Pulmonary Edema Acute systolic heart failure is useful








- Slides: 58
Pulmonary Edema “Acute systolic heart failure” is useful for hospital billing, but pulmonary edema is more descriptive.
Pulmonary Edema Learning Goals n Management of symptomatic pulmonary edema n Management of cardiogenic shock n Not in this talk: Chronic outpatient systolic and diastolic failure
Case #1 n 72 W with dilated ischemic cardiomyopathy, EF=45 %, presents to the ED after waking up at 2 am from shortness of breath. n It is now 6 days after Thanksgiving; “I didn’t eat any salt, ” but she admits to eating canned gravy and canned cranberry sauce
Case #1, HPI, continued n Notes worsening in ankle swelling and worsened orthopnea n Baseline ET 2 blocks, now 20 feet limited by dyspnea; denies chest pain n Usually she makes copious urine after taking furosemide, but had almost no urine output after yesterday’s dose
Case #1, ROS, continued n Denies lightheadedness and syncope n Notes a new decrease in appetite; on further questioning she still feels hungry and wants to eat, but feels full after only 2 -3 bites of food
72 W DICM, ate too much salt PMH: HTN, DM, CAD, CHF n PSH: Cath one year ago showed chronic total occlusion of mid LAD; no other severe lesions on cath; no intervention performed n Medications: Lisinopril 10 mg PO daily Carvedilol 12. 5 mg PO bid Furosemide 40 mg PO daily ASA 81, Simvastatin 40, Insulin n
72 W DICM, ate too much salt n NKDA n Social: Quit tobacco one year ago, drinks 1 -2 8 oz glasses of wine per week, denies drug use Lives next door to her daughter and grandchildren, weighs herself and checks her BP at home daily n Family: Father died age 63 of MI

72 W DICM, ate too much salt n 150/90 P 82 R 28 Sp. O 2=93% 2 L T=98. 4 n Weight is 62 kg; baseline is 57 kg n Jugular venous pressure 12 cm. H 2 O n Crackles to mid lung fields bilaterally n RRR, II/VI apical holosystolic murmur n Bilateral pitting ankle edema; extremities warm

72 W DICM, ate too much salt n CBC normal, coags normal n Na=129 K=4. 9 BUN=18 Cre=1. 1 n Albumin=3. 6, LFT’s otherwise normal n EKG shows normal sinus rhythm, left atrial enlargement, left ventricular hypertrophy, and poor R-wave progression, all unchanged from routine EKG taken three months ago
