The Urinary System ANATOMY AND PHYSIOLOGY CHAPTER 15


- Slides: 31
The Urinary System ANATOMY AND PHYSIOLOGY CHAPTER 15 https: //www. youtube. com/watch? v=cc 8 s. Uv 2 Sua. Y&list=PL 3 n. YDHNcr. Nncbhhd m-8 C 9 NOWTLfy. Htb. PK&index=8
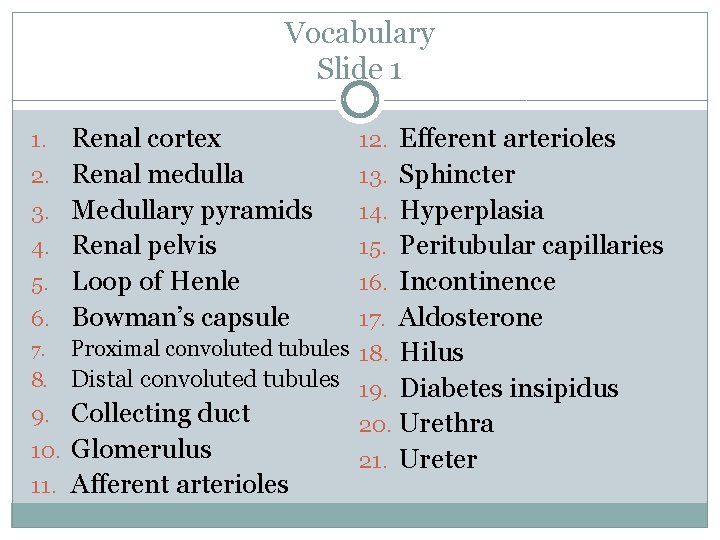
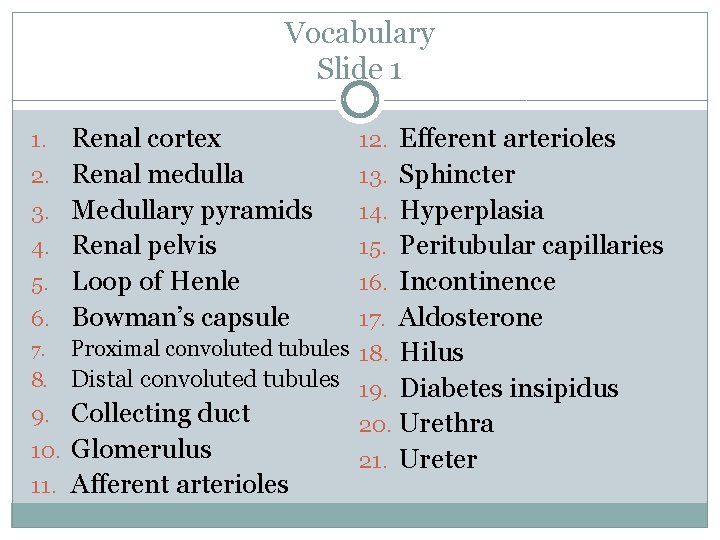
Vocabulary Slide 1 1. 2. 3. 4. 5. 6. Renal cortex Renal medulla Medullary pyramids Renal pelvis Loop of Henle Bowman’s capsule 12. Efferent arterioles 13. Sphincter 14. Hyperplasia 15. Peritubular capillaries 16. Incontinence 17. Aldosterone Proximal convoluted tubules 18. Hilus 8. Distal convoluted tubules 19. Diabetes insipidus 9. Collecting duct 20. Urethra 10. Glomerulus 21. Ureter 11. Afferent arterioles 7.
