HYPERTRIGLYCERIDEMIAINDUCED PANCREATITIS Richa Shukla PGY 5 Faculty Mentor











- Slides: 40
HYPERTRIGLYCERIDEMIAINDUCED PANCREATITIS Richa Shukla, PGY 5 Faculty Mentor: Dr. Suneal Agarwal September 4, 2014
HPI Reason for consult: pancreatitis 31 F G 2 P 1, 24 -weeks pregnant patient who presented as an outside hospital transfer for management of pancreatitis Initially presented to a hospital in Odessa on 1/12/14 with complaints of 2 -3 days of severe epigastric pain. No clear etiology found and patient was discharged after resolution of pain
Case Discussion (cont. ) Patient returned to the OSH on 1/26/14 with ~2 -3 days of worsening epigastric pain radiating to the back On admission, was found to be in diabetic ketoacidosis and had laboratory evidence of pancreatitis with a lipase of 2400. Patient’s triglycerides were found to be >10, 000 Was diagnosed with hypertriglyceridemic pancreatitis.
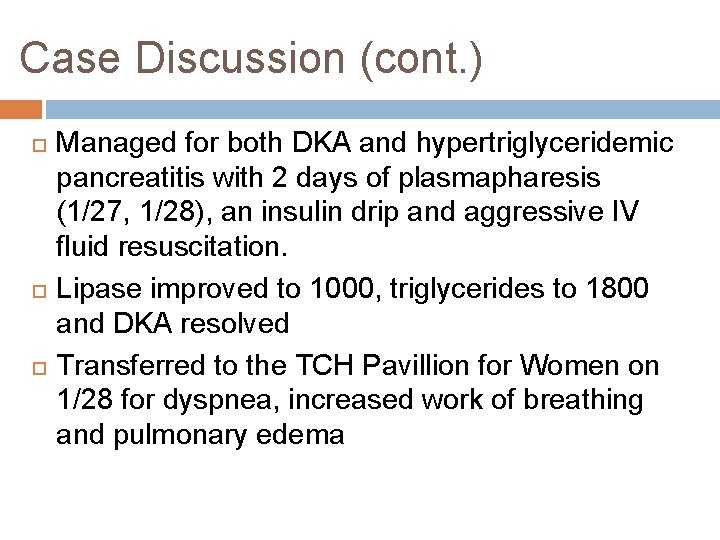
Case Discussion (cont. ) Managed for both DKA and hypertriglyceridemic pancreatitis with 2 days of plasmapharesis (1/27, 1/28), an insulin drip and aggressive IV fluid resuscitation. Lipase improved to 1000, triglycerides to 1800 and DKA resolved Transferred to the TCH Pavillion for Women on 1/28 for dyspnea, increased work of breathing and pulmonary edema
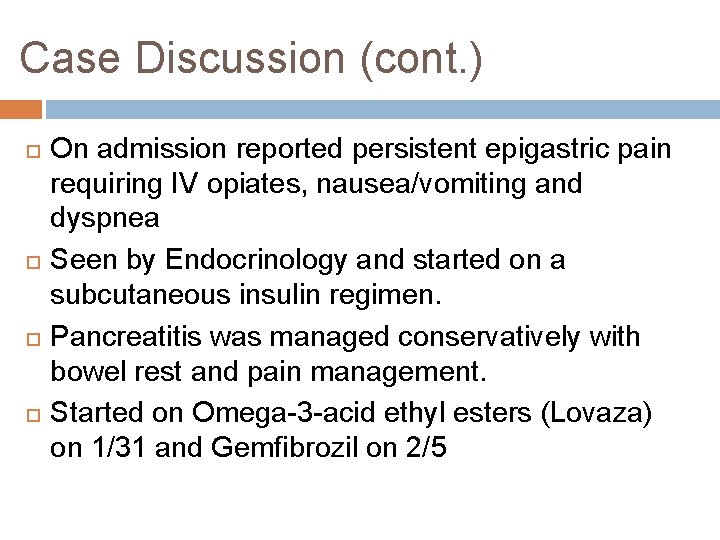
Case Discussion (cont. ) On admission reported persistent epigastric pain requiring IV opiates, nausea/vomiting and dyspnea Seen by Endocrinology and started on a subcutaneous insulin regimen. Pancreatitis was managed conservatively with bowel rest and pain management. Started on Omega-3 -acid ethyl esters (Lovaza) on 1/31 and Gemfibrozil on 2/5
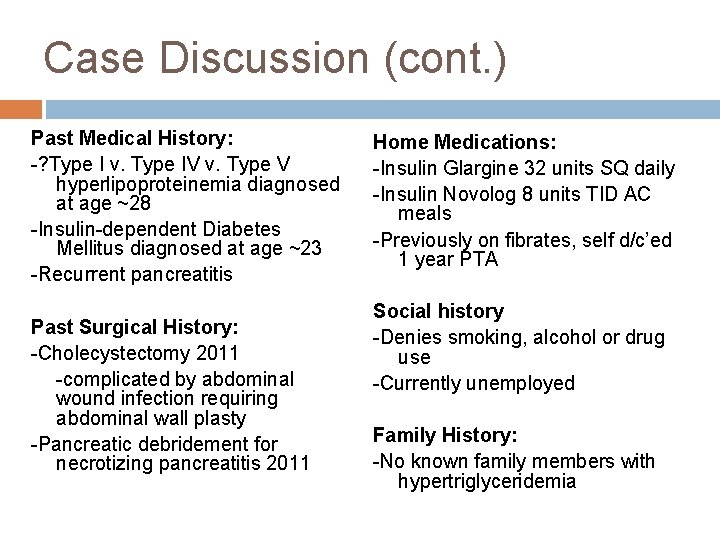
