THYROID CANCER EPIDEMIOLOGY H Delshad M D Endocrinologist






- Slides: 63

THYROID CANCER EPIDEMIOLOGY H. Delshad M. D Endocrinologist Research Institute for Endocrine Sciences
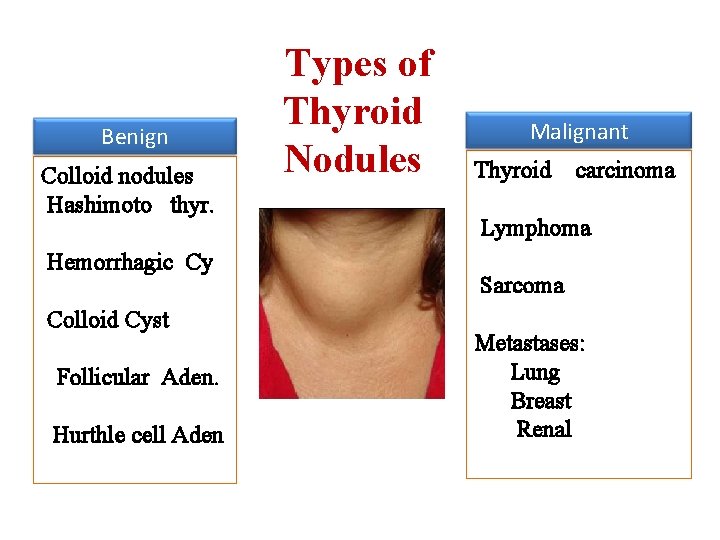
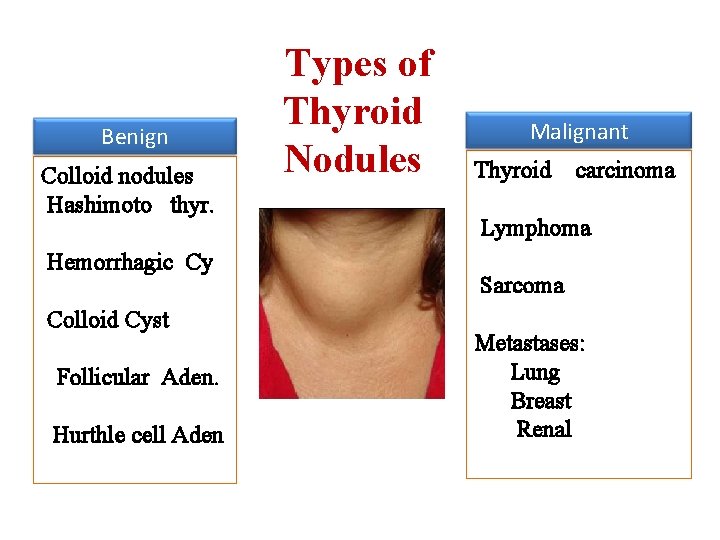
Benign Colloid nodules Hashimoto thyr. Hemorrhagic Cy Colloid Cyst Follicular Aden. Hurthle cell Aden Types of Thyroid Nodules Malignant Thyroid carcinoma Lymphoma Sarcoma Metastases: Lung Breast Renal
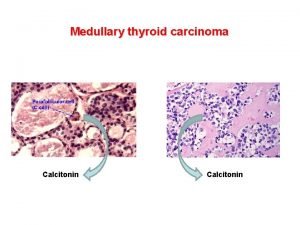
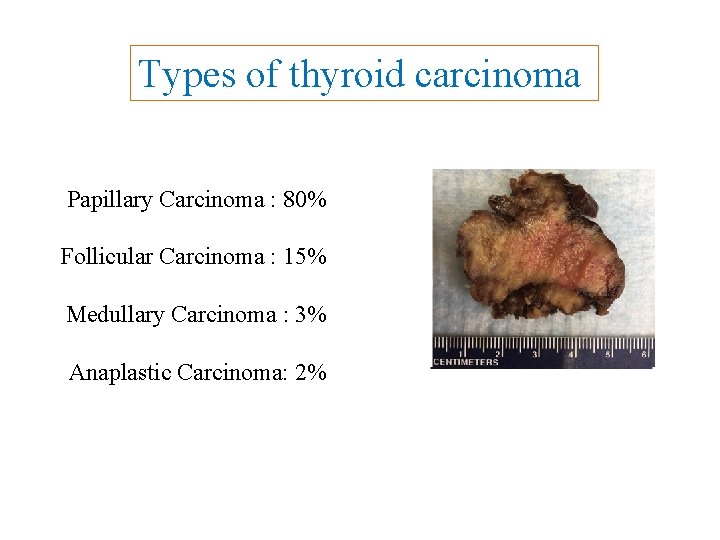
Types of thyroid carcinoma Papillary Carcinoma : 80% Follicular Carcinoma : 15% Medullary Carcinoma : 3% Anaplastic Carcinoma: 2%
Discovery William Stewart Halsted Prominent American Surgeon Late 19 th Century

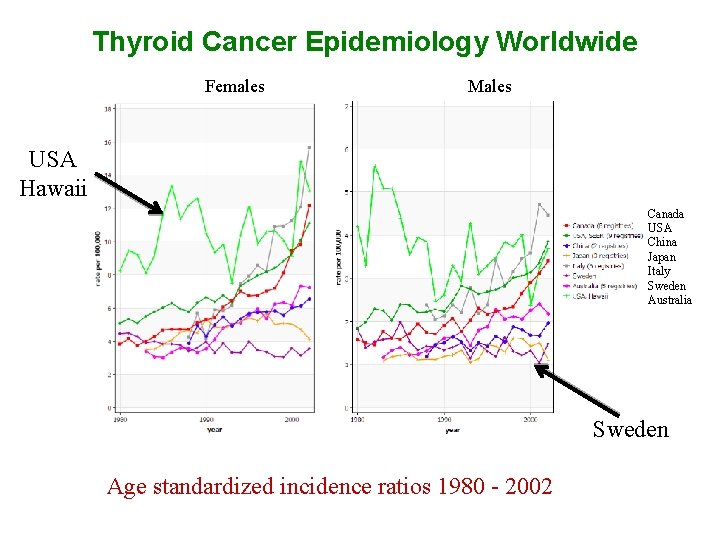
Thyroid Cancer: Key points . ● 1. 5 % of all cancer , 95% of all endocrine cancer ● Female to male ratio: 2. 5 / 1 ● It is now the 5 th most frequent cancer in women ● It ranked 14 th , 20 years ago ● It will be the 4 th most common cancer in the US by 2030 ● High incidence areas ( > 10/ 100000 ): Japan, Pacific Islands, Italy and several countries in the Americas ● The highest incidence of thyroid carcinomas in the world is found among female Chinese residents of Hawaii. ● About 2% of thyroid cancers occur in children and teens
Determinant Of Annual Incidence Rate • Geographic areas • Age • Sex
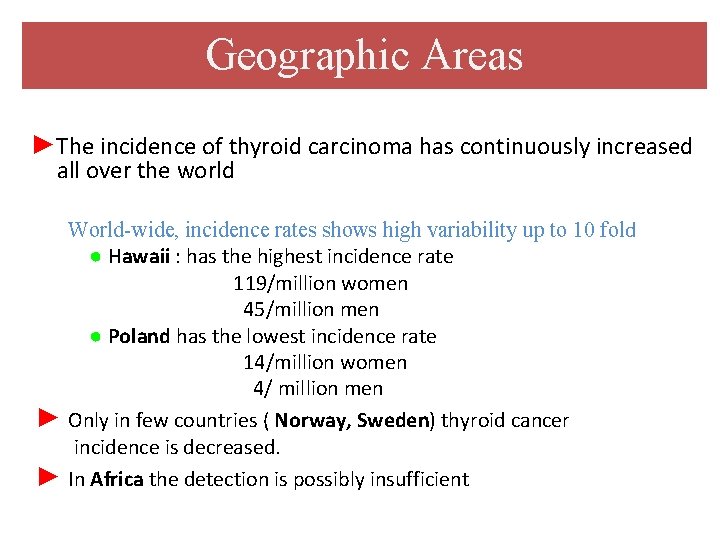
Geographic Areas ►The incidence of thyroid carcinoma has continuously increased all over the world ► ► World-wide, incidence rates shows high variability up to 10 fold ● Hawaii : has the highest incidence rate 119/million women 45/million men ● Poland has the lowest incidence rate 14/million women 4/ million men Only in few countries ( Norway, Sweden) thyroid cancer incidence is decreased. In Africa the detection is possibly insufficient
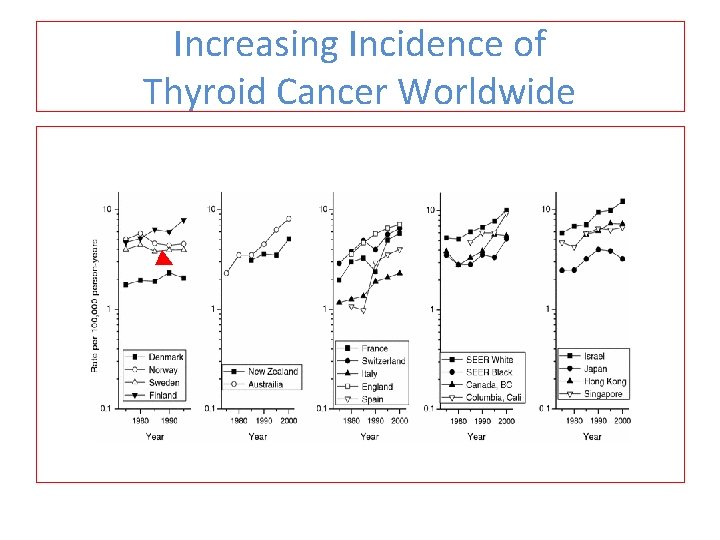
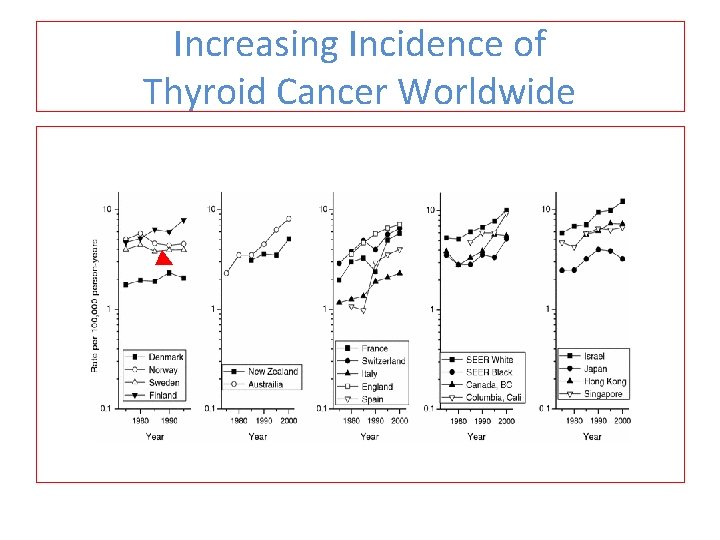
Increasing Incidence of Thyroid Cancer Worldwide ►
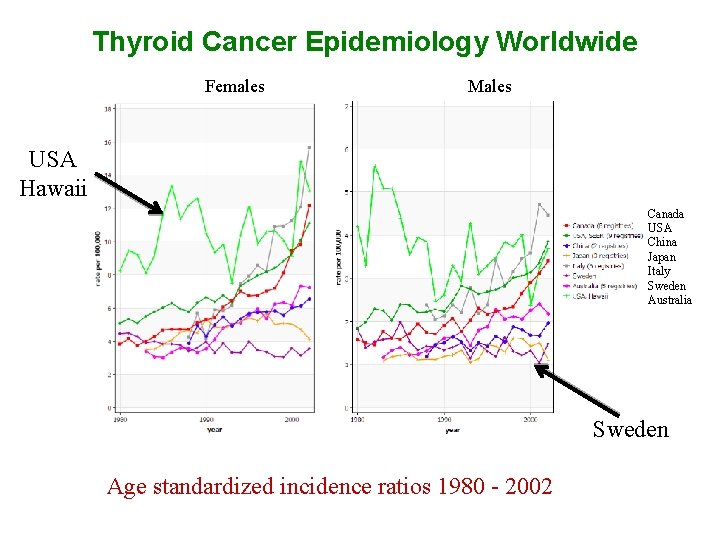
Thyroid Cancer Epidemiology Worldwide Females Males USA Hawaii Canada USA China Japan Italy Sweden Australia Sweden Age standardized incidence ratios 1980 - 2002
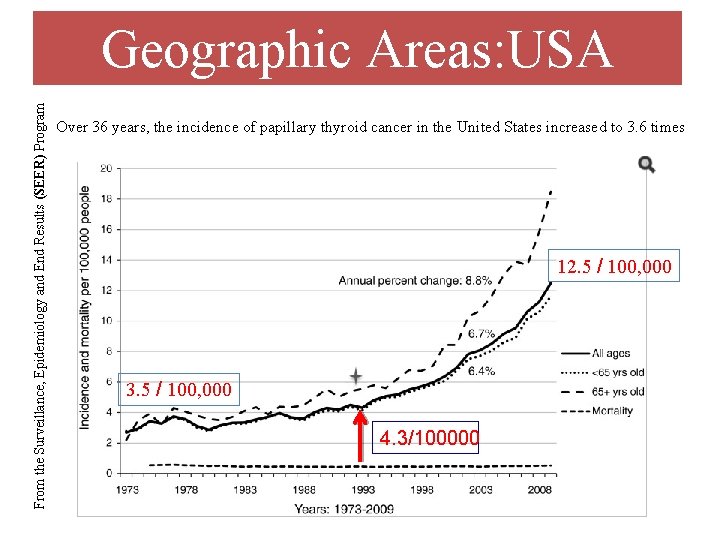
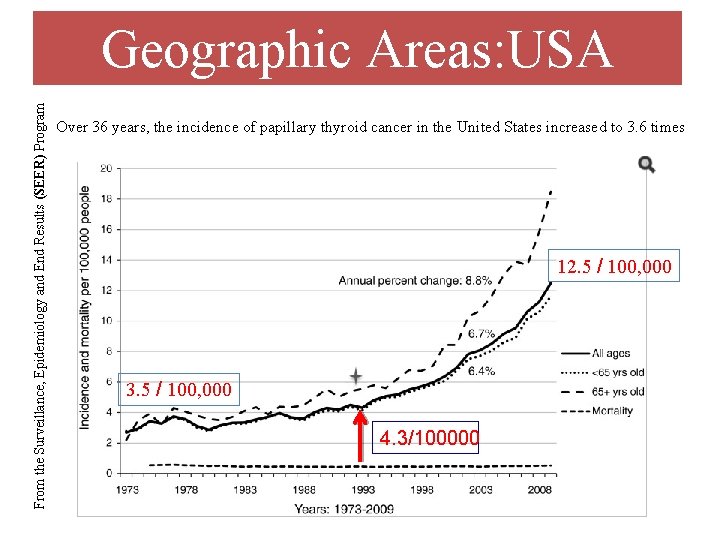
From the Surveillance, Epidemiology and End Results (SEER) Program Geographic Areas: USA Over 36 years, the incidence of papillary thyroid cancer in the United States increased to 3. 6 times 12. 5 / 100, 000 3. 5 / 100, 000 4. 3/100000
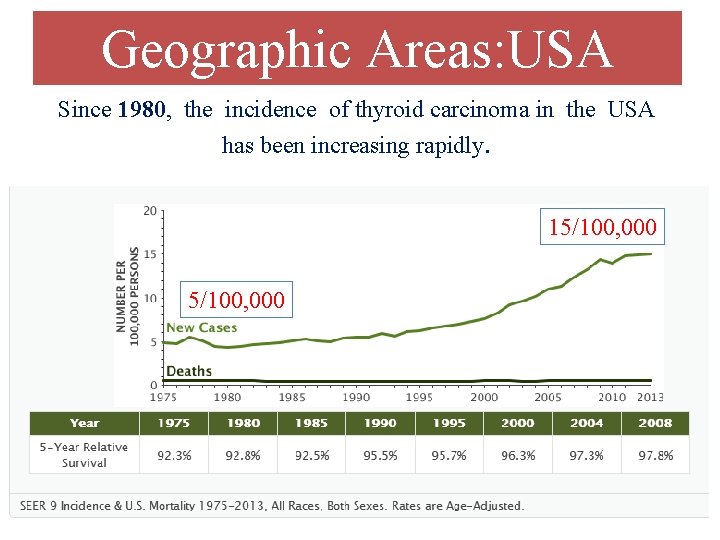
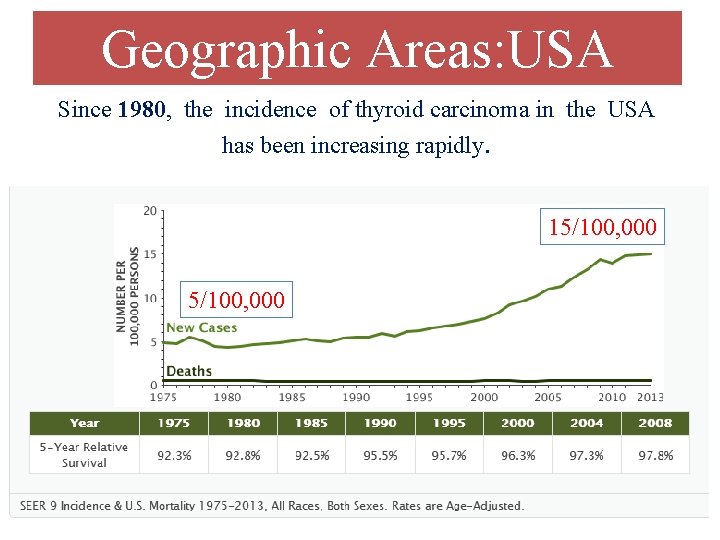
Geographic Areas: USA Since 1980, the incidence of thyroid carcinoma in the USA has been increasing rapidly. 15/100, 000
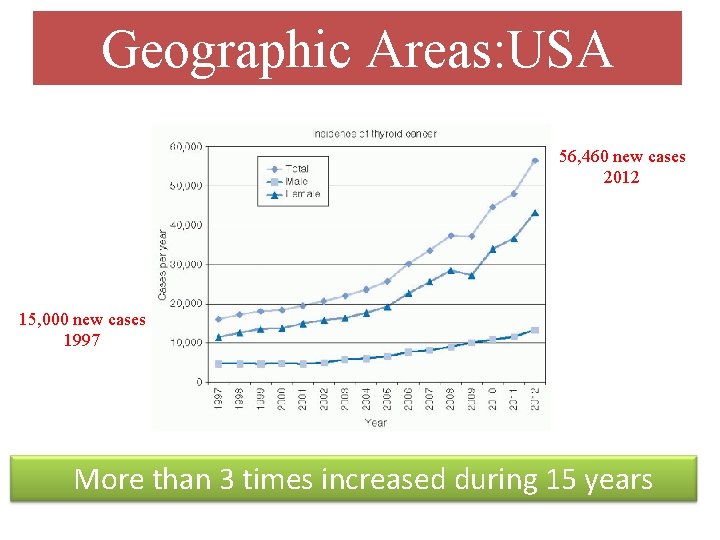
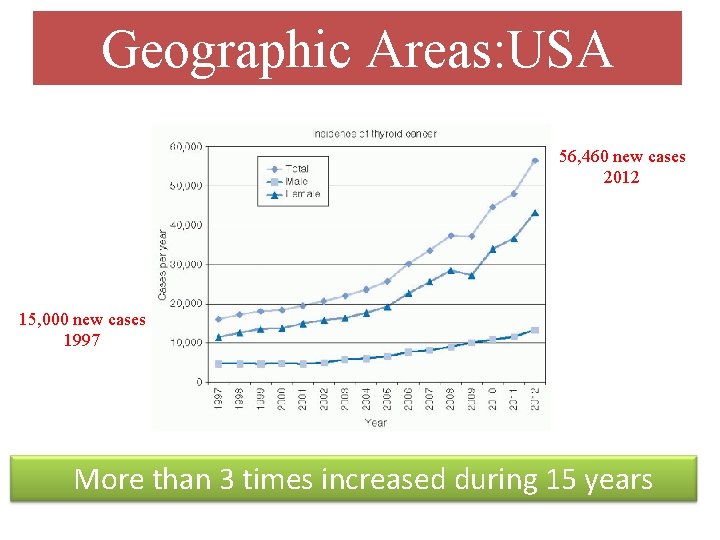
Geographic Areas: USA 56, 460 new cases 2012 15, 000 new cases 1997 More than 3 times increased during 15 years
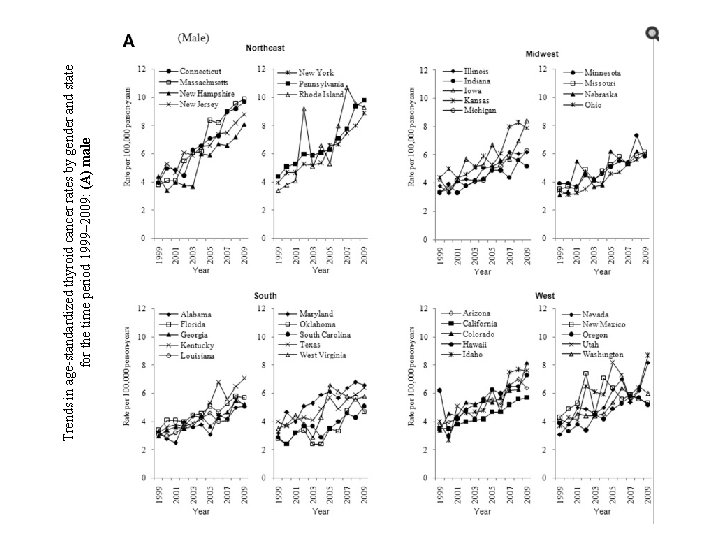
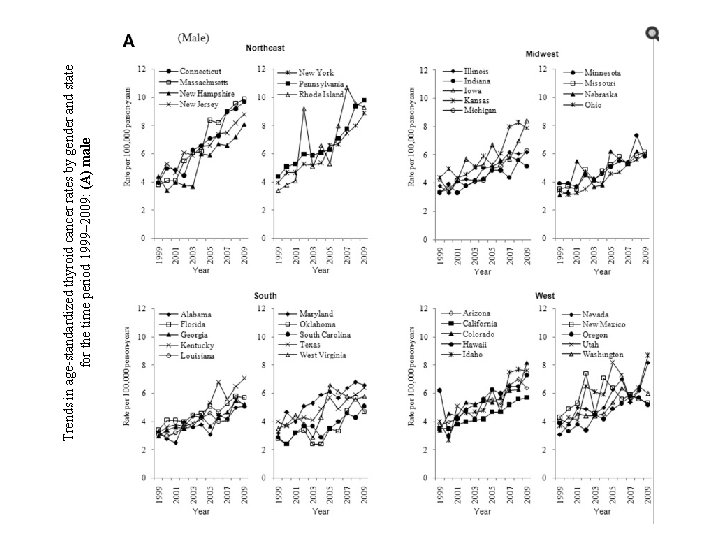
Trends in age-standardized thyroid cancer rates by gender and state for the time period 1999– 2009: (A) male
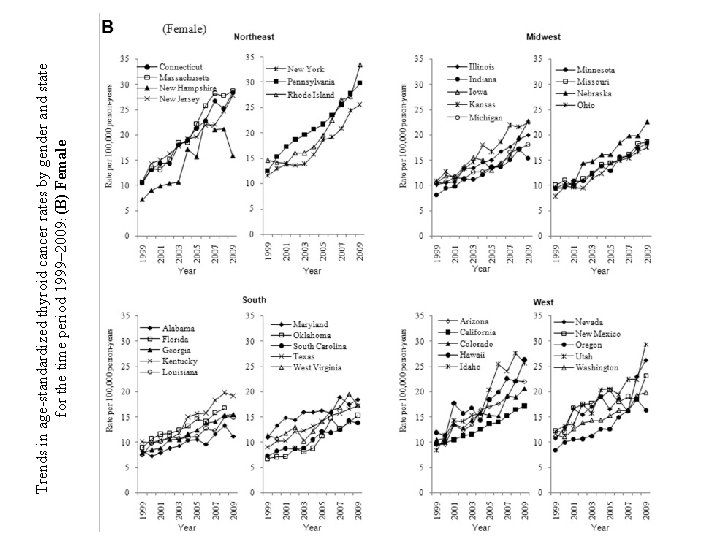
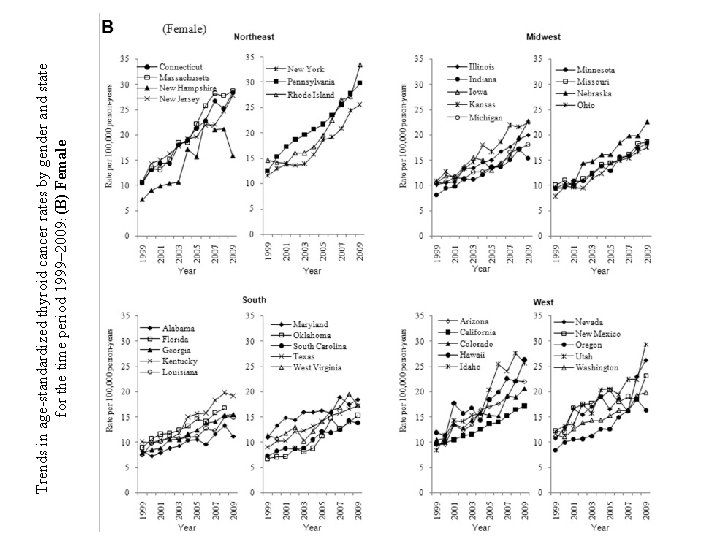
Trends in age-standardized thyroid cancer rates by gender and state for the time period 1999– 2009: (B) Female
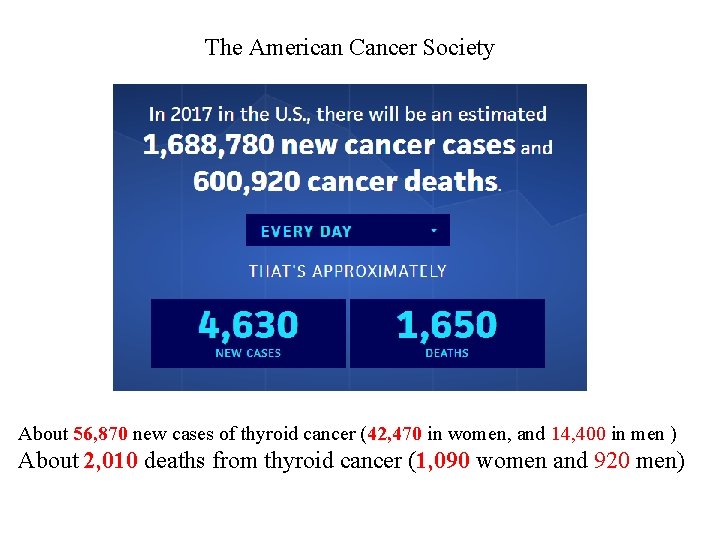
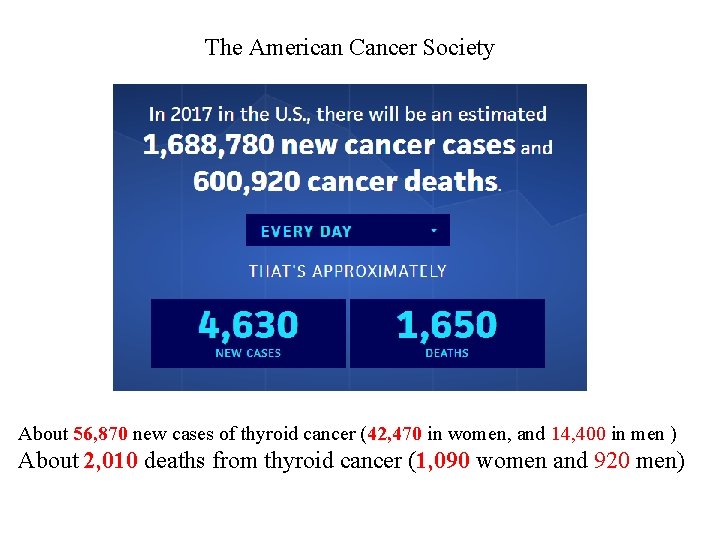
The American Cancer Society About 56, 870 new cases of thyroid cancer (42, 470 in women, and 14, 400 in men ) About 2, 010 deaths from thyroid cancer (1, 090 women and 920 men)
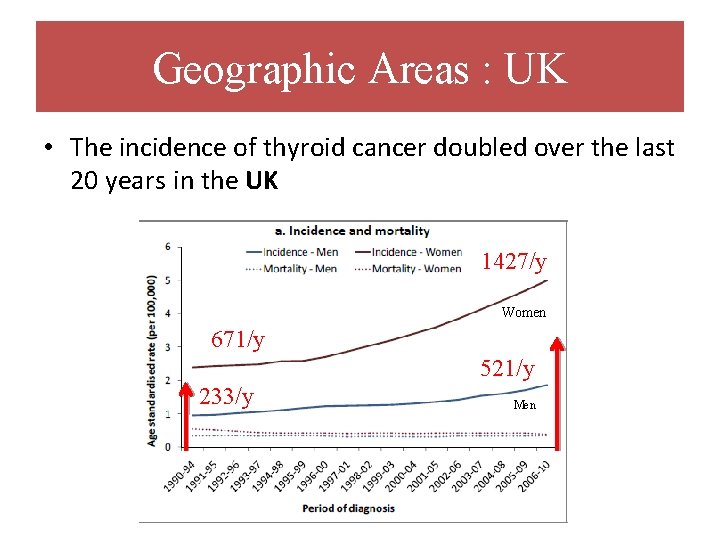
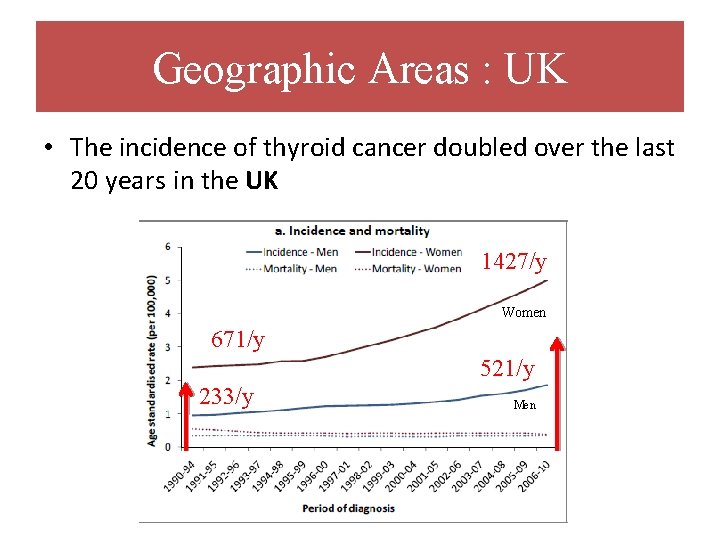
Geographic Areas : UK • The incidence of thyroid cancer doubled over the last 20 years in the UK 1427/y Women 671/y 521/y 233/y Men
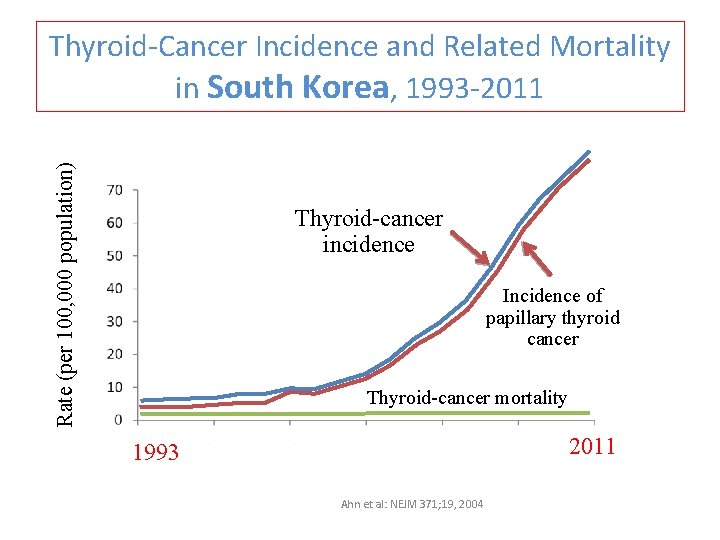
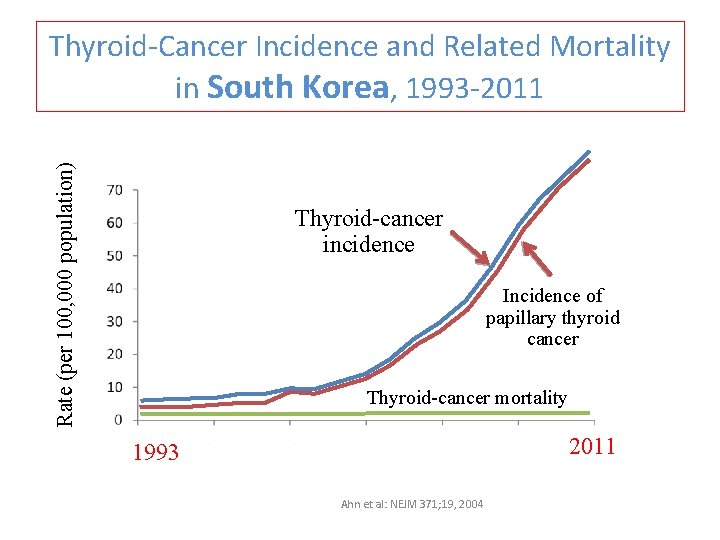
Rate (per 100, 000 population) Thyroid-Cancer Incidence and Related Mortality in South Korea, 1993 -2011 Thyroid-cancer incidence Incidence of papillary thyroid cancer Thyroid-cancer mortality 2011 1993 Ahn et al: NEJM 371; 19, 2004
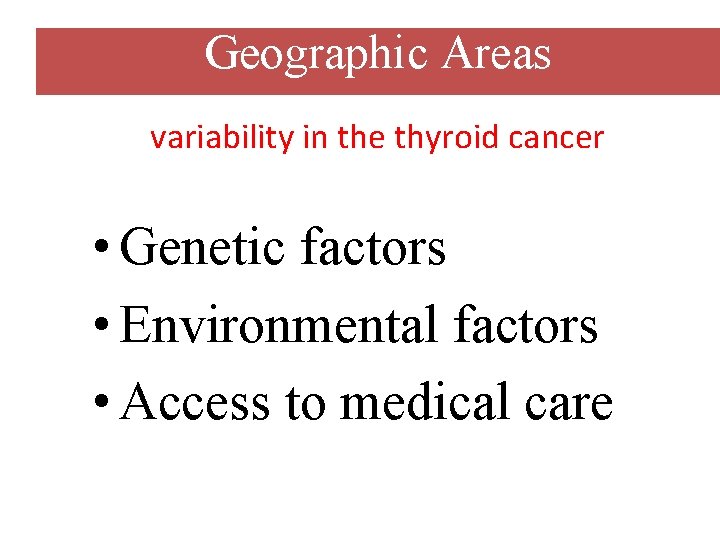
Geographic Areas variability in the thyroid cancer • Genetic factors • Environmental factors • Access to medical care
Determinant Of Annual Incidence Rate • Geographic areas • Age • Sex
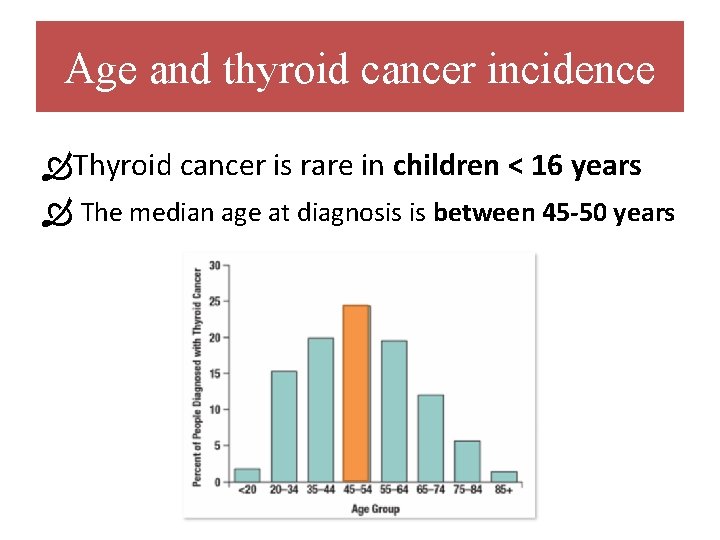
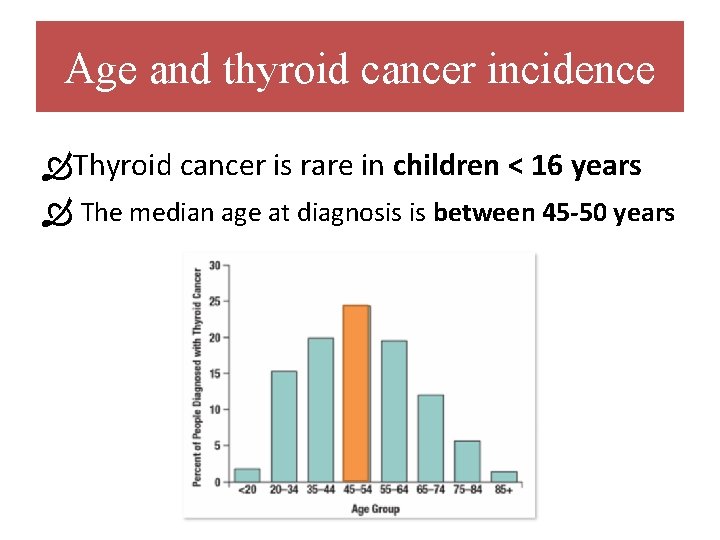
Age and thyroid cancer incidence Thyroid cancer is rare in children < 16 years The median age at diagnosis is between 45 -50 years
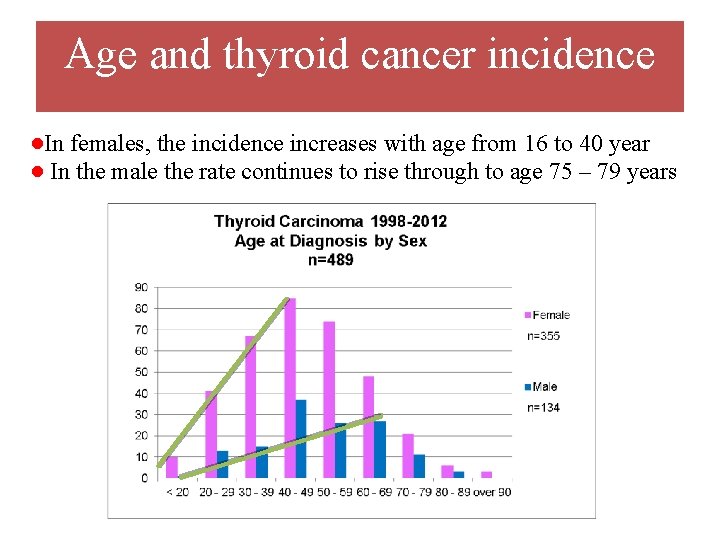
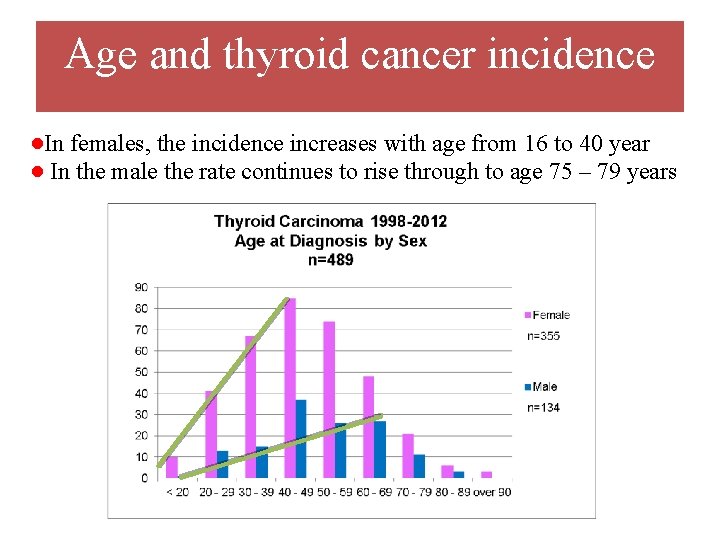
Age and thyroid cancer incidence ●In females, the incidence increases with age from 16 to 40 year ● In the male the rate continues to rise through to age 75 – 79 years

Age adjusted thyroid cancer incidence in the USA between 2003 - 2007 (Rates per 100, 000 persons ) INCIDENCE MORTALITY Data from the Survellance, Epidemiology and End Results (SEER) Program using 12 SEER areas (San Francisco, Connecticut, Detroit, Hawaii, Iowa, New Mexico, Seattle, Utah, Atlanta, San Jose– Monterey, Los Angeles and Alaska)
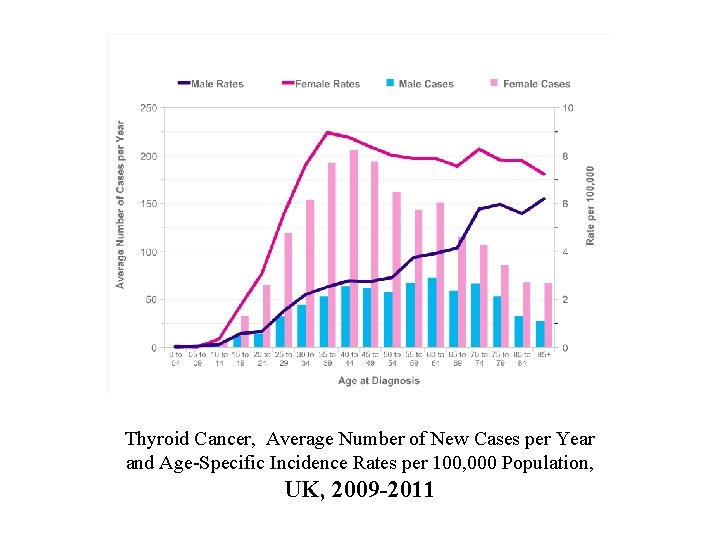
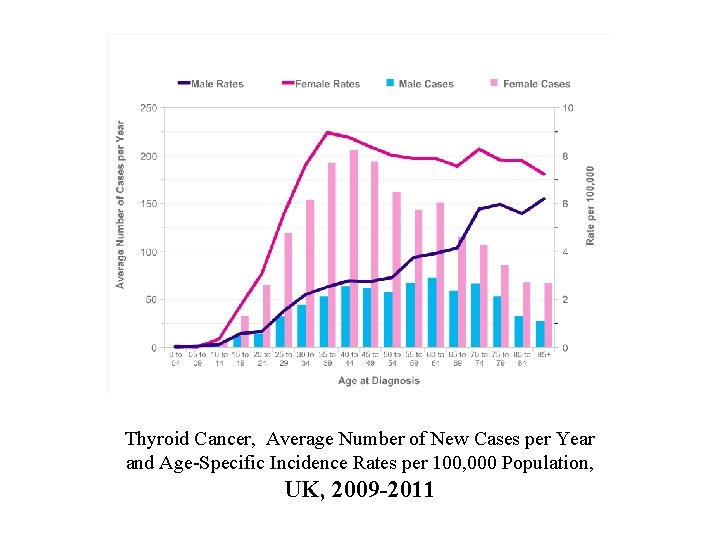
Thyroid Cancer, Average Number of New Cases per Year and Age-Specific Incidence Rates per 100, 000 Population, UK, 2009 -2011
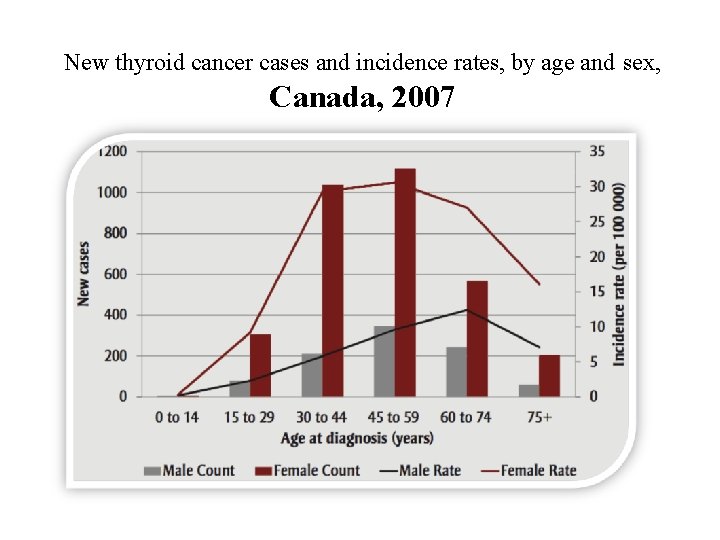
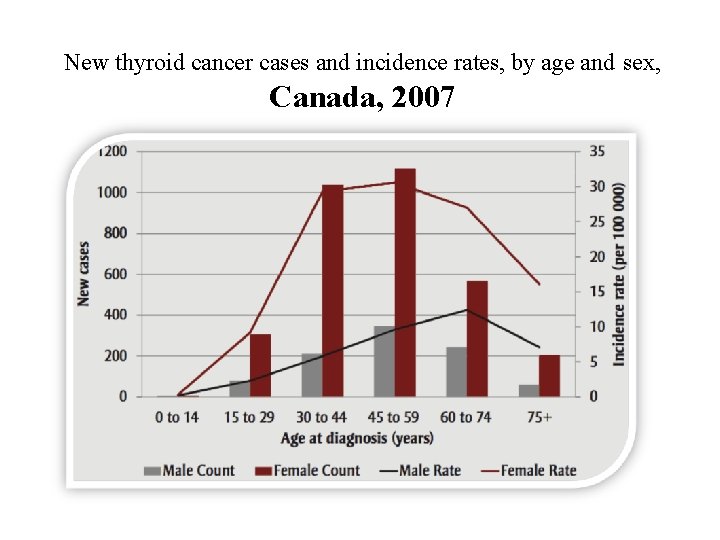
New thyroid cancer cases and incidence rates, by age and sex, Canada, 2007
Determinant Of Annual Incidence Rate • Geographic areas • Age • Sex
Trend by sex ►The incidence of thyroid cancer is approximately the same for males and females before puberty and after menopause. ► F/M : is highest during puberty
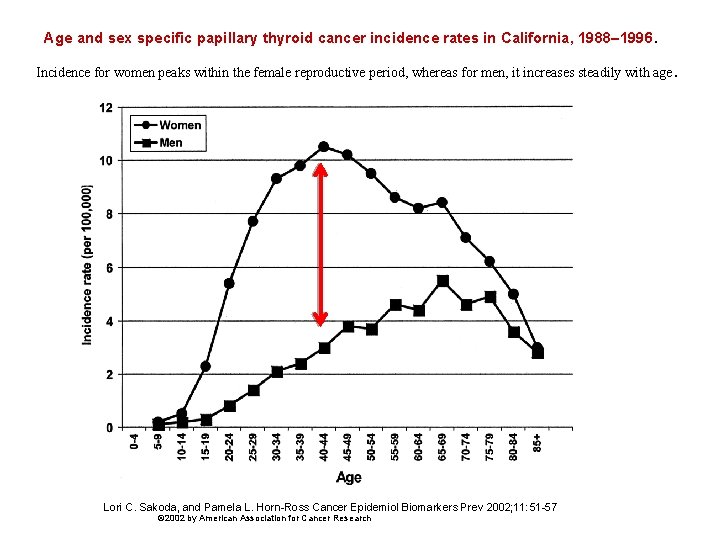
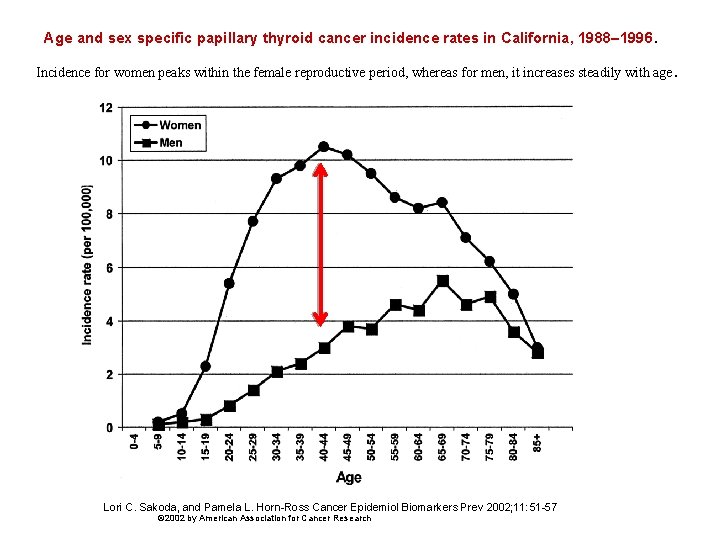
Age and sex specific papillary thyroid cancer incidence rates in California, 1988– 1996. Incidence for women peaks within the female reproductive period, whereas for men, it increases steadily with age Lori C. Sakoda, and Pamela L. Horn-Ross Cancer Epidemiol Biomarkers Prev 2002; 11: 51 -57 © 2002 by American Association for Cancer Research .
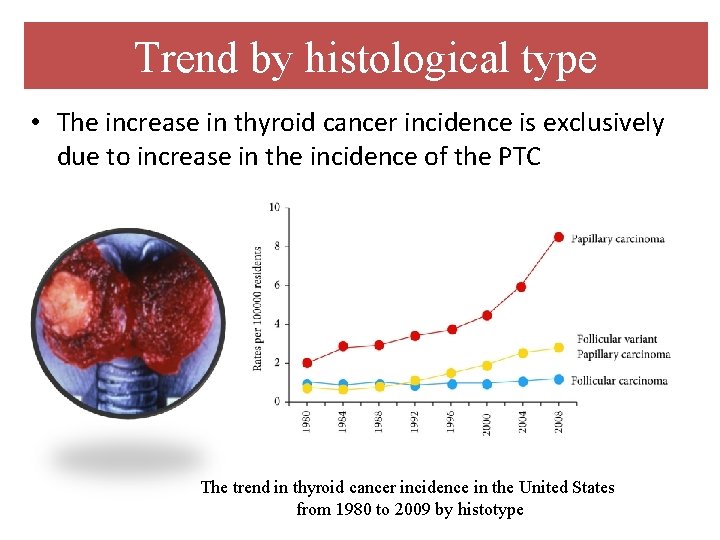
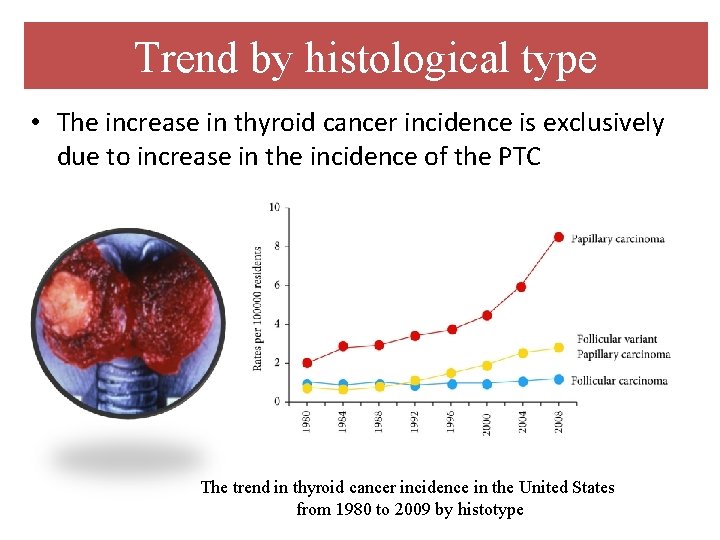
Trend by histological type • The increase in thyroid cancer incidence is exclusively due to increase in the incidence of the PTC The trend in thyroid cancer incidence in the United States from 1980 to 2009 by histotype
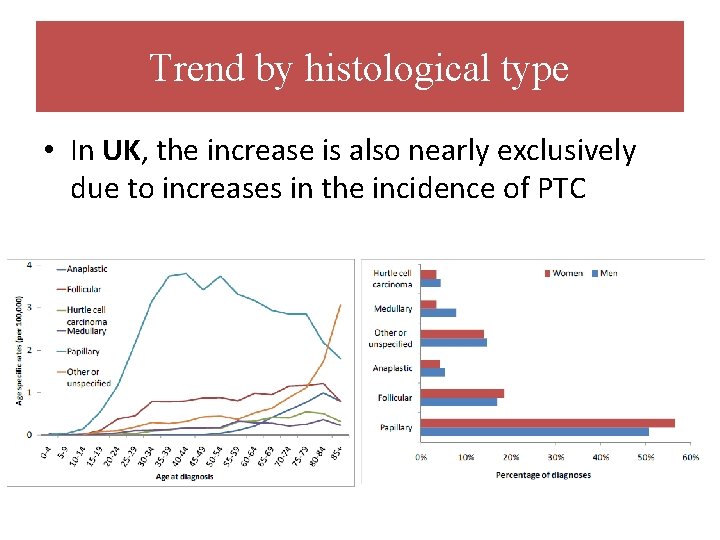
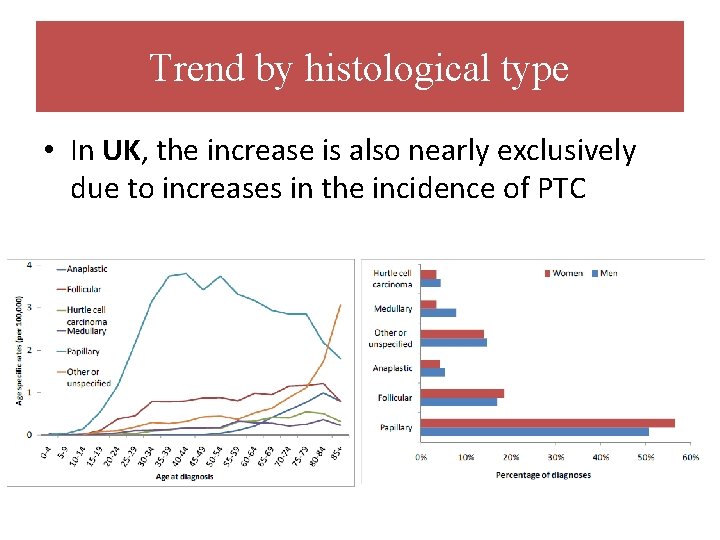
Trend by histological type • In UK, the increase is also nearly exclusively due to increases in the incidence of PTC
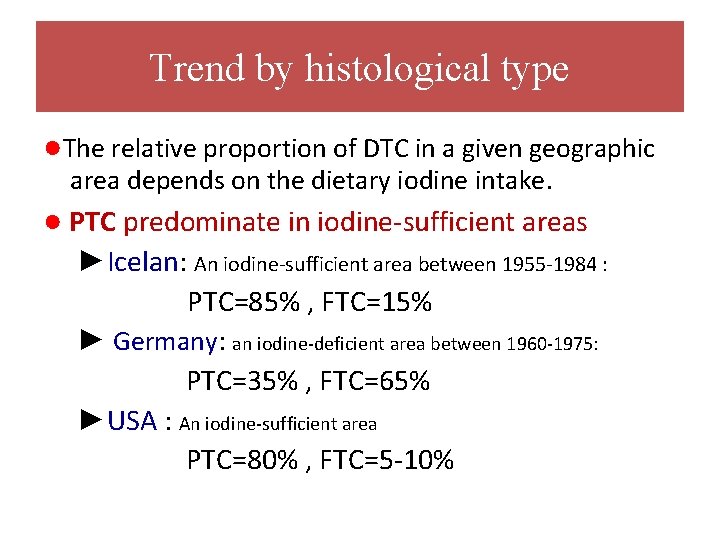
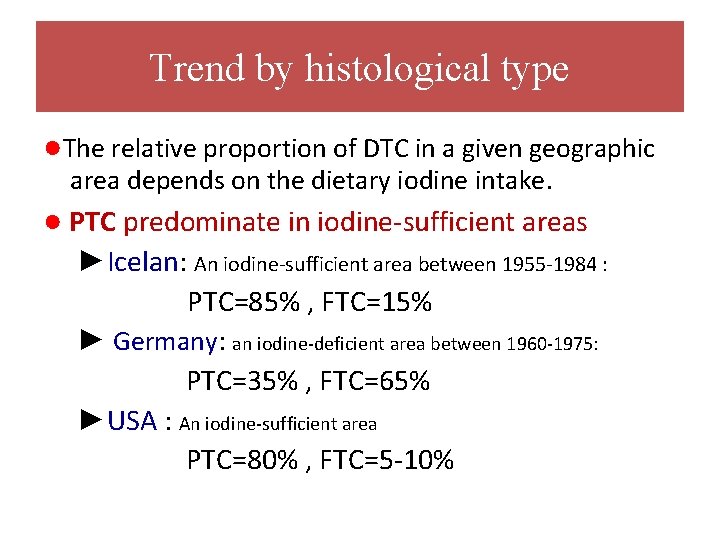
Trend by histological type ●The relative proportion of DTC in a given geographic area depends on the dietary iodine intake. ● PTC predominate in iodine-sufficient areas ►Icelan: An iodine-sufficient area between 1955 -1984 : PTC=85% , FTC=15% ► Germany: an iodine-deficient area between 1960 -1975: PTC=35% , FTC=65% ►USA : An iodine-sufficient area PTC=80% , FTC=5 -10%
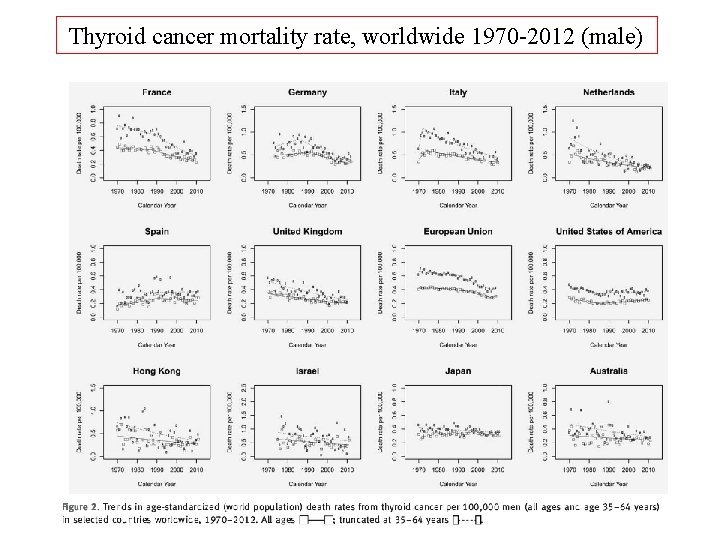
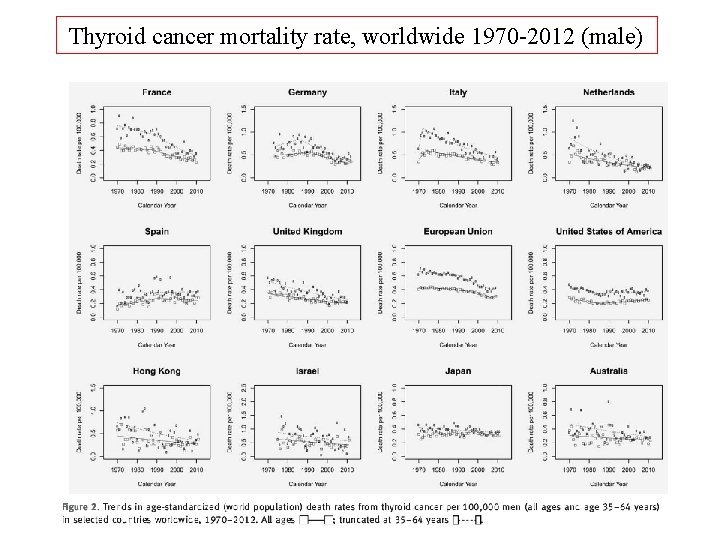
Thyroid cancer mortality rate, worldwide 1970 -2012 (male)
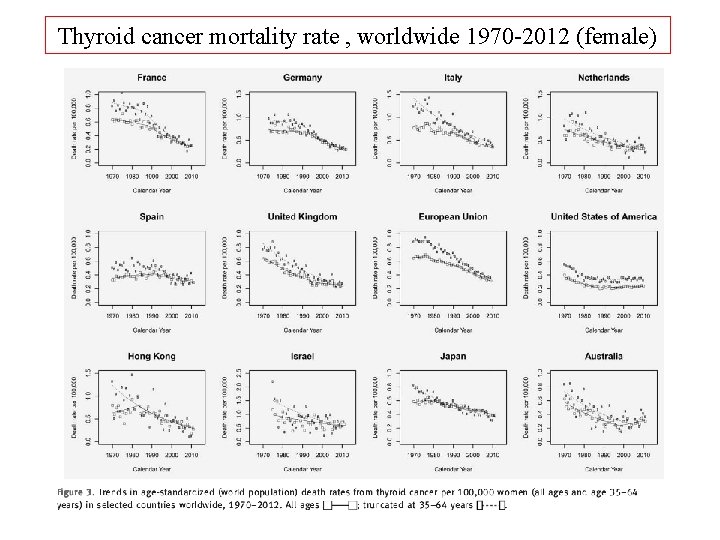
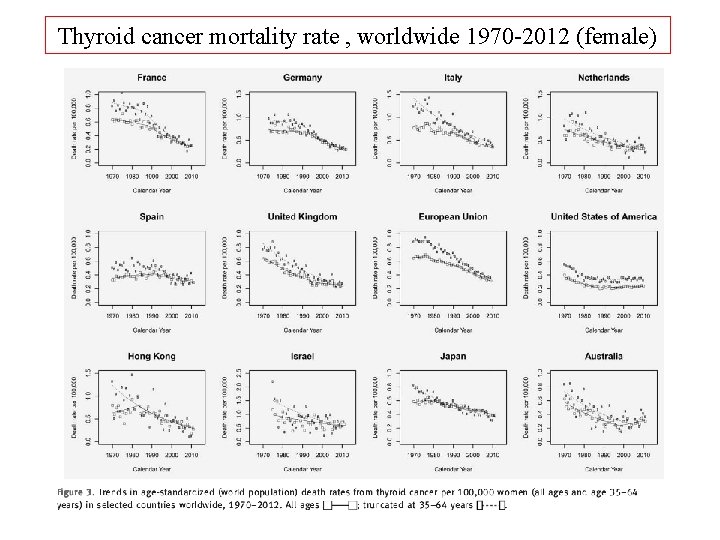
Thyroid cancer mortality rate , worldwide 1970 -2012 (female)
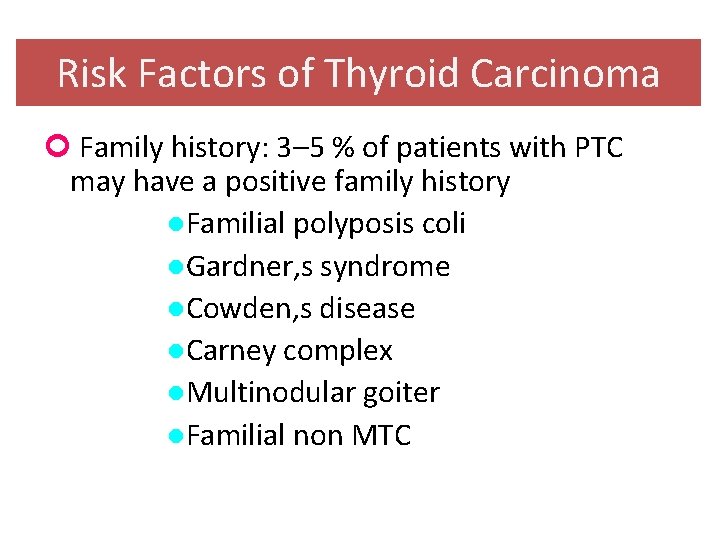
Risk Factors of Thyroid Carcinoma Family history: 3– 5 % of patients with PTC may have a positive family history ●Familial polyposis coli ●Gardner, s syndrome ●Cowden, s disease ●Carney complex ●Multinodular goiter ●Familial non MTC
Risk Factors of Thyroid Carcinoma ●Pre-existing benign thyroid diseases ● Hx. of goiter or benign thyroid nodules ● Graves, (some series) ● Hashimoto, s thyroiditis (lymphoma) ● Hormonal and reproductive factors F/M ratio is highest during puberty ● Dietary iodine intake ● Environmental factors: Smoking Diagnostic X-Ray Wood processing, pulp and paper making ● Body size : overweight and obesity
