Refusal of Consent and Capacity in Healthcare Conference
- Slides: 25
Refusal of Consent and Capacity in Healthcare Conference 2 December 2015 MICHAELA HERRON
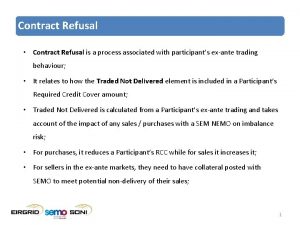
OVERVIEW • Capacity; • Refusing consent to treatment: Ø Patients with Capacity ØPatients with no/doubtful capacity Ø Pregnant patients with capacity (risk to the unborn) • Advanced Care Directives; • Doctrine of Necessity; • Court Applications. 1
FIRST QUESTIONS • How old is the patient? • Does the patient have capacity? • Is the patient’s refusal voluntary? • Is the patient’s refusal informed? 2 2
Refusing Treatment – Competent Patient • “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without his patient’s consent commits an assault for which he is liable in damages” – Schloendorff -v- Society of New York Hospital; • Every adult has the right to decide whether or not he will accept medical treatment, even if the refusal may risk permanent injury to his health and even lead to premature death, and whether the reasons for refusal are rational or irrational, unknown or even non-existent. Re T(adult: refusal of treatment); • The refusal of the conscious and competent patient must always be respected; • Hospital Policy. 3 3
Assessing Capacity • Presumption of capacity – rebuttable; • Matter of clinical judgement – psychiatrist or clinical psychologist? • Three stage test – Judge Laffoy in the K case; The patient does not have capacity if: 4 a) They have not comprehended and retained the treatment information and have not assimilated the information as to the consequences likely to ensue from not accepting the treatment b) They have not believed the treatment information; and c) They have not weighed the treatment information in the balance in arriving at a decision 4
Assessing Capacity • Misunderstanding/Misperception of treatment information -V- an irrational decision or decision made for irrational reasons. The former is linked to the assessment of capacity; • The assessment of capacity must have regard to the gravity of the decision. “A patient’s capacity must be commensurate with the gravity of the decision…. the more serious a decision, the greater the capacity required”. Re T; • Importance of individual consultation: Many factors can temporarily deprive a patient of capacity (e. g. confusion, fatigue, shock, pain or medication) but the mere presence of these does not imply a lack of capacity. 5 5
Refusal: Informed • Never assume the extent of a patient’s awareness of risks. Always discuss, in considerable detail, the risks pertinent to the patient’s condition and those specific to non-treatment including a discussion of the relative efficacy of alternative treatments: ØClear and non-judgmental explanation of risks ØDeath or catastrophic irreversible injury (to patient/baby) ØChoice of language • What is the basis for refusal? • What is the scope of that refusal? 6 6
Refusal: Voluntary • Voluntary – a valid treatment decision must be voluntary and must be free of undue influence, coercion or duress. • Importance of individual consultations with patient • Involvement of patient services/support/social worker • Second opinion/Senior Medical Practitioners • You must be satisfied that the treatment decision is the patient’s own choice. If not: i. Legal Advice ii. Court Application 7
Refusal: Voluntary • Re T (Adult: Refusal of Medical Treatment). 4 In this case a pregnant woman had been involved in a motor accident and was admitted to hospital after complaining of chest and shoulder pains. • The patient had indicated on several occasions that she did not want a blood transfusion and signed a form of refusal. • These refusals were alleged to have arisen in response to the influence of her mother, who was a practising Jehovah's Witness and present at times immediately before the patient had refused blood. The patient was not of that faith. • After giving birth to a stillborn child the patient's condition worsened and she became unconscious. Her father and boyfriend sought judicial approval for the administration of blood products, and blood transfusions were authorized at trial on the basis that there was no binding refusal and that blood could be provided in her best interests. 8
