Lesson 1 Fundamentals of Nutrition Mimi Giri MD



























- Slides: 75
Lesson 1 Fundamentals of Nutrition Mimi Giri, MD, Ph. D Department of Endocrinology, University Hospital of Ghent, Belgium
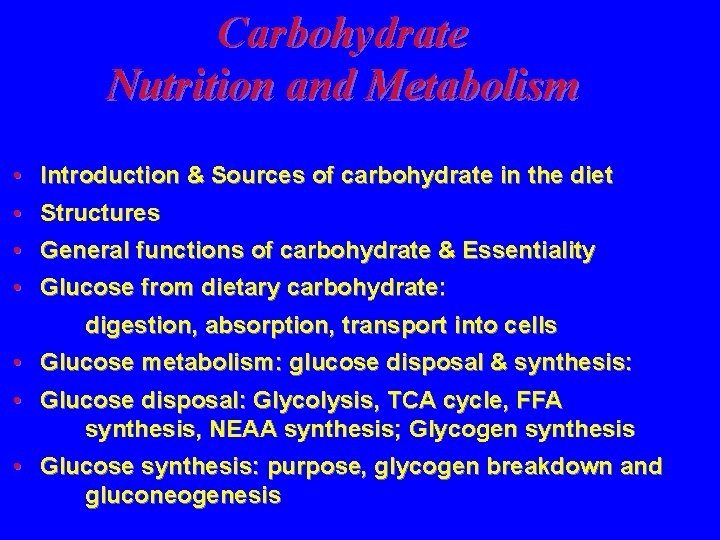
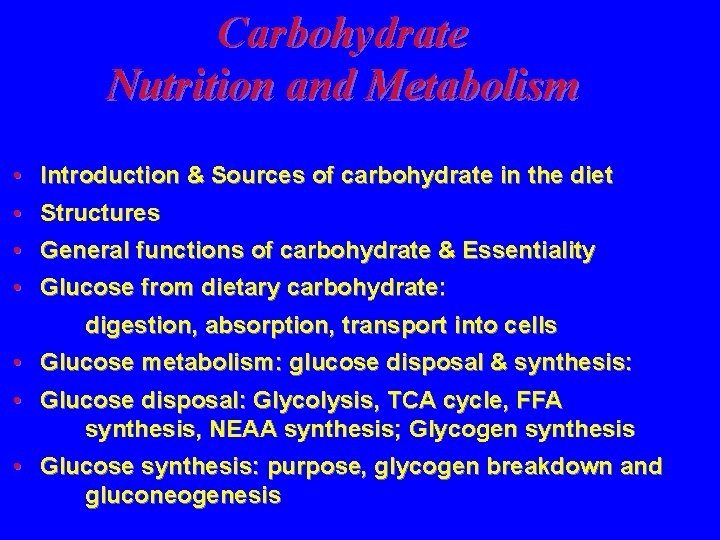
Carbohydrate Nutrition and Metabolism • Introduction & Sources of carbohydrate in the diet • Structures • General functions of carbohydrate & Essentiality • Glucose from dietary carbohydrate: digestion, absorption, transport into cells • Glucose metabolism: glucose disposal & synthesis: • Glucose disposal: Glycolysis, TCA cycle, FFA synthesis, NEAA synthesis; Glycogen synthesis • Glucose synthesis: purpose, glycogen breakdown and gluconeogenesis
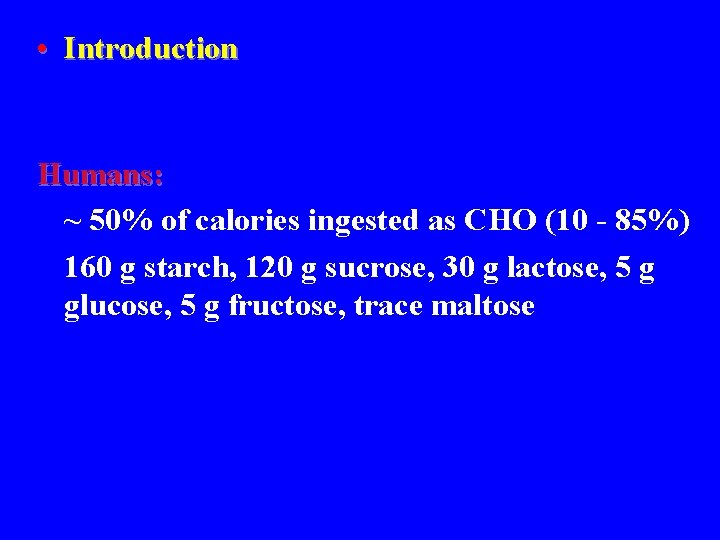
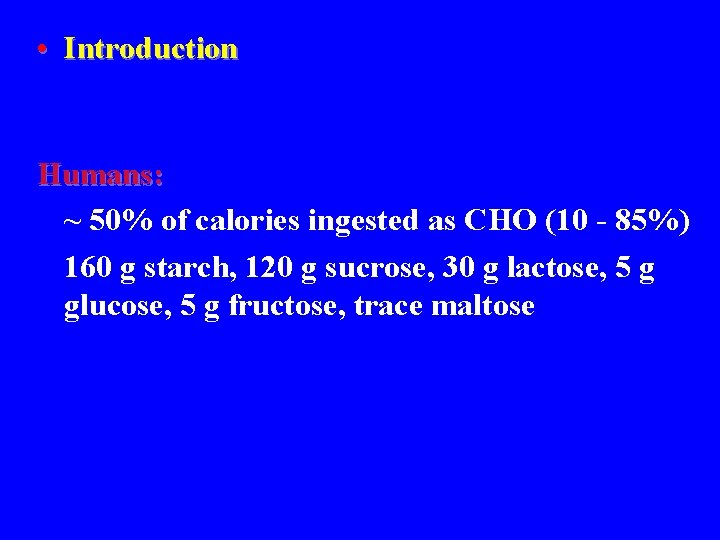
• Introduction Humans: ~ 50% of calories ingested as CHO (10 - 85%) 160 g starch, 120 g sucrose, 30 g lactose, 5 g glucose, 5 g fructose, trace maltose

• Introduction Sources of carbohydrate: sucrose: “sugar” lactose: milk maltose: beer fructose: fruit, corn-syrup “processed foods” starch (amylose & amylopectin): wheat, rice, corn, barley, oats, legumes. . glycogen: muscle and liver
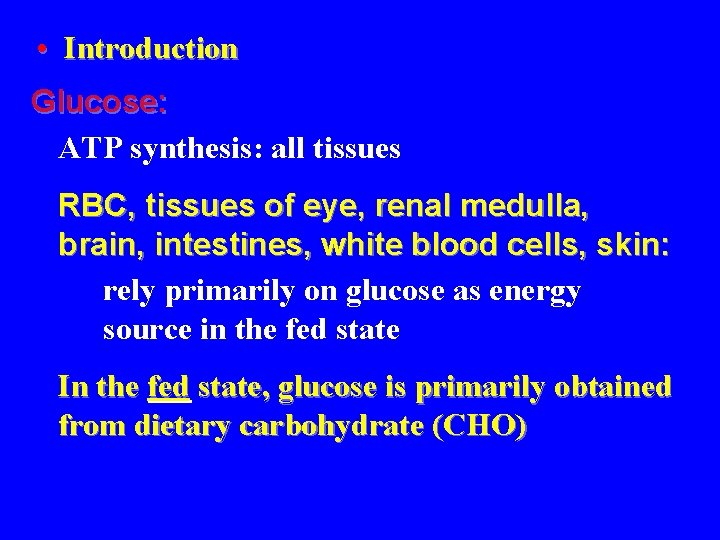
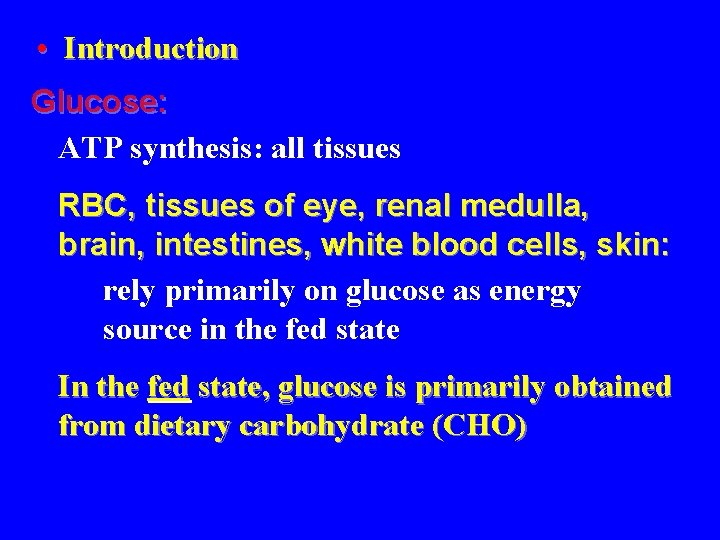
• Introduction Glucose: ATP synthesis: all tissues RBC, tissues of eye, renal medulla, brain, intestines, white blood cells, skin: rely primarily on glucose as energy source in the fed state In the fed state, glucose is primarily obtained from dietary carbohydrate (CHO)
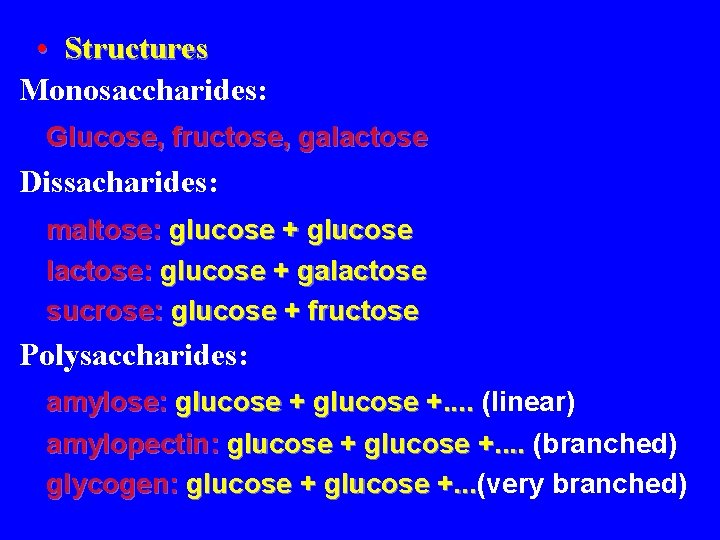
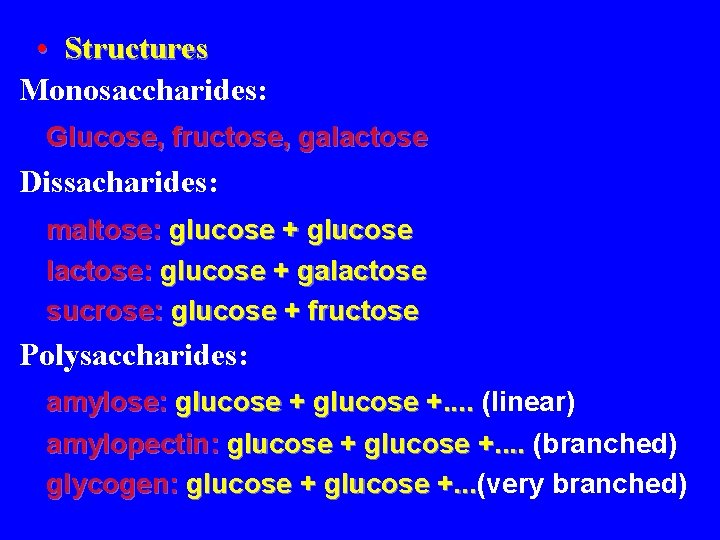
• Structures Monosaccharides: Glucose, fructose, galactose Dissacharides: maltose: glucose + glucose lactose: glucose + galactose sucrose: glucose + fructose Polysaccharides: amylose: glucose +. . (linear) amylopectin: glucose +. . (branched) glycogen: glucose +. . . (very branched) +. . .

• General functions of carbohydrates Energy: ATP synthesis (~ 4 kcal/g) NEAA synthesis: carbon skeleton Fat synthesis: via acetyl-Co. A Glycogen synthesis TCA cycle intermediates Nucleotides: sugar portion Glycoproteins Glycolipids
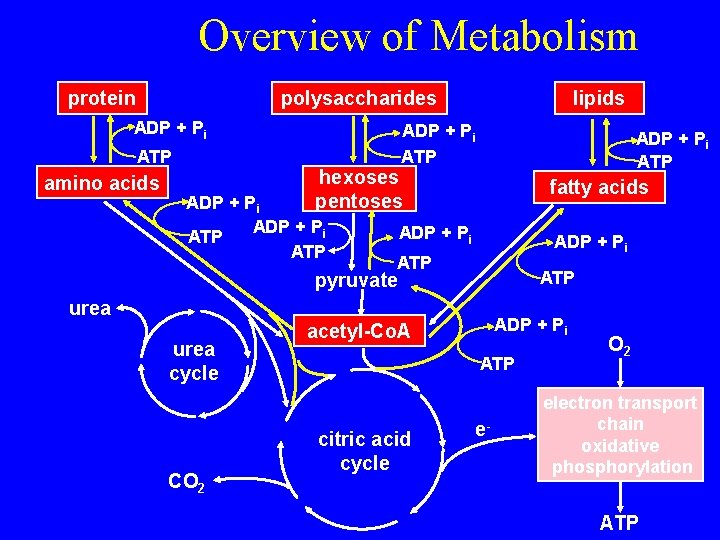
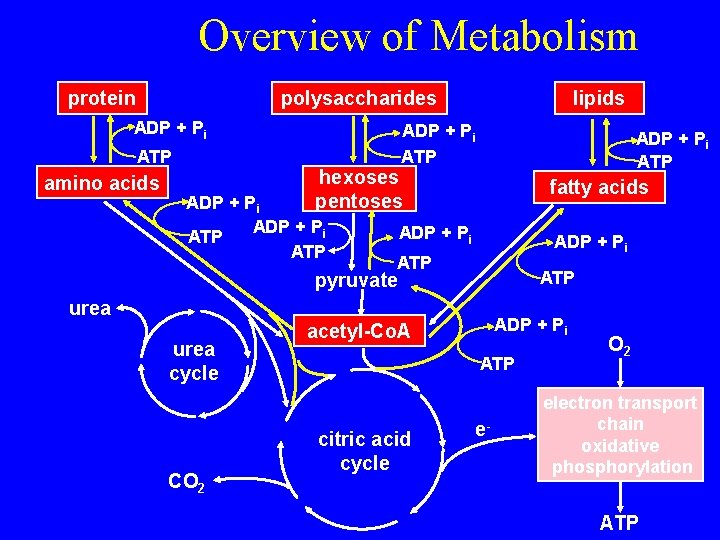
Overview of Metabolism protein polysaccharides ADP + Pi ATP amino acids lipids ADP + Pi ATP hexoses pentoses ADP + Pi ATP fatty acids ADP + Pi ATP pyruvate urea cycle CO 2 ADP + Pi acetyl-Co. A ATP citric acid cycle e- O 2 electron transport chain oxidative phosphorylation ATP

