PREOPERATIVE AND PERIOPERATIVE ISSUES IN THE ELDERLY AGS




- Slides: 66
PREOPERATIVE AND PERIOPERATIVE ISSUES IN THE ELDERLY AGS Sarah M. Mc. Gee, MD, MPH Director of Education Division of Geriatrics November 7, 2008 August 5, 2009 THE AMERICAN GERIATRICS SOCIETY Geriatrics Health Professionals. Leading change. Improving care for older adults.
SOME OF THE FACTS • • Increasing numbers of older adults are having surgery Half of elderly will require surgery at least once Elective surgery has become more common Severity of initial presentation of surgical problem is increased in older adults Emergent surgery is more common in older adults Older adults are more likely than younger patients to have surgery cancelled or postponed because of comorbid conditions Post-op mortality for ages 85+ is twice that for ages 65 69 Slide 2
WHY IS IT IMPORTANT TO EVALUATE PERIOPERATIVE RISK? • Careful and thorough preoperative assessment should help with anticipation, recognition, and management of postoperative issues • Physiological changes associated with normal aging, superimposed upon pre-existing comorbidities, place the older adult at higher risk for complications compared with younger patients Slide 3
PHYSIOLOGICAL CHANGES WITH NORMAL AGING • Decreased functional reserve physiologic decrease in vital organ function Ø Cardiac Ø Pulmonary Ø Renal • Pharmacokinetics affected • Decreased ability to deal with perioperative physiological stress Slide 4
FACTORS THAT AFFECT RECOGNITION OF DISEASE IN OLDER ADULTS • Underreporting of symptoms • Decreased physical activity • Increased prevalence of atypical presentations • Increased prevalence of silent ischemia Slide 5
CASE (1 of 3) • An 84 -year-old man with mild dementia, living at an assisted care facility, is found on the floor complaining of severe left hip and groin pain • Has been able to ambulate independently but is physically inactive • Needs min assistance with ADLs • In the ED is found to have an intertrochanteric hip fracture • Past medical history: CAD with CABG 15 years prior, HTN, CRI, and dementia Slide 6
CASE (2 of 3) • The orthopedic service requests preoperative clearance and co-management by the medical service • Despite his mild dementia, the patient is felt to be competent • He wishes to proceed with surgery and signs the consent form Slide 7
CASE (3 of 3) • Although the patient had CABG years ago: Ø Ø • • No recent chest pain No syncope No SOB, DOE or PND No evidence of CHF on exam Exercise tolerance is poor by report Baseline creatinine is 2. 2 Albumin is 2. 8 Does he need further cardiac testing? Should surgery be delayed? What are some possible predictors of negative outcome? Slide 8
PREOPERATIVE ASSESSMENT: COMPLETE MEDICAL HISTORY • Medical problems • Past surgical history, including any post-op problems, especially delirium • Medications • Allergies/intolerances to pain medication • Baseline functional status Slide 9
OTHER PREOPERATIVE FACTORS TO CONSIDER • Prior functional status • Dementia • Nutritional status Ø Significant predictor of 30 -day mortality Ø Marker for frailty Slide 10
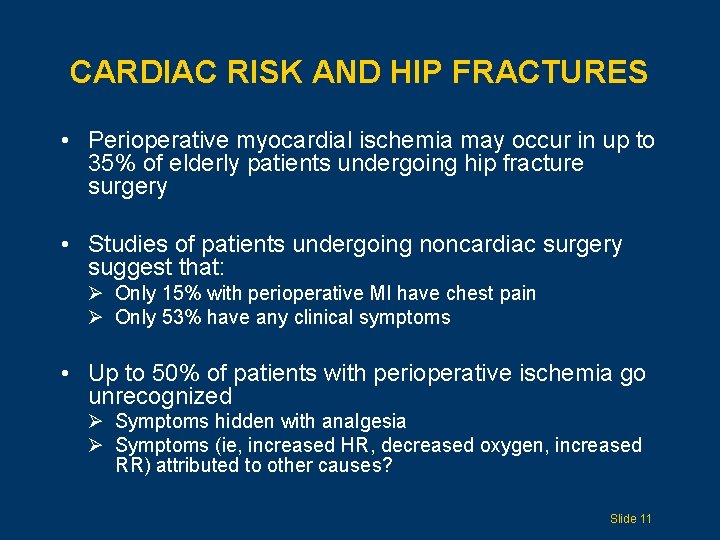
CARDIAC RISK AND HIP FRACTURES • Perioperative myocardial ischemia may occur in up to 35% of elderly patients undergoing hip fracture surgery • Studies of patients undergoing noncardiac surgery suggest that: Ø Only 15% with perioperative MI have chest pain Ø Only 53% have any clinical symptoms • Up to 50% of patients with perioperative ischemia go unrecognized Ø Symptoms hidden with analgesia Ø Symptoms (ie, increased HR, decreased oxygen, increased RR) attributed to other causes? Slide 11
