OXYGEN THERAPY DR RICHA JAIN University College of

























- Slides: 100
OXYGEN THERAPY DR. RICHA JAIN University College of Medical Sciences & GTB Hospital, Delhi
OVERVIEW Introduction Oxygen transport Indications Oxygen delivery systems Hyperbaric oxygen therapy Complications of oxygen therapy
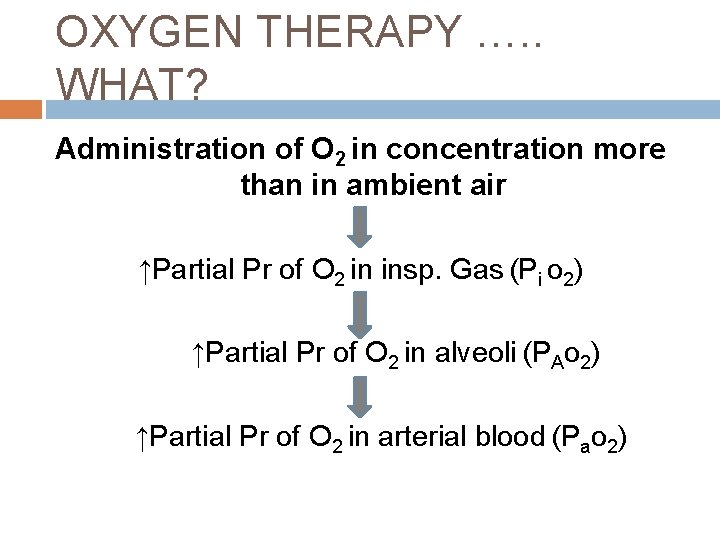
OXYGEN THERAPY …. . WHAT? Administration of O 2 in concentration more than in ambient air ↑Partial Pr of O 2 in insp. Gas (Pi o 2) ↑Partial Pr of O 2 in alveoli (PAo 2) ↑Partial Pr of O 2 in arterial blood (Pao 2)
Why is O 2 required for survival? O 2 is required for the aerobic metabolism Oxidative phosphorylation in mitochondria Glucose + 6 O 2 → 6 H 2 O + 6 CO 2 + 36 ATP Lack of O 2 causes Anaerobic metabolism in cytoplasm Glucose → lactic acid + 2 ATP ↓ H+ + lactate-
“lack of O 2 not only stops the machinery, but also totally ruins the supposed machinery” J. S. Halda ne
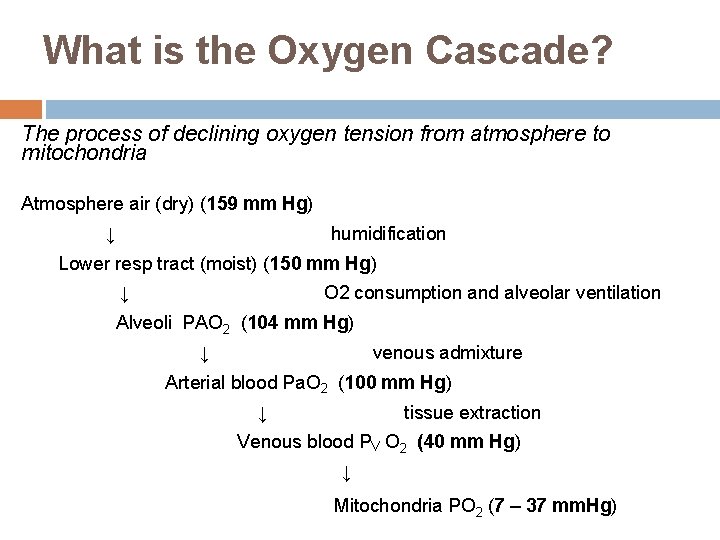
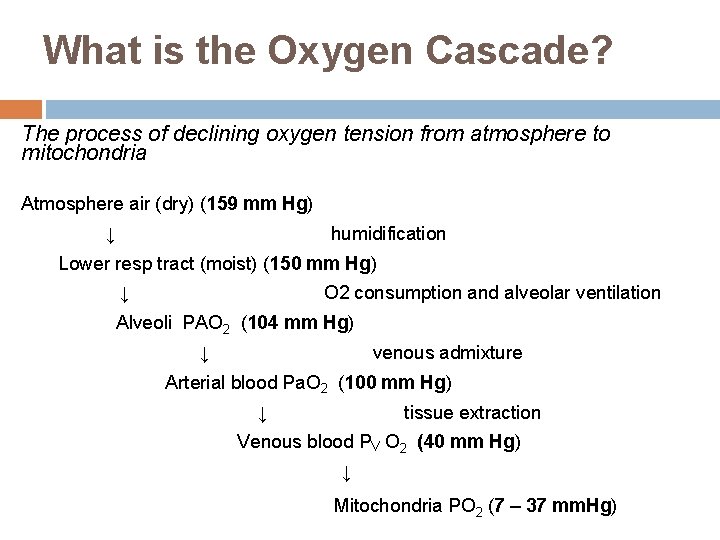
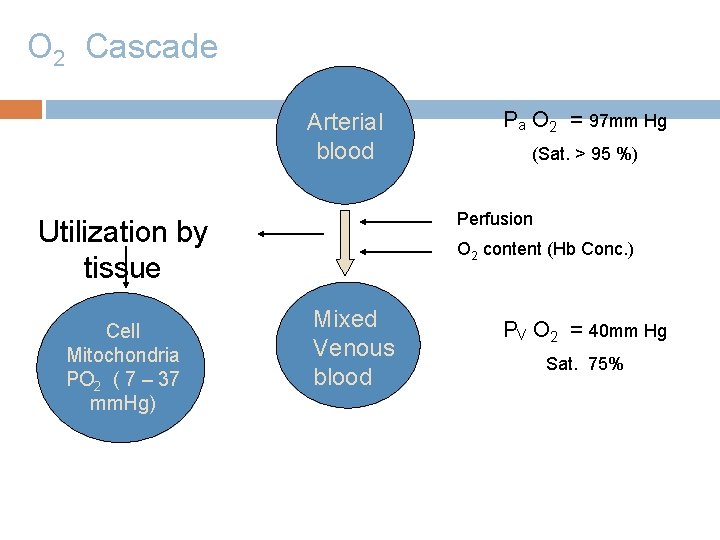
What is the Oxygen Cascade? The process of declining oxygen tension from atmosphere to mitochondria Atmosphere air (dry) (159 mm Hg) ↓ humidification Lower resp tract (moist) (150 mm Hg) ↓ O 2 consumption and alveolar ventilation Alveoli PAO 2 (104 mm Hg) ↓ venous admixture Arterial blood Pa. O 2 (100 mm Hg) ↓ tissue extraction Venous blood PV O 2 (40 mm Hg) ↓ Mitochondria PO 2 (7 – 37 mm. Hg)

O 2 Cascade Alveolar air PA O 2 = 104 mm Hg PI O 2 Venous admixture PV O 2 Arterial blood Pa O 2 = 100 mm Hg A – a = 4 – 25 mm. Hg
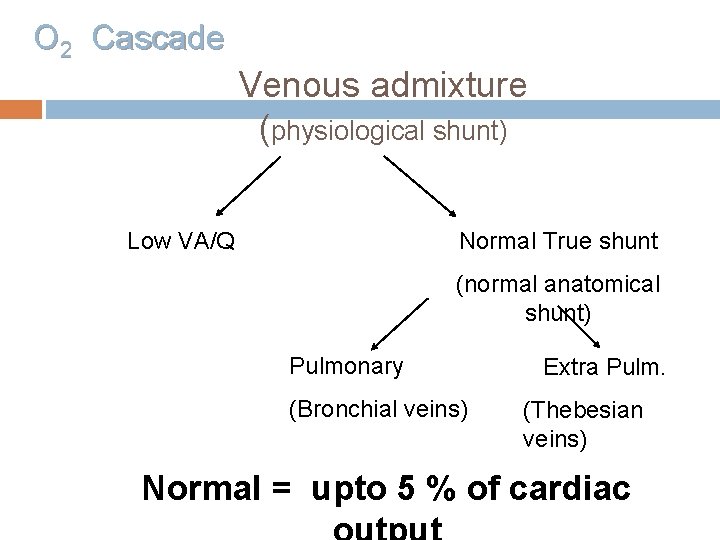
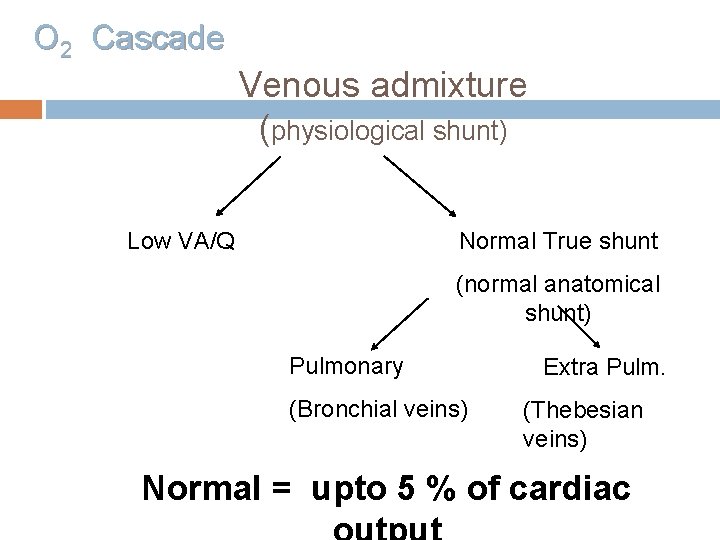
O 2 Cascade Venous admixture (physiological shunt) Low VA/Q Normal True shunt (normal anatomical shunt) Pulmonary (Bronchial veins) Extra Pulm. (Thebesian veins) Normal = upto 5 % of cardiac
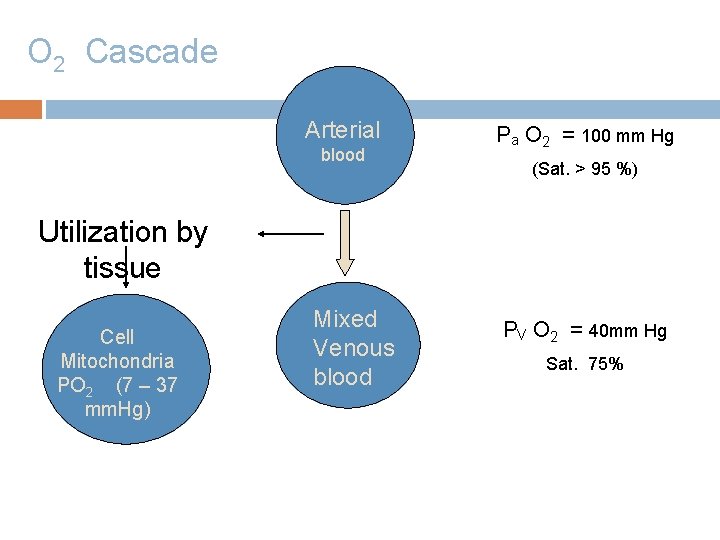
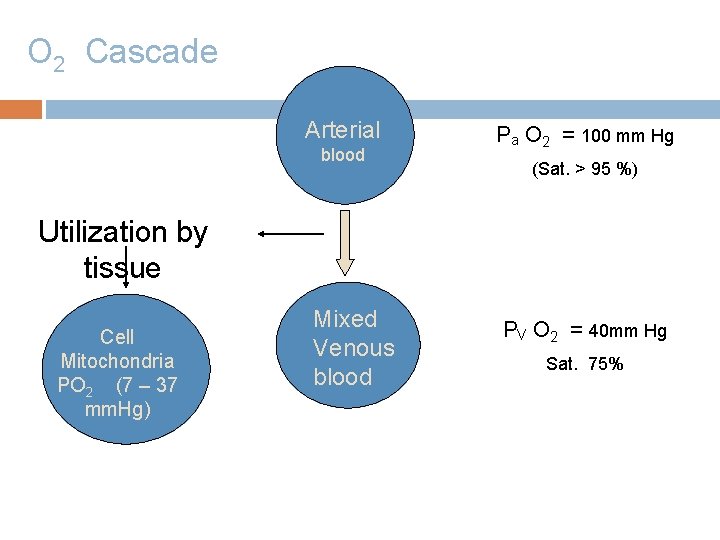
O 2 Cascade Arterial blood Pa O 2 = 100 mm Hg (Sat. > 95 %) Utilization by tissue Cell Mitochondria PO 2 (7 – 37 mm. Hg) Mixed Venous blood PV O 2 = 40 mm Hg Sat. 75%
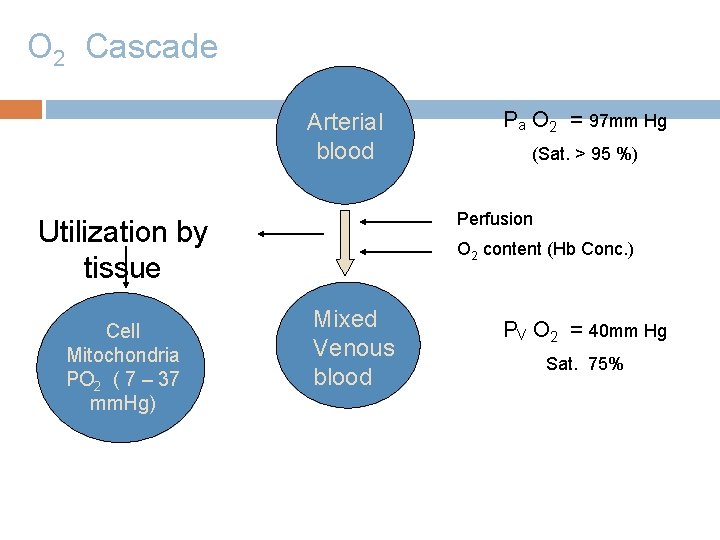
O 2 Cascade Arterial blood (Sat. > 95 %) Perfusion Utilization by tissue Cell Mitochondria PO 2 ( 7 – 37 mm. Hg) Pa O 2 = 97 mm Hg O 2 content (Hb Conc. ) Mixed Venous blood PV O 2 = 40 mm Hg Sat. 75%