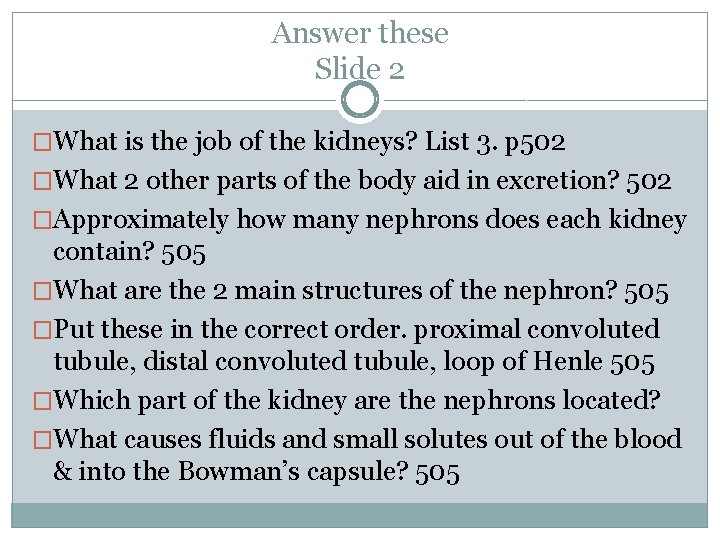
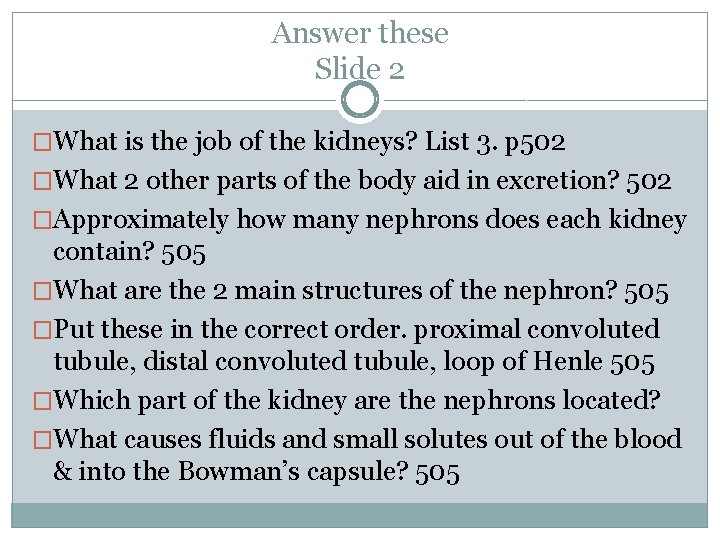
Answer these Slide 2 �What is the job of the kidneys? List 3. p 502 �What 2 other parts of the body aid in excretion? 502 �Approximately how many nephrons does each kidney contain? 505 �What are the 2 main structures of the nephron? 505 �Put these in the correct order. proximal convoluted tubule, distal convoluted tubule, loop of Henle 505 �Which part of the kidney are the nephrons located? �What causes fluids and small solutes out of the blood & into the Bowman’s capsule? 505
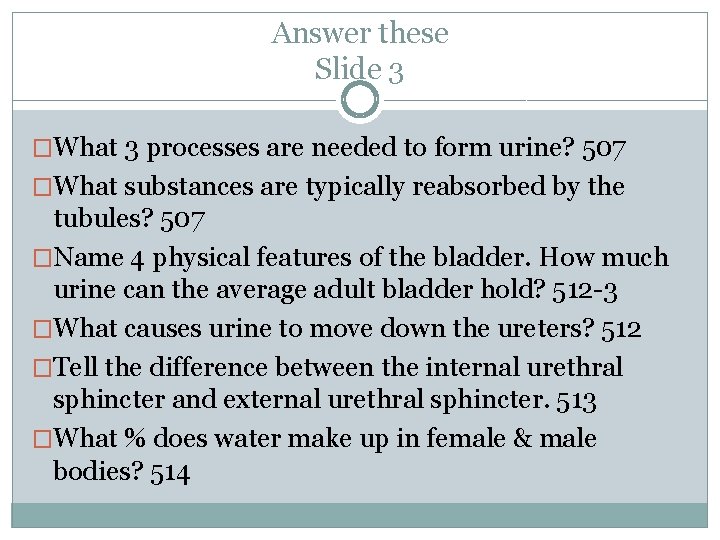
Answer these Slide 3 �What 3 processes are needed to form urine? 507 �What substances are typically reabsorbed by the tubules? 507 �Name 4 physical features of the bladder. How much urine can the average adult bladder hold? 512 -3 �What causes urine to move down the ureters? 512 �Tell the difference between the internal urethral sphincter and external urethral sphincter. 513 �What % does water make up in female & male bodies? 514
Slide 4 �Name 5 situations where incontinence is considered normal? 514 What is one time in life it is normal? 521 �What is the difference of intracellular fluid and extracellular fluid? 515 �When blood p. H rises, the respiratory system is _____. What does this do for the blood? 520 �What organ most controls blood p. H? �What is the average adult urine output per day? 521 �(T/F) Sexually transmitted diseases (STDs) may cause urinary tract infections. 521
