MetforminAssociated Lactic Acidosis At the edge of Death


- Slides: 57
Metformin-Associated Lactic Acidosis At the edge of Death By Dr Chan Chin Pang Ian Resident Specialist Department of Intensive Care United Christian Hospital
Diabetes Mellitus (DM) z. DM represents substantial impact on diabetic patients and their families z. In 1997, about 10. 3 million American had been diagnosed with diabetes-a sixfold increase over the past 4 decades z. In 1996, about 67000 diabetes-related amputation were performed z. In 1992, $92 billion was spent on diabetes 1. CDC, 1997, 1998
Diabetes Mellitus z. Cardiovascular Risk: IHD, CVA, atherosclerosis, aneurysm z. Renal risk: nephropathy, end-stage renal failure z. Metabolic derangement: hyperglycaemia, DKA, hyperosmolar non-ketotic coma, hyperlipidaemia
Diabetes Mellitus z. Diet control z. Alpha-Glucosidase Inhibitors (Acarbose, Miglitol) z. Sulfonylureas (Glimepiride, Glipizide, Tolbutamide) z. Thiazolidinediones (Rosiglitazone) z. Biguanides (Metformin, Phenformin) z. Insulin
Biguanides Metformin Phenformin Buformin
Metformin-Associated Lactic Acidosis (MALA)
Metformin z Mode of Action Decreases hepatic gluconeogenesis, decreases glucose absorption in the intestines, and increases sensitivity to insulin by increasing peripheral glucose uptake and utilization. z Contraindications Hypersensitivity Renal disease (males with serum creatinine >1. 5 mg/d. L, females with serum creatinine >1. 4 mg/d. L) AMI, CHF exacerbation, surgery, or shock Acute or chronic metabolic acidosis z Hutchison TA, Shahan DR, Anderson ML (eds): DRUGDEX System. MICROMEDEX, Inc, Englewood, Colo. (Edition expires 12/2000) z Hebel SK, Katstrup EK (eds): Drug Facts and Comparisons. St. Louis, Mo. 2001 z For conversion of creatinine expressed in conventional units to SI units, multiply by 88. 4
Metformin-Associated Lactic Acidosis z Incidence: 0. 03 cases/1, 000 patient-years (Phenformin, another biguanide introduced into the market around 1950, 10 to 20 times greater risk of developing lactic acidosis, especially the Whites, probably due to its long side chain, which enhances its lipophilicity and results in a greater affinity for binding to mitochondrial membranes, which could account for its greater ability to inhibit aerobic metabolism than metformin)
Metformin-Associated Lactic Acidosis z Mortality: about 50% of cases z Sign and symptoms: non-specific (nausea, vomiting, altered consciousness, fatigue, abdominal pain, and thirst) 1. Gowardman JR. Fatal metformin induced lactic acidosis: case report. N Z Med J 1995; 108: 230 -11. 2. Gan SC, Barr J, Arieff AI, Pearl RG. Biguanide-associated lactic acidosis. Case report and review of the literature. Arch Intern Med 1992; 152: 2333 -6. 3. Bailey CJ, Turner RC. Metformin. N Engl J Med 1996; 334: 574 -9. 4. Lee AJ. Metformin in noninsulin-dependent diabetes mellitus. Pharmacotherapy 1996; 16: 327 -51.
Grave Prognosis? 19 th century Hospital www. iconsofeurope. com/tb 2005. htm
Metformin-Associated Lactic Acidosis Local Data?
Local Experience on Metformin-Associated Lactic Acidosis (MALA): Retrospective Case Review
Objective of the Review z To review demographic data, dosage of metformin, initial presentation, physiological parameters and clinical outcome of patients suffering from MALA and required ICU care. z Life-threatening events, such as unstable arrhythmia, cardiac arrest and treatment would be recorded. z Expected mortality rates for APACHE II scores would be compared with the observed mortality rates.
Data Collection z. Intensive Care Unit, United Christian Hospital z 1/12/2004 to 1/12/2006 z. Clinical Data and Reporting System (CDARS) z. Clinical Management System (CMS)
Data Collection z. Searching Criteria -1/12/2004 to 1/12/2006 and ICU patient and metformin AND one of the followings -renal failure, acute-on-chronic renal failure, renal impairment -hyperkalaemia -metabolic acidosis -lactic acidosis -CVVH -HD
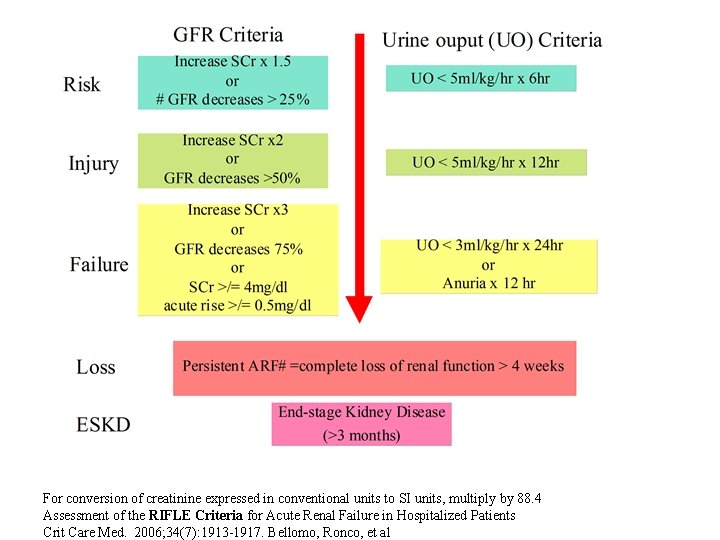
Inclusion Criteria z In-patient between 1/12/2004 and 1/12/2006 z UCH ICU Admission z Age >/=18 z On metformin z Metabolic Acidosis (p. H<7. 35; HCO 3<22 mmol/L) z Raised anion gap (>14 mmo/L) z Serum lactate > 5 mmol/L z Acute or Acute on chronic renal failure
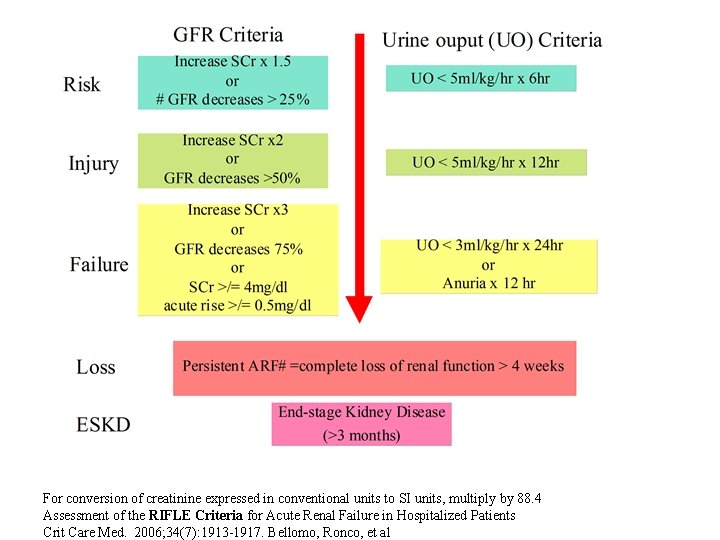
For conversion of creatinine expressed in conventional units to SI units, multiply by 88. 4 Assessment of the RIFLE Criteria for Acute Renal Failure in Hospitalized Patients Crit Care Med. 2006; 34(7): 1913 -1917. Bellomo, Ronco, et al
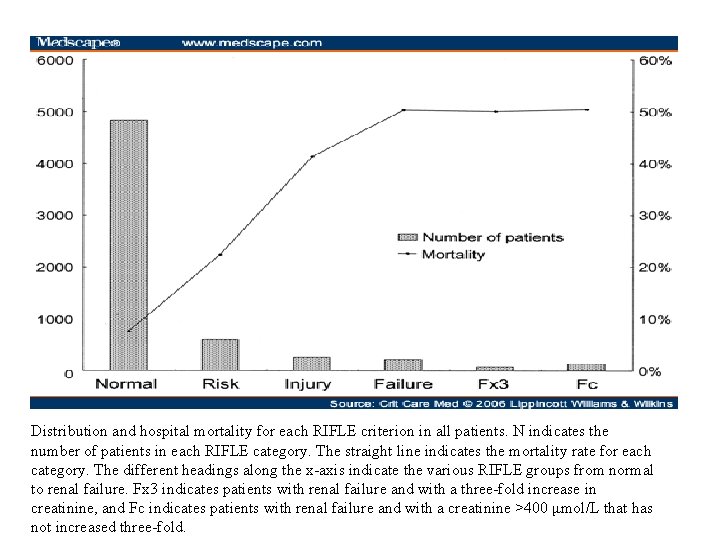
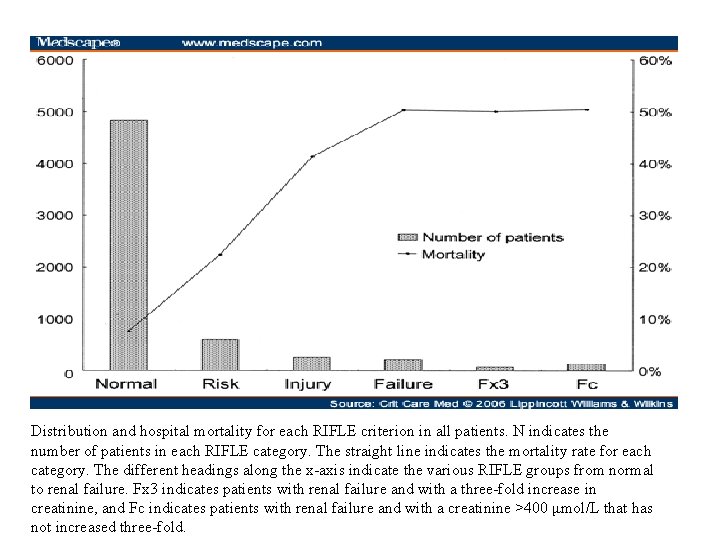
Distribution and hospital mortality for each RIFLE criterion in all patients. N indicates the number of patients in each RIFLE category. The straight line indicates the mortality rate for each category. The different headings along the x-axis indicate the various RIFLE groups from normal to renal failure. Fx 3 indicates patients with renal failure and with a three-fold increase in creatinine, and Fc indicates patients with renal failure and with a creatinine >400 μmol/L that has not increased three-fold.