Overview of Catabolic Processes Proteins Fats Carbohydrates Stage 1 Amino acids Fatty acids Simple Sugars Glycolysis Pyruvate ATP Stage 2 Acetyl Co. A Citric acid cycle Oxidative phosphorylation ATP Stage 3
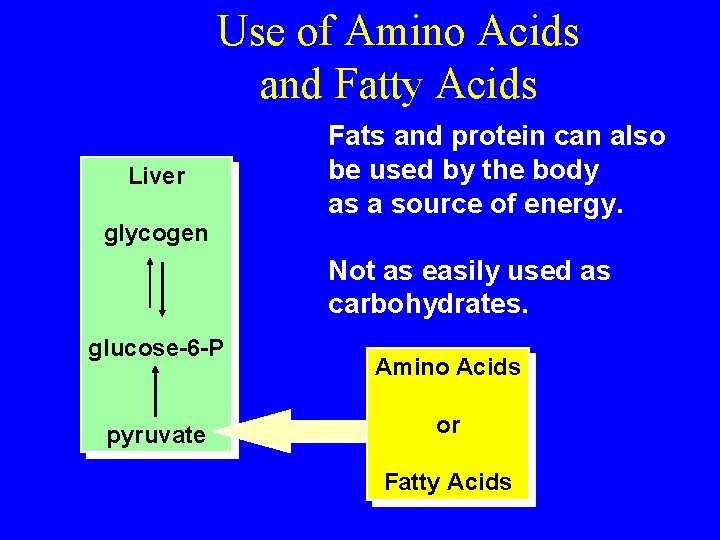
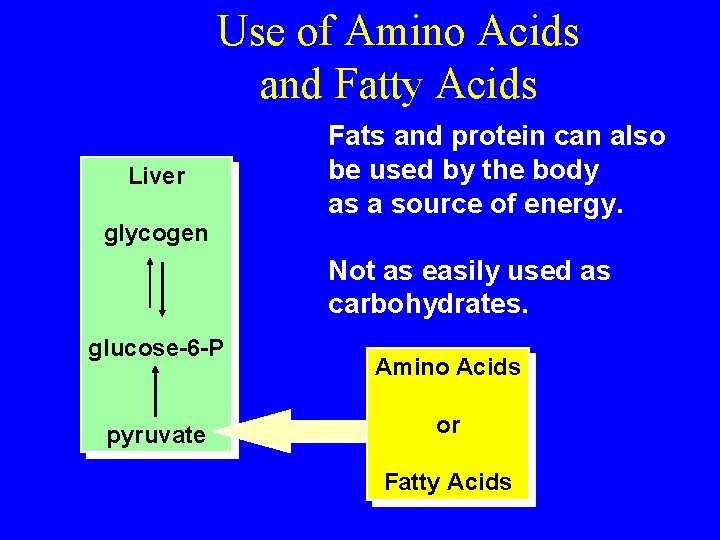
Use of Amino Acids and Fatty Acids Liver Fats and protein can also be used by the body as a source of energy. glycogen Not as easily used as carbohydrates. glucose-6 -P pyruvate Amino Acids or Fatty Acids
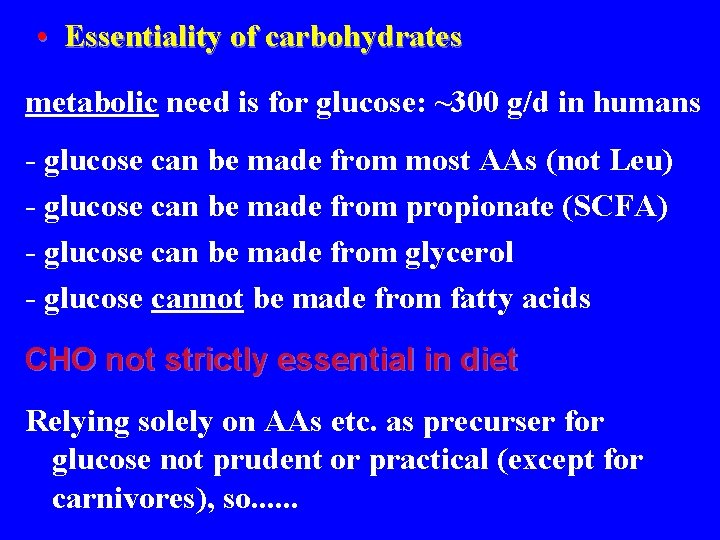
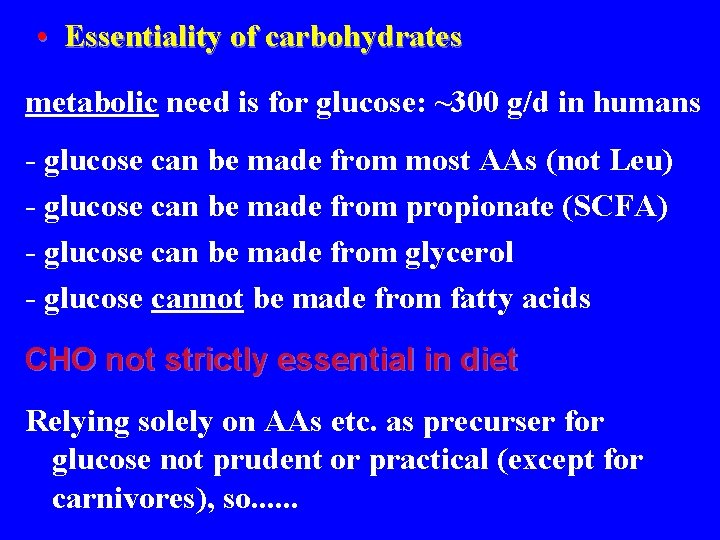
• Essentiality of carbohydrates metabolic need is for glucose: ~300 g/d in humans - glucose can be made from most AAs (not Leu) - glucose can be made from propionate (SCFA) - glucose can be made from glycerol - glucose cannot be made from fatty acids CHO not strictly essential in diet Relying solely on AAs etc. as precurser for glucose not prudent or practical (except for carnivores), so. . .

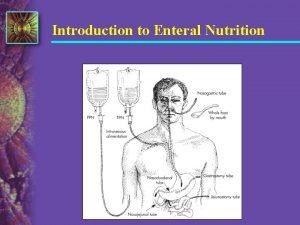
• Glucose from dietary carbohydrate: DIGESTION, ABSORPTION & TRANSPORT into cells Mouth salivary amylase: - hydrolyzes 1 -4 bonds in starch - release: psychic (cephalic) stimuli mechanical stimuli: food in mouth chemical stimuli: food on taste buds - little digestion Stomach: Stomach Negligible
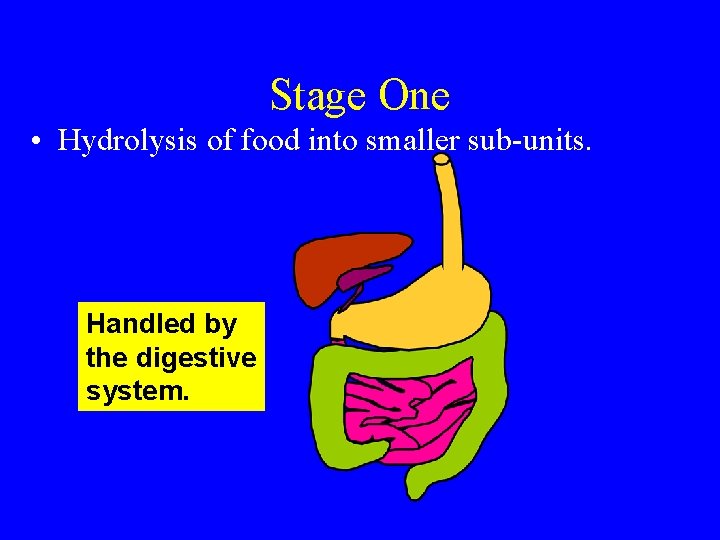
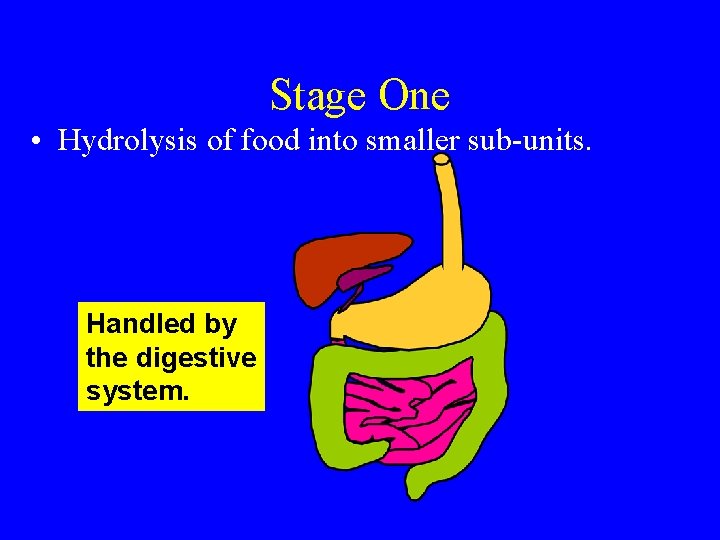
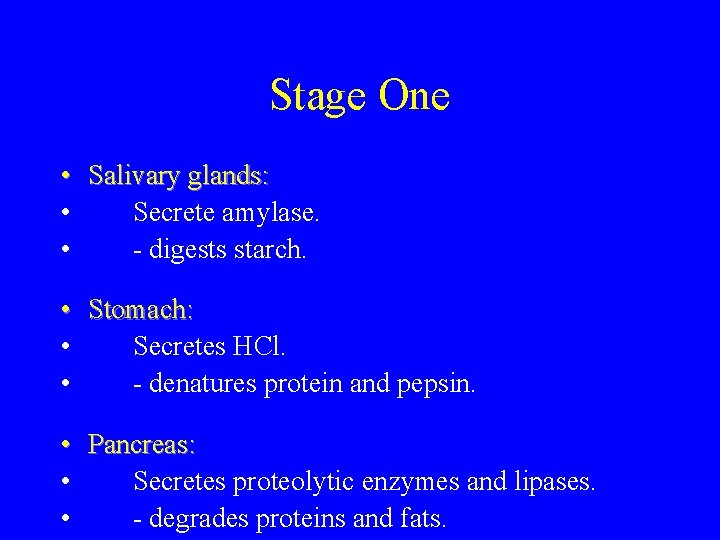
Stage One • Hydrolysis of food into smaller sub-units. Handled by the digestive system.
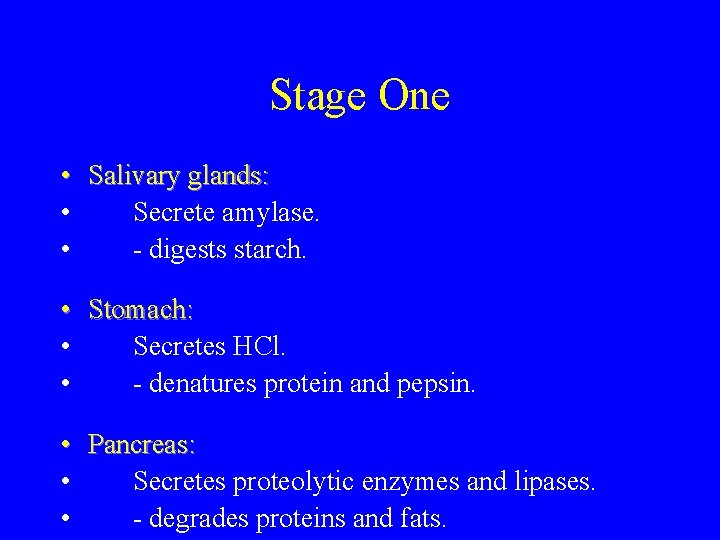
Stage One • Salivary glands: • Secrete amylase. • - digests starch. • Stomach: • Secretes HCl. • - denatures protein and pepsin. • Pancreas: • Secretes proteolytic enzymes and lipases. • - degrades proteins and fats.

Stage One • Liver and gallbladder: • Deliver bile salts. • - emulsify fat globules - easier to digest. • Small intestine: • Further degradation. • Produces amino acids, hexose sugars, fatty acids and glycerol. • Moves materials into blood for transport to cells.

• CHO: Digestion, Absorption & Transport Small Intestine brush border lumen

CHO Digestion: SMALL INTESTINE LUMEN lumen CCK pancreas digesta enzymes CCK = cholecystekinin
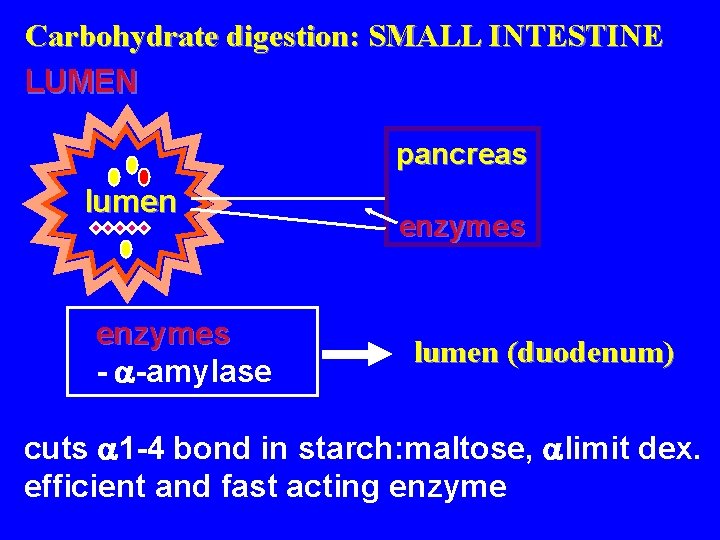
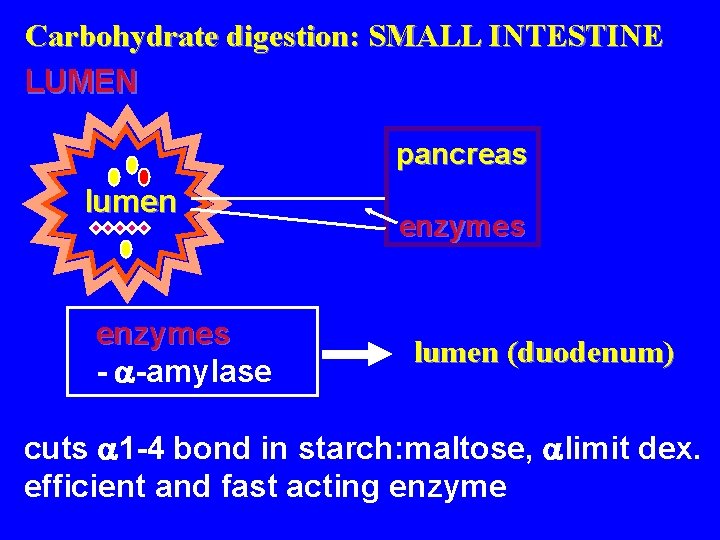
Carbohydrate digestion: SMALL INTESTINE LUMEN pancreas lumen enzymes - -amylase enzymes lumen (duodenum) cuts 1 -4 bond in starch: maltose, limit dex. efficient and fast acting enzyme
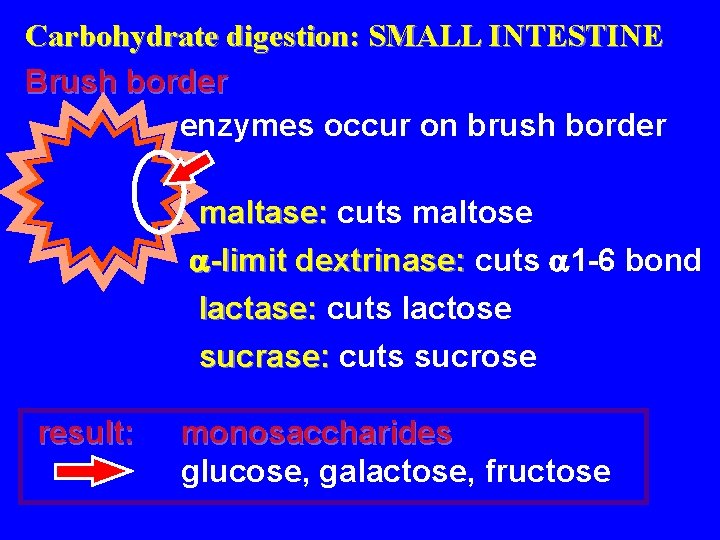
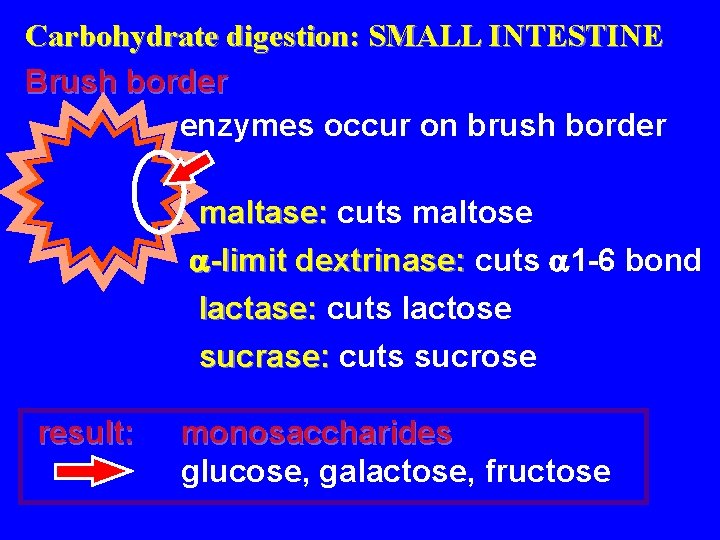
Carbohydrate digestion: SMALL INTESTINE Brush border enzymes occur on brush border maltase: cuts maltose -limit dextrinase: cuts 1 -6 bond lactase: cuts lactose sucrase: cuts sucrose result: monosaccharides glucose, galactose, fructose
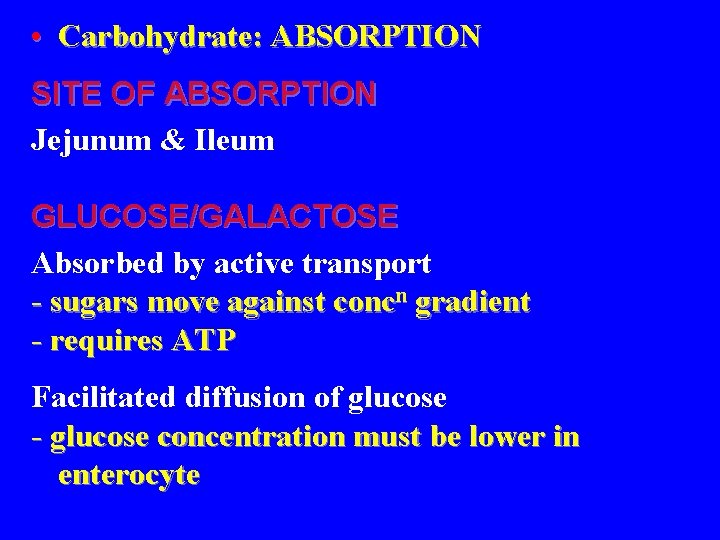
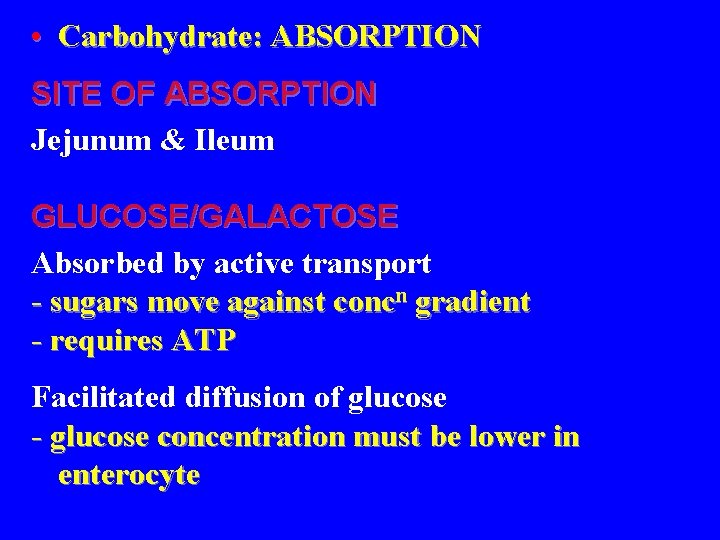
• Carbohydrate: ABSORPTION SITE OF ABSORPTION Jejunum & Ileum GLUCOSE/GALACTOSE Absorbed by active transport - sugars move against concn gradient - requires ATP Facilitated diffusion of glucose - glucose concentration must be lower in enterocyte
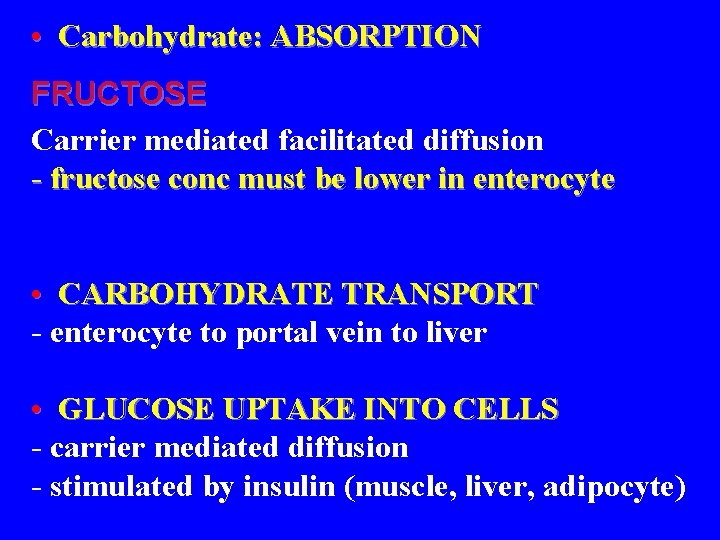
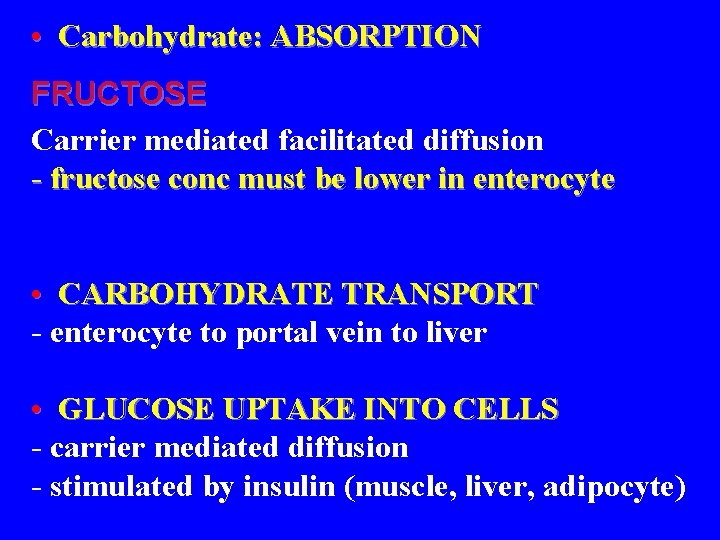
• Carbohydrate: ABSORPTION FRUCTOSE Carrier mediated facilitated diffusion - fructose conc must be lower in enterocyte • CARBOHYDRATE TRANSPORT - enterocyte to portal vein to liver • GLUCOSE UPTAKE INTO CELLS - carrier mediated diffusion - stimulated by insulin (muscle, liver, adipocyte)

