Consent Capacity In Healthcare Conference Rules Governing Consent



![Constitutional Principle • In Re a Ward of Court [1996] 2 IR 79. This Constitutional Principle • In Re a Ward of Court [1996] 2 IR 79. This](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-44.jpg)
![Constitutional Principle In Fitzpatrick & Anor v K. & Anor [2008] IEHC 104, The Constitutional Principle In Fitzpatrick & Anor v K. & Anor [2008] IEHC 104, The](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-51.jpg)

![Tort of Battery v Assault In the case of Reibl v Hughes [1980] 114 Tort of Battery v Assault In the case of Reibl v Hughes [1980] 114](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-72.jpg)
![Assault v Negligence • Assault v Negligence - Chatterton v Gerson [1981] QB 432. Assault v Negligence • Assault v Negligence - Chatterton v Gerson [1981] QB 432.](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-76.jpg)
![Information • Bolam v Friern Hospital Management Committee [1957] HL 1 WLR 583. Although Information • Bolam v Friern Hospital Management Committee [1957] HL 1 WLR 583. Although](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-80.jpg)



![The Professional Standard v The Reasonable Patient Approach • Geoghegan v Harris[2000] IR 536. The Professional Standard v The Reasonable Patient Approach • Geoghegan v Harris[2000] IR 536.](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-90.jpg)
![Causation in Informed Consent • Chester v Afshar [2005] 3 WLR 927 House of Causation in Informed Consent • Chester v Afshar [2005] 3 WLR 927 House of](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-96.jpg)
![Recent Case on Informed Consent Montgomery v Lanarkshire Health Board [2015] UKSC 11. A Recent Case on Informed Consent Montgomery v Lanarkshire Health Board [2015] UKSC 11. A](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-99.jpg)


- Slides: 116
Consent & Capacity In Healthcare Conference Rules Governing Consent Clarified Wednesday, 2 nd December 2015 By Ms. Pat Daly, Solicitor
RULES GOVERNING CONSENT CLARIFIED TOPICS COVERED: • • • Informed consent definition Purpose of the law of consent Protecting ethical principles Right to self determination The range of ethical concepts used to justify informed consent – self-determination – dignity Provision of information Information the patient should be given in the consent process Implied & express consent Lunacy Regulations (Ireland) Act 1871
Consent
The Legal Doctrine of Consent Informed consent is a legal doctrine which is underpinned by the ethical principle of respect for individual autonomy. It has been firmly established internationally that every competent adult has the right of self-determination to decide to consent or refuse any medical treatment, even if such refusal could lead to death.

The Legal Doctrine of Consent • However, autonomy is a rebuttable right, which can be overridden under certain conditions. • When an individual’s right to determine what can be done to his or her own body during medical treatment is challenged, that has a has given rise to a number of legal challenges. There are national statues and there has evolved a doctrine of informed consent consisting of the following: -
The Legal Doctrine of Consent • The Ethical and Professional Principle • The Constitutional Principle • The Legislative Principle • The Tort of Battery • Case Law Consent has become a major evolving medico-legal issue because of a shift, within the Doctor/patient relationship, towards more autonomy for the patient and less paternalism from the Doctor.
The Ethical and Professional Principle Hippocratic Oath • Scholars trace the origins of medicine back to ancient Greece, to Hippocrates, the “Father of Medicine”.
FIRST DO NO HARM
Paternalism Traditional medical ethics were based on the Hippocratic oath. This obliged the Doctor to use his/her skills to the best of their ability to abstain from harming the patient. The obligations did not require a Doctor to consult with or seek permission from the patient for any medical intervention.

Paternalism The relationship that evolved was as follows: As the Doctor had more knowledge about the patient’s condition, he/she would do what was best for the patient and the patient did not need to be informed.
Demise of Paternalism Recommended Reading: “Doctors and Their Patients” by Edward Shorter, Professor of the History of Medicine, Professor of Psychiatry University of Toronto.
Demise of Paternalism Page 171 states as follows: - “the typical patient was willing to tolerate, indeed expected, a kind of medical tyranny that today would produce shocked exposé in the press”
Demise of Paternalism • The Ethical and Professional Principle of Patient Autonomy in Law. Schloendorff v Society of New York Hospital [1914] 211 NY 125. Justice Cardozo in his Judgement stated: “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an Operation without the Patient’s Consent commits an Assault. ”
Demise of Paternalism • In the 1960’s, attitudes began to change and questions began to be raised about whether the Doctor was in a better position to make health care decisions for the patient. This coincided with challenges to traditional authority, civil rights movement, feminism. & • Concerns about certain medical practices - The Tuskegee Syphilis Study - United States Public Health Service (USPHS) began in 1932 by was halted in 1972.
Demise of Paternalism • In 1972, the National Research Act was signed into law in the US. • Creation of National Commission for the Protection of Human Subjects of Biomedical Behavioural Research. Its remit was to identify basic ethical principles in research and ensure that research was conducted in accordance with those principles.
Demise of Paternalism The Belmont Report was published in 1979 and the following principles were identified : 1. Respect for the person – incorporates at least two ethical convictions. Firstly, that individuals should be treated as autonomous agents, and second, that the person with diminished autonomy are entitled to protection.
Demise of Paternalism 2. Beneficence – Persons are treated in an ethical manner not only by respecting their decisions and protecting them from harm, but also by making efforts to secure their wellbeing. It imposes the following obligations: a) Do no harm b) Maximise possible benefits and minimise possible harms.
Demise of Paternalism 3. benefits of research and bear its burdens? The concentration camps experiments and the Tuskegee syphilis study demonstrated that the concepts of justice were relevant. Therefore, the selection of subjects needs to be scrutinised.
Demise of Paternalism Beauchamp and Childress’ 1979 - Four Principles: 1. Respect for autonomy: respecting the decision making capacities of autonomous persons; enabling individuals to make reasoned informed choices. Beneficence: considers ncing the 2. this benefits of treatment against the risks and costs; the healthcare professional should act in a way that benefits the patient
Demise of Paternalism 3. Non maleficence: avoiding the causation of harm; the healthcare professional should not harm the patient. All treatment involves some harm, even if minimal, but the harm should not be disproportionate to the benefits of treatment. 4. Justice: distributing benefits, risks and costs fairly; the notion that patients in similar positions should be treated in a similar manner.

