Peptic Ulcer Wendy Langen Peptic Ulcer Disease PUD













- Slides: 32

Peptic Ulcer Wendy Langen
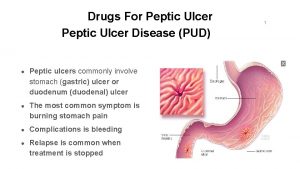
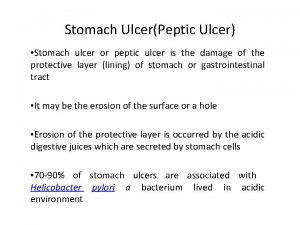
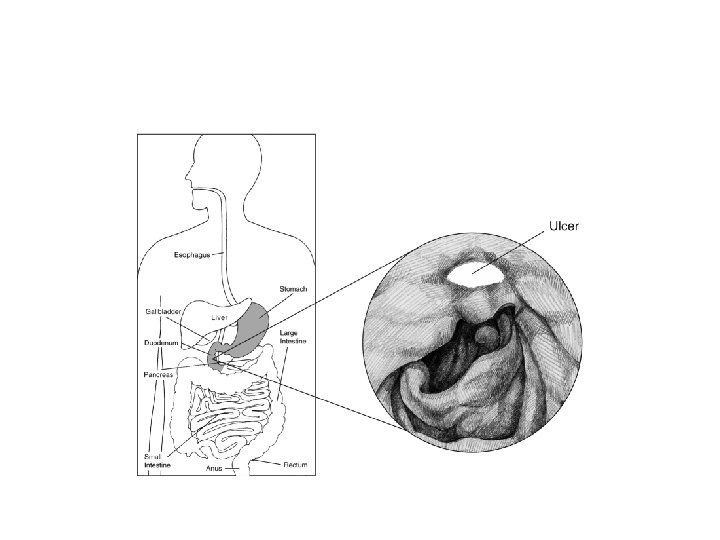
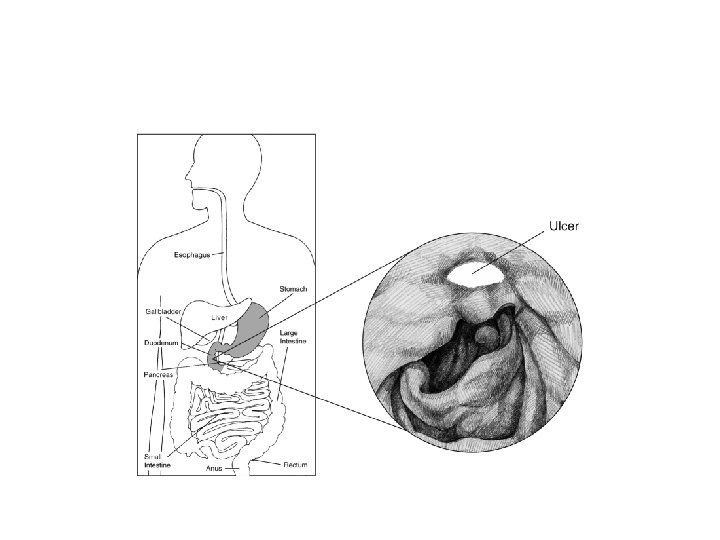
• • Peptic Ulcer Disease= PUD Refers to ulcers of stomach or duodenum Prevalence 10% USA in 96 Am J Public Health 1996 Feb; 86(2): 200 Gastric> duodenal

Ulcer Sx • Gnawing, burning epigastric pain radiating to back • Duodenal- 2 -5 hours post-prandial or with empty stomach, or at night • Peptic- may be worsened with food, feeling of fullness, aggravation with fatty food, even N/V • Relieved with antacids and antisecretories
Risks • • H. pylori NSAIDs list GERD Smoking Crohn’s, CMV Steroid use Bisphonates, chemo http: //www. dynamed. com/topics/dmp~AN~T 116374/Peptic-ulcer-disease#General-Information • Not coffee, nor etoh! http: //www. ncbi. nlm. nih. gov/pubmed/23776588? dopt=Abstract, Neth J Med 2001 Jul; 59(1): 23
DDx • • • GERD Acute upper GI bleed Gastric CA IBS Pancreatitis • Cholecystitis
Evaluation • Ask about NSAIDs, diet, weight loss • Signs of shock- HR, BP, pallor • Abdomen- rigid, tender, rebound, hypoactive BS • Rectal Blood • CBC, breath urea, LFTs, lipase • Endoscopy can Dx, biopsy gastric ulcers
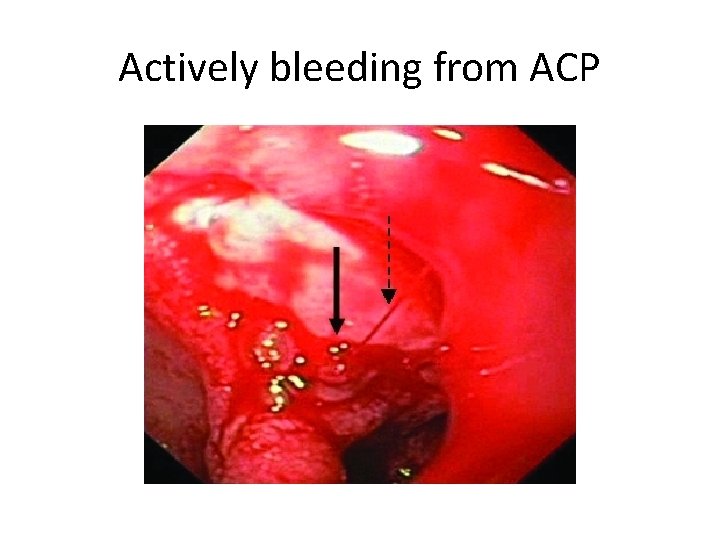
Complications • Bleeding • Perforation • Gastric outlet obstruction- suspect CA
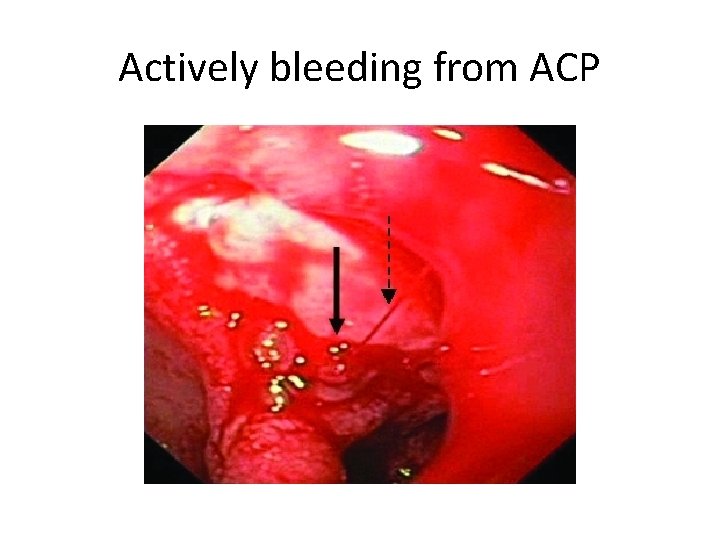
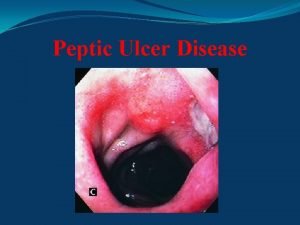
Actively bleeding from ACP

Clotted

Ready to rebleed
Ulcer perforation • Sudden extreme pain (to shoulder) with collapse, vomit, • Rigid abdomen, cold extremities, pale face • Improvement in 2 hours, but abdomen remains rigid, tympany over liver, free air seen in plain film • Then “catastrophe” in 6 -12 hours- peritonitis, shock, death

Free air after perforation

Diagnosis of Ulcer • Contrast imaging can show ulcer • H. pylori test and treat. • Endoscopy definitive Dx, but often unnecessary


This case • Peptic ulcer most likely given NSAIDs use, Hx GERD, gnawing pain worse at night • Peptic ulcer more likely with smoking, NSAIDs
H. Pylori testing • Breath urea test (S&S>90%), or fecal antigen test (S&S>70%) or serology (S&S>60%), No PPIs • My obviate need for endoscopy if Sx match peptic ulcer and H. pylori is positive. (NIHCare. Excellence recommendation) “test and treat” • Retesting (serology) is most consistent recommendation, but some find no evidence to support retesting, and they should not be on PPI

H. Pylori test and treat • Unless “alarm” features: • “bleeding, anemia, early satiety, unexplained weight loss, progressive dysphagia, odynophagia, recurrent vomiting, family history of gastrointestinal cancer, previous esophagogastric malignancy” (Upto. Date)


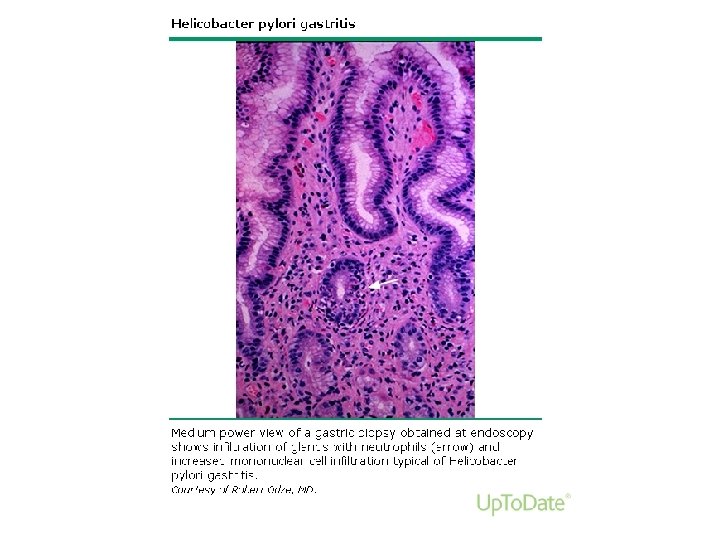
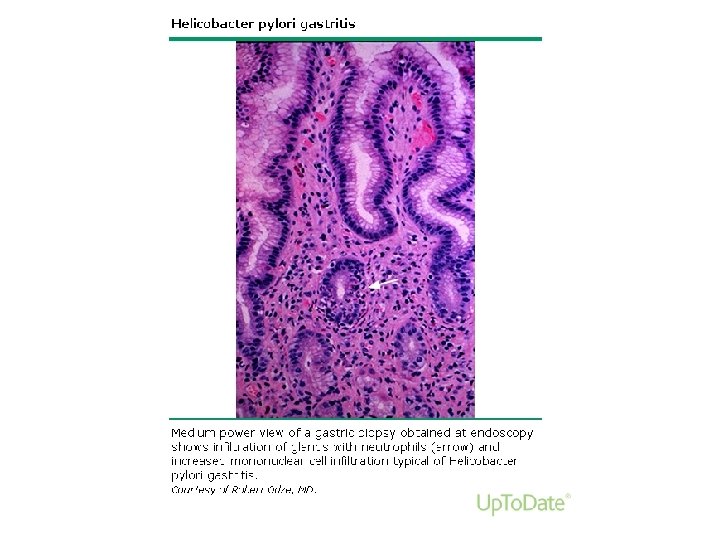
Biopsy • Gastric ulcers, which can be malignant • Not duodenal, unless Crohn’s • Biopsy can include urease testing for H. pylori (S&S>90%), which is cheaper than histology

PUD treatment • If H. pylori, treat • Stop NSAIDs • Antisecretory therapy

Maintenance PPI in some • • • Giant ulcer Refractory ulcer Still H. pylori Recurrent disease NSAIDs
Re-endoscopy “Surveillance” Endoscopy if: • Bleeding, • Persistent symptoms, • Gastric ulcer without NSAIDs nor H. pylori
Osteoarthritis • X-ray can confirm, Ortho can replace joints • Lose weight – Stop etoh – walk – improve diet, – eat breakfast, lunch • Acetaminophen
Control BP, screen • At least BP check within a week • Up lisinopril from 10 to 20 mg is best choice, with BP check in 2 weeks • This patient needs a flu shot, Mammogram and pap smear
References • Upto. Date • Dynamed- as indicated • Cope, Z. (1957) Early Diagnosis of the Acute Abdomen. 19 th Edition, NY: Oxford University Press
OCPs or Pt ed • Everyone, • Give an OCP of this case to a peer • Convince a patient (peer) to follow the instructions given for this patient – Stop NSAIDs – Start PPI – Walk, exercise – Diet, lower etoh
 Pud triple therapy
Pud triple therapy Dicycloamine
Dicycloamine Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Ajeerna symptoms
Ajeerna symptoms Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Gastric ulcer
Gastric ulcer Peptic ulcer disease
Peptic ulcer disease Modified johnson classification for gastric ulcer
Modified johnson classification for gastric ulcer Peptic ulcer case study
Peptic ulcer case study Gastric ulcer definition
Gastric ulcer definition Peptic ulcer diseas
Peptic ulcer diseas Peptic ulcer
Peptic ulcer Nursing management of peptic ulcer
Nursing management of peptic ulcer Mendel sign peptic ulcer
Mendel sign peptic ulcer Stages of peptic ulcer perforation
Stages of peptic ulcer perforation Einsatzgrundsätze tragbare leitern
Einsatzgrundsätze tragbare leitern Wohnbaugenossenschaft murifeld
Wohnbaugenossenschaft murifeld Langen foundation
Langen foundation Dreieichschule langen
Dreieichschule langen Ludwig erk schule langen
Ludwig erk schule langen Gastric ulcer
Gastric ulcer Tea pot deformity of stomach
Tea pot deformity of stomach Typhoid ulcer and tuberculous ulcer
Typhoid ulcer and tuberculous ulcer Types of gastric ulcer
Types of gastric ulcer Pendulous tuberosity
Pendulous tuberosity Pug puz pud
Pug puz pud Nursing diagnosis for pud
Nursing diagnosis for pud Pub mwd
Pub mwd Pud connector
Pud connector Dumping syndrome
Dumping syndrome Pud triple therapy
Pud triple therapy Alarm signs of pud
Alarm signs of pud Horizontální zonálnost
Horizontální zonálnost