Kidneys • • DISPOSE OF METABOLIC WASTE PRODUCTS REGULATE BLOOD VOLUME MANUFACTURE URINE CONVERT VITAMIN D FROM AN INACTIVE TO ACTIVE FORM
Nephrons and Urine Formation
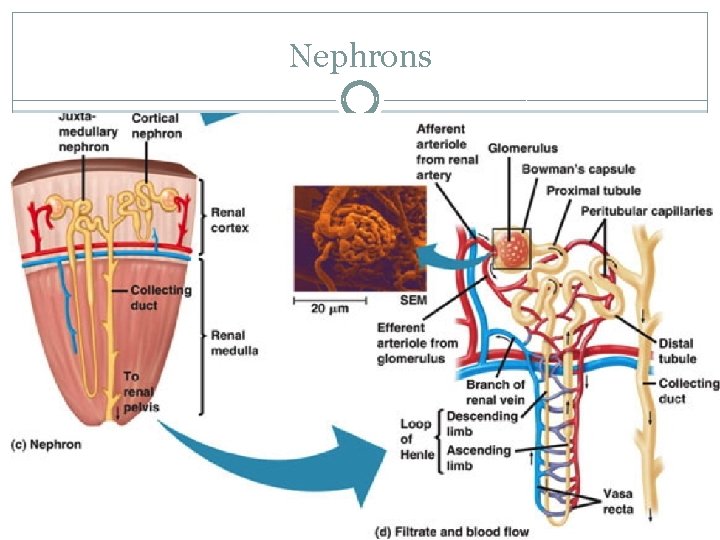
Nephrons �Structural and functional units of the kidneys �Each kidney contains over one million �Responsible forming urine
Nephrons
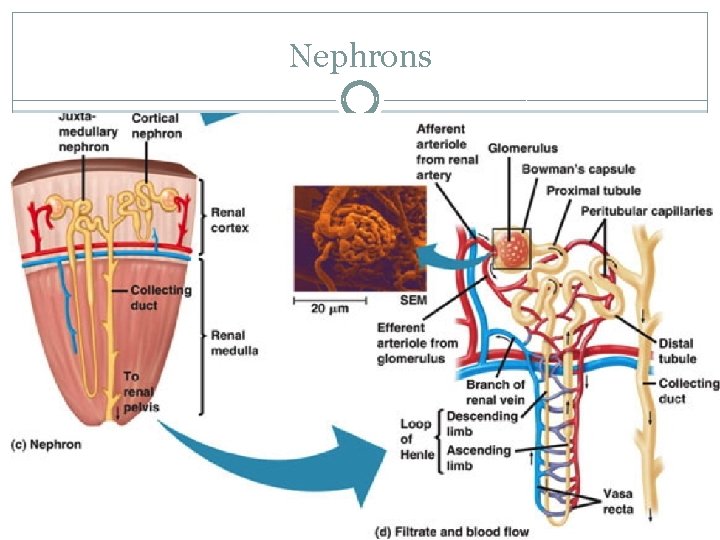
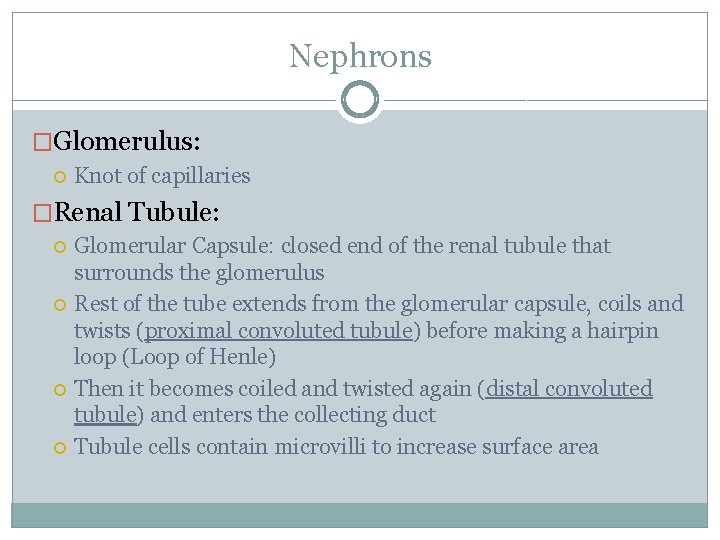
Nephrons �Glomerulus: Knot of capillaries �Renal Tubule: Glomerular Capsule: closed end of the renal tubule that surrounds the glomerulus Rest of the tube extends from the glomerular capsule, coils and twists (proximal convoluted tubule) before making a hairpin loop (Loop of Henle) Then it becomes coiled and twisted again (distal convoluted tubule) and enters the collecting duct Tubule cells contain microvilli to increase surface area
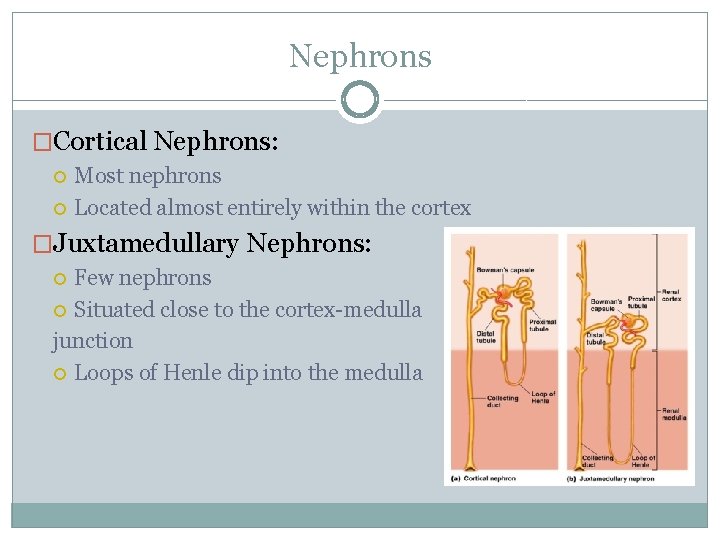
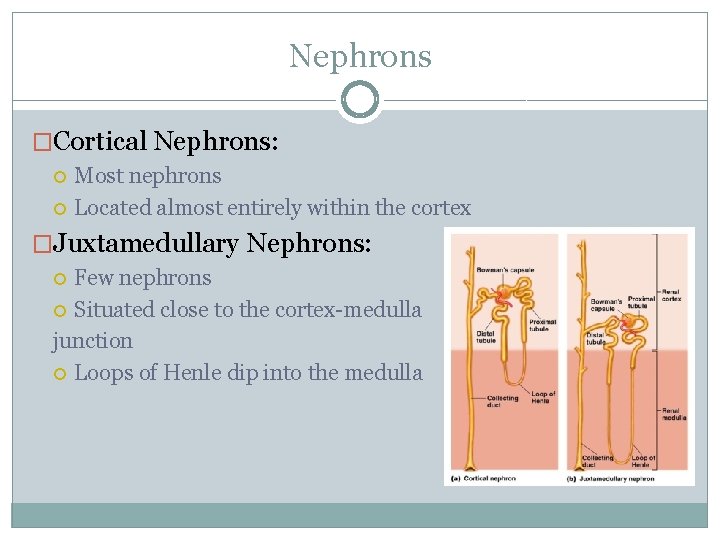
Nephrons �Cortical Nephrons: Most nephrons Located almost entirely within the cortex �Juxtamedullary Nephrons: Few nephrons Situated close to the cortex-medulla junction Loops of Henle dip into the medulla

Nephrons �Collecting Ducts: Each receive urine from many nephrons Run downward through the medullary pyramids Deliver the urine to the renal pelvis
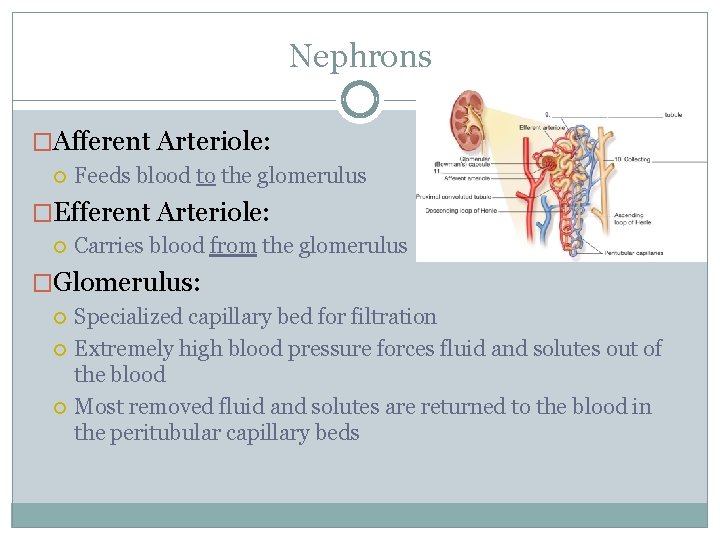
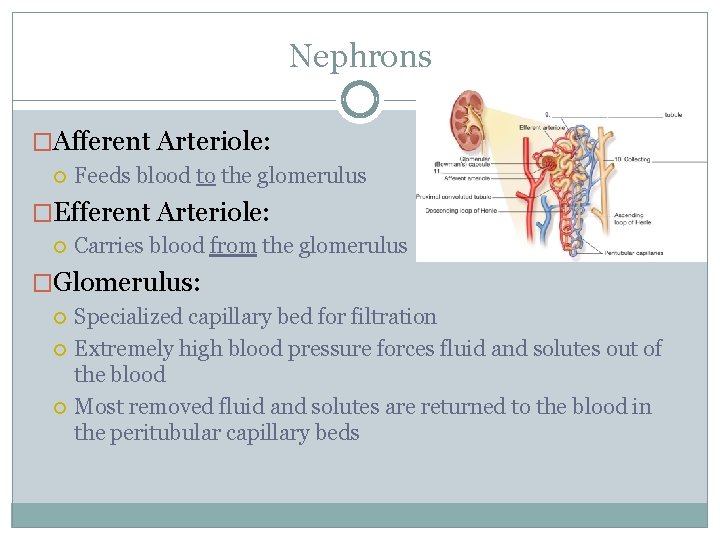
