Navigating United Healthcare Community Plan A Care Provider



- Slides: 35

Navigating United. Healthcare Community Plan A Care Provider Orientation © 2015 United. Health Group. Confidential and proprietary information of United. Health Group. Any use, copying or distribution without written permission from United. Health Group is prohibited. 1
Introduction United. Healthcare Community Plan is contracted with the Texas Department of Health and Human Services Commission (HHSC) to serve people in Texas who have chronic health conditions and/or qualify financially for state health plan benefits. We support the patient-centered Medical Home approach in which primary care providers (PCPs) oversee health care services to help ensure they are accessible, person-centered, sensitive to cultural differences, comprehensive, coordinated and compassionate. Care for every member should integrate health education, wellness and prevention. PCA-1 -001465 -03302016_05122016 2
CHIP and STAR Children’s Health Insurance Program (CHIP) is for children younger than 19 whose families earn too much financially to qualify for Medicaid, yet cannot afford private health insurance. CHIP Perinate allows for limited coverage of a woman’s prenatal and postnatal health care as well as 12 months coverage for CHIP Perinate newborns. State of Texas Access Reform (STAR) covers pregnant women and children who are 20 and younger and qualify for Medicaid. PCA-1 -001465 -03302016_05122016 3
STAR+PLUS and Medicare STAR+PLUS combines acute health care services with long-term services and supports (LTSS) for Medicaid members who have disabilities or are 65 and older. Coverage includes nursing facility long-term care. We also offer the following plans for people 65 and older or who have disabilities and qualify for Medicare: • United. Healthcare Dual Complete® (HMO SNP) • United. Healthcare Connected® (Medicare-Medicaid Plan) PCA-1 -001465 -03302016_05122016 4
STAR Kids We are pleased to be welcoming STAR Kids members beginning Nov. 1, 2016. This program provides health care and LTSS services for children and adolescents who are 20 and younger. Our STAR Kids program will integrate: • • • STAR+PLUS Medical Dependent Children Program (MDCP) waiver program Intellectual and Developmental Disabilities waiver programs Home and Community-based Services (HCBS) Texas Home Living (Tx. Hm. L) Intermediate Care Facilities for Persons with an Intellectual Disability (ICF/IID) program PCA-1 -001465 -03302016_05122016 5
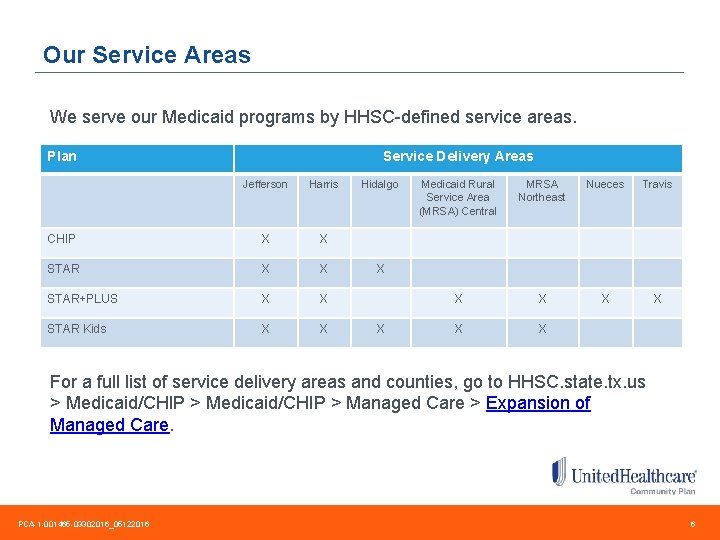
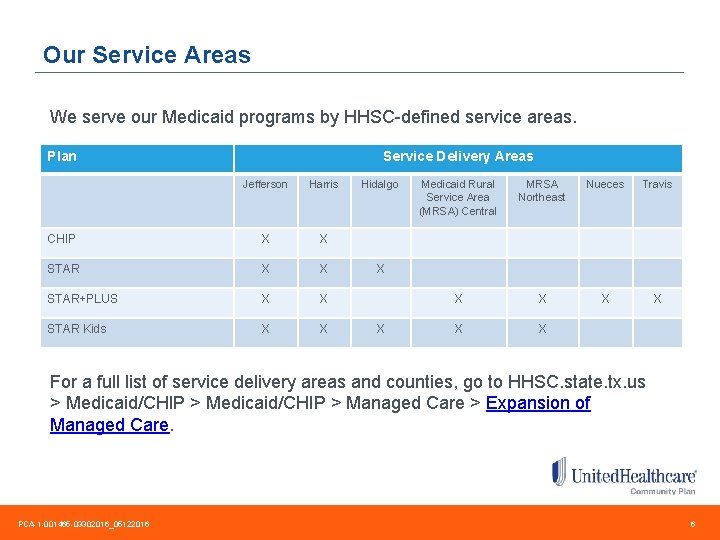
Our Service Areas We serve our Medicaid programs by HHSC-defined service areas. Plan Service Delivery Areas Jefferson Harris CHIP X X STAR+PLUS X X STAR Kids X X Hidalgo Medicaid Rural Service Area (MRSA) Central MRSA Northeast Nueces Travis X X X X For a full list of service delivery areas and counties, go to HHSC. state. tx. us > Medicaid/CHIP > Managed Care > Expansion of Managed Care. PCA-1 -001465 -03302016_05122016 6
Covered Services To see which benefits a member is eligible for, use the Eligibility & Benefits application on Link. Go to United. Healthcare. Online. com and sign in to Link to access the application. Or, visit UHCCommunity. Plan. com > Just show me all plans in the state > Texas. Or, call our Customer Service at 888 -887 -9003. When more than one care provider is involved in a member’s care, be sure to coordinate services, which will allow you to share assessments and treatments. Remember to obtain member consent to release information. PCA-1 -001465 -03302016_05122016 7
Verifying Eligibility There a number of ways to verify that your patient is a current member in our health plan before you deliver services: • Call Texas Medicaid Automated Inquiry System at 800 -925 -9126. • Swipe the member’s Your Texas Benefits Medicaid card through a standard magnetic card reader if your office uses that technology. • Do a member lookup at Tex. Med. Connect on the Texas Medicaid & Healthcare Partnership (TMHP) website at TMHP. com > Providers. Select “Go to Tex. Med. Connect” from the top right of the home page. You will need to log in. • Use the Eligibility & Benefits application on Link. Go to United. Healthcare. Online. com and sign in to Link to access the application. • Call United. Healthcare Community Plan Customer Service at 888 -887 -9003. PCA-1 -001465 -03302016_05122016 8
Early Childhood Intervention (ECI) is a state and federally-funded program created with part C of the Individuals with Disabilities Education Act of 2011. Its goal is to help ensure that children with developmental delays are ready for preschool and kindergarten. PCPs are legal reporters and parents can self-refer. Call 800 -628 -5115 or send an email to DARS. Inquiries@dars. state. tx. us An easy-to-use physician referral form is located at Texas Chapter of the American Academy of Pediatrics at TXPeds. org > Additional Resources > Physician Resources > Forms > Statewide ECI Referral Form. PCA-1 -001465 -03302016_05122016 9
Texas Health Steps Medicaid-enrolled children and young adults ages 20 and younger should receive medical check-ups and screenings according to the Texas Health Steps (THSteps) program. This Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit applies to STAR, STAR+PLUS and STAR Kids. Texas Health Steps policies and procedures are outlined in the Texas Medicaid Provider Procedures Manual, specifically in the Children’s Services Handbook section available at TMHP. com > Providers > Medicaid Provider Manual. Enroll to be a THSteps provider at TMHP. com > Providers > Enroll Today! For more information, go to UHCCommunity. Plan. com > For Health Care Providers > Texas > Provider Training > Texas Health Steps. Visit also TXHealth. Steps. com which includes continuing education credits. PCA-1 -001465 -03302016_05122016 10
Texas Medicaid Non-emergency Transportation Medicaid members can get a ride to the doctor, dentist or pharmacy from the Medicaid Transportation Program. • Hidalgo, Nueces, Travis Service Delivery Areas – Call 877 -633 -8747 • Central and Northeast Medicaid Rural Service Areas – Call 855 -687 -4786 • Harris and Jefferson Service Delivery Areas – Call 855 -687 -4786 When Medicaid transportation is not available, please call Customer Service at 888 -887 -9003 for assistance. PCA-1 -001465 -03302016_05122016 11
Accommodation of Services When one of our members requires assistance to communicate with you due to language barriers, or a need for hearing or visual aids, please call Customer Service at 888 -887 -9003. Many of our members need special accommodations to get health services. You can learn more at ADA. gov > Technical Assistance Materials > Access to Medical Care for Individuals with Mobility Disabilities. PCA-1 -001465 -03302016_05122016 12
Commitment to Culturally Considerate Care Our members require person-centered care that is delivered with respect to their individual preferences and abilities. The National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care (the National CLAS Standards) are intended to advance health equity, improve quality and help eliminate health care disparities by providing a blueprint for culturally and linguistically appropriate services. Learn more at Think. Cultural. Health. HHS. gov. PCA-1 -001465 -03302016_05122016 13

