Hypertension Dr Mustafa Sahin Ankara Universitesi Tp Fakltesi




































- Slides: 73
Hypertension Dr. Mustafa Sahin Ankara Universitesi Tıp Fakültesi Endokrinoloji ve Metabolizma Hastalıkları Bilim Dalı
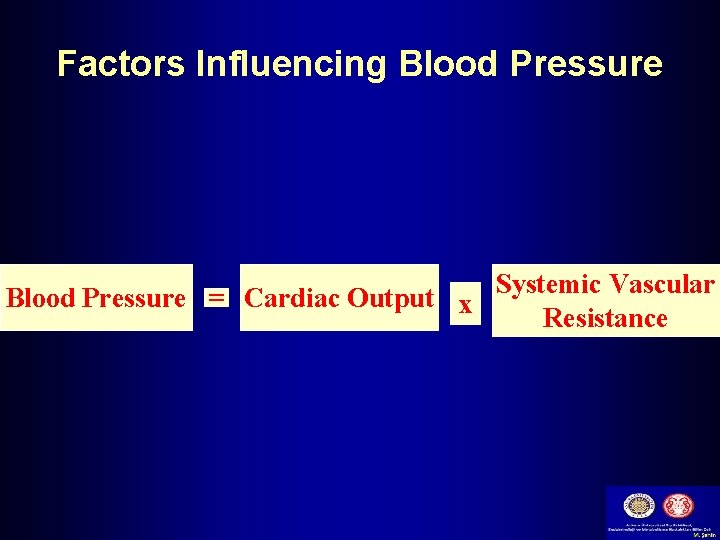
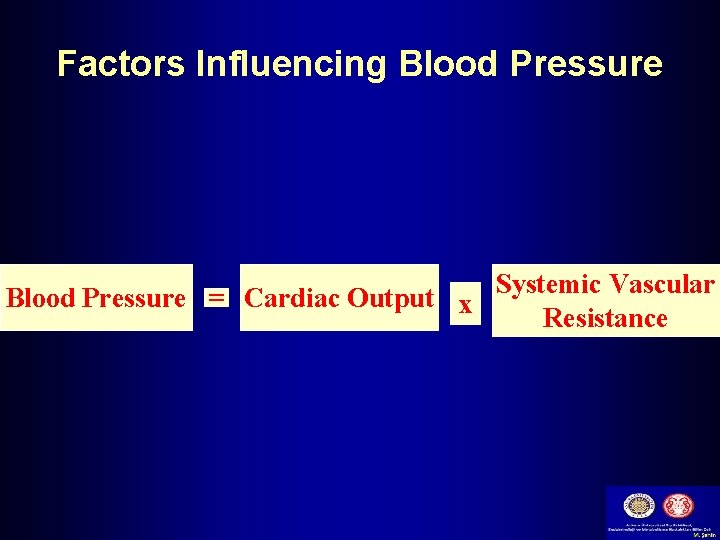
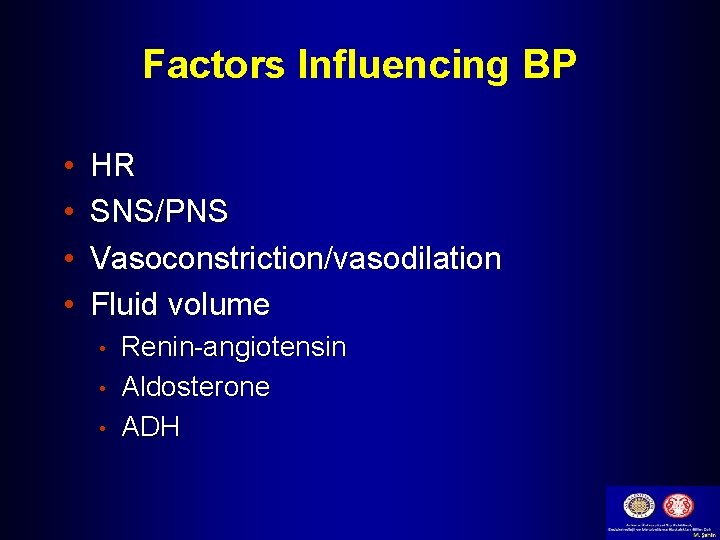
Factors Influencing Blood Pressure = Cardiac Output x Systemic Vascular Resistance
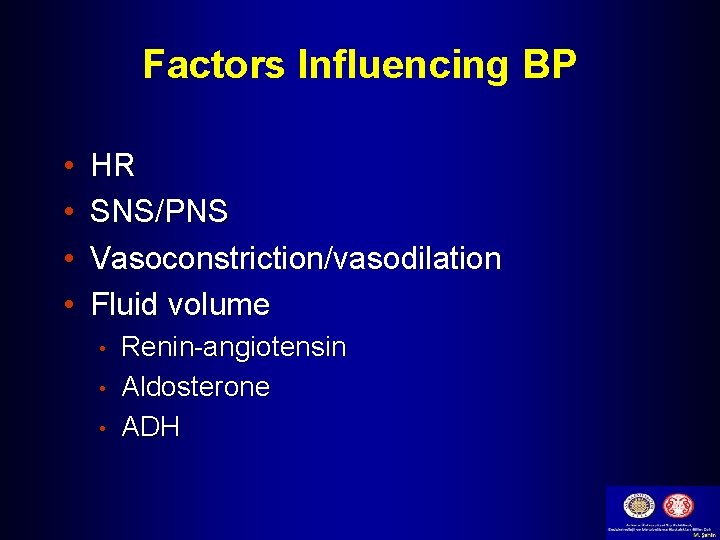
Factors Influencing BP • • HR SNS/PNS Vasoconstriction/vasodilation Fluid volume • • • Renin-angiotensin Aldosterone ADH
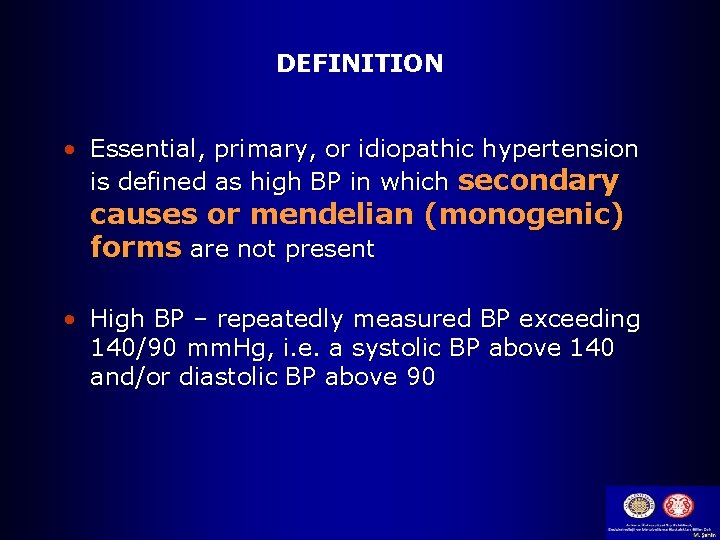
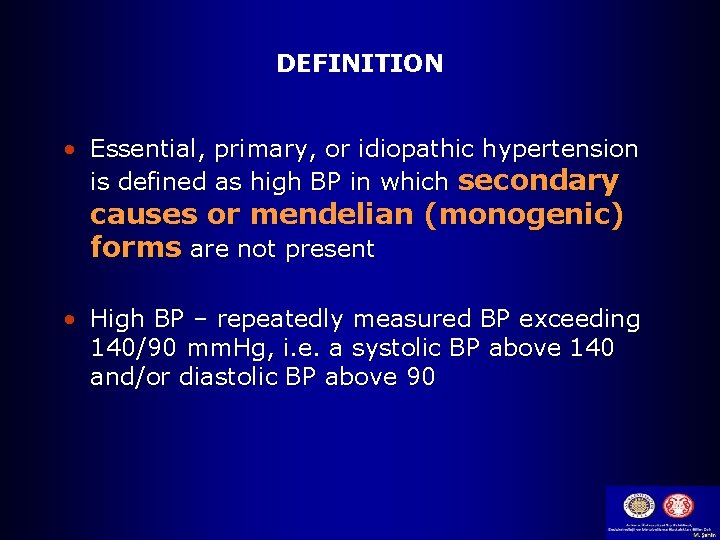
DEFINITION • Essential, primary, or idiopathic hypertension is defined as high BP in which secondary causes or mendelian (monogenic) forms are not present • High BP – repeatedly measured BP exceeding 140/90 mm. Hg, i. e. a systolic BP above 140 and/or diastolic BP above 90
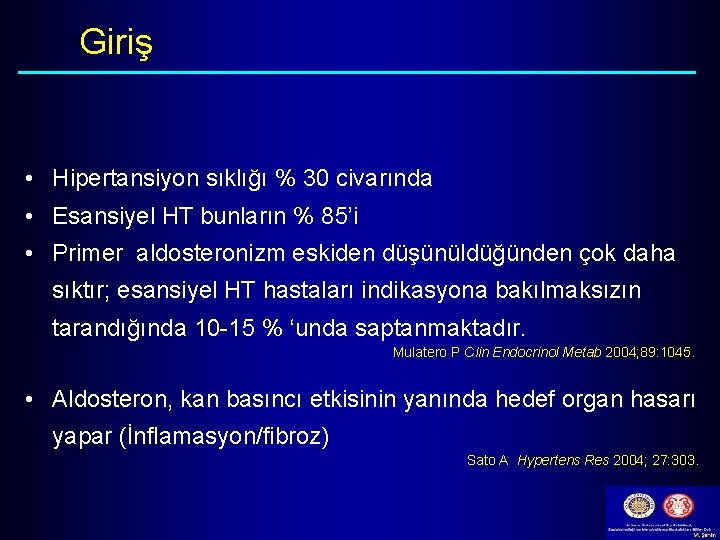
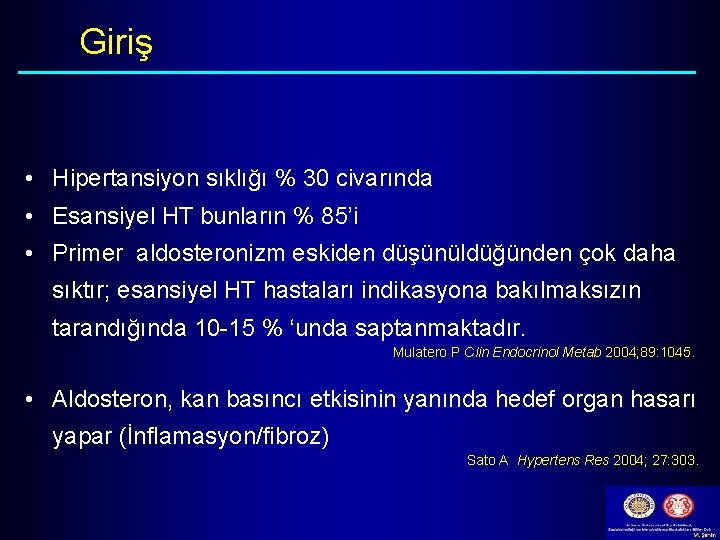
Giriş • Hipertansiyon sıklığı % 30 civarında • Esansiyel HT bunların % 85’i • Primer aldosteronizm eskiden düşünüldüğünden çok daha sıktır; esansiyel HT hastaları indikasyona bakılmaksızın tarandığında 10 -15 % ‘unda saptanmaktadır. Mulatero P Clin Endocrinol Metab 2004; 89: 1045. • Aldosteron, kan basıncı etkisinin yanında hedef organ hasarı yapar (İnflamasyon/fibroz) Sato A Hypertens Res 2004; 27: 303.
