RTECA Week 11 Patient Skills Communication 1 Patient














































































- Slides: 162

RTEC-A Week 11 Patient Skills & Communication 1

Patient Communication 1. Interacting with the patient 2. Interacting with family and friends 3. Methods of Effective Communication 4. Age as a factor in Patient Interactions 2
Radiologic Technologist 1. Helping others 2. Working with people 3. Making a difference 4. Thinking critically 5. Demonstrating creativity 6. Achieving results 3
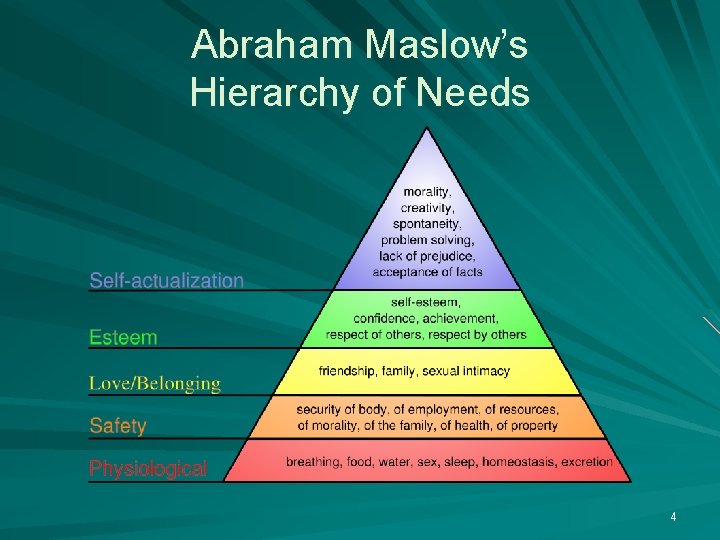
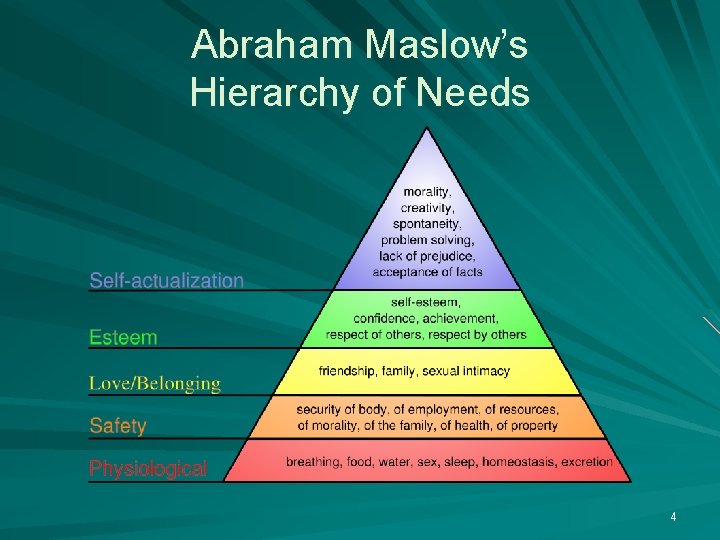
Abraham Maslow’s Hierarchy of Needs 4
Patient Dignity 1. Patients are usually in the lower levels of Maslow’s Hierarchy 2. Must always be remembered and respected 3. Difficult to maintain dignity when ill 5
Why is this important? PATIENT NEEDS 1. Altered states of consciousness 2. Environment 3. Fear of unknown 4. Vulnerable 5. Coping Mechanisms 6
Classification of Patients 1. Inpatients 2. Outpatients – Family – Friends 7
Methods of Communication 1. Verbal 2. Humor 3. Paralanguage 4. 5. 1. Professional Appearance 2. Physical Presence 3. Visual Contact Body Language Touch 1. Palpation 8
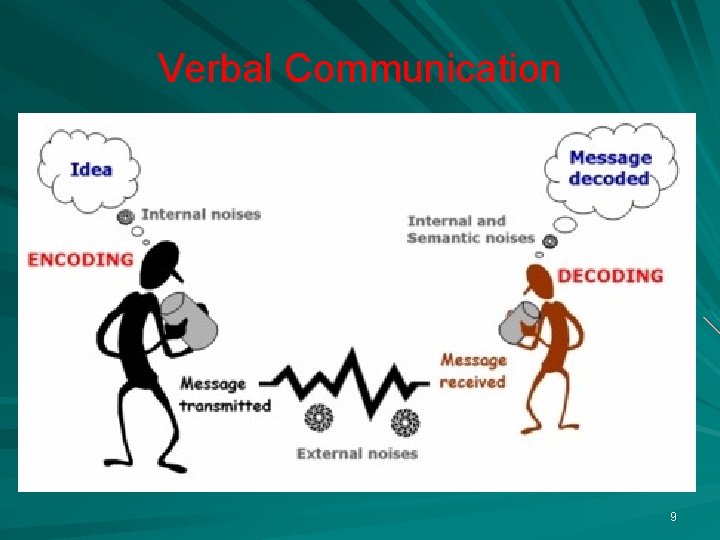
Verbal Communication 9
Communication thru Humor 10
Paralanguage Defines all of the audio information in a conversation beyond word choice Simply listening to someone’s voice, even if you can’t make out the words, conveys their emotional state 11
Body Language You could be talking to someone and your body language will convey something else entirely. Make eye contact occasionally you show an interest in that person and in what he or she is saying. A smile sends a positive message. Smiling adds warmth and confidence about you. Arms crossed or folded over your chest say that you have shut other people out and have no interest in them or what they are saying. Placing your arms at your side can make you look and feel confident and relaxed to other people around you. 12

Touch and Palpation 13
Radiographer’s Responsibility 1. Introduction 2. Explanation of exam 3. Inform patient how they will receive their results 4. Risks of examination 14
Rad Tech’s Role in Clinical Hx 1. Extract as much history as possible 2. Radiologists often do not even speak with the patient. 3. Radiologist can be focus on anatomy of interest 15

Desirable Qualities for Establishing Open Dialogue 1. Respect 2. Genuineness 3. Empathy 4. Polite 5. Professional demeanor 16

Data Collection 1. Objective: Signs that can be seen 2. Subjective: Perceived by the affected individual 17
Questioning Skills 1. Open-ended questions 2. Facilitation – encourages pt to elaborate 3. Silence – give pt time to remember 4. Probing questions – focus interview, provide more information 5. Repetition – rewording, clarifies info 6. Summarization – verifies accuracy 18
Leading Questions This is an UNDESIRABLE method of questioning. – Introduces bias to history 19
Chief Complaint 1. Focuses attention to the single most important issue. 2. Patients often have many complaints – Focus on primary reason for exam 20

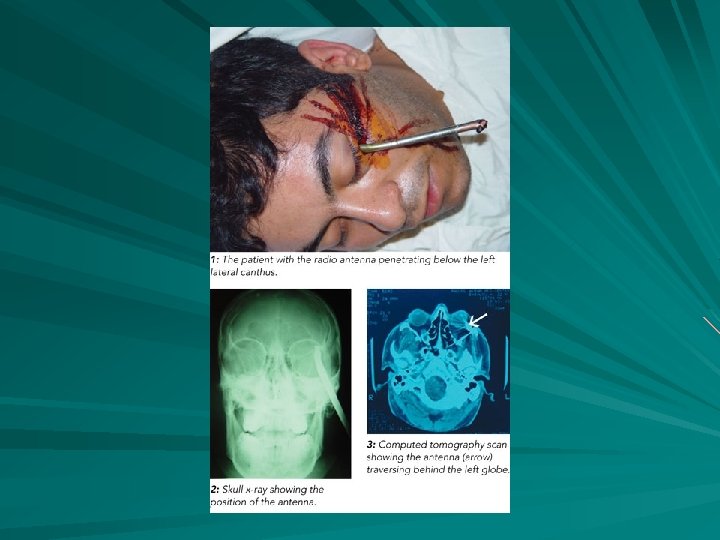
You never know what you are going to get? 21

Special Condition Patients Traumatized Patients Visually Impaired Patients Speech and Hearing Impaired Patients Non-English Speaking Patients Mentally Impaired Patients Substance Abusers 22
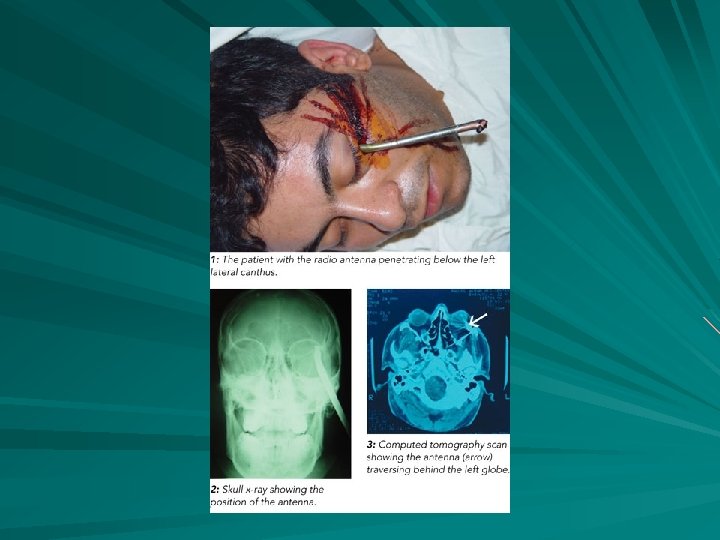
23

Gerontology The study of aging and diseases of the elderly. By the end of the 20 th century 33 million, more than 12% of total population. In 1900 only 4%, of population 24
Key to a Successful Exam Plan of action Systematic problem-solving process – Assessment of data – Setting a goal – Establishing a plan – Safety in completing assignment – Evaluating the work 25
Communication The key to a successful exam for Technologist and Patient. 26

Human Diversity

What is Human Diversity? 1. Is also known as cultural diversity. 2. It means the inherent differences among people. 3. It addresses the entirety of the ways people are different and alike.
Characteristics of Human Diversity Age Disability Economic status Education Geographic location Organizational level Political affiliation Sexual orientation Ethnicity Family status First language Gender Lifestyle Physical characteristics Religion Work style or ethic

Globalization People go into other countries for: – Work – School – Medical care – Visit / Vacation – Live / Relocate – Refuge / Safety
Globalization’s Effect Nation, societies and businesses have become multicultural or cross cultural Strategies must be employed to understand cultural differences Strategies needed to mediate conflicts A concerted effort toward Cultural competency

Significant Diversity Traits Age Ethnicity Race Gender or sexual orientation Mental or physical disability
Age Cultures assign different values Baby Boomers (1946 – 1964) – – – 75 million born Overall healthy and educated Will be in the work force longer Age biases in western society – – Valuing you over age Viewing aging as a “bad” thing Forgetting contributions offered by the aging Considering seniors as mentally inferior
Ethnicity and National Origin Ethnicity refers to a person’s racial, national, religious, linguistic and cultural heritage. Overcoming Linguistic Differences – – Bilingual staff Medical interpreters Encouraging bilingualism Forms in different languages Many different cultures as demonstrated in everyday life and by statistical data: U. S. Census 2000.