Service Coordination Our service coordinators work with members, their families, PCPs and other professional care providers to develop a person-centered plan of care. Community. Care is our online service coordination tool. Go to United. Healthcare. Online. com and sign in to Link to access the application. To reach a service coordinator to report a change in a member’s condition or circumstances, use the messaging functionality in Community. Care or call 800 -349 -0550. For STAR Kids members, call 877352 -7798. PCA-1 -001465 -03302016_05122016 14
Value-added Services Our Value-added Services supplement member benefits and are specifically selected to support our members and help them live healthier lives. Services include healthy weight interventions, incentive gift cards, and access to extra services including vision. These services are offered at no cost to members. To see a full list, visit UHCCommunity. Plan. com > For Health Care Providers > Texas > Bulletins > Provider Reference Guides > Value-added Services. PCA-1 -001465 -03302016_05122016 15
Pharmacy Online formulary and preferred drug information The Texas Medicaid drug formulary and preferred drug list are located at TXVendor. Drug. com > Formulary/PDL or go to Epocrates. com to sign up to view this information on a handheld device. Electronic Prescribing We encourage e-prescribing through Sure. Scripts. com. Emergency Prescriptions If there is a need to start drug therapy without delay and prior authorization is not available, a 72 -hour supply can be issued on a one-time basis per member per drug. For details visit TXVendor. Drug. com > Submit a 72 hour emergency override. PCA-1 -001465 -03302016_05122016 16
DME Available at Pharmacy Limited durable medical equipment (DME) items are available through the medical benefits plan for pharmacies that are Medicaid DME medical providers. Covered items include: • • • Orally administered iron salts Insulin syringes and needles Aerosol holding chambers Blood glucose meters Blood glucose reagent strips Diabetic lancets and devices Hypertonic saline solution Oral bowel evacuants Oral electrolyte solution PCA-1 -001465 -03302016_05122016 17
DME Available at Pharmacy cont’d We encourage network pharmacies to become DME network providers as well in order to dispense these items for our members. For more information, visit TXVendor. Drug. com > Learn more about enrolling in the Comprehensive Care Program or providing DME/supplies. And call United. Healthcare Network Management at 866 -574 -6088 to contract as a DME provider in addition to being a network pharmacy. PCA-1 -001465 -03302016_05122016 18
Prior Authorization Some services require prior authorization. You can request prior authorization in a number of ways: Online: Go to United. Healthcare. Online. com and sign in to Link to access the Eligibility & Benefits application. A notification will pop up when a service requires prior authorization. Follow the pop-up link to submit the request online. Fax: Submit a prior authorization form by fax to 877 -940 -1972. To access the form, go to UHCCommunity. Plan. com > For Health Care Professionals > Texas > Provider Forms > Standard Prior Authorization Form: Texas Department of Insurance. Phone: Call 866 -604 -3267. For a full list of services that require prior authorization, go to UHCCommunity. Plan. com > For Health Care Providers > Texas > Prior Authorization. PCA-1 -001465 -03302016_05122016 19
Non-standard Prior Authorization Some prior authorizations are non-standard: Medications: Access forms at UHCCommunity. Plan. com > For Health Care Professionals > Texas > Pharmacy Program to fax to 866 -940 -7328. Or call Pharmacy Services at 800 -310 -6826. Cardiology and Radiology: Prior authorization procedures can be found at UHCCommunity. Plan. com > For Health Care Professionals > Texas > Cardiology or Radiology. Long Term Services and Supports (LTSS): Prior authorizations for LTSS are secured through the member’s service coordinator. These authorizations should be confirmed prior to service delivery at United. Healthcare. Online. com > Notifications/Prior Authorization Status. PCA-1 -001465 -03302016_05122016 20