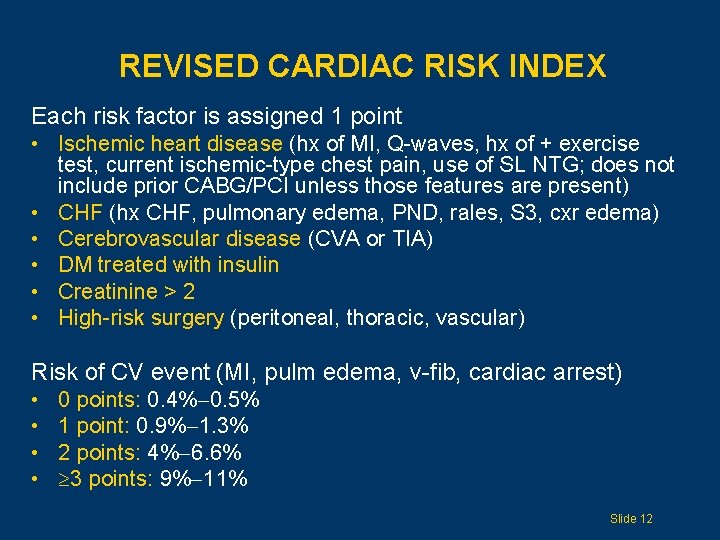
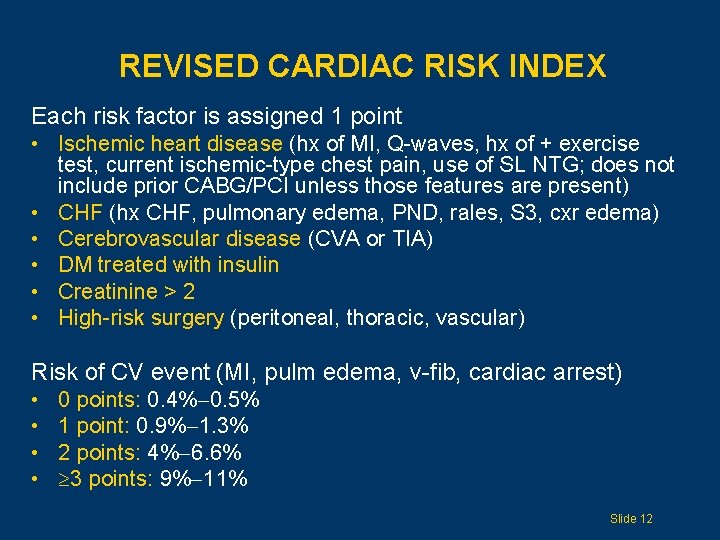
REVISED CARDIAC RISK INDEX Each risk factor is assigned 1 point • Ischemic heart disease (hx of MI, Q-waves, hx of + exercise test, current ischemic-type chest pain, use of SL NTG; does not include prior CABG/PCI unless those features are present) • CHF (hx CHF, pulmonary edema, PND, rales, S 3, cxr edema) • Cerebrovascular disease (CVA or TIA) • DM treated with insulin • Creatinine > 2 • High-risk surgery (peritoneal, thoracic, vascular) Risk of CV event (MI, pulm edema, v-fib, cardiac arrest) • • 0 points: 0. 4% 0. 5% 1 point: 0. 9% 1. 3% 2 points: 4% 6. 6% 3 points: 9% 11% Slide 12
PREOP CARDIAC TESTING Big question: Will results of test change management? Slide 13
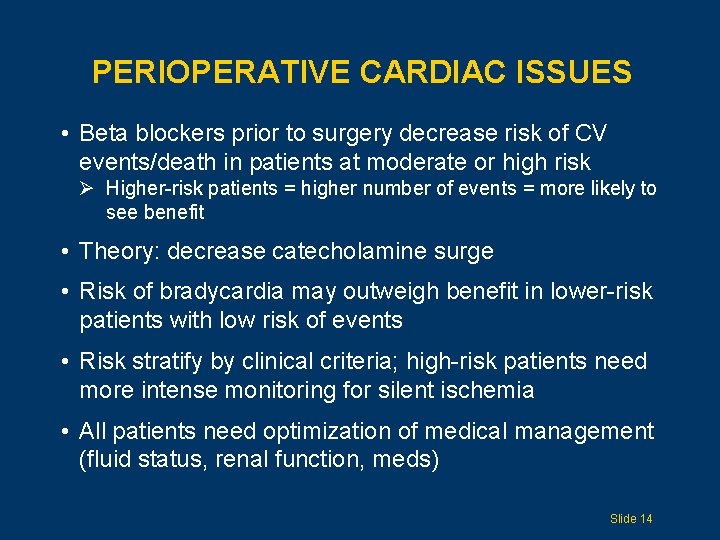
PERIOPERATIVE CARDIAC ISSUES • Beta blockers prior to surgery decrease risk of CV events/death in patients at moderate or high risk Ø Higher-risk patients = higher number of events = more likely to see benefit • Theory: decrease catecholamine surge • Risk of bradycardia may outweigh benefit in lower-risk patients with low risk of events • Risk stratify by clinical criteria; high-risk patients need more intense monitoring for silent ischemia • All patients need optimization of medical management (fluid status, renal function, meds) Slide 14
WHAT ABOUT STATINS? • In retrospective trials, use of statins was associated with decrease in perioperative CV events • Small randomized, controlled trial with 100 patients Ø Atorvastatin vs placebo prior to major vascular surgery (14 days prior, continued for 45 days after) Ø Combined outcome of CV death/MI/stroke found in 8% of patients with treatment, 26% of patients with placebo • May be of benefit • Benefit not clear during urgent procedures Slide 15
PREOPERATIVE MANAGEMENT: DIABETES • Metabolic control • Hyperglycemia without prior diagnosis of DM in elderly with acute event = bad predictor • Discontinue oral agents initially • May need to cover with insulin; usually will need some amount of baseline insulin to avoid extreme fluctuations Slide 16
OTHER PREOPERATIVE NEEDS • Review and discontinue medications that are not needed/potentially harmful • Be attentive to medications that need to be restarted postoperatively (eg, antidepressants, antihypertensives) • Watch for medications that may cause problems during withdrawal (eg, benzodiazepines, SSRIs) • Think about possible alcohol and smoking withdrawal Slide 17
TIMING OF SURGERY • Several studies show that early surgery (first 24 48 hours after fracture) is associated with decreased mortality, pressure ulcers, delirium • General consensus: the earlier the better, once stable Slide 18
PREVENTION OF DVT AND PE Clear guidelines from 7 th Conference on Antithrombotic and Thrombolytic Therapy, 2004 • Hip fracture patients are at high risk of VTE Ø Risk of DVT is 50% without prophylaxis Ø Risk of proximal DVT is 27% Ø Risk of fatal PE is 1. 4% 7. 5% • Factors that increase risk of VTE: advanced age, delayed surgery, general anesthesia Slide 19
SUMMARY OF VTE PREVENTION GUIDELINES • Routine use of low-molecular-weight heparin • Can use warfarin (INR 2 3) • ASA alone is not sufficient • Continue anticoagulation for at least 28 35 days after surgery, possibly longer Slide 20
CONSIDER THE CASE AGAIN • What analgesia should the patient be given? • Should he be monitored for a perioperative cardiac event? • What is his risk of delirium? How can this be prevented or managed? • What other complications is he at risk of developing? • What would be an appropriate level of discharge care? Slide 21
POSTOPERATIVE COMPLICATIONS Although patients and families worry about intraoperative complications and death, the vast majority of adverse events occur in the postoperative period Slide 22
POSTOPERATIVE ANALGESIA Epidural vs PCA vs intermittent administered morphine: • No clear sweeping differences • Some data indicate that epidural route may provide better pain relief; no clear difference in time to recover physical independence • Elderly patients with dementia or delirium may have difficulty with PCA Slide 23
PAIN ASSESSMENT • Should be based on patient’s perception of pain (pain scale) • May be difficult in very demented patients, although direct questioning may still work • Nonverbal cues: agitation, tachycardia, facial expressions Slide 24
PAIN MANAGEMENT • Consider nonpharmacologic treatments • Use scheduled dosing of pharmacologic agents • When adding pharmacologic agents, choose those with the fewest side effects Ø Morphine is most predictable and probably less likely than other agents to increase confusion Ø Avoid propoxyphene, meperidine • Use PRN dosing for breakthrough pain • Reevaluate pain control regimen frequently Slide 25

PAIN RELIEF PYRAMID NARCOTICS ACETAMINOPHEN NONPHARMACOLOGIC Slide 26
NONPHARMACOLOGIC OPTIONS Temperature Education • Cold for acute pain • Heat/cold for chronic pain • To reduce fears, explain cause or mechanism of pain • Engage cooperation and “partner” in management Positioning Physical therapy • Use early Relaxation techniques Biofeedback Massage • Engage nursing, family Slide 27
ACETAMINOPHEN • P. O. 650 1000 mg QID (or Tylenol ER: 2 gelcaps, 650 mg each, q 8 h) • Compatible with NSAIDs and opiates • Keep total dose less than 4 g/24 hours • Patients on scheduled dose of acetaminophen must avoid acetaminophen/narcotic combinations (eg, Vicodin is hydrocodone with acetaminophen) Slide 28
CONSTIPATION: PREDISPOSING FACTORS • • • Prior history Bed rest/inactivity Change in diet Narcotics Diminished fluid intake Slide 29
CONSTIPATION: PREVENTION When prescribing narcotics for the elderly: • Order scheduled and PRN bowel hygiene • Stool softeners are usually not enough • Consider: Ø Senna beginning at 1 2 tablets per day Ø Miralax Slide 30
POSTOPERATIVE CARDIAC RISK • Elderly patients undergoing emergent/urgent hip fracture surgery are at high risk of CV event • 50% of ischemic events in the postoperative period are silent • Highest risk is within first 3 days after fracture Slide 31
POSTOPERATIVE CARDIAC SURVEILLANCE • Have a high index of suspicion • Consider CK-MB and troponin testing, as well as surveillance EKG, immediately postoperatively on all hip fracture patients • Continue monitoring if any changes seen • Continue to optimize medical treatment (ie, statin, ASA, beta-blocker, fluid status) Slide 32
POSTOPERATIVE ISSUES: GENITOURINARY • Overall incidence of UTI after hip fracture: 25% • Best to remove Foley catheter as soon as possible • May be complicated if patient receiving epidural anesthesia • Urinary retention Ø Straight catheterizations restore bladder function earlier Ø D/C medications that can increase retention (sedatives, anticholinergics) Slide 33