Chest X-Ray

72 W pulmonary edema ED Course n Receives furosemide 40 mg IV once, makes 1. 5 L urine n Reports complete resolution of her shortness of breath; now feels normal n BP 130/80 P 80 R 21 Sp. O 2=98% 2 L n JVP=10; ankle edema persists
72 W pulmonary edema What to do next? n Emergent cardiac catheterization n Transfer to CCU, consider inotropes n Admit to telemetry, rule out MI n Discharge home with close clinic f/u
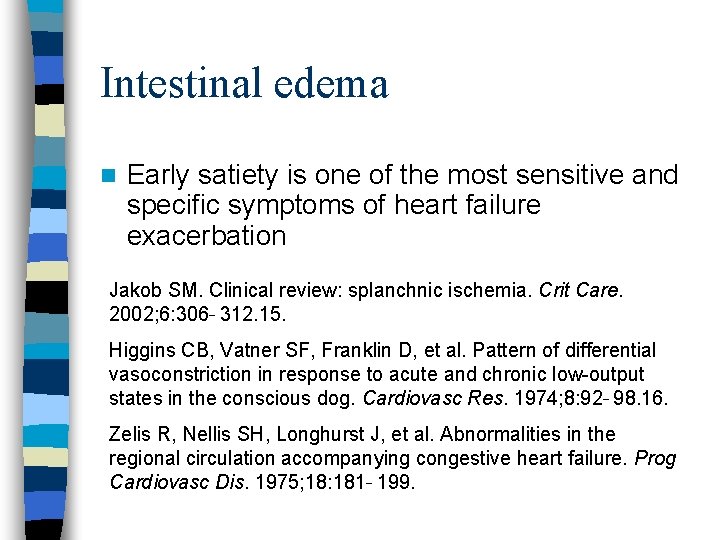
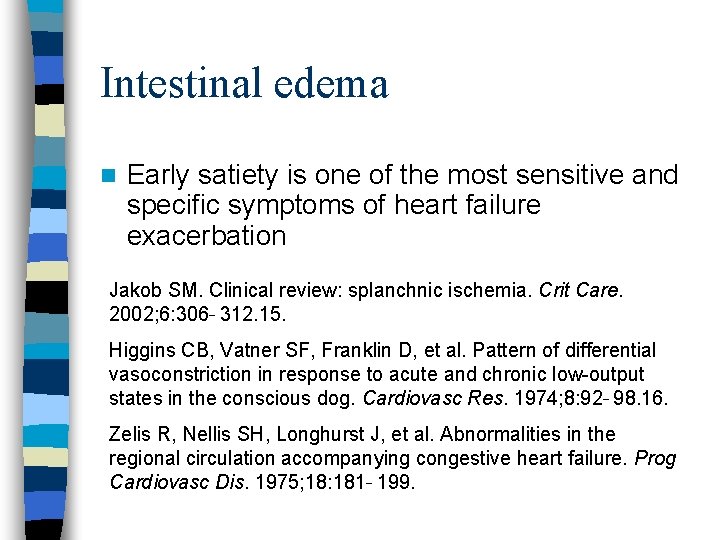
Intestinal edema n Early satiety is one of the most sensitive and specific symptoms of heart failure exacerbation Jakob SM. Clinical review: splanchnic ischemia. Crit Care. 2002; 6: 306 312. 15. Higgins CB, Vatner SF, Franklin D, et al. Pattern of differential vasoconstriction in response to acute and chronic low-output states in the conscious dog. Cardiovasc Res. 1974; 8: 92 98. 16. Zelis R, Nellis SH, Longhurst J, et al. Abnormalities in the regional circulation accompanying congestive heart failure. Prog Cardiovasc Dis. 1975; 18: 181 199.
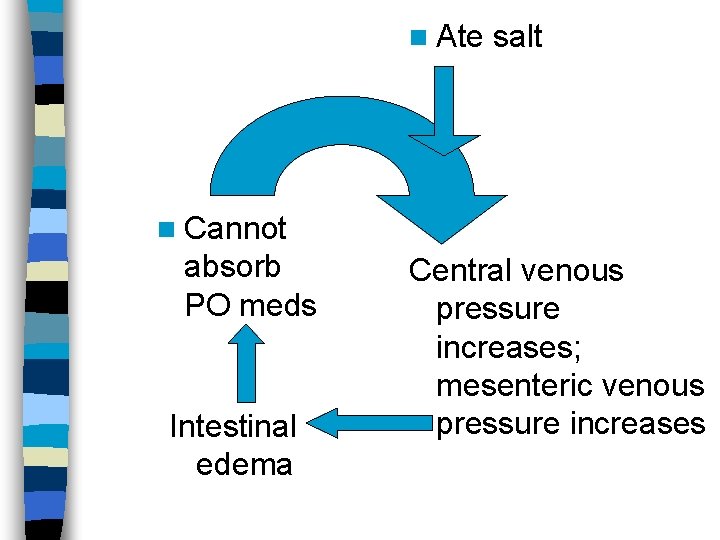
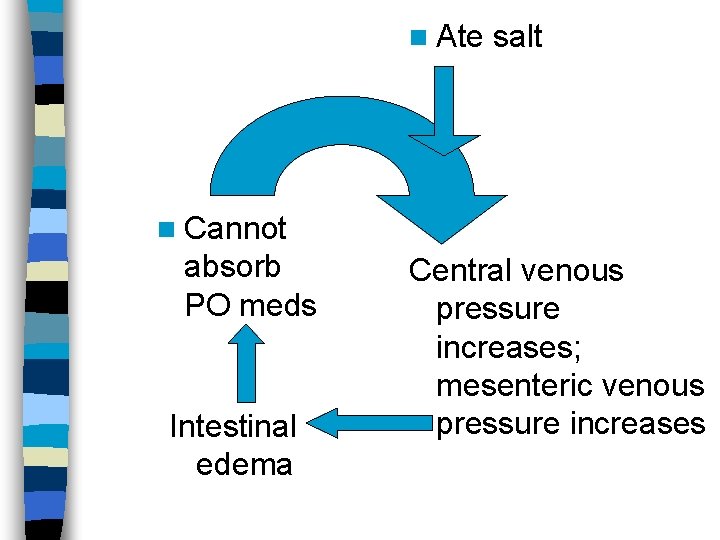
n Ate salt n Cannot absorb PO meds Intestinal edema Central venous pressure increases; mesenteric venous pressure increases
72 W pulmonary edema What to do next? n Emergent cardiac catheterization n Transfer to CCU, consider inotropes n Admit to telemetry, rule out MI n Discharge home with close clinic f/u And increase furosemide dose from 40 mg PO daily to 80 mg PO bid for five days; instruct pt. to return to clinic immediately if weight fails to return to baseline
72 W pulmonary edema What to do next? n Emergent cardiac catheterization n Transfer to CCU, consider inotropes n Admit to telemetry, rule out MI n Discharge home with close clinic f/u “This is not a heart failure exacerbation, it’s Lasix deficiency syndrome. ”
Case #2 n 71 W with a one-year history of asthma treatment from a community physician, presents to the ED after waking up at 2 am with shortness of breath.
