Integrated Treatment Planning for Intensive Outpatient Programs Presented




- Slides: 55

Integrated Treatment Planning for Intensive Outpatient Programs Presented by: Matt Niece Ph. D. , LCPC Idaho State University niecmatt@isu. edu
Course Description This course is intended for Master’s level counselors, social workers and various service providers to expand their knowledge on the planning of effective treatment as it relates to Intensive Outpatient Programs (IOP). Specifically participants will gain a more in depth understanding of the IOP screening and discharge process, become aware of suggested best practices in the development and execution of treatment plans integrating multiple services, and examine effective documentation strategies for IOP.
Learning Outcomes Overview of Intensive Outpatient Programing and how the treatment team collaboratively moves through the IOP stages with the client. Examine specific screening and assessment approaches that yield critical information for the treatment plan, effective rapport with the client, as well as increased client engagement. Identify the fundamental factors of an IOP treatment plan. Learn how the treatment team takes the information gleaned through initial assessment, develops a tailored treatment plan and adapts this plan based on frequent reassessment. Deeper understanding of criteria for program appropriateness and discharge. Understand effective documentation at various stages throughout IOP. Explore cultural factors that impact treatment planning and therapy.
What is IOP Structured program that occurs a minimum of 3 days/week and maintains at least 9 hours/week for adults and 6 hours/week for children Primarily counseling and education about mental health and addiction-related problems Address moderate behavioral health concerns at a level that is less intensive than partial hospitalization and more intensive than traditional outpatient programs Step-up/down care that varies in intensity and duration based on the individual’s needs Most IOPs last 30 -60 days followed by outpatient continuing care
The Purpose of IOP Services Monitor and maintain stability Decrease moderate signs and symptoms Increase functioning Assist members with integrating into community life
Core Services Program orientation and intake Comprehensive biopsychosocial assessment Family psychotherapy Psychoeducational programming Medication management 24 -hour crisis coverage Transition management and discharge planning Psychiatric evaluation Substance use screening and monitoring Individual treatment planning Group psychotherapy Individual psychotherapy
Principles of IOP Treatment availability Treatment access Enhance existing motivation Trust between counselor and client Client retention priority Individualized assessment and treatment
IOP Goals Achieve abstinence Foster behavioral changes that support abstinence and a new lifestyle Facilitate active participation in community-based support systems Assist clients in identifying and addressing a wide range of pyschosocial problems Assist clients in developing a positive social support network Improve clients’ problem solving skills and coping strategies

Stages of Treatment Stage 1: Treatment engagement Stage 2: Early recovery Stage 3: Maintenance Stage 4: Community Support
Treatment Planning
What is Treatment Planning? Treatment planning is the active, dynamic, complex, fully integrated process in which a clinician partners and collaborates with their client, [client’s family/support when possible, and other helping professionals] to assess, explore, examine, analyze, select, and plan a series of related alternative courses of action by which to arrive at a predetermined, mutually agreed upon set of goals and outcomes. (Stelter, 2015)