• Carbohydrate metabolism: FRUCTOSE liver: fructose F-6 -P GALACTOSE liver: galactose gal-1 -P DHAP G-1 -P glycolytic pathway G-6 -P glucose
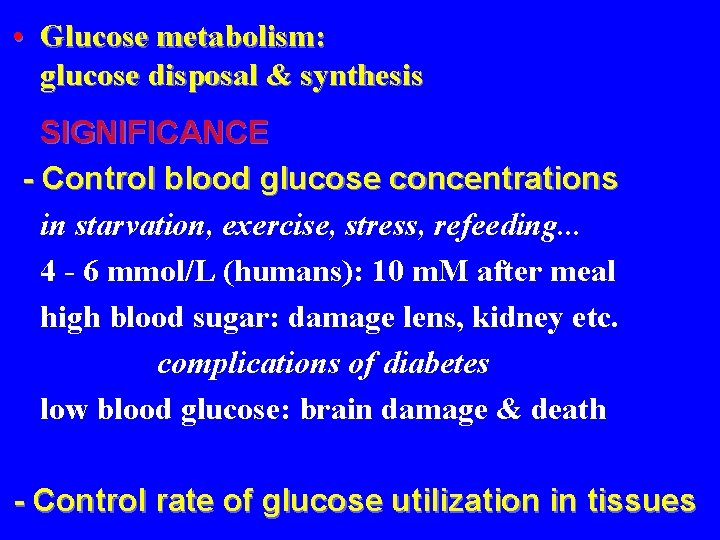
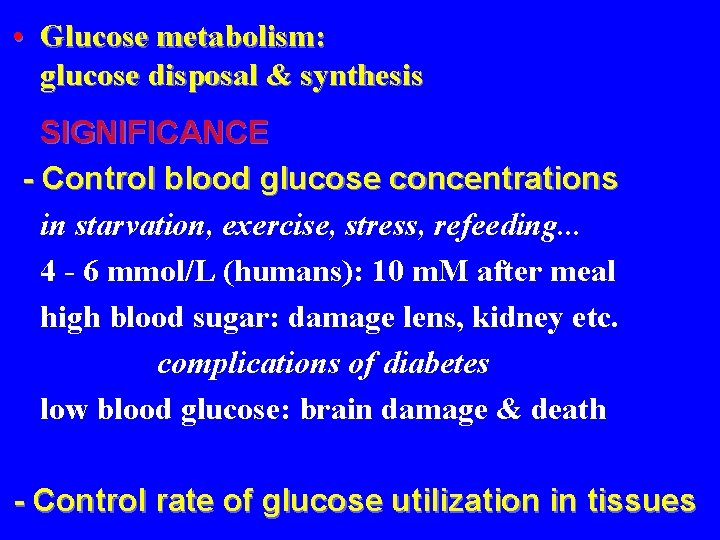
• Glucose metabolism: glucose disposal & synthesis SIGNIFICANCE - Control blood glucose concentrations in starvation, exercise, stress, refeeding. . . 4 - 6 mmol/L (humans): 10 m. M after meal high blood sugar: damage lens, kidney etc. complications of diabetes low blood glucose: brain damage & death - Control rate of glucose utilization in tissues

• Control rate of glucose utilization in tissues e. g. How does liver assess how much glucose is being used by muscle or brain? e. g. When a high CHO meal eaten, rate of glucose absorption is high; to maintain normal blood glucose levels, the rate of glucose use in other tissues such as muscle must increase Control & integration of glucose metabolism (disposal & synthesis) among tissues is required Liver plays a major role!!
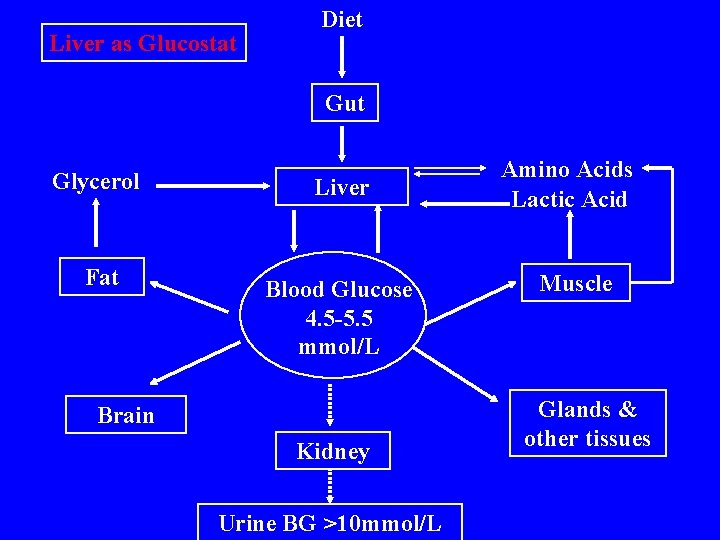
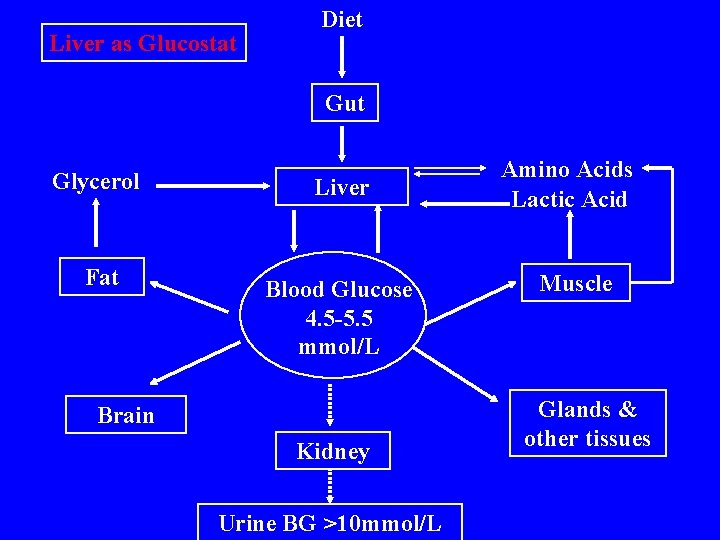
Liver as Glucostat Diet Gut Glycerol Liver Fat Blood Glucose 4. 5 -5. 5 mmol/L Brain Kidney Urine BG >10 mmol/L Amino Acids Lactic Acid Muscle Glands & other tissues

Factors affecting glucose concentration Tend to raise • Hunger • Glucose absorption from gut • Hepatic glycogenolysis – Adrenaline – Glucagon • Gluconeogenesis in liver • Insulin antagonist – Growth Hormone – Cortisol • Insulin destroying enzymes • • Tend to lower Satiety Glucose diffusion in ECF Muscular exercise Insulin – – Glucose oxidation Glycogen deposition Lipogenesis Gluconeogenesis { glucosuria – in diabetes}

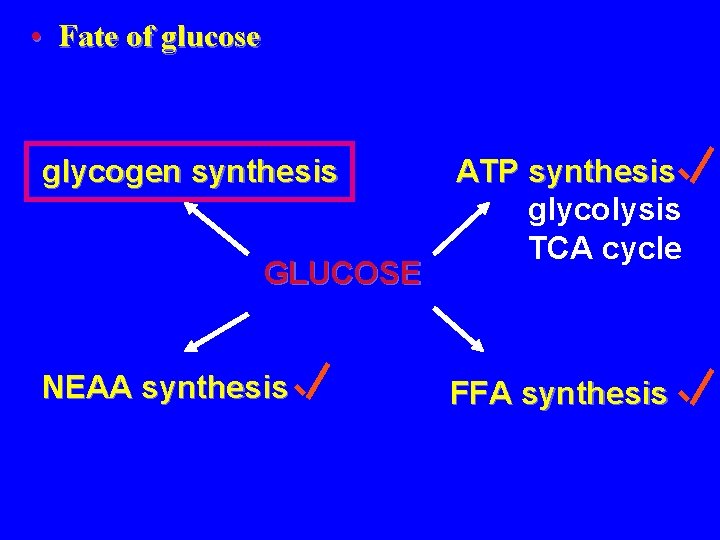
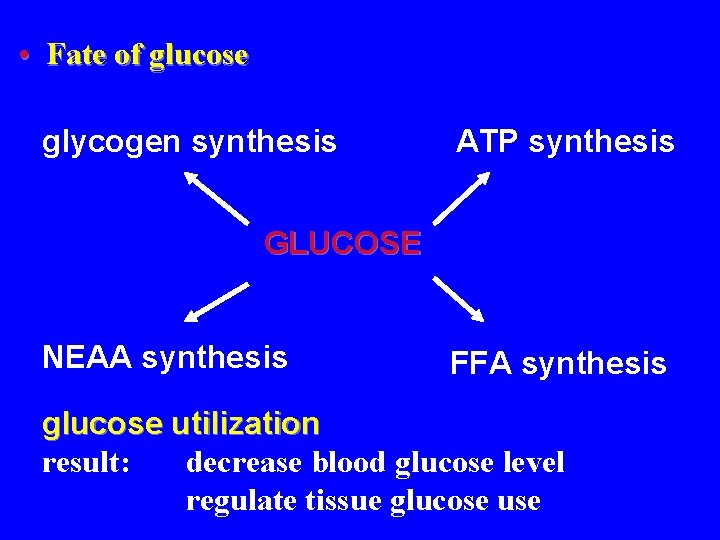
• Fate of glucose glycogen synthesis ATP synthesis GLUCOSE NEAA synthesis FFA synthesis

• Fate of glucose: glycolysis, TCA cycle & FFA synthesis ATP synthesis glucose ATP pyruvate acetyl-Co. A lactate FFA synthesis TCA cycle ATP lots!!
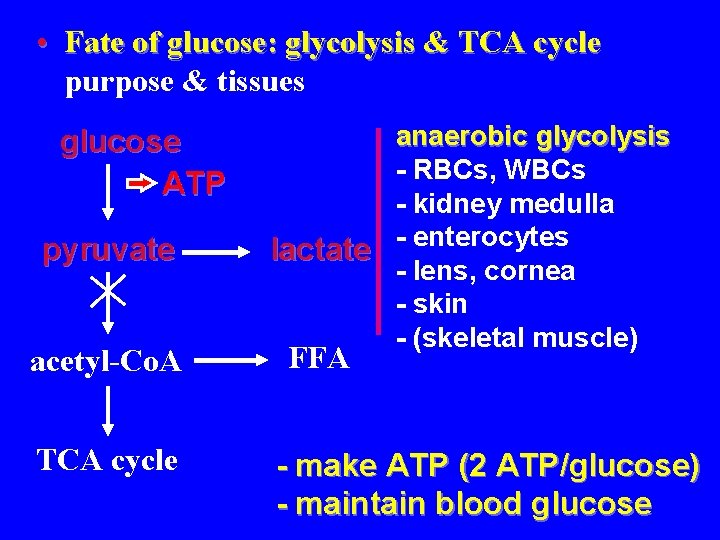
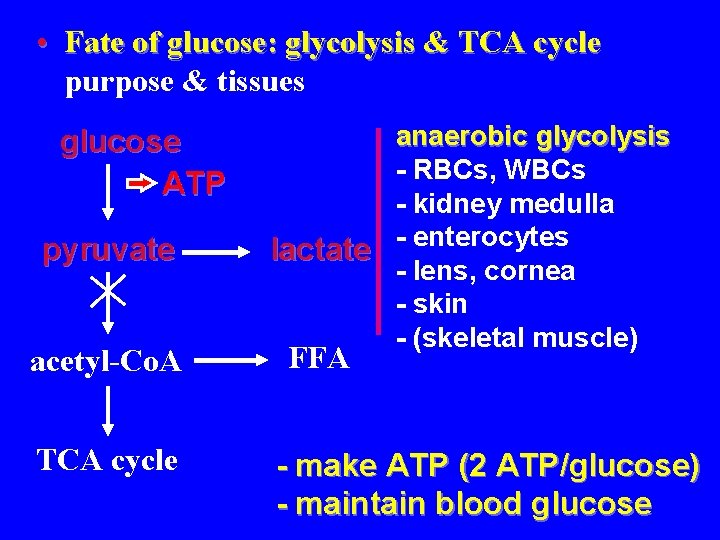
• Fate of glucose: glycolysis & TCA cycle purpose & tissues glucose ATP pyruvate acetyl-Co. A TCA cycle anaerobic glycolysis - RBCs, WBCs - kidney medulla lactate - enterocytes - lens, cornea - skin - (skeletal muscle) FFA - make ATP (2 ATP/glucose) - maintain blood glucose

