Parenteral Nutrition NUTRITION Human nutrition is the provision



- Slides: 31
Parenteral Nutrition
NUTRITION � Human nutrition is the provision to obtain the essential nutrients necessary to support life and health � Nutrients are the substances that are not synthesized in sufficient quantity in the body and therefore must be supplied from diet � Macronutrients mainly carbohydrates, fats, protein, dietary fiber and water � Micronutrients: vitamins, minerals and trace elements
Essential Nutrients � Protein � Fat (Amino acids) � Carbohydrate � Dietary fiber � Water and electrolytes � Vitamins � minerals � Trace elements
ENTERAL NUTRITION � Refers to feeding via a tube placed into the gut to deliver liquid formulas containing all essential nutrients � Preferred route because of benefits derived from maintaining the digestive, absorptive and immunological barrier function of GIT � Enteral/tube feeding is useful in pts who have functional GIT, but who cannot digest or ingest adequate amount of nutrients � Short term (<6 weeks) tube feeding can be achieved by nasogastric, nasoduodenal or nasojejunal tubes
ENTERAL Vs PARENTERAL � � Enteral nutrition is associated with fewer complications than parenteral nutrition and is less expensive to administer. However, the use of enteral nutrition alone often does not achieve caloric targets. In addition, underfeeding is associated with weakness, infection, increased duration of mechanical ventilation, increased duration of hospital stay and death. Combining parenteral nutrition with enteral nutrition constitutes a strategy to prevent nutritional deficit but may risk overfeeding which has been associated with liver dysfunction, infection, and prolonged ventilatory support.
PARENTERAL NUTRITION � The consequences of major surgeries and PEM can lead to hypermetabolism and subsequent malnutrition. A strong association exist between malnutrition and increased post operative morbidity and mortality. � The administration of TPN can prevent the effects of starvation in pts with non functional GIT � Parenteral nutrition should be considered if energy intake has been inadequate for more than 7 -10 days and enteral feeding is not feasible. (based on ICU focused meta- analysis discussed in 2009 ASPEN)
Parenteral nutrition � It involves the continuous infusion of a hyperosmolar solution containing carbohydrates, proteins, fat and other necessary electrolytes through an indwelling catheter inserted into (usually) SVC to meet the nutritional needs of the patient. � PN through a peripheral vein is limited by osmolality and volume constraints � Solutions that contain more than 3% aminoacid and 5% glucose are poorly tolerated peripherally
Types � Peripheral parenteral nutrition (PPN) Øadministered through a peripheral intravenous catheter. ØThe osmolarity of PPN solutions generally is limited to 1, 000 m. Osm (approximately 12% dextrose solution) to avoid phlebitis. ØThus, large volumes (>2, 500 m. L) are needed. ØTemporary nutritional supplementation with PPN may be useful ØGenerally intended as supplement to oral feeding and is not optimal for critically ill pts
� Total parenteral nutrition (TPN) Øprovides complete nutritional support ØThe solution, volume of administration, and additives are individualized based on an assessment of the nutritional requirements.
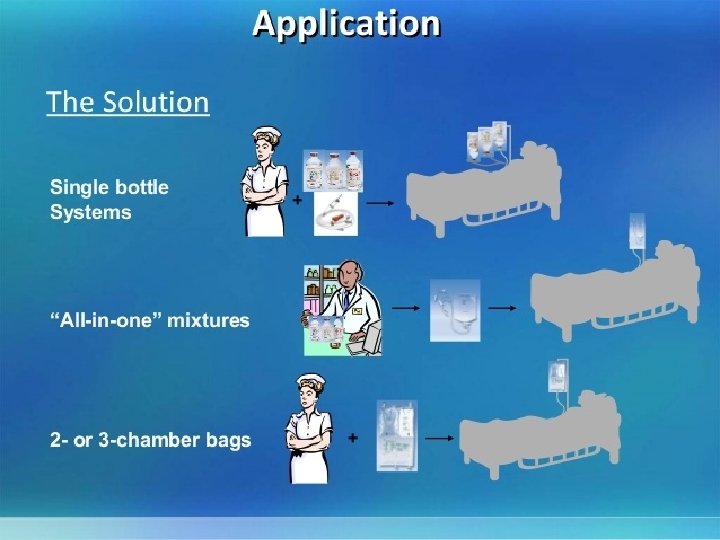
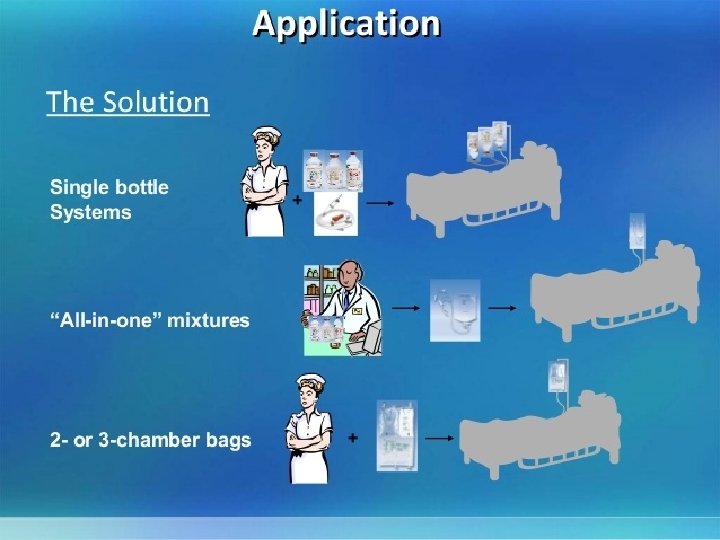
Types of TPN formulations � TPN formulation without lipid (2 -in-1 solution) ØCalories from amino acids- 20 to 25% ØCalories from dextrose- 75 -80% � TPN formulation with lipid ( 3 -in-1 solution) Ø calories from amino acids- 20 to 25% Ø calories from lipids- 20% Ø calories from dextrose- 55 to 60 %
� Special solutions that contain low, intermediate, or high nitrogen concentrations as well as varying amounts of fat and carbohydrate are available for pts with diabetes, renal or pulmonary failure, or hepatic dysfunction.
� Additives: ØElectrolytes (i. e. , sodium, potassium, chloride, acetate, calcium, magnesium, phosphate) should be adjusted daily. ØThe number of cations and anions must balance; this is achieved by altering the concentrations of chloride and acetate. ØIf the serum bicarbonate is low, the solution should contain more acetate. ØThe calcium: phosphate ratio must be monitored to prevent salt precipitation.
� Medications: Ø Albumin, H 2 -receptor antagonists, heparin, iron, dextran, insulin, and metoclopramide can be administered in TPN solutions. However, not all medications are compatible with 3 -in-1 admixtures. Ø Regular insulin should initially be administered subcutaneously according to a sliding scale, based on a determination of the blood glucose level. After a stable insulin requirement has been established, insulin can be administered in the TPN solution, generally at two thirds of the daily subcutaneous insulin dose.
TPN- macronutrient solutions � Crystalline amino acid solutions containing 4050% essential and 50 -60% non essential amino acids are used to provide protein needs � Some amino acid solutions have been modified: rich in branched chain amino acids for hepatic encephalopathy, rich in essential amino acid for renal insufficiency pts � Glucose in IV solutions is hydrated; each gm of dextrose monohydrate provides 3. 4 kcal. While there is no absolute requirement of glucose in most pts, providing >150 g glucose/d maximizes protein balance
TPN- macronutrient solutions � Lipid emulsions are available as 10% (1. 1 kcal/ml) or 20% (2 kcal/ml) solutions and provide energy as well as source of essential fatty acids. � Rate of infusion should not exceed 1 kcal/kg/h
Some commercial available formulations � Climomel N 5 -800 � Clinimix N 9 G-20 E � Kabiven � Vitrimix � Celemix-G
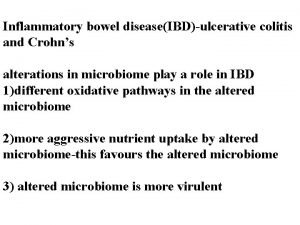
Indications Ø gastrointestinal cutaneous fistula ØRenal failure (ATN) Ø Short bowel syndrome ØSevere burns ØHepatic failure ØCrohn’s disease ØAnorexia nervosa ØAcute radiation enteritis ØAcute chemotherapy toxicity ØProlonged ileus ØWeight loss preliminary to major surgery
ADMINISTRATION OF TPN � Introduction of TPN should be gradual. For example, approximately 1, 000 kcal is provided the first day. If there is metabolic stability (i. e. , normoglycemia), this is increased to the caloric goal over 1 to 2 days. � TPN solutions are delivered most commonly as a continuous infusion. A new 3 -in-1 admixture bag of TPN is administered daily at a constant infusion rate over 24 hours. Additional maintenance intravenous fluids are unnecessary, and total infused volume should be kept constant while nutritional content is increased.
Cyclic Administration � Cyclic administration of TPN solutions may be useful for (1) those who will be discharged from the hospital and subsequently receive home TPN, (2) those with limited intravenous access who require administration of other medications, and (3) those who are metabolically stable and desire a period during the day when they can be free of an infusion pump. � Cyclic TPN is administered for 8 to 16 hours, most commonly at night. This should not be done until metabolic stability has been demonstrated for patients on standard, continuous TPN infusions.
20
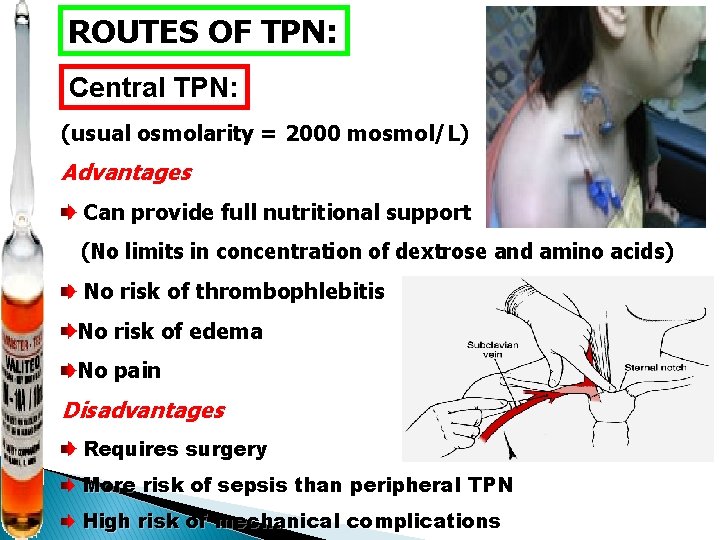
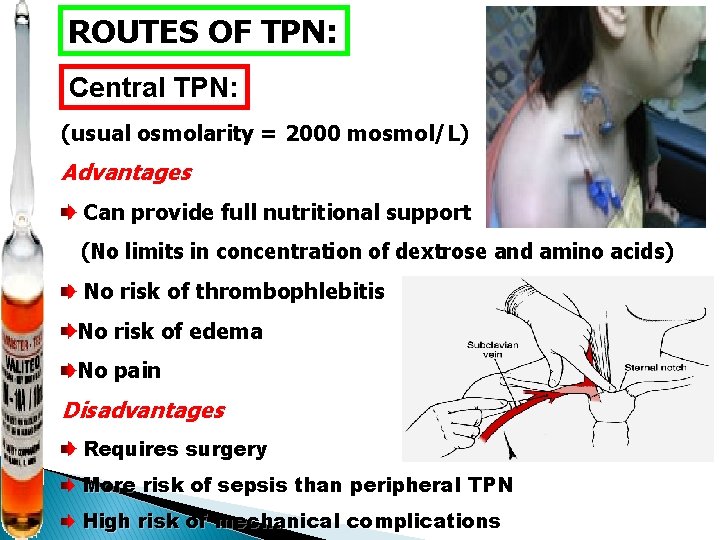
ROUTES OF TPN: Central TPN: (usual osmolarity = 2000 mosmol/L) Advantages Can provide full nutritional support (No limits in concentration of dextrose and amino acids) No risk of thrombophlebitis No risk of edema No pain Disadvantages Requires surgery More risk of sepsis than peripheral TPN High risk of mechanical complications
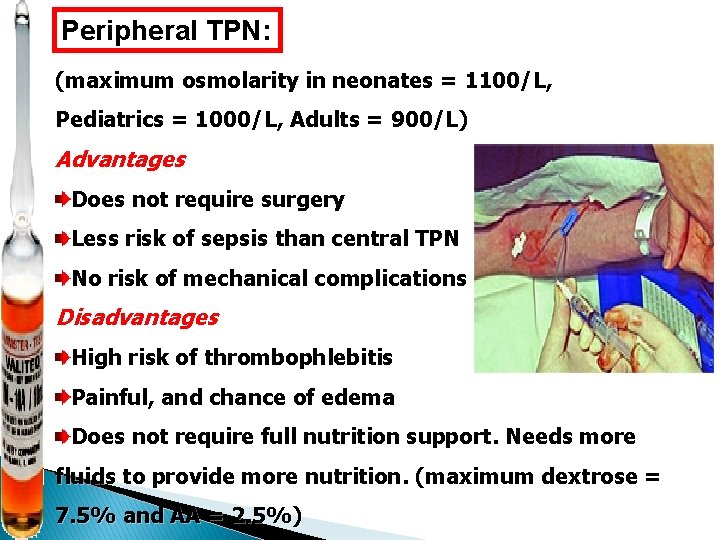
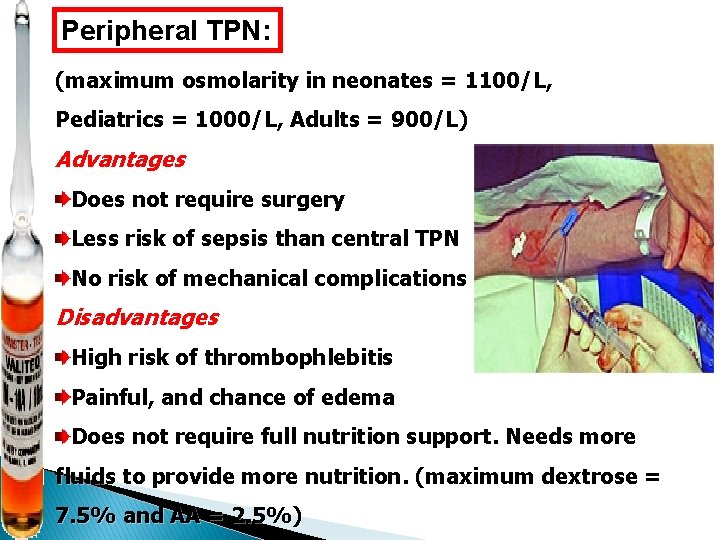
Peripheral TPN: (maximum osmolarity in neonates = 1100/L, Pediatrics = 1000/L, Adults = 900/L) Advantages Does not require surgery Less risk of sepsis than central TPN No risk of mechanical complications Disadvantages High risk of thrombophlebitis Painful, and chance of edema Does not require full nutrition support. Needs more fluids to provide more nutrition. (maximum dextrose = 7. 5% and AA = 2. 5%)

Monitoring of parenteral nutrition


Mechanical Complications Of TPN infectious metabolic
Mechanical Complications ØAir embolism Ø pneumothorax Ø hemothorax ØCardiac tamponade ØInjuries to arteries and veins ØInjury to thoracic duct ØBrachial plexus injury
Metabolic complications � Early Ø Ø or nutrient related hyperglycemia hypoglycemia hyperlipidemia refeeding syndrome � late or related to long term administration Ø hepatic dysfunction ØSteatosis, steatohepatitis, lipidosis, cholestasis, cirrhosis Ø biliary complications: acalculous cholecystitis, Gb sludge, cholelithiasis ØMetabolic bone disease: osteomalaacia, osteopenia
� Fluid overload � Hypo/hypernatremia � Hypercalcemia � Hypo/hyperkalemia Infection : Ø Catheter related sepsis is most common life threatening complication Ø Causes: staph epidermidis and staph aureus, enterococcus, candida, E coli, psuedomonas, klebsiella etc in immunocompromised pts
Refeeding syndrome � Severe electrolyte and fluid shifts that may result from refeeding after severe weight loss (PEM) � Hypophosphatemia is the hallmark of refeeding syndrome due to shift from fat to glucose metabolism. � Hypokalemia and hypomagnesemia � ↓K and ↓PO 4→ ATP deficiency which can be life threatening.
Care of the parenteral nutrition (PN) mixture Store reconstituted PN bags in a refrigerator until use � Always use aseptic techniques while connecting and infusing PN � Always use an infusion set with in-built air vent and 0. 2 m filter � Never insert a needle for air venting in a PN bag � Never add any medication to the PN bag � Avoid frequent changes in the formulation of the PN solution � Infuse the prescribed volume and avoid wastage of PN solution �
 Public provision
Public provision How to calculate tpn calories
How to calculate tpn calories Tpn tapering guidelines
Tpn tapering guidelines Complication of parenteral nutrition
Complication of parenteral nutrition Ppn vs tpn
Ppn vs tpn Parenteral nutrition types
Parenteral nutrition types Complication of parenteral nutrition
Complication of parenteral nutrition Cost of tpn
Cost of tpn Related image
Related image What is catering
What is catering Costed provision map template
Costed provision map template Samba ad domain controller
Samba ad domain controller Summarise types of early years provision
Summarise types of early years provision Core service provision
Core service provision Servicios ecosistémicos de soporte
Servicios ecosistémicos de soporte Prime cost in manufacturing accounts
Prime cost in manufacturing accounts Qué acto aseguro nuestra salvación
Qué acto aseguro nuestra salvación Provision for receivables
Provision for receivables How to compute iaet
How to compute iaet Hire purchase in suspense
Hire purchase in suspense Acf 202
Acf 202 Wim debeuckelaere
Wim debeuckelaere Motor vehicle depreciation
Motor vehicle depreciation Provision of depreciation account
Provision of depreciation account Sparkplugfn the era of relationships.7
Sparkplugfn the era of relationships.7 Provision vs accrual
Provision vs accrual Provision for bad debts
Provision for bad debts Provision for receivables
Provision for receivables Accounting standards 29
Accounting standards 29 How to record contingent liability
How to record contingent liability Returns outwards
Returns outwards Tdg cheat sheet
Tdg cheat sheet