Malaria H 2012 Protozoan Disease 108 countries 3













- Slides: 101
Malaria H 2012 Protozoan Disease 108 countries 3 billion people 1 million deaths each year
In the late twentieth : Eliminated United States, Canada, Europe, Russia Prevalence rose in many parts of the tropics
Resurgence Increases in the drug resistance of the parasite Insecticide resistance of its vectors Human travel and migration
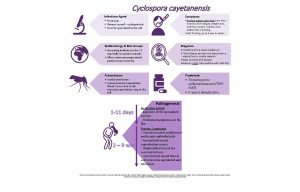
Etiology Five species of the genus Plasmodium cause nearly all malarial infections in humans. Falciparum Vivax Ovale Malariae Knowlesi (in Southeast Asia—the monkey malaria parasite )
Almost all Deaths Falciparum
Female Anopheline Mosquito Sporozoites Liver Asexual Reproduction Single Sporozoite eventually 10, 000 to >30, 000 Daughter Merozoites Liver cell eventually bursts 100 million parasites in the blood of an adult, the symptomatic stage of the infection begins
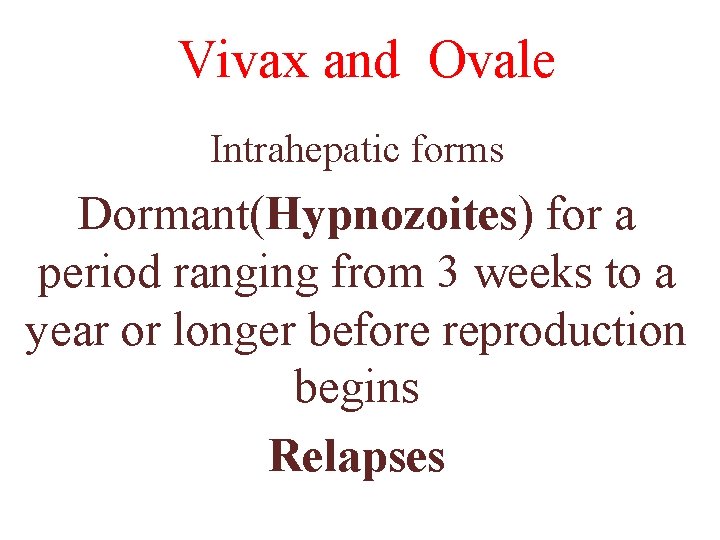
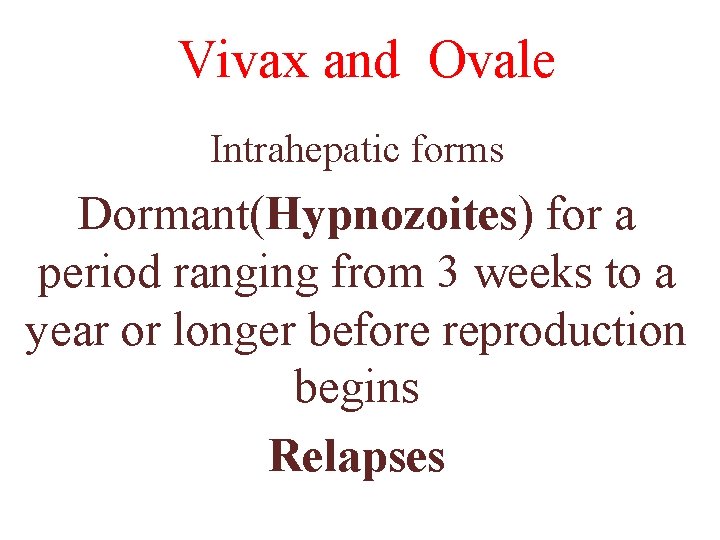
Vivax and Ovale Intrahepatic forms Dormant(Hypnozoites) for a period ranging from 3 weeks to a year or longer before reproduction begins Relapses
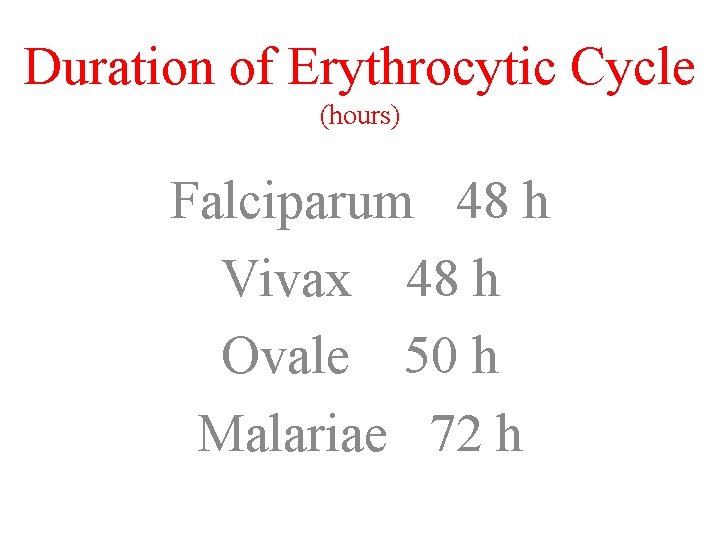
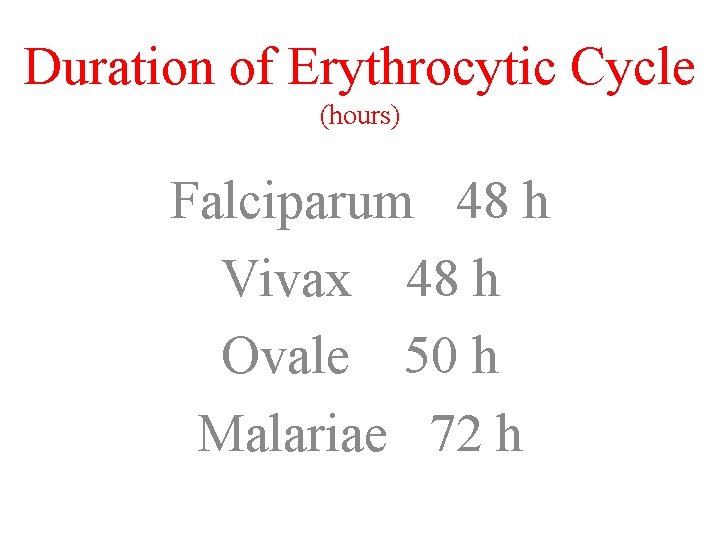
Duration of Erythrocytic Cycle (hours) Falciparum 48 h Vivax 48 h Ovale 50 h Malariae 72 h
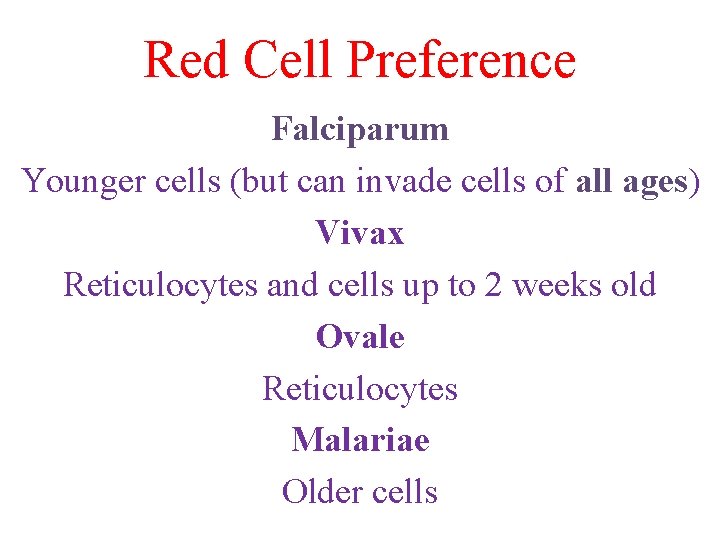
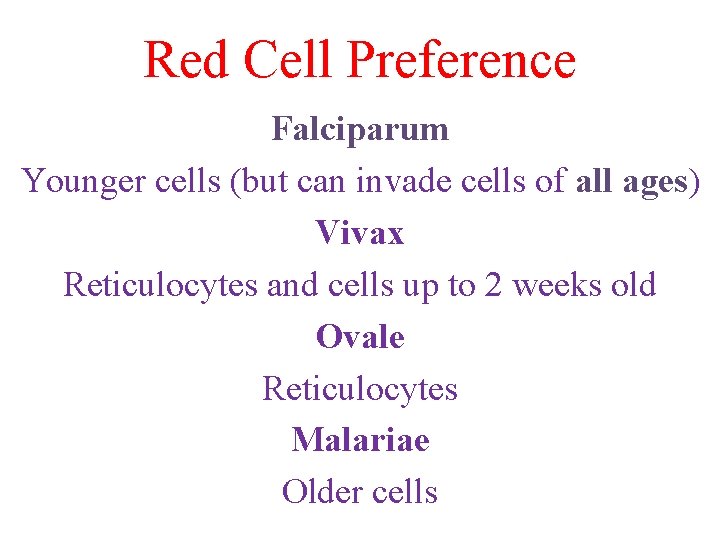
Red Cell Preference Falciparum Younger cells (but can invade cells of all ages) Vivax Reticulocytes and cells up to 2 weeks old Ovale Reticulocytes Malariae Older cells
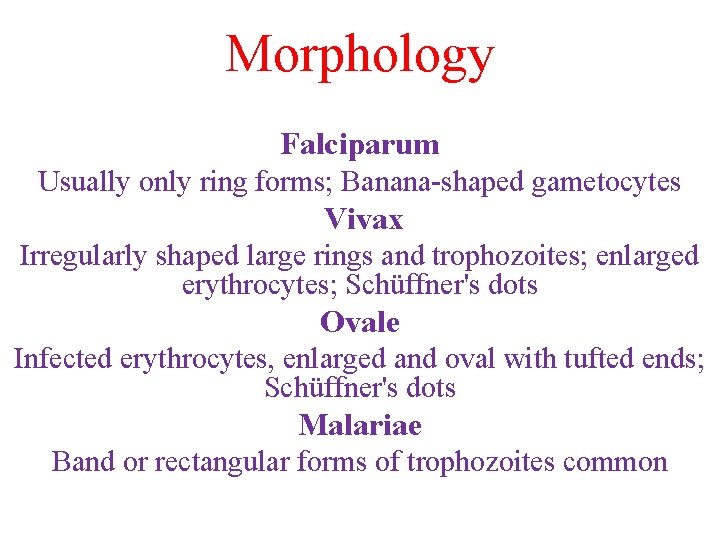
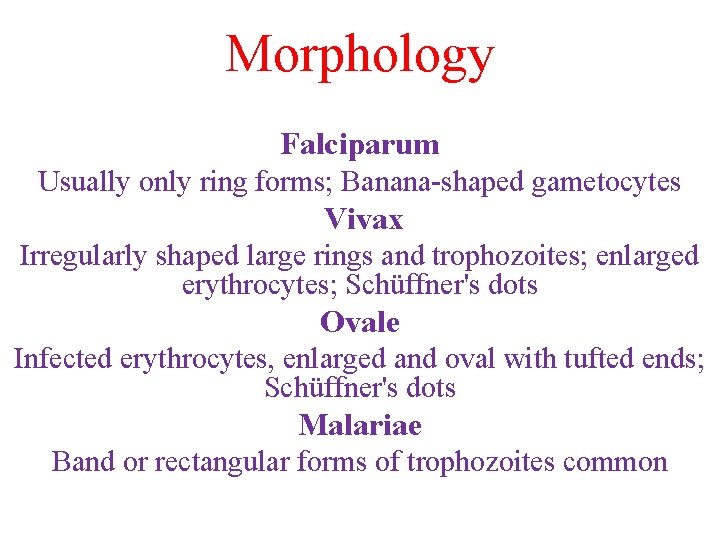
Morphology Falciparum Usually only ring forms; Banana-shaped gametocytes Vivax Irregularly shaped large rings and trophozoites; enlarged erythrocytes; Schüffner's dots Ovale Infected erythrocytes, enlarged and oval with tufted ends; Schüffner's dots Malariae Band or rectangular forms of trophozoites common
Relapses Vivax , Ovale : Yes Falciparum , Malariae : No
Parasitemias of >2% are suggestive of Falciparum infection
Vivax Duffy blood-group antigen Fya or Fyb Most West Africans and people with origins in that region carry the Duffynegative Fy. Fy phenotype and are therefore resistant to P. vivax