Ethnocentrism and Racism Ethnocentrism is the belief that norms and values of their culture should be standard Racism is the belief that one race or culture is superior to others
Gender or Sexual Orientation Male vs. Female – 1900 female roles – Today's women – Glass ceiling Gender role stereotyping Gender identity Sexual orientation – Heterosexual – Homosexual – Bisexual Ksix Homophobia
Mental or Physical Disability Mental or physical ability is the capacity to perform cognitive and psychomotor tasks with average ability Those with disabilities have been shunned – Seen as objects or assistance, protection and treatment 600 million or 10% of the world have some form of disability

Elements of Cultural Competency Valuing Diversity Possessing the capacity for cultural self assessment Having a consciousness of the dynamics of cross cultural interaction Institutionalizing cultural knowledge Developing adaptations of service based on an understanding of multiculturalism

Empathetic Practices Communication Assessment and communication Negotiating

Areas of Cultural Diversity related to Health Care Communication Space Time Environmental control Biologic Variations Social organizations

Patient Vital Signs Medical Emergencies and Infection Control
Homeostasis A constancy in the internal environment of the body Naturally maintained by adaptive responses that promote healthy survival Primary mechanisms: – – – Heartbeat Blood pressure Body temperature Respiratory rate Electrolyte balance
Vital Signs Body Temperature Respiratory Rate Pulse / Heart Rate Blood Pressure Sensorium (mental alertness)

Importance of Vital Signs Indicates the patient’s immediate condition Can show improvement due to treatment Can show a decline in condition
Body Temperature Normal temperature: 98. 6 ° F – 1° - 2°F daily variation – Still considered normal: 97. 7 °F – 99. 5 °F Human body functions within a narrow range of temperature variations – Humans can survive between 93. 2 ° F and 106 ° F

Thermoregulation Shivering when cold Sweating when hot
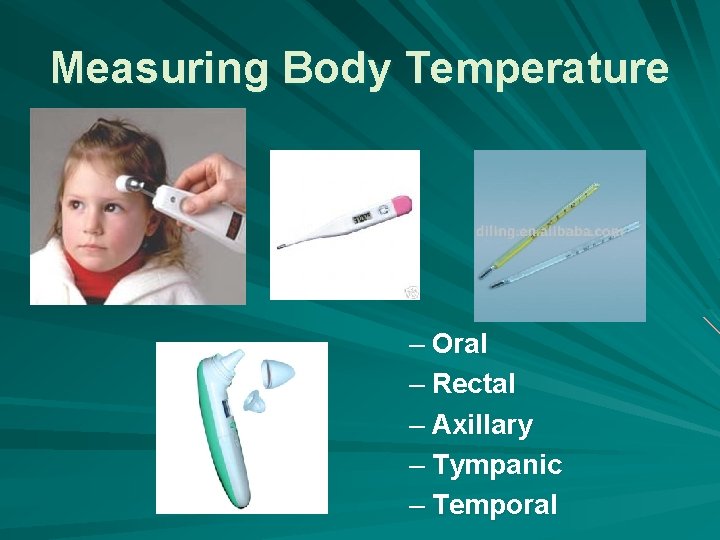
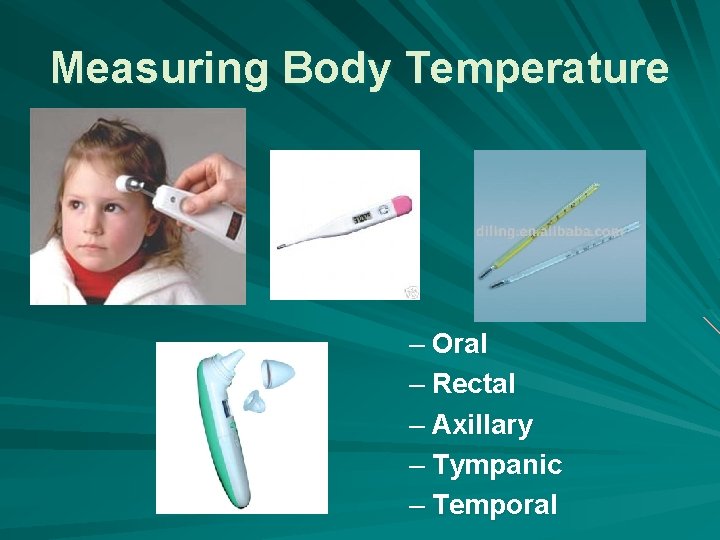
Measuring Body Temperature – Oral – Rectal – Axillary – Tympanic – Temporal
Abnormalities in Body Temperature Hyperthermia – Fever, febrile – Temperature higher than 99. 5 °F Hypothermia – below normal range of 97. 7 °F – Due to Environment Medically induced Damage to hypothalamus
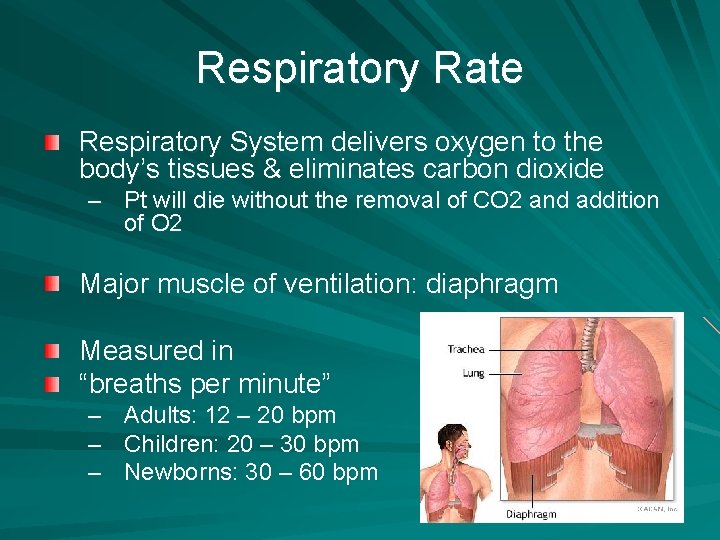
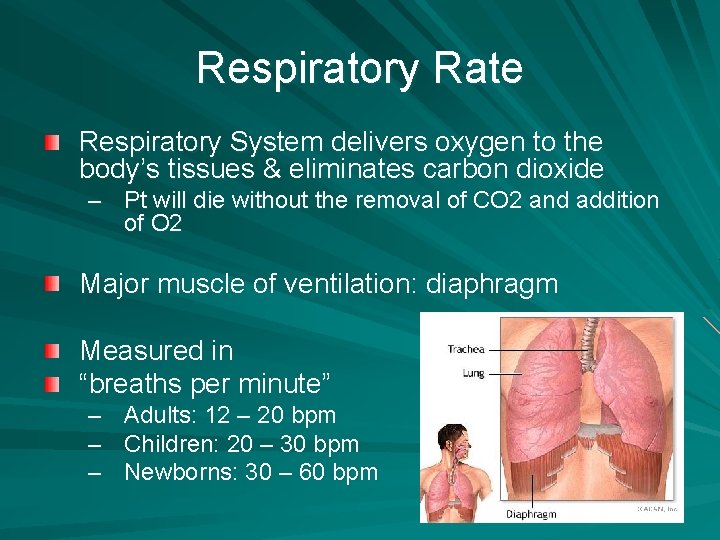
Respiratory Rate Respiratory System delivers oxygen to the body’s tissues & eliminates carbon dioxide – Pt will die without the removal of CO 2 and addition of O 2 Major muscle of ventilation: diaphragm Measured in “breaths per minute” – – – Adults: 12 – 20 bpm Children: 20 – 30 bpm Newborns: 30 – 60 bpm
Abnormalities of Respiratory Rate Tachypnea – Greater than 20 breaths per minute (adult) Bradypnea – decrease is breathing Dyspnea- difficulty breathing Apnea- no breathing

Methods of Delivering Oxygen Nasal Cannula Masks Ventilators Oxyhood

Pulse Oximeter Normal Pulse Oximeter = 95% to 100%
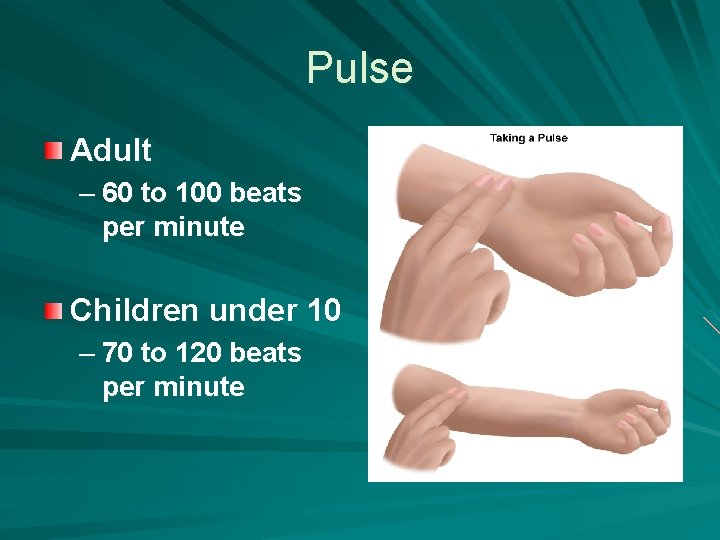
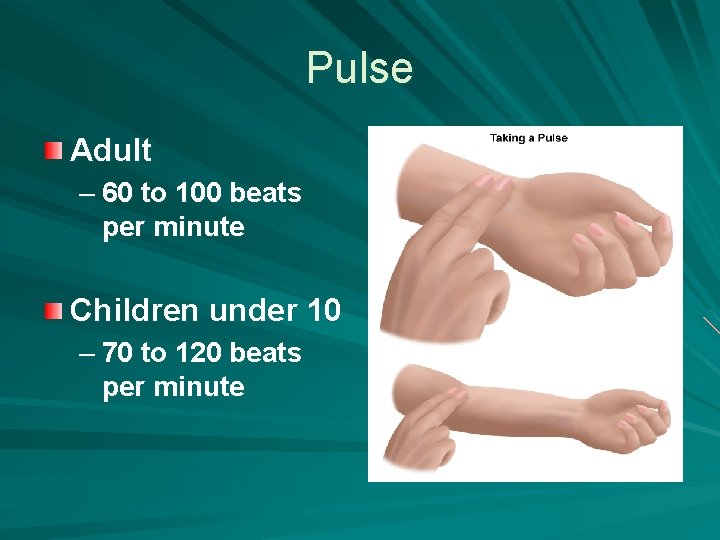
Pulse Adult – 60 to 100 beats per minute Children under 10 – 70 to 120 beats per minute

Measurement Radial artery Brachial Carotid artery Apical pulses
Abnormalities of Pulse Rate Tachycardia – Pulse rate increases by more than 20 bpm in resting adult – Greater than 100 bpm Bradycardia – Decrease in heart rate
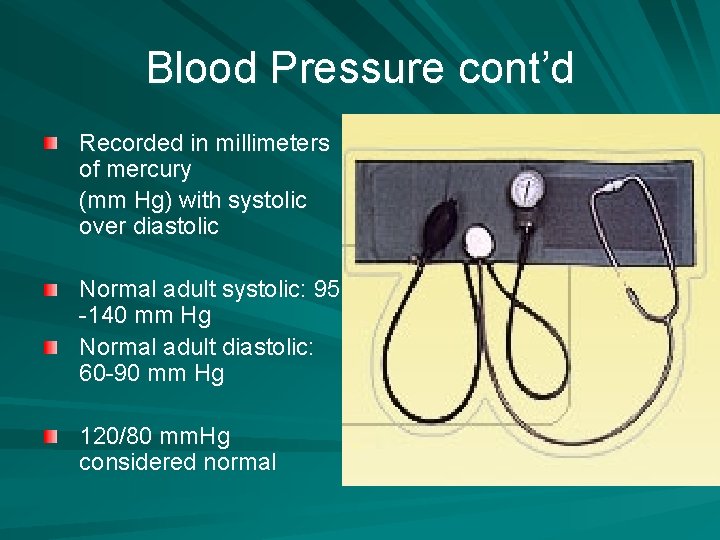
Blood Pressure Measure of the force exerted by blood on the arterial walls during contraction & relaxation. Measured pressure when the heart is relaxed: Diastolic Measured pressure when the heart is contracted: Systolic Measured with a Sphygmomanometer
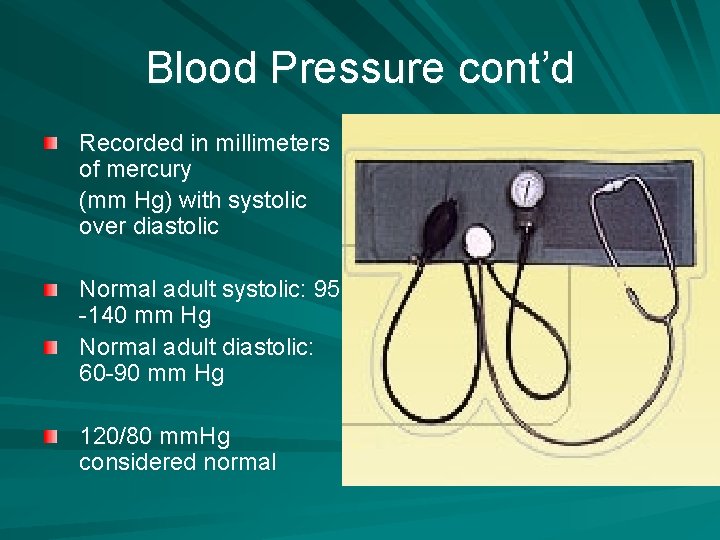
Blood Pressure cont’d Recorded in millimeters of mercury (mm Hg) with systolic over diastolic Normal adult systolic: 95 -140 mm Hg Normal adult diastolic: 60 -90 mm Hg 120/80 mm. Hg considered normal
Abnormalities of Blood Pressure Hypertension – Persistent elevation above 140/90 mm. Hg Hypotension – Persistent less than 95/60 mm. Hg

RTA Medical Emergencies and Infection Control Caution – some images may be disturbing to the viewer …but this is what we may see in the course of our work