Case Discussion (cont. ) Past Medical History: -? Type I v. Type IV v. Type V hyperlipoproteinemia diagnosed at age ~28 -Insulin-dependent Diabetes Mellitus diagnosed at age ~23 -Recurrent pancreatitis Past Surgical History: -Cholecystectomy 2011 -complicated by abdominal wound infection requiring abdominal wall plasty -Pancreatic debridement for necrotizing pancreatitis 2011 Home Medications: -Insulin Glargine 32 units SQ daily -Insulin Novolog 8 units TID AC meals -Previously on fibrates, self d/c’ed 1 year PTA Social history -Denies smoking, alcohol or drug use -Currently unemployed Family History: -No known family members with hypertriglyceridemia

Physical Exam T 99. 7, BP 126/84, HR 113, RR 22, O 2 sat 96% 2 L NC Gen: NAD, AAOx 4 HEENT: anicteric sclera, PERRL, EOMI, MMM, OP clear CV: RRR no m/r/g Chest: bilateral crackles in lower lung fields, no wheezes Abd: soft, tender to palpation in epigastric region, NABS, +gravid uterus Ext: WWP, no clubbing or cyanosis, trace LE edema Neuro: oriented x 4, fatigued, conversational
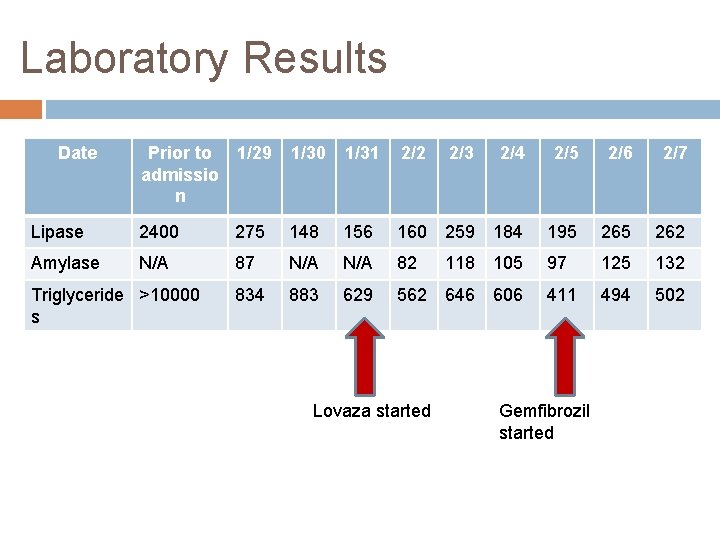
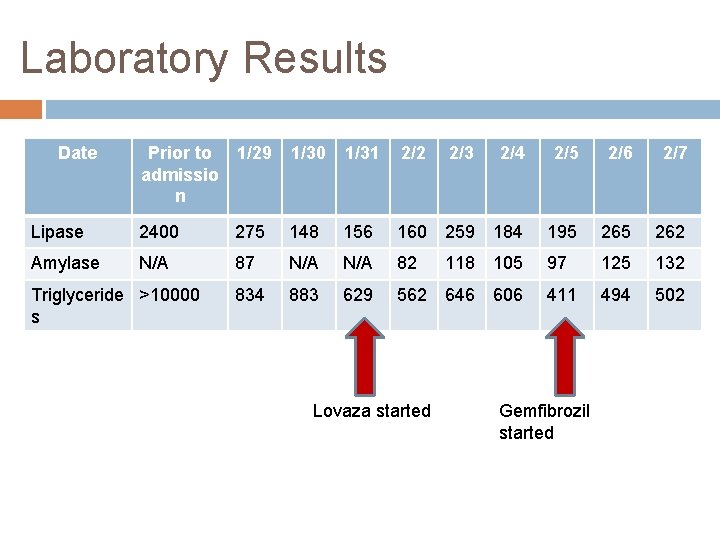
Laboratory Results Date Prior to admissio n 1/29 1/30 1/31 2/2 2/4 2/5 2/6 2/7 Lipase 2400 275 148 156 160 259 184 195 262 Amylase N/A 87 N/A 82 97 125 132 834 883 629 562 646 606 411 494 502 Triglyceride >10000 s Lovaza started 2/3 118 105 Gemfibrozil started
Severity of pancreatitis Not all results from her outside hospital admission were available however notes from the OSH suggest BISAP score of 2 on admission
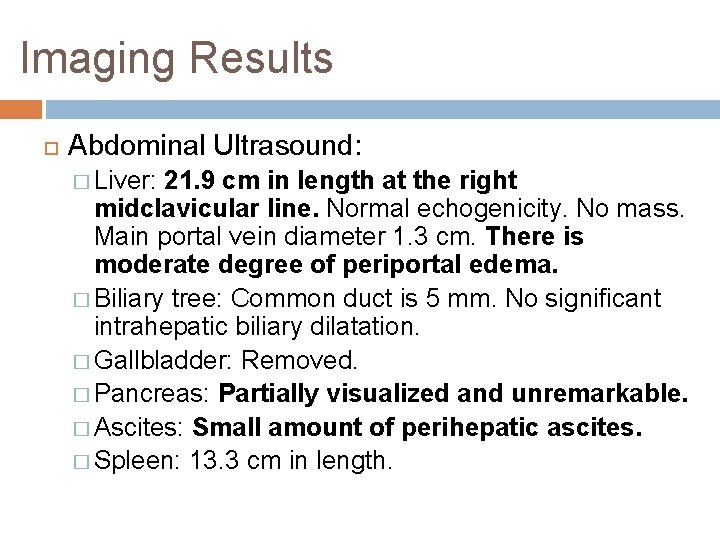
Imaging Results Abdominal Ultrasound: � Liver: 21. 9 cm in length at the right midclavicular line. Normal echogenicity. No mass. Main portal vein diameter 1. 3 cm. There is moderate degree of periportal edema. � Biliary tree: Common duct is 5 mm. No significant intrahepatic biliary dilatation. � Gallbladder: Removed. � Pancreas: Partially visualized and unremarkable. � Ascites: Small amount of perihepatic ascites. � Spleen: 13. 3 cm in length.

Imaging results Chest x-ray 1/29/14 � Bilateral central perihilar and basilar opacities which are nonspecific but may reflect a combination of edema and atelectatic lung.
Case discussion Lipase and triglycerides stabilized on oral lipidlowering regimen Patient placed on low fat diet Weaned off narcotics Pain, nausea, vomiting and dyspnea resolved
Clinical Questions What are the causes of acquired and inherited lipid disorders? How do they cause pancreatitis? How is hypertriglyceridemic pancreatitis managed? Is there any relationship of hypertriglyceridemic pancreatitis to pregnancy? If so, is there a specific treatment in pregnant women?
Clinical Questions What are the causes of acquired and inherited lipid disorders? How do they cause pancreatitis? How is hypertriglyceridemic pancreatitis managed? Is there any relationship of hypertriglyceridemic pancreatitis to pregnancy? If so, is there a specific treatment in pregnant women?
Hyperlipidemia Hyperlipidemia/dysplipidemia results from abnormal levels (>90% percentile) of cholesterol OR triglycerides in the blood Inherited and acquired disorders of lipid metabolism Acquired causes of hyperlipidemia include: obesity, diabetes mellitus (especially DKA), nephrotic syndrome, hypothyroidism, pregnancy, drugs (clomiphene, mirtazapine, tamoxifen, HAART, estrogen, beta-blockers, thiazide diuretics, steroids)

Fredrickson’s classification of inherited lipid disorders Present in adulthood Fredrickson DS, Lees RS. Editorial: A system of phenotyping hyperlipoproteinemia. Circulation 1965; 31: 321 -
Hypertriglyceridemic Pancreatitis HTG: fasting serum triglyceride level of >150 mg/d. L. � mild (150 -199 mg/d. L) � moderate (200 -999 mg/d. L) � severe (1000 to 1999 mg/d. L) � very severe (>2000 mg/d. L) 3 rd most common cause of pancreatitis (~10% of all cases of acute pancreatitis and up to 56% of pancreatitis cases during pregnancy) Risk of AP in patients with serum triglycerides >1000 and >2000 mg/d. L is ∼ 5% and 10% to 20%, respectively. Speck et al. Arch Verin Wissenschaftl Heilkunde. 1865
Presentation of HTGP Similar to that of acute pancreatitis (AP) from other causes: abdominal pain, nausea, and vomiting Amylase may be falsely normal (due to high TG levels), lipase may also be unaffected Labs may also show pseudohyponatremia Poorly controlled DM, alcoholism, obesity, pregnancy, prior pancreatitis, and a personal or family history of hyperlipidemia should suggest HTGP

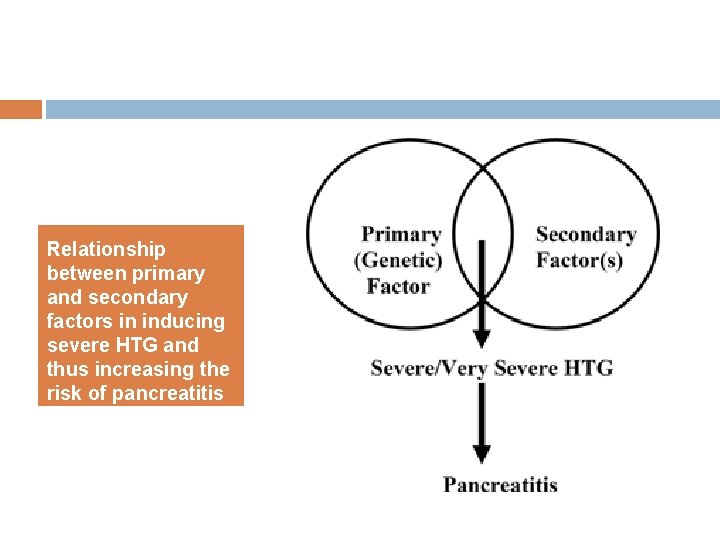
Hypertriglyceridemia-induced Pancreatitis Seen with secondary factors (ex. uncontrolled diabetes, alcoholism, medications, pregnancy) in patients with an underlying common genetic abnormality of lipoprotein metabolism (Fredrickson’s Type IIB and IV) Less commonly, patients with rare genetic abnormalities of lipoprotein metabolism (i. e. Fredrickson’s Type I and V) will develop pancreatitis without additional inciting factors. Scherer J, Singh VP, Pitchumoni CS, Yadav D. Issues in hypertriglyceridemic pancreatitis: an update. J Clin Gastroenterol. 2014 Mar; 48(3): 195 -203.
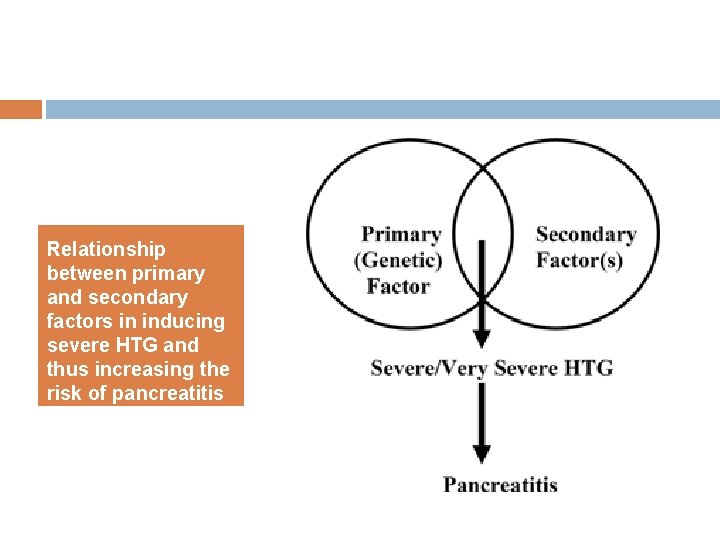
Relationship between primary and secondary factors in inducing severe HTG and thus increasing the risk of pancreatitis

Lactescent serum seen in HTG Chylomicrons: TG-rich lipoprotein particles. Present in circulation when TG > 900 mg/dl Large enough to occlude pancreatic capillaries, leading to ischemia and acinar structural alteration, and also release of pancreatic Photo adapted from Tsuang et al. Hypertriglyceridemic pancreatitis: presentation and management. Am J lipase Gastroenterology 2009 Apr; 104(4): 984 -91
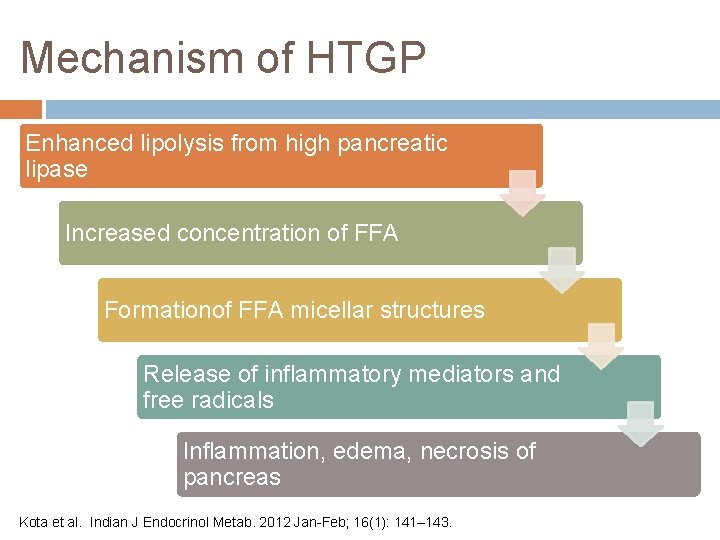
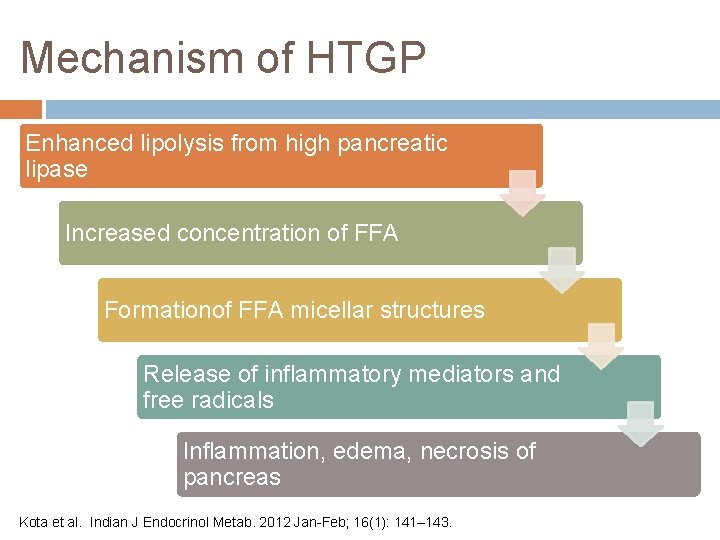
Mechanism of HTGP Enhanced lipolysis from high pancreatic lipase Increased concentration of FFA Formationof FFA micellar structures Release of inflammatory mediators and free radicals Inflammation, edema, necrosis of pancreas Kota et al. Indian J Endocrinol Metab. 2012 Jan-Feb; 16(1): 141– 143.
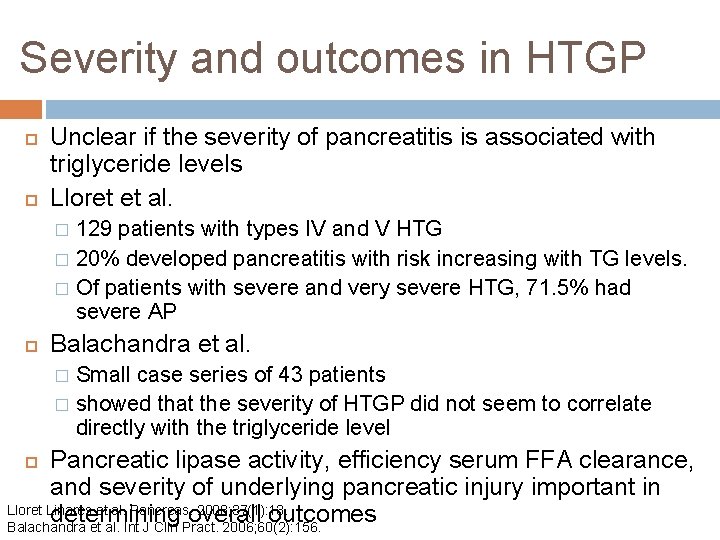
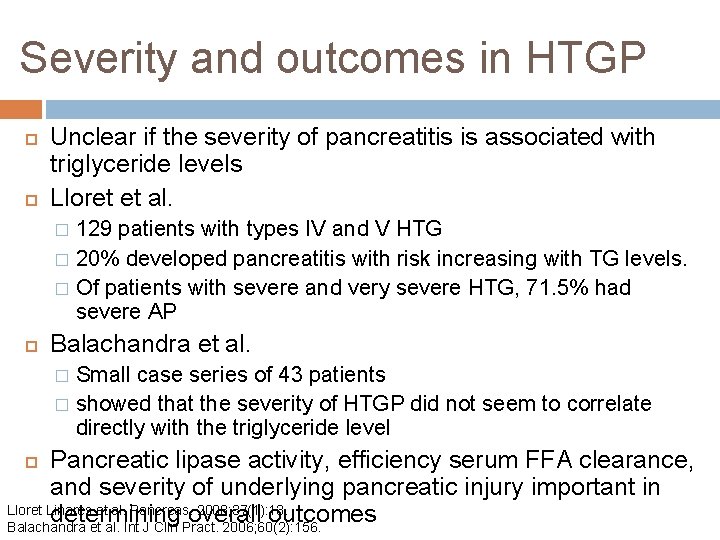
Severity and outcomes in HTGP Unclear if the severity of pancreatitis is associated with triglyceride levels Lloret et al. 129 patients with types IV and V HTG � 20% developed pancreatitis with risk increasing with TG levels. � Of patients with severe and very severe HTG, 71. 5% had severe AP � Balachandra et al. Small case series of 43 patients � showed that the severity of HTGP did not seem to correlate directly with the triglyceride level � Pancreatic lipase activity, efficiency serum FFA clearance, and severity of underlying pancreatic injury important in Lloret Linares et al. Pancreas. 2008; 37(1): 13. determining overall outcomes Balachandra et al. Int J Clin Pract. 2006; 60(2): 156.
Clinical Questions What are the causes of acquired and inherited lipid disorders? How do they cause pancreatitis? How is hypertriglyceridemic pancreatitis managed? Is there any relationship of hypertriglyceridemic pancreatitis to pregnancy? If so, is there a specific treatment in pregnant women?

Management of HTGP Conventional treatment of pancreatitis: aggressive fluid resuscitation, analgesia, bowel rest Insulin infusion Heparin Plasmapharesis Lipid lowering agents – fibrates, omega-3 fatty acids
Insulin Decreases serum TG levels by enhancing lipoprotein lipase activity Inhibits hormone-sensitive lipase in adipocytes HTGP often presents in poorly controlled diabetics and thus should be used both to manage hyperglycemia and HTG Intravenous infusion of regular insulin in D 5 at 0. 1 -0. 3 units/kg/day to maintain blood glucose 150 -200 mg/dl
Heparin Usually used in conjunction with insulin to enhance lipoprotein lipase activity One case report including 5 patients with HTGP with TG levels > 1000 showed decrease in TG levels to < 500 within 3 days in all cases with use of heparin and/or insulin Use of heparin in management of HTGP is controversial Berger et al. heparin and insulin treatment of acute pancreatitis caused by hypertriglyceridemia. Experience of 5 cases. Rev Med Chil. 2001; 129(12): 1373.

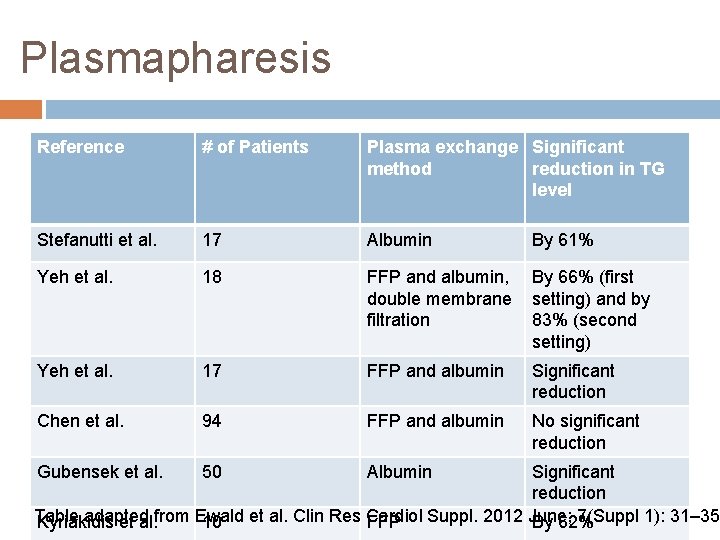
Plasmapharesis First described in 1978 by Betteridge et al. Rapidly removes plasma TG and reduces risk of recurrent pancreatitis. Also reduces inflammation by removal of excess proteases and replacement of protease inhibitors Multiple studies showing success in reducing TG levels Betteridge et al. Lancet 1978, Stefannuti et al Artif Organs. 2009 Dec, Lennertz et al. Ther Apher. 1999 Aug, Yeh et al J Clin Apher. 2003, Szczepiorkowski et al Journal of Clinical Apharesis June 2010
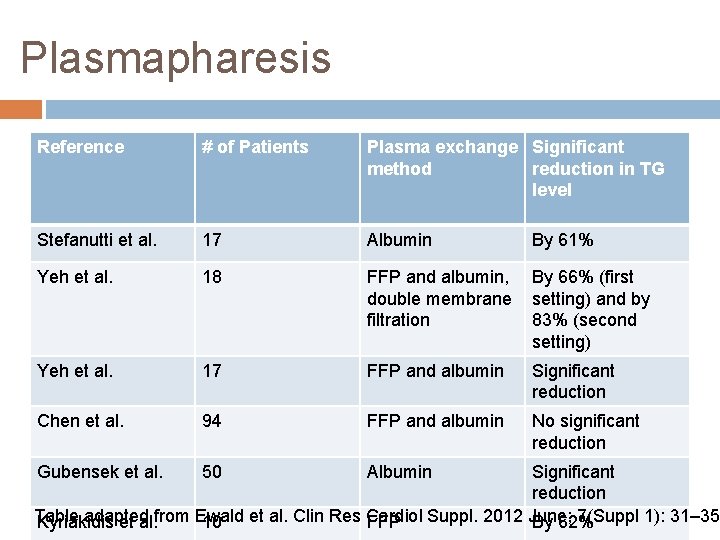
Plasmapharesis Reference # of Patients Plasma exchange Significant method reduction in TG level Stefanutti et al. 17 Albumin Yeh et al. 18 FFP and albumin, By 66% (first double membrane setting) and by filtration 83% (second setting) Yeh et al. 17 FFP and albumin Significant reduction Chen et al. 94 FFP and albumin No significant reduction Gubensek et al. 50 Albumin By 61% Significant reduction Table adapted from Ewald et al. Clin Res Cardiol Suppl. 2012 June; 7(Suppl 1): 31– 35 Kyriakidis et al. 10 FFP By 62%
Plasmapharesis Severe HTG (TG > 1000 mg/dl) and lipase > 3 times upper limit of normal result in very high FFA levels which can result in high levels of systemic inflammation Deng et al demonstrated positive correlation between high TG levels and 24 -h APACHE II score Plasmapharesis is a useful and important tool in the setting of severe HTG and significantly elevated lipase levels Deng et al. World J Gastroenterol. 2008 Jul

Other pharmacologic therapy Oral lipid lowering agents should be initiated when tolerated by the patient as adjuvant therapy in HTGP Fibrates lower TG levels by 40 -60% and raise HDL levels. Should be used as first line therapy for primary HTG Omega-3 fatty acids studied in a prospective, double-blind, placebo-controlled trial proved capable of lowering high TG (500 – 2, 000 mg / dl) by 45 % Tsuang et al. Hypertriglyceridemic pancreatitis: presentation and management. Am J Gastroenterology 2009 Apr; 104(4): 984 -91
Clinical Questions What are the causes of acquired and inherited lipid disorders? How do they cause pancreatitis? How is hypertriglyceridemic pancreatitis managed? Is there any relationship of hypertriglyceridemic pancreatitis to pregnancy? If so, is there a specific treatment in pregnant women?
Pregnancy and HTGP Lipid profile changes in normal pregnancy: marked elevations of total plasma cholesterol and triglyceride levels, primarily through increased liver synthesis of triglyceride and VLDL -C in response to elevated estrogen levels Pregnancy causes an increase in serum TG (peaks in 3 rd trimester) but total serum TG rarely exceeds 300 mg/dl – a concentration that is not sufficient to cause pancreatitis

Pregnancy and HTGP Responsible for ~56% of cases of AP occurring during pregnancy with an estimated overall frequency of 1 in 6790 pregnancies over a 15 year period Most causes of HTGP in pregnancy are attributable to familial HTG however non-genetic, non-familial pregnancy-induced HTGP has been reported Several case reports describe gestational HTGP in patients with underlying hyperchylomicronemia Gursoy et al. Severe Hypertriglyceridemia-Induced Pancreatitis during Pregnancy. Journal of the National Medical Association. VOL. 98, NO. 4, APRIL 2006
Management of HTGP in pregnancy Treatment generally does not differ in pregnancy Case reports have shown success of apharesis in management of HTGP in pregnancy Initiation of fibrates and omega-3 fatty acids reduce risk of recurrent pancreatitis Dietary fat restriction also reduces chance of recurrence of HTGP Achard et al. Pancreatitis related to severe acute hypertriglyceridemia during pregnancy: treatment with lipoprotein apheresis. Intensive Care Med. 1991; 17(4): 236.
Complications of HTGP in pregnancy Some reports suggest up to 20% increased mortality in pregnancies complicated by pancreatitis One of the most common reasons for maternal and fetal mortality are acute pancreatitis itself Very rarely, acute pancreatitis associated with preeclampsia-eclampsia or HELLP syndrome No guidelines exist about the need for early delivery in patients with acute pancreatitis
Conclusion Both inherited and acquired causes of hyperlipidemia HTGP usually multifactorial (underlying lipid disorder exacerbated by secondary factor) Pregnancy itself can cause hypertriglyceridemia Several management strategies for HTGP including plasmapharesis, insulin infusion and oral therapy. Management is similar in pregnant patients Important to recognize this disorder early in pregnant patient to improve overall outcomes

THANK YOU!

References Sunil K. Kota, Siva K. Kota, Sruti Jammula, S. V. S. Krishna, and Kirtikumar D. Modi. Hypertriglyceridemia-induced recurrent acute pancreatitis: a case-based review. Indian J Endocrinol Metab. 2012 Jan-Feb; 16(1): 141– 143. Srinivasa P Munigoti, Alan Rees. Hypertriglyceridaemia, LPL Deficiency and Pancreatitis. British Journal of Diabetes and Vascular Disease. 2011; 11(3): 107 -112. Betteridge DJ, Bakowski M, Taylor KG, Reckless JP, de Silva SR, Galton DJ. Treatment of severe diabetic hypertriglyceridaemia by plasma exchange. Lancet. 1978 Jun 24; 1(8078): 1368. Iskandar SB, Olive KE. Plasmapheresis as an adjuvant therapy for hypertriglyceridemia-induced pancreatitis. Am J Med Sci. 2004 Nov; 328(5): 290 -4. Stefanutti C, Di Giacomo S, Vivenzio A, Labbadia G, Mazza F, D'Alessandri G, Russi G, De Silvestro G, Marson P. Therapeutic plasma exchange in patients with severe hypertriglyceridemia: a multicenter study. Artif Organs. 2009 Dec; 33(12): 1096 -102. Lennertz A, Parhofer KG, Samtleben W, Bosch T. Therapeutic plasma exchange in patients with chylomicronemia syndrome complicated by acute pancreatitis. Ther Apher. 1999 Aug; 3(3): 227 -33. Yeh JH, Chen JH, Chiu HC. Plasmapheresis for hyperlipidemic pancreatitis. J Clin Apher. 2003; 18(4): 181 -5. Yeh JH, Lee MF, Chiu HC. Plasmapheresis for severe lipemia: comparison of serum-lipid clearance rates for the plasmaexchange and double-filtration variants. J Clin Apher. 2003; 18(1): 32 -6. Gubensek J, Buturović-Ponikvar J, Marn-Pernat A, Kovac J, Knap B, Premru V, Ponikvar R. Treatment of hyperlipidemic acute pancreatitis with plasma exchange: a single-center experience. Ther Apher Dial. 2009; 13(4): 314– 317. Chen JH, Yeh JH, Lai HW, Liao CS. Therapeutic plasma exchange in patients with hyperlipidemic pancreatitis. World J Gastroenterol. 2004; 10(15): 2272– 2274. Ewald N, Kloer HU. Treatment options for severe hypertriglyceridemia (SHTG): the role of apheresis. Clin Res Cardiol Suppl. 2012 Jun; 7(Suppl 1): 31 -5. Deng LH, Xue P, Xia Q, Yang XN, Wan MH. Effect of admission hypertriglyceridemia on the episodes of severe acute pancreatitis. World J Gastroenterol. 2008 Jul; 14(28): 4558 -61. Speck L. Fall von lipamia. Arch Verin Wissenschaftl Heilkunde. 1865: 1: 232. Quoated in Thannhauser SJ, Ed. Lipidoses, disease of intracellular lipid metabolism, 1958, 3 rd ed. New York, Grune & Stratton, 307.
References Lloret Linares C, Pelletier AL, Czernichow S, Vergnaud AC, Bonnefont. Rousselot D, Levy P, Ruszniewski P, Bruckert E. Acute pancreatitis in a cohort of 129 patients referred for severe hypertriglyceridemia. Pancreas. 2008; 37(1): 13. Balachandra S, Virlos IT, King NK, Siriwardana HP, France MW, Siriwardena AK. Hyperlipidaemia and outcome in acute pancreatitis. Int J Clin Pract. 2006; 60(2): 156. Berger Z, Quera R, Poniachik J, Oksenberg D, Guerrero J. [heparin and insulin treatment of acute pancreatitis caused by hypertriglyceridemia. Experience of 5 cases]. Rev Med Chil. 2001; 129(12): 1373. Tsuang W, Navaneethan U, Ruiz L, Palascak JB, Gelrud A. Hypertriglyceridemic pancreatitis: presentation and management. Am J Gastroenterol. 2009 Apr; 104(4): 984 -91. doi: 10. 1038/ajg. 2009. 27. Epub 2009 Mar 17. Achard JM, Westeel PF, Moriniere P, Lalau JD, de Cagny B, Fournier A. Pancreatitis related to severe acute hypertriglyceridemia during pregnancy: treatment with lipoprotein apheresis. Intensive Care Med. 1991; 17(4): 236.
 Richa shukla pregnant
Richa shukla pregnant Richa shukla pregnant
Richa shukla pregnant Rekha shukla joint secretary
Rekha shukla joint secretary Dr bk shukla
Dr bk shukla Ruchi shukla ukraine
Ruchi shukla ukraine Jagadish shukla
Jagadish shukla Amol shukla
Amol shukla Dr richa goyal
Dr richa goyal Dr shaleen agarwal
Dr shaleen agarwal Richa rai
Richa rai Reservoir system
Reservoir system Qualities of a good mentor
Qualities of a good mentor Qualities of a good mentor
Qualities of a good mentor Whirlpool archetype examples
Whirlpool archetype examples Object mentor
Object mentor Invitation to notice mentor sentences
Invitation to notice mentor sentences Harvard spark program
Harvard spark program Mentor homme
Mentor homme što prikazuje radionički crtež
što prikazuje radionički crtež Georgia parent mentor partnership
Georgia parent mentor partnership Kartu bimbingan aktualisasi mentor
Kartu bimbingan aktualisasi mentor What does a mentor do
What does a mentor do Supernova mentor
Supernova mentor Mentor
Mentor Mentor circle
Mentor circle Mentor and mentee roles and responsibilities
Mentor and mentee roles and responsibilities Mentor mentee meeting agenda
Mentor mentee meeting agenda Mentor design capture
Mentor design capture Sd doe mentoring
Sd doe mentoring Mentor consulting
Mentor consulting Infomentorhub
Infomentorhub Shrek tests allies and enemies
Shrek tests allies and enemies Mentor foundation
Mentor foundation Juliet's servant and mentor
Juliet's servant and mentor Mentor h10
Mentor h10 Mulan hero's journey
Mulan hero's journey Uconn mentor connection
Uconn mentor connection Objectmentor
Objectmentor Wiesel mentor
Wiesel mentor Mentor pupil relationship archetype examples
Mentor pupil relationship archetype examples Asce mentor match
Asce mentor match