Medicare and the Marketplaces 2017 Medicare Rights Center











- Slides: 47

Medicare and the Marketplaces © 2017 Medicare Rights Center
Medicare Rights Center The Medicare Rights Center is a national, nonprofit consumer service organization that works to ensure access to affordable health care for older adults and people with disabilities through Counseling and advocacy Educational programs © 2017 Medicare Rights Center Public policy initiatives
National Council on Aging This toolkit for State Health Insurance Assistance Programs (SHIPs), Area Agencies on Aging (AAAs), and Aging and Disability Resource Centers (ADRCs) was made possible by grant funding from the National Council on Aging. The National Council on Aging is a respected national leader and trusted partner to help people aged 60+ meet the challenges of aging. They partner with nonprofit organizations, government, and business to provide innovative community programs and services, online help, and advocacy. © 2017 Medicare Rights Center
Learning objectives Explain Medicare basics Explain Health Insurance Marketplaces and Qualified Health Plans (QHPs) Understand what Medicare beneficiaries should know about Marketplace coverage Review Small Business Health Options Program (SHOP) available through Marketplaces Identify how beneficiaries with SHOP coverage should approach Medicare enrollment © 2017 Medicare Rights Center
Medicare basics © 2017 Medicare Rights Center
Medicare • Federal program that provides health insurance for those 65+, those under 65 receiving Social Security Disability Insurance (SSDI) for a certain amount of time, and those under 65 with kidney failure requiring dialysis or transplant § • No income requirements Two ways to receive Medicare benefits Original Medicare Traditional program offered directly through federal government Medicare Advantage Private plans that contract with federal government to provide Medicare benefits © 2017 Medicare Rights Center
Parts of Medicare • Medicare benefits administered in three parts § Part A – Hospital/inpatient benefits § Part B – Doctor/outpatient benefits § Part D – Prescription drug benefit • Original Medicare includes Part A and Part B § Part D benefits offered through stand-alone prescription drug plan • What happened to Part C? Medicare Advantage Plans (e. g. , HMO, PPO) § Way to get Parts A, B, and D through one private plan § Administered by private insurance companies that contract with federal government § Not a separate benefit: everyone with Medicare Advantage still has Medicare © 2017 Medicare Rights Center
Medicare eligibility: 65+ • After turning 65, individual qualifies for Medicare if they § Collect or qualify to collect Social Security or Railroad Retirement benefits § OR are a current U. S. resident and either » A U. S. citizen » OR a permanent resident having lived in the U. S. for five years in a row before applying for Medicare © 2017 Medicare Rights Center