Case #2, HPI, continued n Often awakens in the middle of the night; gets up and takes albuterol, usually feels good enough to go back to sleep n Baseline ET 1 block, now has dyspnea at rest; denies chest pain n Sometimes feels lightheadedness and palpitation after taking albuterol
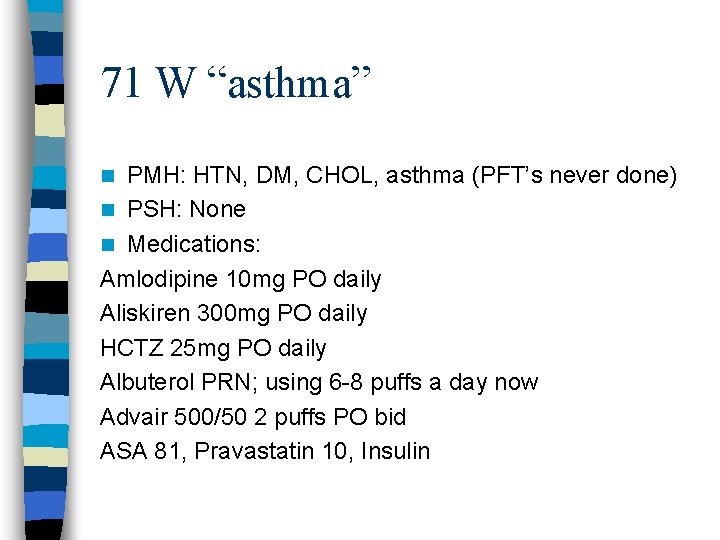
71 W “asthma” PMH: HTN, DM, CHOL, asthma (PFT’s never done) n PSH: None n Medications: Amlodipine 10 mg PO daily Aliskiren 300 mg PO daily HCTZ 25 mg PO daily Albuterol PRN; using 6 -8 puffs a day now Advair 500/50 2 puffs PO bid ASA 81, Pravastatin 10, Insulin n
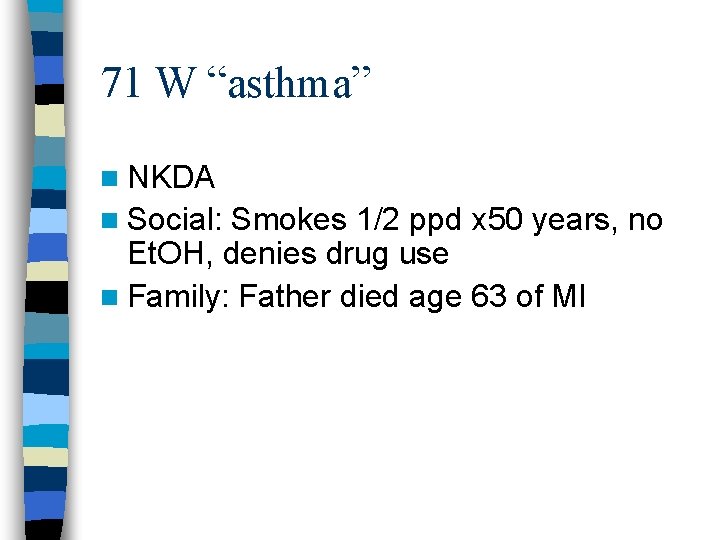
71 W “asthma” n NKDA n Social: Smokes 1/2 ppd x 50 years, no Et. OH, denies drug use n Family: Father died age 63 of MI
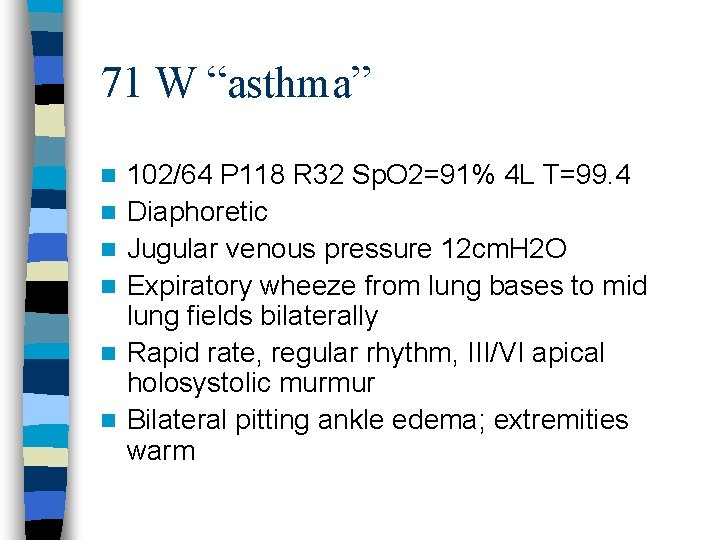
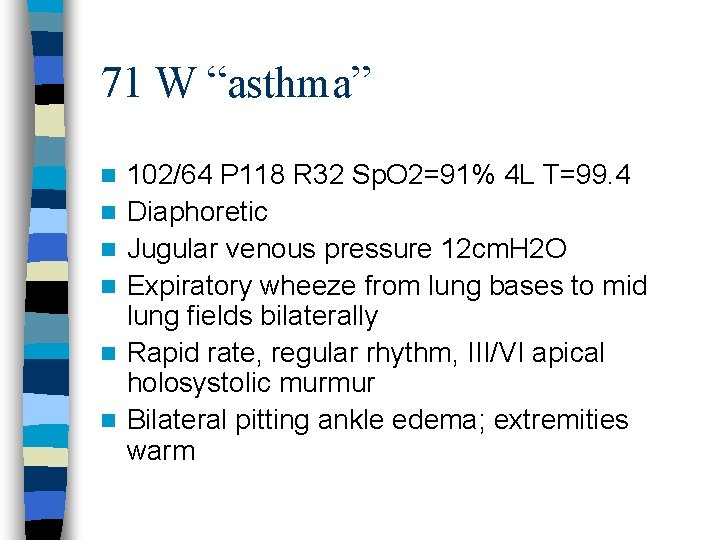
71 W “asthma” n n n 102/64 P 118 R 32 Sp. O 2=91% 4 L T=99. 4 Diaphoretic Jugular venous pressure 12 cm. H 2 O Expiratory wheeze from lung bases to mid lung fields bilaterally Rapid rate, regular rhythm, III/VI apical holosystolic murmur Bilateral pitting ankle edema; extremities warm

71 W “asthma” n Labs drawn; results pending n EKG shows sinus tachycardia, left atrial enlargement, left ventricular hypertrophy with ST-T changes that could be due to hypertrophy or ischemia, and poor Rwave progression No prior EKG for comparison

Chest X-Ray

71 W pulmonary edema ED Course n “Doctor. Please help me. (Gasp. ) I feel terrible. ” n What do you do?
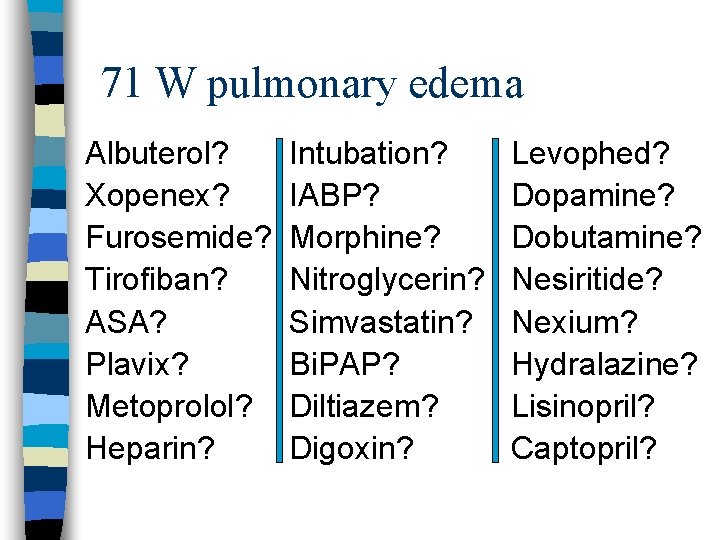
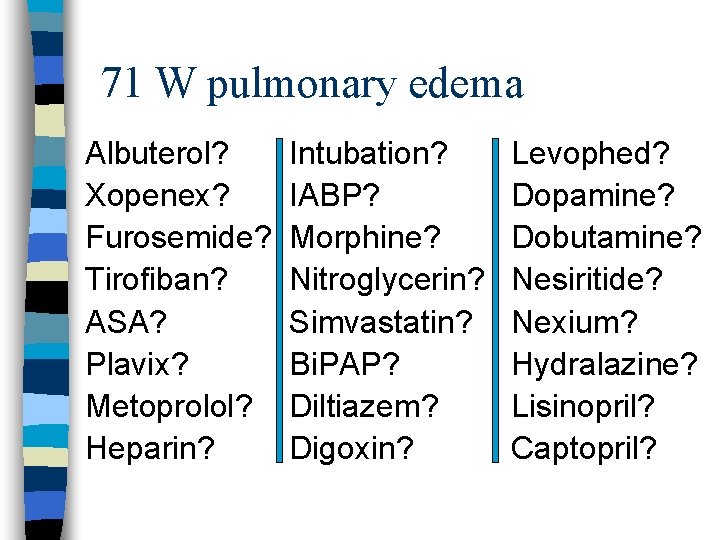
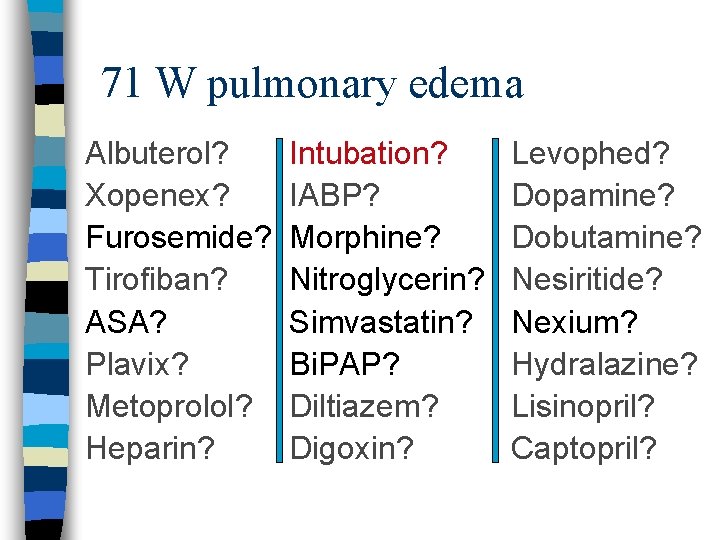
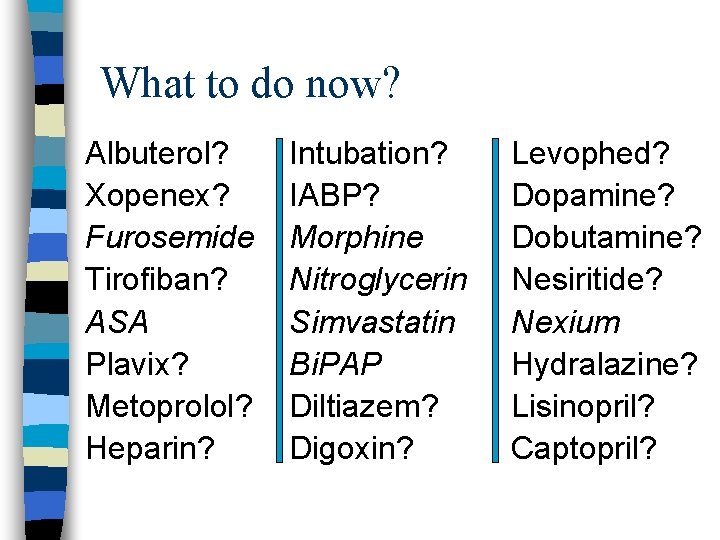
71 W pulmonary edema Albuterol? Xopenex? Furosemide? Tirofiban? ASA? Plavix? Metoprolol? Heparin? Intubation? IABP? Morphine? Nitroglycerin? Simvastatin? Bi. PAP? Diltiazem? Digoxin? Levophed? Dopamine? Dobutamine? Nesiritide? Nexium? Hydralazine? Lisinopril? Captopril?
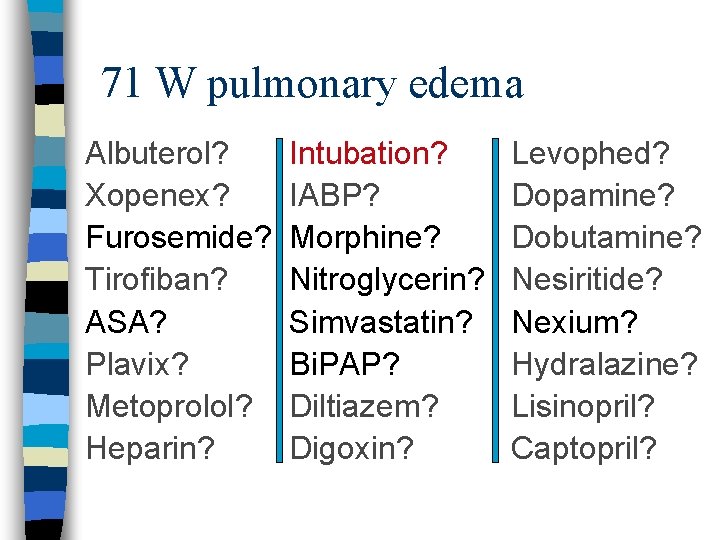
71 W pulmonary edema Albuterol? Xopenex? Furosemide? Tirofiban? ASA? Plavix? Metoprolol? Heparin? Intubation? IABP? Morphine? Nitroglycerin? Simvastatin? Bi. PAP? Diltiazem? Digoxin? Levophed? Dopamine? Dobutamine? Nesiritide? Nexium? Hydralazine? Lisinopril? Captopril?
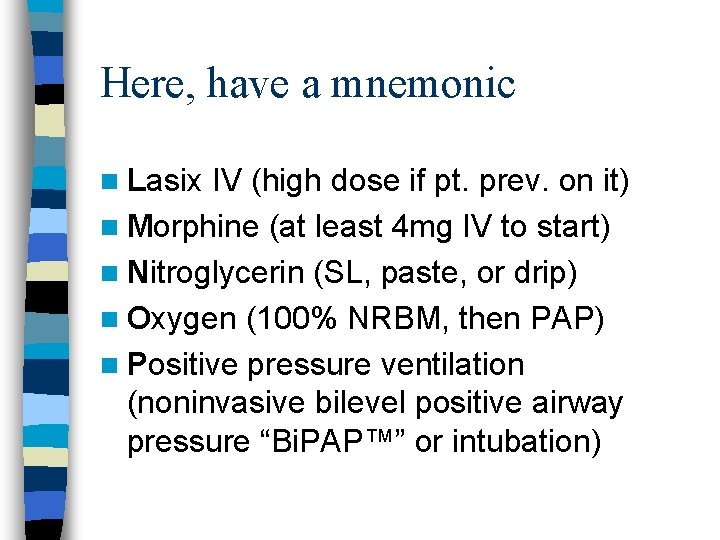
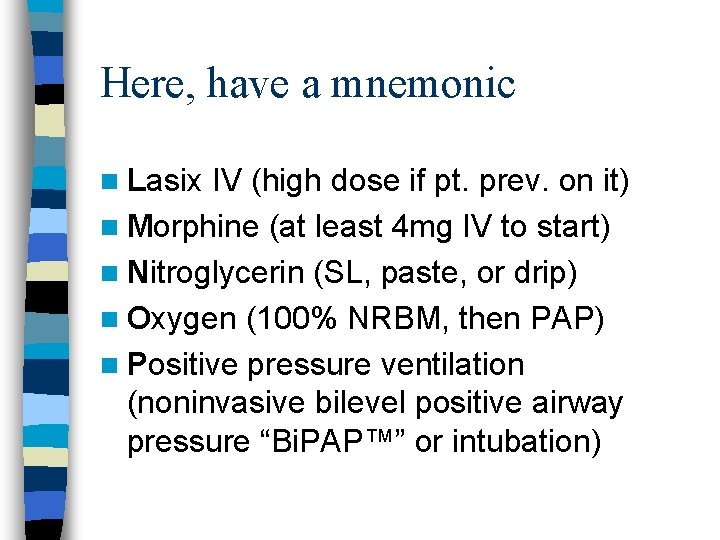
Here, have a mnemonic n Lasix IV (high dose if pt. prev. on it) n Morphine (at least 4 mg IV to start) n Nitroglycerin (SL, paste, or drip) n Oxygen (100% NRBM, then PAP) n Positive pressure ventilation (noninvasive bilevel positive airway pressure “Bi. PAP™” or intubation)
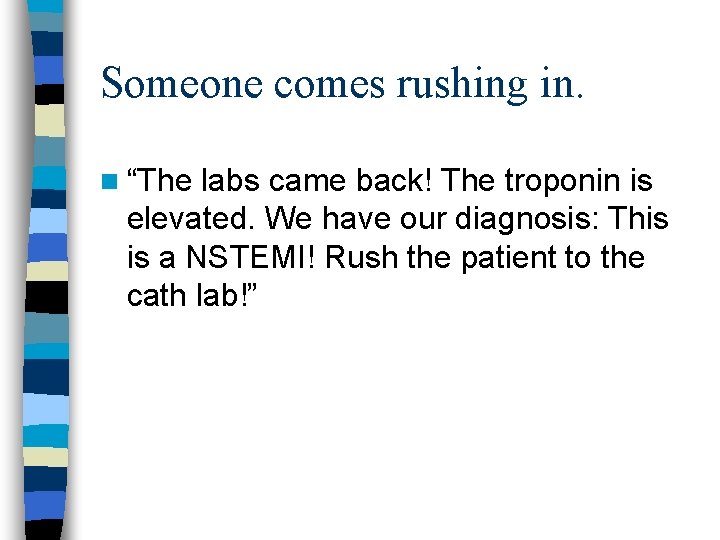
Someone comes rushing in. n “The labs came back! The troponin is elevated. We have our diagnosis: This is a NSTEMI! Rush the patient to the cath lab!”
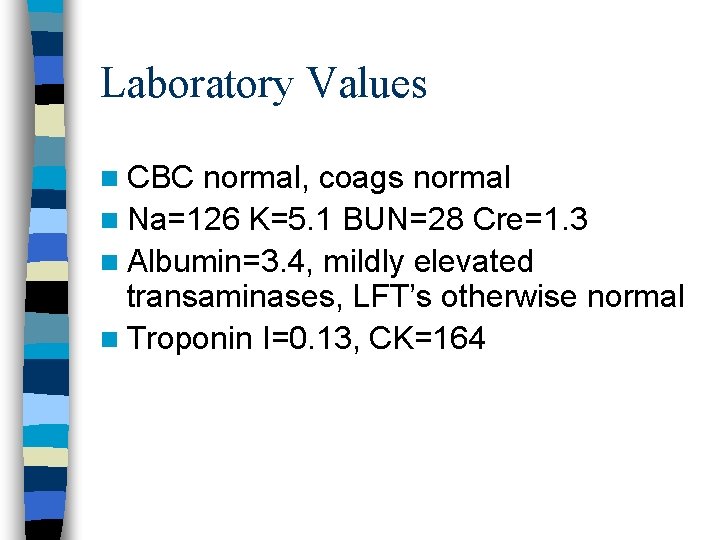
Laboratory Values n CBC normal, coags normal n Na=126 K=5. 1 BUN=28 Cre=1. 3 n Albumin=3. 4, mildly elevated transaminases, LFT’s otherwise normal n Troponin I=0. 13, CK=164
Physical examination now 98/62 P 96 R 26 Sp. O 2=99% on Bilevel PAP set at IPAP=10, EPAP=5, Fi. O 2=60% n Diaphoretic n Bilateral pitting ankle edema; extremities warm n
Yikes! We have troponin! You shout: “Are you having any chest discomfort at all? ” She shakes her head no. “How is your breathing? ” She indicates through the mask that she is starting to feel better. n Repeat EKG shows normal sinus rhythm, otherwise unchanged (LVH, LAE, ST-T wave changes of hypertrophy or ischemia) n
72 W pulmonary edema What to do next? n Emergent cardiac catheterization n Transfer to CCU, consider inotropes n Admit to telemetry, continue LMNOP n Call the cardiology fellow to ask “Should we give heparin? ”
Pt. goes to the CCU: Best case n Pt. continues to feel better with repeat furosemide dosing. Blood pressure improves. Stops Bi. PAP. Echo shows EF=35%, mod MR. Weight drops 4 kg in two days; edema resolves. Cardiac catheterization two days later shows chronic total occlusion of mid LAD. No other significant lesions noted.
Best case scenario, continued n Pt. sent home on ACE, beta blocker, diuretic, statin, aspirin, insulin. Quits smoking. Fires her old internist and chooses a physician at Jacobi’s internal medicine continuity clinic. Echo 3 months later shows EF=45%, mild MR. Doesn’t go to the ED again until shortly after Thanksgiving of the following year.

The worst outcome n Pulmonary edema is not treated promptly. Patient has RR=44, Sp. O 2=89%, then starts to become lethargic. n Intubated for hypoxic respiratory failure. n (After all, intubation is the ultimate form of positive pressure ventilation. )
Why this is bad n This is not bad because of the patient’s long-term prognosis--it’s bad because we physicians failed the patient. n This patient can still recover and turn out just as well as in the best-case scenario long-term (so long as she doesn’t develop ventilator complications). She just had to suffer needlessly to get there.
