Session 7 Key Concepts 1 Consent and refusal

- Slides: 45
Session 7 Key Concepts (1) Consent and refusal of treatment
Intended Outcomes n describe the requirements for a person’s valid consent or refusal of treatment n consider issues relating to elements of the consent process
Consent n Basic ethical principles n autonomy vs beneficence (paternalism) n self-determination vs best interests n Ethics and law n Schloendorff v Society of New York Hospital (1914) 105 NE 92 : classic legal statement: “Every human being of adult years and sound mind has right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent, commits an assault*. . . ” i. e. * battery
Consent n Function of consent n moral function n clinical function – foster patient’s trust, cooperation, confidence, etc. n legal function – provide justification for care; protect healthcare professionals from criminal/civil claims “It is trite law that in general a doctor is not entitled to treat a patient without the consent of someone who is authorised to give that consent. If he does so, he will be liable in damages for trespass to the person and may be guilty of a criminal assault. ” Lord Donaldson Re R (A Minor) (Wardship: Medical Treatment) (1991)
Consent: guidelines n General Medical Council (GMC) guidance n doctors should do their best to find out about patients’ individual needs and priorities when providing information about treatment options n if the patient asks specific questions about the procedure and associated risks these should be answered truthfully n an individual’s personal preferences should also be taken into account when identifying his or her needs in the provision of care.
Absence of consent: trespass to the person n to avoid trespass to the person healthcare professionals need to have a legal justification to avoid the risk of being sued for battery or assault (tort of battery; OAP Act 1861 s 18 s 20, criminal assault etc. ) n no battery where patient understands the broad nature of the treatment i. e. information threshold for battery very low n if valid consent has not been given, patient typically has an action in negligence Chatterton v Gerson [1981] QB 432 “ …once the patient is informed in broad terms of the nature of the procedure which is intended and gives her consent, the consent is real and the cause of the action on which to base a claim for failure to go into risks and implications is negligence, not trespass. ” Bristow J
Absence of consent: trespass to the person n advantages of action in battery: intentional tort – no need to prove physical injury or that had patient been adequately informed, s/he would have rejected the treatment Bristow J, "I think justice requires that in order to vitiate the reality of consent [in battery] there must be a greater failure of communication between doctor and patient than that involved in a breach of duty if the claim is based on negligence. When the claim is based on negligence the plaintiff must prove not only the breach of duty to inform but that had the duty not been broken she would not have chosen to have the operation. Where the claim is based on trespass to the person, once it is shown that the consent is unreal, then what the plaintiff would have decided if she had been given the information which would have prevented the vitiation of the reality of her consent is irrelevant".
Absence of consent: trespass to the person n Sidaway v Board of Governors of the Bethlem Royal Hospital [1984] 1 All ER 1018 “…it would be deplorable to base the law in medical cases of this kind on the torts of assault and battery. ” Lord Scarman n attempts to bring actions for battery claiming invalid consent to medical treatment rarely succeed – why? n limited case law explained by: n n tendency of claimants to pursue claim in negligence declaratory procedure in medical cases – declaration by High Court as to legality of proposed treatment (sought by healthcare professionals/organisations to protect themselves against subsequent litigation)
Absence of consent: trespass to the person n low information threshold means that action in battery only likely in situations such as: n no information at all n treatment against patient’s will n different treatment administered n consent obtained by fraud n n Appleton & Others v Garrett [1997] 8 Med LR 75 gross overtreatment of patients by a dental surgeon action in battery Bartley v Studd (1995) Medical Law Monitor 2(8) 1 removal of ovaries by surgeon when patient had consented to a hysterectomy constituted battery
Absence of consent: trespass to the person: information and negligence n sufficiency of information defined by the Bolam principle n Sidaway v Board of Governors of the Bethlem Royal Hospital [1984] 1 All ER 1018 n n doctor could withhold information on ground of ‘therapeutic privilege’ – if s/he considered information would be detrimental to health of the patient House of Lords rejected the argument that different tests should be applied to different aspects of doctor/patient care n n all but one Law Lord applied Bolam test – a doctor need only disclose such information as would be disclosed by a reasonable body of medical opinion Lord Scarman – thought ‘patient’s rights should be prime concern – ‘prudent-patient’ test Note also: Bolitho v City of Hackney HA [1997] AC 232 Pearce v United Bristol Healthcare NHS Trust [1999] P. I. Q. R 53
Sidaway v Bethlehem Royal Hospital Governors per Lord Diplock: “The only effect that mention of risks can have on the patient’s mind, if it has any at all can be in the direction of deterring the patient from undergoing the treatment which in the expert opinion of the doctor it is in the patient’s interest to undergo. To decide what risks the existence of which a patient should be voluntarily warned and the terms in which such warning, if any, should be given, having regard to the effect that the warning may have, is as much an exercise of professional skill and judgment as any other part of the doctor’s comprehensive duty of care to the individual patient, and expert medical evidence in this matter should be treated in just the same way. The Bolam test should be applied”. Sidaway v Bethlehem Royal Hospital Governors[1985] 1 AC 871 643 - applied Bolam v Friern Hospital Management Committee [1985] 1 WLR 582.
Absence of consent: trespass to the person: information and negligence n Pearce v United Bristol Healthcare NHS Trust [1999] P. I. Q. R 53 “…if there is a significant risk which would affect the judgement of a reasonable patient, then in the normal course, it is the responsibility of the doctor to inform the patient of that significant risk. . . ” Lord Woolf n what is a significant risk? n see also: n Australia (Rogers v Whitaker [1992] 175 CLR 479 n Canada (Reibl v Hughes [1980] 114 DLR (3 d) 1
Principle applied in Rogers v Whitaker “Except in the case of an emergency or where disclosure would prove damaging to the patient, a medical practitioner has a duty to warn the patient of a material risk inherent in proposed treatment. A risk is material if, in the circumstances of the particular case, a reasonable person in the patient’s position, if warned of the risk, would be likely to attach significance to it or if the medical practitioner is or should reasonably be aware that the particular patient, if warned of the risk, would be likely to attach significance to it. The fact that a body of reputable medical practitioners would have given the same advice as the medical practitioner gave does not preclude a finding of negligence. Generally speaking, whether the patient has been given all the relevant information to choose between undergoing and not undergoing the proposed treatment is not a question the answer to which depends upon medical standards or practice. ”
Summary so far n two main areas of law concerned with consent n battery n negligence n patient requires information about the nature of the treatment otherwise battery n patient requires information about risks common/serious side-effects; benefits; reasonable alternatives, etc. (moving towards ‘prudent patient’ standard) otherwise negligence n i. e. failure to inform amounts to negligence; may also amount to battery.
Absence of consent: trespass to the person: burden of proof n The tort of battery is ‘the unconsented to intrusion of another’s bodily integrity…[and] the burden of proving absence of consent is on the claimant. ” Mc. Cowen J Freeman v Home Office [1984] QB 524 – upheld by Court of Appeal
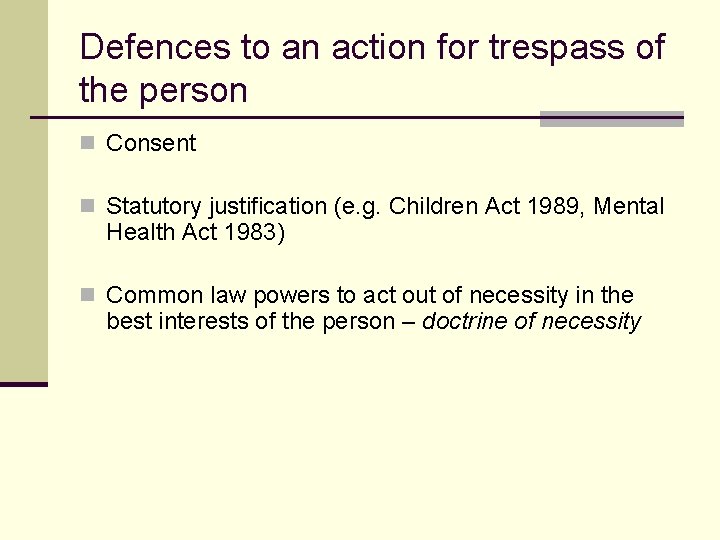
Defences to an action for trespass of the person n Consent n Statutory justification (e. g. Children Act 1989, Mental Health Act 1983) n Common law powers to act out of necessity in the best interests of the person – doctrine of necessity
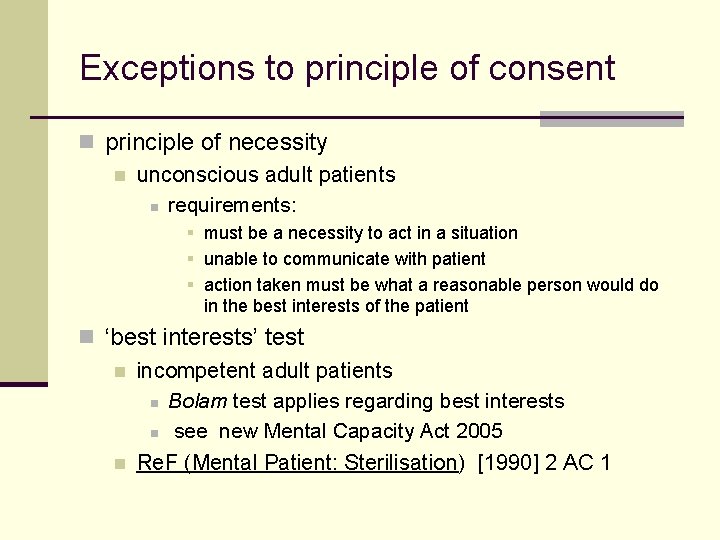
Exceptions to principle of consent n principle of necessity n unconscious adult patients n requirements: § must be a necessity to act in a situation § unable to communicate with patient § action taken must be what a reasonable person would do in the best interests of the patient n ‘best interests’ test n incompetent adult patients n Bolam test applies regarding best interests n see new Mental Capacity Act 2005 n Re. F (Mental Patient: Sterilisation) [1990] 2 AC 1
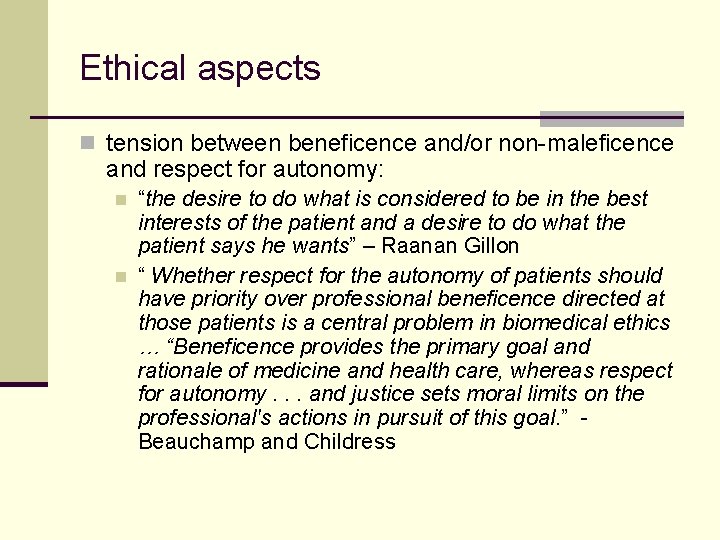
Ethical aspects n tension between beneficence and/or non-maleficence and respect for autonomy: n n “the desire to do what is considered to be in the best interests of the patient and a desire to do what the patient says he wants” – Raanan Gillon “ Whether respect for the autonomy of patients should have priority over professional beneficence directed at those patients is a central problem in biomedical ethics … “Beneficence provides the primary goal and rationale of medicine and health care, whereas respect for autonomy. . . and justice sets moral limits on the professional's actions in pursuit of this goal. ” Beauchamp and Childress
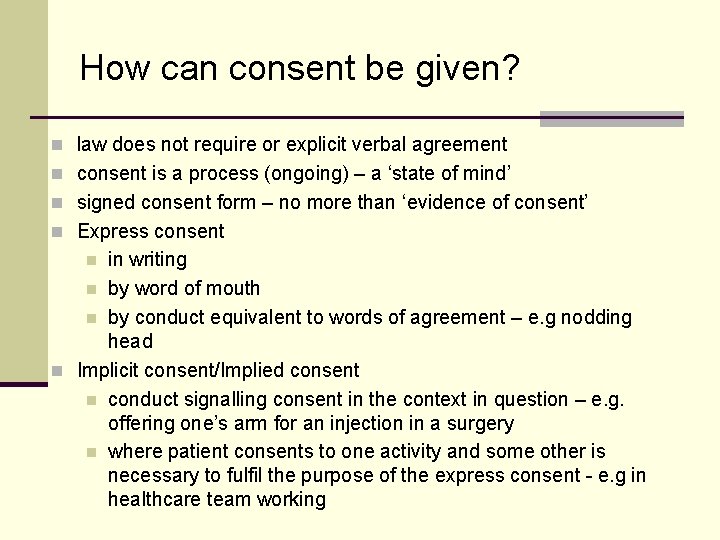
How can consent be given? n law does not require or explicit verbal agreement n consent is a process (ongoing) – a ‘state of mind’ n signed consent form – no more than ‘evidence of consent’ n Express consent in writing n by word of mouth n by conduct equivalent to words of agreement – e. g nodding head n Implicit consent/Implied consent n conduct signalling consent in the context in question – e. g. offering one’s arm for an injection in a surgery n where patient consents to one activity and some other is necessary to fulfil the purpose of the express consent - e. g in healthcare team working n
