Heart Failure Anita Deswal M D M P



![Aldosterone Antagonists • • Aldosterone receptor antagonists [or mineralocorticoid receptor antagonists (MRA)] are recommended Aldosterone Antagonists • • Aldosterone receptor antagonists [or mineralocorticoid receptor antagonists (MRA)] are recommended](https://slidetodoc.com/presentation_image/173846bb467e6df3f6f30e6f195be203/image-28.jpg)






- Slides: 48

Heart Failure Anita Deswal, M. D. , M. P. H. Professor of Medicine Chief of Cardiology Michael E. De. Bakey VAMC & Baylor College of Medicine, Houston
Speaker Disclosures None

Objectives • To discuss the definition of heart failure and clinical presentation of heart failure • • To discuss types of heart failure based on ejection fraction To discuss the guideline-based management of patients with heart failure
Definition of Heart Failure “Heart failure is a clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood” ACC/AHA Guidelines 2013
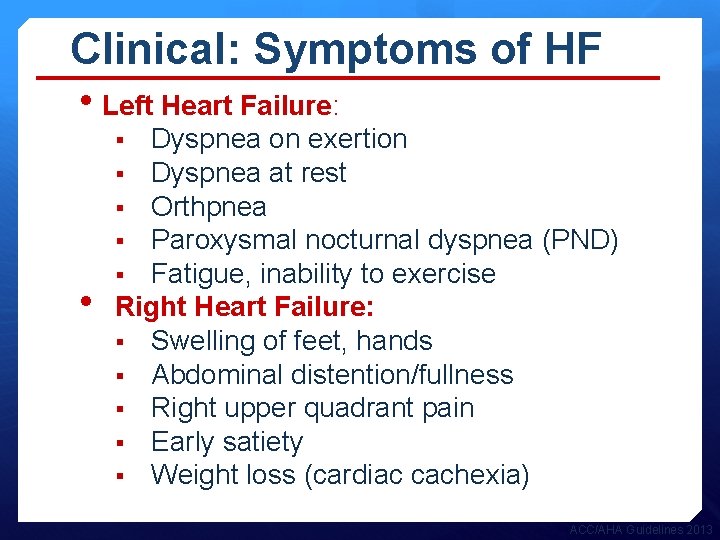
Clinical: Symptoms of HF • Left Heart Failure: Dyspnea on exertion § Dyspnea at rest § Orthpnea § Paroxysmal nocturnal dyspnea (PND) § Fatigue, inability to exercise Right Heart Failure: § Swelling of feet, hands § Abdominal distention/fullness § Right upper quadrant pain § Early satiety § Weight loss (cardiac cachexia) § • ACC/AHA Guidelines 2013
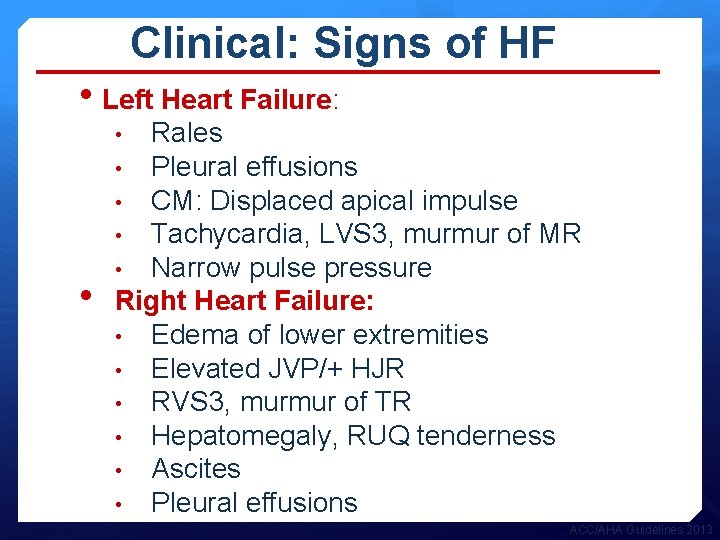
Clinical: Signs of HF • Left Heart Failure: Rales • Pleural effusions • CM: Displaced apical impulse • Tachycardia, LVS 3, murmur of MR • Narrow pulse pressure Right Heart Failure: • Edema of lower extremities • Elevated JVP/+ HJR • RVS 3, murmur of TR • Hepatomegaly, RUQ tenderness • Ascites • Pleural effusions • • ACC/AHA Guidelines 2013

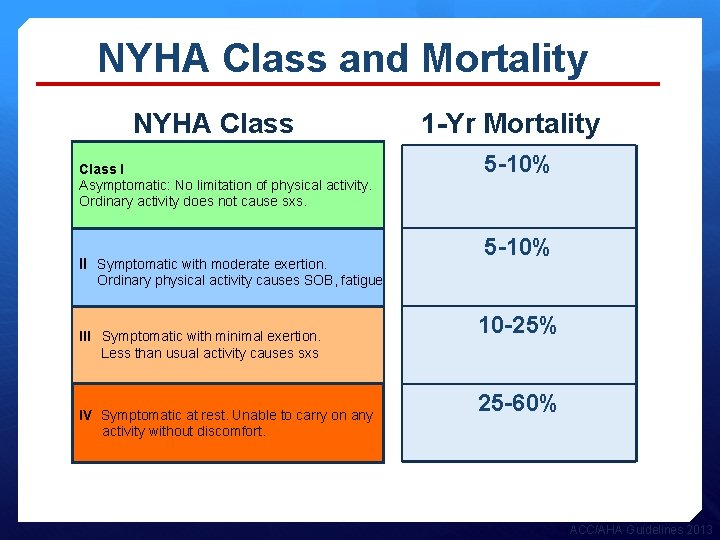
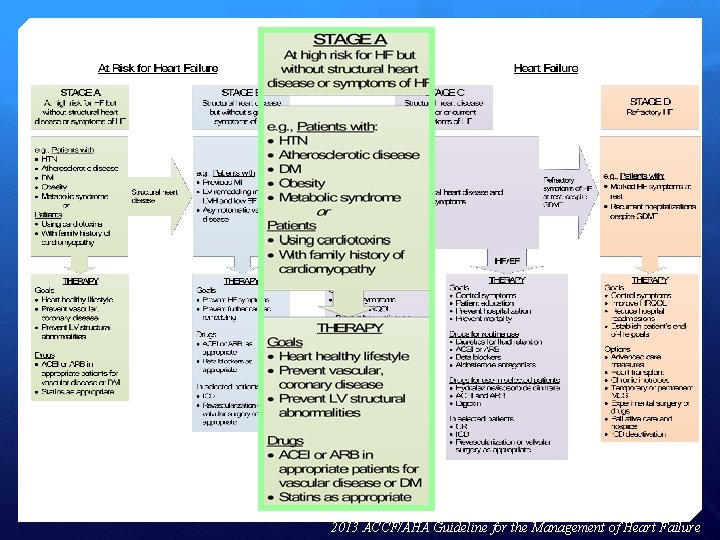
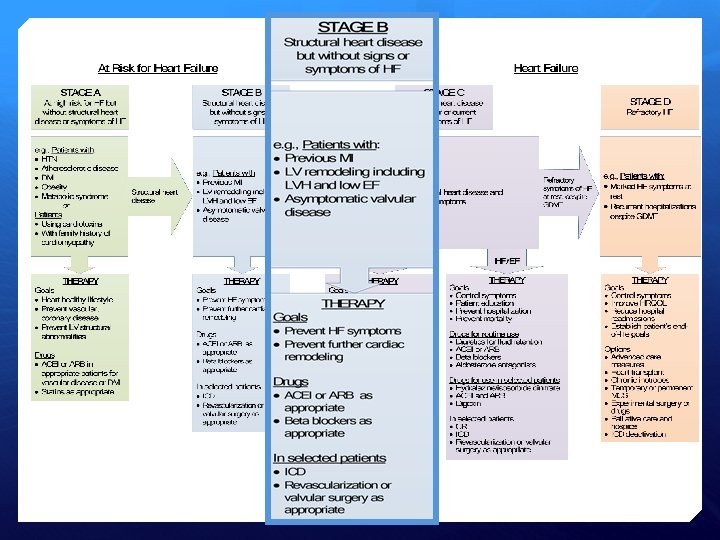
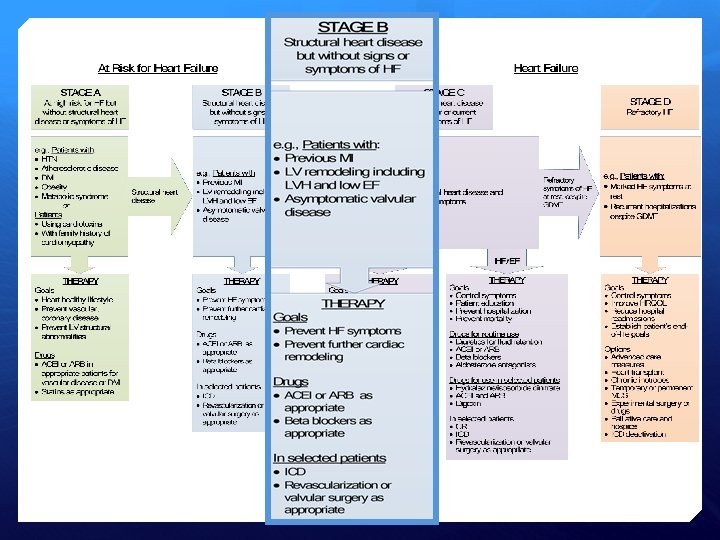
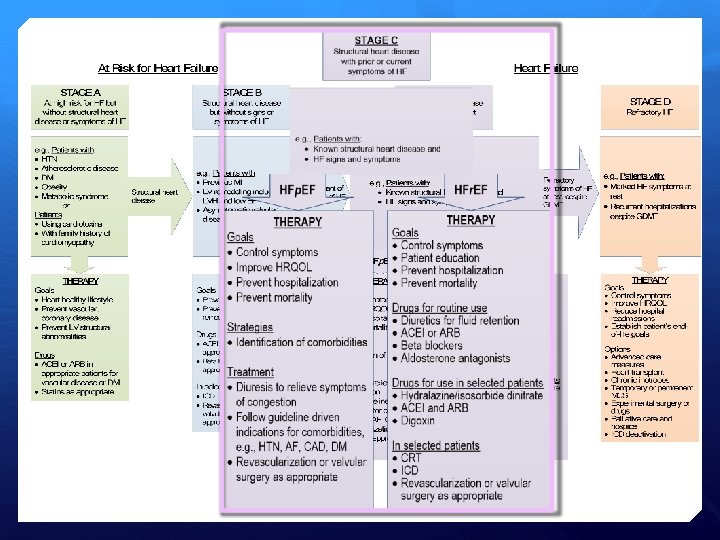
Stages of Heart Failure Asymptomatic A At high risk for HF but without structural heart disease or symptoms of HF (e. g. , patients with HTN or CAD) B Structural heart disease but without symptoms of HF C Structural heart disease with prior or current symptoms of HF D Refractory/advanced HF requiring specialized interventions NYHA Class I Asymptomatic: No limitation of physical activity. Ordinary activity does not cause sxs. II Symptomatic with moderate exertion. Ordinary physical activity causes SOB, fatigue III Symptomatic with minimal exertion. Less than usual activity causes sxs IV Symptomatic at rest. Unable to carry on any activity without discomfort. Symptomatic ACC/AHA Guidelines 2013
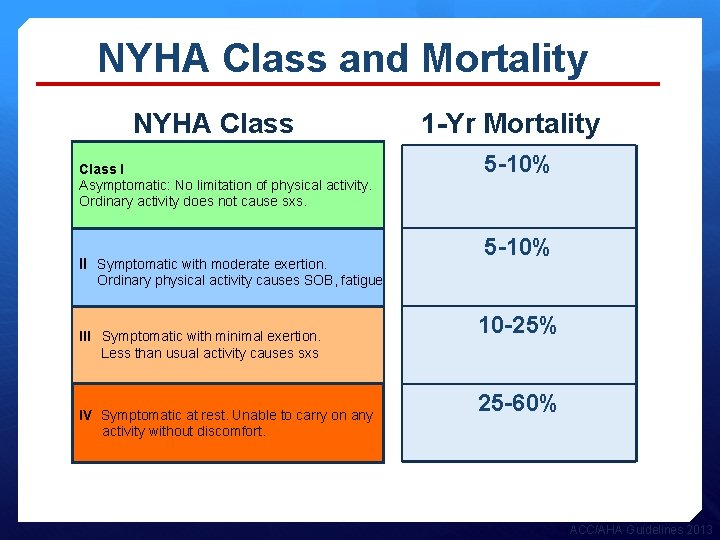
