequency table
How to do a two way frequency table One way anova null hypothesis
One way anova null hypothesis A bottle of rum to fill my tum
A bottle of rum to fill my tum Two way anova
Two way anova One way anova vs two way anova
One way anova vs two way anova Thẻ vin
Thẻ vin Thể thơ truyền thống
Thể thơ truyền thống Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên 101012 bằng
101012 bằng Chúa sống lại
Chúa sống lại Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Cong thức tính động năng
Cong thức tính động năng Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể độ dài liên kết
độ dài liên kết Chó sói
Chó sói Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu điện thế nghỉ
điện thế nghỉ