• Fate of glucose: glycolysis & TCA cycle purpose & tissues glucose ATP pyruvate acetyl-Co. A TCA cycle ATP aerobic glycolysis - brain - liver - skeletal muscle - kidney cortex - etc. - make ATP (32 ATP/glucose) - maintain blood glucose

• Fate of glucose: glycolysis & TCA cycle stimulation and inhibition glucose ATP pyruvate acetyl-Co. A TCA cycle ATP stimulation - high glucose - low ATP lactate - insulin FFA inhibition - high ATP - FFAs
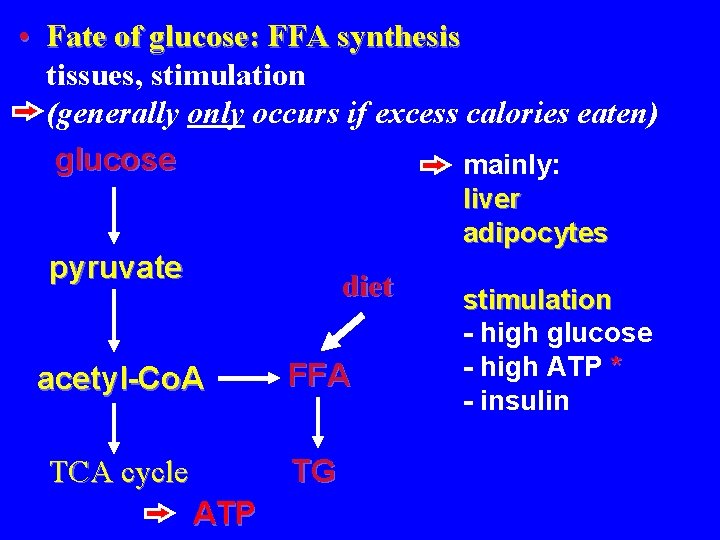
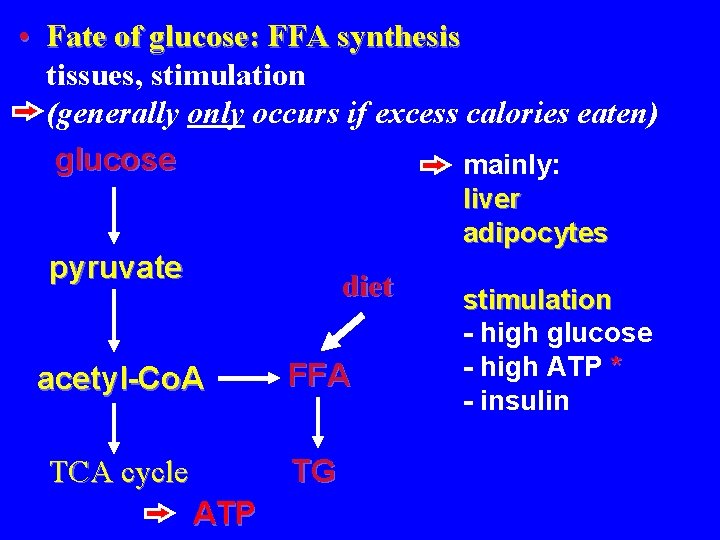
• Fate of glucose: FFA synthesis tissues, stimulation (generally only occurs if excess calories eaten) glucose mainly: liver adipocytes pyruvate diet acetyl-Co. A FFA TCA cycle TG ATP stimulation - high glucose - high ATP * - insulin
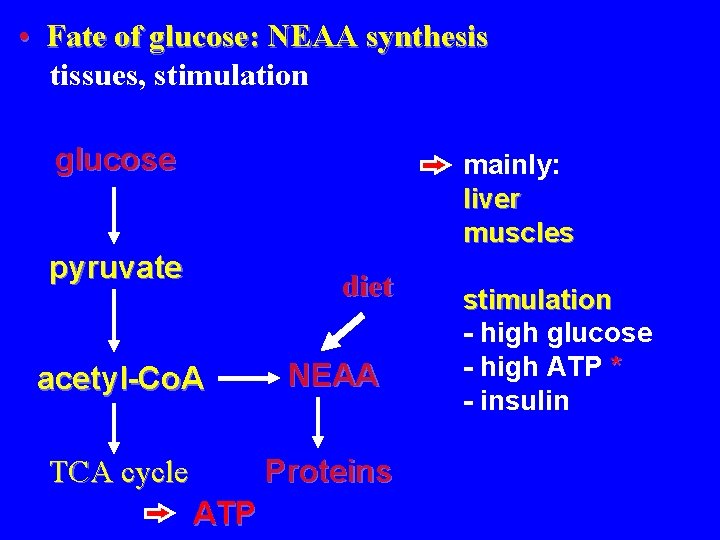
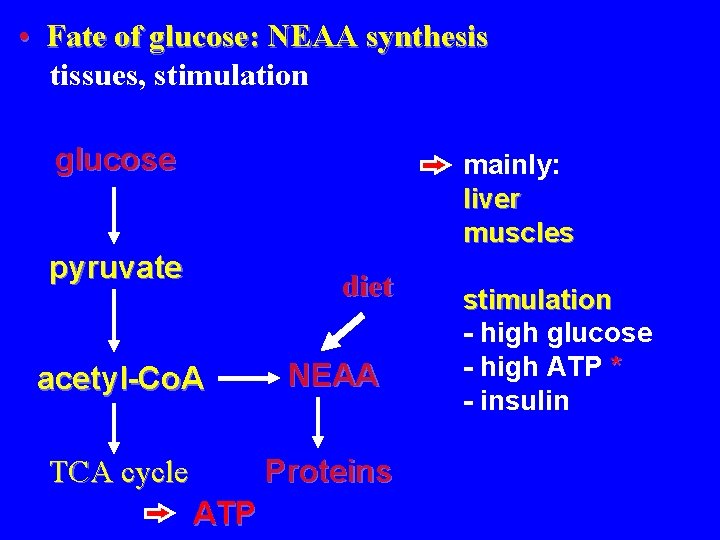
• Fate of glucose: NEAA synthesis tissues, stimulation glucose mainly: liver muscles pyruvate diet acetyl-Co. A NEAA TCA cycle Proteins ATP stimulation - high glucose - high ATP * - insulin
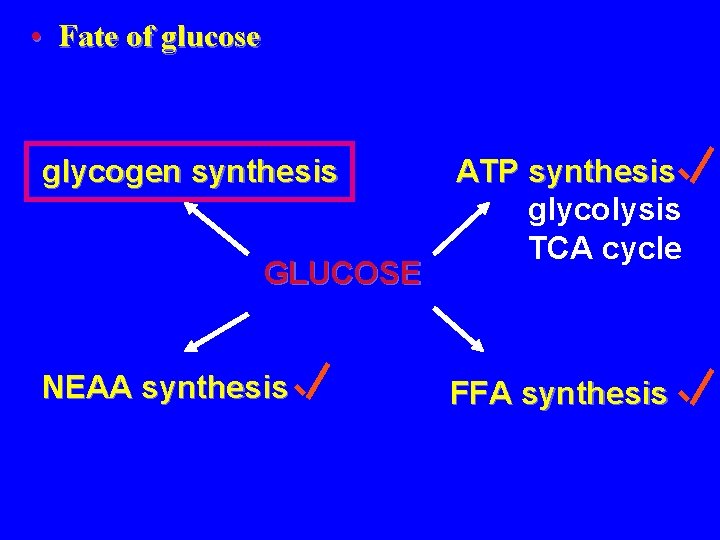
• Fate of glucose glycogen synthesis GLUCOSE NEAA synthesis ATP synthesis glycolysis TCA cycle FFA synthesis
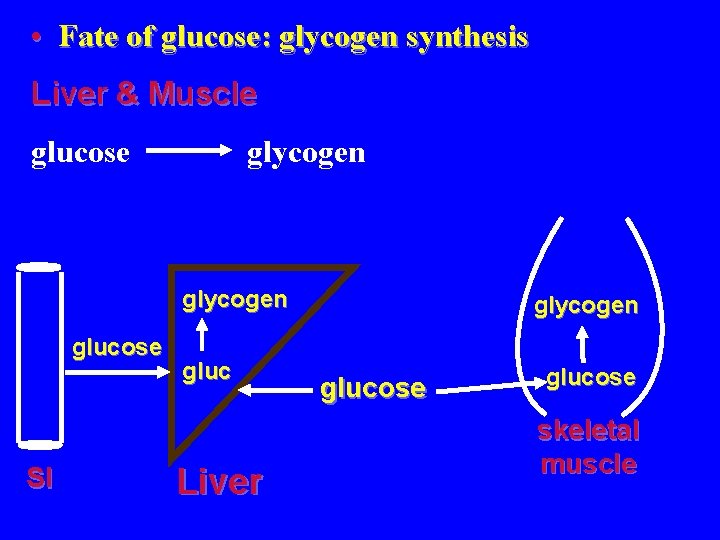
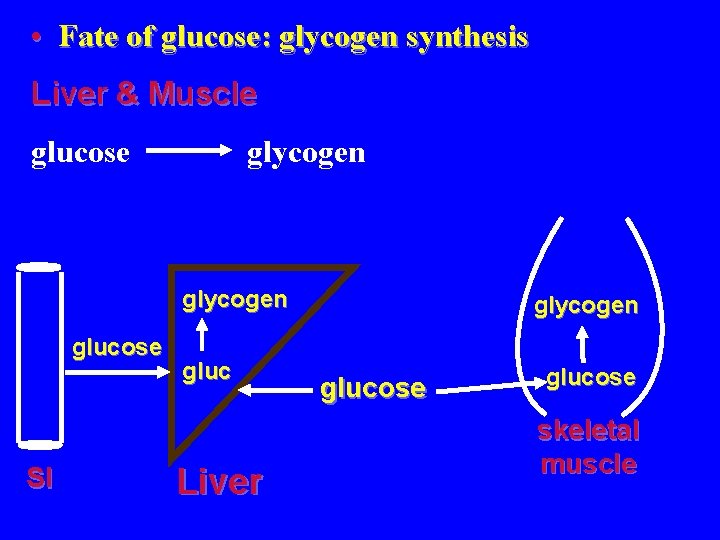
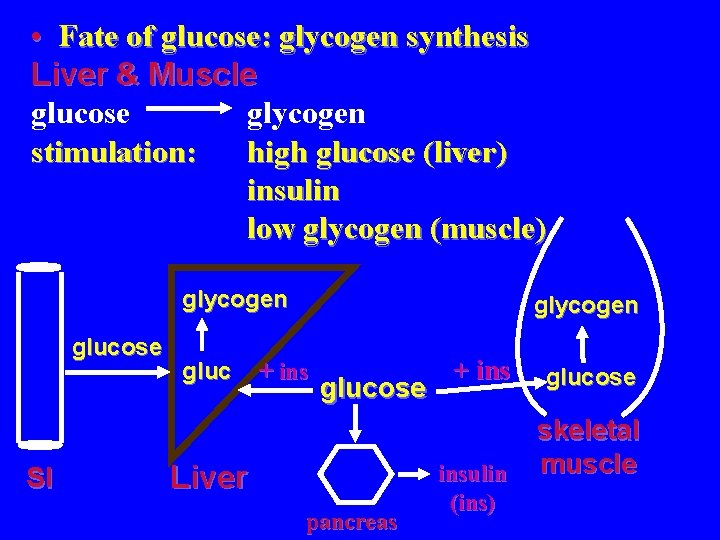
• Fate of glucose: glycogen synthesis Liver & Muscle glucose glycogen glucose SI gluc Liver glycogen glucose skeletal muscle
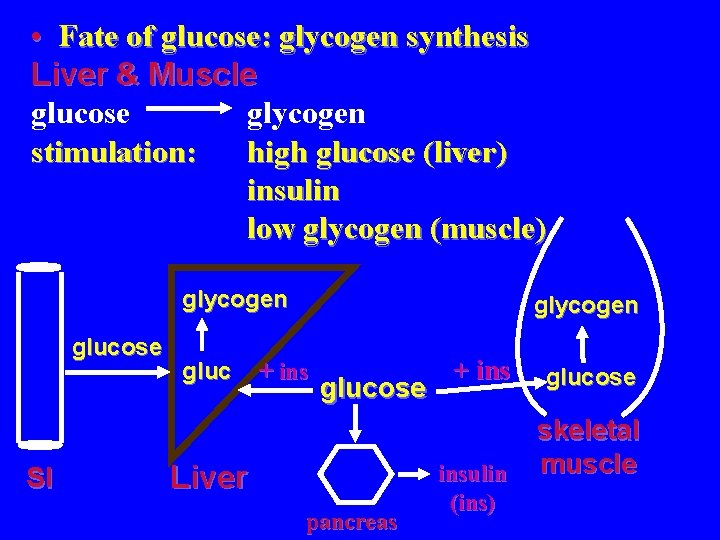
• Fate of glucose: glycogen synthesis Liver & Muscle glucose glycogen stimulation: high glucose (liver) insulin low glycogen (muscle) glycogen glucose SI gluc glycogen + ins glucose Liver pancreas + insulin (ins) glucose skeletal muscle
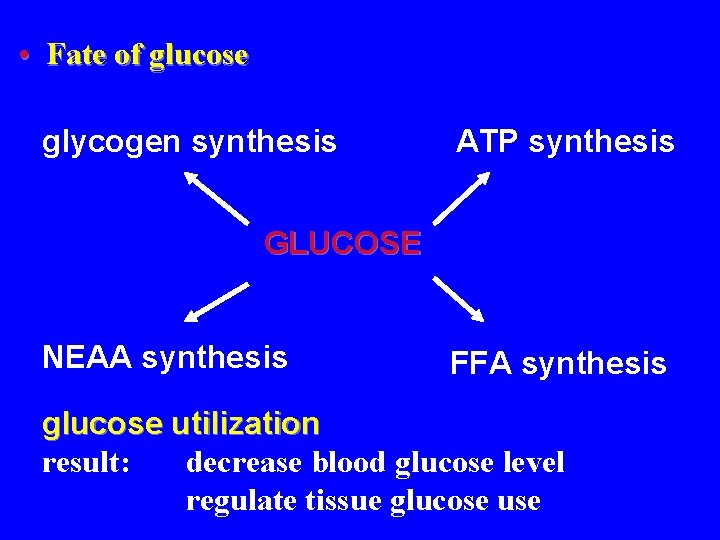
• Fate of glucose glycogen synthesis ATP synthesis GLUCOSE NEAA synthesis FFA synthesis glucose utilization result: decrease blood glucose level regulate tissue glucose use
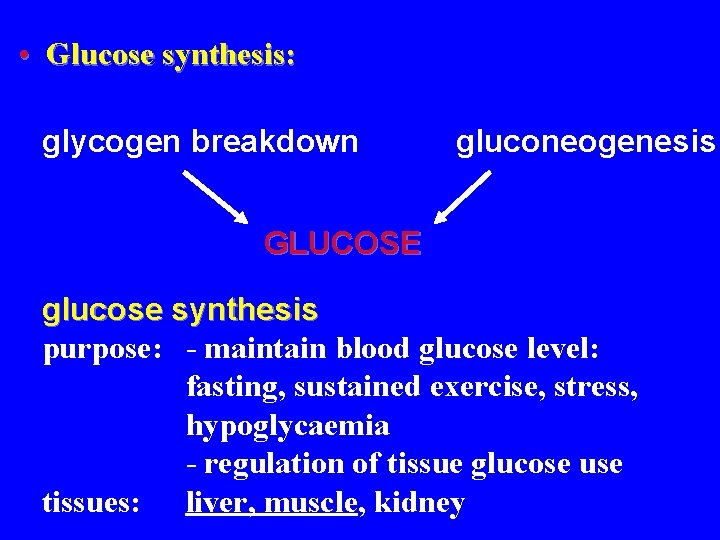
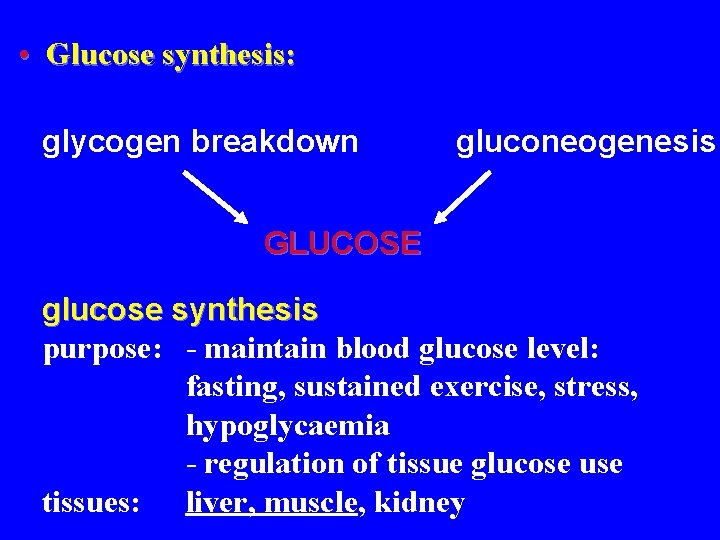
• Glucose synthesis: glycogen breakdown gluconeogenesis GLUCOSE glucose synthesis purpose: - maintain blood glucose level: fasting, sustained exercise, stress, hypoglycaemia - regulation of tissue glucose use tissues: liver, muscle, kidney
