DIPLOMA Ayurvedic Practitioners Course Module 3 26 th







- Slides: 110

DIPLOMA Ayurvedic Practitioners Course Module 3 26 th & 27 th October 2019 2
Ajeerna, Grahani & Arsas Disorders of the digestive tract
Ajeerna, Grahani & Arsas Disorders of the digestive tract The Allopathic perspective
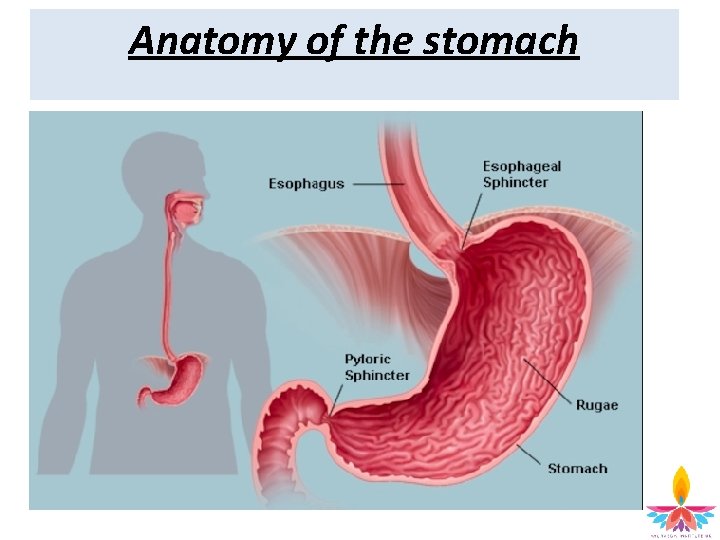
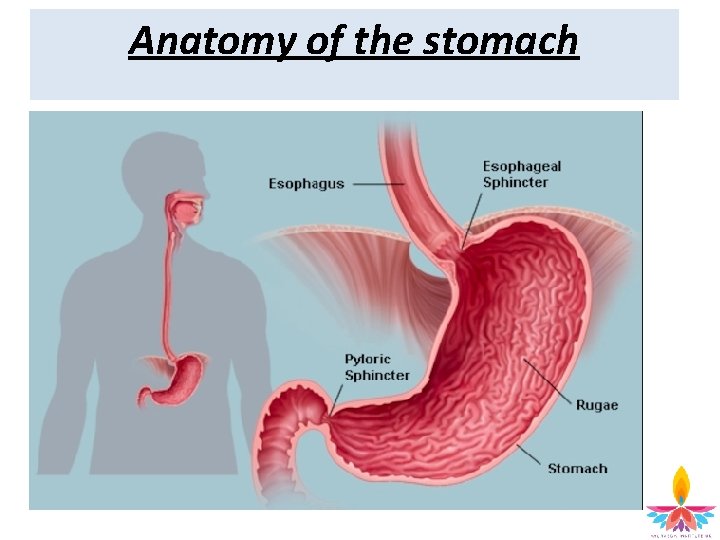
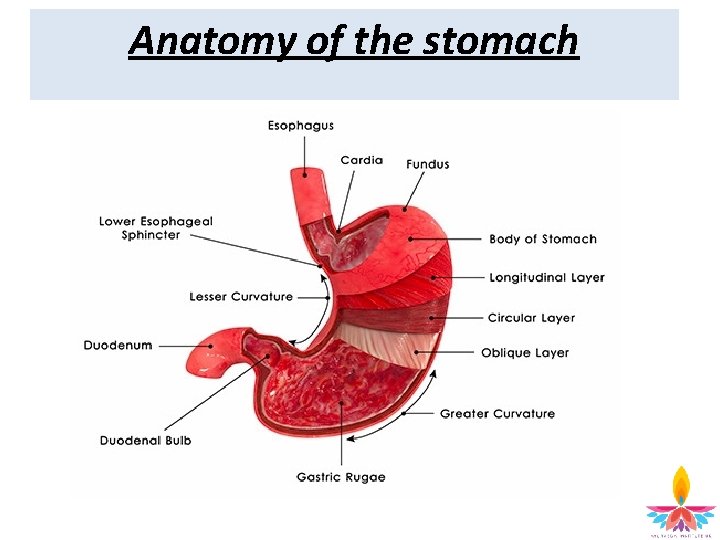
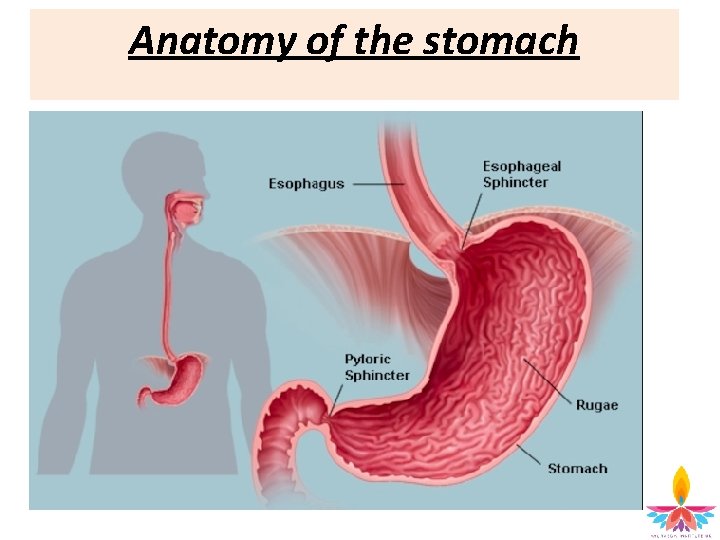
Anatomy of the stomach
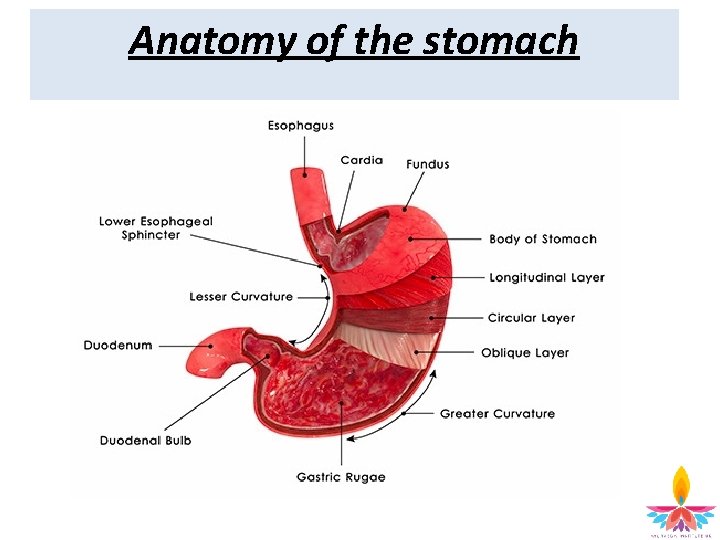
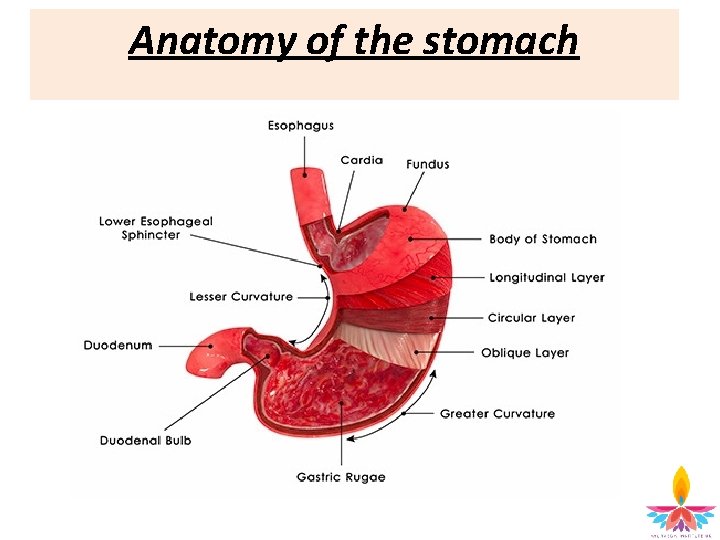
Anatomy of the stomach
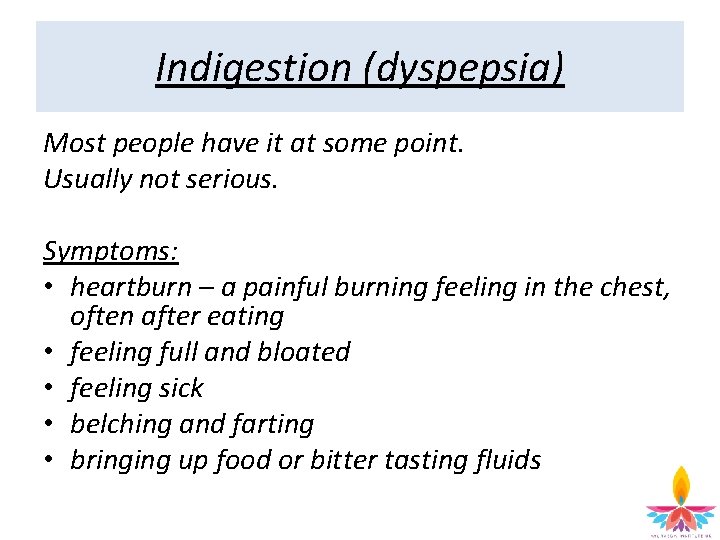
Indigestion (dyspepsia) Most people have it at some point. Usually not serious. Symptoms: • heartburn – a painful burning feeling in the chest, often after eating • feeling full and bloated • feeling sick • belching and farting • bringing up food or bitter tasting fluids
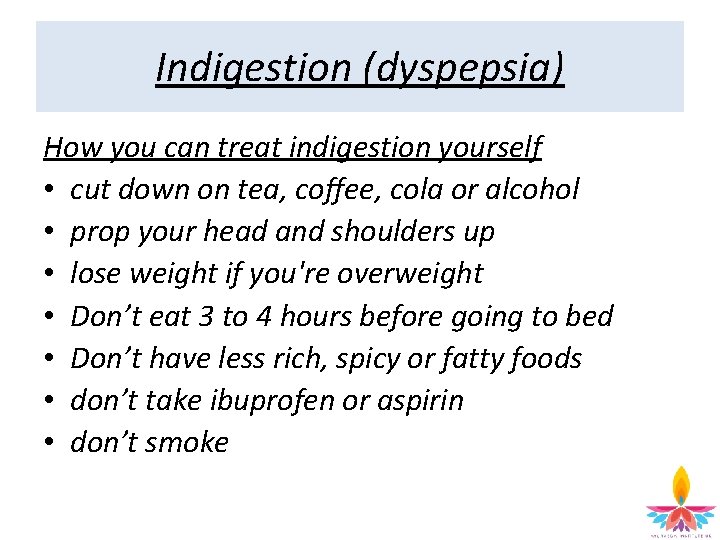
Indigestion (dyspepsia) How you can treat indigestion yourself • cut down on tea, coffee, cola or alcohol • prop your head and shoulders up • lose weight if you're overweight • Don’t eat 3 to 4 hours before going to bed • Don’t have less rich, spicy or fatty foods • don’t take ibuprofen or aspirin • don’t smoke
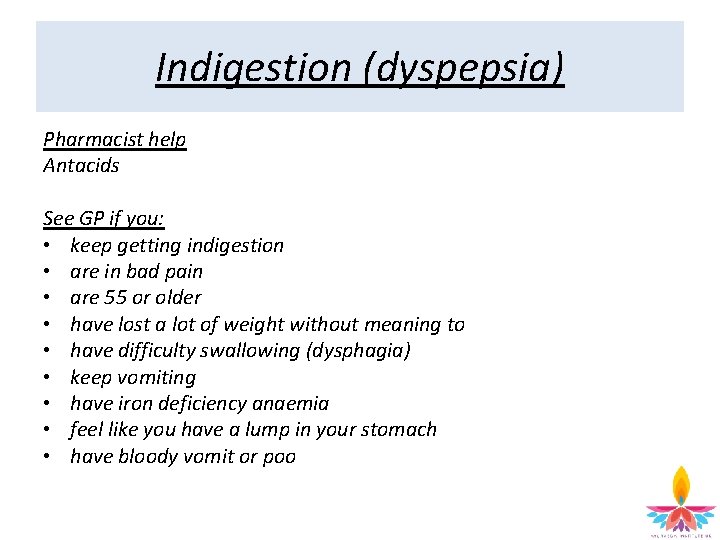
Indigestion (dyspepsia) Pharmacist help Antacids See GP if you: • keep getting indigestion • are in bad pain • are 55 or older • have lost a lot of weight without meaning to • have difficulty swallowing (dysphagia) • keep vomiting • have iron deficiency anaemia • feel like you have a lump in your stomach • have bloody vomit or poo
Indigestion (dyspepsia) Causes of indigestion Acid in stomach irritates the stomach lining or throat. Gives burning feeling and pain due to: • medicines • smoking • alcohol • stress Illnesses that can cause indigestion • hiatus hernia • stomach ulcer • stomach cancer • helicobacter pylori infections • gastro-oesophageal disease (GORD)
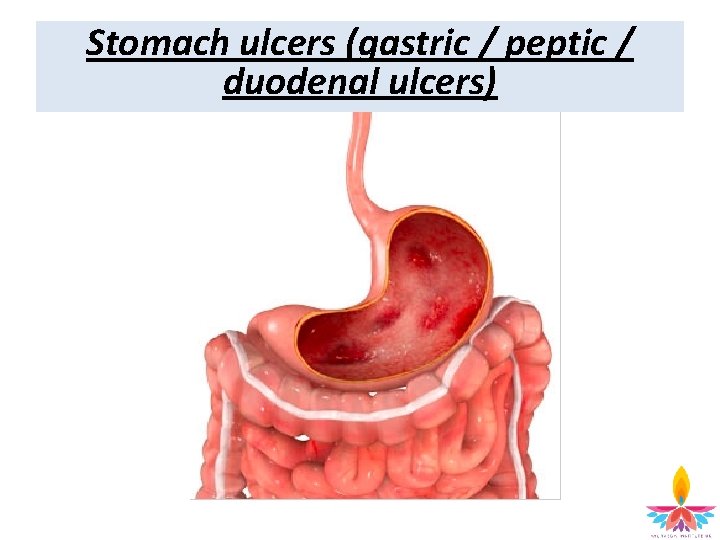
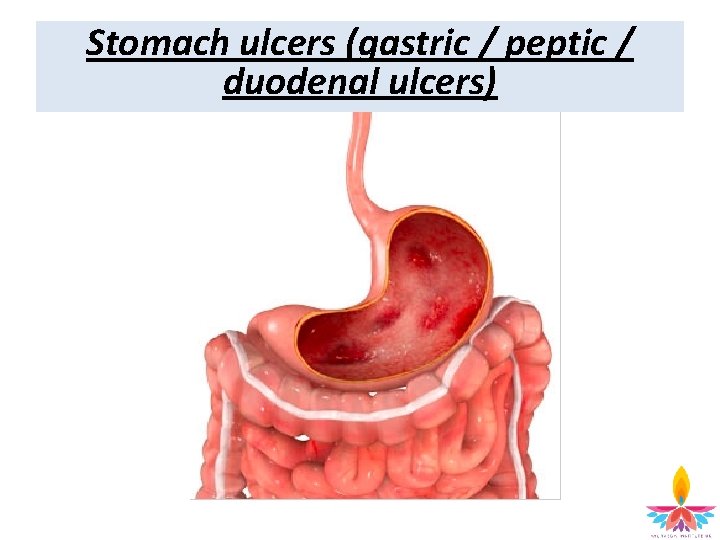
Stomach ulcers (gastric / peptic / duodenal ulcers)
Stomach ulcers (gastric / peptic / duodenal ulcers) Open sores that develop on the lining of the stomach or part of the intestine just beyond the stomach (duodenal ulcers) Signs and symptoms • burning or gnawing pain in the centre of the tummy (abdomen) • indigestion, heartburn • feeling sick Causes • infection with Helicobacter pylori (H. pylori) bacteria • (NSAIDs), such as ibuprofen or aspirin – long time or at high doses • Theory that stress or certain foods cause stomach ulcers, but little evidence to support this.
