Osteoarthritis Degenerative arthritisosteoarthrosishypertrophic arthritis Osteoarthritis is a noninflammatory














- Slides: 62
Osteoarthritis (Degenerative arthritis/osteoarthrosis/hypertrophic arthritis)
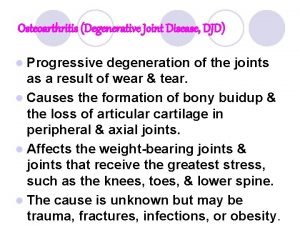
Osteoarthritis is a non-inflammatory, degenerative condition of joints Characterized by degeneration of articular cartilage and formation of new bone i. e. osteophytes.
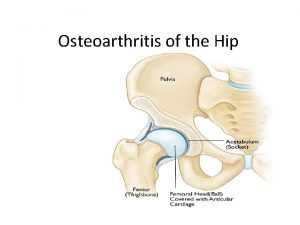
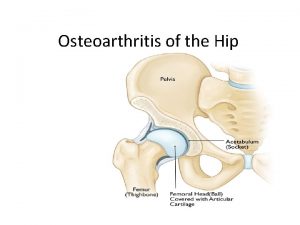
Common in weight-bearing joints such as hip and knee. Also seen in spine and hands. Both male and females areaffected. But more common in older women i. e. above 50 yrs, particularly in postmenopausal age.
Risk factors Obesity esp OA knee Abnormal mechanical loading eg. meniscectomy, instability Inherited type II collagen defects in premature polyarticular OA Inheritance in nodal OA Occupation eg farmers Infection: Non-gonococcal septic arthritis Hereditary
Ageing process in joint cartilage Defective lubricating mechanism Incompletely treated congenital dislocation of hip
Classification of OA OA Primary OA Secondary OA
Primary OA More common than secondary OA Cause –Unknown Common-in elders where there is no previous pathology. Its mainly due to wear and tear changes occuring in old ages mainly in weight bearing joints.
Secondary OA Due to a predisposing cause such as: 1. Injury to the joint 2. Previous infection 3. RA 4. CDH 5. Deformity 6. Obesity 7. hyperthyriodism
Types of OA Nodal Generalised OA • Crystal Associated OA • OA of Premature Onset
Nodal Generalised OA • • Heberden’s nodes • Bouchard’s nodes • CMC of thumb • Hallux valgus/rigidus • Knees & hips • Apophyseal joints
Crystal Associated OA • • • Calcium pyrophosphate dihydrate occurs mainly in elderly women, and principally affects the knee
OA of Premature • • Previous meniscectomy • • Haemochromatosis Onset
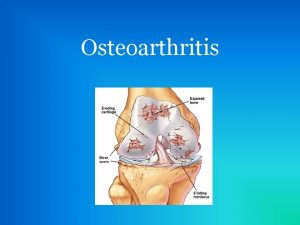