Medicare eligibility: Under 65 • Individual not yet 65 qualifies for Medicare if § They have received Social Security Disability Insurance (SSDI) or Railroad Disability Annuity checks for total disability for at least 24 months o If they have amyotrophic lateral sclerosis (ALS), there is no waiting period, and they are eligible for Medicare when they start receiving SSDI § OR they have End-Stage Renal Disease (ESRD or kidney failure) and they or a family member have enough Medicare work history © 2017 Medicare Rights Center
Medicare Part D • Outpatient prescription drug benefit for anyone with Medicare § Individual is eligible for Part D if they have Part A or Part B • Only available from private insurance companies • Two ways to get Part D drug coverage: § If beneficiary has Original Medicare, they can purchase a standalone prescription drug plan § If beneficiary has MA Plan, Part D is generally included, and beneficiary receives all Medicare benefits from one plan • Stand-alone plans and MA Plans have monthly premium § Beneficiaries with low incomes can get help with costs © 2017 Medicare Rights Center
Creditable coverage • Drug coverage considered as good as or better than Part D • Individuals with creditable coverage will not have to pay a late enrollment penalty if they switch to Part D using Special Enrollment Period (SEP) • Employers or plans should send current and former employees annual notice declaring whether or not their drug coverage is still considered creditable • Beneficiary is eligible for SEP if: § They lost creditable drug coverage through no fault of their own or their benefit was reduced and is no longer creditable © 2017 Medicare Rights Center
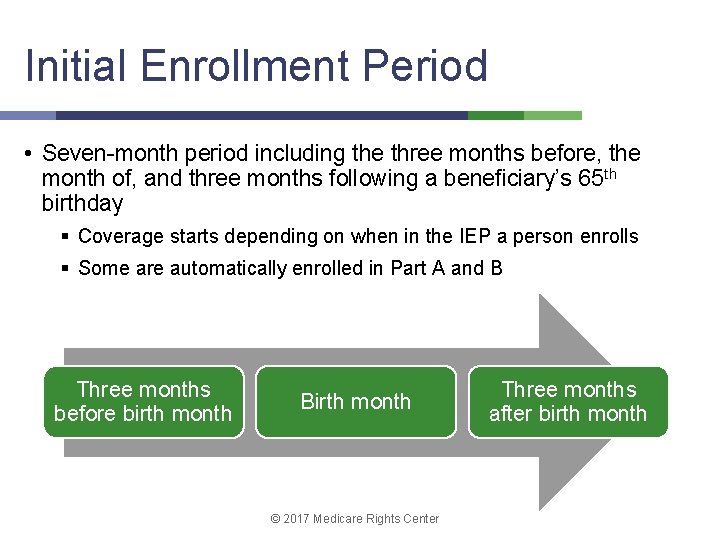
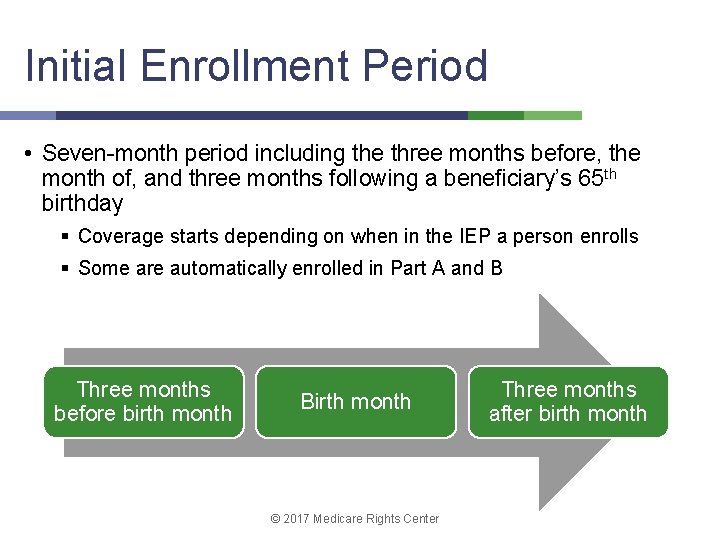
Initial Enrollment Period • Seven-month period including the three months before, the month of, and three months following a beneficiary’s 65 th birthday § Coverage starts depending on when in the IEP a person enrolls § Some are automatically enrolled in Part A and B Three months before birth month Birth month © 2017 Medicare Rights Center Three months after birth month
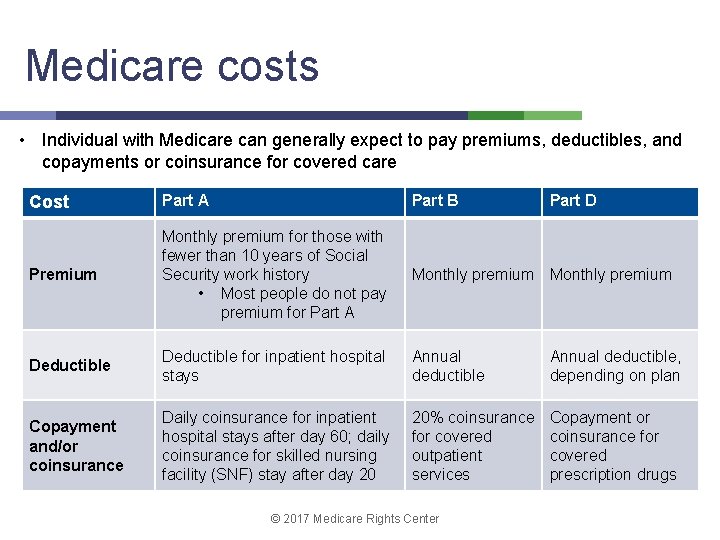
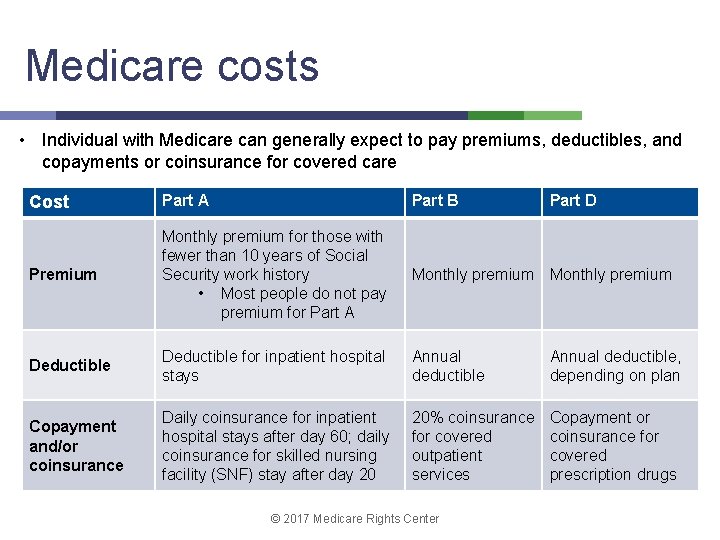
Medicare costs • Individual with Medicare can generally expect to pay premiums, deductibles, and copayments or coinsurance for covered care Cost Part A Part B Premium Monthly premium for those with fewer than 10 years of Social Security work history • Most people do not pay premium for Part A Monthly premium Deductible for inpatient hospital stays Annual deductible, depending on plan Copayment and/or coinsurance Daily coinsurance for inpatient hospital stays after day 60; daily coinsurance for skilled nursing facility (SNF) stay after day 20 20% coinsurance for covered outpatient services Copayment or coinsurance for covered prescription drugs © 2017 Medicare Rights Center Part D
Extra Help • Federal program that helps pay deductibles, premiums, copays, and coinsurances for Medicare Part D (prescription drug benefit) • Has federally set income and asset limits • Individuals pay no premium or very low premium • Individuals pay low copayments for Part D-covered drugs © 2017 Medicare Rights Center