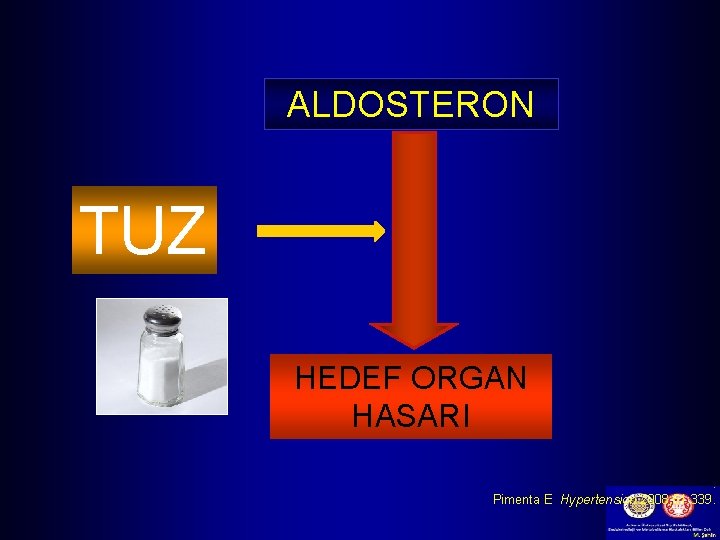
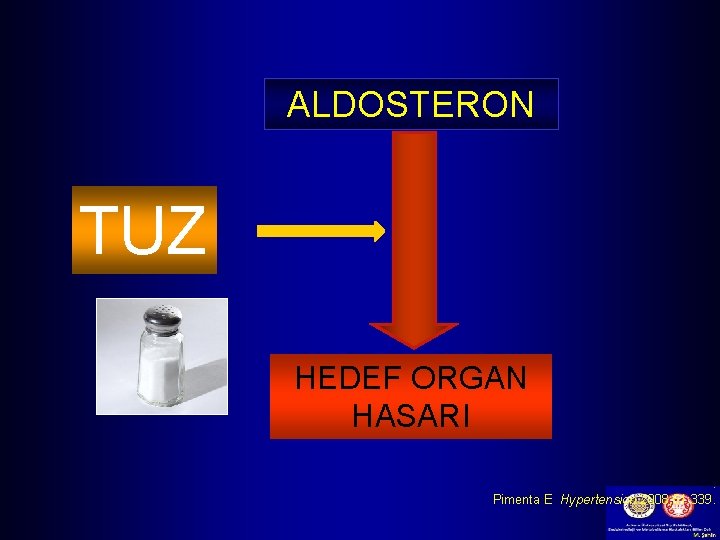
ALDOSTERON TUZ HEDEF ORGAN HASARI. Pimenta E Hypertension 2008; 51: 339.
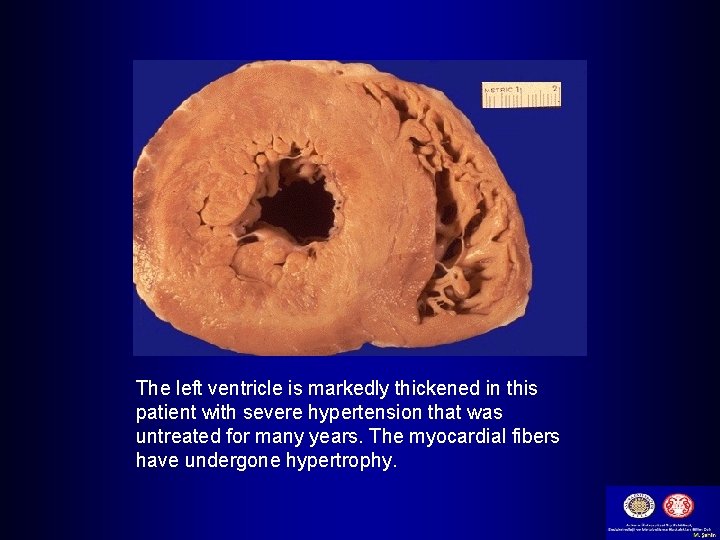
Hypertension Complications § Hypertensive Heart Disease • Coronary artery disease • Left ventricular hypertrophy • Heart failure
Hypertension Complications § Cerebrovascular Disease • Stroke § Peripheral Vascular Disease § Nephrosclerosis § Retinal Damage
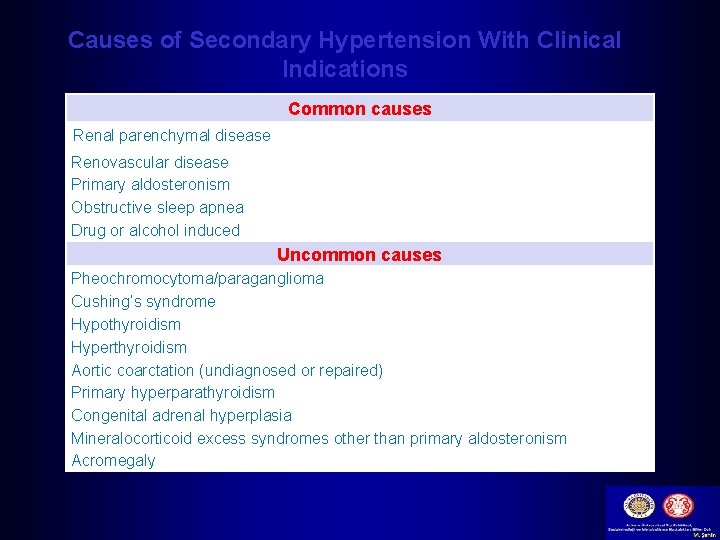
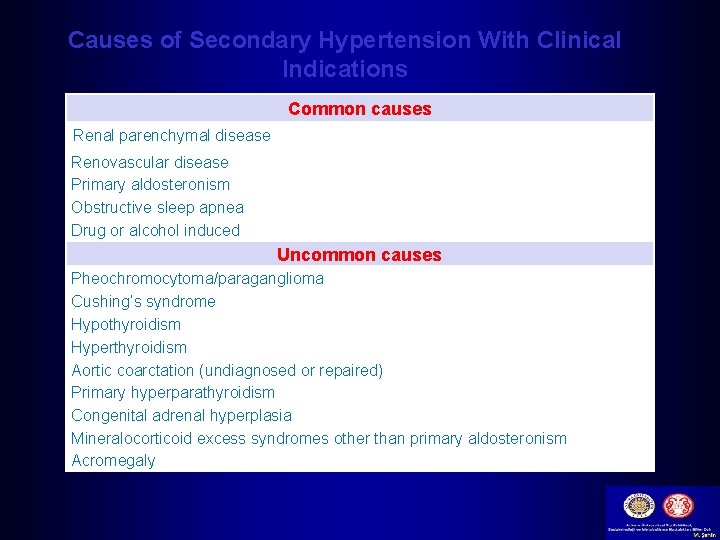
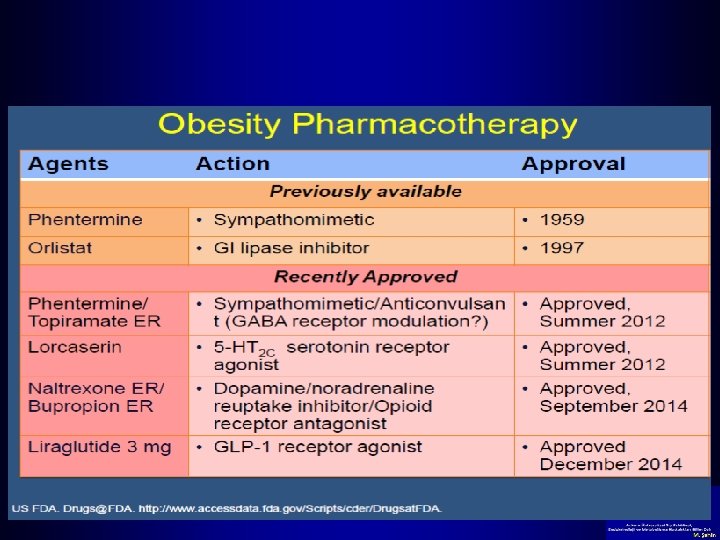
Causes of Secondary Hypertension With Clinical Indications Common causes Renal parenchymal disease Renovascular disease Primary aldosteronism Obstructive sleep apnea Drug or alcohol induced Uncommon causes Pheochromocytoma/paraganglioma Cushing’s syndrome Hypothyroidism Hyperthyroidism Aortic coarctation (undiagnosed or repaired) Primary hyperparathyroidism Congenital adrenal hyperplasia Mineralocorticoid excess syndromes other than primary aldosteronism Acromegaly



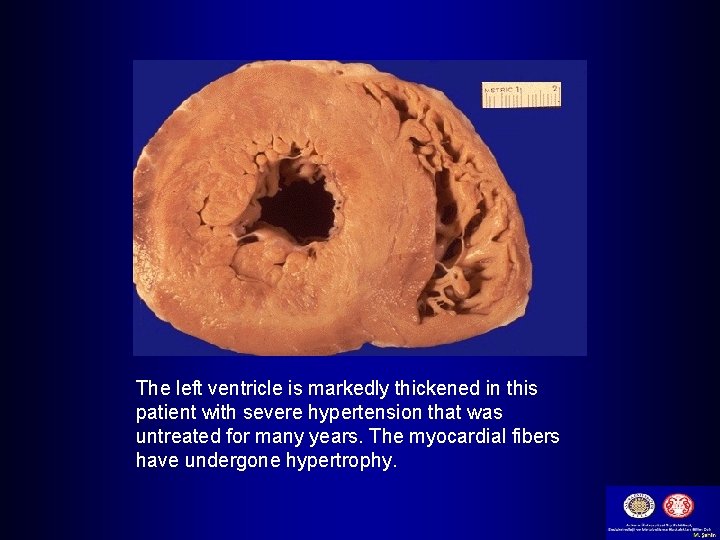
The left ventricle is markedly thickened in this patient with severe hypertension that was untreated for many years. The myocardial fibers have undergone hypertrophy.
