MEDICATION AND INTRAVENOUS CALCULATIONS PYRAMID POINTS Always use
- Slides: 87
MEDICATION AND INTRAVENOUS CALCULATIONS
PYRAMID POINTS • Always use the appropriate formula to calculate the problem • Short cuts should not be used when calculating medication problems • Label the problem and the answer with the correct measurement
PYRAMID POINTS • Place the decimal point in the correct places or the answer will be incorrect • Seek assistance if unsure of the accuracy in calculating • Check the accuracy of the calculation • Be sure that the answer is within reason and makes sense
MEDICATION ADMINISTRATION GUIDELINES • Assess medication order • Ask the client about a history of allergies • Assess client's current condition and the purpose for the medication or intravenous solution • Determine the client's understanding of the purpose of the prescribed medication or need for IV solution
MEDICATION ADMINISTRATION GUIDELINES • Teach the client about the medication and about self-administration at home • Identify and address concerns (social, cultural, religious) that the client may have about taking the medication • Assess the need for conversion when preparing a dose of medication for administration to the client
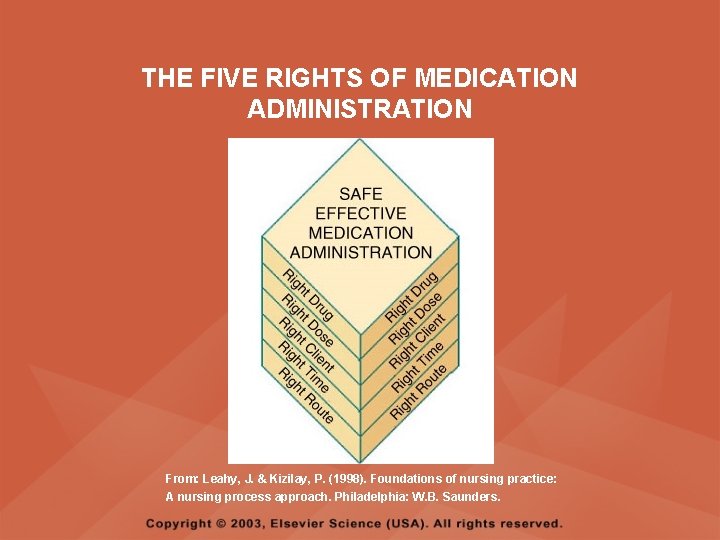
MEDICATION ADMINISTRATION GUIDELINES • ASSESS THE FIVE RIGHTS – Right medication – Right dose – Right client – Right time – Right route
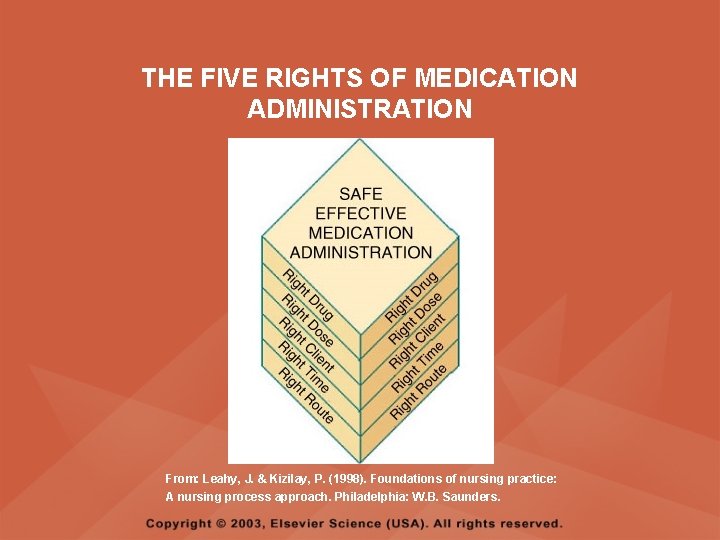
THE FIVE RIGHTS OF MEDICATION ADMINISTRATION From: Leahy, J. & Kizilay, P. (1998). Foundations of nursing practice: A nursing process approach. Philadelphia: W. B. Saunders.
MEDICATION ADMINISTRATION GUIDELINES • Assess vital signs prior to administering medication • Document the administration of the prescribed therapy and client's response to therapy
DRUG MEASUREMENT SYSTEMS • METRIC SYSTEM – The basic units of metric measures are meter, liter, and gram – Meter measures length – Liter measures volume – Gram measures weight
DRUG MEASUREMENT SYSTEMS • APOTHECARY SYSTEM – The four apothecary measures sometimes used are the grain, minim, dram, and ounce – Grain measures weight – Minim, dram, and ounce measures volume
DRUG MEASUREMENT SYSTEMS • HOUSEHOLD SYSTEM – The three household measures commonly used are tablespoon, teaspoon, and drop
DRUG MEASUREMENT SYSTEMS • MILLIEQUIVALENT – Abbreviated m. Eq – Is an expression of the number of grams of a medication contained in 1 ml of a normal solution – Example: potassium chloride
DRUG MEASUREMENT SYSTEMS • UNIT – Abbreviated as U or u; measures a medication in terms of its action, not its physical weight – Examples: penicillin, heparin sodium, insulin
CONVERSION BETWEEN METRIC UNITS • The metric system is a decimal system; therefore, conversions between the units in this system can be done by either dividing or multiplying by 1000 or by moving the decimal point three places to the right or three places to the left • To convert larger to smaller multiply by 1000 or move the decimal 3 places to the right • To convert smaller to larger divide by 1000 or move the decimal 3 places to the left
CONVERSION BETWEEN METRIC UNITS • PROBLEM – Convert 2 grams to milligrams • SOLUTION – Change a larger unit to a smaller unit – Move the decimal 3 places to right – 2. 000 grams = 2000 mg
CONVERSION BETWEEN METRIC UNITS • PROBLEM – Convert 250 ml to liters • SOLUTION – Change a smaller unit to a larger unit – Move the decimal 3 places to left – 250 ml = 0. 250 L or 0. 25 L
CONVERSION BETWEEN METRIC, APOTHECARY, AND HOUSEHOLD SYSTEMS • Conversions between the metric, apothecary, and household systems are equivalent, not equal, measures • Conversion to equivalent measures between systems is necessary when a medication order is written in one system but the medication label is stated in another • Medications are not always ordered and prepared in the same system of measurement; it is therefore necessary to convert units from one system to another
CONVERSION AMONG METRIC, APOTHECARY, AND HOUSEHOLD SYSTEMS • Conversion is the first step in the calculation of dosages • Calculating equivalents between two systems may be done using the method of ratio and proportion
RATIO AND PROPORTION • PROBLEM – The physician orders nitroglycerin, gr 1/150. The medication label reads 0. 4 mg per tablet. The nurse prepares to administer how many tablets to the client? • SOLUTION – gr 1 : 60 mg = gr 1/150 : x mg – 60 mg x gr 1/150 = x – X = 0. 4 mg (1 tablet)
CELSIUS AND FAHRENHEIT TEMPERATURE • FAHRENHEIT TO CELSIUS – To convert Fahrenheit to Celsius, subtract 32 and divide result by 1. 8 • FORMULA – C = ( F – 32 ) / 1. 8
CELSIUS AND FAHRENHEIT TEMPERATURE • CELSIUS TO FAHRENHEIT – To convert Celsius to Fahrenheit, multiply by 1. 8 and add 32 • FORMULA – F = 1. 8 C + 32
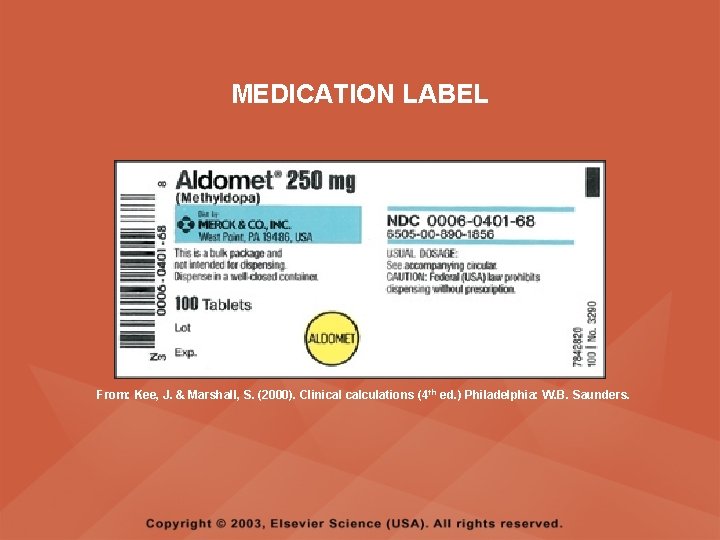
MEDICATION LABELS • A medication label will contain both the generic and trade name of the medication • The trade name, also called brand name, is printed on the label in capital letters or with the first letter capitalized • The generic name is the chemical name of a medication; the generic name may not be capitalized and is usually located below the trade name on a medication label
MEDICATION LABELS • Each medication has only one official name but may have several trade names, each for the exclusive use of the company that manufactures the medication • Always check expiration dates on medication labels
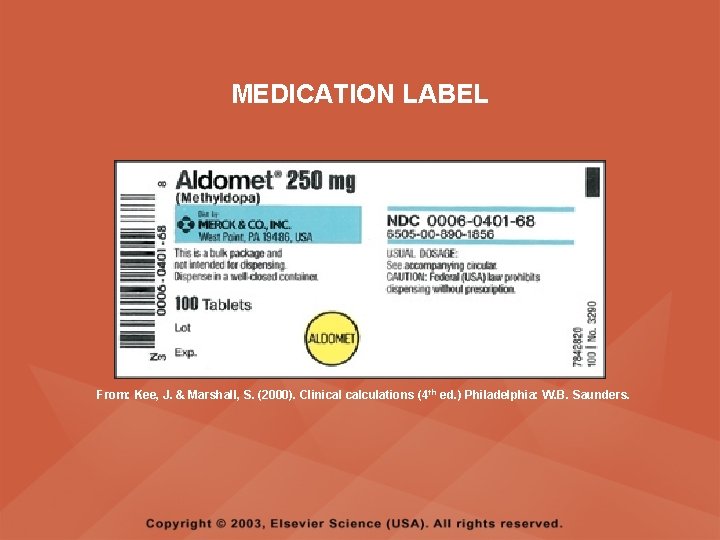
MEDICATION LABEL From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
MEDICATION ORDERS • In a medication order, the name of the medication is written first, followed by the dosage, route, and frequency • If there any questions or inconsistencies with the written order, the person who wrote the order must be contacted immediately, and the order must be verified
MEDICATION ORDERS • COMPONENTS – Name of client – Date and time when order is written – Name of medication to be given – Dosage of medication – Medication route – Time and frequency of administration – Signature of person writing the order
ORAL MEDICATIONS • Scored tablets contain an indented mark to make possible breakage for partial dosages; when necessary, scored tablets (those marked for division) can be divided in halves or quarters • Enteric-coated tablets and sustained-released capsules delay absorption until the medication reaches the small intestine; these medications should not be crushed
ORAL MEDICATIONS • Capsules contain a powered or oily medication in a gelatin cover • Oral liquids are supplied in solution form and contain a specific amount of medication in a given amount of solution, as stated on the label • Volumes of less than 5 ml are measured using a syringe with the needle removed • A calibrated dropper is used when giving medicine to children and when adding small amounts of liquid to water or juice; calibrations are in milliliters, cubic centimeters, drops, or minims
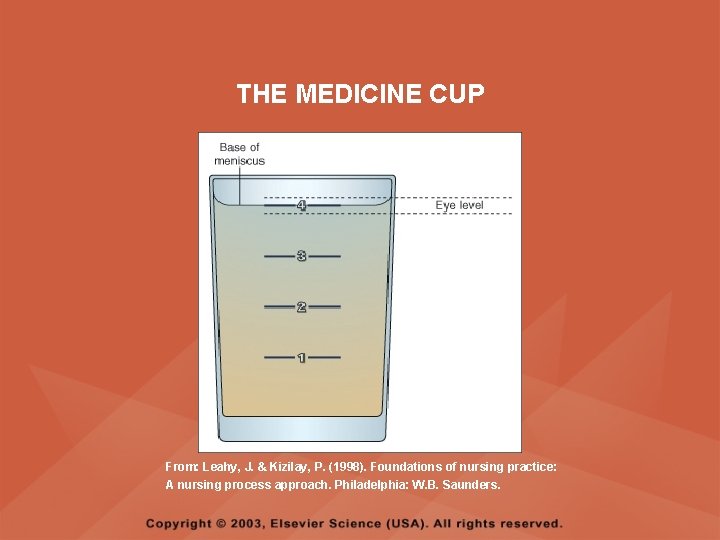
ORAL MEDICATIONS • THE MEDICINE CUP – Has a capacity of 30 ml or 1 ounce – Is used for oral liquids – Is calibrated to measure teaspoons, tablespoons, and drams – To pour accurately, hold the medication cup at eye level, then line up the measure that is needed and pour
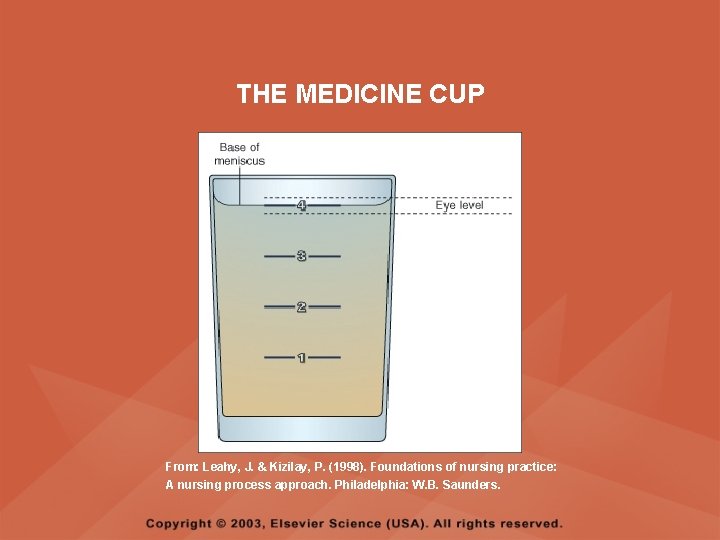
THE MEDICINE CUP From: Leahy, J. & Kizilay, P. (1998). Foundations of nursing practice: A nursing process approach. Philadelphia: W. B. Saunders.