POSTOPERATIVE ISSUES: PULMONARY • Pneumonia Ø Accounts for 25% 50% of all hospital deaths after hip fracture surgery Ø Significant cause of later deaths (after hospital discharge) after hip fracture surgery Ø Risk may be decreased with regional anesthesia, early weight bearing, pulmonary hygiene, incentive spirometry • Pulmonary embolism causes 15% of deaths after hip fracture surgery Slide 34
POSTOPERATIVE DELIRIUM • Most common medical complication following hip fracture • Marker of bad outcome Ø Ø Increased mortality (25% 33%) Increased risk of needing skilled nursing facility Increased length of hospital stay Interferes with rehab and functional status recovery • Goes unrecognized 30% 50% of the time • Prevention is key Ø Multiple studies demonstrate targeted interventions significantly prevent delirium, but have no significant impact once delirium develops Slide 35
DELIRIUM: PATIENT-RELATED RISK FACTORS • • Advanced age Underlying cognitive impairment Prior delirium Alcohol abuse Malnutrition Depression Type of surgery Ø Hip fracture surgery: 30% risk Slide 36
DELIRIUM: IATROGENIC RISK FACTORS • Conventional restraints • Other restraints/tethers: Ø Oxygen tubing Ø Telemetry boxes Ø IV lines • • • Medications Poor pain control Foley catheters Environmental: noise, disturbance of sleep Lack of hearing and visual aids Slide 37
DELIRIUM: HIGH-RISK MEDICATIONS • • • Anticholinergics Antipsychotics Antibiotics such as quinolones H 2 blockers, especially cimetidine Narcotics Sleep aids/sedatives Slide 38
DELIRIUM: PREVENTION • • • Identify high-risk patients Confusion Assessment Method (next slide) Decrease sleep interruptions, improve environment Family, orientation, sitter if needed Avoid restraints and tethers Avoid polypharmacy, no anticholinergics (no Benadryl) Monitor for ischemia, oxygen status, infection Remove Foley catheter ASAP Provide adequate analgesia Provide adequate bowel regimen Monitor for urinary retention, I/O catheters when needed Slide 39
DIAGNOSING DELIRIUM: CONFUSION ASSESSMENT METHOD Acute onset and fluctuating course plus Inattention and one of the following: Disorganized thinking Altered level of consciousness Slide 40
DELIRIUM: MANAGEMENT • Search for predisposing factors • Reevaluate medications • Avoid benzodiazepines (eg, lorazepam) Slide 41
DELIRIUM AND ANTIPSYCHOTICS • No data that antipsychotics improve outcomes; they probably just make delirious patients more sedated • Not approved for this indication • Increased use of atypical antipsychotic agents for management of patients with delirium • Agents and dosing in older patients Ø Haldol 0. 25 0. 5 mg starting dose Ø Risperidone 0. 25 0. 5 mg starting dose Slide 42
DELIRIUM AND ANTIPSYCHOTICS: THE DOWNSIDES • Side effects Ø Ø Ø Sedation Orthostasis Increased delirium CV risks, QT interval prolongation Edema • FDA black-box warning, April 2005 Ø Observation in multiple studies of increased risk of sudden death and stroke in elderly patients Slide 43
OTHER COMPLICATIONS: MALNUTRITION • Poor nutritional status is independently associated with increased morbidity and mortality • Enteral supplements may decrease postoperative complications, length of hospital stay • Postoperative parenteral nutrition: increased complications in elderly Slide 44
OTHER COMPLICATIONS: PRESSURE SORES • Incidence after hip fracture surgery 10% 40% • Risk decreases with: Ø Ø Frequent turning Early out-of-bed status Weight bearing as tolerated Removal of Foley catheter and other lines Slide 45
OTHER COMPLICATIONS: ANEMIA • Anemia and worsening anemia are common in ill elderly and during postoperative period • There is evidence that liberal transfusion to keep Hgb at 10 12 may worsen outcome • Data unclear in elderly in postoperative period Ø May not tolerate as low a Hgb Ø Lower Hgb is associated with worse outcome, but not clear whether the association is causal Slide 46
TRANSFUSION GUIDELINES Recommend moderately restrictive transfusion guidelines: • Keep Hgb at 7 9, likely closer to 8 9 range, especially if underlying myocardial ischemia • No real evidence to support keeping Hbg over 10 Slide 47
POSSIBLE HOSPITAL COURSE 1 • A post-op patient receives PRN analgesia • Because he is restless and physically agitated, trying to get out of bed and pull out his Foley, he is restrained and given 5 mg Haldol • He develops a fever and hematuria and is started on an oral antibiotic for UTI • He develops diarrhea and sacral breakdown • PO intake declines and he is unable to participate in rehab Slide 48
POSSIBLE HOSPITAL COURSE 2 • A post-op patient receives scheduled and PRN morphine on POD 1 and 2 • Analgesia is changed to scheduled Vicodin on POD 3 • The Foley is removed on POD 2 • Though the patient is more confused than at baseline, according to his family, he is able to participate actively in rehab and is able to be discharged to subacute care on POD #4 Slide 49
DISCHARGE PLANNING • Rehab possible at multiple sites • No clear benefit to one over another Ø Home Ø Inpatient rehab Ø Subacute rehab/skilled nursing facility Slide 50
PREDICTORS OF DISCHARGE TO INSTITUTION • • Age > 85 Inability to ambulate Dementia Inability to transfer Fecal incontinence Pressure sores Poor social support Slide 51
TRANSITIONS CAN BE DANGEROUS Guard against incomplete transfer of information • Discharge summaries and PDI need to be consistent and complete • Include most recent events, labs, and meds • Be especially cautious if facilities do not have the same computer system We are on the same team! Slide 52
ADDITIONAL CONSIDERATIONS AT THE TIME OF DISCHARGE • Treatment of osteoporosis • Prevention of fall-related injuries Slide 53
RISK OF OSTEOPOROSIS • 70% patients over age 80 have osteoporosis • Hip fracture without major trauma: diagnosis of osteoporosis • More than BMD: older patient is more likely to have fracture than younger patient with same BMD (falls risk, brittle bones, cognition, visual impairment, etiology of fall, etc) Slide 54
OSTEOPOROSIS: TREATMENT AT DISCHARGE • 5% 6% patients admitted with hip fracture adequately treated for osteoporosis at discharge Ø Only 12% at 5 years Ø Only 20% have any prescription treatment over 2 years • Patients over age 74 (at highest risk) are least likely to receive treatment • Discharge medications carry weight! • No significant contraindication in most to treating at time of discharge Slide 55
OSTEOPOROSIS: SUPPLEMENTS • Calcium Ø Fewer than half of adults take adequate amount Ø 1200 1500 mg/day Ø Calcium and Vitamin D decrease risk of hip fracture • Vitamin D Ø 400 800 IU/day Ø Frail older patients with limited sun exposure may need at least 800 IU/day Ø Concern that many elders and institutionalized adults are at risk of Vitamin D deficiency; most frail adults need calcium and Vitamin D supplements Slide 56
OSTEOPOROSIS: BISPHONATES • • • Decrease bone resorption Decrease in hip and vertebral fractures Alendronate, risedronate Ibandronate (Boniva): once monthly Those at highest risk of fracture shown to have greatest benefit Slide 57

PREVENTION OF FALLS • • • Home assessment Rehab Strengthening and gait assessment Assistive devices Cognitive assessment Urinary incontinence Medication review Peripheral neuropathy Visual impairment Alcohol use Prior falls: fear of falling cycle Slide 58
RISK FACTORS FOR HIP FRACTURE • • • Age over 65 Any prior fracture Benzodiazepine/anticonvulsant use High resting heart rate Inability to rise from chair without using arms Low weight Not walking for exercise Poor depth perception/vision Poor health perception Slide 59
FRACTURE REDUCTION: HIP PROTECTORS • Used most often in long-term-care settings with at-risk elders • Multiple barriers: Ø Ø Patient concern Forgetting to put them on Incontinence Questionable efficacy Slide 60
SUMMARY (1 of 2) • Preoperative assessment: cardiac risk assessment, capacity, delirium risk, nutritional and functional assessment • Noninvasive testing for cardiac assessment usually not needed except for high-risk patients • Surgery should proceed as quickly as possible (24 48 hr) • Perioperative beta-blockers, beginning prior to surgery, are reasonable in patients at moderate or high risk • Treat pain aggressively with scheduled analgesics and reassess frequently Slide 61
SUMMARY (2 of 2) • Postoperative care: weight bearing as tolerated immediately, removal of Foley catheter after 24 hours, I/O catheter for urinary retention, prevention of pressure sores, removal of lines/boxes as soon as possible, surveillance for pulmonary cardiac issues • Watch for delirium; avoid medications such as anticholinergic agents; try to avoid restraints and antipsychotics • Transfuse if unstable, cardiac ischemia, or Hgb < 7 9 range • Discontinue all unnecessary medications; stop meds that increase risk of falls • Follow nutritional status and use supplements • Treat underlying osteoporosis aggressively: calcium, Vitamin D, consider bisphonate • Take steps to reduce the risk of falls Slide 62
REFERENCES (1 of 3) • Beaupre LA. Best practices for elderly hip fracture patients. J Gen Int Med 2005; 20: 1019 -25. • Beliveau MM. Perioperative care for the elderly patient. Med Clinics of North America 2003; 87(1). • Binder EF. JAMA. 2004: 292: 837 -46. • Detsky AS. Predicting cardiac complications in patients undergoing noncardiac surgery. J Gen Int Med 1986; 1: 211 -219. • Devereaux PJ. Are the recommendations to use perioperative beta-blocker therapy in patients undergoing noncardiac surgery based on reliable evidence? Can Med Assoc J 2004; 171(3). • Devereaux PJ. Surveillance and prevention of major perioperative cardiac events in patients undergoing noncardiac surgery: a review. CMAJ 2005; 173(7). • Eagle KA. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: a report of the ACC/AHA task force on practice guidelines 2002. • Eriksson BI. Duration of prophylaxis against VTE with fondaparinux after hip fracture surgery. Arch Int Med. 2003; 163: 1337 -42. • Eriksson BI. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip fracture surgery. NEJM 2001; 345: 1298 -304. • Foss NB. Effect of Postoperative Epidural Analgesia in Rehabilitation and pain after hip fracture surgery. Anesthesiology 2005; 102(16). • Geerts et al. The 7 th AACP conference on antithrombotic and thrombolytic therapy. Chest 2004; 126(3). • Goldman. Multifactorial index of cardiac risk in noncardiac surgical procedures. NEJM 1997; 297. • Grayburn PA. Cardiac events in patients undergoing noncardiac surgery: shifting the paradigm from noninvasive risk stratification to therapy. Ann Int Med 2003; 138: 506 -11. • Haddleston JM. Medical care of elderly patients with hip fractures. Mayo Clin Proc 2001; 76(3): 295 -8. Slide 63

REFERENCES (2 of 3) • Handell HH. Heparin, LMWH, and physical methods for preventing DVT and PE following surgery for hip fractures. Cochrane database systematic review 2002. • Hanson MR. Management of dementia and acute confusional states in the perioperative period. Neurol Clinics 2004; 22(2). • Hassan SA. Outcomes of noncardiac surgery after CABG or coronary angioplasty in the Bypass Angioplasty Revascularization Investigation (BARI). Am J Med 2001; 110: 260 -66. • Herbert PC. A multicenter randomized controlled trial of transfusion requirements in critical care. NEJM 1999; 340: 409 -17. • Huusko TM. Acta Orthop Scand. 2002: 73: 425 -31. • Inouye SK. Clarifying confusion: the Confusion Assessment Method a new method for detection of delirium. Ann Intern Med 1990; 113: 941 -8. • Inouye SK. Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care. Am J Med 1999; 106: 565 -73. • Lee TH. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999; 100: 1043 -49. • Mangano DT. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. NEJM 1996; 335(23): 1713 -20. • Matot I. Preoperative cardiac events in elderly patients with hip fracture randomized to epidural or conventional analgesia. Anesthesiology 2003; 98(1). • Mormino MA. Geriatric hip fractures. Family Med. Review UNMC April 24 -May 5 , 2006. • Morrison RS. The medical consultant’s role in caring for patients with hip fracture. Ann Int Med 1998; 128: 1010 -20. • Perez JV. Death after proximal femoral fracture. Injury 1995; 26(4): 237 -40. Slide 64
REFERENCES (3 of 3) • Poldermans D. The effect of bisoprolol on perioperative mortality and myocardial infarction in high risk patients undergoing vascular surgery. NEJM 1999; 341(24): 1789 -94. • Rao SS. Management of hip fracture: family physician’s role. Am Fam Phys 2006; 73(12). • Rasmussen S. Early discharge in people with hip fracture shifts rather than reduces costs to society. Evidence Based Healthcare 2003; 7(3). • Reilly DF. Self reported exercise tolerance and the risk of serious perioperative complications. Arch Int Med 1999; 159(18): 2185 -92. • Rigg JR. Epidural anesthesia and analgesia and outcome of major surgery: a randomized trial. Lancet 2002; 359(9314): 1276 -82. • Rinfret S. Value of immediate postoperative electrocardiogram to update risk stratification after major noncardiac surgery. Am J Card 2004; 94(8). • Roberts HC. Ageing. 2004; 33: 178 -84. • Roberts SE. Time trends and demography of mortality after fractured neck of femur in an English population. BMJ 2003; 327 (7418): 771 -5. • Rodgers A. Reduction of postoperative mortality and morbidity with epidural or spinal anesthesia: results from overview of randomized trials. BMJ 2000; 321 (7275). • Rosenthal RA. Assessment and management of the geriatric patient. Crit Care Med 2004; 32(4). • Urwin SC. General vs regional anesthesia for hip fracture surgery: a meta-analysis of randomized trials. Br J Anaesth 2000; 84(4): 450 -5. • Wesorick E. The preoperative cardiovascular evaluation of the intermediate risk patient. Am J Med 2005; 118(12). • Wolinsky FD. The effect of hip fracture on mortality, hospitalization, and functional status. Am J Pub Health 1997; 87: 398 -403. • Wu WC. Blood transfusion in elderly patients with acute myocardial infarction. NEJM 2001; 345: 1230 -36. Slide 65

THANK YOU FOR YOUR TIME! Visit us at: www. americangeriatrics. org Facebook. com/American. Geriatrics. Society Twitter. com/Amer. Geriatrics linkedin. com/company/american-geriatricssociety Slide 66