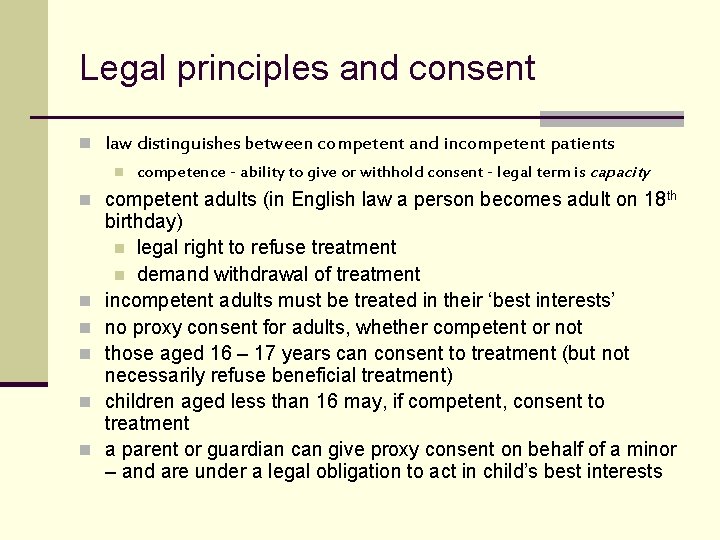
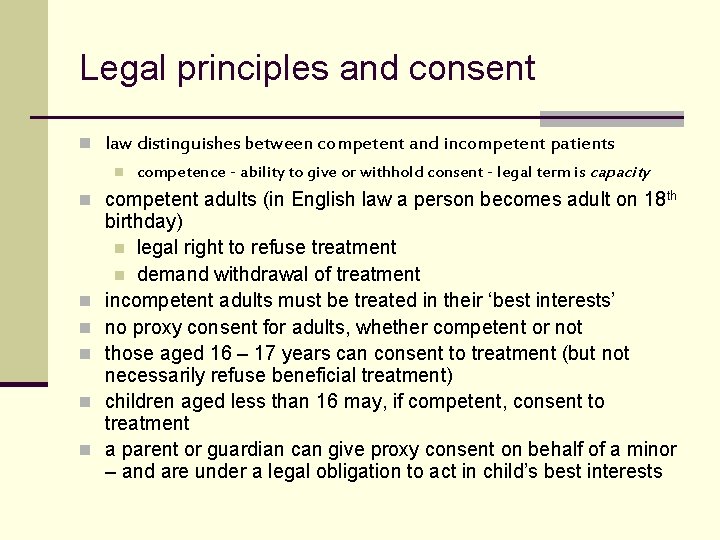
Legal principles and consent n law distinguishes between competent and incompetent patients n competence - ability to give or withhold consent - legal term is capacity n competent adults (in English law a person becomes adult on 18 th n n n birthday) n legal right to refuse treatment n demand withdrawal of treatment incompetent adults must be treated in their ‘best interests’ no proxy consent for adults, whether competent or not those aged 16 – 17 years can consent to treatment (but not necessarily refuse beneficial treatment) children aged less than 16 may, if competent, consent to treatment a parent or guardian can give proxy consent on behalf of a minor – and are under a legal obligation to act in child’s best interests
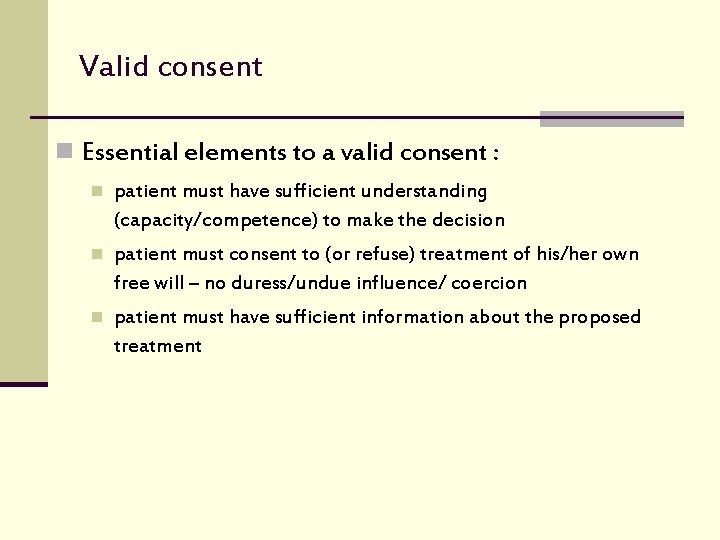
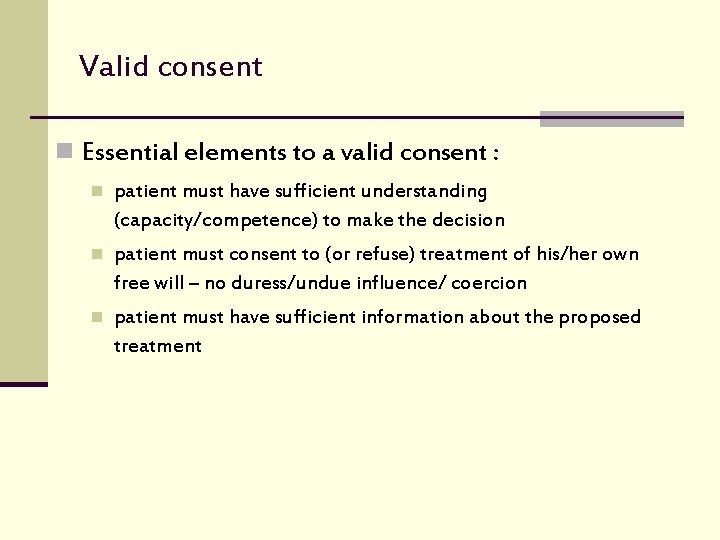
Valid consent n Essential elements to a valid consent : n patient must have sufficient understanding (capacity/competence) to make the decision n patient must consent to (or refuse) treatment of his/her own free will – no duress/undue influence/ coercion n patient must have sufficient information about the proposed treatment
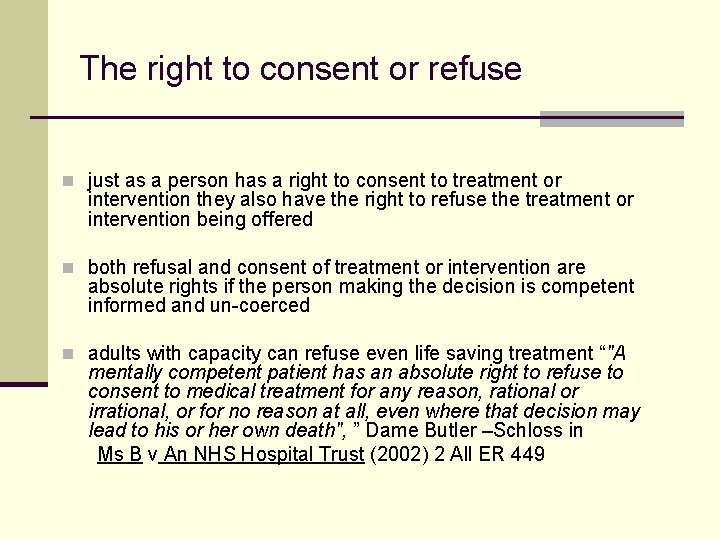
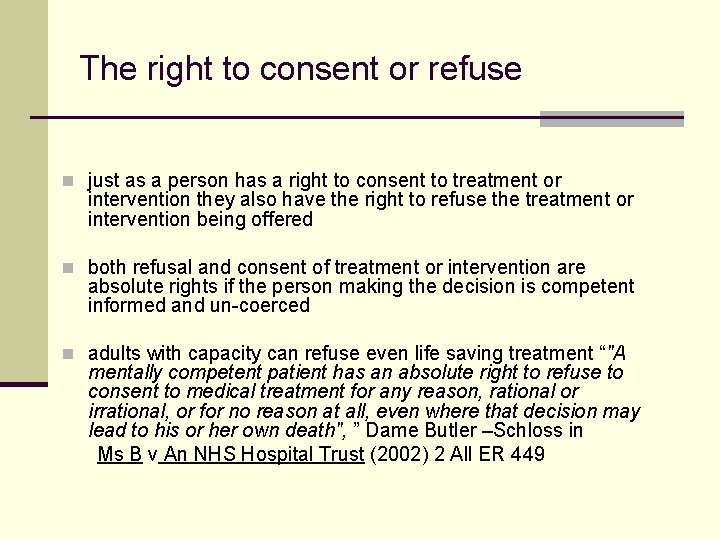
The right to consent or refuse n just as a person has a right to consent to treatment or intervention they also have the right to refuse the treatment or intervention being offered n both refusal and consent of treatment or intervention are absolute rights if the person making the decision is competent informed and un-coerced n adults with capacity can refuse even life saving treatment “"A mentally competent patient has an absolute right to refuse to consent to medical treatment for any reason, rational or irrational, or for no reason at all, even where that decision may lead to his or her own death", ” Dame Butler –Schloss in Ms B v An NHS Hospital Trust (2002) 2 All ER 449
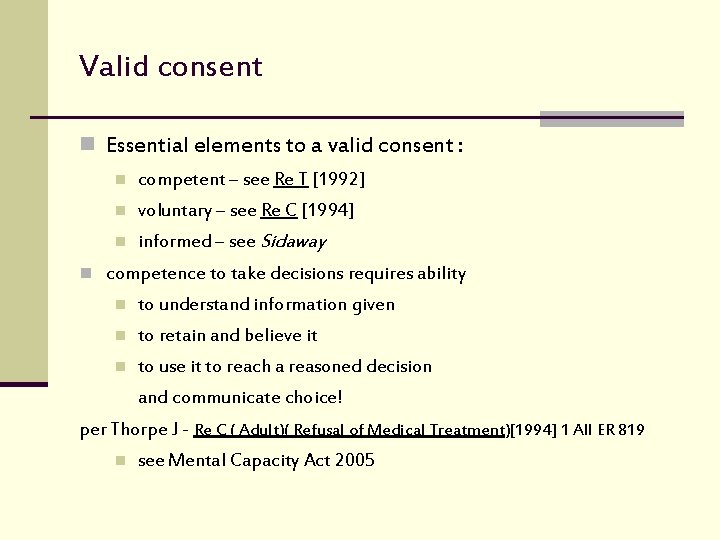
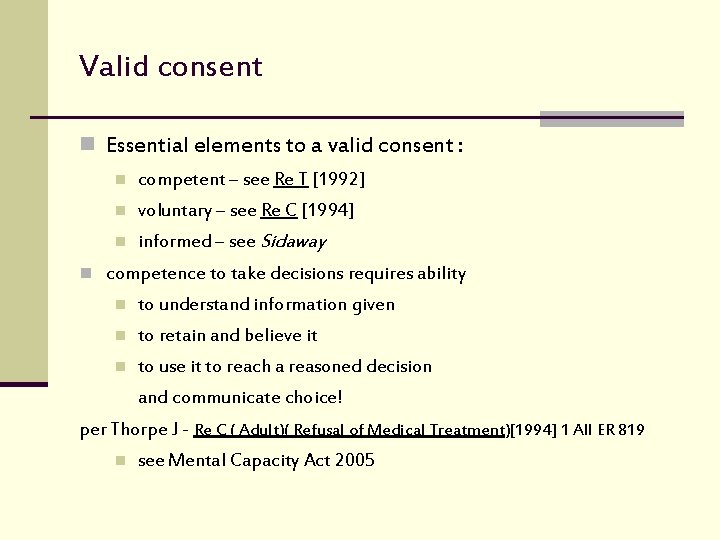
Valid consent n Essential elements to a valid consent : n competent – see Re T [1992] n voluntary – see Re C [1994] n informed – see Sidaway n competence to take decisions requires ability n to understand information given n to retain and believe it n to use it to reach a reasoned decision and communicate choice! per Thorpe J - Re C ( Adult)( Refusal of Medical Treatment)[1994] 1 All ER 819 n see Mental Capacity Act 2005
Valid consent n “For consent to be valid, it must be given voluntarily by an appropriately informed person (the patient or where relevant someone with parental responsibility for a patient under the age of 18*) who has the capacity to consent to the intervention in question. Acquiescence where the person does not know what the intervention entails is not “consent”. Do. H (2001) Reference Guide to Consent for Examination or Treatment * N. B. relevant issues for children and young people
Capacity or competence n ability to comprehend and retain information material to the decision and must be able to use this in the decision-making process n capacity should not be confused with a health professional’s assessment of the reasonableness of a patient’s decision
Capacity (cont) n need to differentiate between reasonableness and rationality n a patient who refuses an amputation for a gangrenous foot and is aware of the consequences of his refusal is making a competent decision based on his own value system n a patient who refuses help denying his foot is gangrenous when it is clearly obvious may not be able to comprehend and make use of the information and hence may lack capacity
Capacity (cont) n A person’s ability to understand may be temporarily affected: n confusion n panic n pain n medication n fatigue n N. B. does not mean they are incapable of consenting
Consent n requires communication of decision n do not underestimate the ability of a patient to communicate n need to take all reasonable steps to facilitate communication n interpreters n communication aids
What information do people need? n enough information in broad terms to make a balanced decision n information such as: n the benefits and the risks of the proposed treatment n in particular those that are ‘material’ or ‘significant’ risks n what the treatment will involve n what the implications of not having the treatment are n what alternatives may be available n the practical effects on their lives of having, or not having, the treatment n patients who ask direct questions? n “. . it is clear that if a patient asks a doctor about a risk, then the doctor is required to give an honest answer. ” Lord Woolf Pearce v United Bristol Healthcare NHS Trust [1999]
Consent n is the consent given voluntarily? n consider who or what may exert undue influence or pressure on the patient during the consenting process n coercion should be distinguished from providing the patient with appropriate reassurance or pointing out the potential benefits of treatment
Consent n different types of influence: n n n coercion: use of force or threats manipulation: non-coercive but uses non-rational methods to achieve control e. g. deliberately withholding information rational persuasion: use of reasons to influence Re T (Adult: refusal of treatment) [1992] 4 All ER 649
Consent and vulnerable groups n minors n mentally incapacitated n anorexics n person with learning disabilities n dementia n prisoners n research/teaching
Consent n Adults without capacity n no-one can give consent on behalf of adults who are not capable of giving consent themselves n unless a valid advance refusal of treatment is applicable to the situation, the law permits interventions to be made where necessary and no more than is reasonably required in the patient’s best interests until capacity has returned
Consent n What is best interests? n “to preserve the life, health or well-being” of a patient will be in their best interests n best interests goes beyond a patient’s best medical interests, to include much wider welfare considerations n not necessary for others to sign consent but strongly recommend good practice of documenting reasons for decision
Consent n Why are family members consulted? n not for consent n to gain insight into a patient’s previous competent beliefs and values n to determine possible preferences of patient n good practice
Consent by 16 and 17 year old The Family Law Reform Act 1969 (section 8) n the consent of a minor who has attained the age of 16 years to any surgical, medical or dental treatment which, in the absence of consent, would constitute a trespass to his person shall be as effective as it would be if he were of full age: and where a minor has by virtue of this section given an effective consent it shall not be necessary to obtain any consent from his parent or guardian n See Mental Capacity Act 2005
Refusal by 16 and 17 year old n the refusal of a 16 or 17 year old patient may in certain circumstances be over-ridden either by someone with parental responsibility or by a court n the principle of best interests must be considered n no definitive guidance exists but it has been suggested that over-ruling the decision of a competent young person’s refusal should be restricted to situations where they are at risk of suffering “grave and irreversible mental or physical harm”
Children under the age of 16 n Gillick v West Norfolk and Wisbech AHA [1986] AC 112: subsequnetly courts have held that children who have sufficient understanding and intelligence to enable them to understand fully what is involved in a proposed intervention will also have the capacity to consent to that intervention. n so-called ‘Gillick’ (or Fraser ) Competence’ will be affected by maturity of child, experience and the health care circumstances n
Child or young person without capacity n Who has parental responsibility under the Children Act 1989? n a mother has automatic parental responsibility for her child n where both parents were married at the time of the child’s birth both parents have parental responsibility n where more than one person has parental responsibility each of them may act alone, this means that consent for treatment is only required from one parent n after divorce, both parents retain parental responsibility for their child in equal measures n a person with a residence order
Parental responsibility under the Adoption and Children Act 2002 n parental responsibility was broadened for any child born after n n 31. 12. 2003 unmarried fathers who register the birth with the mother now have parental responsibility for the child English law is not retrospective children born under the 1989 regulations can be re-registered if the mother and father both request it this gives parental responsibility to both parents