Informed Consent The application of the general principles to the conduct of research led to consideration of the following requirements: - 1. 2. 3. Informed Consent Risk/benefit assessment The selection of subjects
Informed Consent The Belmont Report also stated as follows in respect of Informed Consent – “Respect for persons requires that subjects, to the degree that they are capable, be given the opportunity to choose what shall or shall not happen to them. This opportunity is provided when adequate standards for informed consent are satisfied”
Informed Consent What does Informed Consent actually mean? Controversy still prevails over the nature and extent of informed consent. However, there is widespread agreement that the consent process can be analysed as containing three elements: -
Consent Deconstructed
Consent Deconstructed • Information – sufficient information has to be given. The manner and context is as important as the information. • Voluntariness – consent is valid only if voluntarily given. • Competence – In order for the patient's consent to be valid, he /she must be considered competent.
Consent Deconstructed • Of the above, autotomy appears to have dominance and is central to the healthcare decision making.
The Ethical and Professional Principle Medical Practitioners are assisted Professional body, the Medical Council. by their “GUIDE TO PROFESSIONAL CONDUCT AND ETHICS FOR REGISTERED MEDICAL PRACTITIONERS ( 7 th Edition 2009)” Section D - Consent to Medical Treatment:
The Ethical and Professional Principle • 33 General Principles - 33. 1 states as follows: “You should ensure that informed consent has been given by a patient before medical treatment is carried out. The ethical and legal rational behind this is to respect the patient’s autonomy and their right to control their own life. The basic idea of personal autonomy is that everyone’s actions and decisions are their own. Therefore, the patient has the right to decide what happens to their own body”.
The Ethical and Professional Principle • 35. 1 states as follows: “Consent given by the patient is the exercise of a voluntary choice; it is the giving of permission for the intervention to be carried out by competent professionals, where possible in an appropriate environment. You should explain the process in such a way as to ensure that patients do not feel that their consent is simply a formality or a signature on a page”
The Ethical and Professional Principle • 35. 2 states as follows: “As part of the informed consent process, patients must receive sufficient information, in a way that they can understand, to enable them to exercise their right to make informed decisions about their care. This refers to the disclosure of all significant risks or substantial risks of grave adverse consequences. ”
The Ethical and Professional Principle • 36. 1 states as follows: “Effective communication is the key to achieving informed consent. You should take appropriate steps to find out what patients want to know about their condition and what they ought to know about their condition, its investigation and treatment. ”
The Ethical and Professional Principle • 36. 2 states as follows: “The amount of information given to individual patients will vary according to factors such as the nature of the condition, the mode of investigation, the complexity of the treatment, the risk associated with the procedure and the patient’s own wishes. For example, patients may need more information to make an informed decision about a procedure that carries a high risk of failure or adverse side effects or about an investigation for a condition that, if found to be present, could have serious consequences for the patient’s employment, social or personal life”
The Ethical and Professional Principle Appendix A sets out the following: - • The information that patients want or should know, before deciding whether to consent to treatment or an investigation, may include. • Details of the diagnosis, and prognosis, and the likely prognosis if the condition is left untreated;
The Ethical and Professional Principle • uncertainties about the diagnosis, including options for further investigations before treatment. • options for treatment or management of the condition, including the option not to treat; • the purpose of a proposed investigation or treatment.
The Ethical and Professional Principle • details of the procedure or therapies involved, including methods of pain relief. • preparation for the procedure and what the patient might experience during or after the procedure, including common and serious side effects.
The Ethical and Professional Principle • For each option, explanations of the likely benefits and probabilities of success and discussion of any serious or frequently occurring risk and any lifestyle changes which may be caused or required by the treatment. • advice about whether a proposed treatment is experimental.
The Ethical and Professional Principle • Information about how and when the patient’s condition and any side effects will be monitored or re-assessed; • the name of the Doctor who will have overall responsibility for the treatment and, where appropriate, names of the senior members of their team.
The Ethical and Professional Principle • whether Doctors in training will be involved • the extent to which students may be involved in an investigation or treatment. • a reminder that patients can change their minds about a decision at any time.
The Ethical and Professional Principle • a reminder that patients have a right to seek a second opinion. • where applicable, details of costs or changes which the patient may have to meet.
The Demise of Paternalism • In reality, despite the above ethical and professional principles, paternalism still prevails within hospital settings. This is due, in part, to the hierarchical regimes. Time pressures have also been quoted as being a factor. In reality, practitioners are trained to make decisions for patients, and they put that in the form of advice. By and large, the emphasis is on giving advice rather than there being a discussion.
Constitutional Principle • The Constitutional Principle Autonomy and bodily integrity. of Personal Article 40. 3. 1 states as follows: “The State guarantees in its laws to respect, and as far as is reasonably practicable, by its laws to defend and vindicate the personal rights of the Irish Citizen”.
Constitutional Principle Article 40. 3. 2 states as follows: “The State is obliged to by its laws to protect as best it may from unjust attack and, in the case of injustice done, vindicate the life, person, good name and property rights of every citizen”.
Constitutional Principle There are Supreme Court decisions on consent apply the following: -
![Constitutional Principle In Re a Ward of Court 1996 2 IR 79 This Constitutional Principle • In Re a Ward of Court [1996] 2 IR 79. This](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-44.jpg)
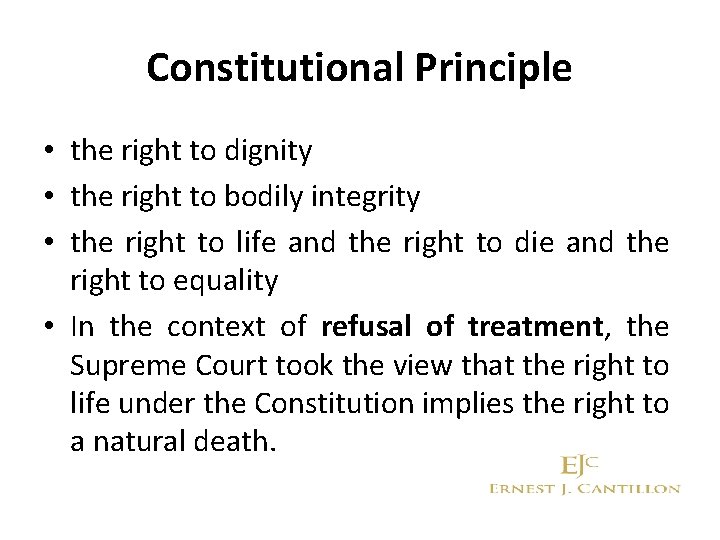
Constitutional Principle • In Re a Ward of Court [1996] 2 IR 79. This case is interesting in that court looked at the issue of capacity to consent where the lady did not have capacity. The patient was a 45 year old woman who had suffered irreversible brain damage as a result of cardiac arrest. She was described as being in an almost persistent vegetative state.
Constitutional Principle In reaching its decision in favour of removing the feeding tube, the Supreme Court regarded as relevant a number of rights protected under the Irish Constitution. These included: - • the right to autonomy or self-determination • the right to privacy
Constitutional Principle • the right to dignity • the right to bodily integrity • the right to life and the right to die and the right to equality • In the context of refusal of treatment, the Supreme Court took the view that the right to life under the Constitution implies the right to a natural death.
Constitutional Principle The Court held that although the woman lacked decision-making capacity, this did not diminish her rights. To distinguish between people with capacity and people without capacity would be ‘invidious’.
Constitutional Principle Hamilton CJ stated : “As the process of dying is part, and an ultimate inevitable consequence, of life, the right to life necessarily implies the right to have nature take its course and to die a natural death and, unless the individual concerned so wishes, not to have life artificially maintained by the provision of nourishment by abnormal artificial means, which have no curative effect and which are intended merely to prolong life. ”
Constitutional Principle The Court stated that this principle does not give a right to accelerate death or to terminate one’s own life; it is confined to a natural death. Of significance - the loss of competence does not result in the loss of one’s constitutional rights.
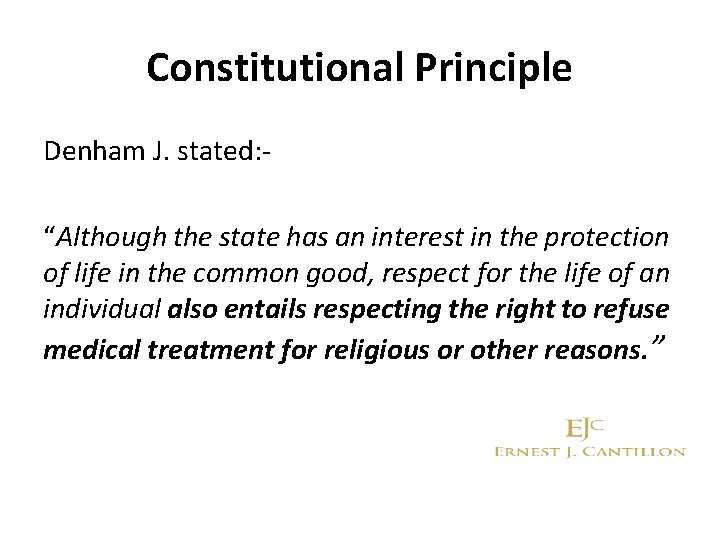
Constitutional Principle Denham J. stated: “Although the state has an interest in the protection of life in the common good, respect for the life of an individual also entails respecting the right to refuse medical treatment for religious or other reasons. ”
![Constitutional Principle In Fitzpatrick Anor v K Anor 2008 IEHC 104 The Constitutional Principle In Fitzpatrick & Anor v K. & Anor [2008] IEHC 104, The](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-51.jpg)
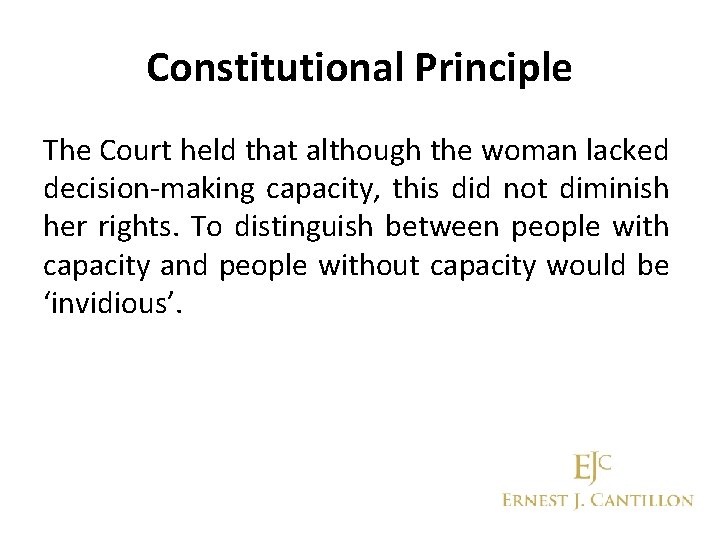
Constitutional Principle In Fitzpatrick & Anor v K. & Anor [2008] IEHC 104, The High Court looked at the issue of capacity to consent. This case is interesting in that the Court was asked to decide whether and, if so, in what circumstances a Court may intervene in the case of an adult patient who has capacity but refused medical treatment.
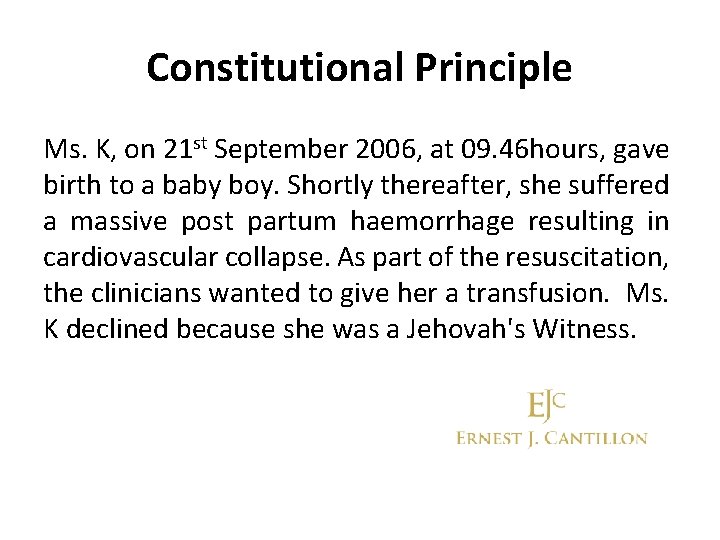
Constitutional Principle Ms. K, on 21 st September 2006, at 09. 46 hours, gave birth to a baby boy. Shortly thereafter, she suffered a massive post partum haemorrhage resulting in cardiovascular collapse. As part of the resuscitation, the clinicians wanted to give her a transfusion. Ms. K declined because she was a Jehovah's Witness.

Constitutional Principle The Master of the Hospital Chris Fitzpatrick, was called for and arrived at about 11. 30 hours. Ms. K was stable and conscious. She reiterated her refusal to accept a blood transfusion. The Master had doubts as to the quality of her refusal, that is to say, whether it was a valid refusal. • At 12. 00 hours, he contacted the Hospital's Solicitors for legal advice. • At 12. 30 hours, he left the Hospital for the Four Courts
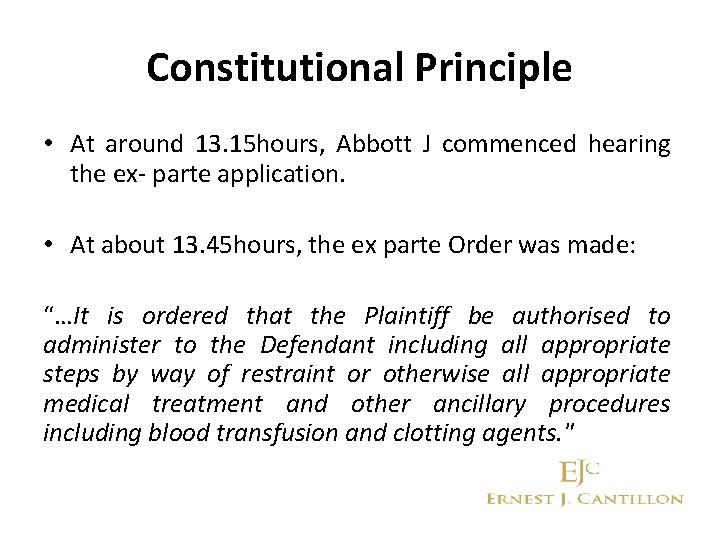
Constitutional Principle • At around 13. 15 hours, Abbott J commenced hearing the ex- parte application. • At about 13. 45 hours, the ex parte Order was made: “…It is ordered that the Plaintiff be authorised to administer to the Defendant including all appropriate steps by way of restraint or otherwise all appropriate medical treatment and other ancillary procedures including blood transfusion and clotting agents. "
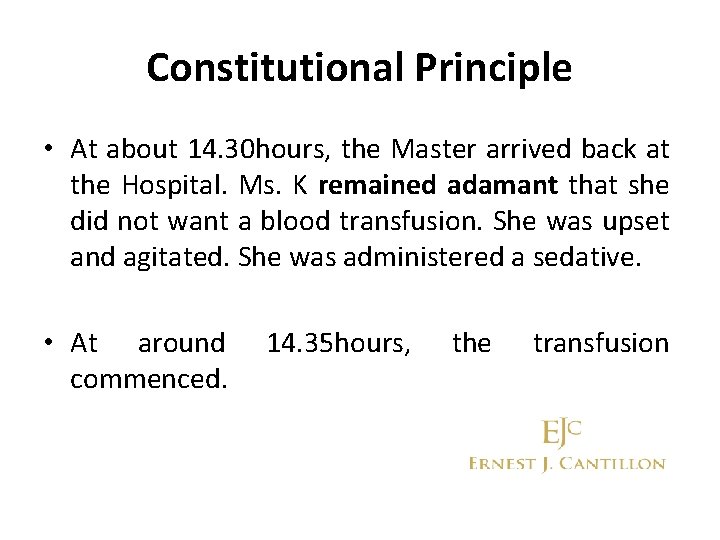
Constitutional Principle • At about 14. 30 hours, the Master arrived back at the Hospital. Ms. K remained adamant that she did not want a blood transfusion. She was upset and agitated. She was administered a sedative. • At around commenced. 14. 35 hours, the transfusion
Constitutional Principle • The hospital subsequently sought, at the Court’s behest, a declaration that it was entitled to seek the Order. • The Master had genuine and real concerns that Ms. K might not have been in a position to give a valid informed refusal of consent to treatment.
Constitutional Principle The Master doubted Ms. K’s capacity to consent for a number of reasons including: - • Ms. K’s seriously compromised medical status; • The communications difficulties which arose given that Ms. K’s first language was not English; • Her late disclosure, after the haemorrhage, that she was a Jehovah’s Witness, having booked into the hospital as a Catholic.
Constitutional Principle • The Hospital invoked Articles 41 and 42 of the constitution: Article 41 “the State recognises the family as the natural primary and fundamental unit group of society, and as a moral institution possessing inalienable and imprescriptible rights, antecedent and superior to all positive law".
Constitutional Principle Article 42 “The State recognises and affirms the natural and imprescriptible rights of all children and shall, as far as practicable, by its laws protect and vindicate those rights” • To safeguard the constitutional rights of Ms. K’s baby to be nurtured and reared by Ms. K.
Constitutional Principle • The State's duty extended to ensuring that all appropriate medical steps were taken to safeguard Ms. K's life, especially since the medical procedures required for the purpose were routine and non life-threatening.
Constitutional Principle Ms. K counterclaimed on a number of grounds: 1. Her rights had been breached under the European Convention of Human Rights; 2. She was entitled to refuse medical treatment;
Constitutional Principle 3. the hospital had committed an assault and trespass on her person by giving her the transfusion; 4. She claimed that she was entitled to damages as a result;
Constitutional Principle In Judgement Ms. Justice Laffoy looked at the “Balancing of Rights” • The Court was entitled to have regard to Ms. K’s baby’s constitutional rights and found that, when balanced against Ms. K’s constitutional rights to autonomy, self determination, and the free practice of her religion, the baby’s rights outweighed Ms. K’s rights so as to entitle the judicial arm of the State to intervene. The issue was ultimately not determined.
Constitutional Principle The Court restated the relevant principles applicable to the determination of capacity: - • An adult has the capacity to refuse treatment, but it is a rebuttable presumption. • The patient’s cognitive ability must be so impaired that s/he does not sufficiently understand the nature, purpose and effect of the treatment and the consequences of accepting or rejecting it, in light of all the choices available.
Constitutional Principle • The cognitive ability will have been impaired to the extent that s/he is incapable of making the decision to refuse by reason of the following factors: Ø The patient has not comprehended and retained the treatment information and the consequences likely to ensue from their refusal;
Constitutional Principle Ø The patient has not believed the treatment information, in particular, that death may be the likely outcome; Ø The patient has not weighed the treatment information, the alternative choices and the likely outcomes, in the balance in arriving at the decision
Constitutional Principle • The clinician is under a duty to impart information as to the medically-advised appropriate treatment, the risks and consequences and the choices available to the patient.
Constitutional Principle • The clinician must recognise and note if misunderstanding and misperception of the treatment information is an issue as this may be evidence of a lack of capacity. An irrational decision or a decision made for irrational reasons is irrelevant to the assessment. • Regard must also be had to the gravity of the decision and the consequences that are likely to ensue
Legislative Principle The Legislative Principle of Autonomy and Freedom of Religious belief. Section 4 (1) of the Health Act 1953 states as follows: “Nothing in this Act or any instrument hereunder shall be construed as imposing an obligation on any person to avail himself or any service provided under this Act or to submit himself or any person for whom he is responsible to health examination or treatment”
Legislative Principle Section 4 (2) of the Health Act 1953 states as follows: “Any person who avails himself of any service provided under this Act shall not be under any obligation to submit himself or any person for whom he is responsible to a health examination or treatment which is contrary to the teaching of his religion. ” The above were Approved by the Supreme Court in the case of North Western Health Board v W (H) [2001] 3 IR 622 (also known as the ‘PKU test’ case)
Tort of Battery The Tort of Battery is committed by intentionally bringing about a harmful or offensive contact with the person of the patient. In Schloendorff v Society of New York Hospital [1914] 211 NY 125 (as described above). “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an Operation without the Patient’s Consent commits an Assault. ” (Battery)
![Tort of Battery v Assault In the case of Reibl v Hughes 1980 114 Tort of Battery v Assault In the case of Reibl v Hughes [1980] 114](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-72.jpg)
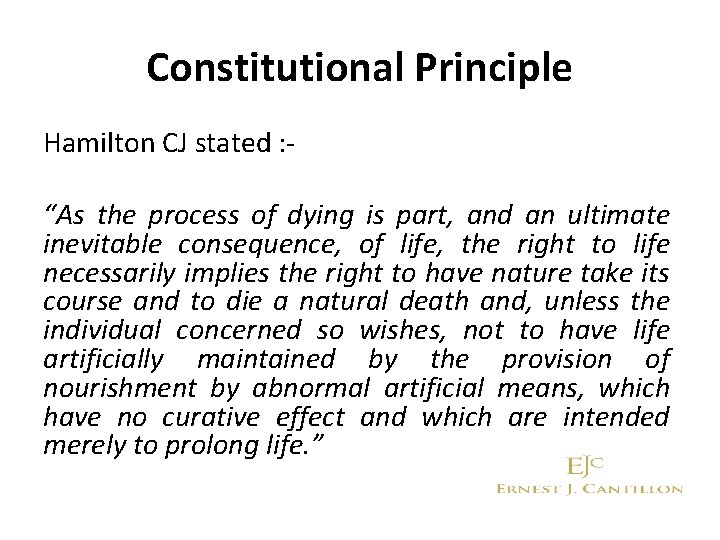
Tort of Battery v Assault In the case of Reibl v Hughes [1980] 114 DLR 1 – Canadian SC, the Plaintiff underwent surgery for the removal of an occlusion in the left internal carotid artery. The Surgeon performed the surgery properly, however, the Plaintiff had a massive stroke that left him paralysed. Prior to the surgery, the Doctor did not inform the Plaintiff specifically about the risk of stroke.
Tort of Battery v Assault Supreme Court held too much deference to doctors. Although medical information is necessary and very helpful in determining if sufficient information was given, it is not determinative. Medical information does not determine whethere has been a breach the duty of care. The test is whether a reasonable person in the appellant's shoes would have elected to have the surgery or not when the proper information was known.
Tort of Battery v Assault Causation was satisfied that with the proper information the Plaintiff would not have had the surgery or the resulting stroke. It was held that the Doctor was not liable for battery. Actions for battery in respect to surgery or other medical procedures should be limited to circumstances where consent has not been given for the particular procedure. This was a breach of the duty of care; there is no invalidity to the consent given.
Tort of Battery v Assault • A claim for Assault under the Criminal Law should be confined to cases where there is no Informed Consent to the particular procedure and it was feasible for the medical practitioner to acquire the Informed Consent from the patient.
![Assault v Negligence Assault v Negligence Chatterton v Gerson 1981 QB 432 Assault v Negligence • Assault v Negligence - Chatterton v Gerson [1981] QB 432.](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-76.jpg)
Assault v Negligence • Assault v Negligence - Chatterton v Gerson [1981] QB 432. In this case, the Doctor failed to explain possible consequences of an operation on a first operation, and on a subsequent corrective operation. • Broad terms → no assault • No sufficient information about the risk → negligence
Assault v Negligence • A Doctor can be held negligent if the patient demonstrates that he would not have accepted an unexplained risk. The Doctor was liable in negligence only if the general nature of the operation was not explained.
Defence to Battery Informed Consent allows the Medical Practitioner to come into contact with the person of the Patient without fear of committing the Tort of Battery. To be effective the following will apply: - • Consent must be freely given • Patient must be capable of giving Consent • Patient’s consent must be an Informed Consent
Implied & Express Consent In general practice for surgery or interventional investigations, express consent is obtained whereby the Doctor explains the risk/benefit to the patient. It can and should where possible, be given in writing and the patient signs a Consent Form. There are incidents where a patient gives implied consent: • Examination • Blood tests
![Information Bolam v Friern Hospital Management Committee 1957 HL 1 WLR 583 Although Information • Bolam v Friern Hospital Management Committee [1957] HL 1 WLR 583. Although](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-80.jpg)
Information • Bolam v Friern Hospital Management Committee [1957] HL 1 WLR 583. Although not a case strictly on consent, it is a very important case to reference as it established that if a Doctor acts in accordance with a responsible body of medical opinion, he or she will not be negligent.
Information • Sidaway -v- Board of Governors of the Bethlem Royal Hospital and the Maudsley Hospital; HL 1 All ER 643, [1985]. The Plaintiff suffered from pain in her neck, right shoulder and arms. Her Neurosurgeon took her consent for cervical cord decompression, but did not include in his explanation that in less than 1% of the cases, decompression caused paraplegia. She developed paraplegia after the spinal operation.
Information The court held that consent did not require an elaborate explanation of remote side effects. The question to be asked is not whether sufficient information had been disclosed to the patient to enable them to make an Informed Consent?

Information The issue to be addressed is whether or not a prudent Medical Practitioner would have acted as the Defendant Medical Practitioner did in releasing only a certain amount of information to the Plaintiff (Bolam Test – UK Professional Standard Approach). • Of note - in dissent, Lord Scarman said that the Bolam Test should not apply to the issue of informed consent and that a Doctor should have a duty to tell the patient of the inherent and material risk of the treatment proposed.
The Professional Standard v The Reasonable Patient Approach • The professional standard approach: This reflects the professional point of view. In this view, the health provider's responsibility is limited to the disclosures that a health professional, practising as a specialist in the field, would make under the same or similar circumstances. (Bolam)

The Professional Standard v The Reasonable Patient Approach • The reasonable patient approach: This test reflects the patient's point of view. A patient orientated standard of disclosure means that the health provider is required to disclose all facts, risks, and alternatives that a reasonable person in the patient's situation would consider important, in deciding to have, or not have, a recommended treatment. (US and Canada – Reasonable Patient Approach)

The Professional Standard v The Reasonable Patient Approach • The distinction may not seem important but strikingly different results can be obtained depending on the test applied. An examination of a few important legal decisions may serve to illustrate the difference between the approaches.
The Professional Standard v The Reasonable Patient Approach • Walsh v Family Planning Service [1992] 1 IR 4 In 1984, the Plaintiff had a vasectomy. He gave evidence that a Doctor explained that the operation was painless and safe. The Plaintiff said that the Doctor had not warned him of any long term side-effects but emphasised that it was irreversible. The Plaintiff developed long term pain, he had a left orchiectomy, pain persisted and affected his life.
The Professional Standard v The Reasonable Patient Approach • Expert evidence pinpointed the Plaintiff as suffering from Orchidalgia, a known but exceptionally rare condition and one not properly accounted for as a consequence of vasectomies. There was no general and approved practice of warning patients as to its incidence (Bolam / Professional Standard Approach).
The Professional Standard v The Reasonable Patient Approach • It was found by the Supreme Court that the vasectomy had been carried out properly and without negligence. The resulting complaint was an unfortunate and rare, but unavoidable side effect. • The members of the Court disagreed as to the test to be applied. The Chief Justice favoured the application of the Professional Standard Approach, while other members favoured the Reasonable Patient Approach. Ultimately, it did not have to decide because it was held that there was no negligence.
![The Professional Standard v The Reasonable Patient Approach Geoghegan v Harris2000 IR 536 The Professional Standard v The Reasonable Patient Approach • Geoghegan v Harris[2000] IR 536.](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-90.jpg)
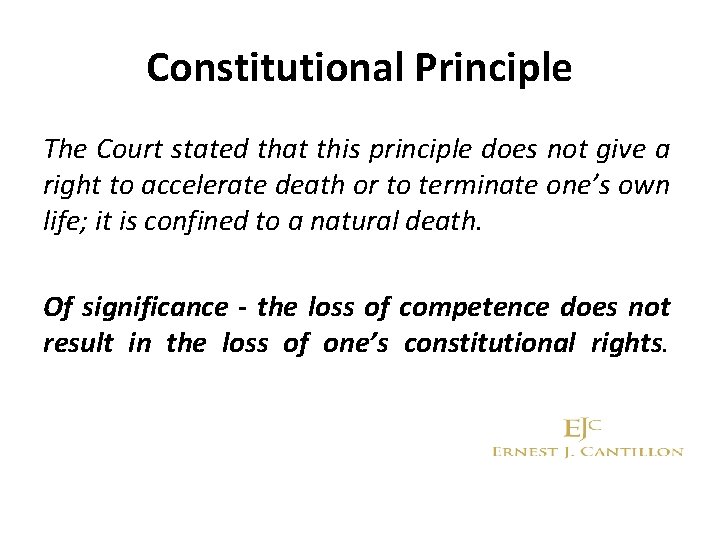
The Professional Standard v The Reasonable Patient Approach • Geoghegan v Harris[2000] IR 536. The Plaintiff alleged clinical negligence in the carrying out of an elective dental procedure which involved a bone graft which was taken from the Plaintiff’s chin. The Plaintiff was left with chronic neuropathic pain. The Dentist accepted he did not disclose this risk as his practice was only to disclose rare complications where the risk exceeded 1%.
The Professional Standard v The Reasonable Patient Approach • Ultimately, Kearns J favoured the Reasonable Patient Test of disclosure. None of the expert witnesses testified that they would give such a warning, yet the judge found that Mr. Geoghegan had been entitled to one. This complication was not insignificant; it involved permanent pain. The Judge found that in such an elective procedure, the practitioner must disclose all known risks, of grave consequence or severe pain, no matter how remote.
The Test of Materiality in Elective Procedures • The Judge felt that such a test would ensure that the patient could make a "real" choice. Introduced the concept of Material Risk. • The requirement to give a warning of any Material Risk which is a known complication of a course of treatment or clinical procedure properly carried out ; AND
The Test of Materiality in Elective Procedures • The Test of Materiality in elective procedures is to enquire whethere is any risk, however exceptional or remote, of grave consequences involving pain for an appreciable time into the future. The statistical frequency of the Material Risk is irrelevant.
Causation in Informed Consent • There are three elements to causation in regard to Informed Consent cases: 1. 2. Was the patient informed of the potential complication? If not, would a respected body of Medical Opinion have informed the Patient of the complication in respect of the proposed treatment or procedure?
Causation in Informed Consent 3. If the patient had been informed of the potential complication, would they have gone ahead with it?
![Causation in Informed Consent Chester v Afshar 2005 3 WLR 927 House of Causation in Informed Consent • Chester v Afshar [2005] 3 WLR 927 House of](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-96.jpg)
Causation in Informed Consent • Chester v Afshar [2005] 3 WLR 927 House of Lords The Plaintiff had suffered back pain for 6 years. This became quite severe and at times she was unable to walk or control her bladder. An MRI scan revealed that there was disc protrusion into her spinal column and she was advised to have surgery by the Defendant Mr Afshar. He failed to advise that the surgery carried a 1 -2% risk of nerve damage even if it was performed without negligence.
Causation in Informed Consent • The risk materialised and she was partially paralysed. She sued claiming that Mr. Afshar’s negligence in failing to tell her of the risk had caused her injury. • The Court of Appeal dismissed the appeal and the Defendant appealed to the House of Lords on the grounds of causation in that she was likely to have consented to the operation and that even if it had been on a different occasion, it carried the same risk. 3: 2 decision appeal dismissed
Causation in Informed Consent A move towards the Reasonable Patient Approach Lord Steyn stated as follows: “A surgeon owes a general duty to a patient to warn him or her in general terms of possible serious risk involved in the procedure…. . . In modern law medical paternalism no longer rules and a patient has a prima facie right to be informed by a surgeon of a small, but well established, risk of serious injury as a result of surgery”
![Recent Case on Informed Consent Montgomery v Lanarkshire Health Board 2015 UKSC 11 A Recent Case on Informed Consent Montgomery v Lanarkshire Health Board [2015] UKSC 11. A](https://slidetodoc.com/presentation_image_h2/8cb7b8335916945a918cafc68b577e49/image-99.jpg)
Recent Case on Informed Consent Montgomery v Lanarkshire Health Board [2015] UKSC 11. A pivotal case on consent “Sounded the death knell for the Bolam test” In 1999, Mrs. Montgomery’s son was born with severe disabilities. Delivery had become complicated by the inability of the baby’s shoulders to pass through the pelvis (an event known as shoulder dystocia).
Recent Case on Informed Consent As a result, following his birth he was diagnosed with both cerebral palsy and Erb’s Palsy. Mrs. Montgomery claimed on the basis that, as a small diabetic woman, she had not been warned about the risks involved in a vaginal delivery and, had she been warned, she would have opted for the safer option of a caesarean section.
Recent Case on Informed Consent • The evidence of the obstetrician was that she did not discuss this complication with diabetic women given that they would invariably elect for a caesarean section and it was “not in the maternal interests for women to have caesarean sections”.
Recent Case on Informed Consent • Their Lordships concluded that the Bolam test was not appropriate to the breach of duty aspect in cases of consent, stating: “An adult person of sound mind is entitled to decide which, if any, of the available forms of treatment to undergo, and her consent must be obtained before treatment interfering with her bodily integrity is undertaken.

Recent Case on Informed Consent The doctor is therefore under a duty to take reasonable care to ensure that the patient is aware of any material risks involved in any recommended treatment, and of any reasonable alternative or variant treatments.
Recent Case on Informed Consent The test of materiality is whether, in the circumstances of the particular case, a reasonable person in the patient’s position would be likely to attach significance to the risk, or the doctor is or should reasonably be aware that the particular patient would be likely to attach significance to it. ”
Recent Case on Informed Consent • The decision confirms that the previous analysis of the law by the House of Lords in the 1985 case of Sidaway v Board of Governors of the Bethlem Royal Hospital, which held that provided the doctor explained the risks of a given treatment – to the extent that it accorded with a responsible body of medical opinion – liability would not attach, (the Bolam test) is no longer to be applied.
Recent Case on Informed Consent The assessment of whether a risk is material is not merely a statistical exercise. The assessment will be fact sensitive and sensitive to the characteristics of the patient. Practitioners must ask the following questions: - 1. Does the patient know about the material risk? 2. Does the patient know about reasonable alternatives? 3. Have I taken reasonable care to ensure that the patient actually knows this?

Recent Case on Informed Consent In a scathing reproach of the Doctors conduct, Lady Hale stated: “Whatever Dr. Mc. Lellan may have had in mind, this does not look like a purely medical judgment. It looks like a judgment that vaginal delivery is in some way morally preferable to a caesarean section: so much so that it justifies depriving the pregnant woman of the information needed for her to make a free choice in the matter…
Recent Case on Informed Consent A patient is entitled to take into account her own values, her own assessment of the comparative merits of giving birth in the “natural” and traditional way and of giving birth by caesarean section, whatever medical opinion may say, alongside the medical evaluation of the risks to herself and her baby… …The medical profession must respect her choice, unless she lacks the legal capacity to decide. ”
Recent Case on Informed Consent • An exception to the duty is if the Doctor reasonably considers that the disclosure of the risk would “be seriously detrimental to the patient’s health”, or in circumstances of necessity. However, the Court made it clear that this exception should not be abused.
Recent Case on Informed Consent • This decision cements that the law on information disclosure are now oriented to safeguarding patient autonomy. Indeed, the Court in this case acknowledged that the Bolam principle in this area served to sanction “divergent attitudes among doctors as to the degree of respect owed to their patients”, rather than providing any credible measure of the amount of information that patients need to receive to make decisions that are consistent with their wishes, beliefs and values.
Definition of Informed Consent • Information – sufficient information has to be given. The manner and context is as important as the information. Following Montgomery, the Clinicians cannot use a pro forma approach to taking consent and must ensure the discussions as to risks and benefits are tailored to meet the particular patient’s needs and circumstances. Ø Explain options, risks and benefits in a way the patient will understand.
Definition of Informed Consent Ø Adequately record the discussion and in particular if any of the exceptions (therapeutic exception, necessity or patient’s choice) apply, rather than just relying on the patient’s signature on a consent form. Ø Avoid delegating the consent process, for example to junior medical professionals or nursing staff.
Definition of Informed Consent • Voluntariness – consent is valid only if voluntarily given. • Competence – In order for the patient's consent to be valid, he /she must be considered competent.
Lunacy Regulation (Ireland) Act 1871 • The Lunacy Act refers to people as ‘idiot’, ‘lunatic’ and ‘unsound mind’ and there are currently over two and a half thousand people in Ireland who are Wards of Court on account of age, intellectual disability, mental illness or brain injury.
Lunacy Regulation (Ireland) Act 1871 • Persons with disabilities waiting eight years for Irish Government to ratify the UN Convention on the Rights of Persons with Disabilities (CRPD). • Ireland’s Lunacy Regulation (Ireland) Act 1871 is at odds with the CRPD’s Article 12 on equal recognition in law.
Lunacy Regulation (Ireland) Act 1871 • The current Government committed to introducing modern capacity legislation in line with the CRPD. The 2013 Assisted Decision. Making (Capacity) is at the committee stage.
 Ethical principles governing informed consent process
Ethical principles governing informed consent process What are the rules in the selection of delta
What are the rules in the selection of delta Ruffles and flourishes protocol
Ruffles and flourishes protocol Electron configuration chart
Electron configuration chart Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sexual coercion definition
Sexual coercion definition Cit international conference
Cit international conference Channel capacity planning
Channel capacity planning Sgc meaning in school
Sgc meaning in school Decs order no 11 s 1987
Decs order no 11 s 1987 Stcw chapter viii
Stcw chapter viii Governing marriage laws and conducting elections
Governing marriage laws and conducting elections Bypass governing of steam turbine
Bypass governing of steam turbine R051 contemporary issues in sport
R051 contemporary issues in sport Inquiry practical research
Inquiry practical research Bac composition ra 9184
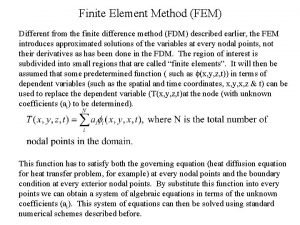
Bac composition ra 9184 Governing equation heat transfer
Governing equation heat transfer Governing equation heat transfer
Governing equation heat transfer Turbine governing system ppt
Turbine governing system ppt Governing body of insurance council
Governing body of insurance council Governing system
Governing system Governing equation
Governing equation Governing ourselves
Governing ourselves What is governing equation
What is governing equation Medicare parts c and d general compliance training answers
Medicare parts c and d general compliance training answers The principles of conduct governing an individual or
The principles of conduct governing an individual or Governing bodys
Governing bodys Medicare parts c and d sponsors are not required
Medicare parts c and d sponsors are not required Irca conference rules
Irca conference rules Logic tree method
Logic tree method Kelvin rodolfo
Kelvin rodolfo Cgu irb
Cgu irb Types of consent
Types of consent 22power dot com
22power dot com What is positive intervention consent
What is positive intervention consent Implicit consent
Implicit consent Voluntary consent meaning
Voluntary consent meaning Age of consent kentucky
Age of consent kentucky Age of consent state by state
Age of consent state by state Genuine consent
Genuine consent Dfps medical consent training
Dfps medical consent training Sebutkan dasar hukum informed consent
Sebutkan dasar hukum informed consent Authentic consent
Authentic consent Usps informed consent
Usps informed consent Health care consent act hierarchy
Health care consent act hierarchy Consent statistics
Consent statistics Law of consent
Law of consent Age of consent la
Age of consent la Legal consent forms for veterinary practices
Legal consent forms for veterinary practices Minority consent dalam sosiologi adalah
Minority consent dalam sosiologi adalah Which act taxed colonists without their consent? *
Which act taxed colonists without their consent? * Advantages of informed consent
Advantages of informed consent Graphical excellence
Graphical excellence Meta consent decree
Meta consent decree Emancipated minors definition
Emancipated minors definition Google consent
Google consent Impax epinephrine injection
Impax epinephrine injection The consent elaine kaye
The consent elaine kaye Uninformed consent
Uninformed consent Broad informed consent
Broad informed consent Ey2 declaration and consent form
Ey2 declaration and consent form Consent
Consent Consent form for case report
Consent form for case report Consent
Consent Continuous consent
Continuous consent What is a gerund example
What is a gerund example Peek vs gurney
Peek vs gurney Informed consent brochure
Informed consent brochure Stanford prison experiment right to withdraw
Stanford prison experiment right to withdraw E consent pro
E consent pro Healtheconnections consent form
Healtheconnections consent form Ib psychology ia consent form
Ib psychology ia consent form Skin pen consent form
Skin pen consent form Essential elements of informed consent
Essential elements of informed consent Group number on united healthcare card
Group number on united healthcare card Vuna healthcare logistics
Vuna healthcare logistics Value stream management for lean healthcare
Value stream management for lean healthcare Va sunshine healthcare network
Va sunshine healthcare network United healthcare underwritten by golden rule
United healthcare underwritten by golden rule Lakeland care district
Lakeland care district Types of torts in healthcare
Types of torts in healthcare Stepps healthcare
Stepps healthcare Healthcare cisco smartnet total care support
Healthcare cisco smartnet total care support Sirius security
Sirius security Service line management
Service line management Infection control isolation signs
Infection control isolation signs Sap business one for healthcare
Sap business one for healthcare Surgical team roles and responsibilities
Surgical team roles and responsibilities Decision making in healthcare
Decision making in healthcare Scraping healthcare
Scraping healthcare Papercut healthcare
Papercut healthcare Nursing informatics and healthcare policy
Nursing informatics and healthcare policy United healthcare community plan
United healthcare community plan Midas healthcare solutions
Midas healthcare solutions Micromedex healthcare series
Micromedex healthcare series Tort examples in healthcare
Tort examples in healthcare Definition of certification in healthcare
Definition of certification in healthcare False imprisonment in healthcare
False imprisonment in healthcare Value stream mapping healthcare examples
Value stream mapping healthcare examples Benefits of knowledge management in healthcare
Benefits of knowledge management in healthcare Https://www.healthcare.gov/see-plans/#/
Https://www.healthcare.gov/see-plans/#/ Innovative healthcare business solutions
Innovative healthcare business solutions Illinois healthcare lien act
Illinois healthcare lien act Skill survey healthcare hiring
Skill survey healthcare hiring Written communication in healthcare
Written communication in healthcare Historical healthcare figures
Historical healthcare figures Introduction to healthcare delivery systems
Introduction to healthcare delivery systems Secondary uses of healthcare data
Secondary uses of healthcare data Emory healthcare organizational chart
Emory healthcare organizational chart Premier healthcare exchange
Premier healthcare exchange Chd meridian healthcare
Chd meridian healthcare Change healthcare
Change healthcare Falck healthcare personalstöd
Falck healthcare personalstöd Leed for healthcare
Leed for healthcare Document management system for healthcare industry
Document management system for healthcare industry Powerchart emory
Powerchart emory