Disease Direct effects of RBC invasion and destruction by the asexual parasite and the host's reaction
Epidemiology Falciparum predominates in Africa, New Guinea, and Hispaniola (i. e. , the Dominican Republic and Haiti) Vivax is more common in Central America Malariae is found in most endemic areas Ovale is relatively unusual outside of Africa
Endemicity Parasitemia rates or palpable-Spleen rates in children 2– 9 years Hypoendemic (<10%) Mesoendemic (11– 50%) Hyperendemic (51– 75%) Holoendemic (>75%)
Holo- and Hyperendemic areas (e. g. , certain regions of tropical Africa or coastal New Guinea) where there is intense Falciparum transmission, people may sustain more than one infectious mosquito bite per day and are infected repeatedly throughout their lives Morbidity and Mortality during early Childhood Adulthood, most infections are Asymptomatic
Stable Transmission Constant Frequent Year-round infection
Unstable Transmission is low, Erratic, or Focal, full protective immunity is not acquired, and symptomatic disease may occur at All Ages Usually exists in Hypoendemic
An Epidemic Changes in Environmental, Economic, or Social conditions, such as heavy rains or migrations (usually of Refugees or Workers) from a nonmalarious region to an area of high transmission; a breakdown in malaria control and prevention service All Age Groups
Anophelines >400 can transmit malaria, and the 40 considerably in their efficiency as malaria vectors Life cycle within the mosquito—from gametocyte ingestion to subsequent inoculation (sporogony)—lasts 8– 30 days mosquito must survive for >7
Sporogony Is not completed at cooler temperatures <16°C for P. vivax and < 21°C for Falciparum; transmission does not occur below
The most effective mosquito vectors such as Anopheles gambiae in Africa, which are long-lived, occur in high densities in tropical climates, breed readily, and bite humans in preference to other animals
Entomologic Inoculation Rate (EIR) the number of sporozoite-positive mosquito bites person per year is the most common measure of malaria transmission and varies from <1 in some parts of Latin America and Southeast Asia to >300 in parts of tropical Africa.