Pathology OA is a degenerative condition primarily affecting the articular cartilage. 1. articular cartilage 2. Bone 3. Synovial membrane 4. capsule 5. Ligament 6. muscle
Articular Cartilage is the 1 ststructure to be affected. Erosion occurs, often central &frequently in wt. bearing areas. Fibrillation, which causes softening, splitting and fragmentation of the cartilage, occur in both wt. bearing &non-wt. bearing areas. Collagen fibres split and there is disorganisation of the proteoglycon collagen relationship such as H 2 O is attracted into cartilage, which causes futher softening and flaking. these flakes of cartilage break off and may be impacted b/w the jt. surfaces causing locking and inflammation.
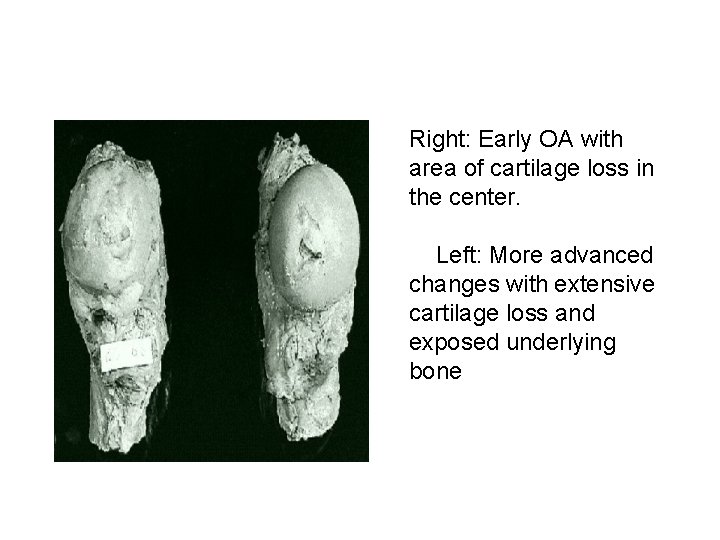
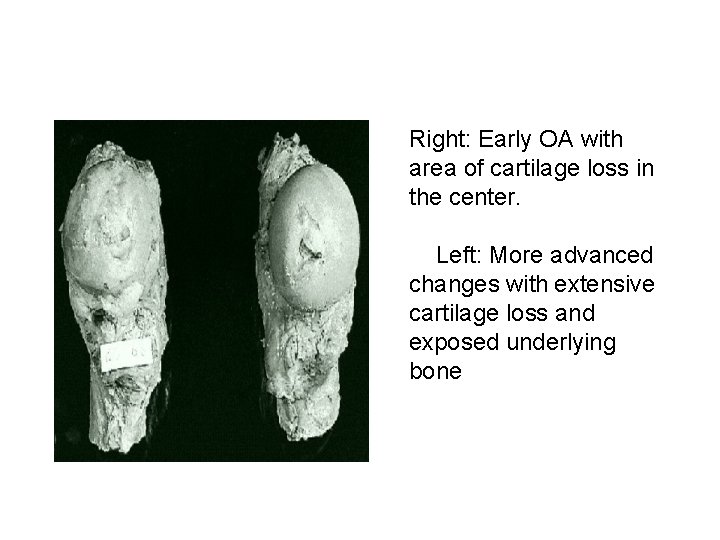
Right: Early OA with area of cartilage loss in the center. Left: More advanced changes with extensive cartilage loss and exposed underlying bone
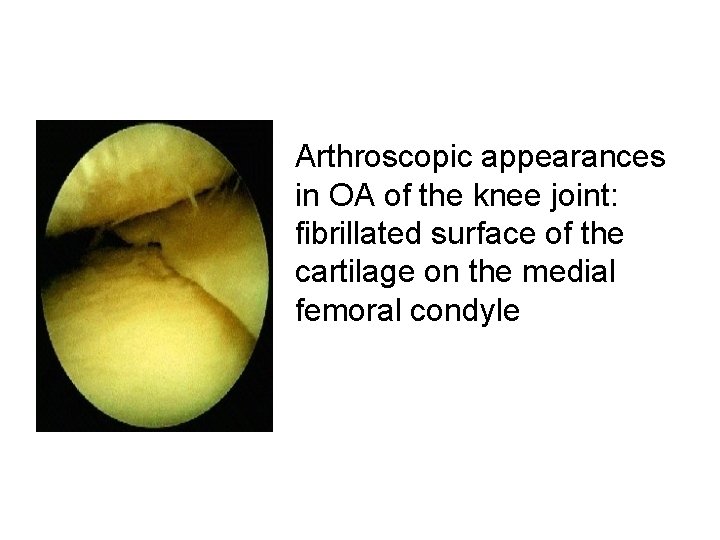
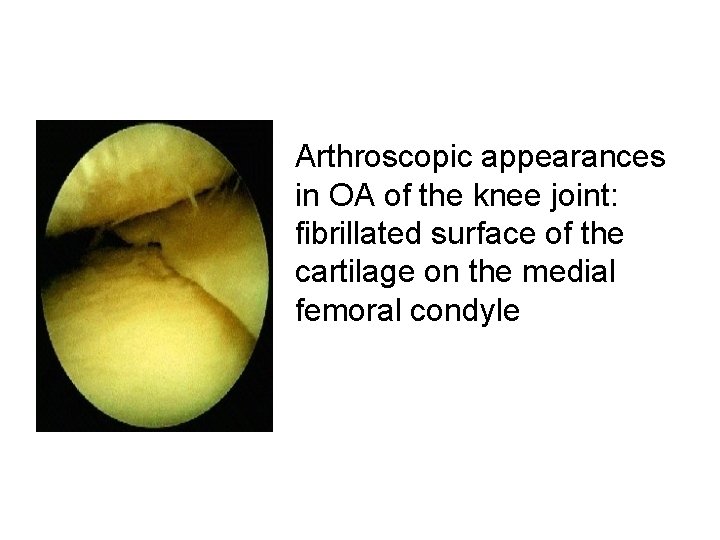
Arthroscopic appearances in OA of the knee joint: fibrillated surface of the cartilage on the medial femoral condyle
Bone(Eburnation) Bone surface become hard &polished as there is loss of protection from the cartilage. Cystic cavities form in the subchondral bone because eburnated bone is brittle and microfractures occur. Venous congestion in the subchondral bone.
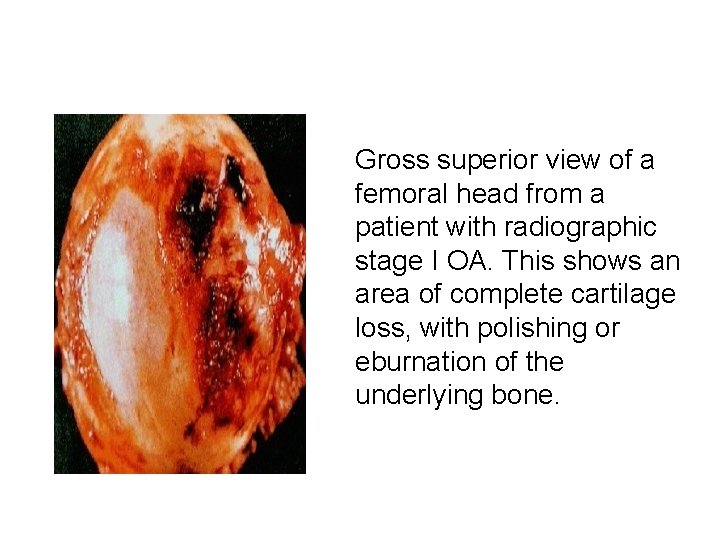
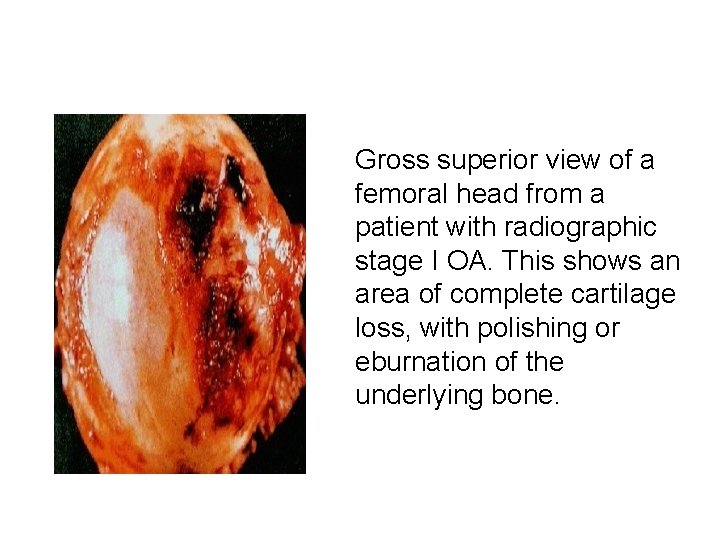
Gross superior view of a femoral head from a patient with radiographic stage I OA. This shows an area of complete cartilage loss, with polishing or eburnation of the underlying bone.
Osteophytes form at the margin of the articular surface, which may get projected into the jt. Or into capsule &ligament, bone of the wt. -bearing jt. There is alteration in the shape of the femoral head which becomes flat and mushroom shaped. Tibial condyles become flatened.