TRAUMA- X-RAY READY

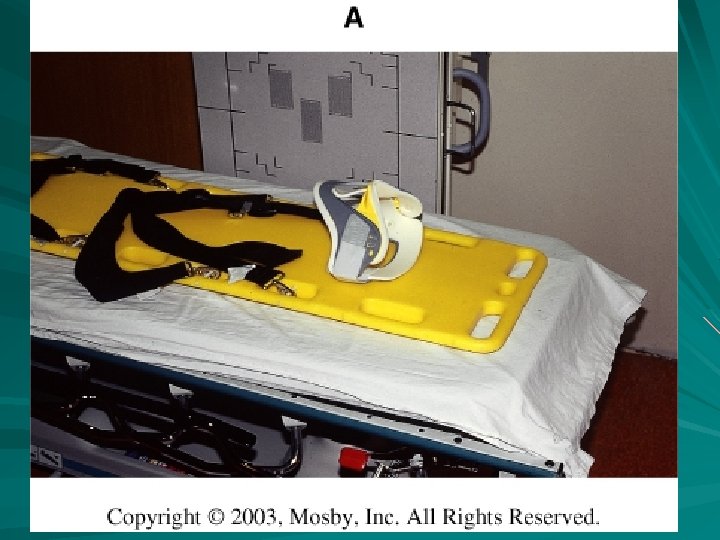
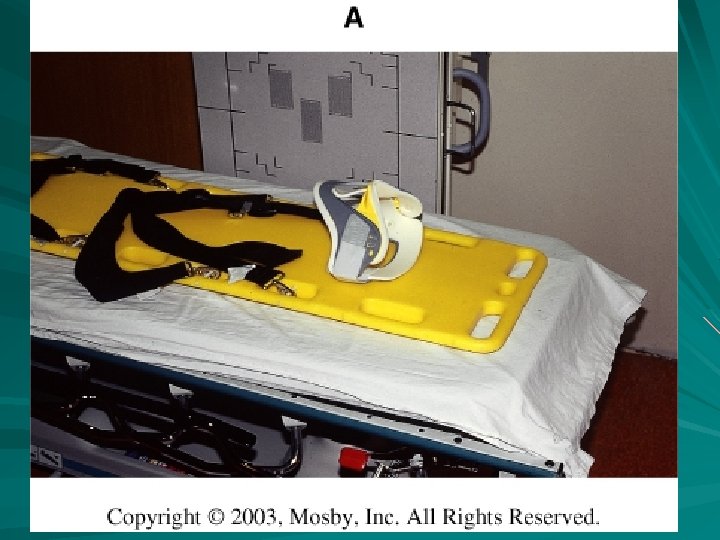
SPINAL INJURY PT
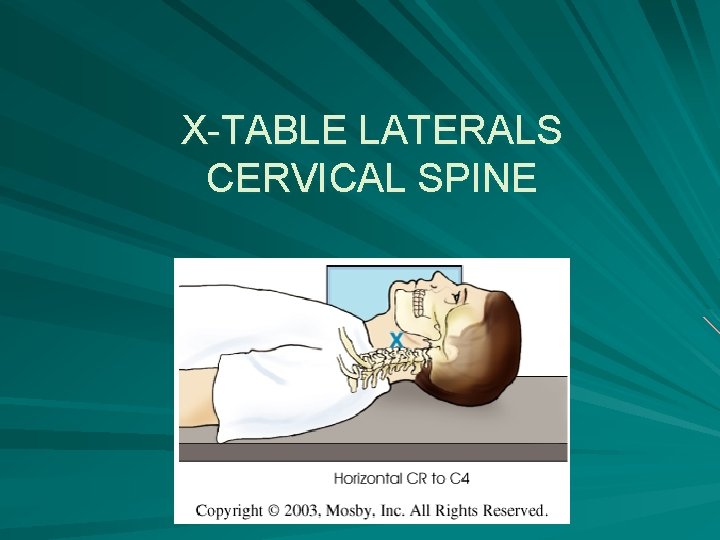
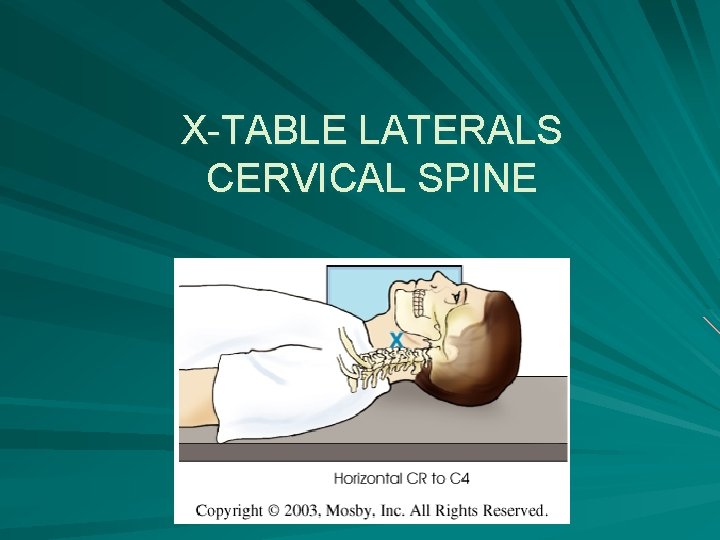
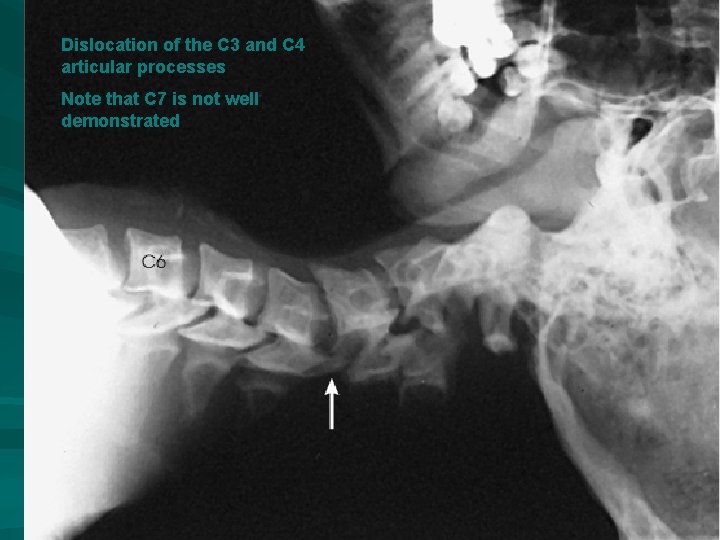
X-TABLE LATERALS CERVICAL SPINE

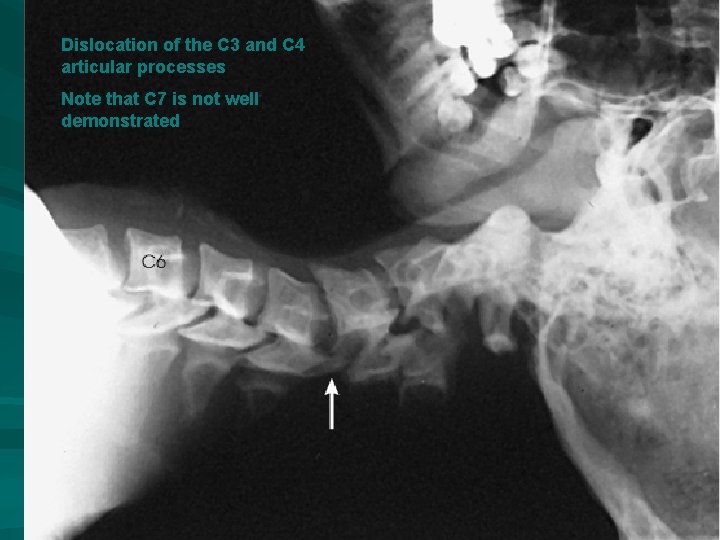
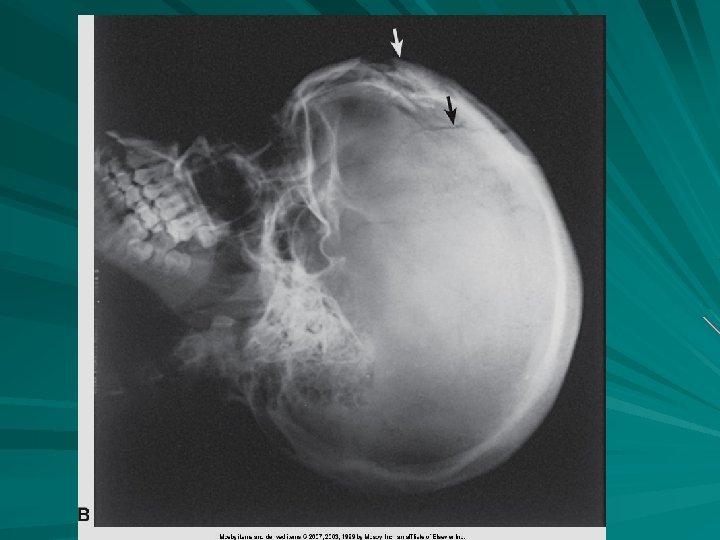
Dislocation of the C 3 and C 4 articular processes Note that C 7 is not well demonstrated

Some studies of spinal trauma have recorded a missed injury rate as high as 33%.




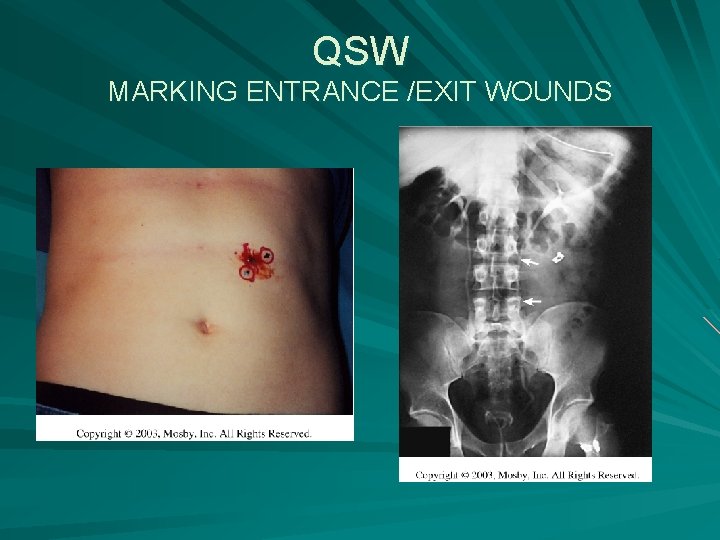
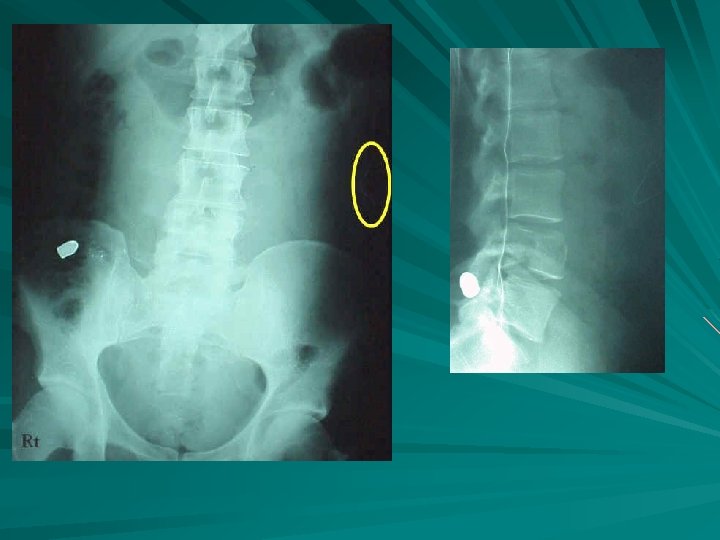
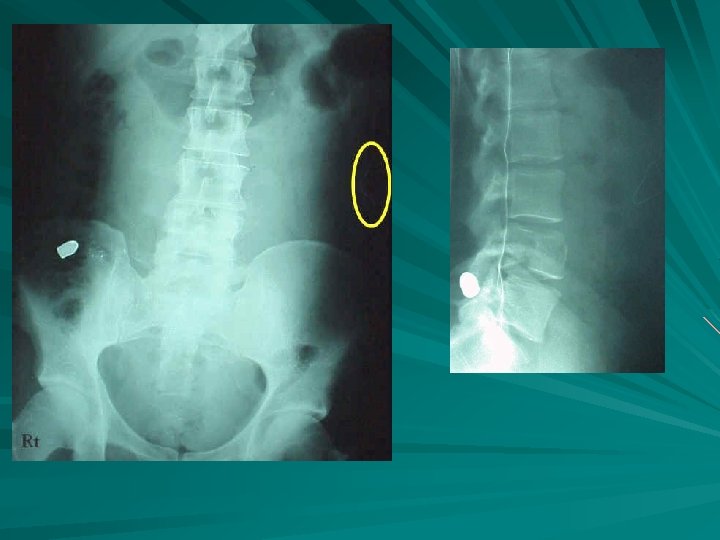
GSW TO ABD
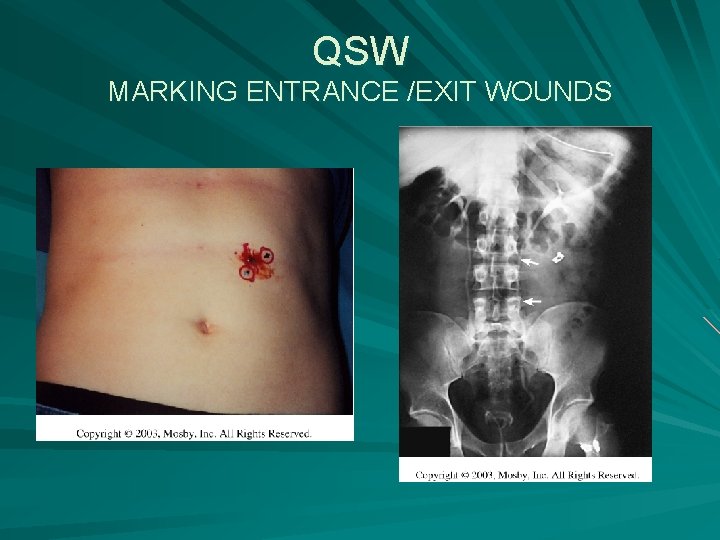
QSW MARKING ENTRANCE /EXIT WOUNDS



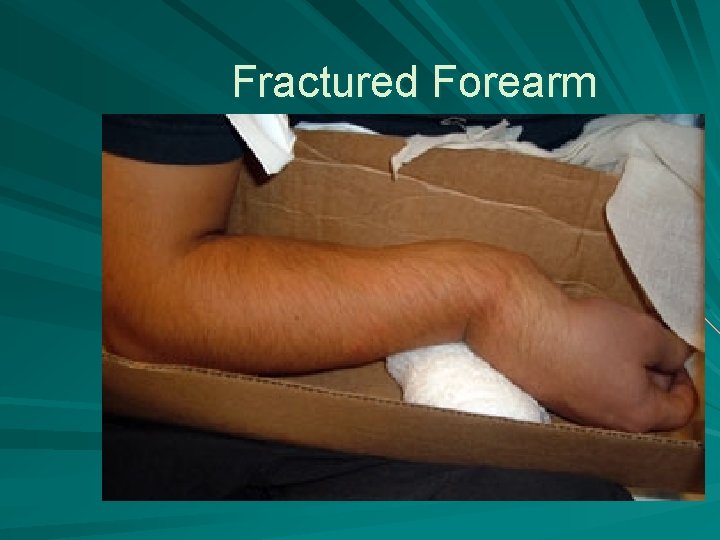
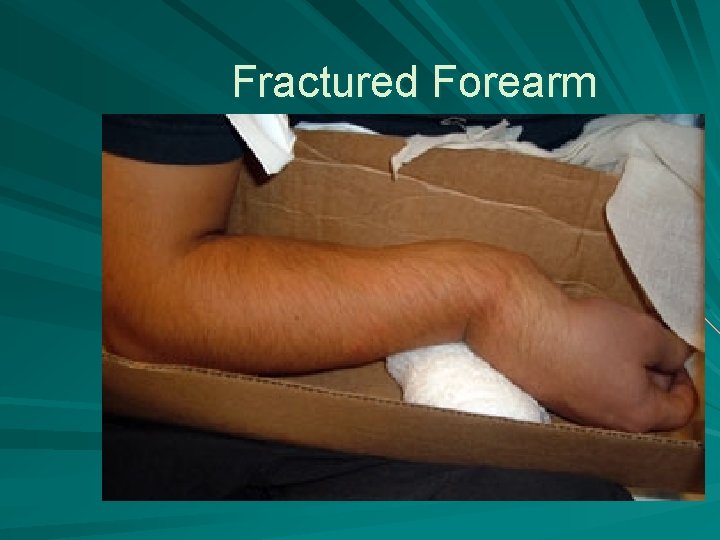
Fractured Forearm




Trauma and Surgical Radiography

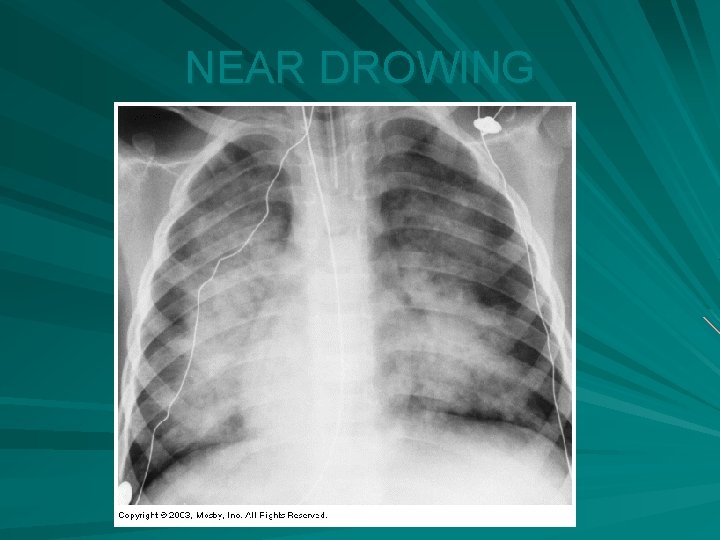
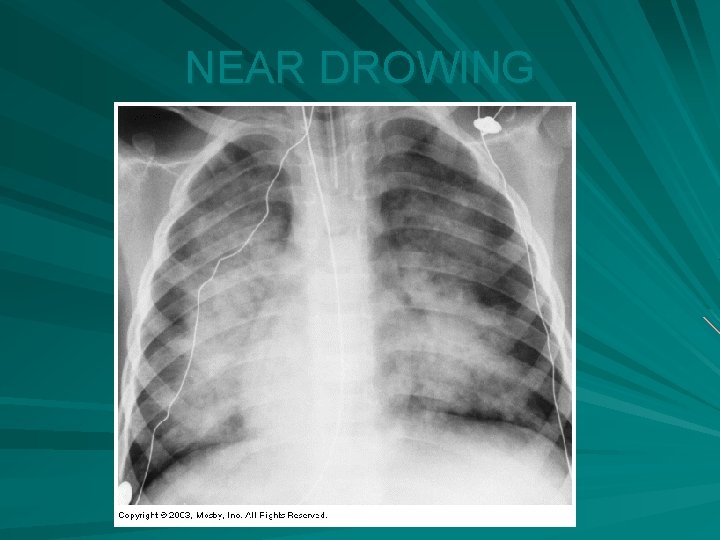
NEAR DROWING

Compound Fx of Femur




General Priorities 1. Ensure an open airway (ABC’s) 2. Control Bleeding 3. Take Measures to Prevent shock 4. Attend to wounds or fractures 5. Provide emotional support 6. Continually reevaluate and follow up

Medical Emergencies • What a Radioilogic technologist should know • Common Radiology Emergencies

Medical Emergencies Sudden change in medical status requiring immediate action. For RT’s medical emergencies are rare – Recognize emergencies – Remain calm and confident – Avoid additional harm to the patient – Obtain appropriate medical assistance quickly – Know where crash cart is, emergency phone and code blue buttons

Major Medical Emergencies 1. 2. 3. 4. 5. 6. 7. ALOC Shock Anaphylactic shock Diabetic Crisis Respiratory Distress Cardiac Arrest Cerebrovascular accident
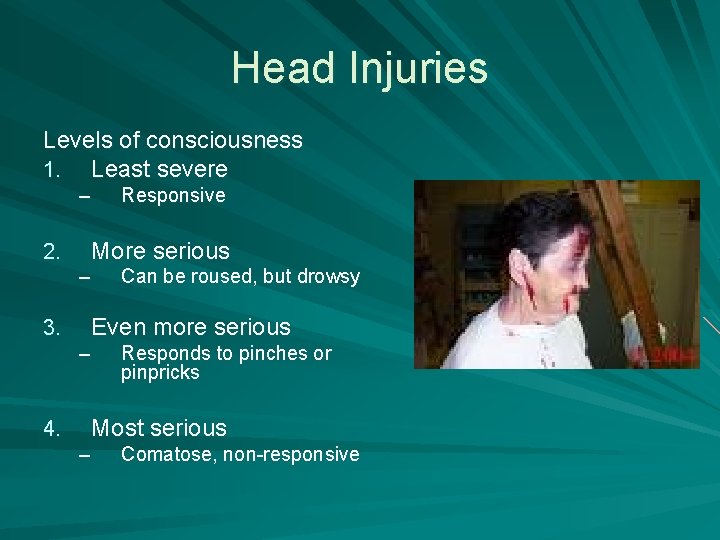
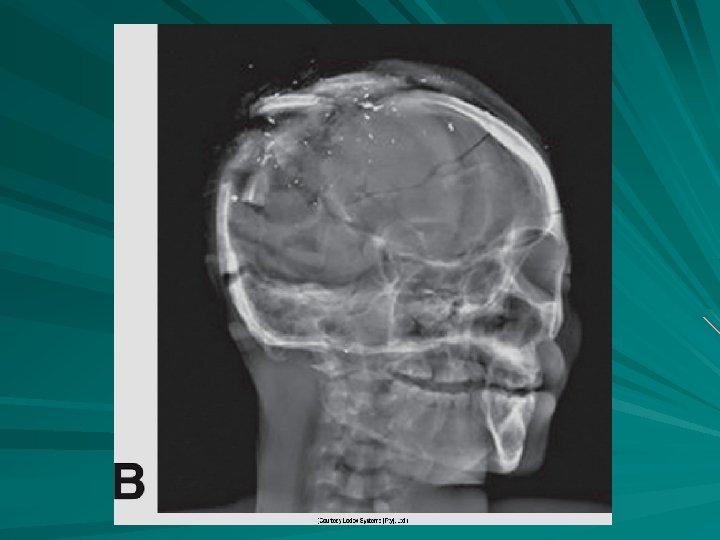
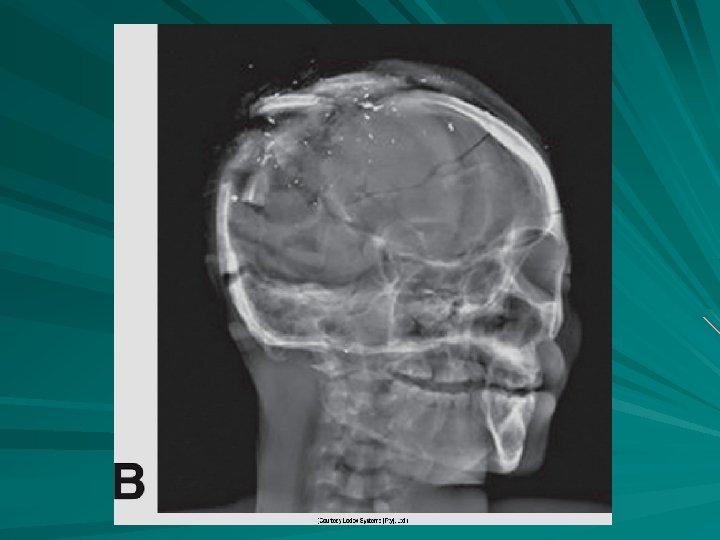
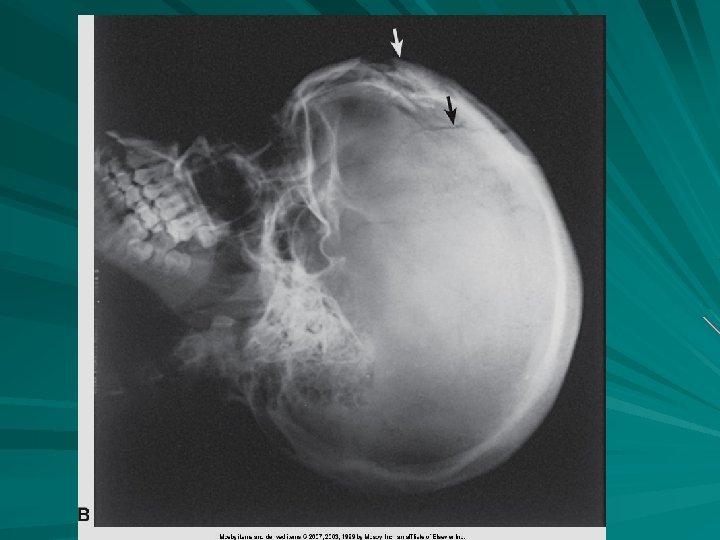
Head Injuries Levels of consciousness 1. Least severe – 2. More serious – 3. Can be roused, but drowsy Even more serious – 4. Responsive Responds to pinches or pinpricks Most serious – Comatose, non-responsive
Shock Hypovolemic – Loss of blood or tissue Cardiogenic – Cardiac disorders Neurogenic – Spinal anesthesia or damage to spinal cord Vasogenic – Caused by sepsis, deep anesthesia or anaphylaxis
Anaphylactic Shock An allergic reaction to contrast media – Iodinated Can happen quickly or have a delayed reaction – Requires prompt recognition and treatment from the technologist – More severe usually have quick onset – Less severe takes longer for reaction
Prevention and Signs - Symptoms Restlessness Maintain normal body temperature Apprehension Handle pt’s gently Tachycardia RT should work calmly and confidently Sudden blood pressure drop – Anxiety Cold –clammy skin – pallor

