Thyroid Pathology Last Updated Oct 5 2006 Jamie

- Slides: 50
Thyroid Pathology Last Updated Oct. 5, 2006 Jamie Tibbo Reviewed with Dr. Jane Thomas
Overview • Benign Pathology – – Hashimoto’s Thyroiditis Grave’s Disease Multi-nodular goiter Follicular Adenoma • Malignant Pathology – – Papillary Carcinoma Follicular Carcinoma Medullary Carcinoma Anaplastic Carcinoma
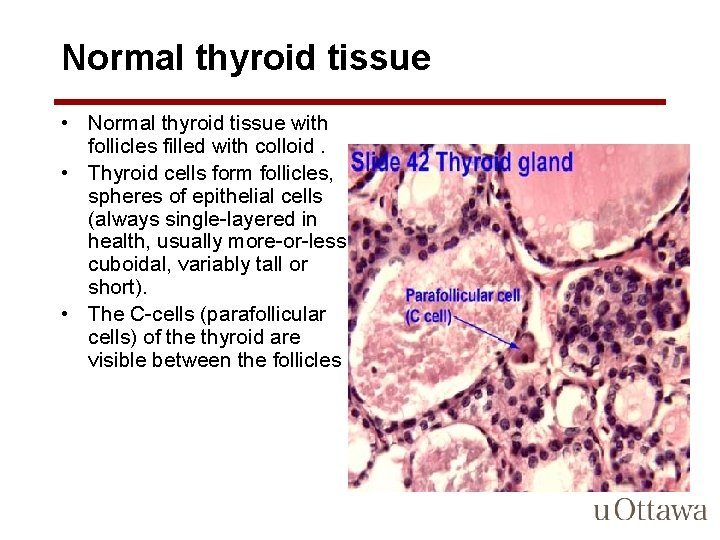
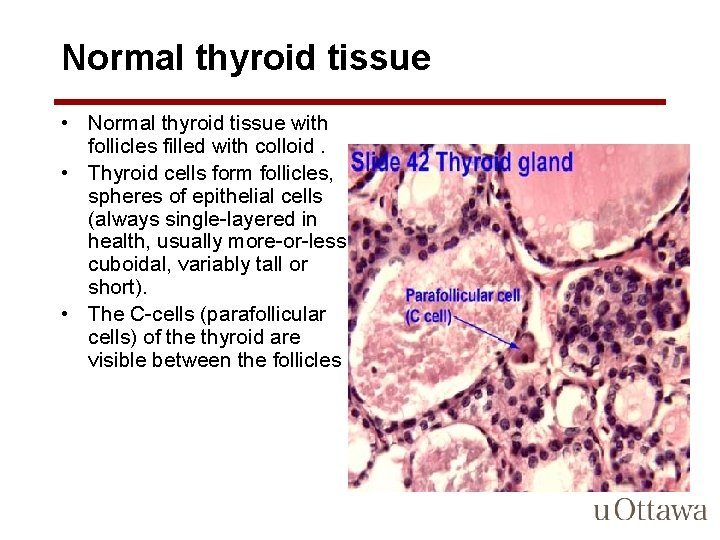
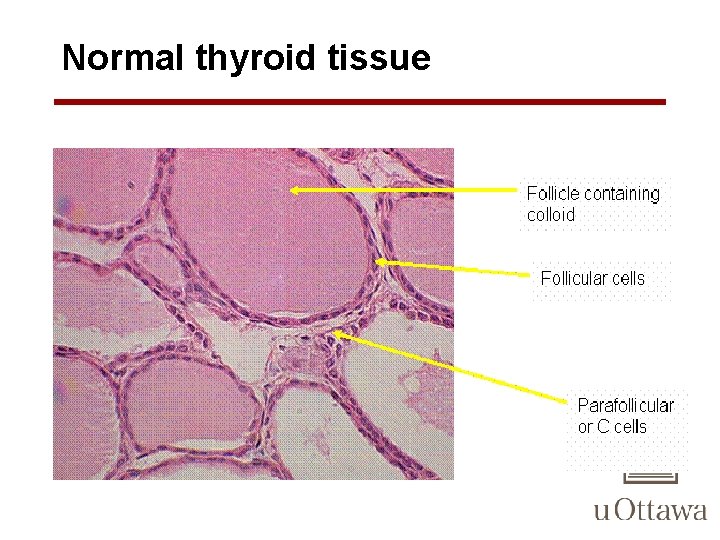
Normal thyroid tissue • Normal thyroid tissue with follicles filled with colloid. • Thyroid cells form follicles, spheres of epithelial cells (always single-layered in health, usually more-or-less cuboidal, variably tall or short). • The C-cells (parafollicular cells) of the thyroid are visible between the follicles
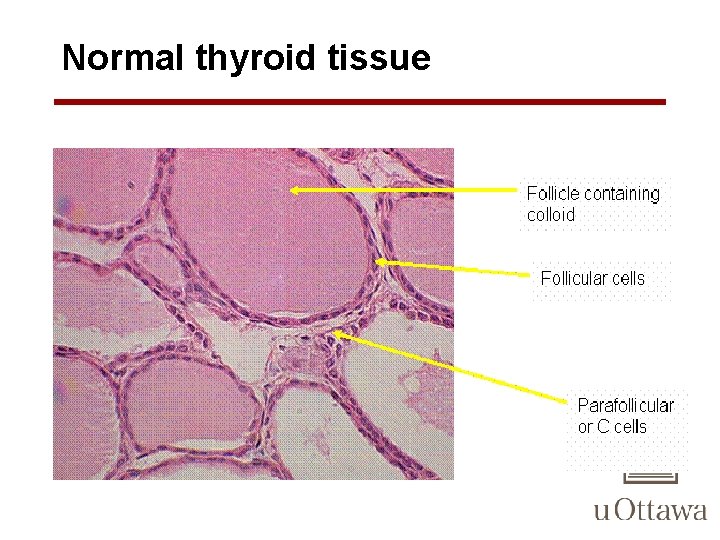
Normal thyroid tissue
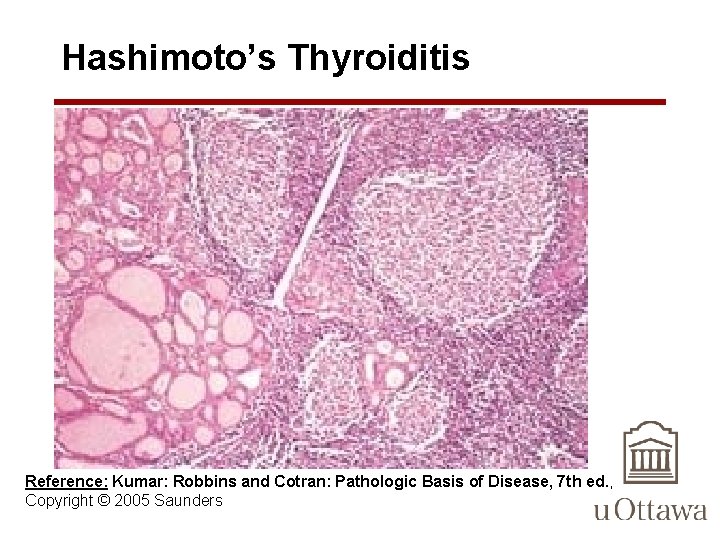
Hashimoto’s Thyroiditis • an autoimmune disease in which the immune system reacts against a variety of thyroid antigens • overriding feature of is progressive depletion of thyroid epithelial cells (thyrocytes), which are gradually replaced by mononuclear cell infiltration and fibrosis
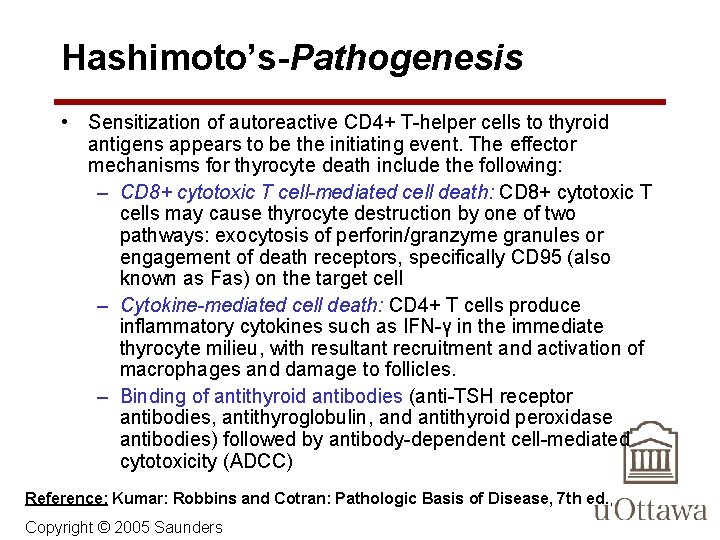
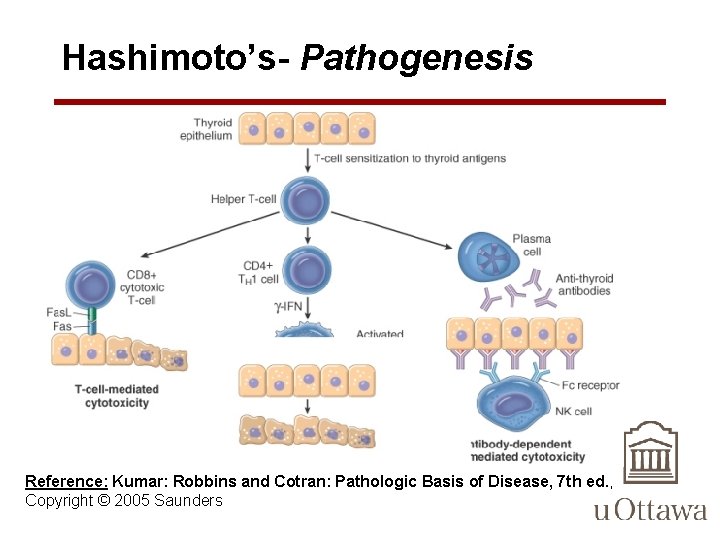
Hashimoto’s-Pathogenesis • Sensitization of autoreactive CD 4+ T-helper cells to thyroid antigens appears to be the initiating event. The effector mechanisms for thyrocyte death include the following: – CD 8+ cytotoxic T cell-mediated cell death: CD 8+ cytotoxic T cells may cause thyrocyte destruction by one of two pathways: exocytosis of perforin/granzyme granules or engagement of death receptors, specifically CD 95 (also known as Fas) on the target cell – Cytokine-mediated cell death: CD 4+ T cells produce inflammatory cytokines such as IFN-γ in the immediate thyrocyte