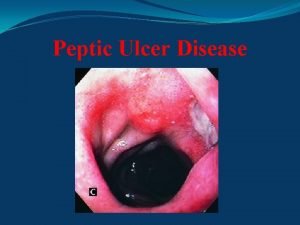
Peptic Ulcer Disease Cengiz Pata MD Dept Gastroenterology






- Slides: 67
Peptic Ulcer Disease Cengiz Pata, MD Dept. Gastroenterology, Yeditepe University, Medical center
Case • 30 year old male • Epigatsric pain radiating to the back Questions? Possible diagnosis Deferential diagnosis Possible complications
Case • Pain: • What type of pain? How often? Awakes at night? Relation to food? • Complications: • Vomiting? (obstruction? ) Stools? (melena? ) • Common deferential diagnosis: • Pnacreatobiliary disease Dyspepsia Tumors
Case • Next diagnostic step? • Endoscopy Abdominal US UGI? • DU Ulcer detected next step? • Test for H. pylori Exclude NSAID use Rare – assess gastrin, mainly in unusual cases

(Benign gastric ulcer (B
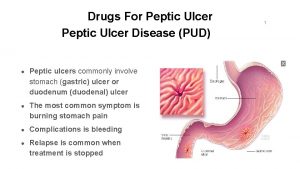
Peptic Ulcer • A defect in the gastrointestinal mucosa extending through the muscularis mucosa. • Two main forms: 1) Helicobacter associated 2) NSAID associated ( Steroids alone – no additional risk, Increased risk when combined with NSAIDS)
Peptic Ulceration : Additional Causes • Acid hypersecretion: Gastrinoma ( ZE) Systemic mastocytosis Basophilia in myeloproliferative disorders • Viral Herpes simplex CMV ( mainly in immune compromised)
Peptic Ulceration : Additional Causes • Vascular Insufficiency ( including due to crack cocaine) • Radiation induced • Chemotherapy induced • Stress ulceration
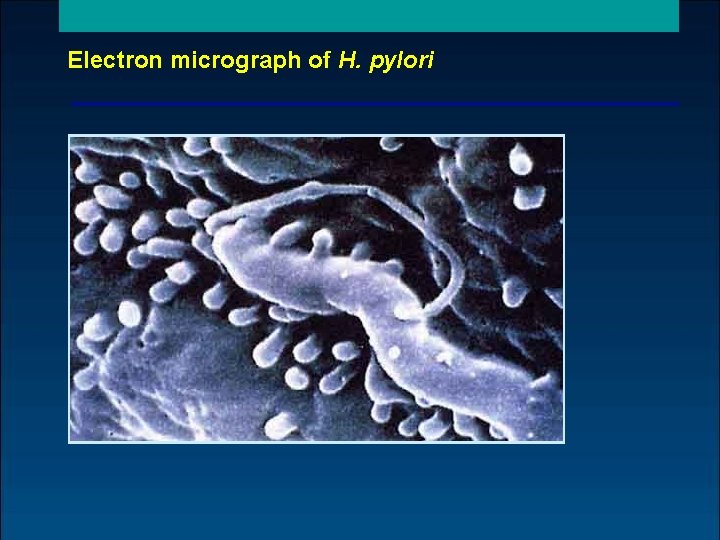
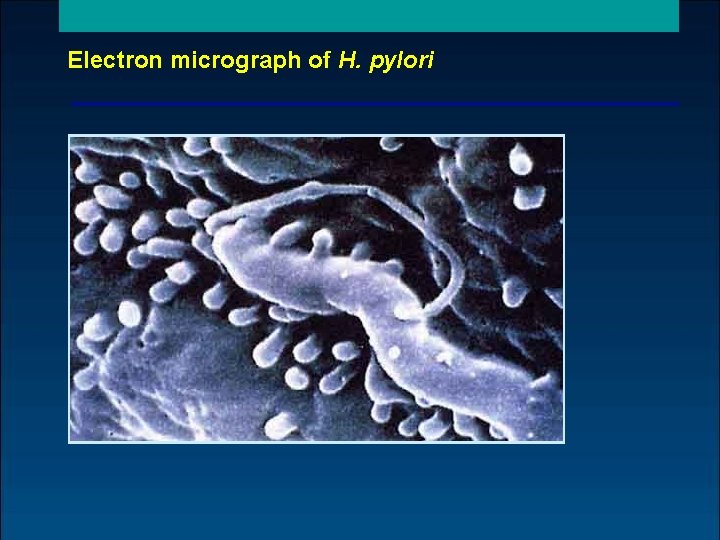
Electron micrograph of H. pylori
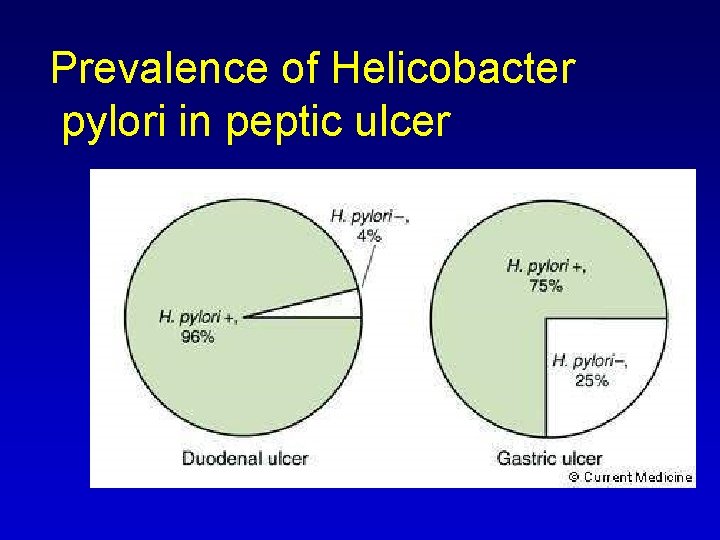
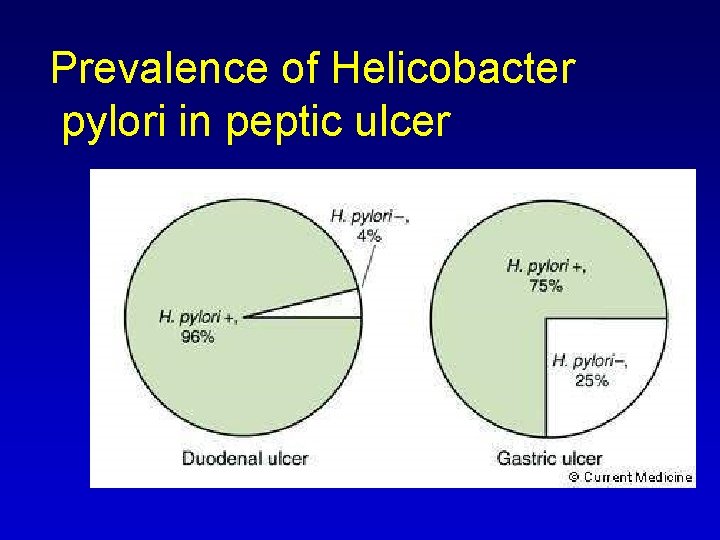
Prevalence of Helicobacter pylori in peptic ulcer
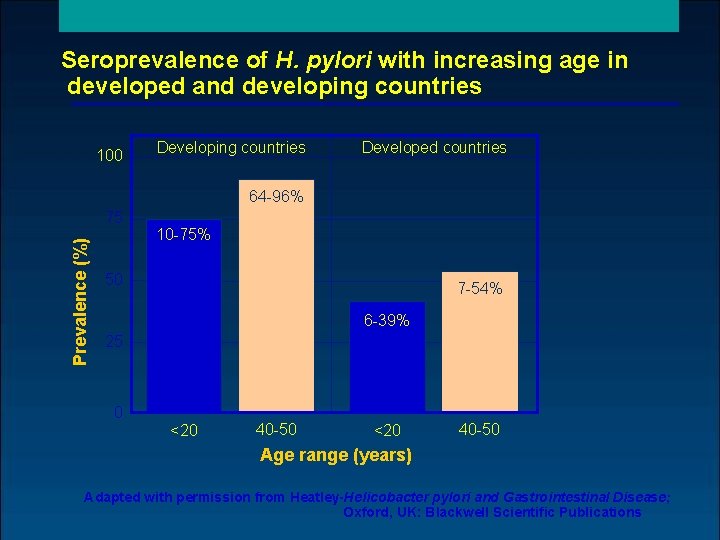
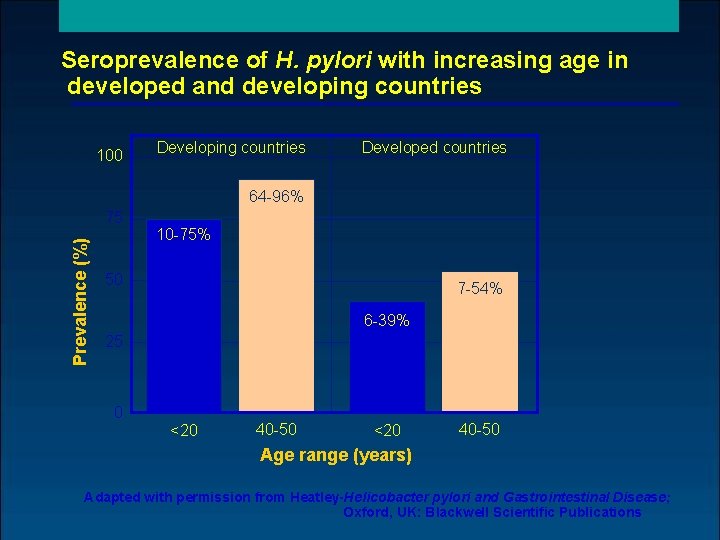
Seroprevalence of H. pylori with increasing age in developed and developing countries 100 Developing countries Developed countries 64 96% Prevalence (%) 75 10 75% 50 7 54% 6 39% 25 0 <20 40 50 Age range (years) Adapted with permission from Heatley-Helicobacter pylori and Gastrointestinal Disease; Oxford, UK: Blackwell Scientific Publications
Risk factors for H. pylori infection • Age • Country of origin • Socio economic status poor housing bed sharing overcrowding large families
Modes of transmission of H. pylori infection • Zoonosis unlikely • Environment unlikely • Person to person oral likely gastro oral likely faecal oral likely
H. pylori infection and disease associations • Chronic gastritis • Duodenal ulcer • Benign gastric ulcer • Gastric carcinoma • Gastric MALT and non Hodgkin‘s lymphoma • Ménétrier‘s disease
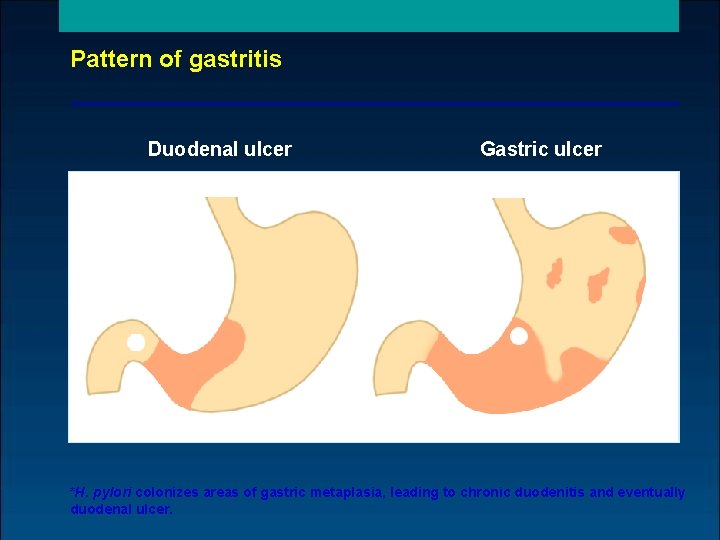
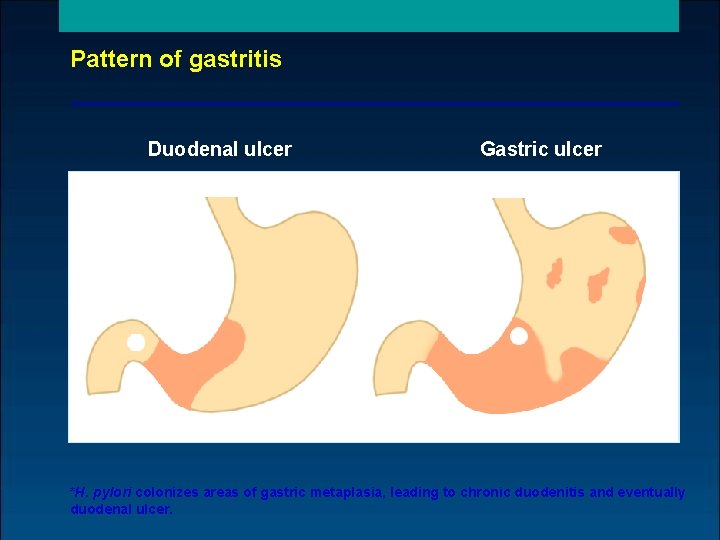
Pattern of gastritis Duodenal ulcer Gastric ulcer Corpusitis * Antral gastritis *H. pylori colonizes areas of gastric metaplasia, leading to chronic duodenitis and eventually duodenal ulcer.