NYHA Class and Mortality NYHA Class I Asymptomatic: No limitation of physical activity. Ordinary activity does not cause sxs. II Symptomatic with moderate exertion. 1 -Yr Mortality 5 -10% Ordinary physical activity causes SOB, fatigue III Symptomatic with minimal exertion. Less than usual activity causes sxs IV Symptomatic at rest. Unable to carry on any activity without discomfort. 10 -25% 25 -60% ACC/AHA Guidelines 2013
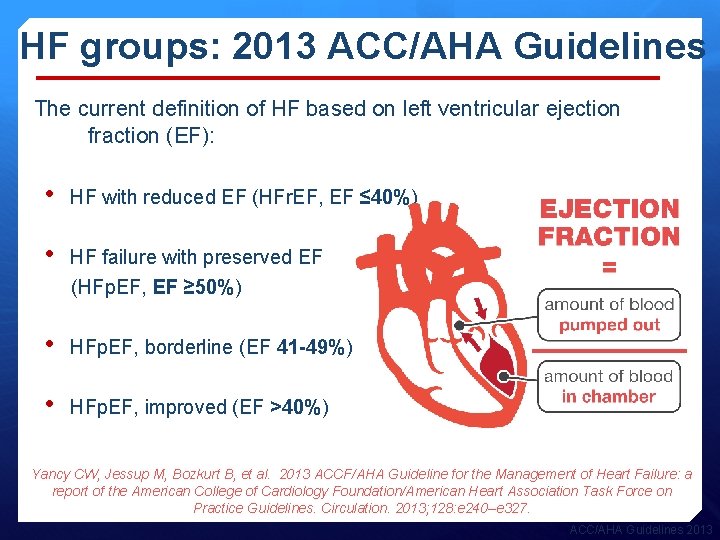
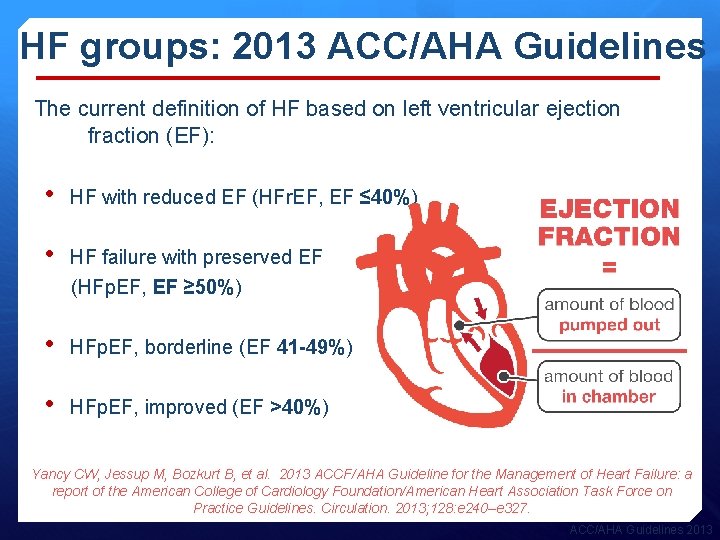
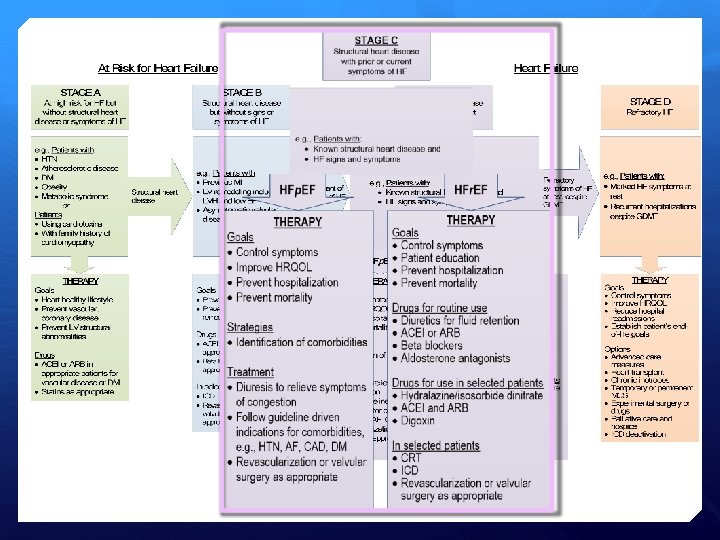
HF groups: 2013 ACC/AHA Guidelines The current definition of HF based on left ventricular ejection fraction (EF): • HF with reduced EF (HFr. EF, EF ≤ 40%) • HF failure with preserved EF (HFp. EF, EF ≥ 50%) • HFp. EF, borderline (EF 41 -49%) • HFp. EF, improved (EF >40%) Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 128: e 240–e 327. ACC/AHA Guidelines 2013
Management of Patients with Heart Failure
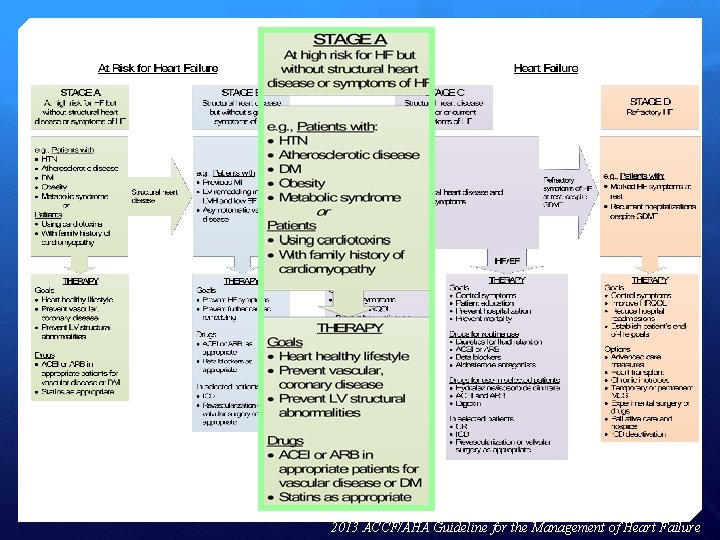
2013 ACCF/AHA Guideline for the Management of Heart Failure
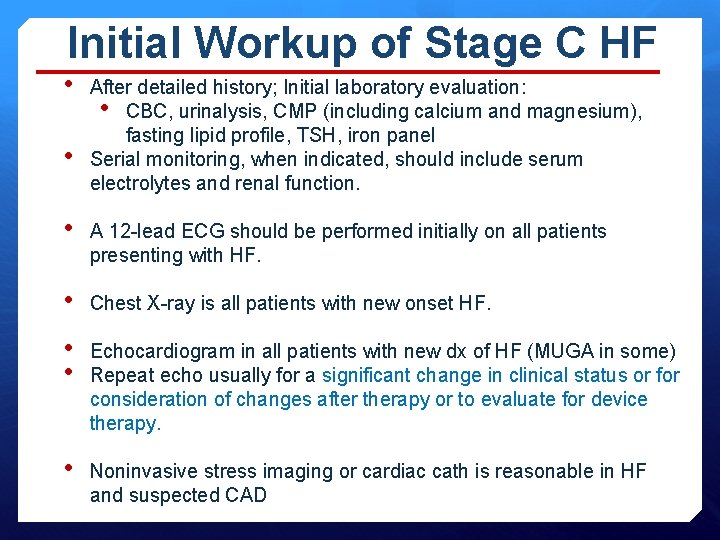
Initial Workup of Stage C HF • • After detailed history; Initial laboratory evaluation: • CBC, urinalysis, CMP (including calcium and magnesium), fasting lipid profile, TSH, iron panel Serial monitoring, when indicated, should include serum electrolytes and renal function. • A 12 -lead ECG should be performed initially on all patients presenting with HF. • Chest X-ray is all patients with new onset HF. • • Echocardiogram in all patients with new dx of HF (MUGA in some) Repeat echo usually for a significant change in clinical status or for consideration of changes after therapy or to evaluate for device therapy. • Noninvasive stress imaging or cardiac cath is reasonable in HF and suspected CAD
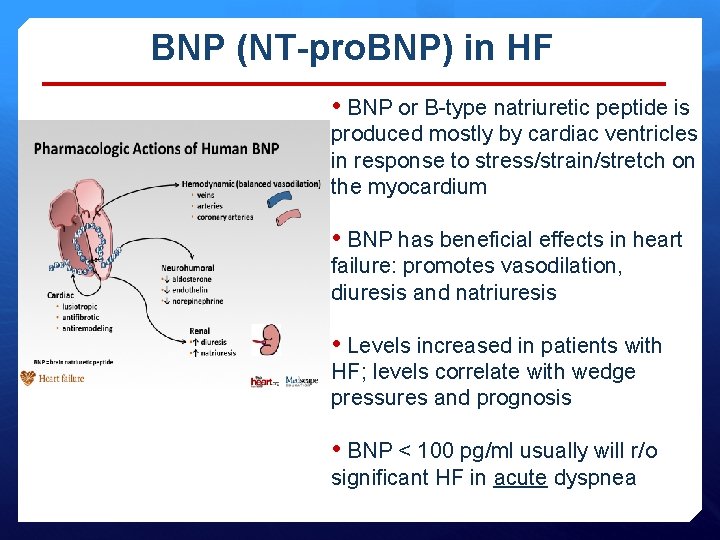
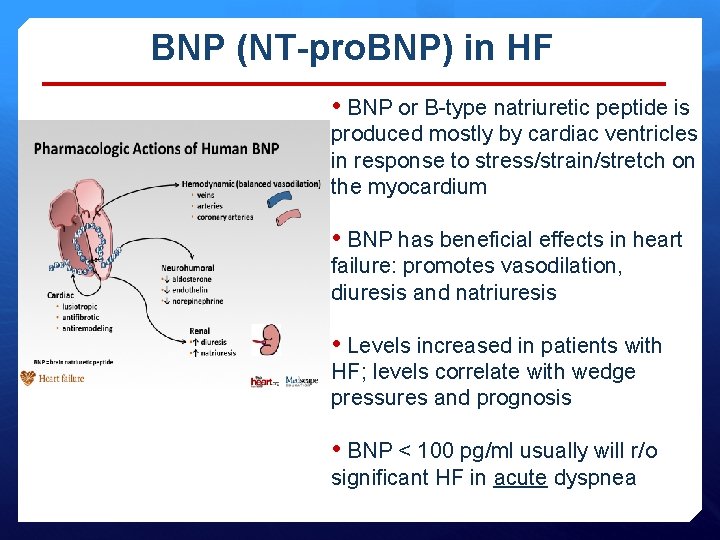
BNP (NT-pro. BNP) in HF • BNP or B-type natriuretic peptide is produced mostly by cardiac ventricles in response to stress/strain/stretch on the myocardium • BNP has beneficial effects in heart failure: promotes vasodilation, diuresis and natriuresis • Levels increased in patients with HF; levels correlate with wedge pressures and prognosis • BNP < 100 pg/ml usually will r/o significant HF in acute dyspnea
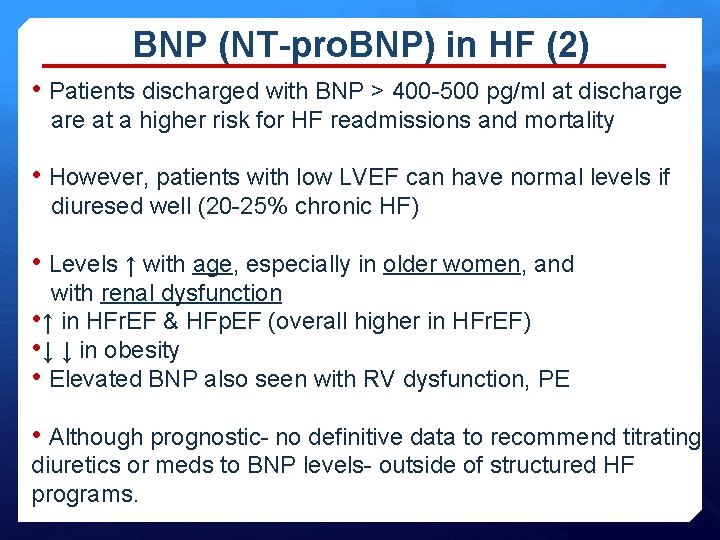
BNP (NT-pro. BNP) in HF (2) • Patients discharged with BNP > 400 -500 pg/ml at discharge are at a higher risk for HF readmissions and mortality • However, patients with low LVEF can have normal levels if diuresed well (20 -25% chronic HF) • Levels ↑ with age, especially in older women, and with renal dysfunction • ↑ in HFr. EF & HFp. EF (overall higher in HFr. EF) • ↓ ↓ in obesity • Elevated BNP also seen with RV dysfunction, PE • Although prognostic- no definitive data to recommend titrating diuretics or meds to BNP levels- outside of structured HF programs.
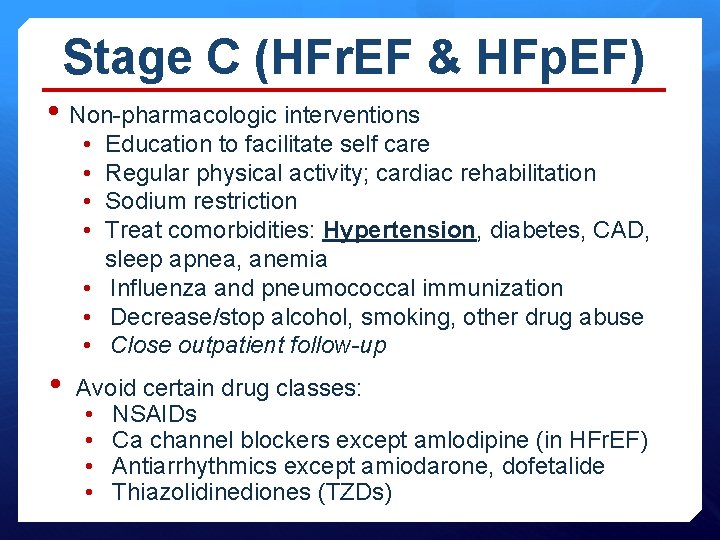
Stage C (HFr. EF & HFp. EF) • Non-pharmacologic interventions • • Education to facilitate self care Regular physical activity; cardiac rehabilitation Sodium restriction Treat comorbidities: Hypertension, diabetes, CAD, sleep apnea, anemia • Influenza and pneumococcal immunization • Decrease/stop alcohol, smoking, other drug abuse • Close outpatient follow-up • Avoid certain drug classes: • NSAIDs • Ca channel blockers except amlodipine (in HFr. EF) • Antiarrhythmics except amiodarone, dofetalide • Thiazolidinediones (TZDs)
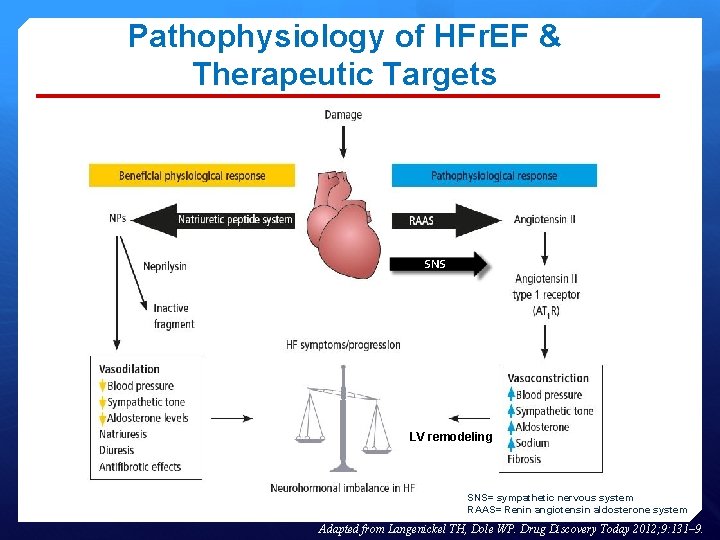
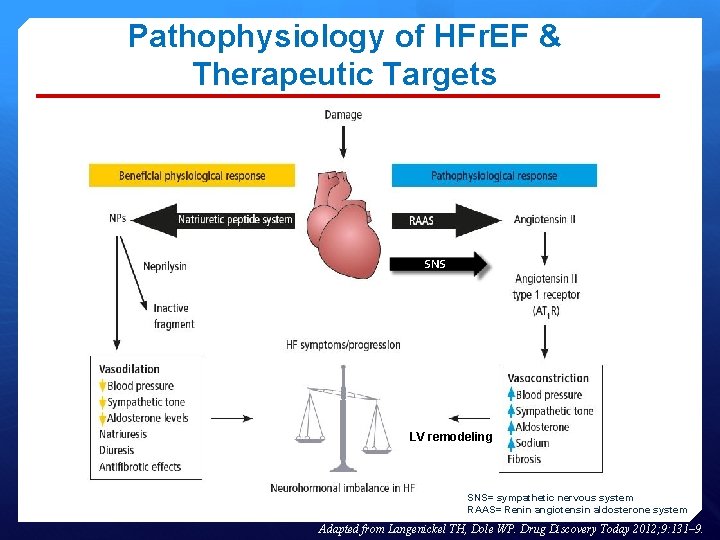
Pathophysiology of HFr. EF & Therapeutic Targets SNS LV remodeling SNS= sympathetic nervous system RAAS= Renin angiotensin aldosterone system Adapted from Langenickel TH, Dole WP. Drug Discovery Today 2012; 9: 131– 9.
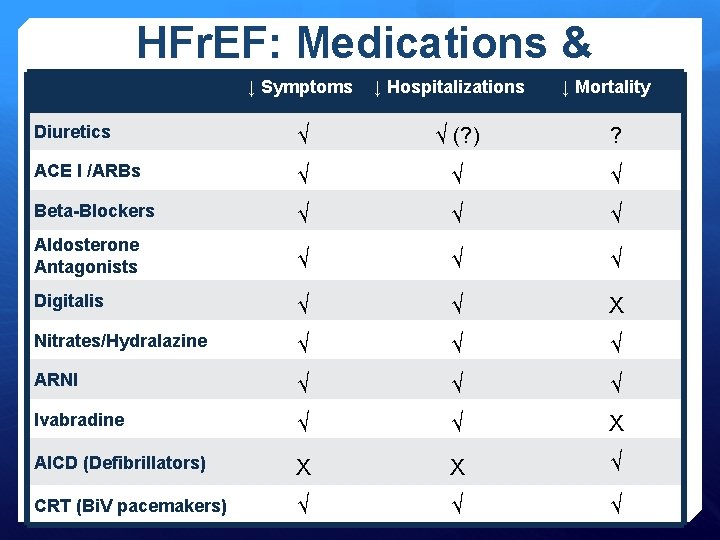
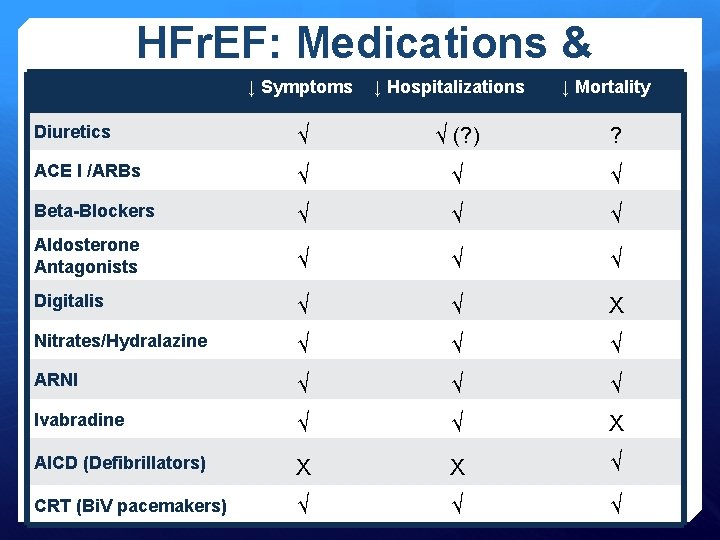
HFr. EF: Medications & ↓ Symptoms ↓ Hospitalizations ↓ Mortality Devices Diuretics √ √ (? ) ? ACE I /ARBs √ √ √ Beta-Blockers √ √ √ Aldosterone Antagonists √ √ √ Digitalis √ √ X Nitrates/Hydralazine √ √ √ ARNI √ √ √ Ivabradine √ √ X AICD (Defibrillators) X X √ CRT (Bi. V pacemakers) √ √ √
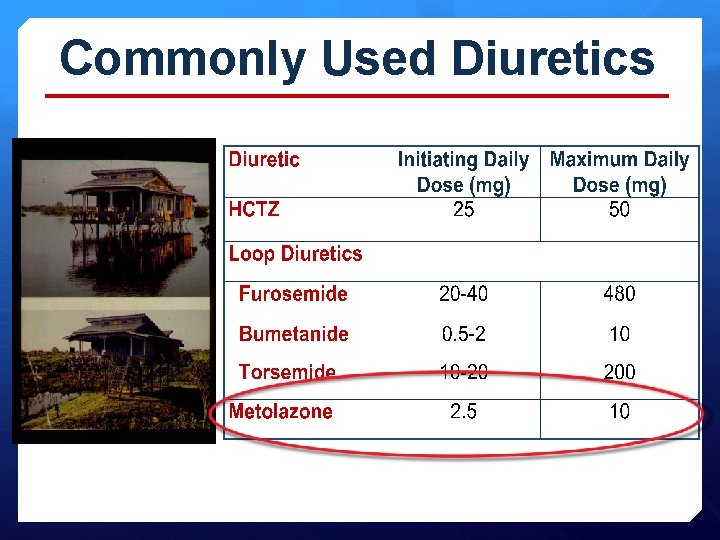
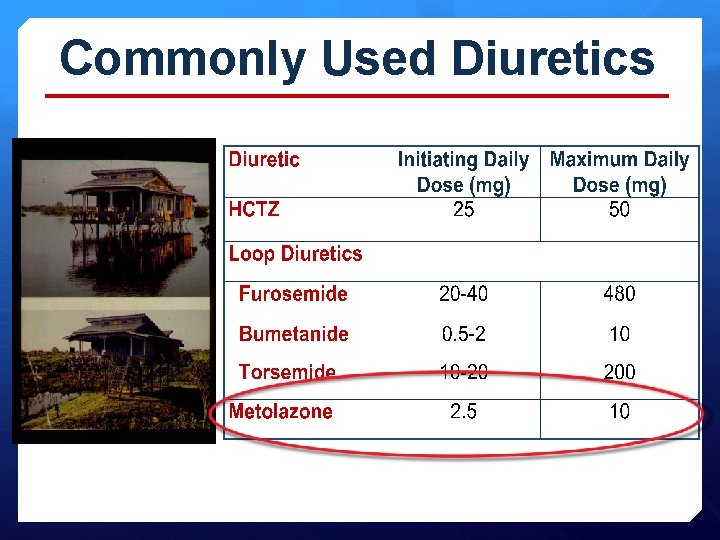
Commonly Used Diuretics
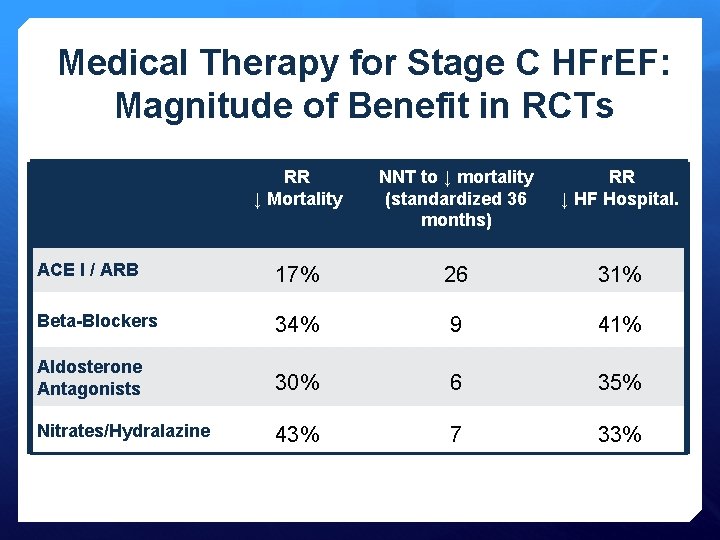
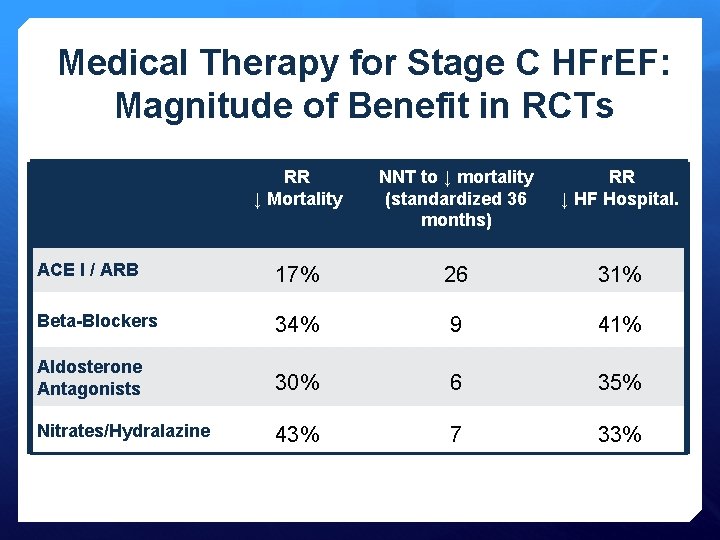
Medical Therapy for Stage C HFr. EF: Magnitude of Benefit in RCTs RR ↓ Mortality NNT to ↓ mortality (standardized 36 months) RR ↓ HF Hospital. ACE I / ARB 17% 26 31% Beta-Blockers 34% 9 41% Aldosterone Antagonists 30% 6 35% Nitrates/Hydralazine 43% 7 33%
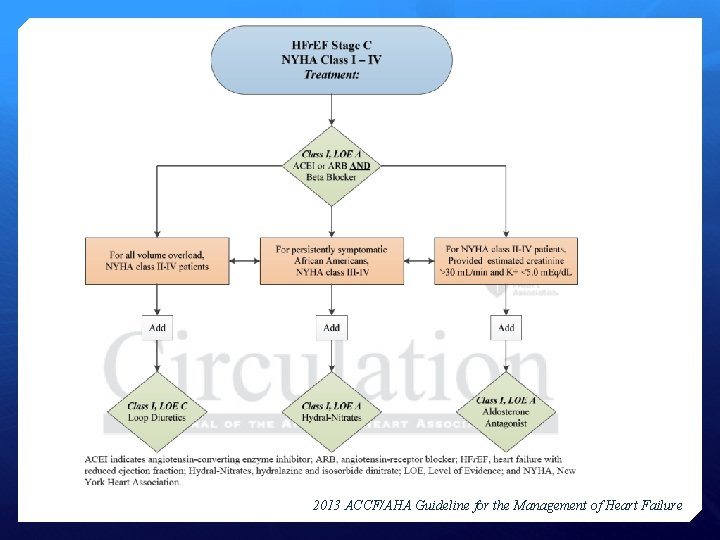
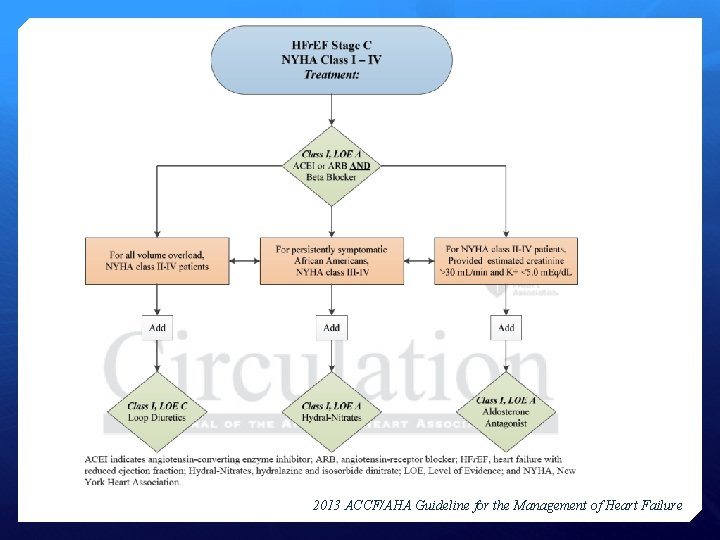
2013 ACCF/AHA Guideline for the Management of Heart Failure
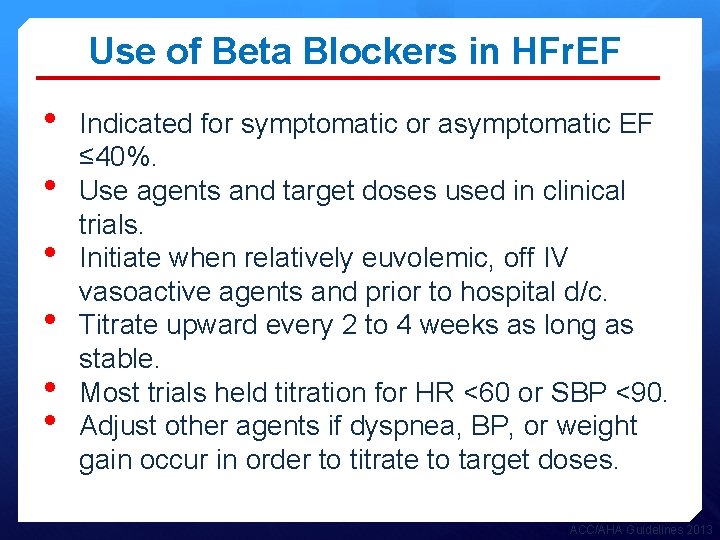
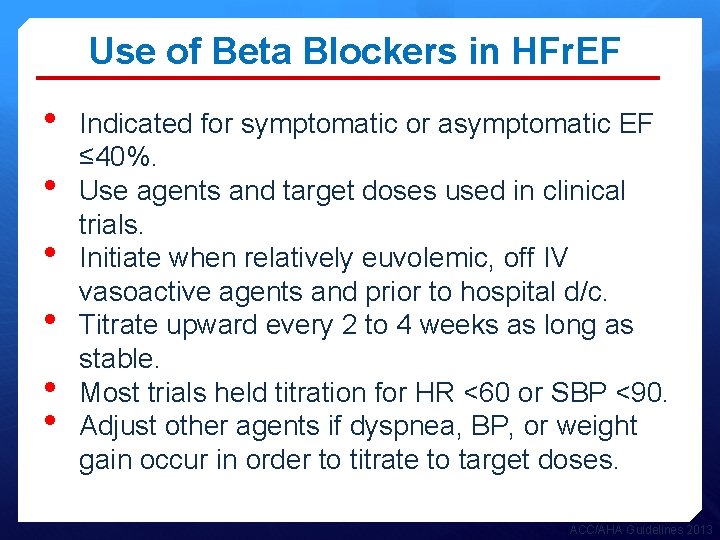
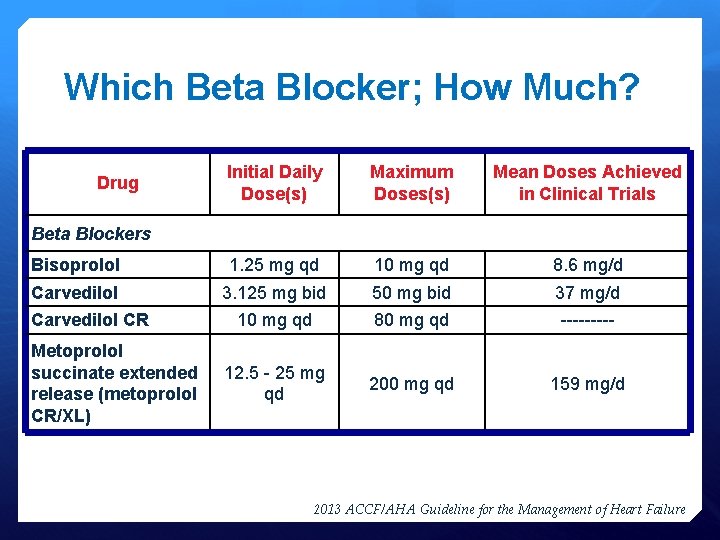
Use of Beta Blockers in HFr. EF • • • Indicated for symptomatic or asymptomatic EF ≤ 40%. Use agents and target doses used in clinical trials. Initiate when relatively euvolemic, off IV vasoactive agents and prior to hospital d/c. Titrate upward every 2 to 4 weeks as long as stable. Most trials held titration for HR <60 or SBP <90. Adjust other agents if dyspnea, BP, or weight gain occur in order to titrate to target doses. ACC/AHA Guidelines 2013
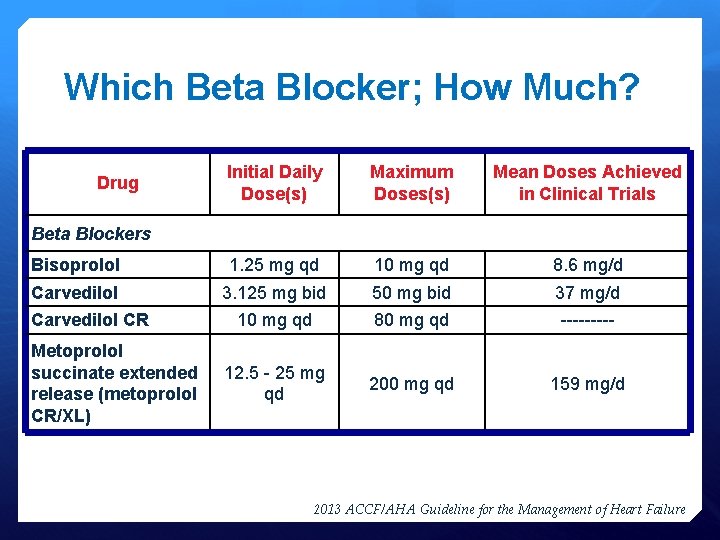
Which Beta Blocker; How Much? Initial Daily Dose(s) Maximum Doses(s) Mean Doses Achieved in Clinical Trials Bisoprolol 1. 25 mg qd 10 mg qd 8. 6 mg/d Carvedilol 3. 125 mg bid 50 mg bid 37 mg/d 10 mg qd 80 mg qd ----- 12. 5 - 25 mg qd 200 mg qd 159 mg/d Drug Beta Blockers Carvedilol CR Metoprolol succinate extended release (metoprolol CR/XL) 2013 ACCF/AHA Guideline for the Management of Heart Failure
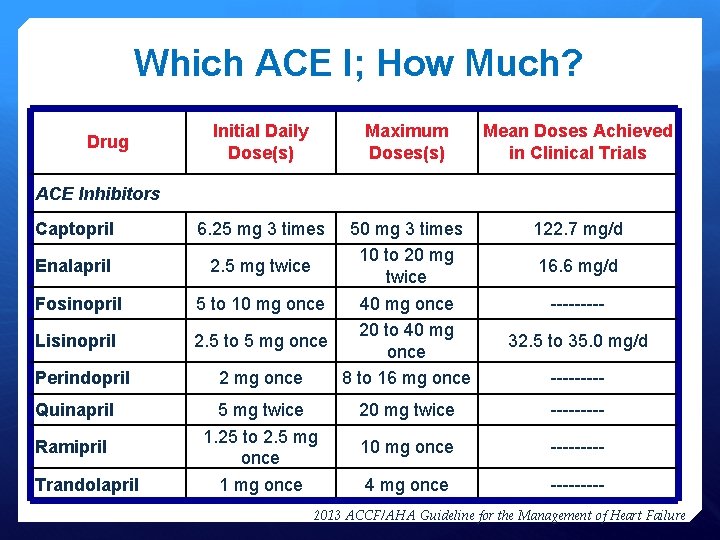
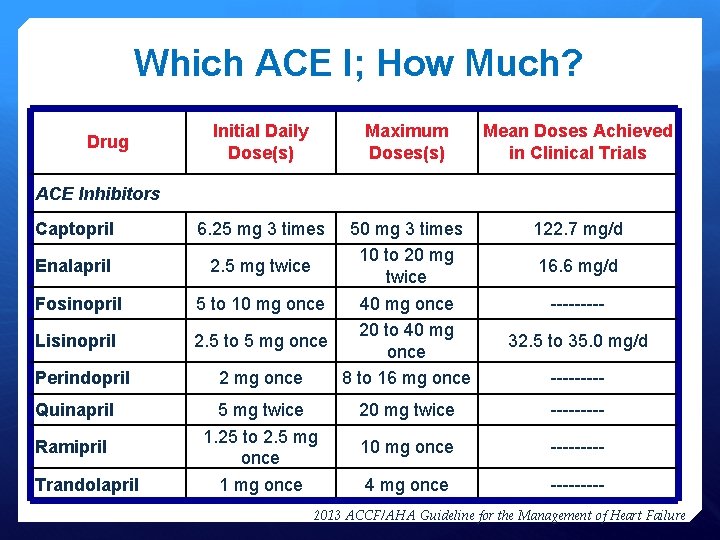
Which ACE I; How Much? Drug Initial Daily Dose(s) Maximum Doses(s) Mean Doses Achieved in Clinical Trials ACE Inhibitors Captopril Enalapril Fosinopril Lisinopril Perindopril Quinapril Ramipril Trandolapril 6. 25 mg 3 times 50 mg 3 times 10 to 20 mg 2. 5 mg twice 5 to 10 mg once 40 mg once 20 to 40 mg 2. 5 to 5 mg once 2 mg once 8 to 16 mg once 5 mg twice 1. 25 to 2. 5 mg once 122. 7 mg/d 16. 6 mg/d ----32. 5 to 35. 0 mg/d ----- 20 mg twice ----- 10 mg once ----- 4 mg once ----- 2013 ACCF/AHA Guideline for the Management of Heart Failure
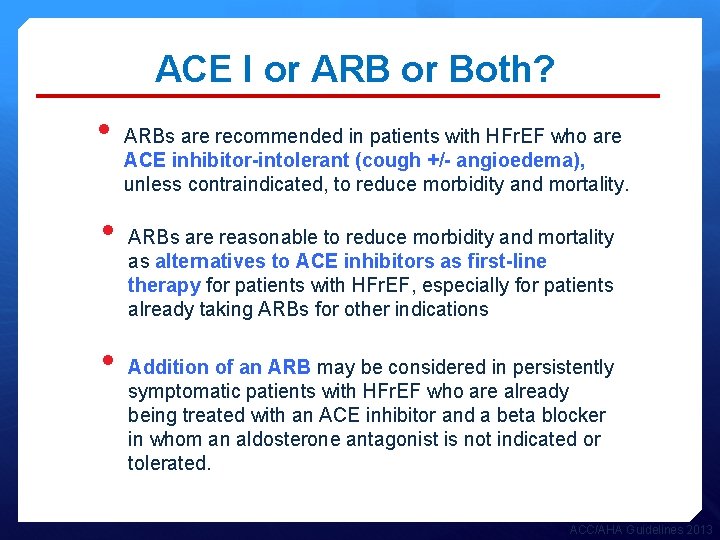
ACE I or ARB or Both? • • • ARBs are recommended in patients with HFr. EF who are ACE inhibitor-intolerant (cough +/- angioedema), unless contraindicated, to reduce morbidity and mortality. ARBs are reasonable to reduce morbidity and mortality as alternatives to ACE inhibitors as first-line therapy for patients with HFr. EF, especially for patients already taking ARBs for other indications Addition of an ARB may be considered in persistently symptomatic patients with HFr. EF who are already being treated with an ACE inhibitor and a beta blocker in whom an aldosterone antagonist is not indicated or tolerated. ACC/AHA Guidelines 2013
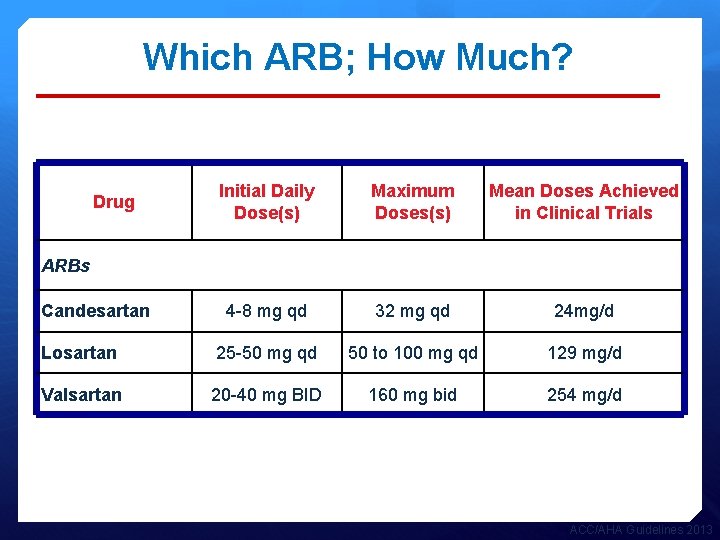
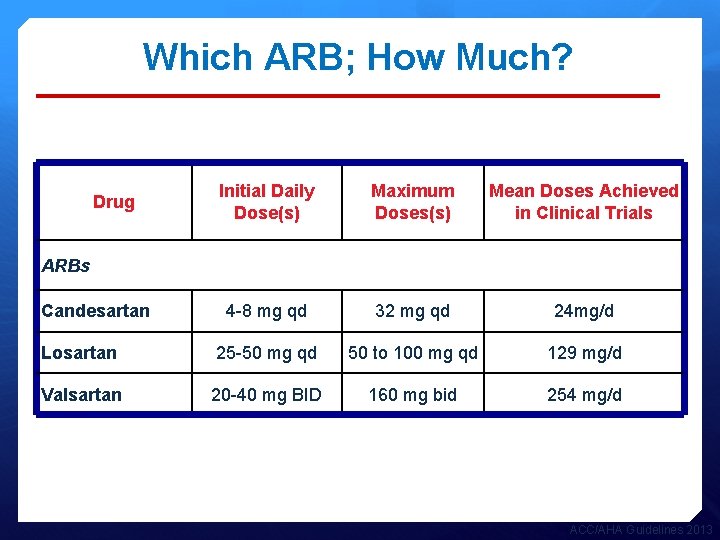
Which ARB; How Much? Initial Daily Dose(s) Maximum Doses(s) Mean Doses Achieved in Clinical Trials 4 -8 mg qd 32 mg qd 24 mg/d Losartan 25 -50 mg qd 50 to 100 mg qd 129 mg/d Valsartan 20 -40 mg BID 160 mg bid 254 mg/d Drug ARBs Candesartan ACC/AHA Guidelines 2013
![Aldosterone Antagonists Aldosterone receptor antagonists or mineralocorticoid receptor antagonists MRA are recommended Aldosterone Antagonists • • Aldosterone receptor antagonists [or mineralocorticoid receptor antagonists (MRA)] are recommended](https://slidetodoc.com/presentation_image/173846bb467e6df3f6f30e6f195be203/image-28.jpg)
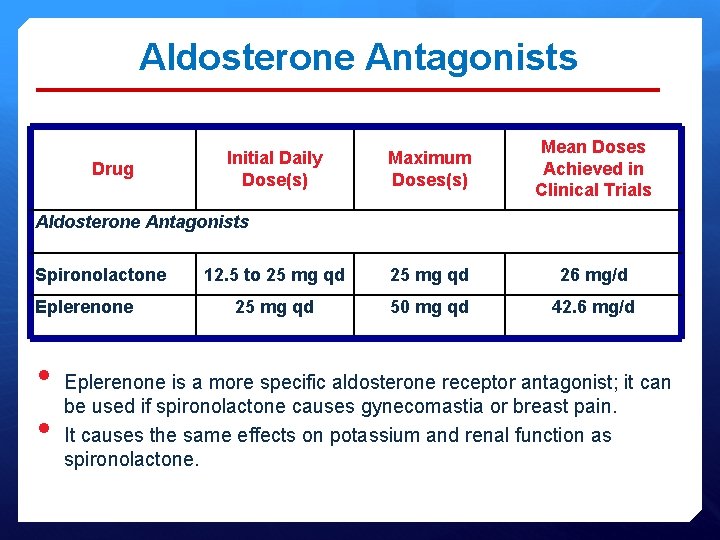
Aldosterone Antagonists • • Aldosterone receptor antagonists [or mineralocorticoid receptor antagonists (MRA)] are recommended in patients with NYHA class IIIV and who have LVEF of < 35%. Patients with NYHA class II should have a history of prior cardiovascular hospitalization or elevated plasma natriuretic peptide levels to be considered for aldosterone receptor antagonists. Creatinine should be < 2. 5 mg/d. L or less in men or < 2. 0 mg/d. L in women (or e. GFR >30 m. L/min/1. 73 m 2) and potassium < 5. 0 m. Eq/L. Careful monitoring of potassium, renal function, and diuretic dosing should be performed at initiation, within 7 -10 days after initiation and followed thereafter to minimize risk of hyperkalemia and renal insufficiency.
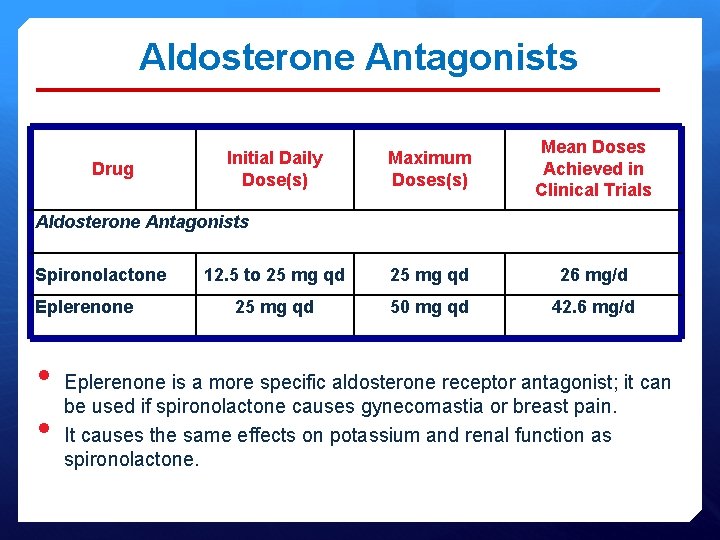
Aldosterone Antagonists Drug Maximum Doses(s) Mean Doses Achieved in Clinical Trials 12. 5 to 25 mg qd 26 mg/d 25 mg qd 50 mg qd 42. 6 mg/d Initial Daily Dose(s) Aldosterone Antagonists Spironolactone Eplerenone • • Eplerenone is a more specific aldosterone receptor antagonist; it can be used if spironolactone causes gynecomastia or breast pain. It causes the same effects on potassium and renal function as spironolactone.

Nitrate/Hydralazine (ISDN/HDZ) • HDZ/ISDN combincation is recommended for African Americans with NYHA class III–IV HFr. EF receiving optimal therapy with ACE inhibitors and beta blockers. • HDZ/ISDN can be useful to reduce morbidity or mortality in patients with current or prior symptomatic HFr. EF who cannot be given an ACE inhibitor or ARB because of drug intolerance, hypotension, or renal insufficiency, unless contraindicated.
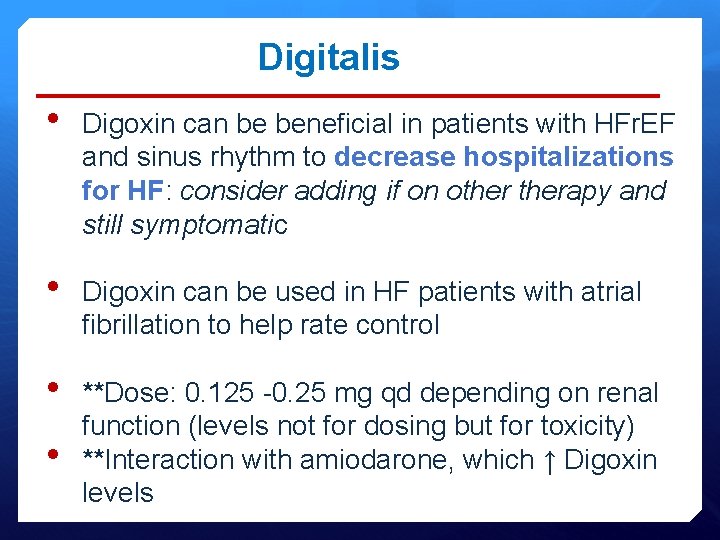
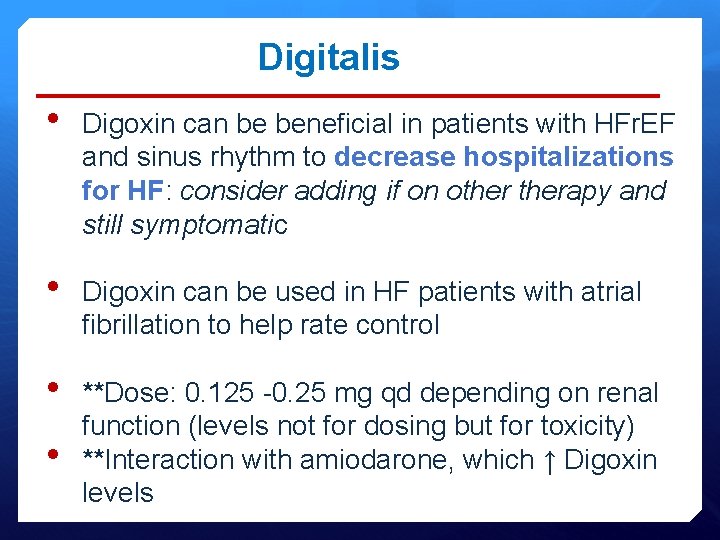
Digitalis • Digoxin can be beneficial in patients with HFr. EF and sinus rhythm to decrease hospitalizations for HF: consider adding if on otherapy and still symptomatic • Digoxin can be used in HF patients with atrial fibrillation to help rate control • **Dose: 0. 125 -0. 25 mg qd depending on renal function (levels not for dosing but for toxicity) **Interaction with amiodarone, which ↑ Digoxin levels •
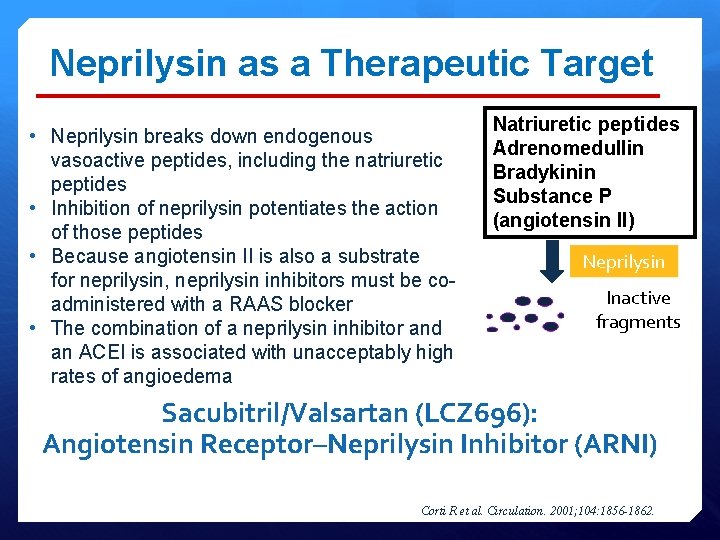
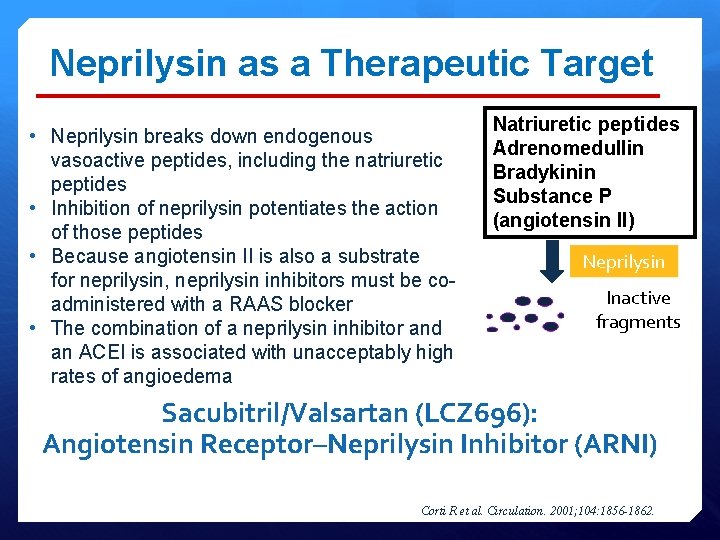
Neprilysin as a Therapeutic Target • Neprilysin breaks down endogenous vasoactive peptides, including the natriuretic peptides • Inhibition of neprilysin potentiates the action of those peptides • Because angiotensin II is also a substrate for neprilysin, neprilysin inhibitors must be coadministered with a RAAS blocker • The combination of a neprilysin inhibitor and an ACEI is associated with unacceptably high rates of angioedema Natriuretic peptides Adrenomedullin Bradykinin Substance P (angiotensin II) Neprilysin Inactive fragments Sacubitril/Valsartan (LCZ 696): Angiotensin Receptor–Neprilysin Inhibitor (ARNI) Corti R et al. Circulation. 2001; 104: 1856 -1862.

PARADIGM-HF: CV Death or HF Hospitalization (Primary Endpoint) 1. Mc. Murray JJ et al. N Engl J Med. 2014; 371: 993 -1004

SHIFT Trial Primary Composite Endpoint: CV Death or Hospitalization for Worsening HF Swedberg K et al. Lancet. 2010; 376: 875 -885.
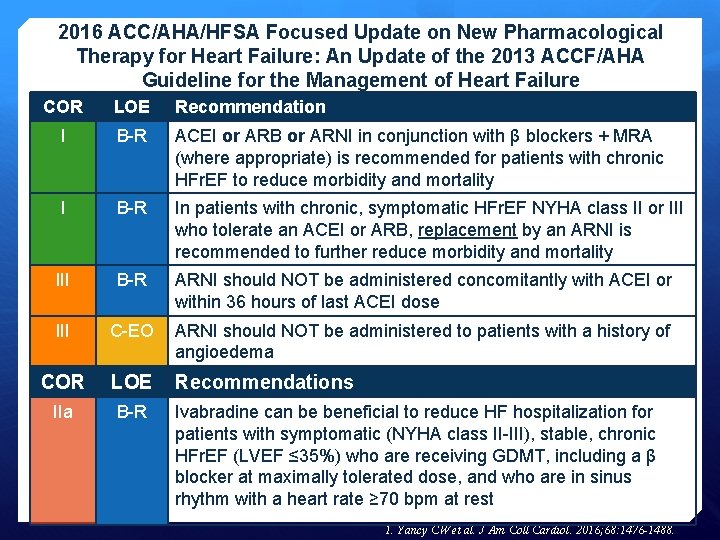
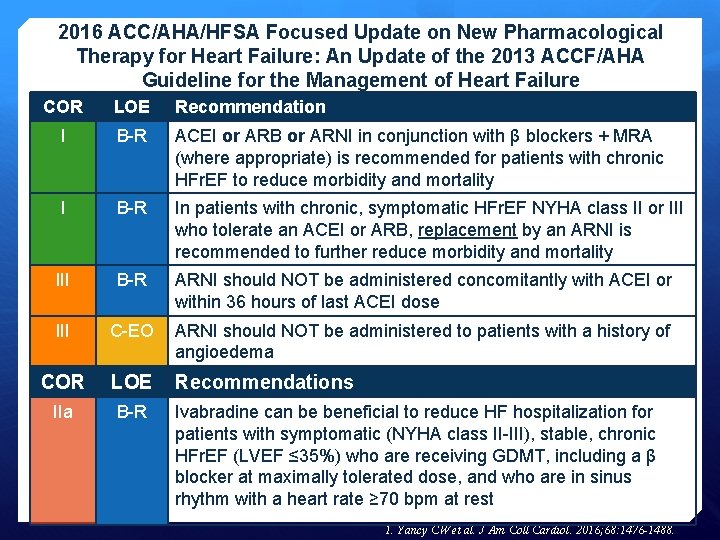
2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure COR LOE Recommendation I B-R ACEI or ARB or ARNI in conjunction with β blockers + MRA (where appropriate) is recommended for patients with chronic HFr. EF to reduce morbidity and mortality I B-R In patients with chronic, symptomatic HFr. EF NYHA class II or III who tolerate an ACEI or ARB, replacement by an ARNI is recommended to further reduce morbidity and mortality III B-R ARNI should NOT be administered concomitantly with ACEI or within 36 hours of last ACEI dose III C-EO ARNI should NOT be administered to patients with a history of angioedema COR LOE Recommendations IIa B-R Ivabradine can be beneficial to reduce HF hospitalization for patients with symptomatic (NYHA class II-III), stable, chronic HFr. EF (LVEF ≤ 35%) who are receiving GDMT, including a β blocker at maximally tolerated dose, and who are in sinus rhythm with a heart rate ≥ 70 bpm at rest 1. Yancy CW et al. J Am Coll Cardiol. 2016; 68: 1476 -1488.
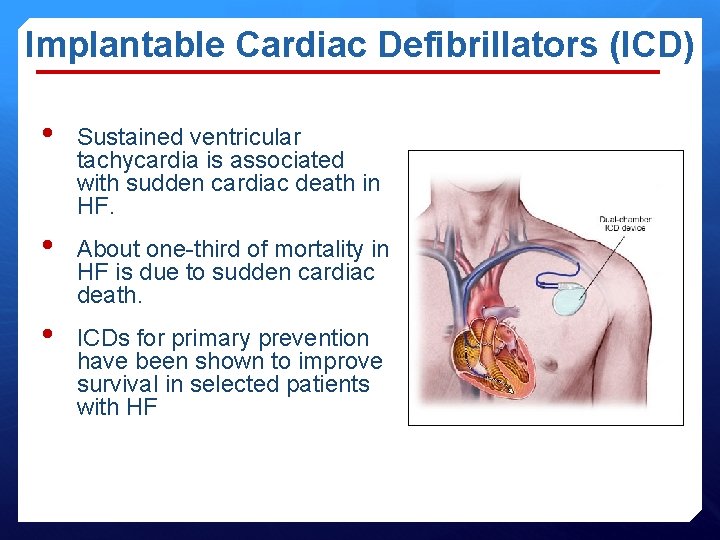
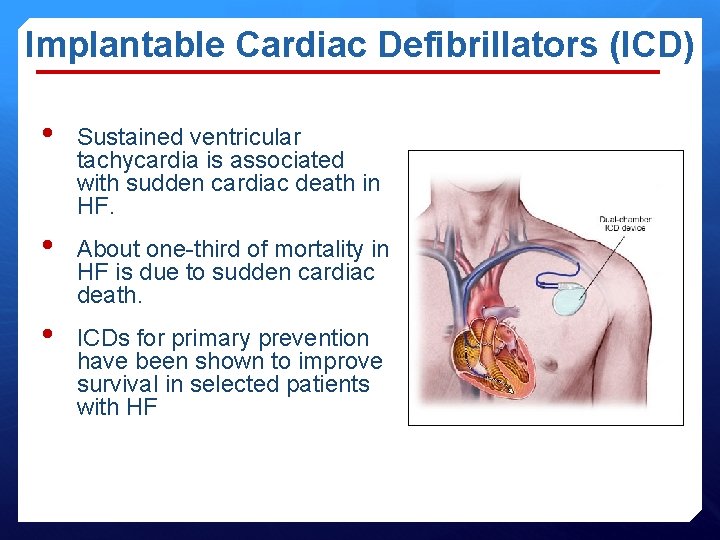
Implantable Cardiac Defibrillators (ICD) • Sustained ventricular tachycardia is associated with sudden cardiac death in HF. • About one-third of mortality in HF is due to sudden cardiac death. • ICDs for primary prevention have been shown to improve survival in selected patients with HF
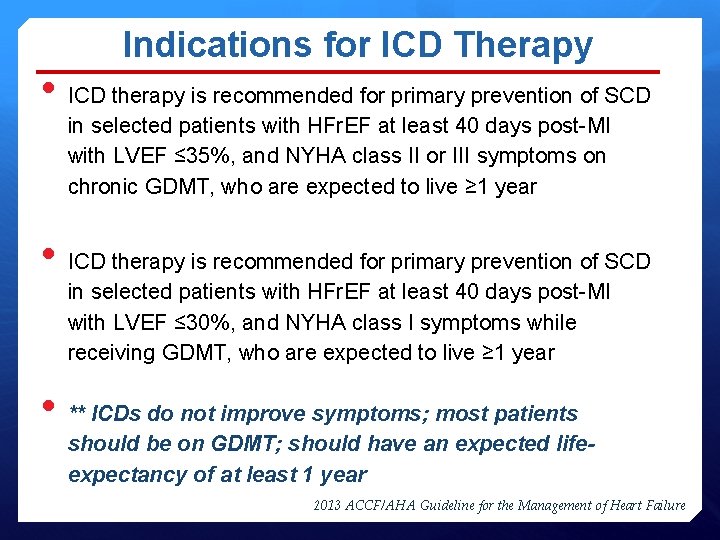
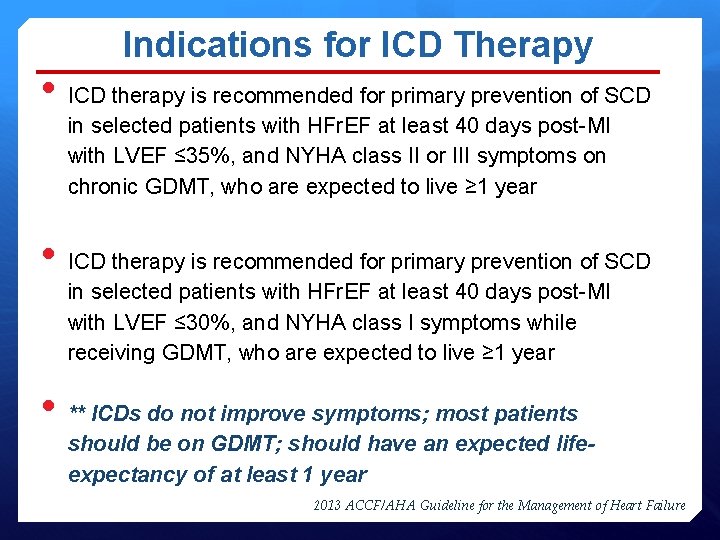
Indications for ICD Therapy • ICD therapy is recommended for primary prevention of SCD in selected patients with HFr. EF at least 40 days post-MI with LVEF ≤ 35%, and NYHA class II or III symptoms on chronic GDMT, who are expected to live ≥ 1 year • ICD therapy is recommended for primary prevention of SCD in selected patients with HFr. EF at least 40 days post-MI with LVEF ≤ 30%, and NYHA class I symptoms while receiving GDMT, who are expected to live ≥ 1 year • ** ICDs do not improve symptoms; most patients should be on GDMT; should have an expected lifeexpectancy of at least 1 year 2013 ACCF/AHA Guideline for the Management of Heart Failure

Cardiac Resynchronization Pacing: Consequences of a Prolonged QRS Delayed Ventricular Activation Sinus node AV node Conduction block Delayed lateral wall contraction Disorganized ventricular contraction Decreased pumping efficiency Reduction in diastolic filling times Prolongation of the duration of mitral regurgitation
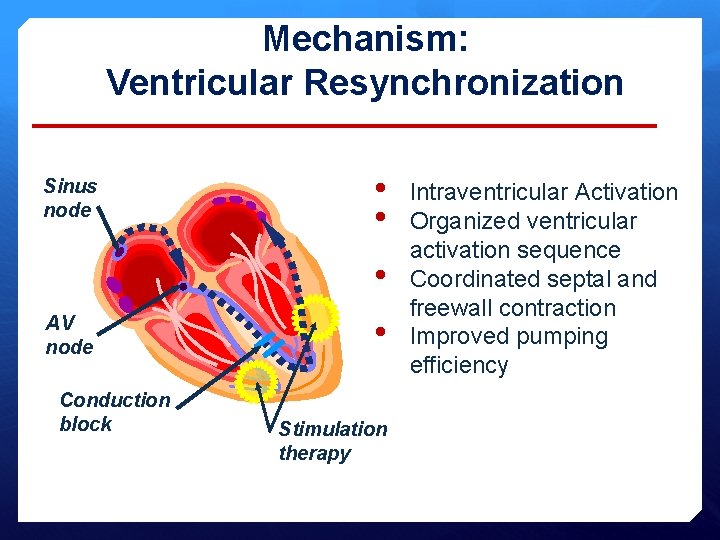
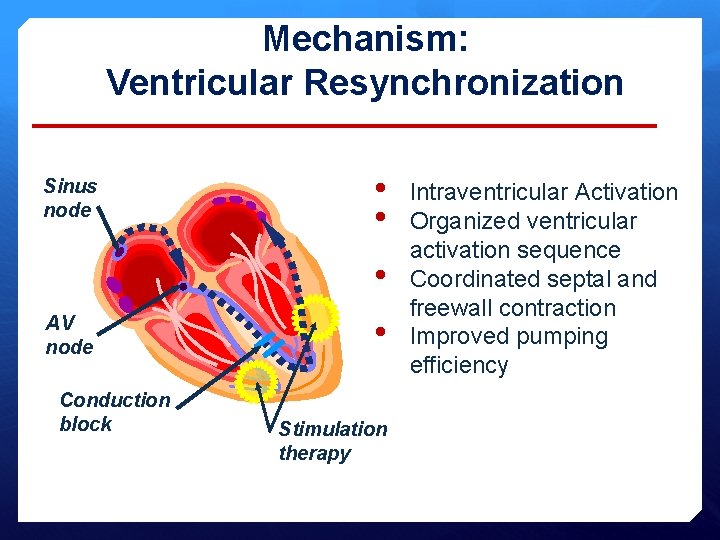
Mechanism: Ventricular Resynchronization Sinus node • • • AV node Conduction block • Stimulation therapy Intraventricular Activation Organized ventricular activation sequence Coordinated septal and freewall contraction Improved pumping efficiency
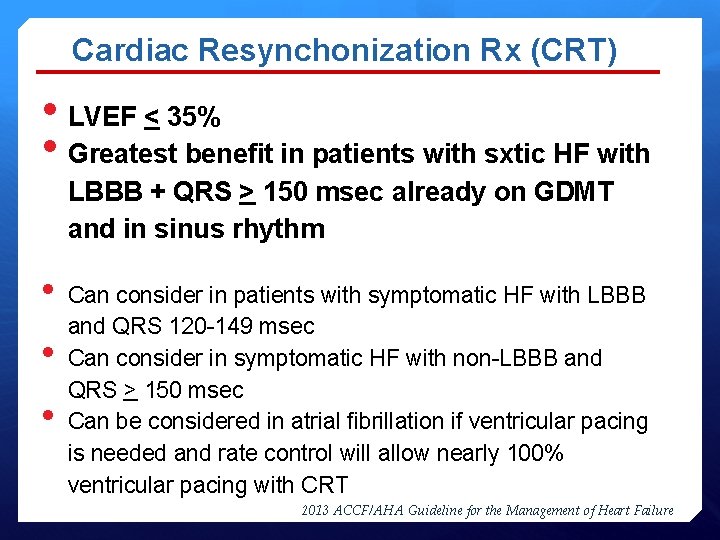
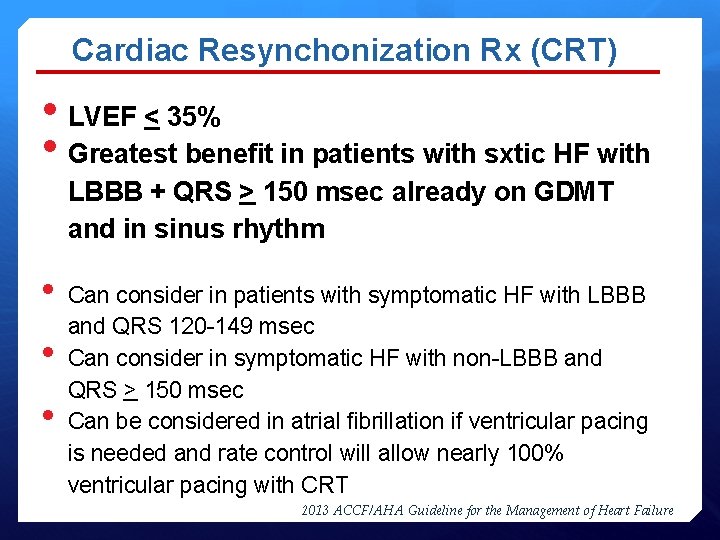
Cardiac Resynchonization Rx (CRT) • LVEF < 35% • Greatest benefit in patients with sxtic HF with LBBB + QRS > 150 msec already on GDMT and in sinus rhythm • • • Can consider in patients with symptomatic HF with LBBB and QRS 120 -149 msec Can consider in symptomatic HF with non-LBBB and QRS > 150 msec Can be considered in atrial fibrillation if ventricular pacing is needed and rate control will allow nearly 100% ventricular pacing with CRT 2013 ACCF/AHA Guideline for the Management of Heart Failure

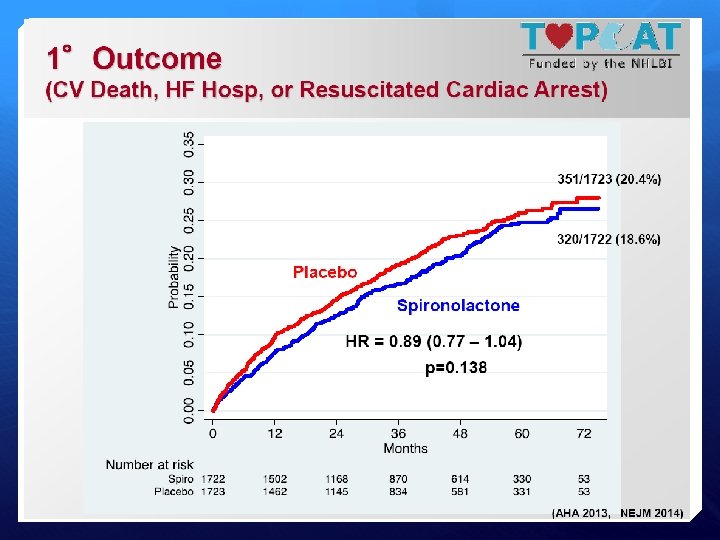
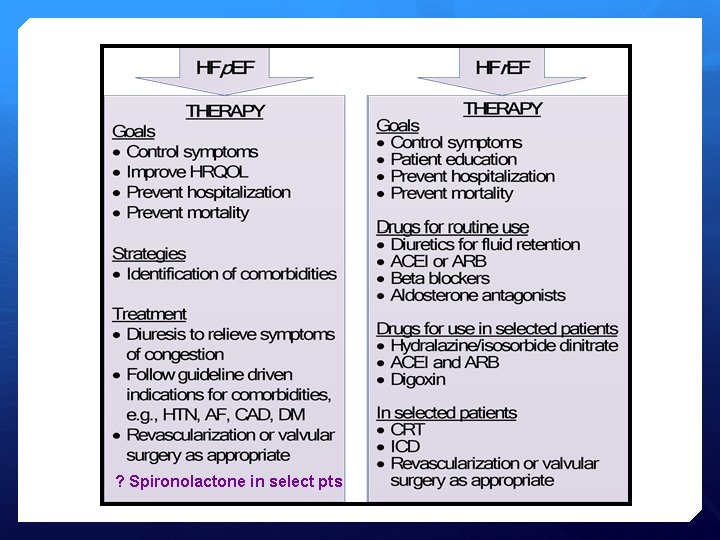
HFp. EF • • • Trials have not shown significant mortality or morbidity benefit with use of ACEI/ARB specifically in HFp. EF No trials showing definite benefit of Beta blockers, sildenafil TOPCAT trial: Randomizeddouble blind trial of spironolactone (15 -45 mg) vs. placebo in HFp. EF patients (LVEF >45%) with • Prior HF hospitalization or • BNP > 100 pg/ml
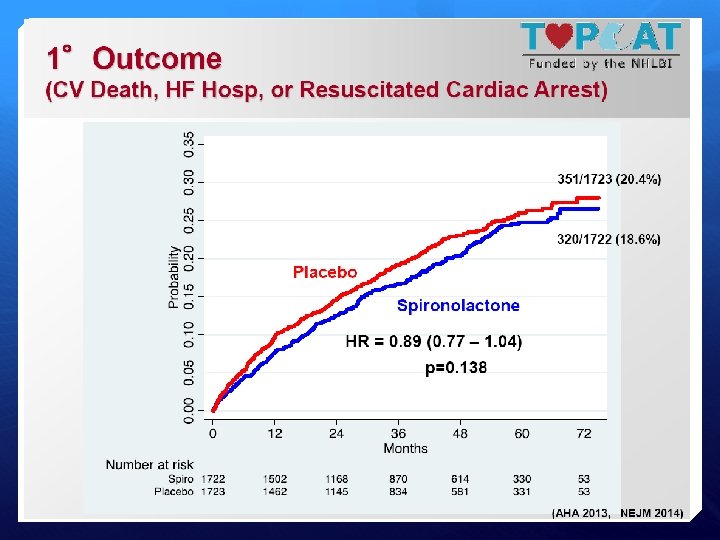

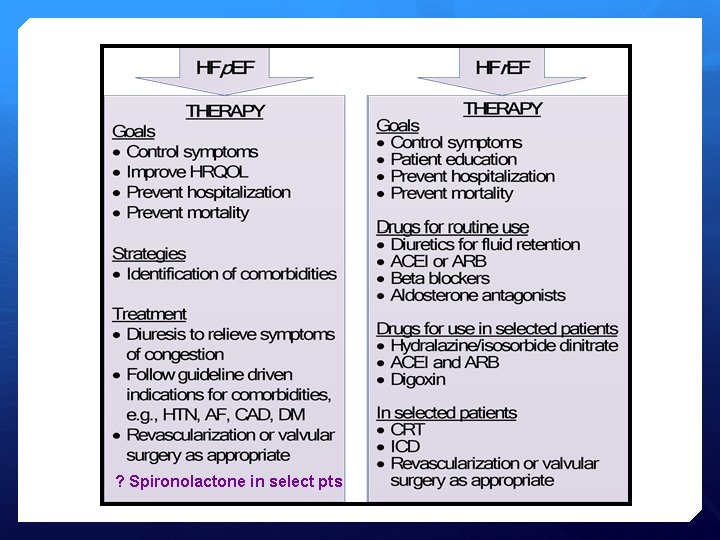
? Spironolactone in select pts
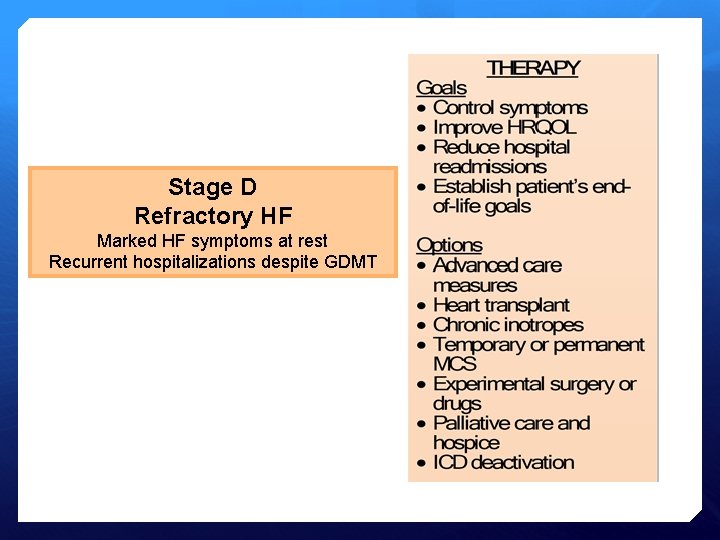
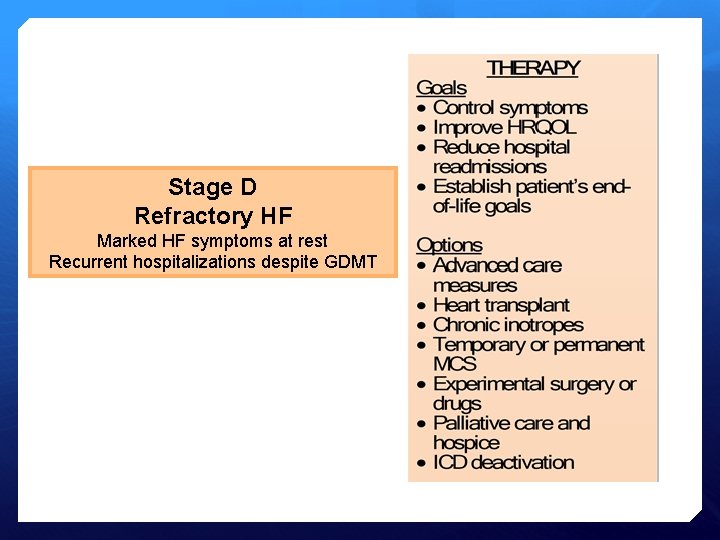
Stage D Refractory HF Marked HF symptoms at rest Recurrent hospitalizations despite GDMT
Summary • Definition of HF • Magnitude of the problem • Symptoms & Signs of HF • Types of HF: HFp. EF & HFr. EF • Stages of HF and NYHA Functional Classification of HF • Management of Patients with HF: Initial work up Medical therapy Device Therapy
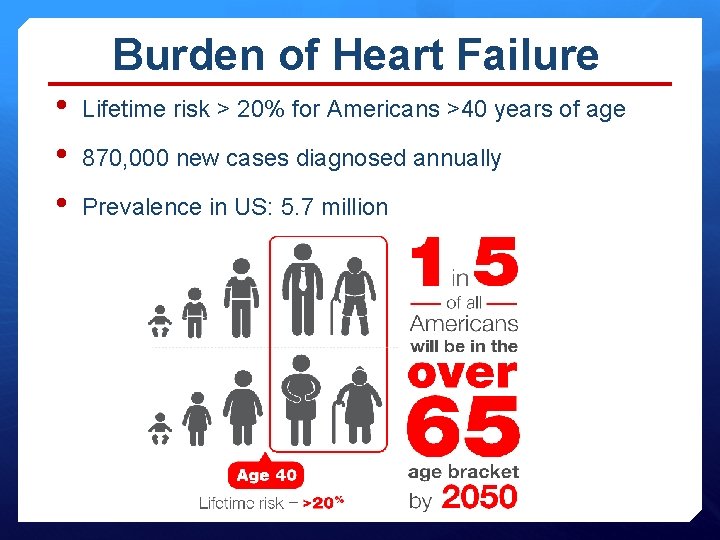
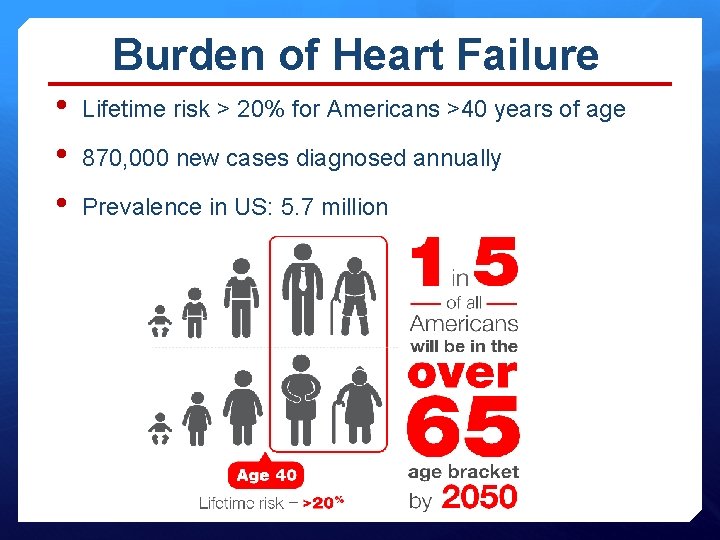
Burden of Heart Failure • • • Lifetime risk > 20% for Americans >40 years of age 870, 000 new cases diagnosed annually Prevalence in US: 5. 7 million
 Nidhi deswal
Nidhi deswal Failure to sense
Failure to sense Supparerk vision center
Supparerk vision center Brittle fracture examples
Brittle fracture examples Chapter 24 heart failure drugs
Chapter 24 heart failure drugs All people enjoy time magazine
All people enjoy time magazine Lvedp normal range
Lvedp normal range Donkey analogy heart failure
Donkey analogy heart failure Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Vetsulin dosage chart for dogs
Vetsulin dosage chart for dogs Heart failure
Heart failure Acute vs chronic heart failure
Acute vs chronic heart failure Heart failure definition
Heart failure definition Cor pulmonale
Cor pulmonale Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Diabetes and heart failure
Diabetes and heart failure Congestive heart failure zones for management
Congestive heart failure zones for management Heart failure definition
Heart failure definition Right vs left-sided heart failure chart
Right vs left-sided heart failure chart Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Heart failure complications
Heart failure complications Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Keith rn heart failure case study
Keith rn heart failure case study Lmnop heart failure
Lmnop heart failure Causes of cardiomegaly in child
Causes of cardiomegaly in child Heart failure forward vs backward
Heart failure forward vs backward Goat heart dissection
Goat heart dissection Hrt 2 hrt
Hrt 2 hrt Right border of the relative cardiac dullness is formed by
Right border of the relative cardiac dullness is formed by Anita āboliņa
Anita āboliņa Anita fletcher
Anita fletcher Anita roman morra
Anita roman morra Anita archer quotes
Anita archer quotes Anita krueger md
Anita krueger md Anita roddick leadership style
Anita roddick leadership style Anita forsyth
Anita forsyth Myeloma euronet
Myeloma euronet Anita d'souza md
Anita d'souza md Johanna koti porvoo
Johanna koti porvoo Anita malfatti a boba
Anita malfatti a boba Anita lilian zuppo abed
Anita lilian zuppo abed Reported speech verbs
Reported speech verbs Anita gudelj
Anita gudelj Após estudar na europa anita malfatti retornou ao brasil
Após estudar na europa anita malfatti retornou ao brasil Anita ravi md
Anita ravi md Annina studer
Annina studer Veres anita
Veres anita Anita walz
Anita walz Gradia wilma inschool
Gradia wilma inschool