milieu, with resultant recruitment and activation of macrophages and damage to follicles. – Binding of antithyroid antibodies (anti-TSH receptor antibodies, antithyroglobulin, and antithyroid peroxidase antibodies) followed by antibody-dependent cell-mediated cytotoxicity (ADCC) Reference: Kumar: Robbins and Cotran: Pathologic Basis of Disease, 7 th ed. , Copyright © 2005 Saunders
Hashimoto’s- Pathogenesis Reference: Kumar: Robbins and Cotran: Pathologic Basis of Disease, 7 th ed. , Copyright © 2005 Saunders
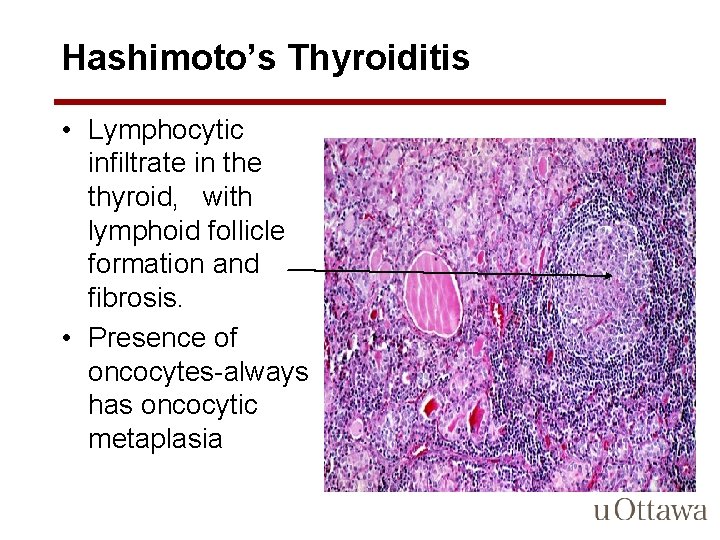
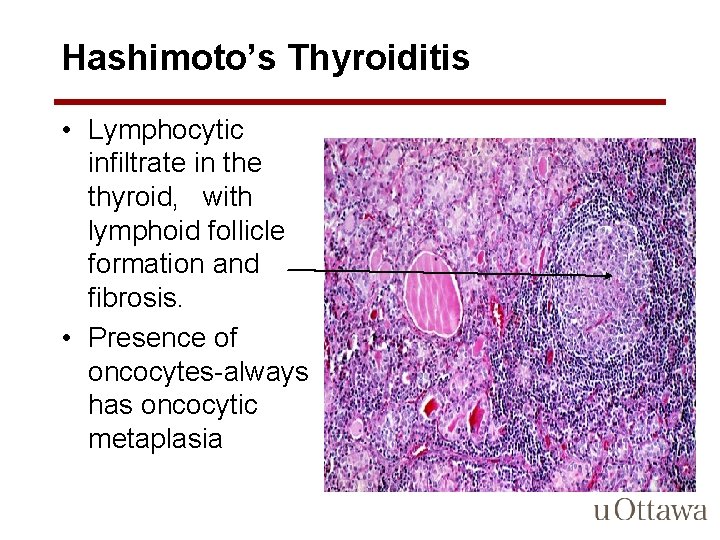
Hashimoto’s Thyroiditis • Lymphocytic infiltrate in the thyroid, with lymphoid follicle formation and fibrosis. • Presence of oncocytes-always has oncocytic metaplasia
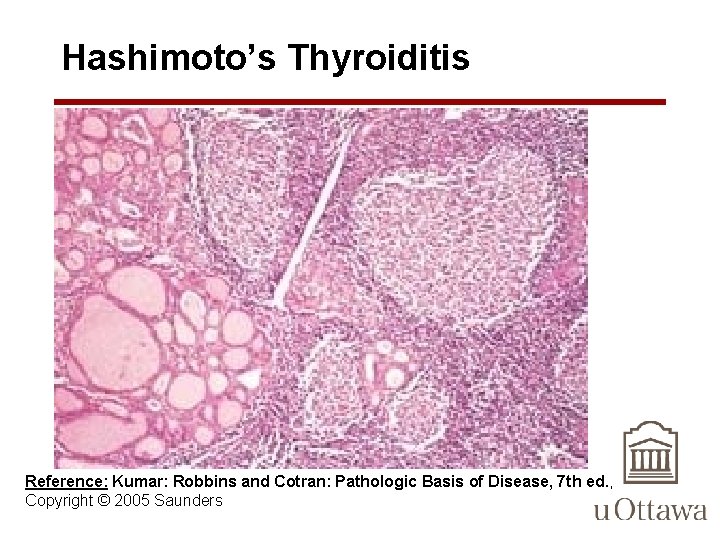
Hashimoto’s Thyroiditis Reference: Kumar: Robbins and Cotran: Pathologic Basis of Disease, 7 th ed. , Copyright © 2005 Saunders
Grave’s Disease
Multi-nodular Goiter

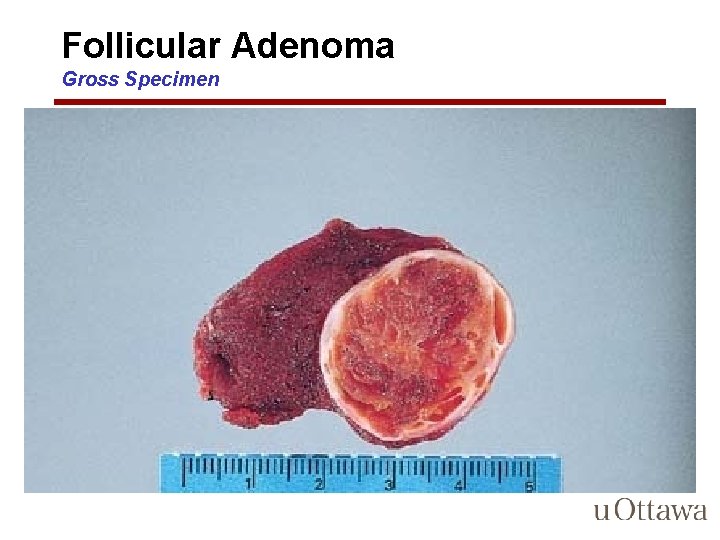
Follicular Adenoma • adenomas are not forerunners of cancer except in rare instances • small proportion produce thyroid hormones and cause clinically apparent thyrotoxicosis • Typically a solitary, spherical, encapsulated lesion that is well demarcated from the surrounding thyroid parenchyma
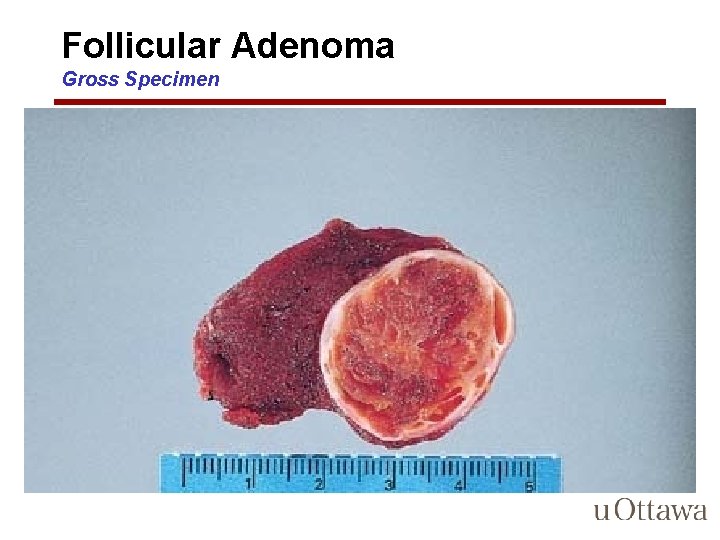
Follicular Adenoma Gross Specimen
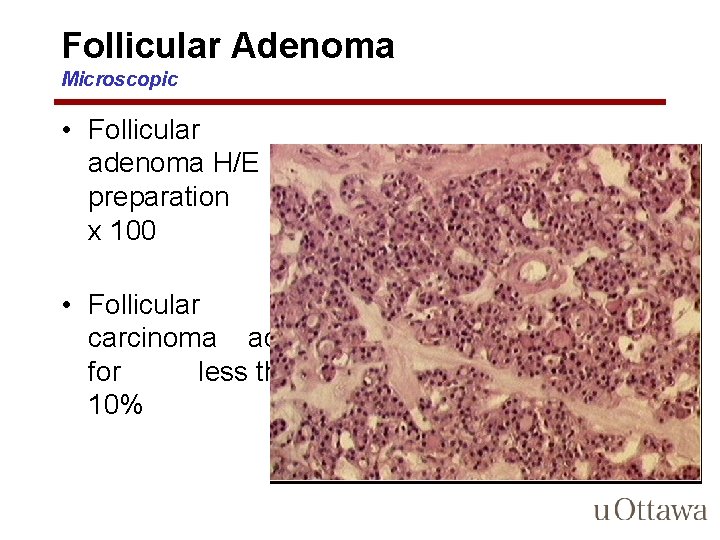
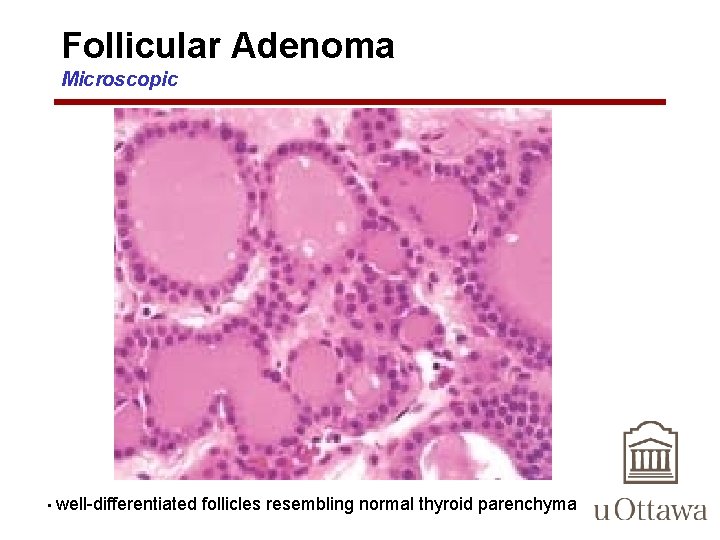
Follicular Adenoma Microscopic • Microscopically, the constituent cells often form uniform-appearing follicles that contain colloid • The follicular growth pattern within the adenoma is usually quite distinct from the adjacent non-neoplastic thyroid – distinguishing feature b/w adenomas and MNG- nodular and uninvolved thyroid parenchyma may have similar growth patterns
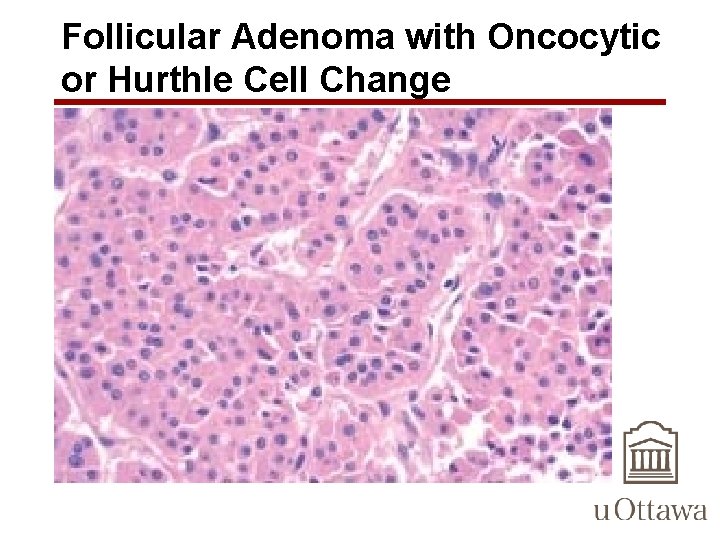
Follicular Adenoma Microscopic • Mitotic figures are rare • papillary change is not a typical feature of adenomas and, if extensive, should raise the suspicion of an encapsulated papillary carcinoma • Occasionally, the neoplastic cells acquire brightly eosinophilic granular cytoplasm (oxyphil or Hürthle cell change)
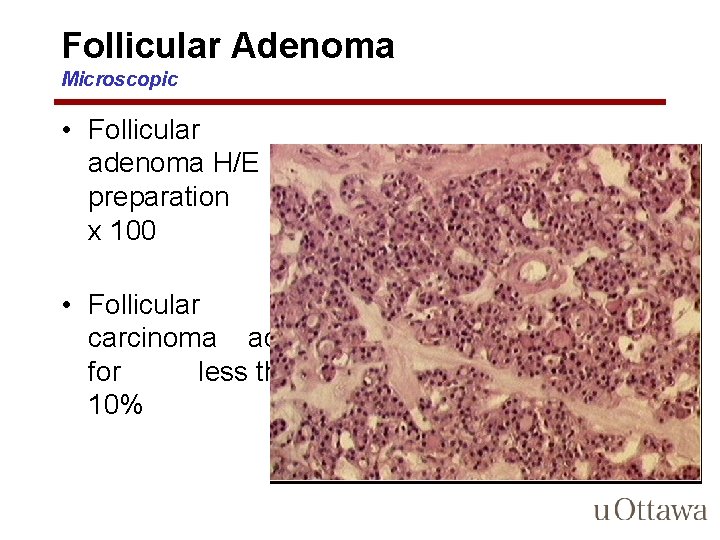
Follicular Adenoma Microscopic • Follicular adenoma H/E preparation x 100 • Follicular carcinoma account for less than 10%
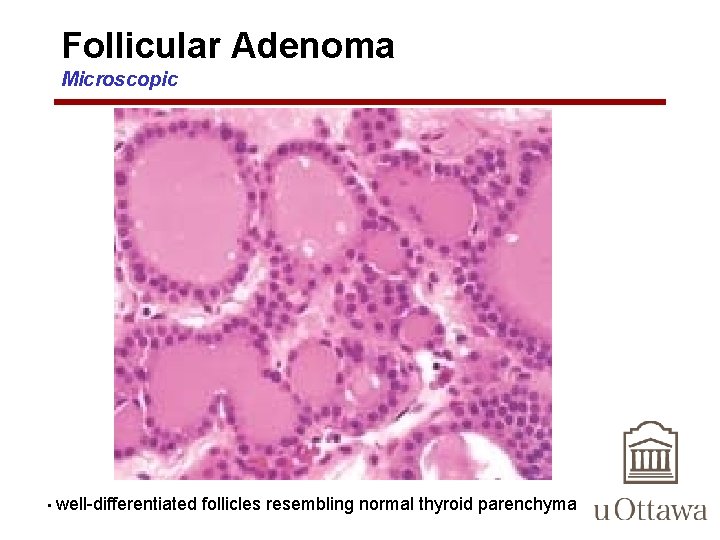
Follicular Adenoma Microscopic • well-differentiated follicles resembling normal thyroid parenchyma
Follicular Adenoma with Oncocytic or Hurthle Cell Change • Also known as: – Hurthle Cell Adenoma • Occasionally, the neoplastic cells acquire brightly eosinophilic granular cytoplasm (oxyphil or Hürthle cell change) – Eosinophilic granules due to enlarged, bizarre mitochondria
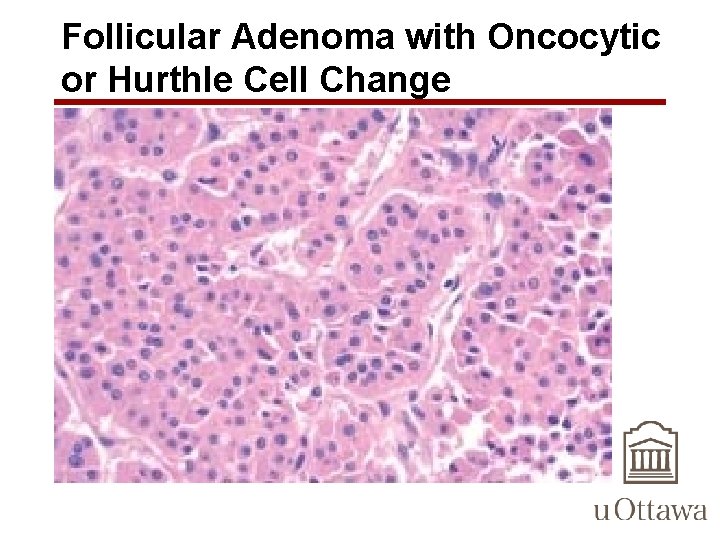
Follicular Adenoma with Oncocytic or Hurthle Cell Change
Thyroid Neoplasms with Follicular Architecture • Non-Neoplastic: – Hyperplastic nodule in Goiter • Neoplastic: – Follicular adenoma – Follicular carcinoma – Follicular variant Papillary carcinoma
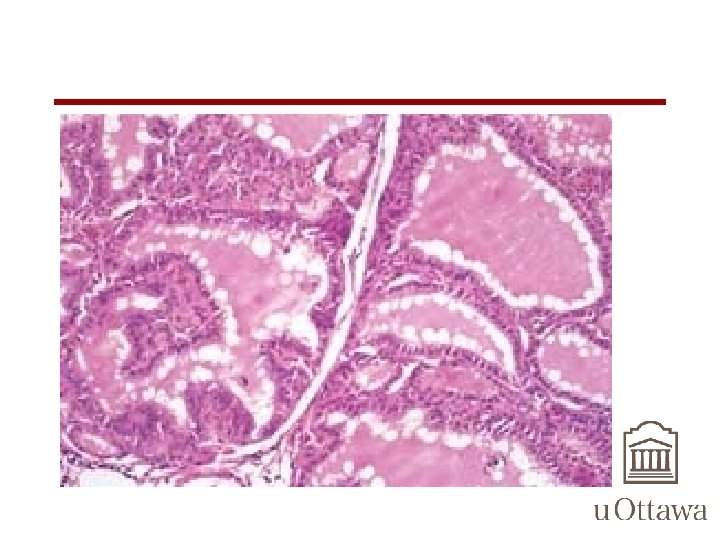
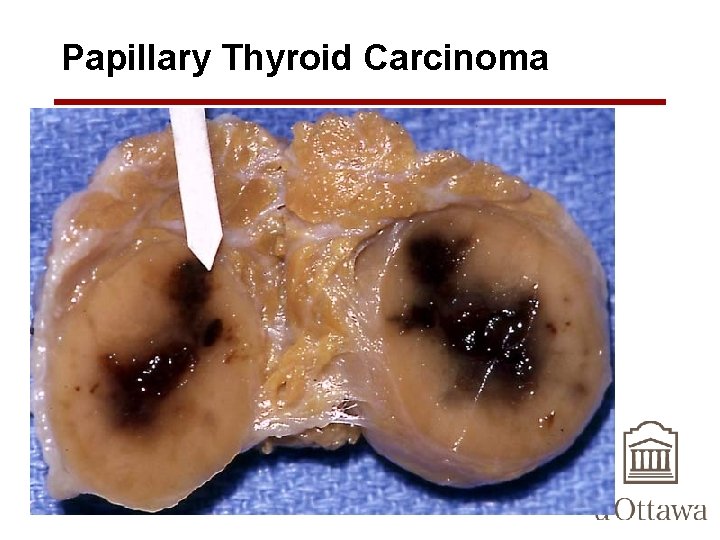
Papillary Thyroid Carcinoma • solitary or multifocal lesions • Some tumors well-circumscribed and encapsulated; others infiltrate the adjacent parenchyma with ill-defined margins • may contain areas of fibrosis and calcification and are often cystic
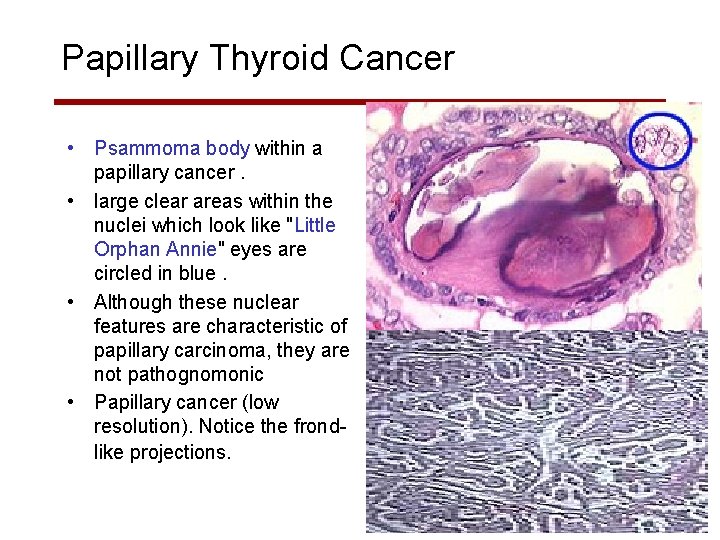
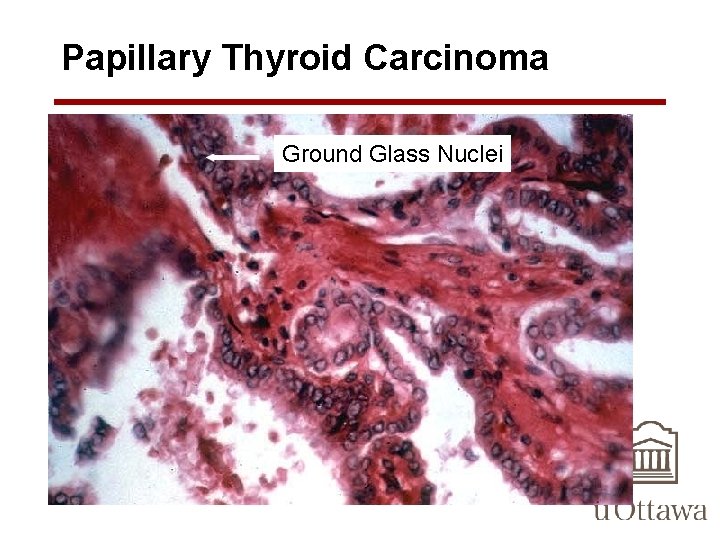
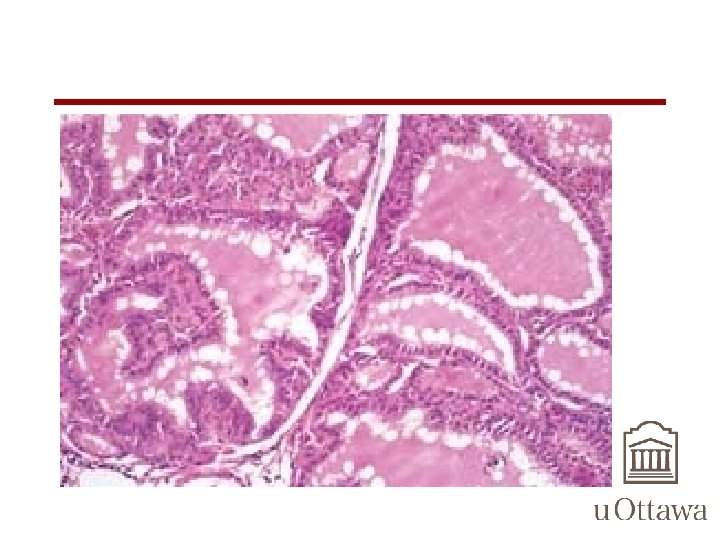