Laying the Foundation Screening/assessing appropriateness for IOP services Assessing the individuals readiness to change Conduct a comprehensive biopsychosocial assessment Conduct a multidimensional assessment Address immediate barriers to treatment Risk Assessment Orientation to the program Summarize findings and provide feedback to client
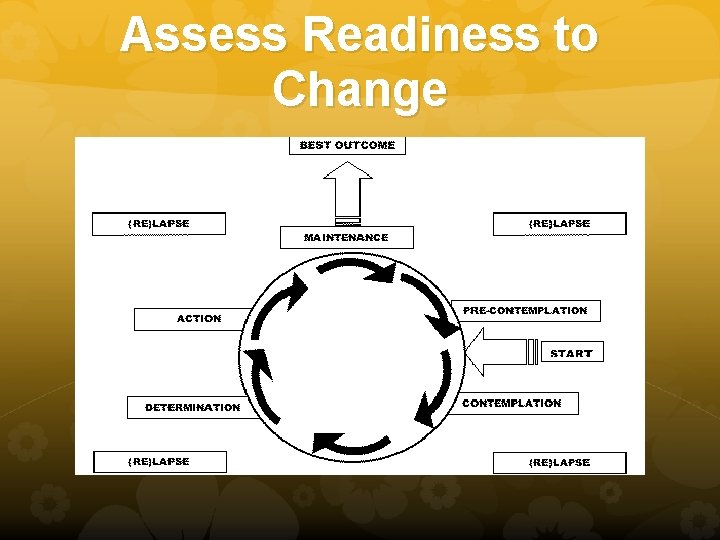
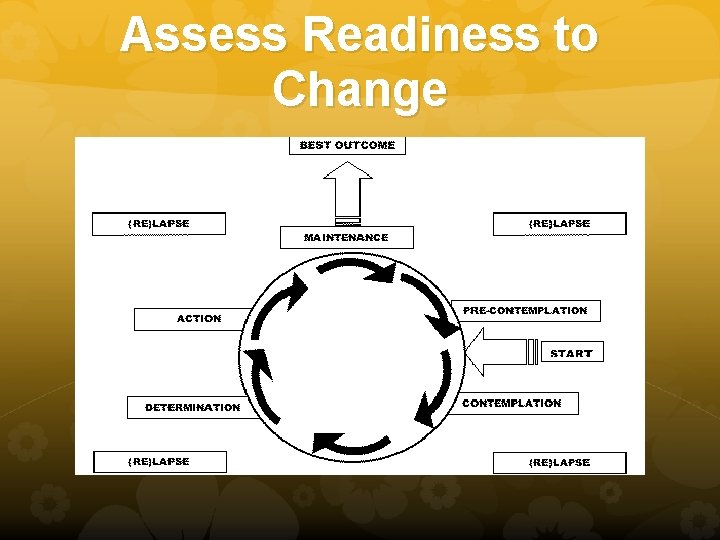
Assess Readiness to Change
4 Profile Types Low importance / Low Confidence - clients do not see change as important or believe they could succeed Low importance / High Confidence – Confident that they could make a change however not motivated to do so High importance / Low Confidence – Express desire to change but have low self-efficacy in changing High importance / High Confidence – They see the importance of changing and also believe that they could succeed
Objectives for Addressing Stage of Change To increase knowledge To increase concern To promote self-efficacy To promote internal attribution To promote self-esteem
A Quality Screener Must be “REAL” R – Respect E – Empathy A – Active collaboration L – Listening
Key Screening Processes Engagement Guiding (Focusing) Evoking Planning
Engagement Warm Greeting Name Role Time Ask Permission Bi-Directional
Guiding (Focusing) Negotiate Agenda Find the Target Behavior (Problem list) Become clear about where the client wants to go (Goals, beginning discussion about discharge)
Evoking Build and Strengthen Motivation Ask about both positives & negatives of target behavior Explore life goals Explore Ambivalence Scale Importance & Confidence Assess Readiness Work to understand a Time & Pace that makes sense for the client AVOID PLANNING TOO SOON!!
Planning Collaborate on setting SMART goals S – Specific M – Meaningful A – Assessable R – Realistic T – Timed
Be careful to avoid the following common mistakes
PLAYING THE EXPERT • • • Having all the answers edges a client into a passive, non-exploratory role. The client is the expert on their life. This stance promotes intrinsic motivation.
Premature focus on change • Does not allow for client’s own pace • Increases resistance
Asking too many questions Client learns to give short answers leading to decreased self-exploration
Intake Session Sample
Biopsychosocial & Multidimensional Assessment The treatment plan must take into account all of the: Physical problems Emotional problems Behavioral problems The Diagnostic Summary is derived from the multidimensional assessment and the interdisciplinary teams’ findings, which include: a summary of the client’s current state and needs, what the problems are, and where they came from.
Address immediate barriers to treatment In the first interactions the treatment team should be cognizant of any immediate barriers to treatment the client might be experiencing Examples: intoxication or withdrawal, acute or chronic medical conditions, psychiatric stability, legal issues, child care issues etc.
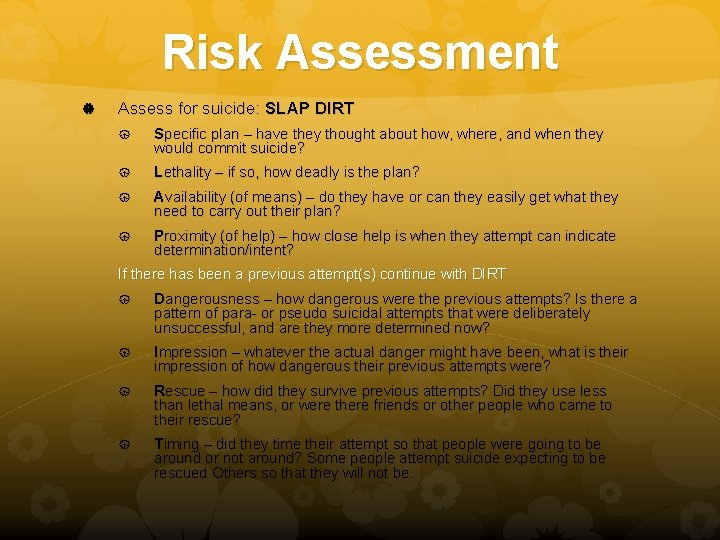
Risk Assessment Assess for suicide: SLAP DIRT Specific plan – have they thought about how, where, and when they would commit suicide? Lethality – if so, how deadly is the plan? Availability (of means) – do they have or can they easily get what they need to carry out their plan? Proximity (of help) – how close help is when they attempt can indicate determination/intent? If there has been a previous attempt(s) continue with DIRT Dangerousness – how dangerous were the previous attempts? Is there a pattern of para- or pseudo suicidal attempts that were deliberately unsuccessful, and are they more determined now? Impression – whatever the actual danger might have been, what is their impression of how dangerous their previous attempts were? Rescue – how did they survive previous attempts? Did they use less than lethal means, or were there friends or other people who came to their rescue? Timing – did they time their attempt so that people were going to be around or not around? Some people attempt suicide expecting to be rescued Others so that they will not be.

Risk Assessment continued Assess immediate threats to client’s safety Do you feel safe at home? Do you feel safe in your relationship? Is someone threatening you now or making you feel unsafe? Take action by connecting to the appropriate resources
Orientation to Program Explanation of program rules and requirements Program’s treatment approach Services offered/required, duration of treatment, frequency and length of sessions, hours of operation, etc. Client’s rights and responsibilities Importance of participation in various areas of treatment, attendance, compliance with program rules, fee payments, follow through, etc. Confidentiality protections and limitations
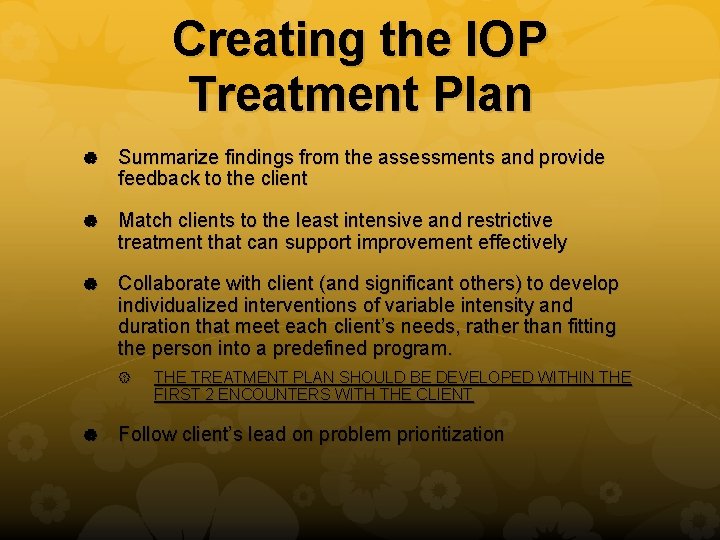
Creating the IOP Treatment Plan Summarize findings from the assessments and provide feedback to the client Match clients to the least intensive and restrictive treatment that can support improvement effectively Collaborate with client (and significant others) to develop individualized interventions of variable intensity and duration that meet each client’s needs, rather than fitting the person into a predefined program. THE TREATMENT PLAN SHOULD BE DEVELOPED WITHIN THE FIRST 2 ENCOUNTERS WITH THE CLIENT Follow client’s lead on problem prioritization
3 Primary Objectives Achieve a lifestyle that is free of the client’s core presenting issue Improve life functioning Prevent relapse or reduce the frequency and severity of relapses SAMHSA 2006
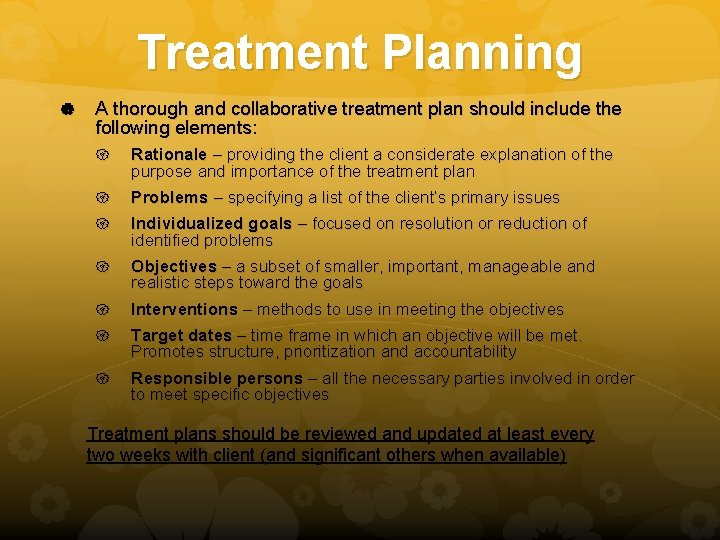
Treatment Planning A thorough and collaborative treatment plan should include the following elements: Rationale – providing the client a considerate explanation of the purpose and importance of the treatment plan Problems – specifying a list of the client’s primary issues Individualized goals – focused on resolution or reduction of identified problems Objectives – a subset of smaller, important, manageable and realistic steps toward the goals Interventions – methods to use in meeting the objectives Target dates – time frame in which an objective will be met. Promotes structure, prioritization and accountability Responsible persons – all the necessary parties involved in order to meet specific objectives Treatment plans should be reviewed and updated at least every two weeks with client (and significant others when available)
Treatment Planning Most treatment plans also include: A few clearly stated, unambiguous goals that do not compete with one another The resources, responsible persons, or activities required Specific dates for reviewing the treatment plan and modifying it to reflect problems addressed or emerging issues to be assessed Specific actions for addressing each goal Objective, easily measureable criteria for monitoring whether actions are completed and goals are accomplished The sequence in which goals are addressed and activities undertaken A specified timeline or target date for goals A signature line for the client to indicate participation in development of the treatment plan and agreement with its specifications
Creating the Problem List This list (like the treatment plan) must be fluid and evolving Problem statements are abstract Problems are evidenced by signs (what you see) and symptoms (what the patient reports) All problems should be substantiated by specific physical, emotional, or behavioral signs and/or symptoms
Goals Are more than the elimination of pathology Are behaviors that will be elicited in the client Are more effective methods of coping that can be learned and implemented Are active not passive Are always client (or client’s family) specific Are inclusive of objectives, interventions, timeframes, and responsible persons
Hints for Developing Initial Goals Increase client’s self-efficacy in order to make beneficial change Follow client’s lead on problem prioritization Choose tasks with high chance of success (keeping appointments, med regiment) Learn from vicarious experiences (group work) Persuade clients that they can and should change (psychoeducation, Person Centered approach, family therapy)
Objectives Are concrete behaviors that can be witnessed Are clearly defined Are measurable Are directed at specific change(s) Are aimed at goals and include interventions, timeframes, and responsible persons
Interventions Even more specific actions that are taken specifically to ensure the identified objectives are accomplished There should be a minimum of one intervention/objective If the objective is not met, additional interventions should be implemented Could include every treatment from any of the multidisciplinary team members. The person(s) responsible for the intervention must develop a target date for the completion of the intervention and be must listed below the intervention in the write up of the treatment plan
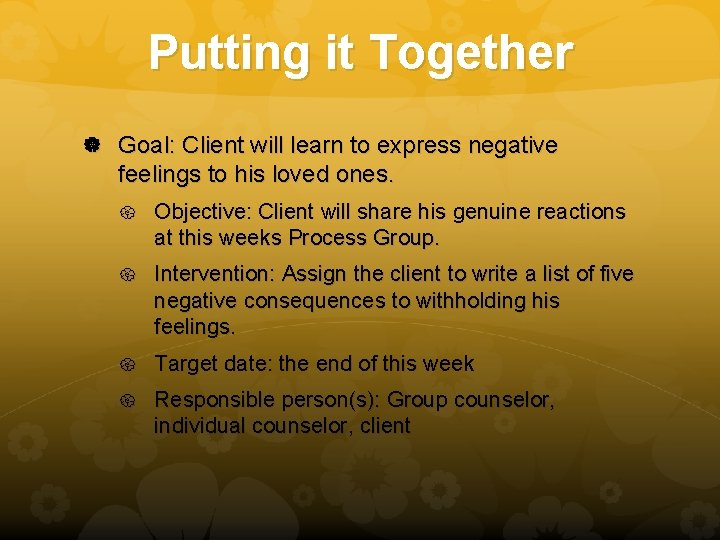
Putting it Together Goal: Client will learn to express negative feelings to his loved ones. Objective: Client will share his genuine reactions at this weeks Process Group. Intervention: Assign the client to write a list of five negative consequences to withholding his feelings. Target date: the end of this week Responsible person(s): Group counselor, individual counselor, client
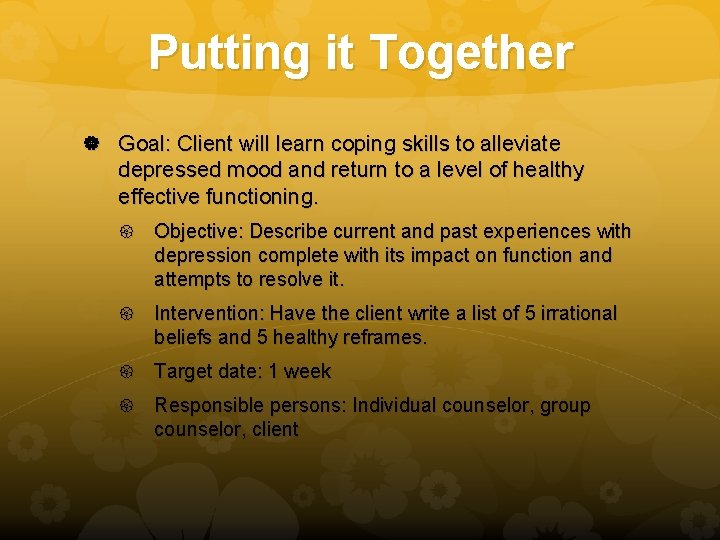
Putting it Together Goal: Client will learn coping skills to alleviate depressed mood and return to a level of healthy effective functioning. Objective: Describe current and past experiences with depression complete with its impact on function and attempts to resolve it. Intervention: Have the client write a list of 5 irrational beliefs and 5 healthy reframes. Target date: 1 week Responsible persons: Individual counselor, group counselor, client
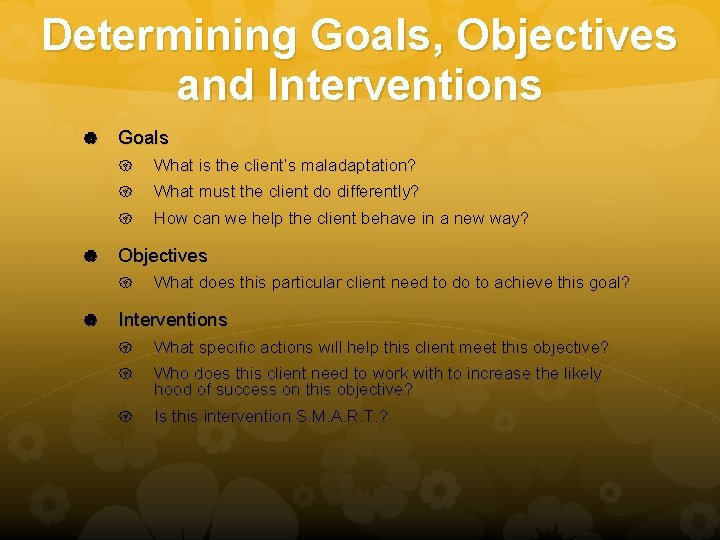
Determining Goals, Objectives and Interventions Goals What is the client’s maladaptation? What must the client do differently? How can we help the client behave in a new way? Objectives What does this particular client need to do to achieve this goal? Interventions What specific actions will help this client meet this objective? Who does this client need to work with to increase the likely hood of success on this objective? Is this intervention S. M. A. R. T. ?
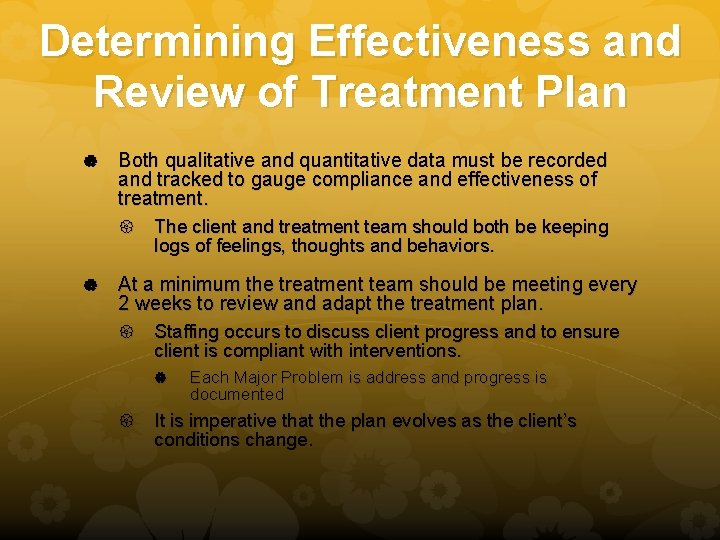
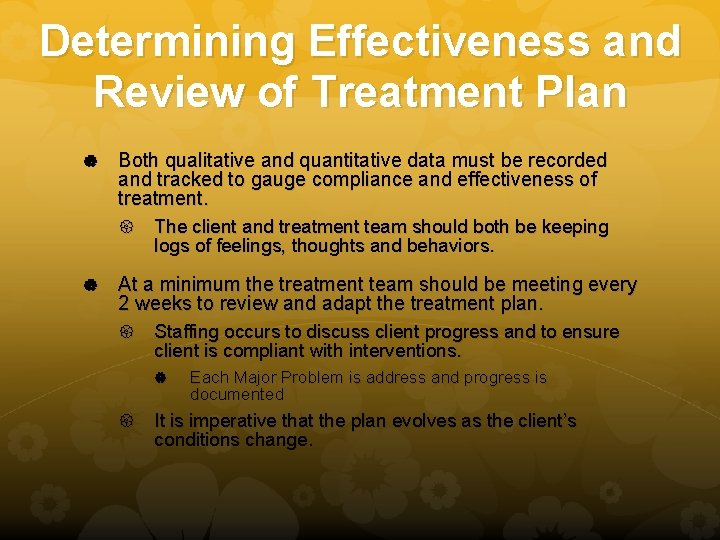
Determining Effectiveness and Review of Treatment Plan Both qualitative and quantitative data must be recorded and tracked to gauge compliance and effectiveness of treatment. The client and treatment team should both be keeping logs of feelings, thoughts and behaviors. At a minimum the treatment team should be meeting every 2 weeks to review and adapt the treatment plan. Staffing occurs to discuss client progress and to ensure client is compliant with interventions. Each Major Problem is address and progress is documented It is imperative that the plan evolves as the client’s conditions change.