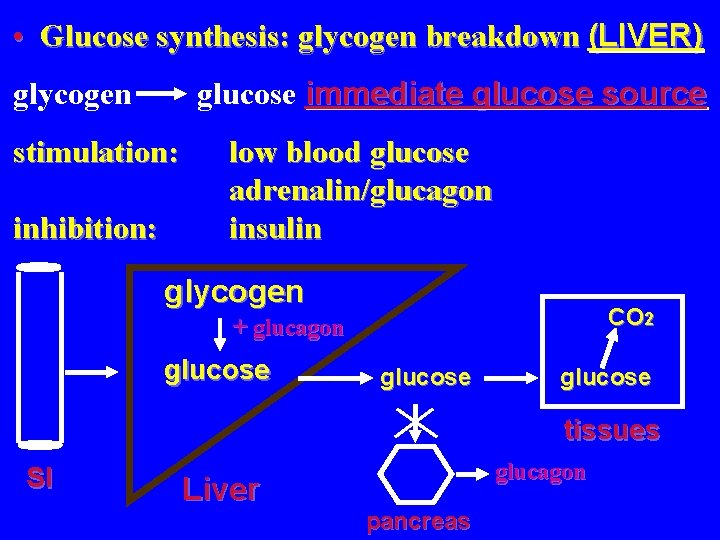
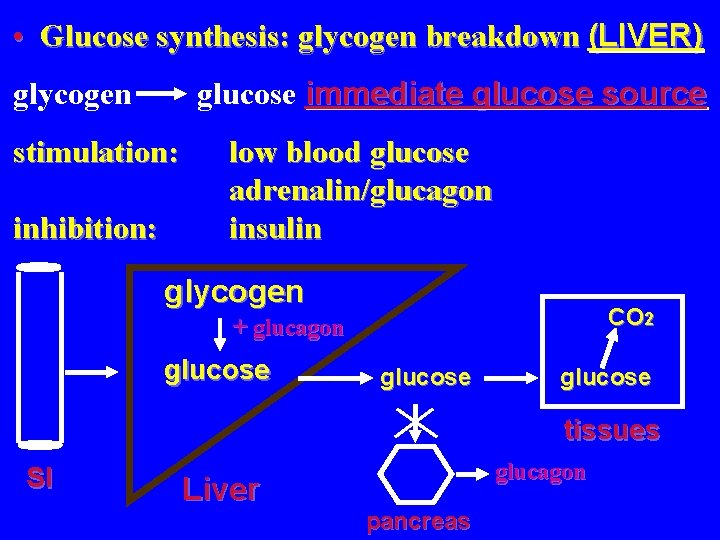
• Glucose synthesis: glycogen breakdown (LIVER) glucose immediate glucose source glycogen stimulation: inhibition: low blood glucose adrenalin/glucagon insulin glycogen CO 2 + glucagon glucose tissues SI Liver glucagon pancreas
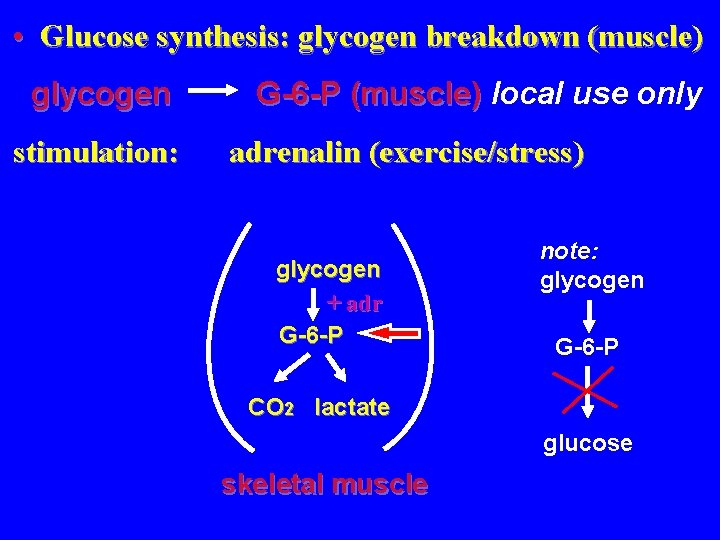
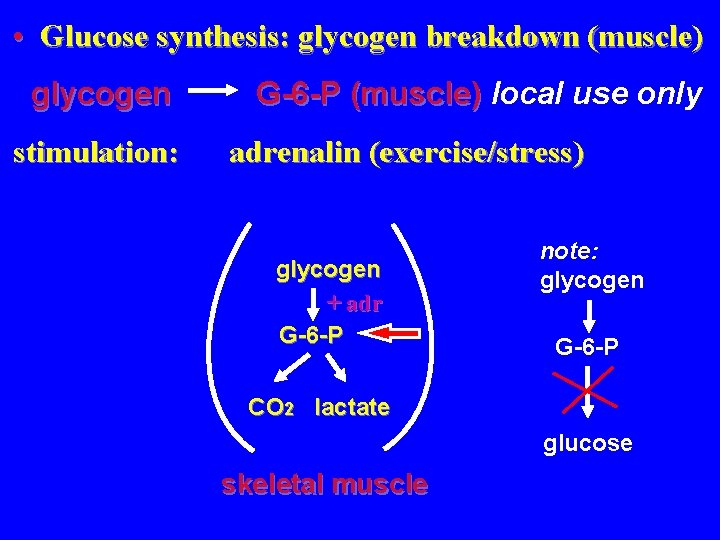
• Glucose synthesis: glycogen breakdown (muscle) glycogen stimulation: G-6 -P (muscle) local use only adrenalin (exercise/stress) glycogen + adr G-6 -P note: glycogen G-6 -P CO 2 lactate glucose skeletal muscle
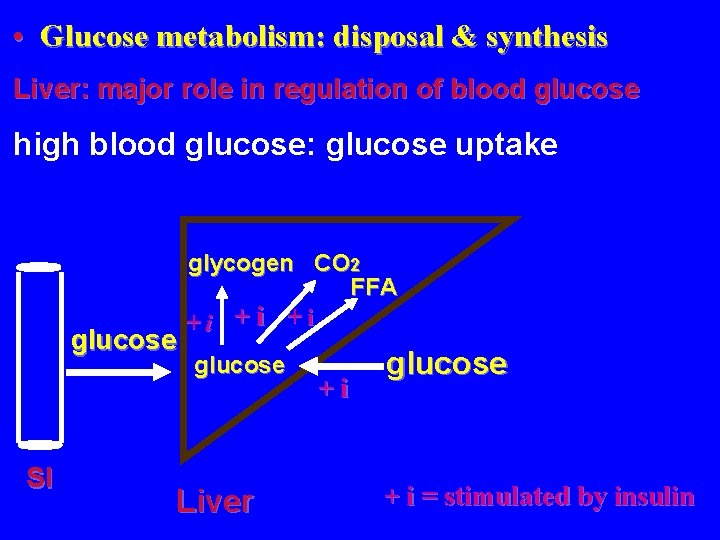
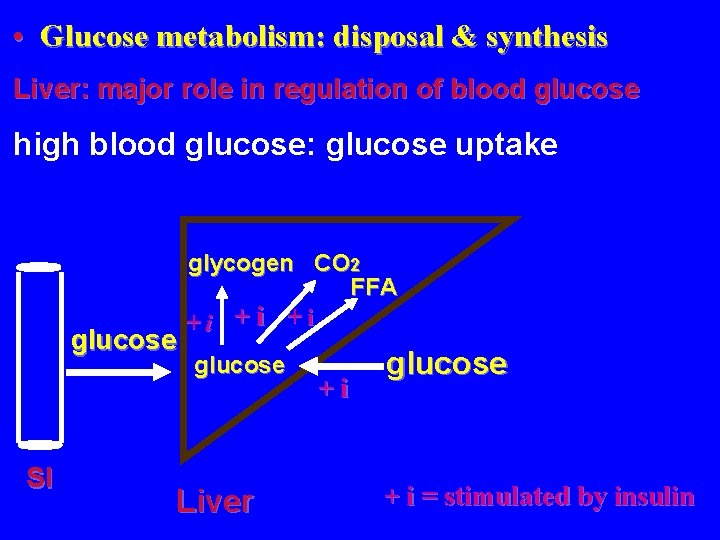
• Glucose metabolism: disposal & synthesis Liver: major role in regulation of blood glucose high blood glucose: glucose uptake glucose SI glycogen CO 2 FFA +i +i +i glucose Liver +i glucose + i = stimulated by insulin
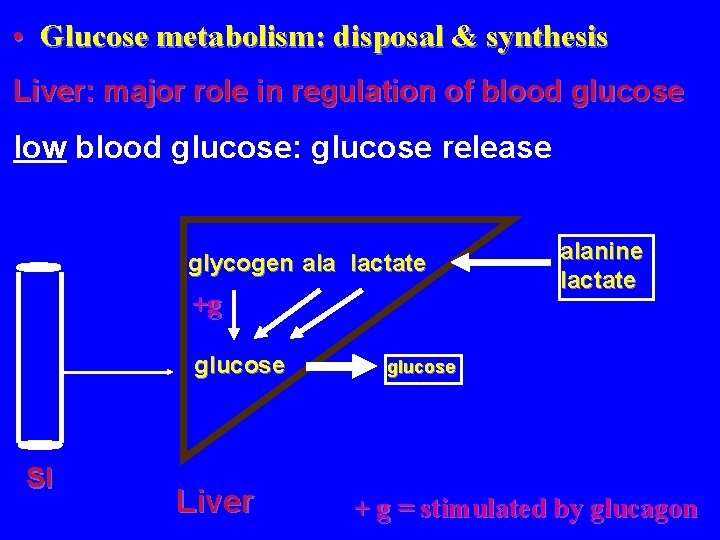
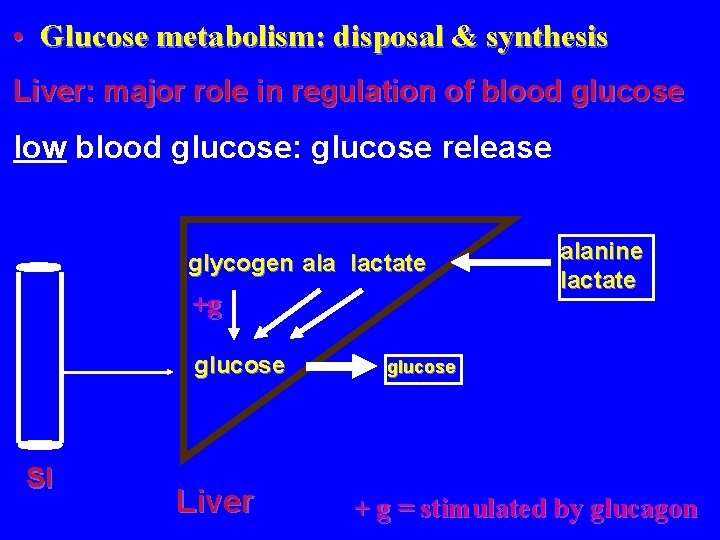
• Glucose metabolism: disposal & synthesis Liver: major role in regulation of blood glucose low blood glucose: glucose release glycogen ala lactate +g glucose SI Liver alanine lactate glucose + g = stimulated by glucagon
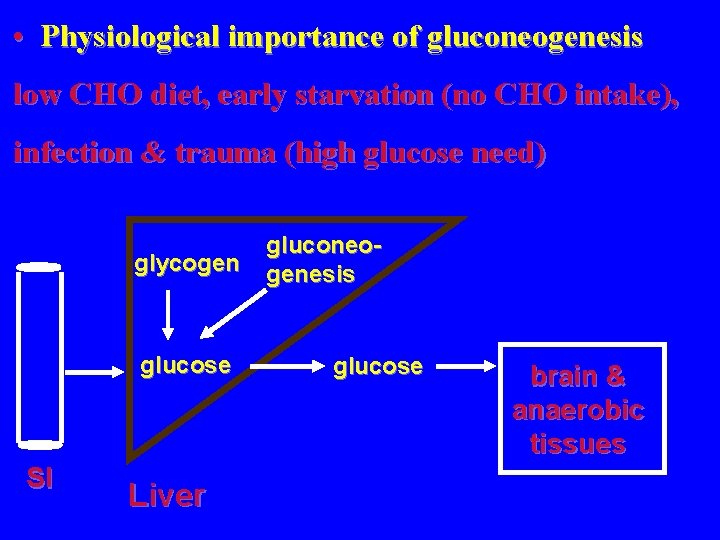
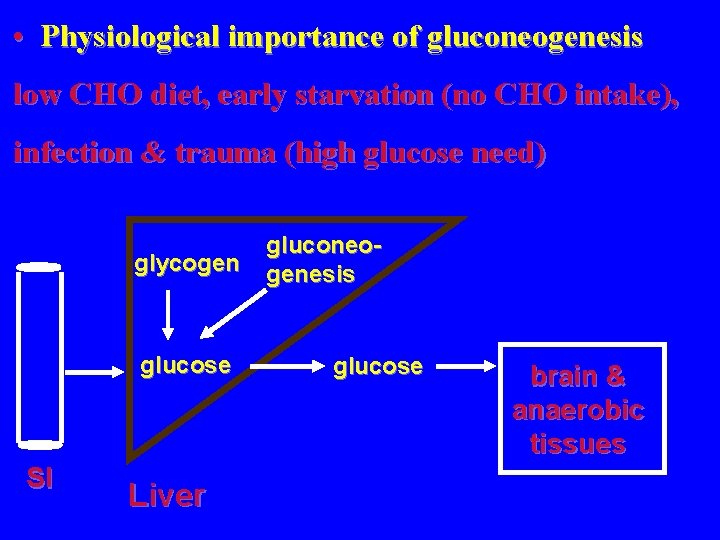
• Physiological importance of gluconeogenesis low CHO diet, early starvation (no CHO intake), infection & trauma (high glucose need) glycogen glucose SI Liver gluconeogenesis glucose brain & anaerobic tissues
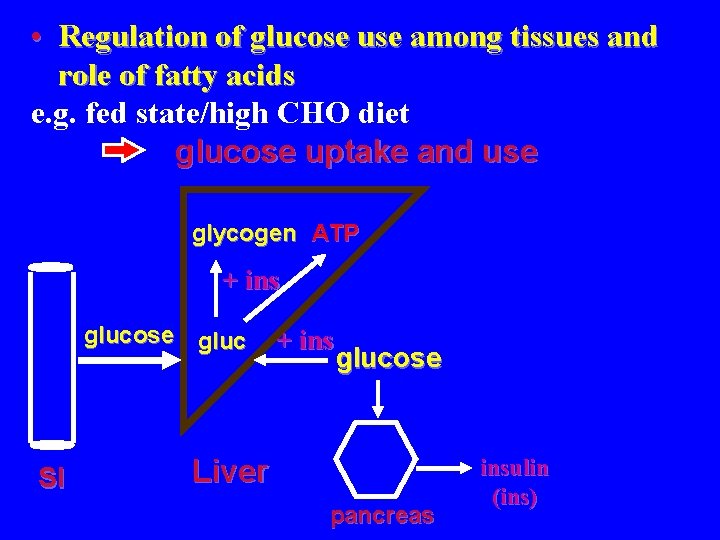
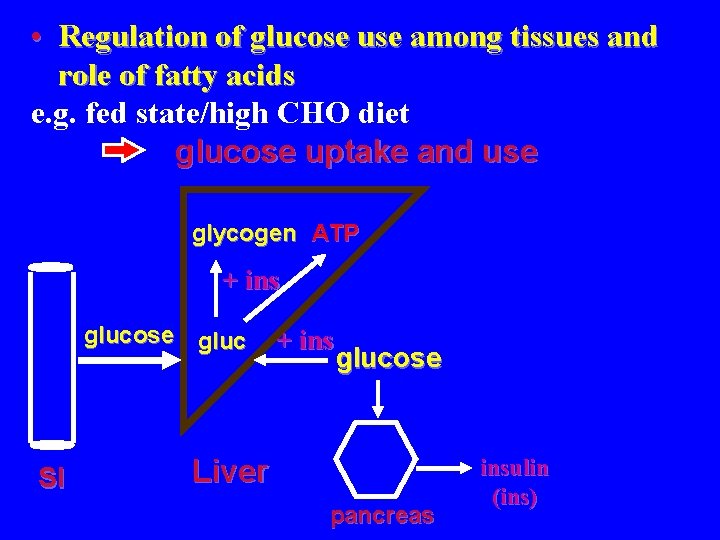
• Regulation of glucose use among tissues and role of fatty acids e. g. fed state/high CHO diet glucose uptake and use glycogen ATP + ins glucose gluc SI + ins glucose Liver pancreas insulin (ins)
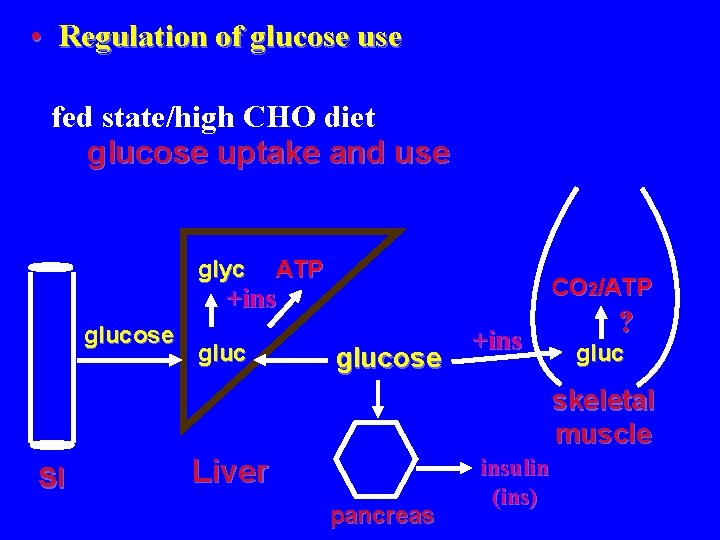
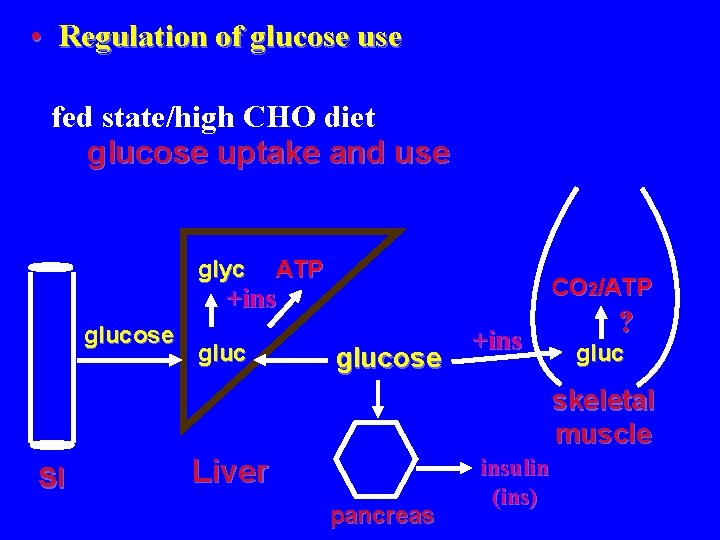
• Regulation of glucose use fed state/high CHO diet glucose uptake and use glyc ATP CO 2/ATP +ins glucose +ins ? gluc skeletal muscle SI Liver pancreas insulin (ins)

• Regulation of glucose use fed state/high CHO diet role of fatty acids adipocyte TG - ins FFA glyc ATP glucose gluc CO 2/ATP glucose + ins - gluc skeletal muscle SI Liver pancreas insulin (ins)

• CHO metabolism: Vitamin & Mineral Co-factors biotin (carboxylation) Thiamine: Vit B 1 Riboflavin: Vit B 2 (FAD) Niacin: Vit B 3 (NAD) pantothenic acid (Acetly-Co. A) glucose biotin B 3 pyruvate B 3 lactate B 1, B 2, B 3, Mg 2+ pantothenic acid acetyl-Co. A TCA cycle B 1, B 3
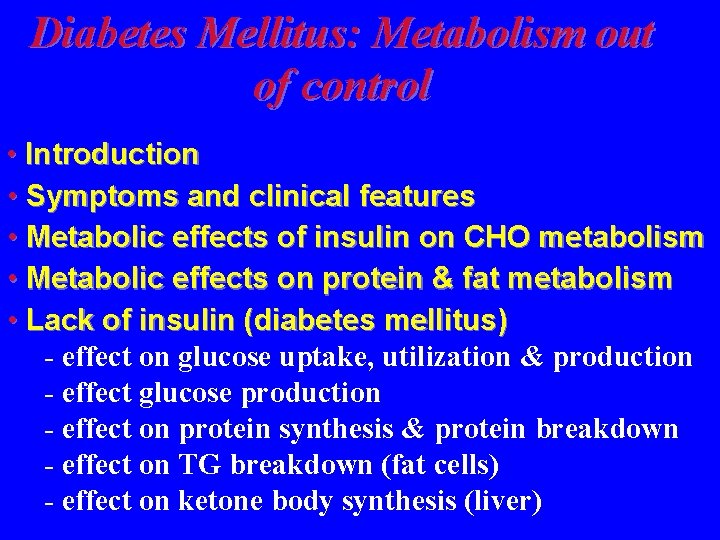
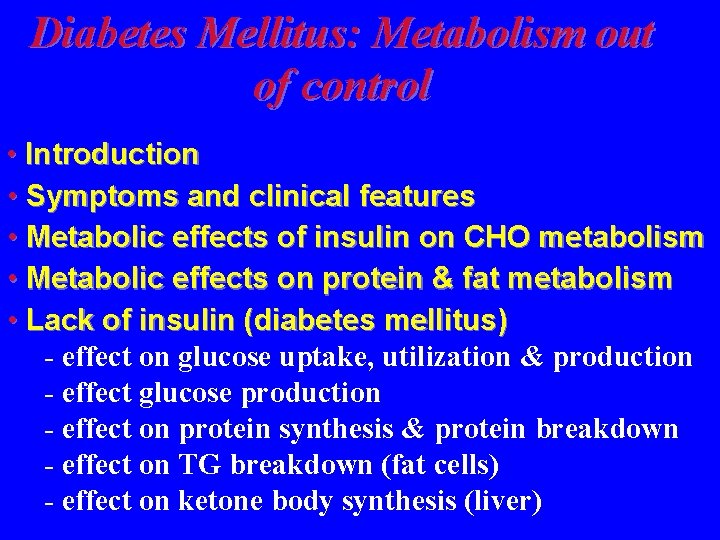
Diabetes Mellitus: Metabolism out of control • Introduction • Symptoms and clinical features • Metabolic effects of insulin on CHO metabolism • Metabolic effects on protein & fat metabolism • Lack of insulin (diabetes mellitus) - effect on glucose uptake, utilization & production - effect glucose production - effect on protein synthesis & protein breakdown - effect on TG breakdown (fat cells) - effect on ketone body synthesis (liver)

• Introduction Diabetes Mellitus or Type 1 (previously juvenile onset) or insulin-dependent diabetes mellitus (IDDM) recognized as a disease for 2000 years -cells of Islets of Langerhans (pancreas) damage: inadequate insulin production Diabetes illustrates problems that arise when integration of metabolism is impaired: carbohydrate, protein & lipid metabolism

• Symptoms and clinical features polyuria polydipsia polyphagia weight loss dehydration glycosuria ketosis/ketoacidosis unconsciousness/coma
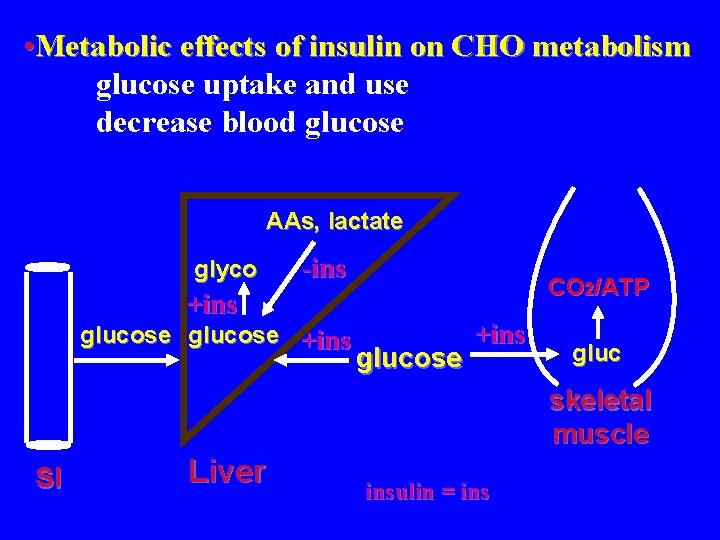
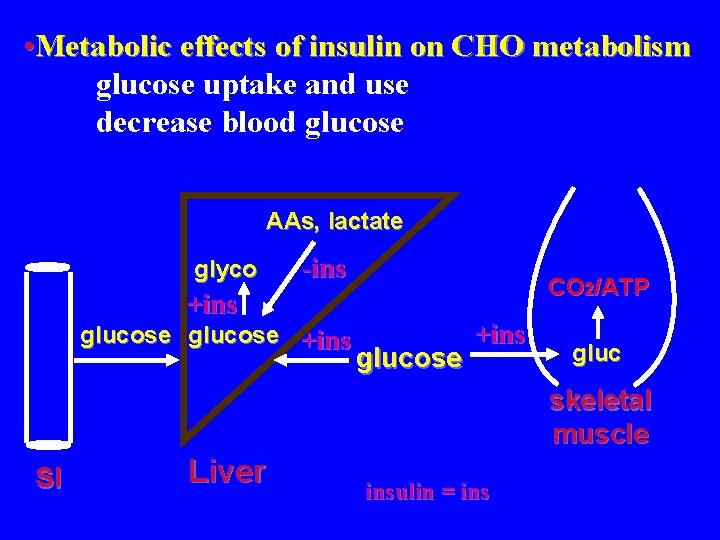
• Metabolic effects of insulin on CHO metabolism glucose uptake and use decrease blood glucose AAs, lactate glyco -ins CO 2/ATP +ins glucose +ins gluc skeletal muscle SI Liver insulin = ins

• Metabolic effects of insulin on protein metabolism - stimulate amino acid uptake - stimulate protein synthesis - inhibit protein degradation protein +ins AAs SI AAs Liver +ins Amino +ins Acids +ins -ins amino acids skeletal muscle insulin = ins
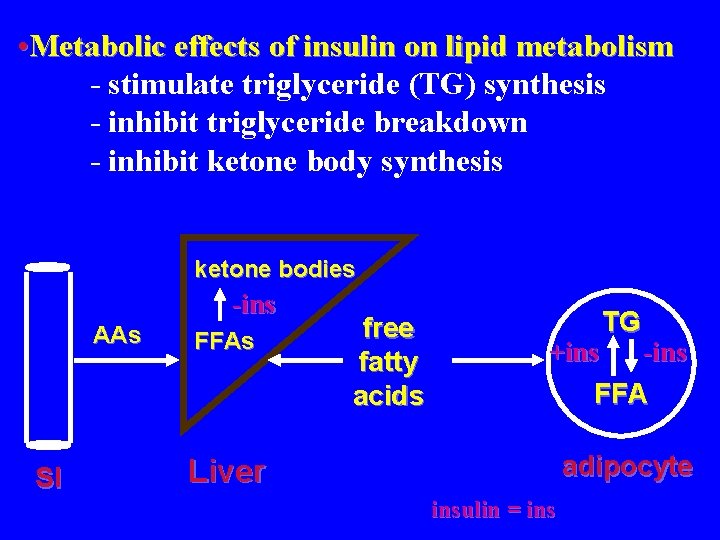
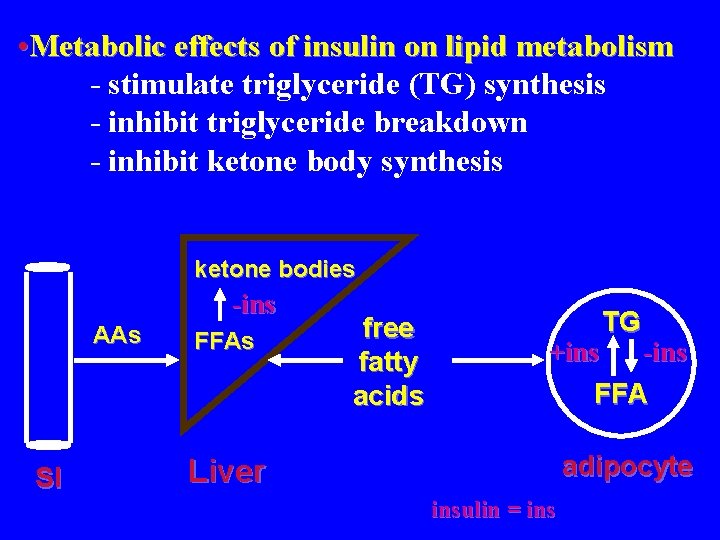
• Metabolic effects of insulin on lipid metabolism - stimulate triglyceride (TG) synthesis - inhibit triglyceride breakdown - inhibit ketone body synthesis ketone bodies -ins AAs SI FFAs free fatty acids TG +ins -ins FFA adipocyte Liver insulin = ins
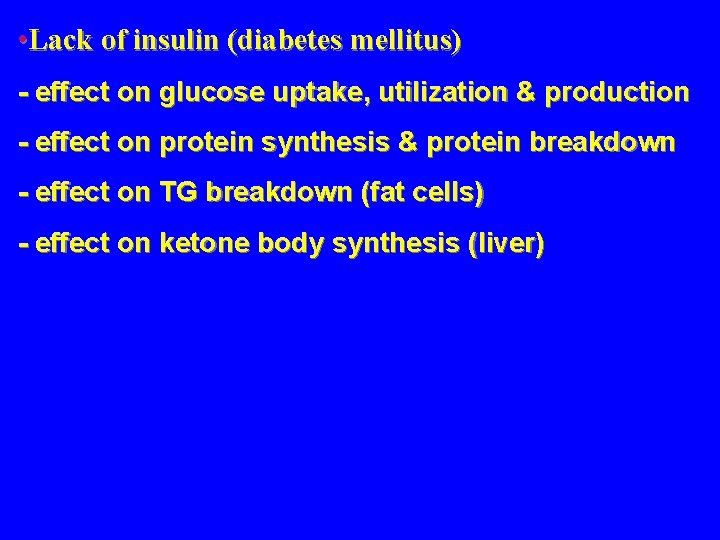
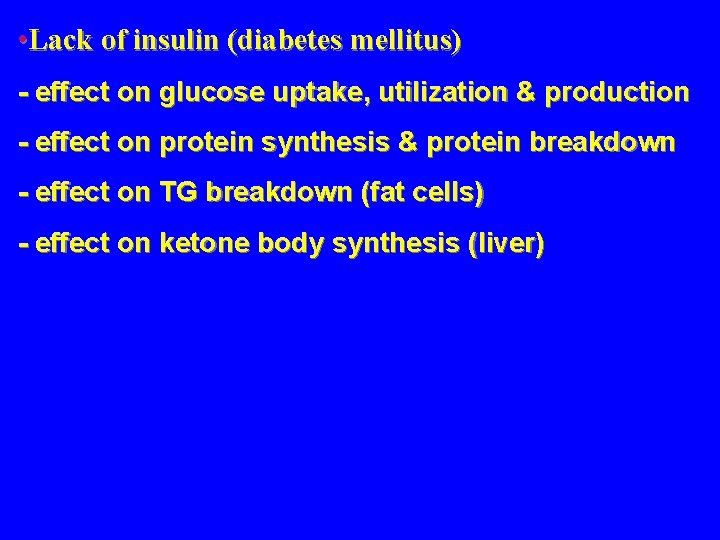
• Lack of insulin (diabetes mellitus) - effect on glucose uptake, utilization & production - effect on protein synthesis & protein breakdown - effect on TG breakdown (fat cells) - effect on ketone body synthesis (liver)
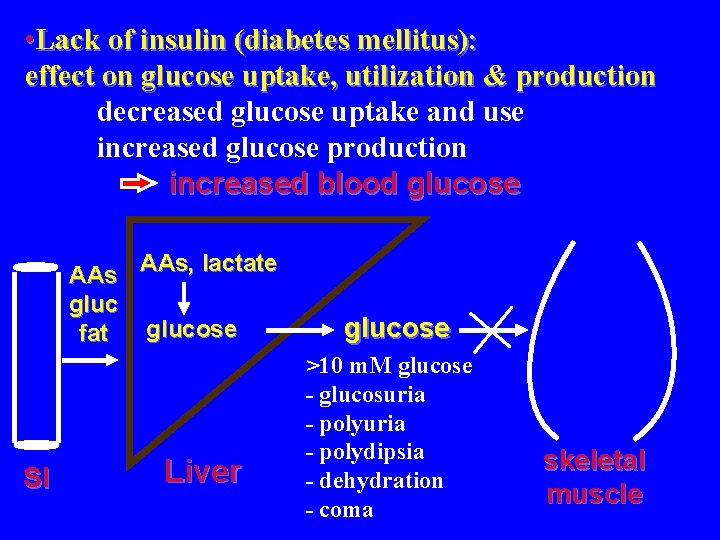
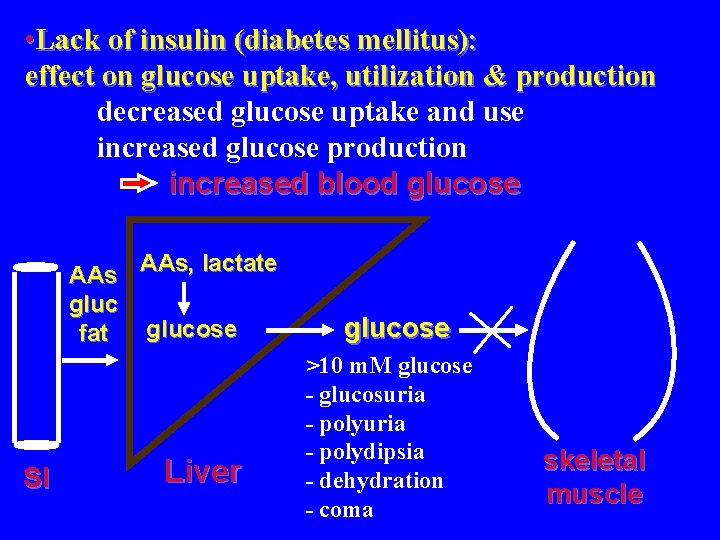
• Lack of insulin (diabetes mellitus): effect on glucose uptake, utilization & production decreased glucose uptake and use increased glucose production increased blood glucose AAs, lactate glucose fat SI Liver glucose >10 m. M glucose - glucosuria - polydipsia - dehydration - coma skeletal muscle
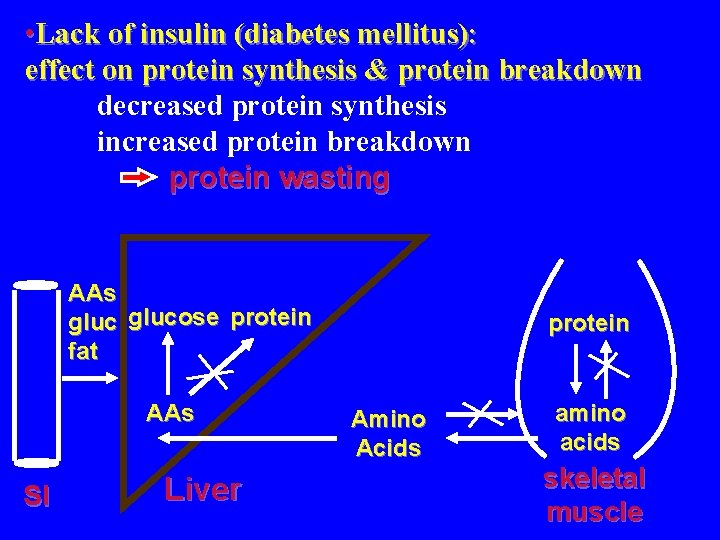
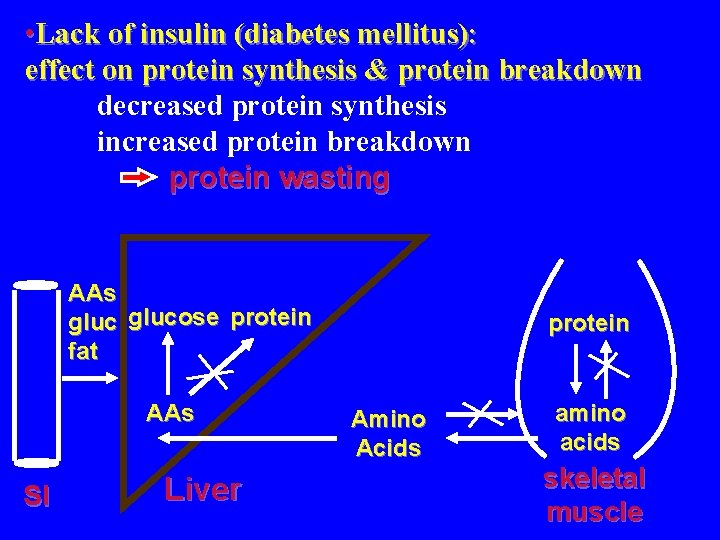
• Lack of insulin (diabetes mellitus): effect on protein synthesis & protein breakdown decreased protein synthesis increased protein breakdown protein wasting AAs glucose protein fat AAs SI Liver protein Amino Acids amino acids skeletal muscle
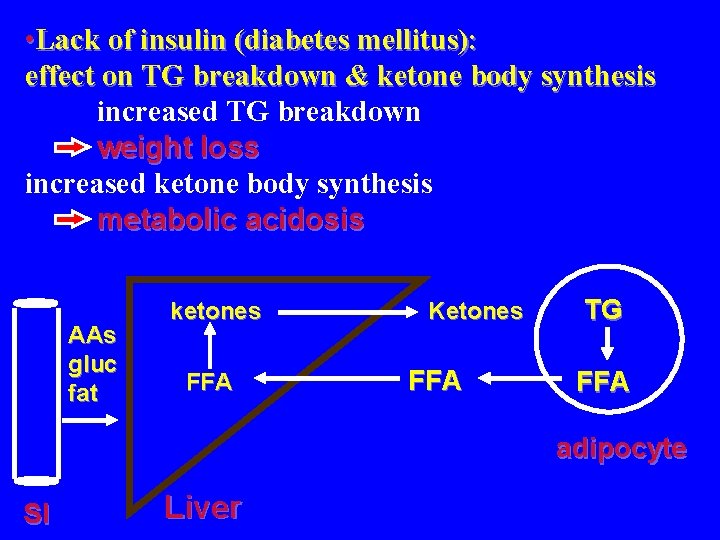
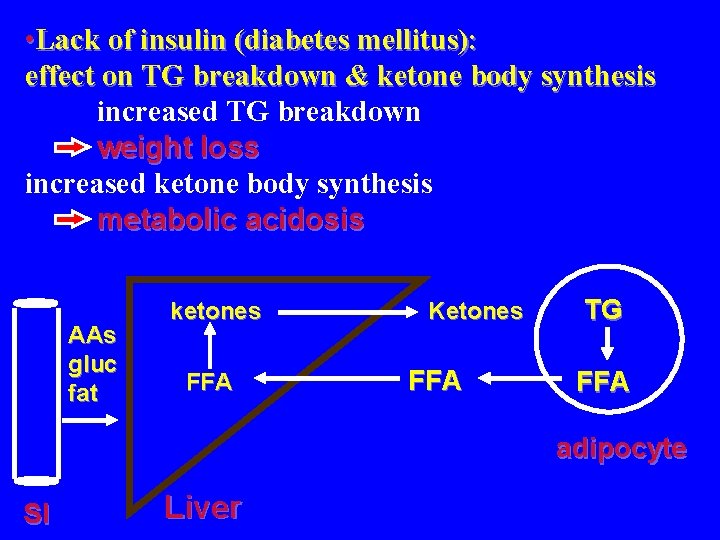
• Lack of insulin (diabetes mellitus): effect on TG breakdown & ketone body synthesis increased TG breakdown weight loss increased ketone body synthesis metabolic acidosis AAs gluc fat ketones FFA Ketones FFA TG FFA adipocyte SI Liver

• Lack of insulin (diabetes mellitus): SUMMARY TG adipocyte FFA AAs glucose fat AAs SI Liver KBs FFA Ketones glucose Amino Acids protein amino acids skeletal muscle
• Lack of insulin (diabetes mellitus): Summary The normal flow of substrates following food intake is largely dependent on the secretion of insulin. Insulin exerts a potent, positive effect on anabolism, while inhibiting catabolic pathways. Diabetes is a vivid negative example that emphasizes the integration of metabolism and the importance of metabolic regulation to continuance of life. from Advanced Nutrition & Human Metabolism Groff & Gropper 2000

. Fibre • Introduction, Definition & Sources • Type of fibre and properties - cellulose, hemicelluloses, -glucans, pectins, lignin - soluble vs. insoluble fibre • Physiological & Metabolic effects - water holding capacity, binding of nutrients, fermentability • Significance • Recommended intakes

• Introduction In humans, pre-1970’s fibre believed to have no nutritional value & antinutrient Since 1970’s, fibre: - energy value - gastrointestinal function - nutrient availability - prevention & treatment of many diseases

• Definition - fibre is not a single entity - difficult to define “Endogenous components of plant material in the diet that are resistant to digestion by enzymes produced by man. They are predominantly non-starch polysaccharides and lignin and may include, in addition, associated substances. ” (Health and Welfare Canada)
• Sources Plant material plant cell wall : 95% of fibre cementing material in plants legumes: beans, peas forages: alpha, timothy hay. . bran of cereals: wheat, oats, corn, rice. . skin of fruits & vegetables
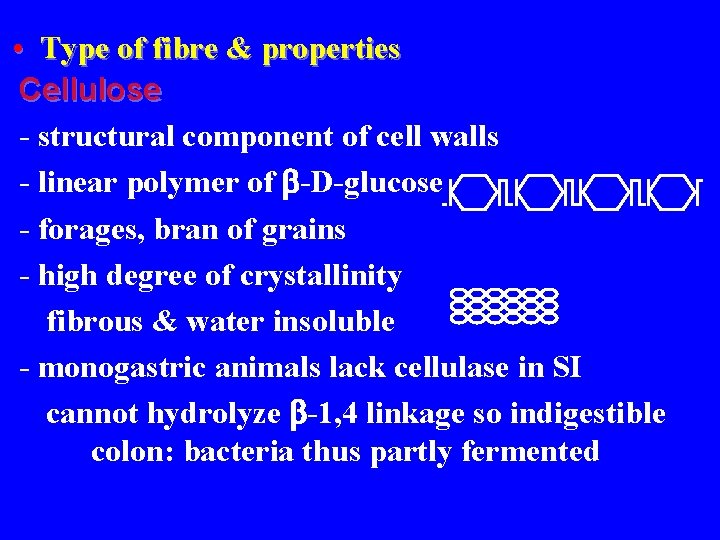
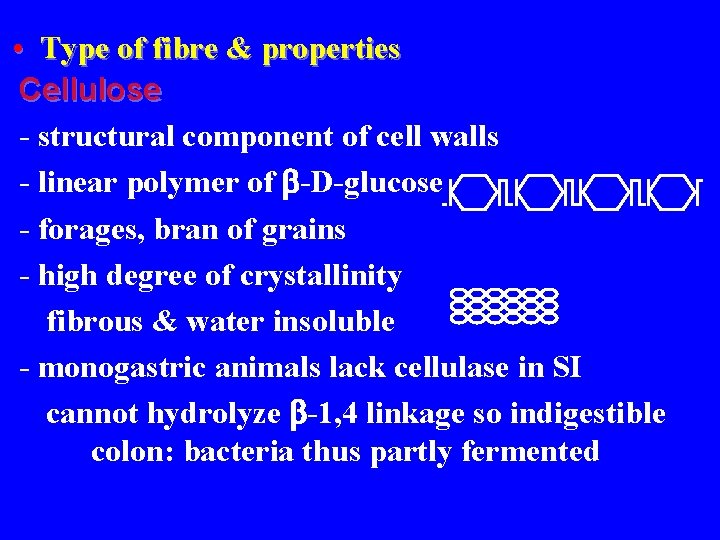
• Type of fibre & properties Cellulose - structural component of cell walls - linear polymer of -D-glucose - forages, bran of grains - high degree of crystallinity fibrous & water insoluble - monogastric animals lack cellulase in SI cannot hydrolyze -1, 4 linkage so indigestible colon: bacteria thus partly fermented
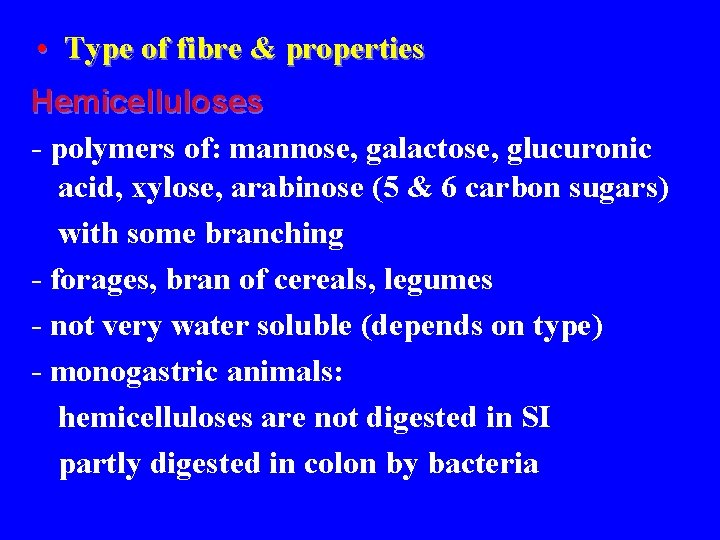
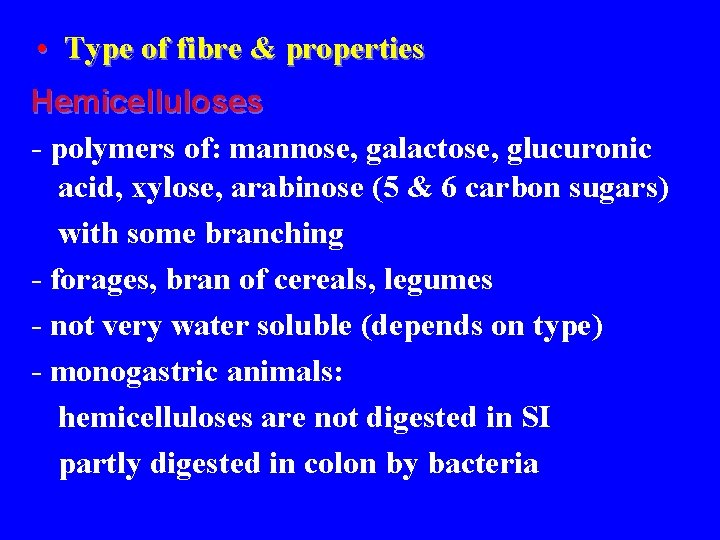
• Type of fibre & properties Hemicelluloses - polymers of: mannose, galactose, glucuronic acid, xylose, arabinose (5 & 6 carbon sugars) with some branching - forages, bran of cereals, legumes - not very water soluble (depends on type) - monogastric animals: hemicelluloses are not digested in SI partly digested in colon by bacteria
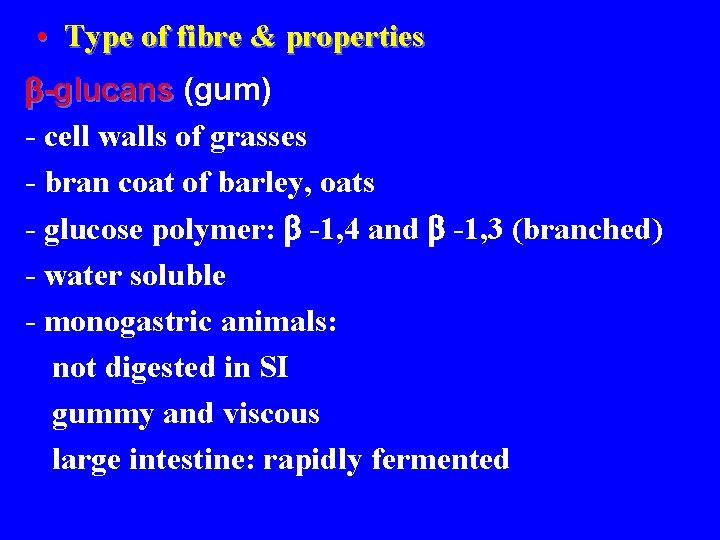
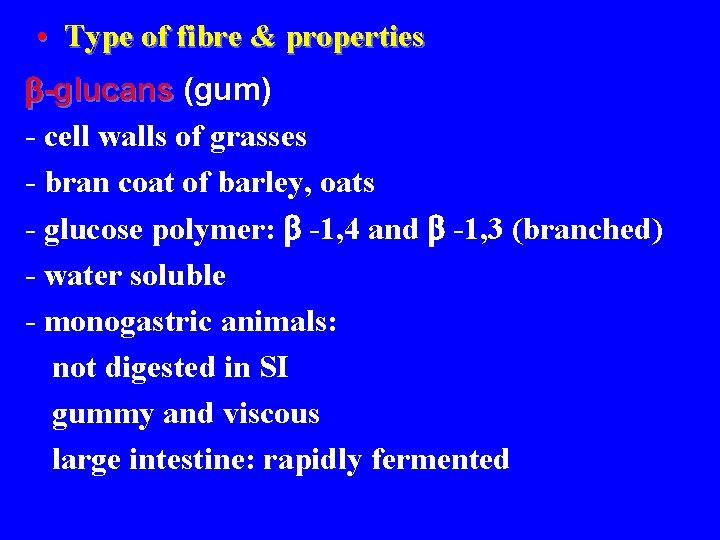
• Type of fibre & properties -glucans (gum) - cell walls of grasses - bran coat of barley, oats - glucose polymer: -1, 4 and -1, 3 (branched) - water soluble - monogastric animals: not digested in SI gummy and viscous large intestine: rapidly fermented
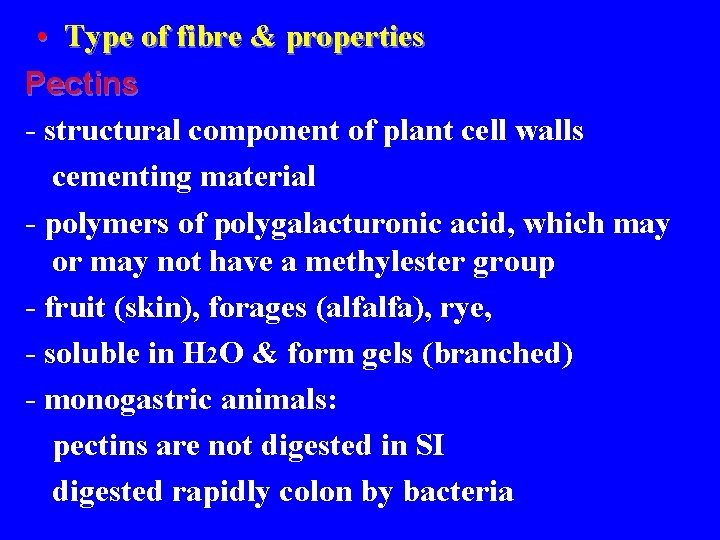
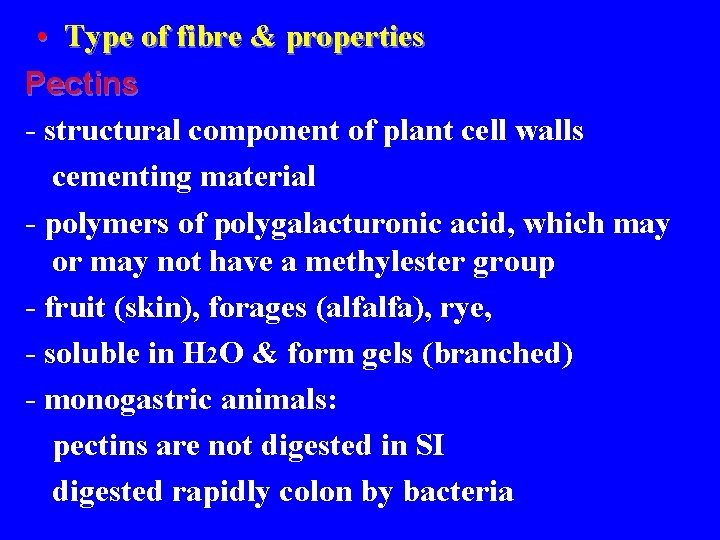
• Type of fibre & properties Pectins - structural component of plant cell walls cementing material - polymers of polygalacturonic acid, which may or may not have a methylester group - fruit (skin), forages (alfalfa), rye, - soluble in H 2 O & form gels (branched) - monogastric animals: pectins are not digested in SI digested rapidly colon by bacteria

• Type of fibre & properties Lignin - NOT a carbohydrate - structural component of plant cell walls - aromatic polymer; polyphenolic (hydrophobic) - insoluble in water - not digestible in SI or by bacteria Mucilages & algal polysaccharides - carragenan, agar - water soluble - highly fermentable

• Type of fibre & properties Dietary Fibre Soluble some hemicelluloses -glucans pectins gums, mucilages Insoluble some hemicelluloses cellulose lignin - solubility affects water-holding capacity, fermentability, nutrient adsorption - these exert physiological & metabolic effects
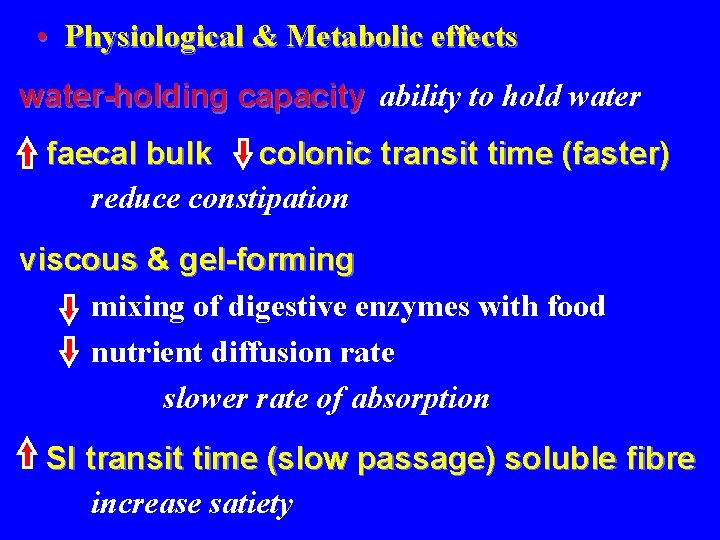
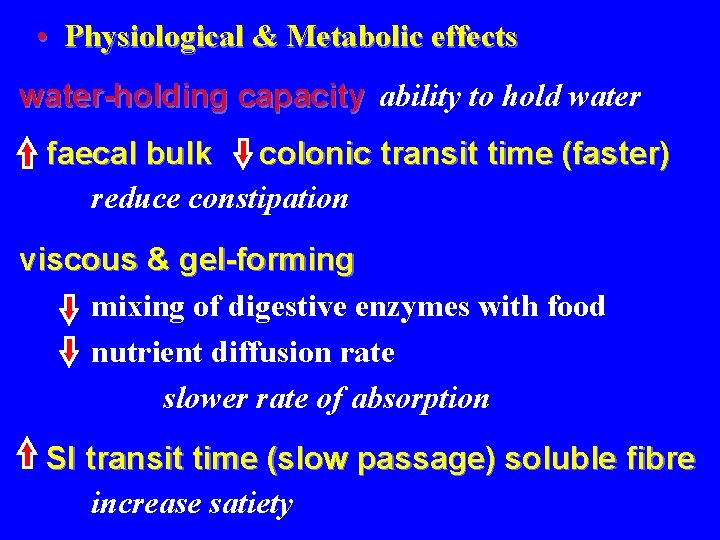
• Physiological & Metabolic effects water-holding capacity ability to hold water faecal bulk colonic transit time (faster) reduce constipation viscous & gel-forming mixing of digestive enzymes with food nutrient diffusion rate slower rate of absorption SI transit time (slow passage) soluble fibre increase satiety
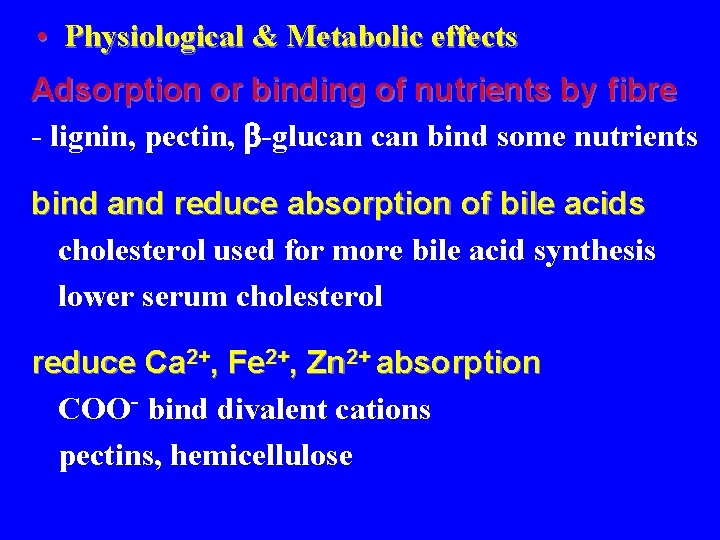
• Physiological & Metabolic effects Adsorption or binding of nutrients by fibre - lignin, pectin, -glucan bind some nutrients bind and reduce absorption of bile acids cholesterol used for more bile acid synthesis lower serum cholesterol reduce Ca 2+, Fe 2+, Zn 2+ absorption COO- bind divalent cations pectins, hemicellulose
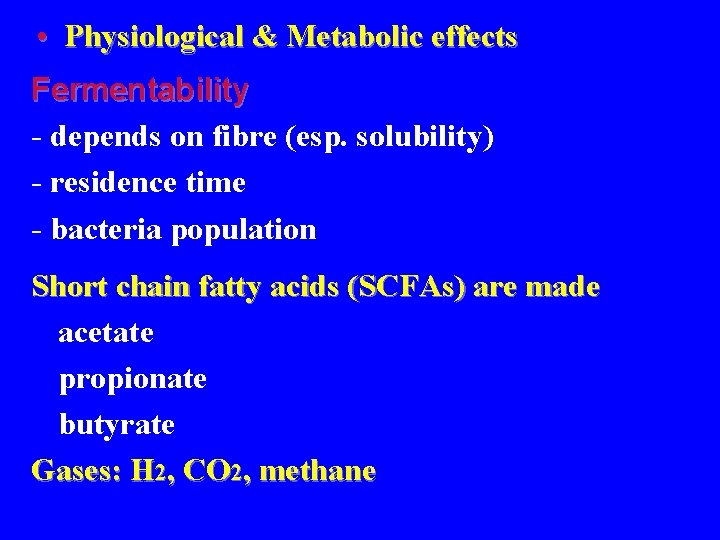
• Physiological & Metabolic effects Fermentability - depends on fibre (esp. solubility) - residence time - bacteria population Short chain fatty acids (SCFAs) are made acetate propionate butyrate Gases: H 2, CO 2, methane

• Physiological & Metabolic effects Short chain fatty acids - absorbed acetate (2 C) acetyl-Co. A propionate (3 C) liver ATP or FFAs glucose butyrate (4 C) used as fuel for intestinal cells Fibre that is fermented in can be a source of energy and glucose
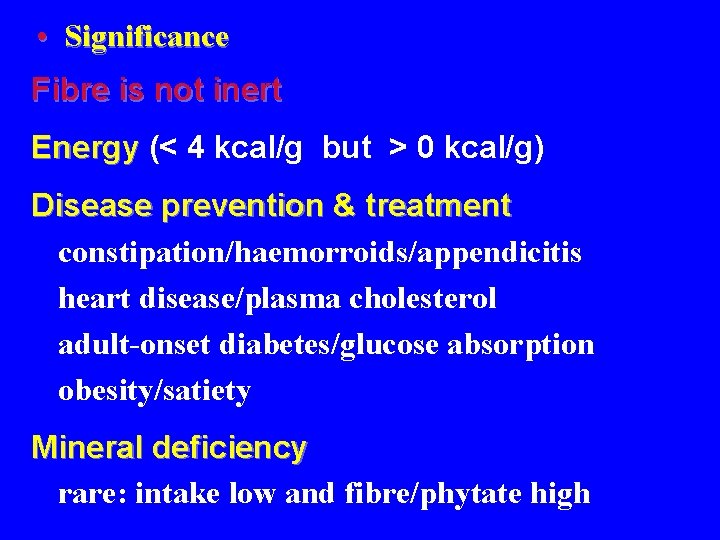
• Significance Fibre is not inert Energy (< 4 kcal/g but > 0 kcal/g) Disease prevention & treatment constipation/haemorroids/appendicitis heart disease/plasma cholesterol adult-onset diabetes/glucose absorption obesity/satiety Mineral deficiency rare: intake low and fibre/phytate high

References • Groff and Gropper, 2000. Advanced Nutrition and Human Metabolism
 Jay giri md
Jay giri md Giri di bussola
Giri di bussola E devlet ile ebaya giriş
E devlet ile ebaya giriş Makan sunan giri
Makan sunan giri Msn giri
Msn giri Nutrition and diet therapy nursing
Nutrition and diet therapy nursing Nutritional needs in fundamentals of nursing
Nutritional needs in fundamentals of nursing Chapter 6 shielded metal arc welding
Chapter 6 shielded metal arc welding Datingoo
Datingoo Lesson 6 anorexia nervosa and bulimia
Lesson 6 anorexia nervosa and bulimia Lesson 4 weight control
Lesson 4 weight control Chapter 10 lesson 4 nutrition labels and food safety
Chapter 10 lesson 4 nutrition labels and food safety Chapter 10 nutrition for health lesson 2 answer key
Chapter 10 nutrition for health lesson 2 answer key Lesson 1 the importance of nutrition
Lesson 1 the importance of nutrition Chapter 10 lesson 4 nutrition labels and food safety
Chapter 10 lesson 4 nutrition labels and food safety Myplate nutrition jeopardy
Myplate nutrition jeopardy Mimi dai math
Mimi dai math Mimi teocrito
Mimi teocrito La mula de memo
La mula de memo Mimi kusimama
Mimi kusimama Dunce hat topology
Dunce hat topology Mimi garcia h
Mimi garcia h Pippa pig alphafriend
Pippa pig alphafriend Mimi lufkin
Mimi lufkin Mimi opkins
Mimi opkins Mimi opkins
Mimi opkins Mimi chinese restaurant
Mimi chinese restaurant Mimi siku casserole
Mimi siku casserole Opkins
Opkins Mimi opkins
Mimi opkins Mimi opkins
Mimi opkins A bruxa mimi no inverno
A bruxa mimi no inverno Thiolisis
Thiolisis Mimi server
Mimi server Mimi opkins
Mimi opkins Mimi hull
Mimi hull Mimi opkins
Mimi opkins Mimi opkins
Mimi opkins Lesson outline lesson 3 describing circuits answers
Lesson outline lesson 3 describing circuits answers Mountain building
Mountain building Lesson outline lesson 2 aquatic ecosystems answer key
Lesson outline lesson 2 aquatic ecosystems answer key Micro teach lesson plans
Micro teach lesson plans L101 introduction to healthcare leadership
L101 introduction to healthcare leadership Class 7 english a gift of chappals lesson plan
Class 7 english a gift of chappals lesson plan Chapter 1 lesson 1 your total health lesson 1 quiz
Chapter 1 lesson 1 your total health lesson 1 quiz Weather forecasts lesson 3 outline answers
Weather forecasts lesson 3 outline answers Sat vocabulary lesson 4
Sat vocabulary lesson 4 Lesson outline physical properties lesson 2
Lesson outline physical properties lesson 2 Lesson 1 thermal energy and the behavior of matter
Lesson 1 thermal energy and the behavior of matter Climates of earth lesson 1 answer key
Climates of earth lesson 1 answer key Lesson outline lesson 2
Lesson outline lesson 2 Lesson 2 measurement and scientific tools
Lesson 2 measurement and scientific tools Fingerprint galton details
Fingerprint galton details Lesson outline lesson 1 land biomes answers
Lesson outline lesson 1 land biomes answers Lesson 4 gravity and motion lesson review
Lesson 4 gravity and motion lesson review Lesson outline lesson 2 the muscular system answer key
Lesson outline lesson 2 the muscular system answer key Wave properties lesson 2
Wave properties lesson 2 Today's lesson or today lesson
Today's lesson or today lesson 1 important lesson that is worth sharing about this lesson
1 important lesson that is worth sharing about this lesson Today's lesson or today lesson
Today's lesson or today lesson Lesson outline magnets and magnetic fields answer key
Lesson outline magnets and magnetic fields answer key The sun-earth-moon system worksheet answers lesson 1
The sun-earth-moon system worksheet answers lesson 1 Hotel industry analytics
Hotel industry analytics Water treatment fundamentals
Water treatment fundamentals Fundamentals of investment notes
Fundamentals of investment notes Ecommerce fundamentals
Ecommerce fundamentals Networking fundamentals
Networking fundamentals Security guide to network security fundamentals
Security guide to network security fundamentals Fundamentals of analyzing real estate investments
Fundamentals of analyzing real estate investments Solid based rapid prototyping manufacturer
Solid based rapid prototyping manufacturer Thermoacoustic refrigeration
Thermoacoustic refrigeration Call center fundamentals
Call center fundamentals Shell process safety fundamentals
Shell process safety fundamentals Duct design fundamentals
Duct design fundamentals Networking fundamentals
Networking fundamentals Mta security fundamentals exam questions and answers
Mta security fundamentals exam questions and answers