Stomach ulcers (gastric / peptic / duodenal ulcers) Who's affected • Common • people aged 60 or over • Men are more commonly affected Treatment recommended depends on cause of ulcer • Proton pump inhibitor (PPI) - reduce acid stomach produces and allow the ulcer to heal naturally • H. pylori infection - antibiotics to kill the bacteria • NSAIDs – PPIs Possible complications • bleeding at the site of the ulcer • stomach lining splitting open (perforation) • ulcer blocking movement of food through digestive system
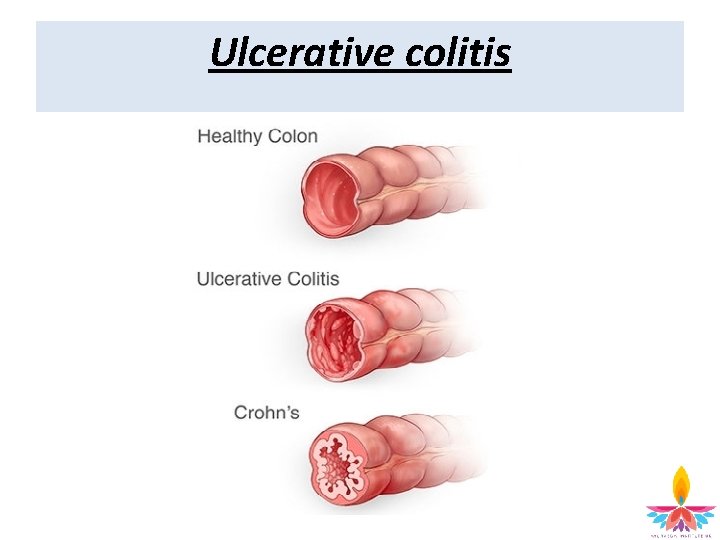
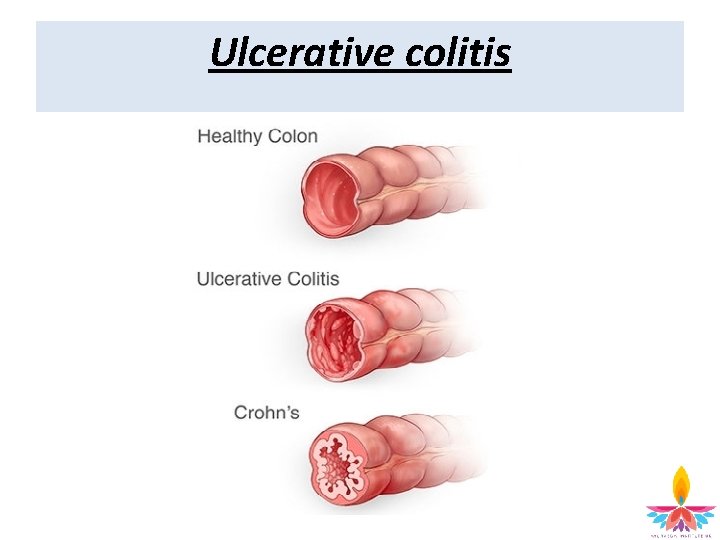
Ulcerative colitis
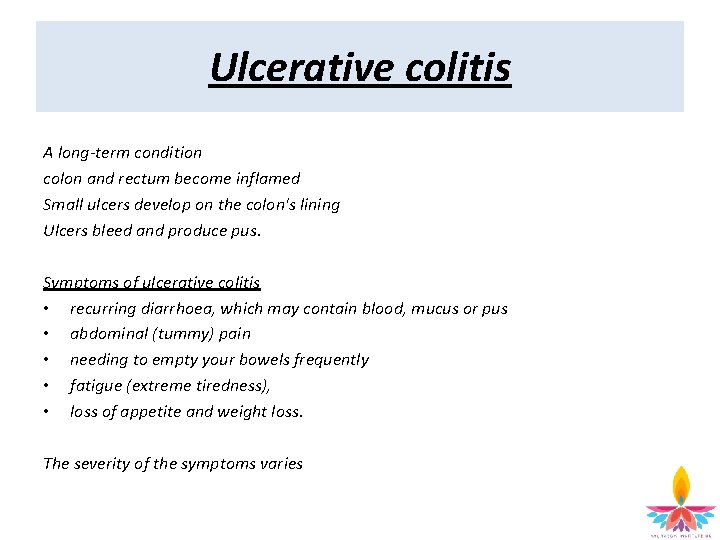
Ulcerative colitis A long-term condition colon and rectum become inflamed Small ulcers develop on the colon's lining Ulcers bleed and produce pus. Symptoms of ulcerative colitis • recurring diarrhoea, which may contain blood, mucus or pus • abdominal (tummy) pain • needing to empty your bowels frequently • fatigue (extreme tiredness), • loss of appetite and weight loss. The severity of the symptoms varies
Ulcerative colitis Symptoms of a flare-up Weeks or months with very mild symptoms, or none at all (known as remission), or periods where the symptoms are particularly troublesome, plus: • painful and swollen joints (arthritis) • mouth ulcers • areas of painful, red and swollen skin • irritated and red eyes • In severe cases, defined as having to empty your bowels six or more times a day, additional symptoms may include: • shortness of breath • a fast or irregular heartbeat • a high temperature (fever) • blood in your stools becoming more obvious
Ulcerative colitis Who's affected? • 1 in every 420 people living in the UK • Mostly 15 to 25 years old • More common in white people of European descent (especially descended from Ashkenazi Jewish communities) and black people. – rarer in people from Asian backgrounds • Both men and women
Ulcerative colitis IBD or IBS? Inflammatory bowel disease (IBD) = inflammation of the gut (gastrointestinal tract). • Ulcerative colitis • Crohn's disease
Ulcerative colitis Causes • The exact cause of ulcerative colitis is unknown • Autoimmune condition • Theories - immune system mistakes "friendly bacteria" in the colon as harmful infection / viral or bacterial infection triggers the immune system / immune system malfunction by itself • Genetics • Environmental factors eg: – – common in urban areas of northern parts of Europe and America air pollution medication and certain diets countries with improved sanitation seem to have a higher population of people with the condition - reduced exposure to bacteria may be an important factor.