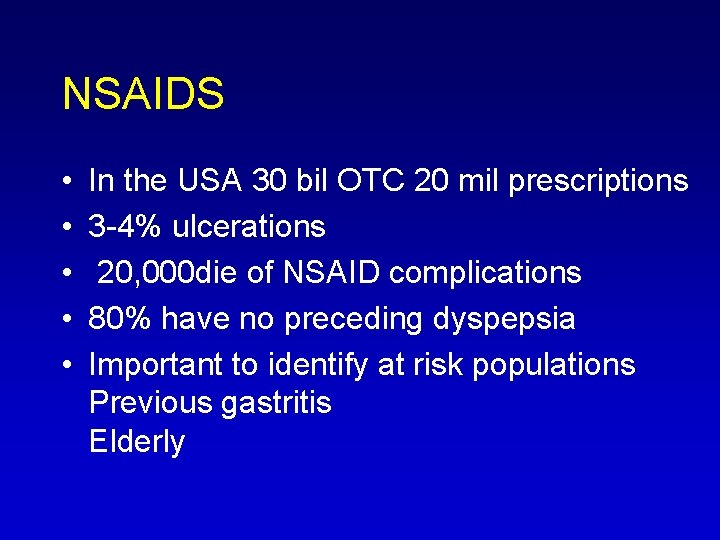
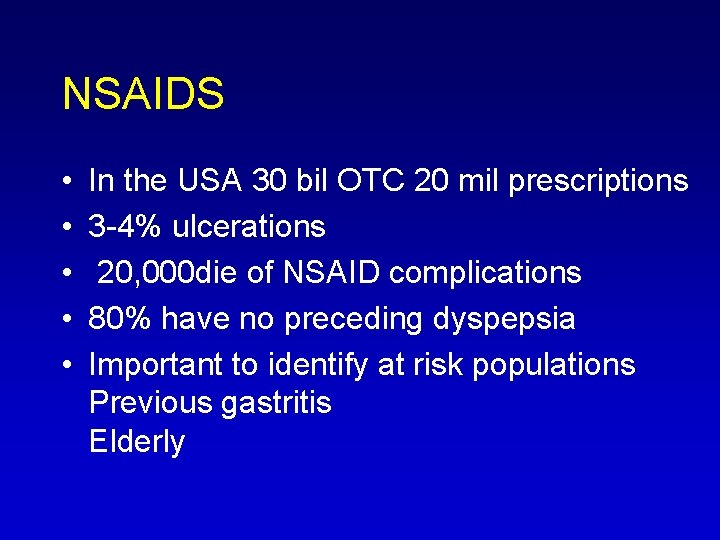
NSAIDS • • • In the USA 30 bil OTC 20 mil prescriptions 3 4% ulcerations 20, 000 die of NSAID complications 80% have no preceding dyspepsia Important to identify at risk populations Previous gastritis Elderly
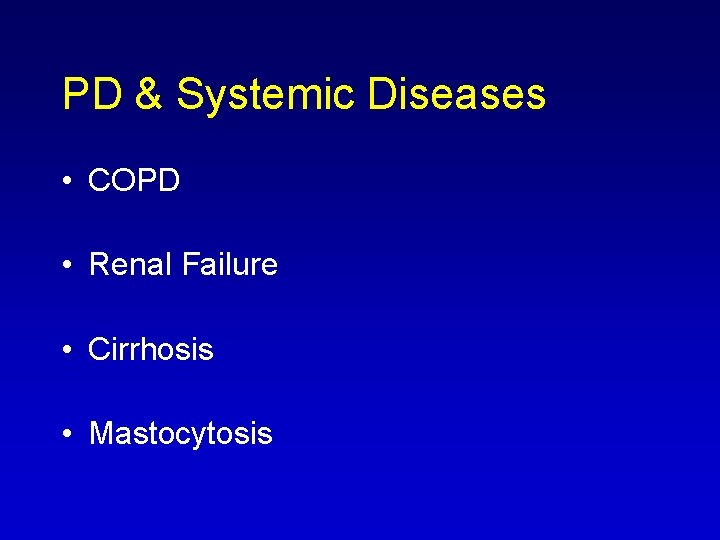
PD & Systemic Diseases • COPD • Renal Failure • Cirrhosis • Mastocytosis
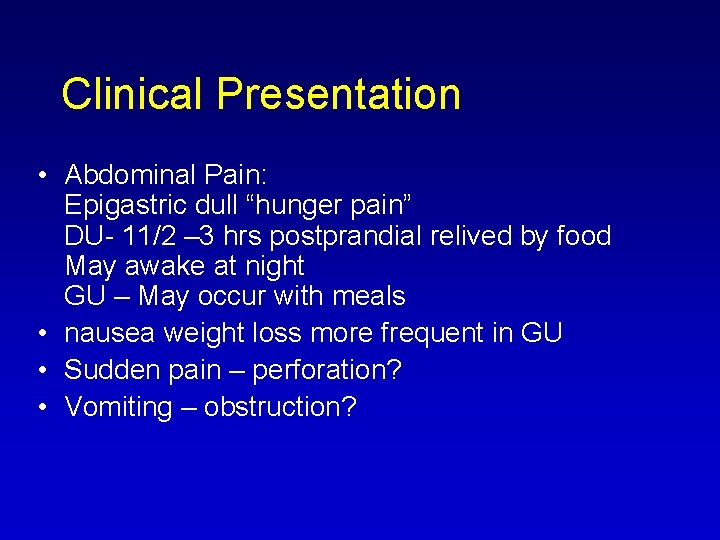
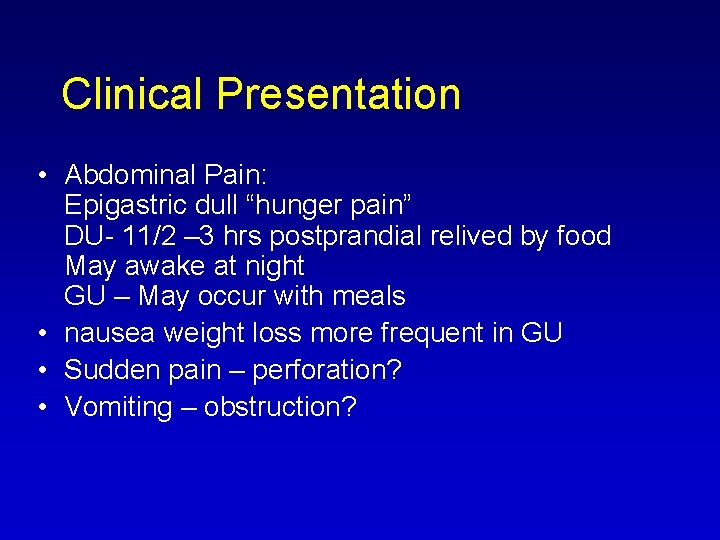
Clinical Presentation • Abdominal Pain: Epigastric dull “hunger pain” DU 11/2 – 3 hrs postprandial relived by food May awake at night GU – May occur with meals • nausea weight loss more frequent in GU • Sudden pain – perforation? • Vomiting – obstruction?
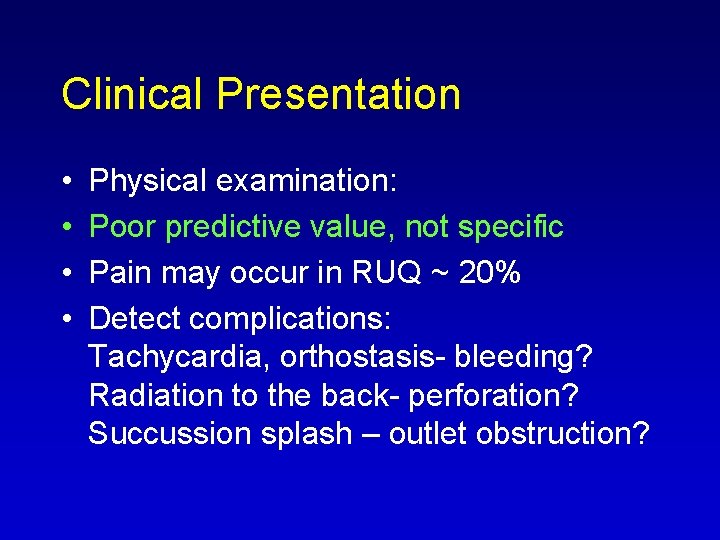
Clinical Presentation • • Physical examination: Poor predictive value, not specific Pain may occur in RUQ ~ 20% Detect complications: Tachycardia, orthostasis bleeding? Radiation to the back perforation? Succussion splash – outlet obstruction?
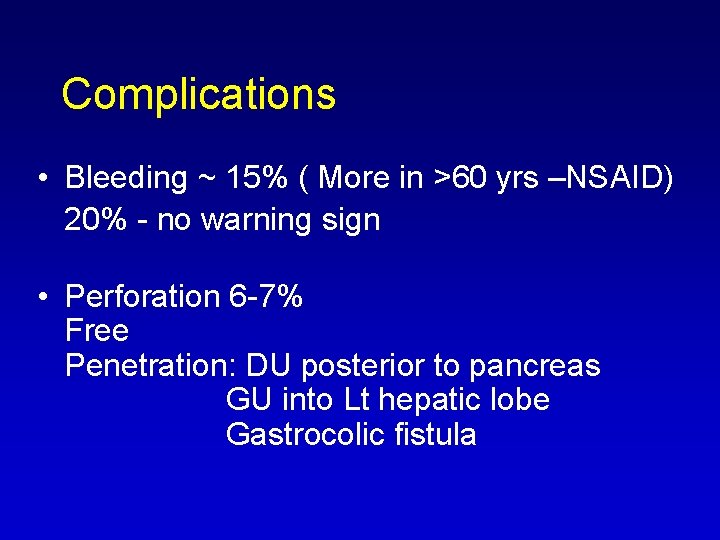
Complications • Bleeding ~ 15% ( More in >60 yrs –NSAID) 20% no warning sign • Perforation 6 7% Free Penetration: DU posterior to pancreas GU into Lt hepatic lobe Gastrocolic fistula
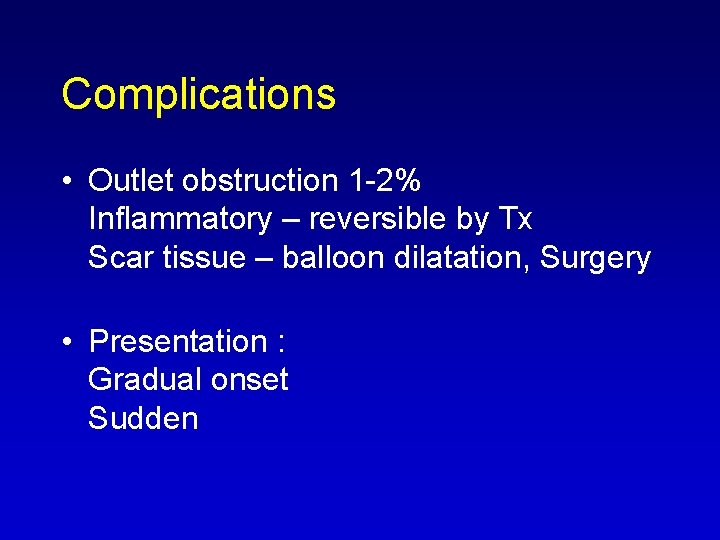
Complications • Outlet obstruction 1 2% Inflammatory – reversible by Tx Scar tissue – balloon dilatation, Surgery • Presentation : Gradual onset Sudden
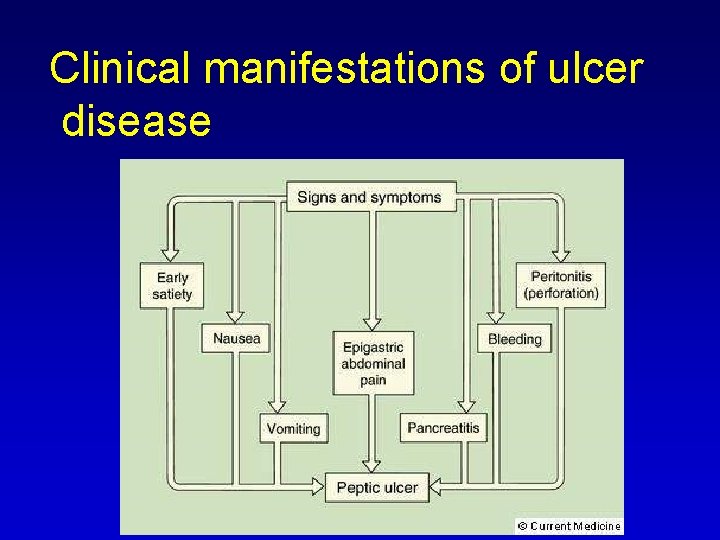
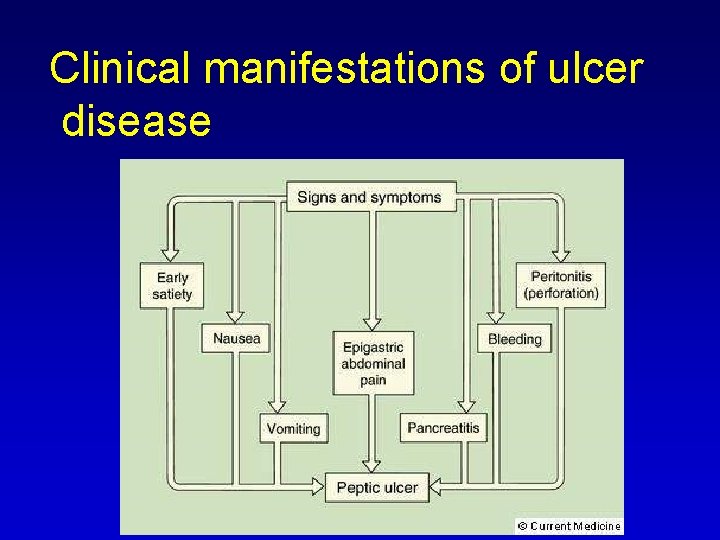
Clinical manifestations of ulcer disease
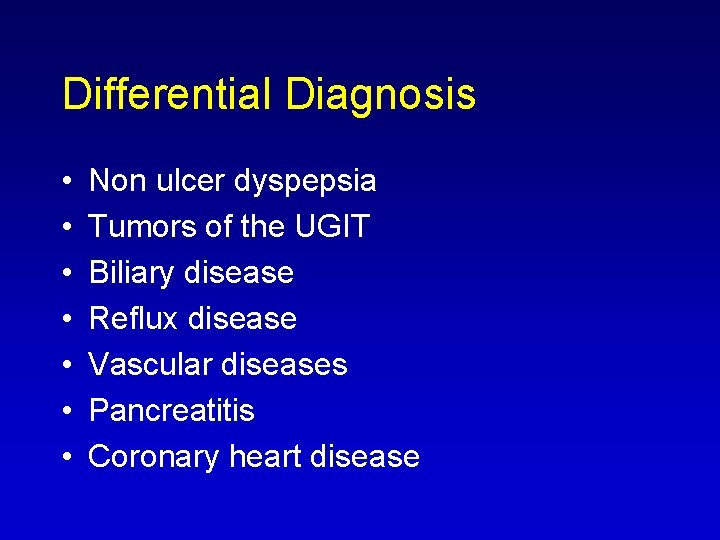
Differential Diagnosis • • Non ulcer dyspepsia Tumors of the UGIT Biliary disease Reflux disease Vascular diseases Pancreatitis Coronary heart disease
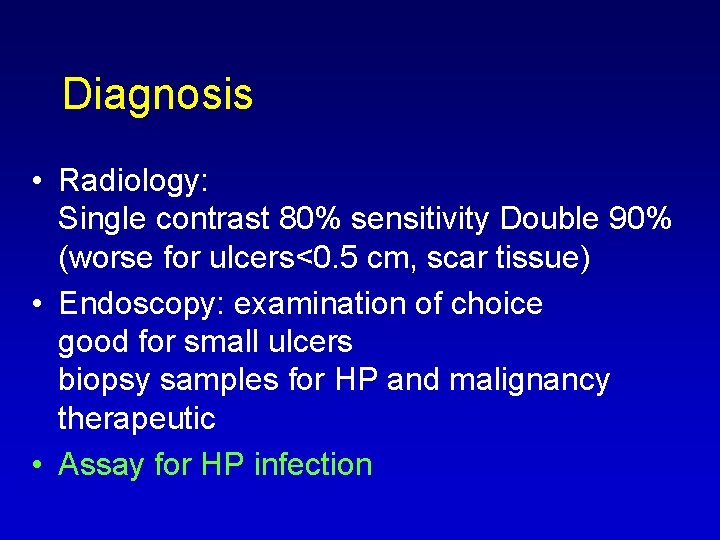
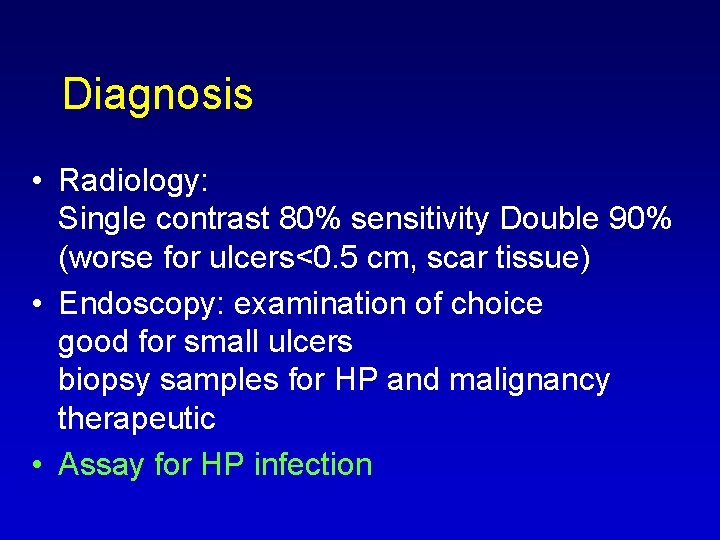
Diagnosis • Radiology: Single contrast 80% sensitivity Double 90% (worse for ulcers<0. 5 cm, scar tissue) • Endoscopy: examination of choice good for small ulcers biopsy samples for HP and malignancy therapeutic • Assay for HP infection
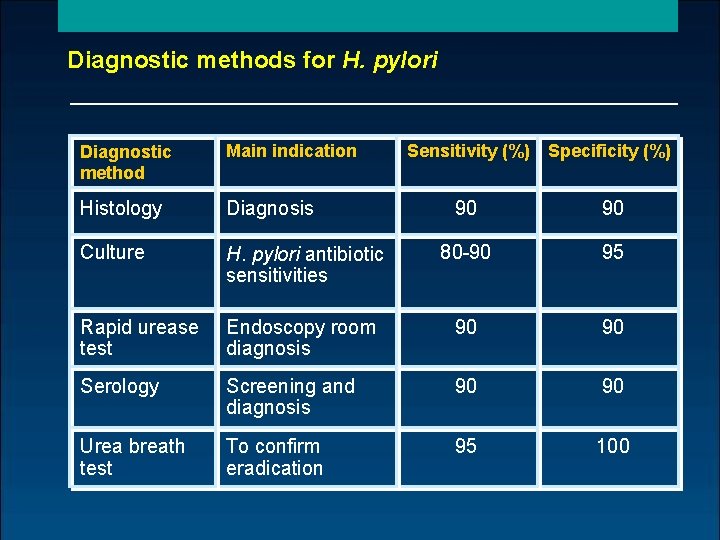
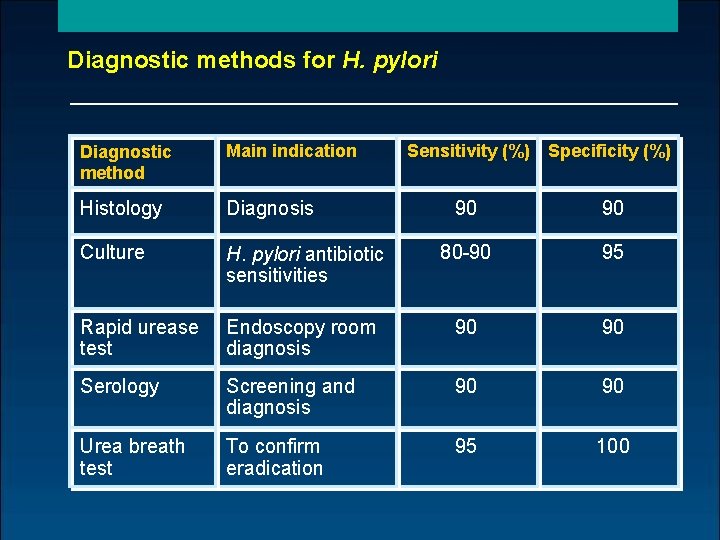
Diagnostic methods for H. pylori Diagnostic method Main indication Sensitivity (%) Specificity (%) Histology Diagnosis 90 90 Culture H. pylori antibiotic sensitivities 80 90 95 Rapid urease test Endoscopy room diagnosis 90 90 Serology Screening and diagnosis 90 90 Urea breath test To confirm eradication 95 100
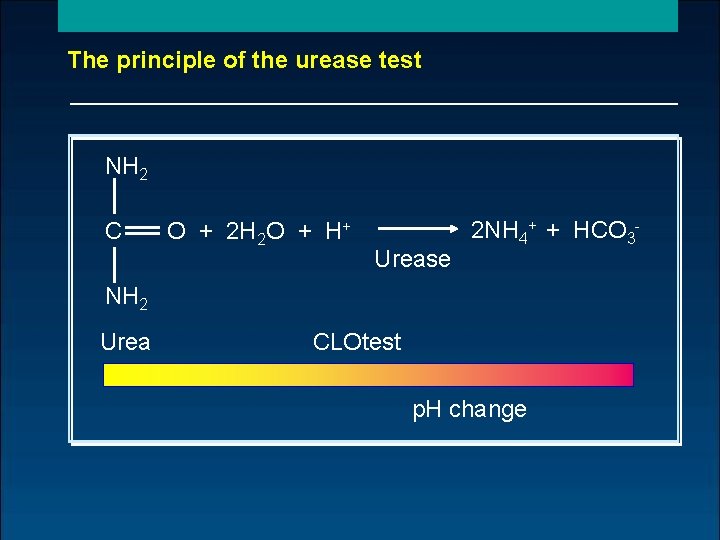
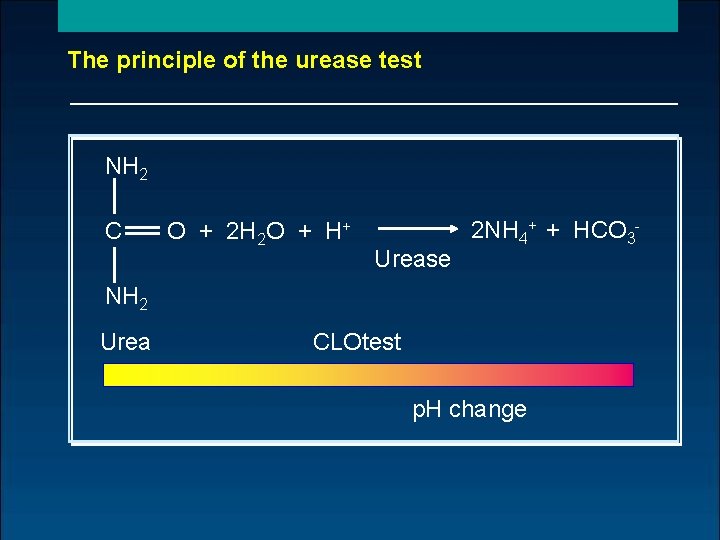
The principle of the urease test NH 2 C O + 2 H 2 O + H+ Urease 2 NH 4+ + HCO 3 NH 2 Urea CLOtest p. H change
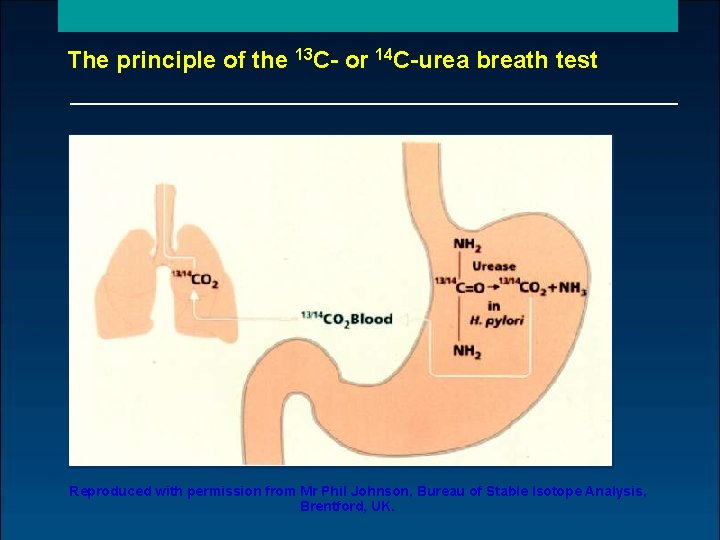
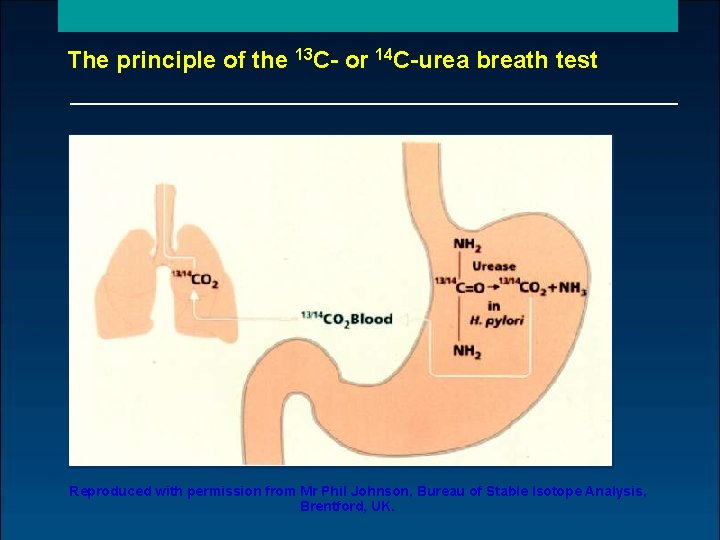
The principle of the 13 C- or 14 C-urea breath test Reproduced with permission from Mr Phil Johnson, Bureau of Stable Isotope Analysis, Brentford, UK.
Therapy • Treat H. pylori • Healing by inhibition of acid secretion: H 2 receptor antagonists (H 2 RA) Proton Pump inhibitors ( PPI) Anti Acid • Cytoprotection Sucralfate Anti Acid Bismuth Based Prostaglandin Analogs
Therapy of DU • H 2 RA – Cure in 80% at 4 wks ~95% at 8 wks Split and once daily equally effective • PPI Cure in 60 93% at 2 wks 80 100 % at 4 wks • Omeprazole Vs ranitidine 14% advantage at 2 wks 9% advantage 4 wks
Therapy of GU • Suppress acid by H 2 RA or PPI • Advantage of PPI less apparent • Sucralfate comparable to H 2 RA • Prepyloric ulcers may resemble more DU in terms of response to acid suppression
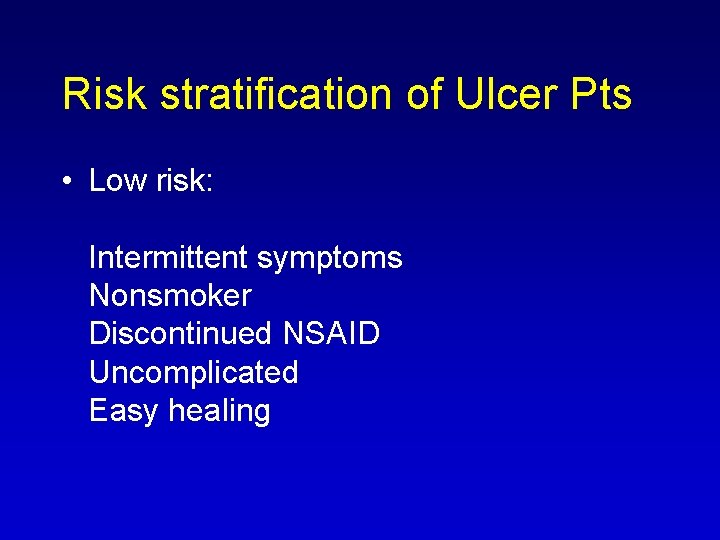
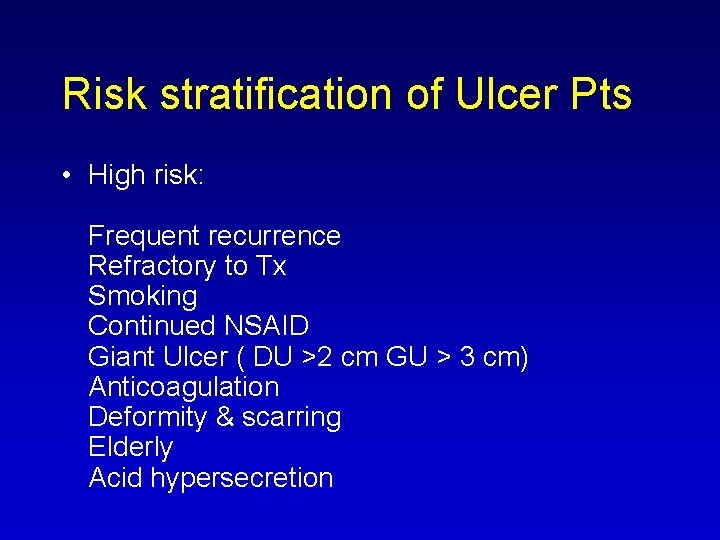
Risk stratification of Ulcer Pts • Low risk: Intermittent symptoms Nonsmoker Discontinued NSAID Uncomplicated Easy healing
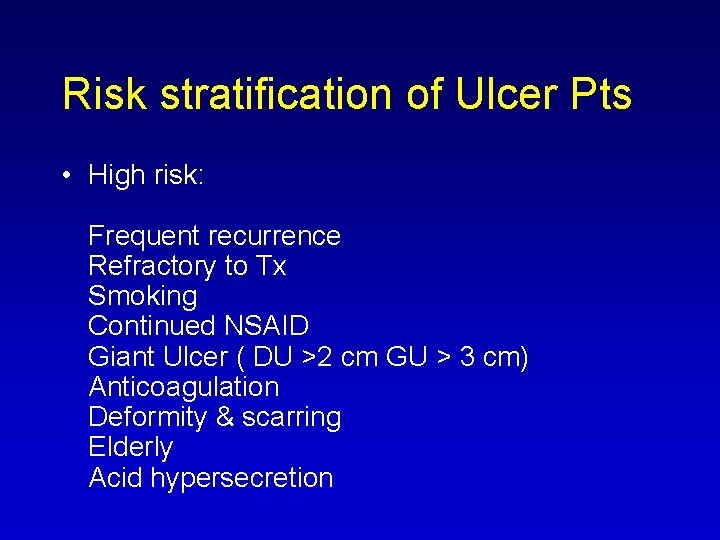
Risk stratification of Ulcer Pts • High risk: Frequent recurrence Refractory to Tx Smoking Continued NSAID Giant Ulcer ( DU >2 cm GU > 3 cm) Anticoagulation Deformity & scarring Elderly Acid hypersecretion
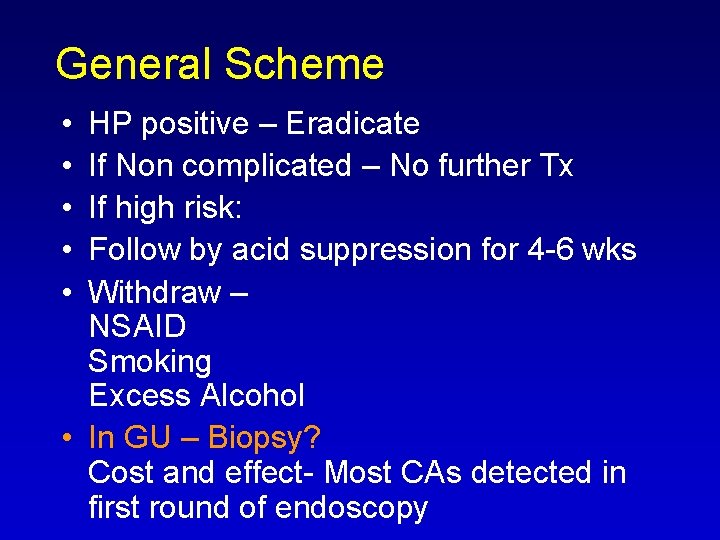
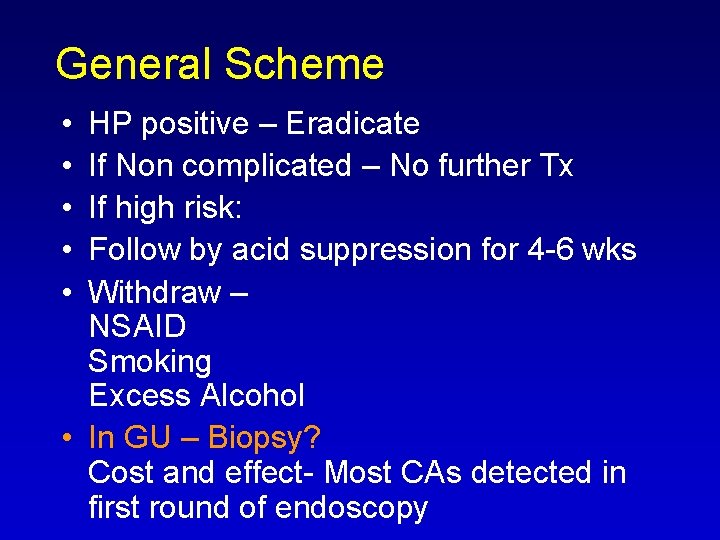
General Scheme • • • HP positive – Eradicate If Non complicated – No further Tx If high risk: Follow by acid suppression for 4 6 wks Withdraw – NSAID Smoking Excess Alcohol • In GU – Biopsy? Cost and effect Most CAs detected in first round of endoscopy
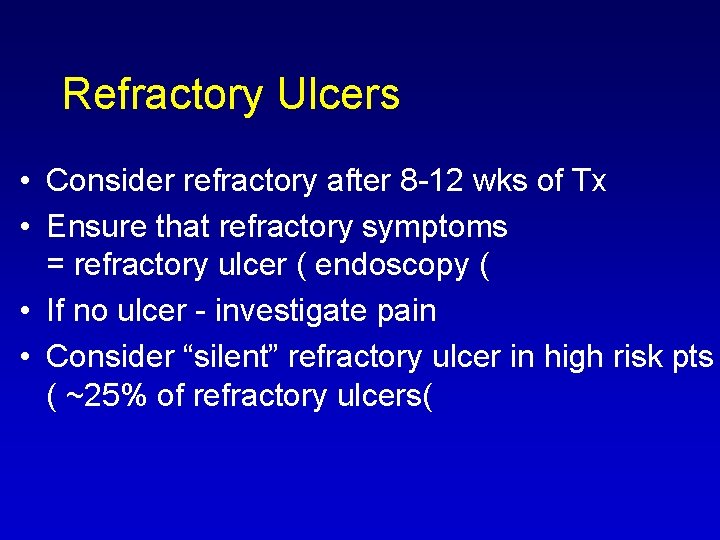
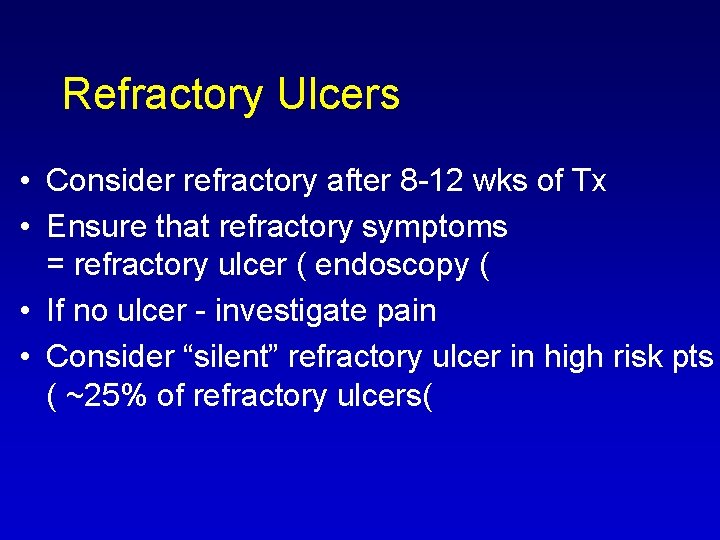
Refractory Ulcers • Consider refractory after 8 12 wks of Tx • Ensure that refractory symptoms = refractory ulcer ( endoscopy ( • If no ulcer investigate pain • Consider “silent” refractory ulcer in high risk pts ( ~25% of refractory ulcers(
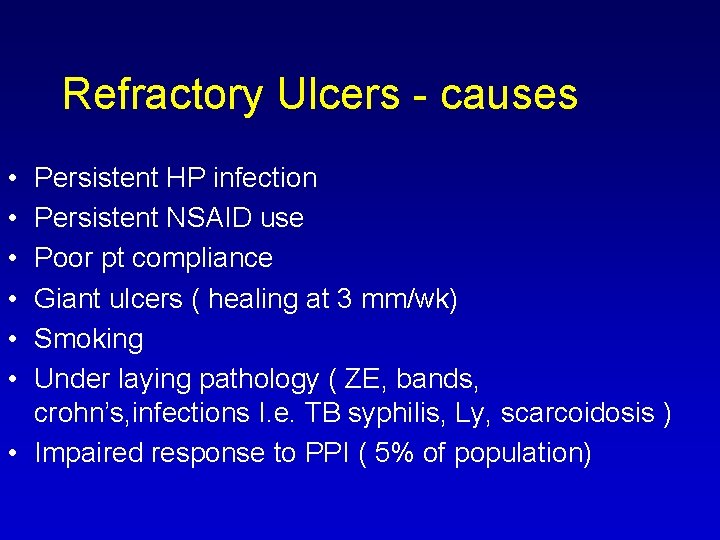
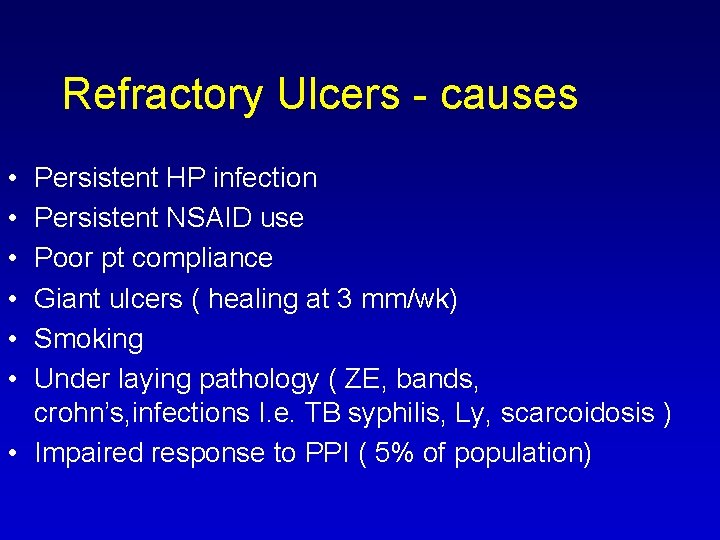