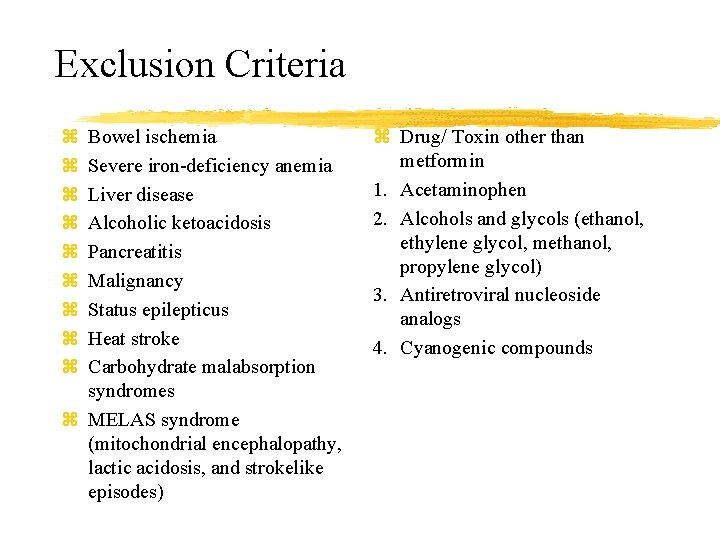
Exclusion Criteria z z z z z Bowel ischemia Severe iron-deficiency anemia Liver disease Alcoholic ketoacidosis Pancreatitis Malignancy Status epilepticus Heat stroke Carbohydrate malabsorption syndromes z MELAS syndrome (mitochondrial encephalopathy, lactic acidosis, and strokelike episodes) z Drug/ Toxin other than metformin 1. Acetaminophen 2. Alcohols and glycols (ethanol, ethylene glycol, methanol, propylene glycol) 3. Antiretroviral nucleoside analogs 4. Cyanogenic compounds
Measurement and Result
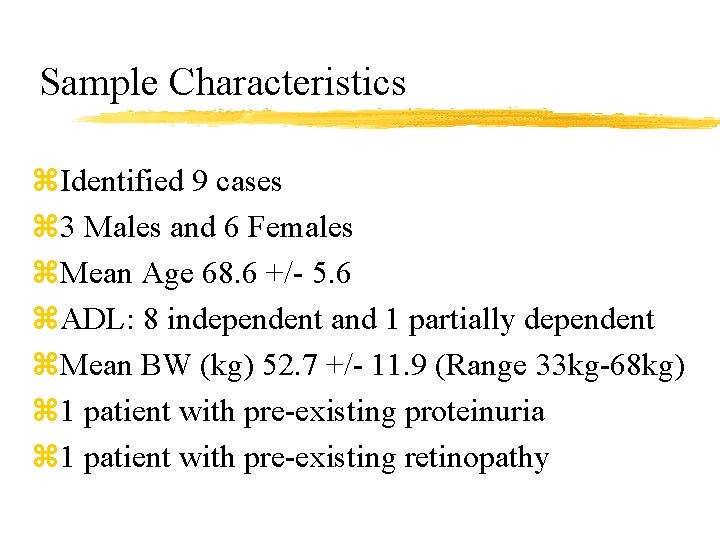
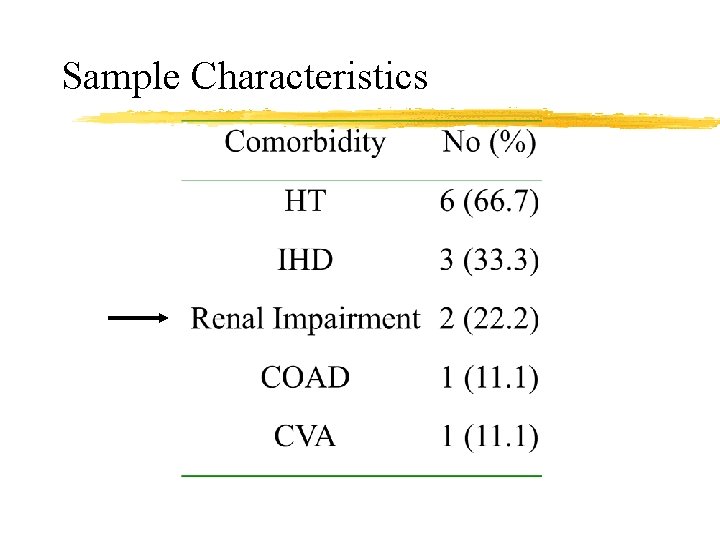
Sample Characteristics z. Identified 9 cases z 3 Males and 6 Females z. Mean Age 68. 6 +/- 5. 6 z. ADL: 8 independent and 1 partially dependent z. Mean BW (kg) 52. 7 +/- 11. 9 (Range 33 kg-68 kg) z 1 patient with pre-existing proteinuria z 1 patient with pre-existing retinopathy
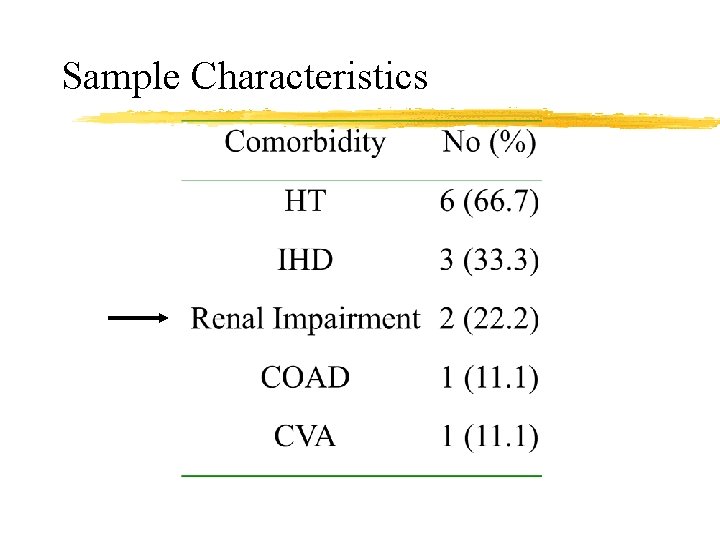
Sample Characteristics
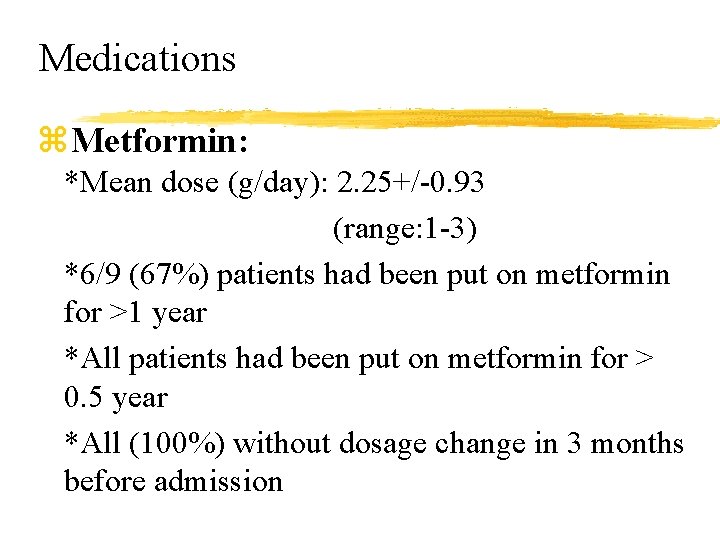
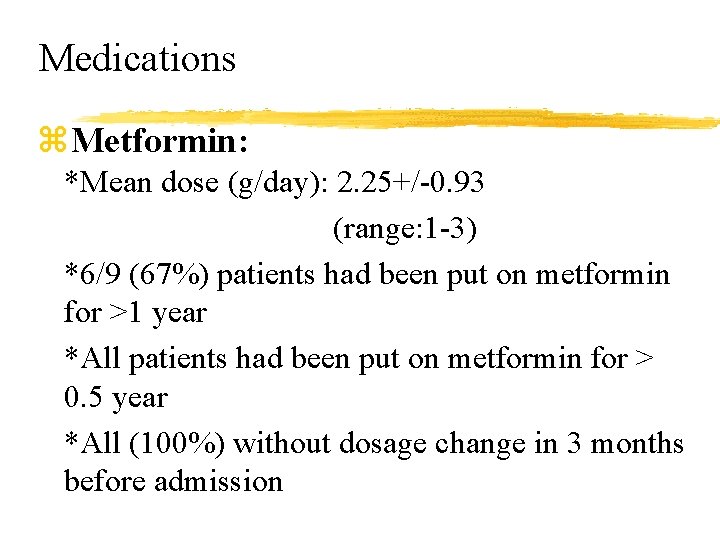
Medications z. Metformin: *Mean dose (g/day): 2. 25+/-0. 93 (range: 1 -3) *6/9 (67%) patients had been put on metformin for >1 year *All patients had been put on metformin for > 0. 5 year *All (100%) without dosage change in 3 months before admission
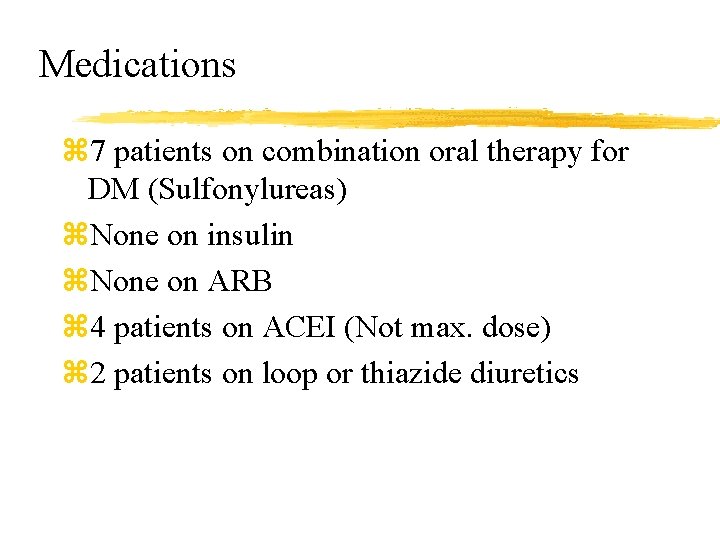
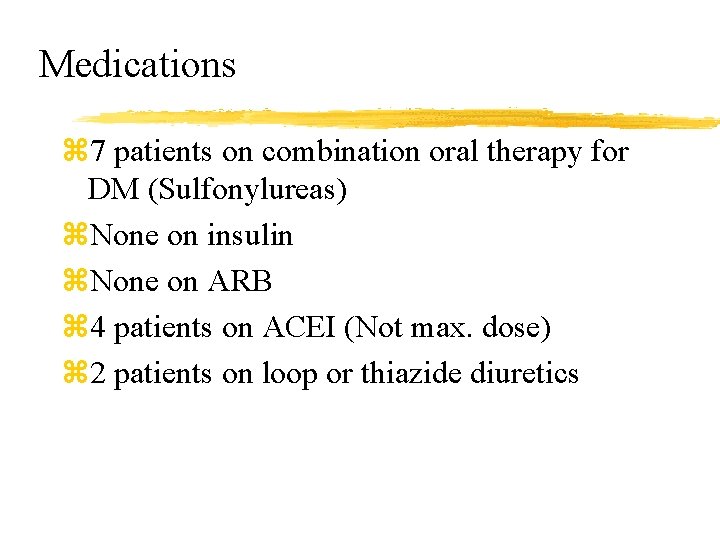
Medications z 7 patients on combination oral therapy for DM (Sulfonylureas) z. None on insulin z. None on ARB z 4 patients on ACEI (Not max. dose) z 2 patients on loop or thiazide diuretics
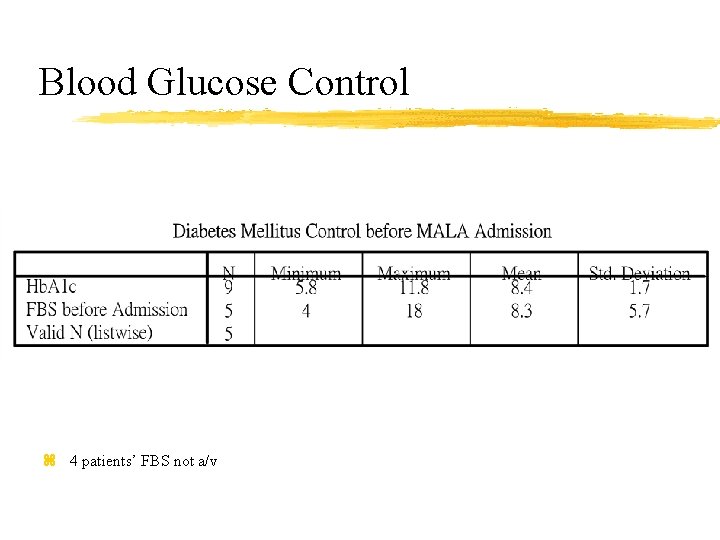
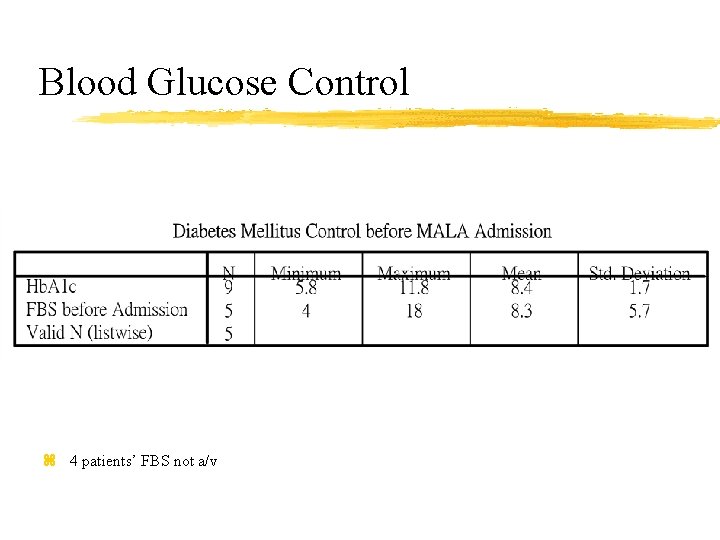
Blood Glucose Control z 4 patients’ FBS not a/v
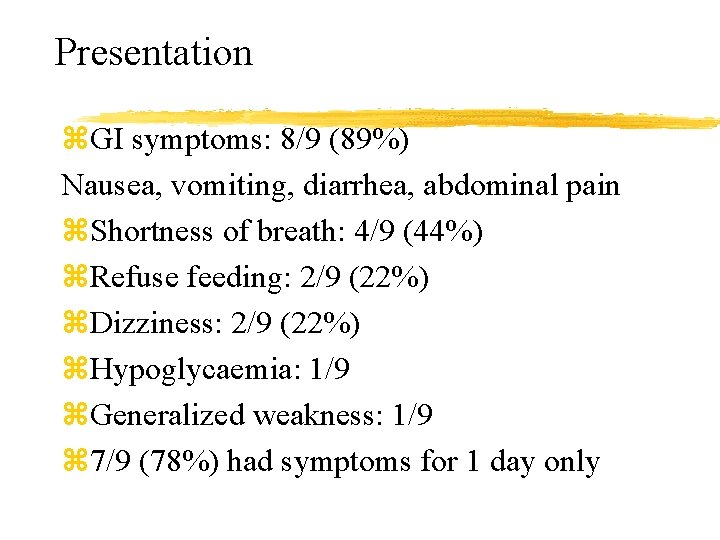
Presentation z. GI symptoms: 8/9 (89%) Nausea, vomiting, diarrhea, abdominal pain z. Shortness of breath: 4/9 (44%) z. Refuse feeding: 2/9 (22%) z. Dizziness: 2/9 (22%) z. Hypoglycaemia: 1/9 z. Generalized weakness: 1/9 z 7/9 (78%) had symptoms for 1 day only
Patient Presentation Non-specific Multiple complaint
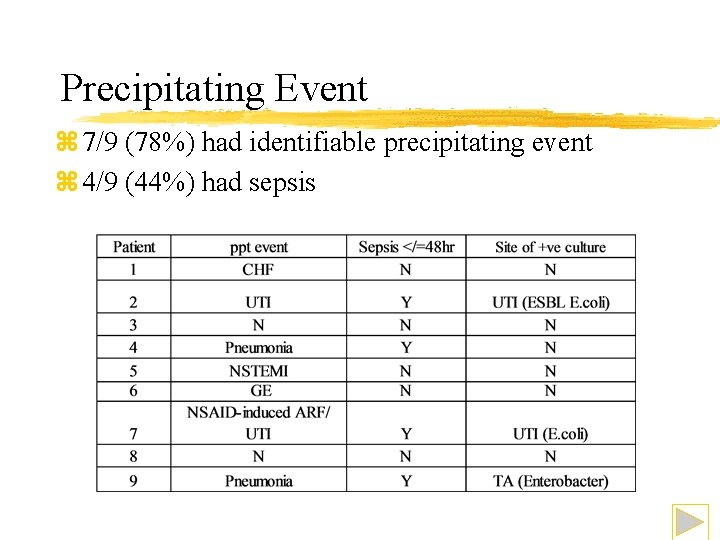
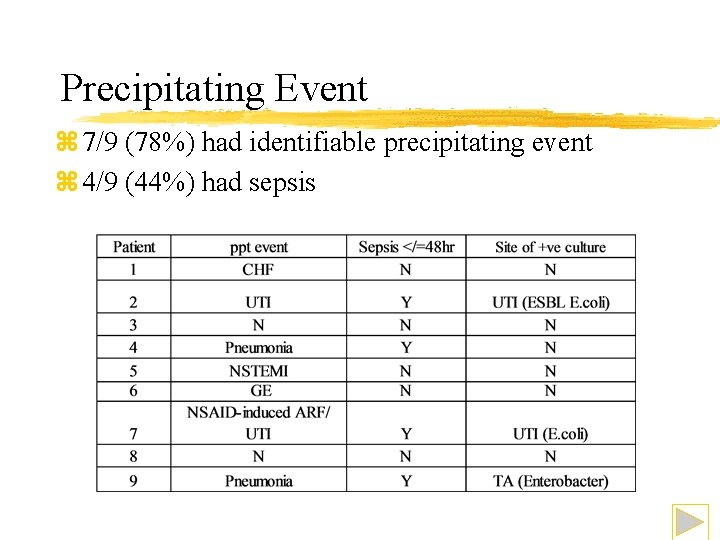
Precipitating Event z 7/9 (78%) had identifiable precipitating event z 4/9 (44%) had sepsis
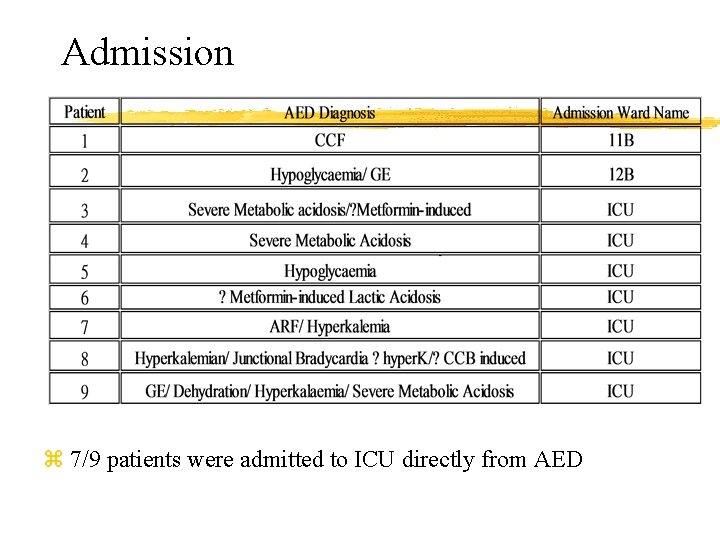
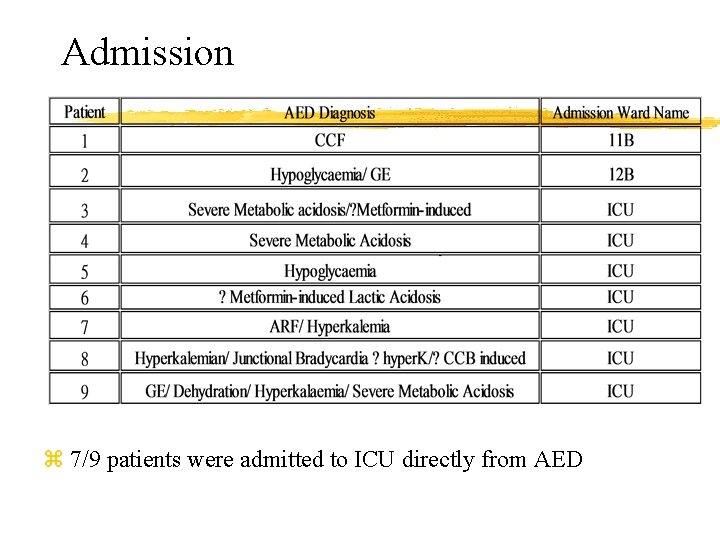
Admission z 7/9 patients were admitted to ICU directly from AED
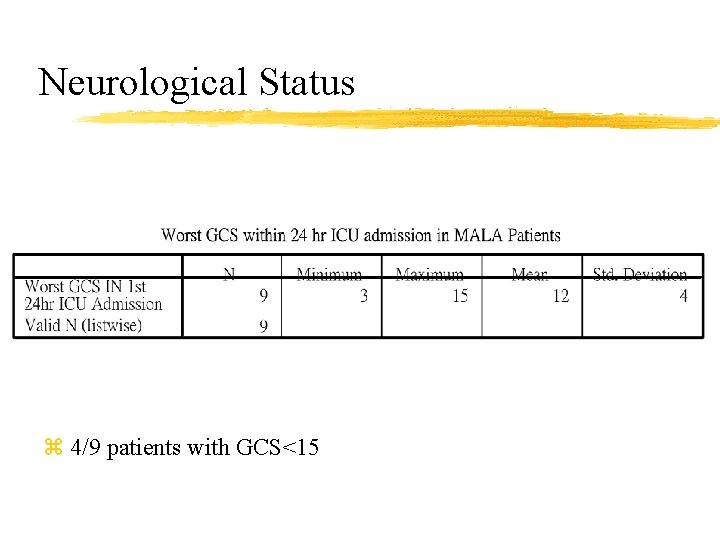
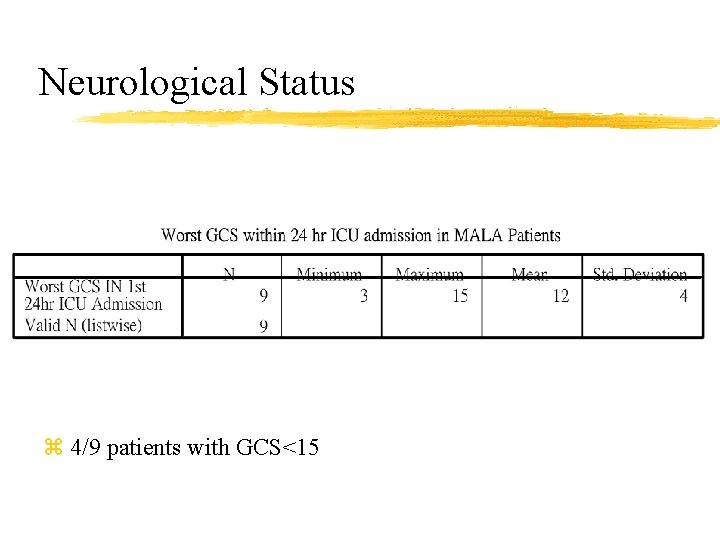
Neurological Status z 4/9 patients with GCS<15
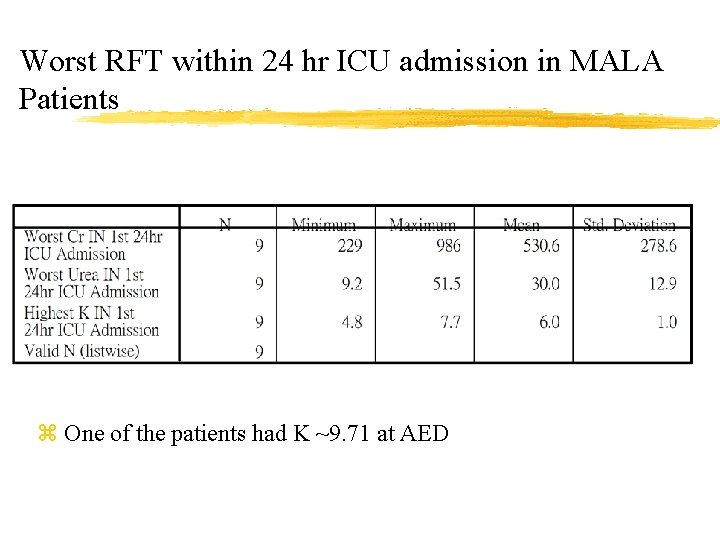
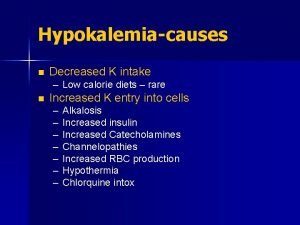
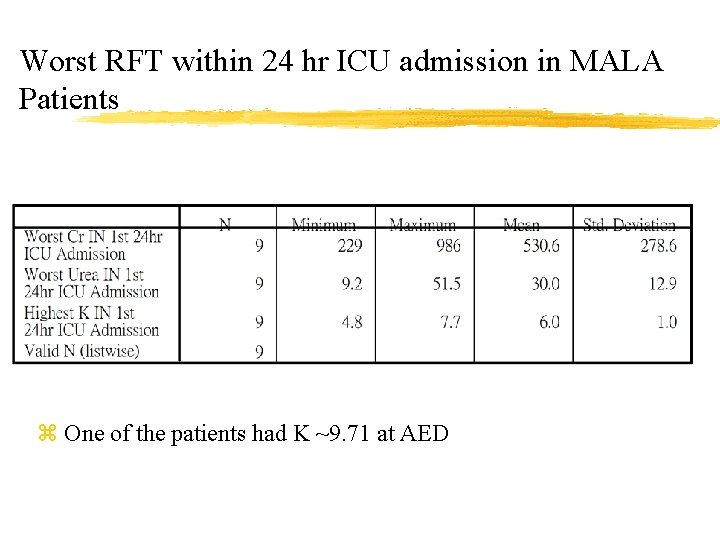
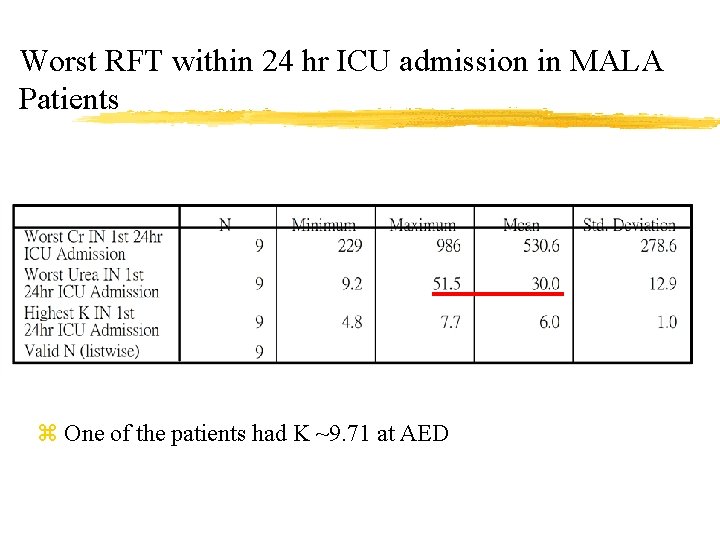
Worst RFT within 24 hr ICU admission in MALA Patients z One of the patients had K ~9. 71 at AED
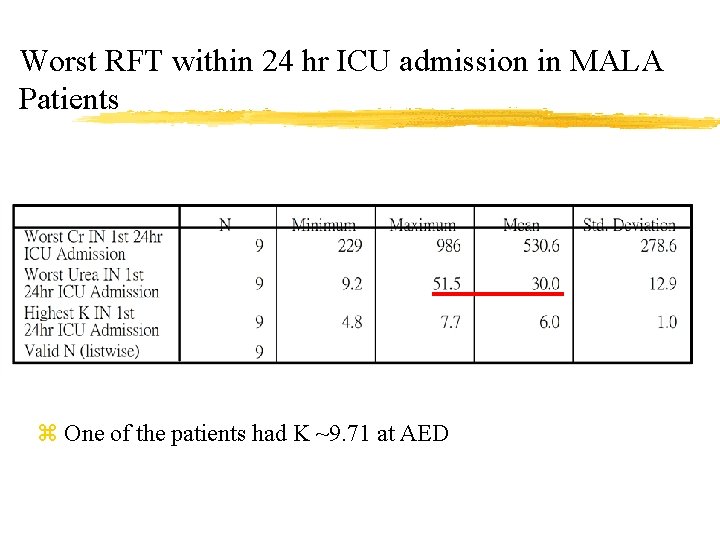
Worst RFT within 24 hr ICU admission in MALA Patients z One of the patients had K ~9. 71 at AED
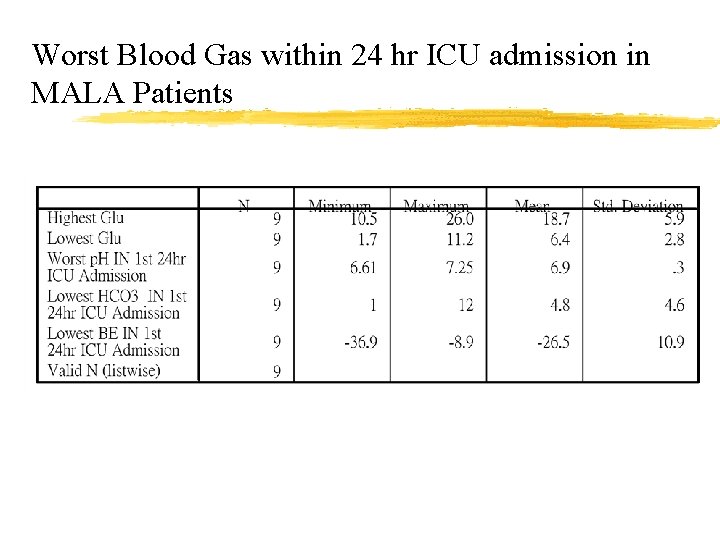
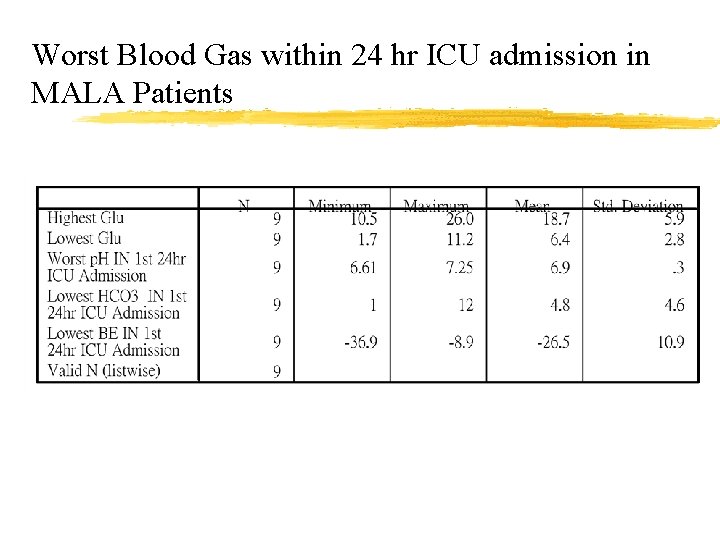
Worst Blood Gas within 24 hr ICU admission in MALA Patients
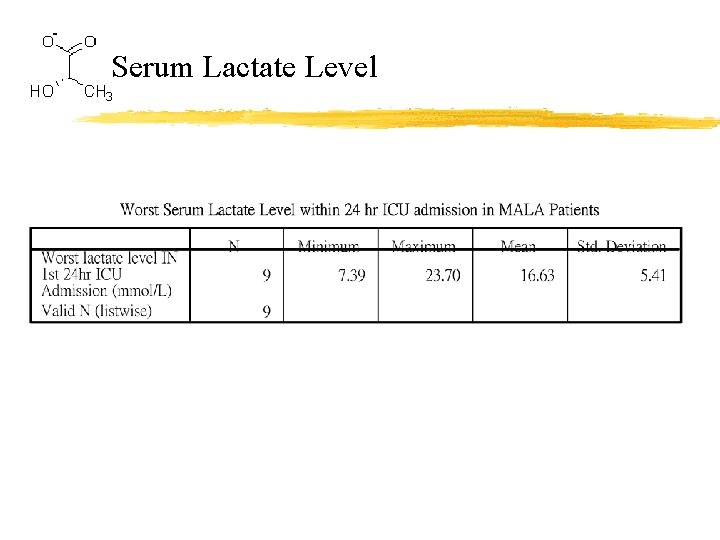
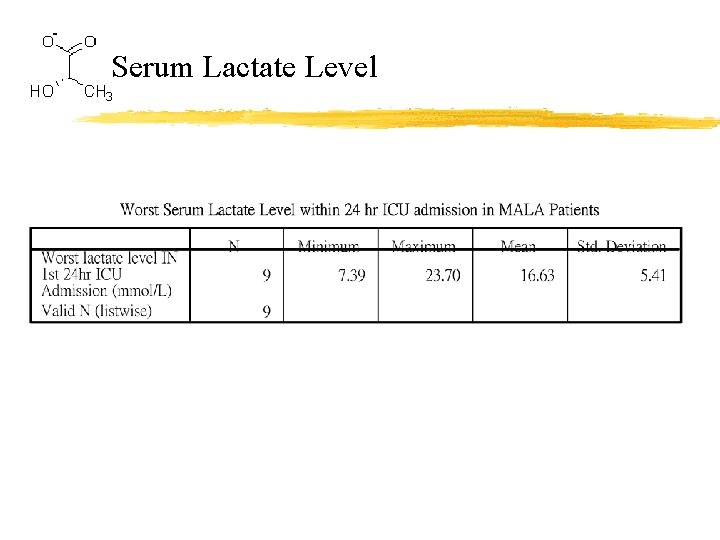