Health Insurance Marketplaces © 2017 Medicare Rights Center
Requirement for health coverage • Starting 1/1/14, U. S. residents must have minimum level of health coverage, called minimum essential health coverage § Requirement known as individual mandate § Resulted from Affordable Care Act (ACA) • Minimum essential health coverage includes: Medicare, Medicaid, most employer insurance, or Marketplace insurance • People who fail to obtain minimum essential coverage need to pay tax penalty unless they meet financial hardship criteria © 2017 Medicare Rights Center
Marketplace basics • Forums where uninsured or under-insured individuals, and also businesses, can shop for health coverage § Sometimes known as Exchanges or state-specific names • Types of insurance offered through Marketplaces include: § Qualified Health Plans (QHPs) § Small Business Health Options Program (SHOP) plans • Consumers can compare available plans based on price, benefits, services, quality © 2017 Medicare Rights Center
State variation • Marketplace in every state and District of Columbia • Marketplace operation may vary from state to state, as states may: § Run their own Marketplace § Partner with federal government § Rely exclusively on federal government to run their Marketplace © 2017 Medicare Rights Center
Qualified Health Plans • Private health insurance policies that meet protections and requirements set by ACA § Follow federally established cost-sharing limits § Provide essential health benefits § Meet minimum essential coverage requirement, also known as individual mandate © 2017 Medicare Rights Center
Paying for QHP coverage • Individuals with income between 100% and 400% of federal poverty level (FPL) can receive QHP premium cost assistance (tax credits) • Individual may be ineligible for tax credits if they are: § Eligible for Medicaid § Or eligible for Medicare » Some exceptions may apply © 2017 Medicare Rights Center

Marketplace Open Enrollment • Used to enroll in Marketplace plan for the first time or make coverage changes § Marketplace Open Enrollment Period (November 15 - December 15) § Overlaps with Medicare Fall Open Enrollment Period (October 15 – December 7) • Important: People with Medicare should use Fall Open Enrollment to make changes to their coverage © 2017 Medicare Rights Center
Medicare and the Marketplaces • Marketplaces do not affect Medicare coverage § Medigap policies, Medicare Advantage Plans, and standalone Part D plans are not sold through Marketplaces • In most cases, beneficiaries should enroll in Medicare when eligible or potentially face: § Gaps in coverage and late enrollment penalties § Loss of tax credits for those with QHP, meaning individual will pay higher monthly premiums to keep QHP coverage • Note: Medicare Part A fulfills ACA’s minimum essential coverage requirement © 2017 Medicare Rights Center
Unwise to drop Medicare for QHP • Illegal for Marketplace sales representatives to sell QHPs to people with Medicare • Medicare beneficiaries should not drop their coverage to enroll in QHP § Note: With some exceptions. See the Marketplace for People with Medicare FAQ for more information. • Medicare is typically less costly than QHP for those who are Medicare-eligible § Most people who qualify for Medicare will not qualify for tax credits to help pay QHP premiums § Part A is premium-free for most beneficiaries § Premiums for Part B, Part D, and Medigaps cost less than QHPs and provide more coverage © 2017 Medicare Rights Center
Transitioning to Medicare from QHP • Most people with QHPs should enroll in Medicare once they become eligible and drop their QHP • Beneficiary should enroll in Medicare Parts A, B, and D during their IEP § Keep track of when beneficiary first qualifies for Medicare § Actively enroll beneficiary if they are not auto-enrolled § Contact Social Security Administration to enroll: 800 -7721213 © 2017 Medicare Rights Center

Marketplace disenrollment • Beneficiary should notify QHP representative of their intent to disenroll at least 14 days before Medicare coverage begins • Ask plan representative for disenrollment steps if enrolled in a family plan § This helps ensure that disenrollment does not affect family members’ coverage © 2017 Medicare Rights Center

Considerations before delaying Medicare enrollment • Delayed enrollment may result in: § Late enrollment penalties on Medicare premiums § Gaps in coverage • Also, Medicare-eligible individuals likely have to pay full QHP premium § Remember, beneficiaries eligible for premium-free Part A lose QHP premium tax credits § Exception: Beneficiaries who pay premium for Part A can continue receiving premium tax credits but should still consider the consequences of delaying Medicare enrollment • Finally, QHPs may not pay claims for Medicare-eligible individuals © 2017 Medicare Rights Center
Part B late enrollment penalty (LEP) • 10% premium penalty for each 12 -month period of delayed enrollment added to current Part B premium ($134 in 2017) • Must be paid every month as long as individual has Medicare, with few exceptions • Individuals who delay Medicare enrollment to stay in a QHP will likely be subject to Part B LEP • Example: Individual delayed Part B enrollment for two years, so LEP = ($134 x 10%) x 2 = $13. 40 x 2 = $26. 80 © 2017 Medicare Rights Center
Strategies for late Part B enrollment • If beneficiary delayed Medicare enrollment, they may be able to remove penalties or gaps in coverage later § If their Medicare eligibility changes » For example, when disabled beneficiary turns 65 and becomes eligible due to age § If they enroll in Medicare Savings Program (MSP) » Must meet income requirements § If they are awarded equitable relief » Federal law lets people request relief from Social Security Administration (SSA) in the form of immediate or retroactive Medicare enrollment and/or elimination of Part B premium penalty—must meet specific requirements © 2017 Medicare Rights Center
Strategies for late Part D enrollment • If beneficiary delayed Part D enrollment and did not have creditable coverage, they may be able to remove penalties or gaps in coverage later § If they are eligible for Extra Help program, which » Lowers prescription drug costs » Provides monthly Special Enrollment Period (SEP), meaning that beneficiaries can switch their Part D plan monthly if plan does not meet their needs § Contact Social Security Administration to enroll: 800 -7721213 © 2017 Medicare Rights Center
General Enrollment Period (GEP) • Beneficiaries who are ineligible for equitable relief or an MSP may need to use GEP to enroll in Medicare • January 1 through March 31 each year • Sign up for Part B with coverage beginning July 1 § Beneficiary may have no coverage until then • Using GEP to sign up typically means incurring late enrollment penalty © 2017 Medicare Rights Center

Medicare and the Small Business Health Options Program (SHOP) © 2017 Medicare Rights Center
SHOP basics • Program within Marketplace where small businesses and their employees can search for and purchase health coverage • SHOP should: § Guarantee small businesses choice of plans to offer employees § Post health plan information on state’s website to allow comparisons among plans © 2017 Medicare Rights Center

Participation in the SHOP • Companies can generally only participate in their state’s SHOP if they have 50 or fewer employees (though states may allow up to 100) § Must offer SHOP plan coverage to all full-time employees (30+ hours) § In many states, at least 70% of employees must be covered (either by SHOP plan or other form of coverage) for business to participate in SHOP • Sole proprietors/self-employed individuals cannot participate in the SHOP § Must buy Marketplace QHPs Who can participate in SHOP? 50 or fewer employees Over 50 employees © 2017 Medicare Rights Center Sole proprietor
SHOP and Medicare eligibility • SHOP plans follow same rules as other insurance based on current work (job-based insurance) • Medicare-eligible individuals may choose to delay Medicare enrollment without penalty depending on: § Size of employer § Whether person’s Medicare eligibility is based on » Age » Disability • The following slides discuss SHOP plans and enrollment in Parts B and D © 2017 Medicare Rights Center

SHOP and Medicare enrollment © 2017 Medicare Rights Center

Part B Special Enrollment Period • Most beneficiaries with SHOP coverage qualify for SEP to delay Part B without incurring late enrollment penalty or facing gaps in coverage* • Two criteria for individual to be eligible for Part B SEP: 1. Must have insurance from current work (their job, spouse’s job, or sometimes a family member’s job)—or have had such insurance within past 8 months 2. Must have been continuously covered since becoming eligible for Medicare, including month they became eligible for Medicare » No SEP if individual has more than 8 consecutive months without coverage from either Medicare or job-based insurance © 2017 Medicare Rights Center
Primary and secondary insurance • When beneficiary has Medicare and another type of insurance, Medicare pays either primary or secondary for medical claims • Primary insurance pays first on claim • Secondary insurance pays after primary insurance § Usually pays all or some of the costs left after primary insurer pays (e. g. , copays, deductibles) § If primary insurer denies claim, secondary insurer may or may not make independent determination on it, depending on plan © 2017 Medicare Rights Center