Refractory Ulcers causes • • • Persistent HP infection Persistent NSAID use Poor pt compliance Giant ulcers ( healing at 3 mm/wk) Smoking Under laying pathology ( ZE, bands, crohn’s, infections I. e. TB syphilis, Ly, scarcoidosis ) • Impaired response to PPI ( 5% of population)
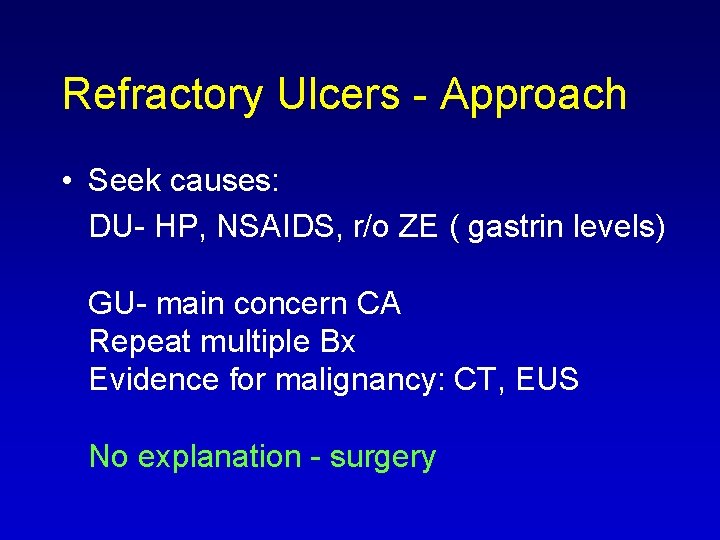
Refractory Ulcers Approach • Seek causes: DU HP, NSAIDS, r/o ZE ( gastrin levels) GU main concern CA Repeat multiple Bx Evidence for malignancy: CT, EUS No explanation surgery
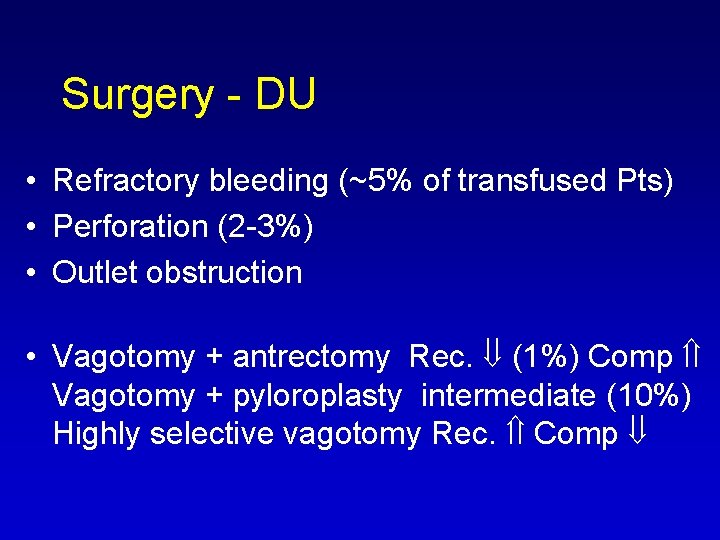
Surgery DU • Refractory bleeding (~5% of transfused Pts) • Perforation (2 3%) • Outlet obstruction • Vagotomy + antrectomy Rec. (1%) Comp Vagotomy + pyloroplasty intermediate (10%) Highly selective vagotomy Rec. Comp

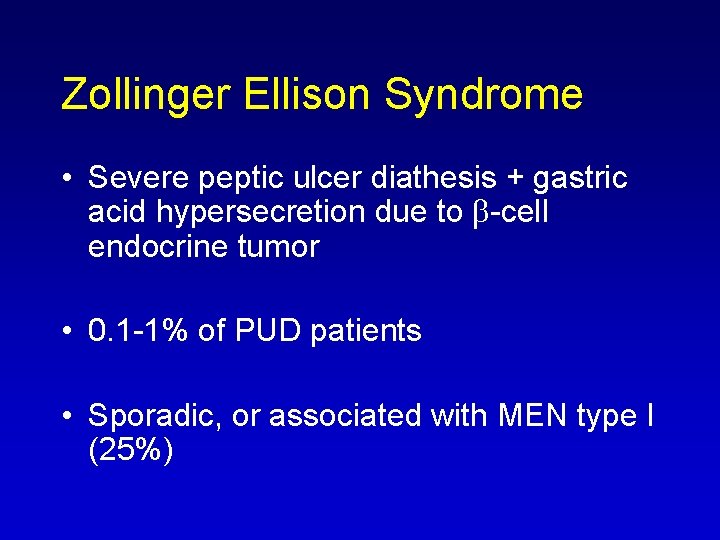
Zollinger Ellison Syndrome • Severe peptic ulcer diathesis + gastric acid hypersecretion due to b cell endocrine tumor • 0. 1 1% of PUD patients • Sporadic, or associated with MEN type I (25%)
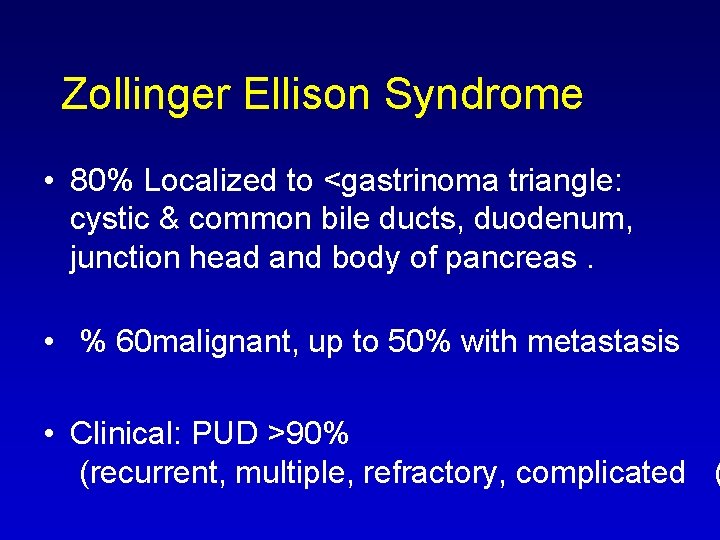
Zollinger Ellison Syndrome • 80% Localized to <gastrinoma triangle: cystic & common bile ducts, duodenum, junction head and body of pancreas. • % 60 malignant, up to 50% with metastasis • Clinical: PUD >90% (recurrent, multiple, refractory, complicated (
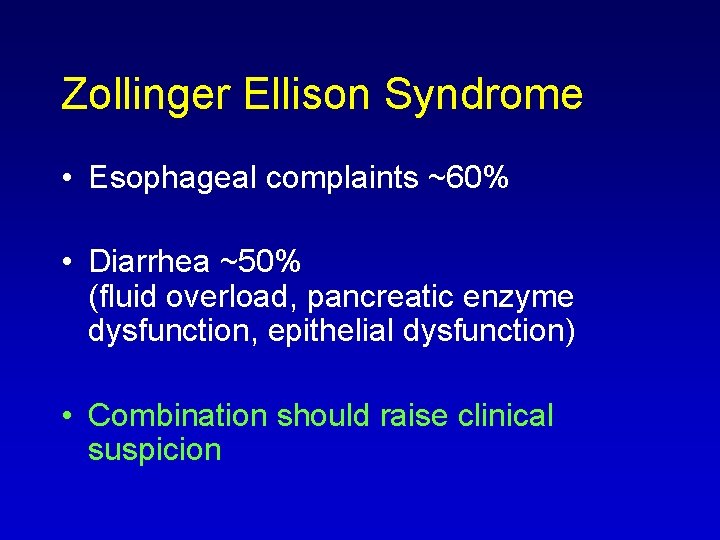
Zollinger Ellison Syndrome • Esophageal complaints ~60% • Diarrhea ~50% (fluid overload, pancreatic enzyme dysfunction, epithelial dysfunction) • Combination should raise clinical suspicion
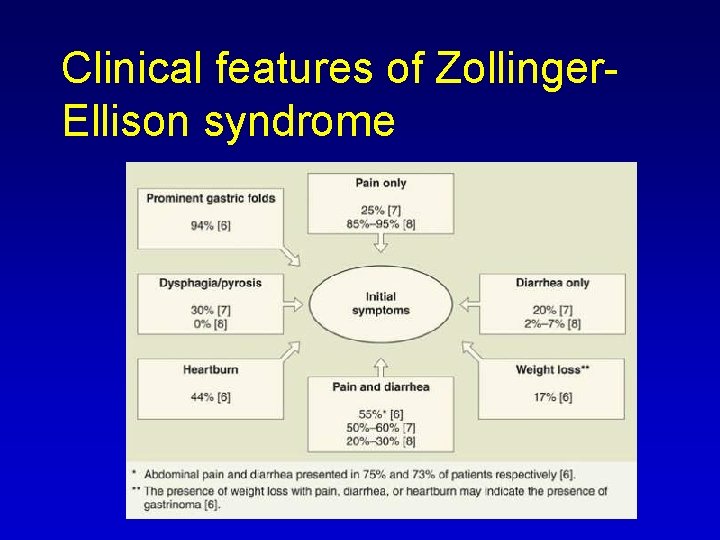
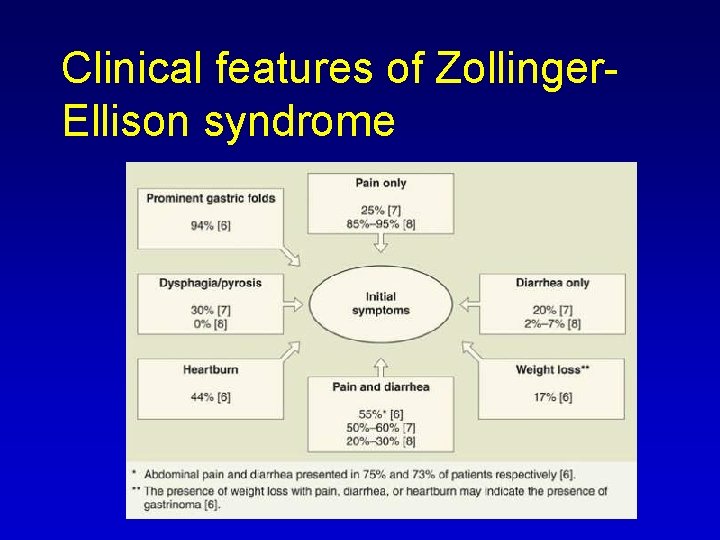
Clinical features of Zollinger Ellison syndrome
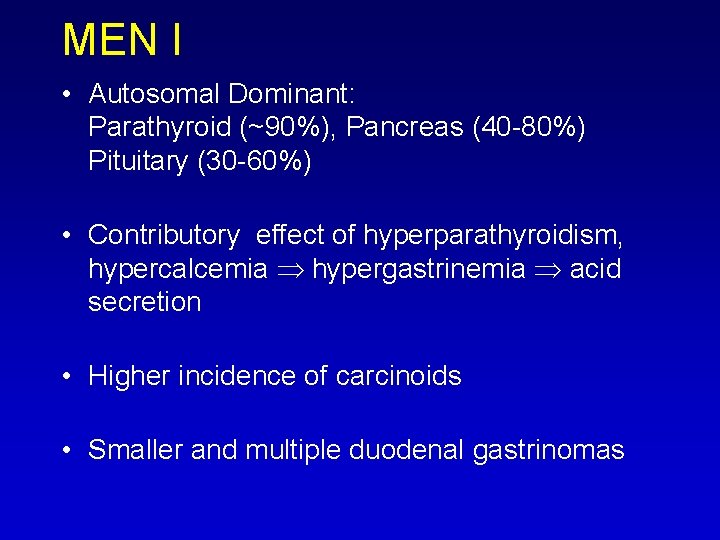
MEN I • Autosomal Dominant: Parathyroid (~90%), Pancreas (40 80%) Pituitary (30 60%) • Contributory effect of hyperparathyroidism, hypercalcemia hypergastrinemia acid secretion • Higher incidence of carcinoids • Smaller and multiple duodenal gastrinomas
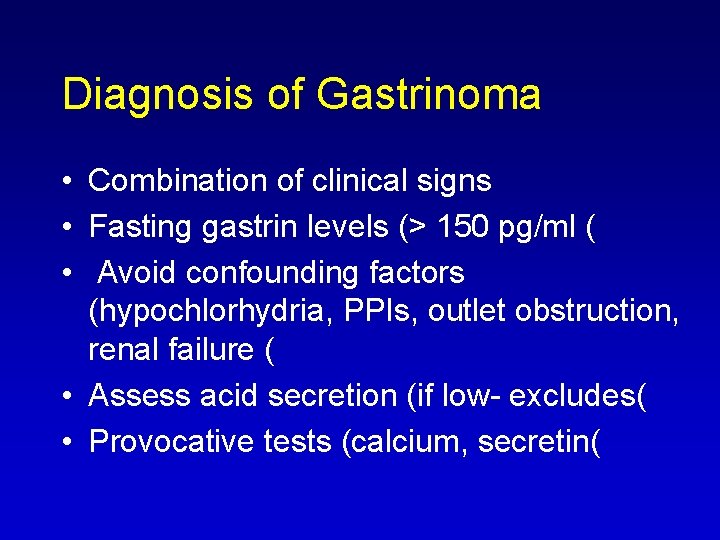