Refusal: Voluntary • Court of Appeal found that her refusals were invalid because of incapacity and also because they did not cover the extreme situation that had arisen. Additionally they would have been invalidated because of the undue influence of the mother. Lord Donaldson: “…But the doctors have to consider whether the decision is really that of the patient. . . The real question in each such case is, does the patient really mean what he says or is he merely saying it for a quiet life, to satisfy someone else or because the advice and persuasion to which he has been subjected is such that he can no longer think and decide for himself? In other words, is it a decision expressed in form only, not in reality? ” 9
Refusal: Voluntary Lord Donaldson held there were two main considerations in circumstances of suspected undue influence: 10 1. The strength of will of the patient. If the patient is in pain, depressed or tired or being treated with drugs, he or she is less likely to resist the influence of others. 2. The patient's relationship with the persuading party. A close family relationship heightens concern, especially in cases where religious beliefs are the reason for refusing treatment. The stronger the relationship the greater the ability of the persuader to override the decision-making process of the patient
Refusal: Consultation Process • Use of psychiatrist/psychologist where there any questions as to the patient’s capacity; • More than 1 consultation; • The first consultation should be with the patient only, if the patient requests, subsequent discussions may be held with family members/members of hospital liaison committees only if their presence is not detrimental to the patient’s peace of mind; • Involvement of Senior Practitioners; • Multi-Disciplinary Approach. 11 11
Refusal – Documenting the Process • Details of all individual consultations recorded and signed by all the parties involved; • Consent form; use of a detailed consent form includes details of at least the following information: a) Patient’s condition b) Risks of the procedure and of non-treatment c) Alternatives/Acceptable products/surgical techniques (e. g. while a blood transfusion may be refused, certain fractions such as haemoglobin based oxygen carriers and clotting factors may be acceptable) d) Declaration by the patient that these issues have been explained and that they are aware of the consequences. Beware of templates • 12 Agree and document a detailed care plan with the patient. 12
Refusal – Medical/Nursing Teams • May conflict with a clinician’s medical and ethical responsibility for preserving life; • In an elective/non-urgent situation, every member of the multi-disciplinary team is entitled to, and must decide whether they are willing to accept these limitations. If not, appropriate referral should be made; • This option may not be available in emergency situations. Obligation to treat patient appropriately (including withholding of treatment); • Hospital/systems issue as well as an individual issue – regular updated list of healthcare staff who are prepared to act should be kept. 13 13
Refusal of Consent by Pregnant Patient with Capacity • Conflict of rights – application of Article 40. 3. 3 of the Constitution. • Legal uncertainty; • Key Question: Will refusal create a risk for the unborn? • Relevant factors to be considered in this context may include whether the risk to life of the unborn is established with a reasonable degree of medical certainty, and whether the imposition of treatment would place a disproportionate burden or risk of harm on the pregnant woman. (HSE National Consent Policy) • Identify early/inform/discuss/involve senior practitioners • Legal Advice/High Court application. 14 14
Refusal – Adults - Doubtful or No Capacity • Can anyone consent on their behalf and over-ride their refusal/consent? No • “No other person such as a family member, friend or carer and no organisation can give or refuse consent on behalf of an adult service user who lacks capacity to consent unless they have specific legal authority to do so”; National Consent Policy • Persisting doubt as to capacity – High Court application and Doctrine of Necessity; • Where no capacity: ØAdvanced Care Directives ØDoctrine of Necessity ØHigh Court application 15 15
Advanced Directives • An advance expression of wishes by a person, at the time they have capacity, about certain treatment that might arise at a future time when they no longer have the capacity to express their wishes; • Is it valid? ØExistence of and the fact that a patient is carrying an ACD is powerful evidence of intention; should be respected unless there is some reason to suppose that the patient has changed their views since the directive was executed (Association of Anaesthetists of Great Britain & Ireland Guidelines) ØAge/capacity/voluntary/informed ØClear and unambiguous and must represent the will of the patient ØPractitioner must make enquiries 16 16