Ulcerative colitis Diagnosis • Physical examination • Stool sample • Blood tests Further tests • X-ray • computerised tomography (CT) scan • examination of your rectum and colon. Sigmoidoscopy • thin, flexible tube containing a camera that's inserted into your rectum • take a sample of tissue for a biopsy. Colonoscopy • flexible tube containing a camera allows your entire colon to be examined • biopsy sample can also be taken
Ulcerative colitis Treatment • Aminosalicylates – • 5 -ASAs can be taken: – – – • Aminosalicylates (5 -ASAs), such as sulphasalazine or mesalazine - reduce inflammation. orally as a suppository through an enema Corticosteroids – – Eg. prednisolone - reduce inflammation Side effects of short-term steroid use can include: • • acne weight gain increased appetite mood changes (such as becoming more irritable) insomnia (difficulty sleeping) osteoporosis and cataracts Immunosuppressants – – Eg. tacrolimus and azathioprine - reduce the activity of the immune system usually take between 2 -3 months to work increased vulnerability to infection More prone to anaemia
Ulcerative colitis • Treating severe flare-ups • Should be managed in hospital – to minimise the risk of dehydration – colon rupturing • Ciclosporin – immunosuppressant medications - more powerful
Ulcerative colitis • Biologic medications – Infliximab, adalimumab, golimumab and vedolizumab - reduce inflammation of the intestine – Target proteins which the immune system uses to stimulate inflammation – block the receptors and reduce inflammation • Surgery – Colectomy - permanently removing the colon – small intestine used to pass waste products out of your body – ileostomy – where the small intestine is diverted out of a hole made in your abdomen. – ileo-anal pouch (also known as a J-pouch) – where part of the small intestine is used to create an internal pouch that is then connected to your anus, allowing you to pass stools normally
Ulcerative colitis Dietary advice Although a specific diet isn't thought to play a role in causing ulcerative colitis, some changes to your diet can help control the condition. • eat small meals – eating five or six smaller meals a day • drink plenty of fluids • avoid caffeine and alcohol and fizzy drinks • take food supplements • Keep a food diary – – • You may find some foods make your symptoms worse and you can eliminate them from your diet. Don’t eliminate entire food groups (such as dairy products) from your diet without speaking to your care team Low residue diet – – – – Designed to reduce the amount and frequency of the stools you pass: white bread refined (non-wholegrain) breakfast cereals, such as cornflakes white rice, refined pasta and noodles cooked vegetables (but not the peel, seeds or stalks) lean meat and fish eggs
Ulcerative colitis Stress relief • Although stress doesn't cause ulcerative colitis, successfully managing stress levels may reduce the frequency of symptoms Complications • Osteoporosis • Poor growth and development • Can affect growth and delay puberty Toxic megacolon • rare and serious complication • where inflammation in the colon causes gas to become trapped • colon becomes enlarged and swollen / rupture • cause infection in the blood (septicaemia) Bowel cancer • Bowel cancer (cancer of the colon, rectum or bowel). The longer you have ulcerative colitis, the greater the risk. • People with ulcerative colitis are often unaware they have bowel cancer as the initial symptoms of this type of cancer are similar. These include: – – – blood in the stools diarrhoea abdominal pain
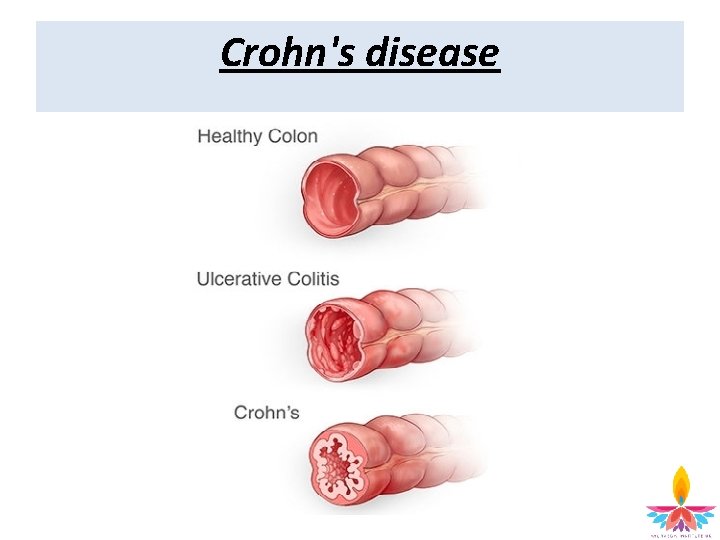
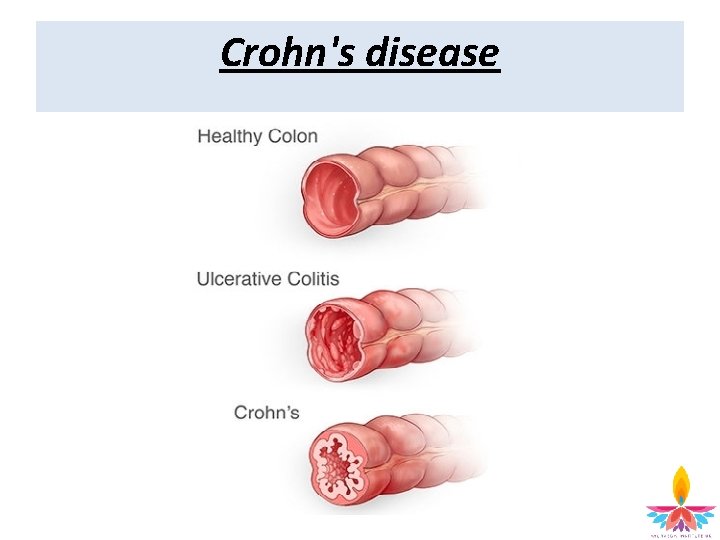
Crohn's disease
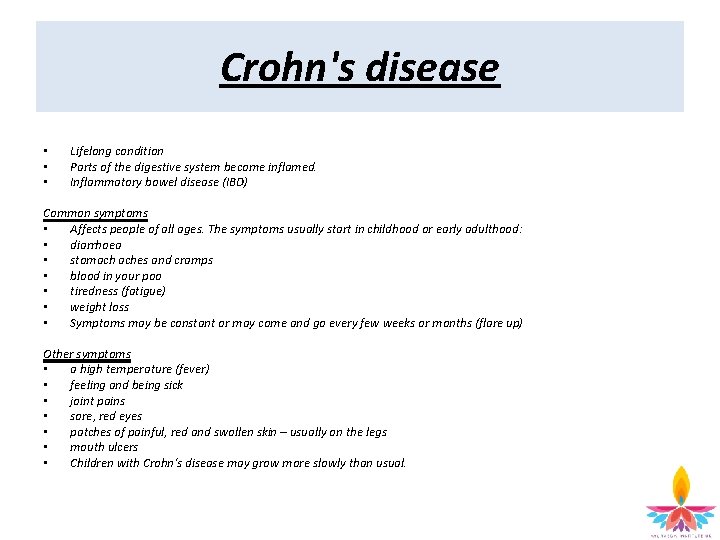
Crohn's disease • • • Lifelong condition Parts of the digestive system become inflamed. Inflammatory bowel disease (IBD) Common symptoms • Affects people of all ages. The symptoms usually start in childhood or early adulthood: • diarrhoea • stomach aches and cramps • blood in your poo • tiredness (fatigue) • weight loss • Symptoms may be constant or may come and go every few weeks or months (flare up) Other symptoms • a high temperature (fever) • feeling and being sick • joint pains • sore, red eyes • patches of painful, red and swollen skin – usually on the legs • mouth ulcers • Children with Crohn's disease may grow more slowly than usual.
Crohn's disease Causes The exact cause of Crohn's disease is unknown. It's thought several things could play a role, including: • your genes • a problem with the immune system • smoking • a previous stomach bug • an abnormal balance of gut bacteria • There's no evidence to suggest a particular diet causes Crohn's disease Tests: • Colonoscopy – a thin, flexible tube with a camera at the end is inserted into your bottom to look for inflammation in your bowel • a biopsy – tiny pieces of your bowel are removed during a colonoscopy and checked for signs of Crohn's disease • an MRI scan or CT scan – you may have a special drink first to make your bowel show up clearly on the scan
Crohn's disease Treatments • • Steriods Immunosuppressants Surgery Liquid diet – • For children and young adults, a liquid diet (enteral nutrition) can also help reduce symptoms (special drinks that contain all the nutrients you need for a few weeks) Biological medicines – adalimumab, infliximab, vedolizumab and ustekinumab. Surgery • Resection - removing a small inflamed section of bowel. • Stitching the healthy parts of bowel together. Diet and lifestyle If you think a particular food is triggering your symptoms, see if avoiding it helps. But don't make any big changes to your diet without speaking to your GP or care team first.
Crohn's disease Possible complications • damage to your bowel – such as scarring and narrowing (strictures) – ulcers – fistulas • difficulty absorbing nutrients from food – leading to osteoporosis or anaemia • bowel cancer – after 10 years the risk is about 1 in 50 – after 20 years the risk is about 1 in 10 – after 30 years the risk is about 1 in 5
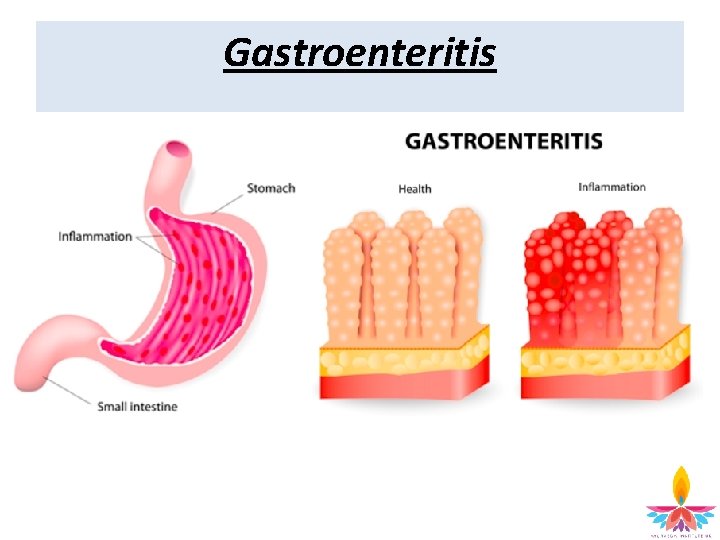
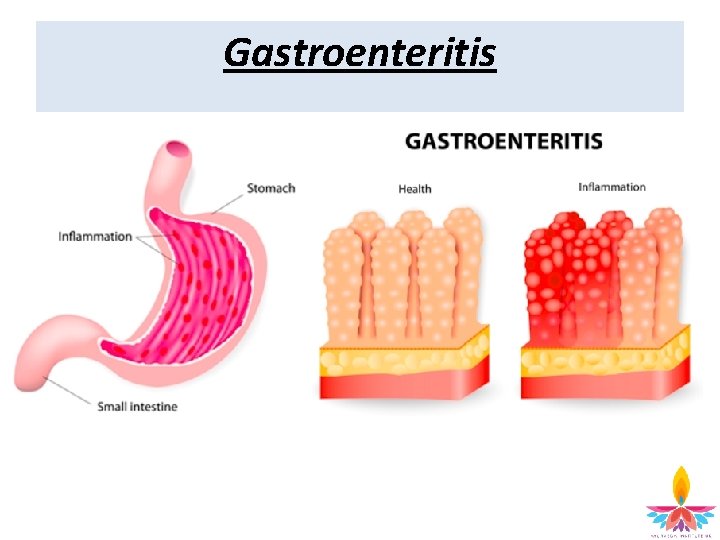
Gastroenteritis
Gastroenteritis • • • common condition causes diarrhoea and vomiting bacterial or viral tummy bug common in young children In children - caused by a virus called rotavirus In adults - caused by norovirus (the "winter vomiting bug") or bacterial food poisoning. Symptoms • sudden, watery diarrhoea • feeling sick • vomiting, which can be projectile • a mild fever • Some people also have other symptoms, such as a loss of appetite, an upset stomach, aching limbs and headaches.
Gastroenteritis Treatment • Stay at home - let the illness run its course • Drink fluids to avoid dehydration • Paracetamol • Rest • Rehydration drinks • Anti-vomiting medication • antidiarrhoeal medication • Can spread very easily
Gastritis Lining of the stomach inflamed after damage Common condition Symptoms • indigestion • gnawing or burning stomach pain • nausea and vomiting • feeling full after eating • If the stomach lining has been worn away (erosive gastritis) symptoms may include pain, bleeding or a stomach ulcer.