Diabetic Crisis 1. Hypoglycemia 2. Hyperglycemia
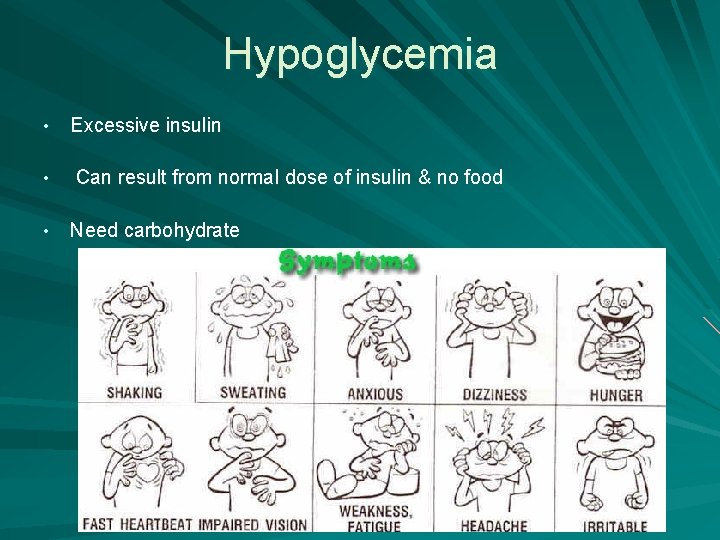
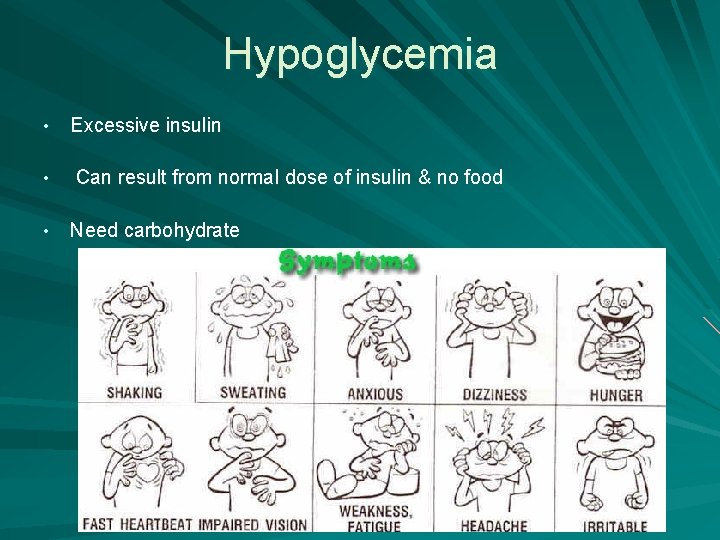
Hypoglycemia • Excessive insulin • Can result from normal dose of insulin & no food • Need carbohydrate
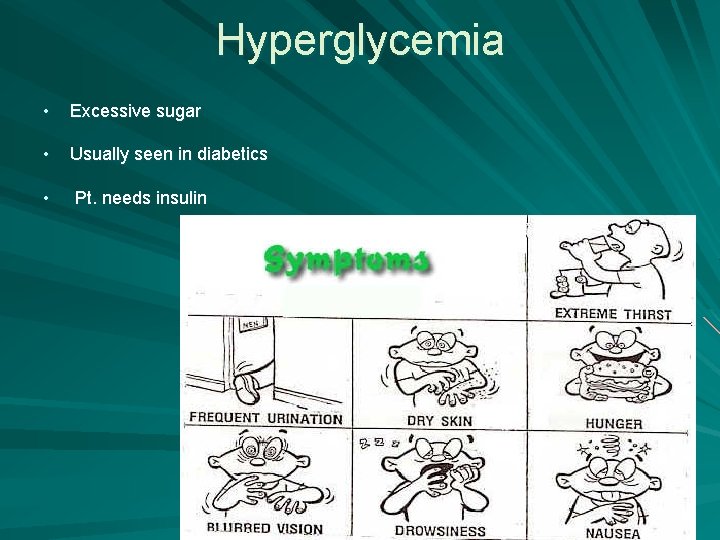
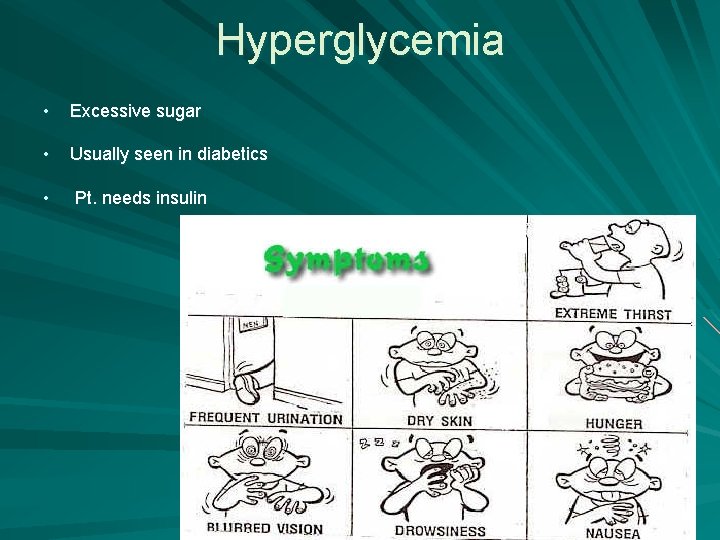
Hyperglycemia • Excessive sugar • Usually seen in diabetics • Pt. needs insulin

Respiratory Distress 1. Asthma 2. Choking
Asthma 1. Stressful situations 2. Inhaler or medical assistance 3. Remain calm and confident
Choking 1. Cannot speak 2. Universal distress signal 3. Encourage to cough 4. Heimlich Maneuver

Cardiac Arrest 1. Crushing pain in chest 2. Pain down arm 3. Begin CPR and use AED
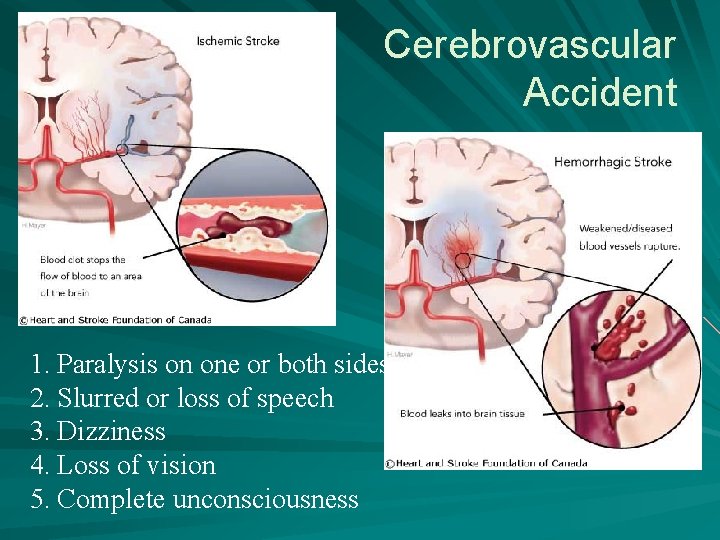
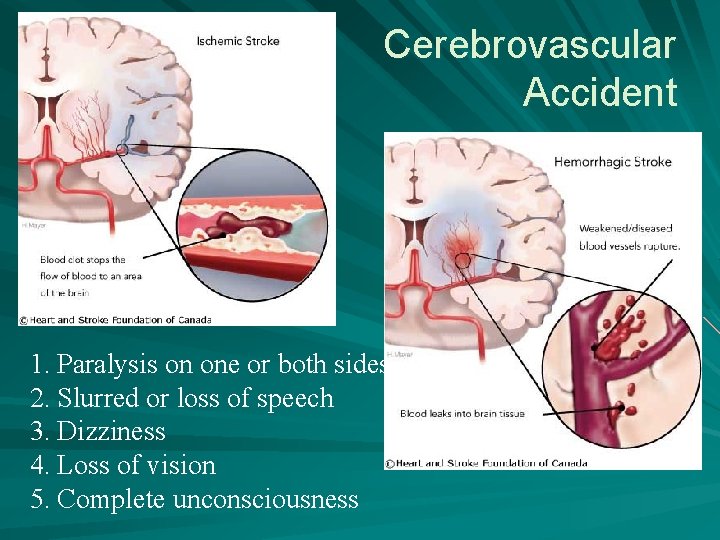
Cerebrovascular Accident 1. Paralysis on one or both sides 2. Slurred or loss of speech 3. Dizziness 4. Loss of vision 5. Complete unconsciousness
Minor Medical Emergencies 1. 2. 3. 4. 5. 6. 7. Nausea and vomiting Epistaxis Vertigo and syncope Seizures Falls Wounds Burns
Nausea and Vomiting Tell pt to breath deeply and slowly Turn on side if possible or turn head Get emesis basin and moist cloths

Epistaxis - nosebleed
Vertigo and Syncope 1. Lack of blood flow to brain 2. Feel dizzy after laying down or standing for awhile 3. Lay patient down 4. Orthostatic hypotension 5. Loosen tight clothes and put moist cloth on head
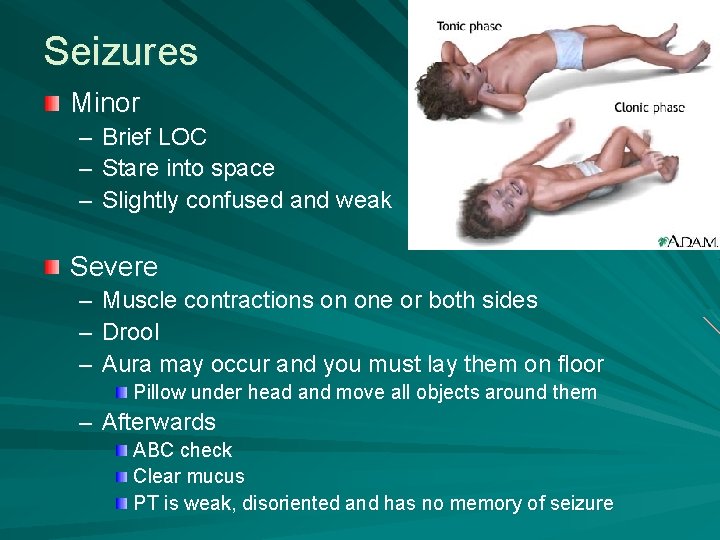
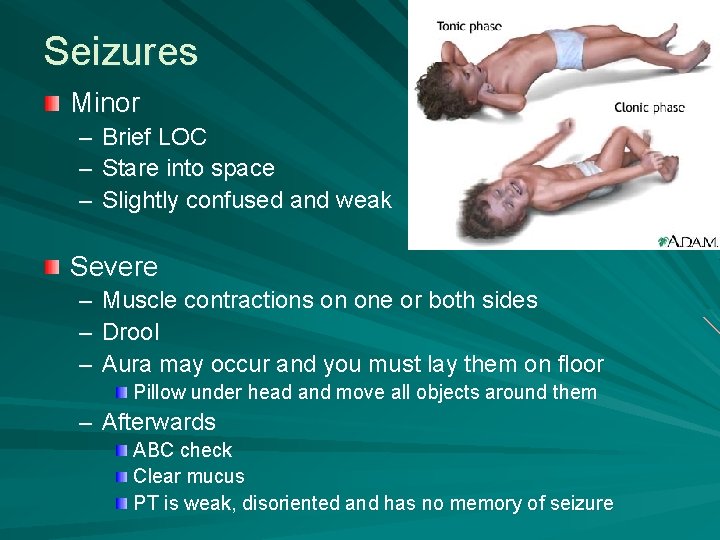
Seizures Minor – – – Brief LOC Stare into space Slightly confused and weak Severe – – – Muscle contractions on one or both sides Drool Aura may occur and you must lay them on floor Pillow under head and move all objects around them – Afterwards ABC check Clear mucus PT is weak, disoriented and has no memory of seizure

Falls, wounds and burns Falls – Get appropriate help as needed and report incident to supervisor and get a medical assessment of pt Wounds – – Do not remove dressing Pay attn to any changes in dressing Place extremity above level of heart Apply pressure Burns – Maintain sterile precautions – Be extra gentle
Radiologic Technology You never know when a medical emergency may occur. Helping your patients depends on your abilities to stay calm and perform you duties!