Elective Procedures • Increased time to engage in a comprehensive consent process brings with it an increased onus to do so; • Meet with the patient well ahead of time; • Agree a detailed care plan with the patient; • Arrange for any prophylactic measures to be instituted (e. g. haemoglobin optimisation). 17 17
When may a Court Application be appropriate? • Refusal by patient with doubtful capacity • Refusal by patient who lacks capacity; • Pregnant woman refusing treatment creating a substantial risk to the unborn; 18 18
Applying to Court - Timetables • Medical procedure/treatment will dictate timing; • Hospital Policy - including access to legal team (out of hours provision) and liaison with Risk Department & Master; • Early engagement of legal team; • Second opinion/multidisciplinary involvement – preparation of medical reports; • Arrangements to safeguard the patient’s rights: a) Notice b) Legal representation c) Service/short service d) Interpreter 19 19
Court Application Procedure Legal papers • • • Notice of Motion; Grounding Affidavits – who? Medical Reports exhibited; Summons; Service on Patient; Affidavit of Service. Hearing • Oral evidence (treating doctors and patient/patient’s behalf); • Order granted or denied; • Appeal. 20 20
What if There is no Time? • In cases of extreme urgency – ØInvolvement of senior clinical decision maker ØSecond opinion/Multi-Disciplinary ØTreat in accordance with Doctrine of Necessity ØCommence court application if practicable ØBeware of the creation of necessity by delay or avoidance of court/legal advice at an earlier stage 21 21
Doctrine of Necessity • Definition – where consent cannot be obtained, doctors should provide treatment which is in the patient’s best interests and is immediately necessary to save life or avoid significant deterioration in health; • Limits; e. g. Life saving blood transfusion v elective procedure in patient’s best interests • Defence to claim of trespass versus optimal care; • Response must be proportionate. • Necessity created by practitioners by avoidance of court. 22 22
Take Homes • Refusals/capacity; • Respect refusal of adult with the capacity; • Refusal and doubt as to/ or no capacity: court; • Refusal of pregnant woman where refusal is likely to endanger the unborn – legal advice/court; • Doctrine of Necessity; • Beware of timeframes; • Hospital Policy required to govern these situations. 23 23
1, 500 1 st 300 40 Lawyers and fee earners worldwide Law Firm of the Year Legal Business Awards 2011 Partners worldwide Offices across Europe, Americas, Middle East, Africa and Asia. Clyde & Co LLP accepts no responsibility for loss occasioned to any person acting or refraining from acting as a result of material contained in this summary. No part of this summary may be used, reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, reading or otherwise without the prior permission of Clyde & Co LLP. © Clyde & Co LLP 2015
 Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine meaning
Sports medicine meaning Production units have an optimal rate of output where
Production units have an optimal rate of output where Cit healthcare conference 2017
Cit healthcare conference 2017 22power dot com
22power dot com Consent and the law
Consent and the law Ey2 declaration and consent form
Ey2 declaration and consent form Peek vs gurney
Peek vs gurney Chapter 8 lesson 2 peer pressure and refusal skills
Chapter 8 lesson 2 peer pressure and refusal skills How might a friend help you resist negative peer pressure
How might a friend help you resist negative peer pressure Chapter 8 lesson 2 peer pressure and refusal skills
Chapter 8 lesson 2 peer pressure and refusal skills Using refusal skills
Using refusal skills Coping cat fear ladder
Coping cat fear ladder Wcu irb
Wcu irb Types of consent
Types of consent What is positive intervention consent
What is positive intervention consent Types of concent
Types of concent A lack of voluntary consent:
A lack of voluntary consent: Age of consent kentucky
Age of consent kentucky Age of consent state by state
Age of consent state by state Genuine consent
Genuine consent Dfps medical consent training
Dfps medical consent training Unsur informed consent
Unsur informed consent Authentic consent
Authentic consent Usps informed consent
Usps informed consent Ethical principles governing informed consent process
Ethical principles governing informed consent process