BP Measurement • At least two measurements should be made and the average recorded. • Clinicians should provide to patients their specific BP numbers and the BP goal of their treatment.
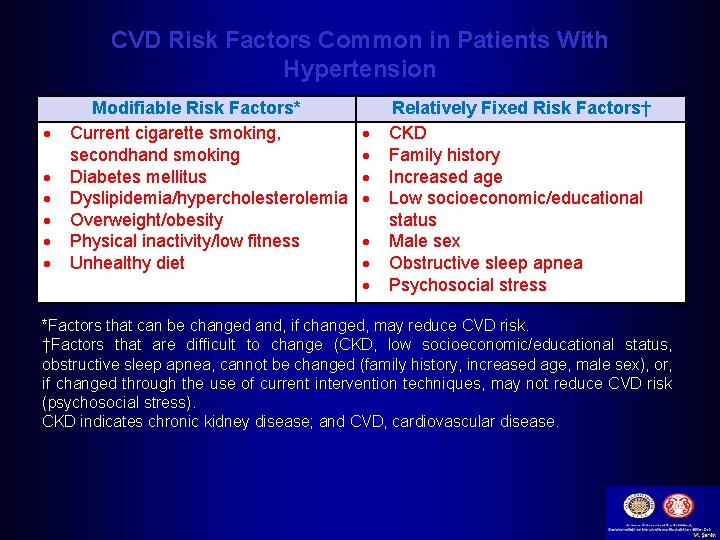
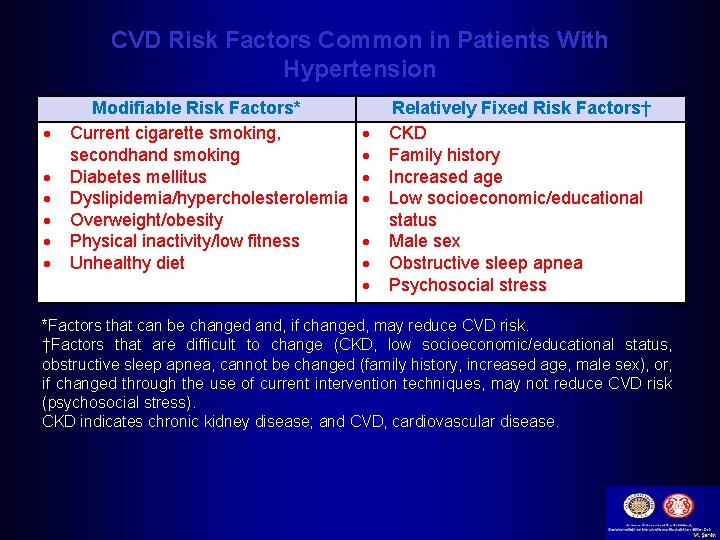
CVD Risk Factors Common in Patients With Hypertension Modifiable Risk Factors* Current cigarette smoking, secondhand smoking Diabetes mellitus Dyslipidemia/hypercholesterolemia Overweight/obesity Physical inactivity/low fitness Unhealthy diet Relatively Fixed Risk Factors† CKD Family history Increased age Low socioeconomic/educational status Male sex Obstructive sleep apnea Psychosocial stress *Factors that can be changed and, if changed, may reduce CVD risk. †Factors that are difficult to change (CKD, low socioeconomic/educational status, obstructive sleep apnea, cannot be changed (family history, increased age, male sex), or, if changed through the use of current intervention techniques, may not reduce CVD risk (psychosocial stress). CKD indicates chronic kidney disease; and CVD, cardiovascular disease.
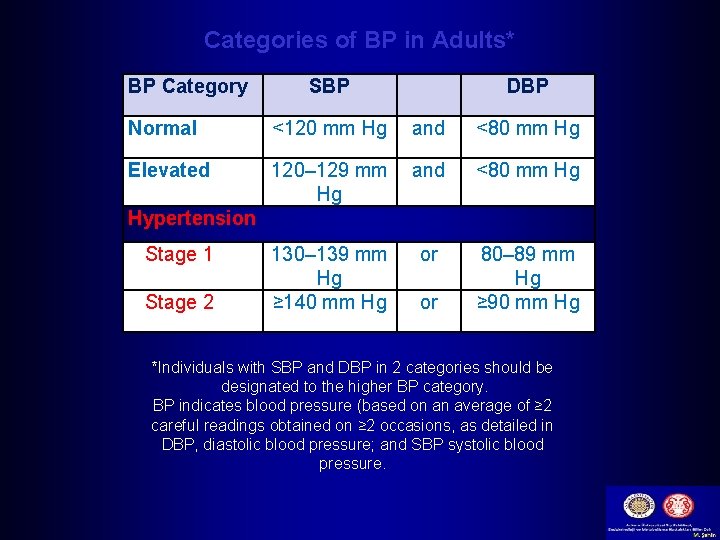
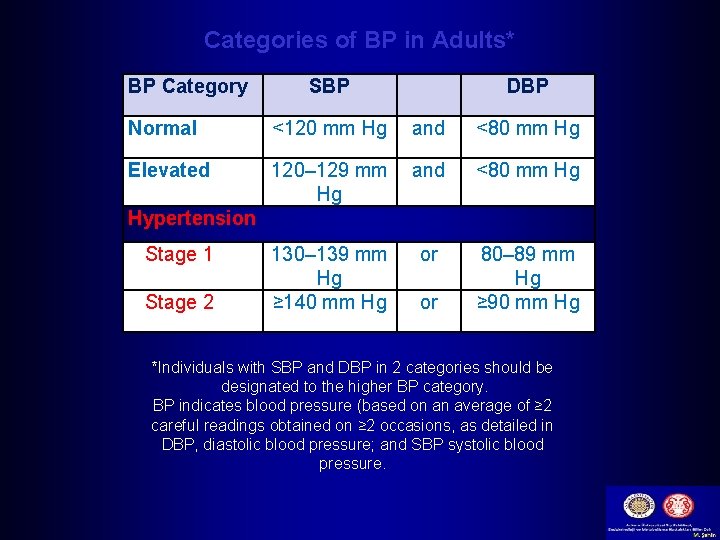
Categories of BP in Adults* BP Category SBP DBP Normal <120 mm Hg and <80 mm Hg Elevated 120– 129 mm Hg and <80 mm Hg 130– 139 mm Hg ≥ 140 mm Hg or 80– 89 mm Hg ≥ 90 mm Hg Hypertension Stage 1 Stage 2 or *Individuals with SBP and DBP in 2 categories should be designated to the higher BP category. BP indicates blood pressure (based on an average of ≥ 2 careful readings obtained on ≥ 2 occasions, as detailed in DBP, diastolic blood pressure; and SBP systolic blood pressure.
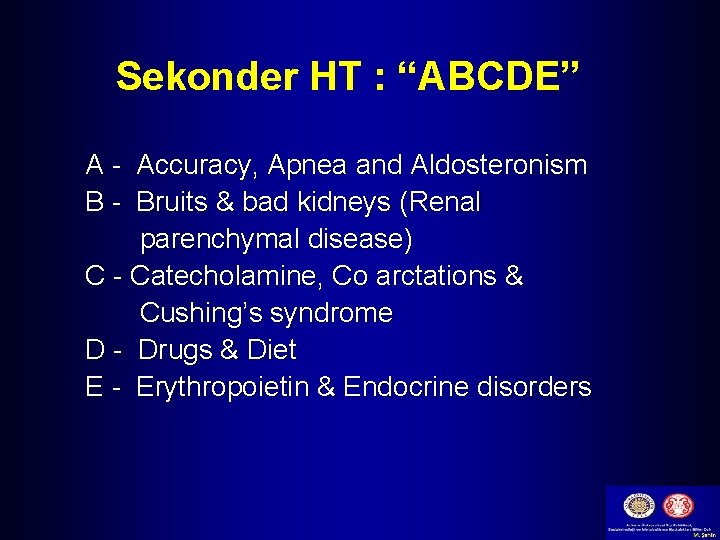
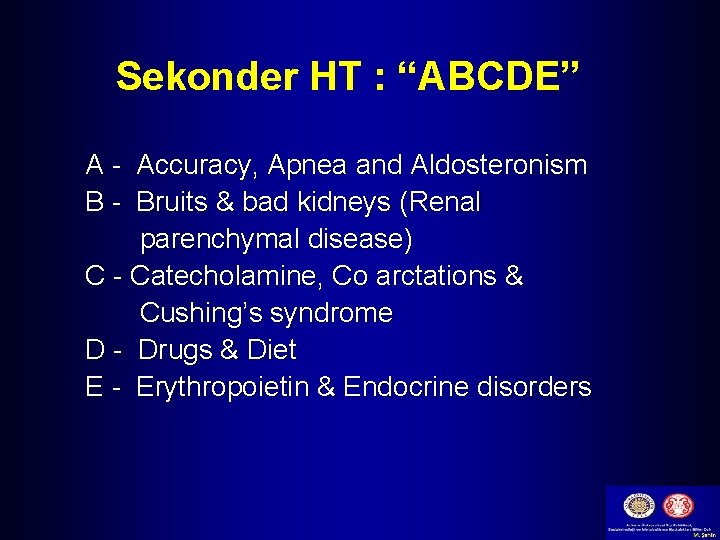
Sekonder HT : “ABCDE” A - Accuracy, Apnea and Aldosteronism B - Bruits & bad kidneys (Renal parenchymal disease) C - Catecholamine, Co arctations & Cushing’s syndrome D - Drugs & Diet E - Erythropoietin & Endocrine disorders
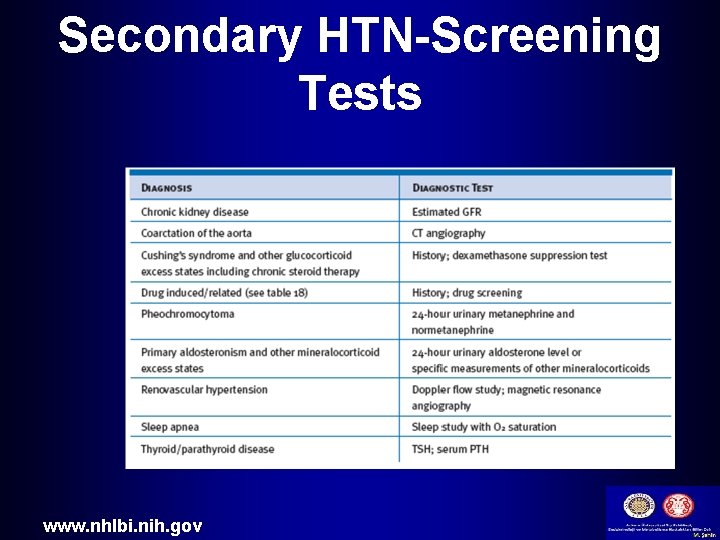
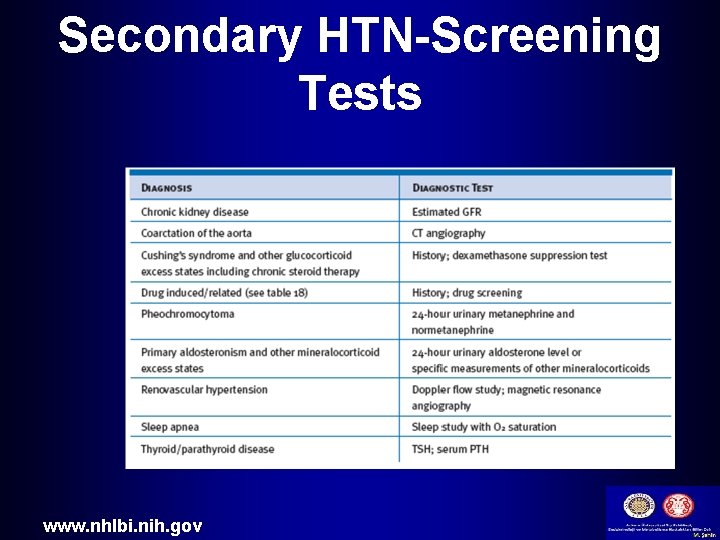
Secondary HTN-Screening Tests www. nhlbi. nih. gov
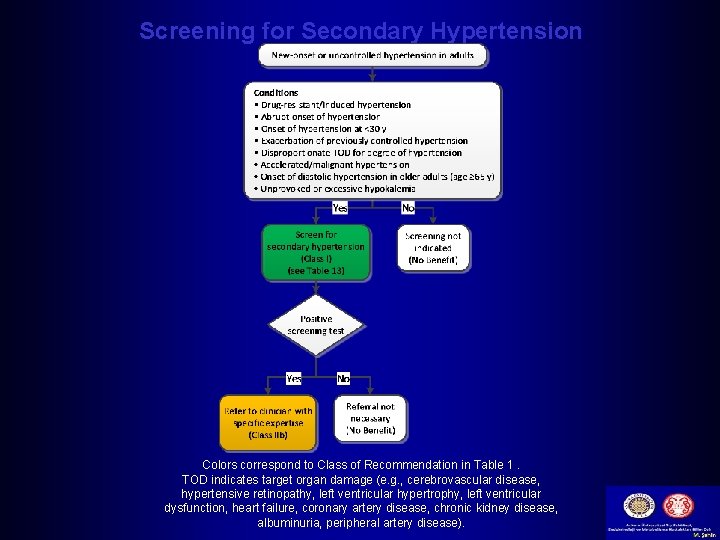
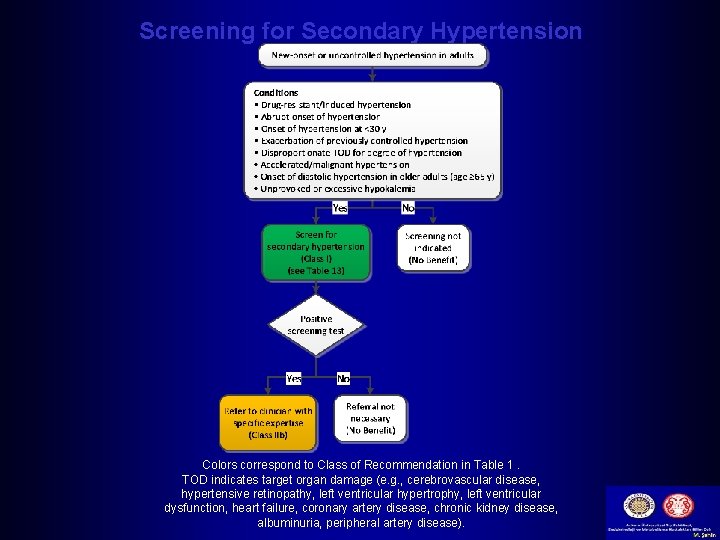
Screening for Secondary Hypertension Colors correspond to Class of Recommendation in Table 1. TOD indicates target organ damage (e. g. , cerebrovascular disease, hypertensive retinopathy, left ventricular hypertrophy, left ventricular dysfunction, heart failure, coronary artery disease, chronic kidney disease, albuminuria, peripheral artery disease).
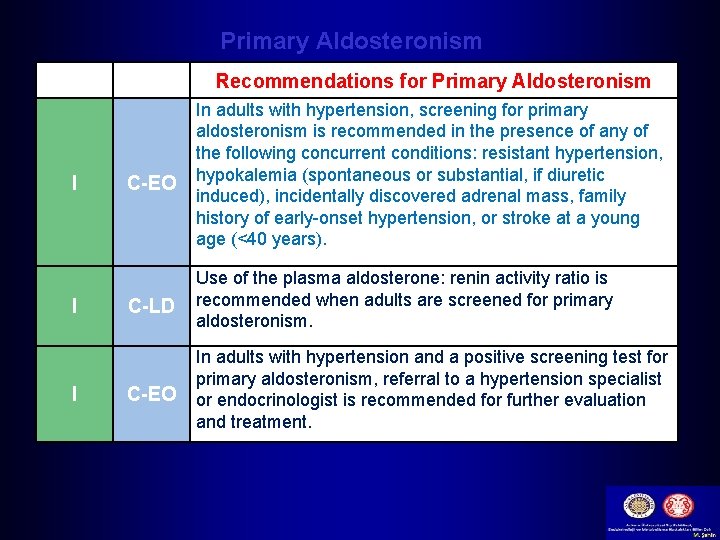
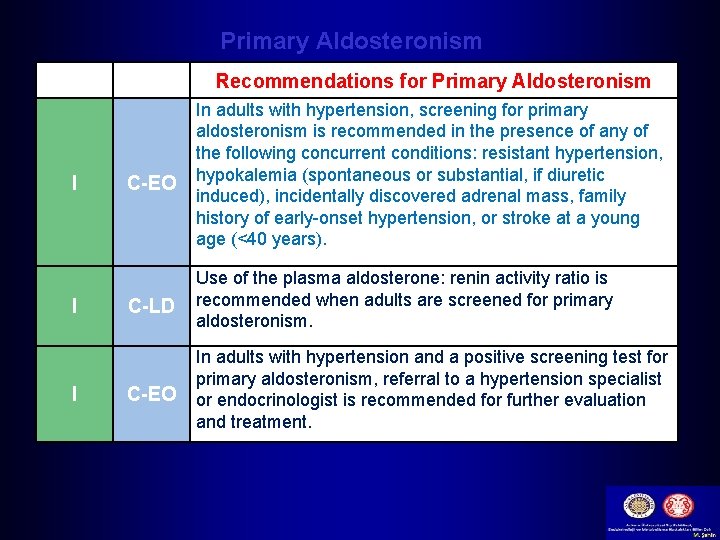
Primary Aldosteronism COR I I I LOE Recommendations for Primary Aldosteronism C-EO In adults with hypertension, screening for primary aldosteronism is recommended in the presence of any of the following concurrent conditions: resistant hypertension, hypokalemia (spontaneous or substantial, if diuretic induced), incidentally discovered adrenal mass, family history of early-onset hypertension, or stroke at a young age (<40 years). C-LD Use of the plasma aldosterone: renin activity ratio is recommended when adults are screened for primary aldosteronism. C-EO In adults with hypertension and a positive screening test for primary aldosteronism, referral to a hypertension specialist or endocrinologist is recommended for further evaluation and treatment.
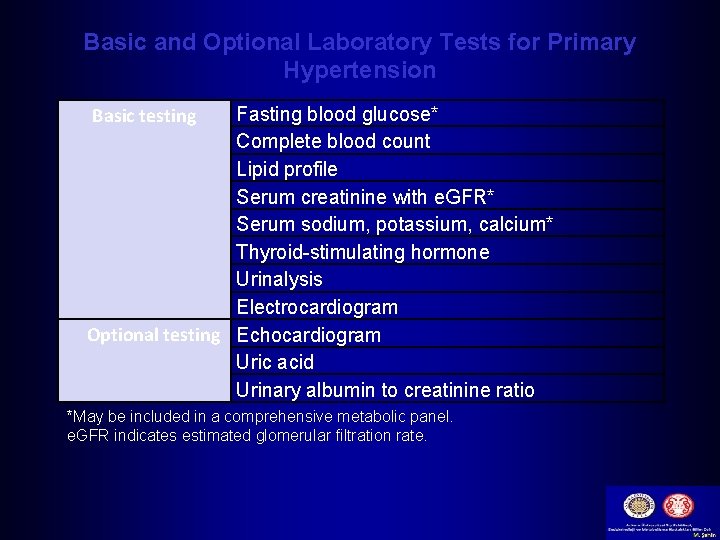
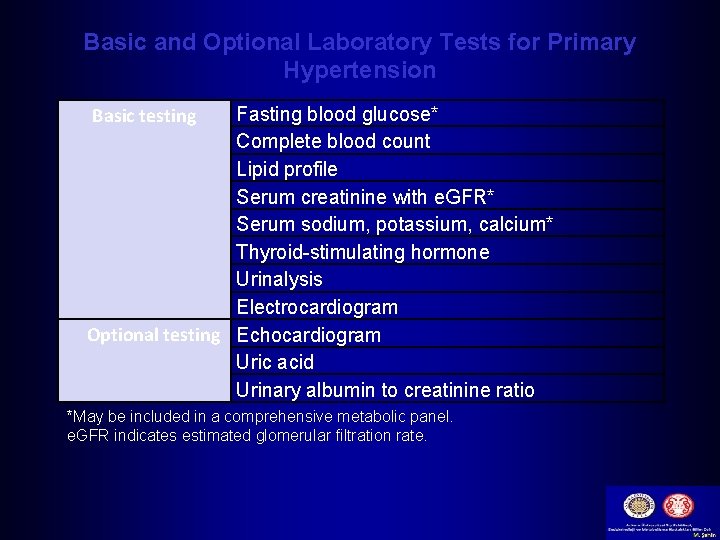
Basic and Optional Laboratory Tests for Primary Hypertension Basic testing Fasting blood glucose* Complete blood count Lipid profile Serum creatinine with e. GFR* Serum sodium, potassium, calcium* Thyroid-stimulating hormone Urinalysis Electrocardiogram Optional testing Echocardiogram Uric acid Urinary albumin to creatinine ratio *May be included in a comprehensive metabolic panel. e. GFR indicates estimated glomerular filtration rate.
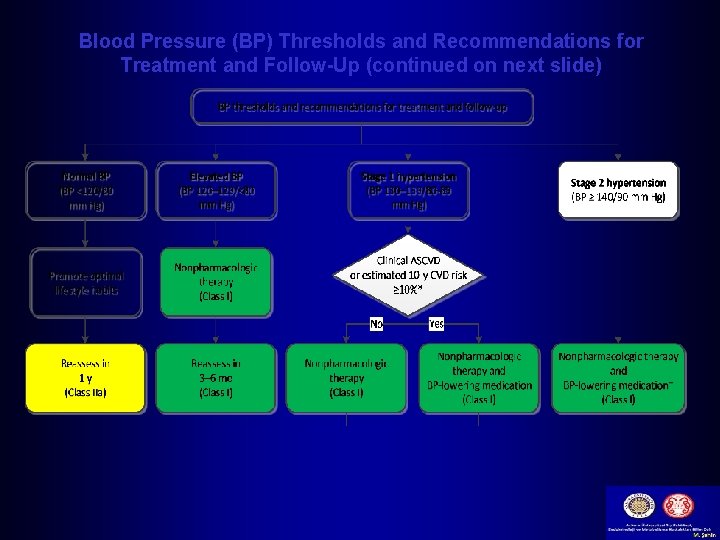
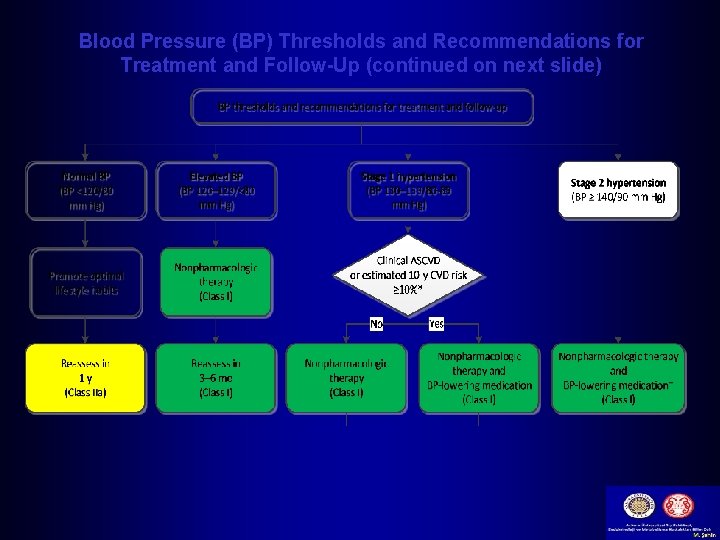
Blood Pressure (BP) Thresholds and Recommendations for Treatment and Follow-Up (continued on next slide)
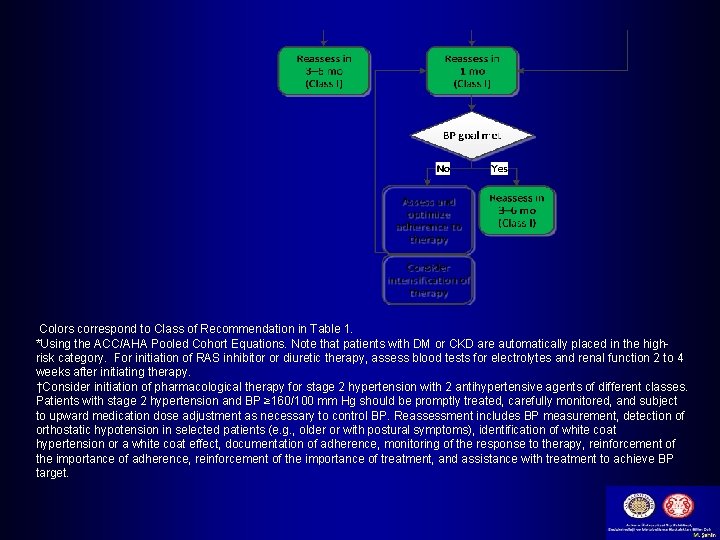
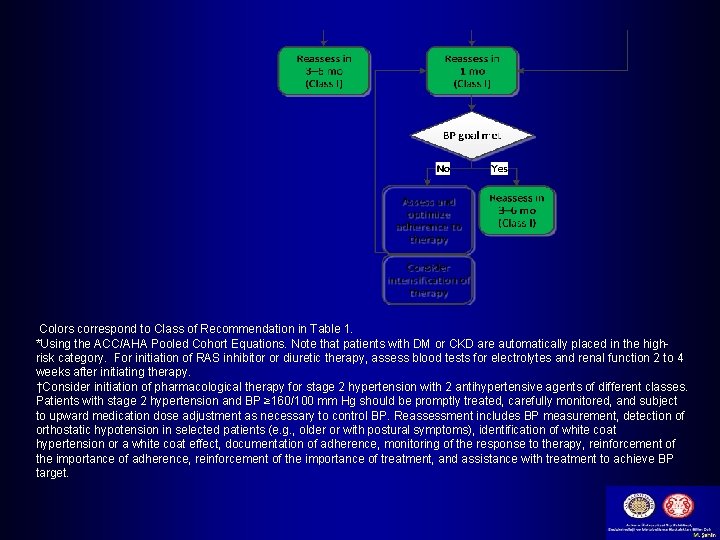
Colors correspond to Class of Recommendation in Table 1. *Using the ACC/AHA Pooled Cohort Equations. Note that patients with DM or CKD are automatically placed in the highrisk category. For initiation of RAS inhibitor or diuretic therapy, assess blood tests for electrolytes and renal function 2 to 4 weeks after initiating therapy. †Consider initiation of pharmacological therapy for stage 2 hypertension with 2 antihypertensive agents of different classes. Patients with stage 2 hypertension and BP ≥ 160/100 mm Hg should be promptly treated, carefully monitored, and subject to upward medication dose adjustment as necessary to control BP. Reassessment includes BP measurement, detection of orthostatic hypotension in selected patients (e. g. , older or with postural symptoms), identification of white coat hypertension or a white coat effect, documentation of adherence, monitoring of the response to therapy, reinforcement of the importance of adherence, reinforcement of the importance of treatment, and assistance with treatment to achieve BP target.
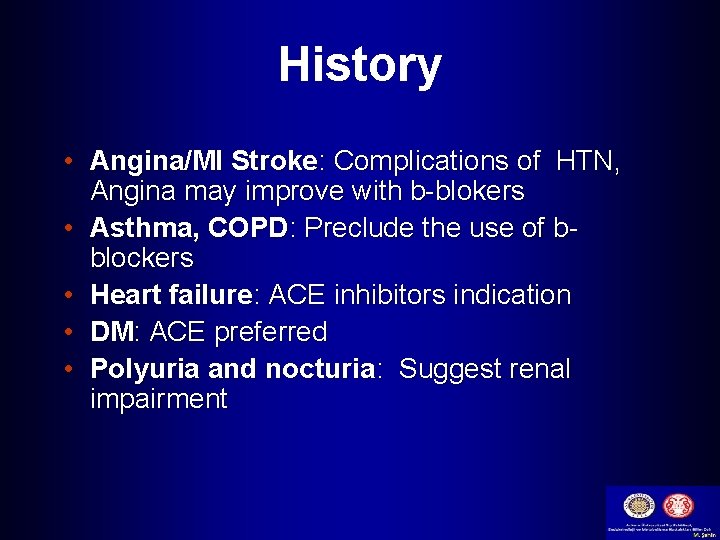
History • Angina/MI Stroke: Complications of HTN, Angina may improve with b-blokers • Asthma, COPD: Preclude the use of bblockers • Heart failure: ACE inhibitors indication • DM: ACE preferred • Polyuria and nocturia: Suggest renal impairment
History-contd. • Claudication: May be aggravated by bblockers, atheromatous RAS may be present • Gout: May be aggravated by diuretics • Use of NSAIDs: May cause or aggravate HTN • Family history of HTN: Important risk factor • Family history of premature death: May have been due to HTN
History-contd. • Family history of DM : Patient may also be Diabetic • Cigarette smoker: Aggravate HTN, independently a risk factor for CAD and stroke • High alcohol: A cause of HTN • High salt intake: Advice low salt intake
Examination • Appropriate measurement of BP in both arms • Optic fundi • Calculation of BMI ( waist circumference also may be useful) • Auscultation for carotid, abdominal, and femoral bruits • Palpation of the thyroid gland.

Examination-contd. • Thorough examination of the heart and lungs • Abdomen for enlarged kidneys, masses, and abnormal aortic pulsation • Lower extremities for edema and pulses • Neurological assessment
Routine Labs • • • EKG. Urinalysis. Blood glucose and hematocrit; serum potassium, creatinine ( or estimated GFR), and calcium. • HDL cholesterol, LDL cholesterol, and triglycerides. • Optional tests urinary albumin excretion. albumin/creatinine ratio.