What is Pasteur point ? The critical level of PO 2 below which aerobic metabolism fails. (1 – 2 mm. Hg PO 2 in mitochondria)
O 2 TRANSPORT Oxygen content Oxygen flux Oxygen uptake O 2 extraction ratio

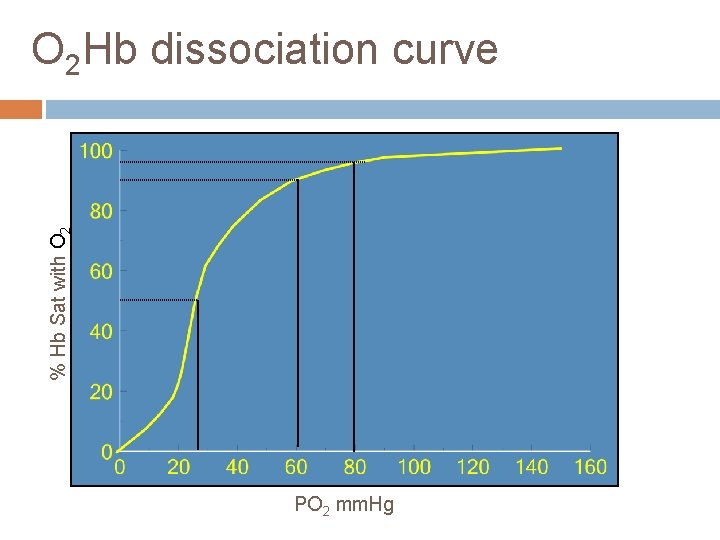
Oxygen Content (Co 2) Amount of O 2 carried by 100 ml of blood Co 2 =Dissolved O 2 + O 2 Bound to hemoglobin Co 2 = Po 2 × 0. 0031 + So 2 × Hb × 1. 34 (Normal Cao 2 = 20 ml/100 ml blood Normal Cvo 2 = 15 ml/100 ml blood) C(a-v)o 2 = 5 ml/100 ml blood Co 2 = arterial oxygen content (vol%) Hb = hemoglobin (g%) 1. 34 = oxygen-carrying capacity of hemoglobin Po 2 = arterial partial pressure of oxygen (mm. Hg) 0. 0031 = solubility coefficient of oxygen in plasma
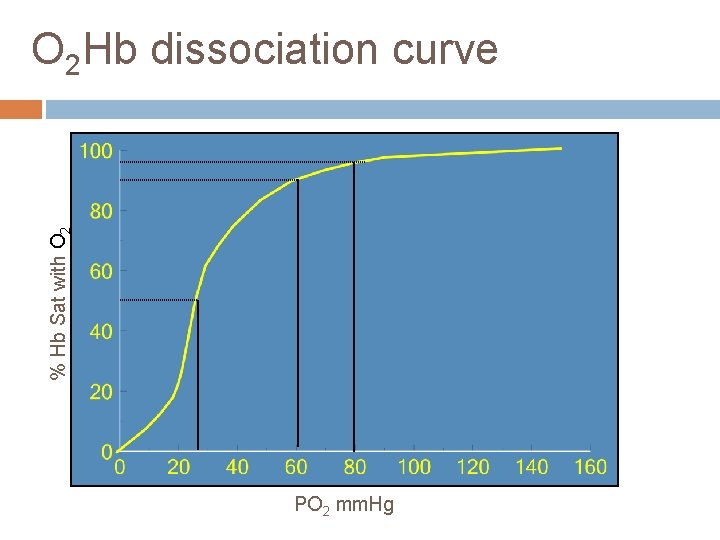
% Hb Sat with O 2 Hb dissociation curve PO 2 mm. Hg
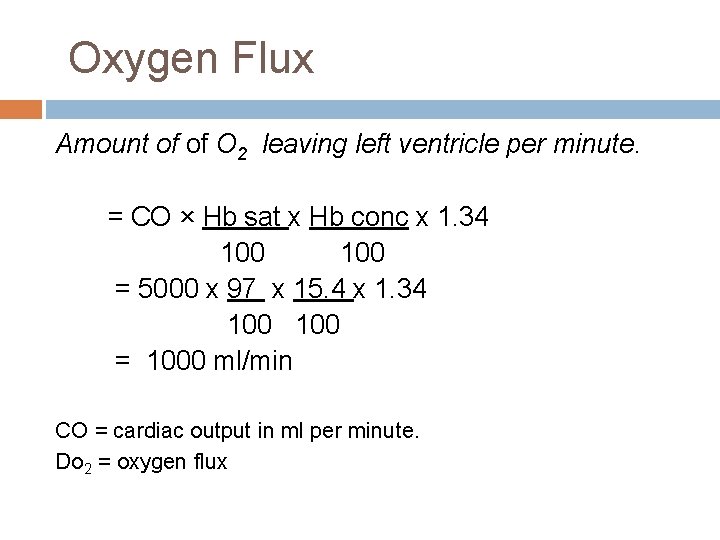
Oxygen Flux Amount of of O 2 leaving left ventricle per minute. = CO × Hb sat x Hb conc x 1. 34 100 = 5000 x 97 x 15. 4 x 1. 34 100 = 1000 ml/min CO = cardiac output in ml per minute. Do 2 = oxygen flux
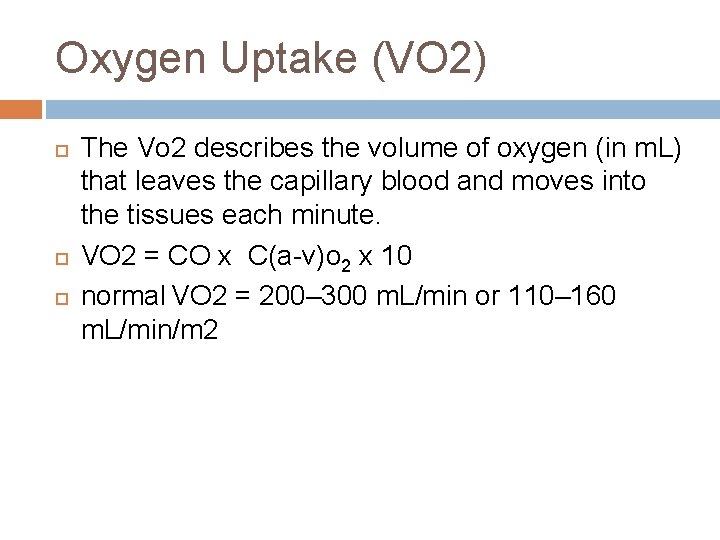
Oxygen Uptake (VO 2) The Vo 2 describes the volume of oxygen (in m. L) that leaves the capillary blood and moves into the tissues each minute. VO 2 = CO x C(a-v)o 2 x 10 normal VO 2 = 200– 300 m. L/min or 110– 160 m. L/min/m 2

Oxygen-Extraction Ratio (O 2 ER) The fraction of the oxygen delivered to the capillaries and then to tissues. An index of the efficiency of oxygen transport. O 2 ER = VO 2 / DO 2 = CO x C(a-v)o 2 x 10 CO x Cao 2 x 10 = Sa. O 2 - Sv. O 2 / Sa. O 2 Normal - 0. 25 (range = 0. 2– 0. 3)
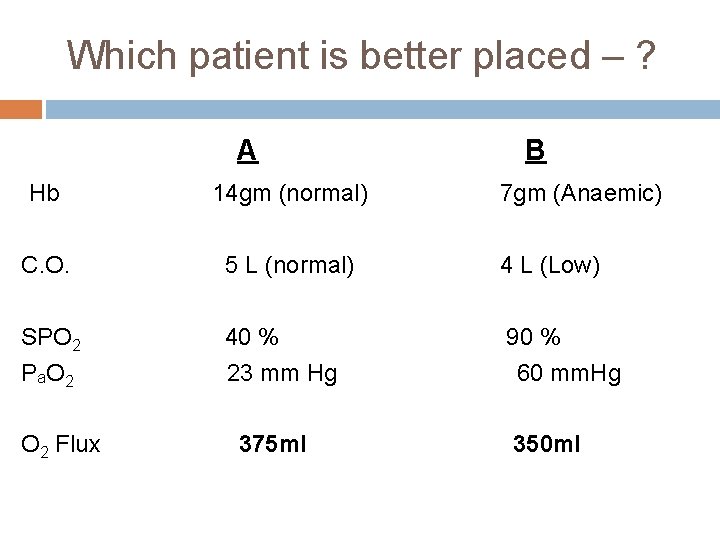
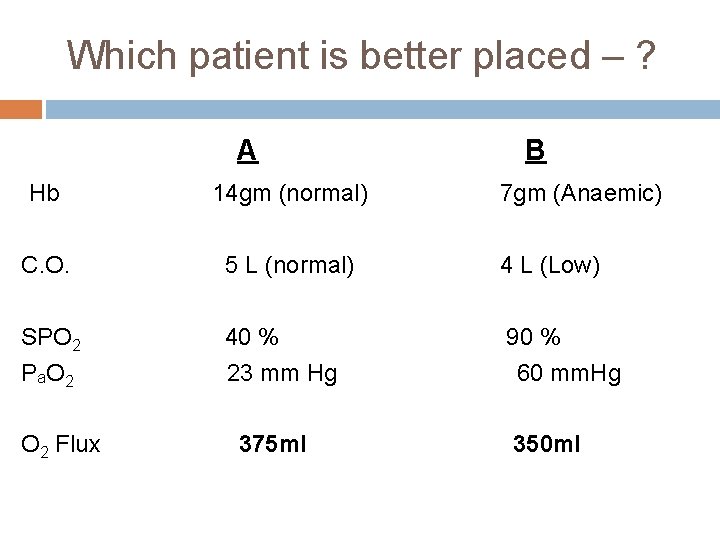
Which patient is better placed – ? A B Hb 14 gm (normal) C. O. 5 L (normal) 4 L (Low) SPO 2 P a. O 2 40 % 23 mm Hg 90 % 60 mm. Hg O 2 Flux 375 ml 7 gm (Anaemic) 350 ml

PO 2 97 mm 40 mm 15 ml O 2 content Per 100 ml Art. blood 14 g x 1. 39 x 100%=20 ml Ven. blood 14 g x 1. 39 x 75% = 97 mm 27 mm Art. blood 7 g x 1. 39 x 100% = 10 ml Ven. Blood 7 g x 1. 39 x 50% = 5 ml Tissue extraction 25% = 5 ml
Goal of oxygen therapy To maintain adequate tissue oxygenation while minimizing cardiopulmonary work
O 2 Therapy : CLINICAL OBJECTIVES 1. 2. 3. Correct documented or suspected hypoxemia Decrease the symptoms associated with chronic hypoxemia Decrease the workload hypoxemia imposes on the cardiopulmonary system

O 2 Therapy : Indications Documented hypoxemia as evidenced by Pa. O 2 < 60 mm. Hg or Sa. O 2 < 90% on room air Pa. O 2 or Sa. O 2 below desirable range for a specific clinical situation Acute care situations in which hypoxemia is suspected Severe trauma Acute myocardial infarction Short term therapy (Post anaesthesia recovery) Respir Care 2002; 47: 707 -720
ASSESSMENT The need for oxygen therapy should be assessed by 1. monitoring of ABG - Pa. O 2, Sp. O 2 2. clinical assessment findings.

Pa. O 2 as an indicator for Oxygen therapy Pa. O 2 : 80 – 100 mm Hg : Normal 60 – 80 mm Hg : cold, clammy extremities < 60 mm Hg : cyanosis < 40 mm Hg : mental deficiency memory loss < 30 mm Hg : bradycardiac arrest Pa. O 2 < 60 mm Hg is a strong indicator for oxygen therapy
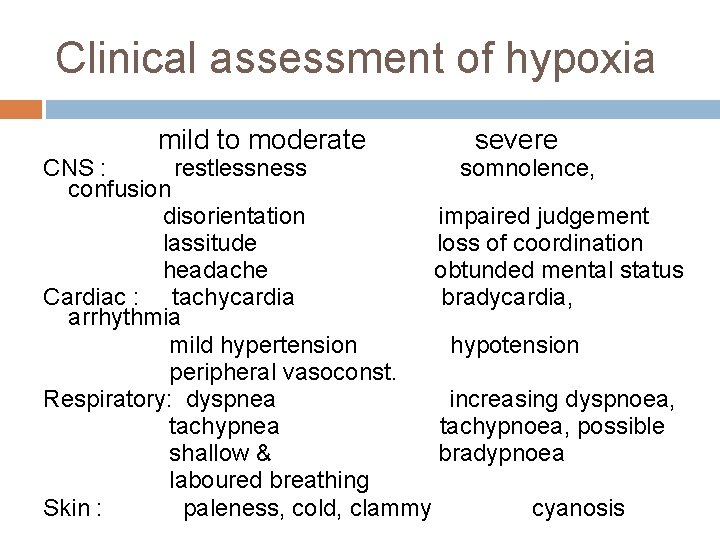
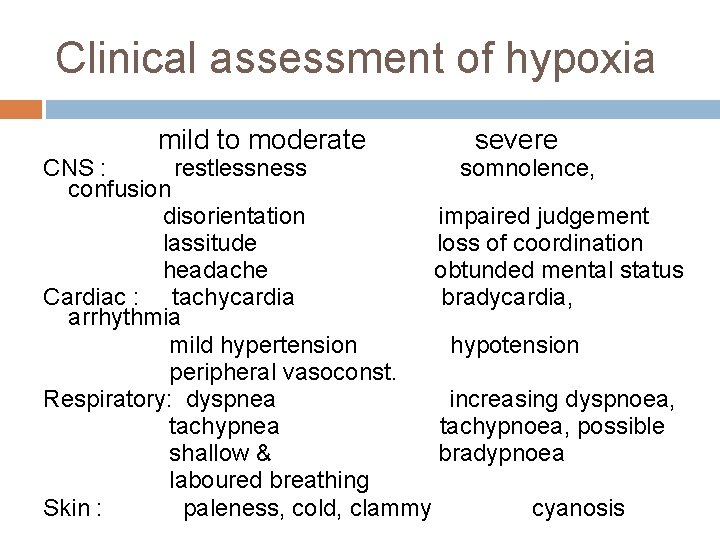
Clinical assessment of hypoxia mild to moderate severe CNS : restlessness somnolence, confusion disorientation impaired judgement lassitude loss of coordination headache obtunded mental status Cardiac : tachycardia bradycardia, arrhythmia mild hypertension hypotension peripheral vasoconst. Respiratory: dyspnea increasing dyspnoea, tachypnea tachypnoea, possible shallow & bradypnoea laboured breathing Skin : paleness, cold, clammy cyanosis
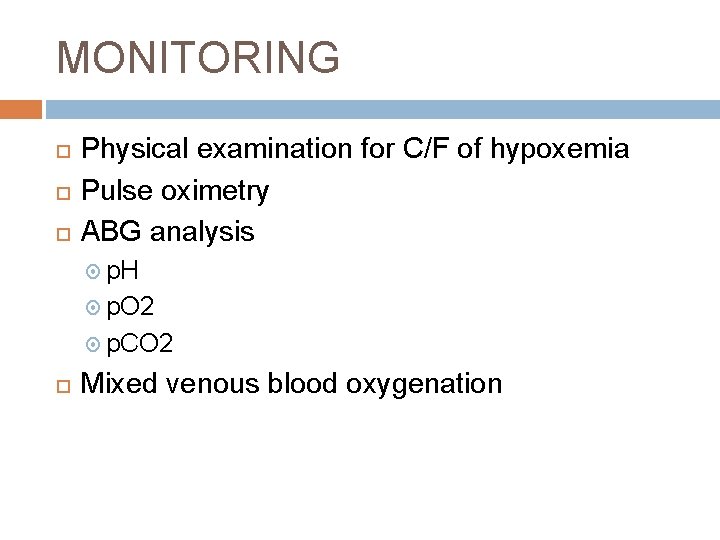
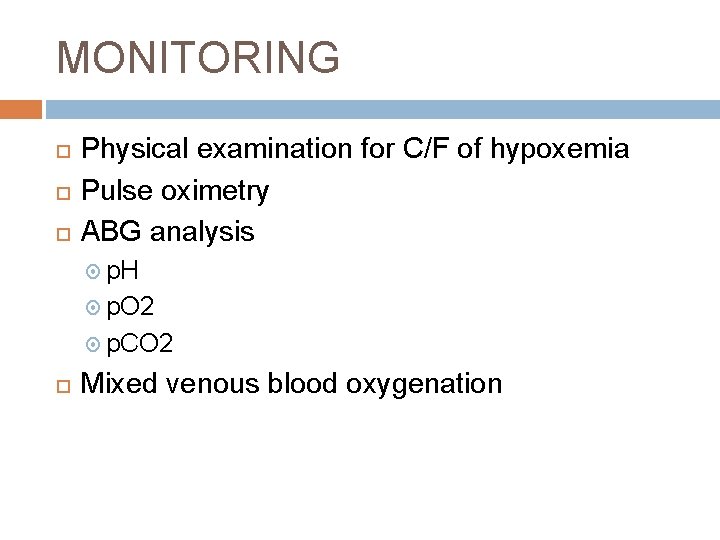
MONITORING Physical examination for C/F of hypoxemia Pulse oximetry ABG analysis p. H p. O 2 p. CO 2 Mixed venous blood oxygenation
O 2 Delivery systems
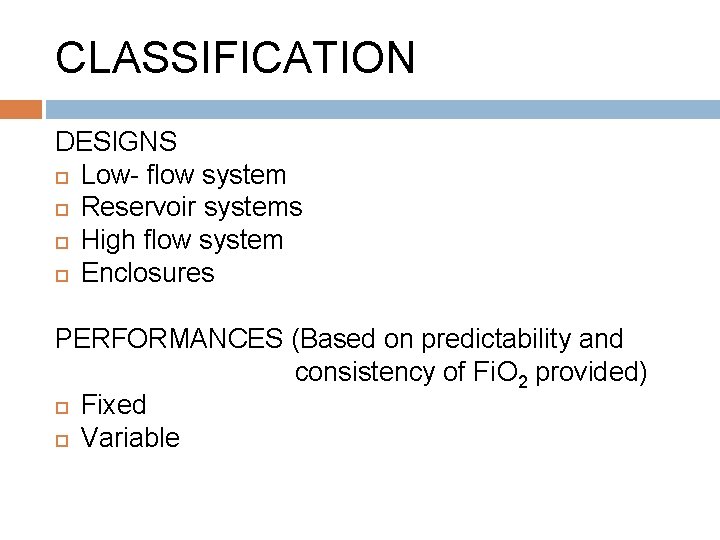
CLASSIFICATION DESIGNS Low- flow system Reservoir systems High flow system Enclosures PERFORMANCES (Based on predictability and consistency of Fi. O 2 provided) Fixed Variable
Low flow system q The gas flow is insufficient to meet patient’s peak inspiratory and minute ventilatory requirement O 2 provided is always diluted with air Fi. O 2 varies with the patient’s ventilatory pattern Deliver low and variable Fi. O 2 → Variable performance device
High flow system • The gas flow is sufficient to meet patient’s peak inspiratory and minute ventilatory requirement. • Fi. O 2 is independent of the patient’s ventilatory pattern Deliver low- moderate and fixed Fi. O 2 → Fixed performance device •
Reservoir System Reservoir system stores a reserve volume of O 2, that equals or exceeds the patient’s tidal volume Delivers mod- high Fi. O 2 Variable performance device To provide a fixed Fi. O 2, the reservoir volume must exceed the patient’s tidal volume
How to judge the performance of an oxygen delivery system? How much oxygen (Fi. O 2) the system delivers? Does the Fi. O 2 remain fixed or varies under changing patient’s condition?
Low flow systems are Variable performance High flow system are Fixed performance Reservoir systems are Variable performance device

O 2 Delivery devices o Low flow (Variable performance devices ) Nasal cannula Nasal catheter Transtracheal catheter o Reservoir system (Variable performance device) Reservoir cannula Simple face mask Partial rebreathing mask Non rebreathing mask Tracheostomy mask o High flow (Fixed performance devices) Ventimask (HAFOE) Aerosol mask and T-piece with nebulisers
Low-Flow Devices

Nasal Cannula A plastic disposable device consisting of two tips or prongs 1 cm long, connected to oxygen tubing Inserted into the vestibule of the nose Fi. O 2 – 24 -40% Flow – ¼ - 8 L/min (adult) < 2 L/min(child)
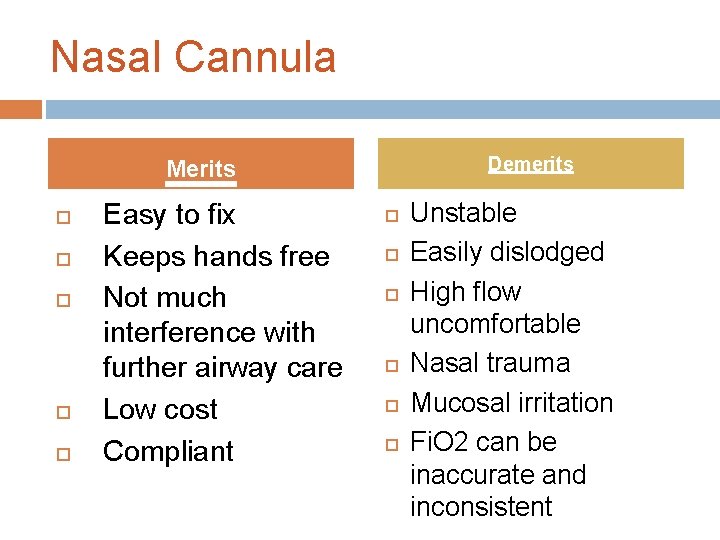
Nasal Cannula Demerits Merits Easy to fix Keeps hands free Not much interference with further airway care Low cost Compliant Unstable Easily dislodged High flow uncomfortable Nasal trauma Mucosal irritation Fi. O 2 can be inaccurate and inconsistent
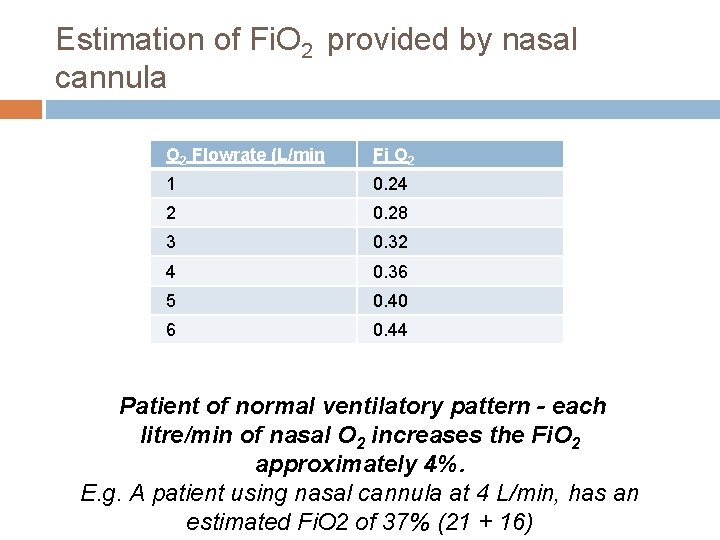
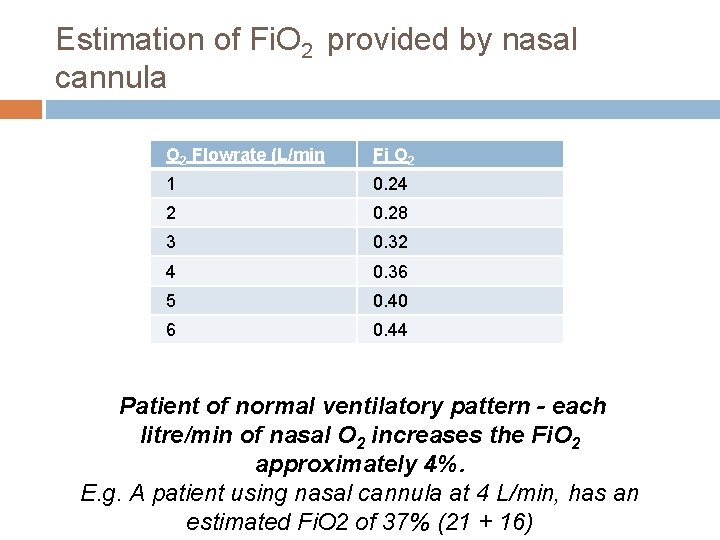
Estimation of Fi. O 2 provided by nasal cannula O 2 Flowrate (L/min Fi O 2 1 0. 24 2 0. 28 3 0. 32 4 0. 36 5 0. 40 6 0. 44 Patient of normal ventilatory pattern - each litre/min of nasal O 2 increases the Fi. O 2 approximately 4%. E. g. A patient using nasal cannula at 4 L/min, has an estimated Fi. O 2 of 37% (21 + 16)
Nasal catheter

Nasal catheter Demerits Merits Good stability Disposable Low cost Difficult to insert High flow increases back pressure Needs regular changing May provoke gagging, air swallowing, aspiration Nasal polyps, deviated septum may block insertion
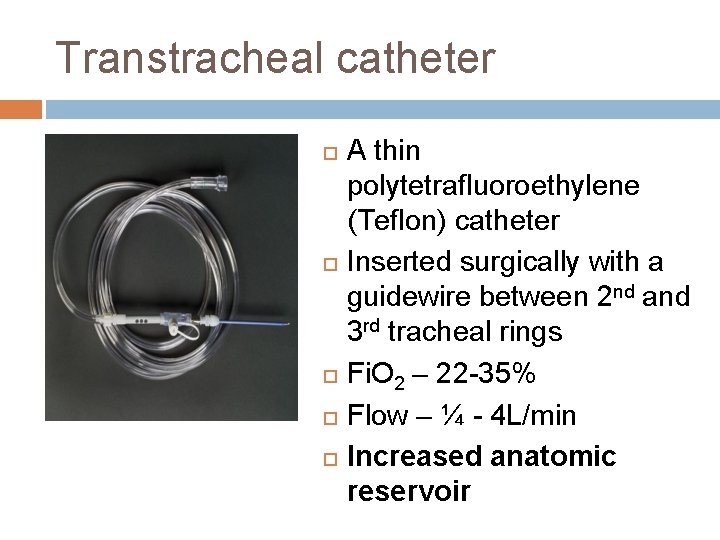
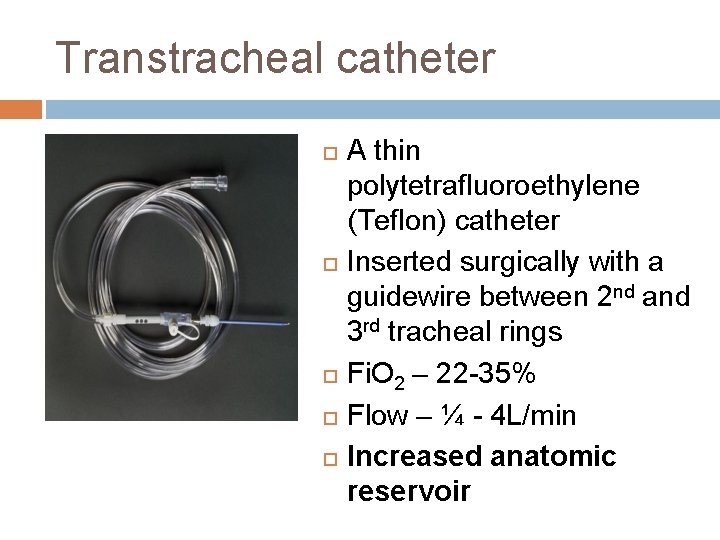
Transtracheal catheter A thin polytetrafluoroethylene (Teflon) catheter Inserted surgically with a guidewire between 2 nd and 3 rd tracheal rings Fi. O 2 – 22 -35% Flow – ¼ - 4 L/min Increased anatomic reservoir

Transtracheal catheter Merits Lower O 2 use and cost Eliminates nasal and skin irritation Better compliance Increased exercise tolerance Increased mobility Demerits High cost Surgical complications Infection Mucus plugging Lost tract
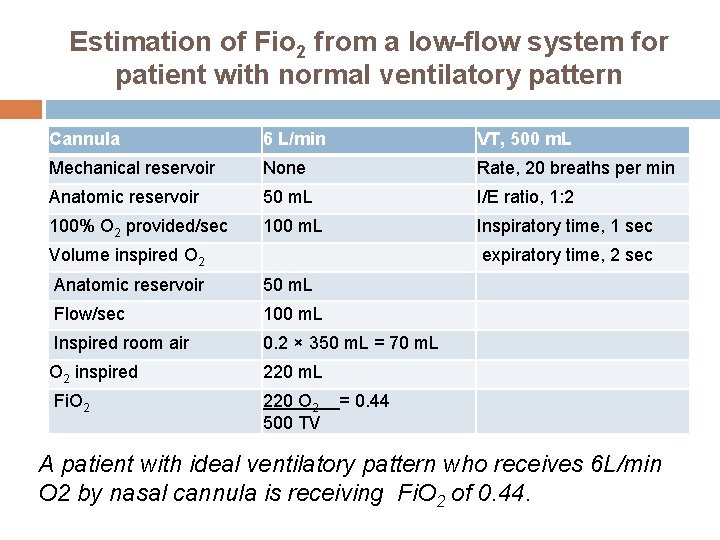
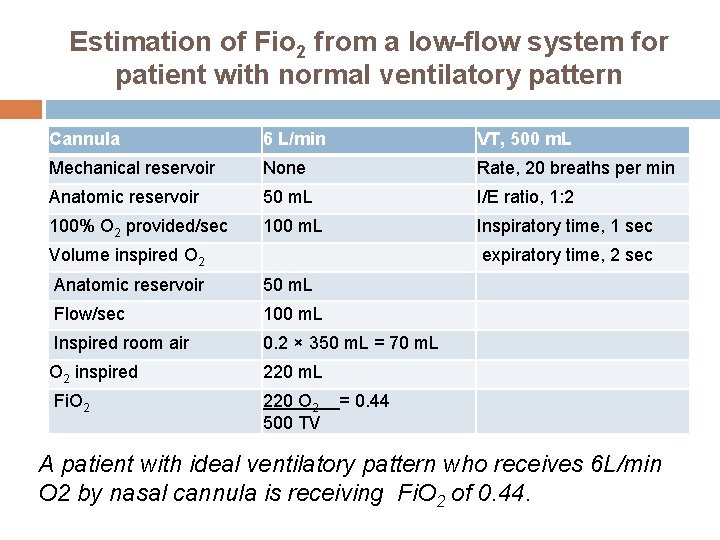
Estimation of Fio 2 from a low-flow system for patient with normal ventilatory pattern Cannula 6 L/min VT, 500 m. L Mechanical reservoir None Rate, 20 breaths per min Anatomic reservoir 50 m. L I/E ratio, 1: 2 100% O 2 provided/sec 100 m. L Inspiratory time, 1 sec Volume inspired O 2 expiratory time, 2 sec Anatomic reservoir 50 m. L Flow/sec 100 m. L Inspired room air 0. 2 × 350 m. L = 70 m. L O 2 inspired 220 m. L Fi. O 2 220 O 2 = 0. 44 500 TV A patient with ideal ventilatory pattern who receives 6 L/min O 2 by nasal cannula is receiving Fi. O 2 of 0. 44.
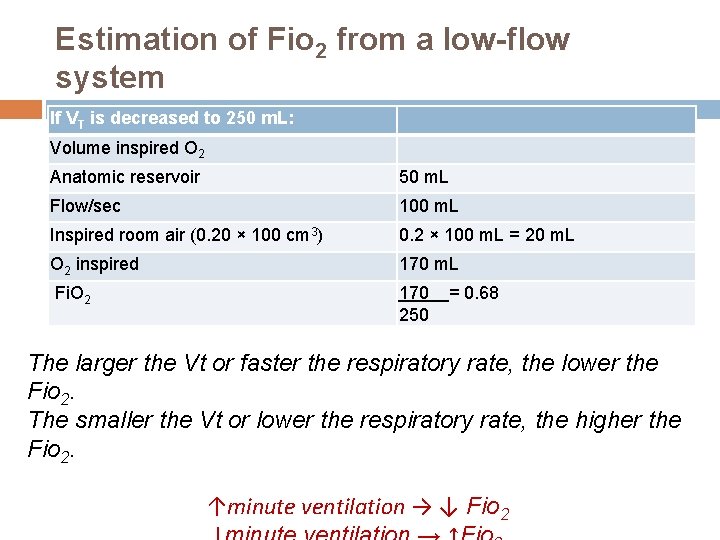
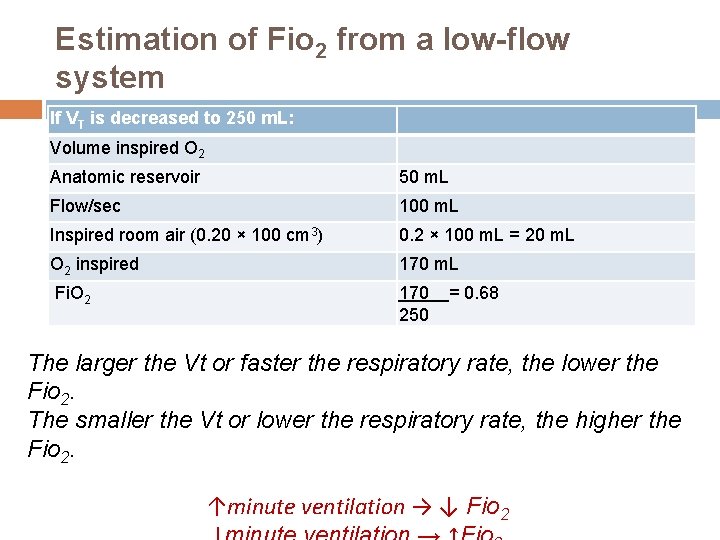
Estimation of Fio 2 from a low-flow system If VT is decreased to 250 m. L: Volume inspired O 2 Anatomic reservoir 50 m. L Flow/sec 100 m. L Inspired room air (0. 20 × 100 cm 3) 0. 2 × 100 m. L = 20 m. L O 2 inspired 170 m. L Fi. O 2 170 250 = 0. 68 The larger the Vt or faster the respiratory rate, the lower the Fio 2. The smaller the Vt or lower the respiratory rate, the higher the Fio 2. ↑minute ventilation → ↓ Fio 2
Reservoir systems

Reservoir cannula NASAL RESERVOIR PENDANT RESERVOIR
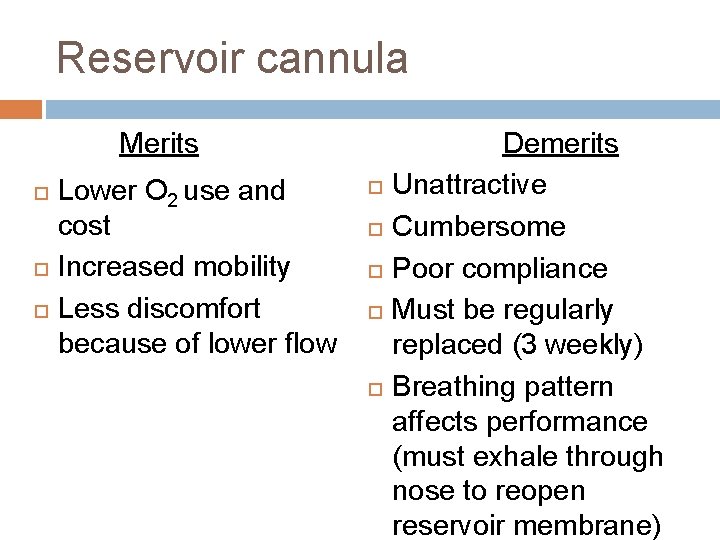
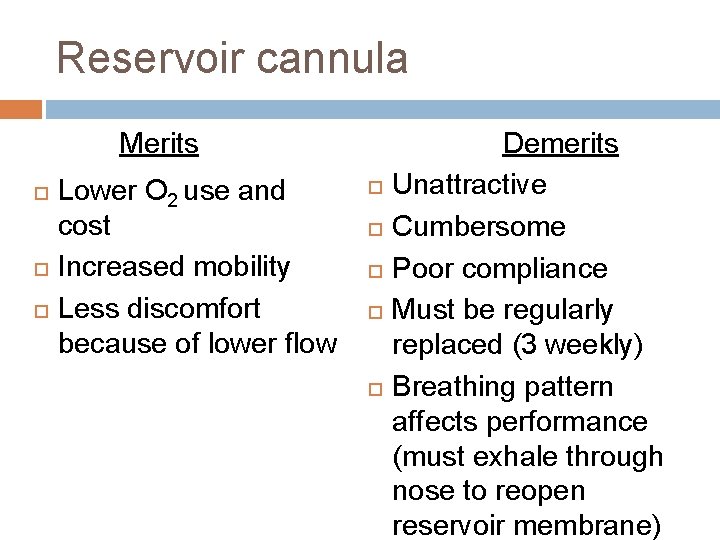
Reservoir cannula Merits Lower O 2 use and cost Increased mobility Less discomfort because of lower flow Demerits Unattractive Cumbersome Poor compliance Must be regularly replaced (3 weekly) Breathing pattern affects performance (must exhale through nose to reopen reservoir membrane)

RESERVOIR MASKS 1. 2. 3. Commonly used reservoir system Three types Simple face mask Partial rebreathing masks Non rebreathing masks
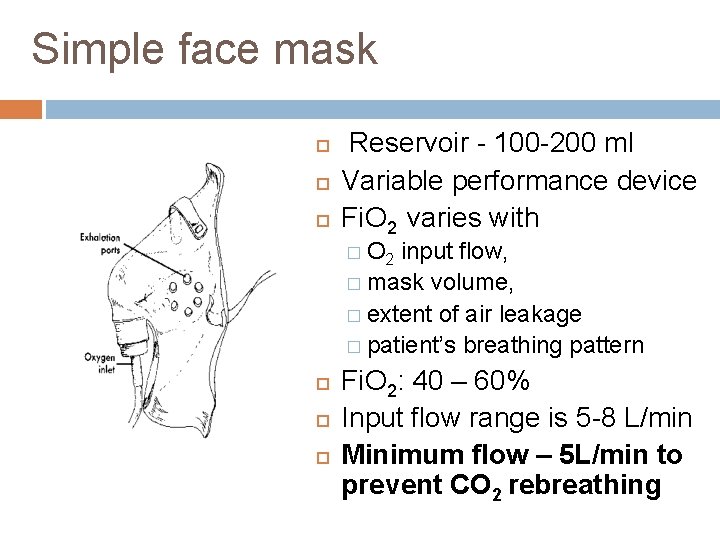
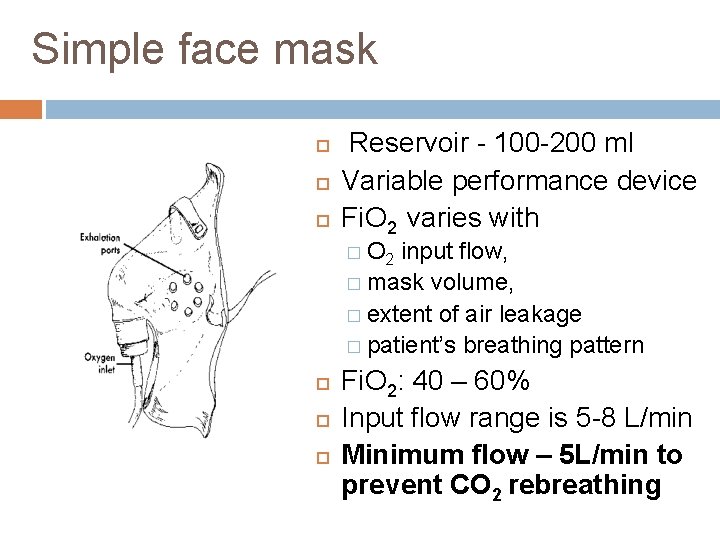
Simple face mask Reservoir - 100 -200 ml Variable performance device Fi. O 2 varies with � O 2 input flow, � mask volume, � extent of air leakage � patient’s breathing pattern Fi. O 2: 40 – 60% Input flow range is 5 -8 L/min Minimum flow – 5 L/min to prevent CO 2 rebreathing
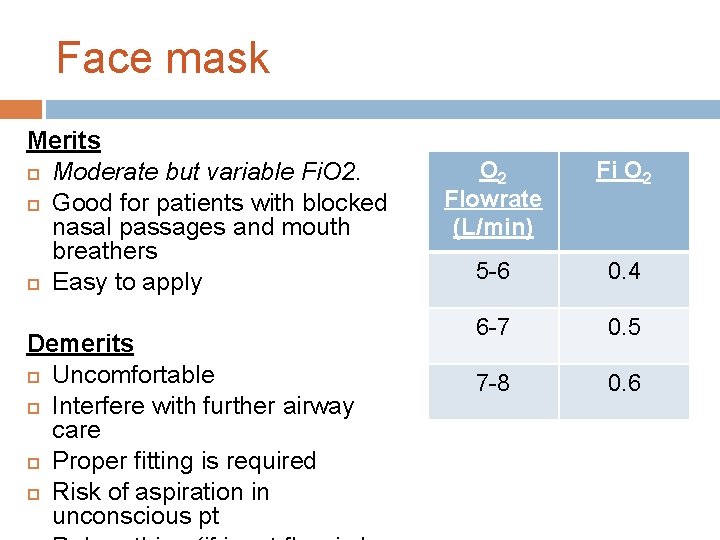
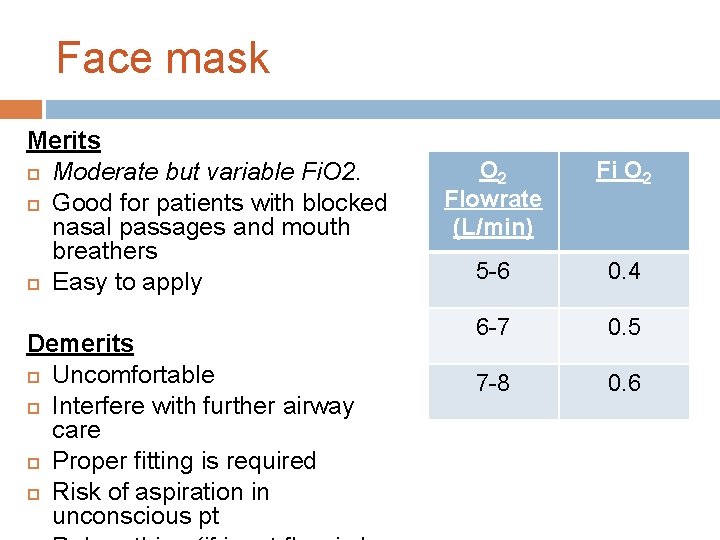
Face mask Merits Moderate but variable Fi. O 2. Good for patients with blocked nasal passages and mouth breathers Easy to apply Demerits Uncomfortable Interfere with further airway care Proper fitting is required Risk of aspiration in unconscious pt O 2 Flowrate (L/min) Fi O 2 5 -6 0. 4 6 -7 0. 5 7 -8 0. 6