Serum Lactate Level
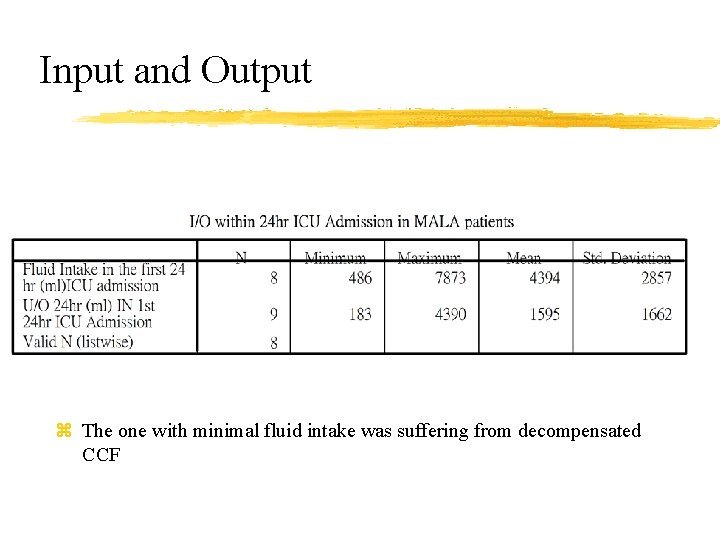
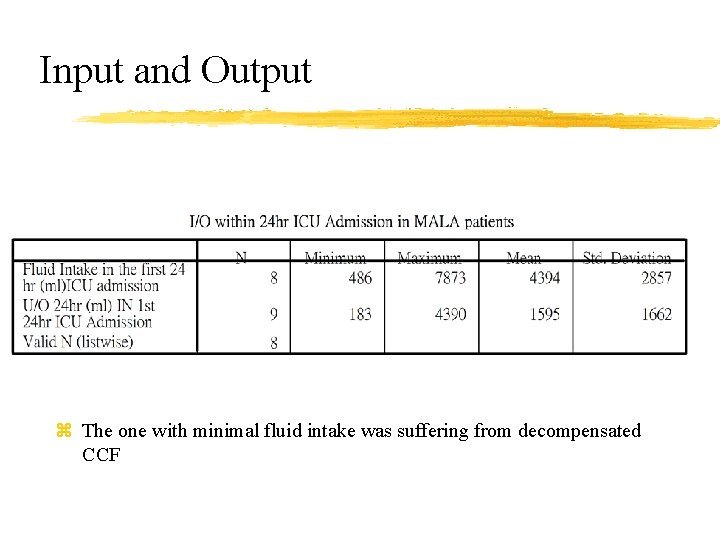
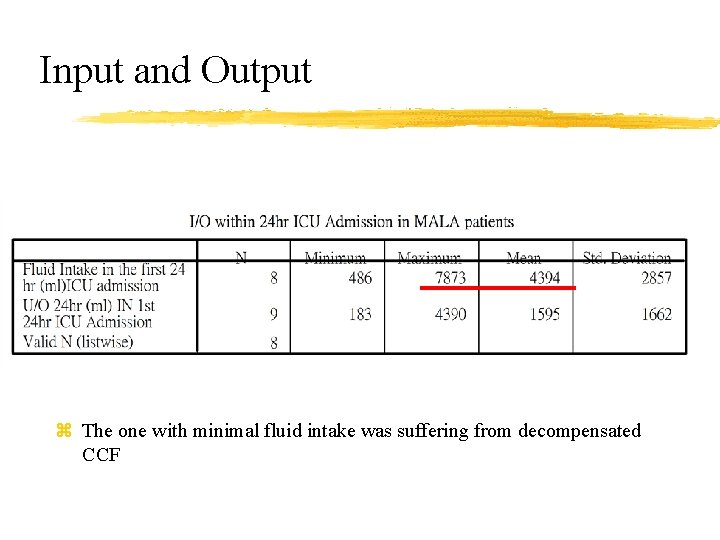
Input and Output z The one with minimal fluid intake was suffering from decompensated CCF
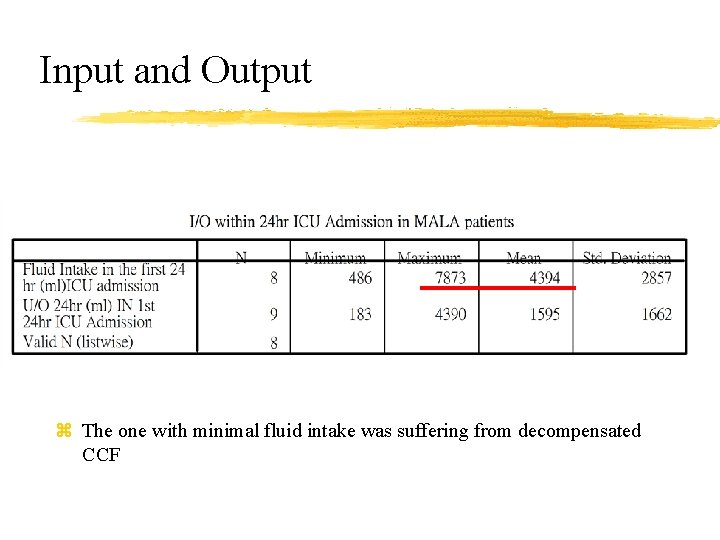
Input and Output z The one with minimal fluid intake was suffering from decompensated CCF
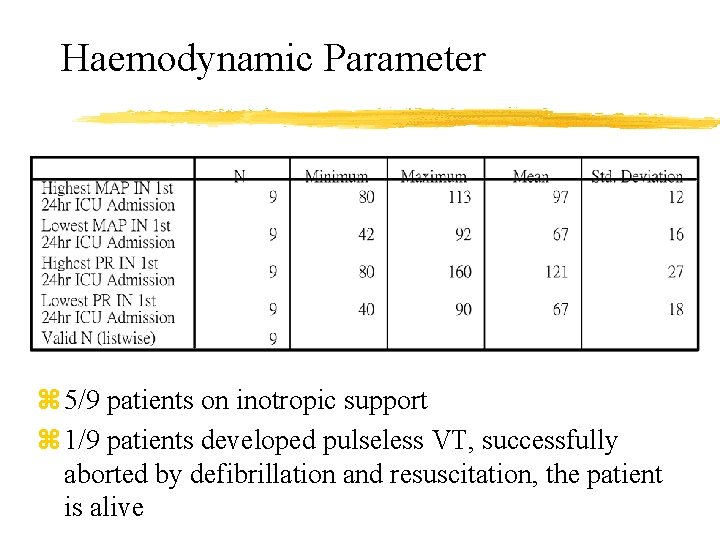
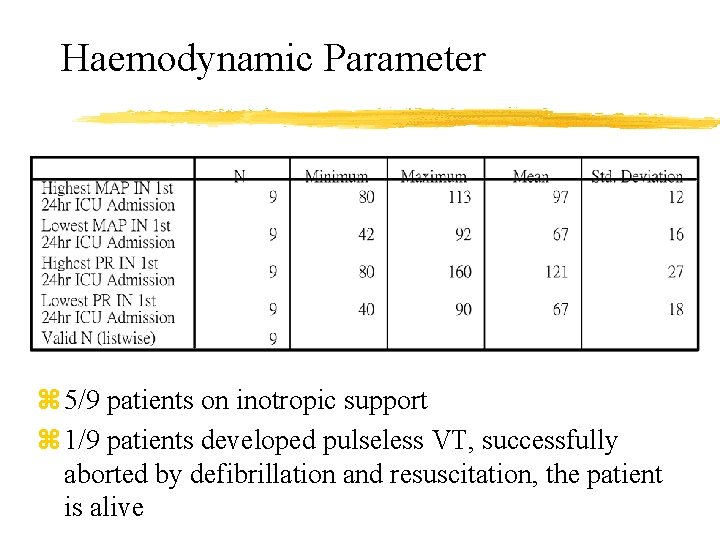
Haemodynamic Parameter z 5/9 patients on inotropic support z 1/9 patients developed pulseless VT, successfully aborted by defibrillation and resuscitation, the patient is alive

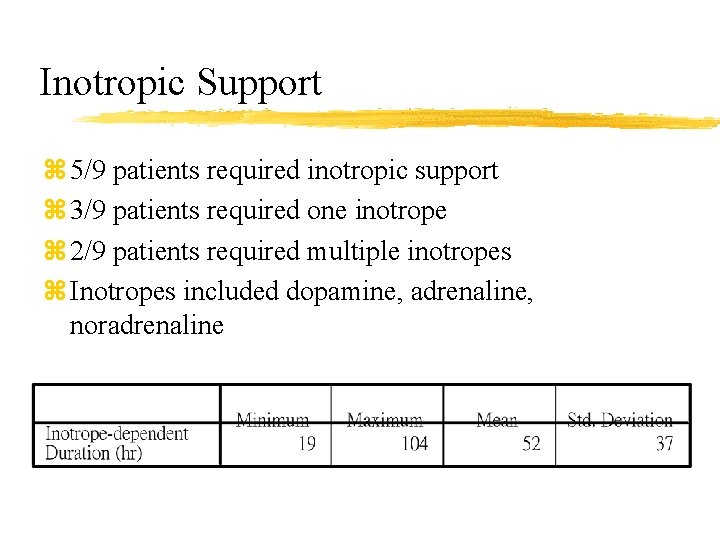
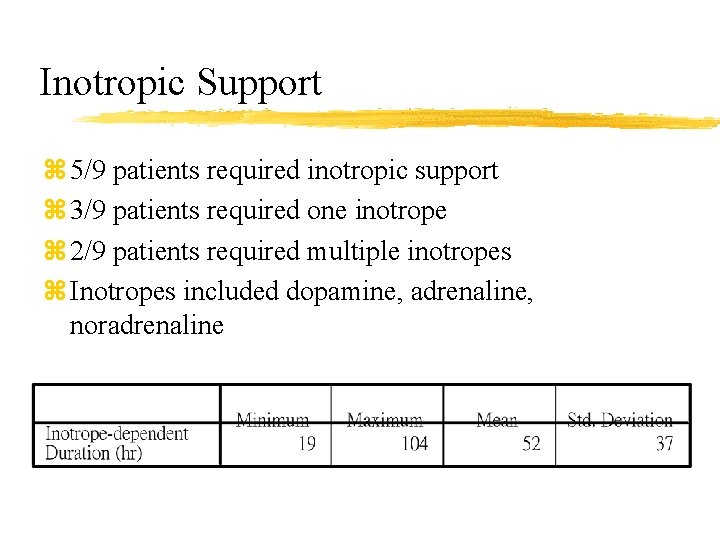
Inotropic Support z 5/9 patients required inotropic support z 3/9 patients required one inotrope z 2/9 patients required multiple inotropes z Inotropes included dopamine, adrenaline, noradrenaline
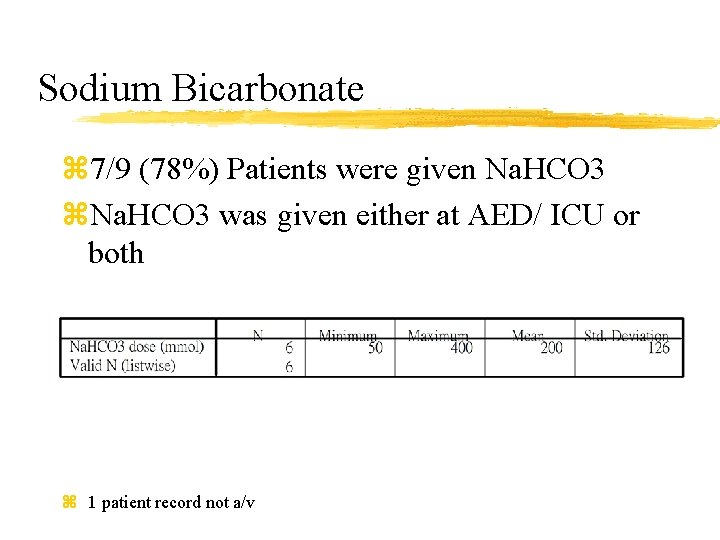
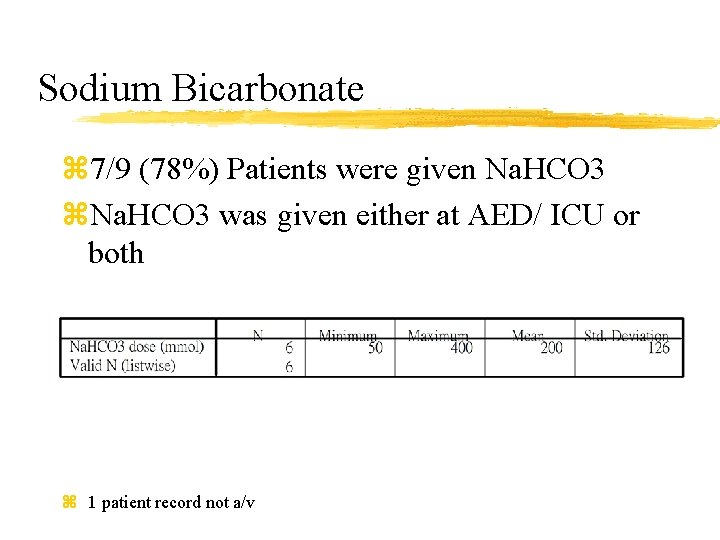
Sodium Bicarbonate z 7/9 (78%) Patients were given Na. HCO 3 z. Na. HCO 3 was given either at AED/ ICU or both z 1 patient record not a/v
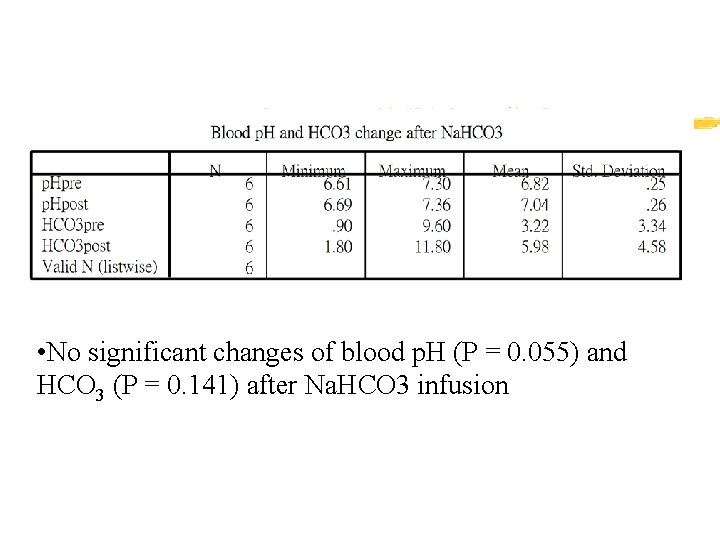
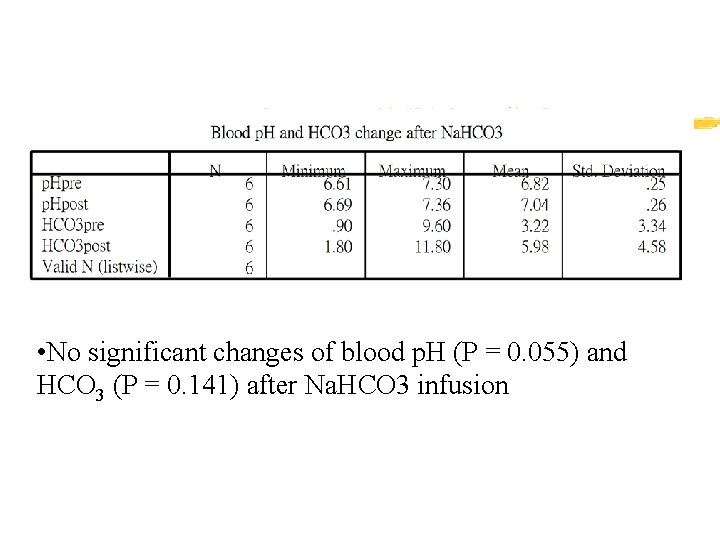
• No significant changes of blood p. H (P = 0. 055) and HCO 3 (P = 0. 141) after Na. HCO 3 infusion
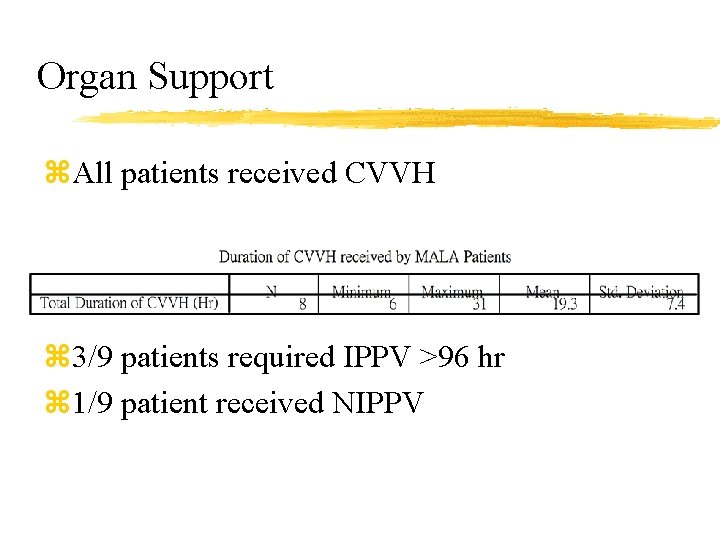
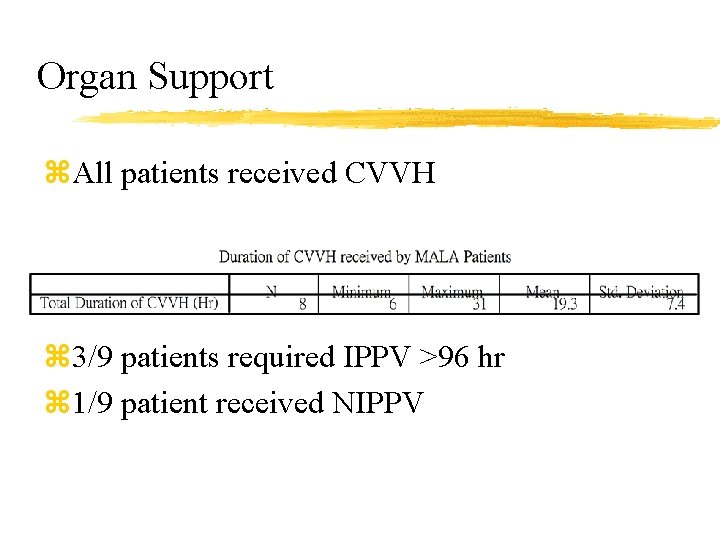
Organ Support z. All patients received CVVH z 3/9 patients required IPPV >96 hr z 1/9 patient received NIPPV
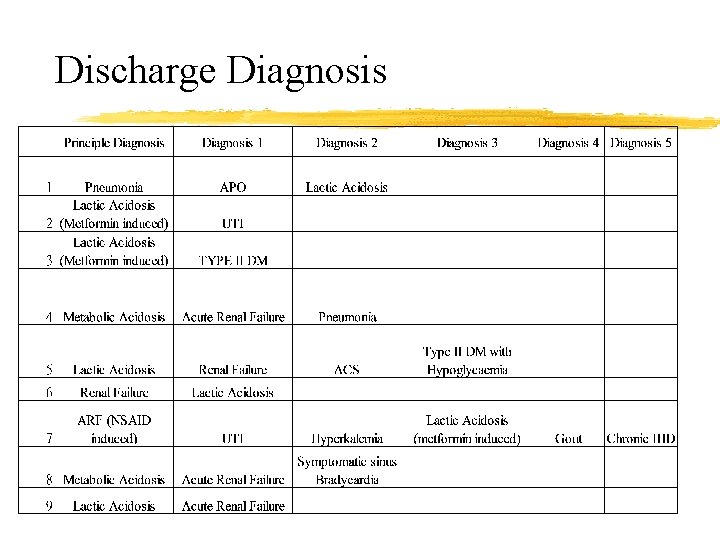
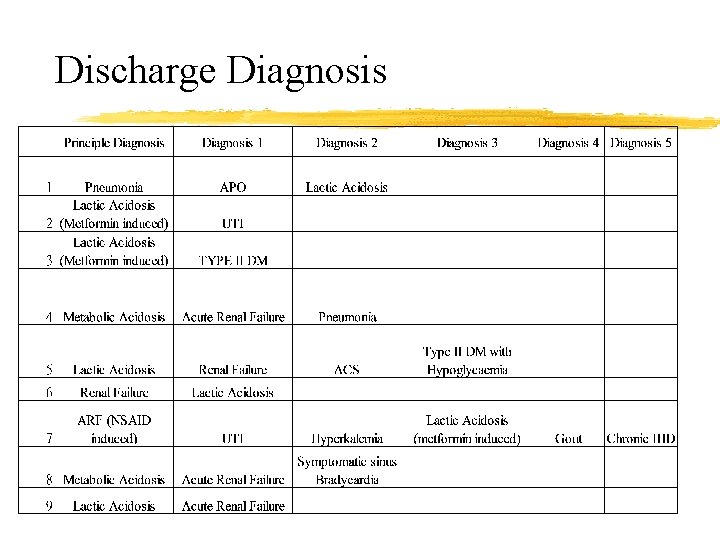
Discharge Diagnosis
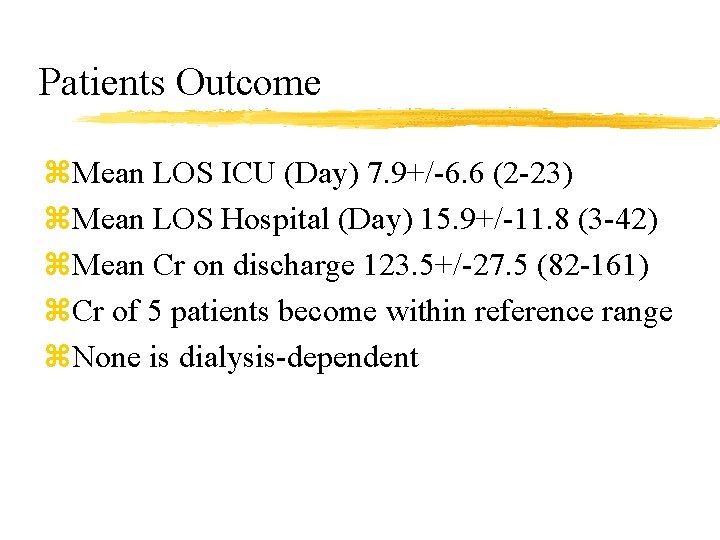
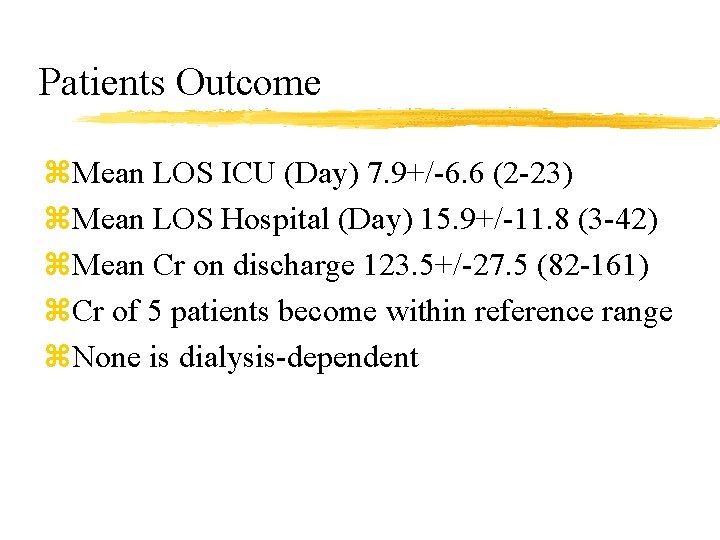
Patients Outcome z. Mean LOS ICU (Day) 7. 9+/-6. 6 (2 -23) z. Mean LOS Hospital (Day) 15. 9+/-11. 8 (3 -42) z. Mean Cr on discharge 123. 5+/-27. 5 (82 -161) z. Cr of 5 patients become within reference range z. None is dialysis-dependent
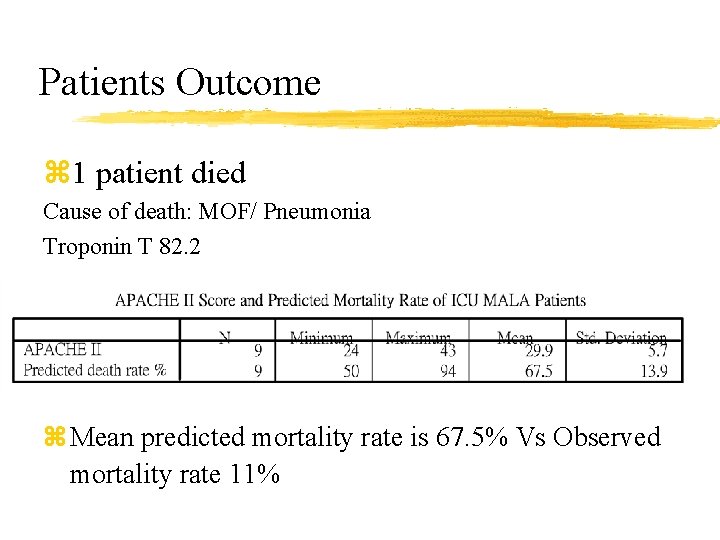
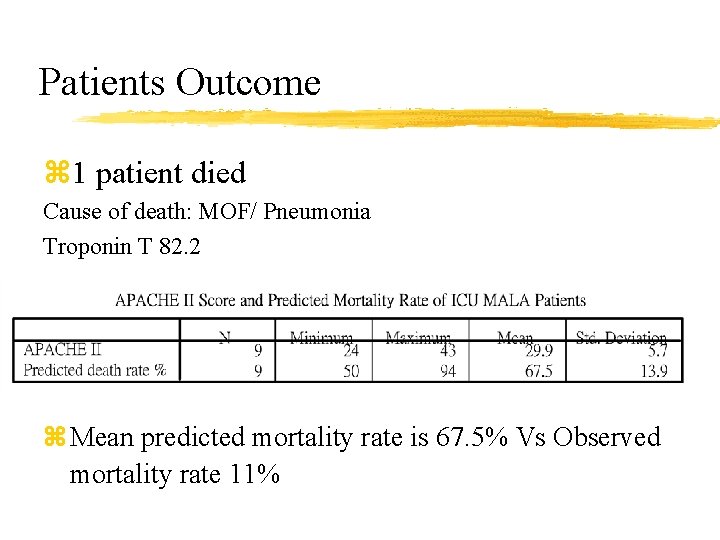
Patients Outcome z 1 patient died Cause of death: MOF/ Pneumonia Troponin T 82. 2 z Mean predicted mortality rate is 67. 5% Vs Observed mortality rate 11%
MALA Discussion
Discussion z. Elderly with age more than 65 years old z. Female seems commoner z. Premorbid renal function is usually normal z. Polypharmacy z. Metformin daily dose not less than 1 g z. Recent initiation or change of dose of metformin may not be essential for the development of MALA
Discussion z. MALA presentations are usually non-specific and subtle. GI symptoms and respiratory compensatory response to severe metabolic acidosis seem dominant z. The onset of symptom is often abrupt (e. g. 1 -2 days)
Discussion z. Usually, precipitating causes can be identified z. Sepsis is not uncommon in MALA z. Patients with MALA are usually very ill with high APACHE II score, elevated Cr and blood lactate level and require organ support, such as IPPV, CRRT, inotropes z. Patients with MALA can deteriorate suddenly if decompensation or unstable arrhythmia develop
Discussion z. The role of Na. HCO 3 infusion is still controversial, needs to balance between potential benefit and risk z. It may be considered in severe metabolic acidosis while waiting for CRRT z. No significant changes of blood p. H and HCO 3 after Na. HCO 3 infusion was demonstrated in this review 1. Horacio J. Adrogue, M. D. , and Nicolaos E. Madias, M. D. Management of Life-Threatening Acid–Base Disorders— First of Two Parts. N Eng J Med Volume 338: 26 -34 January 1, 1998 Number 1
Discussion z. Though the predicted mortality and historical mortality is high, local data shows promising prognosis z. Majority renal function returns within normal range z. All patients in our series (except the one died) do not require long-term renal dialysis
Limitations z The relative small sample size, its heterogeneity and the fact that it represented patients from a local single center limit the present review study. z One drawback of using APACHE II score to predict the expected mortality rate is that it utilized retrospective past data and were not designed to determine individual patient’s mortality. In addition, the adequacy of APACHE II scoring system in patients with acute renal failure is questionable.
Summary z. Patients suffered from MALA usually presented with non- specific complaint z. MALA often had precipitating event z. Sepsis should not be overlooked z. The trend of patients’ outcomes seem better than the outcome predicted by severity score z. Management includes cessation of offending drug, fluid resuscitation, identify and treat the precipitating event, organ support when necessary z. Role of Na. HCO 3 is still debatable
Discussion Question

z. Patient-years Definition Case per 1000 patient years= (number of cases/(sum of all time spent on the patients at risk))*1000
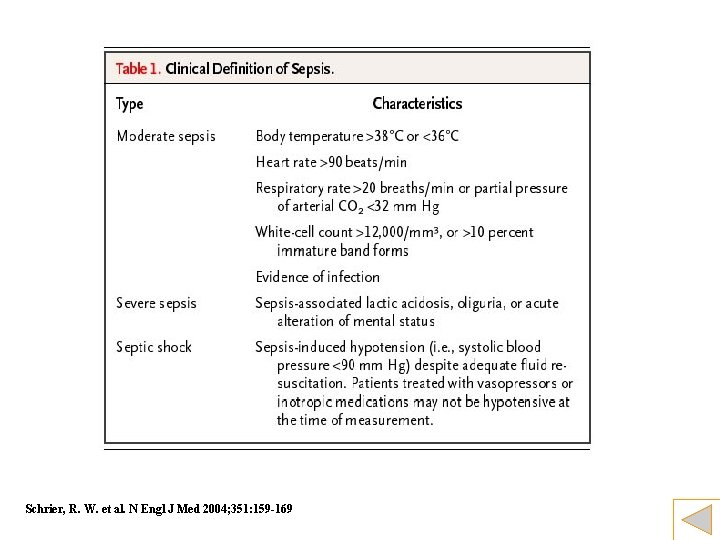
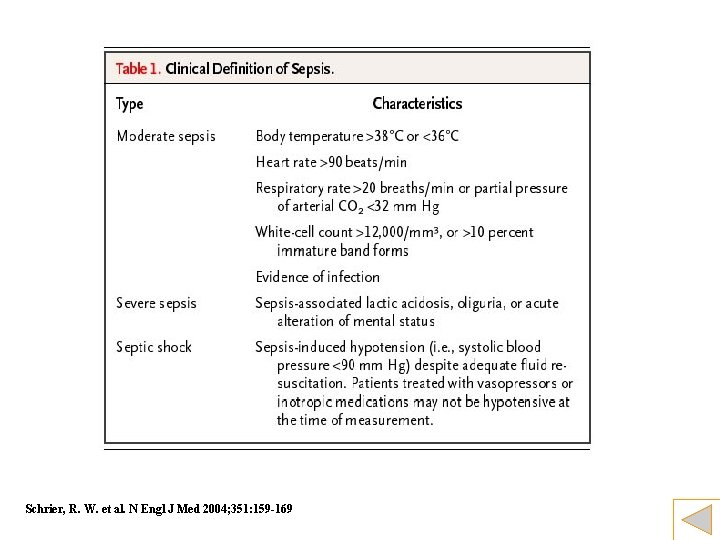
Schrier, R. W. et al. N Engl J Med 2004; 351: 159 -169
 Metformin lactic acidosis symptoms
Metformin lactic acidosis symptoms Metformin lactic acidosis symptoms
Metformin lactic acidosis symptoms Lactate bicarbonate
Lactate bicarbonate Acidosis metabolica y acidosis respiratoria
Acidosis metabolica y acidosis respiratoria Rising edge and falling edge
Rising edge and falling edge Lactic acid fermentation
Lactic acid fermentation Organism
Organism Formula for lactic acid fermentation
Formula for lactic acid fermentation Advantages and disadvantages of atp-pc system
Advantages and disadvantages of atp-pc system Lactic acid
Lactic acid Lactic acid and oxygen
Lactic acid and oxygen Blood flow
Blood flow Blood flow
Blood flow Lactic acid
Lactic acid Empirical formula of lactic acid
Empirical formula of lactic acid Objectives of fermentation
Objectives of fermentation Fermentation process
Fermentation process Acid lactic structura
Acid lactic structura Forensic pathologist definition
Forensic pathologist definition Mudpiles
Mudpiles Alcalosis mixta
Alcalosis mixta Normal electrolytes values
Normal electrolytes values Metabolic acidosis definition
Metabolic acidosis definition Acidosis ph
Acidosis ph Fluid and electrolyte balance ppt
Fluid and electrolyte balance ppt Metabolic acidosis dog treatment
Metabolic acidosis dog treatment Mudpiles anion gap