Gastritis Diagnosing gastritis • a stool test – infection or bleeding from the stomach • a breath test for Helicobacter pylori (H. pylori) infection • an endoscopy – endoscope passed into your oesophagus and stomach to look for signs of inflammation • a barium swallow – you're given some barium solution, which shows up clearly on X-rays as it passes through your digestive system Possible causes of gastritis • a H. pylori bacterial infection • excessive use of cocaine or alcohol • aspirin, ibuprofen or other painkillers classed as (NSAIDs) • a stressful event – bad injury / critical illness / major surgery • an autoimmune reaction

Gastritis Treating gastritis • reduce the amount of acid in the stomach • Antacids • histamine 2 (H 2) blockers such as ranitidine – decrease acid production • proton pump inhibitors (PPIs) such as omeprazole – decrease acid production
Gastritis Possible complications of gastritis • stomach ulcer • polyps (small growths) in stomach • tumours in stomach, which may or may not be cancerous Gastritis vs gastroenteritis: the difference • Gastroenteritis: inflammation (irritation) of the stomach and bowel, caused by an infection • Gastritis: inflammation of the stomach lining specifically, and not always caused by infection
Irritable bowel syndrome (IBS) • • common condition usually a lifelong problem Symptoms • stomach pain or cramps – usually worse after eating and better after doing a poo • bloating • diarrhoea • constipation • farting (flatulence) • passing mucus from your bottom • tiredness and a lack of energy • feeling sick (nausea) • backache • problems peeing – like needing to pee often, sudden urges to pee, and feeling like you can't fully empty your bladder • not always being able to control when you poo (incontinence)
Irritable bowel syndrome (IBS) Tests for IBS • There's no test for IBS • a blood test to check for problems like coeliac disease • tests on a sample of your poo to check for infections and inflammatory bowel disease (IBD) Diet, lifestyle and medicines • cook homemade meals using fresh ingredients when you can • keep a diary of what you eat and any symptoms you get – try to avoid things that trigger your IBS • try to find ways to relax • get plenty of exercise • try probiotics for a month to see if they help • don’t delay or skip meals • don’t eat too quickly • don’t eat lots of fatty, spicy or processed foods • don’t eat more than 3 portions of fresh fruit a day (a portion is 80 g) • don’t’ drink more than 3 cups of tea or coffee a day • don’t drink lots of alcohol or fizzy drinks
Irritable bowel syndrome (IBS) How to ease bloating, cramps and farting • eat oats (such as porridge) regularly • eat up to 1 tablespoon of linseeds a day • avoid foods that are hard to digest – like cabbage, broccoli, cauliflower, brussels sprouts, beans, onions and dried fruit • avoid products containing a sweetener called sorbitol • ask a pharmacist about medicines that can help, like Buscopan or peppermint oil How to reduce diarrhoea • cut down on high-fibre foods, like wholegrain foods (such as brown bread and brown rice), nuts and seeds • avoid products containing a sweetener called sorbitol How to relieve constipation • drink plenty of water • increase how much soluble fibre you eat – good foods include oats, pulses, carrots, peeled potatoes and linseeds • laxatives
Irritable bowel syndrome (IBS) Low FODMAP diet Avoiding foods that aren't easily broken down by the gut, eg: • fruit and vegetables • milk • wheat products IBS medicines • amitriptyline • citalopram • Antidepressants - can also help ease IBS symptoms
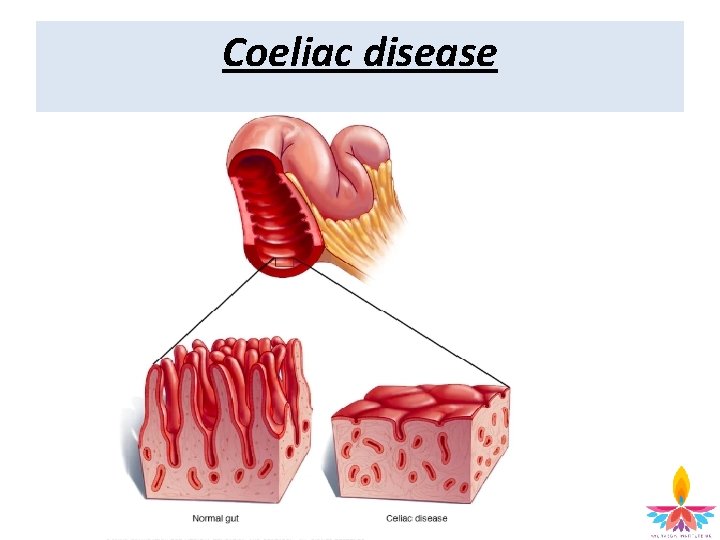
Coeliac disease
Coeliac disease Symptoms • Range from mild to severe, and often come and go. • Mild cases may not cause any noticeable symptoms • Treatment is recommended even when symptoms are mild or non-existent, because complications can still occur. Common symptoms • Diarrhoea (most common - caused by the body not being able to fully absorb nutrients) • Malabsorption (leads to stools with high levels of fat (steatorrhoea) - foul smelling, greasy, frothy, difficult to flush) Other symptoms • abdominal pain • bloating and flatulence (passing wind) • indigestion • constipation • vomiting (usually only affects children)
Coeliac disease More general symptoms • fatigue (extreme tiredness), which may be a sign of iron deficiency anaemia or vitamin B 12 folate deficiency anaemia • unexpected weight loss • an itchy rash (see below) • difficulty getting pregnant • tingling and numbness in your hands and feet (peripheral neuropathy) • disorders that affect co-ordination, balance and speech (ataxia) • swelling of the hands, feet, arms and legs caused by a build-up of fluid (oedema)
Coeliac disease • Malnutrition – Malnutrition in children can result in failure to grow at the expected rate, and delayed puberty. • Dermatitis herpetiformis – skin rash – 1 in 5 with coeliac develop this – Itchiness – blisters that burst when scratched – on elbows, knees and buttocks, anywhere
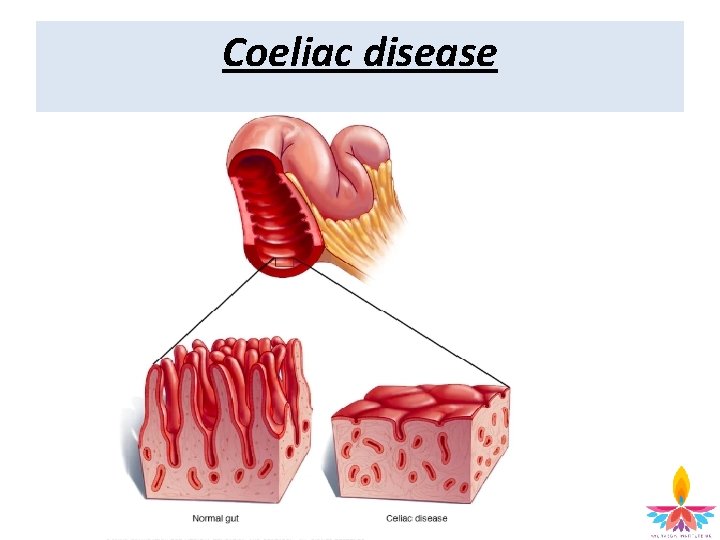
Coeliac disease Causes • • Abnormal immune system reaction to the protein gluten (in foods such as bread, pasta, cereals and biscuits) Autoimmune condition (immune system mistakes gliadin in gluten as a threat to the body). Antibodies cause the surface of your intestine to become inflamed (red and swollen). – surface of the intestine is covered with millions of tiny tube-shaped growths called villi (increase the surface area of gut for more effective digestion) – damage and inflammation to the lining of the gut flattens the villi, reducing their ability to help with digestion. – As a result, intestine isn't able to digest the nutrients from food, which causes the symptoms of coeliac. Oats – oats contaminated by other grains during production / contain a protein called avenin - similar to gluten
Coeliac disease Causes • Family history (10% risk) • Mutations to genes called the HLA-DQ genes (responsible for development of the immune system) • Environmental factors • Digestive system infection (such as a rotavirus infection) during early childhood. • Introducing gluten into your baby's diet < 3 months old • type 1 diabetes • thyroid conditions • ulcerative colitis – a digestive condition that causes inflammation of the colon (large bowel) • neurological disorders (which affect the brain and nervous system) such as epilepsy • Down's syndrome and Turner syndrome
Coeliac disease Diagnosis • blood tests (antibodies usually present) – possible to have coeliac disease and not have antibodies in blood • Biopsy • Endoscope (tube with camera) inserted into mouth to small intestine (to take samples of the lining of small intestine) Tests after diagnosis To assess how the condition has affected body: • blood tests (levels of iron and other vitamins and minerals) • Skin biopsy (for dermatitis herpetiformis) • DEXA scan (X-ray that measures bone density)
Coeliac disease Treatment • • • excluding foods that contain gluten for life “Your symptoms will return if you eat foods containing gluten, and it will cause long-term damage to your health. ” Can take up to two years for your digestive system to heal completely Other treatments • Vaccinations • Extra vaccinations (due to spleen working less effectively and increasing vulnerability to infection), including: – flu (influenza) jab – Hib/Men. C vaccine, which protects against sepsis, pneumonia and meningitis – pneumococcal vaccine (for Streptococcus pneumoniae bacterium) – Supplements – Dermatitis herpetiformis (sometimes Dapsone prescribed to speed up healing time) Refractory coeliac disease • Rarer type of coeliac disease where the symptoms continue, even after switching to a gluten-free diet. • The reasons for this are unclear (affects 1 / 140 people with coeliac) • Treatment options include steroid medication (corticosteroids), such as prednisolone.
Coeliac disease Complications • Malabsorption cause: • iron deficiency anaemia • vitamin B 12 and folate deficiency anaemia • osteoporosis • Malnutrition • Lactose intolerance • Cancer (very rare but serious complication)
Haemorrhoids (piles)
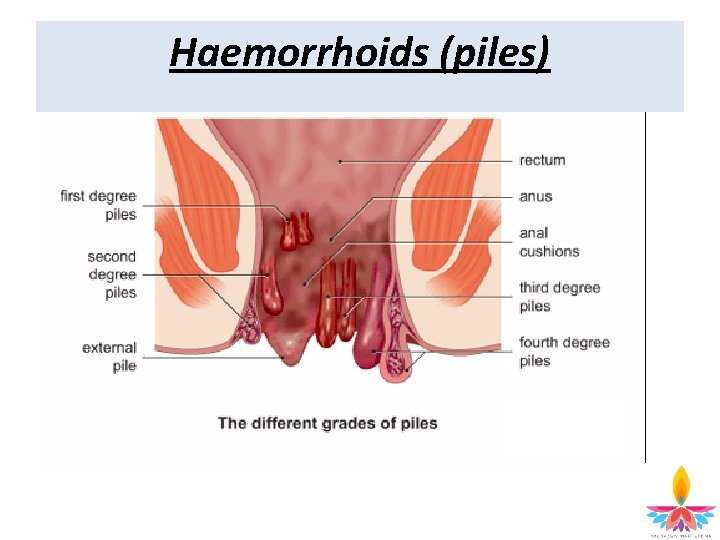
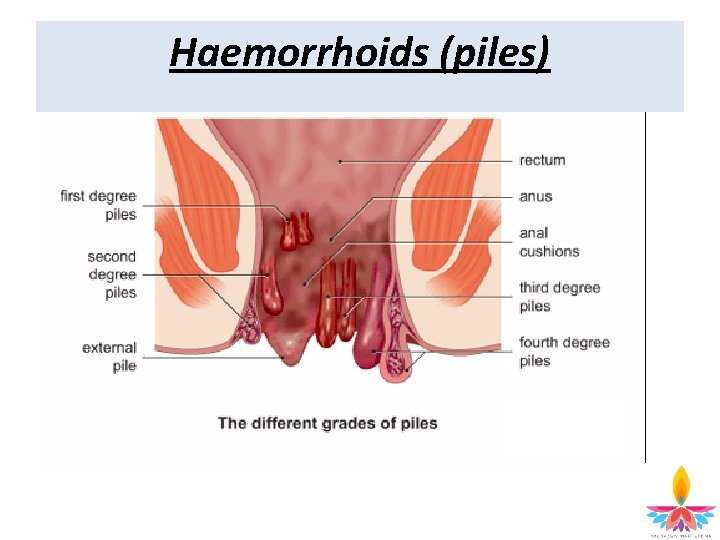
Haemorrhoids (piles) • Swellings containing enlarged blood vessels found inside or around the bottom (the rectum and anus) Symtoms • bleeding after passing a stool – the blood is usually bright red • itchy bottom • a lump hanging down outside of the anus, which may need to be pushed back in after passing a stool • a mucus discharge after passing a stool • soreness, redness and swelling around your anus • Haemorrhoids aren't usually painful, unless their blood supply slows down or is interrupted. Causes • The exact cause of haemorrhoids is unclear • increased pressure in the blood vessels in and around your anus, causing them to become swollen and inflamed • too much straining on the toilet. • Chronic (long-term) diarrhoea can also make you more vulnerable to getting haemorrhoids. • being overweight or obese • age • being pregnant • having a family history of haemorrhoids • regularly lifting heavy objects • a persistent cough or repeated vomiting • sitting down for long periods of time
Haemorrhoids (piles) Preventing and treating haemorrhoids • increasing the amount of fibre in your diet • drinking plenty of fluid • not delaying going to the toilet • avoiding medication that causes constipation • losing weight if you're overweight • exercising regularly Types of haemorrhoids • Internal haemorrhoids - upper two-thirds of your anal canal • External haemorrhoids - lower third, closest to your anus
Haemorrhoids (piles) Over-the-counter topical treatments • creams, ointments and suppositories available without a prescription. • Corticosteroid cream • Painkillers • Laxatives Banding & sclerotherapy • For haemorrhoids in the upper part of anal canal • Banding = placing a very tight elastic band around the base of haemorrhoids to cut off their blood supply • haemorrhoids falls off within a week
Haemorrhoids (piles) Injections (sclerotherapy) • alternative to banding • chemical solution injected into the blood vessels to decrease haemorrhiods Electrotherapy • alternative to banding - smaller haemorrhoid • Device inserted into the anus - electric current is passed through the haemorrhoid – shrinks haemorroid Haemorrhoidectomy • operation to remove haemorrhoids – open anus and cut out Haemorrhoidal artery ligation • reduce the blood flow to your haemorrhoids with ultrasound probe Stapling • the last section of the large intestine is stapled to prevent prolapse of haemorrhoids Other treatments • freezing • laser treatment
Ajeerna, Grahani & Arsas Disorders of the digestive tract The Ayurvedic perspective
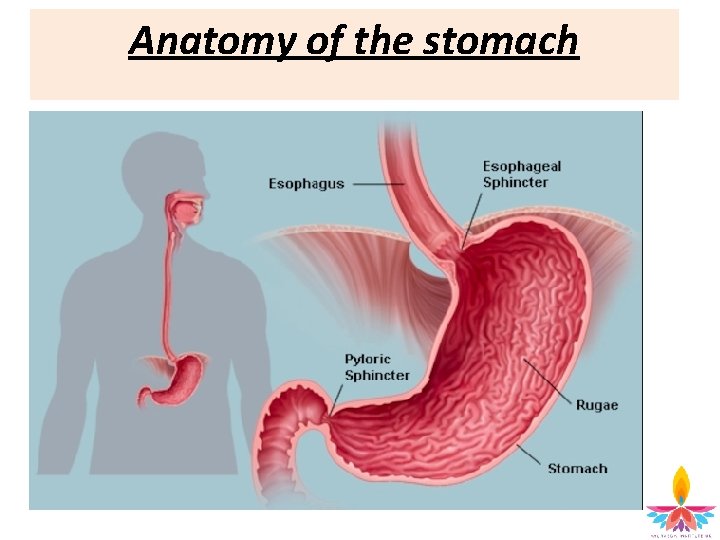
Anatomy of the stomach
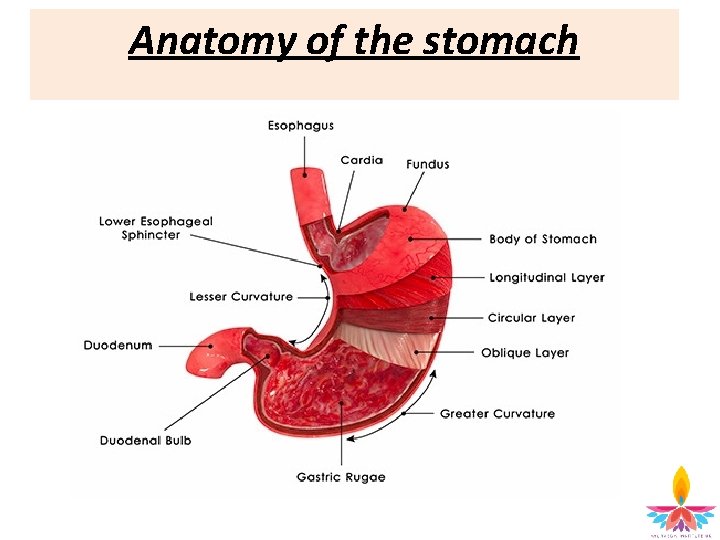
Anatomy of the stomach
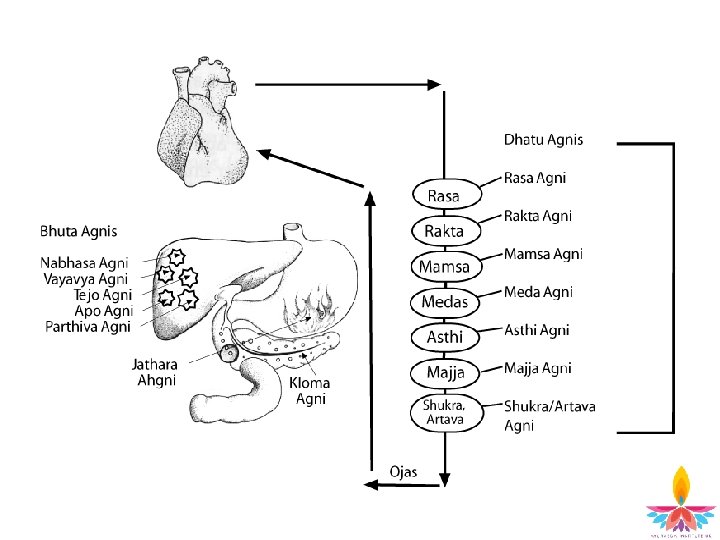
Agni (digestive fire) Agni (Digestive Fire) • is a transformative energy in the body • helps the digestion and assimilation of food • There are 13 agnis: – Jatharagni – Panchabhuta agni (5) – Dhatu agni (7)
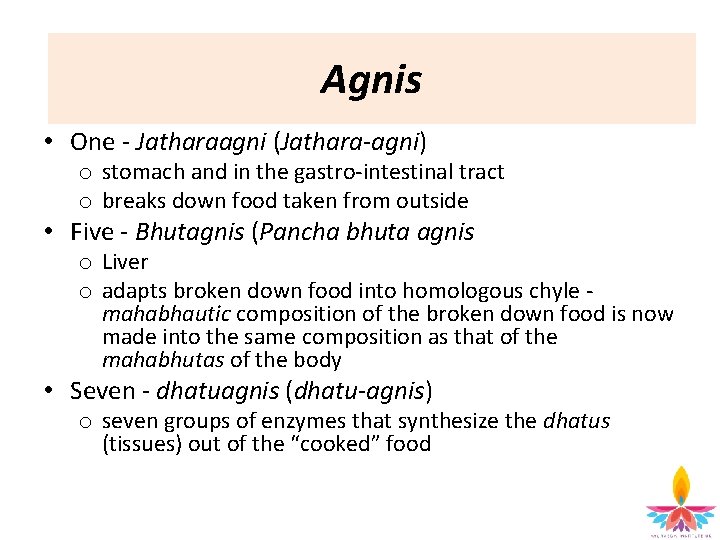
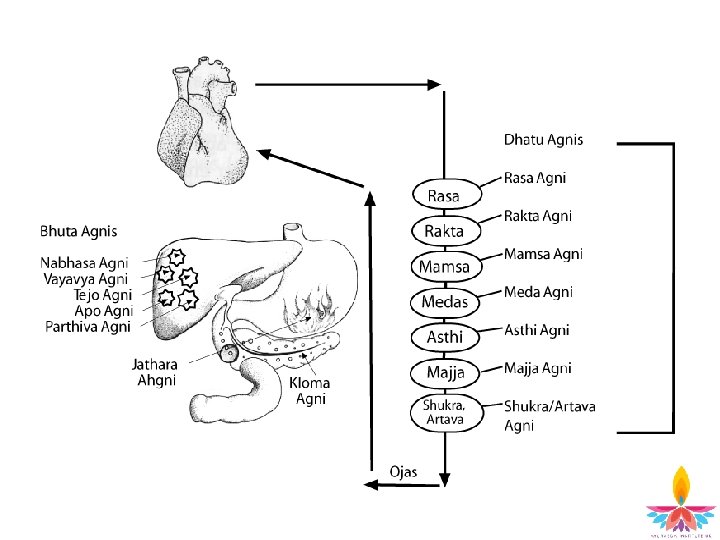
Agnis • One - Jatharaagni (Jathara-agni) o stomach and in the gastro-intestinal tract o breaks down food taken from outside • Five - Bhutagnis (Pancha bhuta agnis o Liver o adapts broken down food into homologous chyle - mahabhautic composition of the broken down food is now made into the same composition as that of the mahabhutas of the body • Seven - dhatuagnis (dhatu-agnis) o seven groups of enzymes that synthesize the dhatus (tissues) out of the “cooked” food

Ama and its Formation Diminution of agni (agni mandya) causes ama (toxicity) Ama settles in parts of the body, eg. lungs, heart or any visera Ama mixed with doshas go to the site of a manifestation of a disease Then signs and symptoms manifest Agnis are then affected by ama If “uncooked“ food remains, the channels get obstructed The organ that is stressed / weakened / similar in mahabhutic composition accepts the ama more easily
Functions of Agni • • Increase lifespan Balance dosha Build dhatu Increase colour / texture of the superficial fascia Improve health and strength of the body Increase enthusiasm Increase vigour, complexion, ojas Increase prana
Balance & extinction of agni Balanced agni (sama agni) If agni is balanced, and the rperson eats appropriate food, according to his hunger and correct quantity, the person experiences: • Pleasant breath • Enthusiasm • Satisfaction of hunger and thirst • Lightness • Energy Extinction of agni • The reduction or extinction of agni = root of disorder & can lead ultimately to death
Four Agnis • Tikshna agni – hyper functioning / increased (associated with pitta constitutions) • Manda agni – hypo-funtioning / decreased (associated with kapha constitutions) • Vishama agni – variable functioning (associated with vata constitutions) • Sama agni – a balanced state of this agni
Ajeerna (indigestion) • Ajeerna = imbalance of digestive fire • Referred to as food intolerance / allergy in Western medicine Nidana Ø Fasting Ø Over-eating Ø Eating before previous meal digested Ø Eating food incompatible with constitution Ø Food with unpleasant taste and appearance Ø Rotten food Ø Very dry and rough food Ø Very cold food Ø Very hot food Ø Improper administration of purgative, emetic and oleation therapies Ø Residing in improper country Ø Seasonal perversions Ø Suppression of natural urges
Nidana Ajeerna Madhava nidhana (ch 6, p 57) • • • Excessive consumption of water Incompatible food Suppression of natural urges Reversal of sleeping habits Failure to properly digest even when consuming food at the correct time and in correct dosage Failure to properly digest food when taken whilst experiencing jealousy, fear and anger As a result of other disorders Food taken not to his liking Eating when suffering with anxiety, sleeping in an uncomfortable bed and insomnia
Ajeerna Purva rupa & Rupa • Tightness of stomach due to dry or imbalanced faeces • Abdominal distension • Feeling of prostration (being scrunched up) • Headache • Fainting • Giddiness • Stiffness of the back and lumbar region • Yawning • Malaise • Morbid thirst
Ajeerna Purva rupa & Rupa • Tenesmus (a continual or recurrent inclination to evacuate the bowels, caused by disorder of the rectum or other illness) • Anorexia • Food poisoning • Flu like feeling • Lack of appetite • Feeling of regurgitation • Foul taste in mouth • Excess production of saliva • Nausea • Feeling overheated
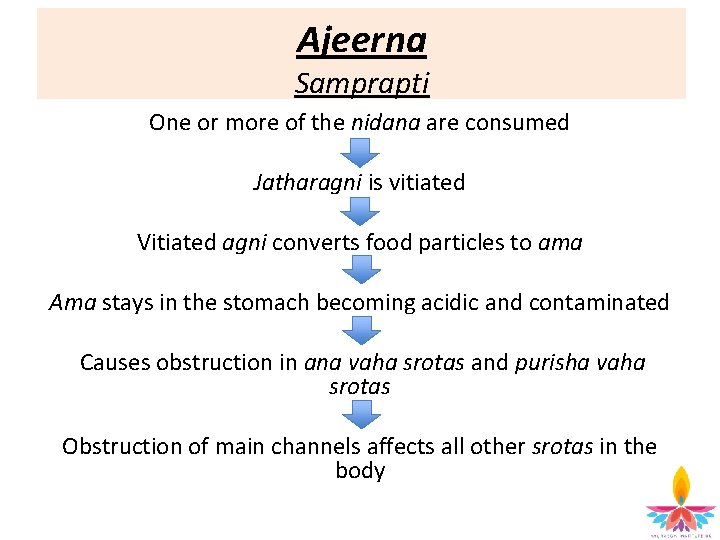
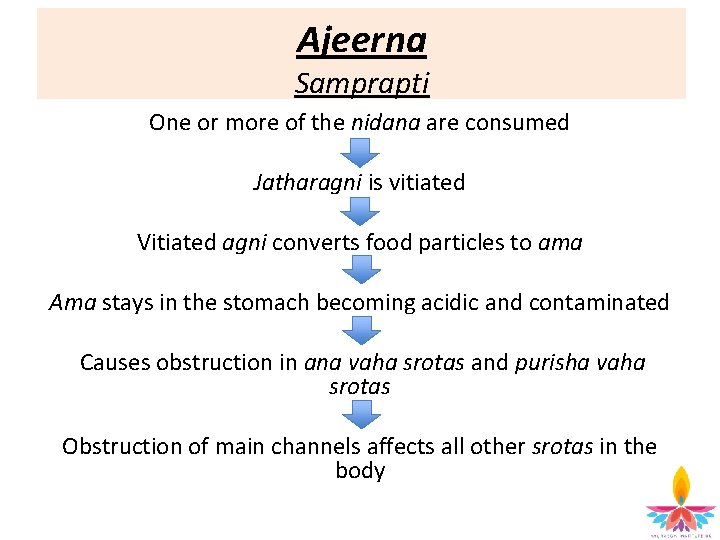
Ajeerna Samprapti One or more of the nidana are consumed Jatharagni is vitiated Vitiated agni converts food particles to ama Ama stays in the stomach becoming acidic and contaminated Causes obstruction in ana vaha srotas and purisha vaha srotas Obstruction of main channels affects all other srotas in the body
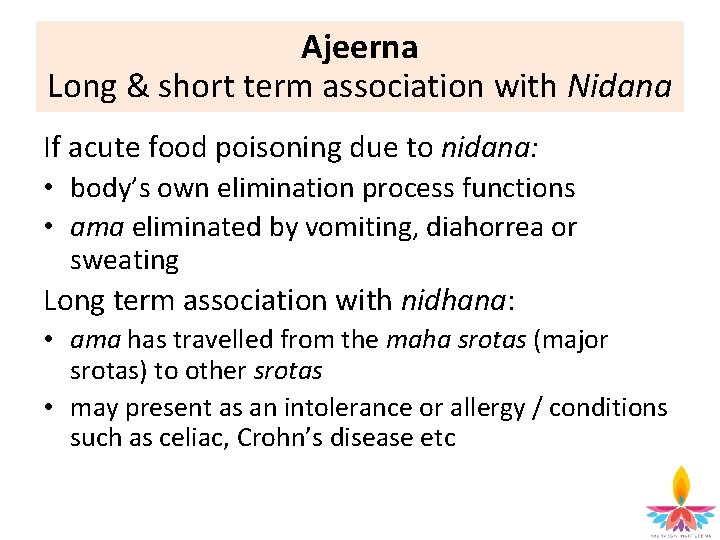
Ajeerna Long & short term association with Nidana If acute food poisoning due to nidana: • body’s own elimination process functions • ama eliminated by vomiting, diahorrea or sweating Long term association with nidhana: • ama has travelled from the maha srotas (major srotas) to other srotas • may present as an intolerance or allergy / conditions such as celiac, Crohn’s disease etc
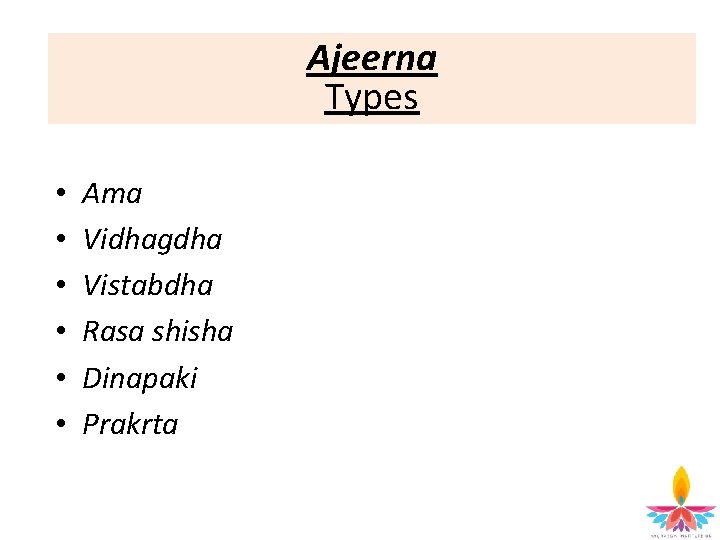
Ajeerna Types • • • Ama Vidhagdha Vistabdha Rasa shisha Dinapaki Prakrta
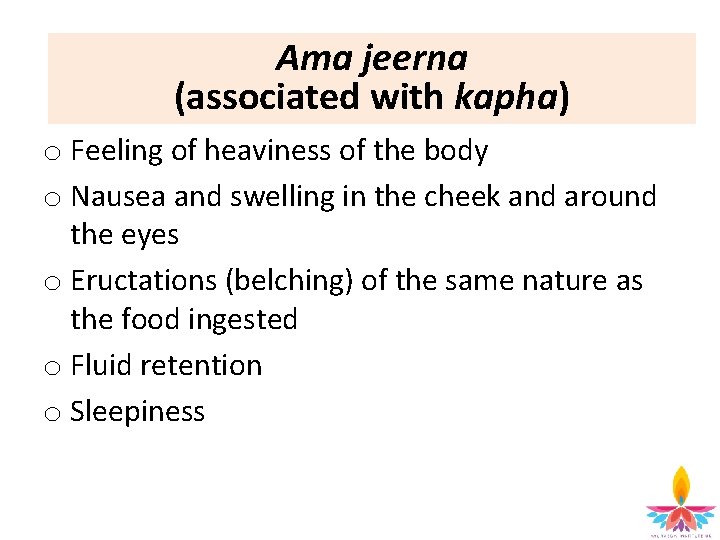
Ama jeerna (associated with kapha) o Feeling of heaviness of the body o Nausea and swelling in the cheek and around the eyes o Eructations (belching) of the same nature as the food ingested o Fluid retention o Sleepiness
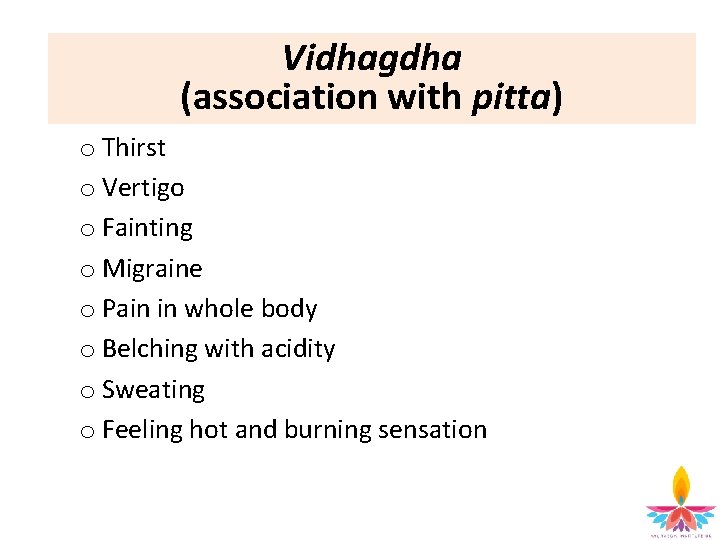
Vidhagdha (association with pitta) o Thirst o Vertigo o Fainting o Migraine o Pain in whole body o Belching with acidity o Sweating o Feeling hot and burning sensation
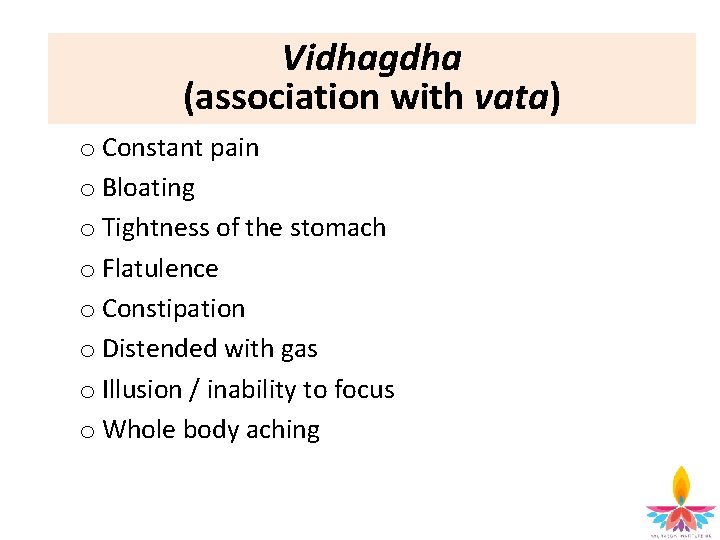
Vidhagdha (association with vata) o Constant pain o Bloating o Tightness of the stomach o Flatulence o Constipation o Distended with gas o Illusion / inability to focus o Whole body aching
Rasa shisha Ajeerna Symptoms always appear at the end of the digestive process: o Body feeling toxic o Bad taste in the mouth o Nausea o Heavy heart / strain o Heaviness of the body o Lethargy
Ajeerna Dinapaki & Prakrta Dinapaki ajeerna • Symptoms appear after every meal • Discomfort Prakrta ajeerna Seasonal changes that affect digestion: • Eg. In winter, more warm and protein prominent foods are required to hibernate. If cold or raw food is consumed during this season, it causes incomplete digestion and creates ama
Ajeerna Upadhrava (complications) • • Fainting Delirium Vomiting Excessive salivation Depression Dizziness Death (due to acute indigestion eg. Such as nut allergy)
Acute Ajeerna The further ajeerna progresses it leads to: • Visuchika (gastroenteritis) • Vilambhika (paralytic ileus or celiac)
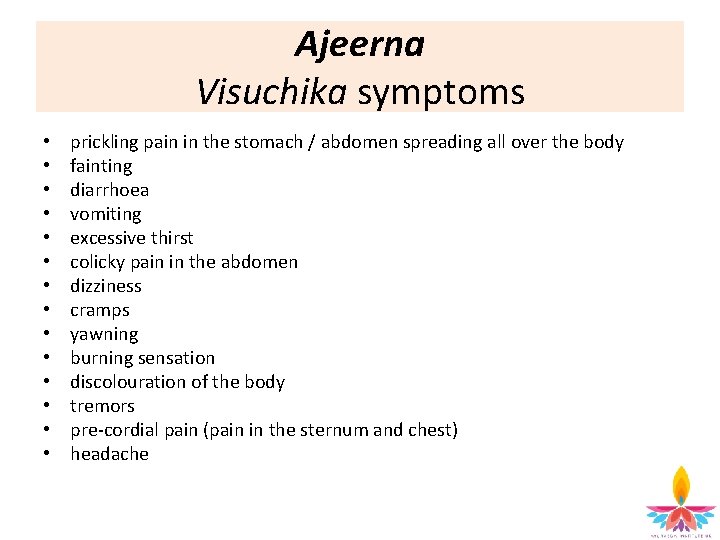
Ajeerna Visuchika symptoms • • • • prickling pain in the stomach / abdomen spreading all over the body fainting diarrhoea vomiting excessive thirst colicky pain in the abdomen dizziness cramps yawning burning sensation discolouration of the body tremors pre-cordial pain (pain in the sternum and chest) headache
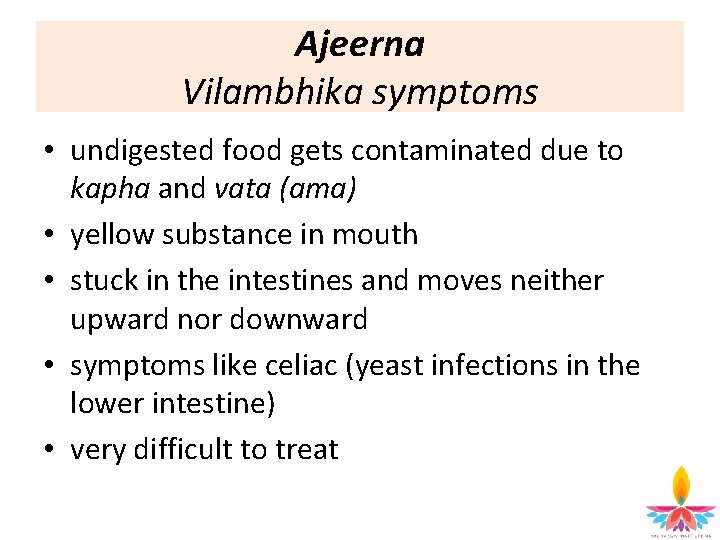
Ajeerna Vilambhika symptoms • undigested food gets contaminated due to kapha and vata (ama) • yellow substance in mouth • stuck in the intestines and moves neither upward nor downward • symptoms like celiac (yeast infections in the lower intestine) • very difficult to treat
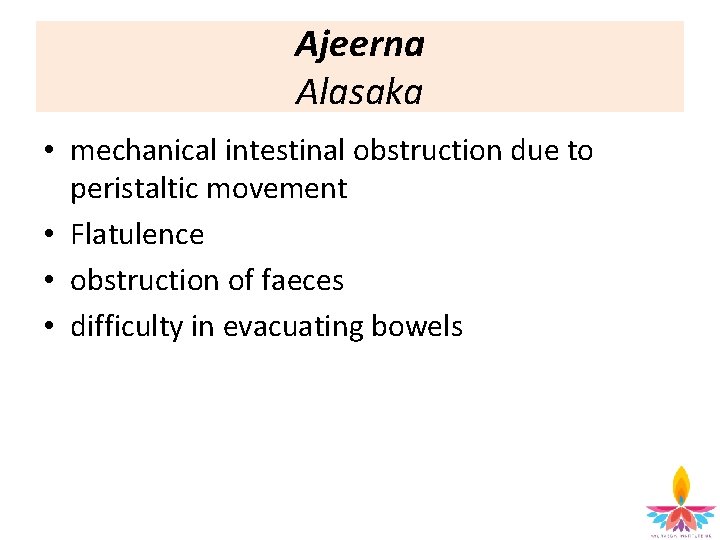
Ajeerna Alasaka • mechanical intestinal obstruction due to peristaltic movement • Flatulence • obstruction of faeces • difficulty in evacuating bowels
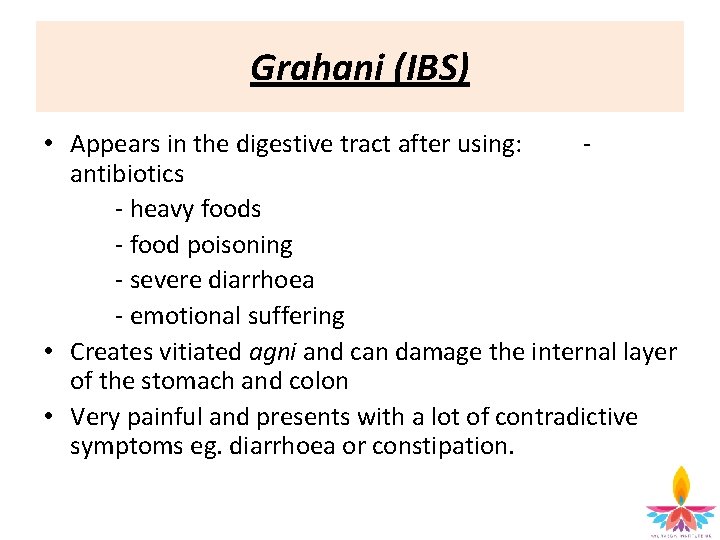
Grahani (IBS) • Appears in the digestive tract after using: - antibiotics - heavy foods - food poisoning - severe diarrhoea - emotional suffering • Creates vitiated agni and can damage the internal layer of the stomach and colon • Very painful and presents with a lot of contradictive symptoms eg. diarrhoea or constipation.

