Investigations for urogynaecologists in underresourced settings The role













- Slides: 60
Investigations for urogynaecologists in under-resourced settings: The role of urodynamics, ultrasound and specialised imaging? Stephen T Jeffery University of Cape Town, South Africa Urogynaecology and laparoscopy clinic www. urogynaecology. co. za
An example 49 yr old, P 3 Has history of severe stress incontinence No urgency, urgency incontinence or nocturia No voiding problems Very obvious stress leak on examination THAT’S EASY
Another example 46 year old, P 2 Has stress incontinence with some significant urgency incontinence, stress worse Nocturia x 4 Leaks on standing up Has bladder pain occasionally No stress incontinence demonstrated
Example 2: Options ① Start on anticholinergics ② Go straight ahead and put in a sling Or ① Start on anticholinergics ② Investigate – but what and why?
Example 2: What the investigations will tell us 1. Urodynamics Give us an idea about voiding dysfunction Will demonstrate stress incontinence May show detrusor overactivity May help our lawyer if we get sued
Example 2: What the investigations will tell us 2. Perineal Ultrasound Quick look at residual Bladder neck mobility Bladder wall thickness Bladder neck funneling Diverticulum Demonstrate any impact that prolapse may be having on her bladder function
Example 2: What the investigations will tell us 3. Positive pressure urethrogram Diverticulum 4. Bladder diary May demonstrate excess nocturnal urine production “Fluid abuse” 5. Cystoscopy Cancer
What is the use of urodynamics?
An interesting statistic 80 % of Dutch gynaecologists said they would operate on women with Stress Incontinence without doing UDS (Van Leijsen)
Why would you not want to do urodynamics? Bother for the patient (time, pain, shame) Hassle for the surgeon Urinary tract infection Costs!!! Risk of wrong conclusions / decisions
Some good news There is data to support not doing UDS
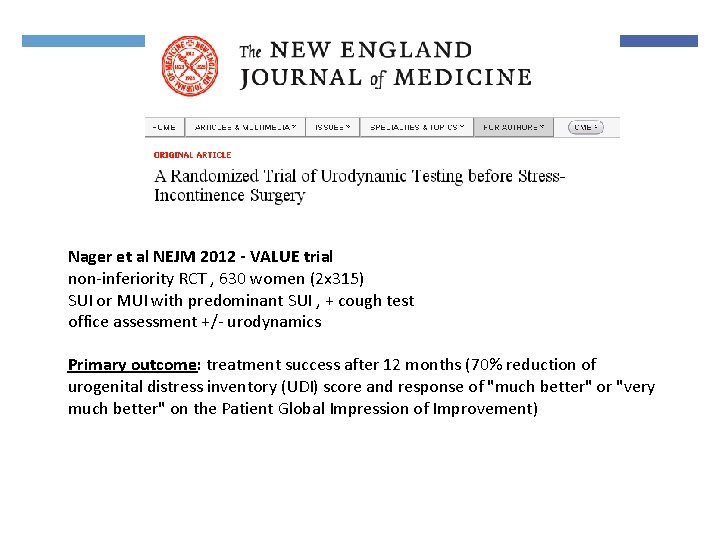
Nager et al NEJM 2012 - VALUE trial non-inferiority RCT , 630 women (2 x 315) SUI or MUI with predominant SUI , + cough test office assessment +/- urodynamics Primary outcome: treatment success after 12 months (70% reduction of urogenital distress inventory (UDI) score and response of "much better" or "very much better" on the Patient Global Impression of Improvement)
Value study Inclusion criteria MESA questionnaire score was important: stress> urge Post Void Residual <150 ml Clinical assessment of urethral hypermobility Positive cough stress test
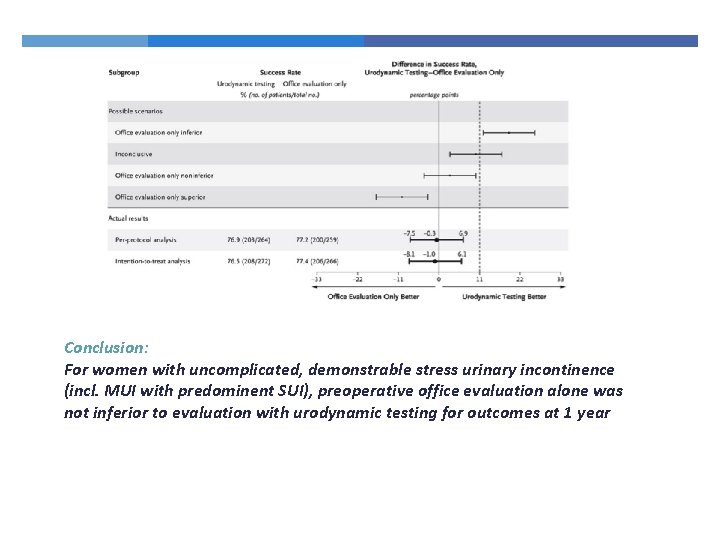
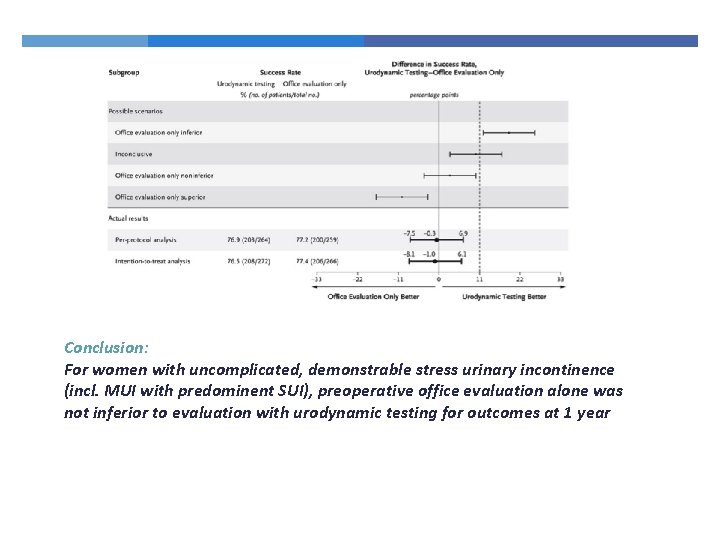
Conclusion: For women with uncomplicated, demonstrable stress urinary incontinence (incl. MUI with predominent SUI), preoperative office evaluation alone was not inferior to evaluation with urodynamic testing for outcomes at 1 year
Urodynamics So – not necessary in all patients When are they necessary?
Use of UDS: 1. Prediction of Intrinsic Sphincter Deficiency
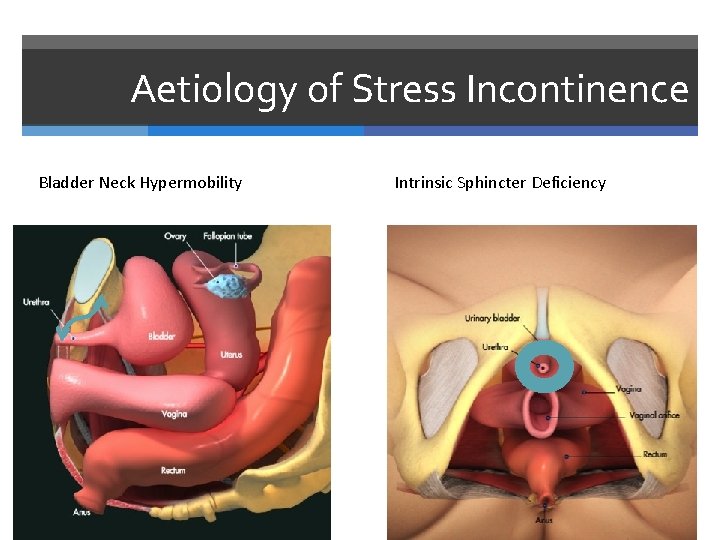
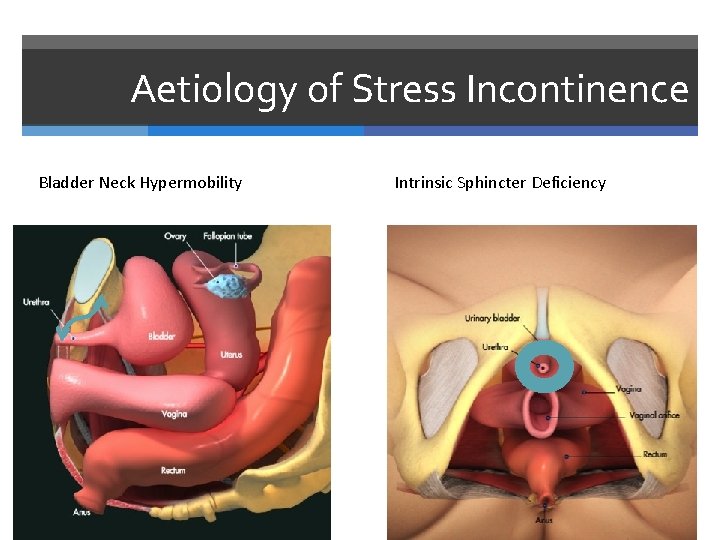
Aetiology of Stress Incontinence Bladder Neck Hypermobility Intrinsic Sphincter Deficiency
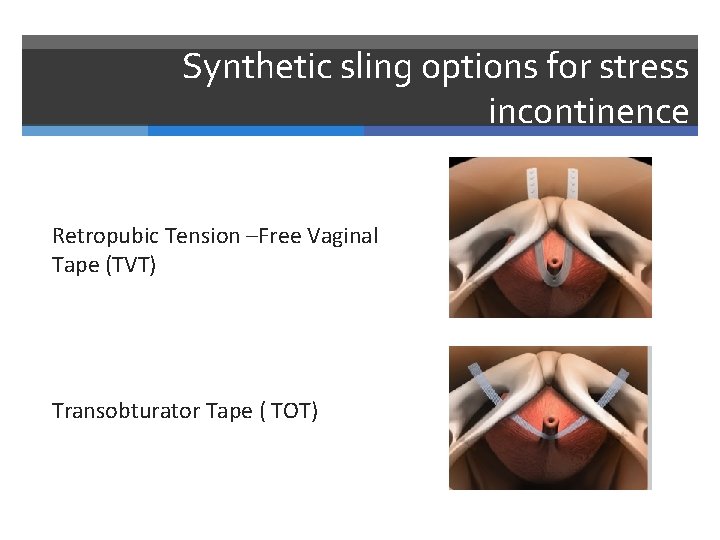
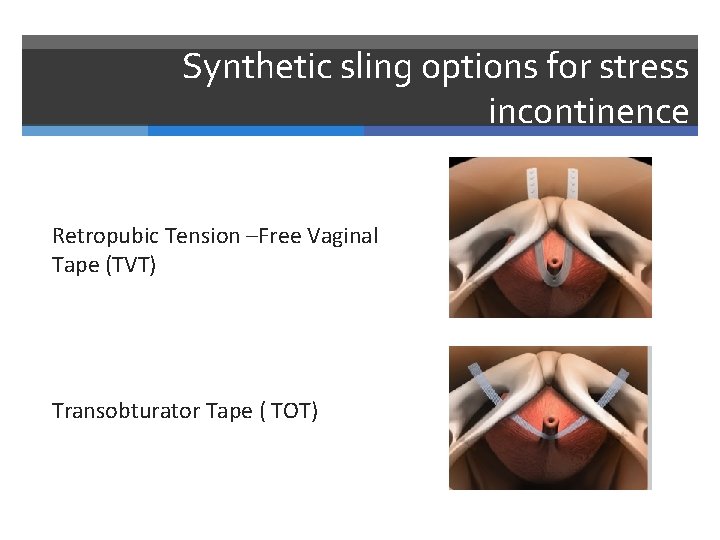
Synthetic sling options for stress incontinence Retropubic Tension –Free Vaginal Tape (TVT) Transobturator Tape ( TOT)
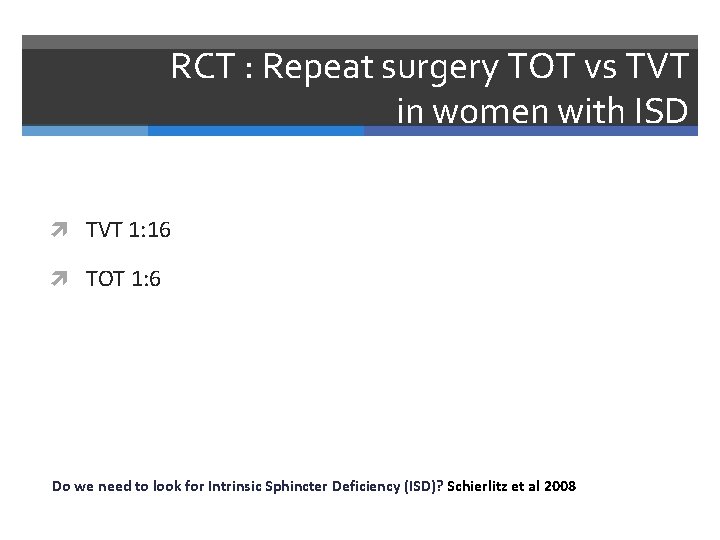
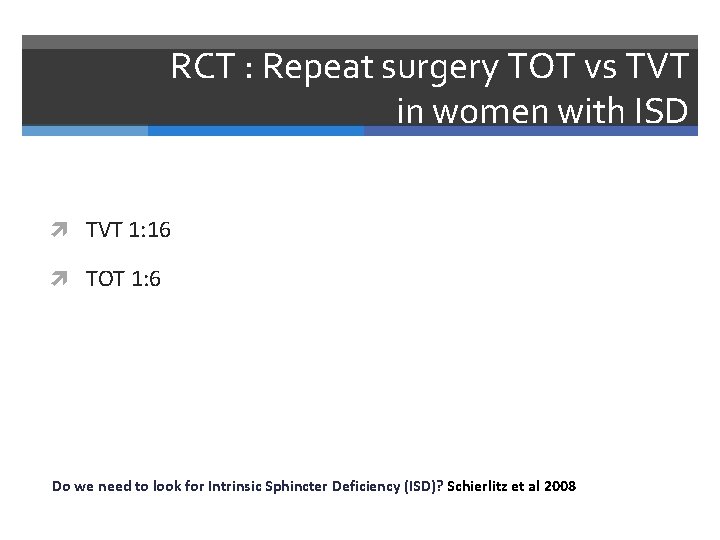
RCT : Repeat surgery TOT vs TVT in women with ISD TVT 1: 16 TOT 1: 6 Do we need to look for Intrinsic Sphincter Deficiency (ISD)? Schierlitz et al 2008
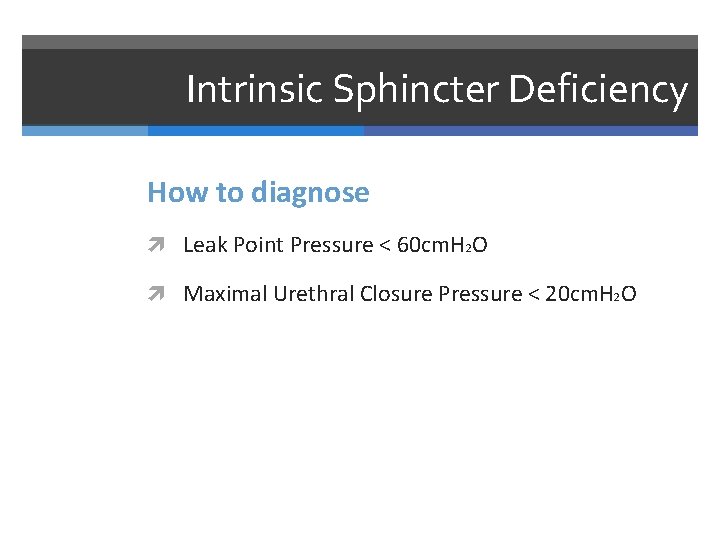
Intrinsic Sphincter Deficiency How to diagnose Leak Point Pressure < 60 cm. H 2 O Maximal Urethral Closure Pressure < 20 cm. H 2 O
For ISD are there alternatives to UDS Bladder neck ultrasound Q-tip test

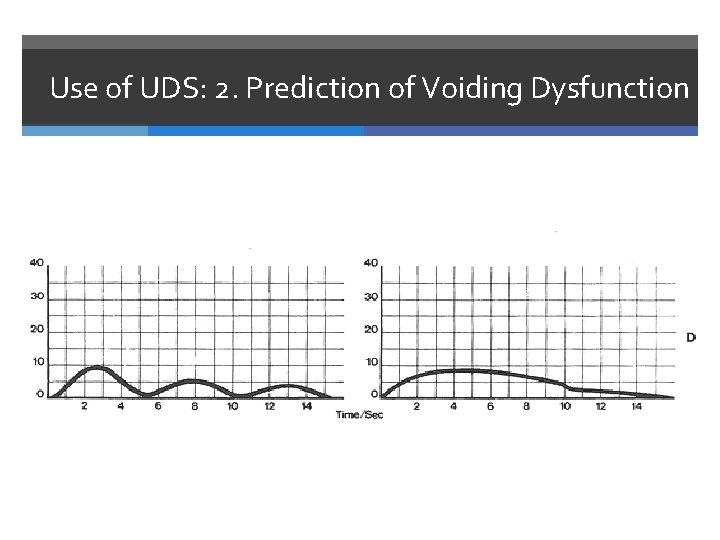
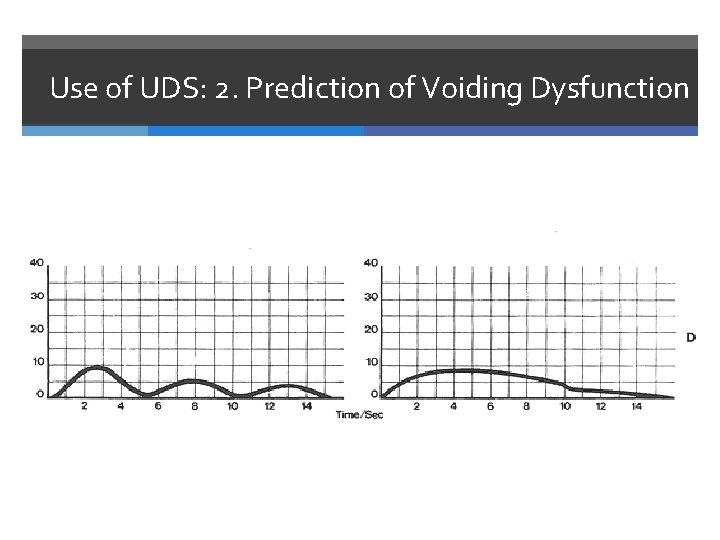
Use of UDS: 2. Prediction of Voiding Dysfunction
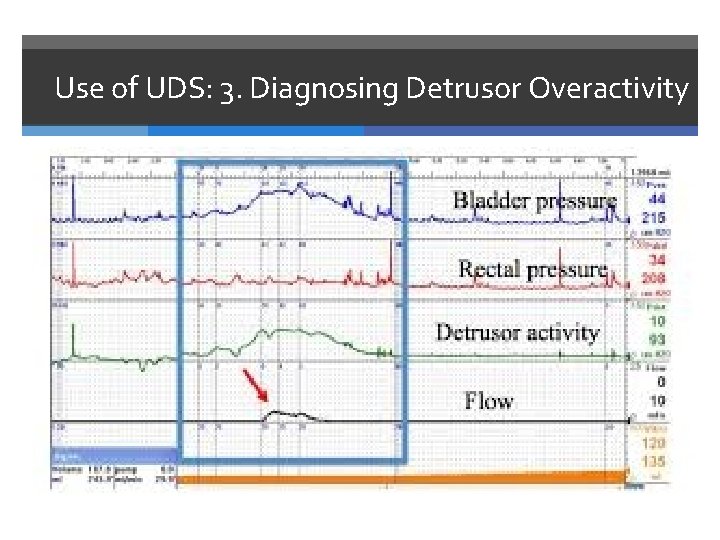
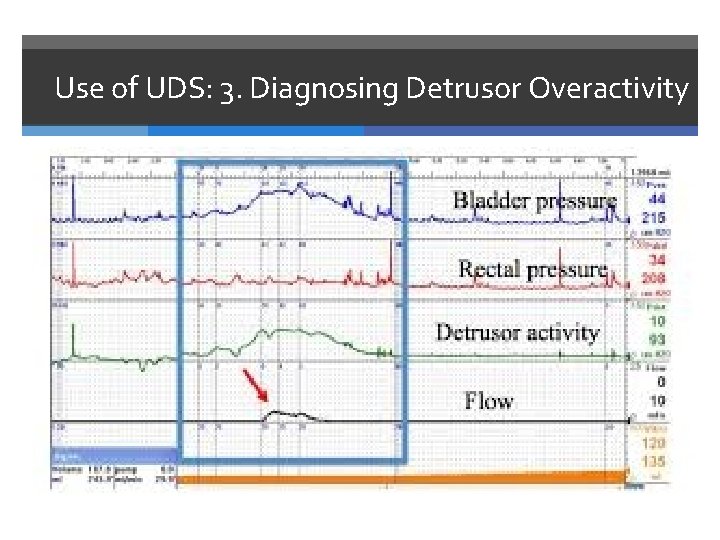
Use of UDS: 3. Diagnosing Detrusor Overactivity
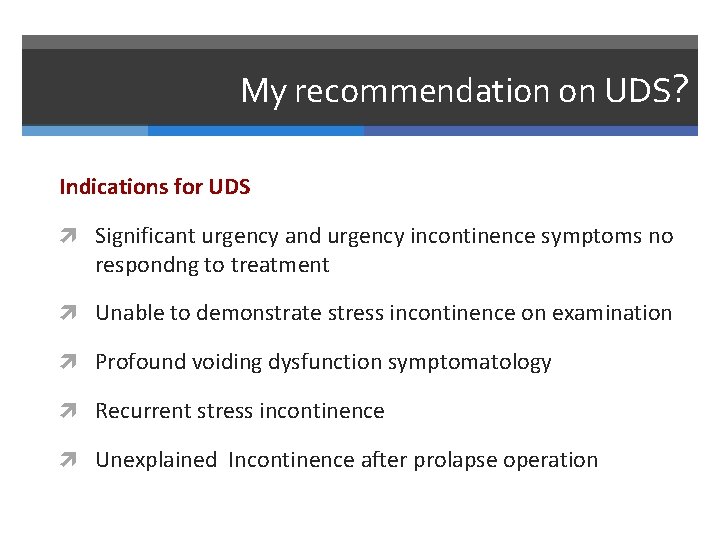
My recommendation on UDS? Indications for UDS Significant urgency and urgency incontinence symptoms no respondng to treatment Unable to demonstrate stress incontinence on examination Profound voiding dysfunction symptomatology Recurrent stress incontinence Unexplained Incontinence after prolapse operation
MESA questionnaire
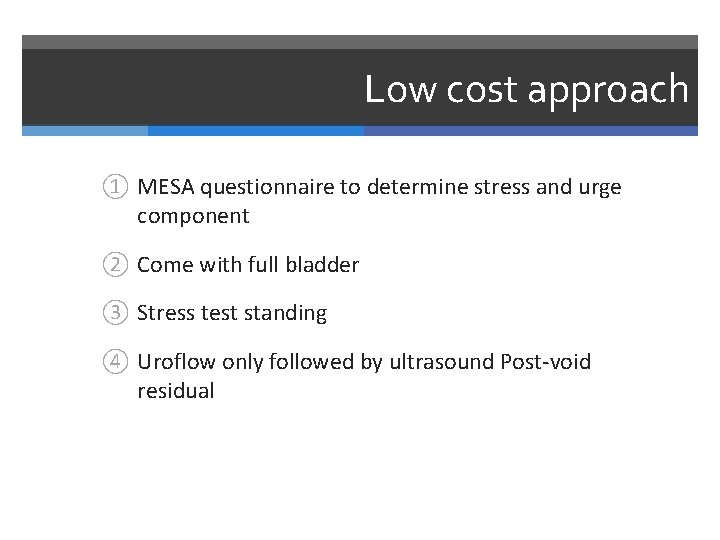
Low cost approach ① MESA questionnaire to determine stress and urge component ② Come with full bladder ③ Stress test standing ④ Uroflow only followed by ultrasound Post-void residual
What about ultrasound?
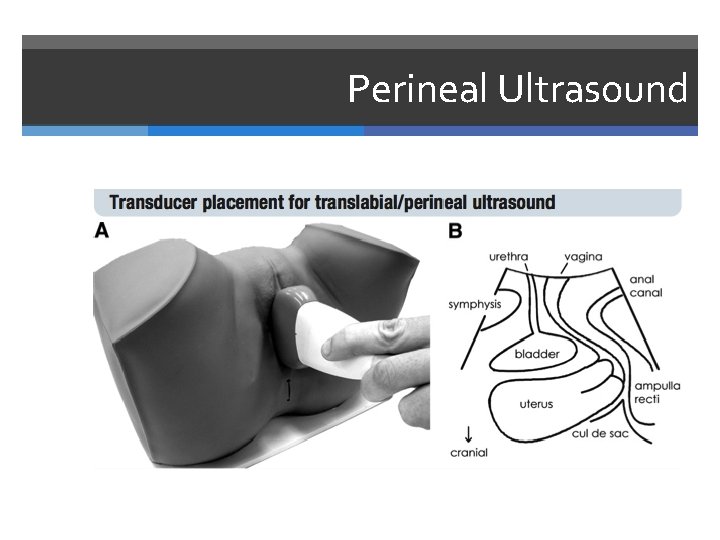
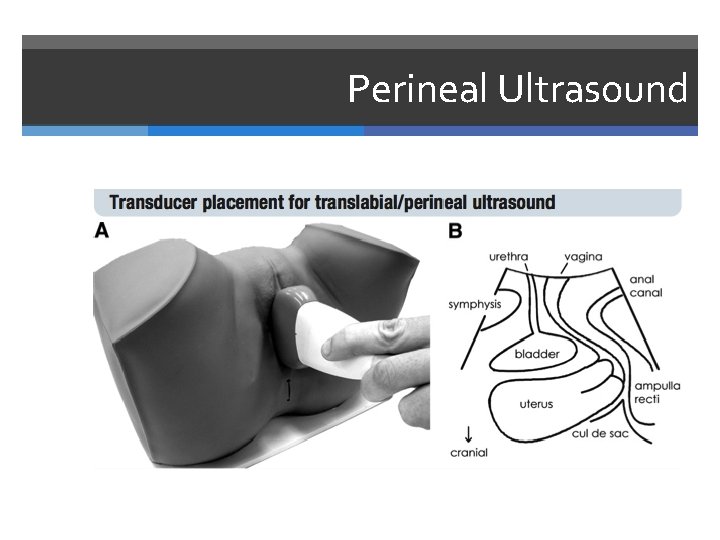
Perineal Ultrasound
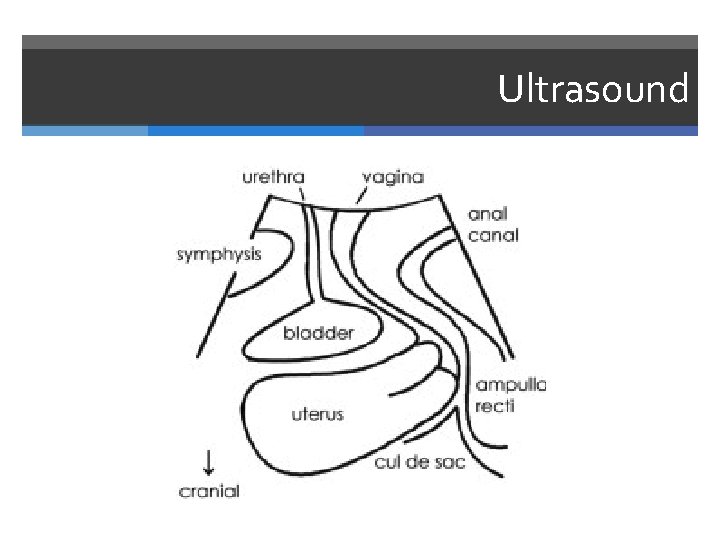
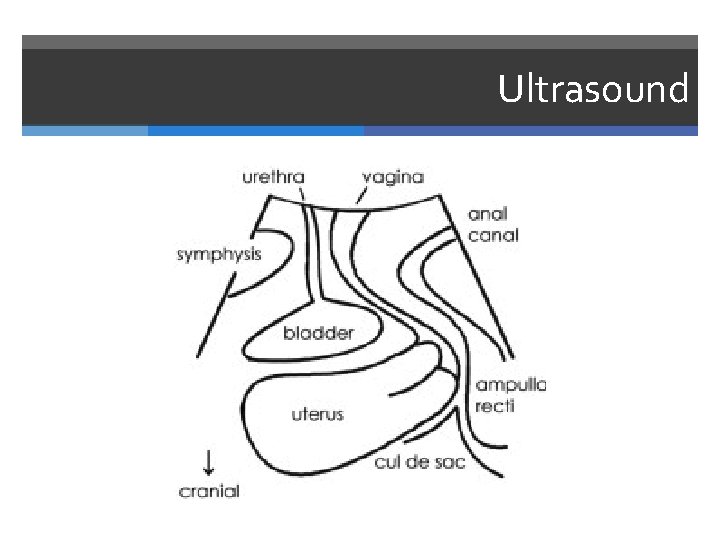
Ultrasound
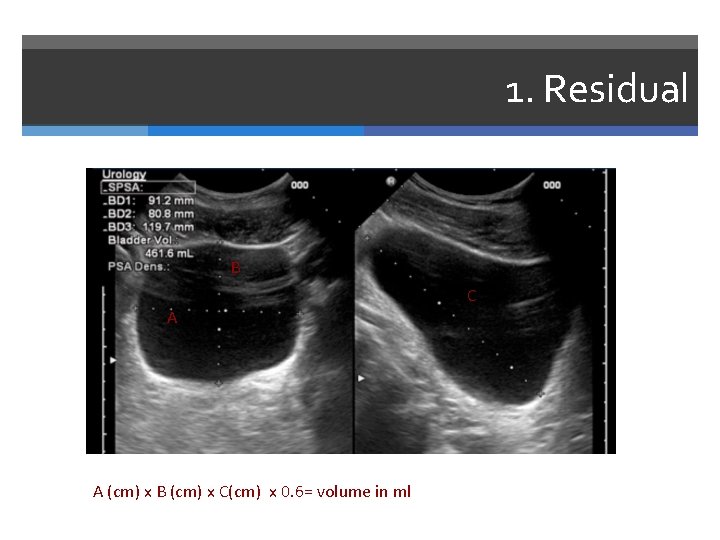
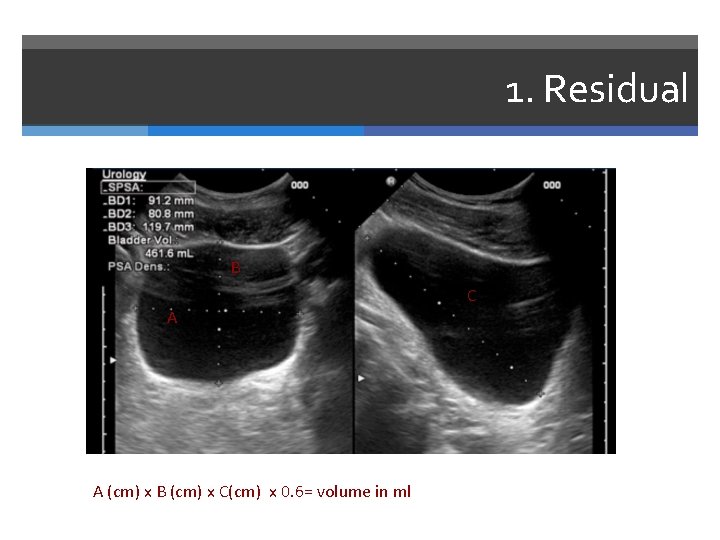
1. Residual B C A A (cm) x B (cm) x C(cm) x 0. 6= volume in ml
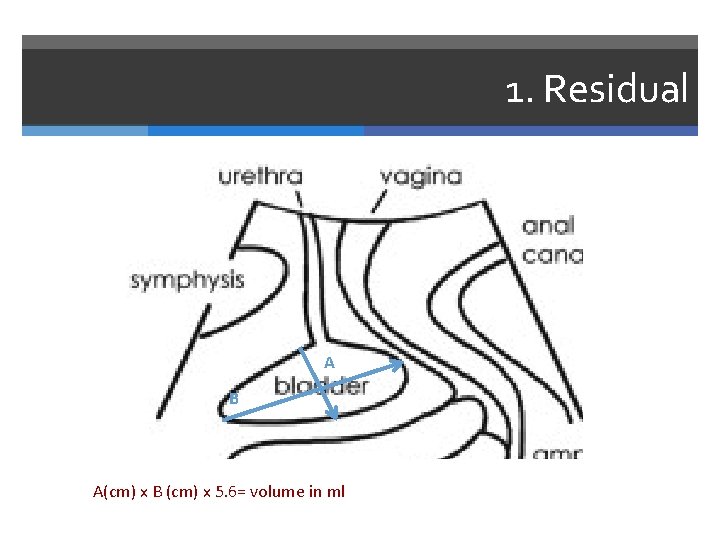
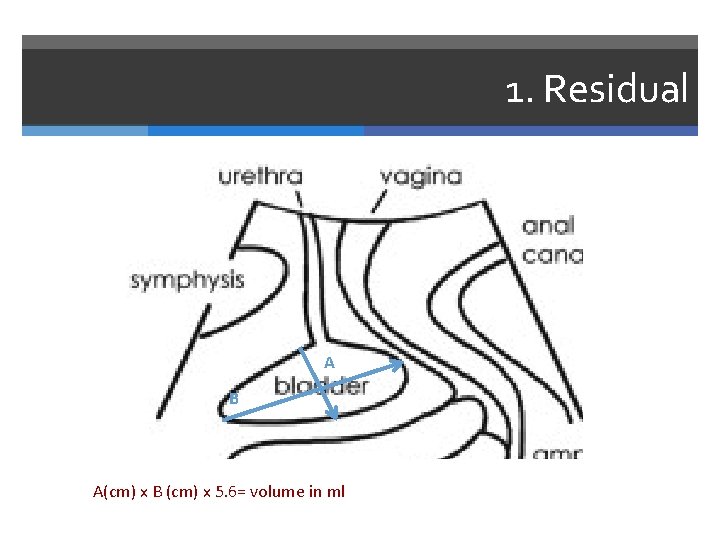
1. Residual B C A A B A(cm) x B (cm) x 5. 6= volume in ml
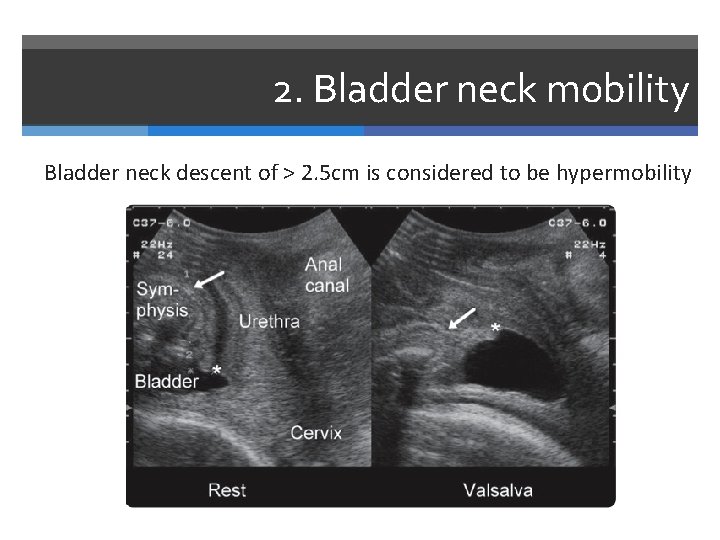
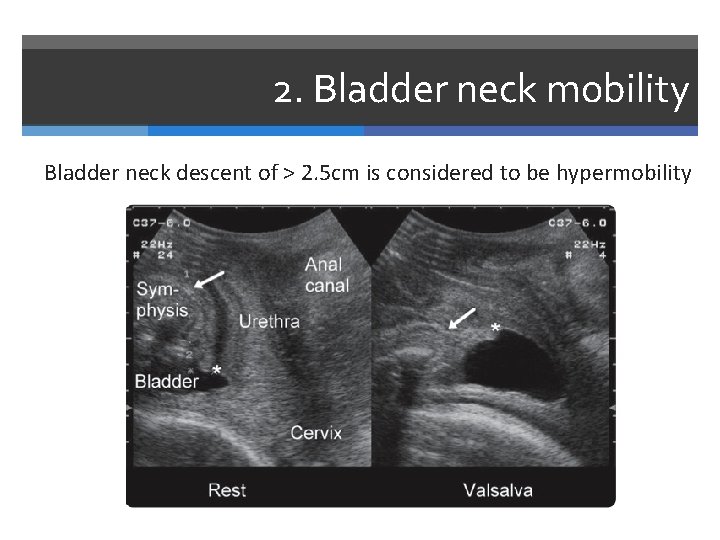
2. Bladder neck mobility Bladder neck descent of > 2. 5 cm is considered to be hypermobility
3. Bladder wall thickness more than 5 mm suggests Detrusor Overactivity
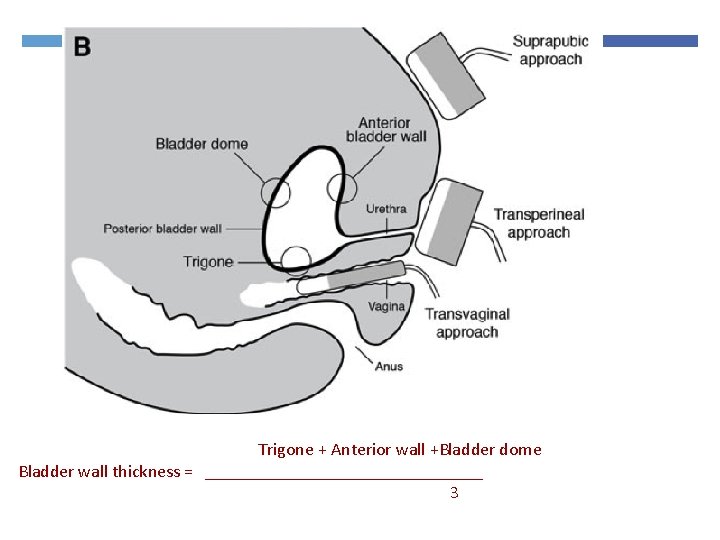
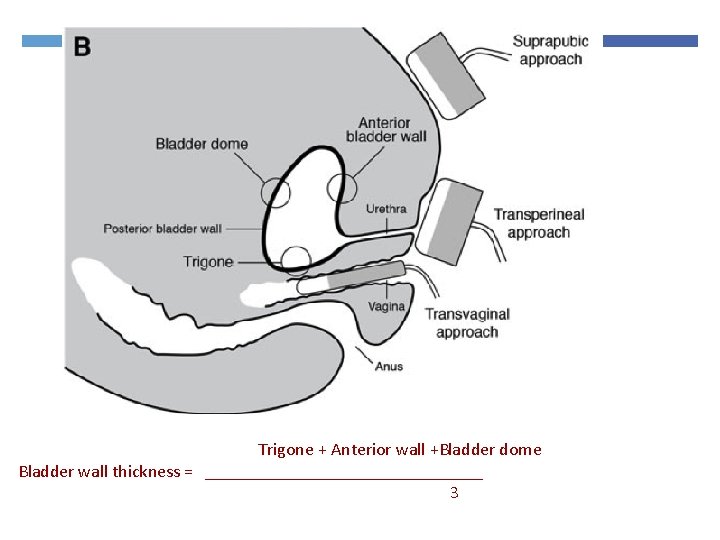
Trigone + Anterior wall +Bladder dome Bladder wall thickness = ________________ 3

4. Funneling

5. Demonstration of stress incontinence

6. Exclude other pathology

7. Evaluate sling complication

Imaging Slings Useful in voiding dysfunction post tape insertion Failed tapes Helps to see if tape has indeed been cut


8. Evaluate voiding dysfunction

Other radiological tests: Cystogram

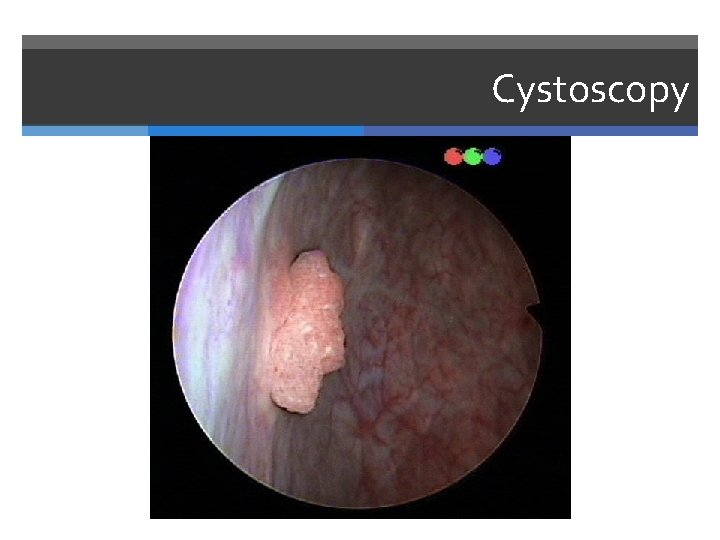
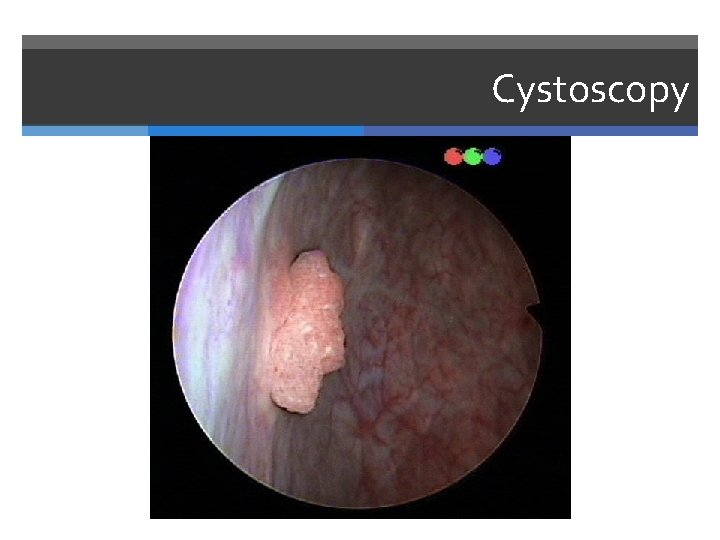
Cystoscopy
Investigations for faecal incontinence
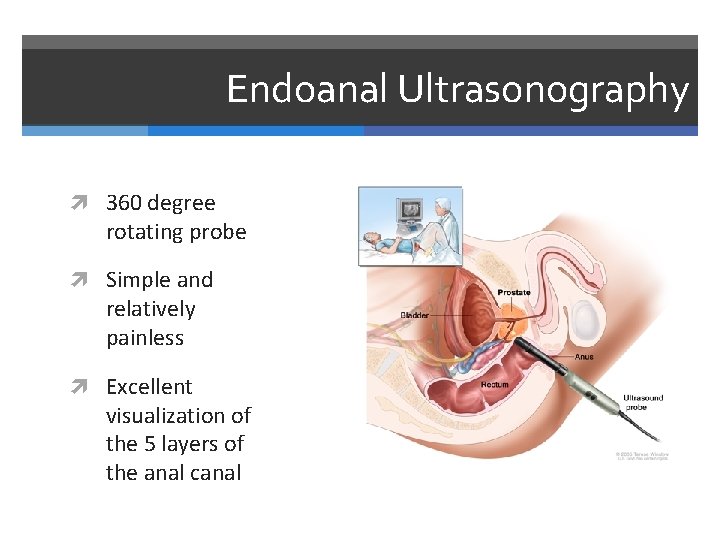
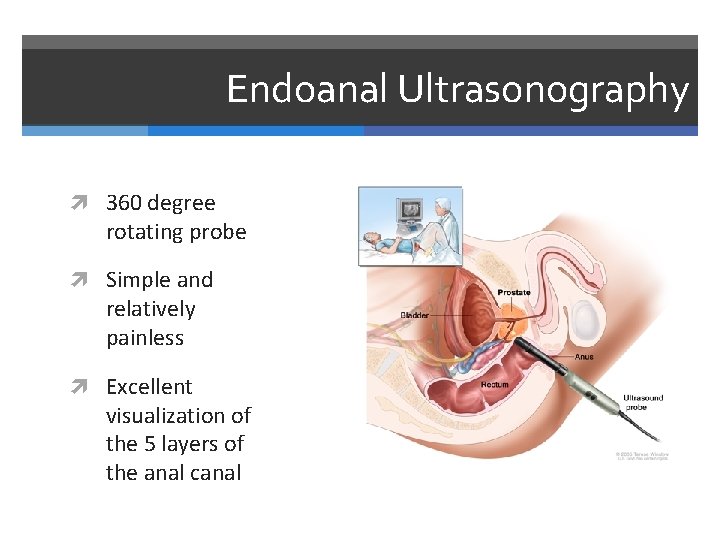
Endoanal Ultrasonography 360 degree rotating probe Simple and relatively painless Excellent visualization of the 5 layers of the anal canal
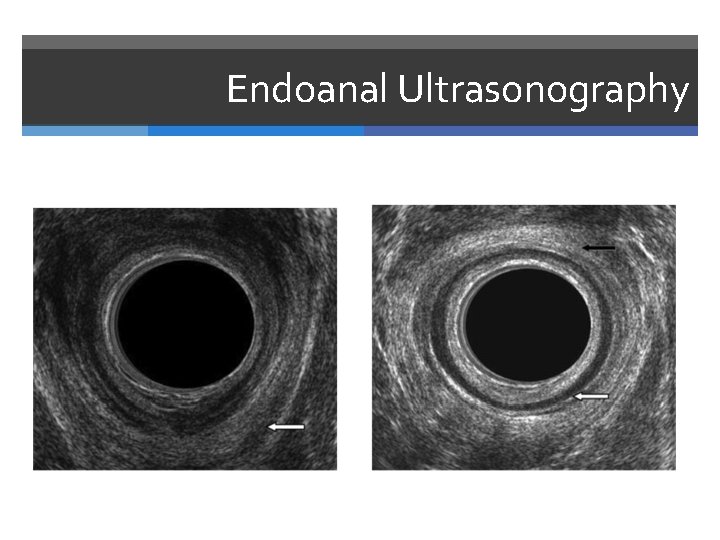
Endoanal Ultrasonography Muscle thickness Scarring Loss of muscle tissue
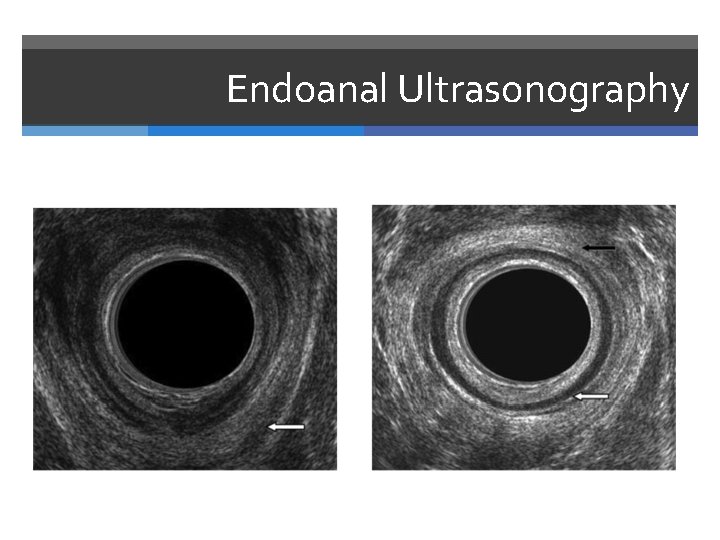
Endoanal Ultrasonography


Take Home UDS not indicated in all cases of SUI Basic ultrasound useful in evaluation of: Residual volume Bladder neck mobility Sling complications Don’t forget to think about other pathology Eg Diverticula and OAB

Download these slides for free at www. urogynaecology. co. za
 Conclusion for scientific method
Conclusion for scientific method Nrich maths investigations
Nrich maths investigations Iliac region
Iliac region Types of statistical investigation
Types of statistical investigation Chs investigations
Chs investigations Pasco county cpi
Pasco county cpi Craigslist wayne
Craigslist wayne Jarrod bowditch
Jarrod bowditch Chapter 6 fingerprints
Chapter 6 fingerprints Chs investigations
Chs investigations Marking bad clusters data hiding technique
Marking bad clusters data hiding technique Investigations
Investigations Antenatal investigations
Antenatal investigations Bmv hours heatherdowns
Bmv hours heatherdowns Why aren t descriptive investigations repeatable
Why aren t descriptive investigations repeatable Guide to computer forensics and investigations 5th edition
Guide to computer forensics and investigations 5th edition Statistical investigations unit 3 section a
Statistical investigations unit 3 section a Tasks performed by computer forensics tools
Tasks performed by computer forensics tools Statuses and their related roles determine the structure
Statuses and their related roles determine the structure What is web role and worker role in azure
What is web role and worker role in azure Role making role taking beispiele
Role making role taking beispiele Fimbrietratt
Fimbrietratt Lågenergihus nyproduktion
Lågenergihus nyproduktion Vad är en punkthöjd
Vad är en punkthöjd Arkimedes princip formel
Arkimedes princip formel Rbk-mätning
Rbk-mätning Förklara densitet för barn
Förklara densitet för barn Elektronik för barn
Elektronik för barn Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Tack för att ni har lyssnat
Tack för att ni har lyssnat Borra hål för knoppar
Borra hål för knoppar Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Bris för vuxna
Bris för vuxna Trög för kemist
Trög för kemist Vad är ett minoritetsspråk
Vad är ett minoritetsspråk Matte större än tecken
Matte större än tecken Autokratiskt ledarskap
Autokratiskt ledarskap Humanitr
Humanitr Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Toppslätskivling dos
Toppslätskivling dos Redogör för vad psykologi är
Redogör för vad psykologi är Mat för idrottare
Mat för idrottare Gumman cirkel sång
Gumman cirkel sång Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Ledarskapsteorier
Ledarskapsteorier Datorkunskap för nybörjare
Datorkunskap för nybörjare Mantel för kvinnor i antikens rom
Mantel för kvinnor i antikens rom Personlig tidbok för yrkesförare
Personlig tidbok för yrkesförare Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Rita perspektiv
Rita perspektiv Fspos vägledning för kontinuitetshantering
Fspos vägledning för kontinuitetshantering Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Bästa kameran för astrofoto
Bästa kameran för astrofoto Tillitsbaserad ledning
Tillitsbaserad ledning Bat mitza
Bat mitza Sju för caesar
Sju för caesar Dikt fri form
Dikt fri form Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Gibbs reflekterande cykel
Gibbs reflekterande cykel Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? Matematisk modellering eksempel
Matematisk modellering eksempel