Nephrons �Afferent Arteriole: Feeds blood to the glomerulus �Efferent Arteriole: Carries blood from the glomerulus �Glomerulus: Specialized capillary bed for filtration Extremely high blood pressure forces fluid and solutes out of the blood Most removed fluid and solutes are returned to the blood in the peritubular capillary beds
Urine
Urine Formation �Three Major Processes: Filtration Tubular Reabsorption Tubular Secretion
Urine Formation �Filtration: Nonselective and passive Filtrate = blood plasma without blood proteins If blood cells or proteins are found in the urine = sign that glomerular filters are malfunctioning Filtrate formation stops if blood pressure drops too low
Urine Formation �Tubular Reabsorption: Filtration removes many useful substances from the blood that must be reclaimed Begins as soon as the filtrate enters the proximal convoluted tubule Some is passive, most is active Needed Substances in the blood: water, glucose, amino acids, and ions Nitrogenous waste products are poorly reabsorbed: urea, uric acid, & creatinine
Urine Formation �Tubular Secretion: Reabsorption in reverse Gets rid of substances not already in the filtrate, such as certain drugs Moves from blood peritubular capillaries into tubules Additional means for controlling blood p. H
Characteristics of Urine �In 24 hours the kidneys filter 150 -180 L of blood plasma and produces 1 -1. 8 L of urine �Freshly voided urine is generally clear and pale to deep yellow �Urochrome pigment from destruction of hemoglobin causes yellow color �More solutes = deeper color �More dense than water �Typically contain ammonia �Sterile (free from bacteria or microorganisms)
Characteristics of Urine �When formed: urine is sterile with a slightly aromatic odor �When allowed to stand: ammonia odor due to bacteria �Some drugs, vegetables, and diseases alter the odor of urine
Characteristics of Urine �Usually slightly acidic – p. H 6 �Lots of protein and whole wheat = more acidic �Vegetarian diet = more basic
Characteristics of Urine �Urine is more dense than distilled water �Specific Gravity: compare how much heavier urine is than distilled water �Ranges from 1. 001 to 1. 035 (dilute to concentrated) Generally low when a person: drinks excess fluids, uses diuretics, or has chronic renal failure Generally high when a person: has inadequate fluid intake, fever, or kidney inflammation
Characteristics of Urine �Solutes Normally Found in Urine: Sodium and potassium ions Urea Uric acid Creatinine Ammonia Bicarbonate ions Other ions
Characteristics of Urine �Substances NOT Normally Found in Urine: Glucose Blood proteins Red blood cells Hemoglobin White blood cells (pus) Bile
Fluid, Electrolyte, and Acid. Base Balance

Blood Composition �Four Major Roles of the Kidneys in Maintaining Stable Blood Composition: Excretion of nitrogenous wastes Maintaining water balance Maintaining electrolyte balance Ensuring proper blood p. H