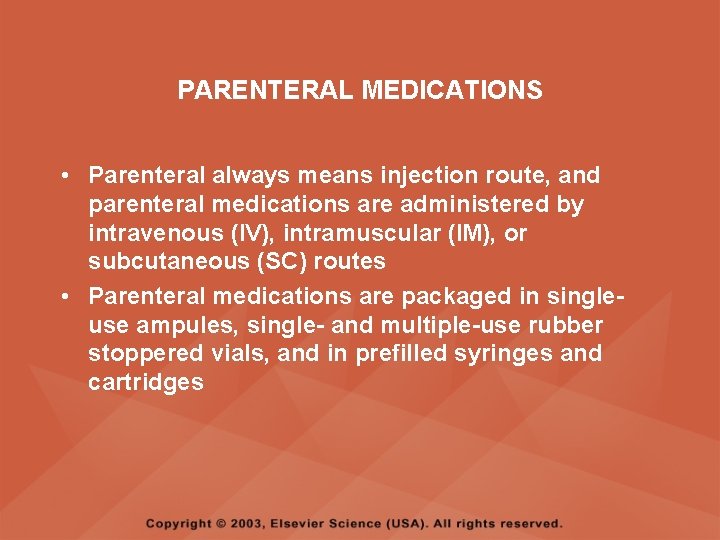
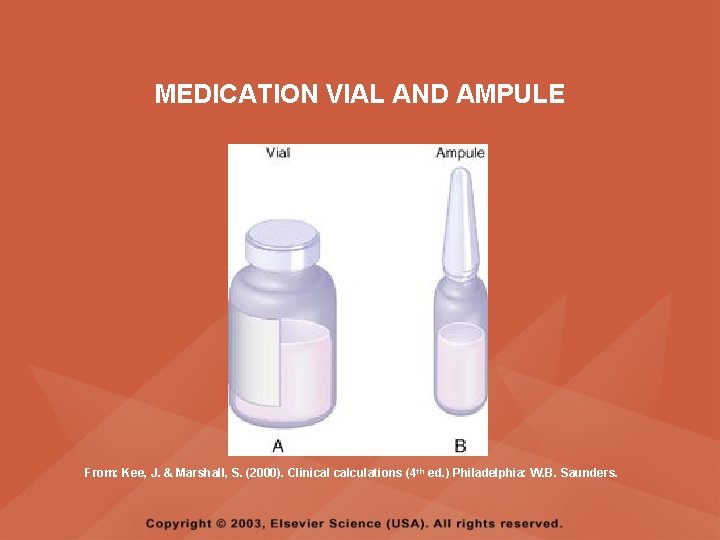
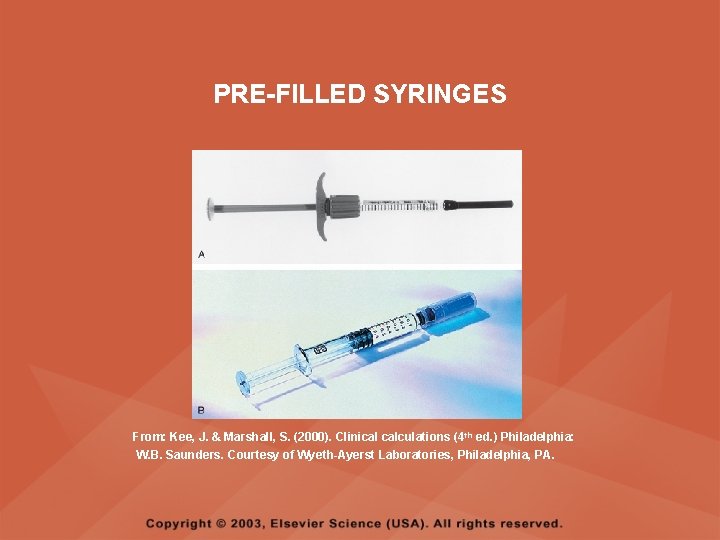
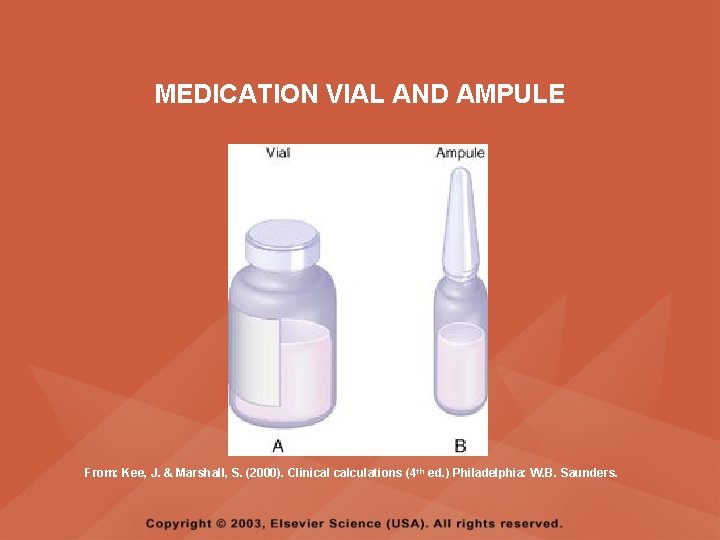
PARENTERAL MEDICATIONS • Parenteral always means injection route, and parenteral medications are administered by intravenous (IV), intramuscular (IM), or subcutaneous (SC) routes • Parenteral medications are packaged in singleuse ampules, single- and multiple-use rubber stoppered vials, and in prefilled syringes and cartridges
MEDICATION VIAL AND AMPULE From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
PRE-FILLED SYRINGES From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders. Courtesy of Wyeth-Ayerst Laboratories, Philadelphia, PA.
PARENTERAL MEDICATIONS • The nurse should not administer more than 3 ml per IM or SC injection site, as volumes larger than 3 ml are difficult for a single injection site to absorb • Always question excessively large or small volumes of medication
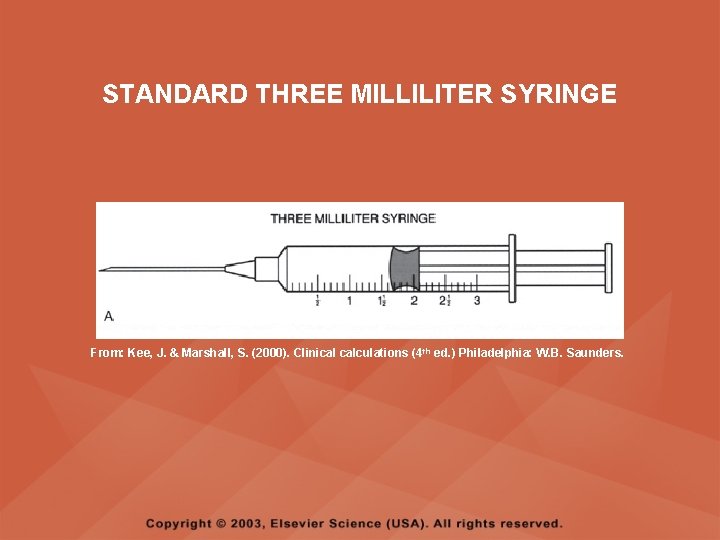
PARENTERAL MEDICATIONS • The standard 3 ml (cc) syringe is used to measure most injectable medications; it is calibrated in tenths (0. 1) of a milliliter • The calibrations on a syringe are read from the top black ring on the syringe, not the raised middle section and not the bottom ring
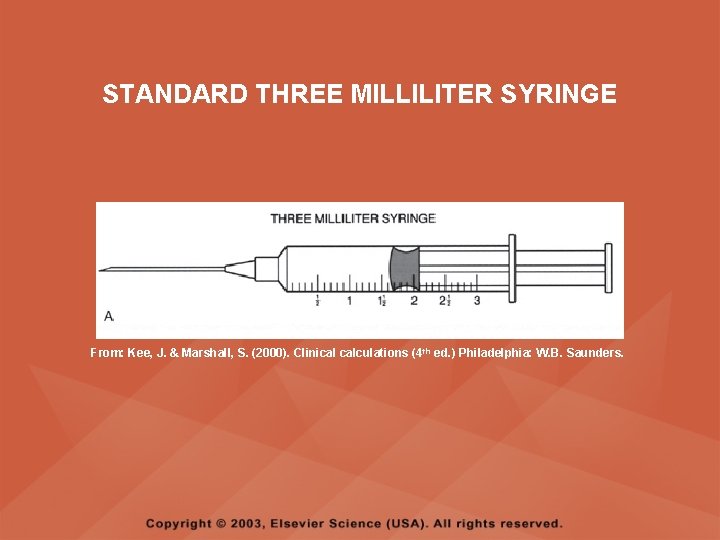
STANDARD THREE MILLILITER SYRINGE From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
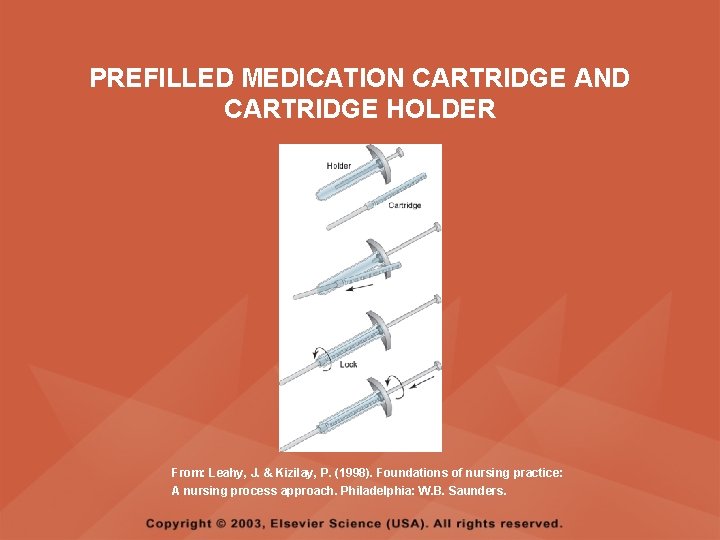
PREFILLED MEDICATION CARTRIDGE AND CARTRIDGE HOLDER • Tubex and Carpuject are trade names of two widely used, reusable, metal or plastic cartridge holders • The medication cartridge slips into the cartridge holder, which provides a plunger for injection of the medication • The medication cartridge is prefilled with sterile medication and is labeled with the medication name and dosage
PREFILLED MEDICATION CARTRIDGE AND CARTRIDGE HOLDER • The medication cartridge is routinely overfilled with 0. 1 to 0. 2 ml of medication to allow for manipulation of the holder to expel air from the needle prior to injection • The medication cartridge is designed to provide sufficient capacity to allow for the addition of a second medication when combined dosages are prescribed
PREFILLED MEDICATION CARTRIDGE AND CARTRIDGE HOLDER • The prefilled medication cartridge is to be used once and discarded; if the nurse is to give less than a full single dose provided, the nurse needs to discard the extra amount before injecting the client following agency policies and procedures
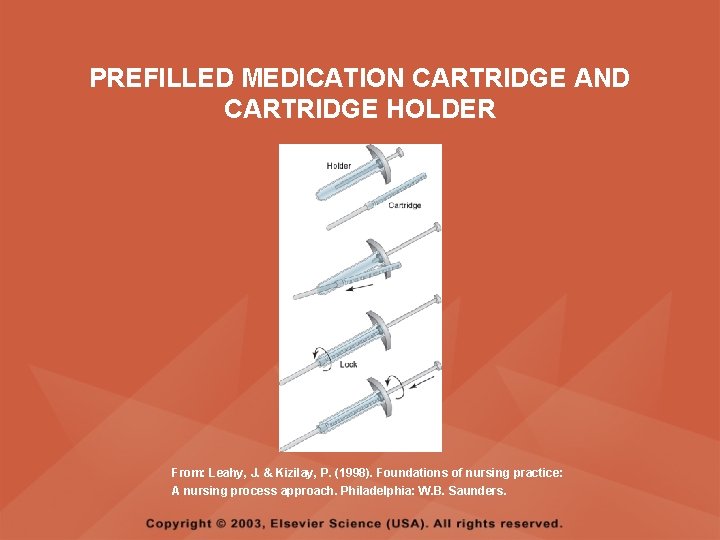
PREFILLED MEDICATION CARTRIDGE AND CARTRIDGE HOLDER From: Leahy, J. & Kizilay, P. (1998). Foundations of nursing practice: A nursing process approach. Philadelphia: W. B. Saunders.
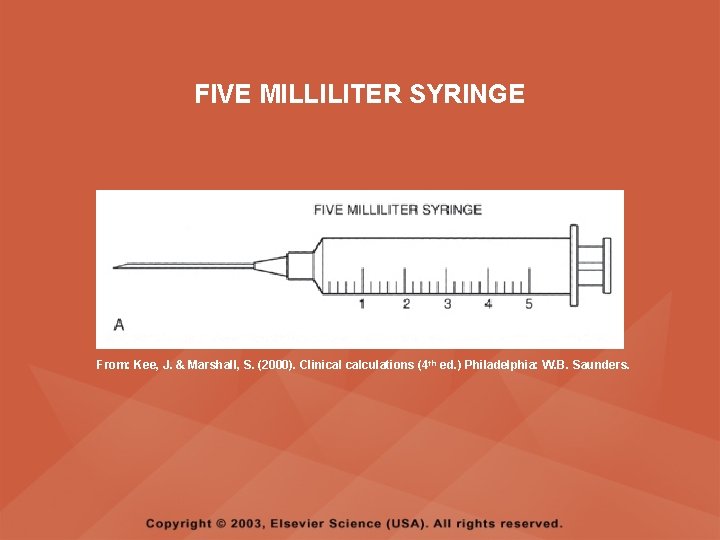
PARENTERAL MEDICATIONS • Standard medication doses for adults are to be rounded to the nearest tenth (0. 1) of a milliliter or cc and measured on the ml scale; for example, 1. 25 ml is rounded to 1. 3 ml • When volumes larger than 3 ml are required, a 5 -, 6 -, 10 -, or 12 -ml syringe may be used; these syringes are calibrated in fifths • Syringes larger than 12 ml are calibrated in full ml measures
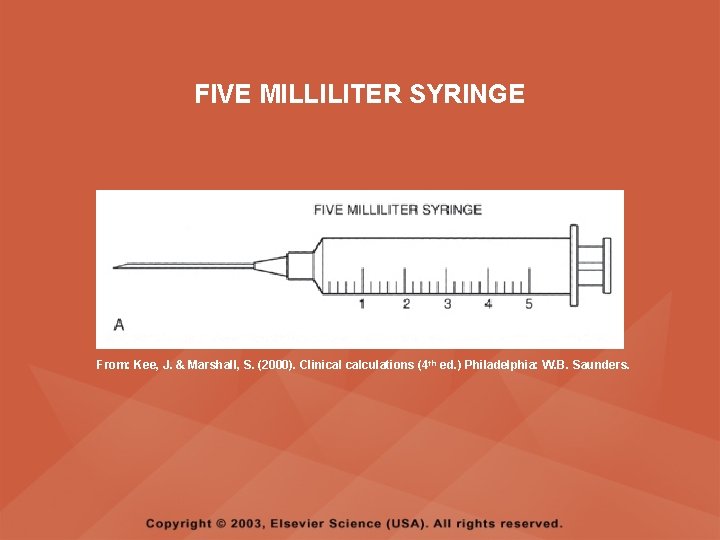
FIVE MILLILITER SYRINGE From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
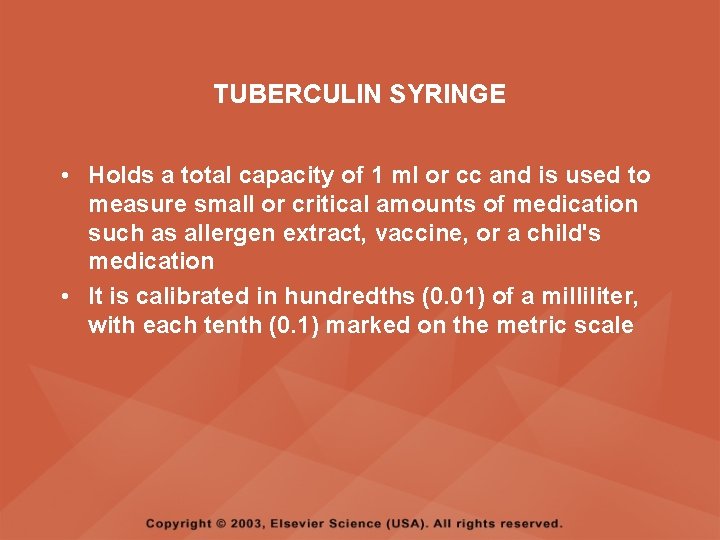
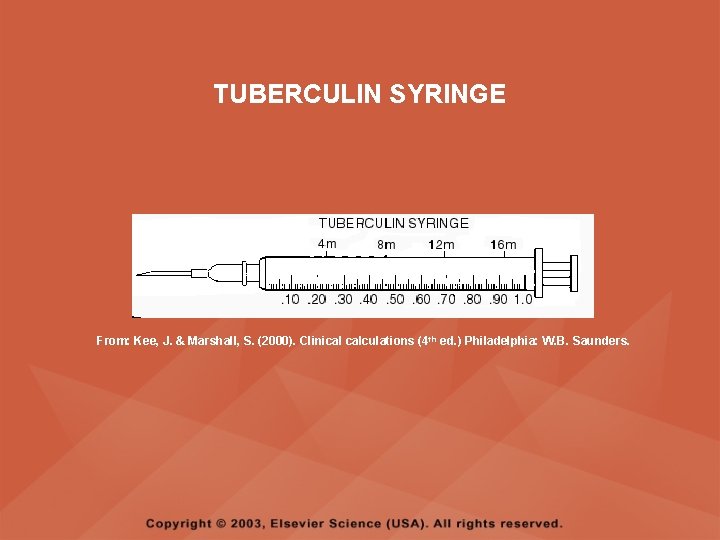
TUBERCULIN SYRINGE • Holds a total capacity of 1 ml or cc and is used to measure small or critical amounts of medication such as allergen extract, vaccine, or a child's medication • It is calibrated in hundredths (0. 01) of a milliliter, with each tenth (0. 1) marked on the metric scale
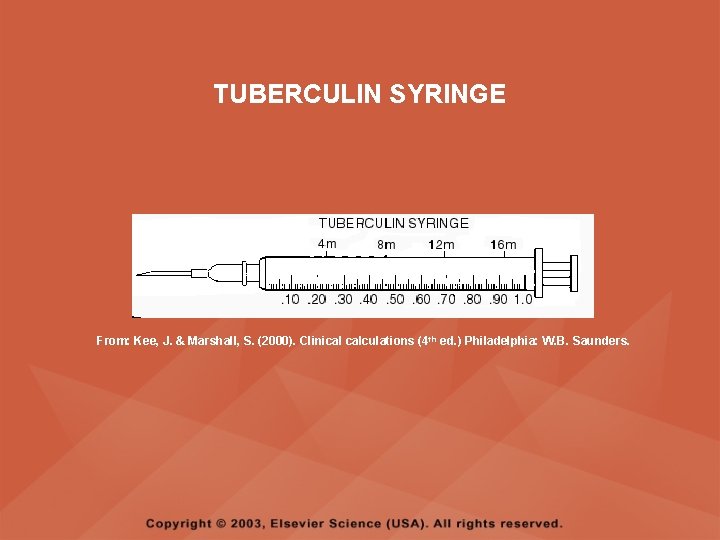
TUBERCULIN SYRINGE From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
INSULIN SYRINGE • The standard U-100 insulin syringe is used to measure U-100 insulin only; it is calibrated for a total of 100 units, or 1 ml (cc) • Insulin should not be measured in any other type of syringe • When the insulin order states to combine Regular and NPH insulin, remember "R. N. " and draw "R"egular insulin first, and then draw the "N"PH insulin
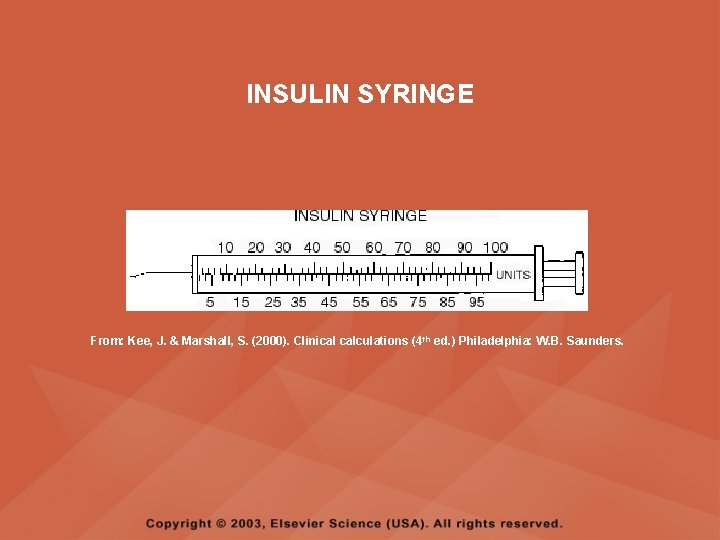
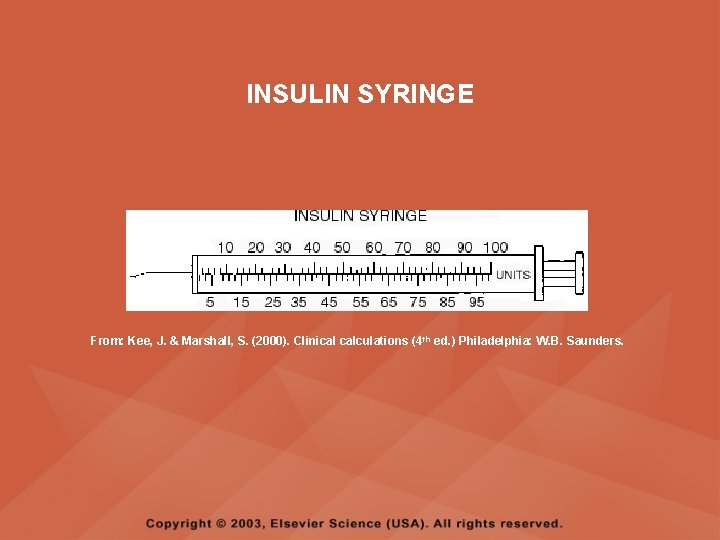
INSULIN SYRINGE From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
INJECTABLE MEDICATIONS IN POWDER FORM • Some medications become unstable when stored in solution form and are therefore packaged in powder form • Powders must be dissolved with a sterile diluent before use; usually sterile water or normal saline is used • The dissolving procedure is called reconstitution
CALCULATING THE CORRECT DOSAGE • When calculating oral medications, check the calculation and question an order if the calculation is for more than three tablets • When calculating parenteral medications, check the calculation and question an order if the amount to be given is too large of a dose • Regardless of the source of the error, if the nurse gives an incorrect dose, the nurse is legally responsible for the action
CALCULATING THE CORRECT DOSAGE • Be sure that all measures are in the same system, and all units are in the same size, converting when necessary; carefully consider the amount of medication that would be reasonable to administer • Round standard injection doses to tenths and measure in a 3 ml syringe • Round small, critical, or children's doses to hundredths and measure in the 1 ml tuberculin syringe
FORMULA FOR CALCULATING A MEDICATION DOSAGE D (Desired) x Q (Quantity) = X A (Available) • D (Desired) = The dosage that the physician ordered • A (Available) = The dosage strength as stated on the medication label • Q (Quantity) = The volume that the dosage strength is available in, such as tablets, capsules, or ml
CALCULATING DOSAGES EXPRESSED AS RATIO OR PERCENT • PERCENTAGE SOLUTIONS – Express the number of grams of the medication per 100 ml of solution – Example: Calcium gluconate 10% = 10 g of pure medication per 100 ml of solution • RATIO SOLUTIONS – Express the number of grams of the medication per total milliliters of solution – Example: Epinephrine 1: 1000 = 1 g pure medication per 1000 ml solution
INTRAVENOUS FLOW RATES • Monitor IVs every 30 minutes for adults and every 15 minutes for children • If the IV is running behind schedule, collaborate with the physician to determine the client's ability to tolerate an increased flow rate, particularly those clients with cardiac, pulmonary, renal, and neurological conditions • The nurse should never arbitrarily speed up an IV to catch up if the IV is running behind schedule
INTRAVENOUS FLOW RATES • Whenever an IV rate is increased, the nurse should assess the client for increased heart rate, increased respirations, or increased lung congestion, which could indicate fluid overload • IV fluids are most frequently ordered on the basis of milliliters (ml) per hour to be administered • The volume per hour ordered is administered by adjusting the rate at which the IV infuses, which is counted in drops (gtt) per minute • Most flow rate calculations involve changing milliliters per hour into drops per minute
FORMULAS FOR INTRAVENOUS CALCULATIONS • FLOW RATES Total volume x gtt factor = gtt per min Time in minutes • INFUSION TIME Total volume to infused = Infusion time ml per hour being infused
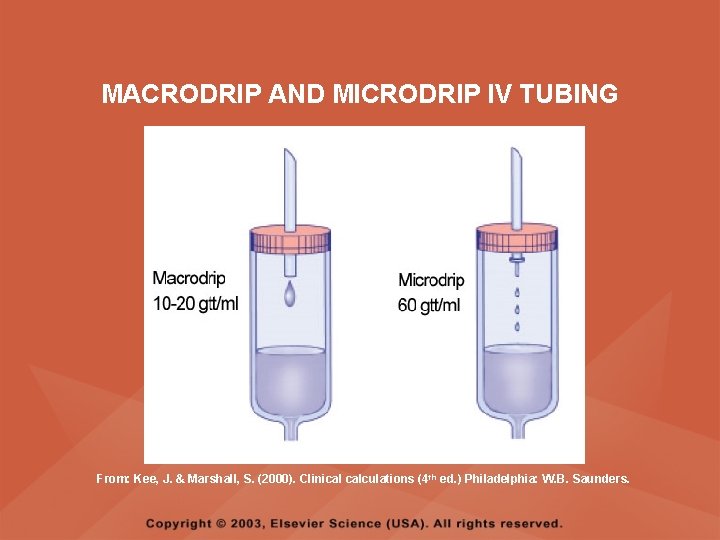
IV TUBING • Calibrated in gtts per milliliters, and this calibration is needed for calculating flow rates • A standard or macrodrip set is used for routine adult IV administrations; depending on the manufacturer and type of tubing, it will require 10, 15, or 20 gtts to equal 1 ml • The calibration, in gtts per ml, is written on the IV tubing package
IV TUBING • A mini- or microdrip set is used when more exact measurements are needed, such as in intensive care units and in pediatric units • In a mini- or microdrip set, 60 gtts is equal to 1 ml
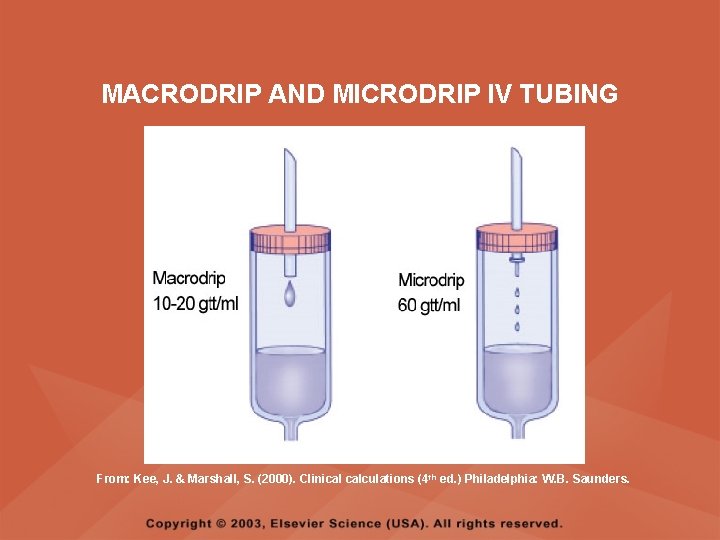
MACRODRIP AND MICRODRIP IV TUBING From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
ELECTRONIC IV FLOW RATE REGULATORS • CONTROLLER – Works on the same principle of gravity as a regular IV drip, with the rate of flow being maintained by rapid compression and decompression of the IV tubing by the machine – The desired flow rate is set on the controller in milliliters per hr – Because controllers work by gravity, the height of the solution bag is critical and must be maintained at a minimum of 36 inches above the controller
ELECTRONIC IV FLOW RATE REGULATORS • PUMP – A pump is different from a controller in that it physically pumps fluids against resistance – Gravity is not a factor in the use of a pump, and the height of the IV solution container is not a critical factor – The flow rate on a pump is set in milliliters per hour – The nurse should continue to assess the amount of IV solution in the IV container and monitor the pump or controller to assure proper functioning of the machine
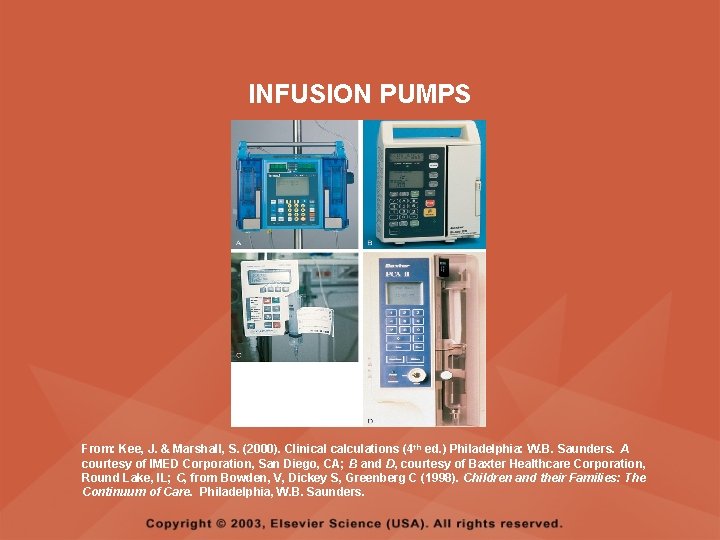
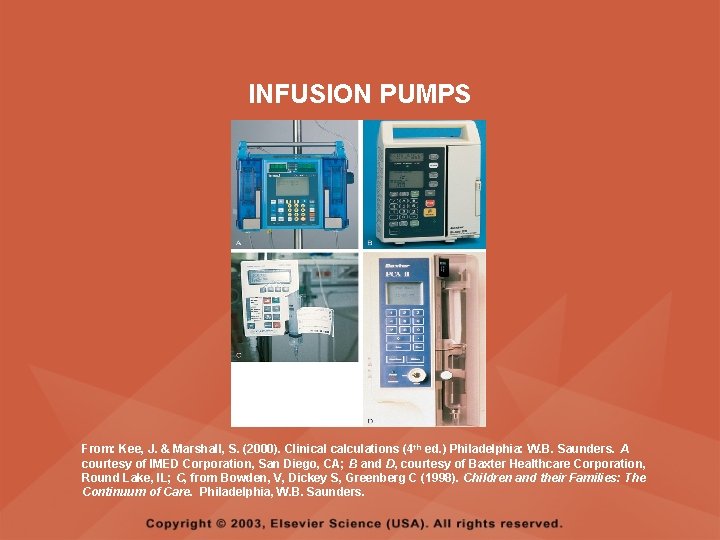
INFUSION PUMPS From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders. A courtesy of IMED Corporation, San Diego, CA; B and D, courtesy of Baxter Healthcare Corporation, Round Lake, IL; C, from Bowden, V, Dickey S, Greenberg C (1998). Children and their Families: The Continuum of Care. Philadelphia, W. B. Saunders.
INFUSIONS ORDERED BY UNIT DOSAGE PER HOUR • The most common medications that will be ordered by unit dosage per hour and to run by continuous infusion are heparin sodium and Regular insulin • Calculation of these problems requires a two-step process – Determine the amount of medication per 1 ml – Determine the infusion rate or milliliters per hour
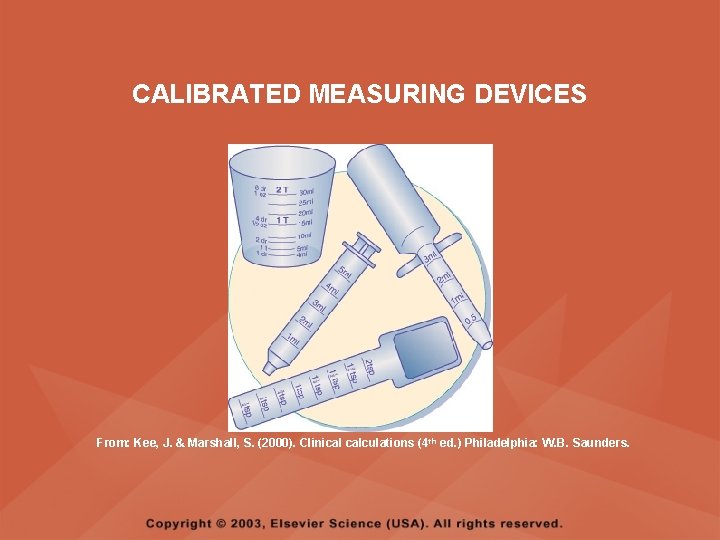
PEDIATRICS: ORAL MEDICATIONS • Most oral pediatric medications are in liquid or suspension form since children usually are not able to swallow a tablet • Solutions may be measured using an oral syringe, a small plastic cup, an oral dropper, or a measuring spoon
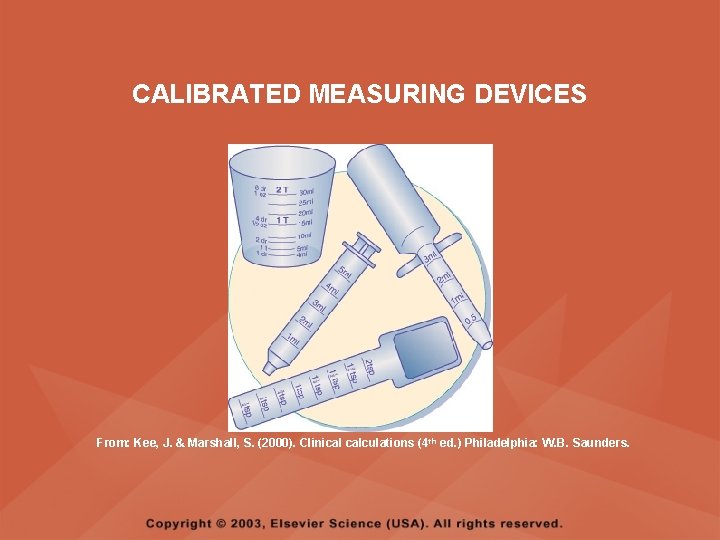
CALIBRATED MEASURING DEVICES From: Kee, J. & Marshall, S. (2000). Clinical calculations (4 th ed. ) Philadelphia: W. B. Saunders.
PEDIATRICS: ORAL MEDICATIONS • Medications in suspension settle to the bottom of the bottle between uses and thorough mixing is required prior to pouring the medication • Suspensions must be administered immediately after measurement to prevent settling and administering an incomplete dose • Administer oral medications with the child sitting in an upright position with the head elevated to prevent aspiration if the child cries or resists
PEDIATRICS: ORAL MEDICATIONS • Never pinch the infant’s or child’s nostrils when administering medication • Do not place medication in a baby’s bottle • Draw the required dose of an unpleasant medication into a small syringe and place the syringe into the side and towards the back of the infant’s mouth; administer the medication slowly, allowing the infant to swallow
PEDIATRICS: ORAL MEDICATIONS • Place the small child sideways on the lap; the child’s closest arm should be placed under the adult’s arm and behind the adult’s back; cradle the child’s head and hold the child’s hand administer the medication slowly with a plastic spoon or small plastic cup • Mix liquid medications with less than an ounce of fluid to disguise the taste if necessary
PEDIATRICS: ORAL MEDICATIONS • Check the child’s mouth if a tablet or capsule has been administered to assure that it has been swallowed; if swallowing is a problem, some tablets can be crushed and given in small amounts of puréed food or flavored syrup (enteric -coated, timed-release tablets, or capsules cannot be crushed)
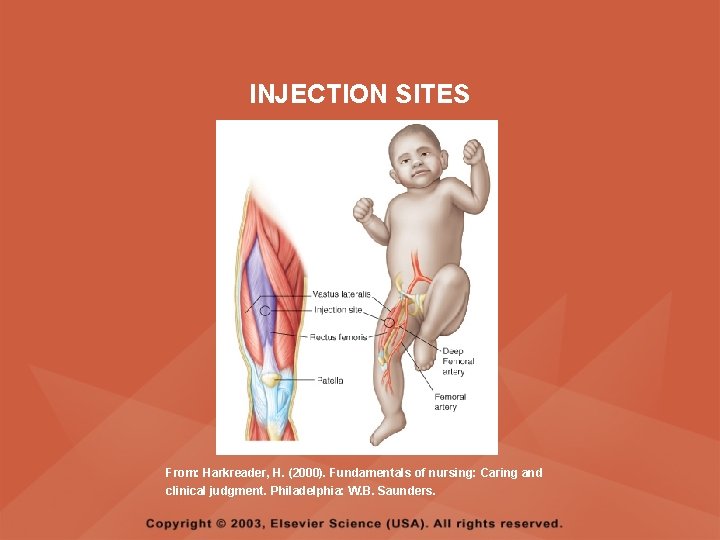
PEDIATRICS: SUBCUTANEOUS (SC) AND INTRAMUSCULAR (IM) MEDICATIONS • Medications most often given via the SC route are insulin and most immunizations • Any site with sufficient subcutaneous tissue may be used for SC injections; common sites include the central third of the lateral aspect of the upper arm, the abdomen, and the center third of the anterior thigh • The safe use of all injection sites is based on normal muscle development and the size of the child; the preferred site for IM injections in infants is the vastus lateralis
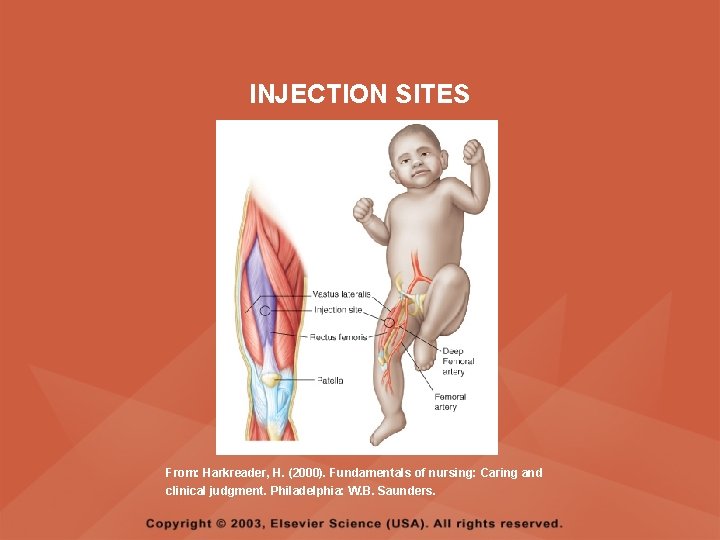
INJECTION SITES From: Harkreader, H. (2000). Fundamentals of nursing: Caring and clinical judgment. Philadelphia: W. B. Saunders.
PEDIATRICS: SUBCUTANEOUS (SC) AND INTRAMUSCULAR (IM) MEDICATIONS • Usually not more than 0. 5 ml (infant) to 2. 0 ml (child) is injected per IM or SC site and the site of injection is rotated if frequent injections are necessary • The usual needle length and gauge for pediatric clients is 1/2 to 1 inch long and 22 - to 25 -gauge • Needle length can also be estimated by grasping the muscle for injection between the thumb and forefinger; half the distance would be the needle length
PEDIATRICS: SUBCUTANEOUS (SC) AND INTRAMUSCULAR (IM) MEDICATIONS • Pediatric dosages for SC and IM administration are calculated to the nearest hundredth and measured using a tuberculin (TB) syringe • For the toddler and preschooler, place an adhesive bandage or decorated bandage over the puncture site
PEDIATRICS: INTRAVENOUS (IV) MEDICATIONS • IV medications are diluted for administration • When an infant or child is receiving an IV medication, the IV site needs to be assessed for signs of infiltration and inflammation immediately before, during, and after completion of each medication • Signs of inflammation include redness, heat, swelling, and tenderness • Signs of infiltration include swelling, coolness, pain, and lack of blood return
PEDIATRICS: INTRAVENOUS (IV) MEDICATIONS • If inflammation or infiltration occurs, the IV is discontinued and restarted at a new site • IV medication may be administered on a continuous basis by adding the medication to an IV solution bag and infusing it through a primary infusion line • IV medications may be administered on an intermittent basis, involving several dosages within a 24 -hour period
PEDIATRICS: INTRAVENOUS (IV) MEDICATIONS • Medications for IV administration are diluted according to the directions accompanying the medication and according to physician’s orders and agency procedures • Infusion time for IV medications is determined based on the directions accompanying the medication, the physician’s orders, and agency procedures
PEDIATRICS: INTRAVENOUS (IV) MEDICATIONS • Determine agency procedures related to the volume of flush for peripheral IV lines and for central lines • The flush volume (3– 20 ml) must be included in the child’s intake; the flush is started after the IV medication is completed and is infused at the same rate as the medication
PEDIATRICS: INTERMITTENT IV MEDICATION ADMINISTRATION • Children receiving IV medications on an intermittent basis may or may not have a primary IV • If a primary IV exists, the medication may be administered by IV piggyback (IVPB) via a secondary line • If a primary line does not exist, an indwelling infusion catheter is used for medication administration
PEDIATRICS: INTERMITTENT IV MEDICATION ADMINISTRATION • All intermittent medication administrations are preceded and followed by a flush to assure that the medication has cleared the IV tubing and that the total dosage has been administered • Electronic controllers and pumps are used to regulate and administer IVs and intermittent IV medications
PEDIATRICS: SPECIAL IV ADMINISTRATION SETS • Special IV administration sets, referred to by their trade names (Buretrol, Soluset, Volutrol), may be used for medication preparation and administration • These special sets are all microdrip sets calibrated to deliver 60 drops (gtt) per ml • The total capacity of these special IV administration sets is between 100 to 150 ml, calibrated in 1 ml increments so that exact measurements of small volumes is possible
PEDIATRICS: SPECIAL IV ADMINISTRATION SETS • The medication is mixed with the appropriate amount of diluent and added to the special IV administration set, and the medication is allowed to infuse at the prescribed rate • Label the special IV administration set to identify the medication and fluid dosage added • Attach a label that states “medication infusing” during the medication infusion time • Attach a label that states “flush infusing” during the flush infusion time
PEDIATRICS: RETROGRADE IV INJECTION • The medication is mixed with the appropriate amount of diluent in a syringe • The IV tubing is clamped close to the child, the medication is injected through the port in the direction of the burette, the tubing is unclamped, the prescribed rate is set, and the medication is allowed to infuse over the prescribed time
PEDIATRICS: SYRINGE PUMP FOR IV MEDICATION ADMINISTRATION • A syringe containing the medication is fitted into a pump that is connected to the IV tubing through a Y-connector • The medication is administered over the prescribed time
CALCULATION OF MEDICATION DOSAGE BY BODY WEIGHT • POUNDS (LB) TO KILOGRAMS (KG) – 1 kg = 2. 2 lb – To convert from pounds to kilograms, divide by 2. 2 – Kilograms are expressed to the nearest tenth • KILOGRAMS (KG) TO POUNDS (LB) – 1 kg = 2. 2 lb – To convert from kilograms to pounds, multiply by 2. 2 – Pounds are expressed to the nearest tenth
CALCULATION OF MEDICATION DOSAGE BY BODY WEIGHT • CALCULATING DAILY DOSAGES – Dosages are expressed in terms of mg/kg/day, mg/lb/day, or mg/kg/dose – The total daily dosage is usually administered in divided (more than one) doses per day – Express the child’s body weight in kilograms or pounds to correlate with the dosage specifications – Calculate the total daily dosage – Divide the total daily dosage by the number of doses to be administered in one day
CALCULATION OF BODY SURFACE AREA (BSA) • The body surface area is determined by comparing body weight and height with averages or norms on a graph called a nomogram • Not all children are the same size at the same age; therefore, the nomogram chart is used to determine the BSA of a child
MEDICATION CALCULATION BASED ON BSA • When dosage recommendations for children specify mg, mcg, or U per m 2, calculating the dosage is simple multiplication • PROBLEM – The dosage recommendation is 4 mg per m 2. The child has a BSA of 1. 1 m 2. What is the dosage to be administered? • SOLUTION – 1. 1 x 4 mg = 4. 4 mg
MEDICATION CALCULATION BASED ON BSA • When dosages are specified only for adults, a formula is used to calculate a child’s dosage from the adult dosage • PROBLEM – The physician has prescribed an antibiotic for a child. The average adult dose is 250 mg. The child has a BSA of 0. 41 m 2. What is the dose for the child?
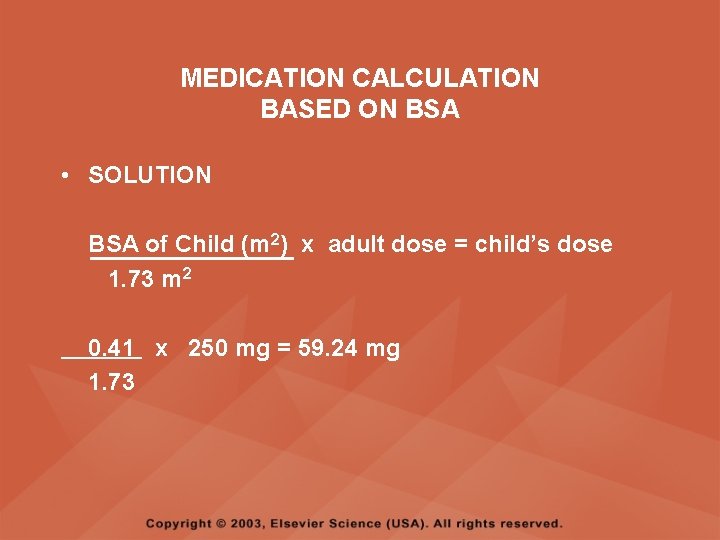
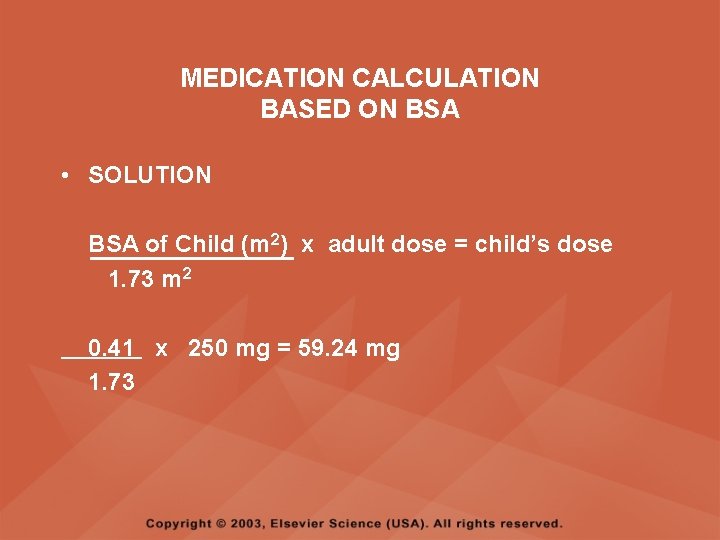
MEDICATION CALCULATION BASED ON BSA • SOLUTION BSA of Child (m 2) x adult dose = child’s dose 1. 73 m 2 0. 41 x 250 mg = 59. 24 mg 1. 73