Grahani Nidana Excessive fasting Eating despite indigestion Excessive eating Unconstitutional eating Eating unpleasant substance eg. snakes and cockroach • Eating heavy foods • Eating very cold foods • Very rough foods • • •
Grahani Nidana • Fermented foods • Excessive vomiting, purgative and enemas treatments • Emaciation (and weakness) as a result of serious disorder • Environmental causes e. g. very hot and humid climates • Stage of life factors eg. stress • Seasonal changes eg. dampness • Suppression of natural urges • Mental stress, heavy workload
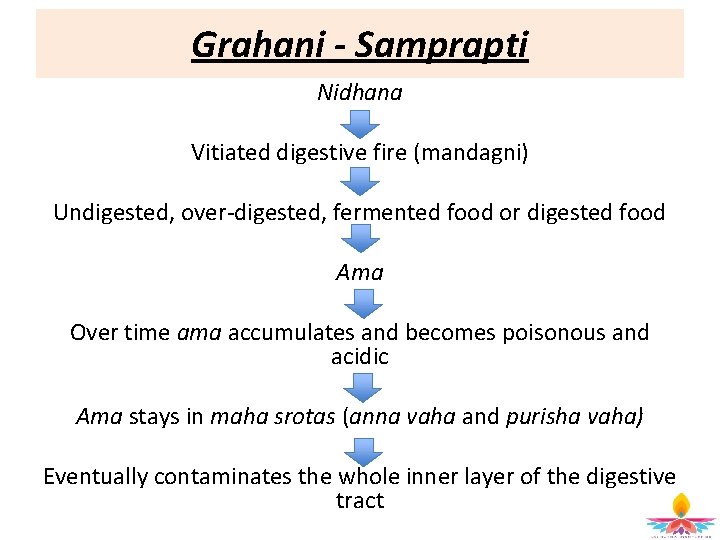
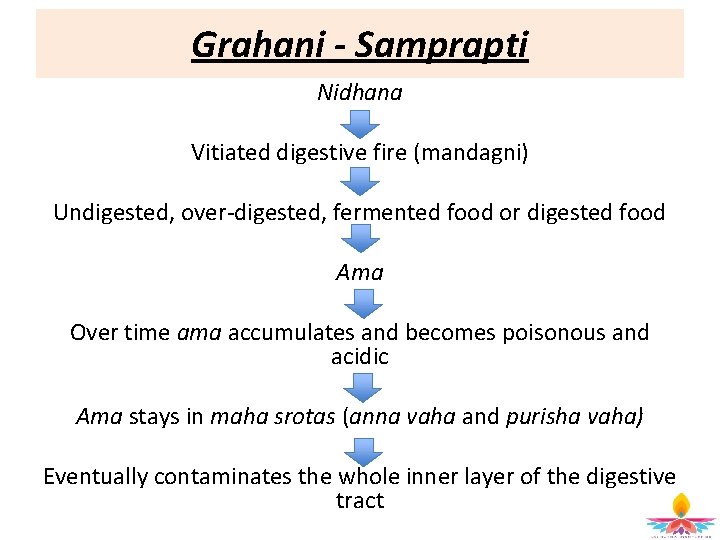
Grahani - Samprapti Nidhana Vitiated digestive fire (mandagni) Undigested, over-digested, fermented food or digested food Ama Over time ama accumulates and becomes poisonous and acidic Ama stays in maha srotas (anna vaha and purisha vaha) Eventually contaminates the whole inner layer of the digestive tract
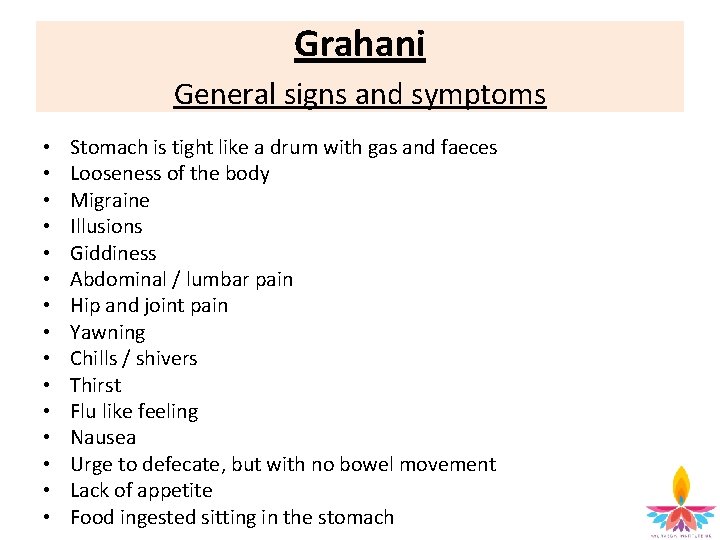
Grahani General signs and symptoms • • • • Stomach is tight like a drum with gas and faeces Looseness of the body Migraine Illusions Giddiness Abdominal / lumbar pain Hip and joint pain Yawning Chills / shivers Thirst Flu like feeling Nausea Urge to defecate, but with no bowel movement Lack of appetite Food ingested sitting in the stomach
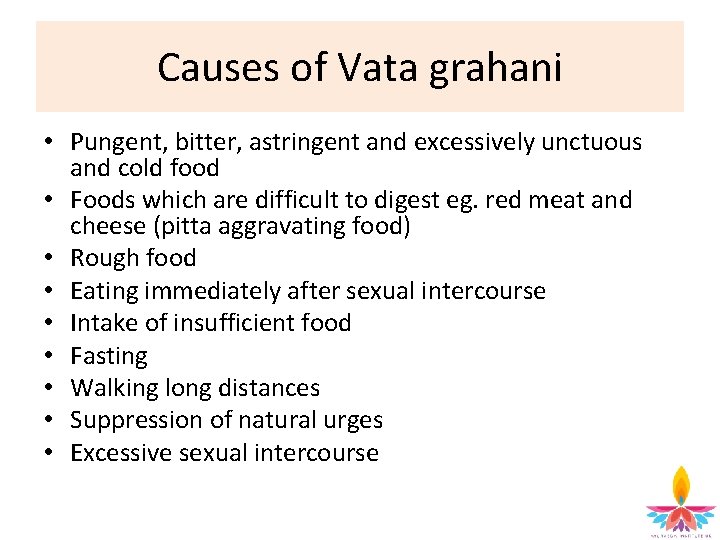
Causes of Vata grahani • Pungent, bitter, astringent and excessively unctuous and cold food • Foods which are difficult to digest eg. red meat and cheese (pitta aggravating food) • Rough food • Eating immediately after sexual intercourse • Intake of insufficient food • Fasting • Walking long distances • Suppression of natural urges • Excessive sexual intercourse
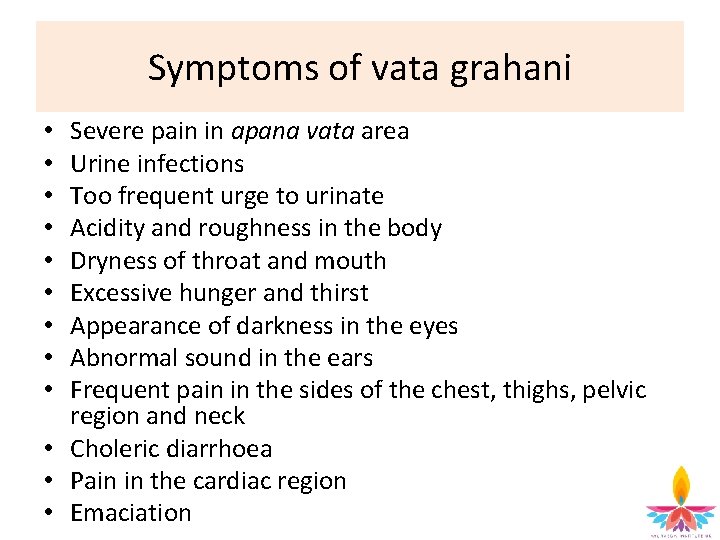
Symptoms of vata grahani Severe pain in apana vata area Urine infections Too frequent urge to urinate Acidity and roughness in the body Dryness of throat and mouth Excessive hunger and thirst Appearance of darkness in the eyes Abnormal sound in the ears Frequent pain in the sides of the chest, thighs, pelvic region and neck • Choleric diarrhoea • Pain in the cardiac region • Emaciation • • •
Symptoms of vata grahani • • • Weakness Distaste in the mouth Sawing pain in the abdomen Craving for ingredients of food having all tastes Mental frustration Flatulence after and during the process of digestion Temporary feeling of relief immediately after the intake of food Patient suspects liver and spleen infected Passing stool with difficulty (liquid mixed with hard stool, thin and associated with mucous, sounds and froth) Voids stools frequently Cough dyspnoea
Causes of pitta grahani • Excessive eating of rough foods eg. roughage / fibrous foods • Foods which are hard to digest eg. beef, cheese, bush meat • Pitta increasing foods • Foods which are pungent, sour, alkaline • As a result of the above causes the digestive fire melts like liquid lava (bile) and is mixed with the food. It becomes yellowish, with a foul and sour taste, fermented and fishy smell.