Quality Our quality program looks at services delivered according to the standards of the Healthcare Effectiveness Data and Information Set (HEDIS®). See more at NCQA. org > HEDIS & Quality Measurement. PCPs can also view care opportunity reporting through Community. Care, our online care coordination tool. Go to United. Healthcare. Online. com and sign in to Link to access the application. Another option is through United. Healthcare. Online. com > sign into Link > Eligibility & Benefits > Gaps in Care Exist. Our adopted Best Clinical Practice Guidelines are posted to UHCCommunity. Plan. com > For Health Care Professionals > Texas > Clinical Practice Guidelines. PCA-1 -001465 -03302016_05122016 21
Claims Submission Professional claims for acute health care and long term services and supports can be submitted in a number of ways: Online: You can submit claims through United. Healthcare. Online. com > Claims Submission > Claims & Payments or use a clearinghouse of your choice. Payer ID is 87726. Mail: Send CMS 1500 or UB-04 forms to the applicable address: CHIP and STAR P. O. Box 5270 Kingston, NY, 12402 -5207 STAR Kids P. O. Box 5290 Kingston, NY 12402 -5290 STAR+PLUS and DSNP P. O. Box 31352 Salt Lake City, UT 84131 -0352 As a reminder, members cannot be balance billed in any circumstances. PCA-1 -001465 -03302016_05122016 22
Claims Submission Deadlines Claims must be received by United. Healthcare Community Plan within 95 days of the date of service to be considered for payment. Clean claims are processed within 30 days of receipt. Clean pharmacy claims are paid within 18 days when submitted online or otherwise paid within 21 days. The claim address must match either the place of service or the billing address listed in our claims processing system for the claim to be processed in a timely manner. PCA-1 -001465 -03302016_05122016 23
110 -Day Rule When a Medicaid member has other health insurance, the other insurance must be billed before billing us. If you do not get a response within 110 days, you can submit the claim to us. We must receive the claim within 12 months from the date of service for it to be paid. PCA-1 -001465 -03302016_05122016 24
Fraud, Waste and Abuse Anyone knowing of suspicious activities that have the potential for fraud, waste and abuse must report such suspicions. • Fraud is intentional deception or misrepresentation of billing and services. • Waste is overutilization, underutilization or misuse of resources. • Abuse is financial actions that are inconsistent with sound fiscal, business or medical practice, and that result in unnecessary cost to the Medicaid program. PCA-1 -001465 -03302016_05122016 25
Reporting Suspected Fraud, Waste or Abuse Fraud, waste or abuse can be reported to: Office of Inspector General (HHSC-OIG) Call 800 -436 -6184 or go to OIG. HHSC. state. tx. us > Report Fraud. United. Healthcare Community Plan Call 888 -887 -9003 or mail to: United. Healthcare Community Plan Attn: Compliance 14141 Southwest Freeway, Suite 800 Sugar Land, TX 77478 Protections for those who report fraud, waste and abuse include the Federal False Claims Act, the Texas False Claims Act and the Whistleblower Act. PCA-1 -001465 -03302016_05122016 26
Electronic Payments & Statements Enroll in Electronic Payments & Statements (EPS) to receive direct deposit payment of your claims and access online provider remittance advices. Go to My. Services. Optum. Health. Payment. Services. com > How to Enroll. To learn more about EPS, go to United. Healthcare. Online. com > Help > Electronic Solutions > Electronic Payments & Statements. PCA-1 -001465 -03302016_05122016 27
Complaints and Appeals If you are not satisfied with the outcome of a claim reconsideration, you may submit a formal claim dispute/appeal using the process outlined in your provider manual which can be found at UHCCommunity. Plan. com > For Health Care Professionals > Texas > Manuals. Care providers may file complaints with United. Healthcare Community Plan by submitting the Provider Complaint/Grievance Form located at UHCCommunity. Plan. com > For Health Care Professionals > Texas > Provider Forms. If you have any questions, call our Customer Service at 888 -887 -9003. Notification of receipt of request will be sent within five business days. A decision is rendered within 30 calendar days. PCA-1 -001465 -03302016_05122016 28
Important Resources • The Texas Medicaid Provider Procedure Manual is available at TMHP. com > Providers > Medicaid Provider Manual. • Access the United. Healthcare Community Plan manuals at UHCCommunity. Plan. com > For Health Care Professionals > Texas > Manuals. • Network Bulletin: Monthly newsletter edition posted to United. Healthcare. Online. com > Tools & Resources > News & Network Bulletin. • Practice Matters: Quarterly newsletter posted to UHCCommunity. Plan. com > For Healthcare Professionals > Texas > Newsletters. • Provider Alerts – Check regularly for updates: • Texas Medicaid & Healthcare Partnership at TMHP. com > Providers • The Texas Health and Human Services Commission at HHSC. state. tx. us > News & Information > News Releases • UHCCommunity. Plan. com > For Health Care Professional > Texas > Bulletins > Provider Alerts PCA-1 -001465 -03302016_05122016 29
Contact Information Help ensure that members can find you and that payments get to you by keeping your practice information current in our systems and directories. Let us know if there is a change in your demographic information, such as your name, service or billing address, phone number, National Provider Identification number (NPI), Texas Provider Identification number (TPI) or Tax Identification Number (TIN). Submit your changes with the form located at UHCCommunity. Plan. com > For Health Care Providers > Texas > Provider Forms > Provider Address and Tax Updates or call 888 -887 -9003. PCA-1 -001465 -03302016_05122016 30
Contact Information cont’d Remember to update your information with the Texas Health and Human Services Commission, as well. Visit TMHP. com > providers > Today I would Like To … > Provider Information Management System (PIMS) User Guide. Changes involving identification numbers, such as tax identification numbers, or name need to be submitted to TMHP using a Provider Information Change Form. Mail the completed form to: Texas Medicaid & Healthcare Partnership, Provider Enrollment, P. O. Box 200795, Austin, TX 78720 -0795. Or you can fax to 512 -514 -4214. PCA-1 -001465 -03302016_05122016 31
Texas Medicaid Enrollment You need to enroll to provide health care to Texas Medicaid recipients. You may enroll with the Texas Medicaid through the Texas Medicaid & Healthcare Partnership. Go to TMHP. com > Providers > Enroll Today! Re-enrollment is required every three to five years, depending on your provider category. For more details, go to TMHP. com > Providers > Federal Reenrollment > Provider Enrollment Tools Quick Reference Guide. PCA-1 -001465 -03302016_05122016 32
For More Information Our Customer Service department has a team of representatives dedicated to network care provider needs. Please call 888 -887 -9003 weekdays, 8: 00 a. m. to 5 p. m. For contract issues, fee schedules or change of demographic information, contact United. Healthcare Network Management at 866 -574 -6088. We re-credential every three years. Providers of Long Term Services and Supports should call 888 -787 -4107. To find an in-network referral and to coordinate services for our members, including behavioral health, please visit UHCCommunity. Plan. com > For Health Care Providers > Texas > Find a Physician or call our Customer Service at 888 -887 -9003. PCA-1 -001465 -03302016_05122016 33
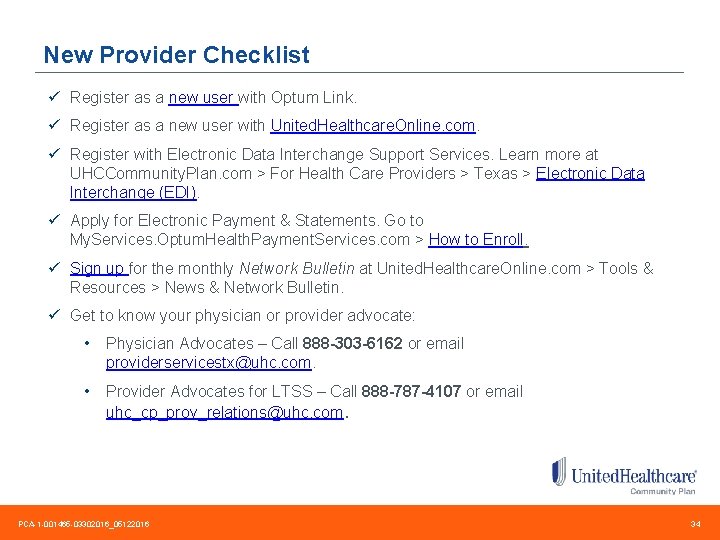
New Provider Checklist ü Register as a new user with Optum Link. ü Register as a new user with United. Healthcare. Online. com. ü Register with Electronic Data Interchange Support Services. Learn more at UHCCommunity. Plan. com > For Health Care Providers > Texas > Electronic Data Interchange (EDI). ü Apply for Electronic Payment & Statements. Go to My. Services. Optum. Health. Payment. Services. com > How to Enroll. ü Sign up for the monthly Network Bulletin at United. Healthcare. Online. com > Tools & Resources > News & Network Bulletin. ü Get to know your physician or provider advocate: • Physician Advocates – Call 888 -303 -6162 or email providerservicestx@uhc. com. • Provider Advocates for LTSS – Call 888 -787 -4107 or email uhc_cp_prov_relations@uhc. com. PCA-1 -001465 -03302016_05122016 34

Thank you!
 Uhc medication prior authorization form
Uhc medication prior authorization form United healthcare community plan delaware
United healthcare community plan delaware Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Group number on united healthcare card
Group number on united healthcare card United healthcare underwritten by golden rule
United healthcare underwritten by golden rule Lakeland care district
Lakeland care district Jim cronin united healthcare
Jim cronin united healthcare United healthcare simply engaged
United healthcare simply engaged Primary secondary and tertiary health care
Primary secondary and tertiary health care Navigating the body
Navigating the body Navigating the digital landscape
Navigating the digital landscape What is the purpose of liquid in the capsule of a compass?
What is the purpose of liquid in the capsule of a compass? Trigonometry used in navigation
Trigonometry used in navigation Gdpr compliance aws
Gdpr compliance aws Navigating the art world
Navigating the art world Aws iaa
Aws iaa Community provider business model
Community provider business model E commerce business models and concepts
E commerce business models and concepts Family care plan in community health nursing
Family care plan in community health nursing Community care plan of eastern carolina
Community care plan of eastern carolina Clearinghouse applicant initiated
Clearinghouse applicant initiated Lakeland care district
Lakeland care district Healthcare cisco smartnet total care support
Healthcare cisco smartnet total care support Plan together in community mobilization
Plan together in community mobilization Papu frankston
Papu frankston Veterans directed home and community based care
Veterans directed home and community based care Community medical care lebanon va
Community medical care lebanon va Community oriented primary care definition
Community oriented primary care definition Vd hcbs
Vd hcbs Central east community care access centre
Central east community care access centre Duty of care outcome care certificate
Duty of care outcome care certificate Magnetii au proprietatea de a atrage corpuri care contin
Magnetii au proprietatea de a atrage corpuri care contin Palliative care vs hospice care
Palliative care vs hospice care Animale care se inmultesc prin pui vii
Animale care se inmultesc prin pui vii Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate