RHEUMATOID ARTHRITIS RA OVERVIEW Definition Immunopathogenesis Clinical findings





















- Slides: 76
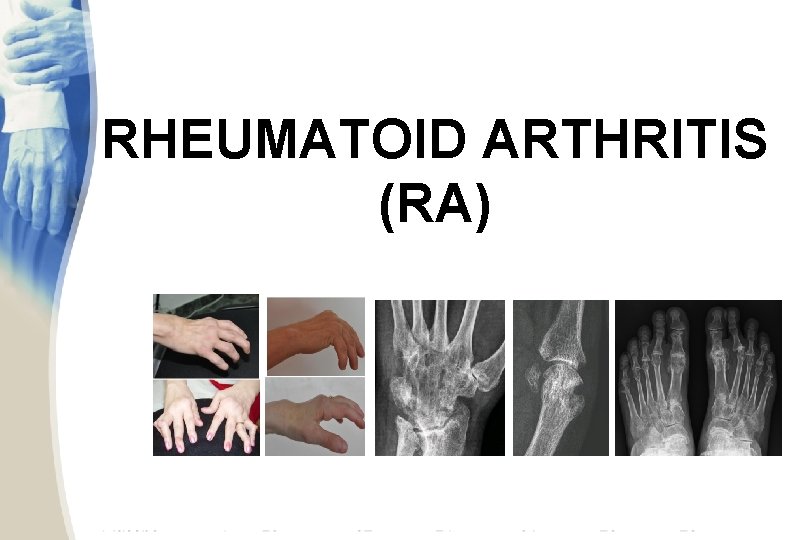
RHEUMATOID ARTHRITIS (RA)

OVERVIEW § Definition § Immuno-pathogenesis § Clinical findings (articular manifestations) § Investigations § Assessment & monitoring § Management and systemic
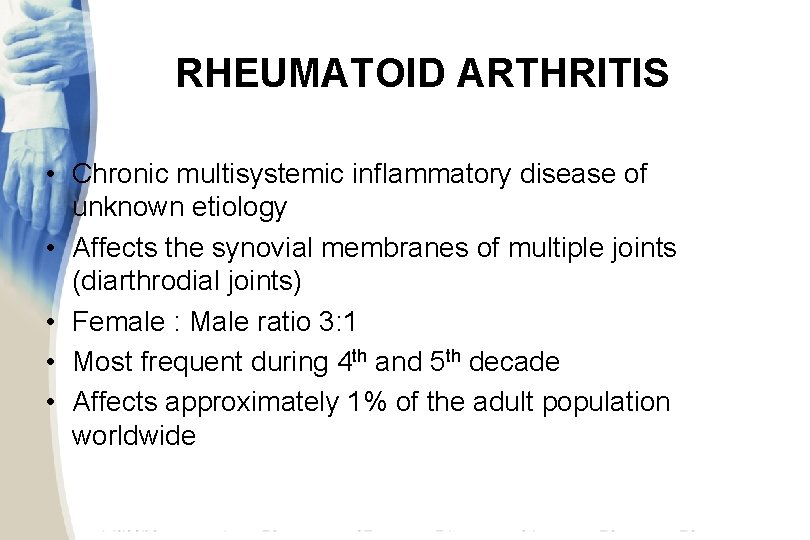
RHEUMATOID ARTHRITIS • Chronic multisystemic inflammatory disease of unknown etiology • Affects the synovial membranes of multiple joints (diarthrodial joints) • Female : Male ratio 3: 1 • Most frequent during 4 th and 5 th decade • Affects approximately 1% of the adult population worldwide

DEFINITION chronic immune inflammatory disorder, with still unknown aetiology, characterized by: § Articular manifestations: chronic destructive and deforming arthritis affecting small joints in a bilateral and symmetrical pattern; § Systemic manifestations: cardio-vascular, respiratory, renal, neurologic, ocular; § Progressive irreversible articular damage; § Significant functional disability and impaired quality of life
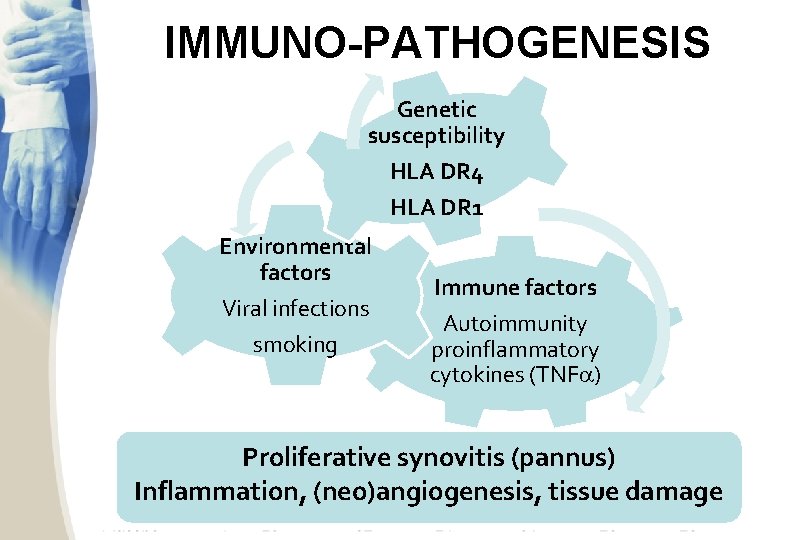
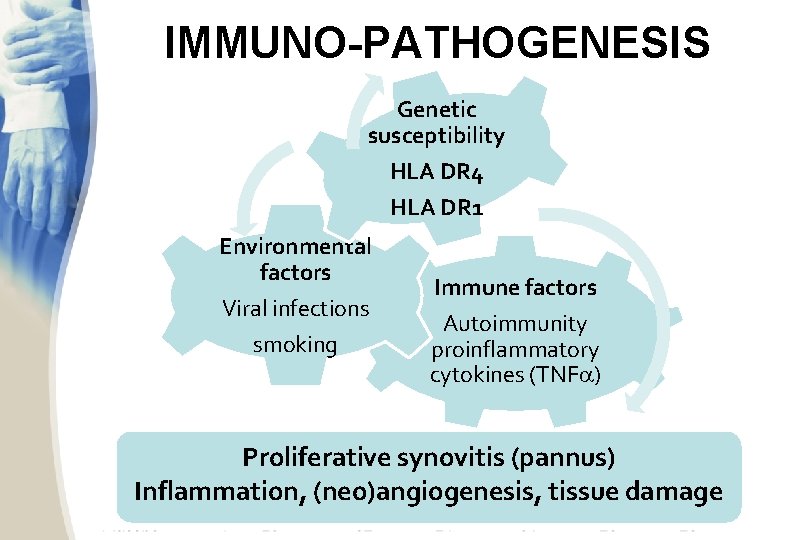
IMMUNO-PATHOGENESIS Genetic susceptibility HLA DR 4 HLA DR 1 Environmental factors Viral infections smoking Immune factors Autoimmunity proinflammatory cytokines (TNF ) Proliferative synovitis (pannus) Inflammation, (neo)angiogenesis, tissue damage
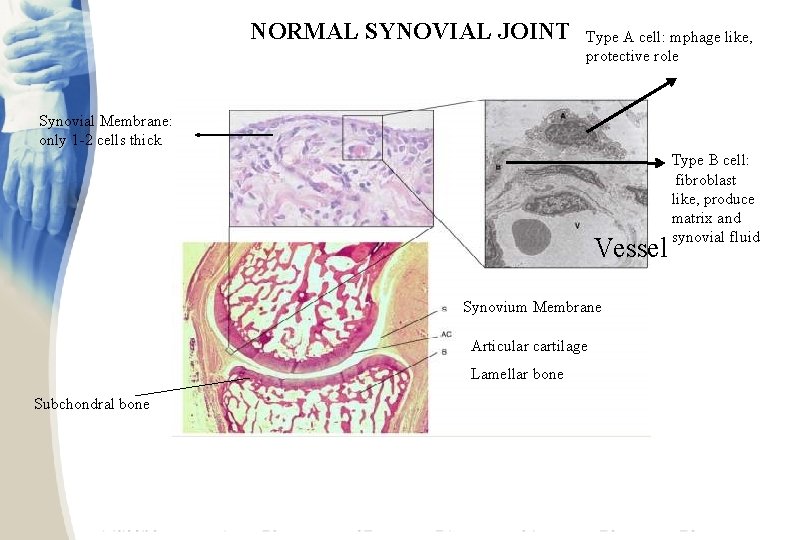
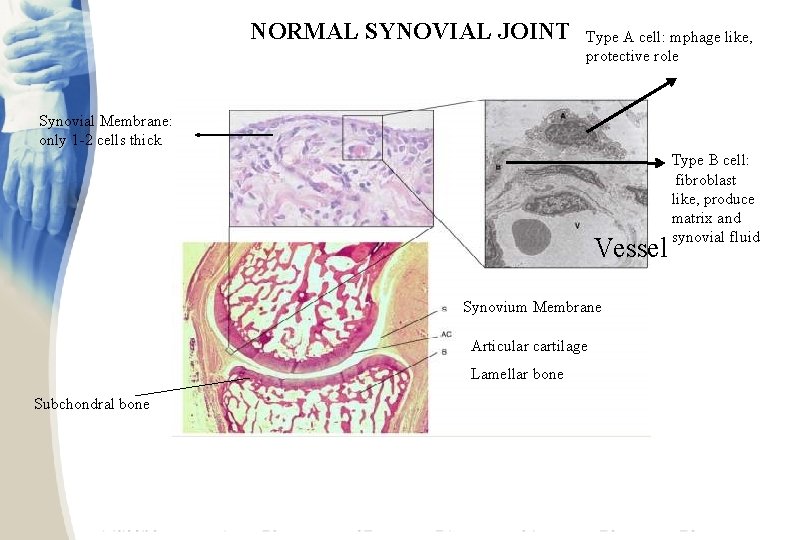
NORMAL SYNOVIAL JOINT Type A cell: mphage like, protective role Synovial Membrane: only 1 -2 cells thick Vessel Synovium Membrane Articular cartilage Lamellar bone Subchondral bone Type B cell: fibroblast like, produce matrix and synovial fluid
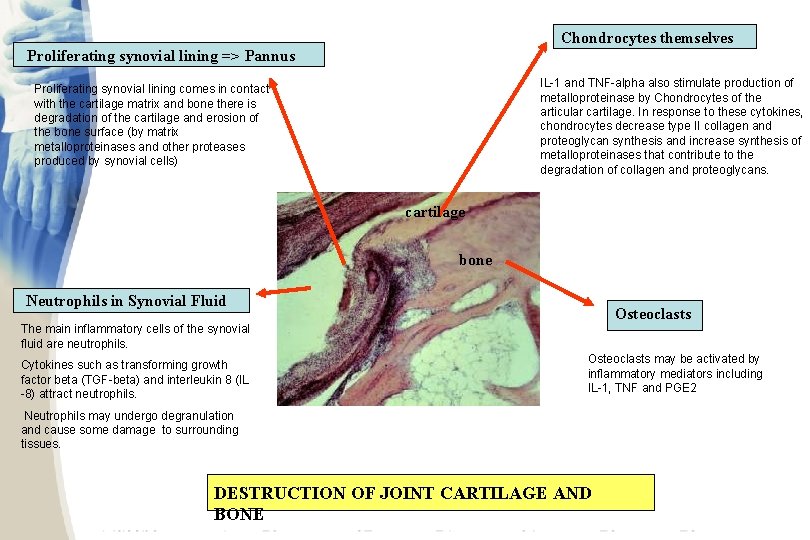
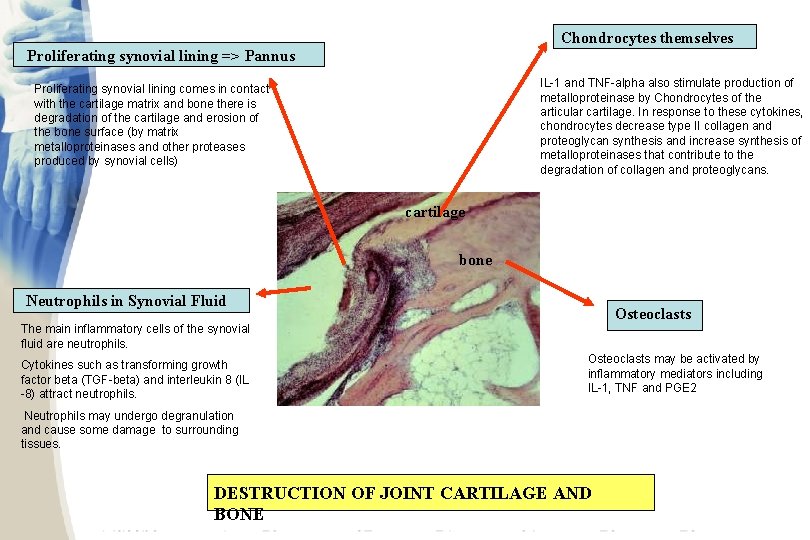
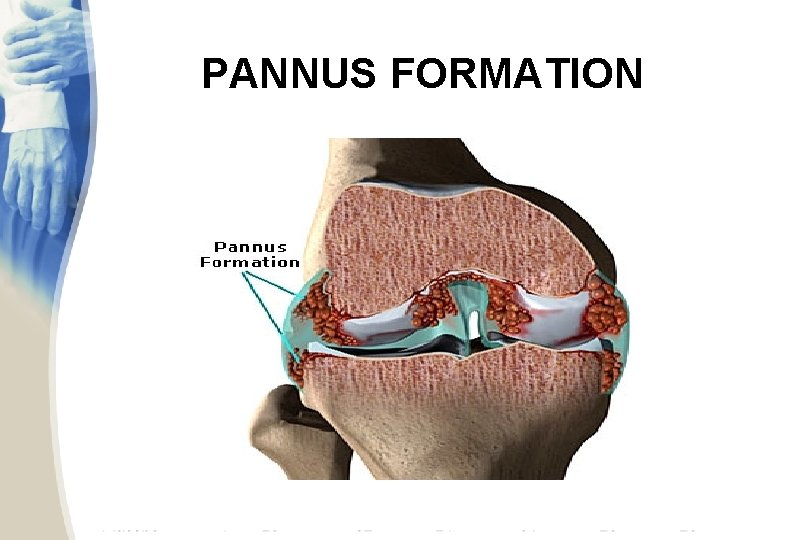
Chondrocytes themselves Proliferating synovial lining => Pannus IL-1 and TNF-alpha also stimulate production of metalloproteinase by Chondrocytes of the articular cartilage. In response to these cytokines, chondrocytes decrease type II collagen and proteoglycan synthesis and increase synthesis of metalloproteinases that contribute to the degradation of collagen and proteoglycans. Proliferating synovial lining comes in contact with the cartilage matrix and bone there is degradation of the cartilage and erosion of the bone surface (by matrix metalloproteinases and other proteases produced by synovial cells) cartilage bone Neutrophils in Synovial Fluid Osteoclasts The main inflammatory cells of the synovial fluid are neutrophils. Cytokines such as transforming growth factor beta (TGF-beta) and interleukin 8 (IL -8) attract neutrophils. Osteoclasts may be activated by inflammatory mediators including IL-1, TNF and PGE 2 Neutrophils may undergo degranulation and cause some damage to surrounding tissues. DESTRUCTION OF JOINT CARTILAGE AND BONE

CENTRAL ROLE OF TNFα IN RA Kirwan JR. J Rheumatol. 1999; 26: 720 -725.

EARLY CHANGES IN RA Thickened Synovium Lymphocytic Infiltrate Neovascularization Major type of cells in synovium are T-cells and macrophages whereas in synovial fluid are neutrophils
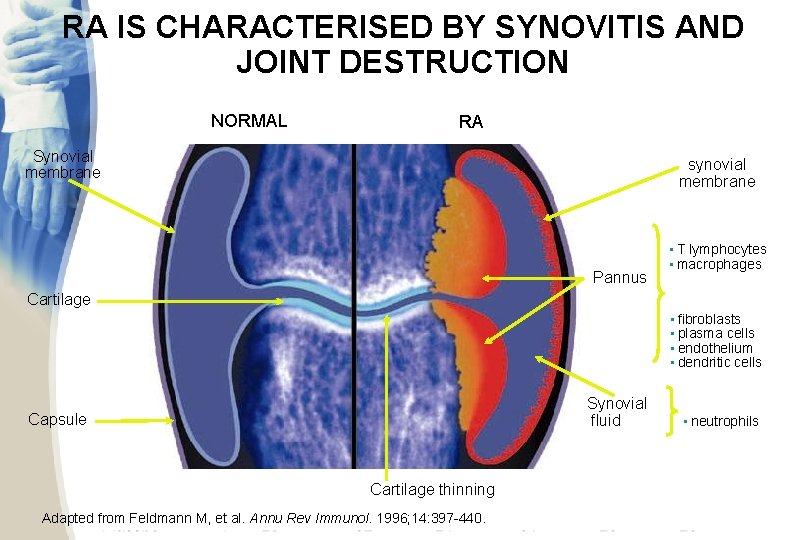
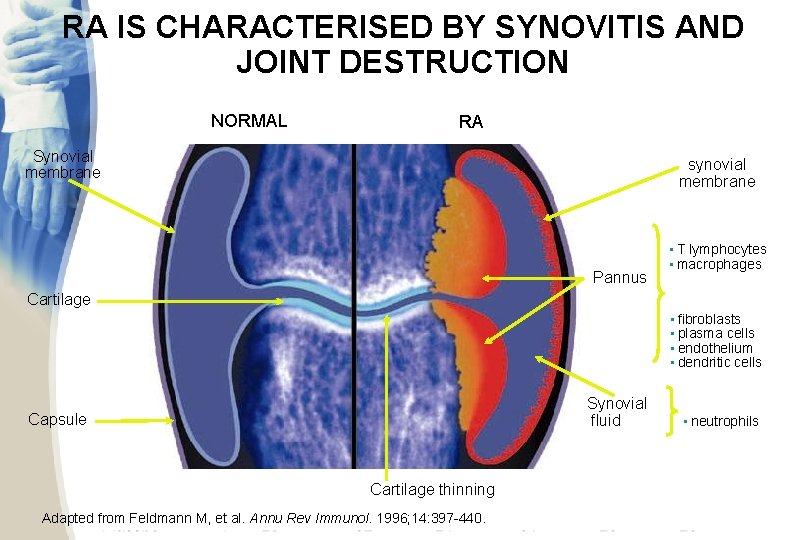
RA IS CHARACTERISED BY SYNOVITIS AND JOINT DESTRUCTION NORMAL RA Inflamed synovial membrane Synovial membrane Pannus Cartilage Major cell types: • T lymphocytes • macrophages Minor cell types: • fibroblasts • plasma cells • endothelium • dendritic cells Synovial fluid Capsule Cartilage thinning Adapted from Feldmann M, et al. Annu Rev Immunol. 1996; 14: 397 -440. Major cell type: • neutrophils
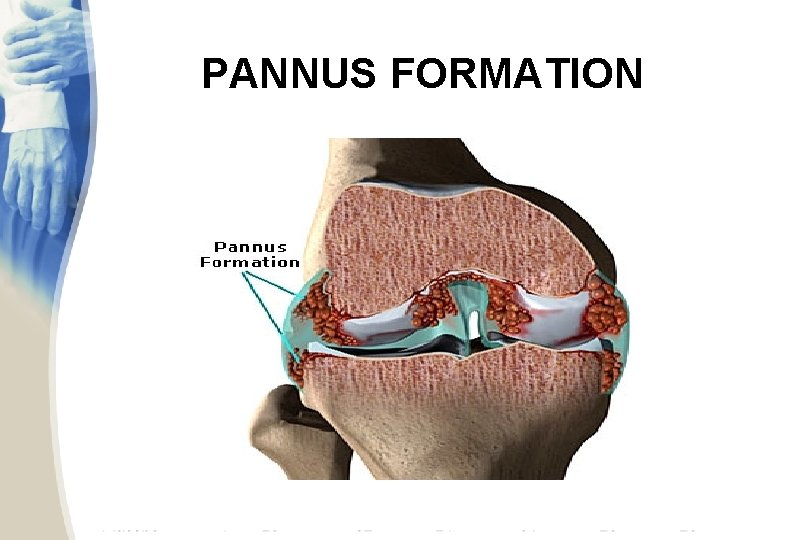
PANNUS FORMATION
CLINICAL MANIFESTATIONS § Articular findings: rheumatoid hand foot; C 1 -C 2 subluxation § Extra-articular findings: cardio-vascular (rhythm troubles, early accelerated atherosclerosis, vasculitis), respiratory (diffuse interstitial fibrosis, nodules, pleurisy), ocular (sicca syndrome), neurologic (peripheral & entrapment neuropathy), renal (amyloidosis), rheumatoid nodules, myositis, osteoporosis § Chronic evolution with flares ACR 1987 Diagnostic Criteria ACR and EULAR 2010 Classification Criteria ACR, American College of Rheumatology EULAR, European League Against Rheumatism
RHEUMATOID ARTHRITIS • Clinical presentation – usually presents insidiously; – prodromal syndrome of malaise, weight loss and vague periarticular pain and stiffness may be seen – less commonly, the onset is acute, triggered by a stressful situation such as infection, trauma, emotional strain or in the postpartum period. – the joint involvement is characteristically symmetric with associated stiffness, warmth tenderness and pain
RHEUMATOID ARTHRITIS • Clinical Features – the stiffness is characteristically worse in the morning and improves during the day; its duration is a useful indicator of the activity of the disease. – the usual joints affected by rheumatoid arthritis are the metacarpophalangeal joints, the PIP joints, the wrists, knees, ankles and toes. – Entrapment syndromes may occur especially carpal tunnel syndrome

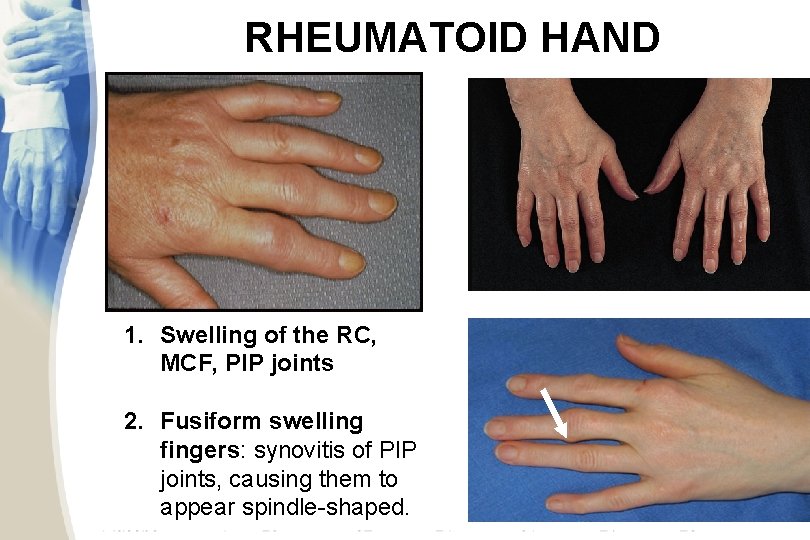
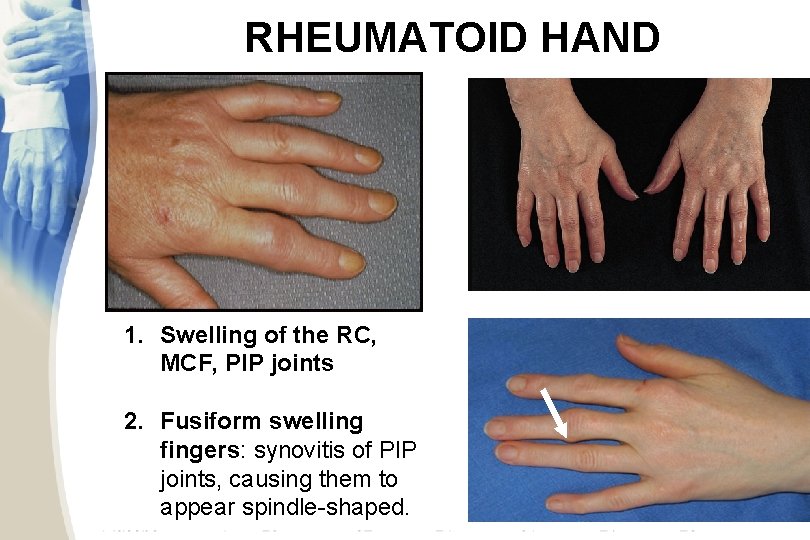
RHEUMATOID HAND 1. Swelling of the RC, MCF, PIP joints 2. Fusiform swelling fingers: synovitis of PIP joints, causing them to appear spindle-shaped. DEVIERE CUBITALA DEGETE POLICE “IN Z”
RHEUMATOID ARTHRITIS • After months to years, deformities can occur; the most common are – ulnar deviation of the fingers – swan neck deformity, which is hyperextension of the distal interphalangeal joint and flexion of the proximal interphalangeal joint – boutonniere deformity, which is flexion of the distal interphalangeal joint and extension of the proximal interphalangeal joint – valgus deformity of the knee

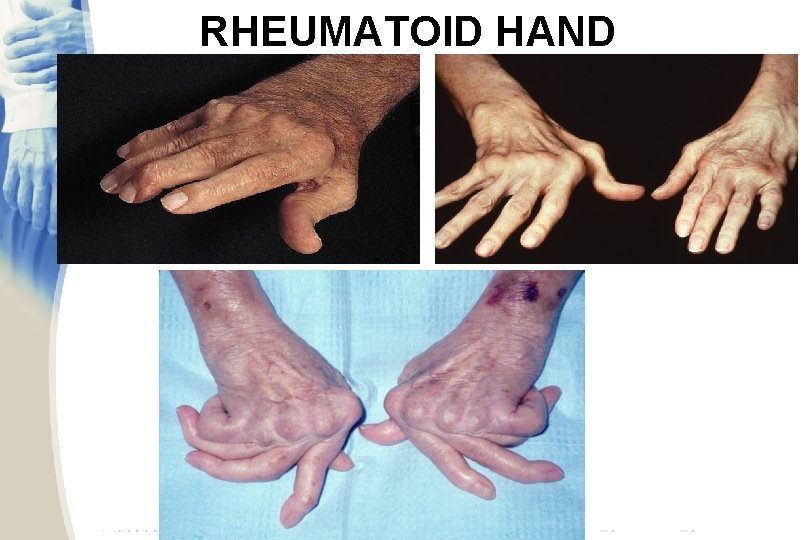
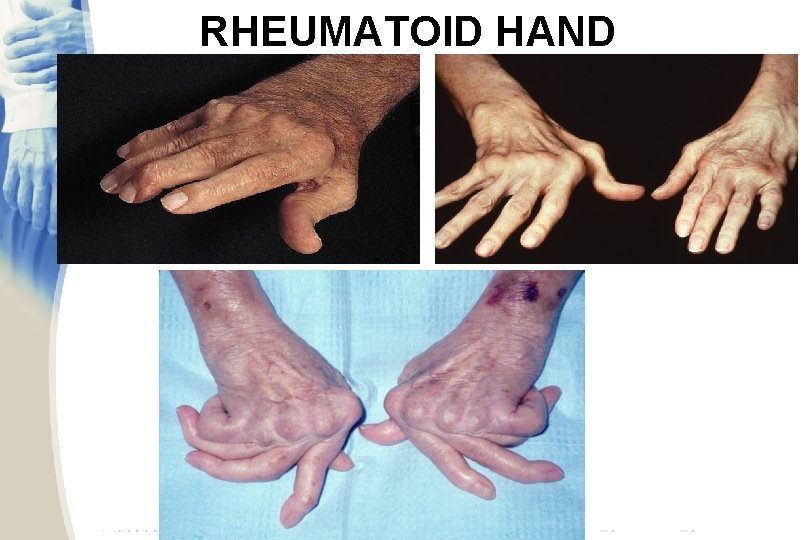
RHEUMATOID HAND
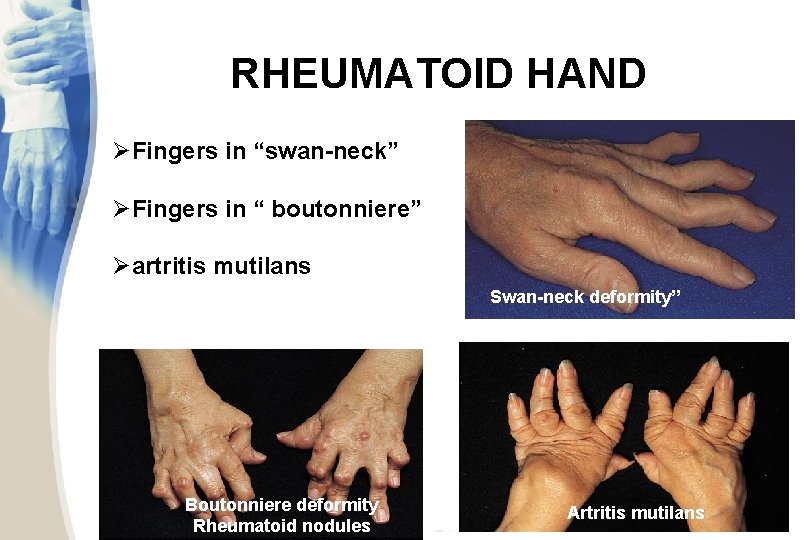
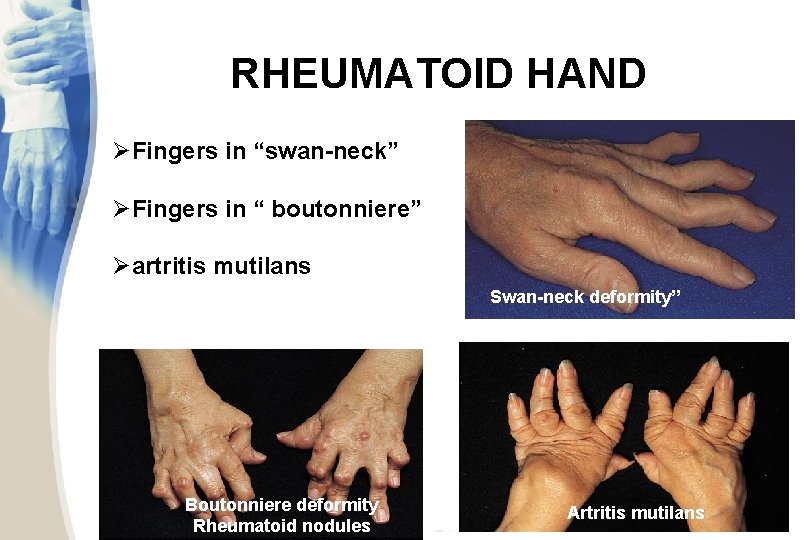
RHEUMATOID HAND ØFingers in “swan-neck” ØFingers in “ boutonniere” Øartritis mutilans Swan-neck deformity” DEGETE “IN GAT DE LEBADA” Boutonniere deformity Rheumatoid nodules Artritis mutilans

RHEUMATOID ARTHRITIS Saurabh Garg
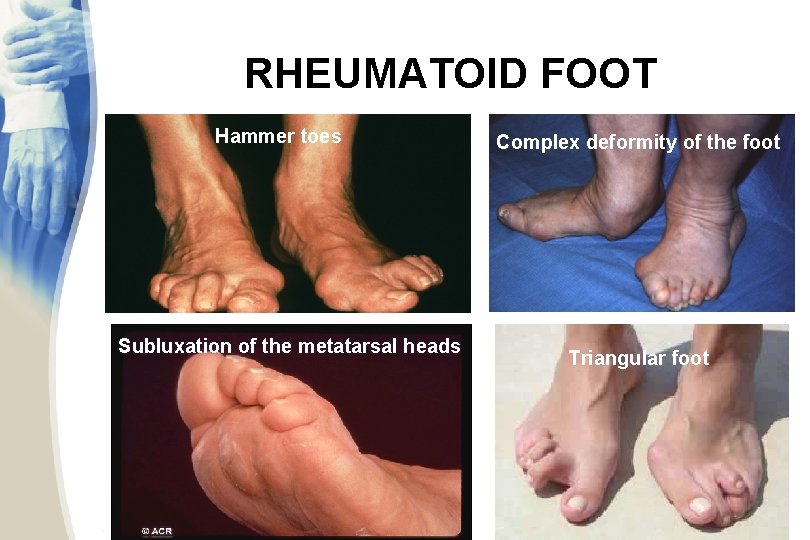
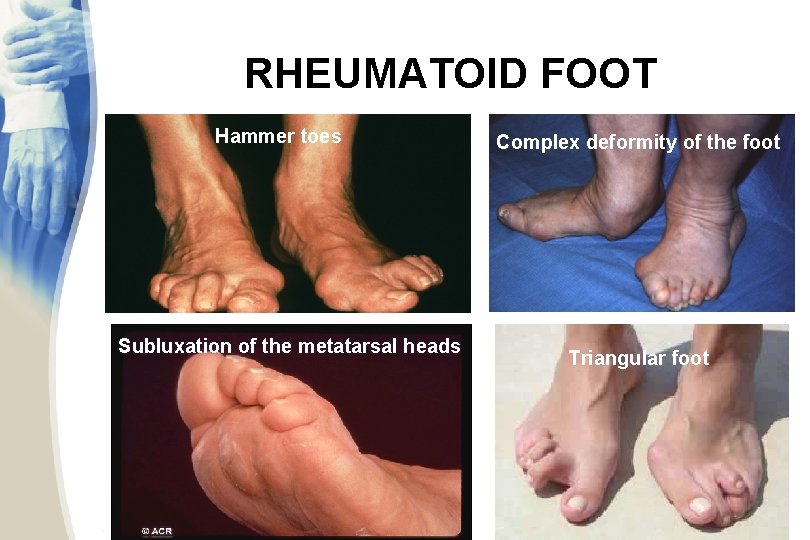
RHEUMATOID FOOT Hammer toes Subluxation of the metatarsal heads Complex deformity of the foot Triangular foot
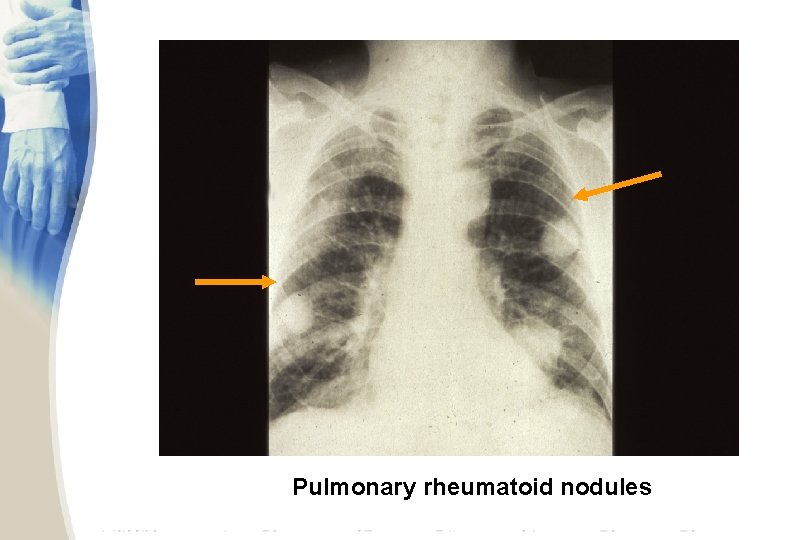
EXTRA-ARTICULAR MANIFESTATIONS • General: fever, lymphadenopaty, weit loss, fatigue • • • Dermatologic: rheumatoid nodules, vasculitis • Pulmonary manifestations: pleural involvement, fibrosing alveolitis , obliterative bronchiolitis Felty’s Syndrome: RA with splenomegaly and neutropenia • Ocular manifestations: Keratoconjunctivitis sicca, episcleritis, choroid and retinal nodules • Cardiac involvement: Constrictive pericarditis, myocarditis, coronary vasculitis, nodules on valves • Renal involvement: secondary amyloidosis • Neurologic manifestations: Mononeuritis multiplex, entrapment neuropathies, peripheral neuropathies • Hematologic manifestations: anemia, thrombocytosis

RHEUMATOID NODULES Subcutaneus nodules Occur 20 -35% of RA patients in severe, active disease with RF positive localisation: on the extensor surface of the forearms, in the olecranon bursa, over joints, and over pressure points, like sacrum and occiput characteristic histology: central area of fibrinoid necrosis surrounded by a zone of palisades of elongated histiocytes and a peripheral layer of cellular connective tissue
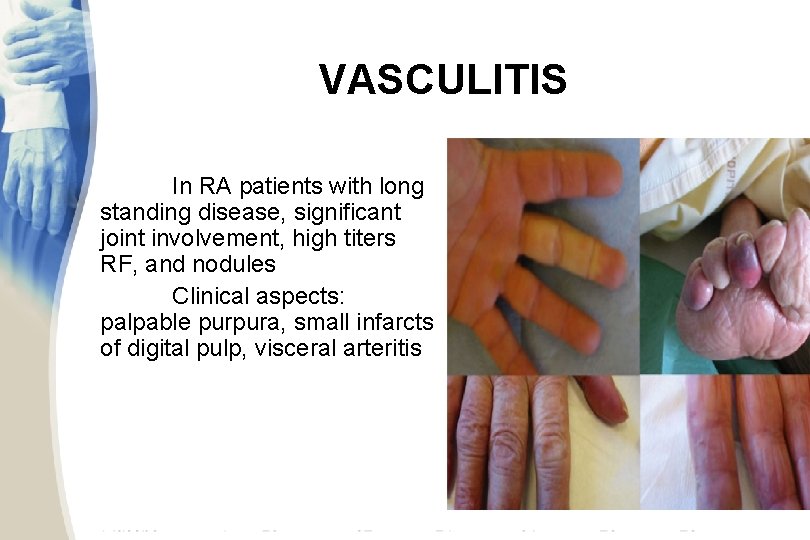
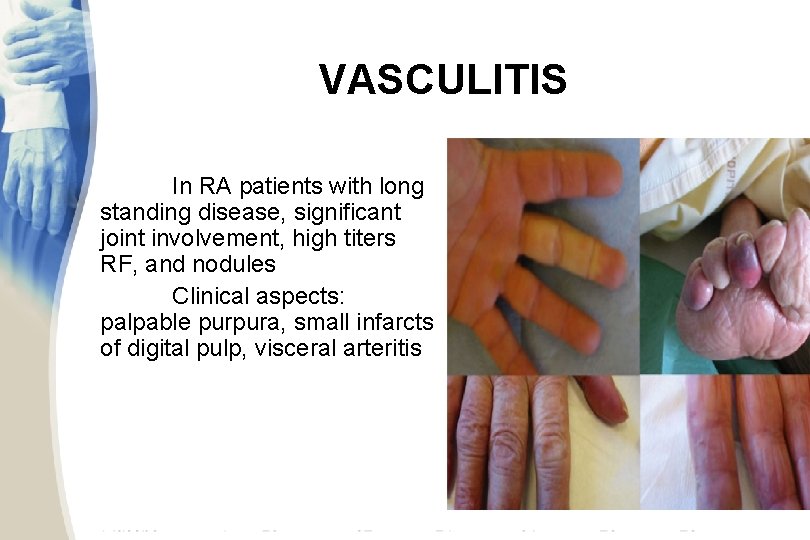
VASCULITIS In RA patients with long standing disease, significant joint involvement, high titers RF, and nodules Clinical aspects: palpable purpura, small infarcts of digital pulp, visceral arteritis
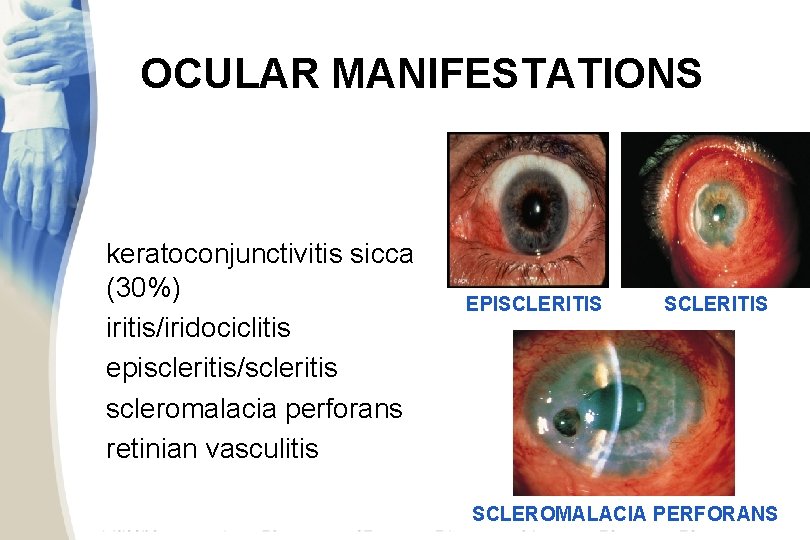
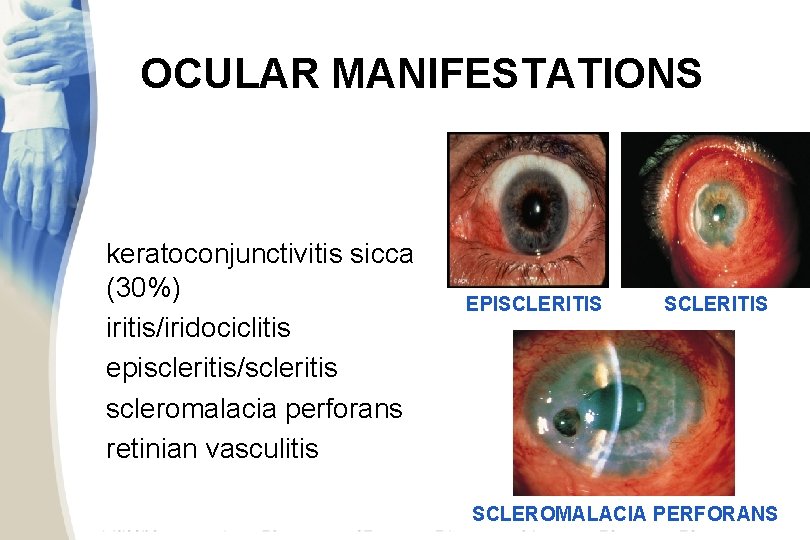
OCULAR MANIFESTATIONS keratoconjunctivitis sicca (30%) iritis/iridociclitis episcleritis/scleritis scleromalacia perforans retinian vasculitis EPISCLERITIS SCLEROMALACIA PERFORANS
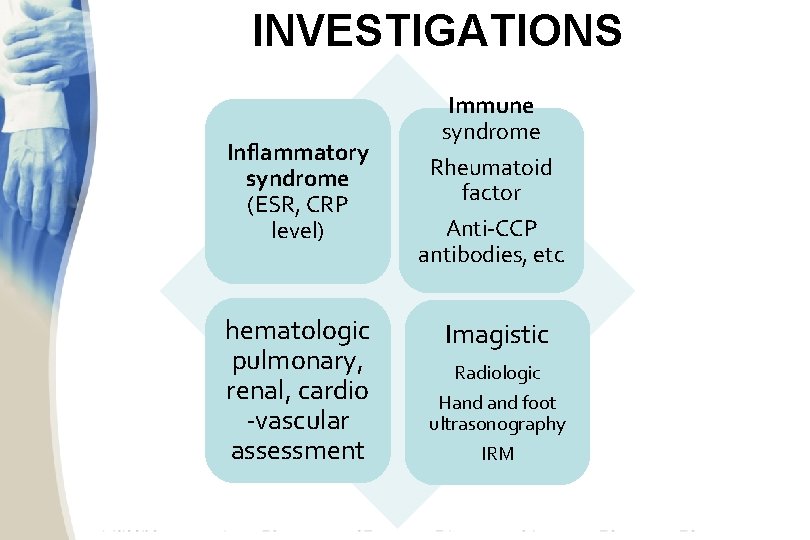
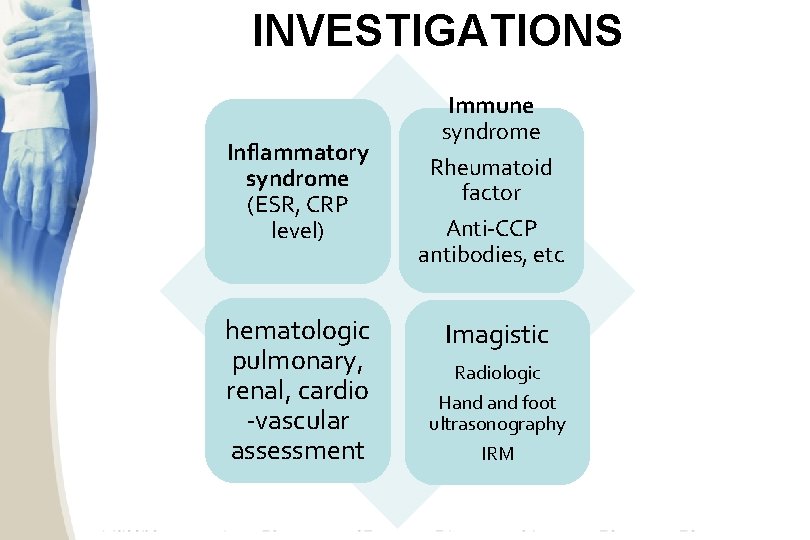
INVESTIGATIONS Inflammatory syndrome (ESR, CRP level) hematologic pulmonary, renal, cardio -vascular assessment Immune syndrome Rheumatoid factor Anti-CCP antibodies, etc Imagistic Radiologic Hand foot ultrasonography IRM
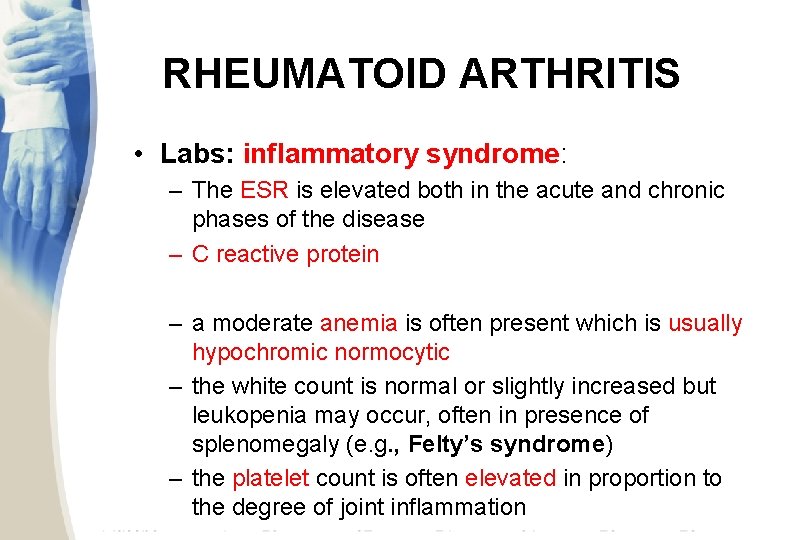
RHEUMATOID ARTHRITIS • Labs: inflammatory syndrome: – The ESR is elevated both in the acute and chronic phases of the disease – C reactive protein – a moderate anemia is often present which is usually hypochromic normocytic – the white count is normal or slightly increased but leukopenia may occur, often in presence of splenomegaly (e. g. , Felty’s syndrome) – the platelet count is often elevated in proportion to the degree of joint inflammation
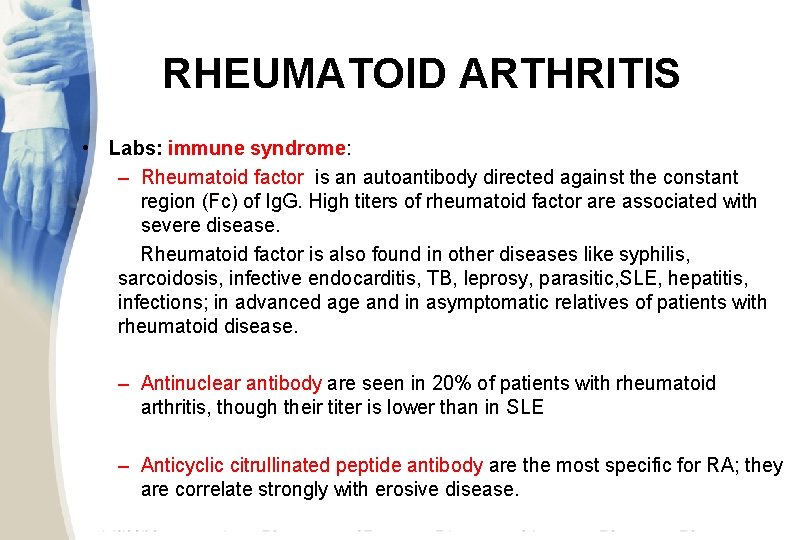
RHEUMATOID ARTHRITIS • Labs: immune syndrome: – Rheumatoid factor is an autoantibody directed against the constant region (Fc) of Ig. G. High titers of rheumatoid factor are associated with severe disease. Rheumatoid factor is also found in other diseases like syphilis, sarcoidosis, infective endocarditis, TB, leprosy, parasitic, SLE, hepatitis, infections; in advanced age and in asymptomatic relatives of patients with rheumatoid disease. – Antinuclear antibody are seen in 20% of patients with rheumatoid arthritis, though their titer is lower than in SLE – Anticyclic citrullinated peptide antibody are the most specific for RA; they are correlate strongly with erosive disease.
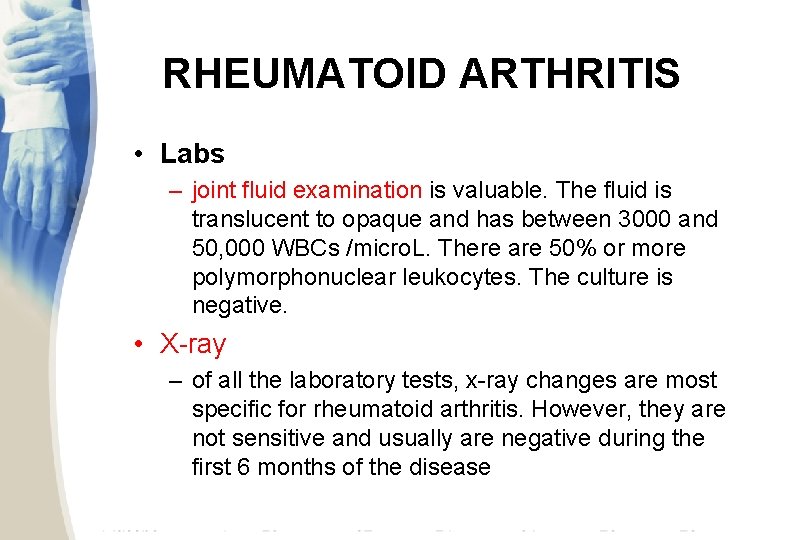
RHEUMATOID ARTHRITIS • Labs – joint fluid examination is valuable. The fluid is translucent to opaque and has between 3000 and 50, 000 WBCs /micro. L. There are 50% or more polymorphonuclear leukocytes. The culture is negative. • X-ray – of all the laboratory tests, x-ray changes are most specific for rheumatoid arthritis. However, they are not sensitive and usually are negative during the first 6 months of the disease
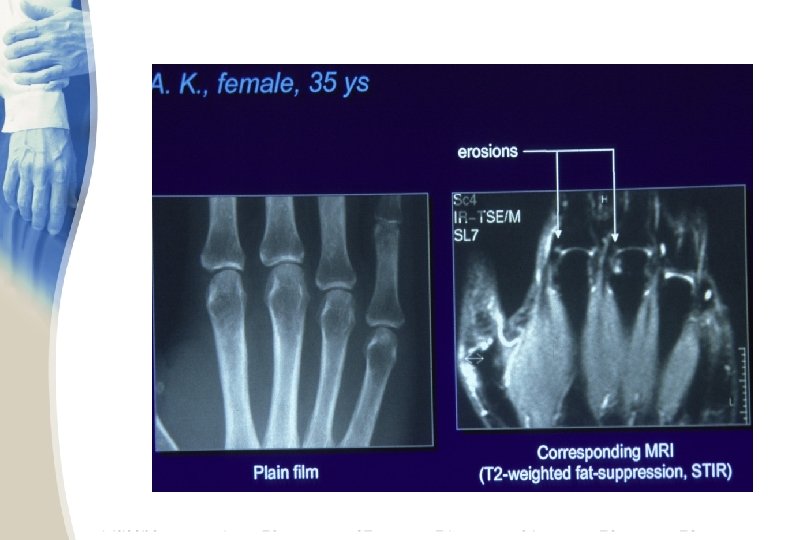
RHEUMATOID ARTHRITIS • X-rays – The earliest changes occur in the wrist or feet and consist of soft tissue swelling and juxta-articular demineralization. – Later, diagnostic changes consisting of joint space narrowing and erosions develop. The erosions are first seen at the ulnar styloid and at the juxtaarticular margin, where the bony surface is not protected by cartilage. – Diagnostic changes also occur in the cervical spine with C 1 -2 subluxation, but this can take several years to develop.

Juxta-articular osteoporosis

Bony erosions

geodes erosion


erosion
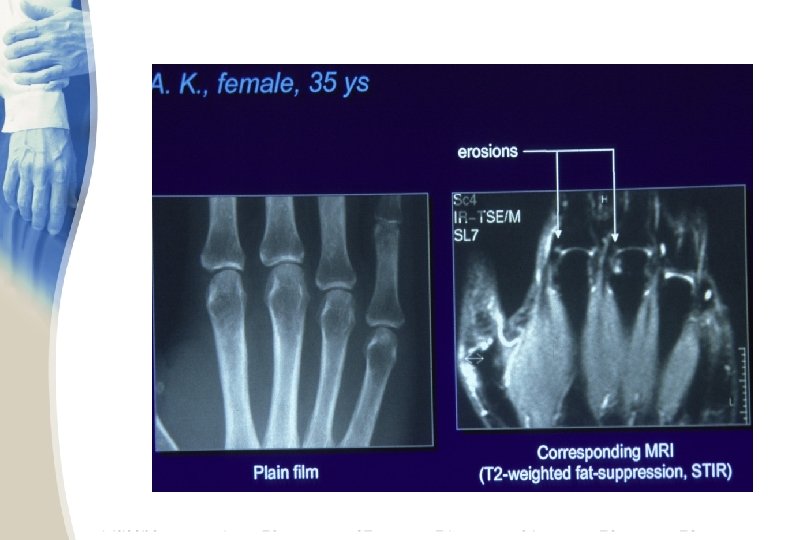

juxta-articular osteoporosis marginal erosions narrow joint space
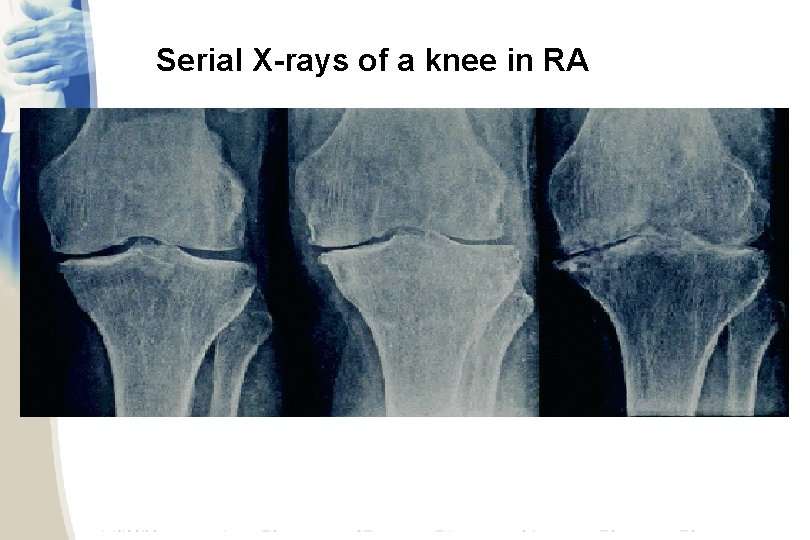
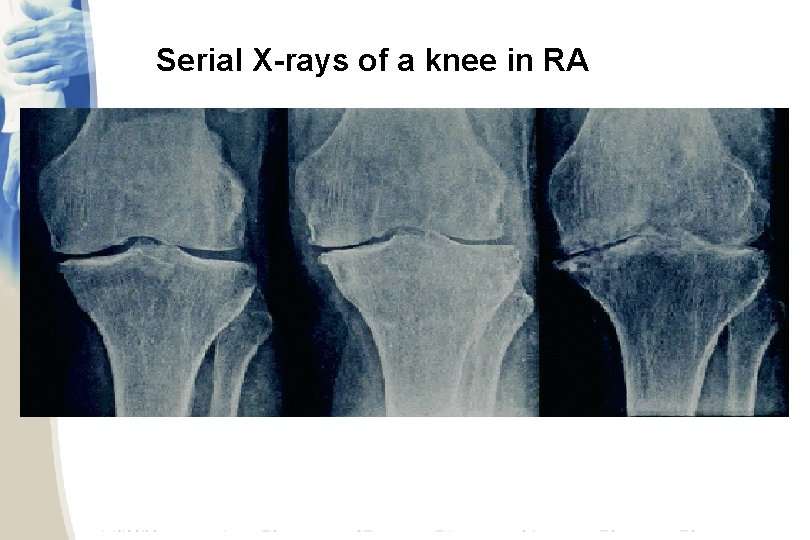
Serial X-rays of a knee in RA

C 1 -C 2 Subluxation
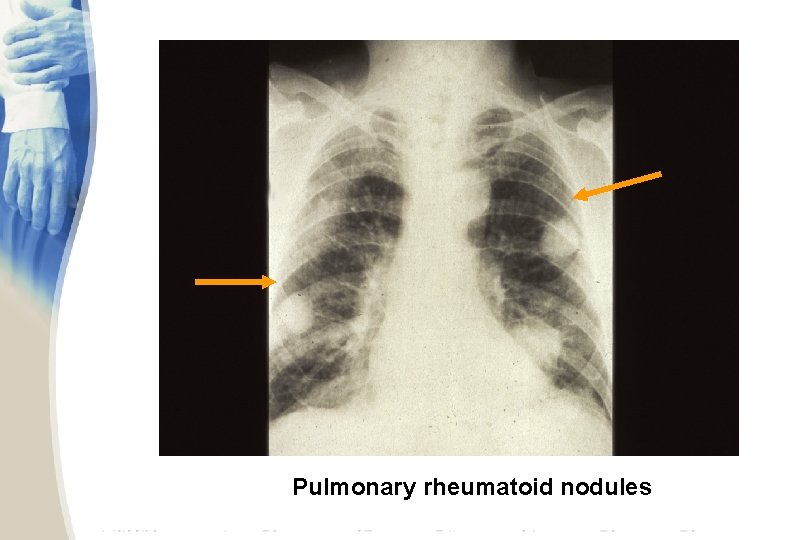
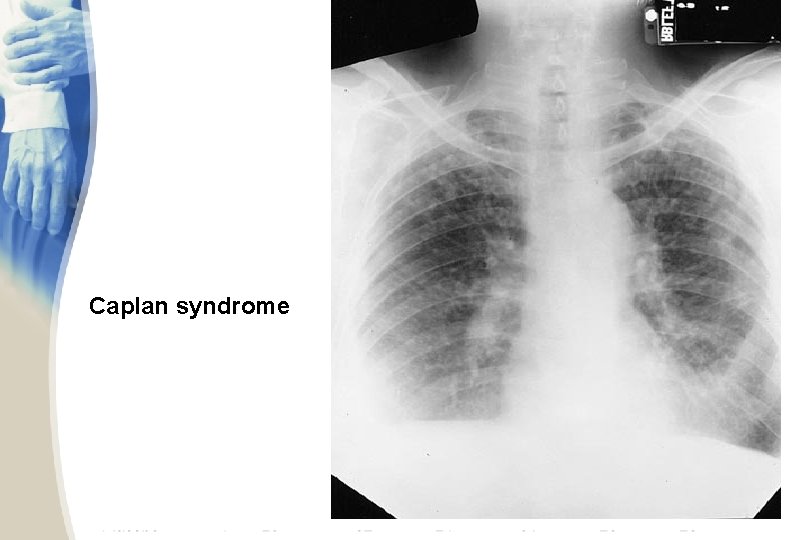
Pulmonary rheumatoid nodules
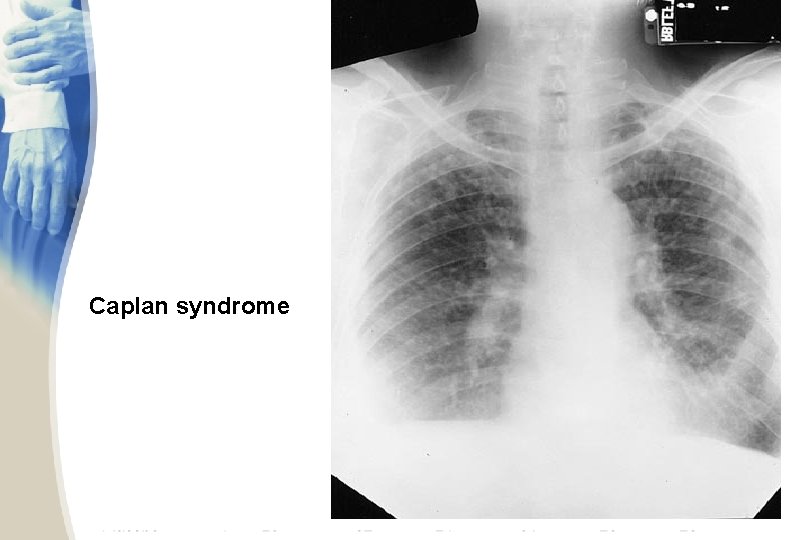
Caplan syndrome
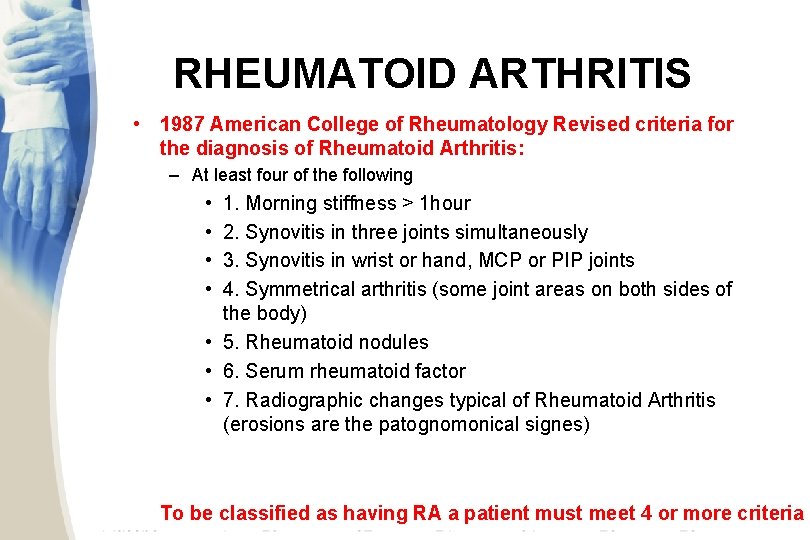
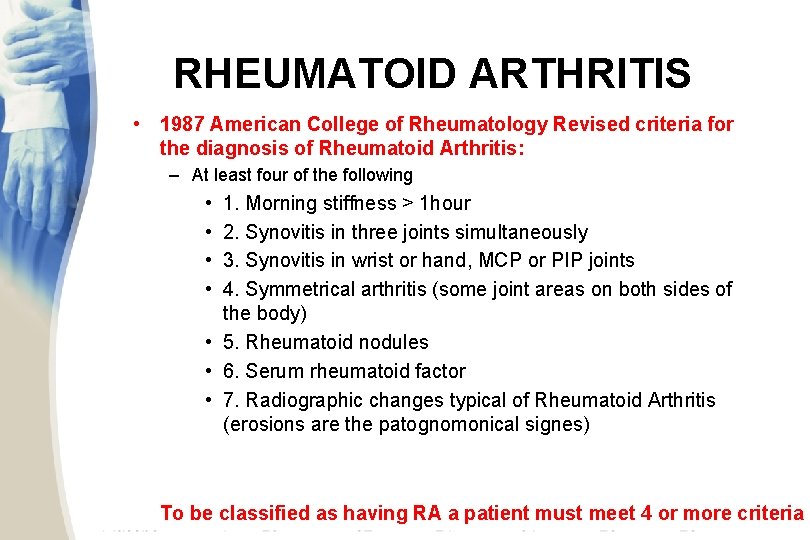
RHEUMATOID ARTHRITIS • 1987 American College of Rheumatology Revised criteria for the diagnosis of Rheumatoid Arthritis: – At least four of the following • • 1. Morning stiffness > 1 hour 2. Synovitis in three joints simultaneously 3. Synovitis in wrist or hand, MCP or PIP joints 4. Symmetrical arthritis (some joint areas on both sides of the body) • 5. Rheumatoid nodules • 6. Serum rheumatoid factor • 7. Radiographic changes typical of Rheumatoid Arthritis (erosions are the patognomonical signes) To be classified as having RA a patient must meet 4 or more criteria

PROBLEMS WITH OLD ACR CRITERIA • Work best in longstanding RA – But DMARDs work best in early RA and the goal is to prevent development of damage • Need criteria addressing earlier diagnosis given the benefits of early treatment • Need to include ACPA (CCP) – Balance with need for use in low resource settings where CCP not available • Goal of new criteria: predict who should be treated with DMARDs
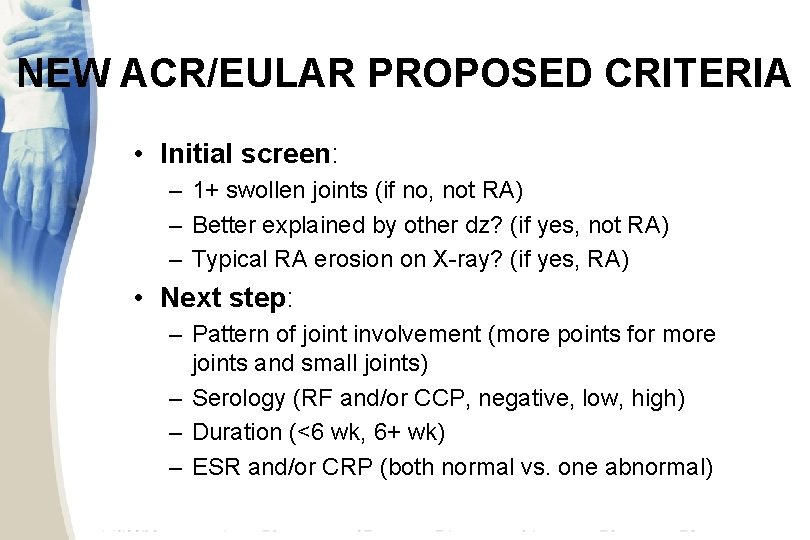
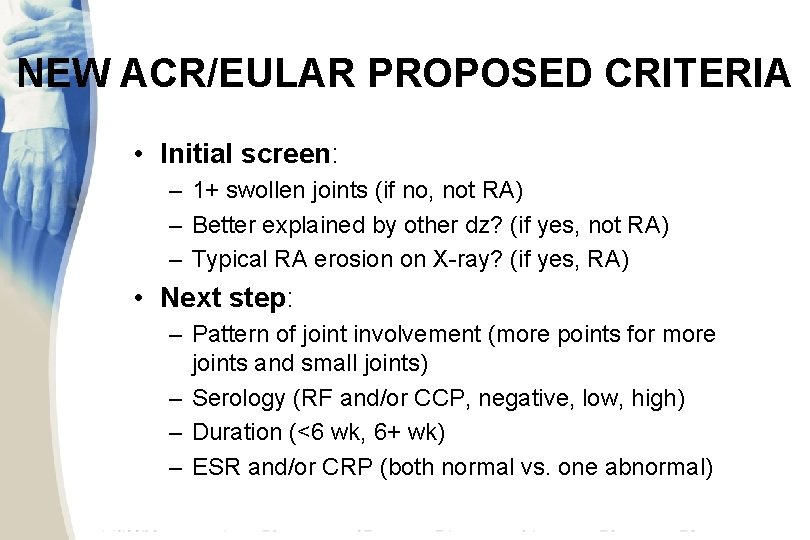
NEW ACR/EULAR PROPOSED CRITERIA • Initial screen: – 1+ swollen joints (if no, not RA) – Better explained by other dz? (if yes, not RA) – Typical RA erosion on X-ray? (if yes, RA) • Next step: – Pattern of joint involvement (more points for more joints and small joints) – Serology (RF and/or CCP, negative, low, high) – Duration (<6 wk, 6+ wk) – ESR and/or CRP (both normal vs. one abnormal)
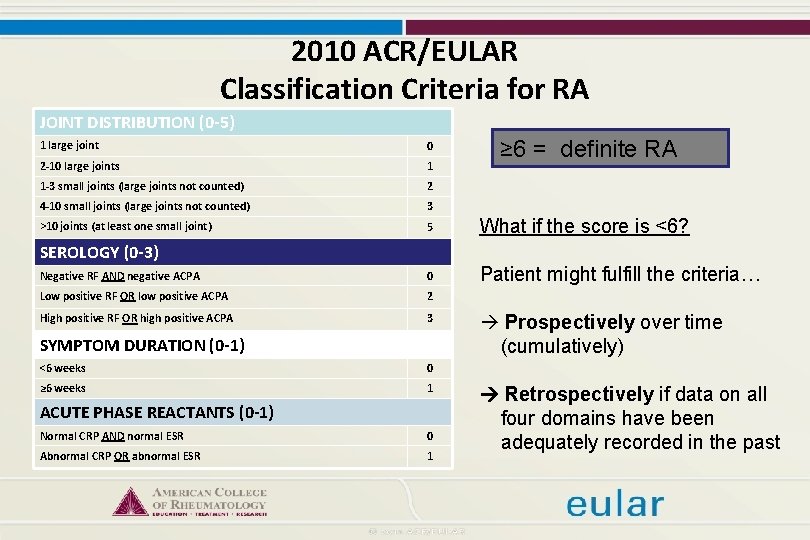
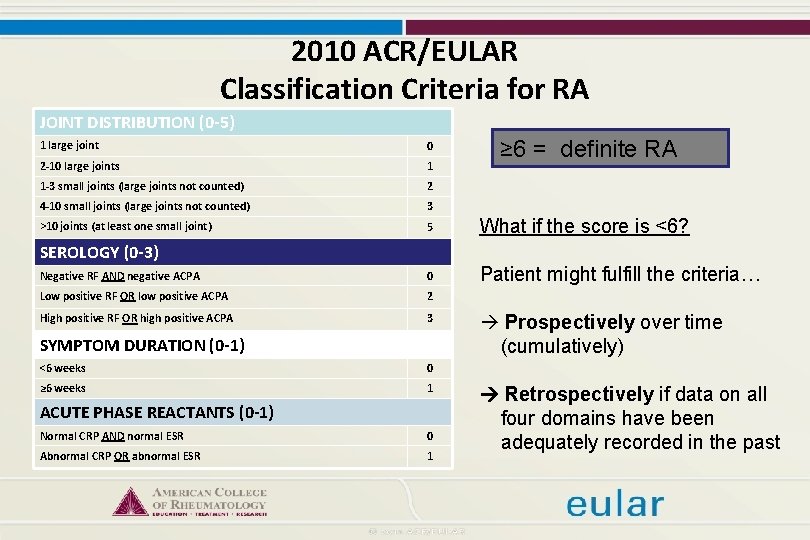
2010 ACR/EULAR Classification Criteria for RA JOINT DISTRIBUTION (0 -5) ≥ 6 = definite RA 1 large joint 0 2 -10 large joints 1 1 -3 small joints (large joints not counted) 2 4 -10 small joints (large joints not counted) 3 >10 joints (at least one small joint) 5 What if the score is <6? Negative RF AND negative ACPA 0 Patient might fulfill the criteria… Low positive RF OR low positive ACPA 2 High positive RF OR high positive ACPA 3 SEROLOGY (0 -3) SYMPTOM DURATION (0 -1) <6 weeks 0 ≥ 6 weeks 1 ACUTE PHASE REACTANTS (0 -1) Normal CRP AND normal ESR 0 Abnormal CRP OR abnormal ESR 1 Prospectively over time (cumulatively) Retrospectively if data on all four domains have been adequately recorded in the past
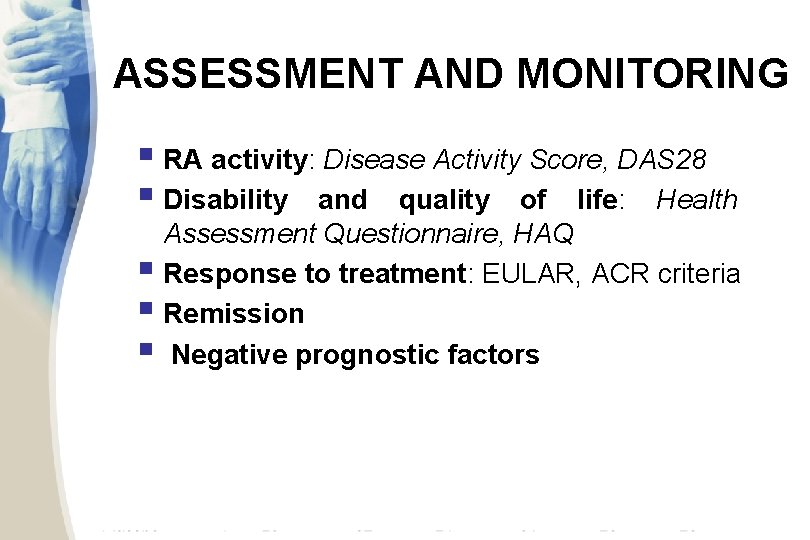
ASSESSMENT AND MONITORING § RA activity: Disease Activity Score, DAS 28 § Disability and quality of life: Health Assessment Questionnaire, HAQ § Response to treatment: EULAR, ACR criteria § Remission § Negative prognostic factors
ACR GUIDELINES FOR MANAGEMENT • Summarize evidence for DMARDs and biologics in different settings • Incorporate the following in treatment decisions – Disease duration (<6 mo, 6 -24, >24 mo) – Disease activity (low, moderate, high) – Features of poor prognosis Saag KG et al. Arthritis Rheum 2008; 59: 762

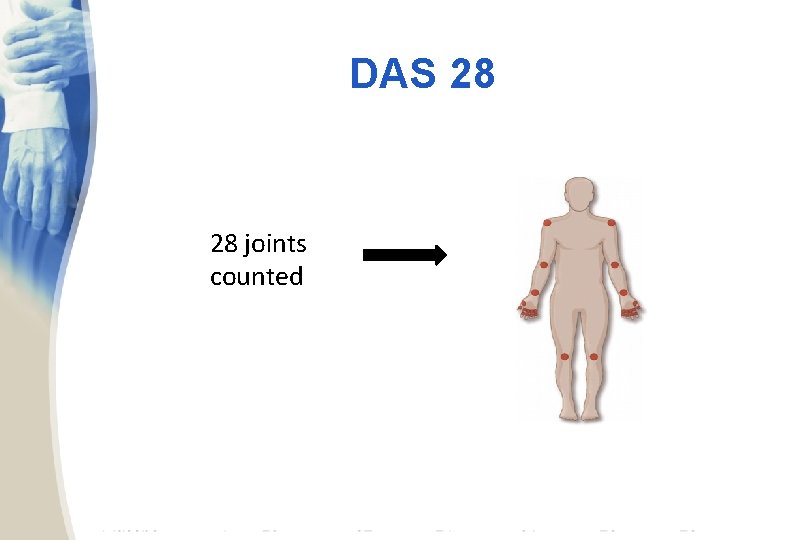
MEASUREMENT OF DISEASE ACTIVITY: DAS 28 AS EXAMPLE DAS 28 = 0. 56 * sqrt(tender 28) + 0. 28 * sqrt(swollen 28) + 0. 70 * ln(ESR) + 0. 014 * GH • Includes: – Tender joint count – Swollen joint count – ESR (or CRP in different version) – GH: Patient global disease activity assessment • Categorized: as low (<3. 2), moderate (3. 2 -5. 1), or high (>5. 1)
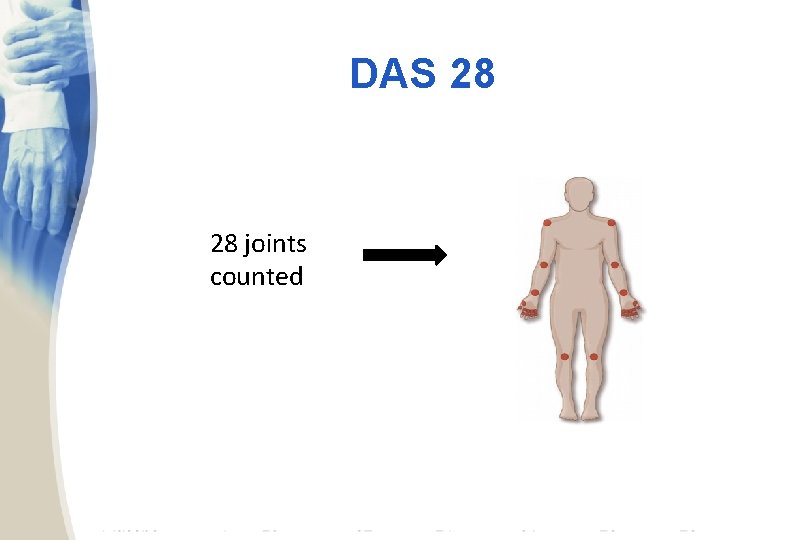
DAS 28 28 joints counted


POOR PROGNOSTIC FACTORS IN RA • • Presence of RF and/or CCP antibodies Radiographic erosions Functional limitation Extraarticular disease
REMISSION CRITERIA • 5 or more must be fulfilled for at least 2 consecutive months: – – – Morning stiffness not exceeding 15 minutes No fatigue No joint pain (by history) No joint tenderness or pain on motion No soft tissue swelling in joints or tendon sheaths ESR (W) < 30 mm/h (f); < 20 mm/h (m)
DIFFERENTIAL DIAGNOSIS – Rheumatic fever: migratory arthritis, elevated ASLO and dramatic response to Aspirin – Systemic Lupus Erythematosus: Butterfly rash, discoid lupus erythematous, photosensitivity, alopecia, high titers of Anti Ds-DNA, renal and CNS disease – Osteoarthritis: no constitutional manifestations and no evidence of joint inflammation – Gouty Arthritis: usually monoarticular initially but can become polyarticular in the later years
DIFFERENTIAL DIAGNOSIS – Pyogenic arthritis: usually monoarticular, fever and chills, abnormal joint fluid – Chronic Lyme disease: commonly monoarticular and associated with positive titers of anti Borrelia antibodies – Human Parvovirus infection: arthralgia more common than arthritis, rash may be present, serologic evidence of parvovirus B 19 infection – Polymyalgia rheumatica is associated with proximal muscle weakness and stiffness – several cancers produce paraneoplastic syndromes including polyarthritis; e. g. , hypertrophic pulmonary osteoarthropathy produced by lung and gastrointestinal cancers. Diffuse swelling of the palmar fascia has been associated with several cancers including ovarian cancer.
MANAGEMENT Objectives Obtaining remission/ minimal activity status – Inhibition of radiologic damage – Improve pain and inflammation – Maintain/improve articular function Drugs • Pathogenic: Disease Modifying Anti-Rheumatic Drugs DMARDs (methotrexate, leflunomide, sulfasalazine, hidroxicloroquine, azathioprine, cyclosporine); biological agents: (infliximab, etanercept, adalimumab, golimumab, certolizumab), anti. CD 20 (rituximab), anti-IL 6 (tocilizumab), anti-costimulation molecules (abatacept) • Corticosteroids (systemic & local) Surgery: Synovectomy, total joint replacement) Rehabilitation: Physical & kynetotherapy

DMARDs (Disease-Modifying Anti. Rheumatic Drugs) Traditional • Hydroxychloroquine (Plaquenil) • Sulfasalazine • Methotrexate • Leflunomide (Arava) • Less commonly used: – Azathioprine – Gold, PO or IM – Cyclosporine Biologics • • • Etanercept (Enbrel) Infliximab (Remicade) Adalimumab (Humira) Golimumab (Simponi) Certolizumab Pegol (Cimzia) Anakinra (Kineret) Rituximab (Rituxan) Abatacept (Orencia) Tocilizumab (Actemra)
RHEUMATOID ARTHRITIS • Treatment – goal of treatment • reduce inflammation and pain, • preservation of function, and • prevention of deformity.

RHEUMATOID ARTHRITIS • Treatment NSAIDs: Ibuprofen, naproxen, sulindac and other NSAIDs may also be effective though they are associated with a number of side effects including • GI irritation and peptic ulcers (misoprostol can reduce the incidence of peptic ulcers associated with NSAIDs) • Kidney damage • Liver damage
BENEFITS OF EARLY DETECTION AND DMARD THERAPY • Decreased RA severity, disability and mortality with DMARDs • Less need for joint replacement surgery • May decrease risk of cardiovascular disease and mortality
RHEUMATOID ARTHRITIS • Treatment (Disease Modifying Agents (DMARDs) – Methotrexate: the gold standard for RA. – It produces a beneficial effect in 2 -6 weeks and is given once weekly. – The usual dose is 10 -25 mg once a week. The most common side effect is gastric irritation and stomatitis. Other side effects are hepatotoxicity, pancytopenia and interstitial pneumonitis. • Combine with folic acid (at least 1 mg per day)
RHEUMATOID ARTHRITIS • Treatment – Antimalarials such as hydroxychloroquine sulfate is effective in 25 -50% of patients and in most cases after 3 -6 months of therapy. It is reserved for mild disease. Doses: 200 -400 mg/day. – Sulfasalazine: 2 -3 g daily – Leflunomide: 20 mg daily; side effects: diarrhea, hepatotoxicity, hypertension.
RHEUMATOID ARTHRITIS • Treatment. – Corticosteroids produce immediate and dramatic anti-inflammatory benefit but are limited by their many side effects – “bridge therapy” to shut off the inflammation rapidly – Prednison 10 mg daily. • Consider using low-dose corticosteroids, if necessary
LIMITATIONS OF TRADITIONAL DMARDS • Lack of efficacy in some patients • May not slow radiographic progression • Toxicity (less common reason for discontinuation)
BIOLOGICS IN RA • All recommended with methotrexate • Biologic agents target: – Tumor necrosis factor- (TNF- ) – Co-stimulation between B and T cells – B cell surface proteins – Interleukin-6 (IL-6) – More likely to come soon….
TNFα INHIBITORS • Generally accepted as first-line biologics • Add to methotrexate when disease activity remains moderate to high (after adequate trial) • Five different agents available
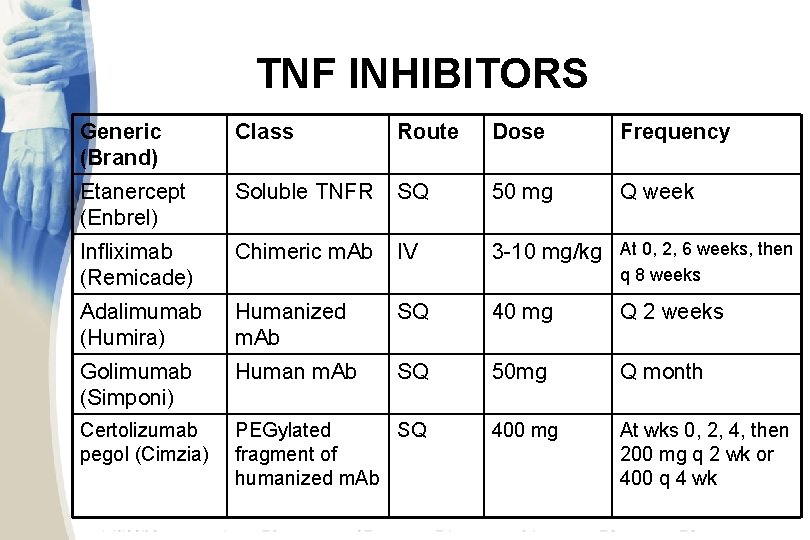
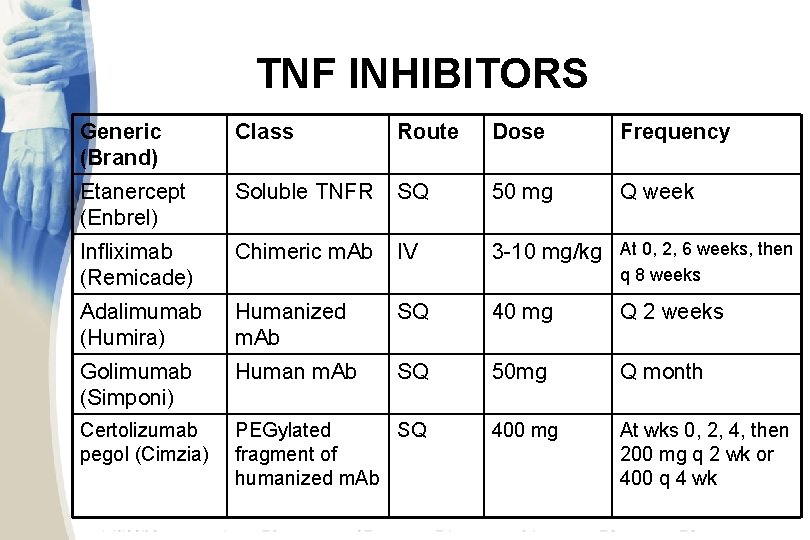
TNF INHIBITORS Generic (Brand) Class Route Dose Frequency Etanercept (Enbrel) Soluble TNFR SQ 50 mg Q week Infliximab (Remicade) Chimeric m. Ab IV 3 -10 mg/kg At 0, 2, 6 weeks, then Adalimumab (Humira) Humanized m. Ab SQ 40 mg Q 2 weeks Golimumab (Simponi) Human m. Ab SQ 50 mg Q month Certolizumab pegol (Cimzia) PEGylated SQ fragment of humanized m. Ab 400 mg At wks 0, 2, 4, then 200 mg q 2 wk or 400 q 4 wk q 8 weeks
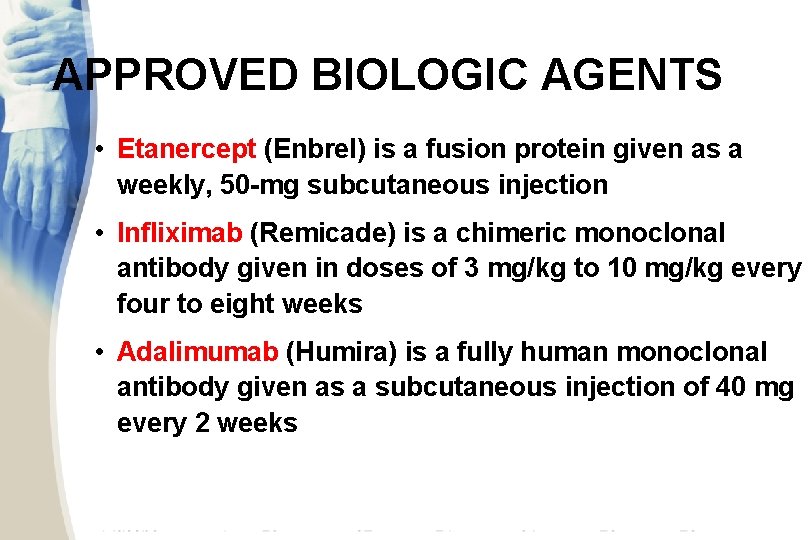
APPROVED BIOLOGIC AGENTS • Etanercept (Enbrel) is a fusion protein given as a weekly, 50 -mg subcutaneous injection • Infliximab (Remicade) is a chimeric monoclonal antibody given in doses of 3 mg/kg to 10 mg/kg every four to eight weeks • Adalimumab (Humira) is a fully human monoclonal antibody given as a subcutaneous injection of 40 mg every 2 weeks
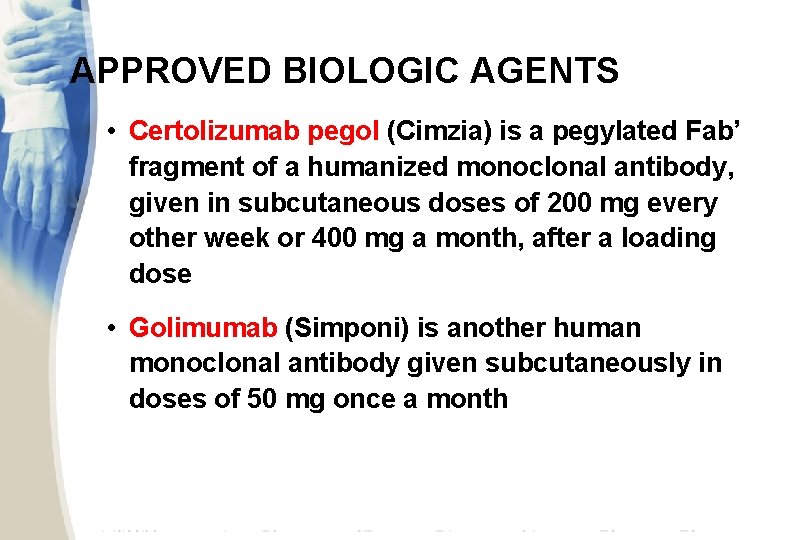
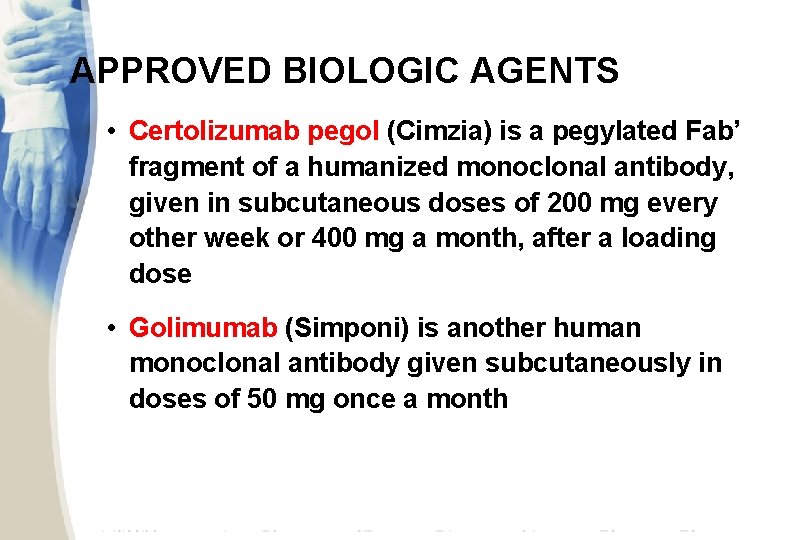
APPROVED BIOLOGIC AGENTS • Certolizumab pegol (Cimzia) is a pegylated Fab’ fragment of a humanized monoclonal antibody, given in subcutaneous doses of 200 mg every other week or 400 mg a month, after a loading dose • Golimumab (Simponi) is another human monoclonal antibody given subcutaneously in doses of 50 mg once a month
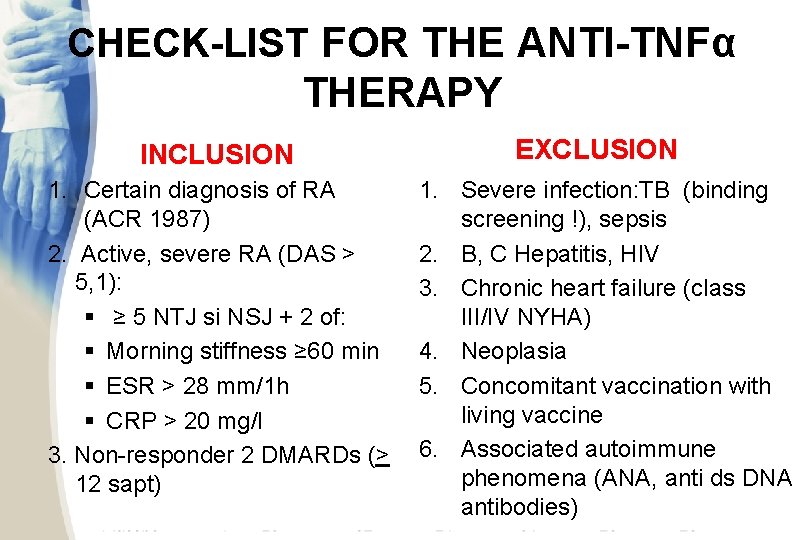
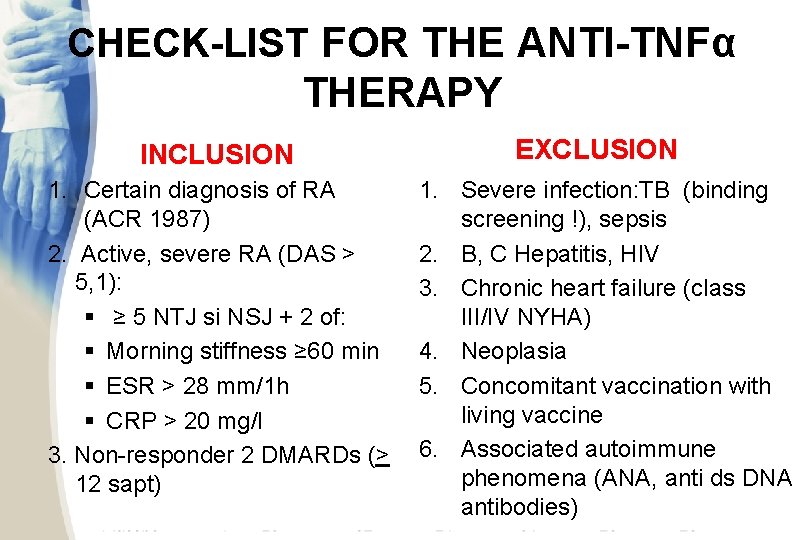
CHECK-LIST FOR THE ANTI-TNFα THERAPY INCLUSION 1. Certain diagnosis of RA (ACR 1987) 2. Active, severe RA (DAS > 5, 1): § ≥ 5 NTJ si NSJ + 2 of: § Morning stiffness ≥ 60 min § ESR > 28 mm/1 h § CRP > 20 mg/l 3. Non-responder 2 DMARDs (> 12 sapt) EXCLUSION 1. Severe infection: TB (binding screening !), sepsis 2. B, C Hepatitis, HIV 3. Chronic heart failure (class III/IV NYHA) 4. Neoplasia 5. Concomitant vaccination with living vaccine 6. Associated autoimmune phenomena (ANA, anti ds DNA antibodies)
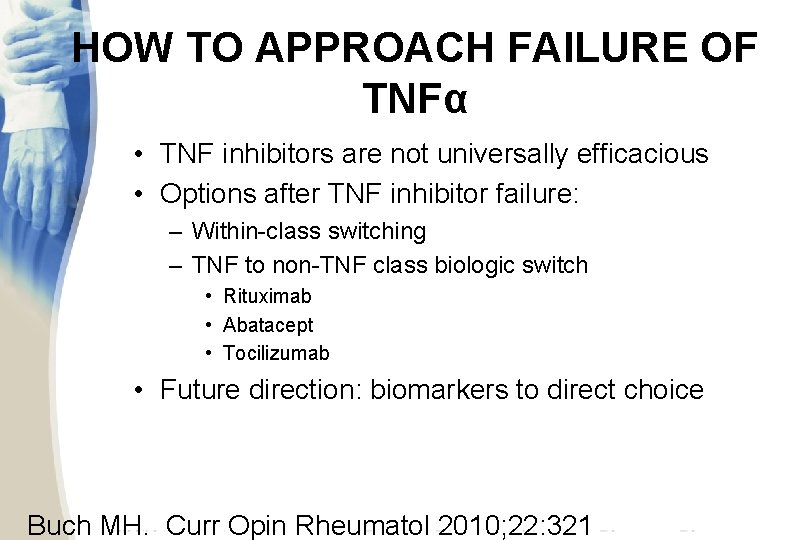
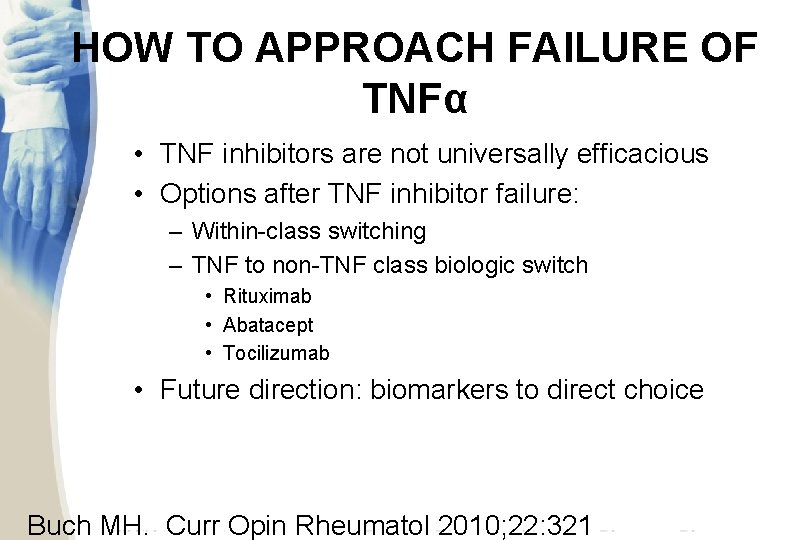
HOW TO APPROACH FAILURE OF TNFα • TNF inhibitors are not universally efficacious • Options after TNF inhibitor failure: – Within-class switching – TNF to non-TNF class biologic switch • Rituximab • Abatacept • Tocilizumab • Future direction: biomarkers to direct choice Buch MH. Curr Opin Rheumatol 2010; 22: 321
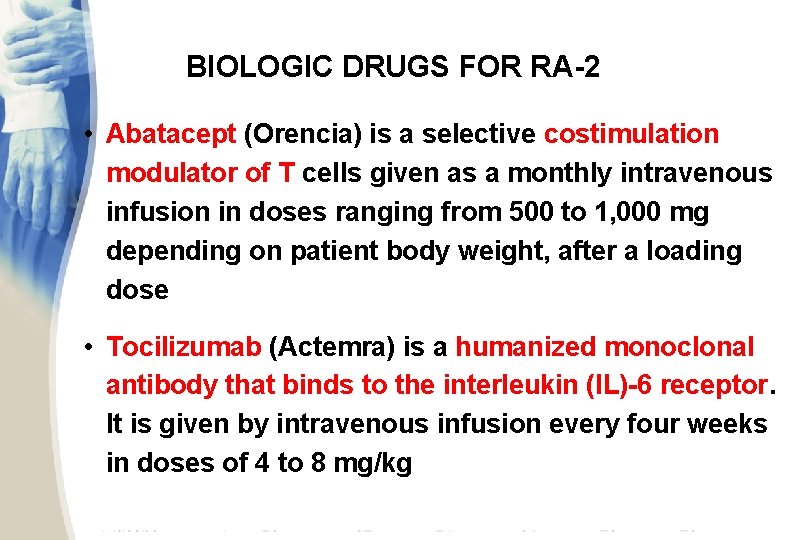
BIOLOGIC DRUGS FOR RA-2 • Abatacept (Orencia) is a selective costimulation modulator of T cells given as a monthly intravenous infusion in doses ranging from 500 to 1, 000 mg depending on patient body weight, after a loading dose • Tocilizumab (Actemra) is a humanized monoclonal antibody that binds to the interleukin (IL)-6 receptor. It is given by intravenous infusion every four weeks in doses of 4 to 8 mg/kg
Biologic Drugs for RA-2 • Rituximab (Mabthera) is a chimeric monoclonal antibody against the CD 20 protein on the surface of B cells. This drug is given as two 1, 000 mg infusions; the frequency of repeat therapy is at 24 weeks after the last infusion
Common Adverse Effects of the Biologic Drugs • Etanercept: Infections and injection site reactions • Infliximab: Upper respiratory tract infections, sinusitis, pharyngitis, infusion reactions, headache, and abdominal pain • Adalimumab: Upper respiratory tract infections, sinusitis, injection site reactions, headache, and rash
Common Adverse Effects of the Biologic Drugs • Certolizumab pegol: Upper respiratory tract infections, rash, and urinary tract infections • Golimumab: Upper respiratory tract infections, nasopharyngitis • Abatacept: Headache, upper respiratory tract infections, nasopharyngitis, and nausea
Common Adverse Effects of the Biologic Drugs • Tocilizumab: Upper respiratory tract infections, nasopharyngitis, headache, hypertension, increased alanine transaminase levels • Rituximab: Upper respiratory tract infection, nasopharyngitis, urinary tract infection, bronchitis. Other potentially important events include infusion reactions, serious infections, cardiovascular events and, progressive multifocal leukoencephalopathy
 Cause of sle
Cause of sle Steinbrocker stage
Steinbrocker stage What is esr
What is esr Polyarticular arthritis
Polyarticular arthritis Abatacept
Abatacept Juvenile rheumatoid arthritis
Juvenile rheumatoid arthritis Rheumatoid arthritis extra-articular manifestations
Rheumatoid arthritis extra-articular manifestations Rheumatoid arthritis in hands
Rheumatoid arthritis in hands Barik meaning
Barik meaning Rheumatoid arthritis side effects
Rheumatoid arthritis side effects Nursing diagnosis for gouty arthritis
Nursing diagnosis for gouty arthritis Z line deformity
Z line deformity Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Rheumatoid arthritis
Rheumatoid arthritis Rheumatoid arthritis
Rheumatoid arthritis Translating research findings to clinical nursing practice
Translating research findings to clinical nursing practice Dr eugene lim
Dr eugene lim Poststreptococcal reactive arthritis
Poststreptococcal reactive arthritis Gossec
Gossec Gonorrhea symptoms female
Gonorrhea symptoms female Anatomi fisiologi asam urat
Anatomi fisiologi asam urat Septic arthritis complications
Septic arthritis complications Septic arthritis antibiotics
Septic arthritis antibiotics Septic arthritis antibiotics
Septic arthritis antibiotics Arthritis foundation indiana
Arthritis foundation indiana Septic arthritis complications
Septic arthritis complications Caprine arthritis encefalitis
Caprine arthritis encefalitis Kode icd 10 bursitis genu
Kode icd 10 bursitis genu Septic arthritis
Septic arthritis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Zveren
Zveren Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Example of gram negative cocci
Example of gram negative cocci Boutonniere nodes
Boutonniere nodes Reactive arthritis
Reactive arthritis Gout treatment
Gout treatment Seronegative arthritis
Seronegative arthritis 강직성척추염 grade
강직성척추염 grade Septic arthritis workup
Septic arthritis workup Arthritis treatment
Arthritis treatment Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Viral arthritis
Viral arthritis Peripheral arthritis
Peripheral arthritis Dorsopathies adalah
Dorsopathies adalah Gardening with arthritis
Gardening with arthritis Arthritis in shoulder nhs
Arthritis in shoulder nhs Psoriasis arthritis nhs
Psoriasis arthritis nhs Left knee arthritis
Left knee arthritis Arthritis infusion treatment
Arthritis infusion treatment Rehaklinik psoriasis arthritis
Rehaklinik psoriasis arthritis Rheumatisches granulom
Rheumatisches granulom Gonococcal vs nongonococcal arthritis
Gonococcal vs nongonococcal arthritis Arthritis and food allergies
Arthritis and food allergies Chapter 10 qualitative research designs
Chapter 10 qualitative research designs Tactile fremitus normal findings
Tactile fremitus normal findings Significant findings example
Significant findings example Findings in research
Findings in research Qualitative and quantitative data analysis
Qualitative and quantitative data analysis Apices of lungs
Apices of lungs Rickets def
Rickets def Qualitative results and discussion
Qualitative results and discussion Conncets
Conncets Application forms qualitative or quantitative
Application forms qualitative or quantitative Presentation of findings
Presentation of findings Quadrant of the abdomen
Quadrant of the abdomen Acute interstitial nephritis urine findings
Acute interstitial nephritis urine findings Desiredresults.us
Desiredresults.us Ecg findings in atrial fibrillation
Ecg findings in atrial fibrillation Difference between megaloblastic and pernicious anemia
Difference between megaloblastic and pernicious anemia Laboratory findings of megaloblastic anemia
Laboratory findings of megaloblastic anemia Vwf deficiency labs
Vwf deficiency labs Semi-tabular presentation
Semi-tabular presentation Mouth assessment normal findings
Mouth assessment normal findings Psychology aqa a level spec
Psychology aqa a level spec Aplastic anemia lab findings
Aplastic anemia lab findings Pathophysiology of aplastic anemia
Pathophysiology of aplastic anemia Megaloblastic anemia lab values
Megaloblastic anemia lab values