OSTEOPOROSIS IN MEN H Delshad M D Endocrinologist







- Slides: 61

OSTEOPOROSIS IN MEN H. Delshad M. D Endocrinologist Research Institute for Endocrine Sciences Shahid Beheshti University of Medical Sciences
Osteoporosis in Men Agenda : • Disease definition • Epidemiology • Burden • Pathophysiology • Diagnosis • Management
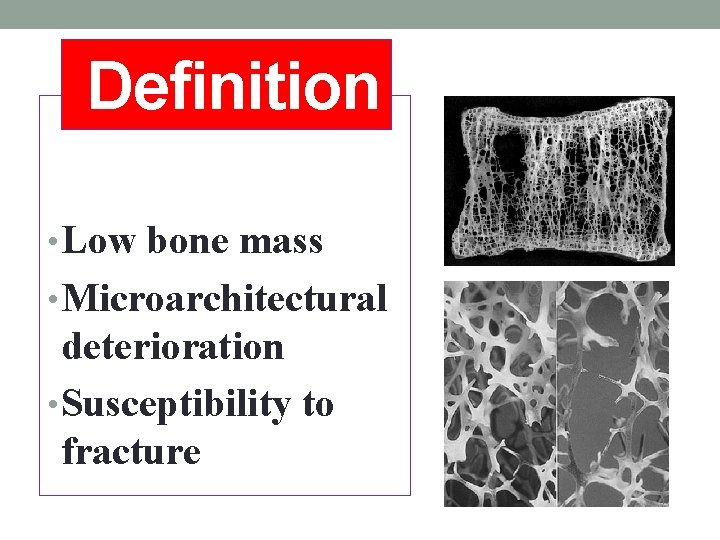
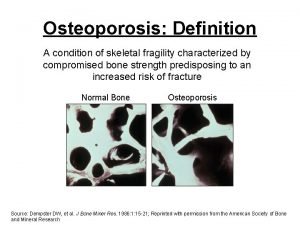
Definition • Low bone mass • Microarchitectural deterioration • Susceptibility to fracture
Epidemiology • Osteoporosis affects women more often than men • Osteoporosis affects a significant number of men, often goes undetected. • 20% of the 44 million Americans with osteoporosis or low BMD, are men( NHANES-III). • Between 30 -40% of osteoporotic Fx occur in men. • The lifetime risk of Fx for men aged> 50 is 13 -30%. • By the age 90, one of every 6 men will have a hip Fx.
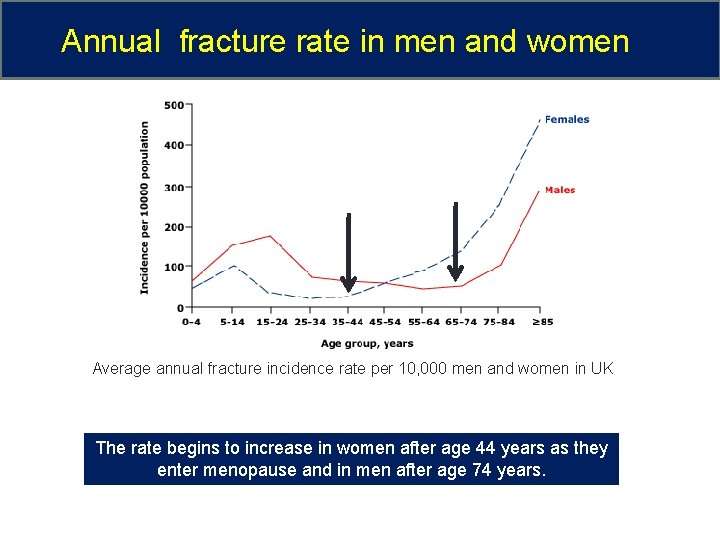
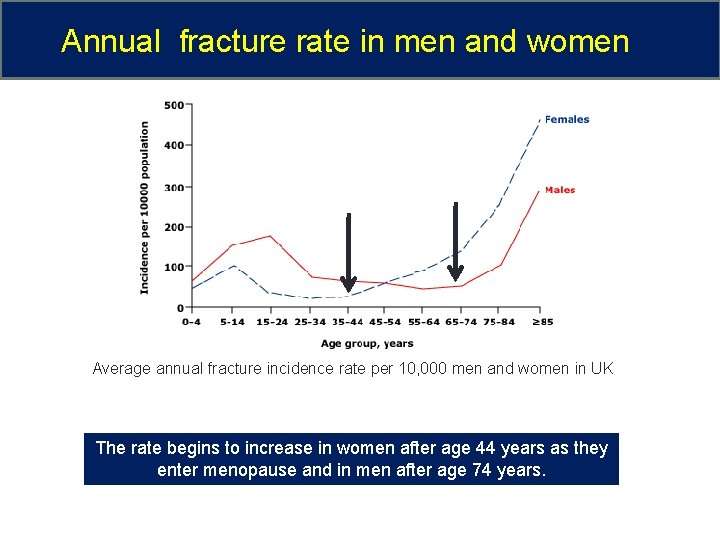
Annual fracture rate in men and women Average annual fracture incidence rate per 10, 000 men and women in UK The rate begins to increase in women after age 44 years as they enter menopause and in men after age 74 years.
Epidemiology • The incidence of osteoporotic Fx in men: - Highest rates in Northern Europe & North America - Lowest rates in Black & Asian • Ratio of hip Fx between women and men: - Caucasians = 3 -4/1 - Asia = 1 / 1 • In Iranian population: 5 -20%
Osteoporosis : Burden • The most common bone disease in humans. • Is a risk factor for Fx just as HTN is for stroke. • Osteoporosis can exist undetected for a long time. • It is a preventable and treatable disease. • Cost : $21, 000 /hip Fx • Cost of treating hip Fx worldwide in 2050 will be $31. 5 billion
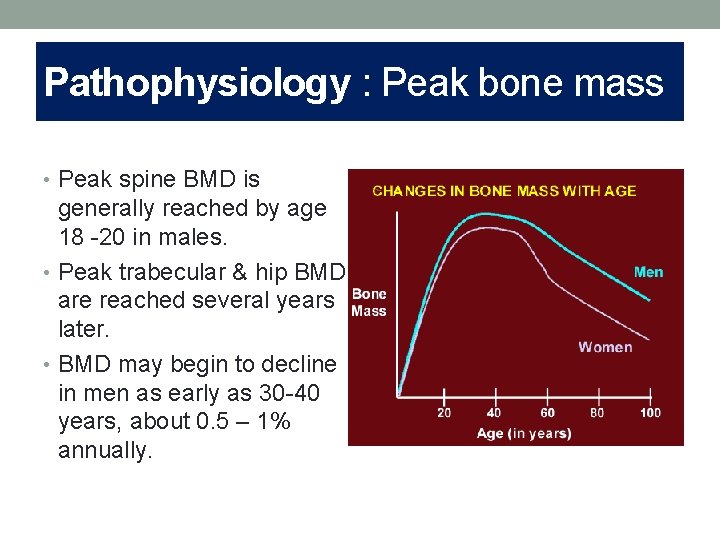
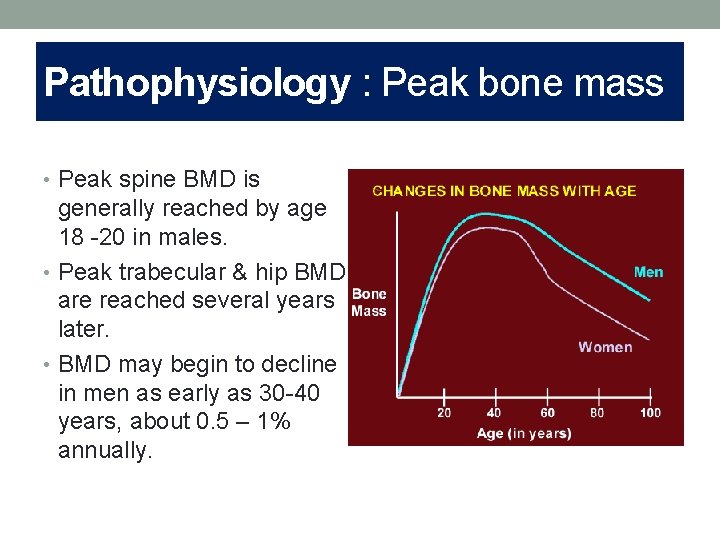
Pathophysiology : Peak bone mass • Peak spine BMD is generally reached by age 18 -20 in males. • Peak trabecular & hip BMD are reached several years later. • BMD may begin to decline in men as early as 30 -40 years, about 0. 5 – 1% annually.
Peak Bone Mass Determinants • Genetics : account for 60% of the variance in bone mass, so far 80 genetic loci have been identified that influence peak bone mass. • Ethnic variation : African Americans have highest BMD & Asian Americans have lower BMD than whites. • Environmental factors: Physical activity, Poor growth, Delayed maturation, Muscle deficits, Chronic inflammations, Glucocorticoids • Old age : the balance between bone formation and resorptione becomes progressively negative with advancing age.
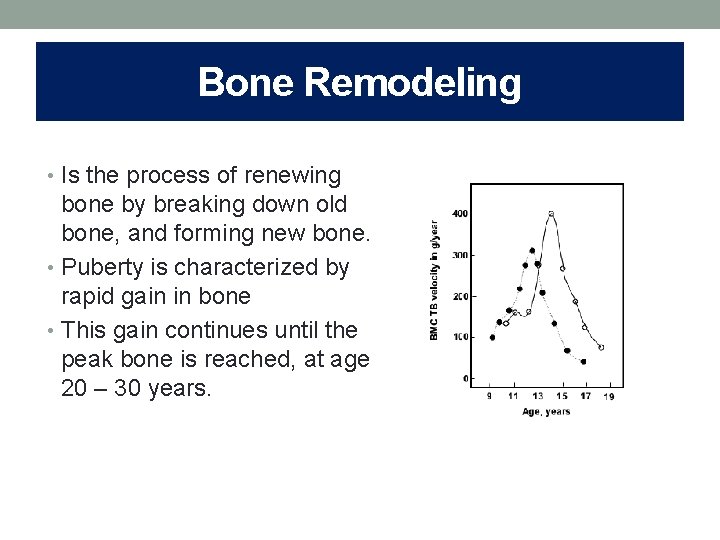
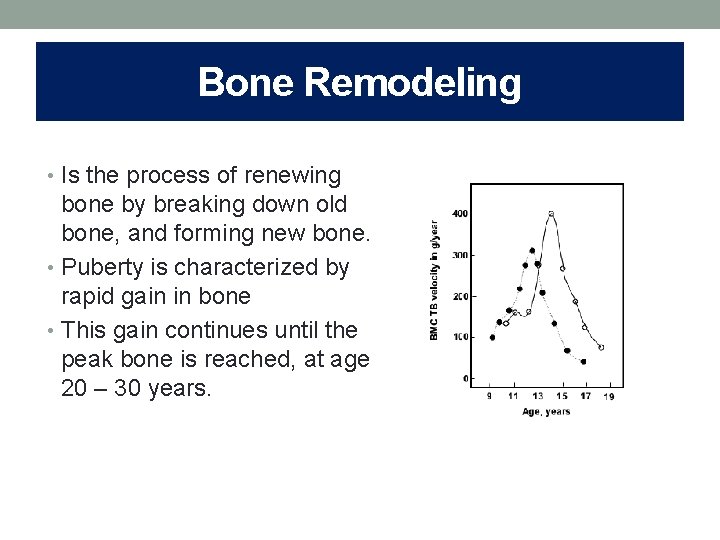
Bone Remodeling • Is the process of renewing bone by breaking down old bone, and forming new bone. • Puberty is characterized by rapid gain in bone • This gain continues until the peak bone is reached, at age 20 – 30 years.
Bone Remodeling In women: ● After peak bone mass, the bone remodeling process is in a state of equilibrium until menopause. ● Low estrogen Rapid bone loss 2 – 3 % per year in the spine for 6 -8 years then 0. 5 % per year In men: ● Bone gain accelerates during adolescence and peak bone mass is reached a little later. ● There is no period of dramatic & accelerated bone loss. ● There is a steady decline of bone mass.
Conclusions ● Men, s bones are larger and the cortices is thicker (Androgen dependent) ● Greater muscle strength and physical activity are associated with greater bone mass in men. ● In general , clear differences in the bone structure of men and women protect men from osteoporosis. ● Most men develop secondary osteoporosis.
Sex steroids • Sex steroids play an important role in both peak bone mass acquisition and age related bone loss. • Numerous epidemiologic studies have examined association between gonadal steroids and BMD or Fx. • These studies suggest that E 2 and Androgens play important roles in establishing and maintaining bone mass in men.
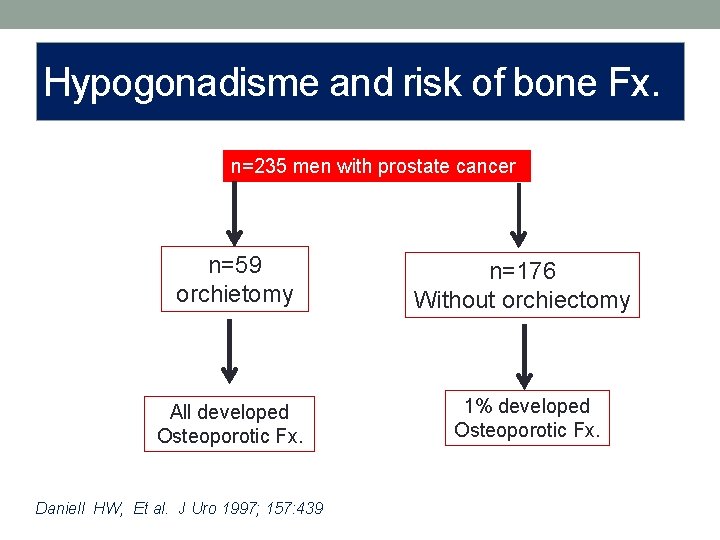
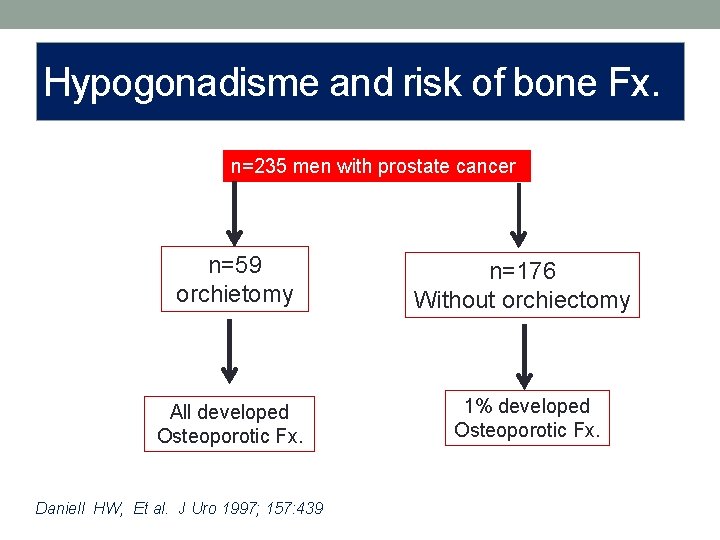
Hypogonadisme and risk of bone Fx. n=235 men with prostate cancer n=59 orchietomy n=176 Without orchiectomy All developed Osteoporotic Fx. 1% developed Osteoporotic Fx. Daniell HW, Et al. J Uro 1997; 157: 439
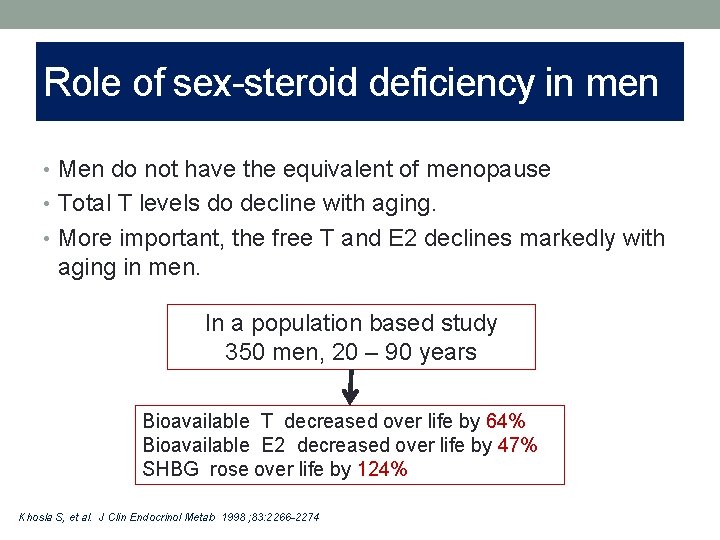
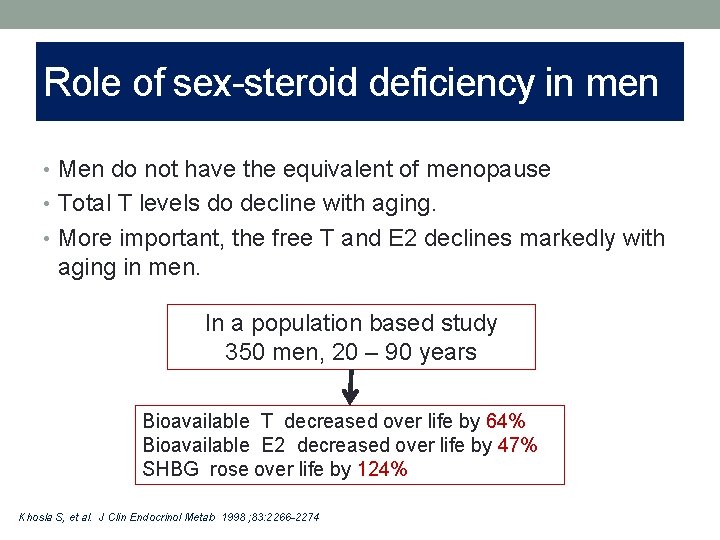
Role of sex-steroid deficiency in men • Men do not have the equivalent of menopause • Total T levels do decline with aging. • More important, the free T and E 2 declines markedly with aging in men. In a population based study 350 men, 20 – 90 years Bioavailable T decreased over life by 64% Bioavailable E 2 decreased over life by 47% SHBG rose over life by 124% Khosla S, et al. J Clin Endocrinol Metab 1998 ; 83: 2266 -2274
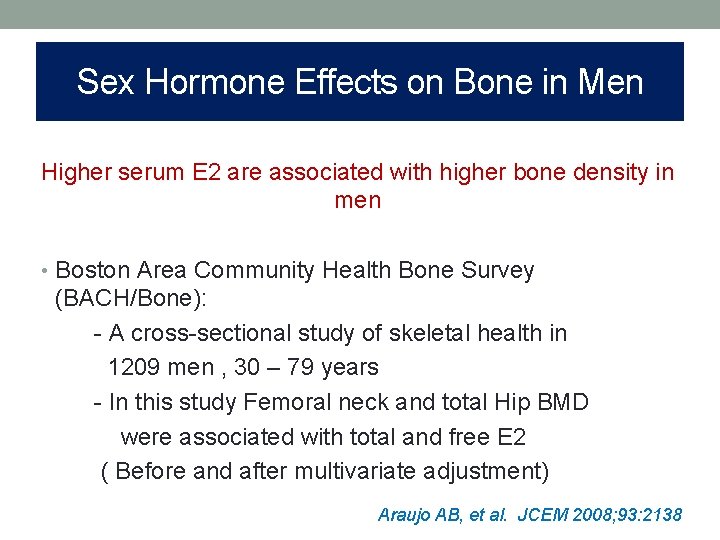
Sex Hormone Effects on Bone in Men Higher serum E 2 are associated with higher bone density in men • Boston Area Community Health Bone Survey (BACH/Bone): - A cross-sectional study of skeletal health in 1209 men , 30 – 79 years - In this study Femoral neck and total Hip BMD were associated with total and free E 2 ( Before and after multivariate adjustment) Araujo AB, et al. JCEM 2008; 93: 2138
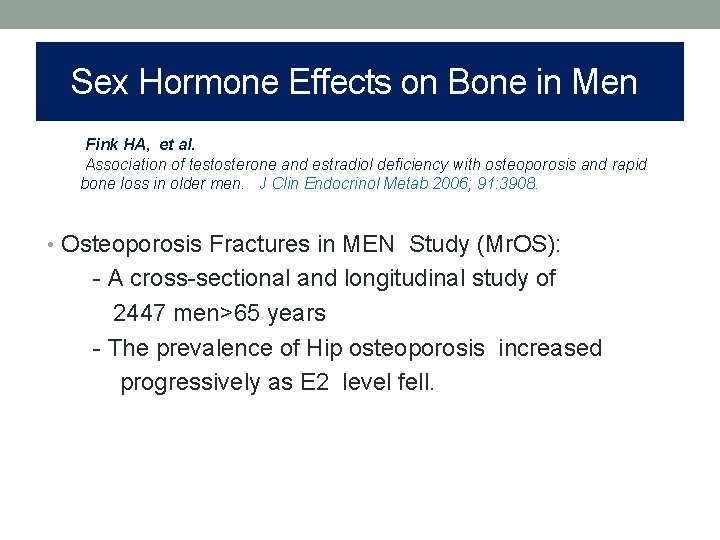
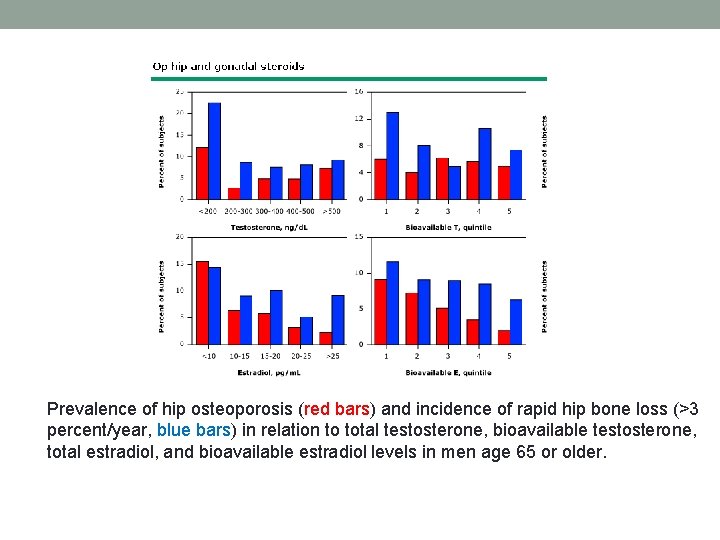
Sex Hormone Effects on Bone in Men Fink HA, et al. Association of testosterone and estradiol deficiency with osteoporosis and rapid bone loss in older men. J Clin Endocrinol Metab 2006; 91: 3908. • Osteoporosis Fractures in MEN Study (Mr. OS): - A cross-sectional and longitudinal study of 2447 men>65 years - The prevalence of Hip osteoporosis increased progressively as E 2 level fell.
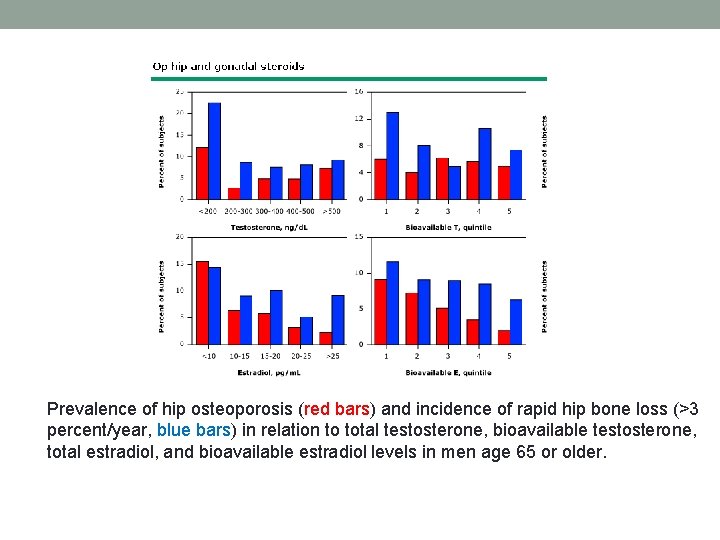
Prevalence of hip osteoporosis (red bars) and incidence of rapid hip bone loss (>3 percent/year, blue bars) in relation to total testosterone, bioavailable testosterone, total estradiol, and bioavailable estradiol levels in men age 65 or older.
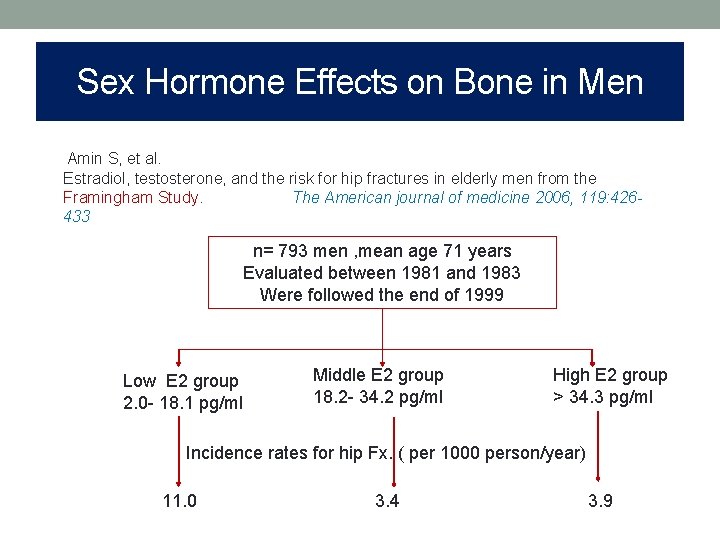
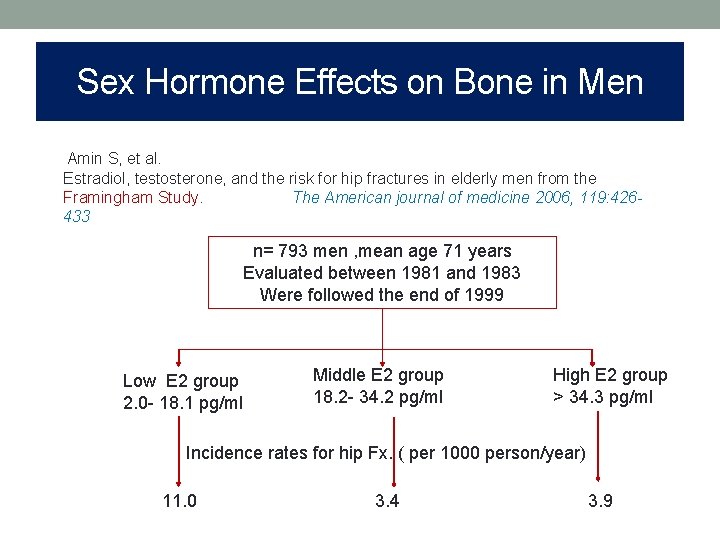
Sex Hormone Effects on Bone in Men Amin S, et al. Estradiol, testosterone, and the risk for hip fractures in elderly men from the Framingham Study. The American journal of medicine 2006, 119: 426433 n= 793 men , mean age 71 years Evaluated between 1981 and 1983 Were followed the end of 1999 Low E 2 group 2. 0 - 18. 1 pg/ml Middle E 2 group 18. 2 - 34. 2 pg/ml High E 2 group > 34. 3 pg/ml Incidence rates for hip Fx. ( per 1000 person/year) 11. 0 3. 4 3. 9
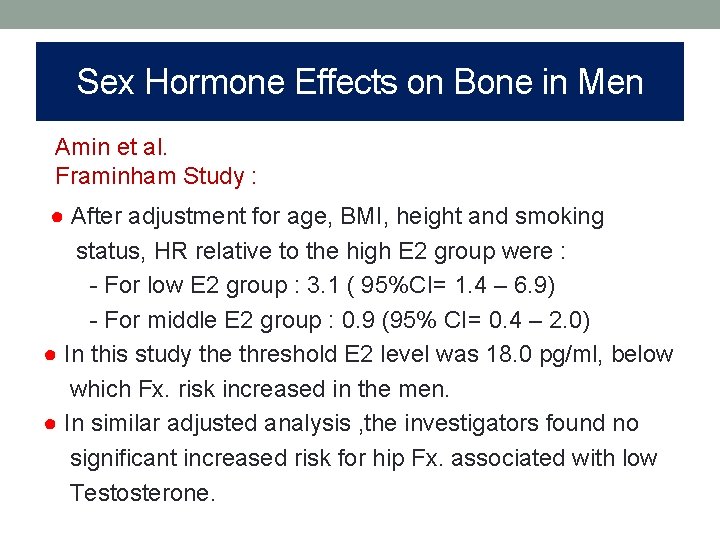
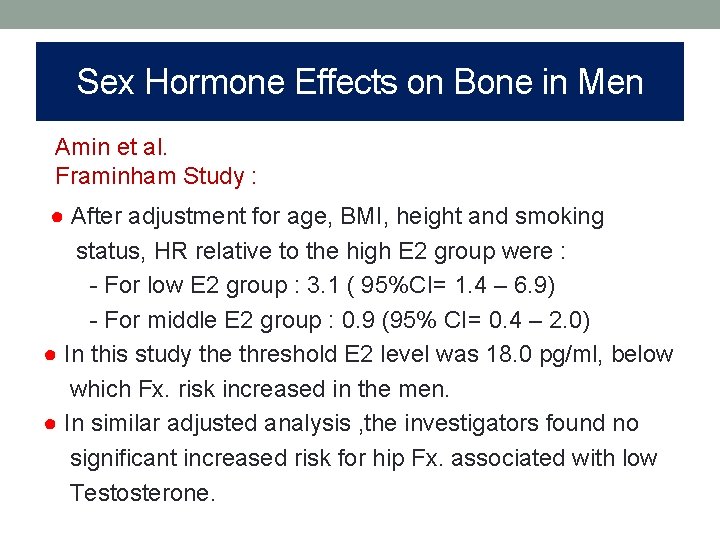
Sex Hormone Effects on Bone in Men Amin et al. Framinham Study : ● After adjustment for age, BMI, height and smoking status, HR relative to the high E 2 group were : - For low E 2 group : 3. 1 ( 95%CI= 1. 4 – 6. 9) - For middle E 2 group : 0. 9 (95% CI= 0. 4 – 2. 0) ● In this study the threshold E 2 level was 18. 0 pg/ml, below which Fx. risk increased in the men. ● In similar adjusted analysis , the investigators found no significant increased risk for hip Fx. associated with low Testosterone.
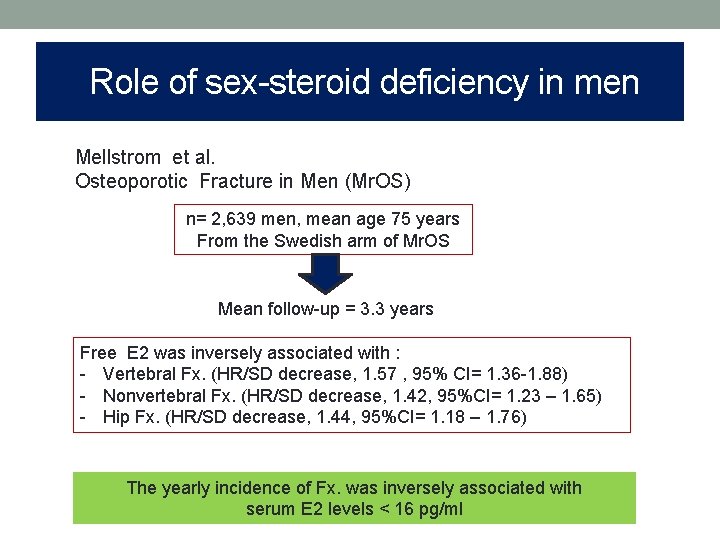
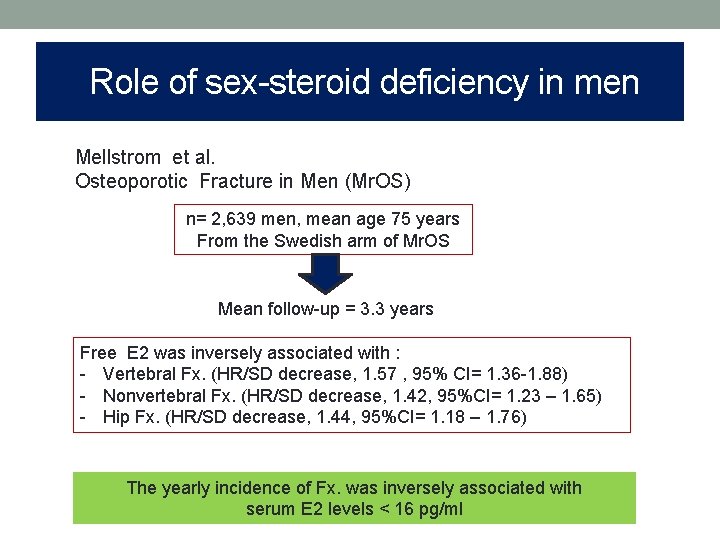
Role of sex-steroid deficiency in men Mellstrom et al. Osteoporotic Fracture in Men (Mr. OS) n= 2, 639 men, mean age 75 years From the Swedish arm of Mr. OS Mean follow-up = 3. 3 years Free E 2 was inversely associated with : - Vertebral Fx. (HR/SD decrease, 1. 57 , 95% CI= 1. 36 -1. 88) - Nonvertebral Fx. (HR/SD decrease, 1. 42, 95%CI= 1. 23 – 1. 65) - Hip Fx. (HR/SD decrease, 1. 44, 95%CI= 1. 18 – 1. 76) The yearly incidence of Fx. was inversely associated with serum E 2 levels < 16 pg/ml
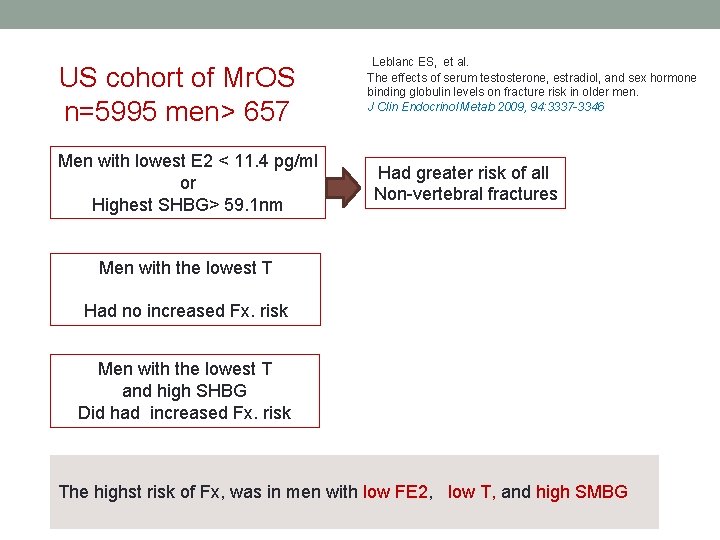
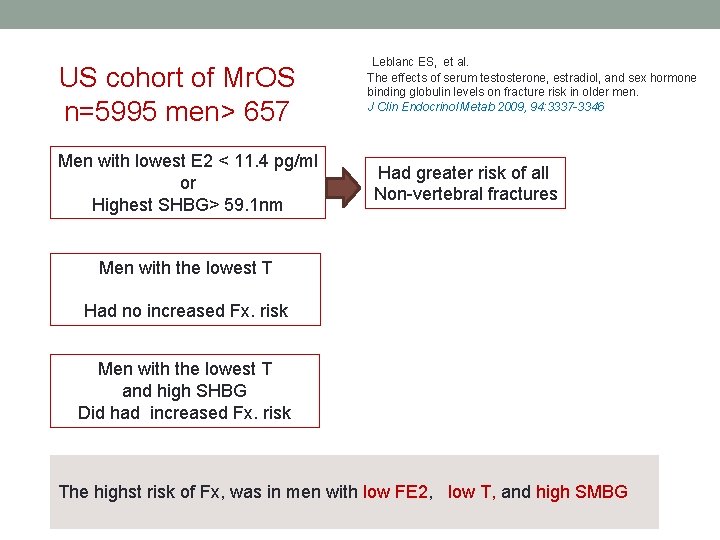
US cohort of Mr. OS n=5995 men> 657 Men with lowest E 2 < 11. 4 pg/ml or Highest SHBG> 59. 1 nm Leblanc ES, et al. The effects of serum testosterone, estradiol, and sex hormone binding globulin levels on fracture risk in older men. J Clin Endocrinol Metab 2009, 94: 3337 -3346 Had greater risk of all Non-vertebral fractures Men with the lowest T Had no increased Fx. risk Men with the lowest T and high SHBG Did had increased Fx. risk The highst risk of Fx, was in men with low FE 2, low T, and high SMBG
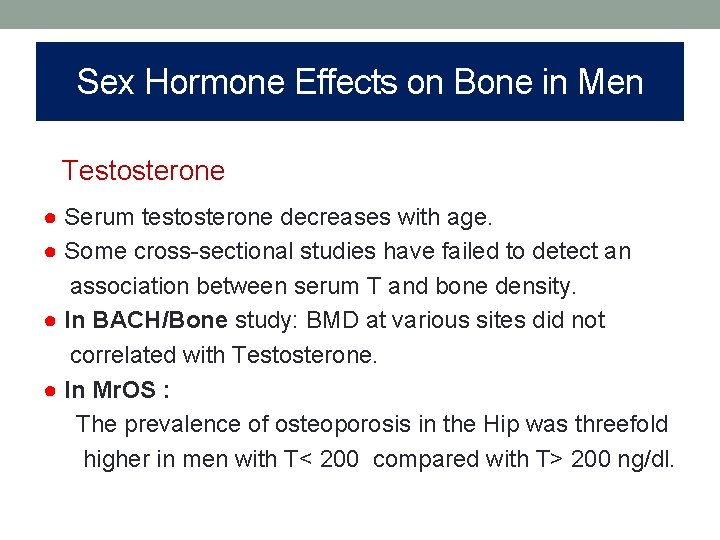
Sex Hormone Effects on Bone in Men Testosterone ● Serum testosterone decreases with age. ● Some cross-sectional studies have failed to detect an association between serum T and bone density. ● In BACH/Bone study: BMD at various sites did not correlated with Testosterone. ● In Mr. OS : The prevalence of osteoporosis in the Hip was threefold higher in men with T< 200 compared with T> 200 ng/dl.
Sex Hormone Effects on Bone in Men Conclusion: ● It is uncertain how much of the osteoporosis in older men results from aging as opposed to sex steroid deficiency. ● Of the hormonal component how much is due to true E 2 Vs androgen deficiency. ● E 2 has a key role in determining Fx. Risk in aging men. ● Testosterone may also contribute to Fx. Risk, particularly in the setting of high SHBG. ● It is probable a significant component of the Testosterone effect or risk of Fx. Is mediated by non-skeletal effects.
Osteoporosis: Diagnosis Osteoporosis: • Clinically asymptomatic • Until there is a fracture • Many Ver. Fxs. : asymptomatic • May be diagnosed incidentally in X-Rays • Pain and height loss
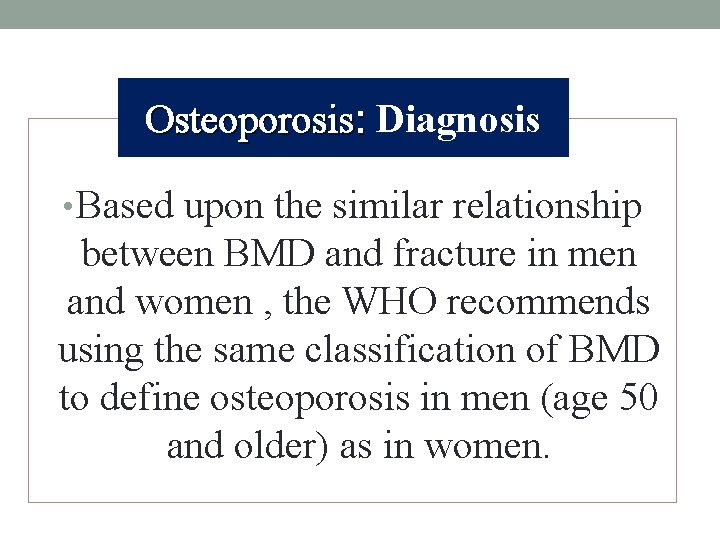
Osteoporosis: Diagnosis • Based upon the similar relationship between BMD and fracture in men and women , the WHO recommends using the same classification of BMD to define osteoporosis in men (age 50 and older) as in women.
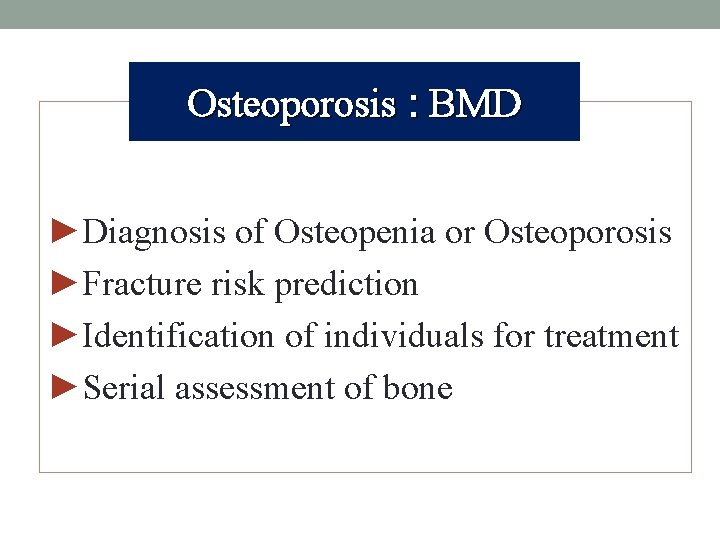
Osteoporosis : BMD ►Diagnosis of Osteopenia or Osteoporosis ►Fracture risk prediction ►Identification of individuals for treatment ►Serial assessment of bone mass
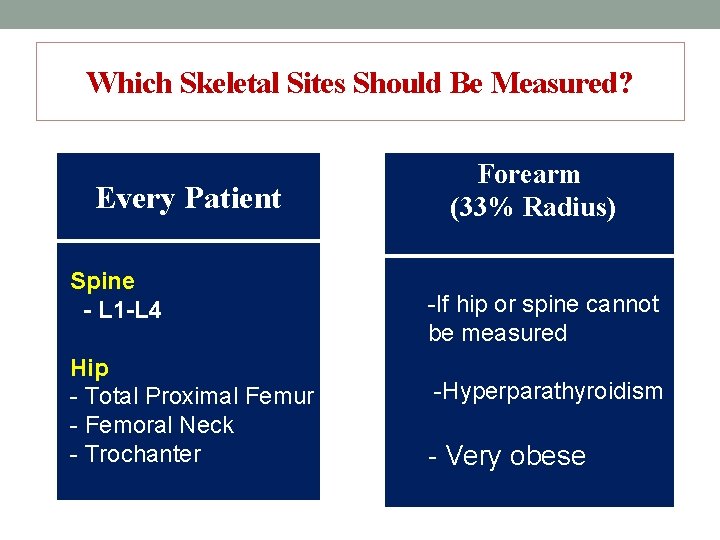
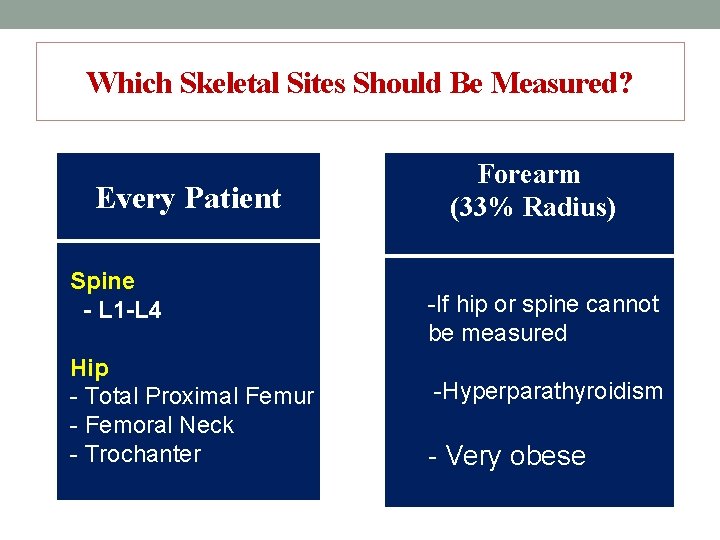
Which Skeletal Sites Should Be Measured? Every Patient Spine - L 1 -L 4 Hip - Total Proximal Femur - Femoral Neck - Trochanter Forearm (33% Radius) -If hip or spine cannot be measured -Hyperparathyroidism - Very obese
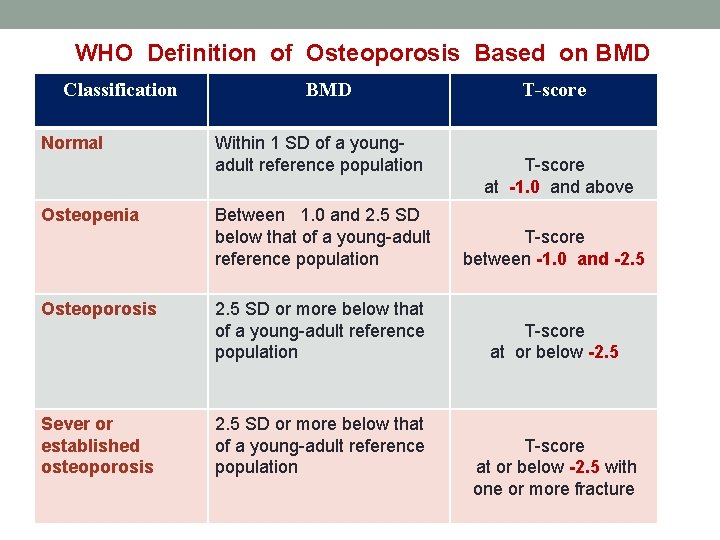
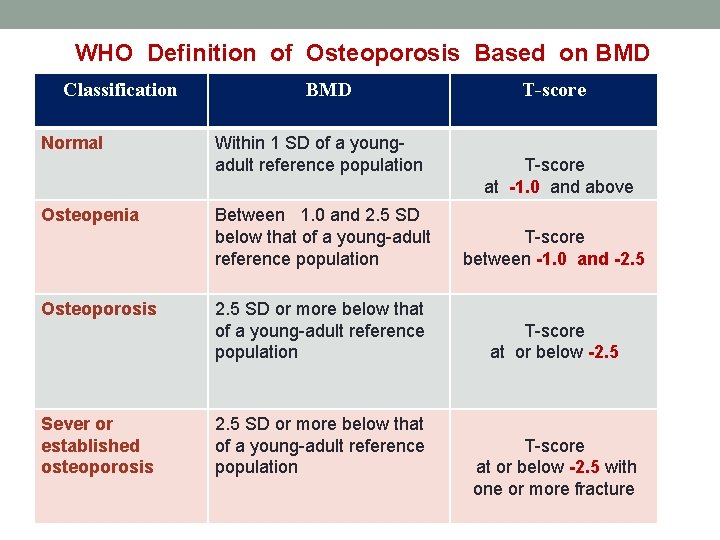
WHO Definition of Osteoporosis Based on BMD Classification Normal Osteopenia Osteoporosis Sever or established osteoporosis BMD Within 1 SD of a youngadult reference population T-score at -1. 0 and above Between 1. 0 and 2. 5 SD below that of a young-adult reference population T-score between -1. 0 and -2. 5 SD or more below that of a young-adult reference population T-score at or below -2. 5 with one or more fracture
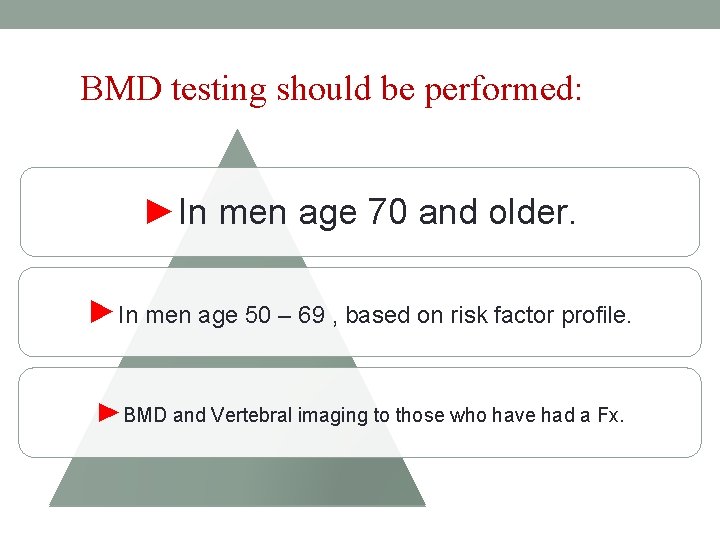
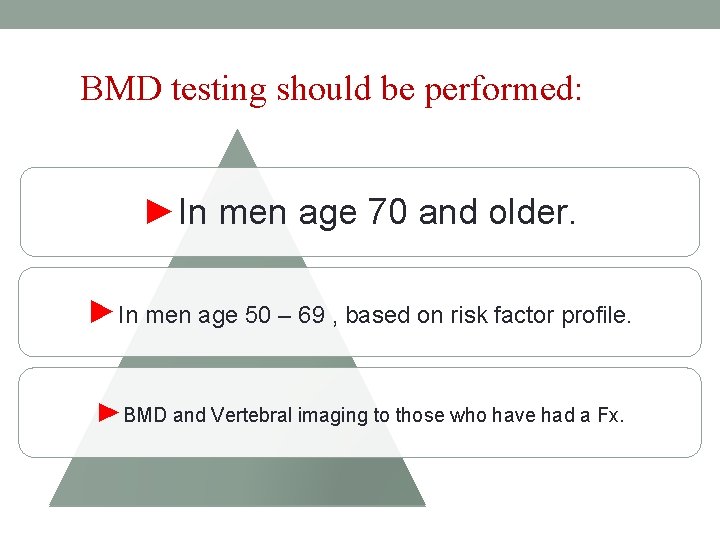
BMD testing should be performed: ►In men age 70 and older. ►In men age 50 – 69 , based on risk factor profile. ►BMD and Vertebral imaging to those who have had a Fx.
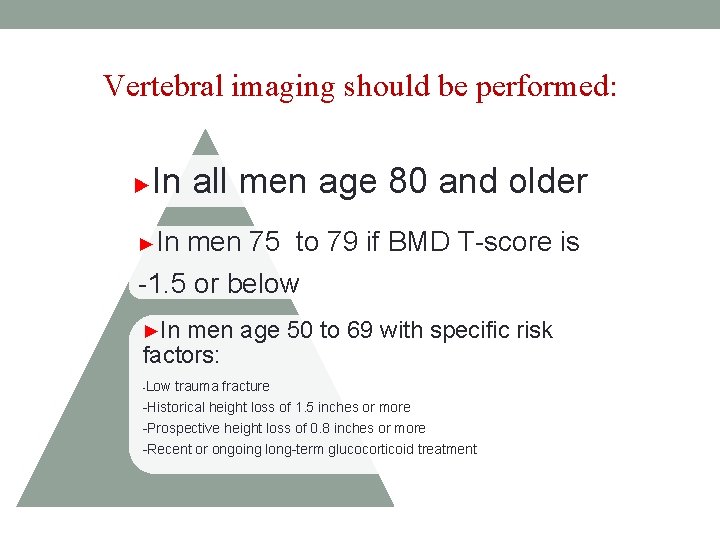
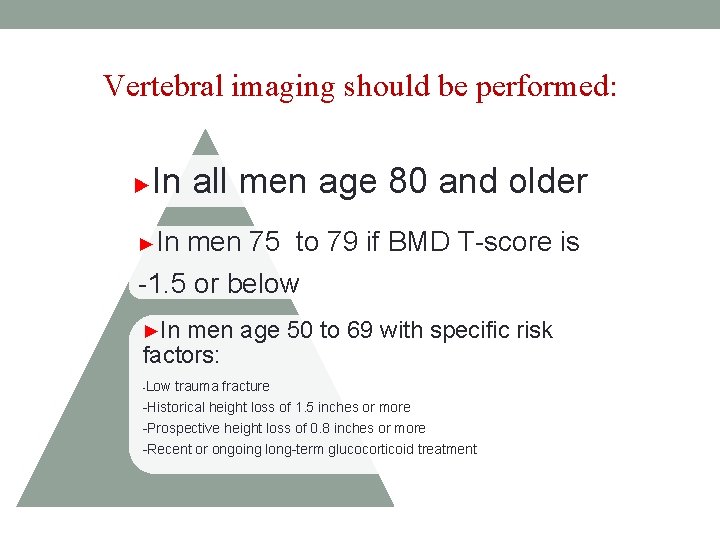
Vertebral imaging should be performed: ► In all men age 80 and older ►In men 75 to 79 if BMD T-score is -1. 5 or below ►In men age 50 to 69 with specific risk factors: -Low trauma fracture -Historical height loss of 1. 5 inches or more -Prospective height loss of 0. 8 inches or more -Recent or ongoing long-term glucocorticoid treatment
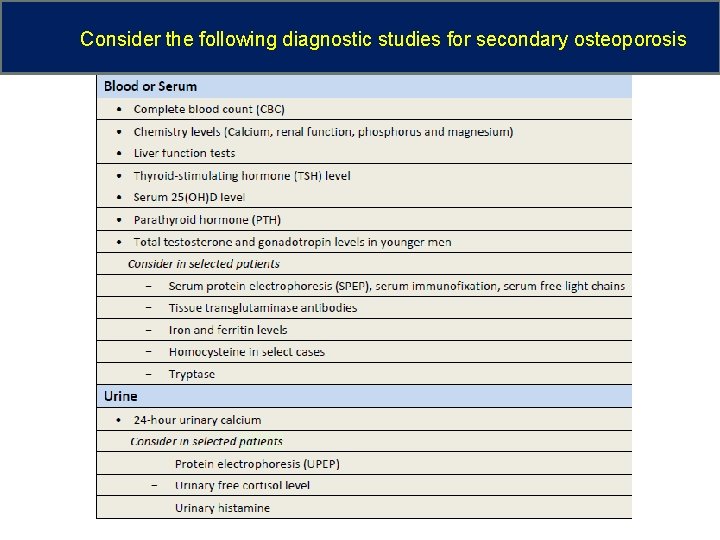
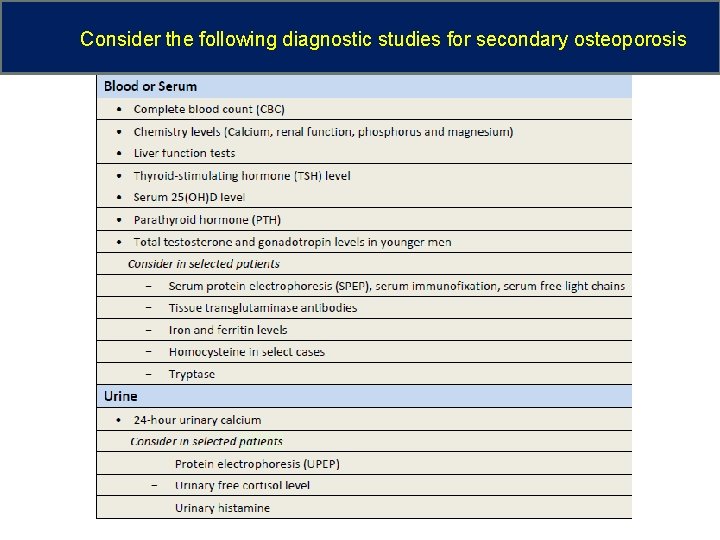
Consider the following diagnostic studies for secondary osteoporosis
OSTEOPOROSIS TREATMENT
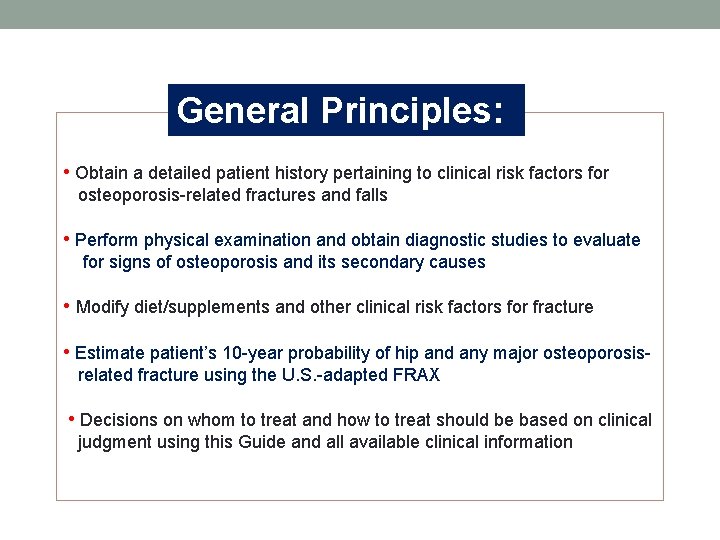
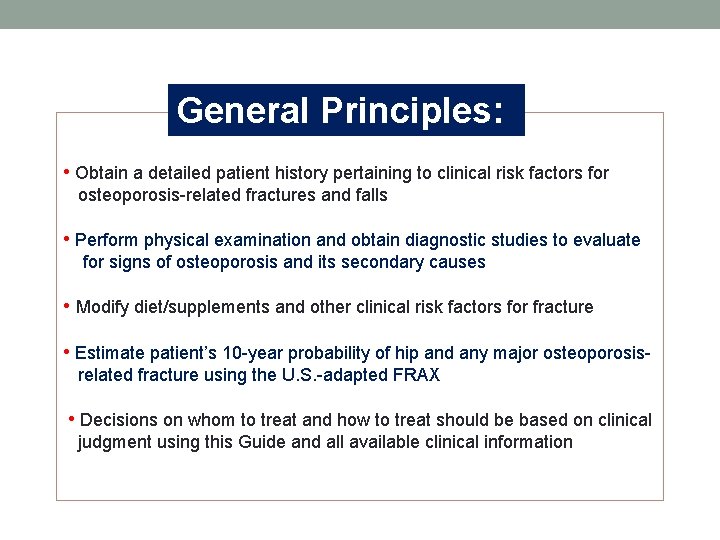
General Principles: • Obtain a detailed patient history pertaining to clinical risk factors for osteoporosis-related fractures and falls • Perform physical examination and obtain diagnostic studies to evaluate for signs of osteoporosis and its secondary causes • Modify diet/supplements and other clinical risk factors for fracture • Estimate patient’s 10 -year probability of hip and any major osteoporosisrelated fracture using the U. S. -adapted FRAX • Decisions on whom to treat and how to treat should be based on clinical judgment using this Guide and all available clinical information
Identifying those at high risk All postmenopausal women and men over 50 years of age should be assessed for the presence of risk factors for osteoporosis.
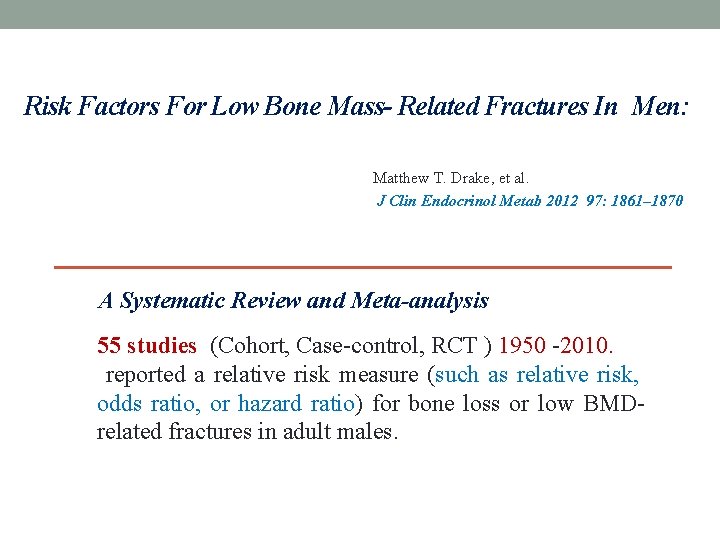
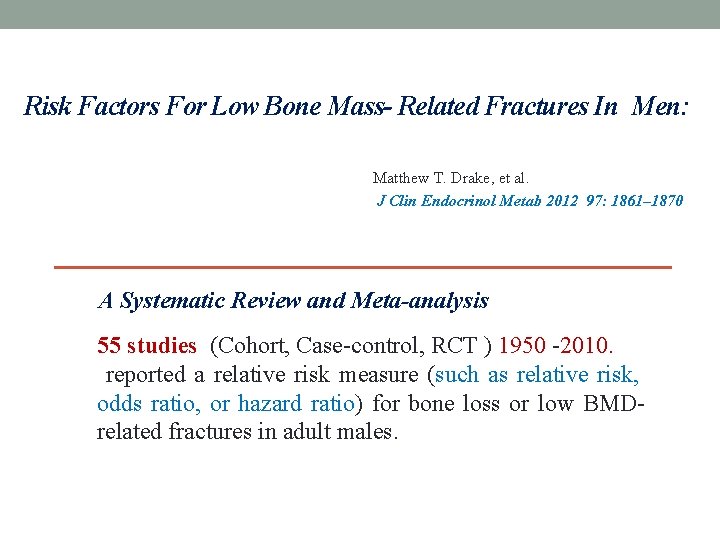
Risk Factors For Low Bone Mass- Related Fractures In Men: Matthew T. Drake, et al. J Clin Endocrinol Metab 2012 97: 1861– 1870 A Systematic Review and Meta-analysis 55 studies (Cohort, Case-control, RCT ) 1950 -2010. reported a relative risk measure (such as relative risk, odds ratio, or hazard ratio) for bone loss or low BMDrelated fractures in adult males.
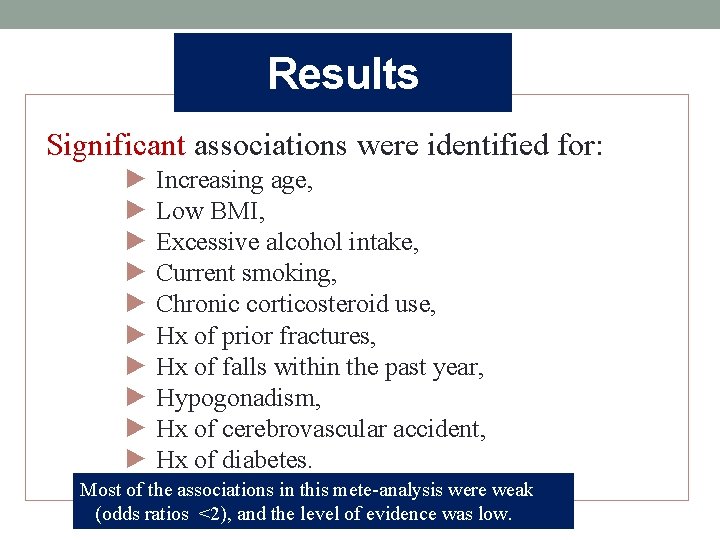
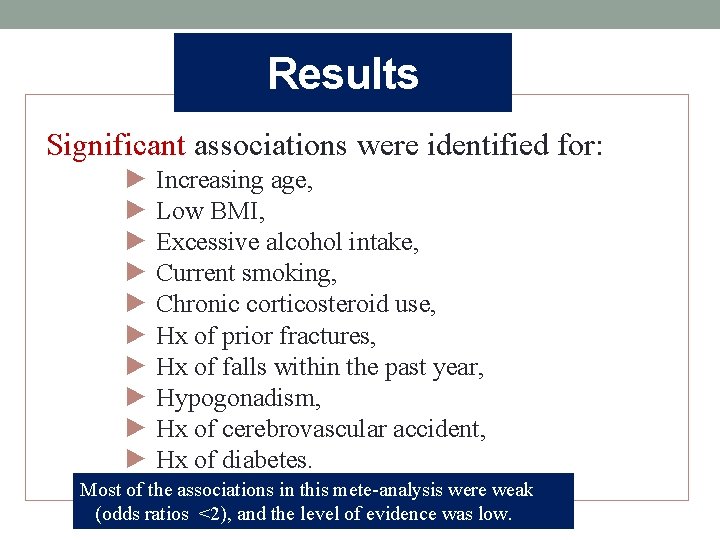
Results Significant associations were identified for: ► Increasing age, ► Low BMI, ► Excessive alcohol intake, ► Current smoking, ► Chronic corticosteroid use, ► Hx of prior fractures, ► Hx of falls within the past year, ► Hypogonadism, ► Hx of cerebrovascular accident, ► Hx of diabetes. Most of the associations in this mete-analysis were weak (odds ratios <2), and the level of evidence was low.
