Peptic Ulcer Disease A Case Study Approach Introduction



- Slides: 19
Peptic Ulcer Disease A Case Study Approach
Introduction: FK: 65 year old male Weight: 116 -123 lbs UBW: 138 lbs per patient. Hx of Tobacco use, ETOH abuse, COPD, cirrhosis of the liver, anemia and cancer of the tongue Admission: Originally referred to Fort Hamilton from University of Cincinnati for a mandibular fracture. Was admitted to ICU due to a severe gastric bleed from a perforated gastric ulcer.
Social History: Single Lives along in a 2 story walk up apartment Moderate assistance from family Takes care of himself 50 -75% of the time. Home meals Uses crockpot or eats mostly canned foods and soups. Alcohol use 24 cans of beer per week, with occasional bourbon Tobacco use 1. 5 packs per day, reportedly quit 8/22/15
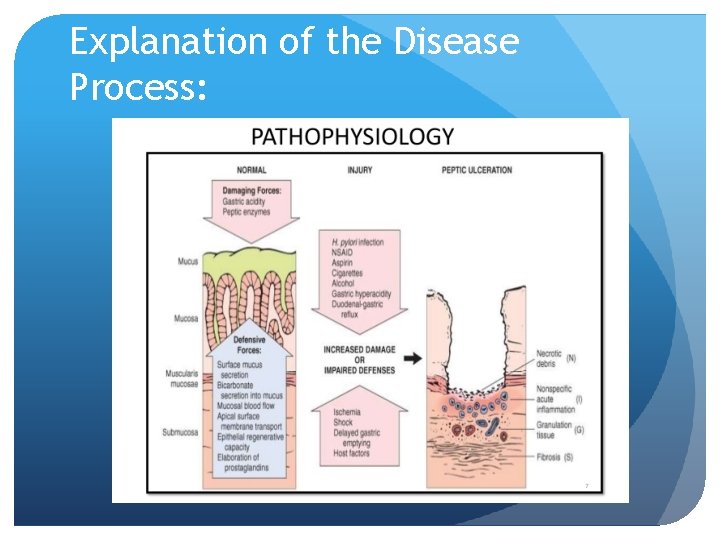
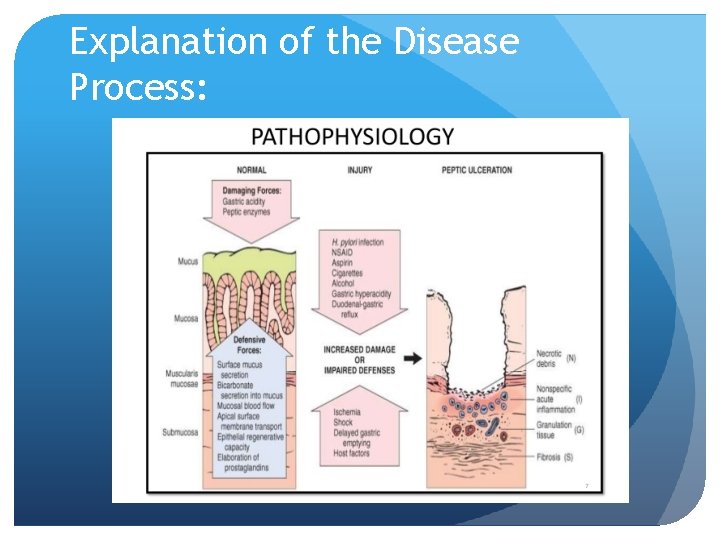
Explanation of the Disease Process:
Explanation of the Disease Process: Most common cause of Peptic Ulcer Disease: H. Pylori Usually transmitted via fecal-oral route Usually found in people with poor socio-economic background Factors that influence an H. Pylori infection: NSAID use can cause an H. pylori infection due to inhibiting Prostaglandin synthesis (maintains homeostatic function in the gut by regulating acid secretion. ) Inflammation and acidic environment allows H. pylori to flourish. Disruption of “protective factors” such as prostaglandins, mucus, bicarbonate and blood flow in the mucosa Usually damaged by “hostile factors” smoking, alcohol abuse, radiation treatments, and regular NSAID use
Explanation of the Disease Process: How a perforation occurs: Under normal conditions the stomach can withstand the corrosiveness of gastric acid. 1. A “hostile factor” is introduced. 2. “Protective factors” are disrupted. 3. Gastric acid begins to break down the lining of the stomach. 4. Tissue becomes inflamed an ulcer occurs (usually in the first layer of the stomach lining. ) 5. Gastric acid continues to erode the lining, causing further damage and potentially a perforation. A perforation cause internal bleeding.