Children: Consent by Others n Consent treated differently to refusal n parents, guardian or court able to over-rule refusal by a ‘Gillick competent’ adolescent to receive treatment which is in her best interests n Re R (A minor) (1992); Re W (A Minor) (Medical Treatment: Court’s Jurisdiction) (1992) n ‘Gillick competence’ depends on seriousness of the decision taken as well as cognitive powers and maturity n Re L(Medical Treatment: Gillick Competence) (1998) n Courts adopt paternalistic approach when adolescents are afflicted with life-threatening situations n Re M (Medical Treatment: Consent) (1999) 2 FLR 1027; Re E (A Minor) (Wardship: Medical Treatment) (1993)
Children: Consent by Others n Rationale for distinguishing between consent and refusal n consent – accepting greater knowledge of medical profession n refusal – decision asks more of the child n Courts reluctant to empower children to refuse treatment against medical opinion; best interest test applied Hierachy for decisions: Court ↓ Parent ↓ Child
Conclusions n a person has a right to consent to or refuse treatment n law assumes adults to be competent unless proved otherwise n legally no one is able to give or refuse consent on behalf of another adult i. e. over 18 (not even the courts) This applies to adults with or without capacity! n healthcare professionals must respect a valid decision n 3 requirements for valid decision n each requirement needs careful consideration because of the individual circumstances and situation of the person receiving care and the knowledge and skills of the healthcare professional n consent/refusal is not a one off decision n capacity can fluctuate n a patient’s capacity may be temporarily affected by factors such as confusion, shock, pain, etc. n capacity should not be confused with unreasonable, eccentric or unwise decisions, nevertheless, irrationality may be evidence of incompetence n need to document adequately discussions around consent and risks etc