Risk Factors of Thyroid Carcinoma History of ionizing radiation exposure during childhood The only clearly demonstrated etiologic factor

Ionizing radiation and thyroid cancer
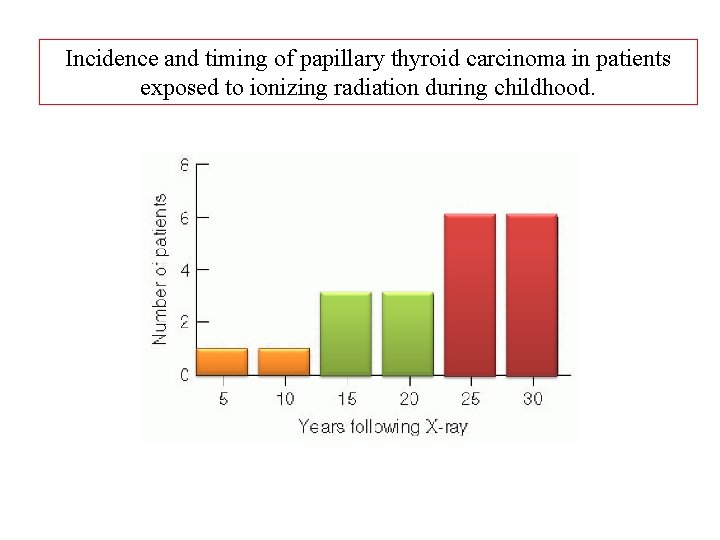
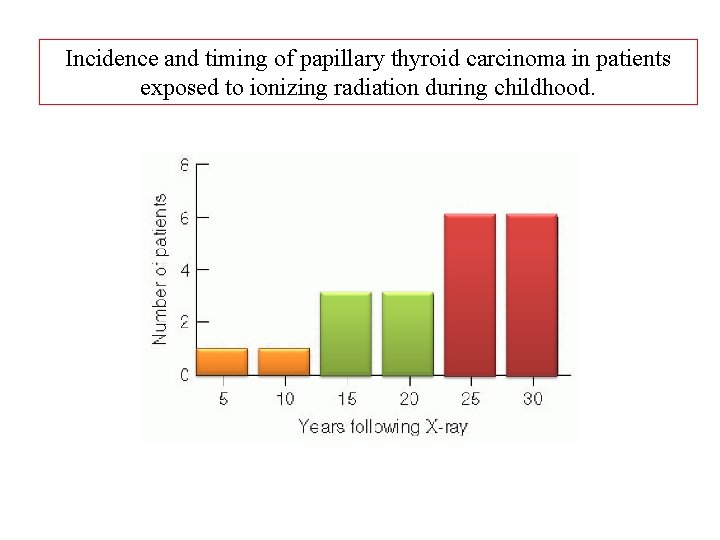
Incidence and timing of papillary thyroid carcinoma in patients exposed to ionizing radiation during childhood.
Ionizing Radiation • The relationship between radiation and thyroid cancer was first recognized in 1950 by Duffy and Fitzgeraled (Cancer 1950) • Thyroid carcinoma was the first solid malignant tumor found to be on the increase among Japanese atomic bomb survivors. (N Eng J Med 1963)
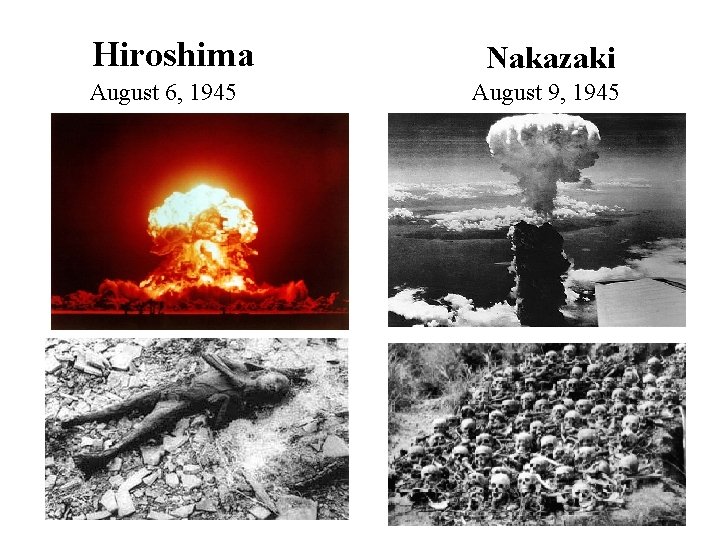
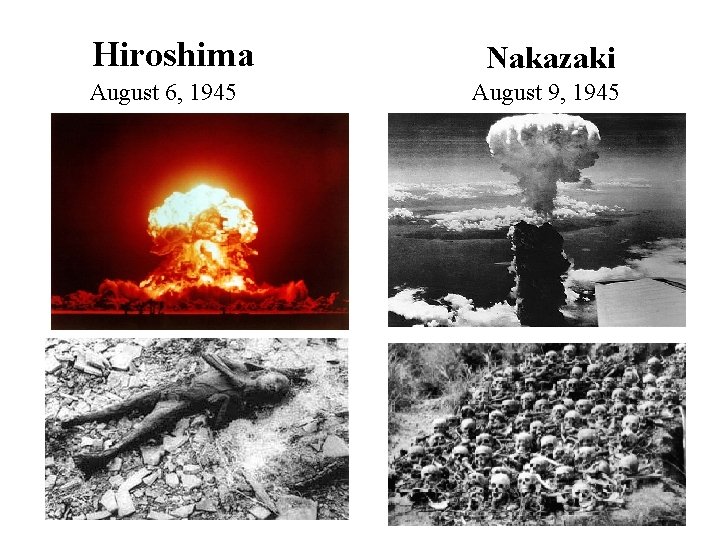
Hiroshima August 6, 1945 Nakazaki August 9, 1945
Ionizing Radiation ■ In 1950 : 284000 atomic bomb survivors included in the Life Span Study(LSS) and followed annually. ■ 225 thyroid cancer/ 79972 who were alive between 1958 -1987 (Radia Res. 1996) ■ Several nuclear tests have performed since 1940 s: ●Hanford=1940 s ●Marshal islanders, Utah, Navada, Arizona=1952 -55 ●French nuclear bomb tests in Mururoa=1966 -74
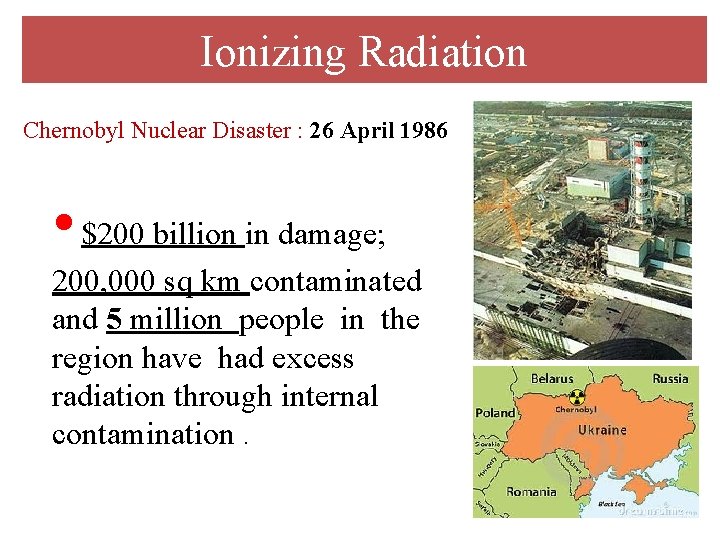
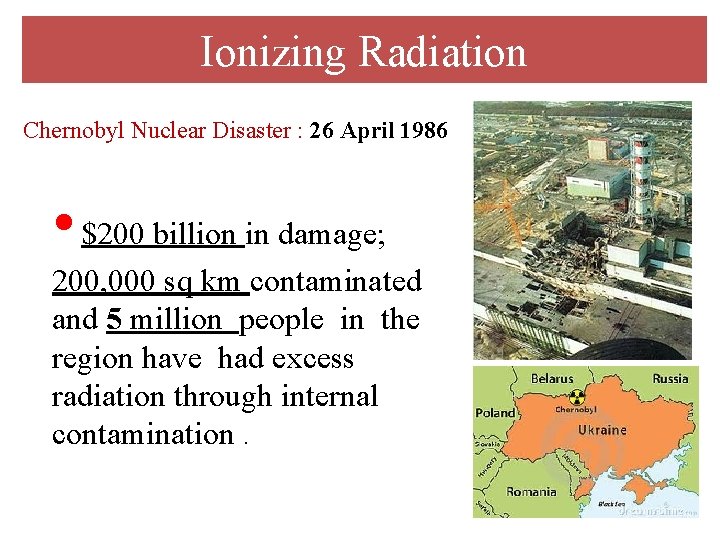
Ionizing Radiation Chernobyl Nuclear Disaster : 26 April 1986 • $200 billion in damage; 200, 000 sq km contaminated and 5 million people in the region have had excess radiation through internal contamination.

Ionizing Radiation Fukushima Nuclear Disaster: 11 March 2011 ●The total number of people who died in the earthquake and the tsunami based on the official estimation was 14000.
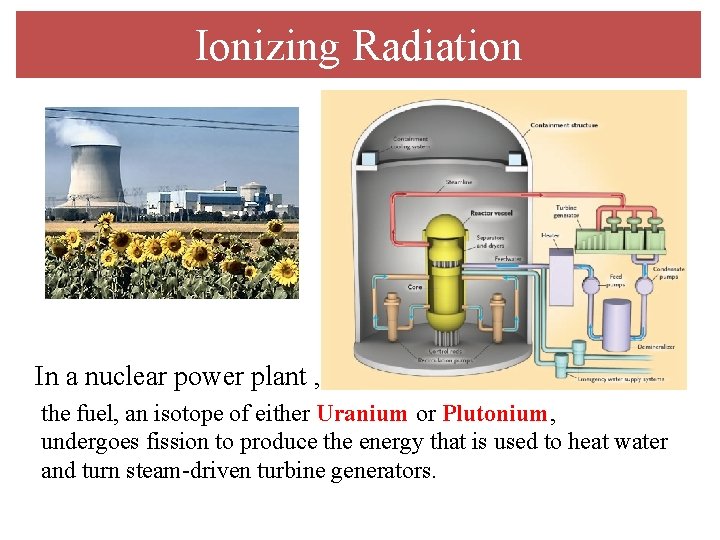
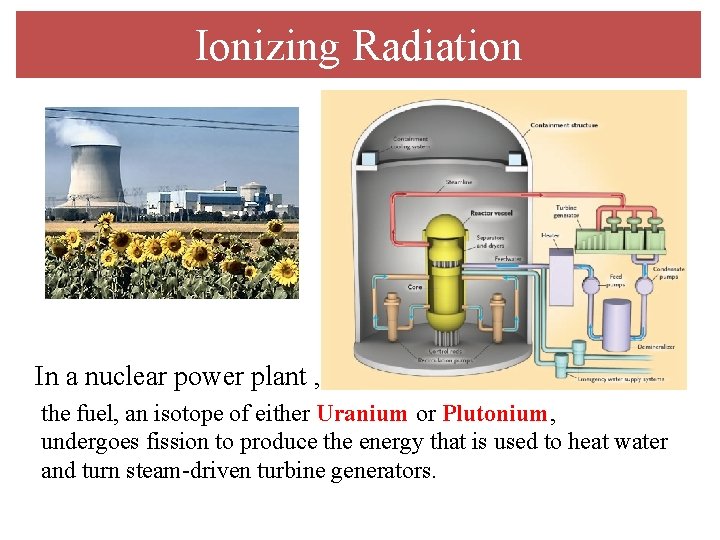
Ionizing Radiation In a nuclear power plant , the fuel, an isotope of either Uranium or Plutonium, undergoes fission to produce the energy that is used to heat water and turn steam-driven turbine generators.
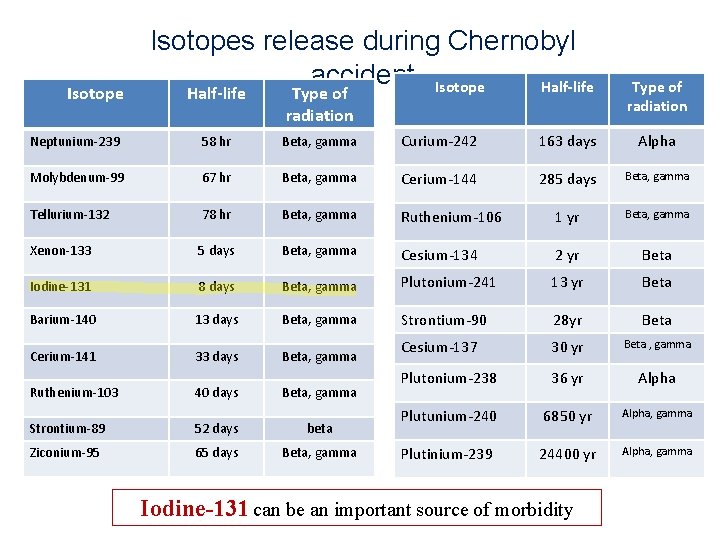
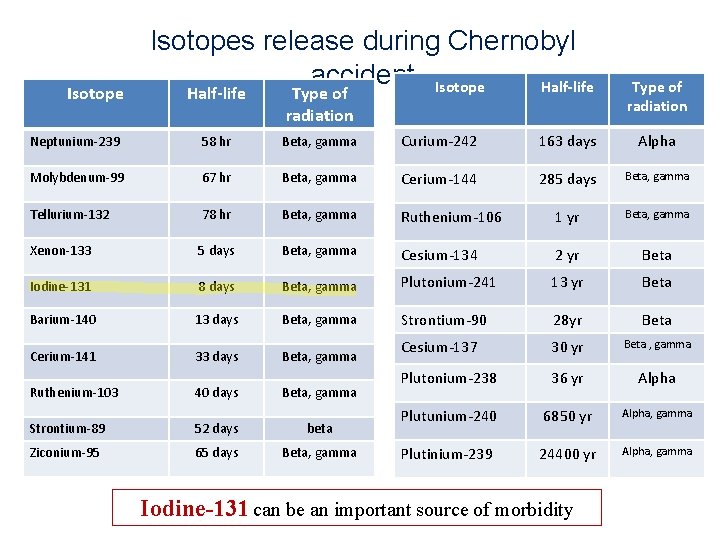
Isotopes release during Chernobyl accident Isotope Half-life Type of radiation Neptunium-239 58 hr Beta, gamma Curium-242 163 days Alpha Molybdenum-99 67 hr Beta, gamma Cerium-144 285 days Beta, gamma Tellurium-132 78 hr Beta, gamma Ruthenium-106 1 yr Beta, gamma Xenon-133 5 days Beta, gamma Cesium-134 2 yr Beta Iodine-131 8 days Beta, gamma Plutonium-241 13 yr Beta Barium-140 13 days Beta, gamma Strontium-90 28 yr Beta Cerium-141 33 days Beta, gamma Cesium-137 30 yr Beta , gamma Plutonium-238 36 yr Alpha Plutunium-240 6850 yr Alpha, gamma Plutinium-239 24400 yr Alpha, gamma Ruthenium-103 40 days Beta, gamma Strontium-89 52 days beta Ziconium-95 65 days Beta, gamma Iodine-131 can be an important source of morbidity
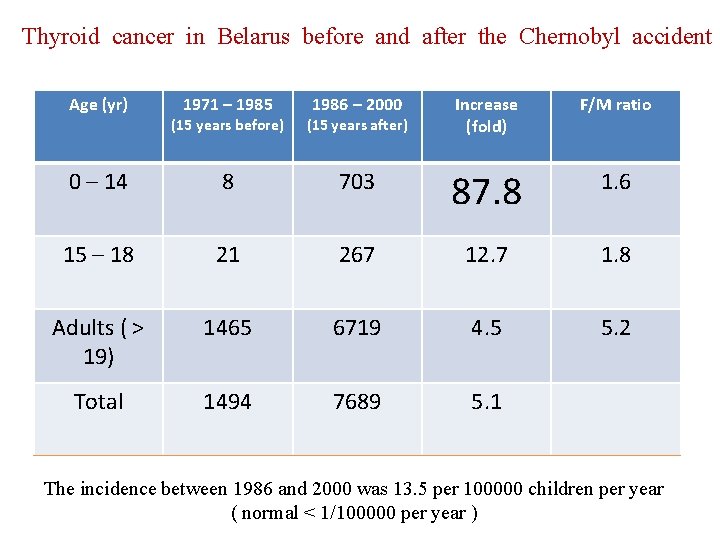
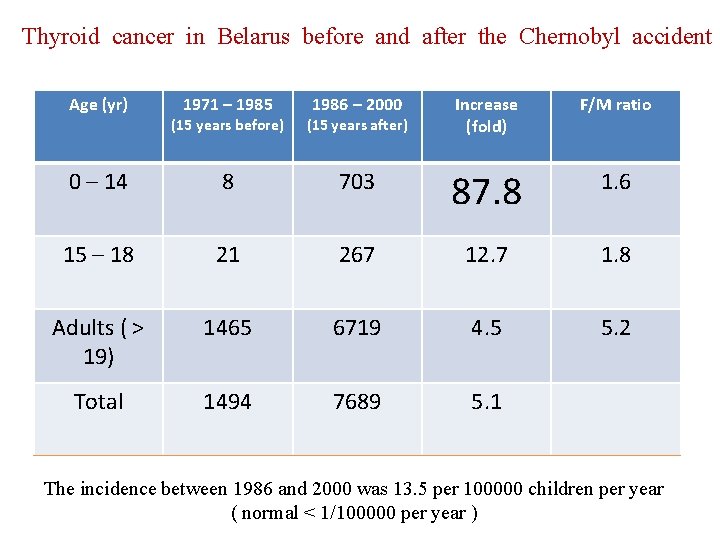
Thyroid cancer in Belarus before and after the Chernobyl accident Age (yr) 1971 – 1985 (15 years before) 1986 – 2000 (15 years after) Increase (fold) F/M ratio 0 – 14 8 703 87. 8 1. 6 15 – 18 21 267 12. 7 1. 8 Adults ( > 19) 1465 6719 4. 5 5. 2 Total 1494 7689 5. 1 The incidence between 1986 and 2000 was 13. 5 per 100000 children per year ( normal < 1/100000 per year )
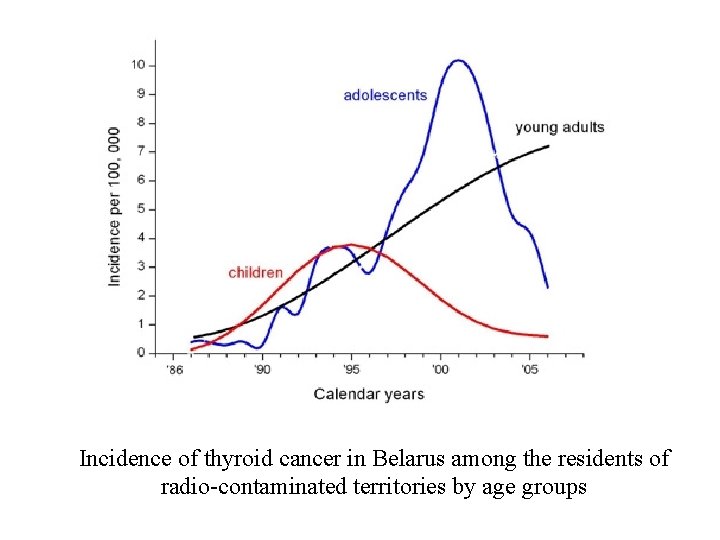
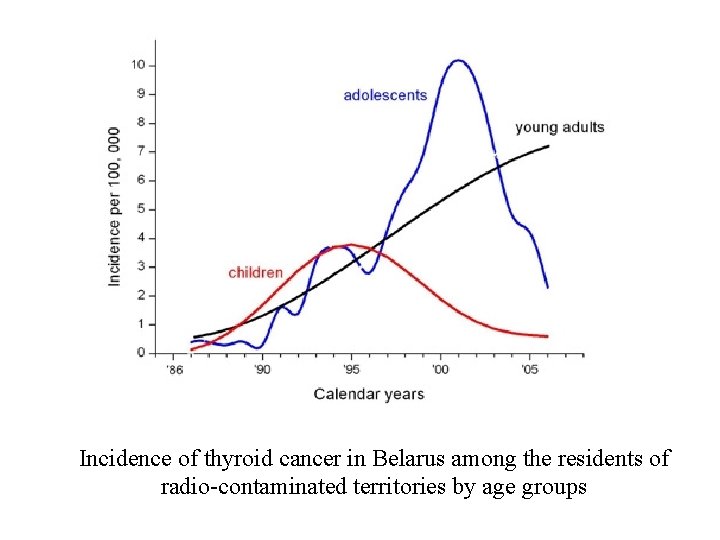
Incidence of thyroid cancer in Belarus among the residents of radio-contaminated territories by age groups
y h s i e c W den ? i e c d n i i w d i d l o r r o y h w t g n i s a e r c in
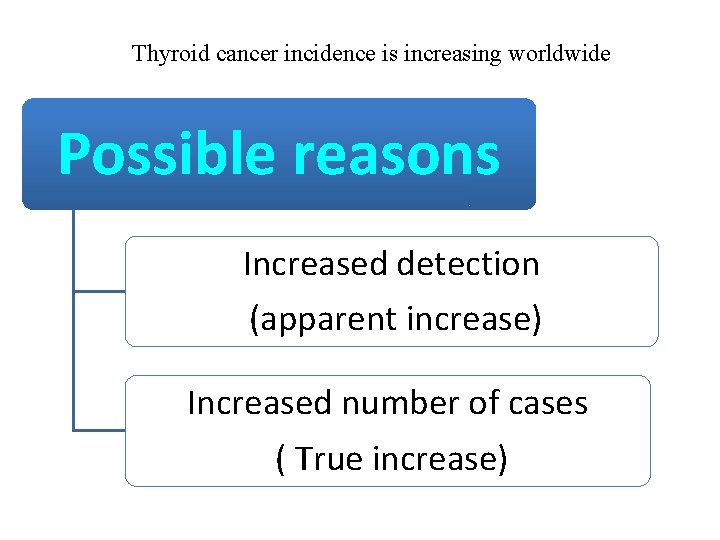
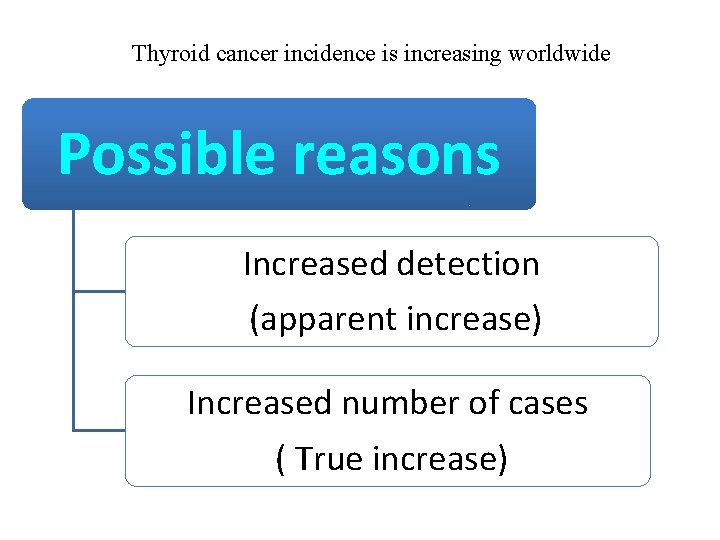
Thyroid cancer incidence is increasing worldwide Possible reasons Increased detection (apparent increase) Increased number of cases ( True increase)
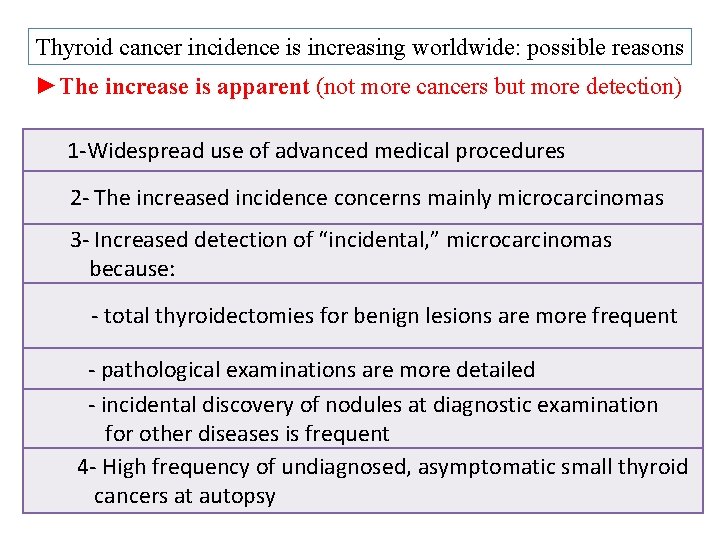
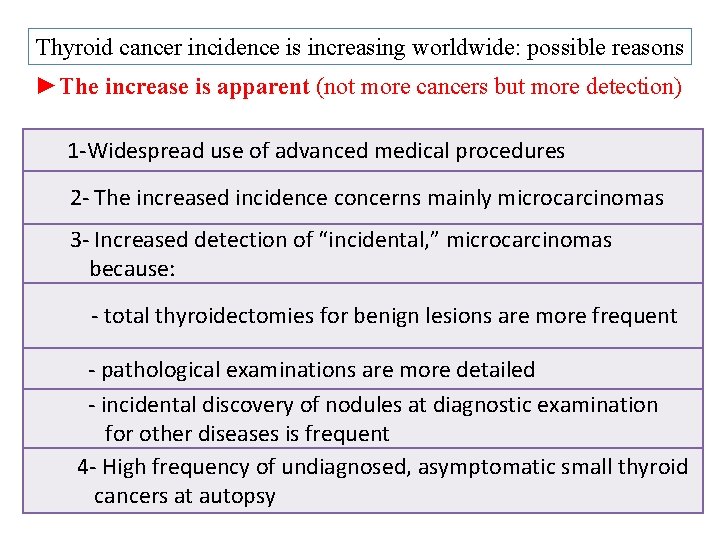
Thyroid cancer incidence is increasing worldwide: possible reasons ►The increase is apparent (not more cancers but more detection) 1 -Widespread use of advanced medical procedures 2 - The increased incidence concerns mainly microcarcinomas 3 - Increased detection of “incidental, ” microcarcinomas because: - total thyroidectomies for benign lesions are more frequent - pathological examinations are more detailed - incidental discovery of nodules at diagnostic examination for other diseases is frequent 4 - High frequency of undiagnosed, asymptomatic small thyroid cancers at autopsy
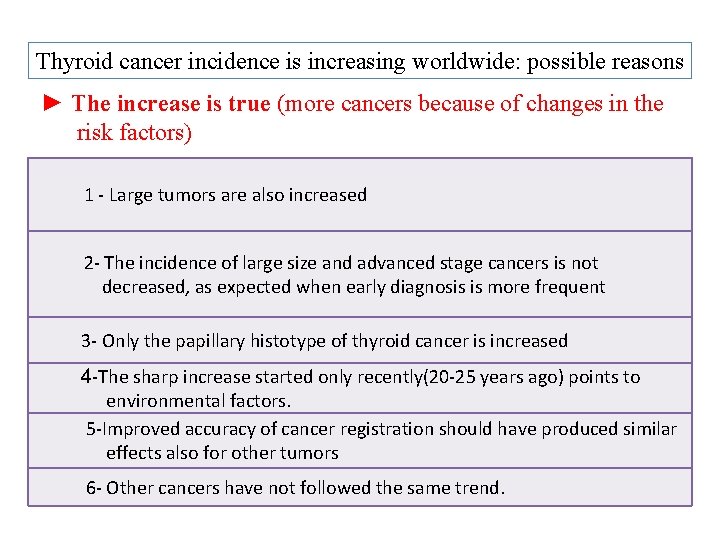
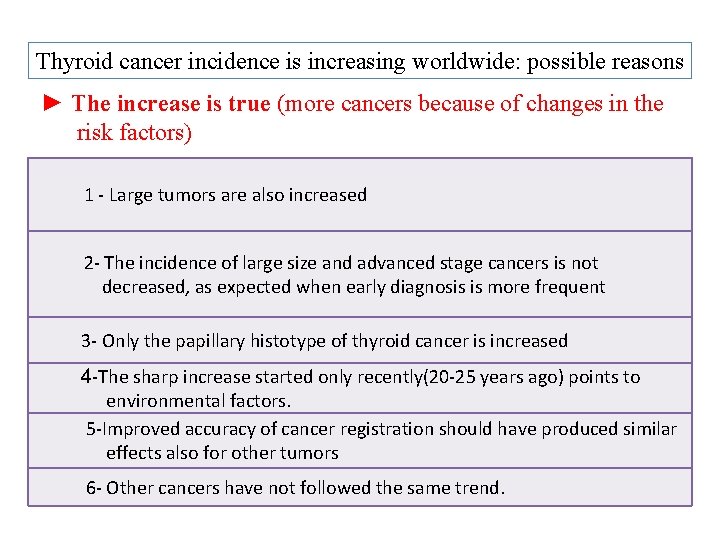
Thyroid cancer incidence is increasing worldwide: possible reasons ► The increase is true (more cancers because of changes in the risk factors) 1 - Large tumors are also increased 2 - The incidence of large size and advanced stage cancers is not decreased, as expected when early diagnosis is more frequent 3 - Only the papillary histotype of thyroid cancer is increased 4 -The sharp increase started only recently(20 -25 years ago) points to environmental factors. 5 -Improved accuracy of cancer registration should have produced similar effects also for other tumors 6 - Other cancers have not followed the same trend.
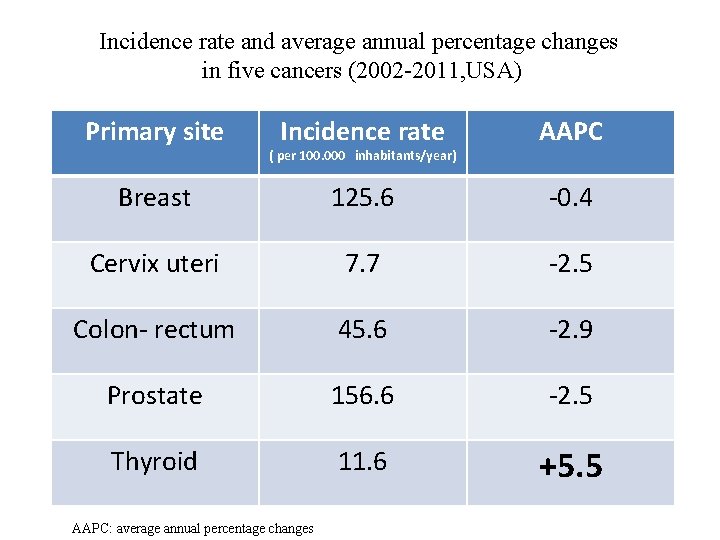
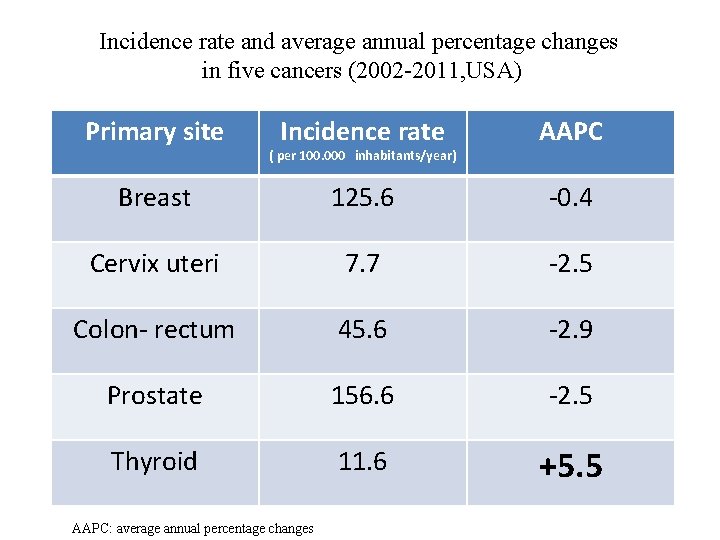
Incidence rate and average annual percentage changes in five cancers (2002 -2011, USA) Primary site Incidence rate AAPC Breast 125. 6 -0. 4 Cervix uteri 7. 7 -2. 5 Colon- rectum 45. 6 -2. 9 Prostate 156. 6 -2. 5 Thyroid 11. 6 +5. 5 ( per 100. 000 inhabitants/year) AAPC: average annual percentage changes
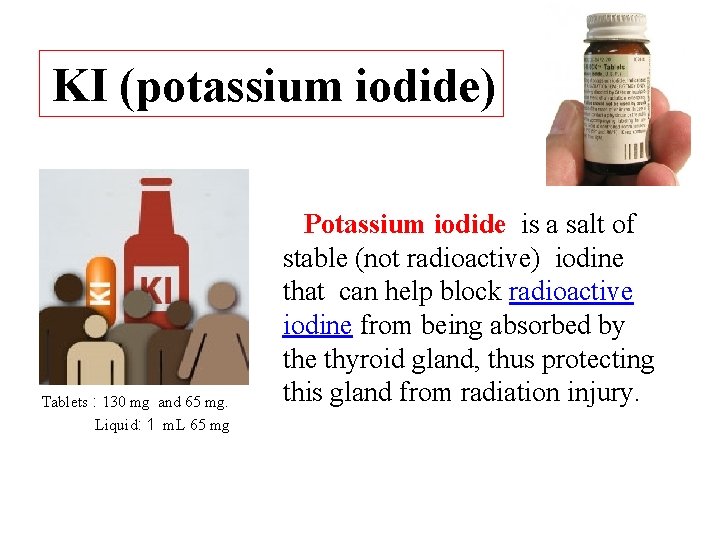
KI (potassium iodide) Tablets : 130 mg and 65 mg. Liquid: 1 m. L 65 mg Potassium iodide is a salt of stable (not radioactive) iodine that can help block radioactive iodine from being absorbed by the thyroid gland, thus protecting this gland from radiation injury.
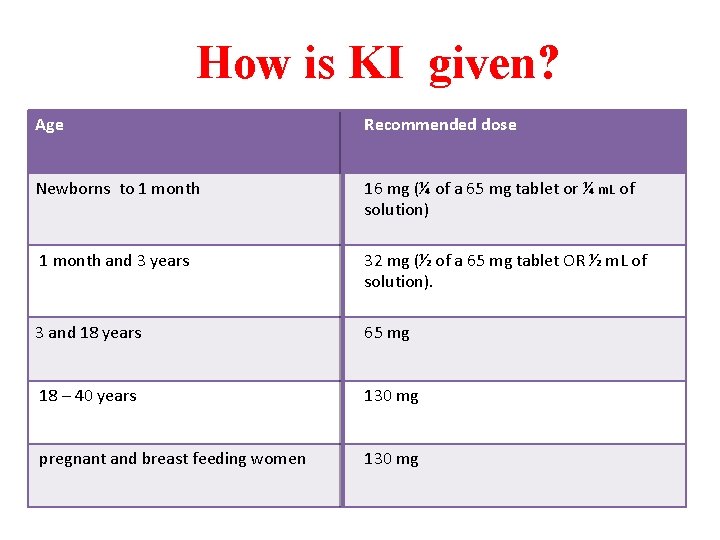
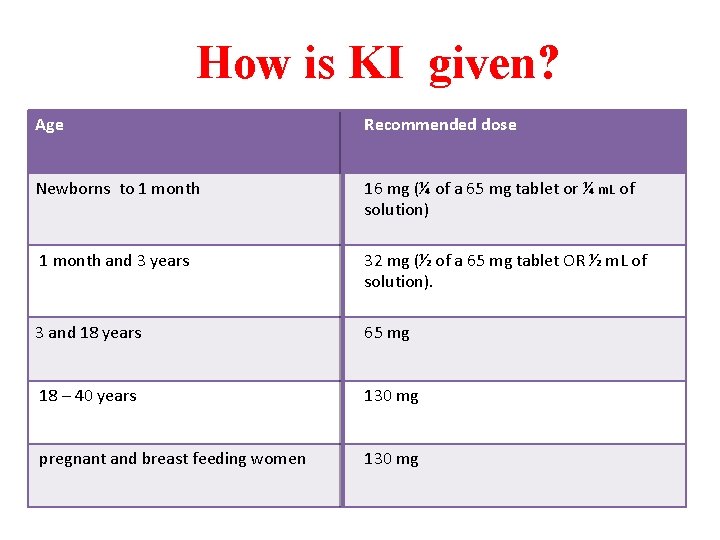
How is KI given? Age Recommended dose Newborns to 1 month 16 mg (¼ of a 65 mg tablet or ¼ m. L of solution) 1 month and 3 years 32 mg (½ of a 65 mg tablet OR ½ m. L of solution). 3 and 18 years 65 mg 18 – 40 years 130 mg pregnant and breast feeding women 130 mg
KI (potassium iodide) Adults older than 40 years should not take KI unless contamination with a very large dose of radioactive iodine is expected. Adults older than 40 years have the lowest chance of developing thyroid cancer or thyroid injury after contamination with radioactive iodine. Adults older than 40 are more likely to have allergic reactions to or adverse effects from KI.
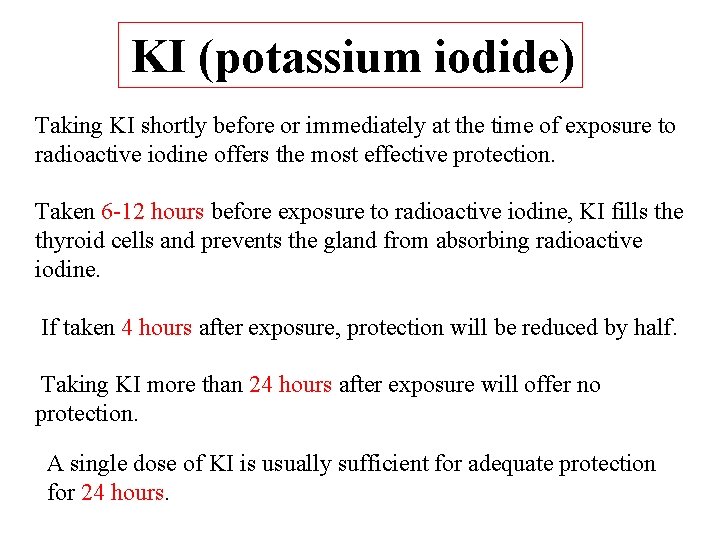
KI (potassium iodide) Taking KI shortly before or immediately at the time of exposure to radioactive iodine offers the most effective protection. Taken 6 -12 hours before exposure to radioactive iodine, KI fills the thyroid cells and prevents the gland from absorbing radioactive iodine. If taken 4 hours after exposure, protection will be reduced by half. Taking KI more than 24 hours after exposure will offer no protection. A single dose of KI is usually sufficient for adequate protection for 24 hours.
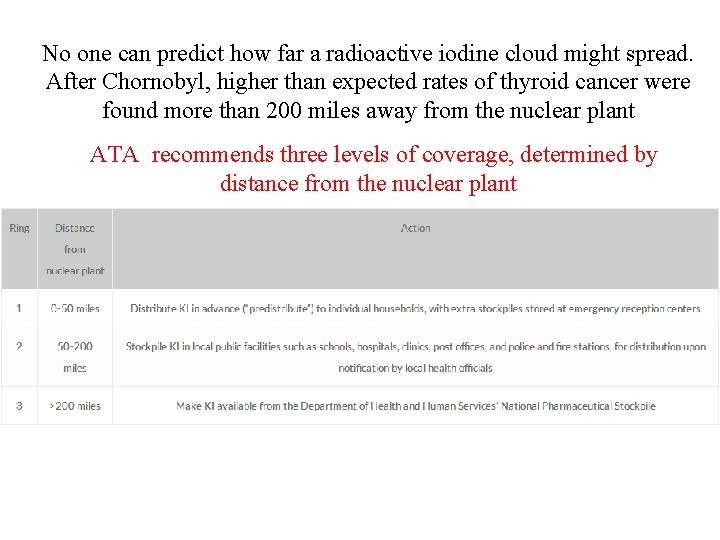
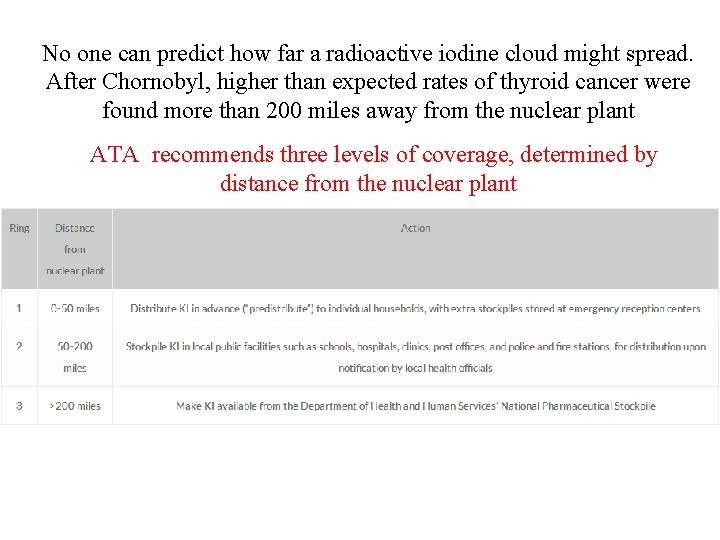
No one can predict how far a radioactive iodine cloud might spread. After Chornobyl, higher than expected rates of thyroid cancer were found more than 200 miles away from the nuclear plant ATA recommends three levels of coverage, determined by distance from the nuclear plant
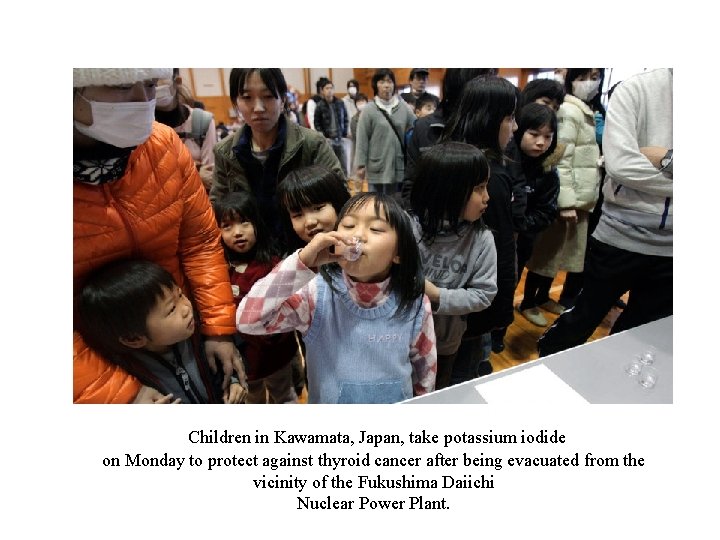
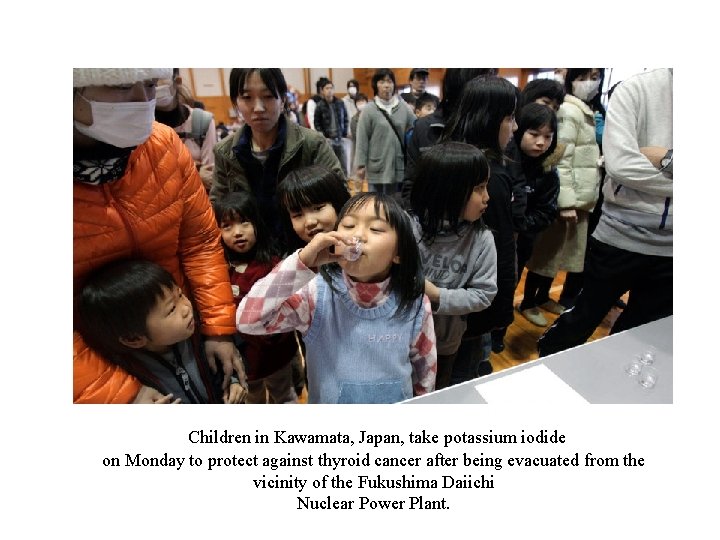
Children in Kawamata, Japan, take potassium iodide on Monday to protect against thyroid cancer after being evacuated from the vicinity of the Fukushima Daiichi Nuclear Power Plant.
Drs. Ernest Mazzaferri, Hossein Gharib, Martin Surks, and David Cooper

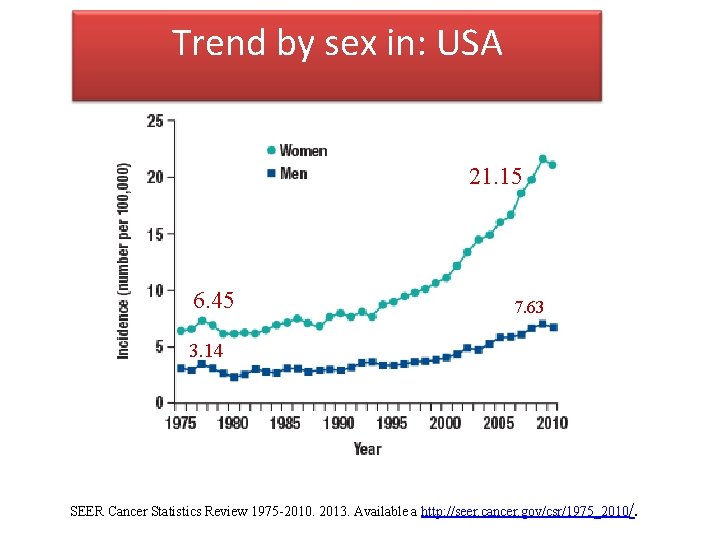
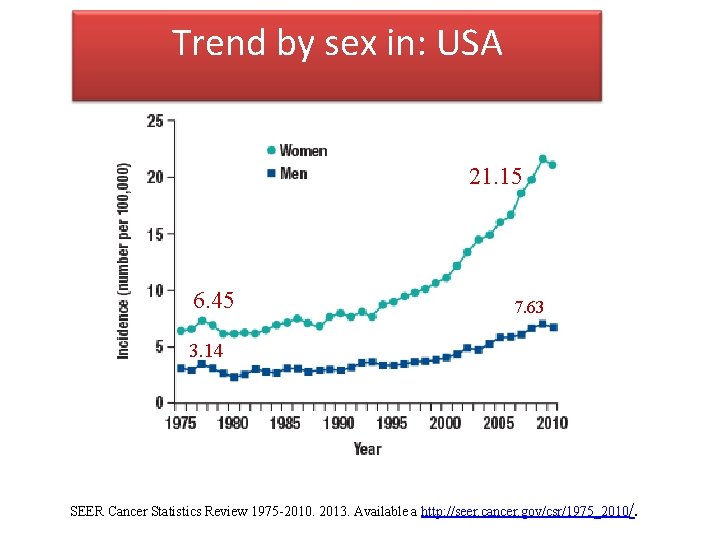
Trend by sex in: USA 21. 15 6. 45 7. 63 3. 14 SEER Cancer Statistics Review 1975 -2010. 2013. Available a http: //seer. cancer. gov/csr/1975_2010/.
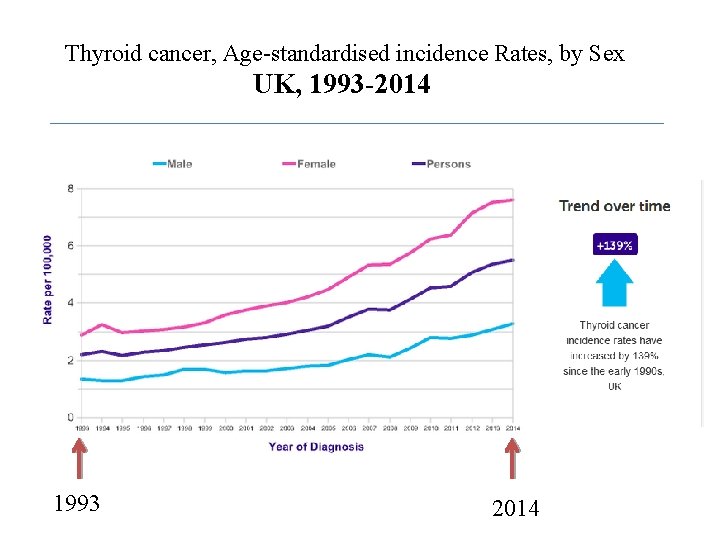
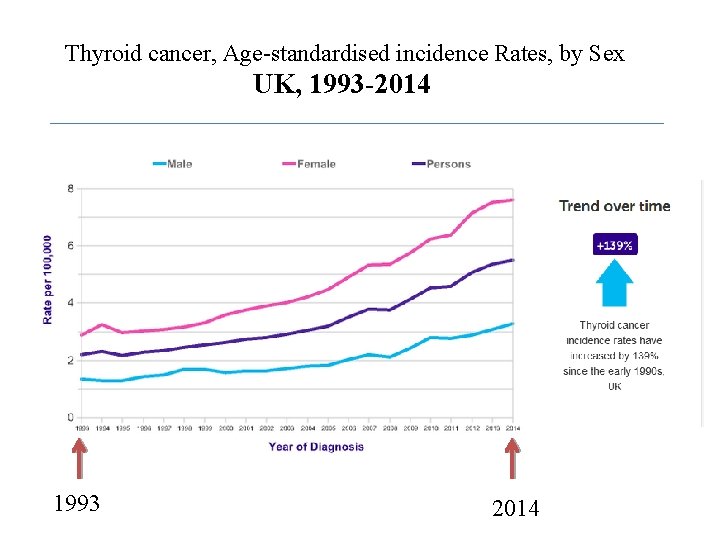
Thyroid cancer, Age-standardised incidence Rates, by Sex UK, 1993 -2014 1993 2014
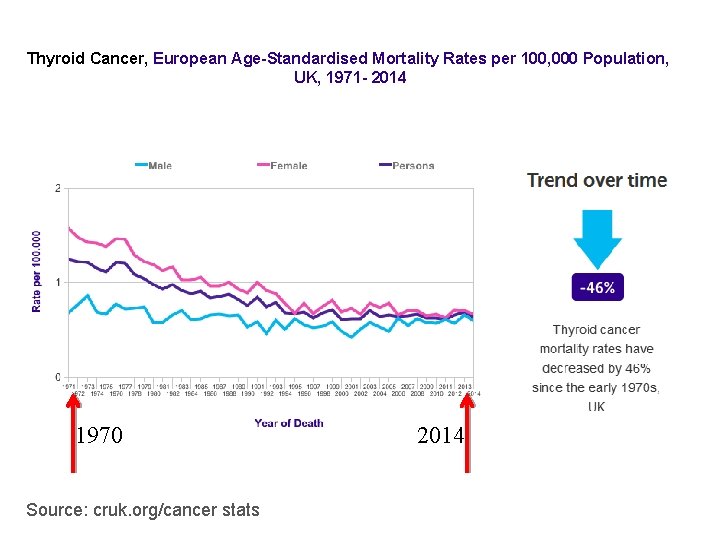
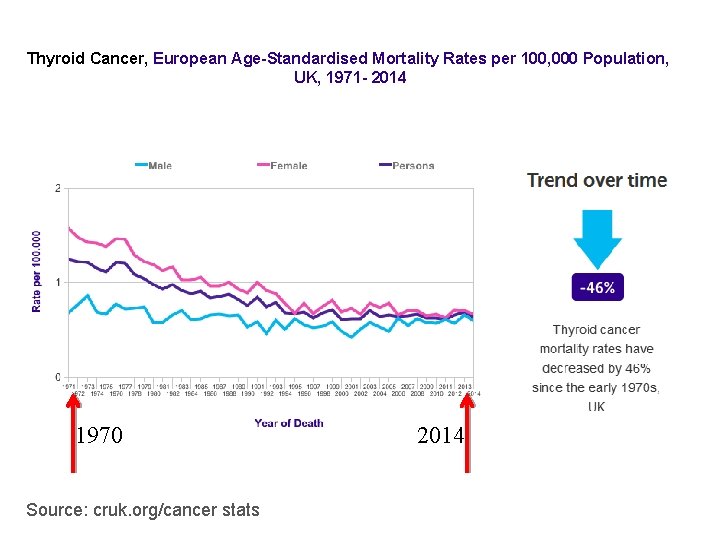
Thyroid Cancer, European Age-Standardised Mortality Rates per 100, 000 Population, UK, 1971 - 2014 1970 Source: cruk. org/cancer stats 2014
 Jeff lobe
Jeff lobe Euthyroid hashimoto's
Euthyroid hashimoto's Thyroid cancer: a case-based approach
Thyroid cancer: a case-based approach Calcitonin
Calcitonin Follicular adenoma
Follicular adenoma Esmo guidelines thyroid cancer
Esmo guidelines thyroid cancer Carbimazole side effect
Carbimazole side effect Dr swade endocrinologist
Dr swade endocrinologist Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Oha drugs
Oha drugs Endocrinologist newcastle
Endocrinologist newcastle Endocrinologist lifestyle
Endocrinologist lifestyle Dr ponder endocrinologist
Dr ponder endocrinologist Dr pang endocrinologist
Dr pang endocrinologist Terrence swade
Terrence swade Endocrinologist in parbhani
Endocrinologist in parbhani Maeve durkin
Maeve durkin Dimitrios thomas endocrinologist
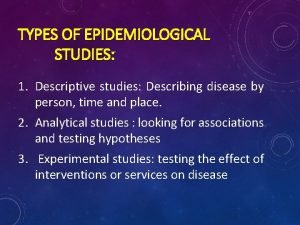
Dimitrios thomas endocrinologist Distribution in epidemiology
Distribution in epidemiology Gordon nichols
Gordon nichols Defination of epidemiology
Defination of epidemiology Thesourceagents
Thesourceagents Epidemiology definition
Epidemiology definition Meaning of epidermiology
Meaning of epidermiology Field epidemiology ppt
Field epidemiology ppt Ramboman acronym
Ramboman acronym Pros and cons of cross sectional study
Pros and cons of cross sectional study How to calculate prevalence
How to calculate prevalence Malaria parasites under microscope
Malaria parasites under microscope Confounding vs effect modification
Confounding vs effect modification Epidemiology kept simple
Epidemiology kept simple Epornithic
Epornithic Descriptive epidemiology
Descriptive epidemiology Orlies
Orlies Perbedaan relative risk dan odds ratio
Perbedaan relative risk dan odds ratio Define epidemiology
Define epidemiology Prevalence definition epidemiology
Prevalence definition epidemiology Define epidemiology
Define epidemiology Wheel of causation vs web of causation
Wheel of causation vs web of causation Descriptive vs analytic epidemiology examples
Descriptive vs analytic epidemiology examples Secondary attack rate formula
Secondary attack rate formula Distribution in epidemiology
Distribution in epidemiology Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology What is descriptive study in epidemiology
What is descriptive study in epidemiology Recall bias example
Recall bias example Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Advantages and disadvantages of nutritional epidemiology
Advantages and disadvantages of nutritional epidemiology Epidemiological triad
Epidemiological triad How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Period prevalence formula
Period prevalence formula Attack rate calculation
Attack rate calculation How dr. wafaa elsadr epidemiology professor
How dr. wafaa elsadr epidemiology professor Ramboman analysis
Ramboman analysis Spurious association
Spurious association Formula for attack rate
Formula for attack rate Incidence vs prevalence
Incidence vs prevalence John snow epidemiology
John snow epidemiology Logistic regression epidemiology
Logistic regression epidemiology Epi
Epi Nodular goiter
Nodular goiter Negative feedback of thyroid hormone
Negative feedback of thyroid hormone Ames thyroid
Ames thyroid