NOF 2010 Risk factors of male OP & broken bones: ♦ Age 70 or older ♦ Family history of osteoporosis or broken bones ♦ Age 50 or older and have broken any bones or lost an inch or more in height ♦ Certain medicines or have certain medical conditions that can cause bone loss

Treatment Recommendations ►In those with hip or vertebral fractures. ►In those with T-score < - 2. 5 (Osteoporosis) ►In men age 50 and older with Osteopenia and a 10 -year hip Fx. probability > 3% or a 10 -year major osteoporosis-related Fx. probability>20% ( based on FRAX)
Treatment Recommendations ► Men who are receiving long-term glucocorticoid therapy in pharmacological doses. ►Men with prostate cancer receiving ADT who have a high risk of fracture
Universal Treatment Strategies • Fall prevention • Smoking cessation • Hip protectors • Weight-bearing exercise • Diet : - Calcium: 1000– 1200 mg/day - Vitamin D

Selection of therapeutic agent Individualized based on: • Fracture history, • Severity of osteoporosis (T-scores), • The risk for hip fracture, • Patterns of BMD [i. e. whether BMD is worse at sites where cortical bone (e. g. 1/3 radius) or trabecular bone (e. g. spine) predominates], • Comorbid conditions(peptic ulcer disease, gastro esophageal reflux, mal absorption syndromes, malignancy, etc. ), • Cost, and other factors.
Selection of therapeutic agent • In men with a recent hip fracture : Zoledronic acid. • Teriparatide : without anti-resorptive therapy. • Agents, not approved: Calcitonin, Ibandronate, Strontium ranelate, should be used only if the approved agents for male osteoporosis can not be administered.
The evidence for efficacy of osteoporosis treatment in men with primary osteoporosis: A systematic review and meta- analysis of Antiresorptive and Anabolic treatment in men Peter Schwarz, et al. Journal of Osteoporosis, 2011
Study characteristics: Seven RCT (1945 -2010) on clinical efficacy of : • Antiresorptive (at least 12 months duration ) • Anabolic (at least 6 months duration ) in the reduction of fracture risk in elderly and old men with primary Osteoporosis. •
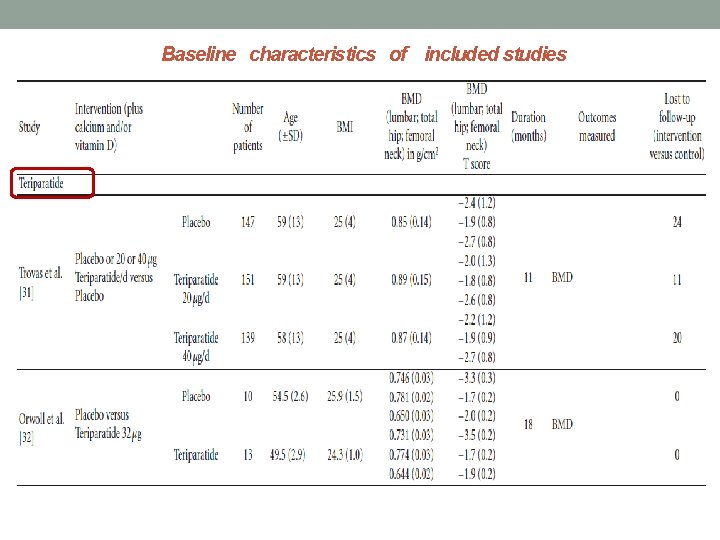
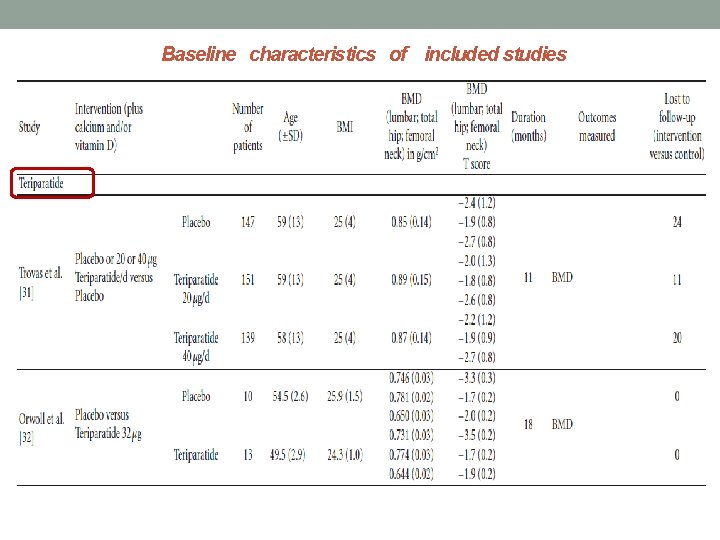
Baseline characteristics of included studies

Results: Changes in BMD üGonnelli et al. : increase in BMD with Alendronate : LS 4. 2% , FN 2. 1% , Hip 1. 6% at year 1 LS 6. 3% , FN 3. 2% , Hip 2. 6% at year 2 LS 8. 8% , FN 4. 2% , Hip 3. 9% at year 3 ü Boonen et al. treatment with Risedronate 4. 5% (95% CI: 3. 5– 5. 6%; P < 0. 001) increase in lumbar spine BMD compared with placebo.
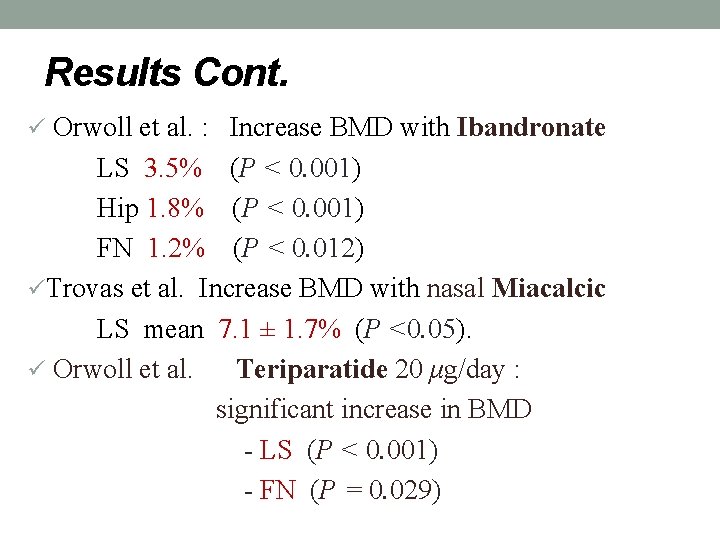
Results Cont. ü Orwoll et al. : Increase BMD with Ibandronate LS 3. 5% (P < 0. 001) Hip 1. 8% (P < 0. 001) FN 1. 2% (P < 0. 012) üTrovas et al. Increase BMD with nasal Miacalcic LS mean 7. 1 ± 1. 7% (P <0. 05). ü Orwoll et al. Teriparatide 20 μg/day : significant increase in BMD - LS (P < 0. 001) - FN (P = 0. 029)
(Intention - to - treat study) N Engl J Med 2012; 367: 1714 -23
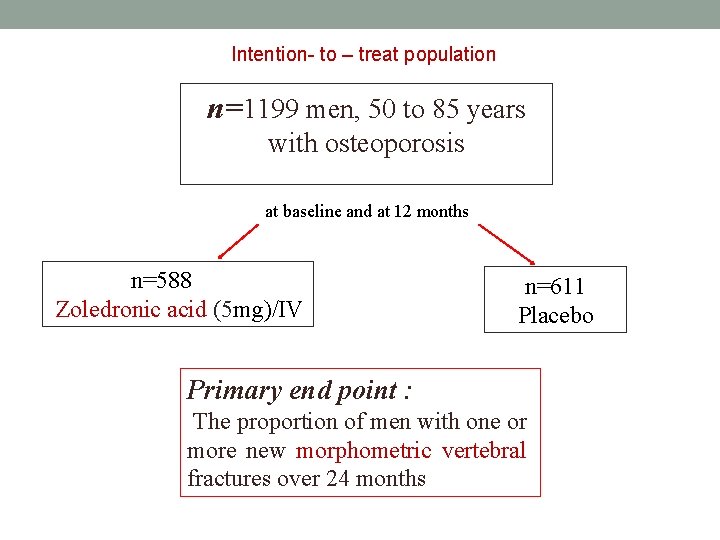
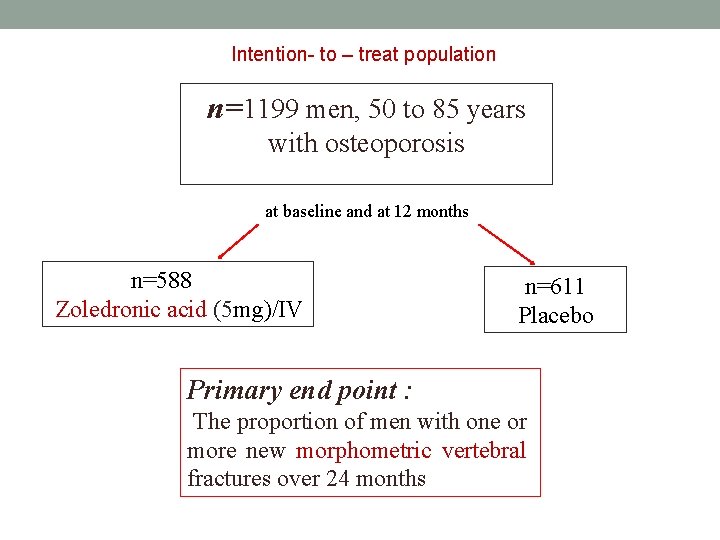
Intention- to – treat population n=1199 men, 50 to 85 years with osteoporosis at baseline and at 12 months n=588 Zoledronic acid (5 mg)/IV n=611 Placebo Primary end point : The proportion of men with one or more new morphometric vertebral fractures over 24 months


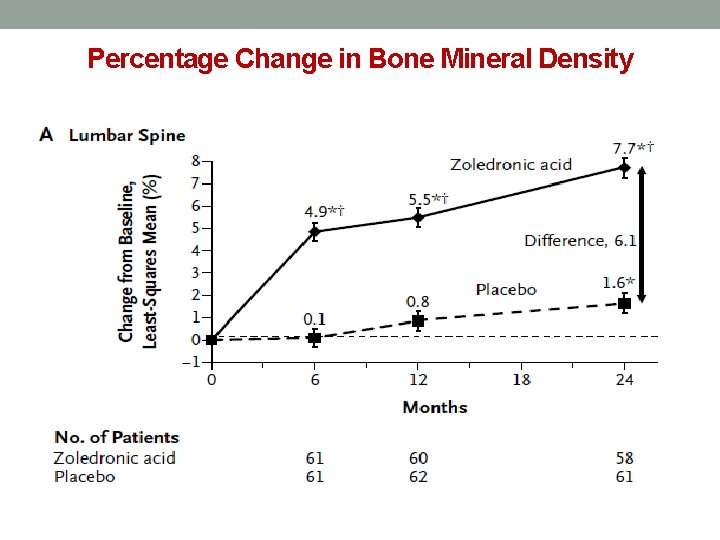
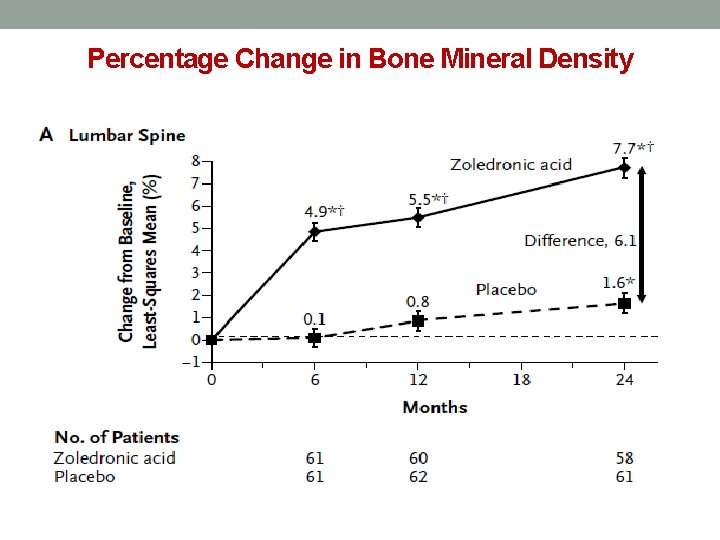
Percentage Change in Bone Mineral Density
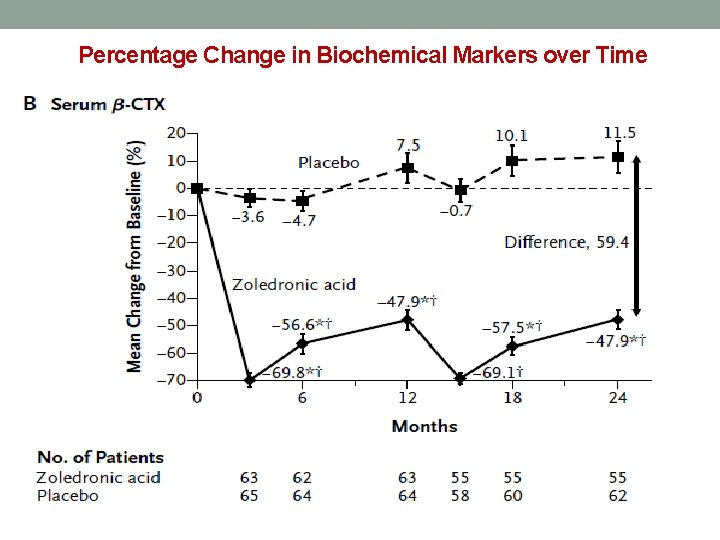
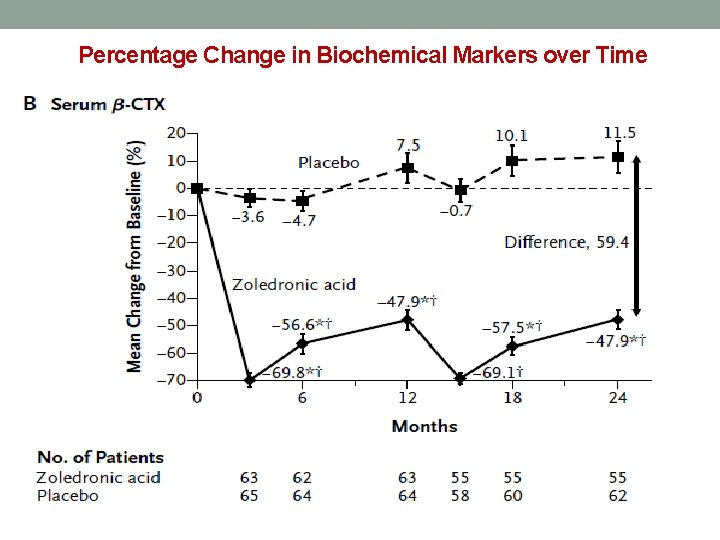
Percentage Change in Biochemical Markers over Time
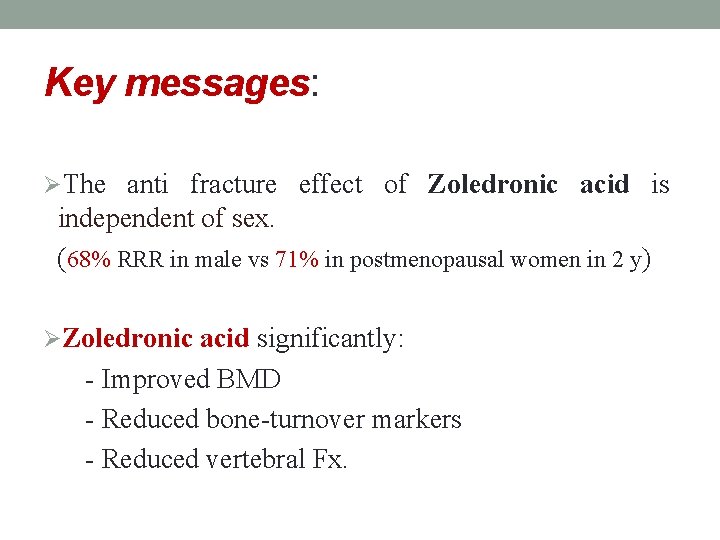
Key messages: ØThe anti fracture effect of Zoledronic acid is independent of sex. (68% RRR in male vs 71% in postmenopausal women in 2 y) ØZoledronic acid significantly: - Improved BMD - Reduced bone-turnover markers - Reduced vertebral Fx.
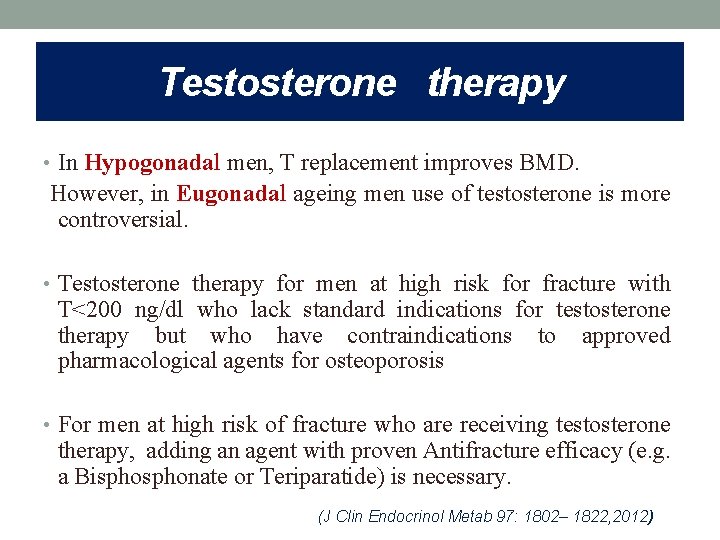
Testosterone therapy • In Hypogonadal men, T replacement improves BMD. However, in Eugonadal ageing men use of testosterone is more controversial. • Testosterone therapy for men at high risk for fracture with T<200 ng/dl who lack standard indications for testosterone therapy but who have contraindications to approved pharmacological agents for osteoporosis • For men at high risk of fracture who are receiving testosterone therapy, adding an agent with proven Antifracture efficacy (e. g. a Bisphonate or Teriparatide) is necessary. (J Clin Endocrinol Metab 97: 1802– 1822, 2012)

 Jeff lobe
Jeff lobe Hyperpigmentation in cushing syndrome
Hyperpigmentation in cushing syndrome Dr pang endocrinologist
Dr pang endocrinologist Endocrinologist in parbhani
Endocrinologist in parbhani Dr maeve hogan
Dr maeve hogan Dr swade endocrinologist
Dr swade endocrinologist Dimitrios thomas endocrinologist
Dimitrios thomas endocrinologist Dr suri endocrinologist
Dr suri endocrinologist Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Endocrinologist lifestyle
Endocrinologist lifestyle Endocrinologist newcastle
Endocrinologist newcastle Dr ponder endocrinologist
Dr ponder endocrinologist White men are saving brown women from brown men
White men are saving brown women from brown men Royal osteoporosis society leaflets
Royal osteoporosis society leaflets Tbs osteoporosis
Tbs osteoporosis Subjective data for osteoporosis
Subjective data for osteoporosis Osteoporosis
Osteoporosis T score osteoporosis
T score osteoporosis Osteoporosis defination
Osteoporosis defination Woc atrial fibrilasi
Woc atrial fibrilasi Dr eva decroli
Dr eva decroli Is osteoporosis hypokinetic or hyperkinetic
Is osteoporosis hypokinetic or hyperkinetic International osteoporosis foundation
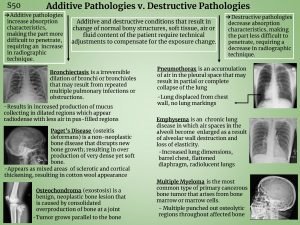
International osteoporosis foundation Additive and destructive pathology in radiography
Additive and destructive pathology in radiography Alendronate brand name
Alendronate brand name Pes statement for osteoporosis
Pes statement for osteoporosis Defination of osteoporosis
Defination of osteoporosis Osteoporosis
Osteoporosis Kinh mến
Kinh mến Of mice and men banned
Of mice and men banned Metaphor in of mice and men
Metaphor in of mice and men Simile for trust
Simile for trust Where im from poems
Where im from poems @jesus david pineda j:men. swap part 1
@jesus david pineda j:men. swap part 1 Pelvic inflammatory disease men
Pelvic inflammatory disease men Chapter one of mice and men
Chapter one of mice and men Men should weep notes
Men should weep notes Concentric zone model
Concentric zone model Man vs society conflict definition
Man vs society conflict definition Of mice and men poem
Of mice and men poem Plural foot
Plural foot X men
X men Poem the blind man and the elephant
Poem the blind man and the elephant Of mice and men background
Of mice and men background Of mice and men eal
Of mice and men eal James madison if men were angels
James madison if men were angels Of mice and men section 2 summary
Of mice and men section 2 summary Hpv test for men
Hpv test for men Four men with leprosy
Four men with leprosy Setting of mice and men
Setting of mice and men Bestey
Bestey Shakespeare love sonnet 29
Shakespeare love sonnet 29 Of mice and men jeopardy
Of mice and men jeopardy Setting of mice and men
Setting of mice and men Men's saturday morning study
Men's saturday morning study What causes uti
What causes uti Of mice and men-webquest answer key
Of mice and men-webquest answer key Gyro error
Gyro error Issachar understood the times
Issachar understood the times Things men wish women knew
Things men wish women knew Of mice and men quote
Of mice and men quote