Erythrocyte Changes Consumes and degrades intracellular proteins principally hemoglobin Alters the RBC membrane by changing its transport properties, exposing cryptic surface antigens, and inserting new parasite-derived proteins. The RBC becomes more irregular in shape, more antigenic, and less deformable.
Severe malaria is also associated with reduced deformability of the uninfected erythrocytes, which compromises their passage through the partially obstructed capillaries and venules and shortens RBC survival.
In the other three ("benign") human malarias, sequestration does not occur, and all stages of the parasite's development are evident on peripheral-blood smears. Whereas Vivax, Ovale, and Malariae show a marked predilection for either young RBCs (Vivax, Ovale) or old cells (Malariae) and produce a level of parasitemia that is seldom >2%, Falciparum can invade erythrocytes of all ages and may be associated with very high levels of parasitemia.
Host Response Initially, nonspecific defense mechanisms Splenic immunologic and filtrative clearance Removal of both parasitized and uninfected erythrocytes Strain-specific immune response then controls the infection
Exposure to sufficient strains confers protection from high-level parasitemia and disease but not from infection Infection without illness , asymptomatic parasitemia is common among adults and older children living in regions with stable and intense transmission (holo- or hyperendemic areas). Immunity is mainly specific for both the species and the strain of infecting malarial parasite. Both humoral immunity and cellular immunity are necessary for protection
Passively transferred Ig. G from immune adults has been shown to reduce levels of parasitemia in children; although parasitemia in very young infants can occur, passive transfer of maternal antibody contributes to the relative (but not complete) protection of infants from severe malaria in the first months of life
Immunity to disease declines when a person lives outside an endemic area for several months or longer. Parasites may persist in the blood for months (or, in the case of P. malariae, for many years)
Temperatures of 40°C damage mature parasites Tertian, every 2 days; Quartan, every 3 days) are seldom seen today
Geographic Distributions Sickle Cell disease Hemoglobins C and E Hereditary Ovalocytosis Thalassemias G 6 PD (glucose-6 -phosphate dehydrogenas edeficiency ) closely resemble that of falciparum malaria before the introduction of control measures. This similarity suggests that these genetic disorders confer protection against death from falciparum
Clinical Features First symptoms of malaria are nonspecific Lack of a sense of well-being Headache Fatigue Abdominal discomfort Muscle aches Fever similar to the symptoms of a minor viral illness followed by
Headache Chest pain Abdominal pain Arthralgia Myalgia Diarrhea
Common Nausea Vomiting Orthostatic hypotension
Classic malarial paroxysms Fever spikes Chills and rigors occur at regular intervals, are relatively unusual and suggest infection with P. Vivax or P. Ovale
Fever Irregular at first (that of falciparum malaria may never become regular); the temperature of nonimmune individuals and children often rises above 40°C in conjunction with Tachycardia and sometimes Delirium.
Childhood Febrile Convulsions may occur with any of the malarias, generalized seizures are specifically associated with falciparum malaria
Physical Findings Fever Malaise Mild Anemia Palpable Spleen (in some cases)
Anemia Common among young children living in areas with stable transmission
Slight enlargement of the liver Common, particularly among Young Children
Mild jaundice Common among adults; it may develop in patients with otherwise uncomplicated malaria and usually resolves over 1– 3 weeks
Malaria is not associated with a rash Petechial hemorrhages in the skin or mucous develop only rarely in severe falciparum malaria
Severe Falciparum Malaria Appropriately and promptly treated, uncomplicated falciparum malaria (i. e. , the patient can swallow medicines and food) Mortality rate of 0. 1%
Severe Falciparum Malaria Cerebral malaria/convulsion Acidemia/acidosis Severe normochromic, normocytic anemia Renal failure Pulmonary edema/adult respiratory distress syndrome Hypoglycemia Hypotension/shock Bleeding/disseminated intravascular coagulation Hemoglobinuria
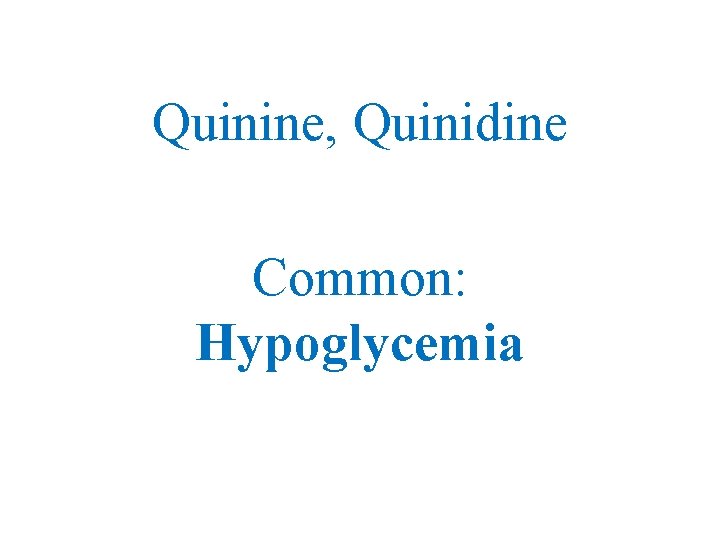
Hypoglycemia Important and common complication of severe malaria, is associated with a poor prognosis and is particularly problematic in Children and Pregnant women. Hepatic Gluconeogenesis Increase in the consumption of glucose by both host and, to a much lesser extent, the malaria parasites Quinine , Quinidine
Jaundice Mild hemolytic jaundice is common in malaria Severe jaundice is associated with P. falciparum; is more common among adults and results from: Hemolysis Hepatocyte injury Cholestasis
Other HIV/AIDS predisposes to more severe malaria in nonimmune individuals Worsened by intestinal helminths, Hookworm in particular Septicemia may complicate severe malaria, particularly in children(specifically Salmonella bacteremia ) Aspiration Pneumonia
ﺩﺭ ﺑچﻪ ﻫﺎ ﺷﺎیﻌﺘﺮ Anemia Convulsions Hypoglycemia
ﺩﺭ ﺑﺎﻟﻐیﻦ ﺷﺎیﻌﺘﺮ Jaundice Renal failure Pulmonary edema
Pregnancy Stable transmission area: Mothers Asymptomatic Falciparum malaria in primi- and secundigravid women is associated with Low Birth Weight Increased infant and childhood mortality Maternal HIV infection predisposes newborns to congenital malarial
Pregnancy Unstable Transmission Mother: High-level parasitemia Anemia Hypoglycemia Acute pulmonary edema Fetal distress, premature labor, and stillbirth or low birth weight are common
Pregnancy Congenital malaria occurs in <5% of newborns P. Vivax malaria in pregnancy is also associated with a reduction in birth weight but, in contrast to the situation in falciparum malaria, this effect is more pronounced in Multigravid
Transfusion Blood Transfusion Needle-Stick Injury IVDU Organ Transplantation Incubation period in these settings is often short because there is no preerythrocytic stage Clinical features and management are the same as for naturally acquired infections. Primaquine is unnecessary for transfusiontransmitted P. vivax and P. ovale infections.