Mudpiles anion gap Difference between compensated and uncompensated
Difference between compensated and uncompensated Arritmias ventriculares
Arritmias ventriculares Acidosis respiratoria pediatria
Acidosis respiratoria pediatria High ag metabolic acidosis
High ag metabolic acidosis Correccion anion gap albumina
Correccion anion gap albumina Criterios de resolucion de cetoacidosis
Criterios de resolucion de cetoacidosis Acidosis
Acidosis Causas de acidosis respiratoria
Causas de acidosis respiratoria Pseudohipokalemia
Pseudohipokalemia Peripheral chemoreceptor
Peripheral chemoreceptor Metabolic acidosis abg
Metabolic acidosis abg Component of abg
Component of abg Alcoholic ketoacidosis
Alcoholic ketoacidosis Mudpiles anion gap
Mudpiles anion gap Halo oxigenoterapia
Halo oxigenoterapia Normal abg values
Normal abg values Hypochloremic hypokalemic metabolic alkalosis
Hypochloremic hypokalemic metabolic alkalosis Abg correction formula
Abg correction formula Causas de acidosis lactica
Causas de acidosis lactica Insuficiencia respiratoria
Insuficiencia respiratoria What is a homeostatic process
What is a homeostatic process Metabolic acidosis
Metabolic acidosis Causas de alcalosis metabolica
Causas de alcalosis metabolica Paul l marino
Paul l marino Mudpiles acidosis
Mudpiles acidosis Respiratory acidosis
Respiratory acidosis Anion gap formula
Anion gap formula Acid base metabolic acidosis
Acid base metabolic acidosis Why hyperkalemia in acidosis
Why hyperkalemia in acidosis Delta delta gap
Delta delta gap Mudpiles
Mudpiles