Diagnosis of Gastrinoma • Combination of clinical signs • Fasting gastrin levels (> 150 pg/ml ( • Avoid confounding factors (hypochlorhydria, PPIs, outlet obstruction, renal failure ( • Assess acid secretion (if low excludes( • Provocative tests (calcium, secretin(
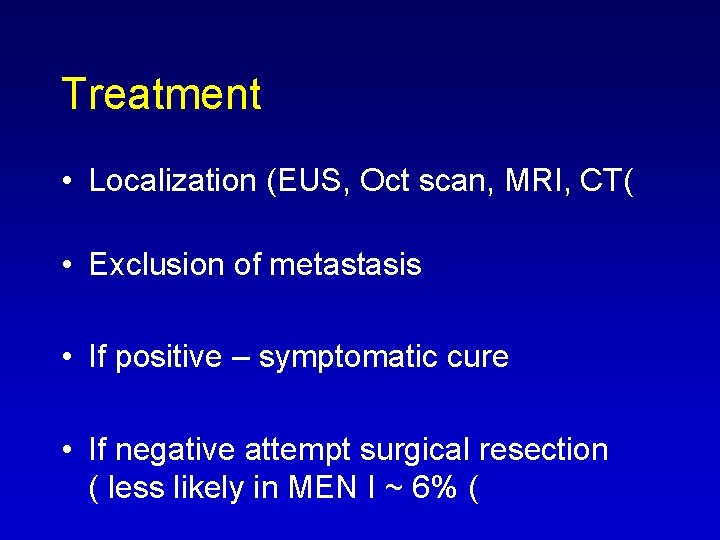
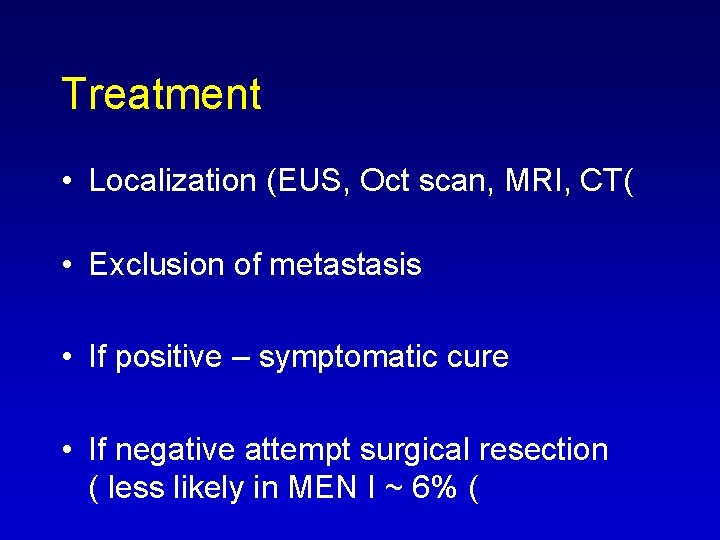
Treatment • Localization (EUS, Oct scan, MRI, CT( • Exclusion of metastasis • If positive – symptomatic cure • If negative attempt surgical resection ( less likely in MEN I ~ 6% (
Case 2 • 70 year old lady , RA • Dizziness and weakness for the last week. • Mild abdominal pain • Questions?
Case 2 • • • Stools? Melena Drugs? NSAIDS Next action? Gastroscopy

Gastric Ulcer with Stigma
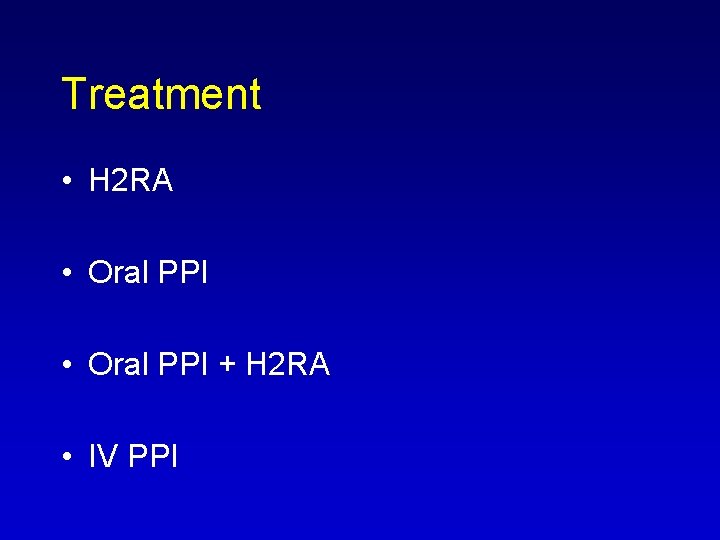
Treatment • H 2 RA • Oral PPI + H 2 RA • IV PPI
H 2 RA • Very safe drugs • Tolerance after 48 hrs IV treatment • Less effective than PPIs in suppressing acid secretion (block only histamin(
Treatment • Heavy consumption of NSAID • Should H. pylori be tested for? Treated? • YES
Drugs for treatment of acid disorders and H. pylori infection • H 2 Receptor antagonists • PPI • Anti H. pylori regimens
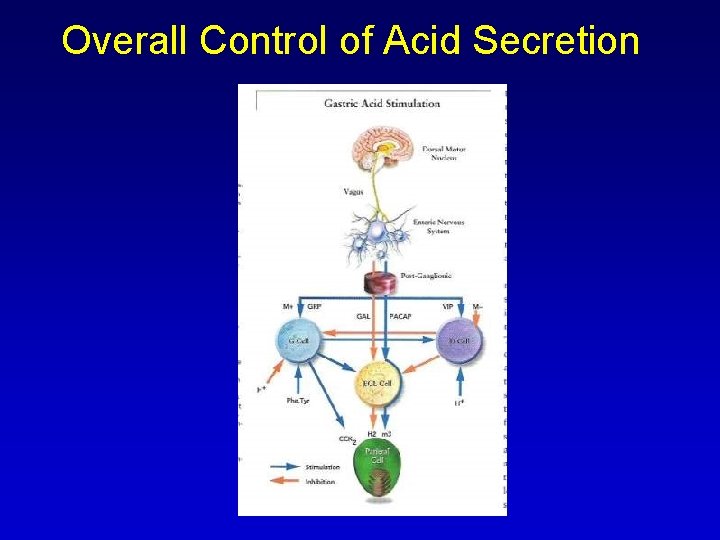
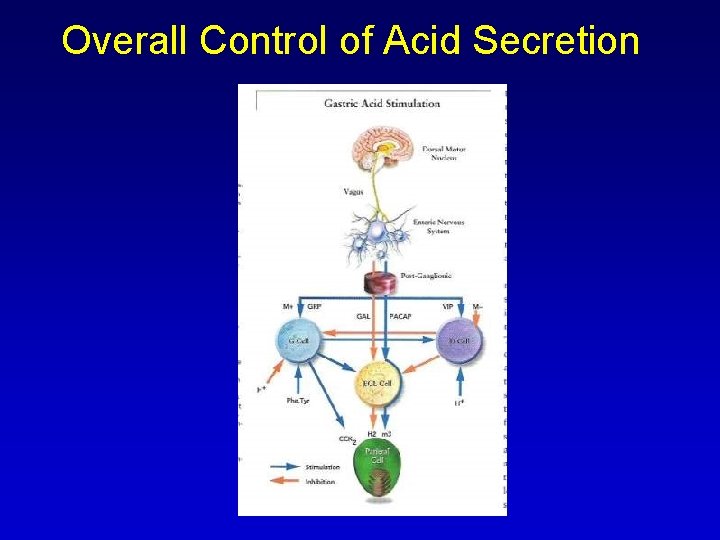
Overall Control of Acid Secretion
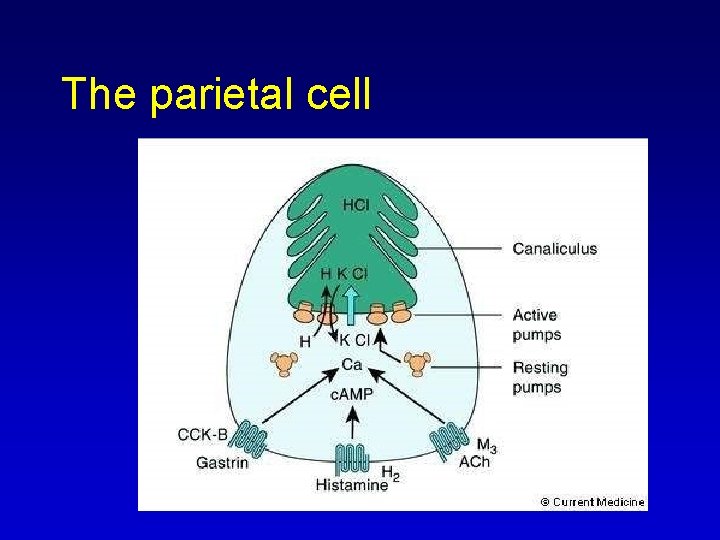
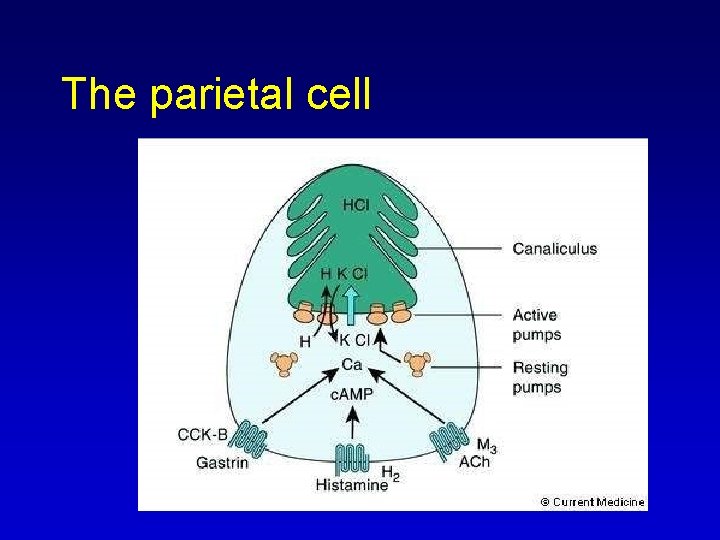
The parietal cell
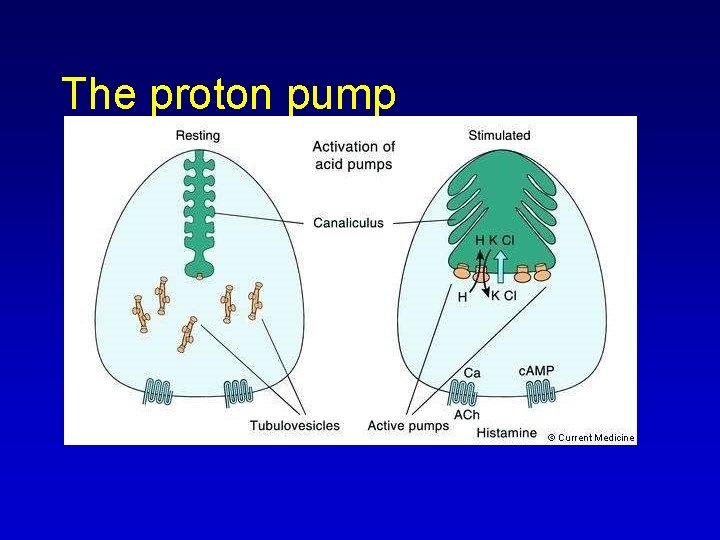
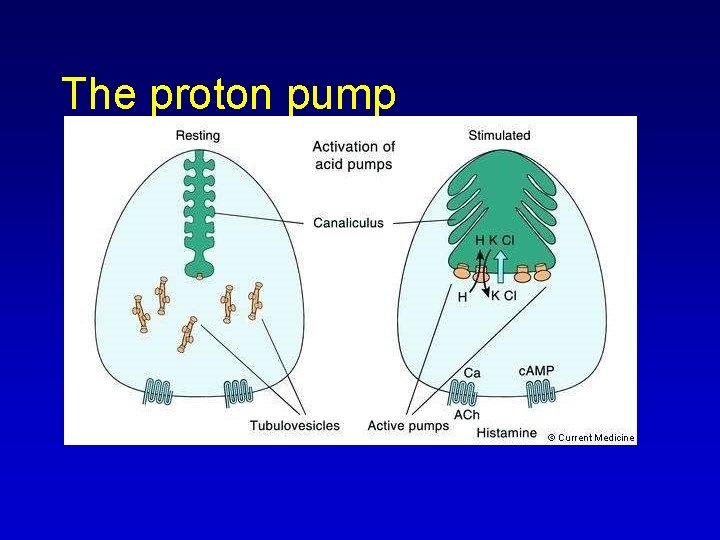
The proton pump

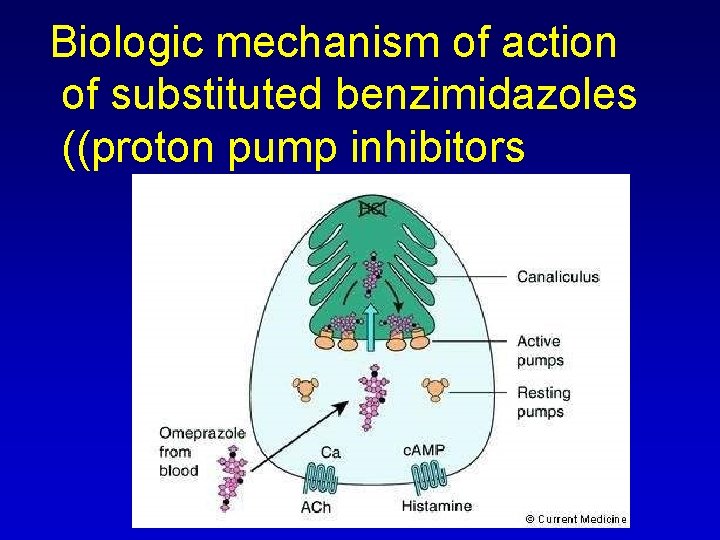
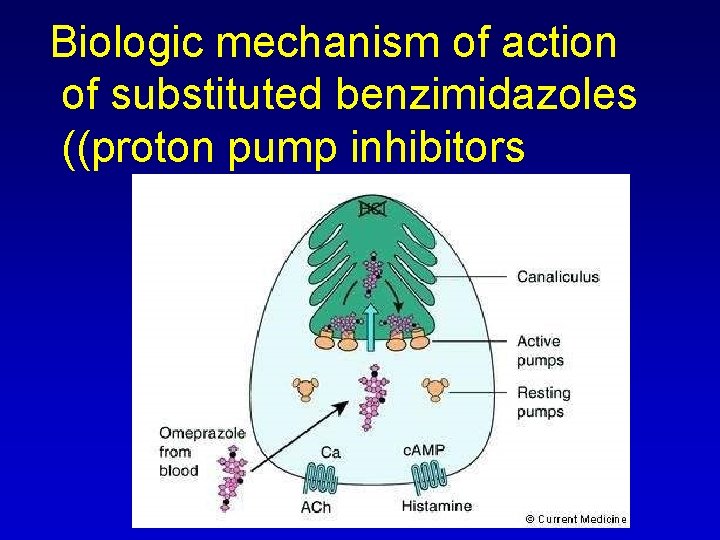
Biologic mechanism of action of substituted benzimidazoles ((proton pump inhibitors
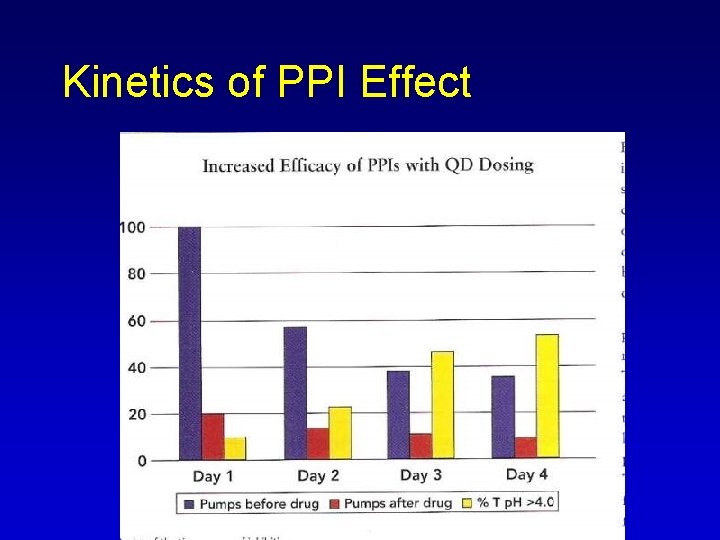
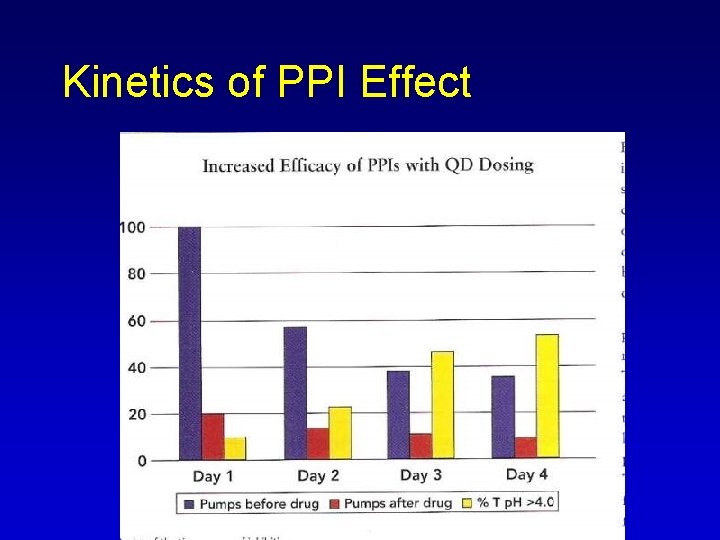
Kinetics of PPI Effect
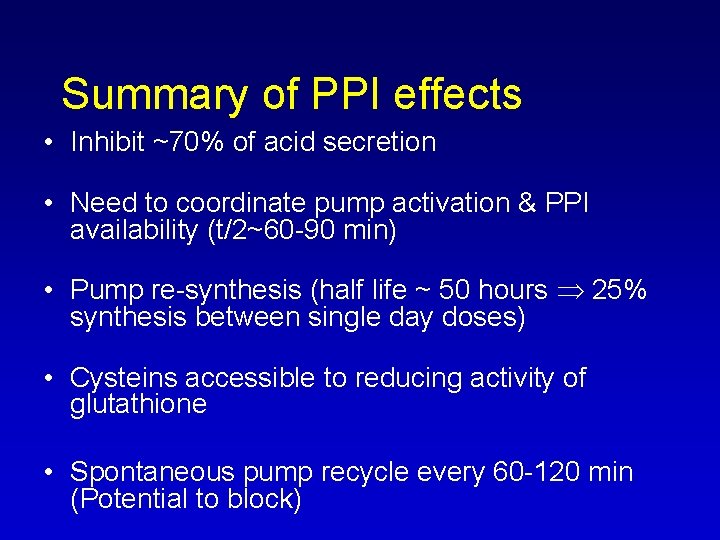
Summary of PPI effects • Inhibit ~70% of acid secretion • Need to coordinate pump activation & PPI availability (t/2~60 90 min) • Pump re synthesis (half life ~ 50 hours 25% synthesis between single day doses) • Cysteins accessible to reducing activity of glutathione • Spontaneous pump recycle every 60 120 min (Potential to block)
