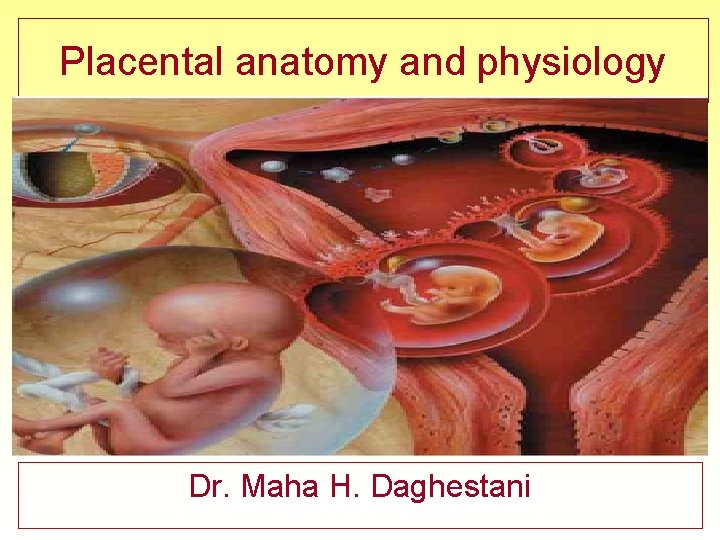
Placental anatomy and physiology Dr Maha H Daghestani



















- Slides: 92
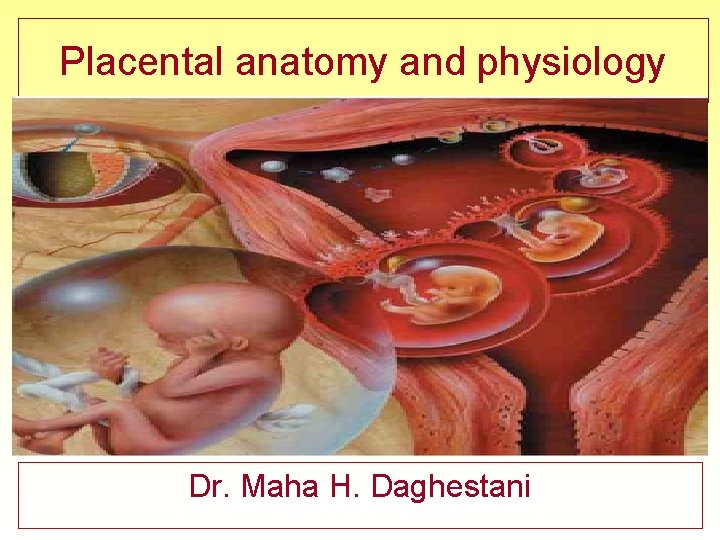
Placental anatomy and physiology Dr. Maha H. Daghestani
Formation of the Placenta The formation of the placenta, or placentation, involves two major processes: ü implantation and ü chorionic villi formation. Implantation is when the blastocyst sinks completely into the uterine wall, and chorionic villi formation refers to the development of the baby’s blood vessels into the uterine wall, thereby establishing the main site of gas and nutrients exchange
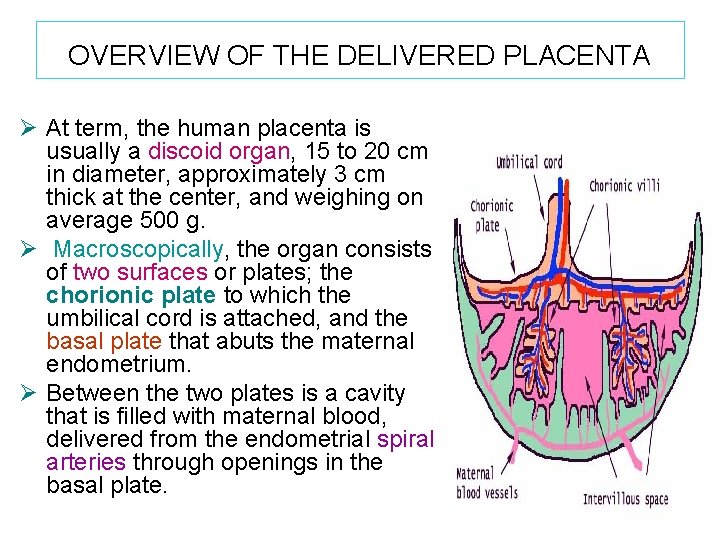
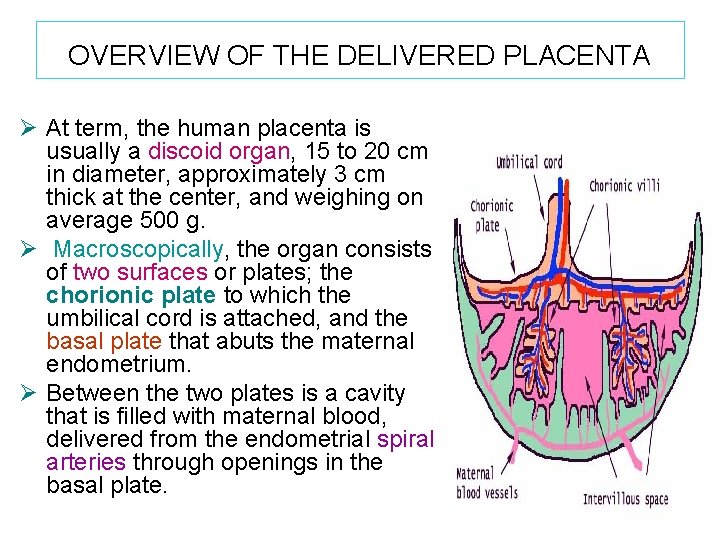
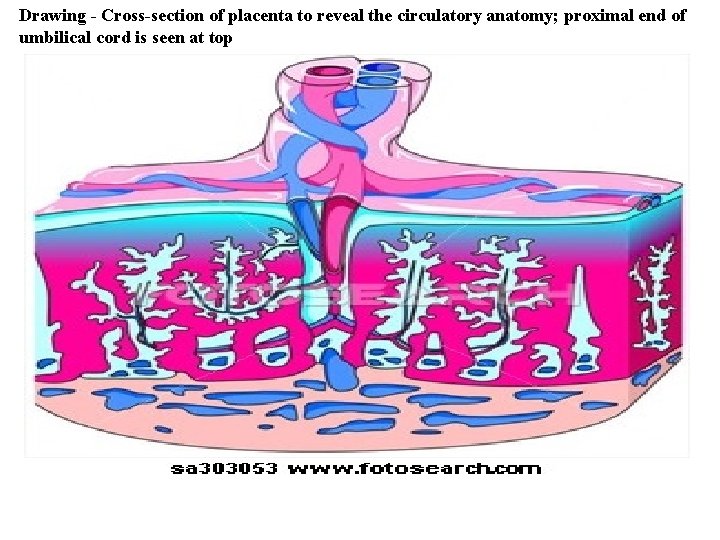
OVERVIEW OF THE DELIVERED PLACENTA Ø At term, the human placenta is usually a discoid organ, 15 to 20 cm in diameter, approximately 3 cm thick at the center, and weighing on average 500 g. Ø Macroscopically, the organ consists of two surfaces or plates; the chorionic plate to which the umbilical cord is attached, and the basal plate that abuts the maternal endometrium. Ø Between the two plates is a cavity that is filled with maternal blood, delivered from the endometrial spiral arteries through openings in the basal plate.


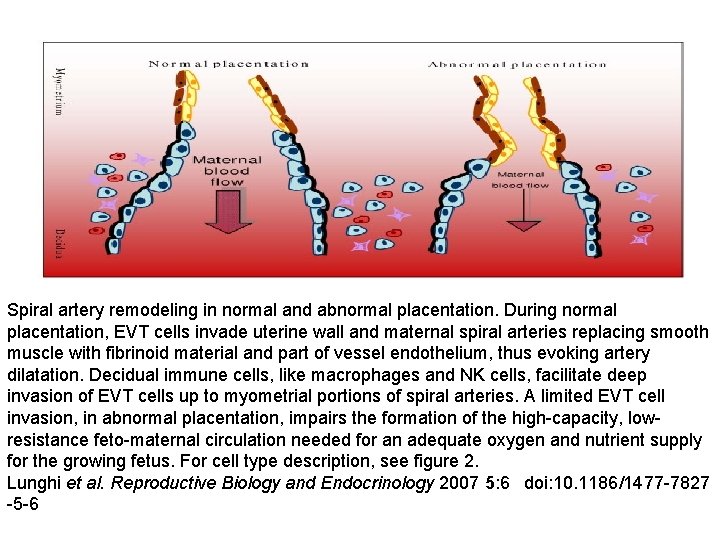
• On the mother's side, she has a richly vascular tissue, the uterine lining. This tissue contains many blood vessels, in particular an interesting kind of squiggly artery called a spiral artery. It's a typical arterial tube, lined with connective tissue and smooth muscle, and capable of regulating blood flow by contraction of the muscle.

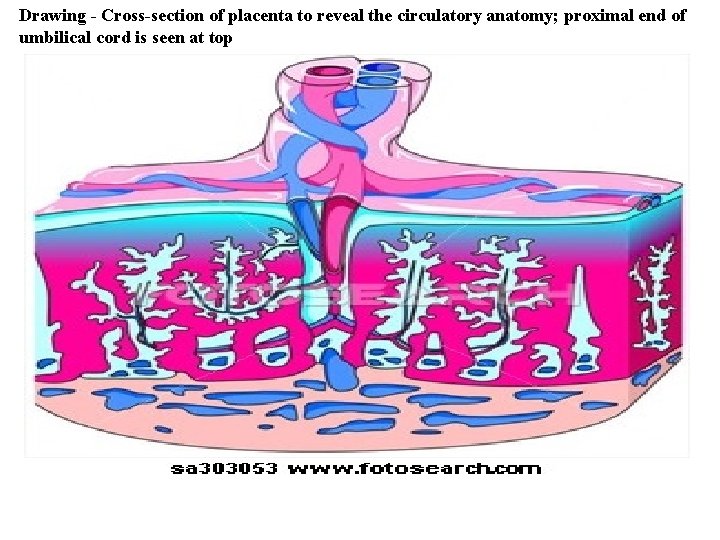
Drawing - Cross-section of placenta to reveal the circulatory anatomy; proximal end of umbilical cord is seen at top
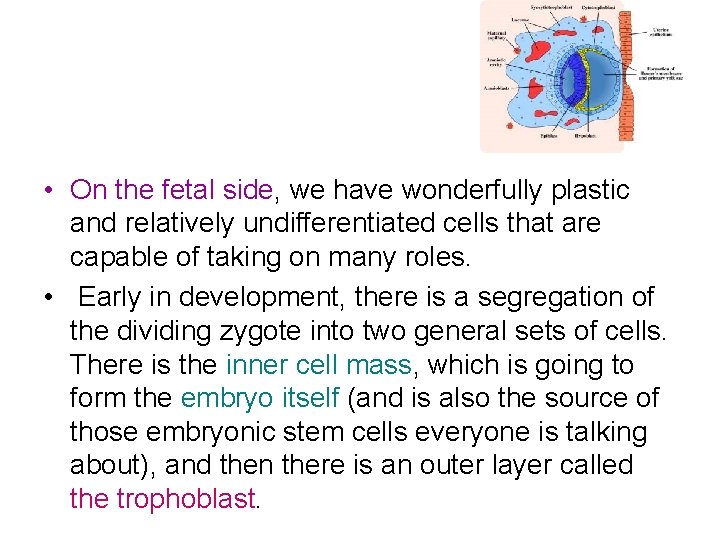
• On the fetal side, we have wonderfully plastic and relatively undifferentiated cells that are capable of taking on many roles. • Early in development, there is a segregation of the dividing zygote into two general sets of cells. There is the inner cell mass, which is going to form the embryo itself (and is also the source of those embryonic stem cells everyone is talking about), and then there is an outer layer called the trophoblast.
• The placenta actually contains a mix of maternal and fetal tissues. • The maternal part is the decidua, and contains many maternal blood vessels. The fetal part is the chorion, which is flush with the decidua, and contains networks of fetal blood vessels. • It is at this close apposition between the circulatory systems of the two organisms that gas, nutrient and waste exchange takes place.
Pregnancy does have many of the characteristics of a parasitic invasion.
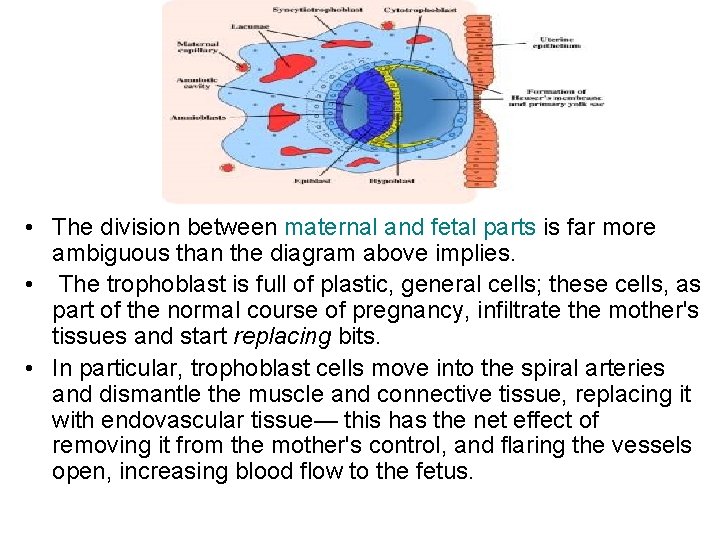
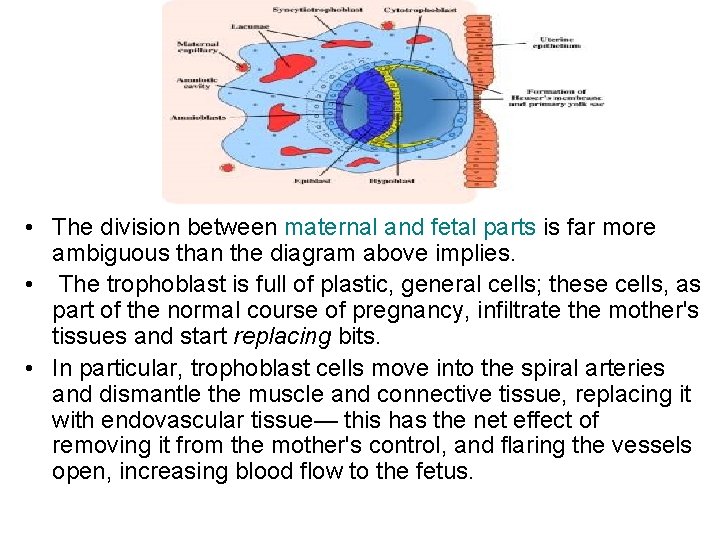
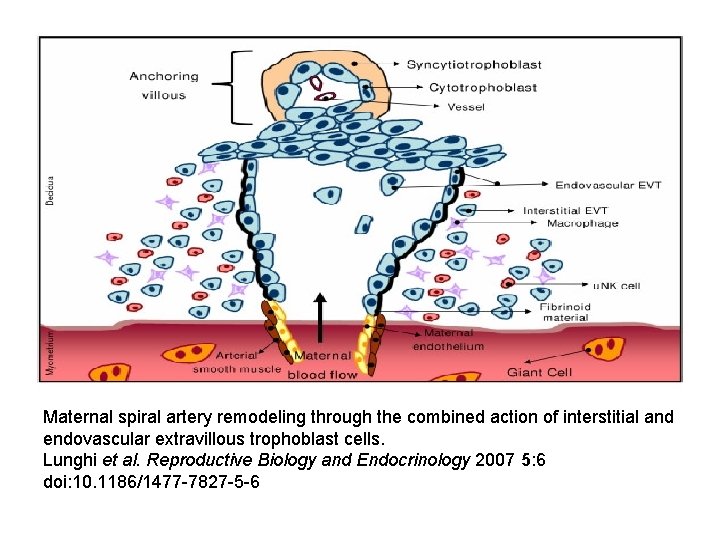
• The division between maternal and fetal parts is far more ambiguous than the diagram above implies. • The trophoblast is full of plastic, general cells; these cells, as part of the normal course of pregnancy, infiltrate the mother's tissues and start replacing bits. • In particular, trophoblast cells move into the spiral arteries and dismantle the muscle and connective tissue, replacing it with endovascular tissue— this has the net effect of removing it from the mother's control, and flaring the vessels open, increasing blood flow to the fetus.
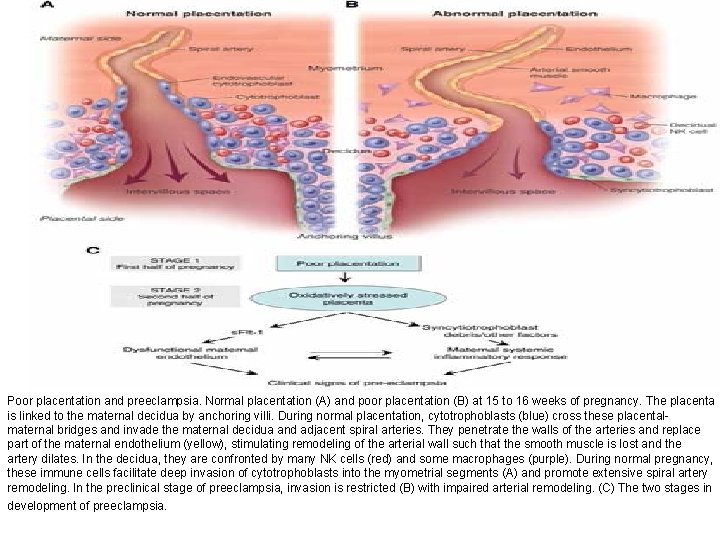
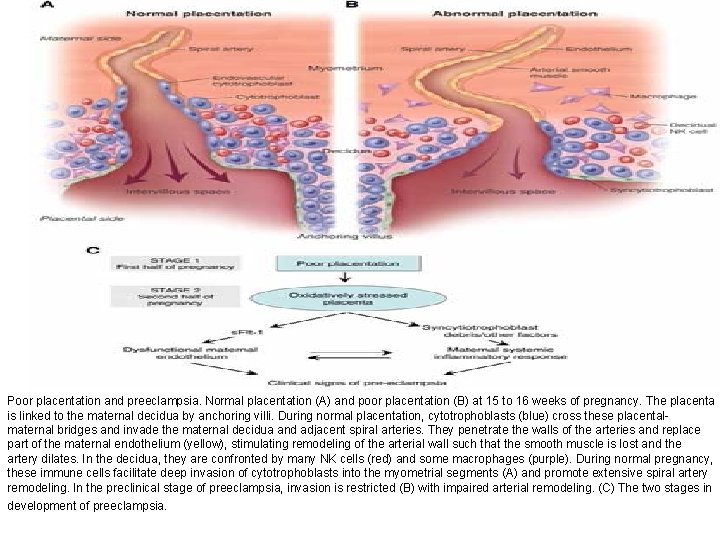
Poor placentation and preeclampsia. Normal placentation (A) and poor placentation (B) at 15 to 16 weeks of pregnancy. The placenta is linked to the maternal decidua by anchoring villi. During normal placentation, cytotrophoblasts (blue) cross these placentalmaternal bridges and invade the maternal decidua and adjacent spiral arteries. They penetrate the walls of the arteries and replace part of the maternal endothelium (yellow), stimulating remodeling of the arterial wall such that the smooth muscle is lost and the artery dilates. In the decidua, they are confronted by many NK cells (red) and some macrophages (purple). During normal pregnancy, these immune cells facilitate deep invasion of cytotrophoblasts into the myometrial segments (A) and promote extensive spiral artery remodeling. In the preclinical stage of preeclampsia, invasion is restricted (B) with impaired arterial remodeling. (C) The two stages in development of preeclampsia.
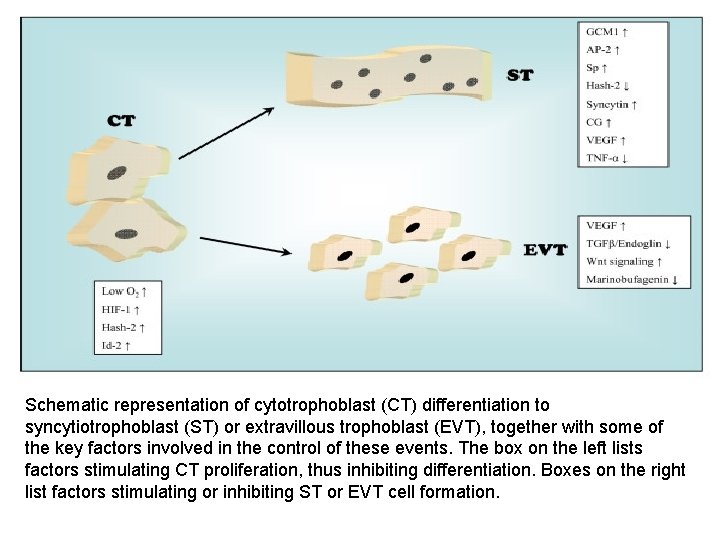
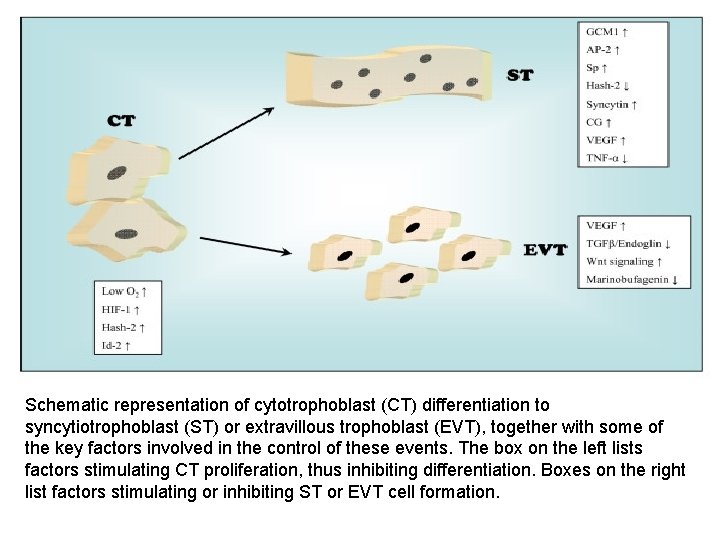
Schematic representation of cytotrophoblast (CT) differentiation to syncytiotrophoblast (ST) or extravillous trophoblast (EVT), together with some of the key factors involved in the control of these events. The box on the left lists factors stimulating CT proliferation, thus inhibiting differentiation. Boxes on the right list factors stimulating or inhibiting ST or EVT cell formation.
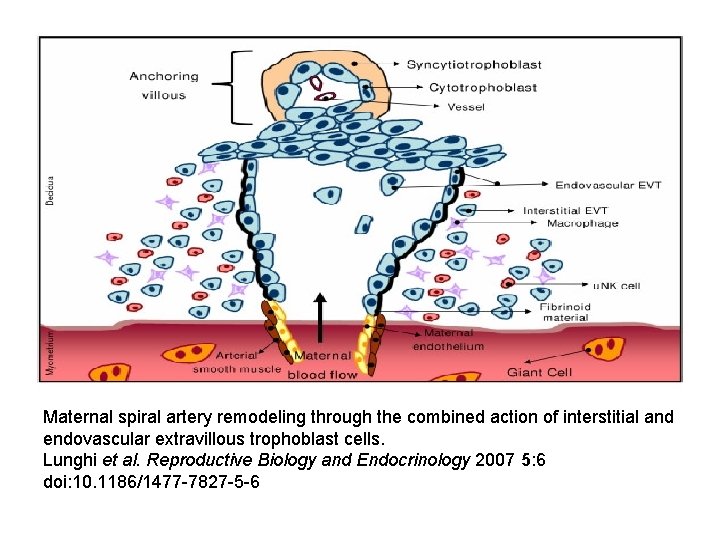
Maternal spiral artery remodeling through the combined action of interstitial and endovascular extravillous trophoblast cells. Lunghi et al. Reproductive Biology and Endocrinology 2007 5: 6 doi: 10. 1186/1477 -7827 -5 -6
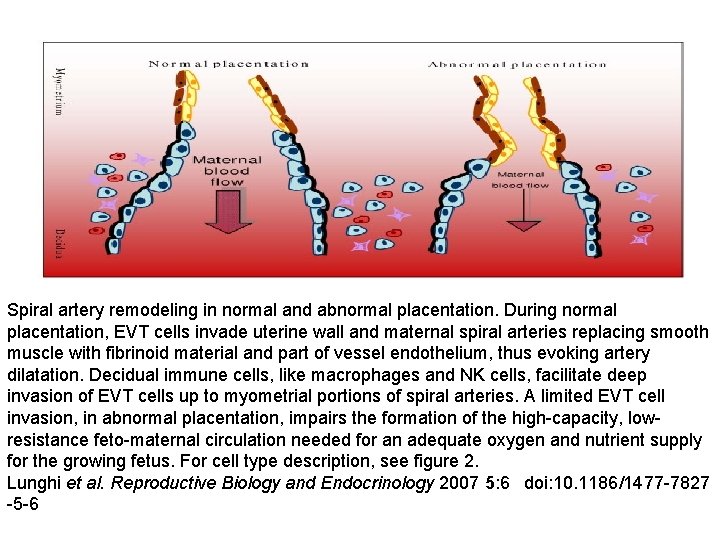
Spiral artery remodeling in normal and abnormal placentation. During normal placentation, EVT cells invade uterine wall and maternal spiral arteries replacing smooth muscle with fibrinoid material and part of vessel endothelium, thus evoking artery dilatation. Decidual immune cells, like macrophages and NK cells, facilitate deep invasion of EVT cells up to myometrial portions of spiral arteries. A limited EVT cell invasion, in abnormal placentation, impairs the formation of the high-capacity, lowresistance feto-maternal circulation needed for an adequate oxygen and nutrient supply for the growing fetus. For cell type description, see figure 2. Lunghi et al. Reproductive Biology and Endocrinology 2007 5: 6 doi: 10. 1186/1477 -7827 -5 -6
• It's a parasitic invasion with some interesting examples of maternal cooperation, however. • The uterine tissue contains a population of immune system cells, the NK cells (in red in the diagram above) which express a special class of surface proteins that recognize the invading trophoblast cells. • This is good, in ways that haven't yet been determined: stimulating a strong immune response by these specific NK cells helps to promote a more thorough placentation and reduces the probability of preeclampsia.
• A normal, healthy pregnancy requires a balance between the demands of the fetus and the needs of the mother. • In preeclampsia, the balance is imperfect. As shown in B in the diagram above slide. • The remodeling of the spiral arteries by trophoblast cells is less complete, and placentation is not as solid. • What this means is that less blood nutrients and gasses are delivered to the fetus, so the placenta is in oxidative stress. • Placental tissues die under these conditions, and spew cells, membrane fragments, nucleic acids, and cell contents into the maternal circulation, and this stuff stimulates a maternal immune response, leading to more inflammation and general distress to the mother.
Implantation – First step of Placentation • • The placenta begins to form when the blastocyst implants into the uterus. Halfway through the menstrual cycle, women’s hormones stimulate the endometrium, the inside layer of the uterus, to become full of blood vessels. The endometrium at this stage is called decidua. About six days after ovulation, the blastocyst starts sinking into the decidua, initiating implantation. The outer layer of the blastocyst, the trophoblast, tests whether the endometrium is ready for implantation. The receptivity of the endometrium to implantation depends on the proper levels of ovarian hormones in the blood. If the endometrium is ready early, the blastocyst implants high in the uterus; otherwise, it detaches and floats to a lower level.
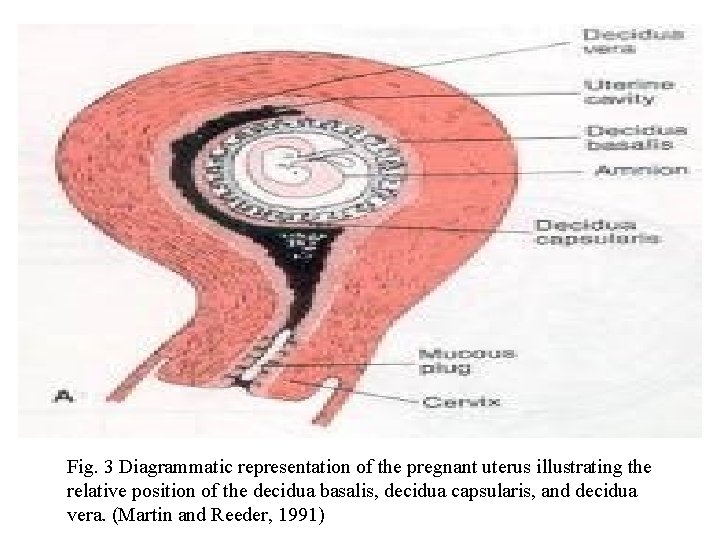
• Once the blastocyst has found the optimal site for implantation, the trophoblast cells proliferate and secrete digestive enzymes to eat into the decidua. • The digested decidua passes across the trophoblast wall and serves to nourish the growing embryo. • By the 10 th day, the blastocyst should sink completely below the surface of decidua, and the decidua is now classified into three portions. • The side lying in contact with the blastocyst at the site of implantation is the decidua basalis; the decidua lining over the surface of the implanted blastocyst is the decidua capsularis; the remainder of the decidua lining the inside of the uterus is the decidua vera (Fig. 3).
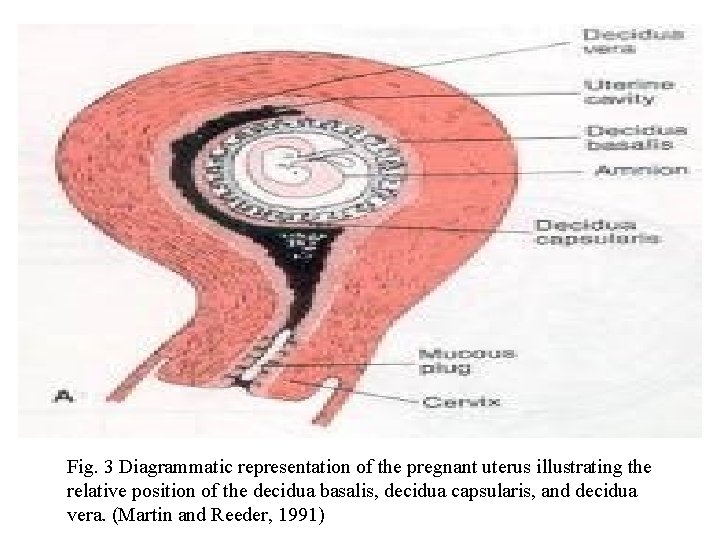
Fig. 3 Diagrammatic representation of the pregnant uterus illustrating the relative position of the decidua basalis, decidua capsularis, and decidua vera. (Martin and Reeder, 1991)
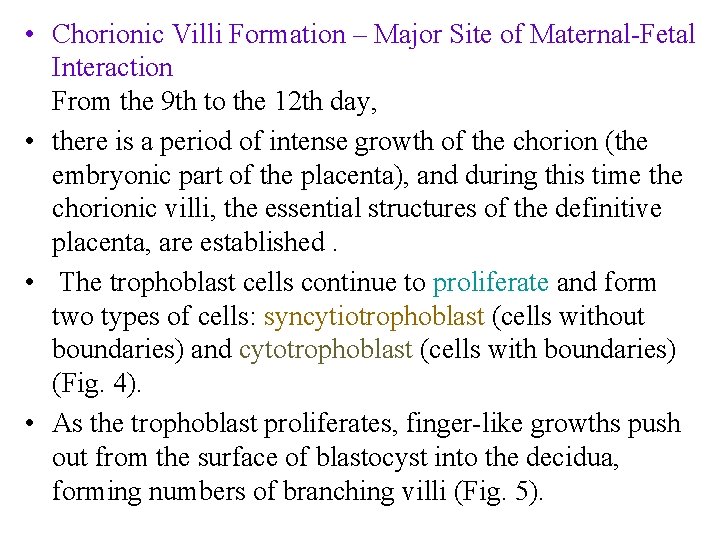
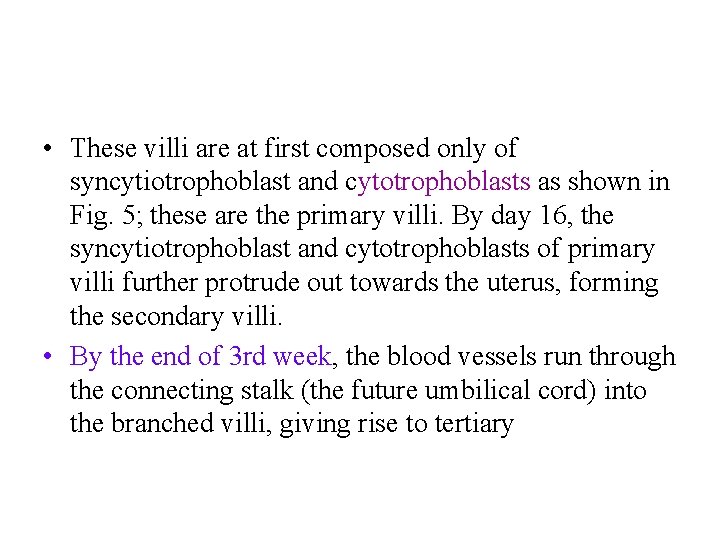
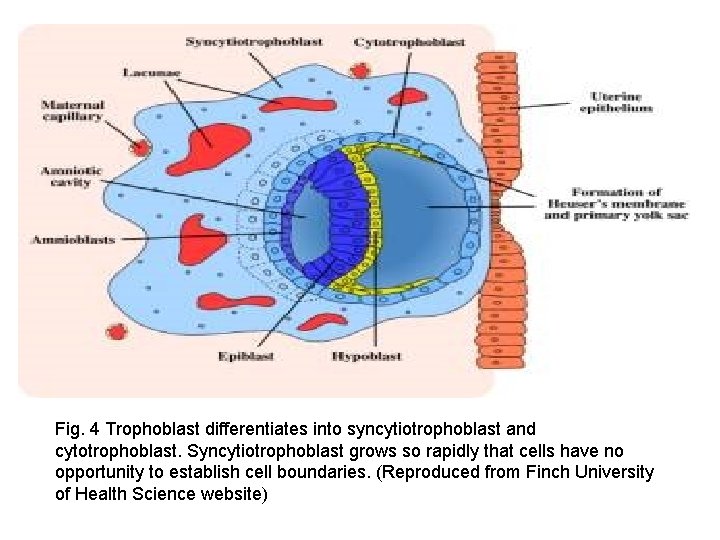
• Chorionic Villi Formation – Major Site of Maternal-Fetal Interaction From the 9 th to the 12 th day, • there is a period of intense growth of the chorion (the embryonic part of the placenta), and during this time the chorionic villi, the essential structures of the definitive placenta, are established. • The trophoblast cells continue to proliferate and form two types of cells: syncytiotrophoblast (cells without boundaries) and cytotrophoblast (cells with boundaries) (Fig. 4). • As the trophoblast proliferates, finger-like growths push out from the surface of blastocyst into the decidua, forming numbers of branching villi (Fig. 5).
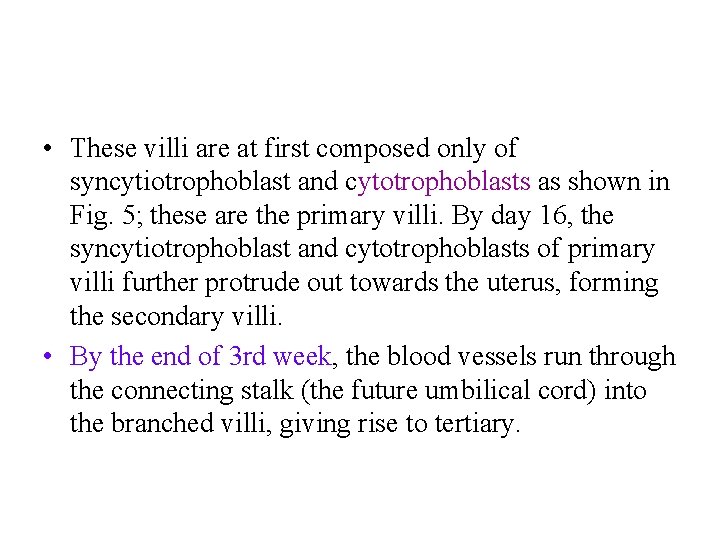
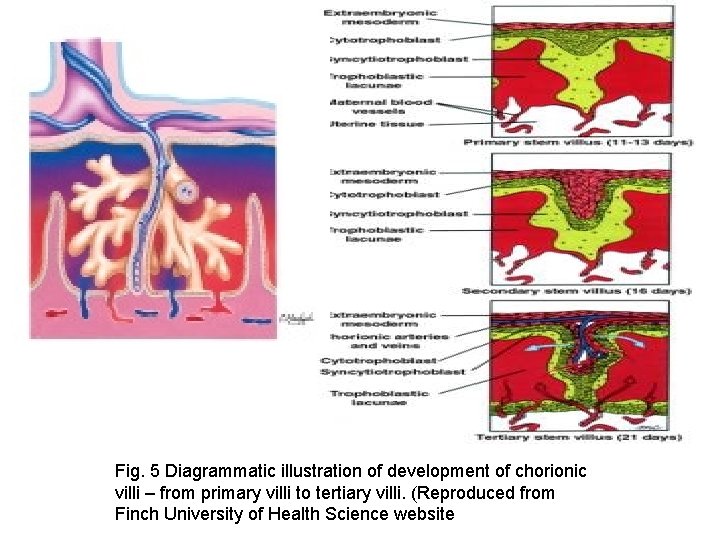
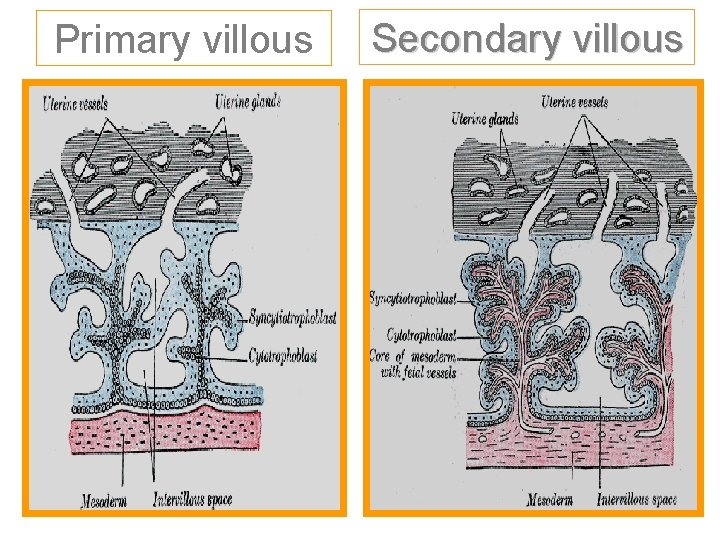
• These villi are at first composed only of syncytiotrophoblast and cytotrophoblasts as shown in Fig. 5; these are the primary villi. By day 16, the syncytiotrophoblast and cytotrophoblasts of primary villi further protrude out towards the uterus, forming the secondary villi. • By the end of 3 rd week, the blood vessels run through the connecting stalk (the future umbilical cord) into the branched villi, giving rise to tertiary
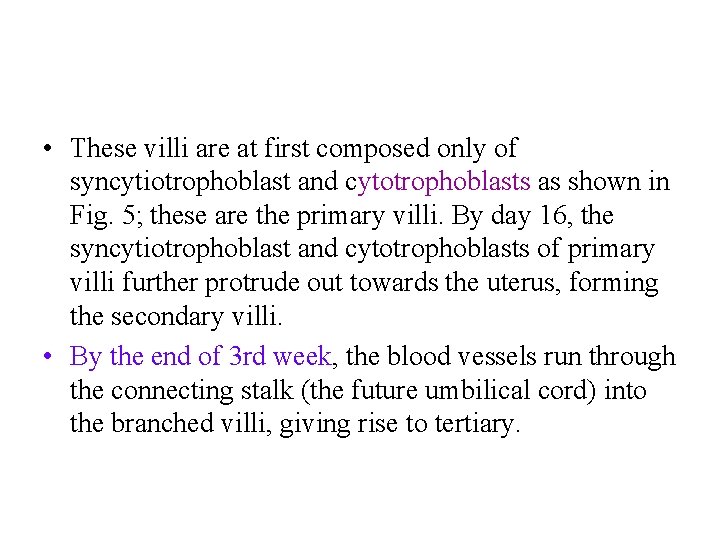
• These villi are at first composed only of syncytiotrophoblast and cytotrophoblasts as shown in Fig. 5; these are the primary villi. By day 16, the syncytiotrophoblast and cytotrophoblasts of primary villi further protrude out towards the uterus, forming the secondary villi. • By the end of 3 rd week, the blood vessels run through the connecting stalk (the future umbilical cord) into the branched villi, giving rise to tertiary.
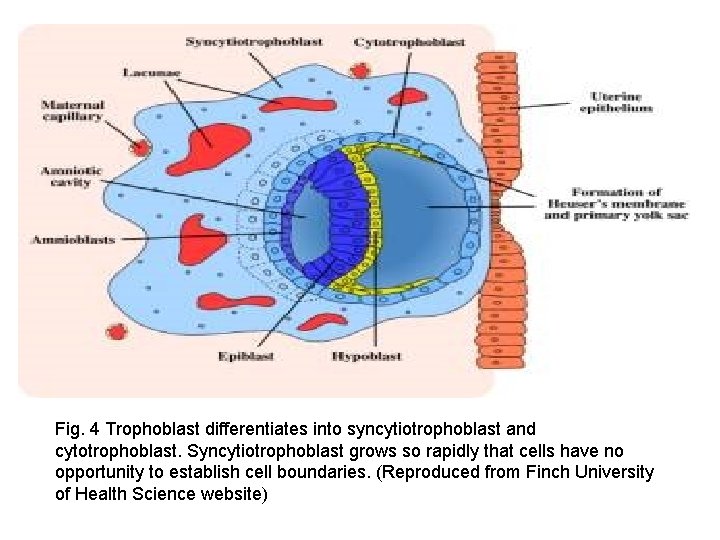
Fig. 4 Trophoblast differentiates into syncytiotrophoblast and cytotrophoblast. Syncytiotrophoblast grows so rapidly that cells have no opportunity to establish cell boundaries. (Reproduced from Finch University of Health Science website)

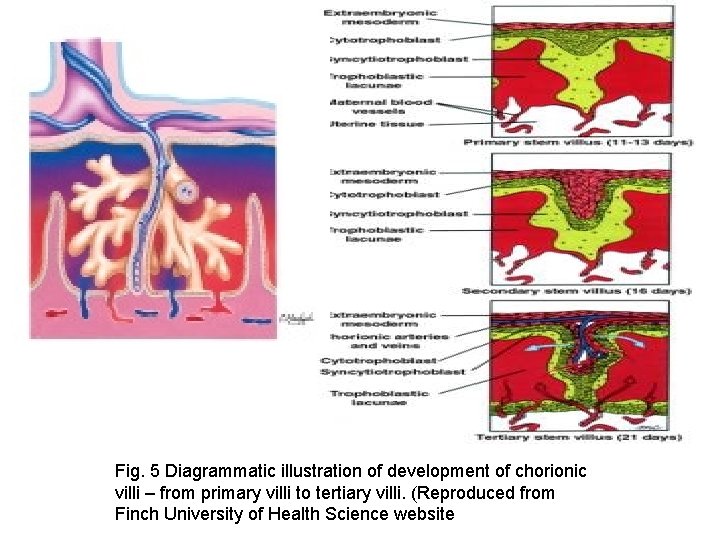
Fig. 5 Diagrammatic illustration of development of chorionic villi – from primary villi to tertiary villi. (Reproduced from Finch University of Health Science website
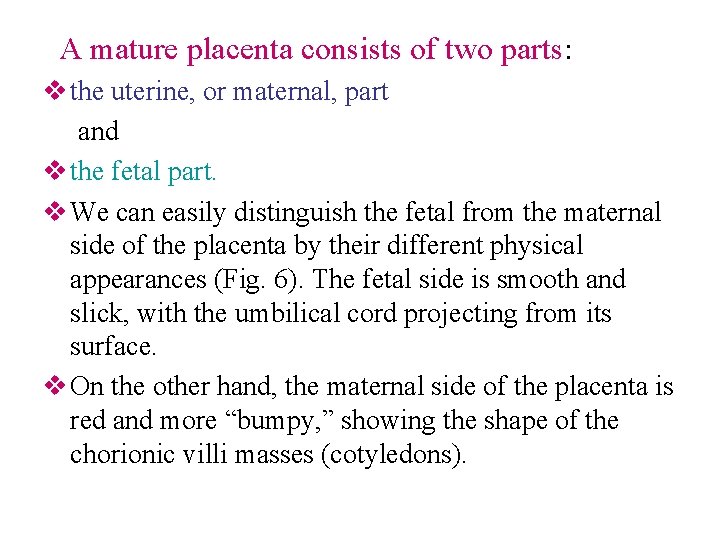
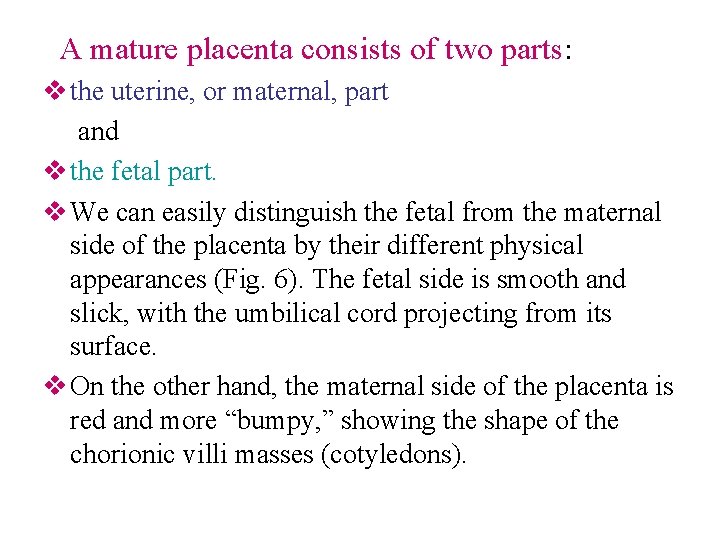
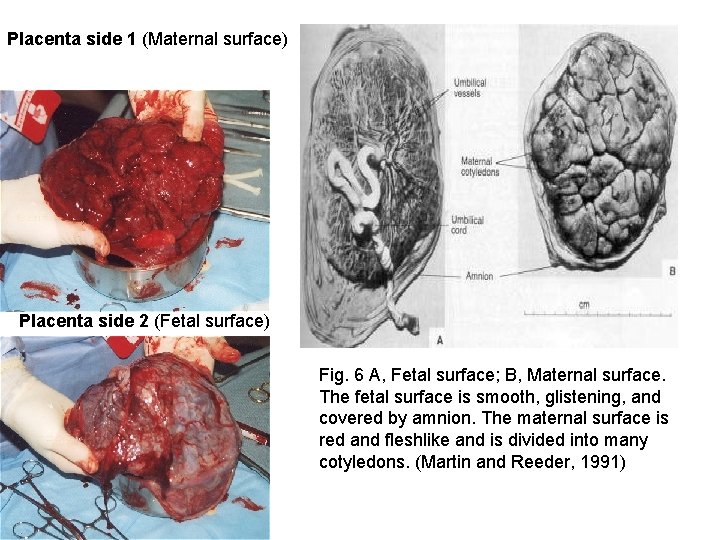
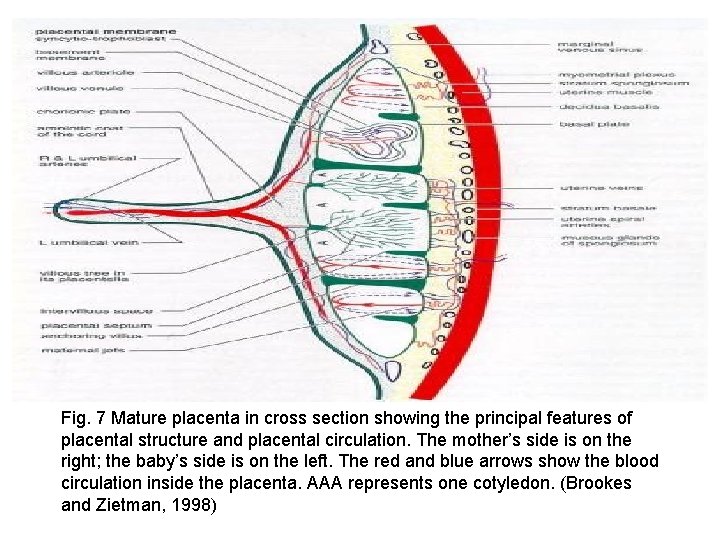
A mature placenta consists of two parts: v the uterine, or maternal, part and v the fetal part. v We can easily distinguish the fetal from the maternal side of the placenta by their different physical appearances (Fig. 6). The fetal side is smooth and slick, with the umbilical cord projecting from its surface. v On the other hand, the maternal side of the placenta is red and more “bumpy, ” showing the shape of the chorionic villi masses (cotyledons).

v. The bumpy shape of the placenta is caused by some chorionic villi attaching directly to the decidua basalis and acting as anchoring villi. v. The anchoring villi divide the placenta into seven to ten villous masses called cotyledons (Fig. 7). v. Most of the villi hang floating freely in the blood spaces, providing the major site of maternal-fetal exchange.
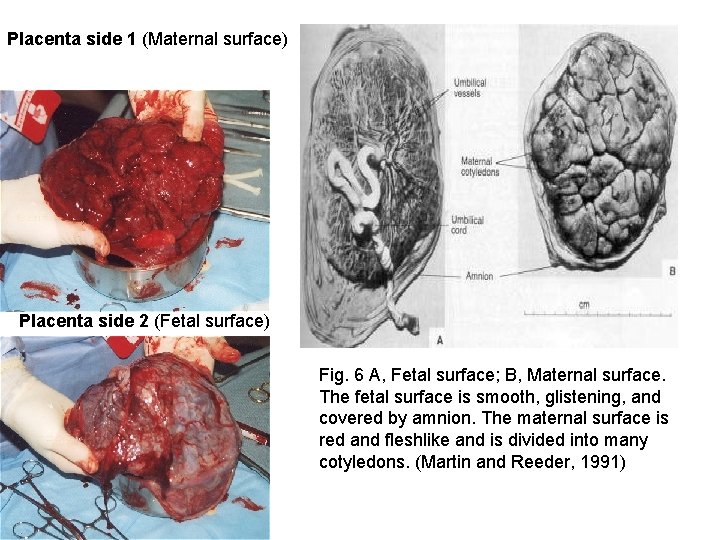
Placenta side 1 (Maternal surface) Placenta side 2 (Fetal surface) Fig. 6 A, Fetal surface; B, Maternal surface. The fetal surface is smooth, glistening, and covered by amnion. The maternal surface is red and fleshlike and is divided into many cotyledons. (Martin and Reeder, 1991)

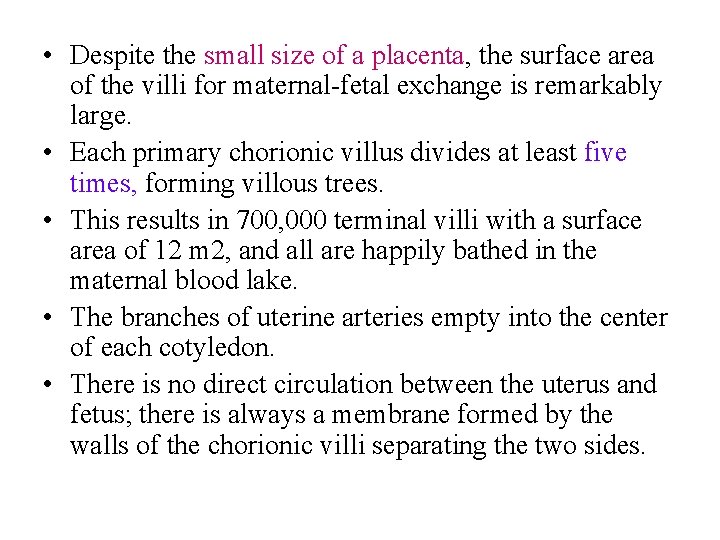
• Despite the small size of a placenta, the surface area of the villi for maternal-fetal exchange is remarkably large. • Each primary chorionic villus divides at least five times, forming villous trees. • This results in 700, 000 terminal villi with a surface area of 12 m 2, and all are happily bathed in the maternal blood lake. • The branches of uterine arteries empty into the center of each cotyledon. • There is no direct circulation between the uterus and fetus; there is always a membrane formed by the walls of the chorionic villi separating the two sides.
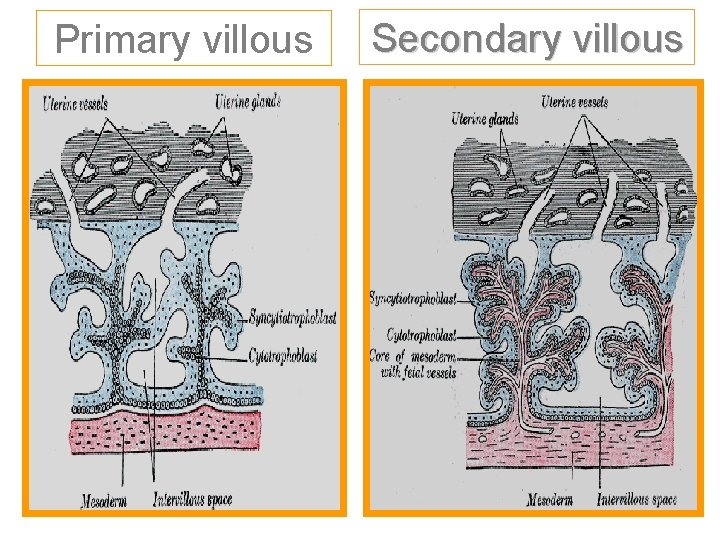
Primary villous Secondary villous

Ø Placental structure is complete by the 12 th week of pregnancy. Ø A normal mature placenta is discoidal in shape (like a flattened cake). Ø The placenta normally develops on the posterior or, less frequently, the anterior wall of the uterus. Normal placental development and function are critical for fetal growth and development and birth for a healthy baby.
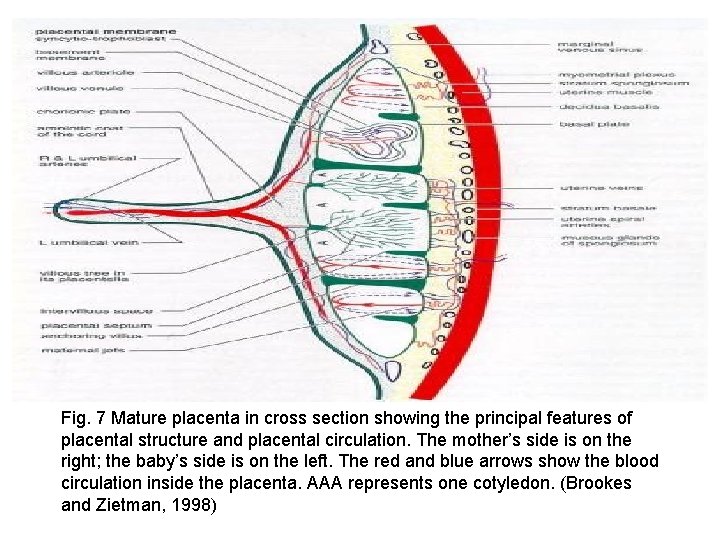
Fig. 7 Mature placenta in cross section showing the principal features of placental structure and placental circulation. The mother’s side is on the right; the baby’s side is on the left. The red and blue arrows show the blood circulation inside the placenta. AAA represents one cotyledon. (Brookes and Zietman, 1998)

Function of Placenta – Hormone Synthesis One important function of the placenta is production and secretion of hormones. The syncytiotrophoblast cells of the placenta secrete four main kinds of hormones: estrogen, progesterone, and two hormones peculiar to the placenta, h. PL and h. CG.

Estrogen § Estrogen is one of the most important hormones during and after pregnancy. § During pregnancy, estrogen stimulates the growth of the uterus, enhances the blood flow between the uterus and the placenta, and causes the breast to enlarge as a preparation for milk production. § During baby delivery, estrogen stimulates contractions of the uterus muscle to help pushing the baby out. § After delivery, it stimulates the breast to produce milk.

§ The amount of estrogen secreted increases along with time during pregnancy, and the secretion reaches its maximum point just before birth, telling the doctors that the baby is coming out soon. § Since the synthesis of estrogen depends mainly on the integrity of the fetal adrenal and liver as well as the placenta doctors often measure the level of estrogen in the mother’s urine and blood to determine the baby’s well being.
Progesterone • The main function of progesterone is to maintain the inner layer of the uterus; it stimulates this inner layer to grow in order to provide a supportive environment for the developing embryo. • In addition, progesterone inhibits the movement of uterus muscle during the first few weeks of pregnancy so that the blastocyst can implant into the wall of uterus and develop the placenta more easily. • Secretion of progesterone increases gradually during pregnancy and reaches and stays at a constant value for the rest of the pregnancy period.
h. PL (human placental lactogen) • The h. PL (human placental lactogen) has two major functions. • First, the h. PL helps to regulate the mother’s metabolism, or the balancing between energy sources and wastes during pregnancy. • The mother’s metabolism is changed during pregnancy because, carrying one more life in the body, she needs more energy sources and produces more wastes than usual.
• Second, the h. PL ensures sufficient amount of nutrient supply for the fetus by aiding some nutrient transports across the placenta. • The h. PL also stimulates breast development and preparation of milk along with estrogen. • The level of h. PL is proportional to the mass of the placenta; larger placenta usually requires more h. PL secretion.
h. CG (human chorionic gonadotropin) • The h. CG (human chorionic gonadotropin) supports the production of estrogen and progesterone in the first 10 weeks of pregnancy until the syncytiotrophoblast cells can produce these two crucial hormones by themselves. • This is why the level of h. CG in the mother’s blood usually rises until the end of second month and decline sharply by the fourth month. •
• Because h. CG is usually detectable in the mother’s blood one week after fertilization while other hormones are still low in amount. • The doctors commonly use the presence of h. CG in a woman’s blood or urine as a pregnancy test.
Function of Placenta – Immunological barrier • The placenta plays two important roles in fetalmaternal immunological balance: passive immunity and immunosuppression, suppression of the mother’s immune response against the fetus. • Before birth, the baby’s immune system is not fully developed yet, so the baby does not produce most of the antibodies by itself. • Therefore, most of the antibodies needed by the baby are acquired from the mother directly. •
• The membrane permeability of placenta enables the transport of antibodies from the mother to the baby; this is called passive immunity. • The baby does not yet actively make its own antibodies but instead accepts the mother’s antibodies passively.

v While receiving antibodies from the mother, the placenta enables the baby to survive in the mother’s body as a genetically foreign tissue. v Normally when a human body detects a foreign tissue inside the body, its immune system would reject and try to eliminate this tissue. v The fetus contains a genetic make-up that comes from both the mother and the father; therefore, its genetic make-up is different from the mother’s and may be recognized by the mother’s body as a foreign invader. v Nevertheless, the fetus can still survive by suppressing the mother’s immune responses.
v There are two major suppression methods: v Non-selective and v Specific. v In non-selective suppression, the placenta secretes several molecules that suppress the immune system; one of them is the hormone progesterone (Gilbert, 1997). v For specific suppression, the cells in the mother’s immune system that can recognize the father’s part of genetic make-up are selectively abrogated, hence reducing the total number of cells recognizing the father’s gene and blunting the immune response against the fetus (Gilbert, 1997). v The immune system returns to normal after delivery.
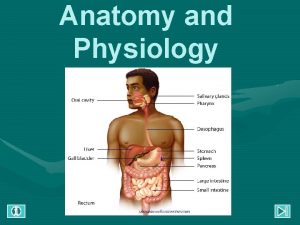
Function of Placenta – Gas, nutrient and waste product exchange- Blood circulation in the Placenta • The blood from the mother acts as the nutrient deliverer and waste remover. • In the placenta, the blood supply comes from the arteries in the uterus and enters the blood lake. • It then travels toward the chorionic plate (the baby’s side). After hitting the chorionic plate, the blood returns to the mother’s side and leaves through the veins in the uterus.
• To ensure fresh blood supply at all times, in every minute, the blood in the placenta replaces completely for about two to three times, and the volume of blood flowing through the villi is approximately 400 c. c. • Interestingly, the total surface area of the villi in a mature placenta corresponds to the total absorptive area of the adult intestinal tract, thereby enabling effective transfer of gas, nutrient and waste between the mother and the baby.

Mechanisms of transport and exchange • Transport of molecules inside the placenta depends on two major driving forces: Ø The concentration gradient and Ø The electrical gradient.
Concentration gradient refers to the differences in gas, nutrient or waste concentrations between the mother’s and the baby’s side. Most substances tend to go from places of higher concentration to places of lower concentration. For example, if the amount of certain waste in the baby’s blood is greater than those in the mother’s blood at the blood lake, the waste will tend to diffuse out of the villi into the blood lake.
Electrical gradient means the concentration of different charged molecules across the placental membrane. Again molecules travel from high to low concentrations; thus the transporting direction depends on whether the mother’s or the baby’s side has greater number of molecules.
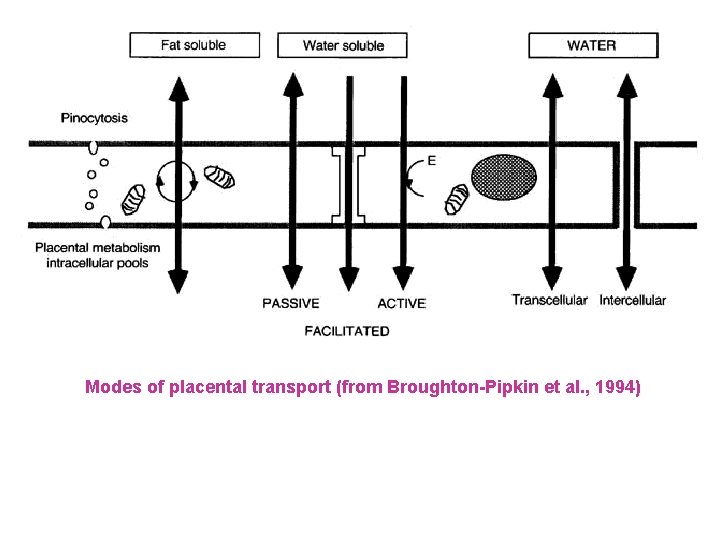
• The mechanism of transport across the placenta depends on the nature of the substance. • Some large substances can be transported from cell to cell by packing them into small bubbles. • Smaller molecules can usually travel freely across the placenta by simple diffusion depending on the gradient concentration on both sides of the placenta. • However, some substances cannot easily diffuse through the placenta or have to go against their gradients (from low to high concentrations). • In this case, they have to cross the placenta with the help of certain proteins located in the mother’s and the baby’s cells.
Transferred Substances ü The four major categories of substances a placenta transports are 1. gas 2. waste 3. antibodies and 4. nutrients. Gases: O 2 and CO 2 are the two essential gases the placenta transports; they pass across the placenta by simple diffusion. ü The amount of CO 2 in the baby’s blood is higher than that in the blood lake, so CO 2 travels directly down the gradient towards the mother’s side. On the other hand, the amount of O 2 in the blood lake is higher than that in the baby’s blood, thus O 2 travels from the mother to the baby. ü
ü Another special property that allows efficient O 2 transport is that the baby’s red blood cells tend to hold on to O 2 more tightly than a normal adult’s red blood cells. ü O 2 and CO 2 are not the only gases the placenta can transport; this is why pregnant women should especially stay away from smoking and air-polluted environment. Harmful gases such as CO (carbon monoxide) can cross the placenta in the same way the O 2 does and thereby affect the baby’s development.
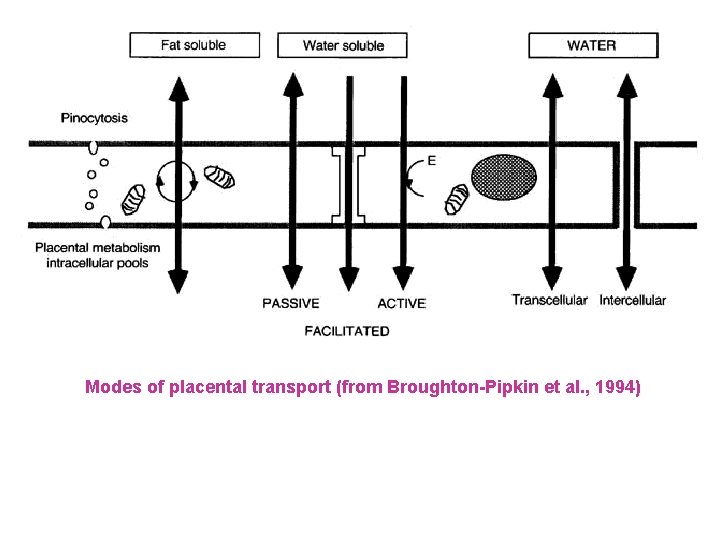
Modes of placental transport (from Broughton-Pipkin et al. , 1994)
v. Wastes and antibodies: The baby’s blood contains more wastes than the blood lake, so these wastes diffuse down the gradient into the mother’s blood. v. The antibodies give the baby passive immunity, and they are packed into small bubbles for easier transportation
Ø Nutrients: Smaller nutrients like water, sodium, and calcium can pass to the baby by simple diffusion, whereas larger nutrients such as protein molecules cross the placenta by the cells’ packaging them into bubble sacks. Ø Other nutrients travel across the placenta with the help of the proteins specialized in transportation. Part of everything the mother eats eventually reaches the baby in one of the three ways mentioned above. Therefore, it is very important for pregnant women to eat balanced meals and to prevent unhealthy food and drinks like drugs and alcohol.
Amniocentesis v One of the most common procedures for detecting abnormalities before birth is amniocentesis. v In this procedure, a sample of the fluid that surrounds the fetus (amniotic fluid) is removed. v Amniocentesis is usually performed at 14 weeks of pregnancy or later. v If the reason for performing amniocentesis is a high alphafetoprotein level in the woman's blood, the procedure is best performed between 15 and 17 weeks of pregnancy. Amniocentesis enables doctors to measure the alphafetoprotein level in the amniotic fluid. v This measurement more reliably indicates whether the fetus has a brain or spinal cord defect than measurement of this level in the woman's blood.
• After anesthetizing an area of skin over the abdomen, a doctor inserts a needle through the abdominal wall into the amniotic fluid. • During the procedure, ultrasonography is performed so that the fetus can be monitored and the needle guided into place. • Fluid is withdrawn, and the needle is removed. Results are usually available in 1 to 3 weeks. • Women who have Rh-negative blood are given Rh 0(D) immune globulin after the procedure to prevent them from producing antibodies to Rh factor, which can cause problems in a fetus with Rh-positive blood
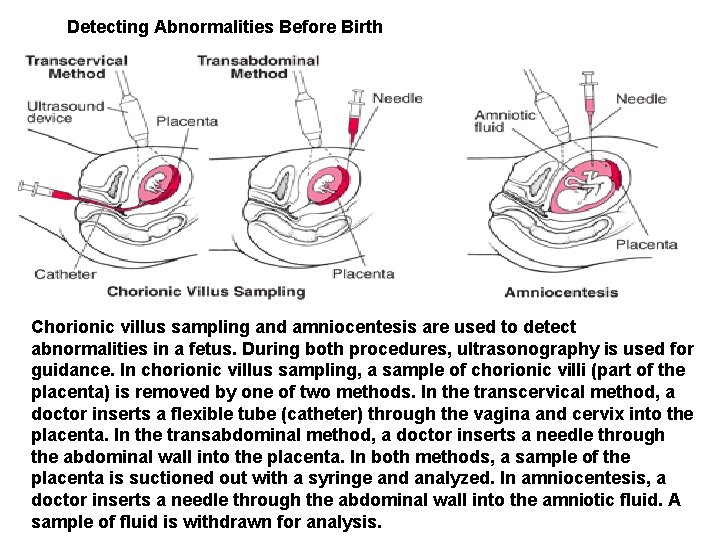
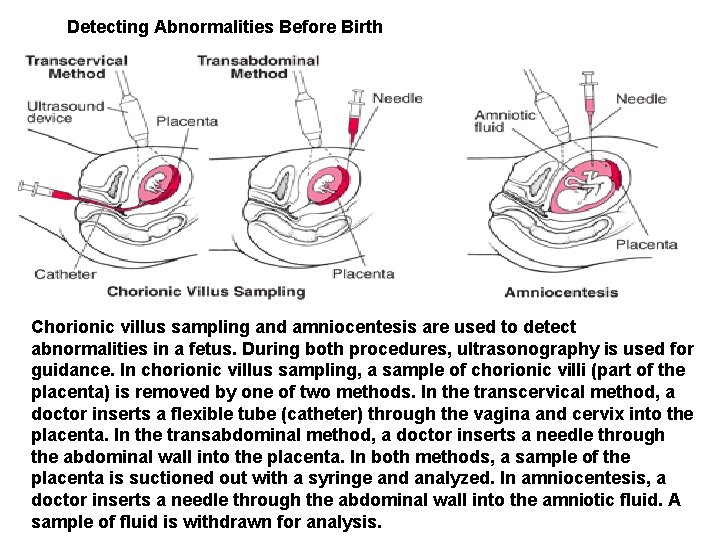
Detecting Abnormalities Before Birth Chorionic villus sampling and amniocentesis are used to detect abnormalities in a fetus. During both procedures, ultrasonography is used for guidance. In chorionic villus sampling, a sample of chorionic villi (part of the placenta) is removed by one of two methods. In the transcervical method, a doctor inserts a flexible tube (catheter) through the vagina and cervix into the placenta. In the transabdominal method, a doctor inserts a needle through the abdominal wall into the placenta. In both methods, a sample of the placenta is suctioned out with a syringe and analyzed. In amniocentesis, a doctor inserts a needle through the abdominal wall into the amniotic fluid. A sample of fluid is withdrawn for analysis.
• Amniocentesis rarely causes any problems for the woman or the fetus. • Some women feel slightly sore for an hour or two afterward. • About 1 to 2% of the women have spotting of blood or leakage of amniotic fluid from the vagina, but these effects do not last long and usually stop without treatment. • After amniocentesis, the chance of miscarriage due to the procedure is about 1 in 200. • Needle injuries to the fetus are very rare. Amniocentesis can usually be performed when a woman is pregnant with twins or even more fetuses.
• Percutaneous Umbilical Blood Sampling • Percutaneous umbilical blood sampling is used when rapid chromosome analysis is needed, particularly toward the end of pregnancy when ultrasonography has detected abnormalities in the fetus. Often, results can be available within 48 hours. • The doctor first anesthetizes an area of skin over the abdomen. • Guided by ultrasonography, the doctor then inserts a needle through the abdominal wall into the umbilical cord. • A sample of the fetus's blood is withdrawn and analyzed, and the needle is removed. • Percutaneous umbilical blood sampling is an invasive procedure and has risks for the woman and fetus.
Development of the Embryo • The next stage in development is the embryo, which develops under the lining of the uterus on one side. This stage is characterized by the formation of most internal organs and external body structures. • Organ formation begins about 3 weeks after fertilization, when the embryo elongates, first suggesting a human shape. • Shortly thereafter, the area that will become the brain and spinal cord (neural tube) begins to develop. • The heart and major blood vessels begin to develop by about day 16 or 17. • The heart begins to pump fluid through blood vessels by day 20, and the first red blood cells appear the next day. • Blood vessels continue to develop in the embryo and placenta.
• Almost all organs are completely formed by about 8 weeks after fertilization (which equals 10 weeks of pregnancy). • The exceptions are the brain and spinal cord, which continue to mature throughout pregnancy. • Most malformations (birth defects) occur during the period when organs are forming. • During this period, the embryo is most vulnerable to the effects of drugs, radiation, and viruses. • Therefore, a pregnant woman should not be given any live-virus vaccinations or take any drugs during this period unless they are considered essential to protect her health
• At the end of the 8 th week after fertilization (10 weeks of pregnancy), the embryo is considered a fetus. • During this stage, the structures that have already formed grow and develop. • The following are markers during pregnancy: • By 12 weeks of pregnancy: The fetus fills the entire uterus. • By about 14 weeks: The sex can be identified. • By about 16 to 20 weeks: Typically, the pregnant woman can feel the fetus moving. • Women who have been pregnant before typically feel movements about 2 weeks earlier than women who are pregnant for the first time. • By about 24 weeks: The fetus has a chance of survival outside the uterus.
• The lungs continue to mature until near the time of delivery. • The brain accumulates new cells throughout pregnancy and the first year of life after birth. • As the placenta develops, it extends tiny hairlike projections (villi) into the wall of the uterus. • The projections branch and rebranch in a complicated treelike arrangement. • This arrangement greatly increases the area of contact between the wall of the uterus and the placenta, so that more nutrients and waste materials can be exchanged. • The placenta is fully formed by 18 to 20 weeks but continues to grow throughout pregnancy. • At delivery, it weighs about 1 pound.


Placenta and Embryo at 8 Weeks • At 8 weeks of pregnancy, the placenta and fetus have been developing for 6 weeks. • The placenta forms tiny hairlike projections (villi) that extend into the wall of the uterus. Blood vessels from the embryo, which pass through the umbilical cord to the placenta, develop in the villi. • A thin membrane separates the embryo's blood in the villi from the mother's blood that flows through the space surrounding the villi (intervillous space).
• This arrangement allows materials to be exchanged between the blood of the mother and that of the embryo. • It also prevents the mother's immune system from attacking the embryo because the mother's antibodies are too large to pass through the membrane. • The embryo floats in fluid (amniotic fluid), which is contained in a sac (amniotic sac). The amniotic fluid provides a space in which the embryo can grow freely. The fluid also helps protect the embryo from injury. The amniotic sac is strong and resilient.


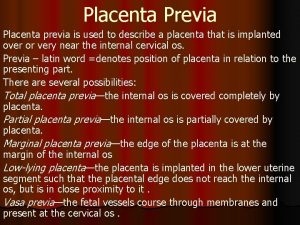
What Is Placenta Previa?
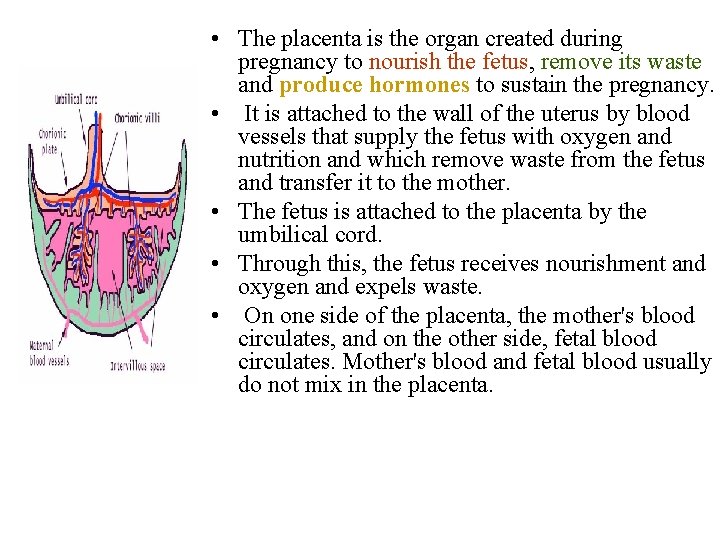
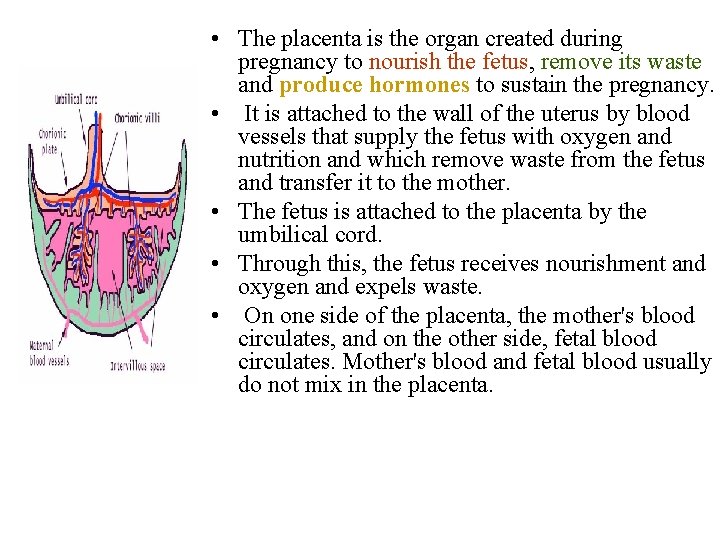
• The placenta is the organ created during pregnancy to nourish the fetus, remove its waste and produce hormones to sustain the pregnancy. • It is attached to the wall of the uterus by blood vessels that supply the fetus with oxygen and nutrition and which remove waste from the fetus and transfer it to the mother. • The fetus is attached to the placenta by the umbilical cord. • Through this, the fetus receives nourishment and oxygen and expels waste. • On one side of the placenta, the mother's blood circulates, and on the other side, fetal blood circulates. Mother's blood and fetal blood usually do not mix in the placenta.
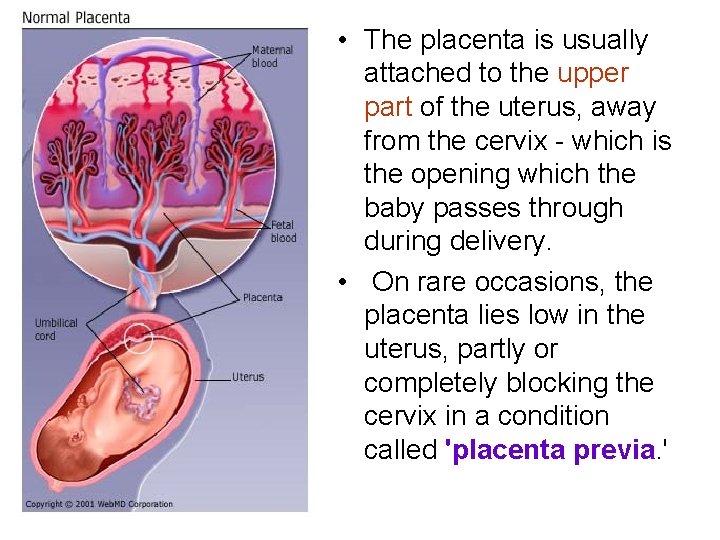
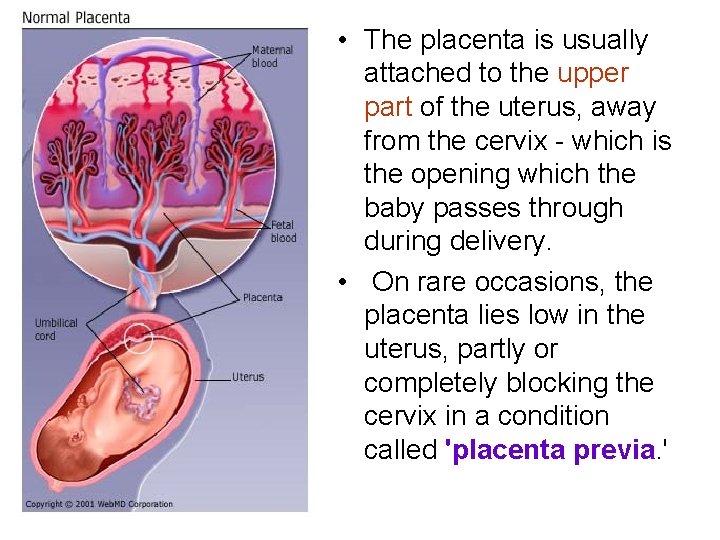
• The placenta is usually attached to the upper part of the uterus, away from the cervix - which is the opening which the baby passes through during delivery. • On rare occasions, the placenta lies low in the uterus, partly or completely blocking the cervix in a condition called 'placenta previa. '
• It's very common to have some form of placenta previa before the 20 th week of pregnancy - in as many as one in 3 -5 pregnancies. • However, usually as the uterus grows, the placenta moves with it higher in the uterus, away from the cervix. • If it remains near the cervix as your due date nears, which happens in about one in 200 pregnancies, you are at risk for bleeding, especially during labor as the cervix thins (effaces) and opens (dilates). • This can cause major blood loss in the mother. • For this reason, women with a placenta previa are usually delivered by cesarean section.
FREQUENT SIGNS & SYMPTOMS • Sudden, painless bleeding during the second or third trimester of pregnancy is the primary symptom. • Bleeding may begin slight or moderately and become severe and is bright red in color. Bleeding can occur as early as the 20 th week of pregnancy but is most common during the third trimester. • Cramping in some women. Signs of preterm labor. • One in 5 women with signs of placenta previa also has uterine contractions.
• Bleed from placenta previa may taper off and even stop for a while. However, it nearly always starts again days or weeks later. • Abnormal fetal position in the uterus. • Some women with placenta previa do not have any symptoms. In this case, placenta previa may only be diagnosed by an ultrasound done for other reasons.
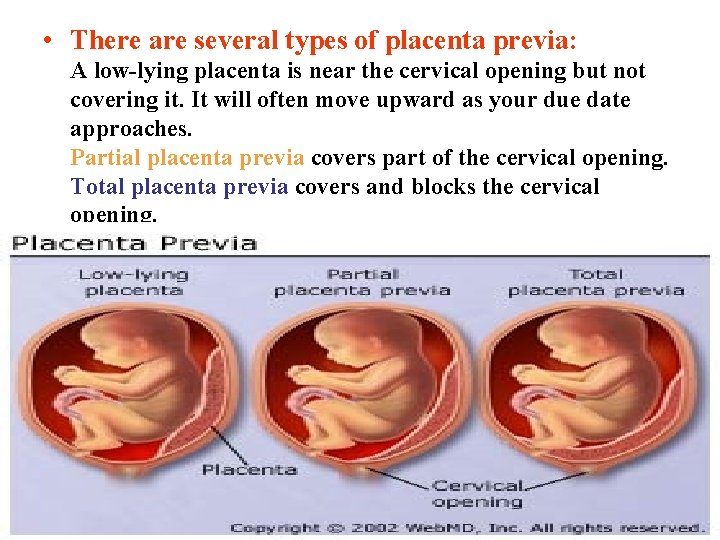
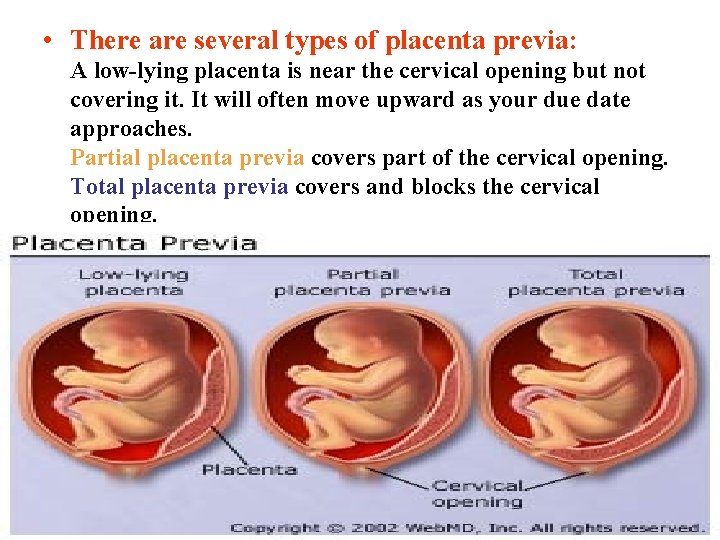
• There are several types of placenta previa: A low-lying placenta is near the cervical opening but not covering it. It will often move upward as your due date approaches. Partial placenta previa covers part of the cervical opening. Total placenta previa covers and blocks the cervical opening.



Ø Persistent excessive prenatal bleeding may seriously threaten the mother. The maternal (not fetal) circulation is the source of bleeding. Ø Vaginal or rectal examination or attempts to deliver from below may lacerate or separate the placenta, and as a consequence, the draining of blood (exsanguinating) maternal or fetal hemorrhage may occur. Ø Placenta previa is a major cause of maternal and perinatal morbidity and mortality.
What Causes It?
• The cause of placenta previa is usually unknown though it occurs more commonly among women who are older, smoke, have had children before, have had a cesarean section or other surgery on the uterus, or have scars inside the uterus. • Women with placenta previa - specifically if they have a placenta previa after having delivered a previous baby by cesarean section are at increased risk of placenta accreta, placenta increta, or placenta percreta.
• In placenta accreta, the placenta is firmly attached to the uterus; in placenta increta, the placenta has grown into the uterus; and in placenta percreta, it has grown through the uterus. This condition is often first suspected because the woman has both a previa and a prior cesarean section. It can be confirmed by ultrasound, CT scan, or MRI, though those tests are not completely reliable. • Women with one of these conditions usually require a hysterectomy after delivery of the baby, because the placenta does not separate from the uterus.
References • Pregnancy, Birth, and Parenthood. San Francisco: Jossey-Bass Inc. 306 p. Hamilton W. J. , Boyd J. D. , and Mossman H. W. 1962. • Human Embryology. Baltimore: The Williams & Wilkins Company. 493 p. Harrison R. G. 1963. A Textbook of Human Embryology. • Philadelphia: F. A. Davis Company. 248 p. Marieb E. N. 1998. Human Anatomy and Physiology. • California: Benjamin/Cummings Science Publishing Company, • Inc. 1030 -1107 p. Martin L. and Reeder S. 1991. Essentials of Maternity Nursing. • Philadelphia: J. B. Lippincott Company. 820 p. O’Rahilly R. and Muller F. 1987. Developmental Stages • in Human Embryos. Washington: Carnegie Institution of Washington Publication. 306 p.
Question? Maha H. Daghestani / King Saud University
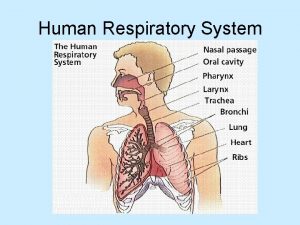
 Upper respiratory system
Upper respiratory system Tattoo anatomy and physiology
Tattoo anatomy and physiology Science olympiad anatomy and physiology
Science olympiad anatomy and physiology Structure anatomy and physiology in agriculture
Structure anatomy and physiology in agriculture Bone anatomy and physiology
Bone anatomy and physiology Anatomy and physiology of peptic ulcer
Anatomy and physiology of peptic ulcer Liver anatomy and physiology
Liver anatomy and physiology Epigastric region
Epigastric region Epigastric region
Epigastric region Anatomy and physiology of rbc
Anatomy and physiology of rbc Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Endomysium
Endomysium Http://anatomy and physiology
Http://anatomy and physiology Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Appendix anatomy and physiology
Appendix anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomy and physiology of swine
Anatomy and physiology of swine Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Teks anatomy and physiology
Teks anatomy and physiology Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Chapter 2 basic chemistry anatomy and physiology
Chapter 2 basic chemistry anatomy and physiology Stomach anatomy and physiology ppt
Stomach anatomy and physiology ppt Anatomy and physiology diabetes
Anatomy and physiology diabetes Heat and cold
Heat and cold Art labeling activity: figure 14.1 (3 of 3)
Art labeling activity: figure 14.1 (3 of 3) Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology
Anatomy and physiology Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology Anatomy and physiology ninth edition
Anatomy and physiology ninth edition Anatomy and physiology chapter 1
Anatomy and physiology chapter 1 Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Gi tract histology
Gi tract histology Anatomy and physiology
Anatomy and physiology Medial lateral distal proximal
Medial lateral distal proximal The speed at which the body consumes energy
The speed at which the body consumes energy Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Chapter 1 an introduction to anatomy and physiology
Chapter 1 an introduction to anatomy and physiology Anatomy and physiology exam 1
Anatomy and physiology exam 1 Welcome to anatomy and physiology
Welcome to anatomy and physiology Physiology of the foot and ankle
Physiology of the foot and ankle Skin cancer
Skin cancer Pancreas anatomy and physiology
Pancreas anatomy and physiology Anatomy and physiology vocabulary
Anatomy and physiology vocabulary Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Body landmarks diagram
Body landmarks diagram Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Figure 11-8 arteries
Figure 11-8 arteries Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Figure 10-1 blood
Figure 10-1 blood Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Uterus perimetrium
Uterus perimetrium Brain histology labeled
Brain histology labeled Anatomy and physiology of eye
Anatomy and physiology of eye Oblongata
Oblongata Irn.org anatomy and physiology
Irn.org anatomy and physiology Anatomy and physiology body parts
Anatomy and physiology body parts Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition Figure 14-1 anatomy and physiology
Figure 14-1 anatomy and physiology Anatomy and physiology of the retina
Anatomy and physiology of the retina Mucous connective tissue
Mucous connective tissue Anatomy and physiology of meningitis ppt
Anatomy and physiology of meningitis ppt Jeopardy anatomy and physiology game
Jeopardy anatomy and physiology game Anatomy and physiology definition
Anatomy and physiology definition Anatomy and physiology
Anatomy and physiology Nostrils
Nostrils Anatomy and physiology trivia
Anatomy and physiology trivia Cycloid scales
Cycloid scales Transverse fissure
Transverse fissure Anatomy and physiology
Anatomy and physiology Body planes and axes
Body planes and axes 2012 pearson education inc anatomy and physiology
2012 pearson education inc anatomy and physiology Esophagus wall
Esophagus wall Fish anatomy and physiology
Fish anatomy and physiology Anatomy and physiology chapter 8 skeletal system
Anatomy and physiology chapter 8 skeletal system Chapter 6 general anatomy and physiology
Chapter 6 general anatomy and physiology Cengage anatomy and physiology
Cengage anatomy and physiology Pse4u
Pse4u Villamentous cord insertion
Villamentous cord insertion Placental cotyledon
Placental cotyledon Placental migration
Placental migration