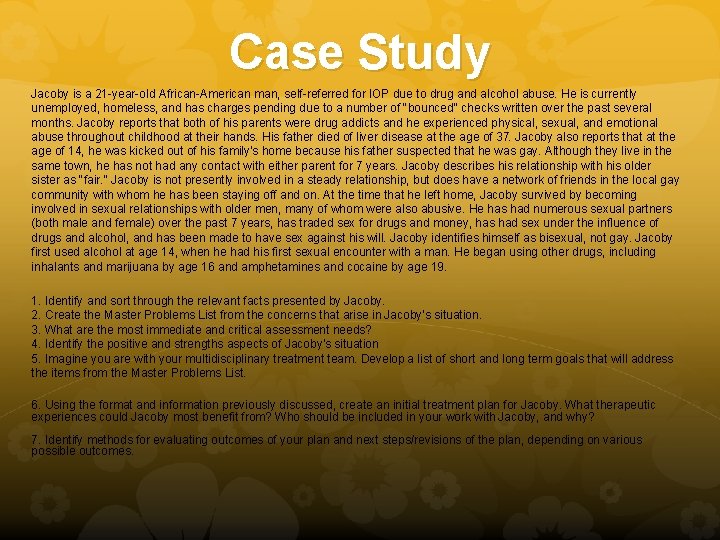
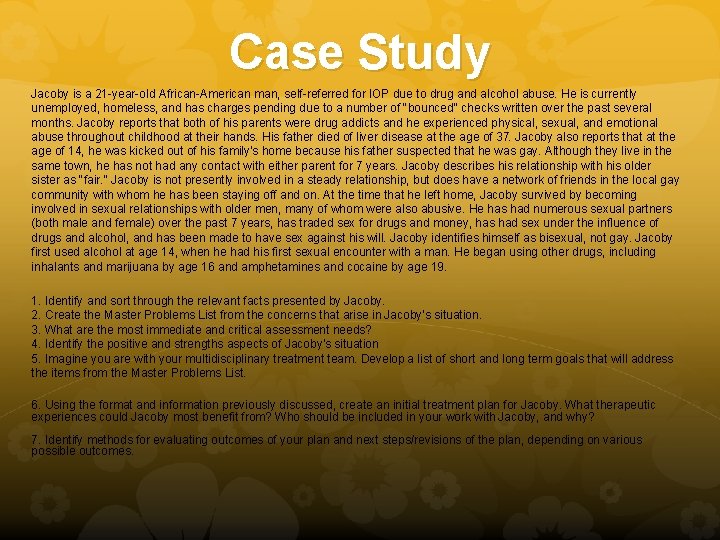
Case Study Jacoby is a 21 -year-old African-American man, self-referred for IOP due to drug and alcohol abuse. He is currently unemployed, homeless, and has charges pending due to a number of "bounced" checks written over the past several months. Jacoby reports that both of his parents were drug addicts and he experienced physical, sexual, and emotional abuse throughout childhood at their hands. His father died of liver disease at the age of 37. Jacoby also reports that at the age of 14, he was kicked out of his family's home because his father suspected that he was gay. Although they live in the same town, he has not had any contact with either parent for 7 years. Jacoby describes his relationship with his older sister as "fair. " Jacoby is not presently involved in a steady relationship, but does have a network of friends in the local gay community with whom he has been staying off and on. At the time that he left home, Jacoby survived by becoming involved in sexual relationships with older men, many of whom were also abusive. He has had numerous sexual partners (both male and female) over the past 7 years, has traded sex for drugs and money, has had sex under the influence of drugs and alcohol, and has been made to have sex against his will. Jacoby identifies himself as bisexual, not gay. Jacoby first used alcohol at age 14, when he had his first sexual encounter with a man. He began using other drugs, including inhalants and marijuana by age 16 and amphetamines and cocaine by age 19. 1. Identify and sort through the relevant facts presented by Jacoby. 2. Create the Master Problems List from the concerns that arise in Jacoby's situation. 3. What are the most immediate and critical assessment needs? 4. Identify the positive and strengths aspects of Jacoby's situation 5. Imagine you are with your multidisciplinary treatment team. Develop a list of short and long term goals that will address the items from the Master Problems List. 6. Using the format and information previously discussed, create an initial treatment plan for Jacoby. What therapeutic experiences could Jacoby most benefit from? Who should be included in your work with Jacoby, and why? 7. Identify methods for evaluating outcomes of your plan and next steps/revisions of the plan, depending on various possible outcomes.
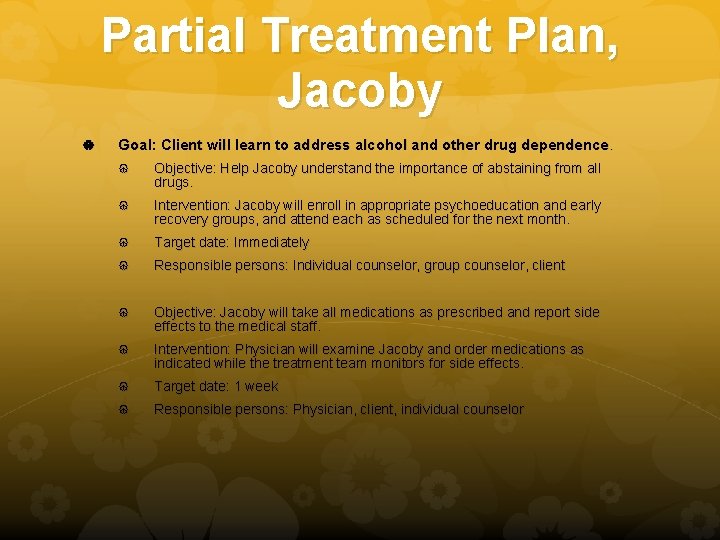
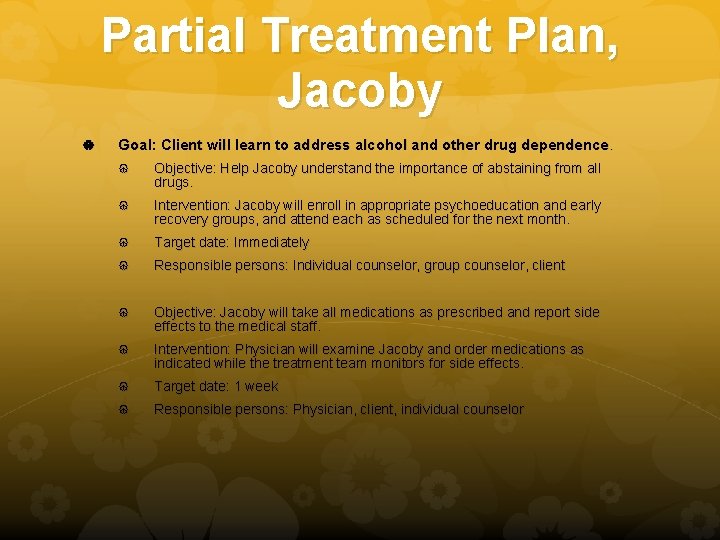
Partial Treatment Plan, Jacoby Goal: Client will learn to address alcohol and other drug dependence. Objective: Help Jacoby understand the importance of abstaining from all drugs. Intervention: Jacoby will enroll in appropriate psychoeducation and early recovery groups, and attend each as scheduled for the next month. Target date: Immediately Responsible persons: Individual counselor, group counselor, client Objective: Jacoby will take all medications as prescribed and report side effects to the medical staff. Intervention: Physician will examine Jacoby and order medications as indicated while the treatment team monitors for side effects. Target date: 1 week Responsible persons: Physician, client, individual counselor
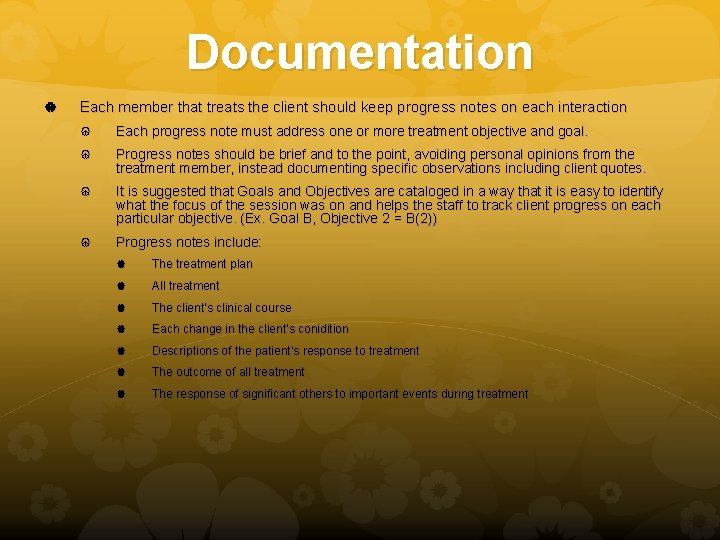
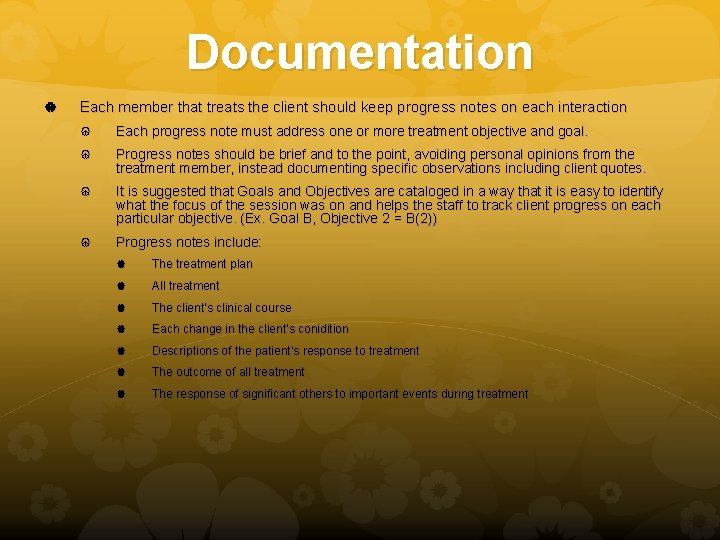
Documentation Each member that treats the client should keep progress notes on each interaction Each progress note must address one or more treatment objective and goal. Progress notes should be brief and to the point, avoiding personal opinions from the treatment member, instead documenting specific observations including client quotes. It is suggested that Goals and Objectives are cataloged in a way that it is easy to identify what the focus of the session was on and helps the staff to track client progress on each particular objective. (Ex. Goal B, Objective 2 = B(2)) Progress notes include: The treatment plan All treatment The client’s clinical course Each change in the client’s conidition Descriptions of the patient’s response to treatment The outcome of all treatment The response of significant others to important events during treatment
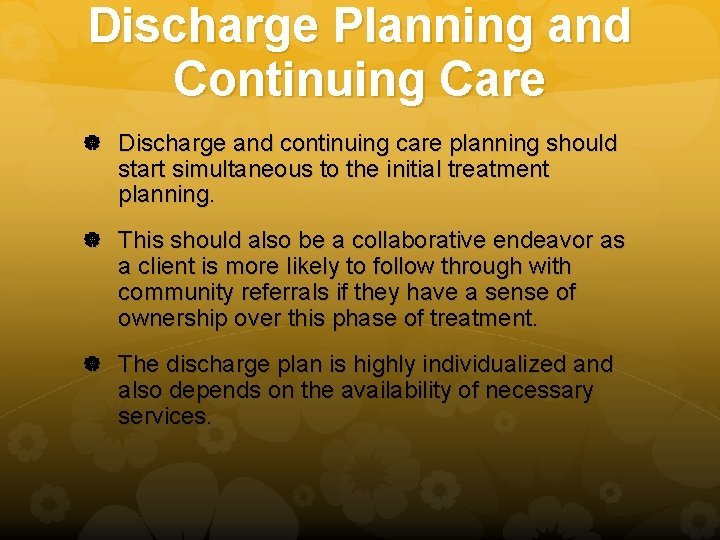
Discharge Planning and Continuing Care Discharge and continuing care planning should start simultaneous to the initial treatment planning. This should also be a collaborative endeavor as a client is more likely to follow through with community referrals if they have a sense of ownership over this phase of treatment. The discharge plan is highly individualized and also depends on the availability of necessary services.
Discharge Guidelines It is appropriate to transfer or discharge a client from a current level of care if they meet the following criteria: The individual has achieved the goals articulated in his or her individualized treatment plan thus resolving the problems that justified admission to the present level of care. The individual has been unable to resolve the problems that justified admission to the present level of care, despite amendments to the treatment plan. Treatment at another level of care or type of service is therefore indicated. OR The individual has demonstrated a lack of capacity to resolve their problems. Treatment at another level of care or type of service is therefore indicated. OR OR The individual has experienced an intensification of his or her problems, or has developed a new problem(s), and can be treated effectively only at a more intensive level of care. Before transferring or being discharged each of the six dimensions of ASAM criteria should be reviewed.
Continuing Community Care Goals Maintain abstinence and a healthy lifestyle Develop independence from the treatment program Maintain social network connections Establish strong connections with support groups Establish recreational activities and develop new interests Duration Years, ongoing Counselor Activities Assist in developing a plan for continuing recovery Acquaint client with local resources Encourage attendance at alumni or booster sessions Provide biannual checkups Completion Criteria Clients may need community support for the rest of their lives.
Specific Populations Generally speaking there are specific populations that inherently have additional concerns and circumstances that require specialized programs to address their needs and increase the likelihood of successful treatment. Justice System Population problems: Employment, finances, housing, education, transportation, unresolved legal matters, substance use, medical issues, sanctioned treatment, etc. Women: victims of violence/abuse, pregnancy/postpartum, child care, partner support, stigma, isolation, gender insensitivity of IOPs, etc. Adolescents: developmental stages, variety of cognitive functioning and attention issues, existential awareness, family involvement, consent for treatment, habilitative vs. rehabilitative services, etc.
Cultural Considerations Culture – a broad concept that refers to a shared set of beliefs, norms, and values among any group of people, whether based on ethnicity or on a shared affiliation and identity. “Most IOP counselors are White and come from the dominant Western culture, but nearly half of clients seeking treatment are not White” (Mulvey et al. 2003)
Culturally Competent Clinicians Counselor Self-awareness Have a deep understanding of your own morals, values, beliefs. More specifically know your biases and assumptions while continually working to uncover personal blind spots. Client worldview Know the general shared set of beliefs, norms and values of different cultures, while remembering that each client is an individual and not simply an extension of their identified culture. Therapeutic relationship Understand how the counselor and client worldviews might intersect and impact how the client benefits from treatment (or not). Adapt therapeutic approach to maximize the client’s benefit. Areas where worldviews differ: Spirituality, collectivism, definition of family, communication styles, learning styles, etc. Issues affecting therapeutic relationship: Issues with authority, respect and dignity, acceptance of help, sense of stigma, level of acculturation, etc. Counseling and Advocacy Interventions Ensure that interventions devised to meet therapeutic objectives are tailored to the individual and address cultural considerations. Identify how the treatment team can intervene with, and on behalf of the client at intrapersonal, interpersonal, institutional, community, and public policy levels.
Return to Case Study How would you describe Jacoby’s culture? How does Jacoby’s sexual orientation affect the treatment plan and process? What is your personal reaction to his being bisexual? It what ways does Jacoby’s age and ethnicity factor in to treatment planning and his individual program? What kinds of reactions might you expect from him throughout treatment, and how do you plan to respond? What are the implications for community interventions and advocacy that are associated with Jacoby’s case?

Resources See Appendices for additional resources