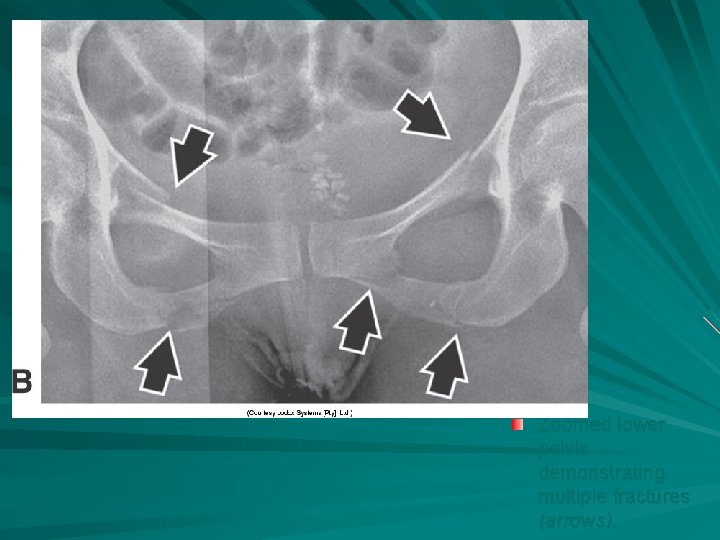
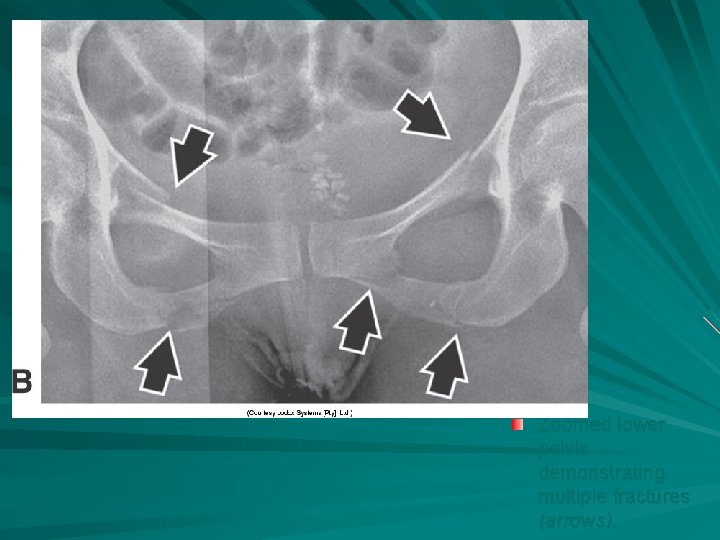
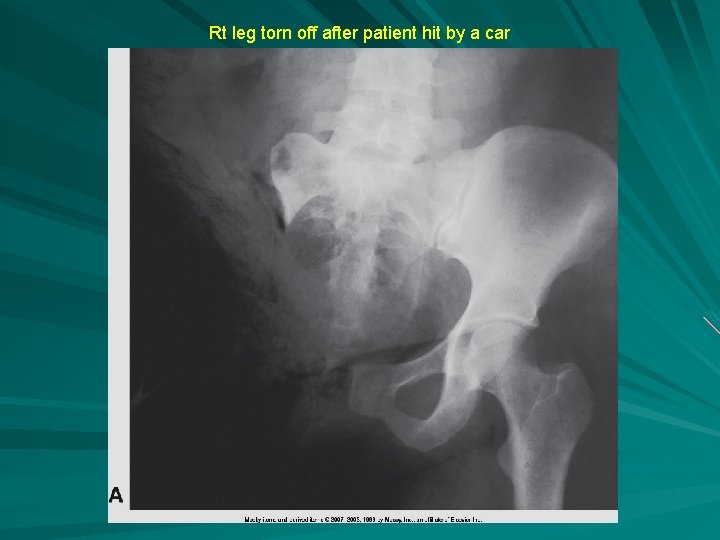
Zoomed lower pelvis demonstrating multiple fractures (arrows).
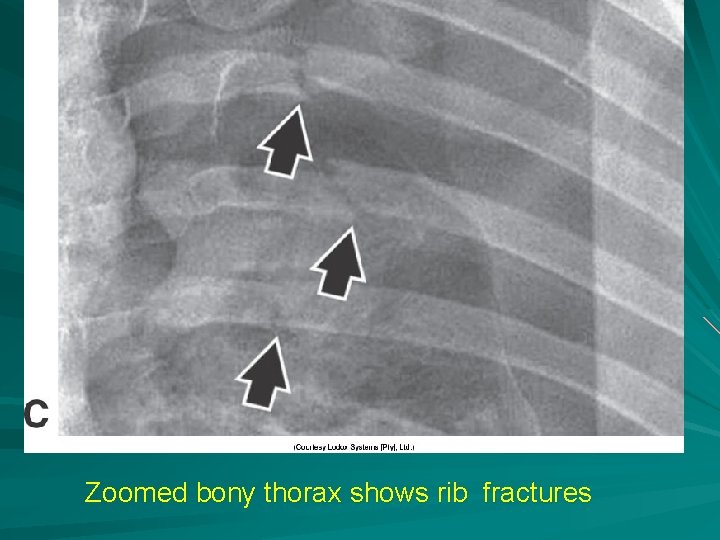
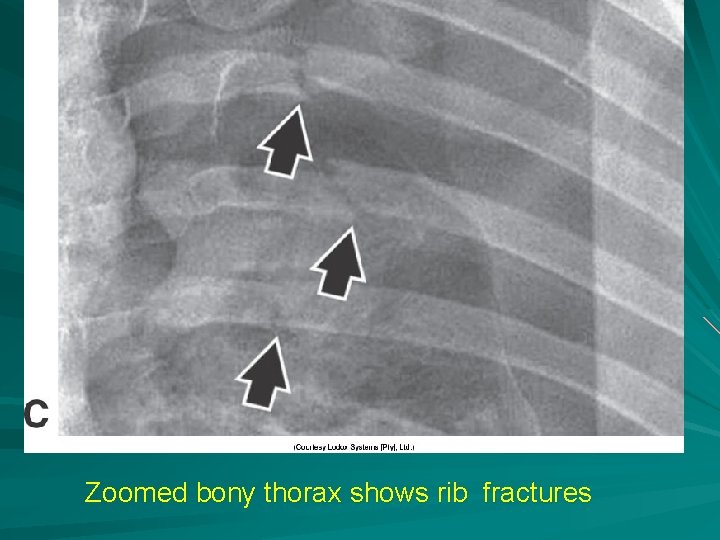
Zoomed bony thorax shows rib fractures









FX RADIAL HEAD


greenstick

comminuted Open fracture
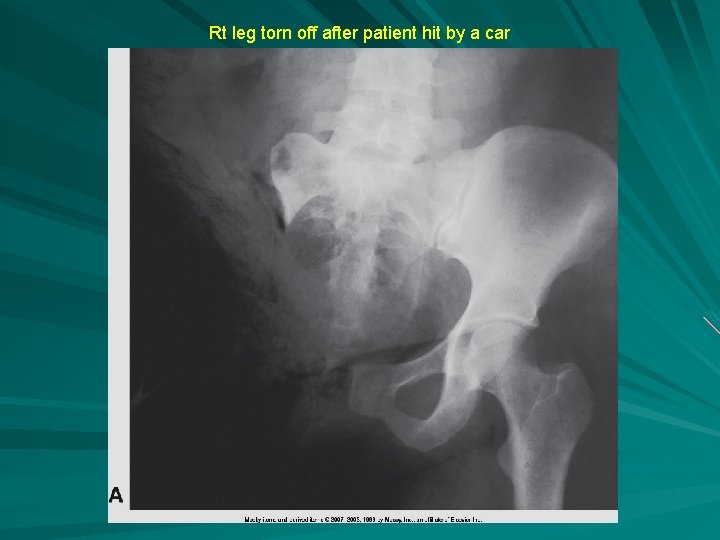
Rt leg torn off after patient hit by a car

Third Degree Burn

INFECTION CONTROL

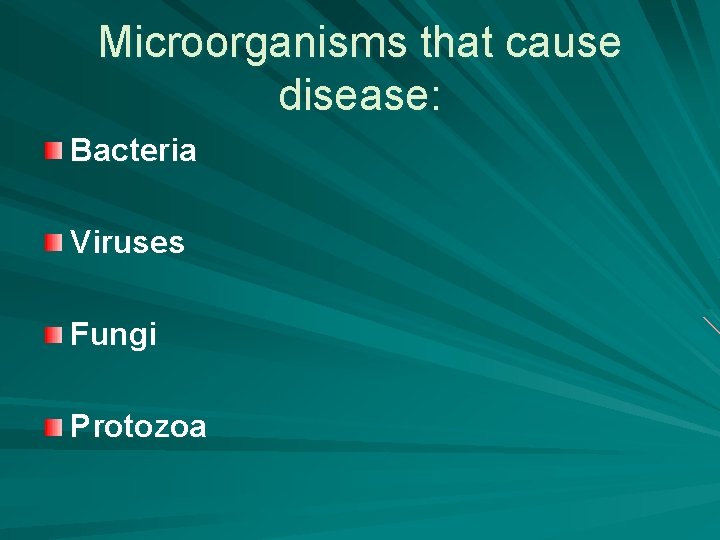
Microorganisms that cause disease: Bacteria Viruses Fungi Protozoa
Microorganisms Can grow in or on an animal or plant and cause diseases. Host: animal or plant that provides life support to another organism. Disease: Any change from the normal structure or function in the human body. Infection: Growth of a microorganism on or in a host.
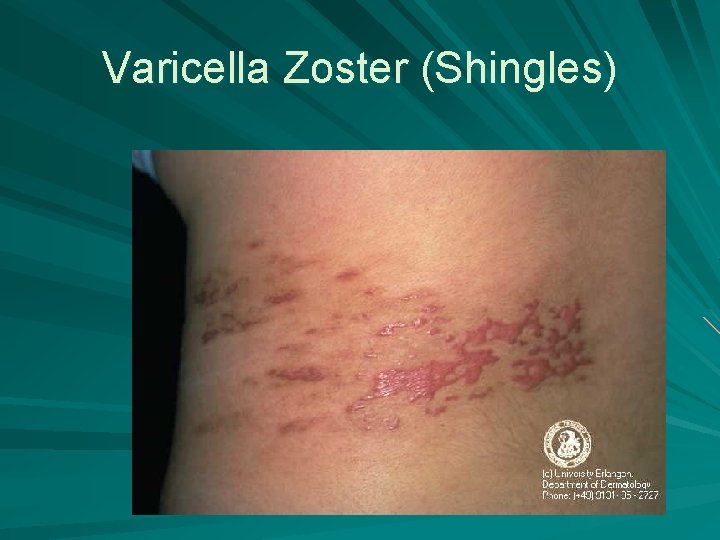
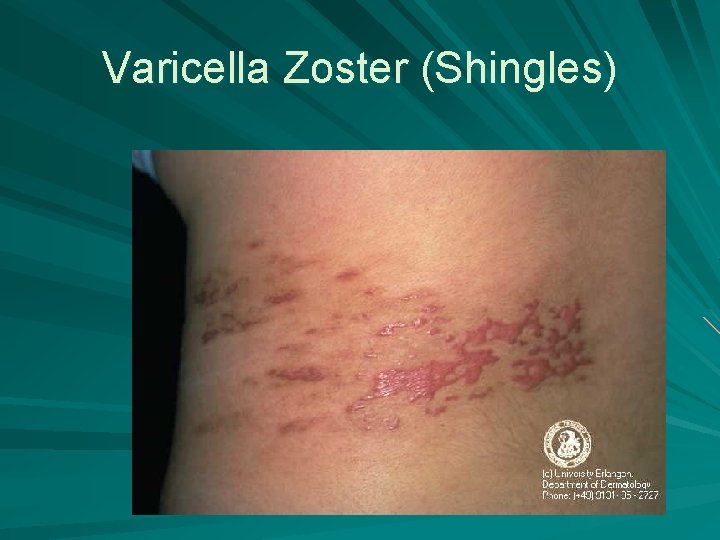
Varicella Zoster (Shingles)
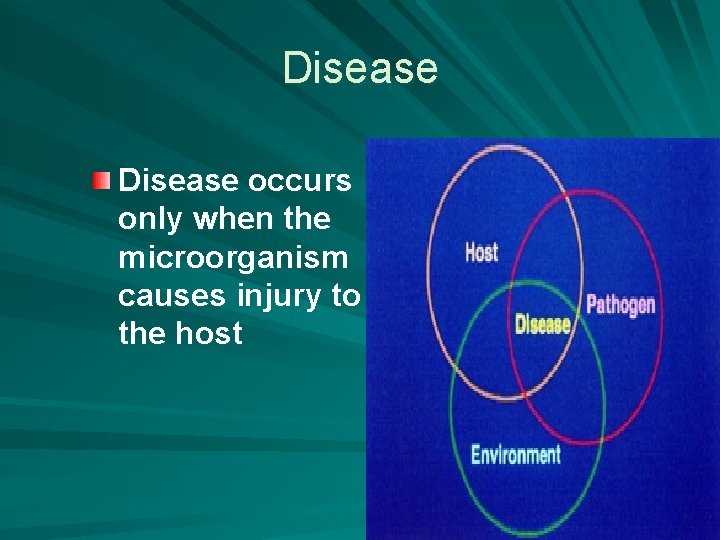
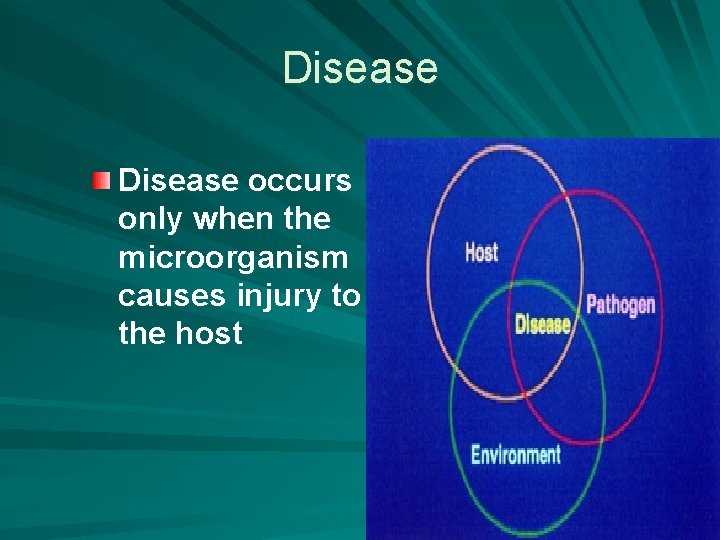
Disease occurs only when the microorganism causes injury to the host