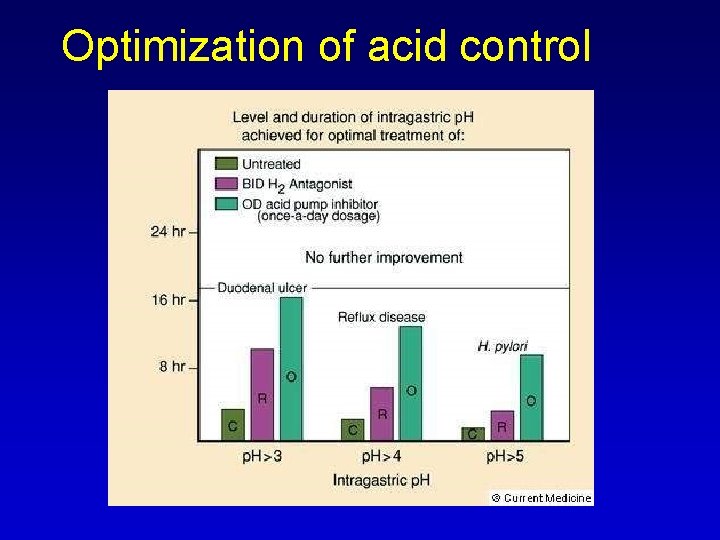
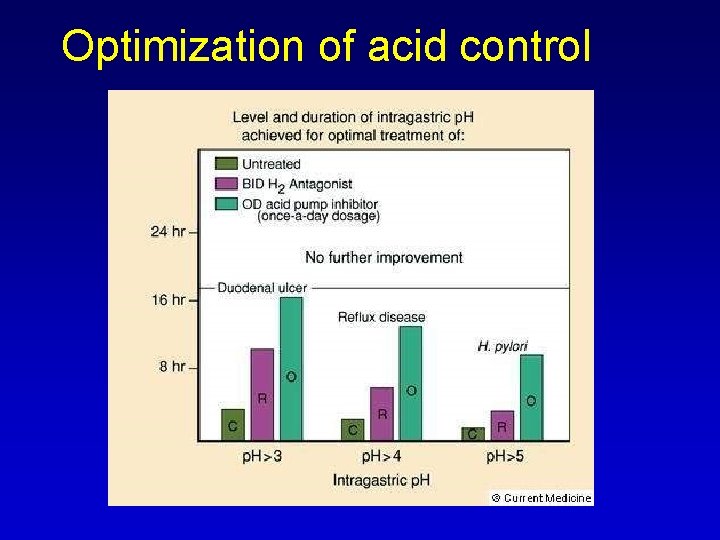
Optimization of acid control
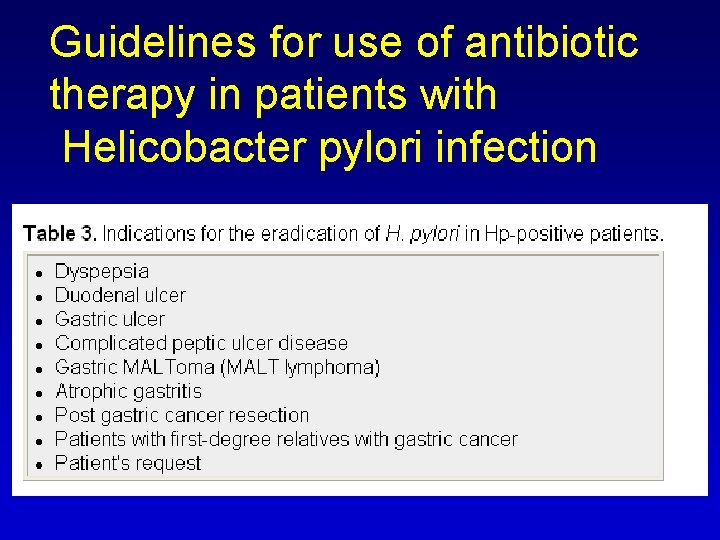
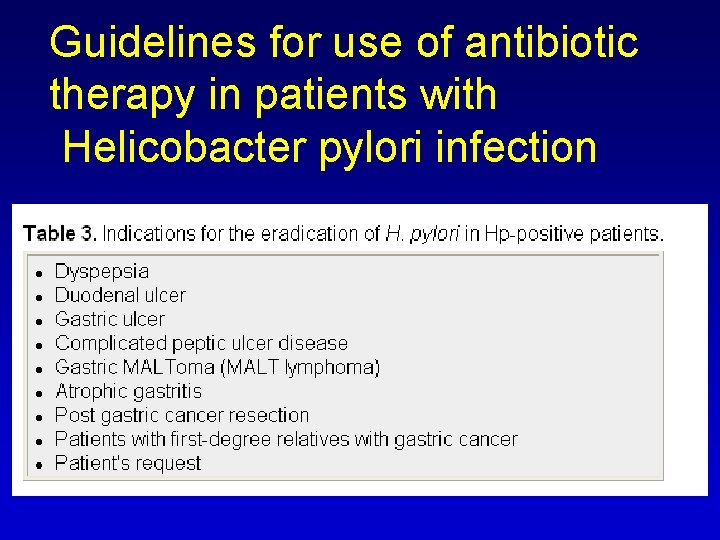
Guidelines for use of antibiotic therapy in patients with Helicobacter pylori infection
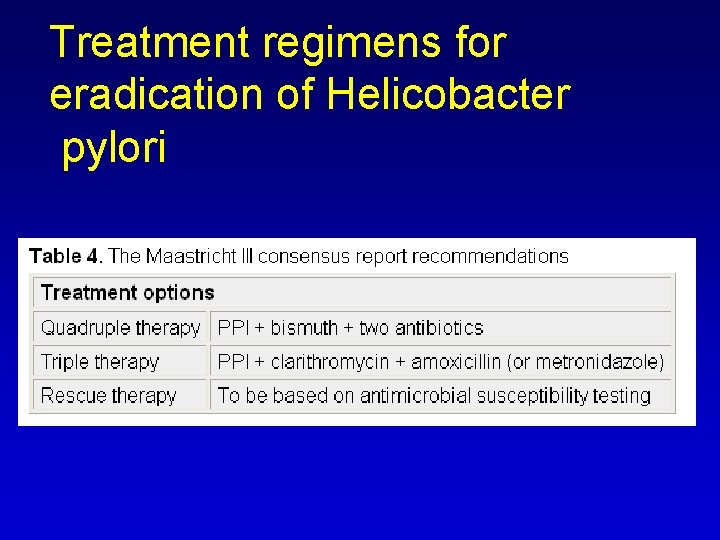
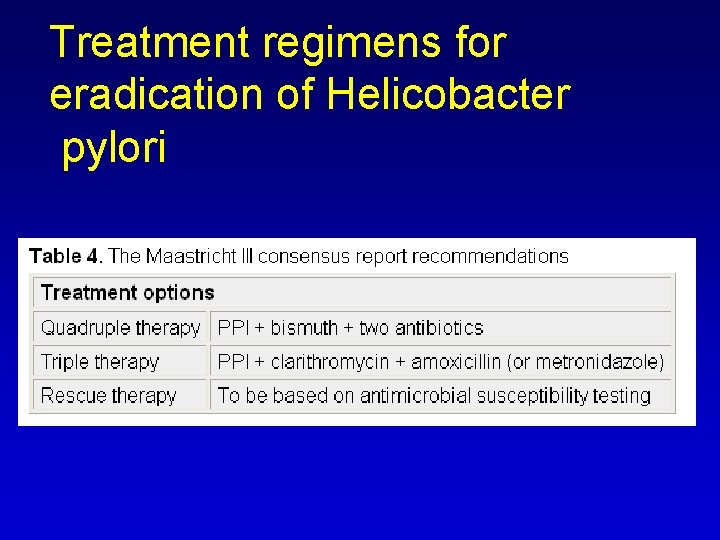
Treatment regimens for eradication of Helicobacter pylori
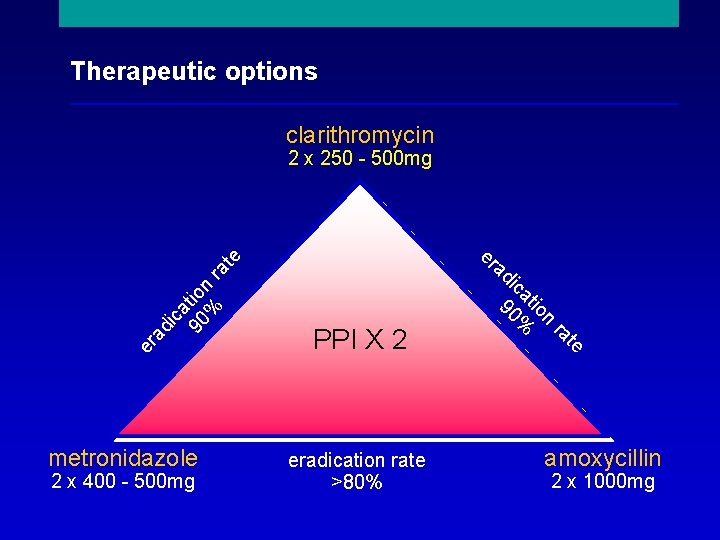
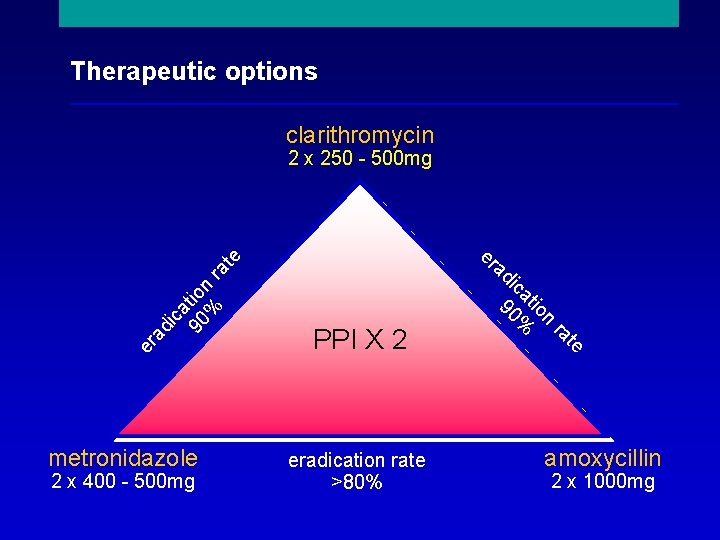
Therapeutic options clarithromycin a 90 tio % nr ic ad er _ eradication rate >80% < _ 2 x 400 500 mg PPI X 2 te ra n io at ic 90% < metronidazole ad at er e 2 x 250 500 mg amoxycillin 2 x 1000 mg
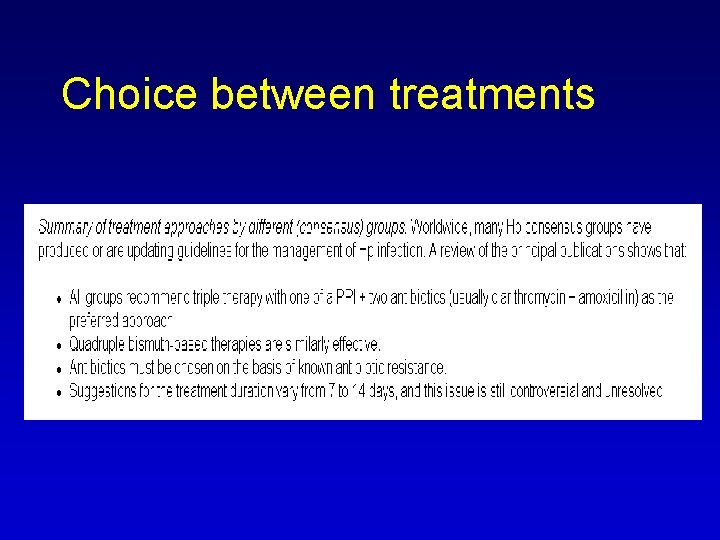
Choice between treatments
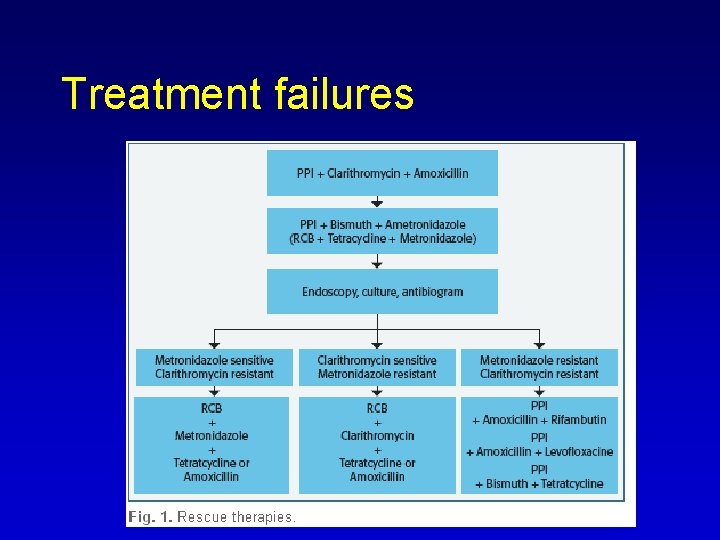
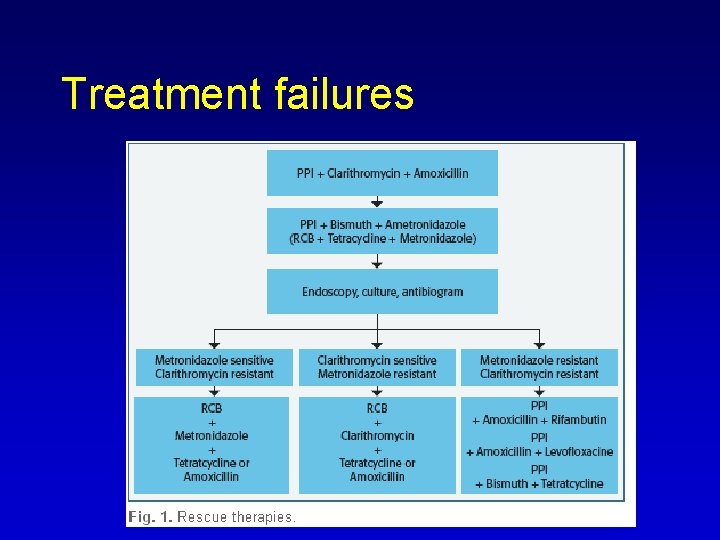
Treatment failures

 Arsas symptoms
Arsas symptoms Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Gastric ulcer vs duodenal ulcer
Gastric ulcer vs duodenal ulcer Peptic ulcer disease
Peptic ulcer disease Objectives of peptic ulcer
Objectives of peptic ulcer Emetics
Emetics Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease What are the different types of laxatives
What are the different types of laxatives Ascites yellow color
Ascites yellow color Cengiz pata
Cengiz pata Theropatic
Theropatic Peptic ulcer diseas
Peptic ulcer diseas Peptic ulcer morphology
Peptic ulcer morphology Vicaline pill application
Vicaline pill application Acholorhydria
Acholorhydria Modified johnson classification
Modified johnson classification Mondor triad
Mondor triad Proton pump inhibitor
Proton pump inhibitor Pud
Pud Teapot deformity of stomach
Teapot deformity of stomach Tuberculous ulcer and typhoid ulcer
Tuberculous ulcer and typhoid ulcer Classification of ulcer