Tropical Splenomegaly (Hyperreactive Malarial Splenomegaly) Chronic or repeated in some cases malarial parasites cannot be found in peripheral-blood smears Massive Splenomegaly, Hepatomegaly Hypergammaglobulinemia; normochromic, normocytic anemia Antimalarial chemoprophylaxis; results usually good
Quartan Malarial Nephropathy Chronic or repeated infections with P. Malariae (and possibly with other malarial species soluble immune-complex Nephrotic Syndrome
Burkitt's Lymphoma Strongly associated with Epstein-Barr virus The prevalence of this childhood tumor is high in malarious areas of Africa.
Diagnosis Asexual Giemsa Field's Wright's Leishman's stain Both thin and thick (preferred)
RDTs Rapid, simple, sensitive, and specific antibody-based diagnostick or card tests that detect P. falciparum–specific, in finger-prick blood samples are now being used widely in control programs RDTs are replacing microscopy in many areas because of their simplicity and speed, but they are relatively expensive and do not quantify parasitemia.
PCR Antibody and PCR tests have NO role in the diagnosis of malaria except that PCR is increasingly used for genotyping and speciation in mixed infections
Gametocytemia may persist for days or weeks after clearance of asexual parasites
Phagocytosed malarial Pigment is sometimes seen inside peripheral-blood Monocytes or Polymorphonuclear leukocytes and may provide a clue to recent infection if malaria parasites are not detectable
Laboratory Findings Normochromic, Normocytic Anemia is usual WBC count is generally normal, although it may be raised in very severe infections Monocytosis, Lymphopenia, and Eosinopenia, with reactive Lymphocytosis and Eosinophilia in the weeks after the acute infection ESR, CRP High Severe infections may be accompanied by prolonged PT and partial thromboplastin times and by more severe Thrombocytopenia
Treatment Repeat blood smears at least every 12– 24 h for 2 days Alternatively, a rapid antigen detection card or stick test
Any doubt about the resistance, it should be considered resistant Antimalarial drug susceptibility testing can be performed but is rarely available, has poor predictive value in an individual case, and yields results too slowly to influence the choice of treatment
Chloroquine Choice for the non-falciparum malarias Vivax Ovale Malariae Knowlesi except in Indonesia and Papua New Guinea, where high levels of resistance in P. vivax are prevalent.
Chloroquine-Sensitive Vivax Malariae Ovale, Knowlesi Falciparuma
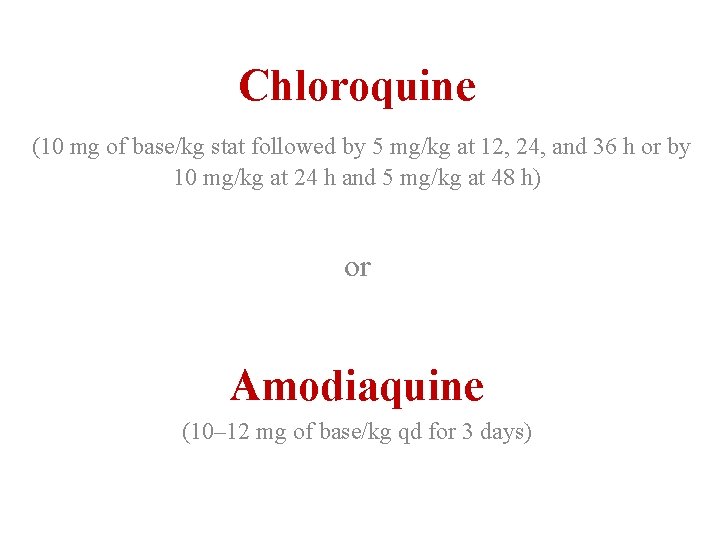
Chloroquine (10 mg of base/kg stat followed by 5 mg/kg at 12, 24, and 36 h or by 10 mg/kg at 24 h and 5 mg/kg at 48 h) or Amodiaquine (10– 12 mg of base/kg qd for 3 days)
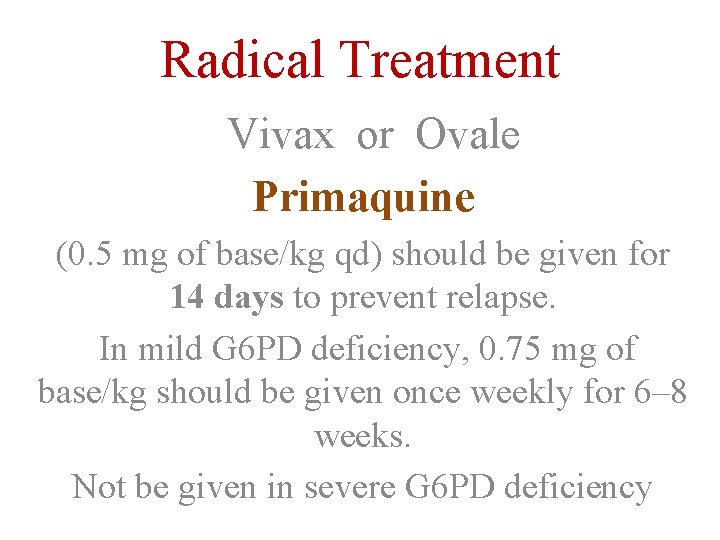
Radical Treatment Vivax or Ovale Primaquine (0. 5 mg of base/kg qd) should be given for 14 days to prevent relapse. In mild G 6 PD deficiency, 0. 75 mg of base/kg should be given once weekly for 6– 8 weeks. Not be given in severe G 6 PD deficiency