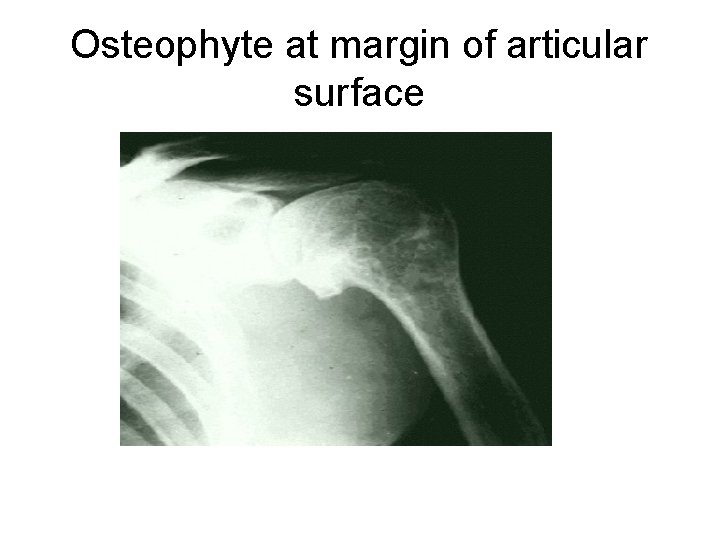
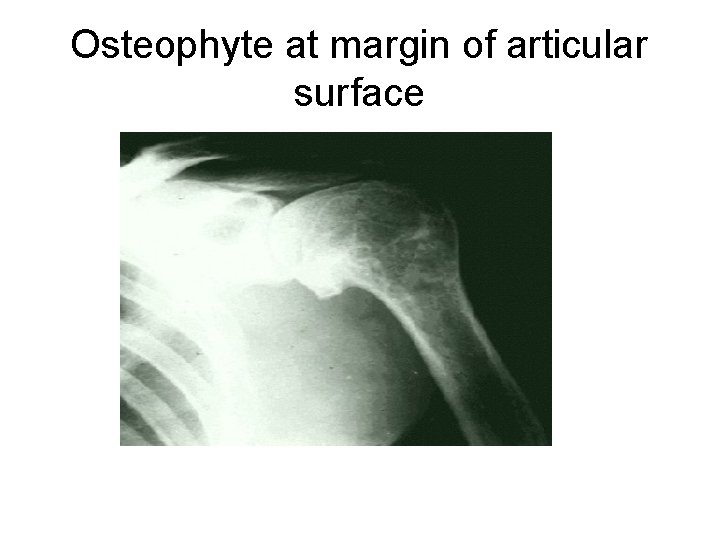
Osteophyte at margin of articular surface
Synovial Membrane Synovial membrane undergo hypertrophy and become oedematous (which can lead to ‘cold’ effusions). Reduction of synovial fluid secretion results in loss of nutrition and lubricating action of articular cartilage. Capsule It undergoes fibrous degeneration and there are low-grade chronic inflammatory changes


Ligament Undergoesfibrous degernation Thereislowgradechronicinflammatory changesandacc. to theaspectjoint becomecontractedorelongated. • Muscles • Undergoesatrophy, aspt. isnotabletousethejt. Becauseofpainwhichfurtherlimitsmovts. and function.


Clinical features of OA Pain Stiffness Muscle spasm Restricted movement Deformity Muscle weakness or wasting Joint enlargement and instability Crepitus • Joint Effusion
Clinical features 1 • Pain and tenderness – Usually slow onset of discomfort, with gradual and intermittent increase – Pain is more on wt. bearing due to stress on the synovial membrane & later on due to bone surface, which r rich in nerve endings coming in contact. -initially relieved by rest but later on disturb sleep. -Diffuse/ sharp and stabbing local pain

Clinical features • Pain and tenderness (cont) – Types of pain • Mechanical: increases with use of the joint • Inflammatory phases • Rest pain later on in 50% • Night pain in 30% later on
Clinical features 2 • Movement abnormalities – ‘Gelling’: stiffness after periods of inactivity, passes over within minutes (approx 15 min. ) of using joint again – Coarse crepitus: palpate/hear (due to flaked cartilage & eburnated bone ends) – Reduced ROM: capsular thickening and bony changes in joint, ms. Spasm or soft tissue contracture.
Clinical features 3 • Deformities – Soft tissue swelling: • mild synovitis • small effusions – Osteophytes – Joint laxity – Asymmetrical joint destruction leading to angulation
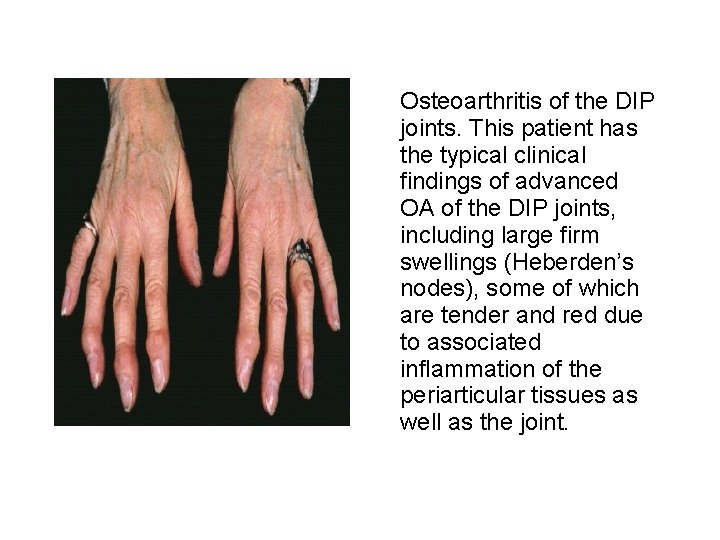
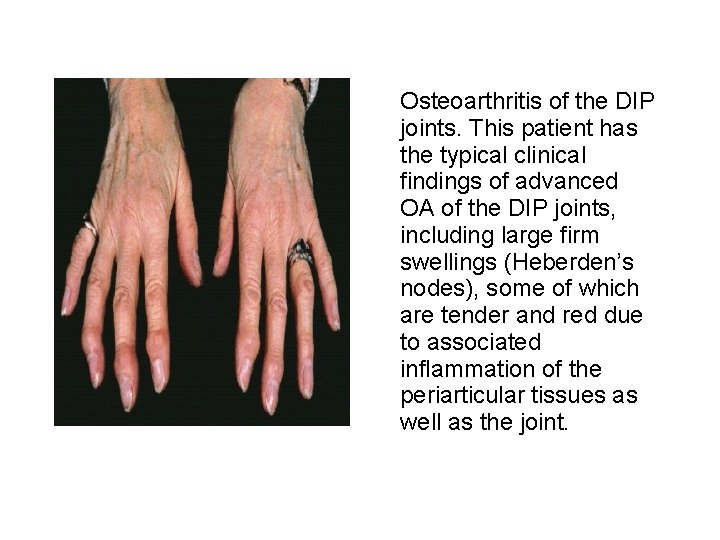
Osteoarthritis of the DIP joints. This patient has the typical clinical findings of advanced OA of the DIP joints, including large firm swellings (Heberden’s nodes), some of which are tender and red due to associated inflammation of the periarticular tissues as well as the joint.
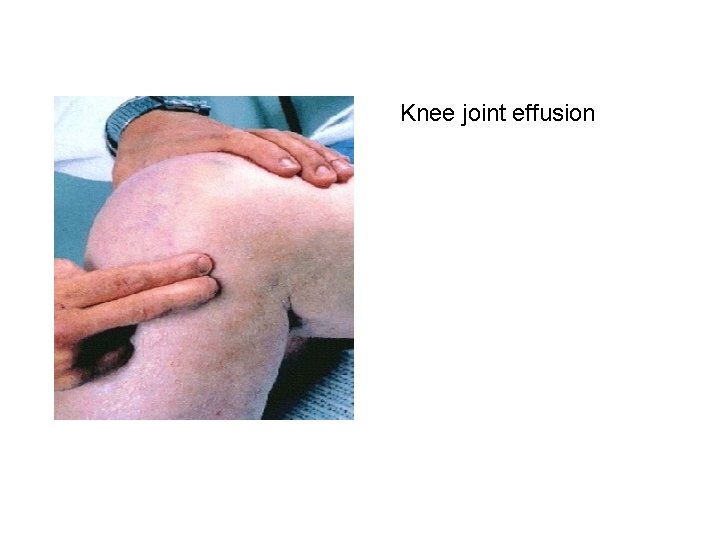
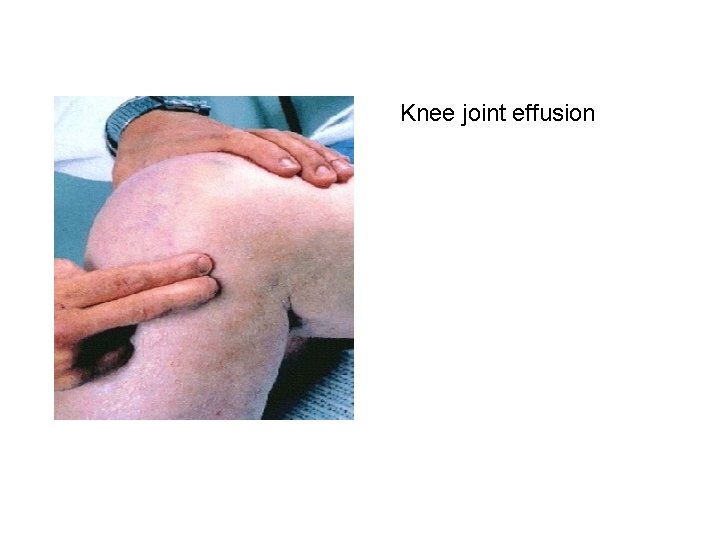
Knee joint effusion
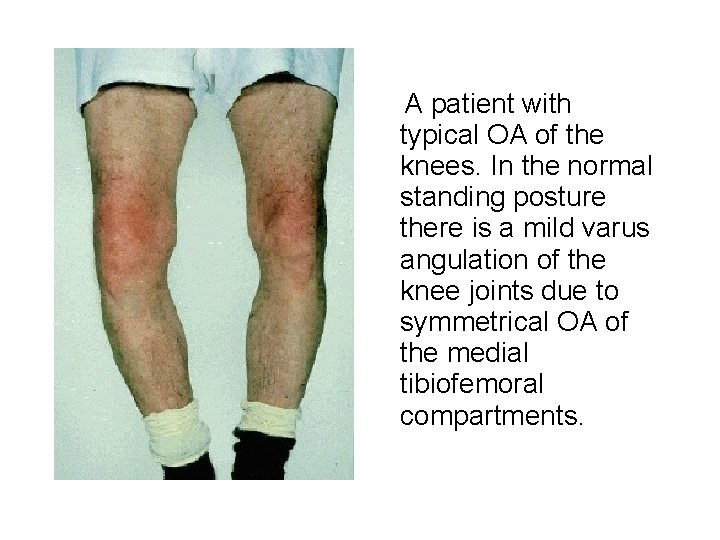
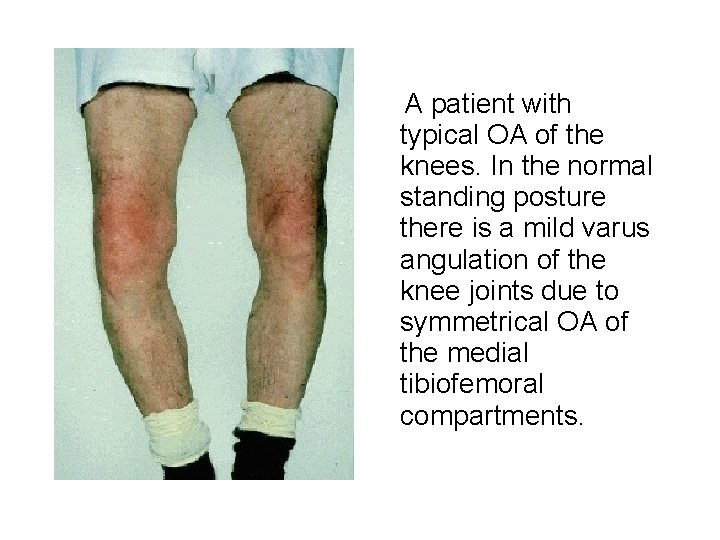
A patient with typical OA of the knees. In the normal standing posture there is a mild varus angulation of the knee joints due to symmetrical OA of the medial tibiofemoral compartments.
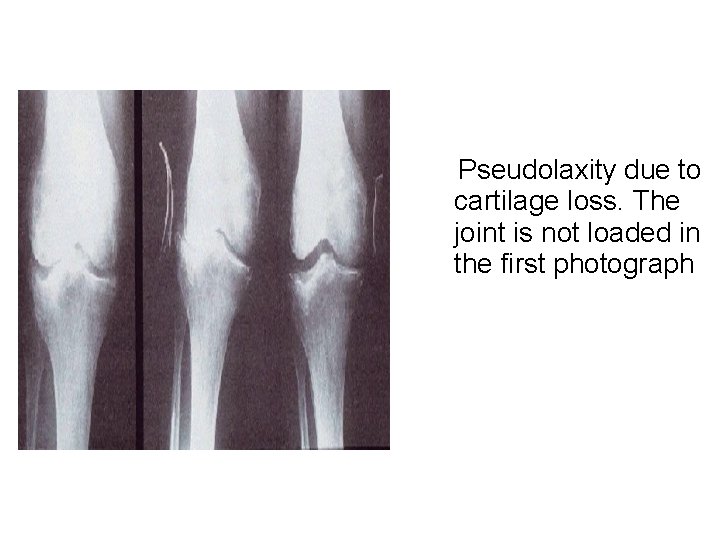
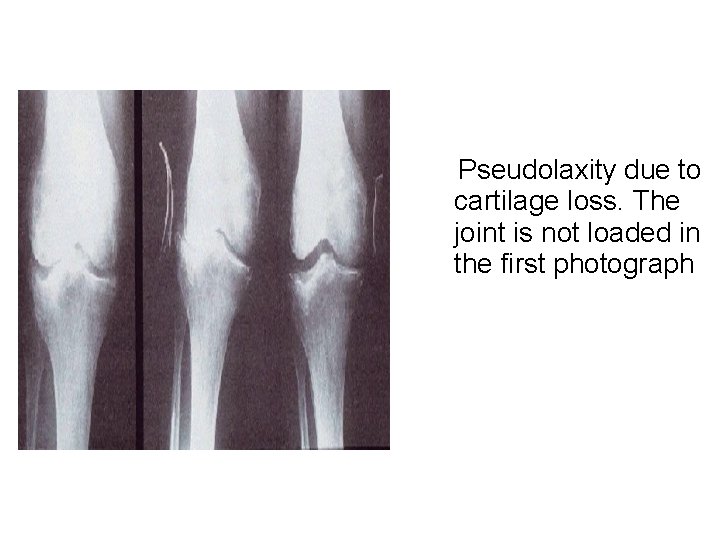
Pseudolaxity due to cartilage loss. The joint is not loaded in the first photograph
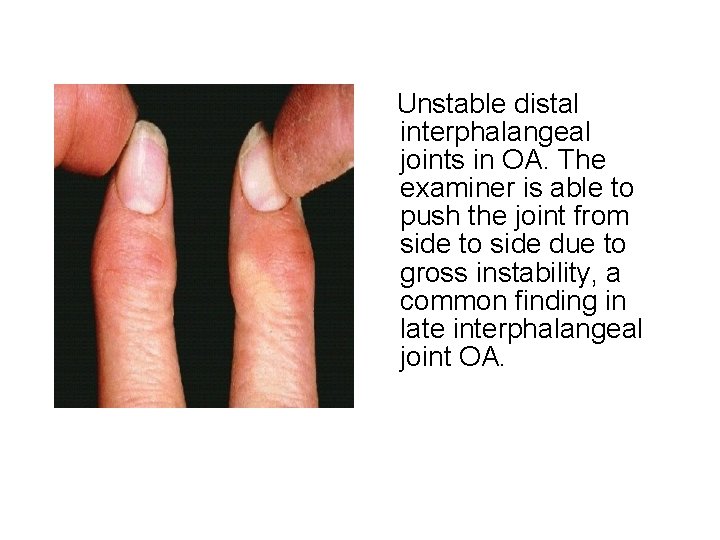
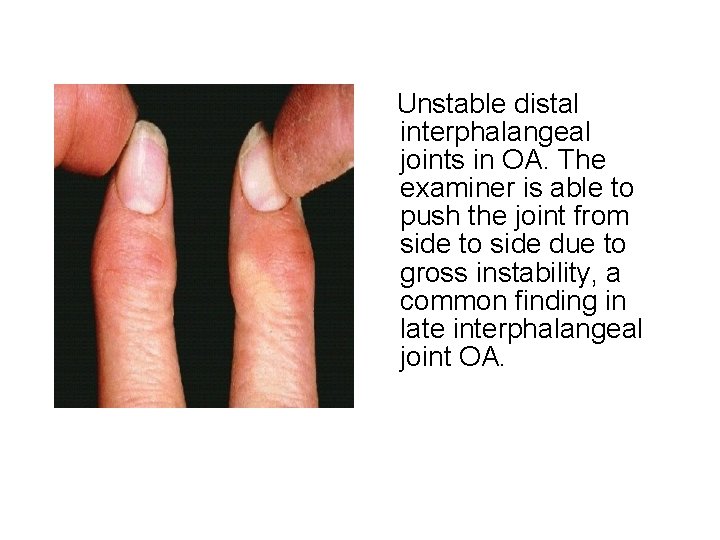
Unstable distal interphalangeal joints in OA. The examiner is able to push the joint from side to side due to gross instability, a common finding in late interphalangeal joint OA.