Classification of ulcer Stomach ulcer diet menu
Stomach ulcer diet menu Gastroenterology medical terminology
Gastroenterology medical terminology Dr vallina gastroenterology
Dr vallina gastroenterology Decompensated liver disease
Decompensated liver disease Gastroenterology diagnosis codes
Gastroenterology diagnosis codes Bilitec
Bilitec Dr alix lanoue
Dr alix lanoue Immunity organized
Immunity organized Bharathi viswanathan
Bharathi viswanathan Cengiz balkan
Cengiz balkan Labil duygulanım nedir
Labil duygulanım nedir Cengiz camci
Cengiz camci Cengiz canpolat
Cengiz canpolat Cengiz polat uzunoğlu
Cengiz polat uzunoğlu Prof dr cengiz kılıç
Prof dr cengiz kılıç Cengiz akay
Cengiz akay Cengiz polat art
Cengiz polat art Prof dr cengiz yalçınkaya
Prof dr cengiz yalçınkaya Cengiz canpolat
Cengiz canpolat Cengiz kurtman
Cengiz kurtman Mehmet cengiz çolakoğlu
Mehmet cengiz çolakoğlu Periferik yayma boyama
Periferik yayma boyama Cengiz topel cesedi fotoğrafları
Cengiz topel cesedi fotoğrafları Cengiz kılıç psikiyatri
Cengiz kılıç psikiyatri Dr mustafa cengiz
Dr mustafa cengiz Cengiz yaman
Cengiz yaman Tansın cengiz
Tansın cengiz Stomach cells secrete
Stomach cells secrete Pata case study solution
Pata case study solution Test de la pata negra
Test de la pata negra Pata connector
Pata connector Trabalenguas de las copas
Trabalenguas de las copas Frazeologizmus pichľavý
Frazeologizmus pichľavý Pata cable
Pata cable Detalet e makinave
Detalet e makinave Piel de tiburón y pata de mosca
Piel de tiburón y pata de mosca Kai pata
Kai pata Decorticacion de judet
Decorticacion de judet Fekete bikapata kopog a patika pepita kövén
Fekete bikapata kopog a patika pepita kövén Tratarea decorativa
Tratarea decorativa Dau operační
Dau operační Lm lubenica
Lm lubenica Elephants foot
Elephants foot It essentials chapter 3
It essentials chapter 3 Jkr pata
Jkr pata Por un caminito oscuro va caminando un bicho
Por un caminito oscuro va caminando un bicho