Pathogen A disease producing microorganism. – Multiply in large numbers and cause an obstruction – Cause tissue damage – Secrete substance that produce effects in the body Exotoxins ( high body temp, nausea, vomiting)
Bacteria Strep Throat Bacterial Pneumonia Food Poisoning
Viruses Common cold Mononucleosis Warts

Oral Warts

Smallpox

Fungi Athlete’s Foot – Tinea pedis Ringworm
Protozoan Trichomonas Vaginalis – STD Plasmodium Vivax – Malaria

Chain of Infection
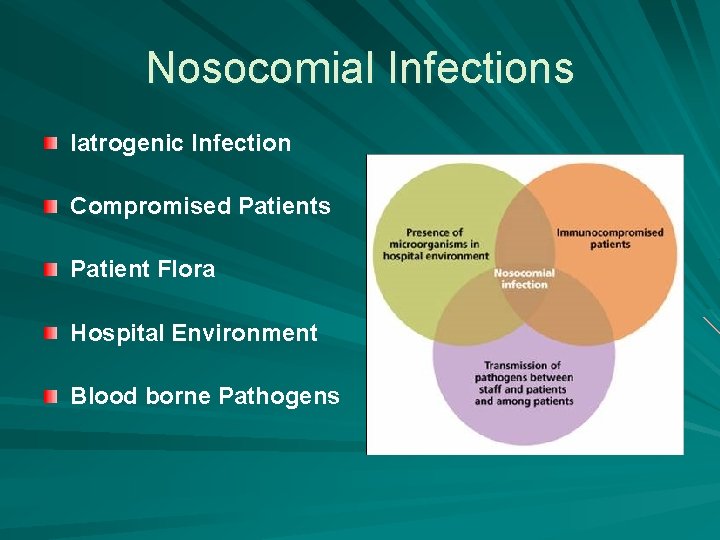
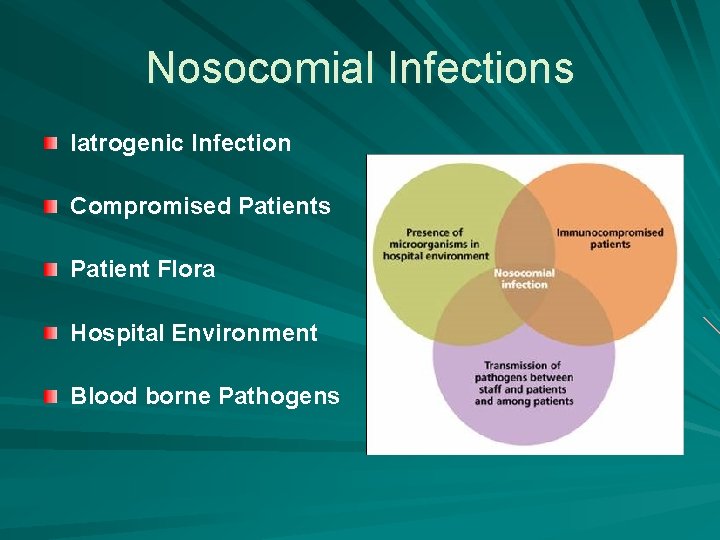
Nosocomial Infections Iatrogenic Infection Compromised Patients Patient Flora Hospital Environment Blood borne Pathogens

Types of Nosocomial Infections Iatrogenic Infection – related to physician activities Compromised Patients - weakened resistance; immunosuppressed Patient Flora - microbes in healthy people Contaminated Hospital Environment Blood borne Pathogens – Hepatitis B and HIV
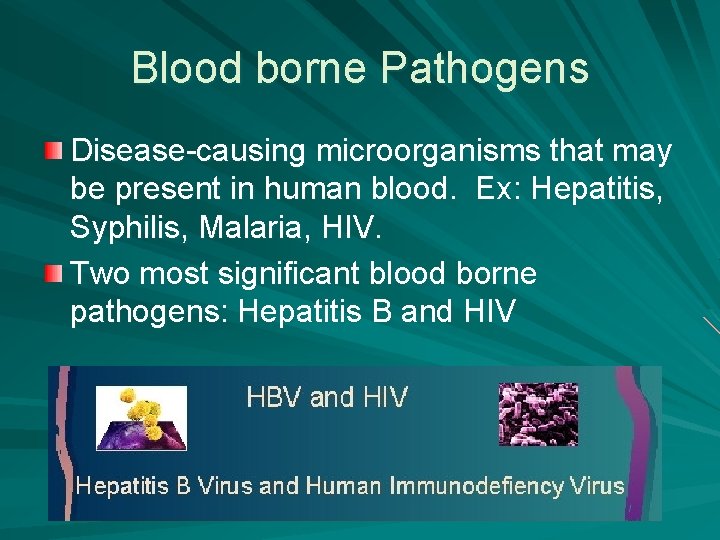
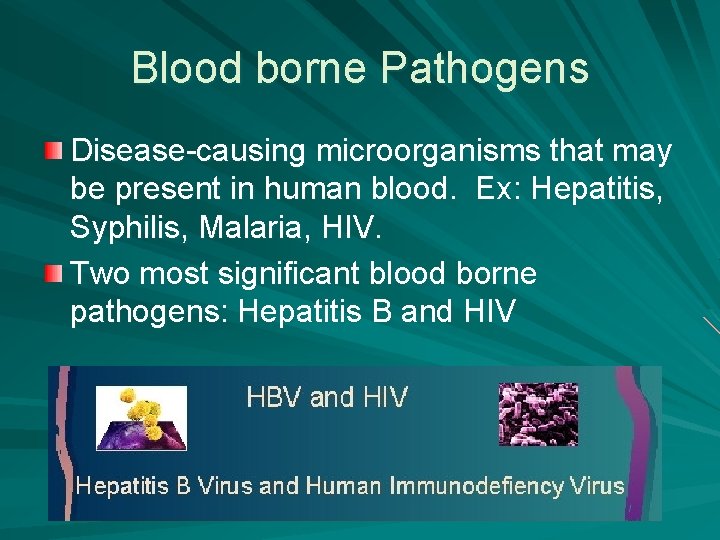
Blood borne Pathogens Disease-causing microorganisms that may be present in human blood. Ex: Hepatitis, Syphilis, Malaria, HIV. Two most significant blood borne pathogens: Hepatitis B and HIV
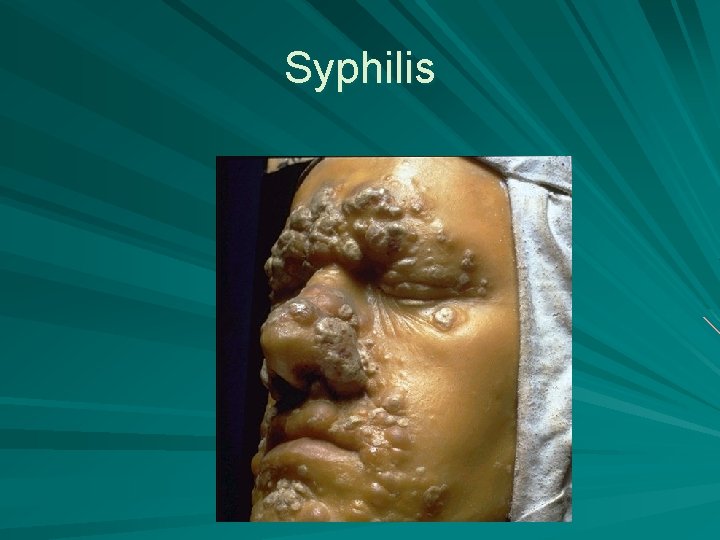
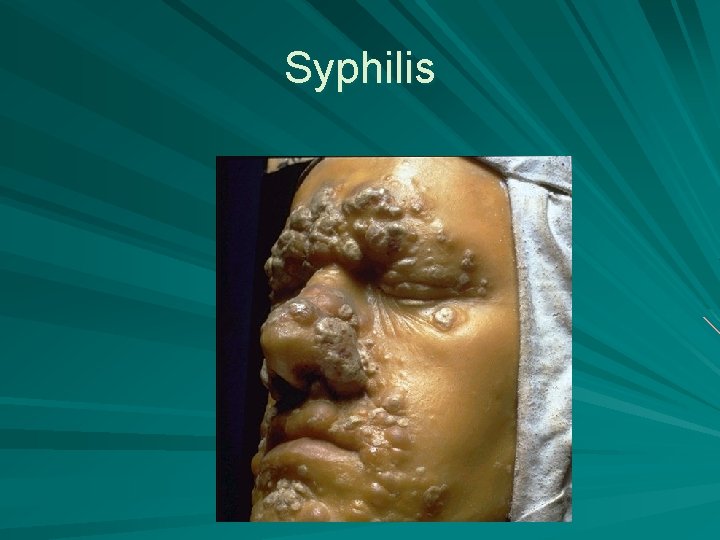
Syphilis

Syphilis in the eye
How Blood borne Pathogens are Transmitted: You must make contact with contaminated fluids and permit them a way to enter your body. Contaminated body fluids can be saliva, semen, vaginal secretions, or other fluids containing blood (urine).