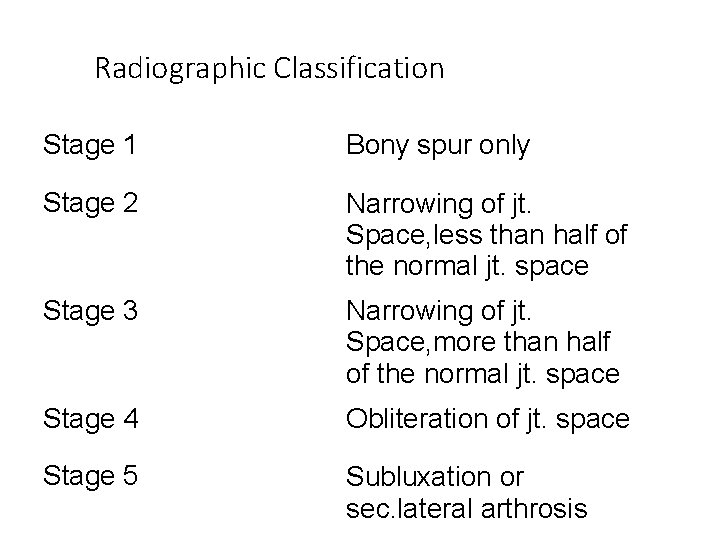
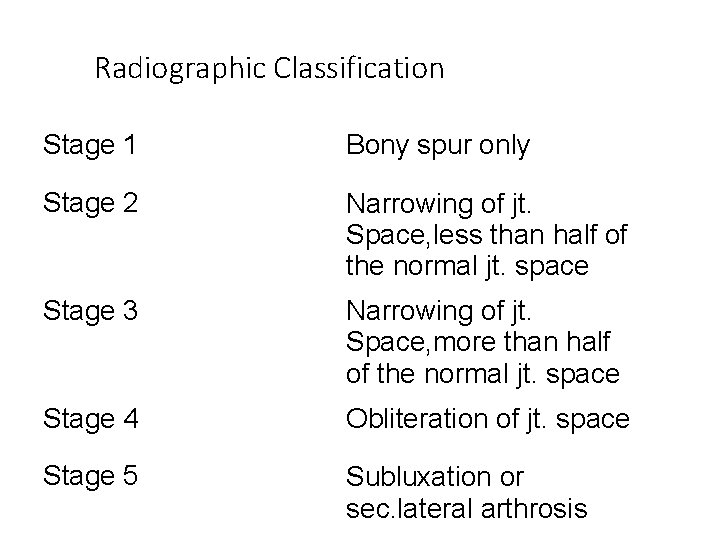
Radiographic Classification Stage 1 Bony spur only Stage 2 Narrowing of jt. Space, less than half of the normal jt. space Stage 3 Narrowing of jt. Space, more than half of the normal jt. space Stage 4 Obliteration of jt. space Stage 5 Subluxation or sec. lateral arthrosis
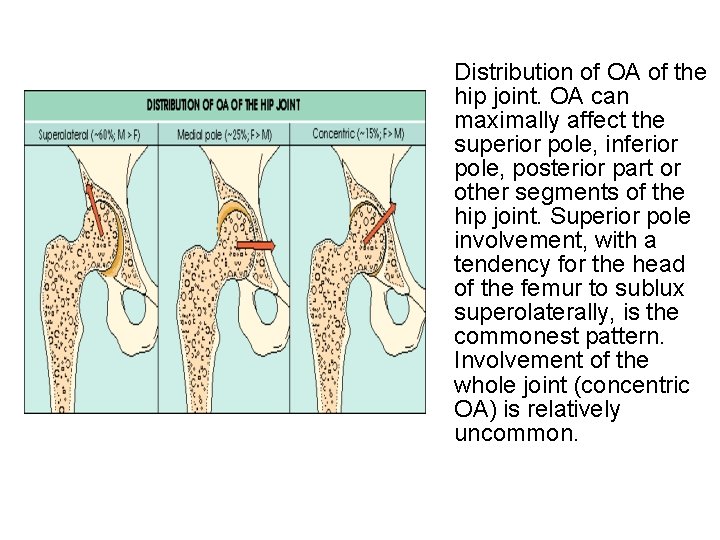
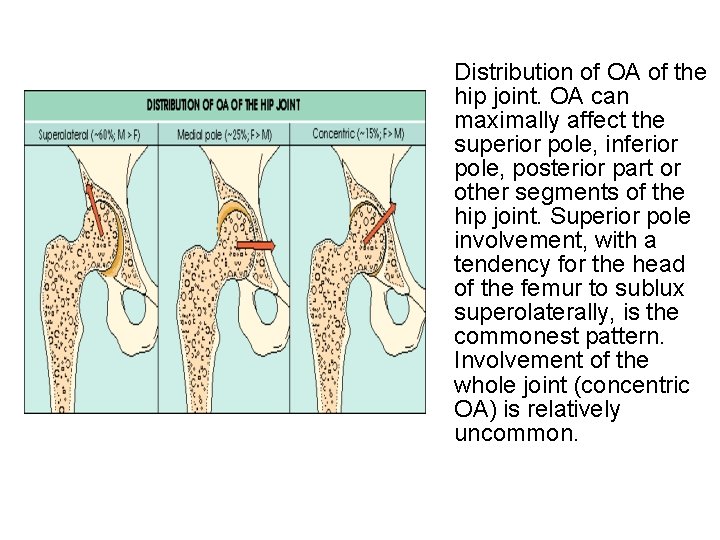
Distribution of OA of the hip joint. OA can maximally affect the superior pole, inferior pole, posterior part or other segments of the hip joint. Superior pole involvement, with a tendency for the head of the femur to sublux superolaterally, is the commonest pattern. Involvement of the whole joint (concentric OA) is relatively uncommon.

Special Investigations • Blood tests: Normal • Radiological features: – Cartilage loss – Subchondral sclerosis – Cysts – Osteophytes

Management

Treatment Principles • Education • Physiotherapy – Exercise program – Pain relief modalities • Aids and appliances • Medical Treatment • Surgical Treatment
Education • Nonsystemic nature of disease • Prevent overloading of joint. Obesity!! • Appropriate use of treatment modalities – Importance of exercise program – Aids, apliances, braces – Medial treatments – Surgical treatments

Exercise • Will not ‘wear the joint out’ • Important for cartilage nutrition • Some evidence that lack of exercise leads to progression of OA
Exercise • Encourage full range low impact movements eg swimming, cycling • Avoid – Prolonged loading – Activities that cause pain – Contact sports – High impact sports eg running
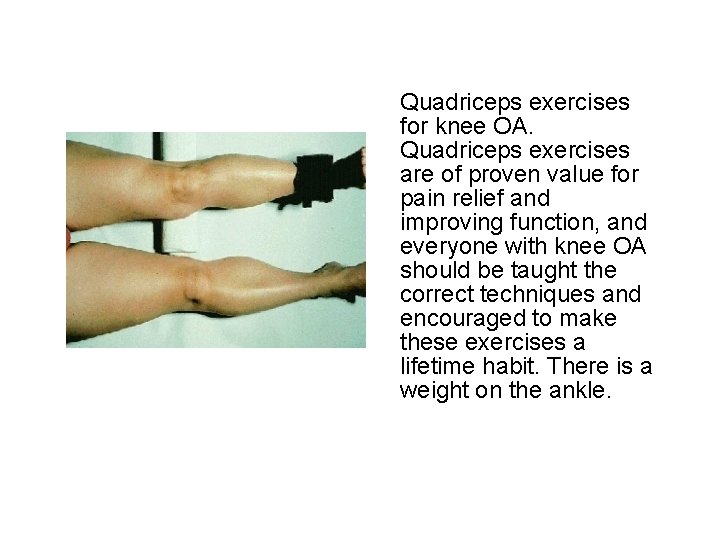
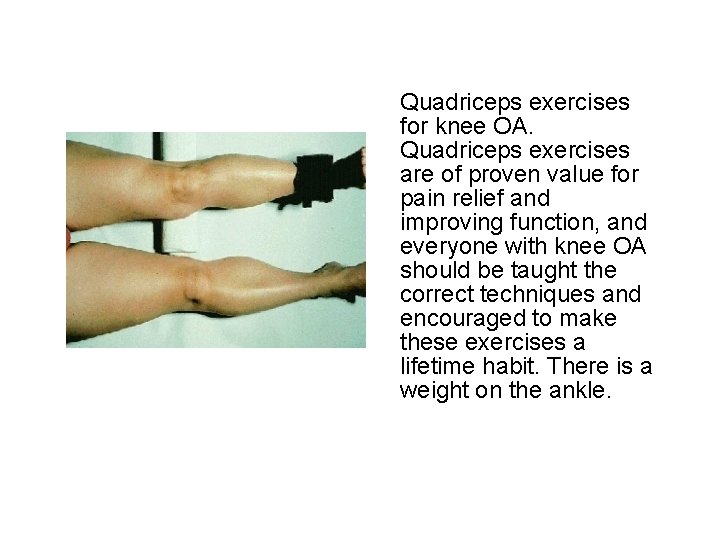
Quadriceps exercises for knee OA. Quadriceps exercises are of proven value for pain relief and improving function, and everyone with knee OA should be taught the correct techniques and encouraged to make these exercises a lifetime habit. There is a weight on the ankle.
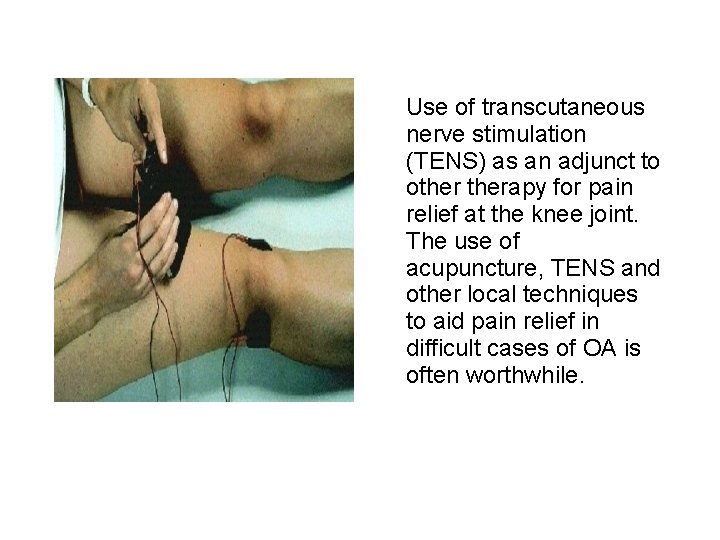
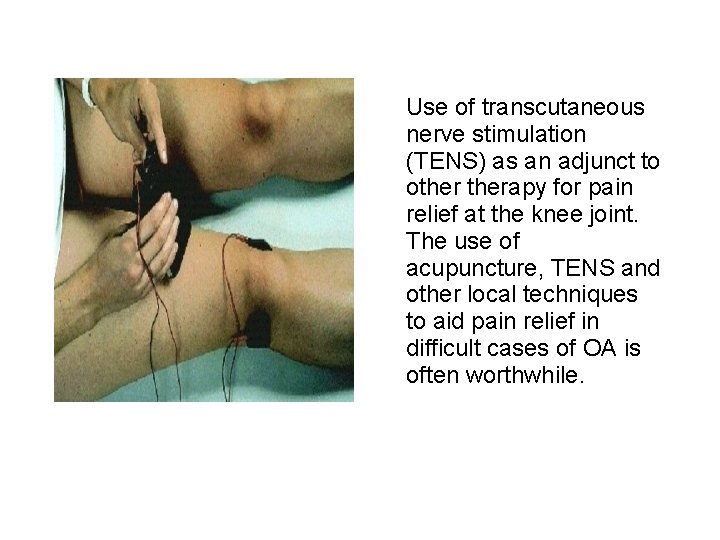
Use of transcutaneous nerve stimulation (TENS) as an adjunct to otherapy for pain relief at the knee joint. The use of acupuncture, TENS and other local techniques to aid pain relief in difficult cases of OA is often worthwhile.
Aids • • and appliances Braces / splints Special shoes/insoles Mobility aids Aids: dressing, reaching, tap openers, kitchen aids • Taping of patella in patello femoral OA
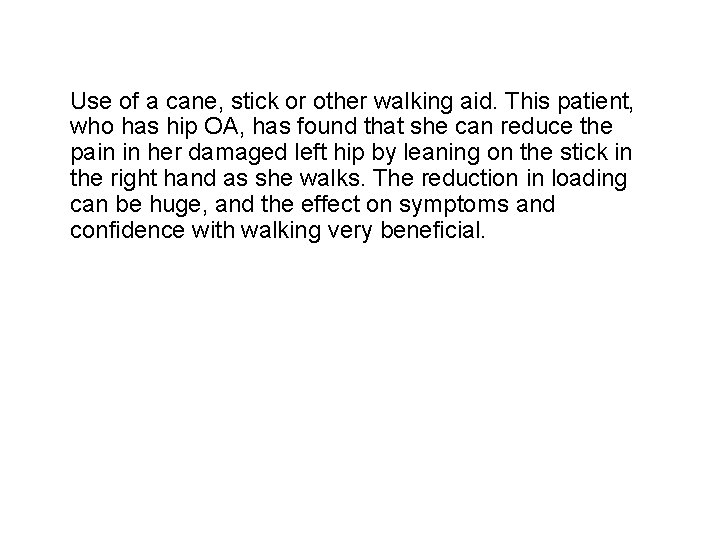
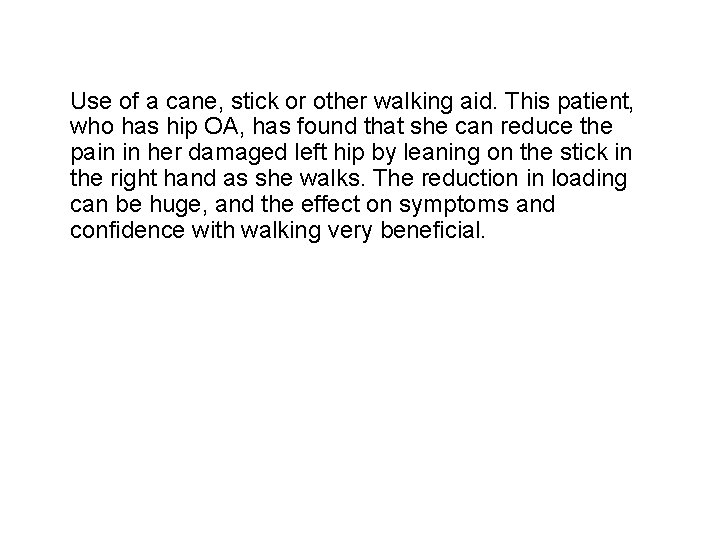
Use of a cane, stick or other walking aid. This patient, who has hip OA, has found that she can reduce the pain in her damaged left hip by leaning on the stick in the right hand as she walks. The reduction in loading can be huge, and the effect on symptoms and confidence with walking very beneficial.
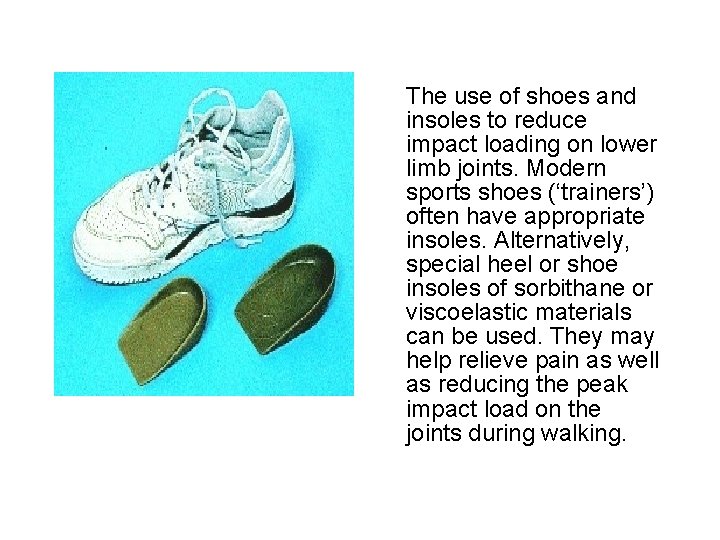
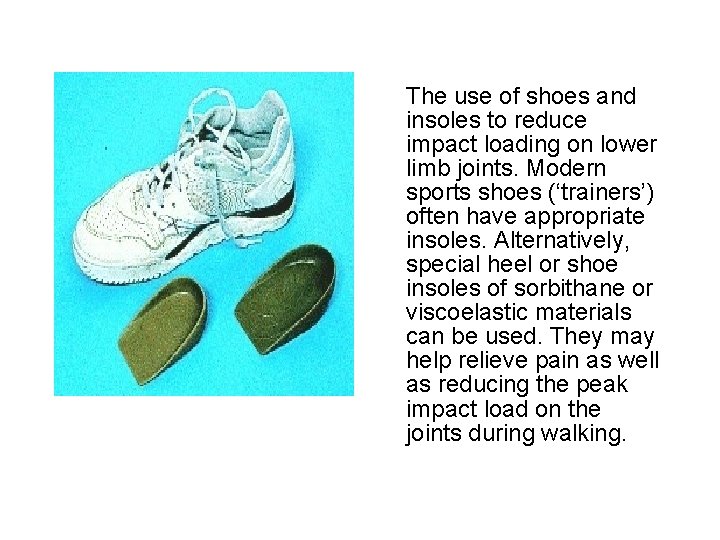
The use of shoes and insoles to reduce impact loading on lower limb joints. Modern sports shoes (‘trainers’) often have appropriate insoles. Alternatively, special heel or shoe insoles of sorbithane or viscoelastic materials can be used. They may help relieve pain as well as reducing the peak impact load on the joints during walking.
Medical Treatment • Simple analgesics: paracetamol, low dose ibuprofen • NSAID’s/Coxibs PRN regular • Intra-articular corticosteroids • Topical treatment eg NSAID creams, capsaicin • ‘Chondroprotective agents’
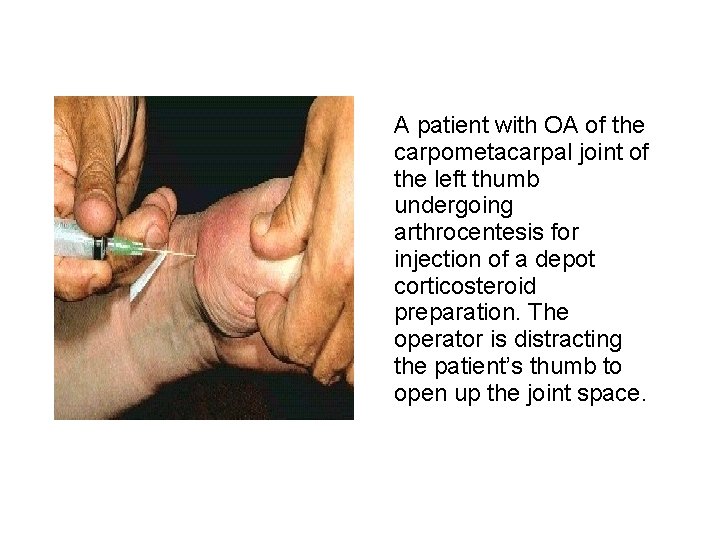
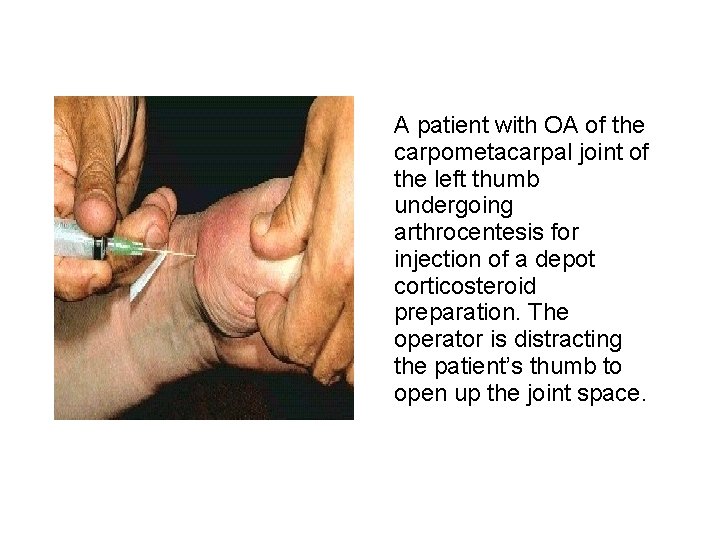
A patient with OA of the carpometacarpal joint of the left thumb undergoing arthrocentesis for injection of a depot corticosteroid preparation. The operator is distracting the patient’s thumb to open up the joint space.
Joint replacement surgery • Indications: pain affecting work, sleep, walking and leisure activities • Complications – sepsis – loosening – lifespan of materials (mechanical failure)





 Difference between osteoarthritis and rheumatoid arthritis
Difference between osteoarthritis and rheumatoid arthritis Degenerative disc
Degenerative disc Degenerative myelopathy wayne
Degenerative myelopathy wayne Generalised osteoarthritis
Generalised osteoarthritis Osteoarthritis
Osteoarthritis Osteoarthritis grade
Osteoarthritis grade Nursing management of gonococcal arthritis
Nursing management of gonococcal arthritis Osteoarthritis location
Osteoarthritis location Musculoskeletal injury icd 10
Musculoskeletal injury icd 10 Osteoarthritis soap note
Osteoarthritis soap note Atlantoaxial osteoarthritis
Atlantoaxial osteoarthritis Osteoarthritis
Osteoarthritis Gambaran radiologi osteoarthritis
Gambaran radiologi osteoarthritis Osteoarthritis
Osteoarthritis Reiter's syndrome
Reiter's syndrome Haart side effects
Haart side effects Septic arthritis antibiotics
Septic arthritis antibiotics Pauciarticular juvenile rheumatoid arthritis
Pauciarticular juvenile rheumatoid arthritis Psoriasis arthritis nhs
Psoriasis arthritis nhs Septic arthritis workup
Septic arthritis workup Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Enthesitis
Enthesitis Kode icd 10 rhabdomyosarcoma
Kode icd 10 rhabdomyosarcoma Narbentypen
Narbentypen Arthritis and food allergies
Arthritis and food allergies Septic arthritis complications
Septic arthritis complications Rheumatoid arthritis
Rheumatoid arthritis Gout treatment
Gout treatment Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Arthritis foundation indiana
Arthritis foundation indiana Poststreptococcal reactive arthritis
Poststreptococcal reactive arthritis Eular psoriatic arthritis guidelines
Eular psoriatic arthritis guidelines Ans
Ans Viral arthritis
Viral arthritis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis What is subluxation
What is subluxation Eular criteria
Eular criteria Septic arthritis antibiotics
Septic arthritis antibiotics Rheumatoid arthritis
Rheumatoid arthritis Gardening with arthritis
Gardening with arthritis Deformities in rheumatoid arthritis
Deformities in rheumatoid arthritis Seronegative arthritis
Seronegative arthritis Nursing diagnosis for rheumatoid arthritis
Nursing diagnosis for rheumatoid arthritis Septic arthritis complications
Septic arthritis complications Symptoms of gonorrhea
Symptoms of gonorrhea Arthritis infusion treatment
Arthritis infusion treatment Extra articular manifestations of rheumatoid arthritis
Extra articular manifestations of rheumatoid arthritis Food allergies and arthritis
Food allergies and arthritis Extra articular manifestations of rheumatoid arthritis
Extra articular manifestations of rheumatoid arthritis Barik meaning
Barik meaning Soft tissue rheumatoid arthritis
Soft tissue rheumatoid arthritis Steinbrocker stage
Steinbrocker stage Carol maury
Carol maury 강직성척추염 grade
강직성척추염 grade Arthritis treatment
Arthritis treatment Zveren
Zveren Caprine arthritis encefalitis
Caprine arthritis encefalitis Rehaklinik psoriasis arthritis
Rehaklinik psoriasis arthritis Sclérite
Sclérite Anatomi fisiologi gout arthritis
Anatomi fisiologi gout arthritis Peripheral arthritis
Peripheral arthritis