Oxygen Therapy Dr jarahzadeh MD Intensivist Oxygen Therapy



- Slides: 40

Oxygen Therapy Dr jarahzadeh MD. Intensivist
Oxygen Therapy Administration of oxygen at an FIO 2 > 21%
Introduction • Oxygen is a drug – Has a Drug Identification Number (DIN) – Colorless, odorless, tasteless gas – Makes up 21% of room air – Is NOT flammable but does support combustion. 4
Indications for Oxygen Therapy • Hypoxemia – Inadequate amount of oxygen in the blood – SPO 2 < 90% – Pa. O 2 < 60 mm. Hg • Excessive work of breathing • Excessive myocardial workload 5
Factors Influencing Oxygen Transport • • Cardiac output Arterial oxygen content Concentration of Hgb Metabolic requirements
• Hypoxemia • decrease in the arterial oxygen content in the blood • Hypoxia • decreased oxygen supply to the tissues.
Causes of Hypoxemia • Shunt • Hypoventilation – As carbon dioxide increases oxygen falls • V/Q mismatching (ventilation/perfusion) – Pneumonia – Pulmonary edema – ARDS • Increased diffusion gradient – asbestosis – Early pulmonary edema 8
Clinical Manifestations of Hypoxia • Impaired judgment, agitation (restlessness), disorientation, confusion, lethargy, coma • Dyspnea • Tachycardia, dysrhythmias • Elevated BP • Diaphoresis • Central cyanosis
Need For Oxygen Is Assessed By • Clinical evaluation • Pulse oximetry • ABG
Cautions For Oxygen Therapy • Oxygen toxicity – can occur with Fio 2 > 60% longer than 36 hrs • Fio 2>80%longer than 24 hrs Fio 2>100%longer than 12 hrs • Suppression of ventilation – will lead to increased CO 2 and carbon dioxide narcosis • Danger of fire • Absorbtion Atelectasia • Premature retrolental fibroplasia
Methods of Dispensing Oxygen • Piped in • Cylinder • Oxygen concentrator
Classification of Oxygen Delivery Systems • Low flow systems – contribute partially to inspired gas client breathes – do not provide constant FIO 2 – Ex: nasal cannula, simple mask • High flow systems – deliver specific and constant percent of oxygen independent of client’s breathing – Ex: Venturi mask, non-rebreather mask, trach collar, T-piece
Nasal Cannula • Used for low-medium concentrations of O 2 • Simple • Can use continuously with meals and activity • Flow rates in excess of 4 L cause drying and irritation • Depth and rate of breathing affect amount of O 2 reaching lungs • adults 6 LPM • infants/toddlers 2 LPM • children 3 LPM • FIO 2 is not affected by mouth breathing • 1 lit o 2=FIO 2 4% • 6 lito 2=Fio 2 24% • 21%+24%=Fio 2 45%
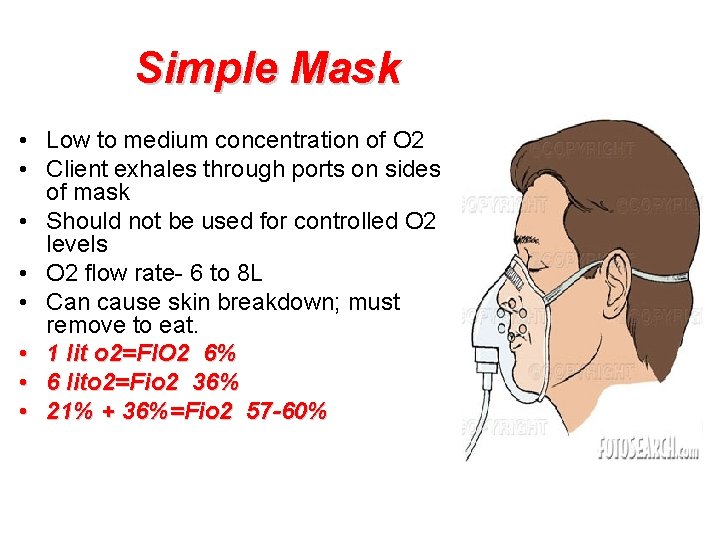
Simple Mask • Low to medium concentration of O 2 • Client exhales through ports on sides of mask • Should not be used for controlled O 2 levels • O 2 flow rate- 6 to 8 L • Can cause skin breakdown; must remove to eat. • 1 lit o 2=FIO 2 6% • 6 lito 2=Fio 2 36% • 21% + 36%=Fio 2 57 -60%
Partial Rebreather Mask • Consists of mask with exhalation ports and reservoir bag • Reservoir bag must remain inflated • O 2 flow rate - 6 to 10 L FIO 2=60%-80% • Client can inhale gas from mask, bag, exhalation ports • Poorly fitting; must remove to eat
Non-Rebreathing Mask • Consists of mask, reservoir bag, 2 one-way valves at exhalation ports and bag • Client can only inhale from reservoir bag • Bag must remain inflated at all times • O 2 flow rate- 10 to 15 L Fio 2= 95 -100% • Poorly fitting; must remove to eat
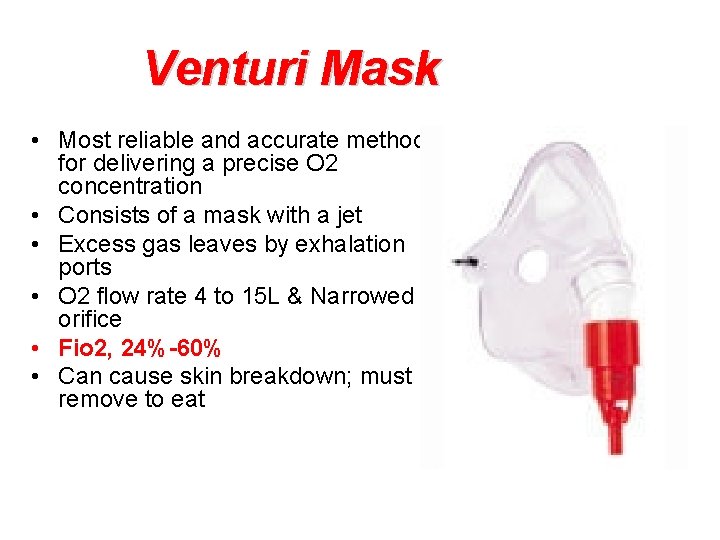
Venturi Mask • Most reliable and accurate method for delivering a precise O 2 concentration • Consists of a mask with a jet • Excess gas leaves by exhalation ports • O 2 flow rate 4 to 15 L & Narrowed orifice • Fio 2, 24%-60% • Can cause skin breakdown; must remove to eat
Tracheostomy Collar/Mask • O 2 flow rate 8 to 10 L • Provides accurate FIO 2 • Provides good humidity; comfortable
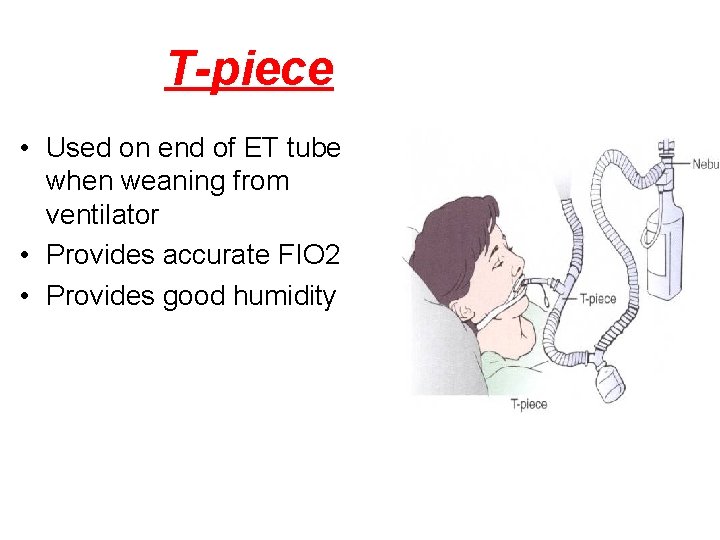
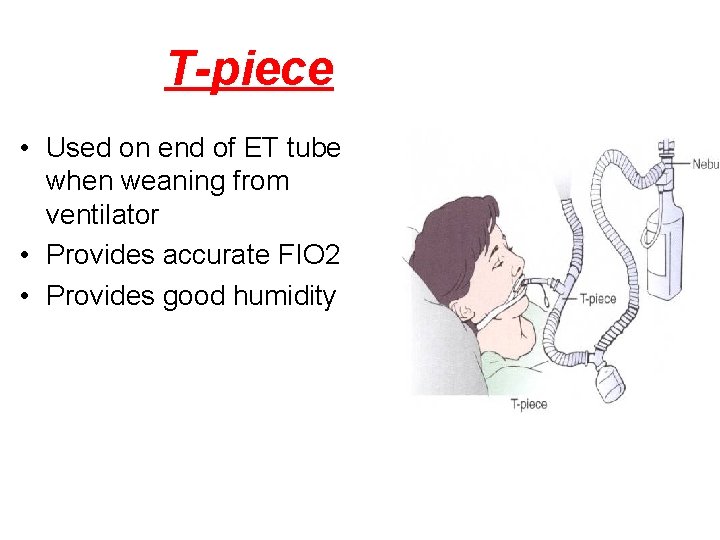
T-piece • Used on end of ET tube when weaning from ventilator • Provides accurate FIO 2 • Provides good humidity
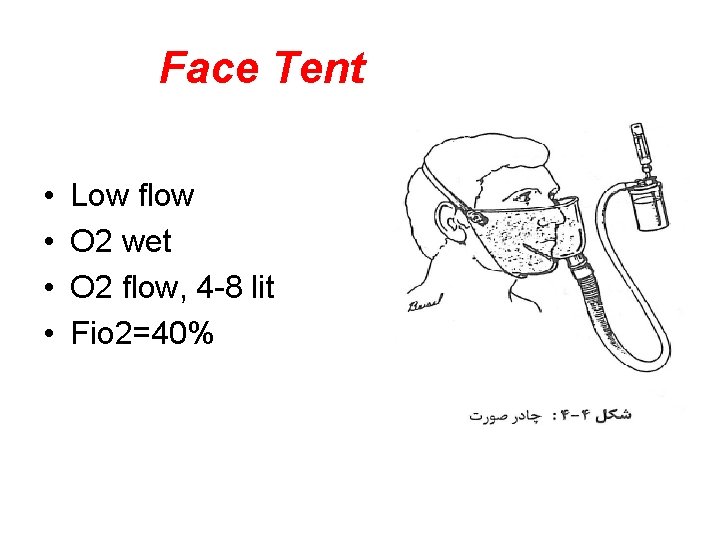
Face Tent • • Low flow O 2 wet O 2 flow, 4 -8 lit Fio 2=40%
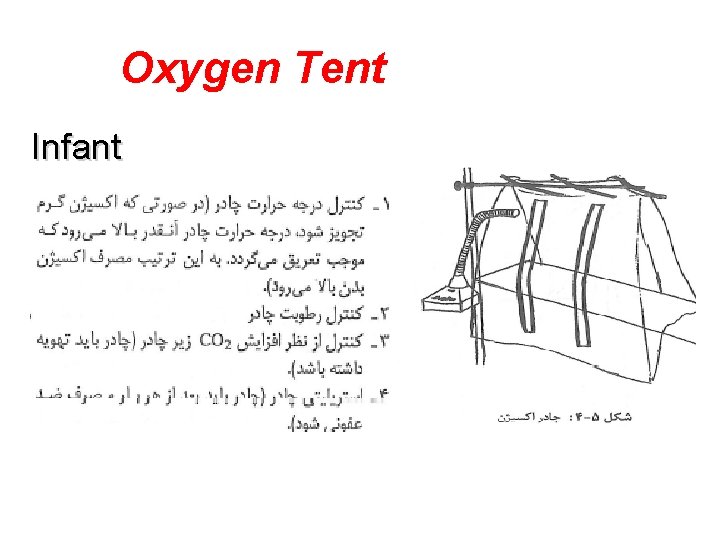
Oxygen Tent Infant
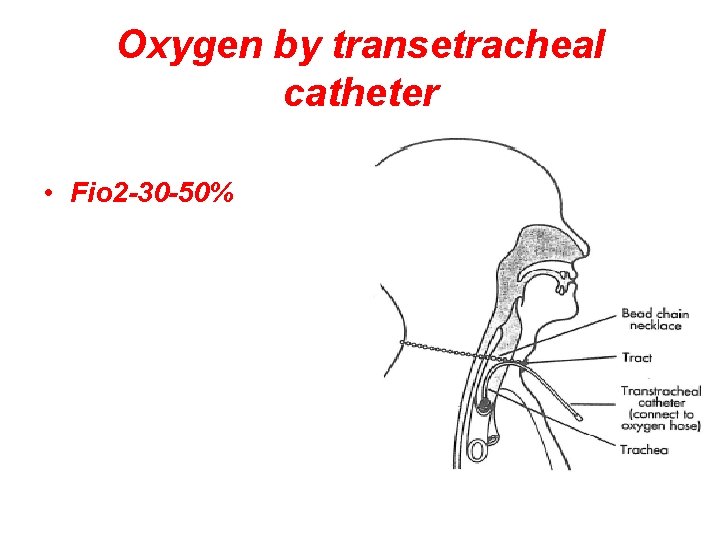
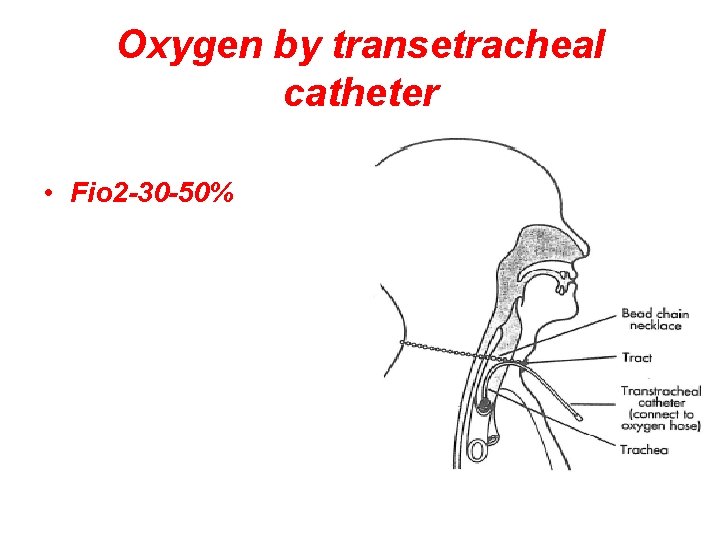
Oxygen by transetracheal catheter • Fio 2 -30 -50%
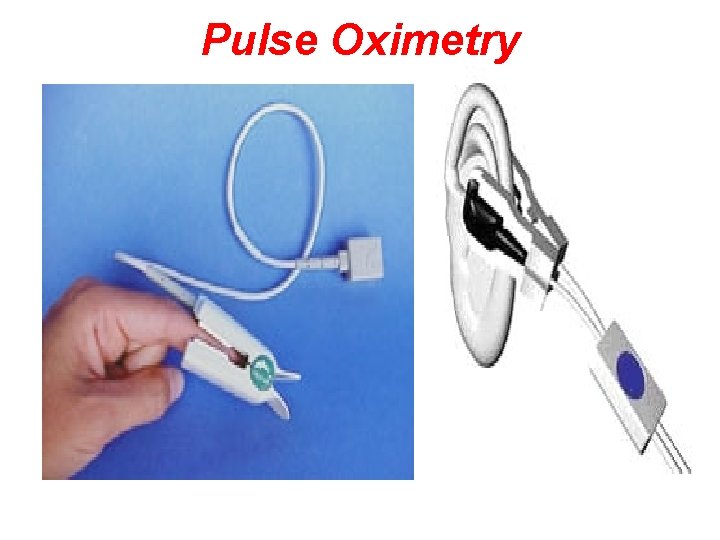
Pulse Oximetry • Non-invasive monitoring technique that estimates the oxygen saturation of Hgb (Sa. O 2) • May be used continuously or intermittently • Must correlate values with physical assessment findings • Normal Sa. O 2 values – 95 to 100%
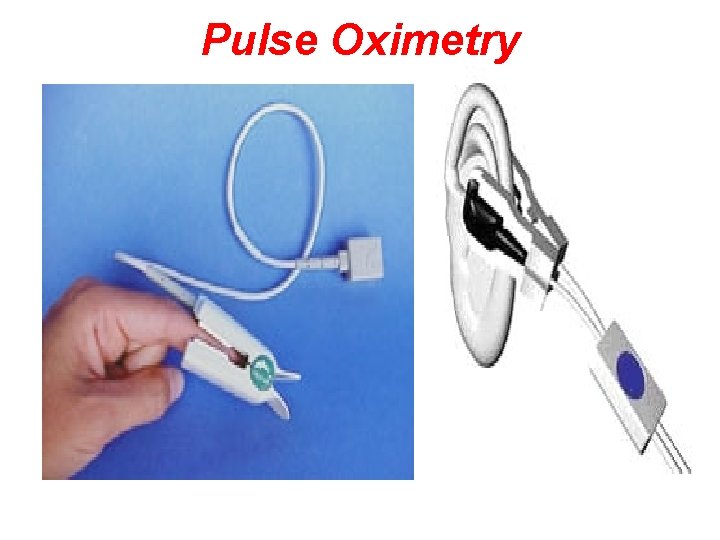
Pulse Oximetry
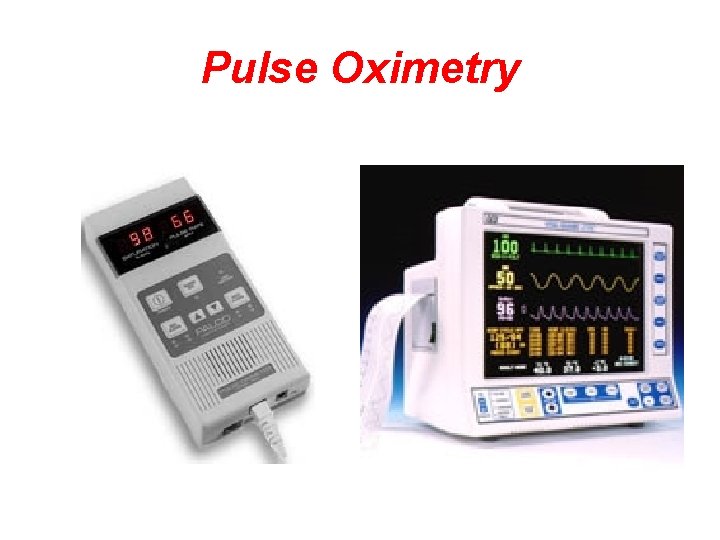
Pulse Oximetry
Factors Affecting Sa. O 2 Measurements • • Low perfusion states Motion artifact Nail polish(Blue) when using a finger probe Intravascular dyes(methylen blue, indocyanine green, indigocarmine) • Vasoconstrictor medications • Abnormal Hgb(met-Co. Hb) • Too much light exposure
Nursing Interventions Related to Pulse Oximetry Monitoring • Determine if strength of signal is adequate • Notify physician if Sa. O 2 < 92% or outside specific ordered limits • If continuously monitored, evaluate sensor site every 8 hrs and move PRN • Document Sa. O 2, O 2 requirements, client’s activity according to policy
Oxygen Therapy • Goal of therapy is an SPO 2 of >90% or for documented COPD patients(Spo 2 88– 92%)-(Pao 2=55 -60) • As SPO 2 normalizes the patients vital signs should improve” – Heart rate should return to normal for patient – Respiratory rate should decrease to normal for patient – Blood pressure should normalize for patient 29
Optimization • My Sp. O 2 is < 90%, what next? – Is the pulse oximeter working/accurate • • • Do I have a good signal? Heart rate plus/minus ? Is there adequate perfusion at the probe site? Can the probe be repositioned? Do other vital signs or clinical manifestations give evidence of hypoxemia? 30
Optimization cont. • Check my source! – Ensure the O 2 delivery device is attached to oxygen not medical air. – Follow tubing back to source and ensure patency – Are all connections tight? • Is the flow set high enough? – All nebs especially high flow large volume nebs need to be run at the highest rate. – Turn flow meter to maximum for large volume nebs. 31
Optimization cont. • Reposition patient. – Avoid laying patient flat on back. – Raise head of bed. – Encourage deep breathing/coughing • Listen to chest. – Wheezing? • Do they need a bronchodilator? – Crackles? • Encourage deep breathing/cough. • Are they fluid overloaded? 32
optimization cont. • Can I improve the mechanics of breathing? – Patient position – Pursed lip breathing – Abdominal breathing. – Anxiety relief? 33
Optimization cont. • Increase the flow: – With nasal prongs, increase the flow rate by 1 -2 lpm increments until target Sp. O 2 is reached. – High flow nasal prongs can be maximally set at 15 lpm. – Call for physician assessment Medical if high oxygen flows are required. 34
Optimization cont. • What do I do if my patient is really hypoxemic (on low flow oxygen)? – Assess patient to determine cause of increasing oxygen requirements. – Best short term solution is non-rebreathe mask at 15 lpm. (reservoir stays inflated) – Goal saturation is still 88 – 92%. – Increase flow as required until re-assessed by physician 35
Optimization cont. • What do I do if my patient is really hypoxemic (on high flow oxygen)? – Assess patient to determine cause of increasing oxygen requirements. – Adjust FIO 2 upwards in 10% increments titrating for target SPO 2. – Call physician for further assessment 36
H 1 N 1 points of emphasis • H 1 N 1 decompensation requiring ICU admission usually begins with a systemic inflammatory response and pulmonary edema • CXR may not correlate with degree of oxygenation impairment • Gradually increasing oxygen requirement is a sentinel sign of impending respiratory failure 37
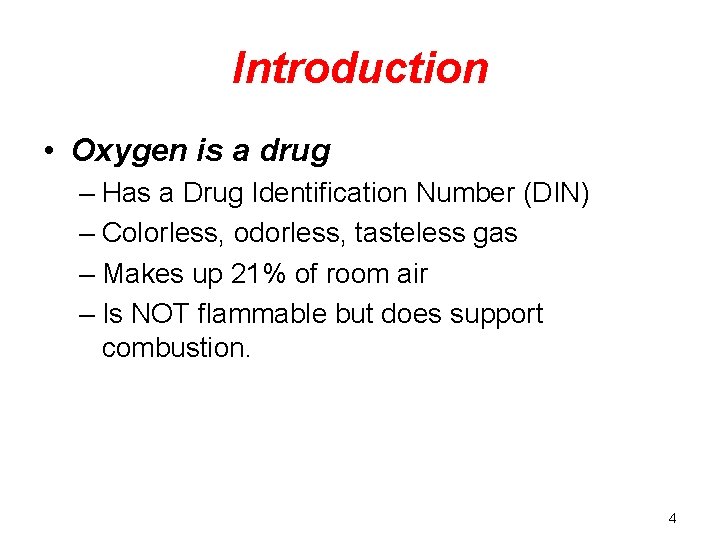
H 1 N 1 points of emphasis • H 1 N 1 Patients with escalating O 2 needs warrant frequent monitoring for signs of impending respiratory failure • If a critical care triage system is operative, know the patient’s classification and prepare equipment accordingly – endotracheal intubation may not be an option 38


Questions? Thank you for attention !