Medicare is primary: Fewer than 20 employees (65+) • Medicare is primary for those covered by SHOP plan from employer with fewer than 20 employees § Plan can be individual’s or their spouse’s • May be able to keep SHOP plan as secondary • Part B SEP still applies § Medicare primary/secondary status doesn’t change this © 2017 Medicare Rights Center
Medicare is secondary: 20+ employees (65+) • SHOP plan is primary • Individual covered by their or their spouse’s SHOP plan don’t necessarily need to take Part B § Can delay enrollment and use Part B SEP for up to 8 months after they no longer have job-based insurance © 2017 Medicare Rights Center

Medicare is primary: Fewer than 100 employees (disability) • Medicare is primary for those with disabilities who are covered by SHOP plan from employer with fewer than 100 employees § Plan can be individual’s, their spouse’s, or other family member’s • May be able to keep SHOP plan as secondary • Part B SEP may still apply § Only eligible for SEP if health coverage is from their own or their spouse’s employer, not from another family member © 2017 Medicare Rights Center
SHOP coverage and Part B • Beneficiaries with SHOP plans that are secondary should take Part B for primary coverage § Delaying Part B coverage may result in their SHOP plan: » Paying little or nothing for care » Recouping payments it made when Medicare should have been primary • If the SHOP plan pays first, beneficiaries may consider delaying Part B © 2017 Medicare Rights Center 41
SHOP and Part D • Beneficiaries with creditable coverage from SHOP may choose to delay Part D enrollment § Can enroll in Part D within 63 days of losing creditable coverage to avoid penalties and gaps in coverage • Those without creditable coverage should enroll in Part D when Medicare-eligible § Must enroll in either Part A or Part B to get Part D coverage • If beneficiary did not have creditable coverage, see slide #29 for strategies for eliminating penalties and gaps in coverage © 2017 Medicare Rights Center
Review © 2017 Medicare Rights Center
Review • Medicare beneficiaries should not look to Marketplaces for health insurance • Most Medicare-eligible individuals should disenroll from their QHP and get Medicare • Medicare is primary for eligible individuals in SHOP plans if they are: § Under 65 and qualify for Medicare due to a disability § Over 65 and their SHOP plan is through an employer with fewer than 20 employees • Medicare is secondary for eligible individuals in SHOP plans if they are: § Over 65 and their SHOP plan is through employer with 20+ employees © 2017 Medicare Rights Center
Resources for information and help Local State Health Insurance Assistance Program (SHIP) • www. shiptacenter. org • www. eldercare. gov Medicare Rights Center • 800 -333 -4114 • www. medicareinteractive. org Social Security Administration • 800 -772 -1213 • www. ssa. gov National Council on Aging Medicare • 1 -800 -MEDICARE (633 -4227) • www. medicare. gov • • www. ncoa. org www. centerforbenefits. org www. mymedicarematters. org www. benefitscheckup. org © 2017 Medicare Rights Center
Medicare Interactive • www. medicareinteractive. org • Web-based compendium developed by Medicare Rights for use as a look-up guide and counseling tool to help people with Medicare § § Easy to navigate Clear, simple language Answers to Medicare questions and questions about related topics 2+ million annual visits © 2017 Medicare Rights Center
Medicare Interactive Pro (MI Pro) • Web-based curriculum that empowers professionals to better help clients, patients, employees, retirees, and others navigate Medicare § Four levels with four to five courses each § Quizzes and downloadable course materials • Builds on 25 years of Medicare Rights Center counseling experience • For details, visit www. medicareinteractive. org/learningcenter/courses or contact Jay Johnson at 212 -204 -6234 or jjohnson@medicarerights. org © 2017 Medicare Rights Center
 Global marketplaces and business centers
Global marketplaces and business centers Subsistence marketplaces definition
Subsistence marketplaces definition Positive rights and negative rights
Positive rights and negative rights Conclusion of rights
Conclusion of rights Legal rights vs moral rights
Legal rights vs moral rights Negative right
Negative right 2017 all rights reserved
2017 all rights reserved Littoral water rights
Littoral water rights Negative right
Negative right Negative right
Negative right Negative rights vs positive rights
Negative rights vs positive rights Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worm breton là gì
Tư thế worm breton là gì Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì