HIV AIDS Claire OGorman Claire Pettipas Michle WeirCotnoir




![Diagnosis of HIV infection n EIA (enzyme immunoassay) [formerly ELISA (enzyme-linked immunosorbent assay)] identifies Diagnosis of HIV infection n EIA (enzyme immunoassay) [formerly ELISA (enzyme-linked immunosorbent assay)] identifies](https://slidetodoc.com/presentation_image_h/1a24ba8cc03b1f8a00c2f84c564c71f8/image-29.jpg)

- Slides: 82
HIV & AIDS Claire O’Gorman Claire Pettipas Michèle Weir-Cotnoir
Objectives n n n Describe the pathophysiology of HIV the consequential infections that occur Understand the Epidemiology of the disease and the effects of HIV/AIDS on a society, including Canada Understand the risk factors associated with contracting HIV and how to prevent infection Describe how to protect yourself as a HCP from infectious blood borne diseases Understand the nursing management of this terminal illness and the conditions associated with it.
What Is HIV? H – Human I – Immunodeficiency V – Virus
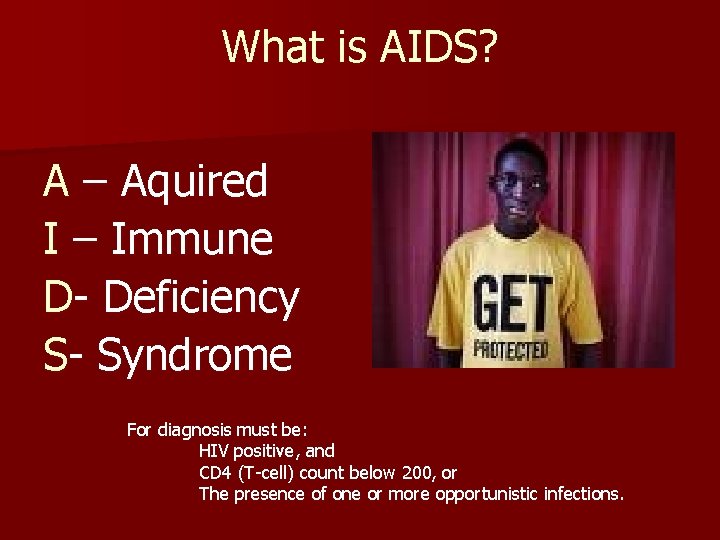
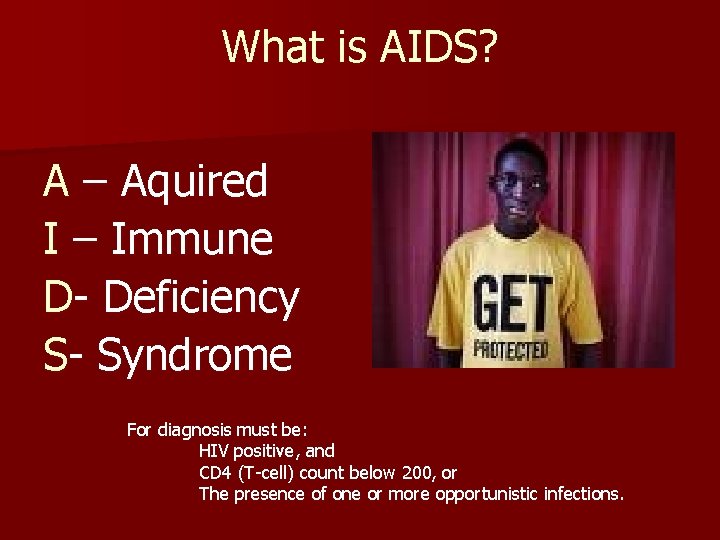
What is AIDS? A – Aquired I – Immune D- Deficiency S- Syndrome For diagnosis must be: HIV positive, and CD 4 (T-cell) count below 200, or The presence of one or more opportunistic infections.
Class Activity STAND UP!
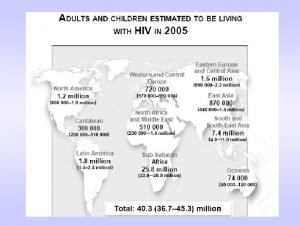
Global Epidemiology n 39. 5 2006 million people living with HIV/AIDS in – 4. 3 million newly infected with HIV (more than half are younger than 25) – 2. 9 million people died from AIDS n More than 25 million people have died from AIDS since 1981 n Africa has over 12 million AIDS orphans
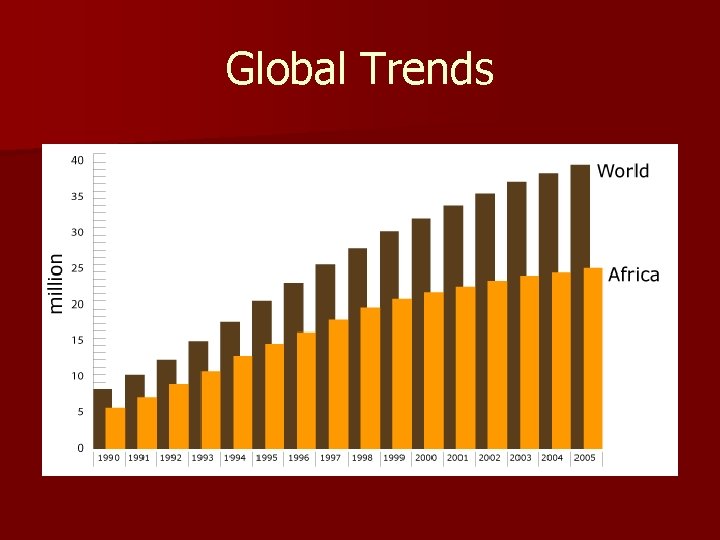
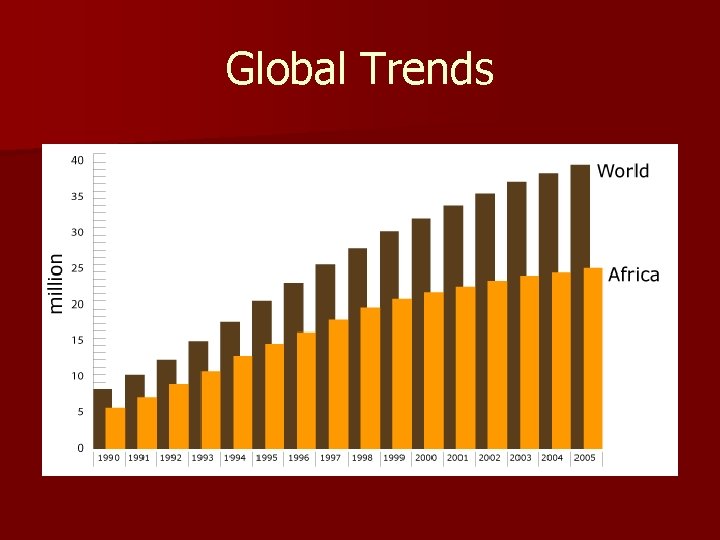
Global Trends

Xtending Hope n What can you do on campus to address the global AIDS epidemic?
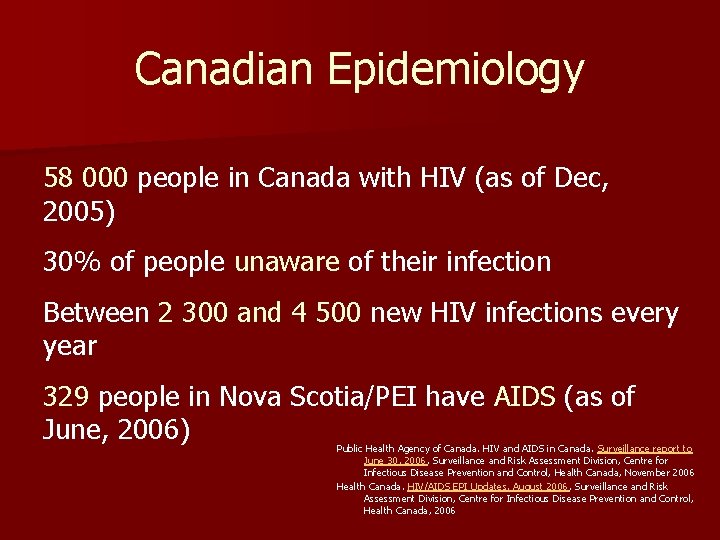
Canadian Epidemiology 58 000 people in Canada with HIV (as of Dec, 2005) 30% of people unaware of their infection Between 2 300 and 4 500 new HIV infections every year 329 people in Nova Scotia/PEI have AIDS (as of June, 2006) Public Health Agency of Canada. HIV and AIDS in Canada. Surveillance report to June 30, 2006. Surveillance and Risk Assessment Division, Centre for Infectious Disease Prevention and Control, Health Canada, November 2006 Health Canada. HIV/AIDS EPI Updates, August 2006, Surveillance and Risk Assessment Division, Centre for Infectious Disease Prevention and Control, Health Canada, 2006
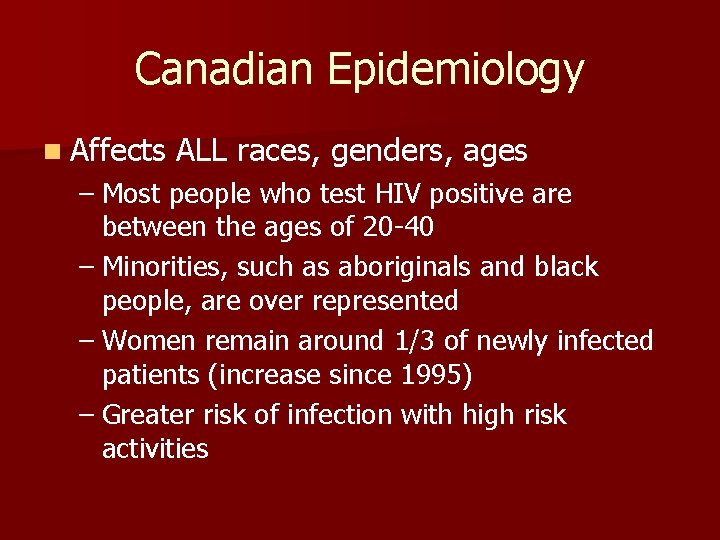
Canadian Epidemiology n Affects ALL races, genders, ages – Most people who test HIV positive are between the ages of 20 -40 – Minorities, such as aboriginals and black people, are over represented – Women remain around 1/3 of newly infected patients (increase since 1995) – Greater risk of infection with high risk activities
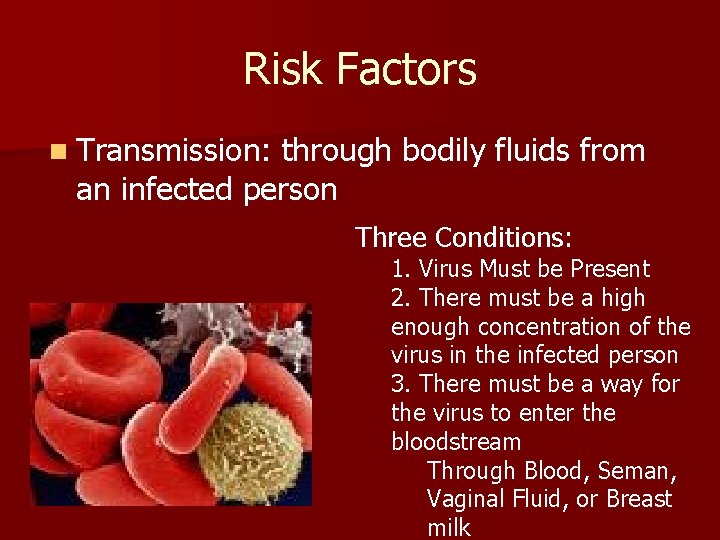
Risk Factors n Transmission: through bodily fluids from an infected person Three Conditions: 1. Virus Must be Present 2. There must be a high enough concentration of the virus in the infected person 3. There must be a way for the virus to enter the bloodstream Through Blood, Seman, Vaginal Fluid, or Breast milk

Transmission Possible Sources of Transmission: – Blood products/ transfusions § Before 1985 – Mother to child § Pregnancy, birth, and breastfeeding – Contaminated needles § Injection drug use, tattoos, peircings, acupunture – Sexual contact § § Unprotected sex Unwashed sexual devices Greater risk with other STI due to breaks in skin Greater risk with increased number of partners

Risk Factors n NOT transmitted through – – – Casual contact (shaking hands) Hugging Kissing Sweat Tears Donating Blood Swimming Pools Toilet seats Telephones Sharing bed linens, towels, eating utensils, or food Insect bites
Societal Risk Factors Many determinants of health! n These, in turn, become consequences of an epidemic n Societal factors that contribute to the epidemic: n – – – People on the move People in conflict Poverty Stigma and Denial Cultural factors § Role of Women
Prevention n Prevention is the most realistic strategy – Vaccine or cure unlikely anytime soon Prevention is done by decreasing both societal and individual risk factors n Barriers to prevention include: n – Political instability – Lack of resources – Existence of other endemic health problems (ie: malaria and childhood diseases) – Inefficiency – Apathy and silence – Misconceptions and lack of knowledge

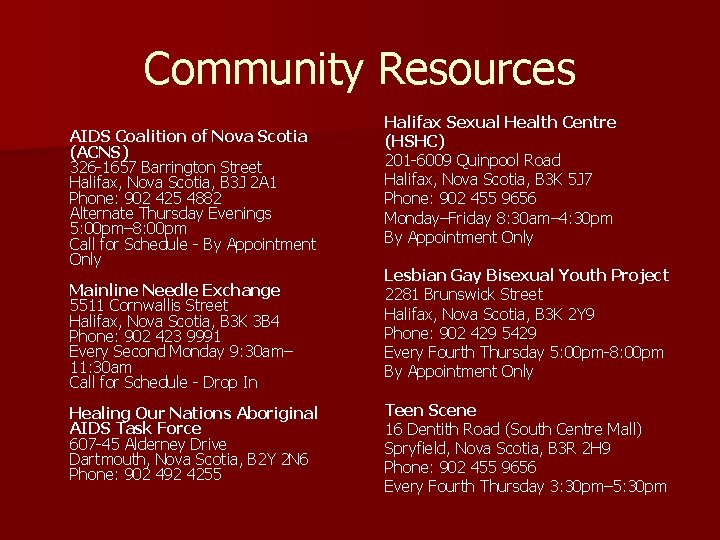
Decreasing Individual Risk Factors Nurses are responsible for educating their clients about how to protect themselves from HIV/AIDS! n Literacy appropriate teaching n Use multiple teaching methods – Provide visual/auditory/written material for different learning styles – Provide for kinetic learners, too, such as having the client demonstrate how put on a condom n Direct clients to community resources – Where they can be tested for HIV/AIDS and other STI’s – Support groups
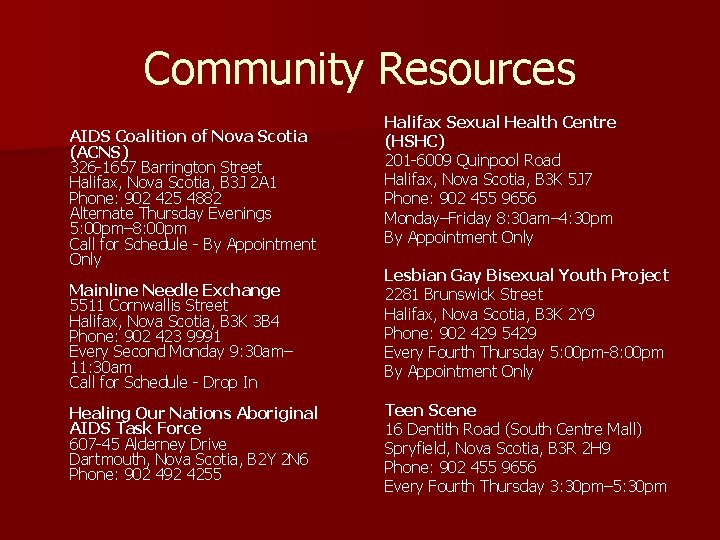
Community Resources AIDS Coalition of Nova Scotia (ACNS) 326 -1657 Barrington Street Halifax, Nova Scotia, B 3 J 2 A 1 Phone: 902 425 4882 Alternate Thursday Evenings 5: 00 pm– 8: 00 pm Call for Schedule - By Appointment Only Mainline Needle Exchange 5511 Cornwallis Street Halifax, Nova Scotia, B 3 K 3 B 4 Phone: 902 423 9991 Every Second Monday 9: 30 am– 11: 30 am Call for Schedule - Drop In Healing Our Nations Aboriginal AIDS Task Force 607 -45 Alderney Drive Dartmouth, Nova Scotia, B 2 Y 2 N 6 Phone: 902 492 4255 Halifax Sexual Health Centre (HSHC) 201 -6009 Quinpool Road Halifax, Nova Scotia, B 3 K 5 J 7 Phone: 902 455 9656 Monday–Friday 8: 30 am– 4: 30 pm By Appointment Only Lesbian Gay Bisexual Youth Project 2281 Brunswick Street Halifax, Nova Scotia, B 3 K 2 Y 9 Phone: 902 429 5429 Every Fourth Thursday 5: 00 pm-8: 00 pm By Appointment Only Teen Scene 16 Dentith Road (South Centre Mall) Spryfield, Nova Scotia, B 3 R 2 H 9 Phone: 902 455 9656 Every Fourth Thursday 3: 30 pm– 5: 30 pm
Prevention: Practice SAFER sex n Nurses must be comfortable discussing their clients’ sexual activites – Assess: number of partners, protection being used, and whether it is being used properly – Ask everyone! Don’t assume! – Educate: know STI status of sexual partners, HIV/AIDS and other STI testing, use of latex condoms, dental dams, latex gloves, water-based lubricants
Prevention: Clean Needles Risk reduction school of thought n Nurse can : n – Direct client to addiction services – Direct client to needle exchange program if quitting is not an option at this time – Alcohol kills HIV – Educate! Sharing needles with friends is just as risky as sharing with strangers
Prevention: Screening Many STI’s are tested with gyne exams, but HIV requires a blood test n HIV antibody test n
Prevention: Education n Many myths and misconceptions ie: – HIV doesn’t exist within this community – HIV only affects sex-trade workers, homosexuals and injection drug users – If you get HIV you will show symptoms – Having sex with a virgin will cure you of HIV n Nurses facts! play a large role in providing the
Prevention: Policy n Society contributes to HIV transmission! – Empowering women – Promoting Justice – Addressing Poverty – Providing Education – Addressing Stigma
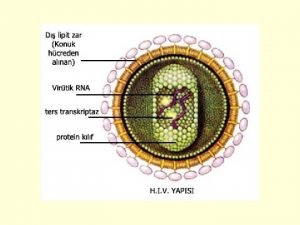
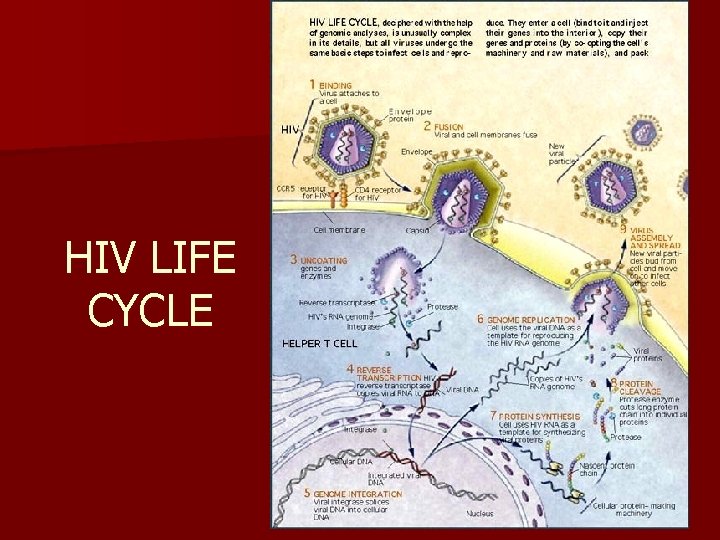
What exactly is HIV? n n n Human Immunodeficiency Virus- a retrovirus belonging to the family of lentiviruses. Uses their RNA and host DNA to make viral DNA Uses CD 4+ cell to replicate itself and destroying CD 4+ Two types: HIV-1 + HIV-2 Leads to Acquired Immunodeficiency Syndrome
HIV n 2 types: HIV-1 and HIV-2 n Subtypes of HIV-1: A, B, C, D, E, F, G, H, O. (No subtypes of HIV-2) n HIV-1 subtype C makes up for more than 50% of all new HIV infections worldwide. n HIV-2 progresses slower n HIV-2 makes up the majority of cases of HIV infection in Africa
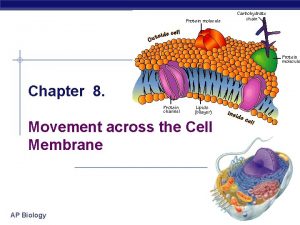
Pathophysiology of HIV/AIDS
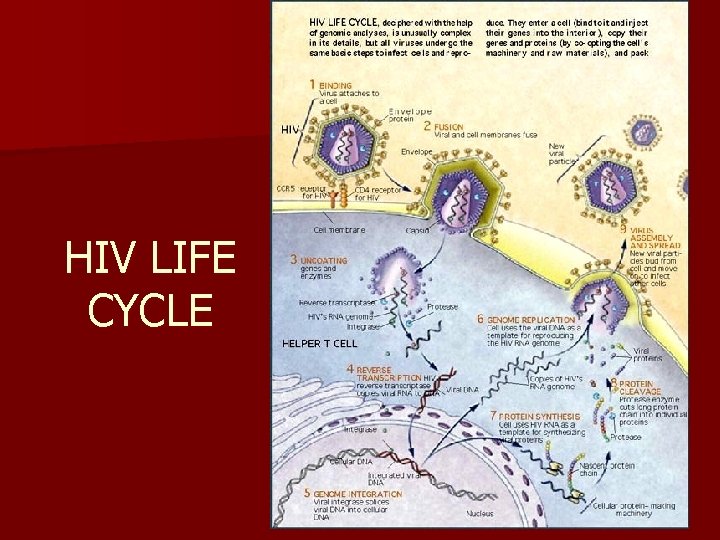
HIV LIFE CYCLE
![Diagnosis of HIV infection n EIA enzyme immunoassay formerly ELISA enzymelinked immunosorbent assay identifies Diagnosis of HIV infection n EIA (enzyme immunoassay) [formerly ELISA (enzyme-linked immunosorbent assay)] identifies](https://slidetodoc.com/presentation_image_h/1a24ba8cc03b1f8a00c2f84c564c71f8/image-29.jpg)
Diagnosis of HIV infection n EIA (enzyme immunoassay) [formerly ELISA (enzyme-linked immunosorbent assay)] identifies antibodies that are specifically directed against HIV. n Western blot assay: used to confirm seropositivity when the EIA is positive n Seropositivity: when blood or saliva contains HIV antibodies
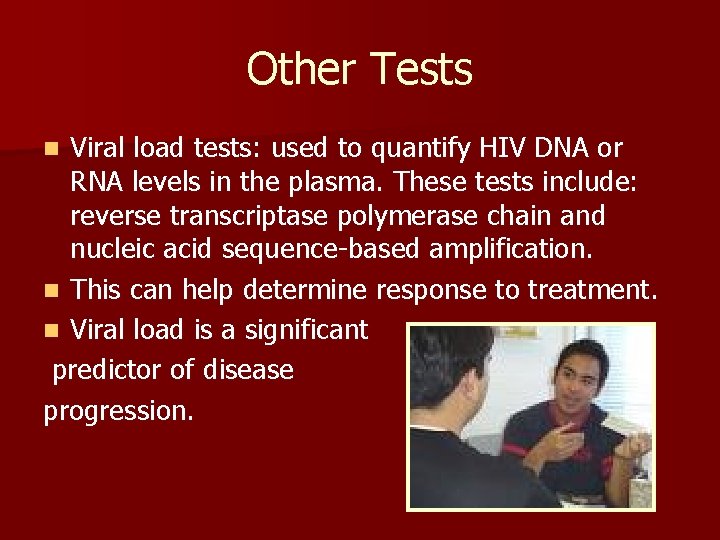
Other Tests Viral load tests: used to quantify HIV DNA or RNA levels in the plasma. These tests include: reverse transcriptase polymerase chain and nucleic acid sequence-based amplification. n This can help determine response to treatment. n Viral load is a significant predictor of disease progression. n
Home Testing Kits Home testing kits are available, but are of concern to HCP. n Why? n The lack of counselling, as well as the possibility of inaccurate results. n
S&S of HIV infection n Often, there are no S&S in the early stages of HIV infection n Why? n The CD 4 lymphocytes are still numerous enough to fight off infections
S&S of HIV infection n There may be slight flu-like symptoms 2 -6 weeks after initial infection. Other S&S (generally advanced infection): Lymphadenopathy (often the first sign) profuse night sweats, rapid weight loss, recurrent fever, chronic diarrhea, unexplained fatigue, persistent headaches (http: //www. mayoclinic. com/health/hivaids/DS 00005/DSECTION=2) n
Stages of HIV disease Based on “clinical history, physical examination, laboratory evidence of immune dysfunction, signs and symptoms, and infections and malignancies” (Smeltzer & Bare, 2004, 1559) n 3 categories: A, B, C n
Clinical Category A n n n This category is asymptomatic. The virus reaches a “set point” level after about 6 months. The “set point” generally determines rate of disease progression. In general, 8 -10 years can pass before HIVrelated complications occur. Why asymptomatic? CD 4 levels are high enough to fight off other pathogens (>500 CD 4+ Tlymphocytes/mm^3)
Clinical Category B n CD 4 cell level starts dropping (200 -499 CD 4+ T-lymphocytes/mm^3). n This category consists of conditions that are not covered under category C. The conditions must: – Be due to HIV infection – Require management that is complicated by HIV infection
Clinical Category B n Some of the conditions under this category include: – Candidiasis (oropharyngeal or vulvovaginal) – Cervical carcinoma in situ – Fever (38. 5 C), or diarrhea > 1 month duration – Herpes zoster (shingles) – Pelvic inflammatory disease – Peripheral neuropathy
Clinical Category C n When CD 4 T-cell levels drop below 200 CD 4+ T-lymphocytes/mm^3, the client is said to have AIDS. Below 100, the immune system is significantly impaired. n Once a client is classified as having category C infection, s/he remains in this category.
Clinical Category C n Some conditions in this category include: – Candidiasis (bronchi, trachea, lungs, or esophagus) – Cervical cancer, invasive – HIV-related encephalopathy – Kaposi’s sarcoma – Pneumocystis carinii pneumonia – Toxoplasmosis of brain – Wasting syndrome due to HIV
Treatment of HIV Antiretroviral treatments Compliance may be decreased by the side effects of the drugs, or by clients deficiency of knowledge about the treatment. n In developing and transitional countries, 7. 1 million people are in immediate need of lifesaving AIDS drugs; of these, only 2. 015 million (28%) are receiving the drugs. n n
Nucleoside Reverse Transcriptase Inhibitors (NRTI’s) n These were the first antiretrovirals approved by the European and American regulatory agencies. n Becomes part of the viral DNA, stopping the building process. n These are the cornerstone for HIV therapy.
Side Effects of NRTI’s Some possible adverse effects of this class of drugs: Peripheral neuropathy, pancreatitis, lactic acidosis, bone marrow suppression, neutropenia, anemia, arthralgia, myopathy, kidney dysfunction, hepatomegaly, liver failure, hypersensitivity, abdominal pain, oral ulcers, irritability, anxiety. (Smeltzer & Bare, 2004, 1563) n
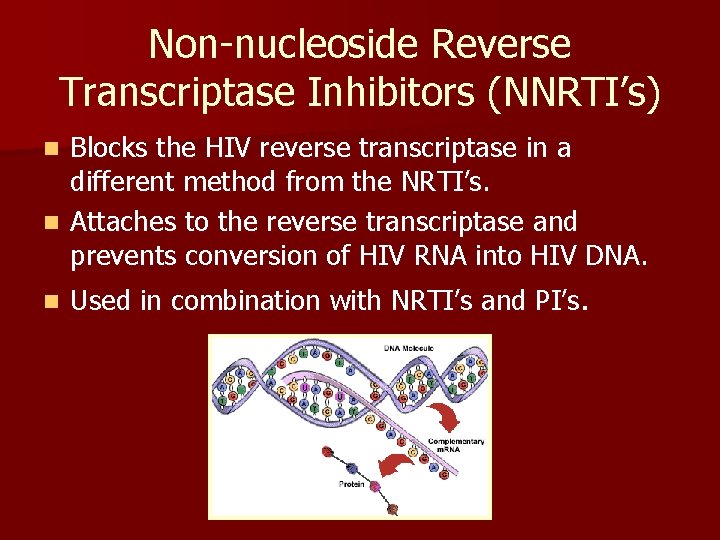
Non-nucleoside Reverse Transcriptase Inhibitors (NNRTI’s) Blocks the HIV reverse transcriptase in a different method from the NRTI’s. n Attaches to the reverse transcriptase and prevents conversion of HIV RNA into HIV DNA. n n Used in combination with NRTI’s and PI’s.
Side Effects of NNRTI’s n Possible adverse reactions of this class of drug include: Abnormal liver function tests, hepatitis, stomatitis, numbness, muscle pain, drowsiness, changes in dreams, trouble concentrating.
Protease Inhibitors (PI’s) Prevents protease enzyme from cleaving HIV proteins into the smaller, functional units. When PI’s are taken, the HIV copies that are made cannot infect CD 4+ cells and lymphocytes. n When taken alone, the virus quickly develops resistance to its effects, so PI’s are always taken with other drugs. n Missed doses leads to virus resistance and drug failure. n
Side Effects of PI’s n The following may be some of the adverse effects associated with PI’s: Hemolytic anemia, parasthesia, kidney stones, asymptomatic hyperbilirubinemia, dyspepsia, altered taste, mood alterations, drowsiness.
HAART n Highly active antiretroviral treatment n A regimen that consists of 2 NRTI’s + a PI (or NNRTI) OR n 2 PI’s + one other antiretroviral agent
Decision Making n Treatment decisions for every patient is individualized and based on 3 factors: – Viral load – CD 4 T-cell count – Clinical condition of patient
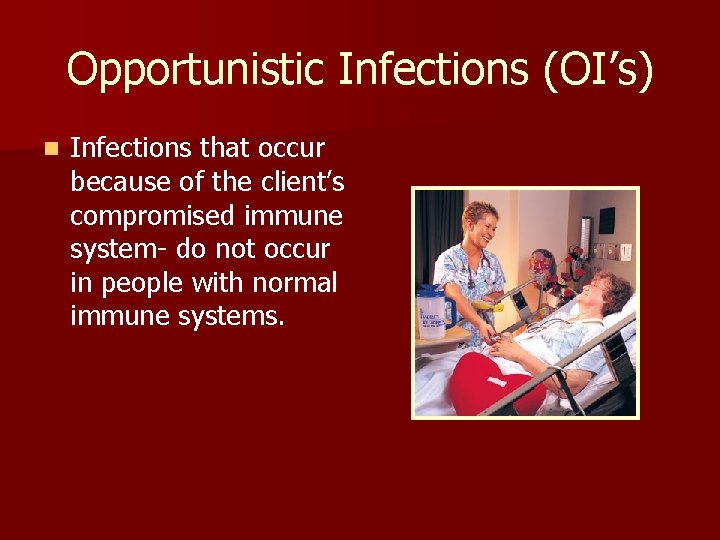
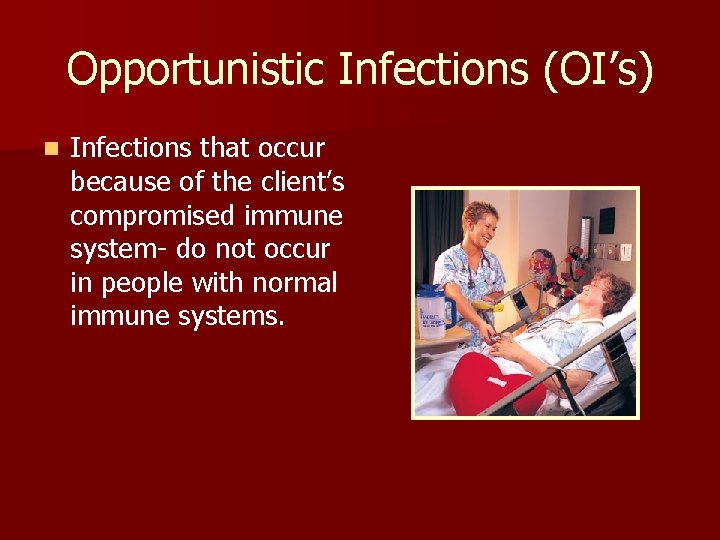
Opportunistic Infections (OI’s) n Infections that occur because of the client’s compromised immune system- do not occur in people with normal immune systems.
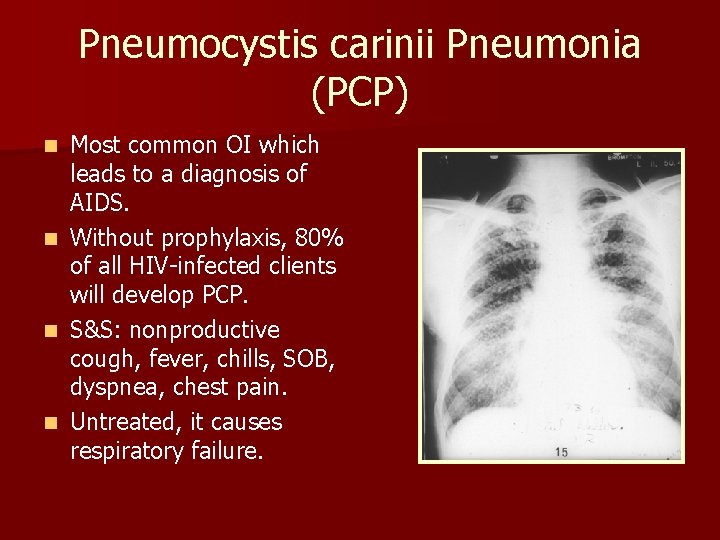
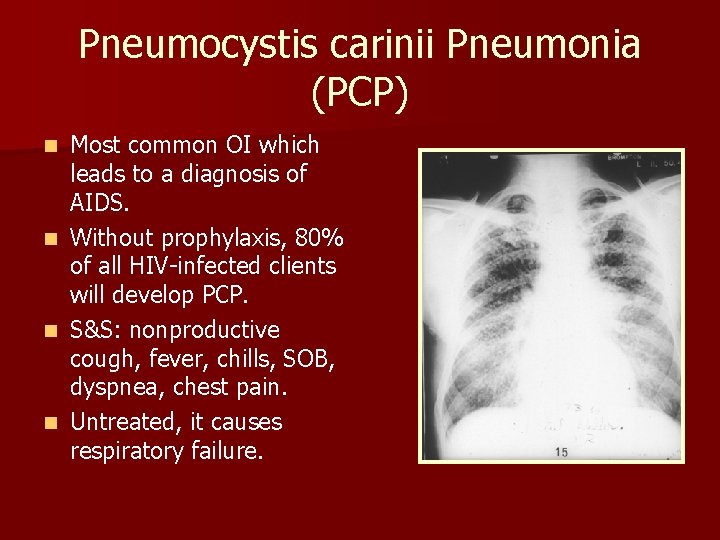
Pneumocystis carinii Pneumonia (PCP) Most common OI which leads to a diagnosis of AIDS. n Without prophylaxis, 80% of all HIV-infected clients will develop PCP. n S&S: nonproductive cough, fever, chills, SOB, dyspnea, chest pain. n Untreated, it causes respiratory failure. n
Mycobacterium avium complex (MAC) n MAC is a group of bacilli that usually causes respiratory infection. n May also be found in the GI tract, lymph nodes, and bone marrow.
Tuberculosis (TB) n TB tends to occur early in HIV infection. n If it occurs late in HIV infection, there may be no response to a tuberculin skin test. (This is called anergy, which happens due to the immune system that can no longer respond to the TB antigen. )
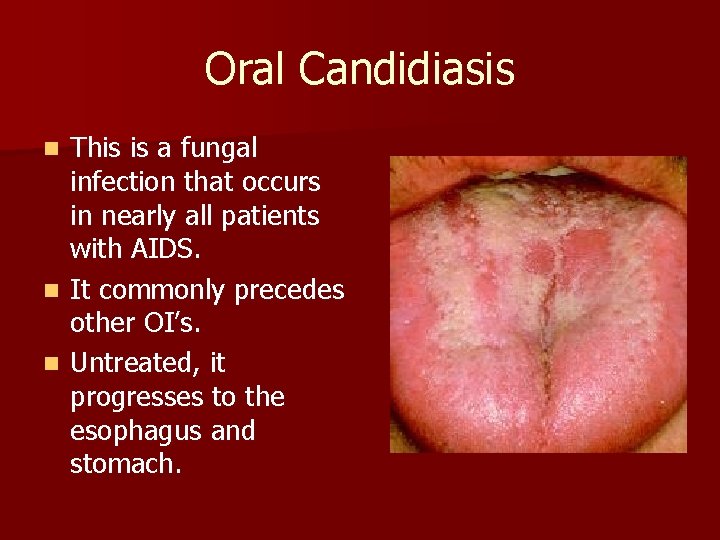
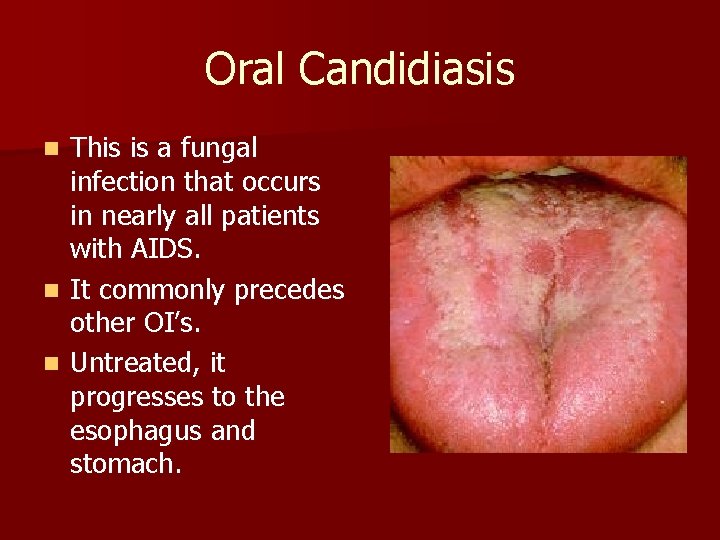
Oral Candidiasis This is a fungal infection that occurs in nearly all patients with AIDS. n It commonly precedes other OI’s. n Untreated, it progresses to the esophagus and stomach. n
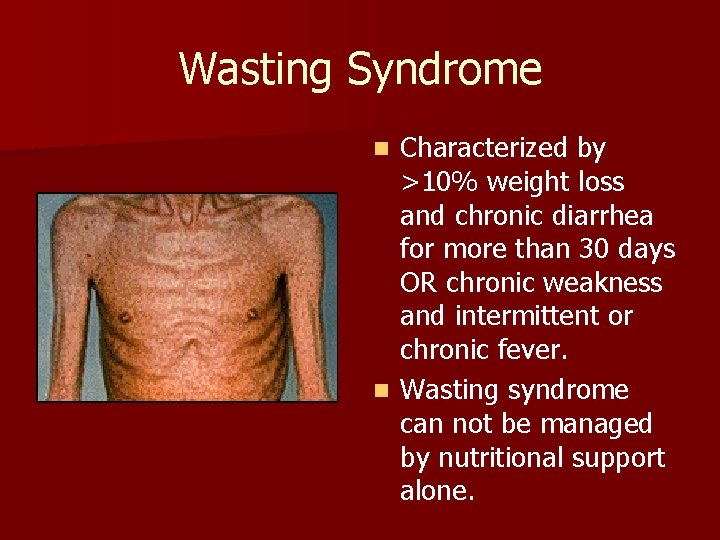
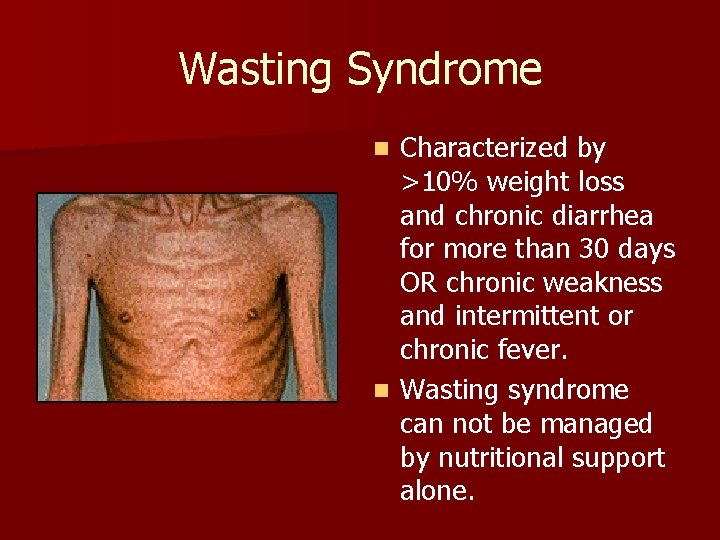
Wasting Syndrome Characterized by >10% weight loss and chronic diarrhea for more than 30 days OR chronic weakness and intermittent or chronic fever. n Wasting syndrome can not be managed by nutritional support alone. n
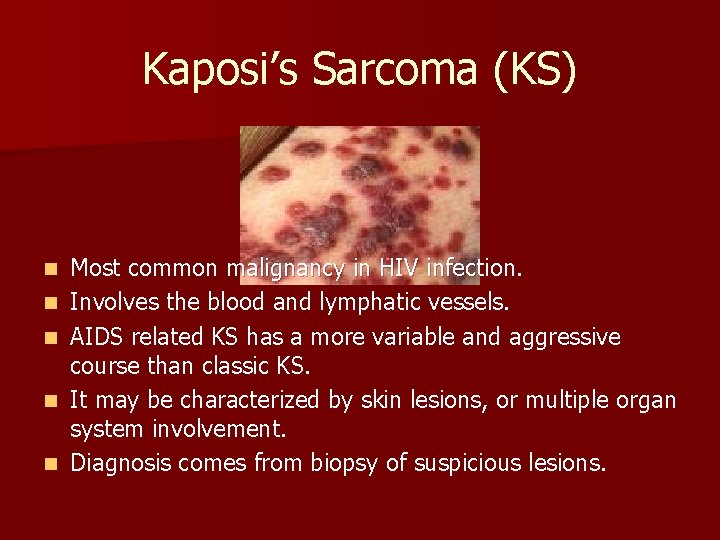
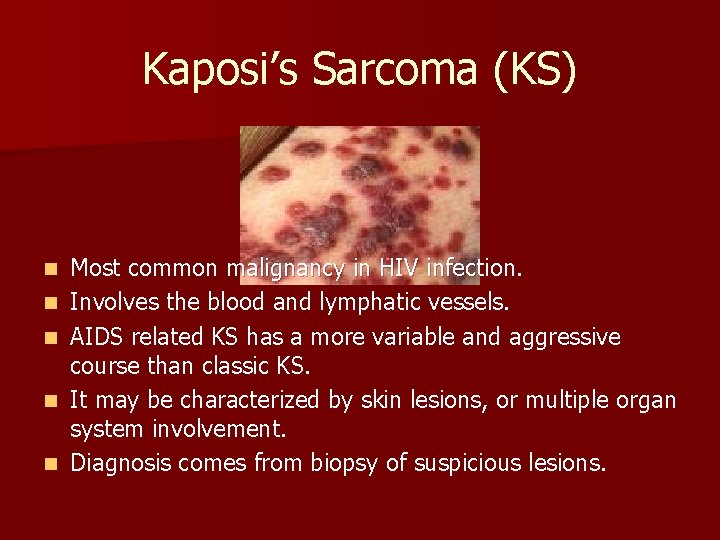
Kaposi’s Sarcoma (KS) n n n Most common malignancy in HIV infection. Involves the blood and lymphatic vessels. AIDS related KS has a more variable and aggressive course than classic KS. It may be characterized by skin lesions, or multiple organ system involvement. Diagnosis comes from biopsy of suspicious lesions.
B-Cell Lymphomas n Second most common malignancy in HIVinfected clients. n Often occurs in the brain, bone marrow and GI tract. n Chemotherapy is not as effective in HIVrelated lymphomas.
HIV Encephalopathy n Formerly referred to as AIDS dementia complex. n Clinical syndrome consisting of a progressive decline in cognitive, behavioral, and motor function. n HIV has been found in the CSF of patients with this syndrome.
S&S of HIV Encephalopathy n Early stage: memory loss, difficulty concentrating, headache, confusion, psychomotor slowing, apathy, ataxia. n Later stage: Global cognitive impairments, delay in verbal responses, hyperreflexia, psychosis, hallucinations, tremor, incontinence, seizures, mutism, death. n (Smeltzer & Bare, 2004, 1567).
Nursing Management There are many complications associated with AIDS! n Nursing interventions remain the same as other people with those conditions n Don’t forget about the pyschosocial implications n – – – Terminal illness Isolation (physical and emotional) Coping Grief Guilt and anger : associated with transmitting the disease – Stigma
Nursing Managment n Don’t contribute to the stigma associated with AIDS – – – Don’t make assumptions Don’t treat your patient any different Use universal precautions with ALL patients
Nursing Management Protect Yourself!!!
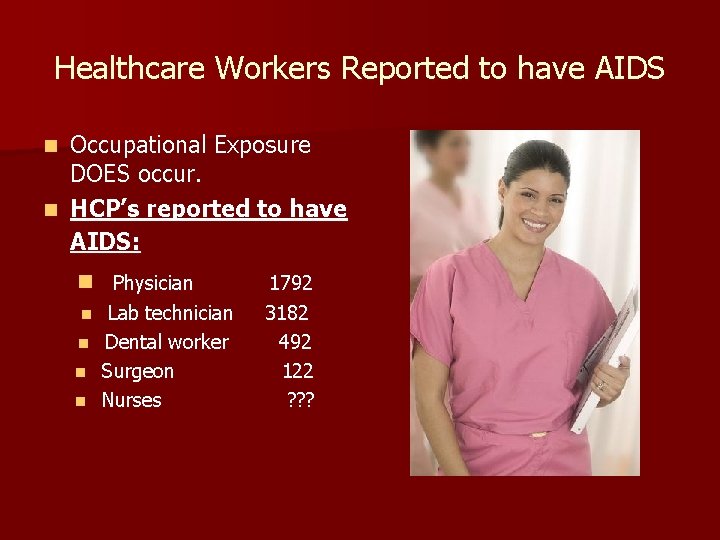
Healthcare Workers Reported to have AIDS Occupational Exposure DOES occur. n HCP’s reported to have AIDS: n n Physician Lab technician n Dental worker n Surgeon n Nurses n 1792 3182 492 122 ? ? ?
Occupational Exposure to HIV n Exposure to HIV–infected blood via percutaneous injury: n 3/1000 n Mucocutaneous exposure: n Less than 1/1000 n Intact Skin: n No known risk
Post-Exposure Prophylaxis (PEP) n Administration of antiretroviral medications (ARV’s) after exposure to HIV. n Given as soon as possible after exposure n Must be within 72 hours n 4 -week treatment with 2 -3 different ARV’s n Standard procedure since 1996. n Reduces transmission by 79%
PEP cont’d… n n n Page 2145, Smeltzer & Bare Table 70 -5 Recommended Algorithm used to determine PEP
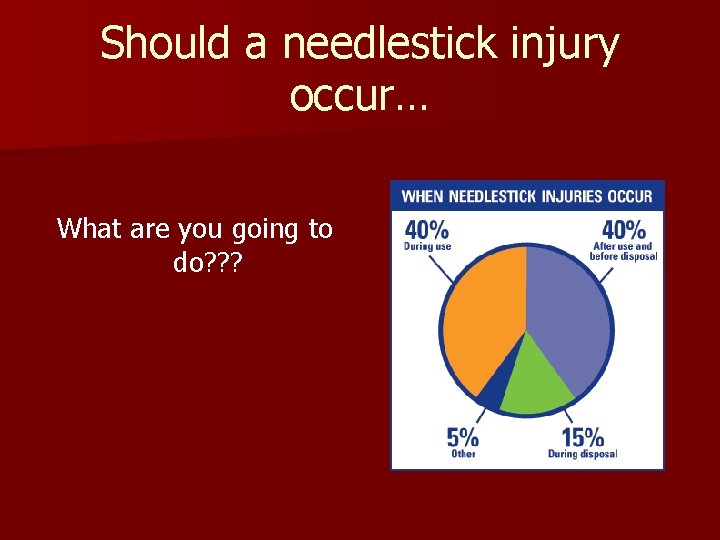
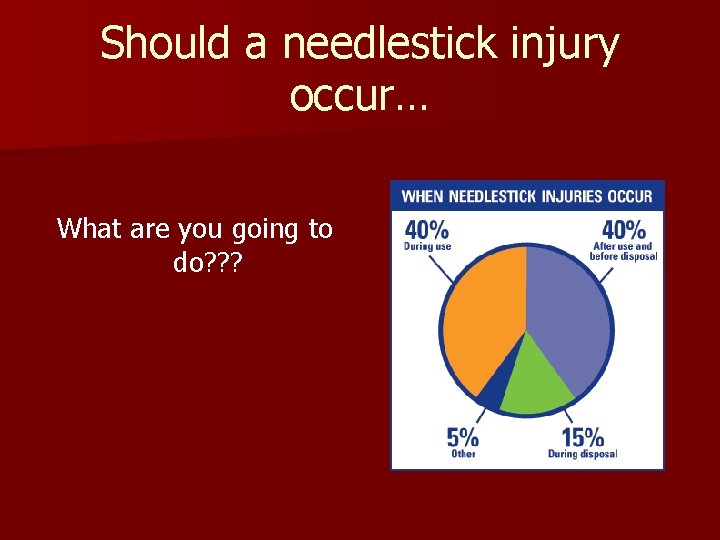
Should a needlestick injury occur… What are you going to do? ? ?
n Wash area thoroughly with soap and water n Alert supervisor, documentation. n Identify source patient n Give consent for baseline testing n PEP n Follow-up with PEP testing 6 weeks , 3 months and 6 months after beginning treatment n Documentation Day et al. , 2007.
PEP use for non-occupation exposure n Non-occupational HIV exposures, commonly related to unsafe behaviors. n Would PEP encourage unsafe behaviors? n No research indicated PEP works for nonoccupational exposure. n PEP not a ‘morning after’ pill
Preventative Strategies: Universal Precautions n n n n Routine use of barriers (gloves, gowns, masks, goggles) Washing skin surfaces immediately after contact with blood or body fluids. Disinfecting instruments and contaminated equipment. Properly handling soiled linens Careful handling/disposal of sharp instruments. Documentation of sterilization quality following procedures. page 1557 Smeltzer & Bare, Chart 52 -3
Building Better Prevention Programs Administrative Efforts n Development/ Promotion of the use of safety devices. n Sharp disposal containers n Disposable instrument use n n Monitoring of the effectiveness of PEP.
Pre-Exposure Prophylaxis for HIV n n “Various studied have shown that antiretroviral treatment given at or shortly after HIV exposure can reduce likelihood of transmission…” “…this lead to the hypothesis that transmission may be decreased even further if treatment were delivered before exposure to HIV” – Paxton, 2007). Tenofir Safety/ effectiveness still unknown.
Ethics - Tenofir n n n Think about… Obligations of gov’t to provide pre-exposure prophylaxis Appropriate indications for prescribing Tenofir ( think high-risk populations) Who should have priority for pre-exposure prophylaxis? Stigmatization: - Stigma attached to engagement in risky behaviors - Decision making clouded by underlying beliefs
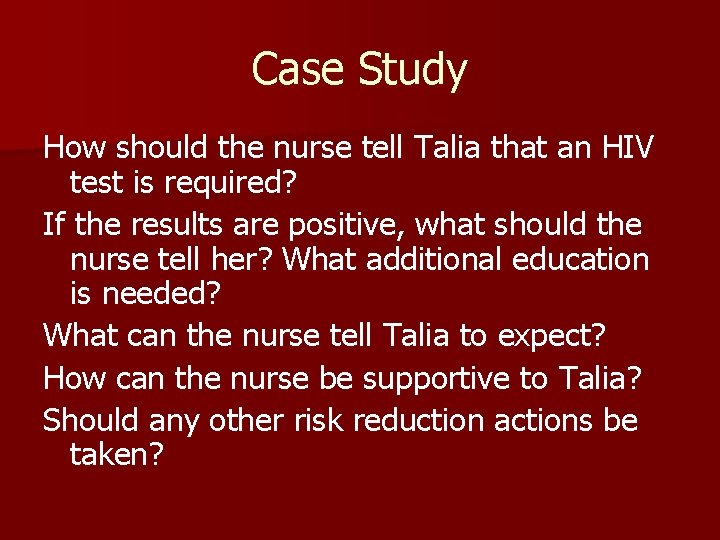
CASE STUDY Talia is a 23 year old female from Halifax. She is an arts student at St. FX university in her third year. She likes to go to the pub on Saturdays and is the hockey team’s biggest fan. Talia is single but had dated several boys since her first year. She used a condom most of the time and goes for regular pap smears. Around Christmas Exams Talia noticed that she is feeling tired all the time. She wakes up in the middle of the night with night sweats and has a rash. She is having a really hard time studying for her exams. Her mom thought that she was probably stressed about exams. But when Talia got her second yeast infection since September she decided to seek medical attention from her friendly neighborhood nurse. Upon examination Talia’s nurse noticed that she had lost 8 lbs since her last visit in September. Her gums appear swollen and so are her lymph nodes. She is anxious to get back to studying.
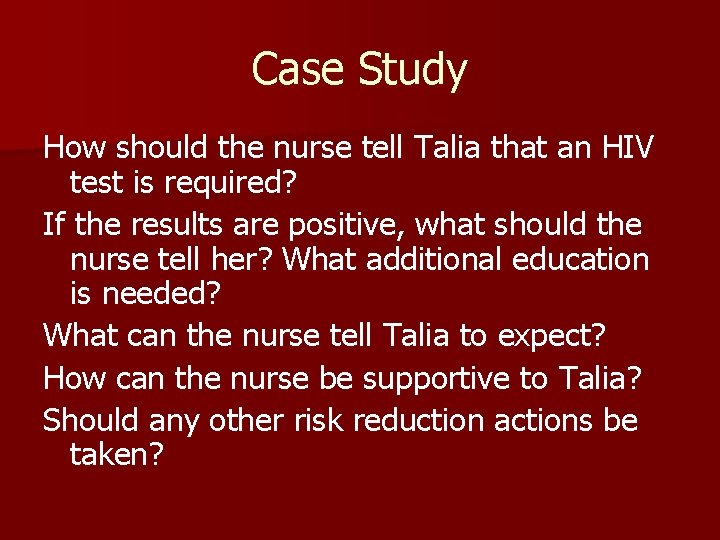
Case Study How should the nurse tell Talia that an HIV test is required? If the results are positive, what should the nurse tell her? What additional education is needed? What can the nurse tell Talia to expect? How can the nurse be supportive to Talia? Should any other risk reduction actions be taken?
Nursing Care of the HIV positive client: THE NURSING PROCESS ASSESSMENT
-identify risk factors - unsafe sexual practices - IV drug use - Physical Assessment – focus on Immune system - Psychological status - Nutritional status - Skin integrity - Respiratory status - Neurological status - Fluid and electrolyte balance - Knowledge level
NSG DIAGNOSIS Impaired skin integrity r/t percutaneous manifestations of HIV infection. n Risk for fluid volume deficit r/t diarrhea n Risk for infection r/t immunodeficiency n Activity intolerance r/t weakness, fatigue. n Pain r/t impaired skin integrity n Anticipatory greiving r/t changes in lifetsyle 2° diagnosis of AIDS n Social isolation r/t stigma of the disease, fear of infecting others n Ineffective A/W clearance r/t increased bronchial secretions, decreased ability to cough.
PLANNING Goals for Patient? ? ?

n Achievement/Maintenance of skin integrity n Maintenance of usual bowel habits n Absence of infection n Improved activity tolerance n Increased comfort n Increased socialization n Improved nutritional status n Increased knowledge base n Absence of complications
NSG INTERVENTIONS n n n n n Promote skin integrity Promote usual bowel habits Prevent infections Improve activity intolerance Maintaining health Improving A/W clearance Relieving pain. increasing comfort Nutritional status Coping Monitor for complications
EVALUATION n n n n Expected Patient Outcomes: Maintains skin integrity Experiences no infections Maintains adequate activity tolerance Experiences increased sense of comfort Progresses through grieving process Remains free of complications
Ethical considerations n n n n Many patients with HIV have engaged in ‘stigmatized’ behaviors. Challenges traditional, religious and moral values of HCP’s. Fear and anxiety re: disease transmission. The impact of an epidemic on a culture/society (lost generation, orphans, etc) Nurses encouraged to examine own personal beliefs / values clarification. Challenges legal and political systems End of Life Care Pg. 1584, Smeltzer & Bare Chart 52 -10
 Causative organism of hiv/aids
Causative organism of hiv/aids Test wiedzy o hiv i aids z odpowiedziami
Test wiedzy o hiv i aids z odpowiedziami Chapter 17 oral pathology
Chapter 17 oral pathology A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Kasus hiv aids
Kasus hiv aids Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Jacqui michle
Jacqui michle Choroby wskaznikowe aids
Choroby wskaznikowe aids What does hiv stand
What does hiv stand Simon collins hiv
Simon collins hiv Feedbackstart
Feedbackstart Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Hiv siv
Hiv siv Most complex characters evolve
Most complex characters evolve Negative hiv test result
Negative hiv test result Murder by hiv
Murder by hiv Aids symptoms
Aids symptoms Incubation period of hiv
Incubation period of hiv Hiv
Hiv Procentowe ryzyko zakażenia hiv
Procentowe ryzyko zakażenia hiv Progmas
Progmas Stadium hiv
Stadium hiv Basic hiv course
Basic hiv course Procentowe ryzyko zakażenia hiv
Procentowe ryzyko zakażenia hiv Iris hiv
Iris hiv Hiv life cycle
Hiv life cycle Hiv vaccinr
Hiv vaccinr Itil wikipedia fr
Itil wikipedia fr Arv copenhagen
Arv copenhagen Im szuhjang
Im szuhjang Hiv
Hiv Dot
Dot 4.jenerasyon vidas hıv duo ultra testi güvenilir mi
4.jenerasyon vidas hıv duo ultra testi güvenilir mi Types of hiv counselling
Types of hiv counselling What does hiv stand
What does hiv stand Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Hiv retrovirus
Hiv retrovirus Fiebig hiv
Fiebig hiv Hiv stays alive in dried blood
Hiv stays alive in dried blood Hiv transmissions
Hiv transmissions Herpes syntom
Herpes syntom Hiv
Hiv Hiv diagnosis algorithm
Hiv diagnosis algorithm Vertical resposta
Vertical resposta Hiv in adults
Hiv in adults Phdp in hiv
Phdp in hiv Notifikasi pasangan adalah
Notifikasi pasangan adalah Stakeholders in hiv prevention
Stakeholders in hiv prevention Hiv
Hiv Hiv test results
Hiv test results Global hiv prevention coalition
Global hiv prevention coalition Hiv
Hiv Ciclo do hiv
Ciclo do hiv Syptoms of hiv
Syptoms of hiv Tabela perímetro cefálico por idade
Tabela perímetro cefálico por idade Pola progresi penyakit typical progressor berlangsung mulai
Pola progresi penyakit typical progressor berlangsung mulai Hiv lifecycle
Hiv lifecycle Dr shabani
Dr shabani Hiv reverse transcription
Hiv reverse transcription Risk of receiving unprotected oral
Risk of receiving unprotected oral Hiv test window period
Hiv test window period Hiv
Hiv Hiv case-based surveillance in ethiopia
Hiv case-based surveillance in ethiopia Nsradio
Nsradio Hiv
Hiv Hiv
Hiv Burkitt lymphoma
Burkitt lymphoma Yu1u
Yu1u Vidas hiv duo ultra package insert
Vidas hiv duo ultra package insert Kuchecheudzwa
Kuchecheudzwa Hiv adalah
Hiv adalah Stadium hiv
Stadium hiv Hiv treatments
Hiv treatments Abcde hiv
Abcde hiv Objawy hiv
Objawy hiv Ciclo vitale hiv
Ciclo vitale hiv Hiv risk factors
Hiv risk factors Phagocytosis ap bio
Phagocytosis ap bio Hiv
Hiv Hiv life cycle
Hiv life cycle Nefropatia
Nefropatia Hiv
Hiv Hiv
Hiv