Symptoms of pitta grahani • Diarrhoea or loose stools containing undigested material which is bluish- yellow or yellow • Eructation (belching) with foul smell and sour taste • Burning sensation in the stomach • Burning sensation in the cardiac region and throat • Excessive thirst • Mouth ulcers • Halitosis (bad breath) • Bile coming into the mouth • Acidic or fishy smell in the mouth and body area • Anorexia
Causes of kapha grahani • • Heavy food Excessive intake of unctuous or cold food Excessive intake of food Sleeping immediately after meals
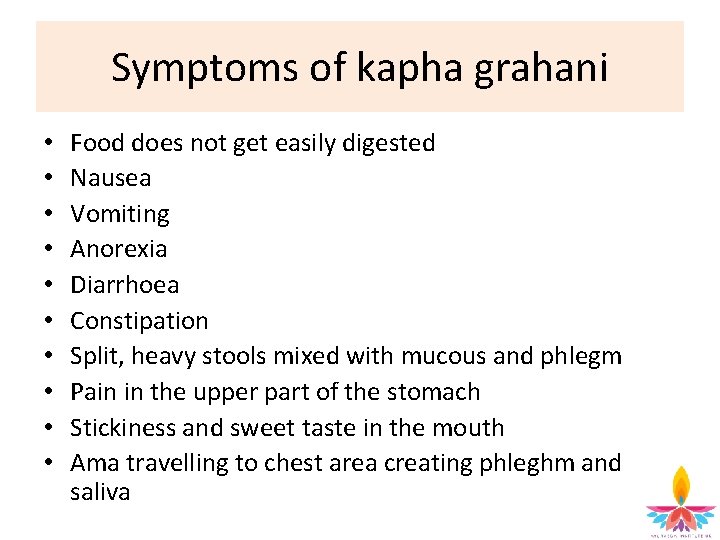
Symptoms of kapha grahani • • • Food does not get easily digested Nausea Vomiting Anorexia Diarrhoea Constipation Split, heavy stools mixed with mucous and phlegm Pain in the upper part of the stomach Stickiness and sweet taste in the mouth Ama travelling to chest area creating phleghm and saliva
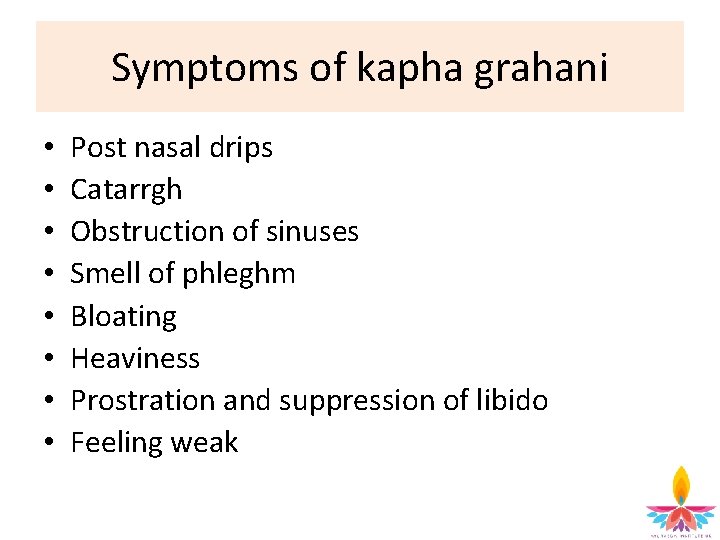
Symptoms of kapha grahani • • Post nasal drips Catarrgh Obstruction of sinuses Smell of phleghm Bloating Heaviness Prostration and suppression of libido Feeling weak
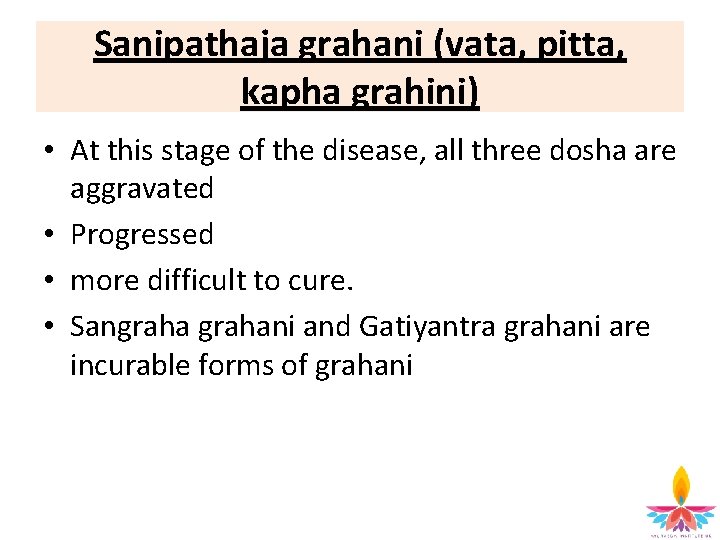
Sanipathaja grahani (vata, pitta, kapha grahini) • At this stage of the disease, all three dosha are aggravated • Progressed • more difficult to cure. • Sangrahani and Gatiyantra grahani are incurable forms of grahani

Chikitsa Grahani and Ajeerna • Guru snigdha – eliminate heavy and oily foods • Pitta balancing treatment such as virechana (purgatives) • Agni balancing treatment • Accumulated ama is attached to the bowel and colon – must be scraped from this area using agni deepana and virechana • Ama needs to be dislodged and eliminated regularly • Langana – correct eating habits according to the progress of the treatment
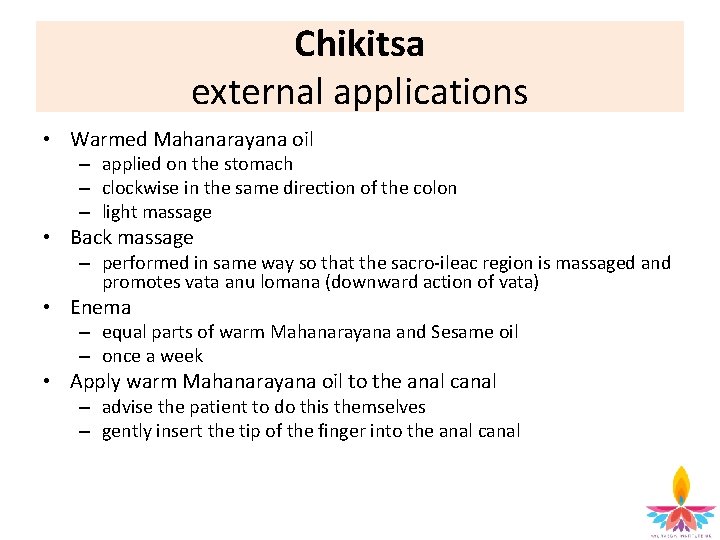
Chikitsa external applications • Warmed Mahanarayana oil – applied on the stomach – clockwise in the same direction of the colon – light massage • Back massage – performed in same way so that the sacro-ileac region is massaged and promotes vata anu lomana (downward action of vata) • Enema – equal parts of warm Mahanarayana and Sesame oil – once a week • Apply warm Mahanarayana oil to the anal canal – advise the patient to do this themselves – gently insert the tip of the finger into the anal canal

Chikitsa internal treatments • Choorna for agni deepana – amahara or – paaka choorna or – hinguashtaka • Ama pachana – Triphala or – Dhatri or – Paaka choorna • To reduce inflammation – nimbhadi choorna or – pitta hara tablets • To reduce bloating – thalisadi in ghee – grita preparation (made with ghee) eg. ghee and cumin, ghee and long pepper etc. • To rejuvenate if the patient is emaciated – ashwagandha choorna or – grita or – shatavari choorna
Chikitsa Other treatments • • Trikatu Bukthapaaka Mani mantha Abyadhi arista Pancha tikthaka grita Dhashamoola arista Chayawanaprash
Arsas (piles) 6 types of arsas: • Vata • Pitta • Kapha • Sannipatika • Raktaja • Sahaja (congenital) The last three types require surgical treatment.
Arsas Nidana Arsas can occur due to: • atisara (diarrhoea) • grahani (chronic mal-absorption disorder or indigestion) • aggravated by a pitta-increasing diet and lifestyle, stress and emotional imbalances
Vata type arsas • Vata suffers from piles more often because of constipation Nidana: • vata increasing foods such as cold, light, dry, astringent or bitter foods • strong wines (beer and wine affect the piles the most) • excessive sexual intercourse • prolonged exposure to wind and sun
Vata type arsas Samprapti • Apana vata is vitiated • Apana vata puts pressure on the first layer of the anus (samvarani) • Causes lumps or pouches, muscle tone loosens and there is rough texture to the anus (like kerala fruit) Signs and symptoms • vata arsas are very dry, no mucous, dark blackish in colour • sharp, irritating pain • twisted appearance to the external piles • anal fissures occur in the next stage of vataja type piles • stools are infrequent, dry and small

Pitta type arsas Nidana • alcohol is most common cause • sour, salty and spicy foods and drinks • strenuous exercise • hot weather • anger and jealousy • drugs Samprapti & signs and symptoms • rakta dhatu is affected • arsas are bleeding, dark red or blackish colouration • warm to the touch with mucous • Arsas emit a foul odour and are only few in number • raktaja arsas can bleed and pittaja arsas can sometimes rupture • stools they are yellow and hard
Kapha type arsas Nidana • sweet, fatty, cold, salty, sour and heavy foods • sleeping during the day • sedentary habits • living in cold climate Samprapti • Excess of kapha dosha accumulates and overflows into the rasa dhatu and then to the mamsa dhatu and affects the third layer of the anus (pravahani) Signs and symptoms • affects the third layer of the anus • big and swollen, internalised piles • piles are also oily and shiny with mucous and of a pink hue and very itchy • patient feels heavy, lethargic • pale looking • has mandagni • anaemic • cough and cold • constipation • lack of appetite because of mandagni • stools are passed with mucous
Raktaja & Sannipataja Arsas Raktaja type arsas • occurs due to the vitiated condition of the blood (rakta) • arsas appear the colour of red coral or dark red. • symptoms of pittaja type arsas • pressed hard by the faeces in their passage through the anus • suddenly give rise to a haemorrhage of vitiated venous blood and excessive bleeding tend to follow Sannipataja type arsas • In the case of haemorrhoids, due to deranged vata, pitta and kapha, symptoms characteristic of each type manifest • all three layers of the anus are affected • very painful and incurable
Sahaja arsas (congenital) • • • • • Caused by defects in the semen and ovum of the parents polypi are hardly visible rough and yellowish polypi with faces turned inward extremely painful Patient gets thinner every day eats very little large veins (siras) appear on the surface of the body patient becomes irritable semen decreases in quantity voice becomes feeble digestion is impaired vitality weak excessively lethargic and suffer with disorders affecting the head, nose, ears and eyes continuous croaking sound in the intestine rumbling in the abdomen little enthusiasm for food region of the heart seems to be smeared with a sticky kind of paste (mucous)
Arsas Chikitsa External applications • wash with luke warm water and light disinfectant such as soap • keep area clean and dry • Each time the patients voids stools or urinate, area must be washed and cleaned thoroughly and moisturiser applied • Dermaved is an extremely good external application – – – absorbs the external heat gives instant relief moisturises the area for a long time can be applied even to broken skin heals tears in skin
Internal treatments Pitta reducing • • • Arsas Chikitsa Nimbhadi choorna Chandanadi choorna Pitta hara tablet Triphala choorna Dhatri choorna • (can cause diarrhoea which makes the anus painful and inflamed) • Amahara / paaka choorna • (never prescribe hinguashtaka or trikatu) • • Soma jam Chayawanaprash Shatavari Follow pitta reducing diet for all types of arsas but consider the individual types for the diet