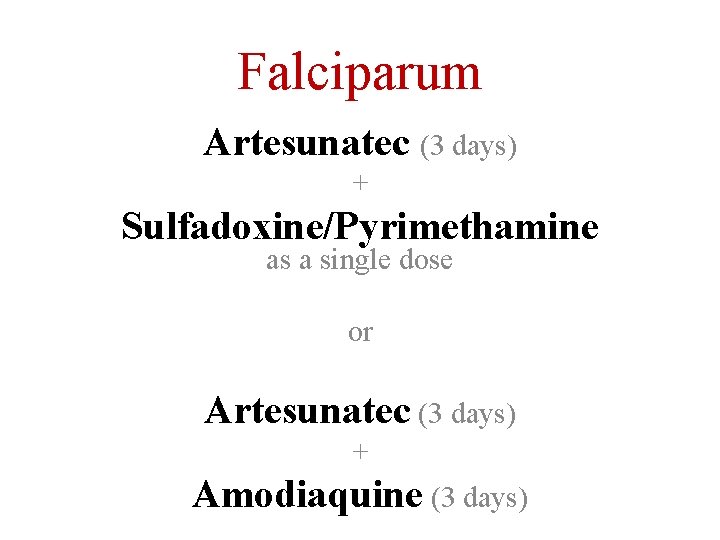
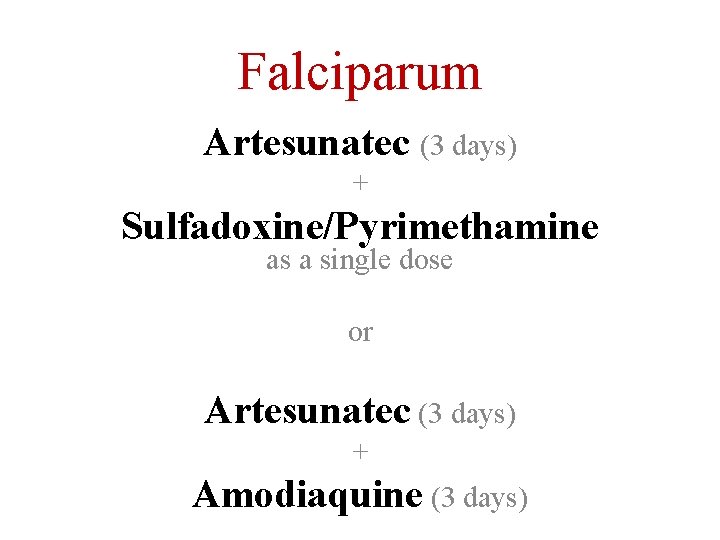
Falciparum Artesunatec (3 days) + Sulfadoxine/Pyrimethamine as a single dose or Artesunatec (3 days) + Amodiaquine (3 days)
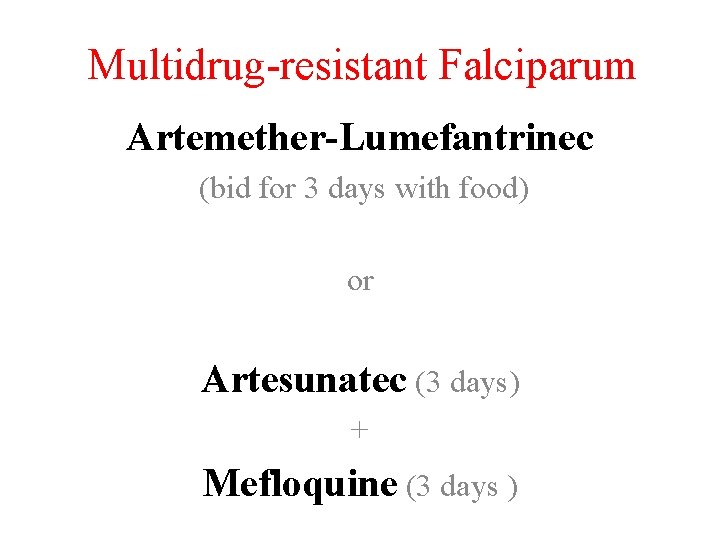
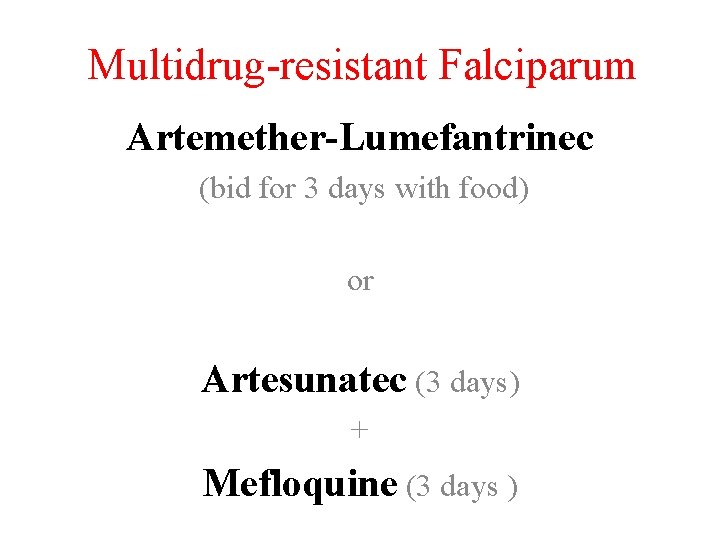
Multidrug-resistant Falciparum Artemether-Lumefantrinec (bid for 3 days with food) or Artesunatec (3 days) + Mefloquine (3 days )
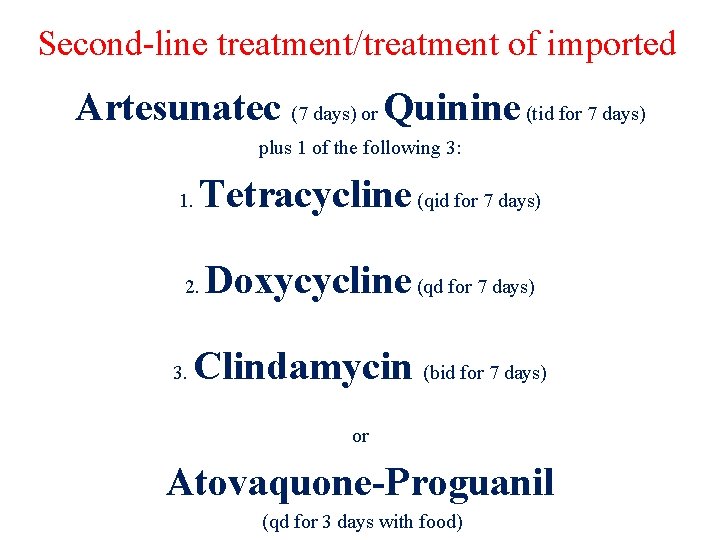
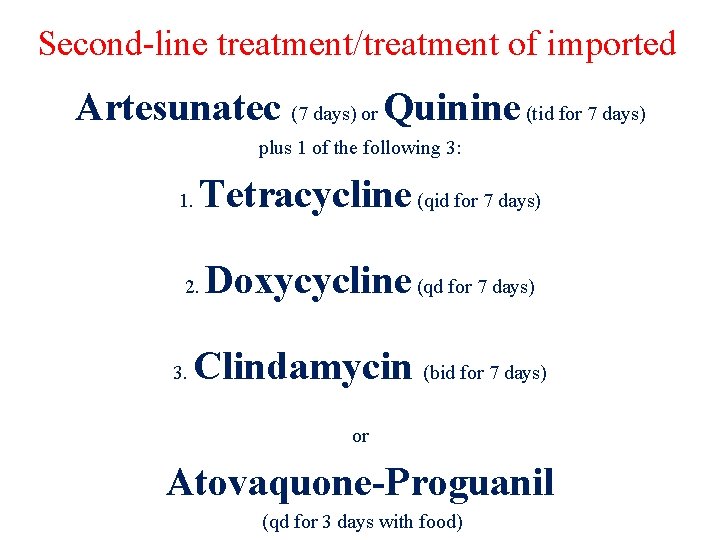
Second-line treatment/treatment of imported Artesunatec (7 days) or Quinine (tid for 7 days) plus 1 of the following 3: 1. Tetracycline (qid for 7 days) 2. 3. Doxycycline (qd for 7 days) Clindamycin (bid for 7 days) or Atovaquone-Proguanil (qd for 3 days with food)
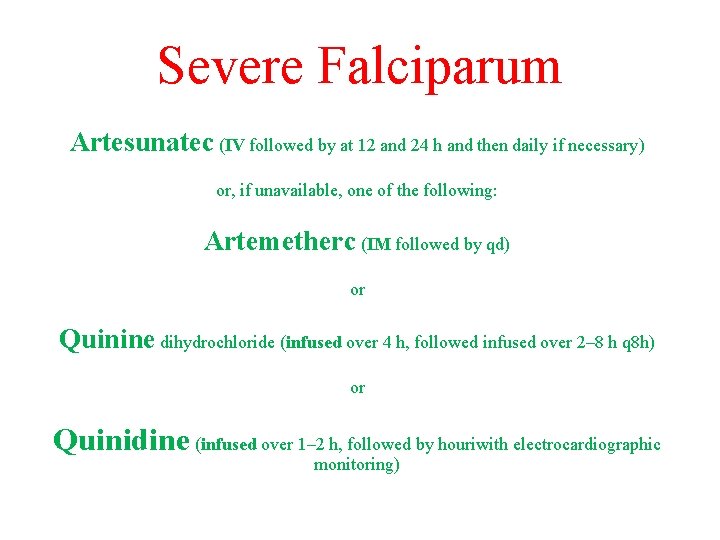
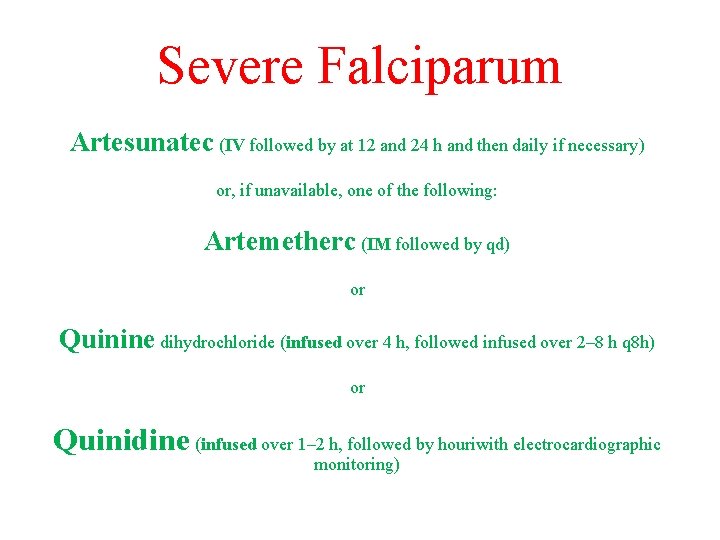
Severe Falciparum Artesunatec (IV followed by at 12 and 24 h and then daily if necessary) or, if unavailable, one of the following: Artemetherc (IM followed by qd) or Quinine dihydrochloride (infused over 4 h, followed infused over 2– 8 h q 8 h) or Quinidine (infused over 1– 2 h, followed by houriwith electrocardiographic monitoring)
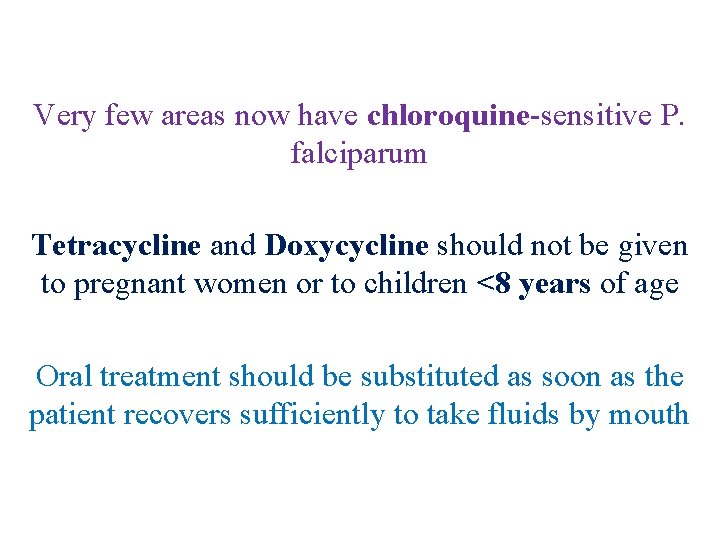
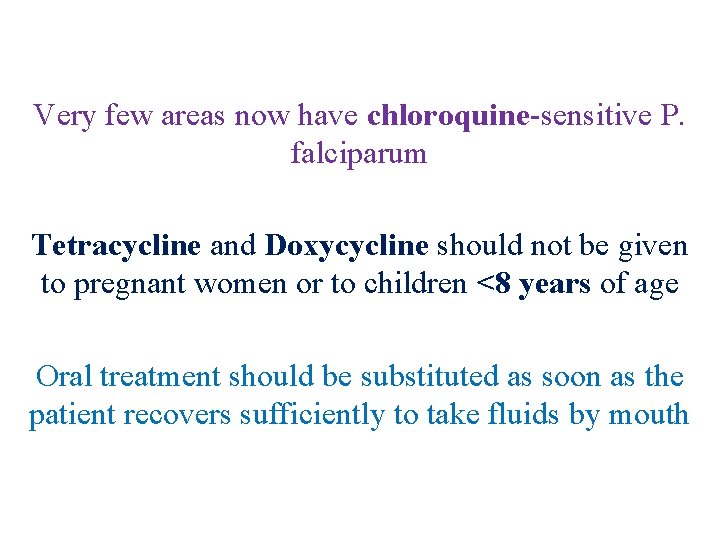
Very few areas now have chloroquine-sensitive P. falciparum Tetracycline and Doxycycline should not be given to pregnant women or to children <8 years of age Oral treatment should be substituted as soon as the patient recovers sufficiently to take fluids by mouth
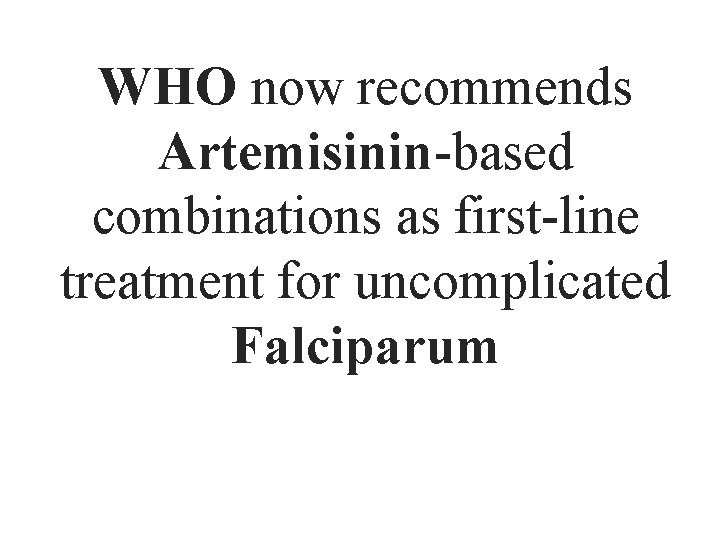
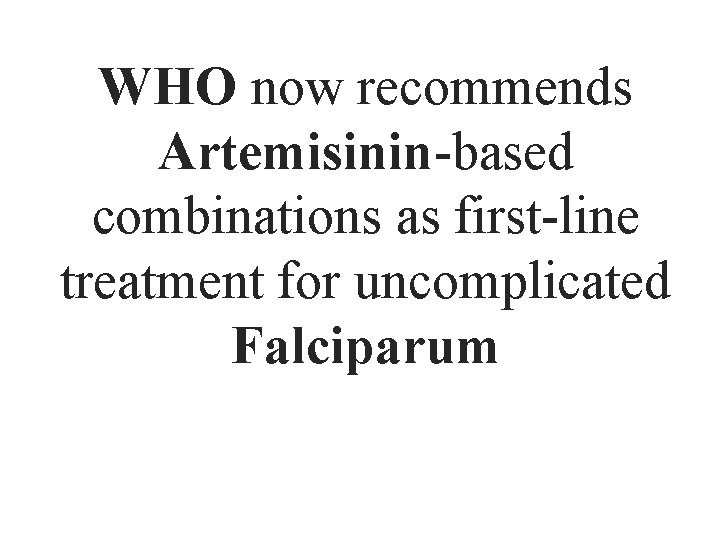
WHO now recommends Artemisinin-based combinations as first-line treatment for uncomplicated Falciparum
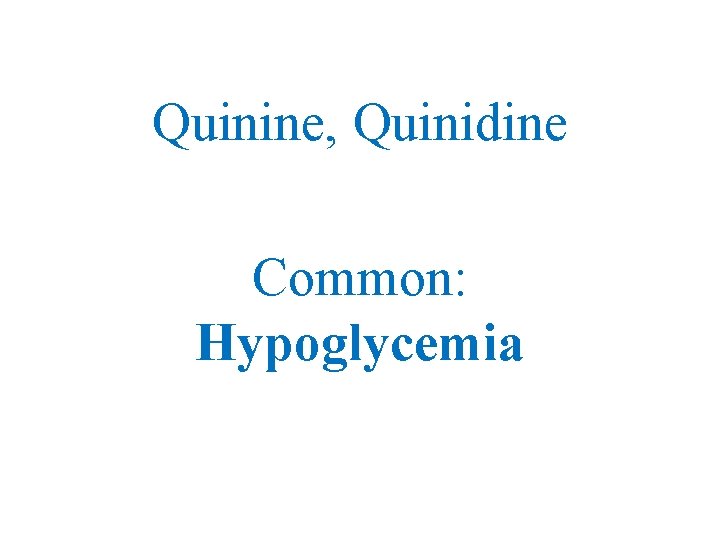
Quinine, Quinidine Common: Hypoglycemia
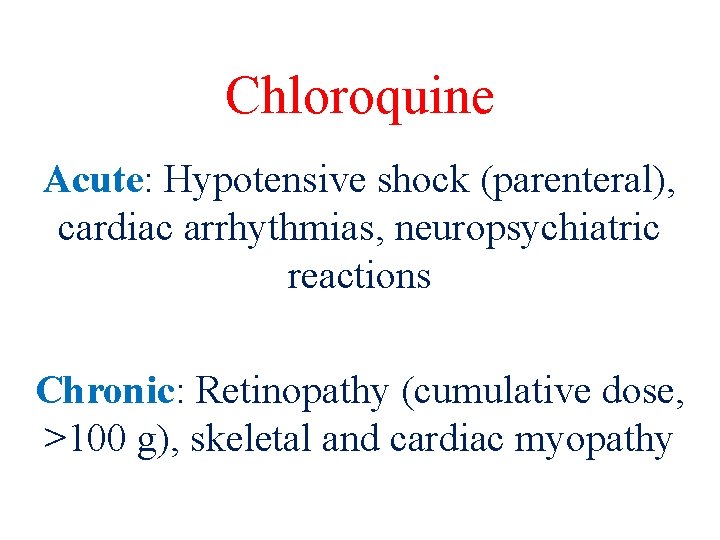
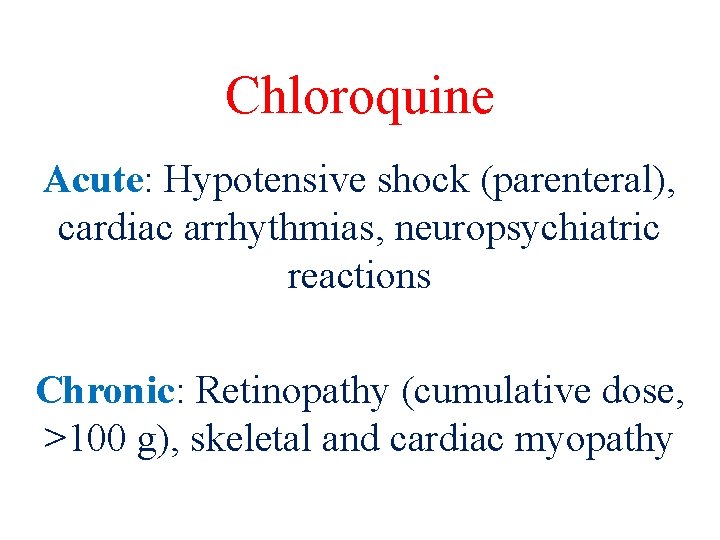
Chloroquine Acute: Hypotensive shock (parenteral), cardiac arrhythmias, neuropsychiatric reactions Chronic: Retinopathy (cumulative dose, >100 g), skeletal and cardiac myopathy
Primaquine Massive hemolysis in subjects with severe G 6 PD deficiency
Severe Malaria
Uncomplicated Malaria
…. . If there is any doubt as to the identity of the infecting malarial species, treatment for falciparum malaria should be given Nonimmune patients receiving treatment , daily parasite counts performed until the thick films are negative. If the level of parasitemia does not fall below 25% of the admission value in 48 h or if parasitemia has not cleared by 7 days (and adherence is assured), drug resistance is likely and the regimen should be changed
Radical Treatment Primaquine (0. 5 mg of base/kg, adult dose) should be given daily for 14 days to patients with P. vivax or P. ovale infections after laboratory tests for G 6 PD deficiency have proved negative. If the patient has a mild variant of G 6 PD deficiency, primaquine can be given in a dose of 0. 75 mg of base/kg (45 mg maximum) once weekly for 6 weeks.
Radical Treatment Pregnant women with vivax or ovale malaria should not be given Primaquine but should receive suppressive prophylaxis with Chloroquine (5 mg of base/kg per week) until delivery, after which radical treatment can be given.
Complications Acute Renal Failure Acute Pulmonary Edema (Acute Respiratory Distress Syndrome) Hypoglycemia Spontaneous Bleeding Convulsions Aspiration pneumonia Bacterial Sepsis
Prevention no safe, effective, long-lasting vaccine is likely to be available for general use in the near future
Personal Protection Against Avoidance of exposure to mosquitoes at their peak feeding times (usually dusk to dawn) Insect repellents containing 10– 35% DEET (or, if DEET is unacceptable, 7% Picaridin), Suitable Clothing Insecticide-impregnated bed nets or other materials. Widespread use of bed nets treated with residual Pyrethroids reduces the incidence of malaria in areas where vectors bite indoors at night
Chemoprophylaxis is never entirely reliable Chloroquine phosphate Atovaquone-Proguanil (Malarone) Doxycycline Mefloquine













 Pvifa equation
Pvifa equation 360-108-108
360-108-108 Bharathi viswanathan
Bharathi viswanathan Thick and thin malaria smear
Thick and thin malaria smear Tuberculosis cutanea
Tuberculosis cutanea Icd 10 malaria falciparum
Icd 10 malaria falciparum Cheryl cole malaria
Cheryl cole malaria Sporontocides
Sporontocides Causative agent malaria
Causative agent malaria Plasmodium sp doença
Plasmodium sp doença Obat malaria dhp
Obat malaria dhp Schistomomiasis
Schistomomiasis Malaria in pregnancy definition
Malaria in pregnancy definition Skizont
Skizont Etiologia de malaria
Etiologia de malaria Surveilans terpadu adalah
Surveilans terpadu adalah Plasmodium vivax forma infectante
Plasmodium vivax forma infectante Cause of splenomegaly in malaria
Cause of splenomegaly in malaria Thick and thin malaria smear
Thick and thin malaria smear Plasmodium species malaria
Plasmodium species malaria Malaria
Malaria History of malaria
History of malaria Schuffner dots malaria
Schuffner dots malaria Epidemiological triad
Epidemiological triad Quartan malaria nephropathy
Quartan malaria nephropathy Algid malaria
Algid malaria Malaria parasite in thick film
Malaria parasite in thick film Malaria
Malaria Malaria references
Malaria references Dot
Dot Complicated malaria
Complicated malaria Malaria and dengue
Malaria and dengue Malaria prophylaxis
Malaria prophylaxis Class of sporozoa
Class of sporozoa Falciparum
Falciparum Cause of splenomegaly in malaria
Cause of splenomegaly in malaria Makalah surveilans malaria
Makalah surveilans malaria Malaria in uganda facts
Malaria in uganda facts Pbf staining
Pbf staining Costa rica malaria
Costa rica malaria Imep full form in malaria
Imep full form in malaria Plazmodium
Plazmodium Malaria life cycle
Malaria life cycle Site:slidetodoc.com
Site:slidetodoc.com Malaria in pregnancy definition
Malaria in pregnancy definition Mp test for malaria
Mp test for malaria Cause of splenomegaly in malaria
Cause of splenomegaly in malaria Malaria
Malaria 648 factor tree
648 factor tree Factors of 108
Factors of 108 Crspd
Crspd 1 mustang way
1 mustang way 4-sinf dars ishlanma ona tili
4-sinf dars ishlanma ona tili 1. 4-1 work together, p. 97
1. 4-1 work together, p. 97 Lcm of 108
Lcm of 108 Phy 108
Phy 108 108 x 300
108 x 300 Aadac recovery centre
Aadac recovery centre Hasil dari 108+132-134
Hasil dari 108+132-134 şura ismi
şura ismi Prime factorization of 144 using exponents
Prime factorization of 144 using exponents 192,168,1,108
192,168,1,108 Engineering 108.com
Engineering 108.com 108 vaishnava temples
108 vaishnava temples 466560/108
466560/108 Gcf of 18 and 36
Gcf of 18 and 36 Convention 108 data protection
Convention 108 data protection Right hand rule 3
Right hand rule 3 Maximo comun divisor mcd
Maximo comun divisor mcd Round the factors and estimate the products exit ticket
Round the factors and estimate the products exit ticket Plain scale can measure upto
Plain scale can measure upto Simplifying radicals calculator
Simplifying radicals calculator 108 mln km to km
108 mln km to km Prime numbers from 1 to 100
Prime numbers from 1 to 100 105 106 107
105 106 107 Dante's inferno xxx
Dante's inferno xxx Nrs 108
Nrs 108 108 lab
108 lab Mesohippus
Mesohippus 101 102 103 104 105 106 107 108 109 110
101 102 103 104 105 106 107 108 109 110 Multibit synchronizing
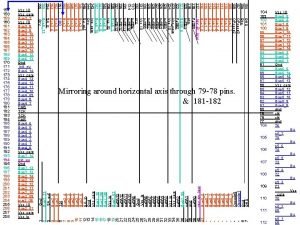
Multibit synchronizing Corso toscana 108
Corso toscana 108 Lcm and gcm
Lcm and gcm Muhasebe örnek monografi
Muhasebe örnek monografi 108 semester
108 semester How celebrate new year in different countries
How celebrate new year in different countries Japan neighboring countries
Japan neighboring countries Countries near fiji
Countries near fiji First wolrd countries
First wolrd countries Who was in wwi
Who was in wwi Wallace's line
Wallace's line Few countries are as great as india
Few countries are as great as india We learn more different countries
We learn more different countries Fumigation certificate sri lanka
Fumigation certificate sri lanka What is a developing country definition
What is a developing country definition Neighbouring countries of france
Neighbouring countries of france Countries in the baltic sea region
Countries in the baltic sea region Why are some countries poorer than others
Why are some countries poorer than others Where does the mekong river flow
Where does the mekong river flow Warsaw pact countries
Warsaw pact countries Countries that border afghanistan
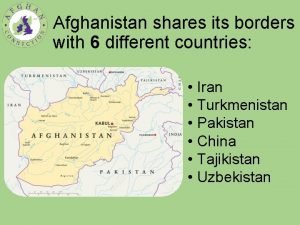
Countries that border afghanistan How did wwi begin
How did wwi begin