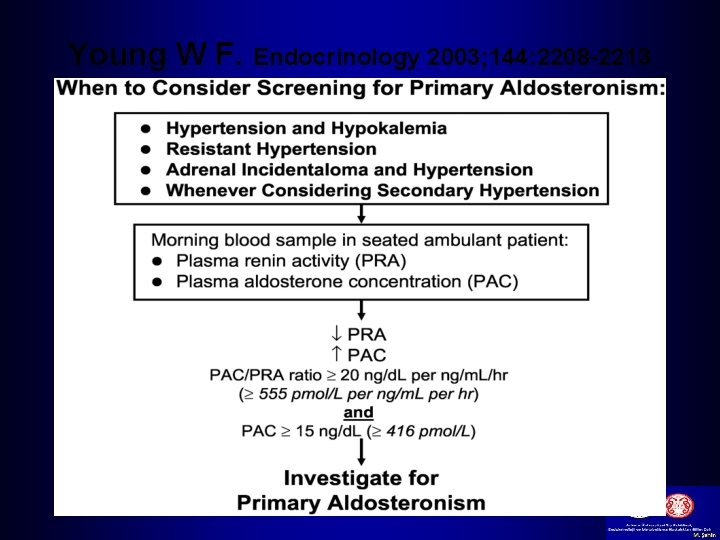
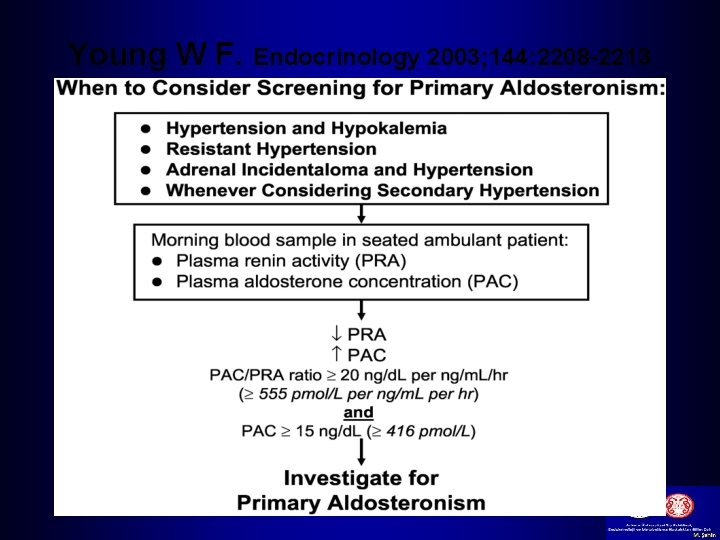
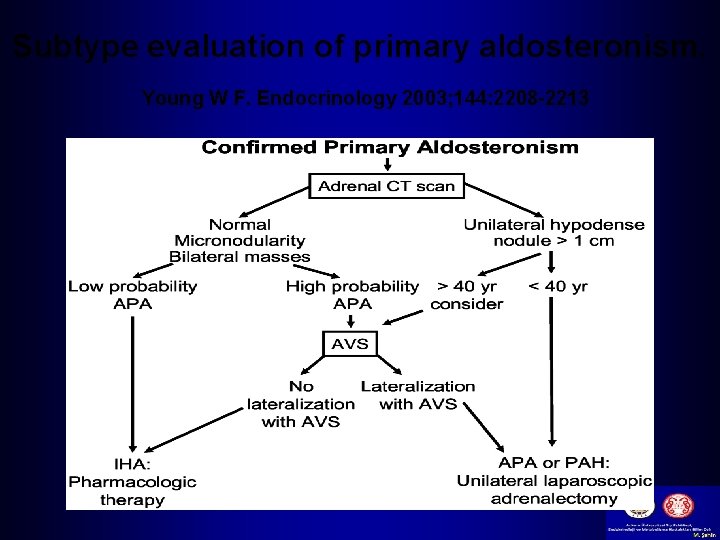
Young W F. Endocrinology 2003; 144: 2208 -2213
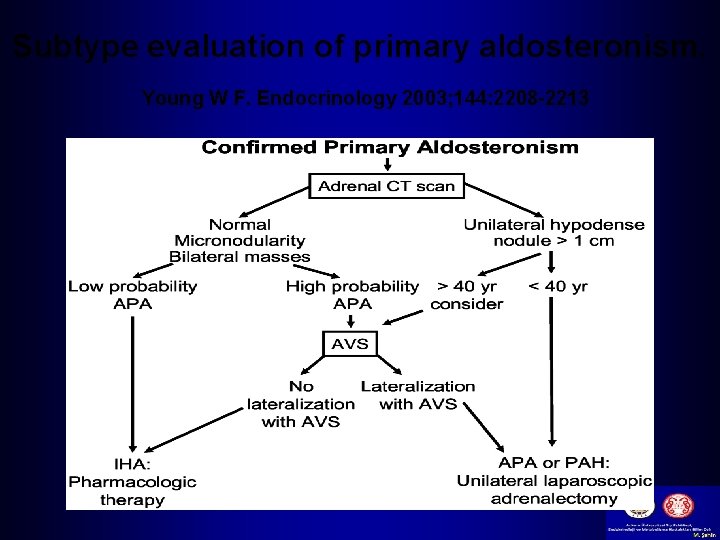
Subtype evaluation of primary aldosteronism. Young W F. Endocrinology 2003; 144: 2208 -2213
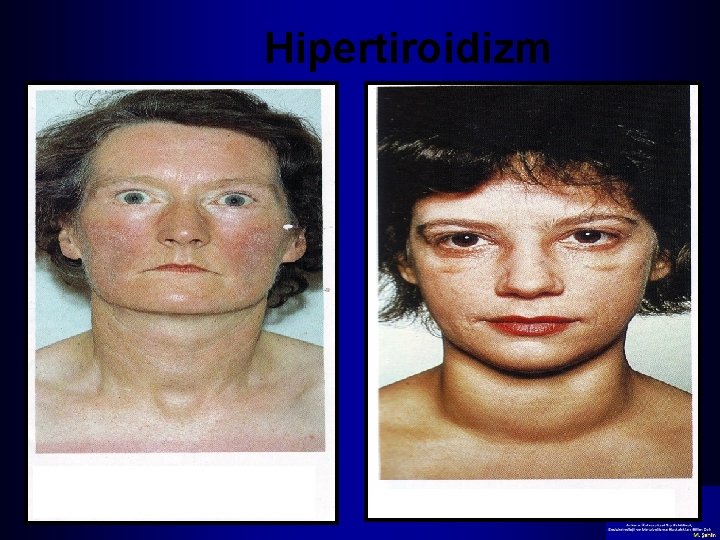
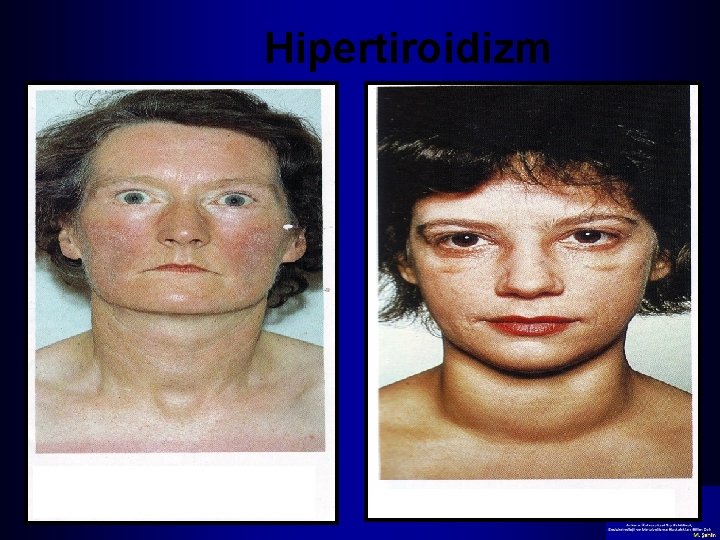
Hipertiroidizm 32
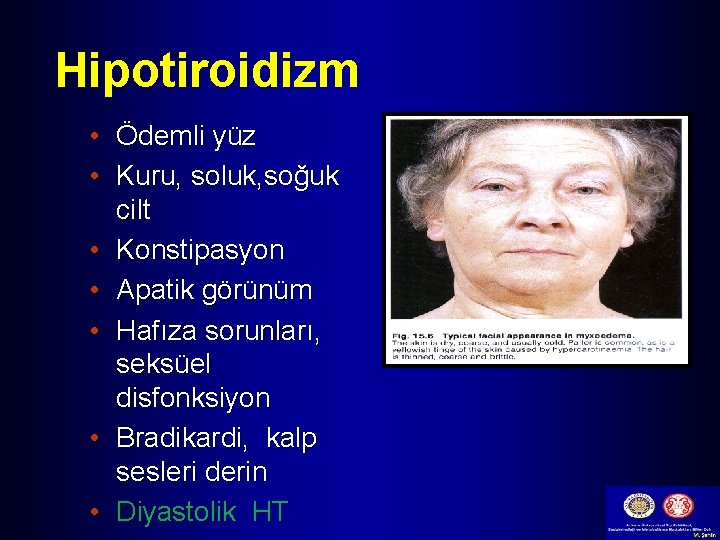
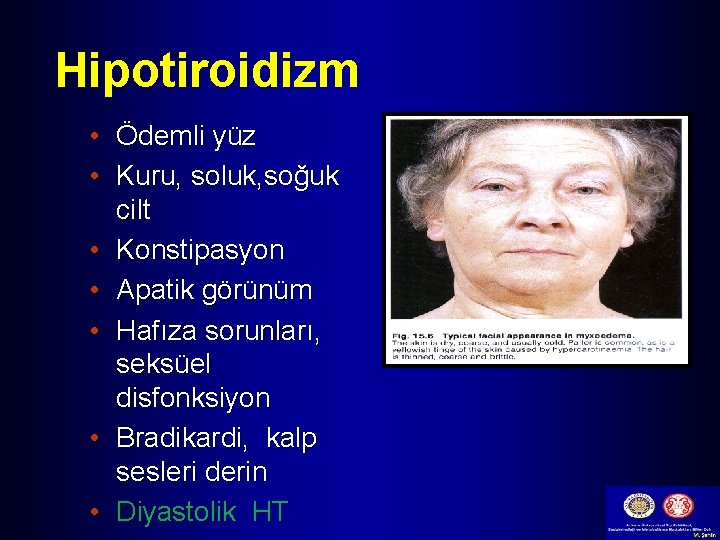
Hipotiroidizm • Ödemli yüz • Kuru, soluk, soğuk cilt • Konstipasyon • Apatik görünüm • Hafıza sorunları, seksüel disfonksiyon • Bradikardi, kalp sesleri derin • Diyastolik HT

Akromegali- Klinik şüphe 1991 2005

PLATORE; SUPRAKLAVİKULER YAĞLANMA; HİRSUTİZM AKNE; PLATORE; AYDEDE YÜZ

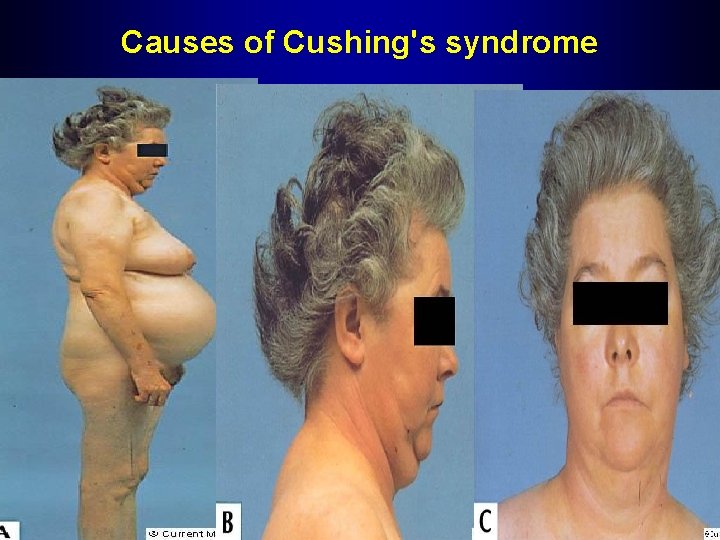
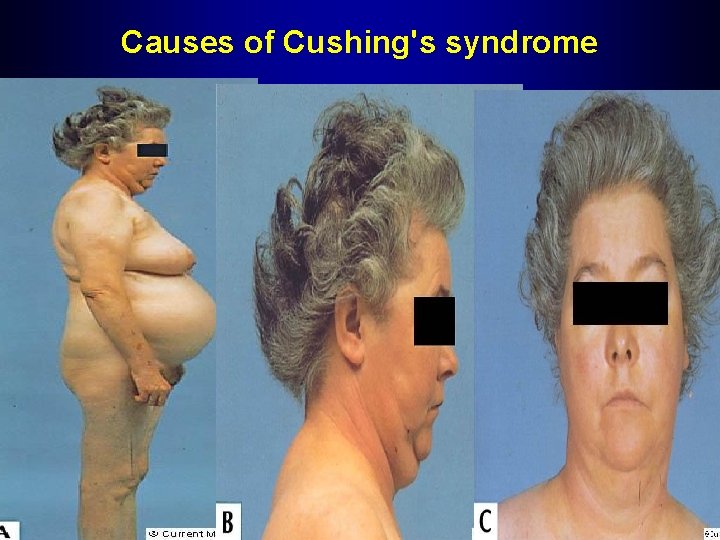
Causes of Cushing's syndrome

Abdominal striae caused by excess cortisol production
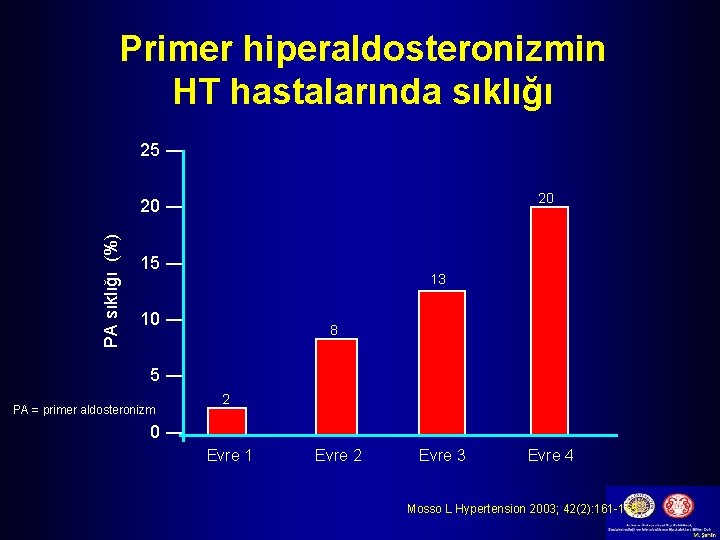
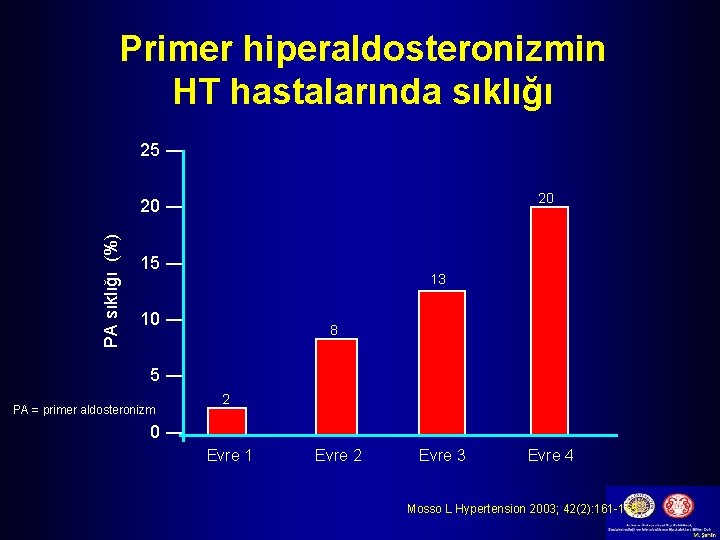
Primer hiperaldosteronizmin HT hastalarında sıklığı 25 ― 20 PA sıklığı (%) 20 ― 15 ― 13 10 ― 8 5― PA = primer aldosteronizm 2 0― Evre 1 Evre 2 Evre 3 Evre 4 Mosso L Hypertension 2003; 42(2): 161 -165













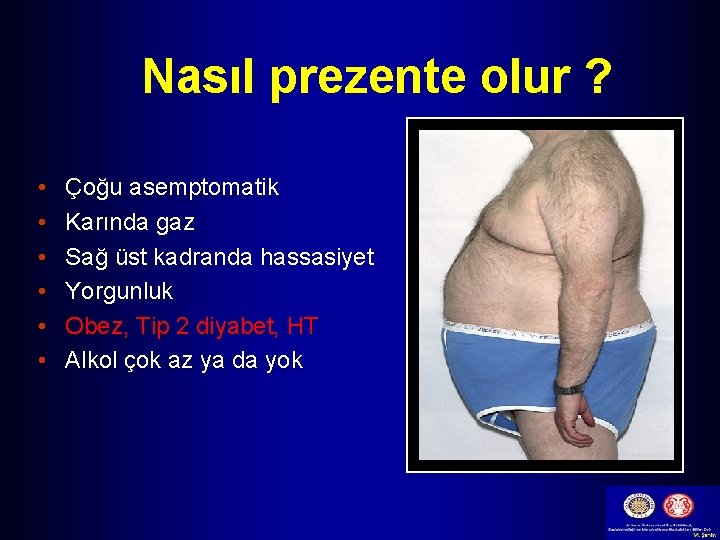
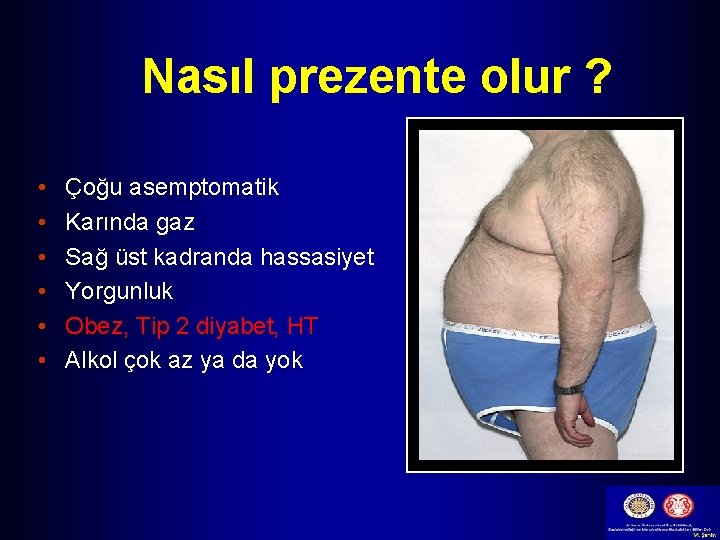
Nasıl prezente olur ? • • • Çoğu asemptomatik Karında gaz Sağ üst kadranda hassasiyet Yorgunluk Obez, Tip 2 diyabet, HT Alkol çok az ya da yok


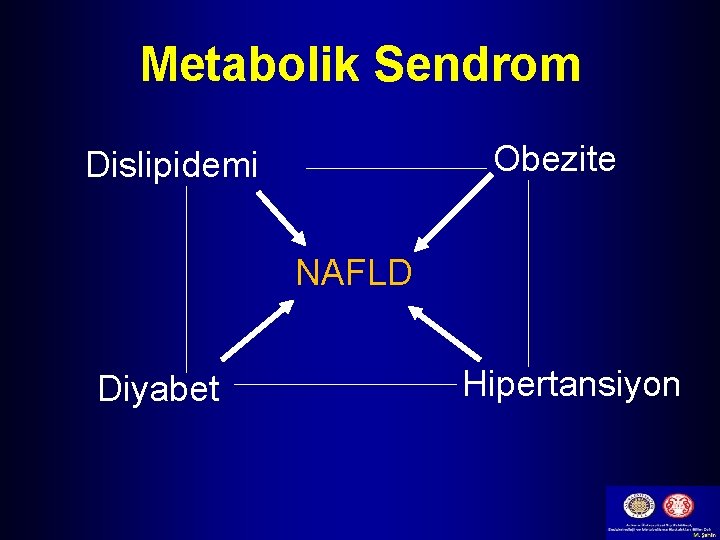
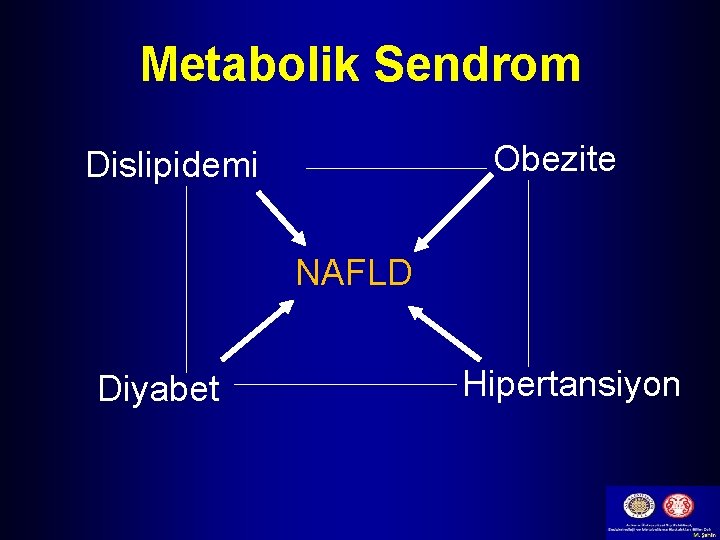
Metabolik Sendrom Obezite Dislipidemi NAFLD Diyabet Hipertansiyon
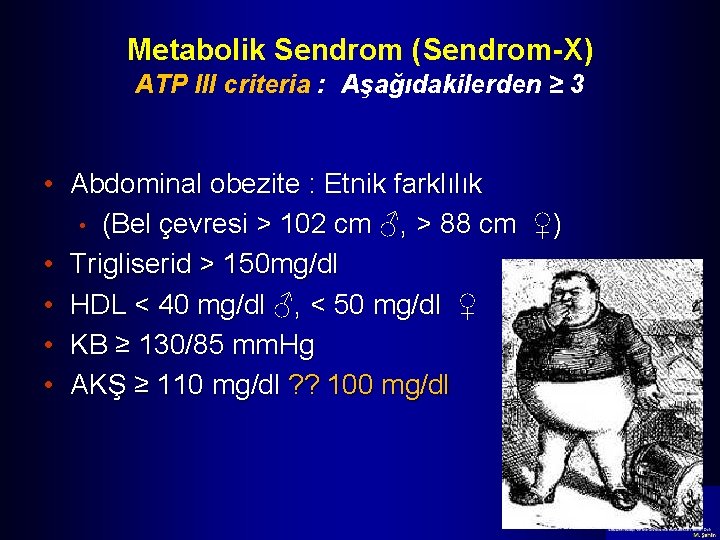
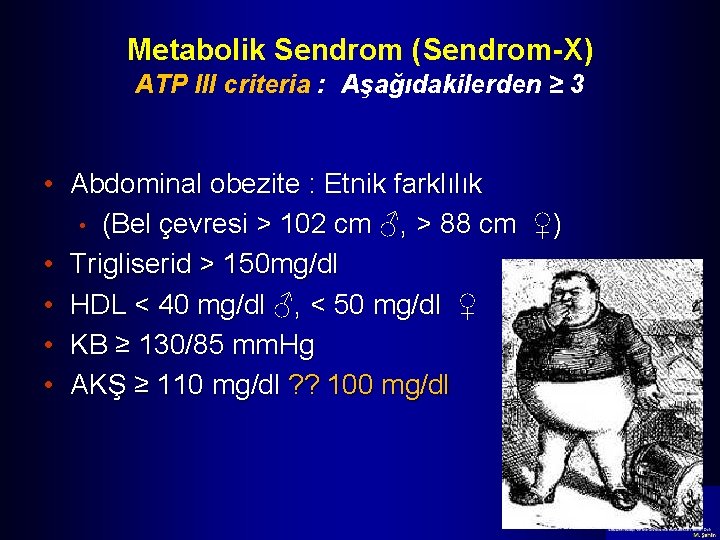
Metabolik Sendrom (Sendrom-X) ATP III criteria : Aşağıdakilerden ≥ 3 • Abdominal obezite : Etnik farklılık • (Bel çevresi > 102 cm ♂, > 88 cm ♀) • Trigliserid > 150 mg/dl • HDL < 40 mg/dl ♂, < 50 mg/dl ♀ • KB ≥ 130/85 mm. Hg • AKŞ ≥ 110 mg/dl ? ? 100 mg/dl












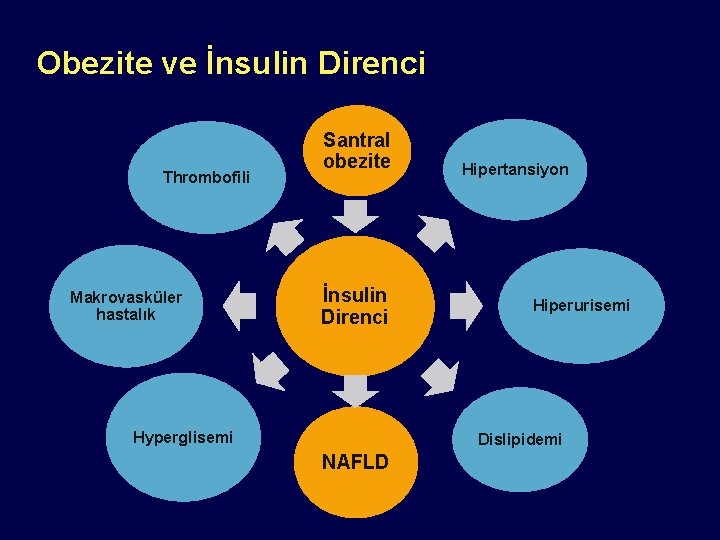
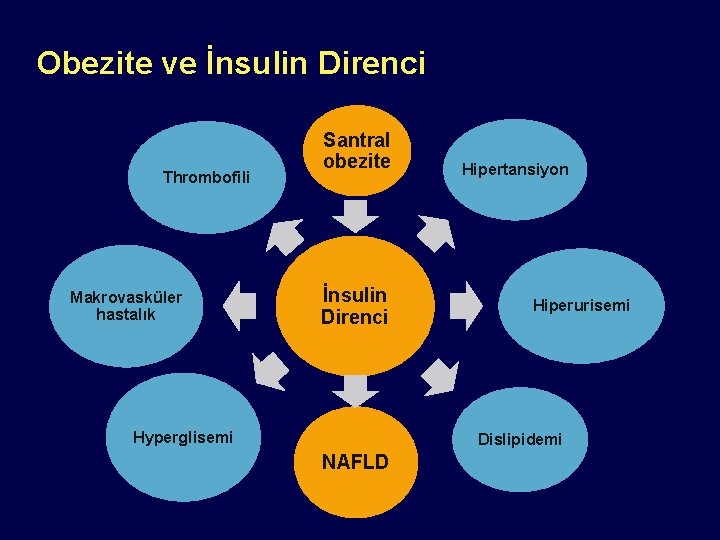
Obezite ve İnsulin Direnci Thrombofili Makrovasküler hastalık Santral obezite İnsulin Direnci Hyperglisemi Hipertansiyon Hiperurisemi Dislipidemi NAFLD

Teşekkürler
 Mustafa şahin endokrinoloji
Mustafa şahin endokrinoloji Prof dr mustafa şahin endokrin
Prof dr mustafa şahin endokrin Ankara üniversitesi
Ankara üniversitesi Doç dr volkan atmış
Doç dr volkan atmış Ankara üniversitesi bmyo
Ankara üniversitesi bmyo Yeniden sevedebilirim
Yeniden sevedebilirim Dr tamer kala
Dr tamer kala Ankara üniversitesi harf notu
Ankara üniversitesi harf notu Dr erdem ercan
Dr erdem ercan Hatay mustafa kemal üni yatay geçiş
Hatay mustafa kemal üni yatay geçiş Duygunur şahin arslan
Duygunur şahin arslan Ebubekir şahin
Ebubekir şahin Ankara niversitesi
Ankara niversitesi çirmen savaşı
çirmen savaşı Ankara istasyon caddesi
Ankara istasyon caddesi Ankara niversitesi
Ankara niversitesi Ankara university
Ankara university T.c.devlet protokol sıralaması
T.c.devlet protokol sıralaması Ted koleji ib programı
Ted koleji ib programı Ankara ymm odası
Ankara ymm odası Ankara paratoner raporu
Ankara paratoner raporu Sentroiller
Sentroiller Ymm mustafa soydemir
Ymm mustafa soydemir Kosgeb ankara ostim müdürlüğü
Kosgeb ankara ostim müdürlüğü Ankara population
Ankara population Ankara niversitesi
Ankara niversitesi Ankara market derne
Ankara market derne Eee 322
Eee 322 Ankara scene online
Ankara scene online Ankara yabdil
Ankara yabdil Rics türkiye
Rics türkiye Ankara kordon kanı
Ankara kordon kanı Dogm meb gov tr anket
Dogm meb gov tr anket Ankara batı adliyesi yargı çevresi
Ankara batı adliyesi yargı çevresi Ankara golf sahası
Ankara golf sahası Itola nedir
Itola nedir Gate elektronik ankara
Gate elektronik ankara Intratübüler germ hücre neoplazisi
Intratübüler germ hücre neoplazisi Ankara baro sdd
Ankara baro sdd Ankara niversitesi
Ankara niversitesi Ankara niversitesi
Ankara niversitesi Panik atak belirtileri
Panik atak belirtileri Ankara kordon kanı
Ankara kordon kanı Ankara ymm odası
Ankara ymm odası Mezenkimal kök hücre
Mezenkimal kök hücre Dcld vs cld
Dcld vs cld Presinusoidal portal hypertension
Presinusoidal portal hypertension Hypertension
Hypertension Pulmonary hypertension
Pulmonary hypertension Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Hypertension
Hypertension Hypertensive encephalopathy
Hypertensive encephalopathy Pathophysiology of pulmonary hypertension
Pathophysiology of pulmonary hypertension Calcium channel blockers examples
Calcium channel blockers examples Missed some points on the visual field test for dvla'
Missed some points on the visual field test for dvla' Isolated systolic hypertension
Isolated systolic hypertension Modifiable risk factors for hypertension
Modifiable risk factors for hypertension Masked hypertension
Masked hypertension Health coaches for hypertension control
Health coaches for hypertension control Hypertension
Hypertension Nursing management of portal hypertension
Nursing management of portal hypertension Hypertensive crisis
Hypertensive crisis Pulmonary hypertension
Pulmonary hypertension Dash diet
Dash diet Pulmonary hypertension definition
Pulmonary hypertension definition Malignant hypertension ppt
Malignant hypertension ppt Hypertension vs hypotension
Hypertension vs hypotension Jnc 8 classification of hypertension
Jnc 8 classification of hypertension Demadex
Demadex Sachin gupta md
Sachin gupta md Jnc 7 hypertension
Jnc 7 hypertension Case scenario for hypertension
Case scenario for hypertension What is a good pico question
What is a good pico question