Past and Current Admissions Past visits to Fort Hamilton: Cellulitis in 2012 Pain in right ankle from a fall in 2014 During this visit he was diagnosed with peripheral vascular disease. Current and recurrent admissions: 11/11/15 Weakness and malaise due to a perforated gastric ulcer 2 repairs during admission Mass found on tongue, referred patient to his ENT for further testing Patient had a broken jaw Was severely malnourished. 11/20/15 readmission, recurrent gastric bleed. Ulcer was repaired a 3 rd time.

Past Medical Hx and Comorbidities Hypertension Radiation - 42 treatments Hx antineoplastic chemo Peripheral vascular disease ETOH abuse Cirrhosis Seizures - with ETOH withdrawal COPD (chronic obstructive pulmonary disease) Cancer - Base of tongue Forgetfulness Anemia
Recurrence and mortality Recurrence of a gastric bleed from peptic ulcer disease Populations over 60 years of age Mortality is also increased in this population. Alcohol abuse increases recurrence almost 2 fold. Mortality is also increased in this population regardless of age.
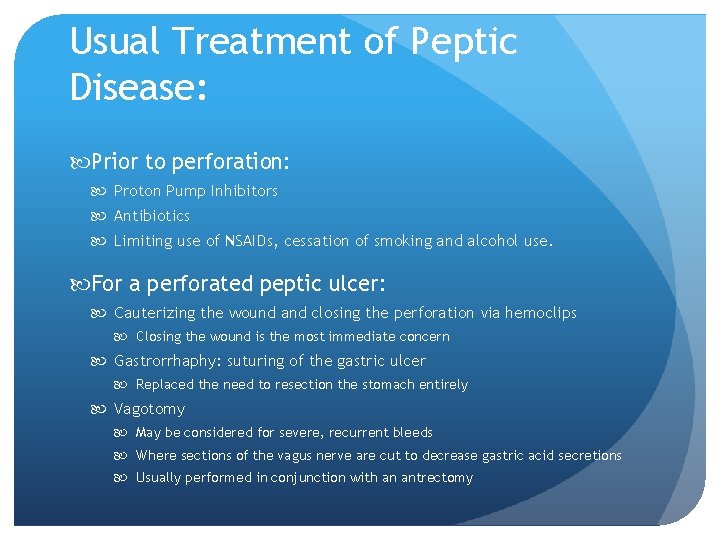
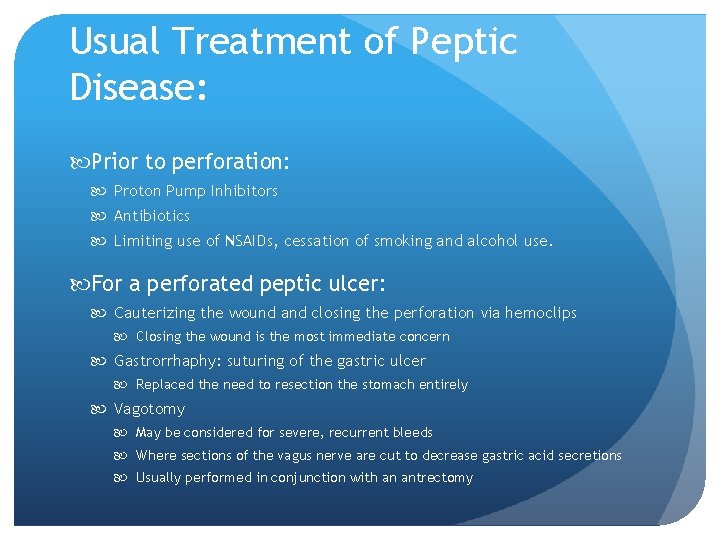
Usual Treatment of Peptic Disease: Prior to perforation: Proton Pump Inhibitors Antibiotics Limiting use of NSAIDs, cessation of smoking and alcohol use. For a perforated peptic ulcer: Cauterizing the wound and closing the perforation via hemoclips Closing the wound is the most immediate concern Gastrorrhaphy: suturing of the gastric ulcer Replaced the need to resection the stomach entirely Vagotomy May be considered for severe, recurrent bleeds Where sections of the vagus nerve are cut to decrease gastric acid secretions Usually performed in conjunction with an antrectomy

Patient’s Symptoms: Bloody or dark tarry stools Fatigue Vomiting Weight loss Abdominal discomfort
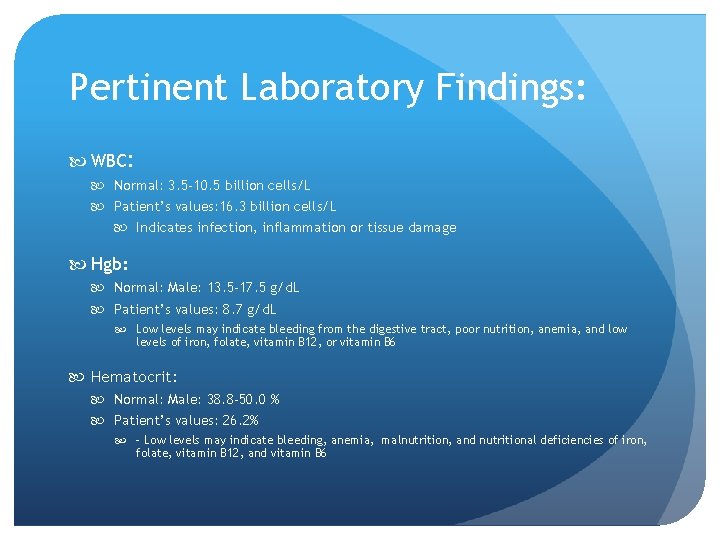
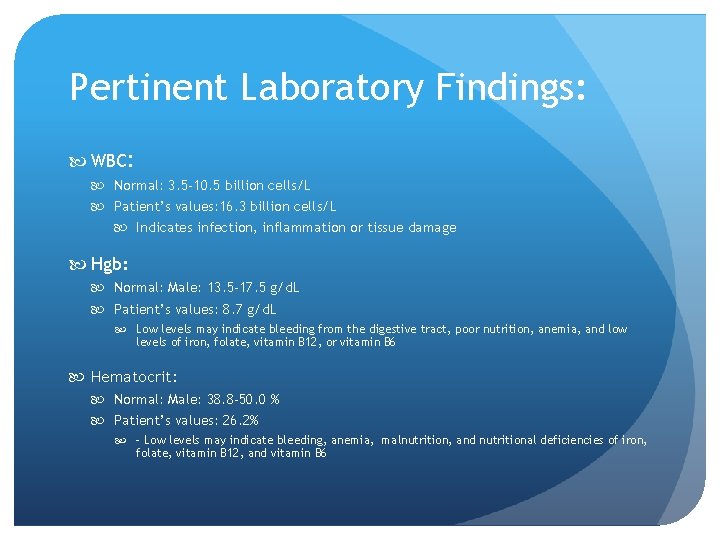
Pertinent Laboratory Findings: WBC: Normal: 3. 5 -10. 5 billion cells/L Patient’s values: 16. 3 billion cells/L Indicates infection, inflammation or tissue damage Hgb: Normal: Male: 13. 5 -17. 5 g/d. L Patient’s values: 8. 7 g/d. L Low levels may indicate bleeding from the digestive tract, poor nutrition, anemia, and low levels of iron, folate, vitamin B 12, or vitamin B 6 Hematocrit: Normal: Male: 38. 8 -50. 0 % Patient’s values: 26. 2% - Low levels may indicate bleeding, anemia, malnutrition, and nutritional deficiencies of iron, folate, vitamin B 12, and vitamin B 6
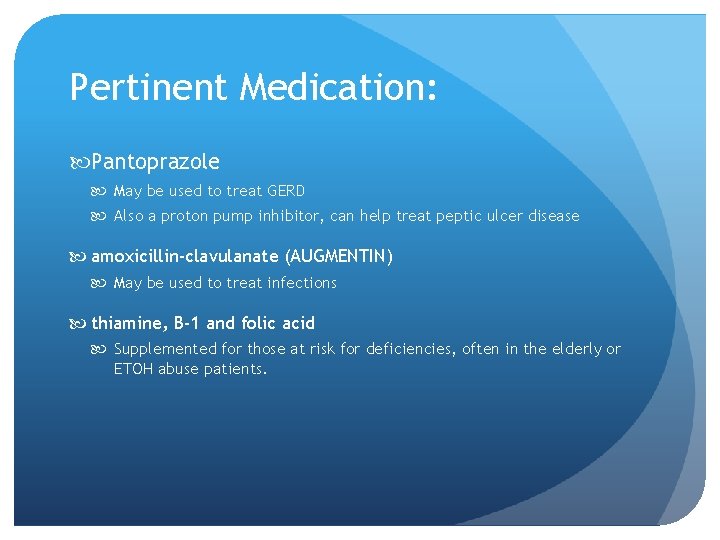
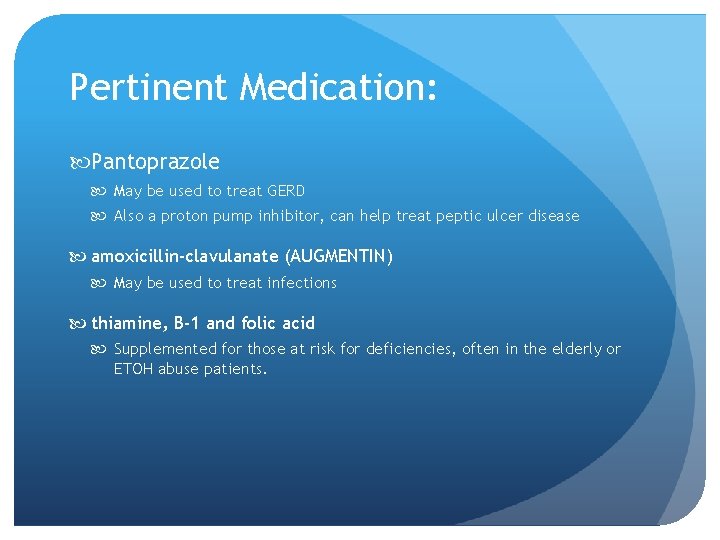
Pertinent Medication: Pantoprazole May be used to treat GERD Also a proton pump inhibitor, can help treat peptic ulcer disease amoxicillin-clavulanate (AUGMENTIN) May be used to treat infections thiamine, B-1 and folic acid Supplemented for those at risk for deficiencies, often in the elderly or ETOH abuse patients.
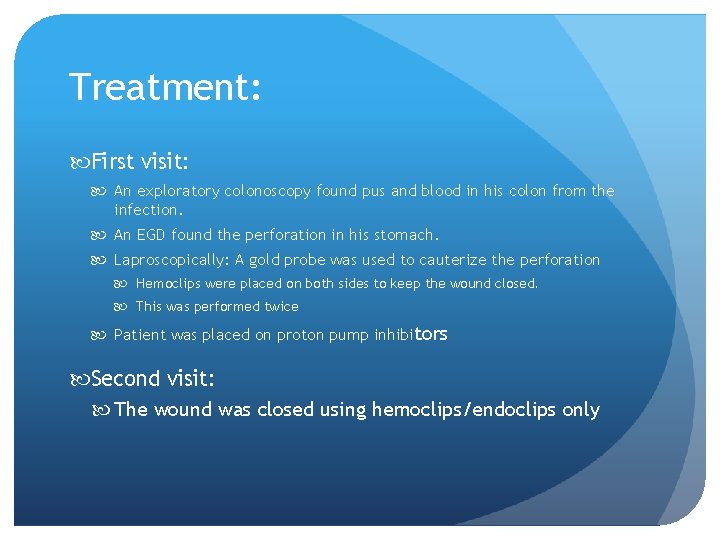
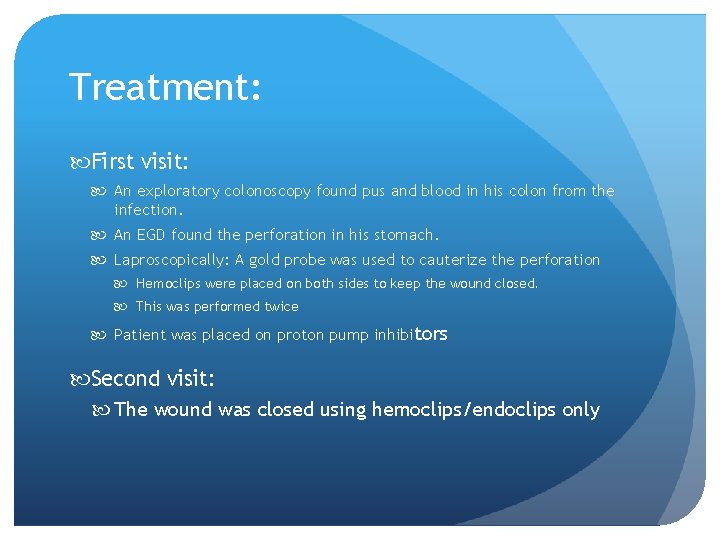
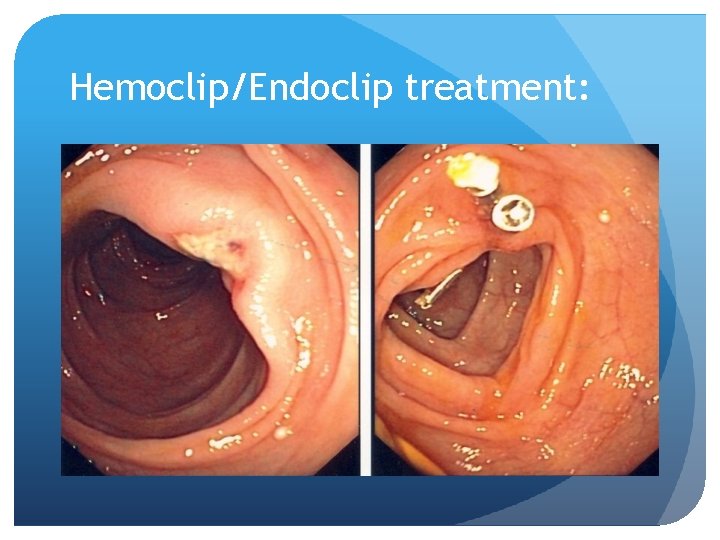
Treatment: First visit: An exploratory colonoscopy found pus and blood in his colon from the infection. An EGD found the perforation in his stomach. Laproscopically: A gold probe was used to cauterize the perforation Hemoclips were placed on both sides to keep the wound closed. This was performed twice Patient was placed on proton pump inhibitors Second visit: The wound was closed using hemoclips/endoclips only
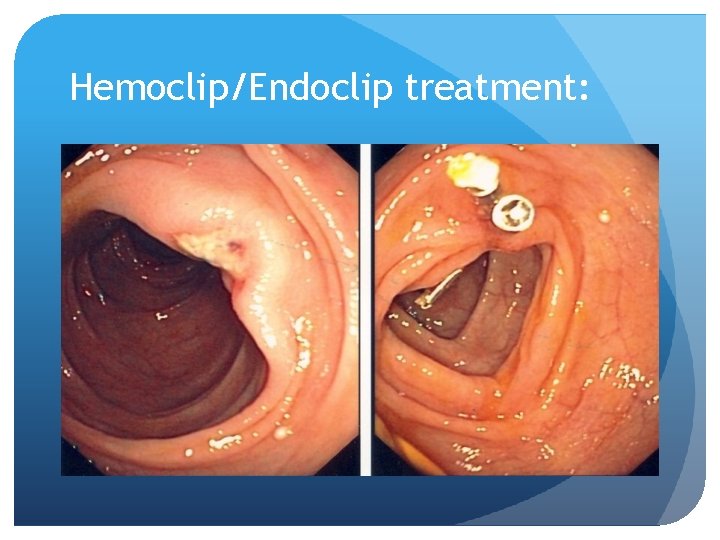
Hemoclip/Endoclip treatment:
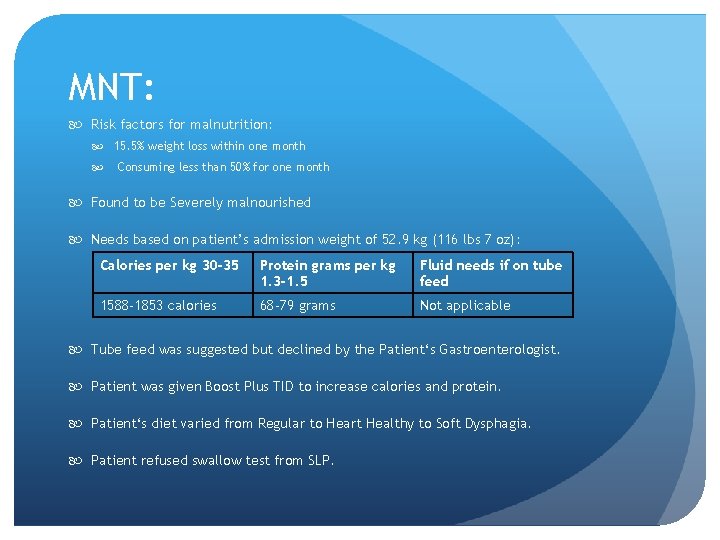
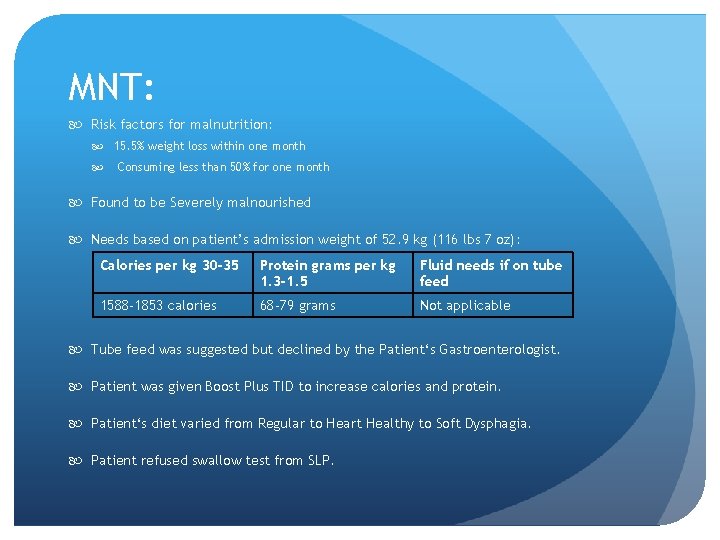
MNT: Risk factors for malnutrition: 15. 5% weight loss within one month Consuming less than 50% for one month Found to be Severely malnourished Needs based on patient’s admission weight of 52. 9 kg (116 lbs 7 oz): Calories per kg 30 -35 Protein grams per kg 1. 3 -1. 5 Fluid needs if on tube feed 1588 -1853 calories 68 -79 grams Not applicable Tube feed was suggested but declined by the Patient‘s Gastroenterologist. Patient was given Boost Plus TID to increase calories and protein. Patient‘s diet varied from Regular to Heart Healthy to Soft Dysphagia. Patient refused swallow test from SLP.

Diet analysis:
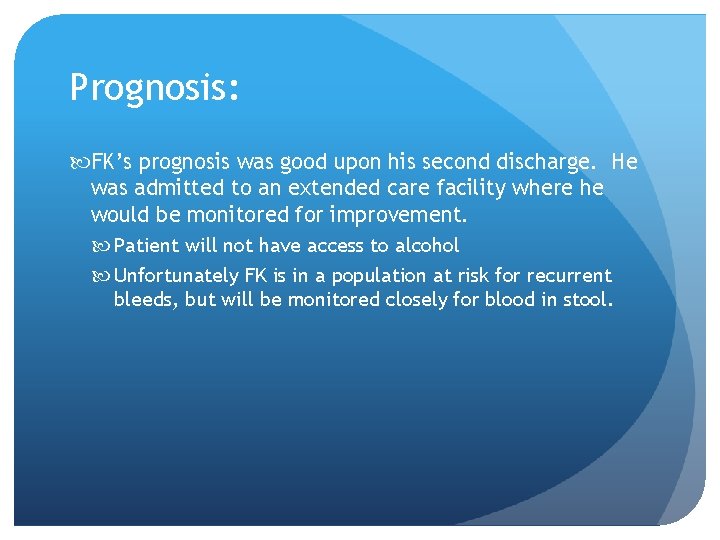
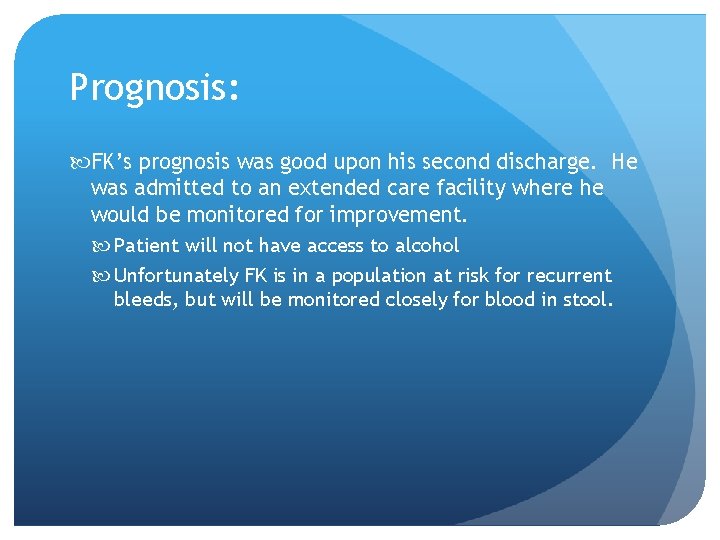
Prognosis: FK’s prognosis was good upon his second discharge. He was admitted to an extended care facility where he would be monitored for improvement. Patient will not have access to alcohol Unfortunately FK is in a population at risk for recurrent bleeds, but will be monitored closely for blood in stool.
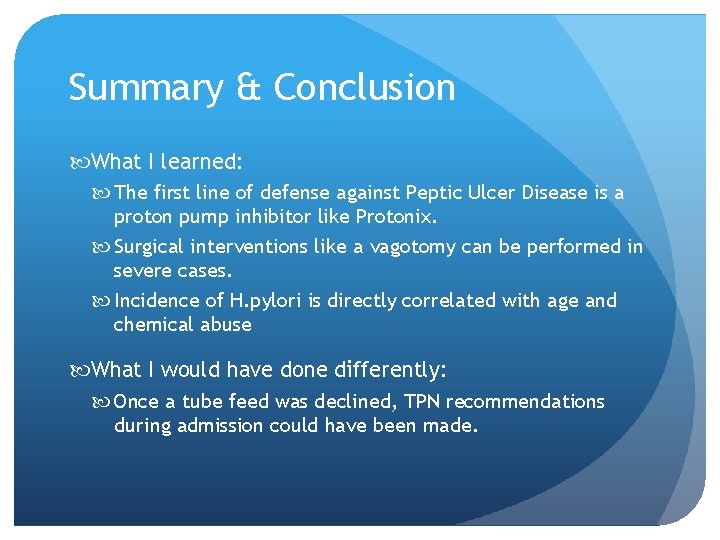
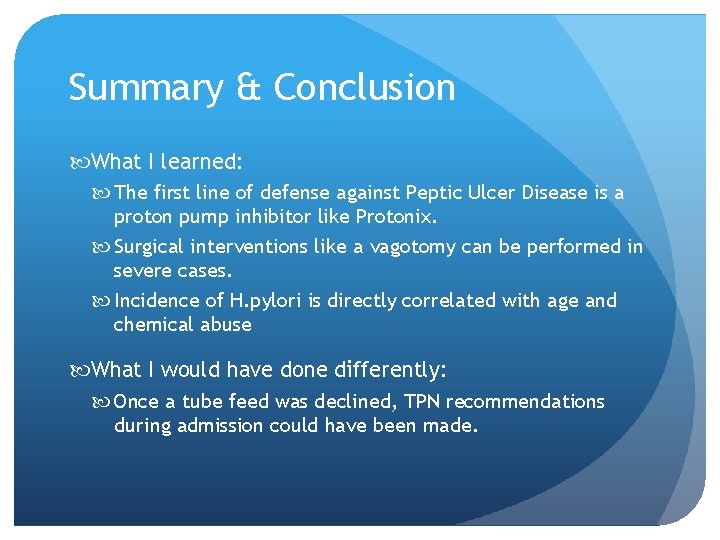
Summary & Conclusion What I learned: The first line of defense against Peptic Ulcer Disease is a proton pump inhibitor like Protonix. Surgical interventions like a vagotomy can be performed in severe cases. Incidence of H. pylori is directly correlated with age and chemical abuse What I would have done differently: Once a tube feed was declined, TPN recommendations during admission could have been made.