Reservoir masks Partial rebreathing mask Nonrebreathing mask
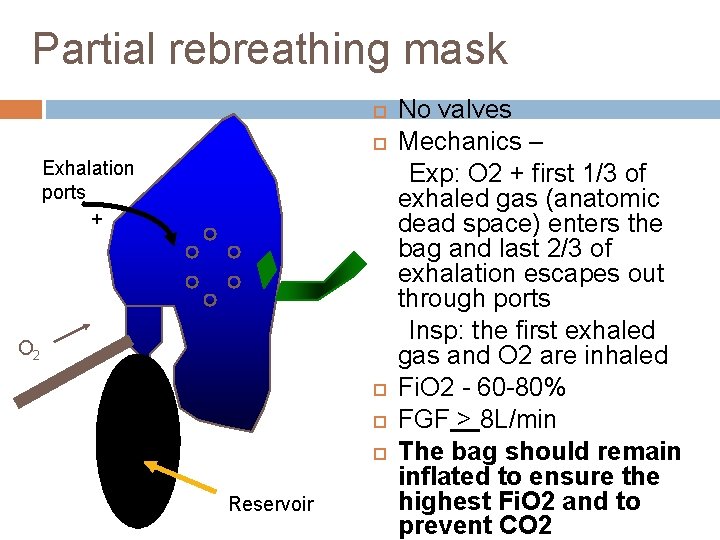
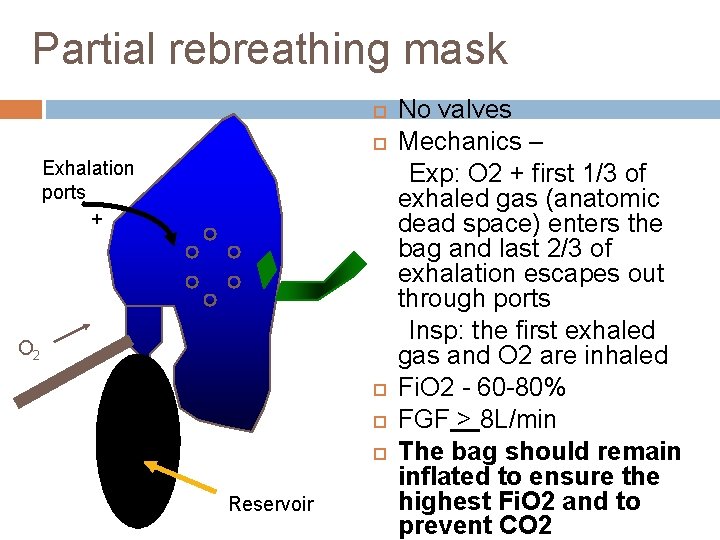
Partial rebreathing mask Exhalation ports + O 2 Reservoir No valves Mechanics – Exp: O 2 + first 1/3 of exhaled gas (anatomic dead space) enters the bag and last 2/3 of exhalation escapes out through ports Insp: the first exhaled gas and O 2 are inhaled Fi. O 2 - 60 -80% FGF > 8 L/min The bag should remain inflated to ensure the highest Fi. O 2 and to prevent CO 2

Non-rebreathing mask One-way valves O 2 Reservoir ü ü Has 3 unidirectional valves Expiratory valves prevents air entrainment Inspiratory valve prevents exhaled gas flow into reservoir bag Fi. O 2 - 0. 80 – 0. 90 FGF – 10 – 15 L/min To deliver ~100% O 2, bag should remain inflated Factors affecting Fi. O 2 air leakage and pt’s breathing pattern

Tracheostomy Mask Used primarily to deliver humidity to patients with artificial airways. Variable performance device
High-Flow systems Air entrainment devices Blending systems
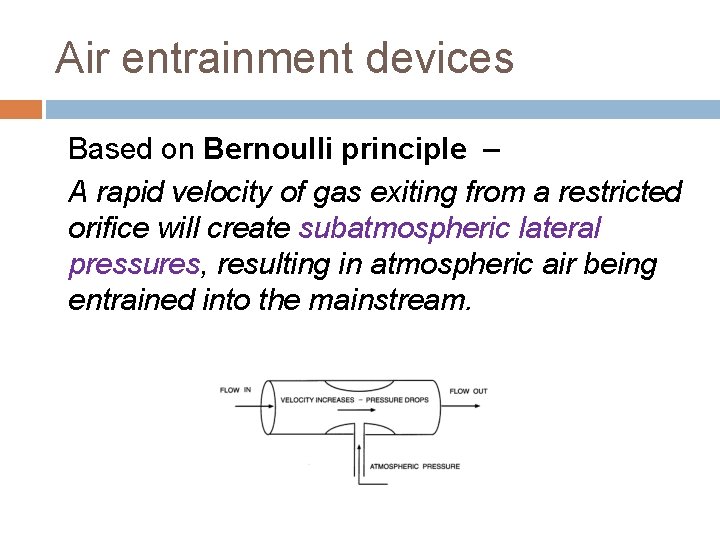
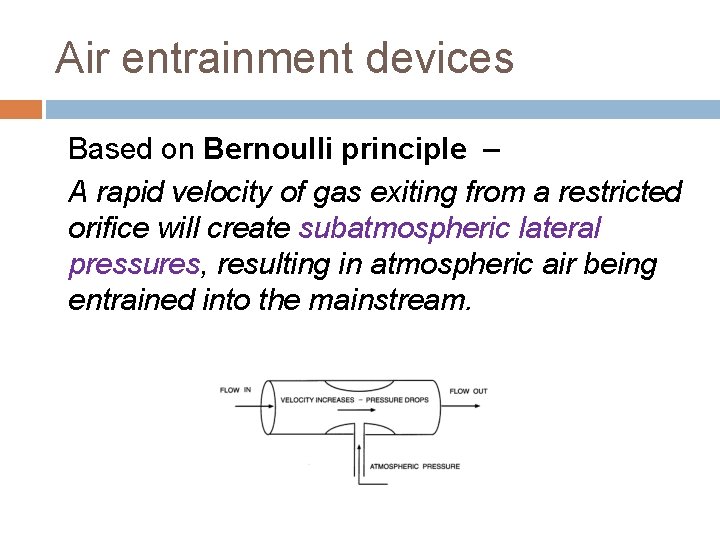
Air entrainment devices Based on Bernoulli principle – A rapid velocity of gas exiting from a restricted orifice will create subatmospheric lateral pressures, resulting in atmospheric air being entrained into the mainstream.
Principle of Air entrainment devices Principle of constant-pressure jet mixing – a rapid velocity of gas through a restricted orifice creates “viscous shearing forces” that entrain air into the mainstream. (Egan’s fundamentals of respiratory care; Shapiro’s Clinical application of blood gases)
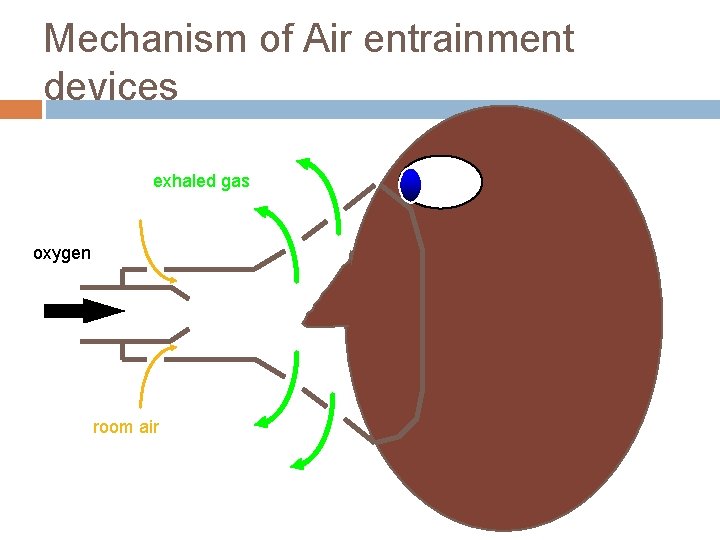
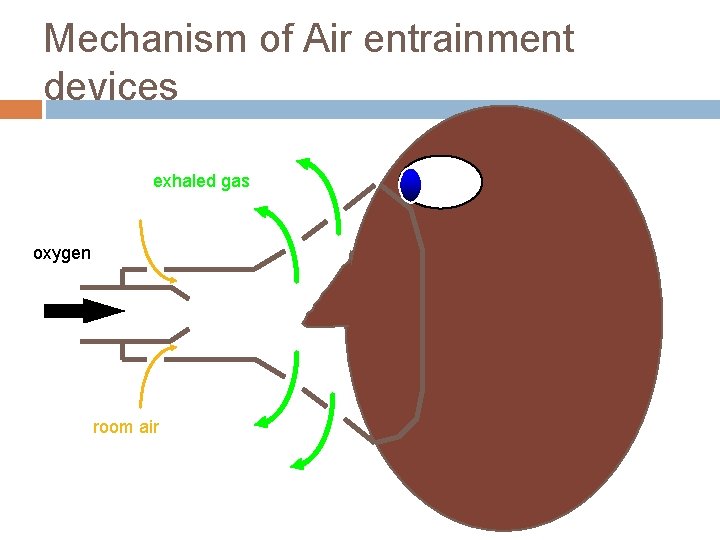
Mechanism of Air entrainment devices exhaled gas oxygen room air

Characteristics of Air entrainment devices Amount of air entrained varies directly with size of the port and the velocity of O 2 at jet They dilute O 2 source with air - Fi. O 2 < 100% The more air they entrain, the higher is the total output flow but the lower is the delivered Fi. O 2

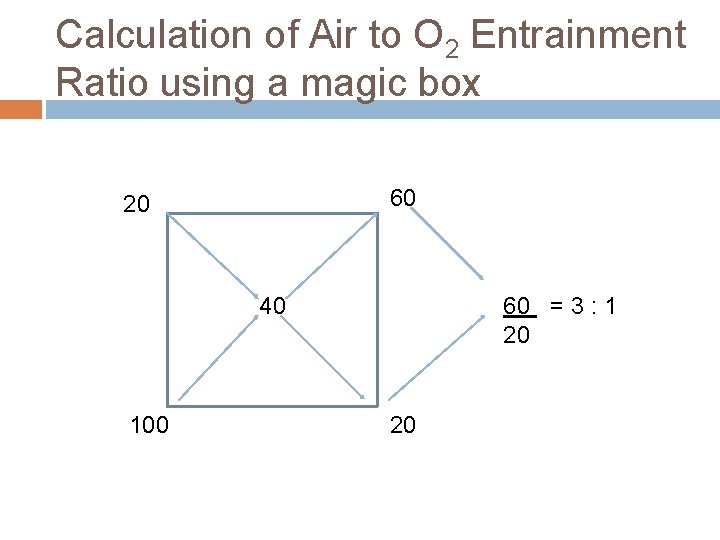
Principles of gas mixing All High flow systems mix air and O 2 to achieve a given Fi. O 2 An air entrainment device or blending system is used V F C F = V 1 C 1 + V 2 C 2 V 1 and V 2 - volumes of 2 gases mixed C 1 and C 2 - oxygen conc in these 2 volumes VF - the final volume CF - conc of resulting mixture % O 2 = ( air flow x 21) + (O 2 flow x 100) total flow Air-to O 2 entrainment ratio: Air = 100 - %O 2
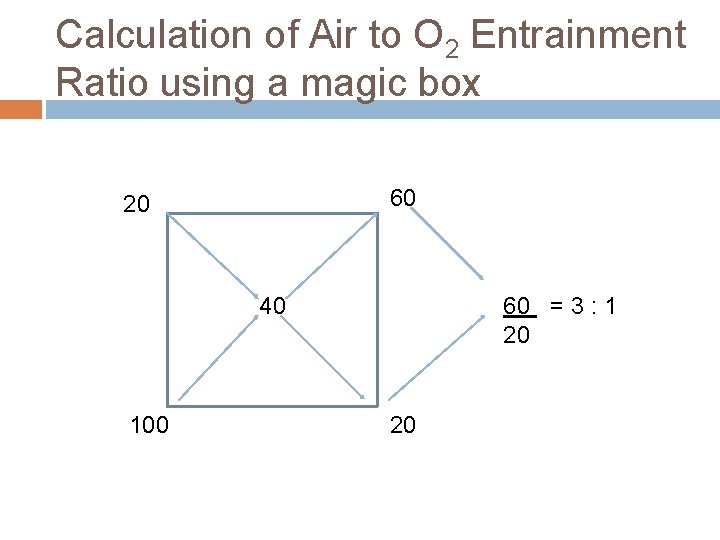
Calculation of Air to O 2 Entrainment Ratio using a magic box 60 20 40 100 60 = 3 : 1 20 20
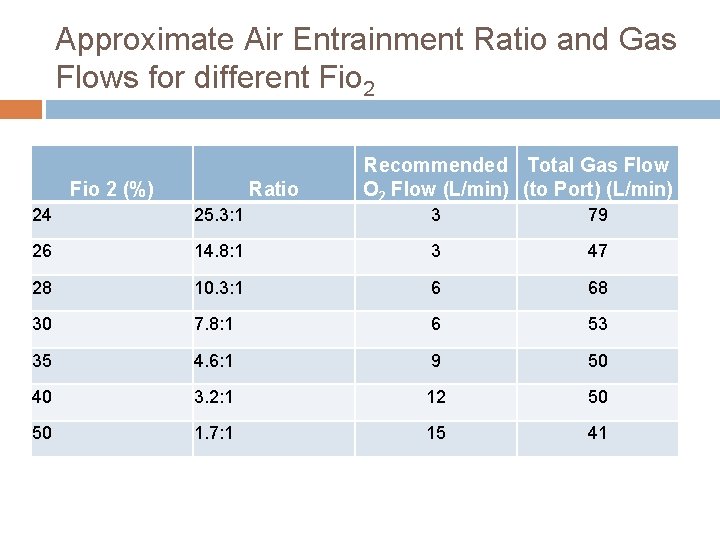
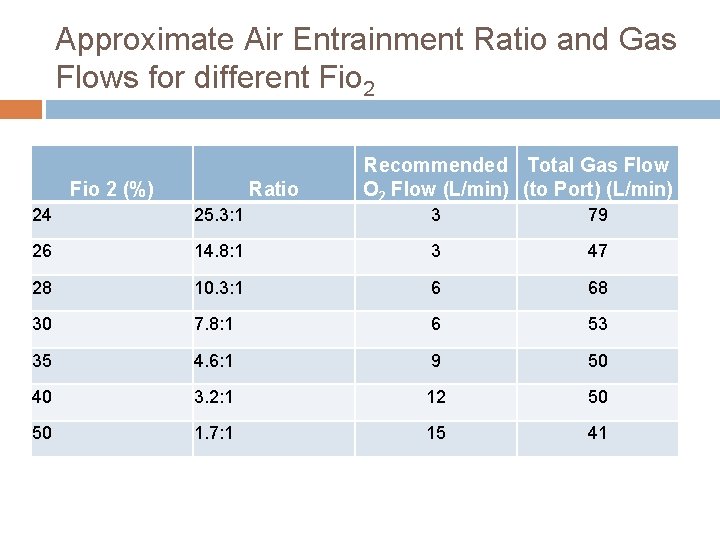
Approximate Air Entrainment Ratio and Gas Flows for different Fio 2 (%) Ratio Recommended Total Gas Flow O 2 Flow (L/min) (to Port) (L/min) 24 25. 3: 1 3 79 26 14. 8: 1 3 47 28 10. 3: 1 6 68 30 7. 8: 1 6 53 35 4. 6: 1 9 50 40 3. 2: 1 12 50 50 1. 7: 1 15 41
2 most common air-entrainment systems are 1. Air-Entrainment mask (venti-mask) 2. Air-Entrainment nebulizer

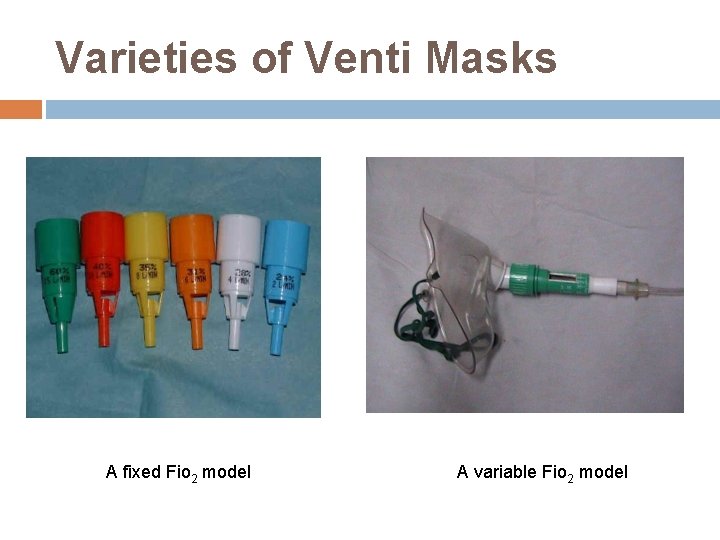
Venturi / Venti / HAFOE Mask consists of a jet orifice around which is an air entrainment port. Fi. O 2 regulated by size of jet orifice and air entrainment port Fi. O 2 – Low to moderate (0. 24 – 0. 60) HIGH FLOW FIXED PERFORMANCE DEVICE
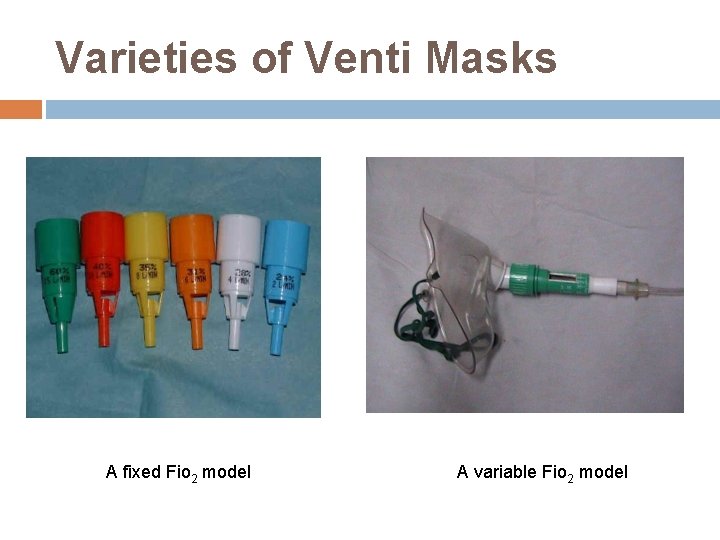
Varieties of Venti Masks A fixed Fio 2 model A variable Fio 2 model
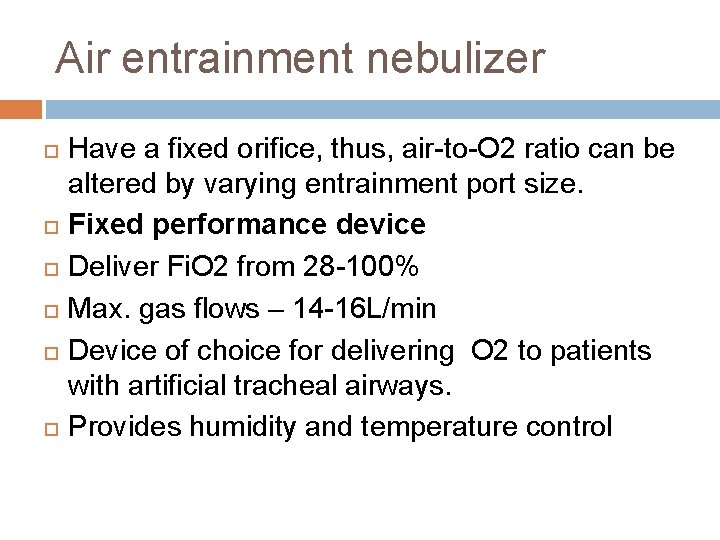
Air entrainment nebulizer Have a fixed orifice, thus, air-to-O 2 ratio can be altered by varying entrainment port size. Fixed performance device Deliver Fi. O 2 from 28 -100% Max. gas flows – 14 -16 L/min Device of choice for delivering O 2 to patients with artificial tracheal airways. Provides humidity and temperature control
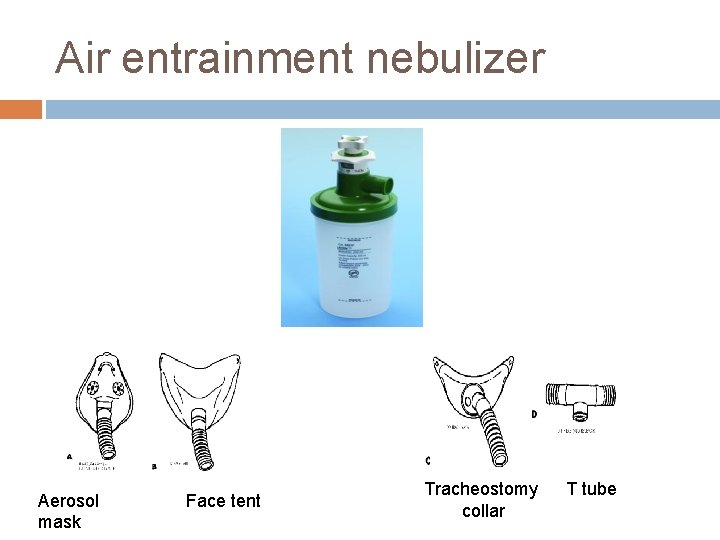
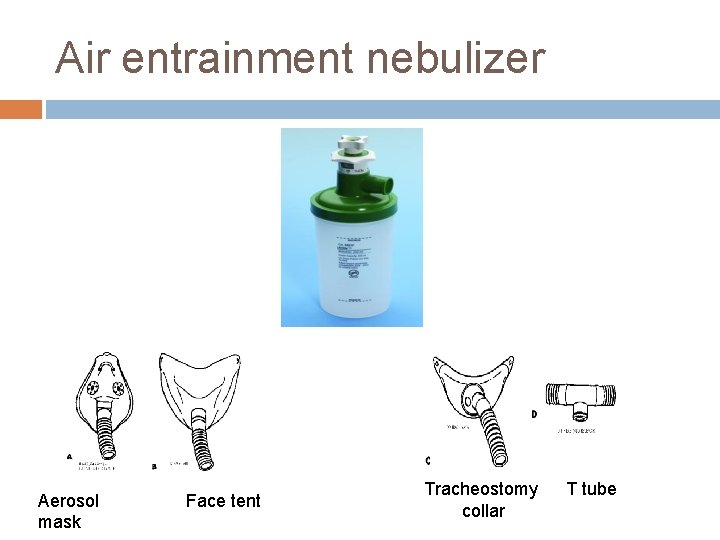
Air entrainment nebulizer Aerosol mask Face tent Tracheostomy collar T tube

How to increase the Fi. O 2 capabilities of airentrainment nebulizers? 1. 2. 3. 4. Adding open reservoir (50 -150 ml aerosol tube) Provide inspiratory reservoir (a 3 -5 L anaesthesia bag) with a one way expiratory valve Connect two or more nebulizers in parallel Set nebulizer to low conc (to generate high flow) and providing supplemental O 2 into delivery tube
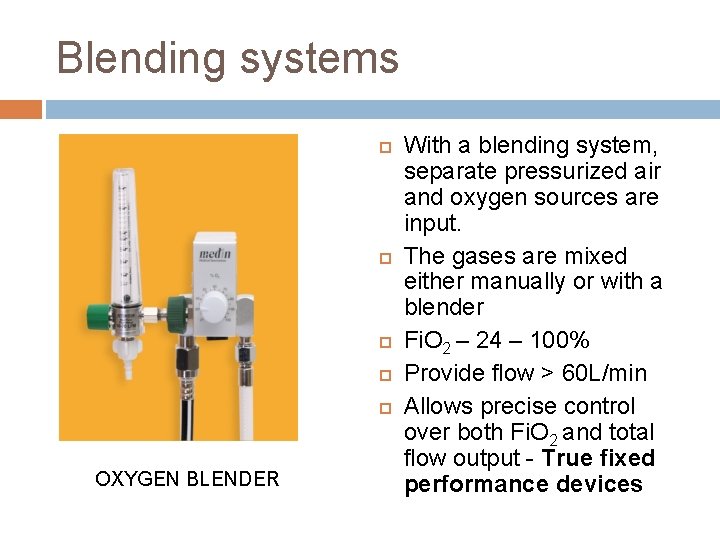
Blending systems OXYGEN BLENDER With a blending system, separate pressurized air and oxygen sources are input. The gases are mixed either manually or with a blender Fi. O 2 – 24 – 100% Provide flow > 60 L/min Allows precise control over both Fi. O 2 and total flow output - True fixed performance devices
ENCLOSURES Oxygen tent Ø Hood Ø Incubator Ø
OXYGEN TENT Consists of a canopy placed over the head and shoulders or over the entire body of a patient Fi. O 2 – 40 -50% @1215 L/min. O 2 Variable performance device Provides concurrent aerosol therapy Disadvantage § § § Expensive Cumbersome Difficult to clean Constant leakage Limits patient mobility
OXYGEN HOOD An oxygen hood covers only the head of the infant O 2 is delivered to hood through either a heated entrainment nebulizer or a blending system Fixed performance device Fio 2 – 21 -100% Minimum Flow > 7/min to prevent CO 2 accumulation

INCUBATOR Incubators are polymethyl methacrylate enclosures that combine servocontrolled convection heating with supplemental O 2 Provides temperature control Fi. O 2 – 40 -50% @ flow of 815 L/min Variable performance
Hyperbaric O 2 Therapy (HBOT)
DEFINITION A mode of medical treatment wherein the patient breathes 100% oxygen at a pressure greater than one Atmosphere Absolute (1 ATA) 1 ATA is equal to 760 mm Hg at sea level
Basis of Hyperbaric O 2 Therapy Dissolved O 2 in plasma : 0. 003 ml / 100 ml of blood / mm PO 2 (Henry’s Law -The concentration of any gas in solution is proportional to its partial pressure. ) Breathing Air (Pa. O 2 100 mm Hg) 0. 3 ml / 100 ml of blood Breathing 100% O 2 (Pa. O 2 600 mm Hg) 1. 8 ml / 100 ml of blood Breathing 100% O 2 at 3 AT. A (Pa. O 2 2000 mm Hg) 6. 0 ml / 100 ml blood the concentration of dissolved o The basis is toofincrease
Physiological effects of HBO Bubble reduction ( boyle’s law) Hyperoxia of blood Enhanced host immune function Neovascularization Vasoconstriction
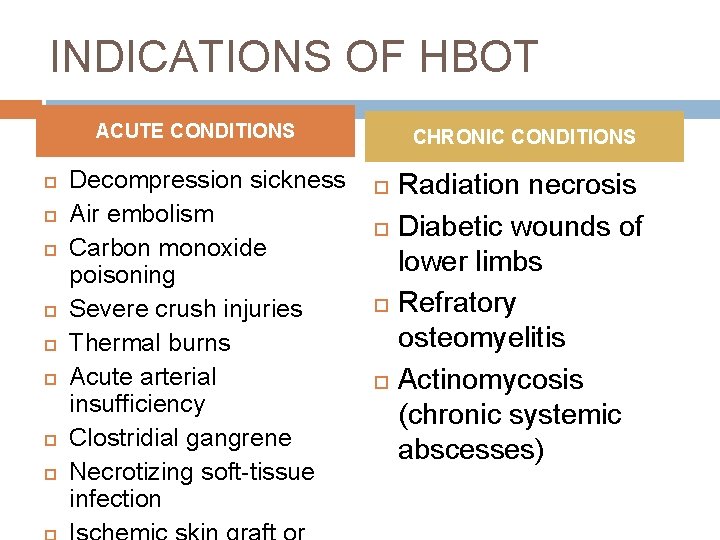
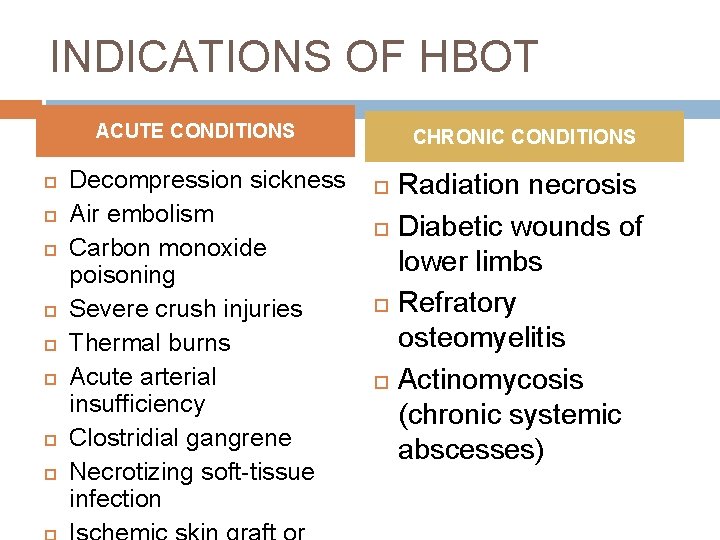
INDICATIONS OF HBOT ACUTE CONDITIONS Decompression sickness Air embolism Carbon monoxide poisoning Severe crush injuries Thermal burns Acute arterial insufficiency Clostridial gangrene Necrotizing soft-tissue infection CHRONIC CONDITIONS Radiation necrosis Diabetic wounds of lower limbs Refratory osteomyelitis Actinomycosis (chronic systemic abscesses)
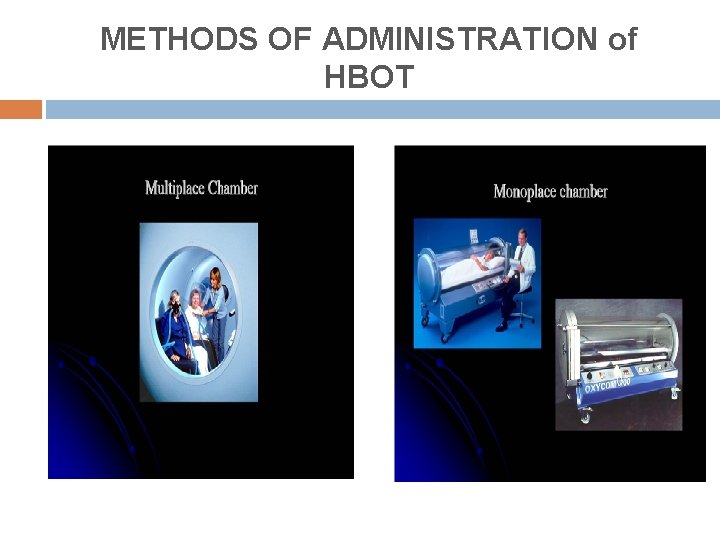
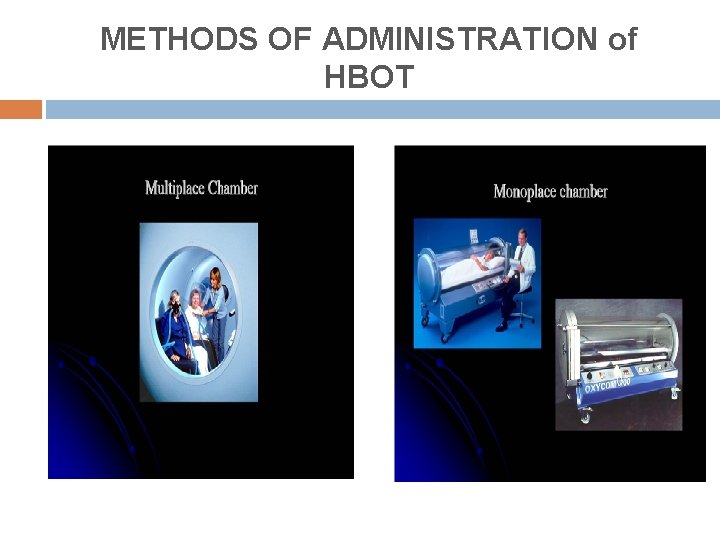
METHODS OF ADMINISTRATION of HBOT
Problems with HBOT Barotrauma Ear/ sinus trauma Tympanic membrane rupture Pneumothorax Oxygen toxicity Fire hazards Clautrophobia Sudden decompression

Complications of Oxygen therapy
Complications of Oxygen therapy 1. Oxygen toxicity 2. Depression of ventilation 3. Retinopathy of Prematurity 4. Absorption atelectasis 5. Fire hazard
1. O 2 Toxicity Primarily affects lung and CNS. 2 factors: Pa. O 2 & exposure time CNS O 2 toxicity (Paul Bert effect) occurs on breathing O 2 at pressure > 1 atm tremors, twitching, convulsions
Pulmonary Oxygen toxicity C/F q acute tracheobronchitis Cough and substernal pain ARDS like state

Pulmonary O 2 Toxicity (Lorrain. Smith effect) Mechanism: High p. O 2 for a prolonged period of time ↓ intracellular generation of free radicals e. g. : superoxide, H 2 O 2 , singlet oxygen ↓ react with cellular DNA, sulphydryl proteins &lipids ↓ cytotoxicity ↓ damages capillary endothelium,
Interstitial edema Thickened alveolar capillary membrane. ↓ Pulmonary fibrosis and hypertension
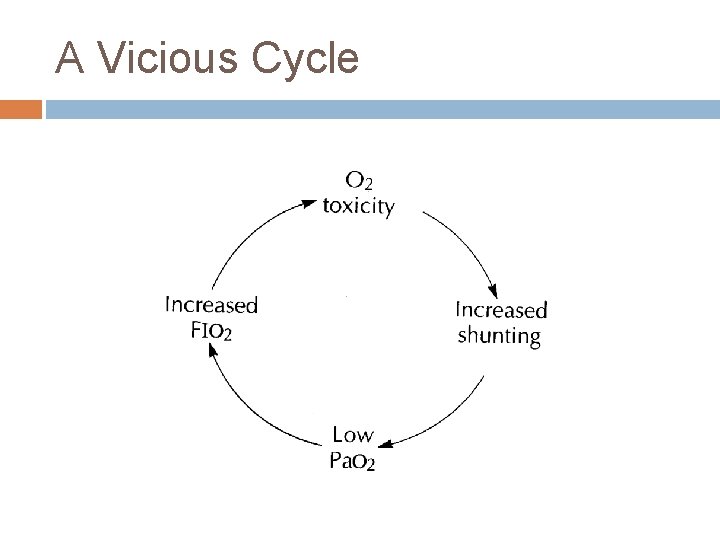
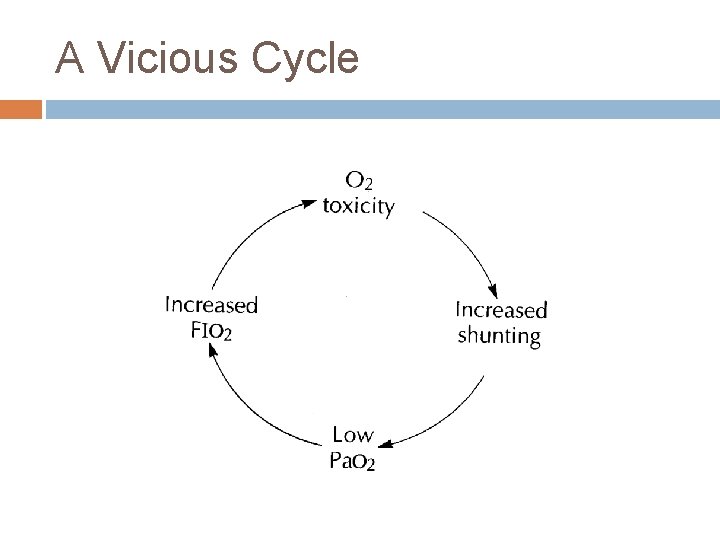
A Vicious Cycle
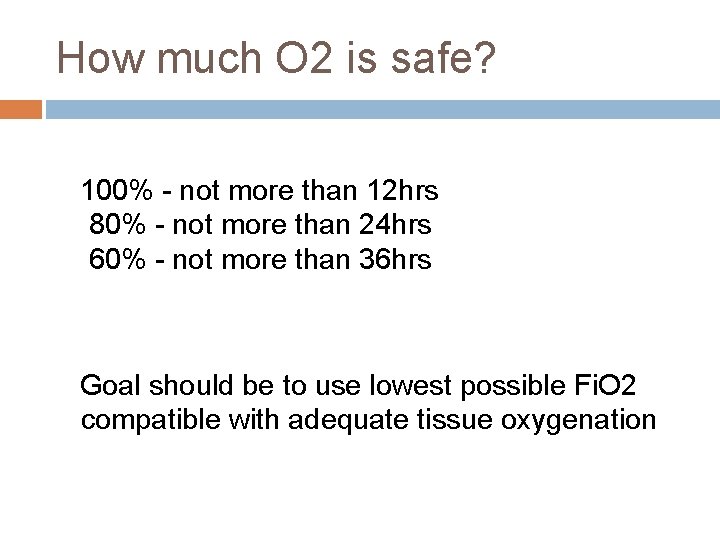
How much O 2 is safe? 100% - not more than 12 hrs 80% - not more than 24 hrs 60% - not more than 36 hrs Goal should be to use lowest possible Fi. O 2 compatible with adequate tissue oxygenation
Indications for 70% - 100% oxygen therapy 1. 2. 3. Resuscitation Periods of acute cardiopulmonary instability Patient transport
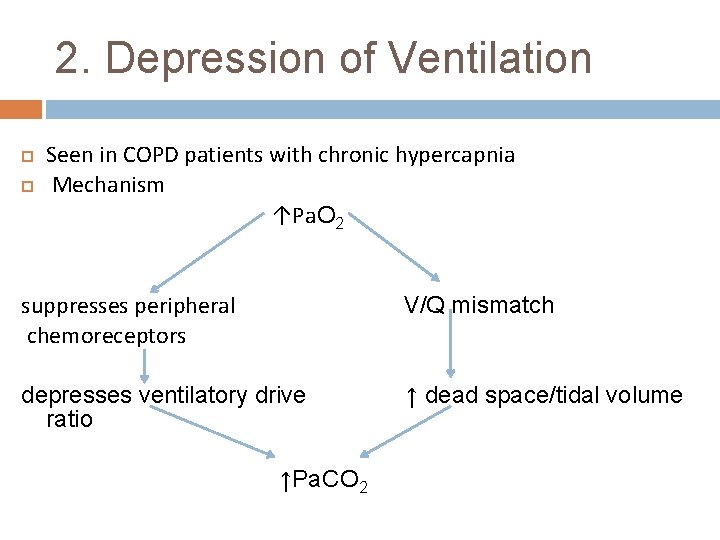
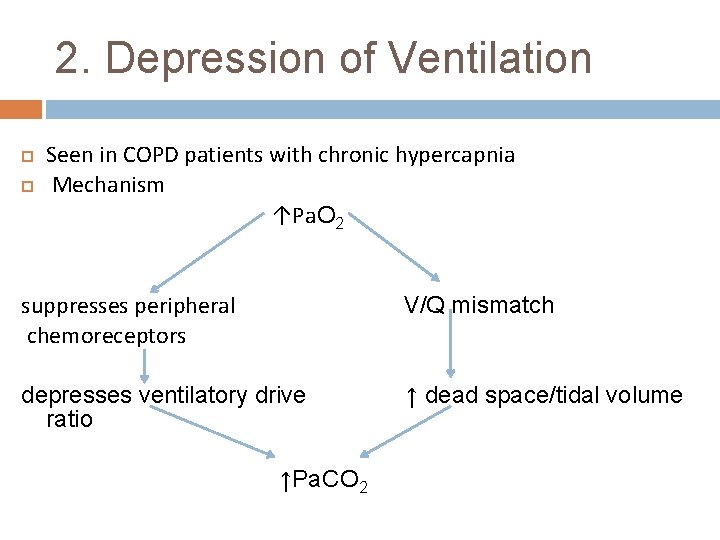
2. Depression of Ventilation Seen in COPD patients with chronic hypercapnia Mechanism ↑Pa. O 2 suppresses peripheral chemoreceptors V/Q mismatch depresses ventilatory drive ratio ↑ dead space/tidal volume ↑Pa. CO 2
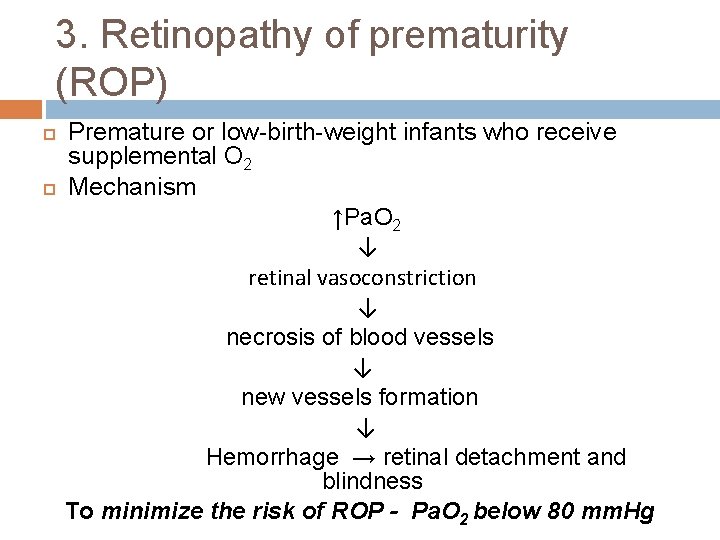
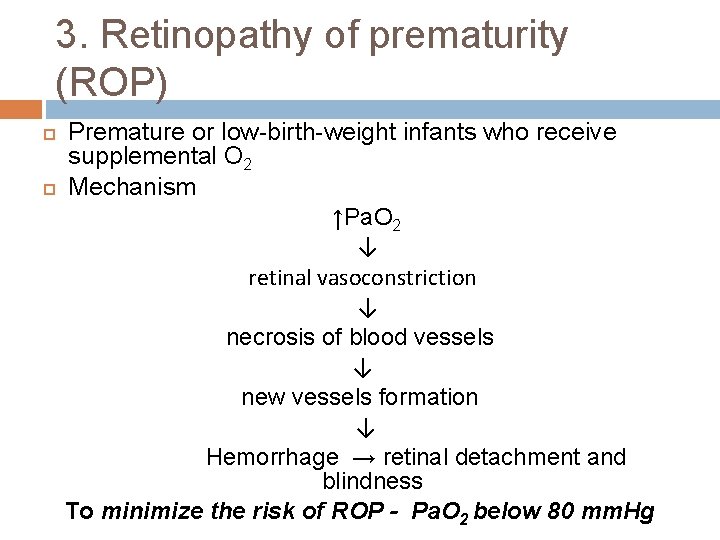
3. Retinopathy of prematurity (ROP) Premature or low-birth-weight infants who receive supplemental O 2 Mechanism ↑Pa. O 2 ↓ retinal vasoconstriction ↓ necrosis of blood vessels ↓ new vessels formation ↓ Hemorrhage → retinal detachment and blindness To minimize the risk of ROP - Pa. O 2 below 80 mm. Hg
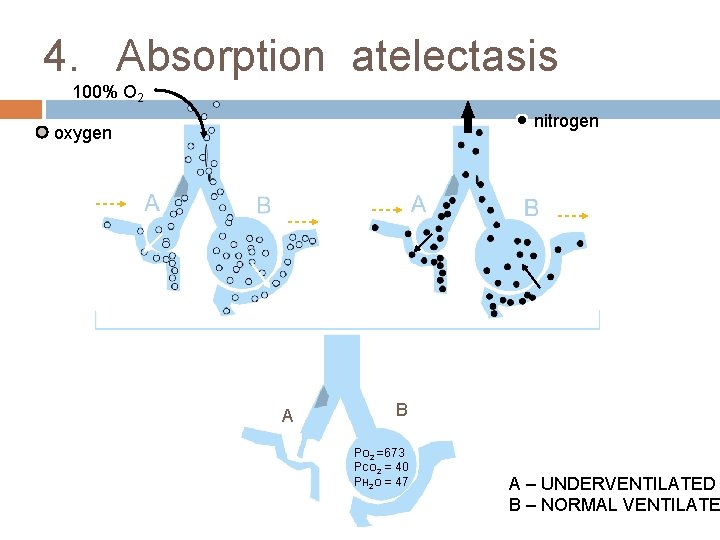
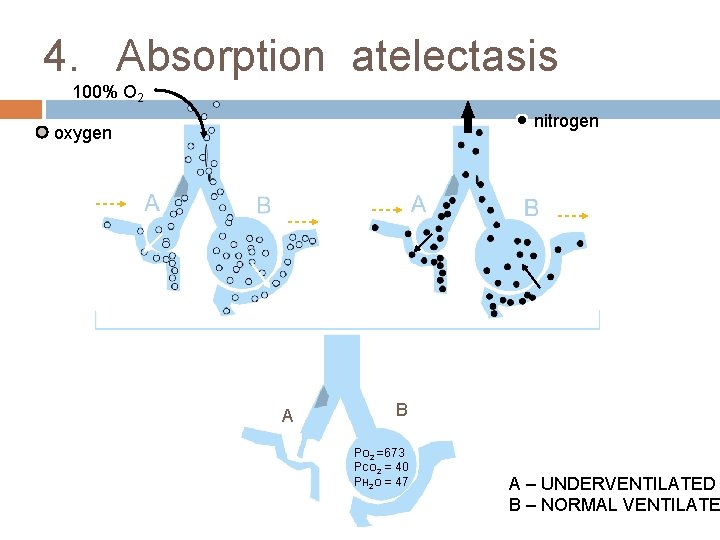
4. Absorption atelectasis 100% O 2 nitrogen oxygen A B PO 2 =673 PCO 2 = 40 PH 2 O = 47 A – UNDERVENTILATED B – NORMAL VENTILATE
Denitrogenation Absorption atelectasis The “denitrogenation” absorption atelectasis is because of collapse of underventilated alveoli (which depends on nitrogen volume to remain above critical volume ) ↓ Increased physiological shunt
5. Fire hazard High Fi. O 2 increases the risk of fire Preventive measures Lowest effective Fi. O 2 should be used Use of scavenging systems Avoid use of outdated equipment such as aluminium gas regulators Fire prevention protocols should be followed for hyperbaric O 2 therapy
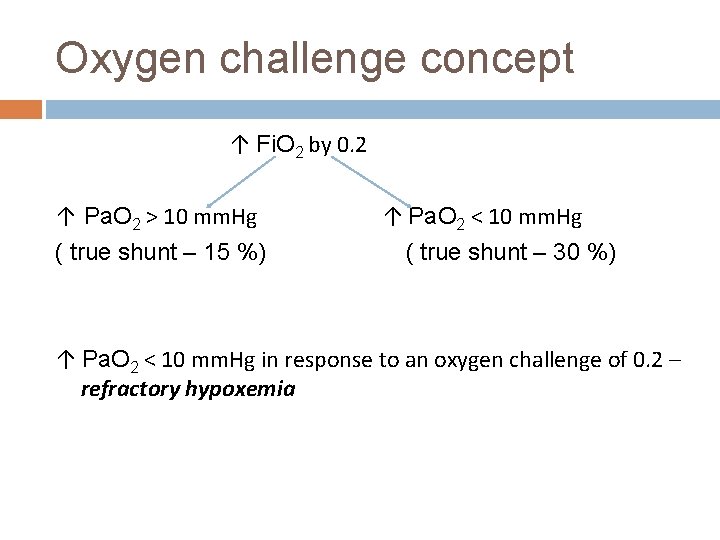
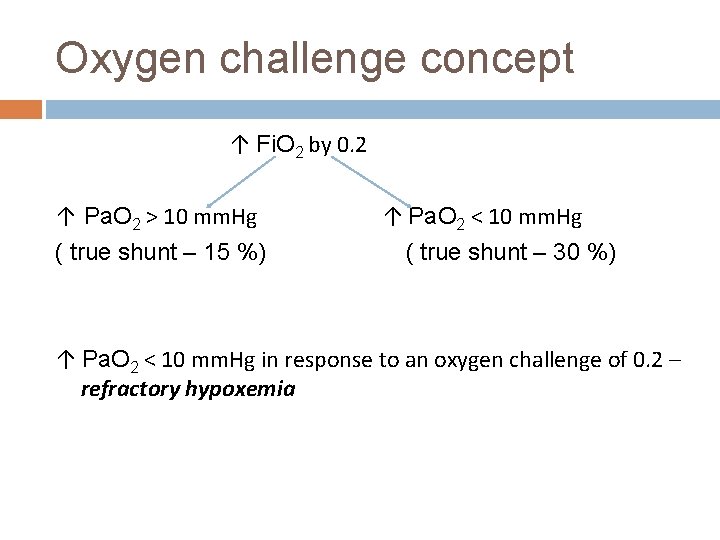
Oxygen challenge concept ↑ Fi. O 2 by 0. 2 ↑ Pa. O 2 > 10 mm. Hg ( true shunt – 15 %) ↑ Pa. O 2 < 10 mm. Hg ( true shunt – 30 %) ↑ Pa. O 2 < 10 mm. Hg in response to an oxygen challenge of 0. 2 – refractory hypoxemia
Implications of Oxygen challenge concept q q q To identify refractory hpoxemia (as it does not respond to increased Fi. O 2) Refractory hpoxemia depends on increased cardiac output to maintain acceptable Fi. O 2 Potentially deleterious effect of increased Fi. O 2 can be avoided
SUMMARY q • • • q Therapeutic effectiveness of oxygen therapy is limited to 25% - 50% Low V/Q hypoxemia is reversed with less than 50% DAA occurs with Fi. O 2 more than 50% Pulmonary oxygen toxicity is a potential risk factor with Fi. O 2 more than 50% Bronchodilators, bronchial hygiene therapy and diuretic therapy decreases the need for high Fi. O 2

Oxygen is a drug. When appropriately used, it is extremely beneficial When misused or abused, it is potentially harmful
References Medical gas therapy. Egan’s Fundamentals of respiratory care. 9 th ed. Oxygen delivery systems, inhalation therapy and respiratory therapy. Benumof’s Airway management. 2 nd ed. Shapiro BA. Hypoxemia and oxygen therapy. Clinical application of blood gases. 5 TH ed. Oxygen and associated gases. Wiley 5 th ed. Miller’s Anaesthesia 7 th ed. Paul L. Marino. The ICU Book. 3 rd ed.

THANK YOU….
 Pasteur point oxygen cascade
Pasteur point oxygen cascade Richa goyal
Richa goyal Richa shukla pregnant
Richa shukla pregnant Dr shaleen agarwal
Dr shaleen agarwal Richa shukla md
Richa shukla md Richa rai
Richa rai Fraction of inspired oxygen
Fraction of inspired oxygen Oxygen therapy
Oxygen therapy 沈榮麟
沈榮麟 Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Humanistic therapies aim to boost
Humanistic therapies aim to boost Right sided vs left sided murmurs
Right sided vs left sided murmurs Nus myedu
Nus myedu Jain bcn
Jain bcn Dr piyush jain rml hospital
Dr piyush jain rml hospital Ashish jain microsoft
Ashish jain microsoft Anu jain
Anu jain Dr salil jain
Dr salil jain Jain center of northern california
Jain center of northern california Prateek jain
Prateek jain Jain society of central florida
Jain society of central florida Pramod lunawat
Pramod lunawat Jsne
Jsne Religion
Religion Mitthu jain
Mitthu jain Eric jain
Eric jain Vaibhav.14v
Vaibhav.14v Earpiece
Earpiece Pankaj jain kanpur
Pankaj jain kanpur Meru rajju
Meru rajju Jain
Jain Vivek jain
Vivek jain Conclusion of jainism
Conclusion of jainism Jain temple boston
Jain temple boston Functional encryption
Functional encryption Cherry hill jain sangh
Cherry hill jain sangh Jain way of life
Jain way of life 14 rajlok
14 rajlok Agam sutras
Agam sutras Melena management
Melena management Vidya jain case
Vidya jain case Aagam jain nlsiu
Aagam jain nlsiu Preet jain
Preet jain Vinod jain ca
Vinod jain ca Aparajita jain
Aparajita jain Qhe
Qhe Temple
Temple Javax.sip
Javax.sip Vaibhav jain
Vaibhav jain Principles of jainism
Principles of jainism Jain portal
Jain portal Jain society of toronto
Jain society of toronto Jain
Jain Prateek jain msr
Prateek jain msr Jain geography
Jain geography Unified mpls
Unified mpls Dr tulika jain
Dr tulika jain Raina jain dartmouth
Raina jain dartmouth Eakta jain
Eakta jain Csu otd
Csu otd Florida occupational therapy association
Florida occupational therapy association Grand valley occupational medicine
Grand valley occupational medicine University of cumbria occupational therapy
University of cumbria occupational therapy Wake tech admissions
Wake tech admissions Early college high school at midland college
Early college high school at midland college Tourism definition
Tourism definition Stranmillis university college
Stranmillis university college Norwegian police university college
Norwegian police university college Lincoln memorial university college of veterinary medicine
Lincoln memorial university college of veterinary medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine University of iowa college of dentistry
University of iowa college of dentistry Clark university college board
Clark university college board Artesis plantijn university college of antwerp
Artesis plantijn university college of antwerp Norwegian defence university college
Norwegian defence university college King saud university college of pharmacy
King saud university college of pharmacy King saud university college of medicine
King saud university college of medicine Jubail university college
Jubail university college Oslo and akershus university college
Oslo and akershus university college University b.t. & evening college
University b.t. & evening college University college of norwegian correctional service
University college of norwegian correctional service Queen's university early childhood education
Queen's university early childhood education Bangkok university international
Bangkok university international Stranmillis university college
Stranmillis university college Al mustansiriya university college of medicine
Al mustansiriya university college of medicine Ethiopian police university logo
Ethiopian police university logo University bt and evening college
University bt and evening college Telemark university college
Telemark university college Midwestern university college of dental medicine
Midwestern university college of dental medicine King saud university college of pharmacy
King saud university college of pharmacy King saud university college of pharmacy
King saud university college of pharmacy College of engineering, king abdulaziz university
College of engineering, king abdulaziz university Seoul national university medical school
Seoul national university medical school Ukcom curriculum
Ukcom curriculum Boston university metropolitan college
Boston university metropolitan college Salahaddin university college of education
Salahaddin university college of education King saud university college of business administration
King saud university college of business administration Lms juc
Lms juc Hawler medical university college of nursing
Hawler medical university college of nursing