Body Fluids and Fluid Compartments �Three Major Fluid Compartments in the Body: Intracellular Fluid � Contained within living cells Interstitial Fluid � Fluid found between living cells, CSF, serous fluid, humors of the eye, lymph, etc Plasma � Blood plasma
Water In and Water Out �Water Intake: 10% Metabolism 30% Food 60% Beverages �Water Output: 4% Feces 8% Sweat 28% Loss through skin and lungs 60% Urine
NASA recycles in space �https: //www. youtube. com/watch? v=BCj. H 3 k 5 g. ODI &list=PL 3 n. YDHNcr. Nncbhhdm 8 C 9 NOWTLfy. Htb. PK&index=11 Water recycling on the ISS �https: //www. youtube. com/watch? v=DX 7 HKzk 7 x. Gg &index=10&list=PL 3 n. YDHNcr. Nncbhhdm 8 C 9 NOWTLfy. Htb. PK Recycling urine
Regulation of Reabsorption �When blood volume drops, arterial blood pressure drops, and filtrate formation drops �Osmoreceptors in the hypothalamus react to changes in blood composition by becoming more active �Antidiuretic Hormone: prevents excessive water loss in urine, causes the collecting ducts to reabsorb more water
Maintaining Acid-Base Balance of Blood �Blood p. H must remain between 7. 35 and 7. 45 �Respiratory System Controls Release more carbon dioxide when blood p. H drops Release less carbon dioxide when blood p. H rises �Bicarbonate Buffer System Mixture of carbonic acid and sodium bicarbonate Weak acid minimizes effect of bases Conjugate base minimizes effect of acids