Papillary Thyroid Carcinoma • can contain branching papillae having a fibrovascular stalk covered by a single to multiple layers of cuboidal epithelial cells • NUCLEI of papillary carcinoma cells contain finely dispersed chromatin, which imparts an optically clear or empty appearance, giving rise to the designation ground glass or Orphan Annie eye nuclei • invaginations of the cytoplasm may in cross-sections give the appearance of intranuclear inclusions ("pseudo-inclusions") or intranuclear grooves
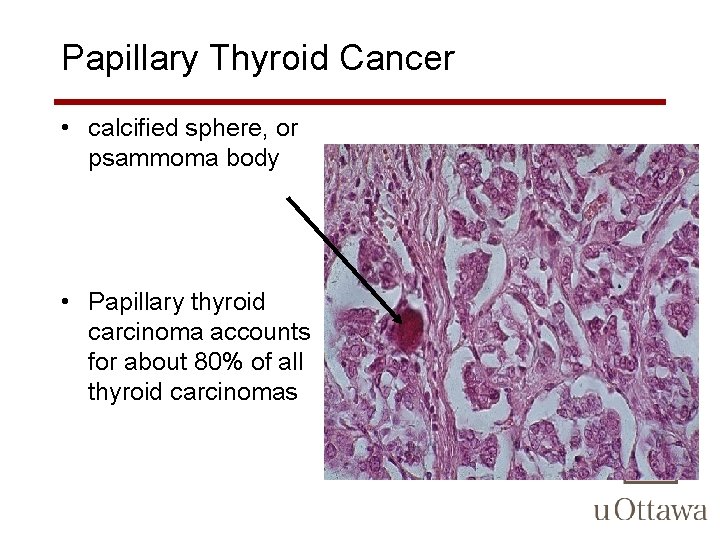
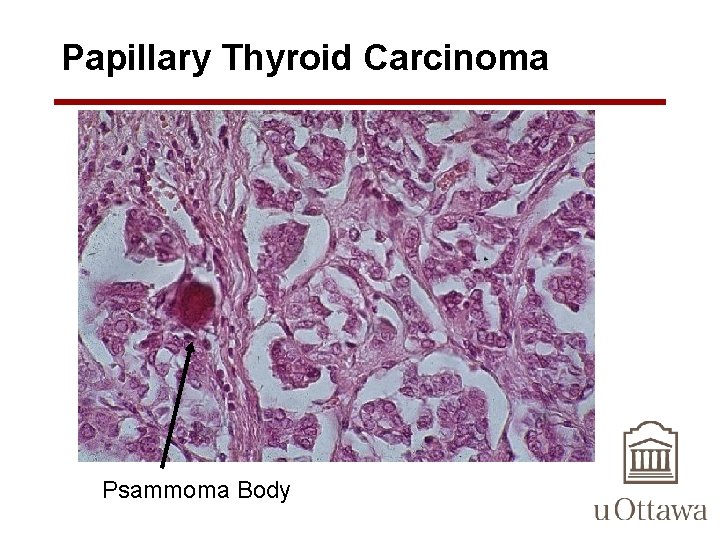
Papillary Thyroid Carcinoma • the diagnosis of papillary carcinoma is based on these nuclear features even in the absence of papillary architecture. • Concentrically calcified structures termed psammoma bodies are often present within the lesion, usually within the cores of papillae – These structures are almost never found in follicular and medullary carcinomas, and so, when present, they are a strong indication that the lesion is a papillary carcinoma – whenever a psammoma body is found within a lymph node or perithyroidal tissues, a hidden papillary carcinoma must be considered
Papillary Thyroid Carcinoma • Foci of lymphatic invasion by tumor are often present, but involvement of blood vessels is relatively uncommon • Metastases to adjacent cervical lymph nodes are estimated to occur in up to half the cases ? ? ?
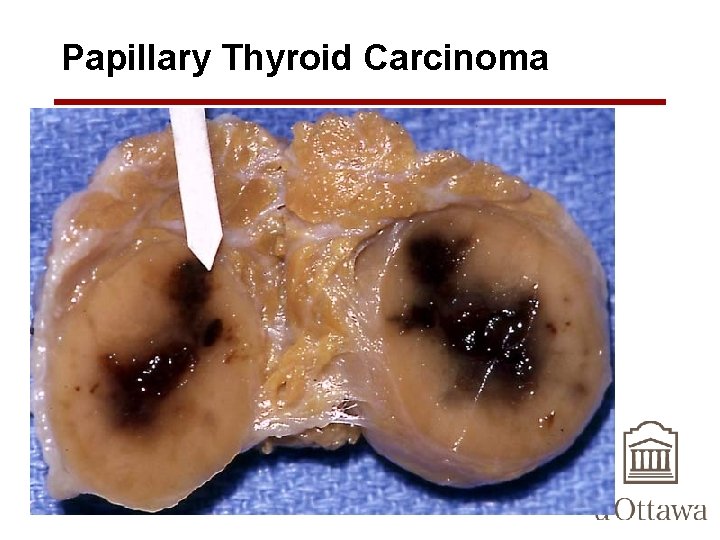
Papillary Thyroid Carcinoma
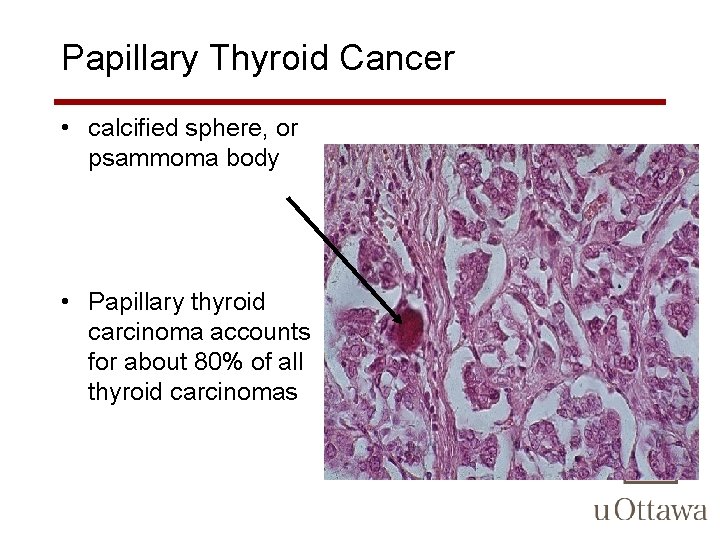
Papillary Thyroid Cancer • calcified sphere, or psammoma body • Papillary thyroid carcinoma accounts for about 80% of all thyroid carcinomas
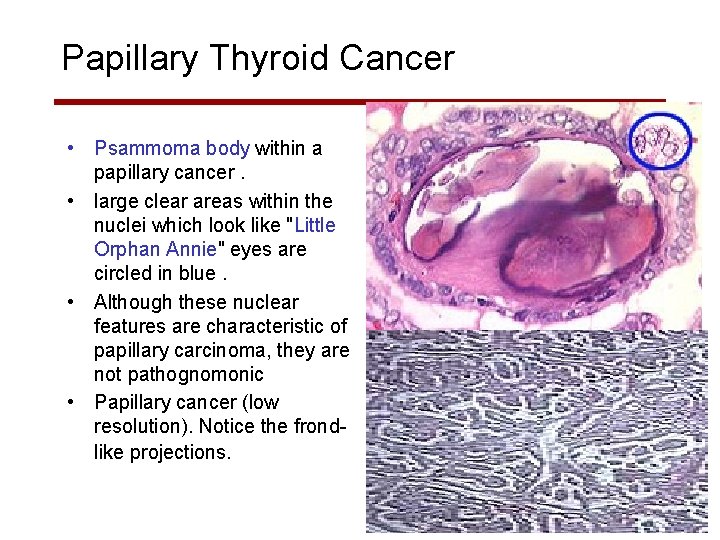
Papillary Thyroid Cancer • Psammoma body within a papillary cancer. • large clear areas within the nuclei which look like "Little Orphan Annie" eyes are circled in blue. • Although these nuclear features are characteristic of papillary carcinoma, they are not pathognomonic • Papillary cancer (low resolution). Notice the frondlike projections.
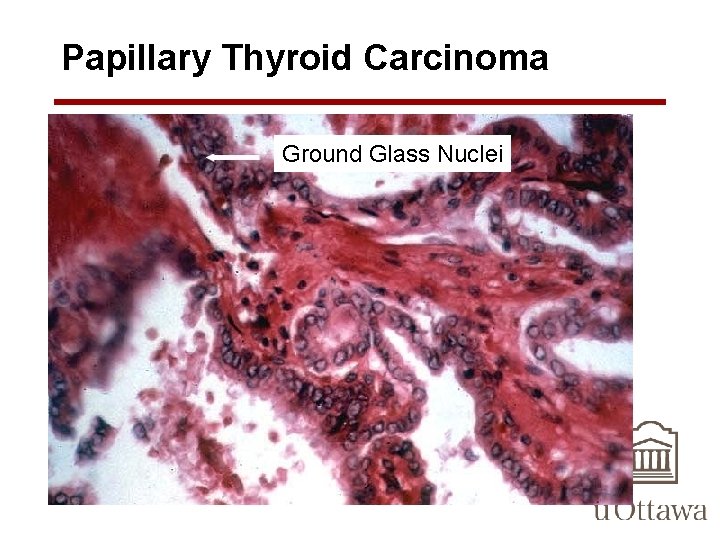
Papillary Thyroid Carcinoma Ground Glass Nuclei
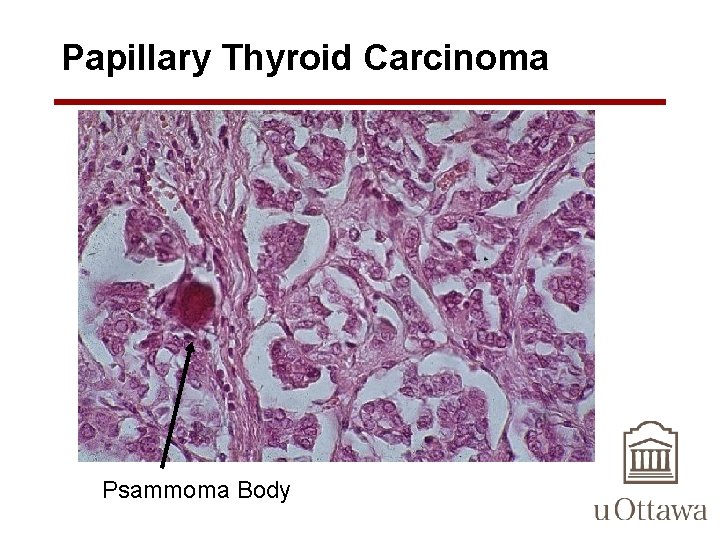
Papillary Thyroid Carcinoma Psammoma Body
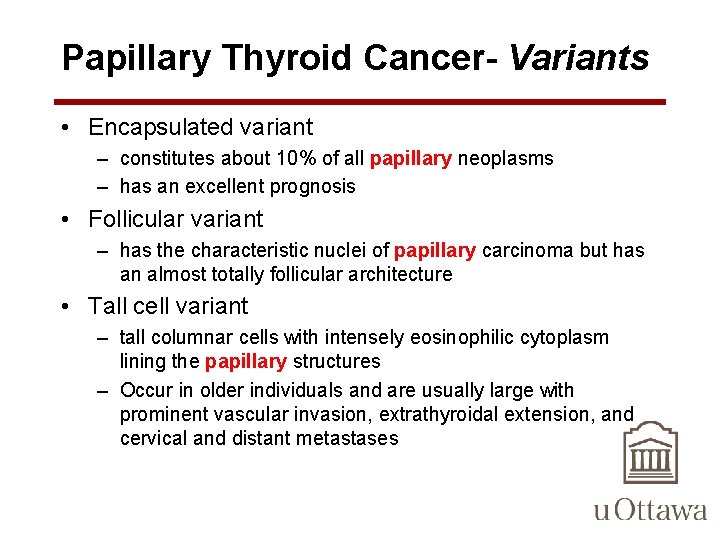
Papillary Thyroid Cancer- Variants • Encapsulated variant – constitutes about 10% of all papillary neoplasms – has an excellent prognosis • Follicular variant – has the characteristic nuclei of papillary carcinoma but has an almost totally follicular architecture • Tall cell variant – tall columnar cells with intensely eosinophilic cytoplasm lining the papillary structures – Occur in older individuals and are usually large with prominent vascular invasion, extrathyroidal extension, and cervical and distant metastases
Papillary Thyroid Cancer- Variants • Diffuse sclerosing variant – occurs in younger individuals, including children. These tumors do not present with a mass, but rather with a bilateral goiter – nodal metastases are present in almost all cases • Hyalizing trabecular tumors – includes both adenomas and carcinomas, have recently been reconsidered as a variant of papillary carcinomas, based on the presence of ret/PTC gene rearrangements in 30% to 60% of these tumors
Follicular Thyroid Carcinoma • 2 nd most common thyroid cancer – 10% to 20% of all thyroid cancers • tend to present in women, and at an older age than do papillary carcinomas – peak incidence in the forties and fifties • incidence increased in areas of dietary iodine deficiency, suggesting that in some cases, nodular goiter may predispose to the development of the neoplasm • high frequency of RAS mutations in follicular adenomas and carcinomas suggests that the two may be related tumors
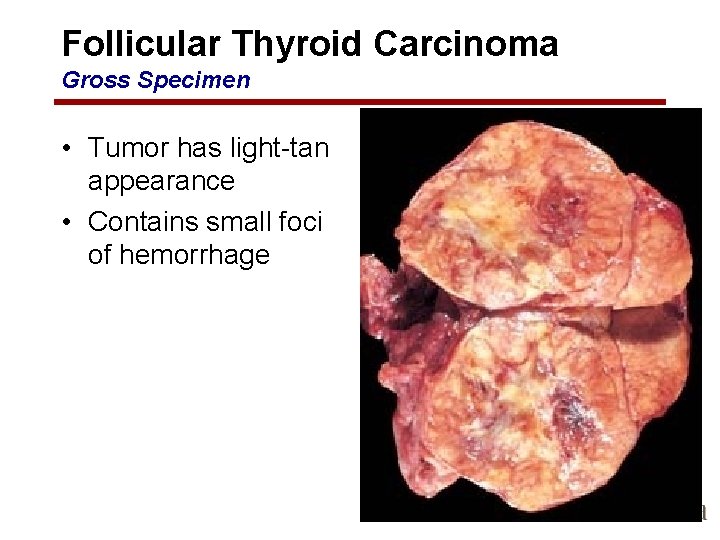
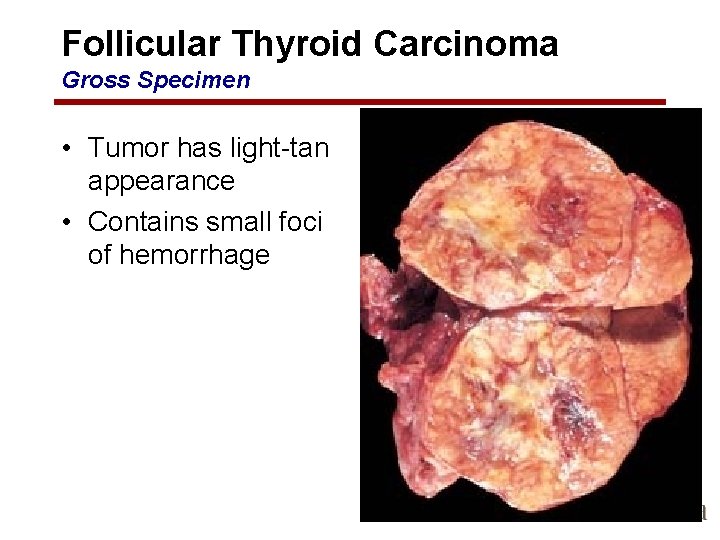
Follicular Thyroid Carcinoma Gross Specimen • Tumor has light-tan appearance • Contains small foci of hemorrhage
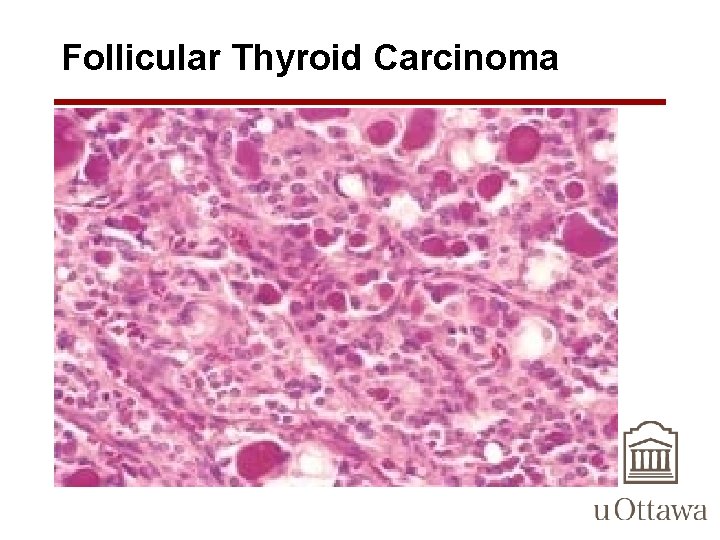
Follicular Thyroid Carcinoma Microscopic Features • Most composed of fairly uniform cells forming small follicles containing colloid appearance of normal thyroid • In other cases, follicular differentiation may be less apparent – may be nests or sheets of cells without colloid • Occasional tumors are dominated by cells with abundant granular, eosinophilic cytoplasm (Hürthle cells). • nuclei lack the features typical of papillary carcinoma • psammoma bodies are NOT present
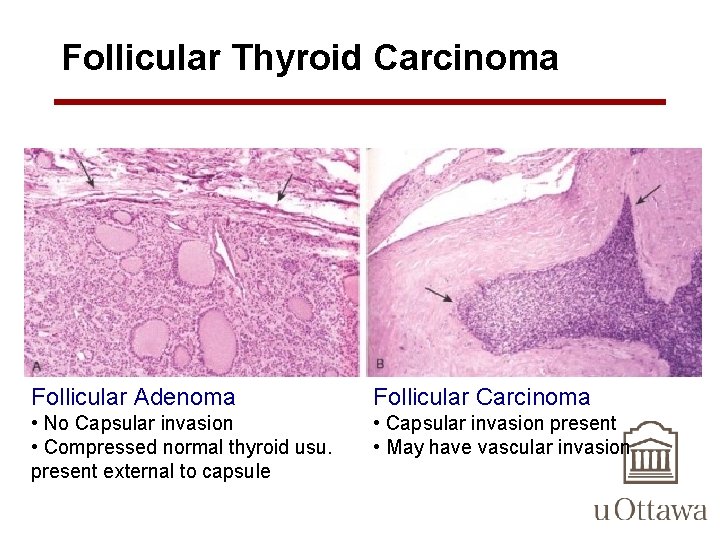
Follicular Thyroid Carcinoma Microscopic Features • Follicular lesions with nuclear features typical of papillary carcinomas should be treated as papillary cancers • Nuclear features NOT helpful in distinguishing follicular adenomas from minimally invasive follicular carcinomas – Requires extensive sampling of the tumor-thyroid capsule interface to exclude capsular or vascular invasion. • the presence of tumor plugs within intratumoral blood vessels has little prognostic significance • Unlike in papillary cancers, lymphatic spread is distinctly uncommon in follicular cancers
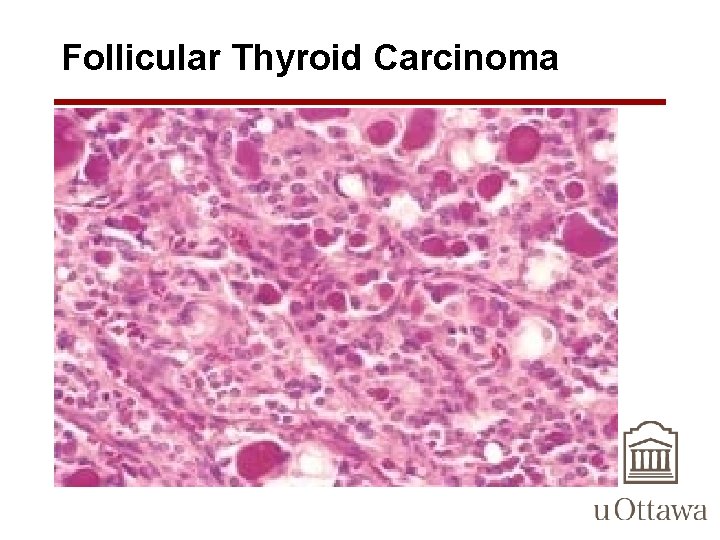
Follicular Thyroid Carcinoma
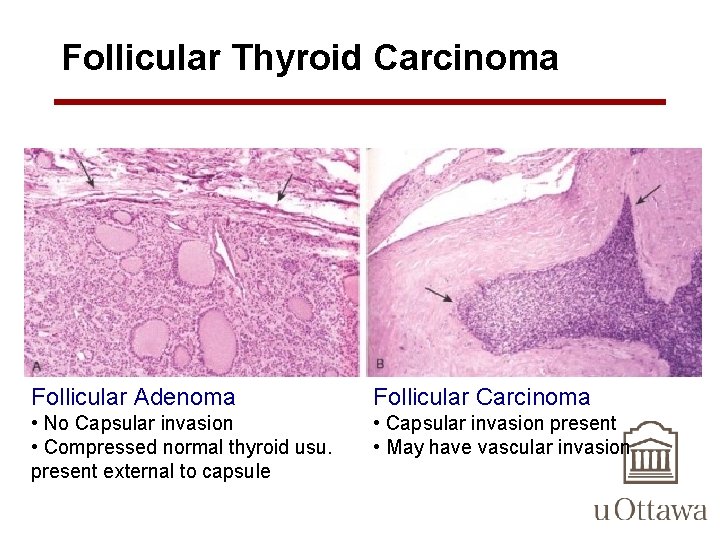
Follicular Thyroid Carcinoma Follicular Adenoma Follicular Carcinoma • No Capsular invasion • Compressed normal thyroid usu. present external to capsule • Capsular invasion present • May have vascular invasion
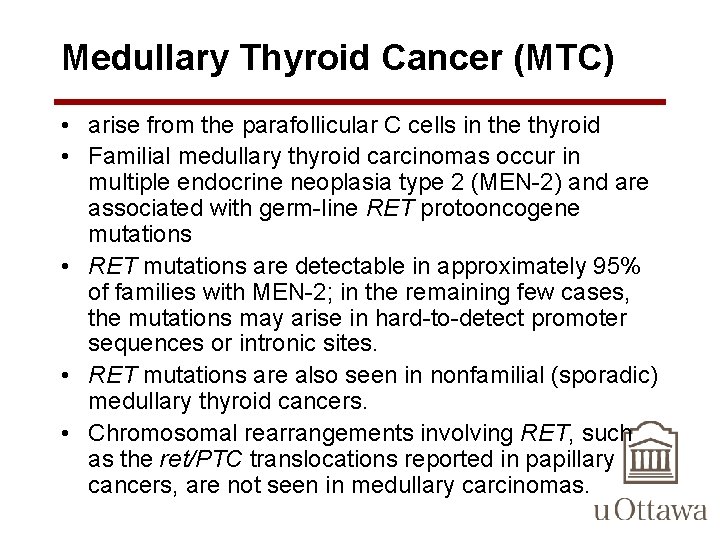
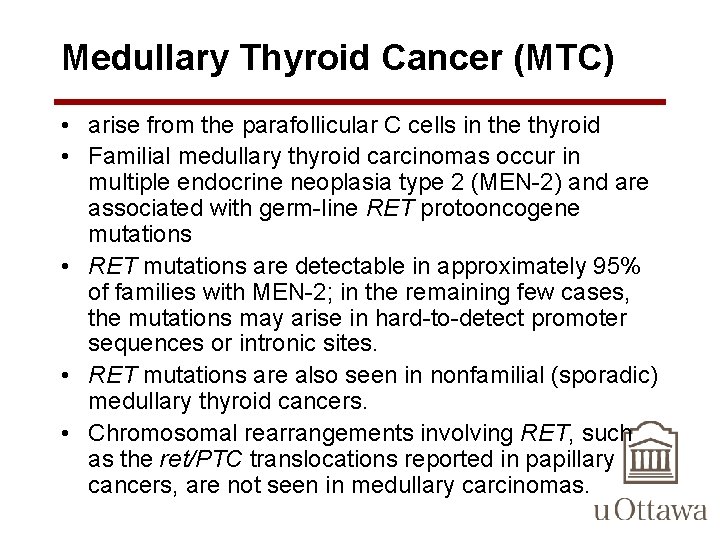
Medullary Thyroid Cancer (MTC) • arise from the parafollicular C cells in the thyroid • Familial medullary thyroid carcinomas occur in multiple endocrine neoplasia type 2 (MEN-2) and are associated with germ-line RET protooncogene mutations • RET mutations are detectable in approximately 95% of families with MEN-2; in the remaining few cases, the mutations may arise in hard-to-detect promoter sequences or intronic sites. • RET mutations are also seen in nonfamilial (sporadic) medullary thyroid cancers. • Chromosomal rearrangements involving RET, such as the ret/PTC translocations reported in papillary cancers, are not seen in medullary carcinomas.
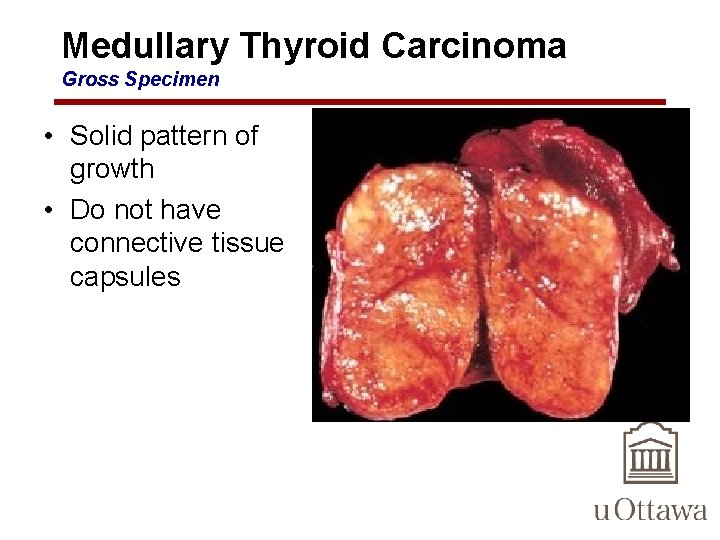
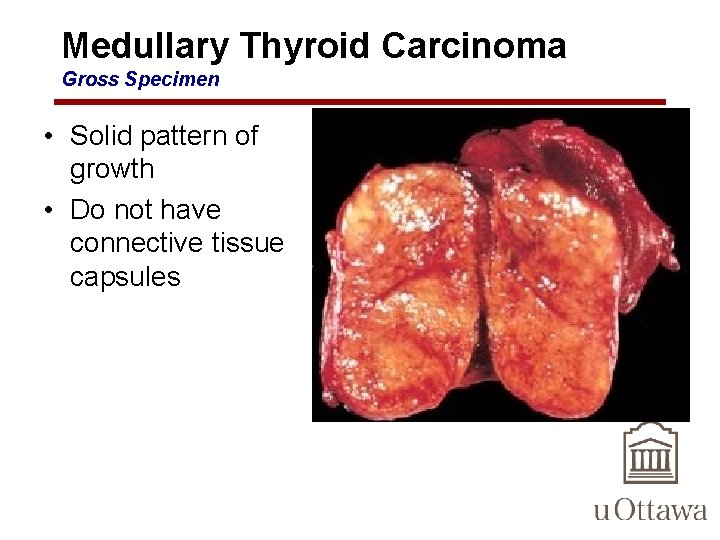
Medullary Thyroid Carcinoma Gross Specimen • Solid pattern of growth • Do not have connective tissue capsules
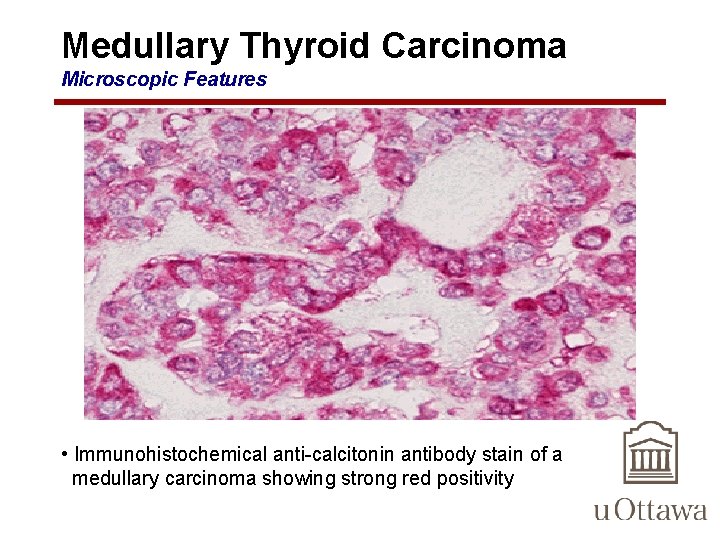
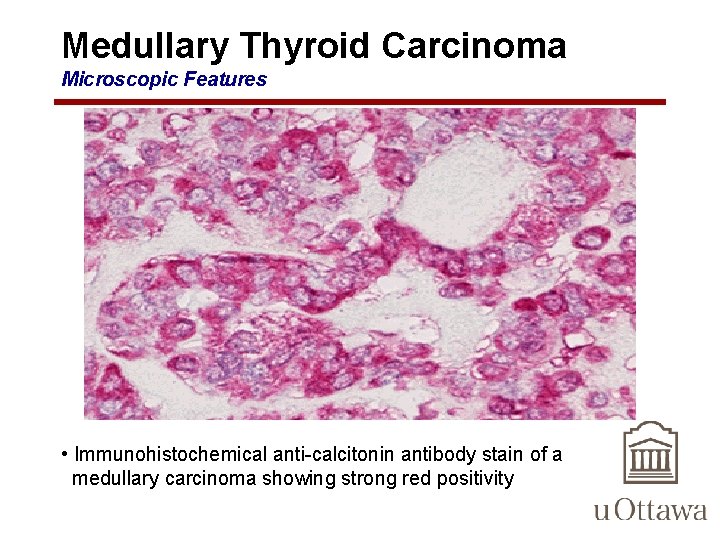
Medullary Thyroid Carcinoma Microscopic Features • Immunohistochemical anti-calcitonin antibody stain of a medullary carcinoma showing strong red positivity
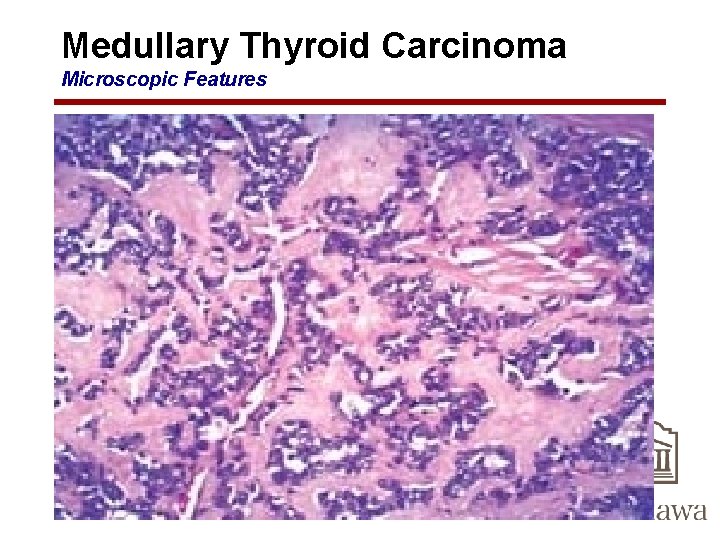
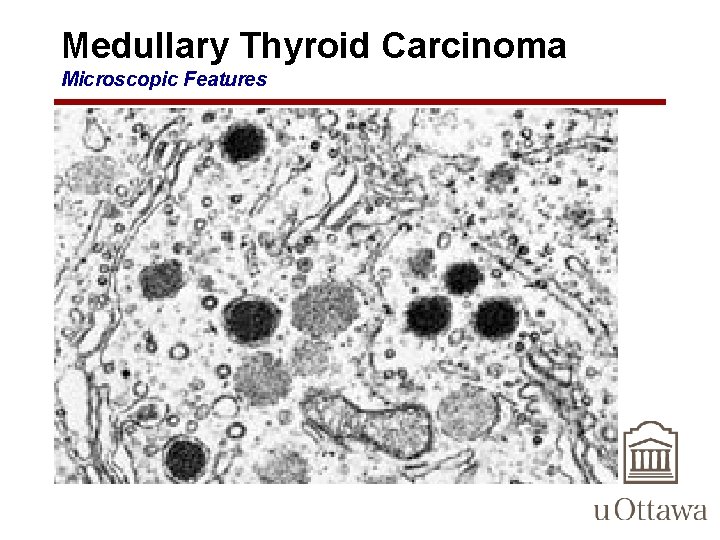
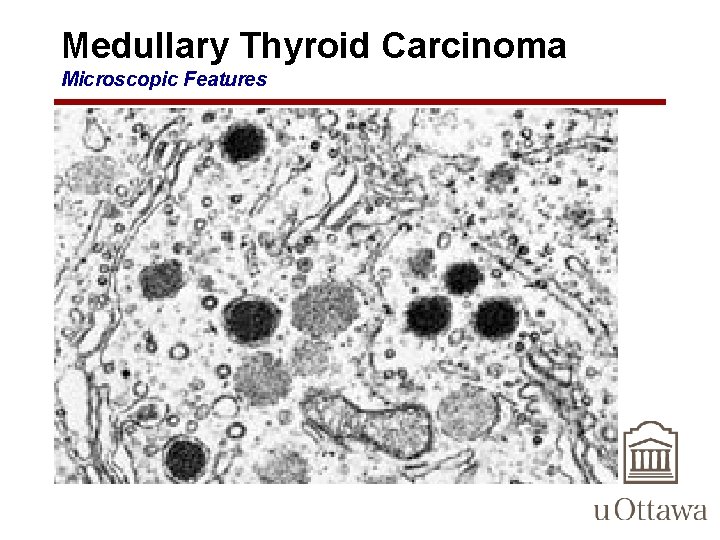
Medullary Thyroid Carcinoma Microscopic Features • composed of polygonal to spindle-shaped cells – may form nests, trabeculae, and even follicles • Small, more anaplastic cells are present in some tumors and may be the predominant cell type • Acellular amyloid deposits, derived from altered calcitonin molecules, are present in the adjacent stroma in many cases • Electron microscopy reveals variable numbers of membrane-bound electron-dense granules within the cytoplasm of the neoplastic cells.
Medullary Thyroid Carcinoma Microscopic Features • Familial medullary cancers – presence of multicentric C-cell hyperplasia in the surrounding thyroid parenchyma, a feature that is usually absent in sporadic lesions
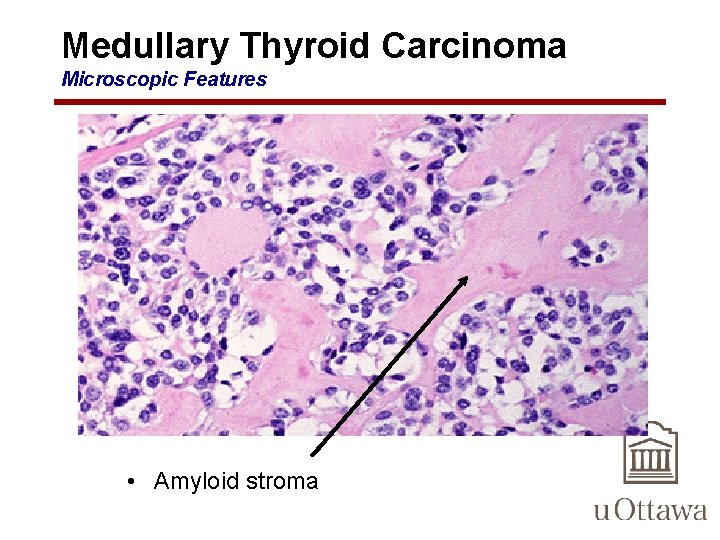
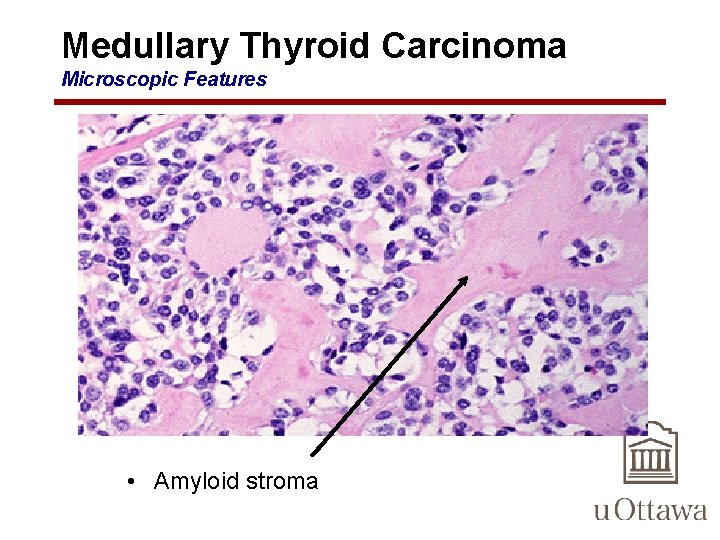
Medullary Thyroid Carcinoma Microscopic Features • Amyloid stroma
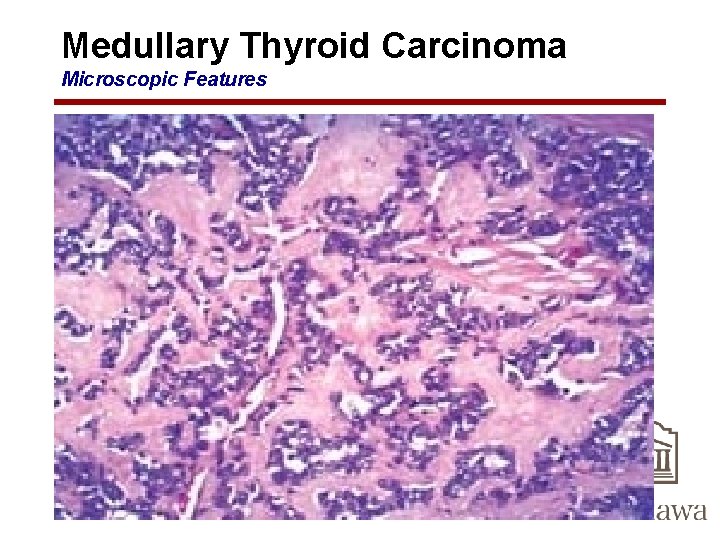
Medullary Thyroid Carcinoma Microscopic Features
Medullary Thyroid Carcinoma Microscopic Features
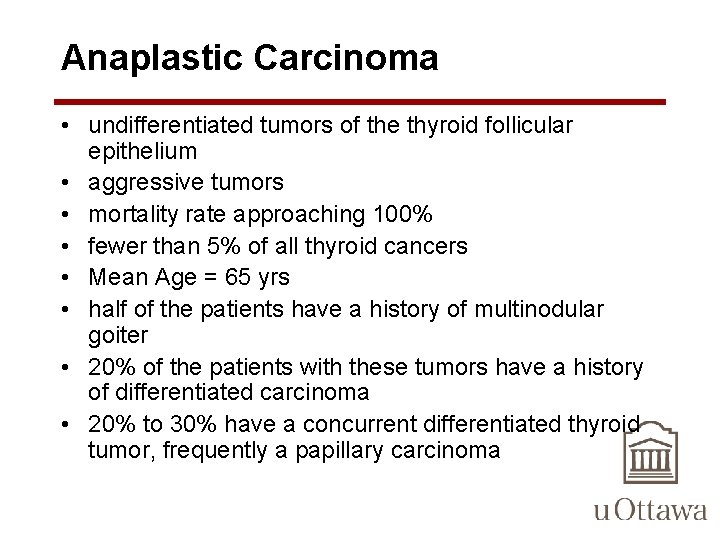
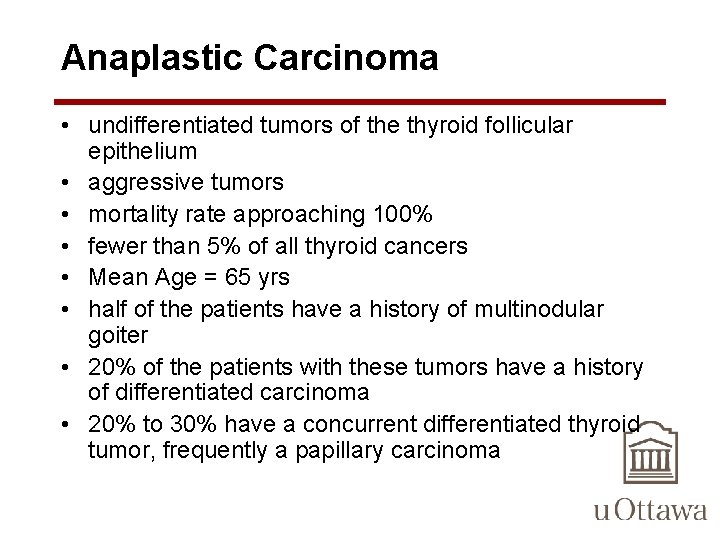
Anaplastic Carcinoma • undifferentiated tumors of the thyroid follicular epithelium • aggressive tumors • mortality rate approaching 100% • fewer than 5% of all thyroid cancers • Mean Age = 65 yrs • half of the patients have a history of multinodular goiter • 20% of the patients with these tumors have a history of differentiated carcinoma • 20% to 30% have a concurrent differentiated thyroid tumor, frequently a papillary carcinoma
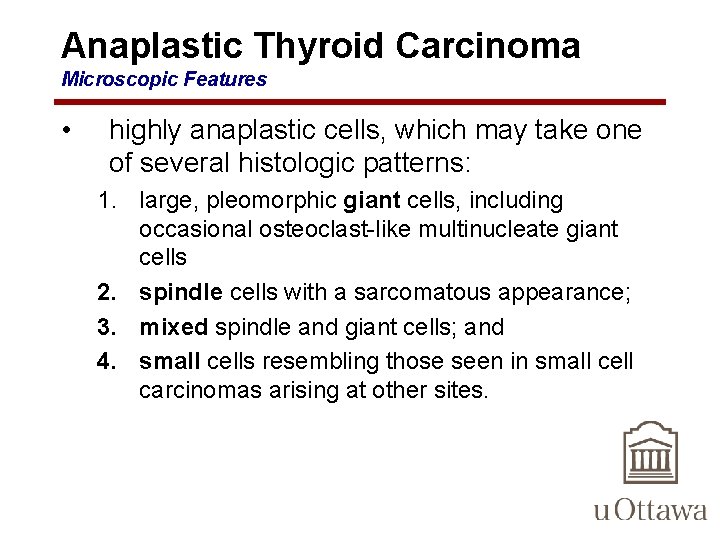
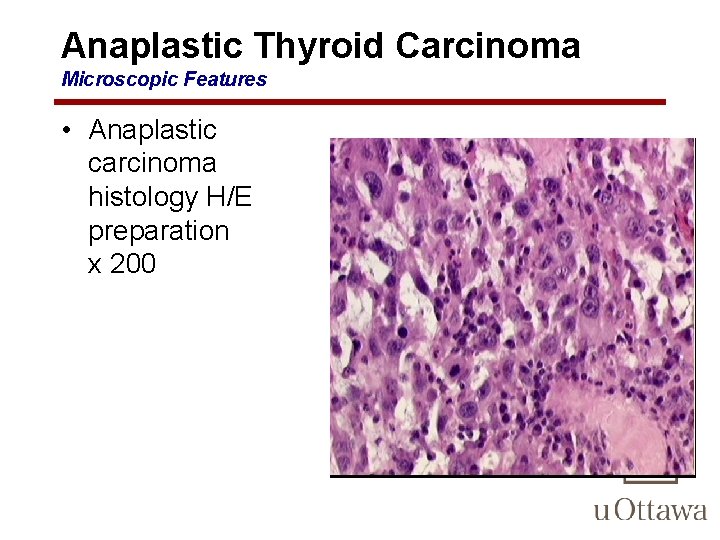
Anaplastic Thyroid Carcinoma Microscopic Features • highly anaplastic cells, which may take one of several histologic patterns: 1. large, pleomorphic giant cells, including occasional osteoclast-like multinucleate giant cells 2. spindle cells with a sarcomatous appearance; 3. mixed spindle and giant cells; and 4. small cells resembling those seen in small cell carcinomas arising at other sites.
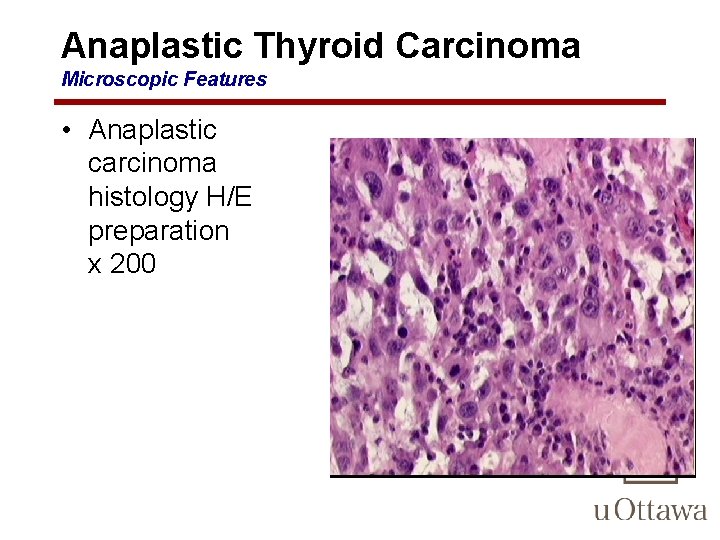
Anaplastic Thyroid Carcinoma Microscopic Features • Anaplastic carcinoma histology H/E preparation x 200