Controlling the spread of Disease Chemotherapy Immunization Asepsis – Medical – Surgical Disinfectants
Physical Methods of Controlling Diseases Handwashing Standard Precautions – Gloving – Gowns – Face masks – Eyewear
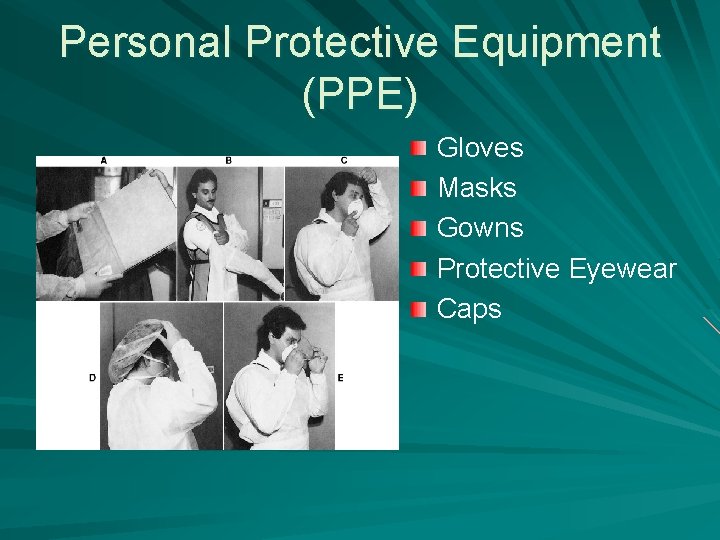
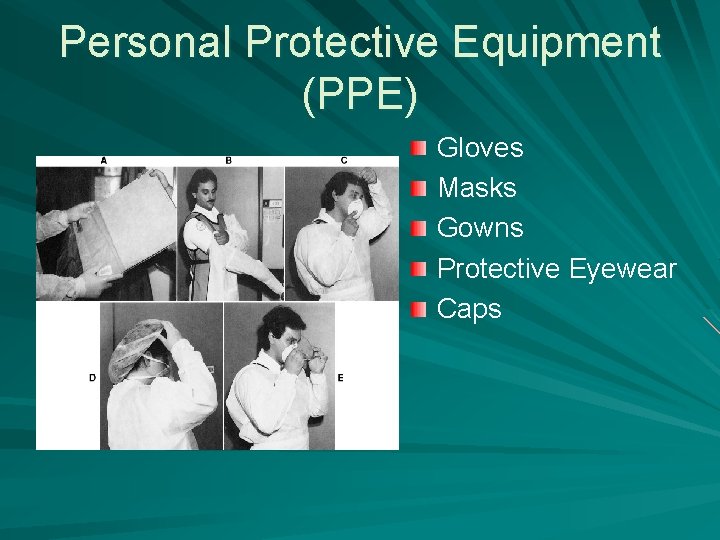
Personal Protective Equipment (PPE) Gloves Masks Gowns Protective Eyewear Caps
Universal Precautions Since there is no way you can know if a person is infected, you should ALWAYS use universal precautions: Wash your hands Wear gloves Handle sharp objects carefully Properly clean all spills Wear mask, eye protection, and apron if splashing is a possibility.
Airborne Precautions Patients infected with pathogens that remain suspended in air for long periods on aerosol droplets or dust. TB, Chickenpox, Measles Respiratory protection must be worn when entering pt room. Pt should wear mask.
Droplet Precautions Patients infected with pathogens that disseminate through large particulate droplets expelled from coughing, sneezing, or even talking. Rubella, Mumps, Influenza Surgical mask must be worn when within 3 feet of the pt. Pt should wear a mask.
Contact Precautions Patients infected with pathogens that spread by direct contact with the pt or by indirect contact with a contaminated object (bedrail, pt dressing). Methicillin-resistant staphylococcus aureus (MRSA), Hepatitis A, Varicella, Flesh-eating Virus All PPE should be used and equipment must be disinfected after use.
So What, and Who Cares? Students and Techs are challenged both physically and mentally by the microbial world. In this world of newly found, life-threatening diseases, education has become the key to survival. Health care providers must be committed to infection control so that diseases can be conquered!
 Week by week plans for documenting children's development
Week by week plans for documenting children's development 18 week patient pathway
18 week patient pathway Patient 2 patient
Patient 2 patient Unit 16 the patient's mobility transfer skills
Unit 16 the patient's mobility transfer skills 15 intrapersonal skills
15 intrapersonal skills Hard skills and soft skills
Hard skills and soft skills Skills passport
Skills passport E16 tracabilite
E16 tracabilite Chapter 8 health team communication
Chapter 8 health team communication Communication and employability
Communication and employability Tactical communications board questions
Tactical communications board questions Integrating communications assessment and tactics
Integrating communications assessment and tactics What are speaking skills
What are speaking skills What is skimming
What is skimming Download communication skills | مهارات التواصل
Download communication skills | مهارات التواصل Example of a schematic report
Example of a schematic report Types of reading skills
Types of reading skills Communication skills chapter 3
Communication skills chapter 3 Png
Png Mastering team skills and interpersonal communication
Mastering team skills and interpersonal communication Basic interpersonal communication skills
Basic interpersonal communication skills Skills for a job application
Skills for a job application Introduction to communication skills
Introduction to communication skills Communication and interpersonal skills
Communication and interpersonal skills Field diary and lab record
Field diary and lab record Written communication skills
Written communication skills Communication skills objectives
Communication skills objectives Proficient communication skills
Proficient communication skills 00107-15 basic communication skills
00107-15 basic communication skills Quotes about communication skills
Quotes about communication skills Sales communication as a collaborative process
Sales communication as a collaborative process Module 3 communication/interpersonal skills
Module 3 communication/interpersonal skills Written communication skills
Written communication skills Chapter 2 multicultural therapeutic communication
Chapter 2 multicultural therapeutic communication Communication skills definition
Communication skills definition Slidetodoc. com
Slidetodoc. com Communication and employability skills for it
Communication and employability skills for it Business communication skills ppt
Business communication skills ppt Social work communication skills
Social work communication skills Notice writing in business communication
Notice writing in business communication Mastering soft skills for workplace success
Mastering soft skills for workplace success Letter writing in communication skills
Letter writing in communication skills Responsibilities of a secretary
Responsibilities of a secretary Communication skills in architecture
Communication skills in architecture Communication skills
Communication skills Communication skills
Communication skills Module 7 basic communication skills
Module 7 basic communication skills Bad attitude examples
Bad attitude examples Define communication
Define communication Unit 1 employability skills
Unit 1 employability skills Grapevine communication
Grapevine communication Supportive
Supportive Communication skills listening speaking reading and writing
Communication skills listening speaking reading and writing Interpersonal skills in social care
Interpersonal skills in social care Interpersonal skills in business communication
Interpersonal skills in business communication Communication skills of senior high school students
Communication skills of senior high school students Chapter 8 communication skills worksheet answers
Chapter 8 communication skills worksheet answers Chapter 4 therapeutic communication skills
Chapter 4 therapeutic communication skills Interpersonal communication chapter 3
Interpersonal communication chapter 3 Objectives of listening in communication
Objectives of listening in communication Communication skills in dentistry
Communication skills in dentistry Crisis communication skills
Crisis communication skills Elon musk teamwork
Elon musk teamwork Meaning of presentation skills
Meaning of presentation skills Elements of communication process
Elements of communication process Proxemics in communication skills
Proxemics in communication skills Communication skills in public services
Communication skills in public services Reading skills in business communication
Reading skills in business communication Jesus communication skills
Jesus communication skills Effectively communicate meaning
Effectively communicate meaning Observation skills in health and social care
Observation skills in health and social care Unit 1 communication and employability skills for it
Unit 1 communication and employability skills for it 101 ways to work with communicative skills
101 ways to work with communicative skills Communication skills
Communication skills Factors which influence the medium of communication
Factors which influence the medium of communication Job skills jeopardy
Job skills jeopardy Presentation skills training st. paul, minnesota
Presentation skills training st. paul, minnesota N parallel
N parallel What is oral communication and written communication
What is oral communication and written communication Serial and parallel interface in microprocessor
Serial and parallel interface in microprocessor Types of nonverbal communication chronemics
Types of nonverbal communication chronemics Definition of oral communication
Definition of oral communication Serial communication vs parallel communication
Serial communication vs parallel communication Htcondor week
Htcondor week Htcondor vs slurm
Htcondor vs slurm Med tech week
Med tech week Dgp week 9 answers
Dgp week 9 answers The girl who sits behind rafael is a better student than i
The girl who sits behind rafael is a better student than i Compound words with pea
Compound words with pea Dgp week 16
Dgp week 16 Barbecue sentence
Barbecue sentence Dgp week 30
Dgp week 30 Dgp week 20 answers
Dgp week 20 answers Tv turn off week
Tv turn off week Remeber asl
Remeber asl What did you do last weekend essay 150 words
What did you do last weekend essay 150 words What __________ you _________ last weekend?
What __________ you _________ last weekend? Kanji days of the week
Kanji days of the week 4형식
4형식 Week names
Week names Omer meroz
Omer meroz Inductive vs deductive learning
Inductive vs deductive learning Cfnc free application week
Cfnc free application week Stem person of the week
Stem person of the week Sats week
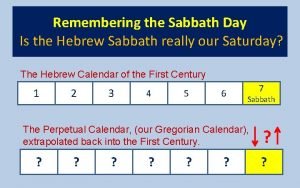
Sats week Sabbath day calendar
Sabbath day calendar Tu fais quoi le week end
Tu fais quoi le week end Proper noun of book example
Proper noun of book example Compound semiconductor week
Compound semiconductor week Chorionic villi
Chorionic villi Personal fitness merit badge answers
Personal fitness merit badge answers Did you play football yesterday in which tense
Did you play football yesterday in which tense The court will try the case next week
The court will try the case next week Passion week timeline
Passion week timeline A deli sells 640 sandwiches
A deli sells 640 sandwiches Greek or latin root/affix cruc-cross
Greek or latin root/affix cruc-cross Writing about my friend birthday party
Writing about my friend birthday party 2 week dating challenge
2 week dating challenge 40-hour work week schedule examples
40-hour work week schedule examples 1 week darkening areola early pregnancy pictures
1 week darkening areola early pregnancy pictures Hyde amendment
Hyde amendment Leestekens schema
Leestekens schema Stations of the cross holy week
Stations of the cross holy week Learning outcomes of holy week
Learning outcomes of holy week What is easter
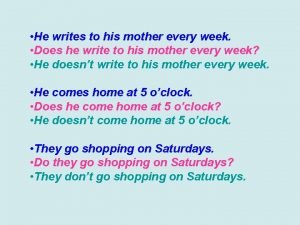
What is easter He wrote to his mother every week
He wrote to his mother every week A new nation and its growing pains
A new nation and its growing pains Greek week themes
Greek week themes Iugr causes
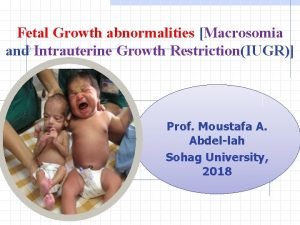
Iugr causes Latin days of the week
Latin days of the week English 4 quarter 4 week 6
English 4 quarter 4 week 6 Embedded systems week
Embedded systems week Dyslexia awareness week 2020
Dyslexia awareness week 2020 Week 14 dgp
Week 14 dgp Ensnare in a sentence
Ensnare in a sentence Creative writing week 3
Creative writing week 3 Week 1: congruence transformations
Week 1: congruence transformations Alyson klein education week
Alyson klein education week 10 hour workday schedule
10 hour workday schedule Naidoc week meaning
Naidoc week meaning Abbreviations of months of the year
Abbreviations of months of the year Stages of implantation pregnancy
Stages of implantation pregnancy Dgp week 11
Dgp week 11 Dgp week 13 answers
Dgp week 13 answers List of things a to z
List of things a to z What was the weather like yesterday?
What was the weather like yesterday? Anglo saxon days of the week
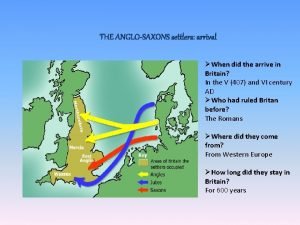
Anglo saxon days of the week Welcome to week 3
Welcome to week 3 Week 6 dgp
Week 6 dgp Dgp week 10 answers
Dgp week 10 answers Dgp week 4 answers
Dgp week 4 answers Bell ringer week 17
Bell ringer week 17 This week's lesson
This week's lesson Chapter 16-19 things fall apart
Chapter 16-19 things fall apart Week of peace things fall apart
Week of peace things fall apart Los das
Los das Cfnc free application week
Cfnc free application week Where did anglo saxons originate from
Where did anglo saxons originate from 2019 week 22
2019 week 22 Sentence of the week kelly gallagher
Sentence of the week kelly gallagher Cfnc free application week
Cfnc free application week Red ribbon week slides
Red ribbon week slides Red ribbon week 2020 ideas
Red ribbon week 2020 ideas