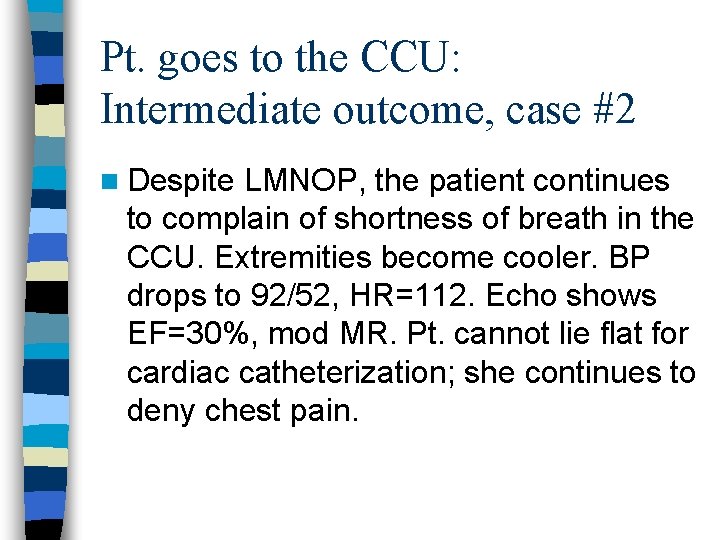
Pt. goes to the CCU: Intermediate outcome, case #2 n Despite LMNOP, the patient continues to complain of shortness of breath in the CCU. Extremities become cooler. BP drops to 92/52, HR=112. Echo shows EF=30%, mod MR. Pt. cannot lie flat for cardiac catheterization; she continues to deny chest pain.
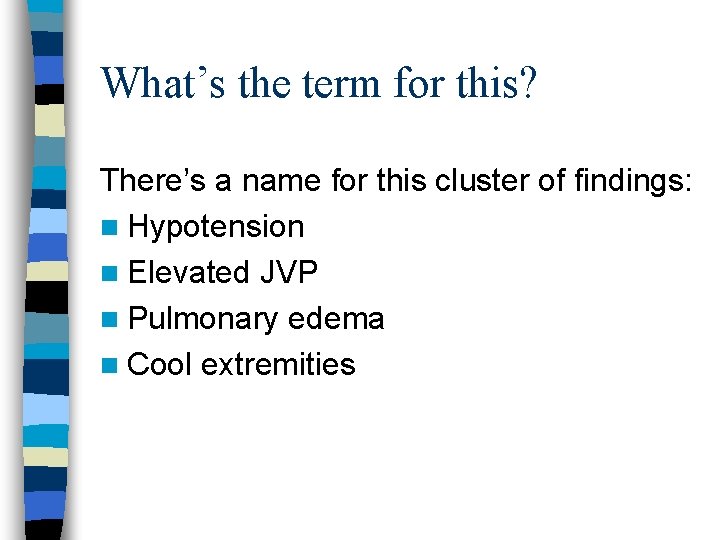
What’s the term for this? There’s a name for this cluster of findings: n Hypotension n Elevated JVP n Pulmonary edema n Cool extremities
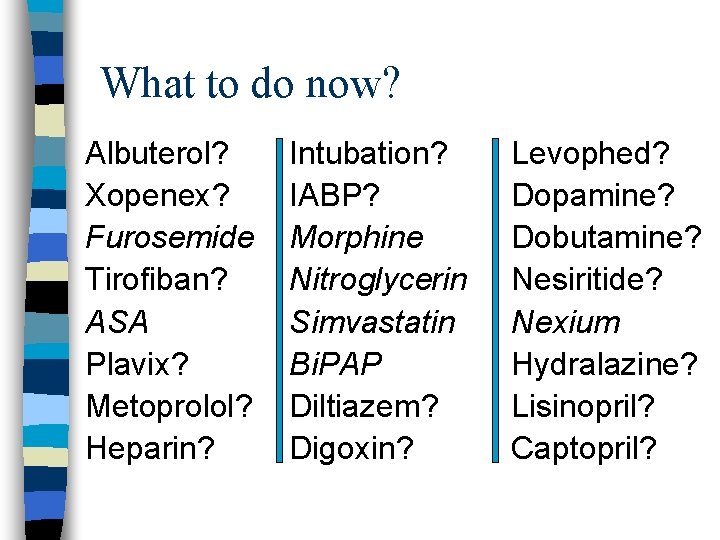
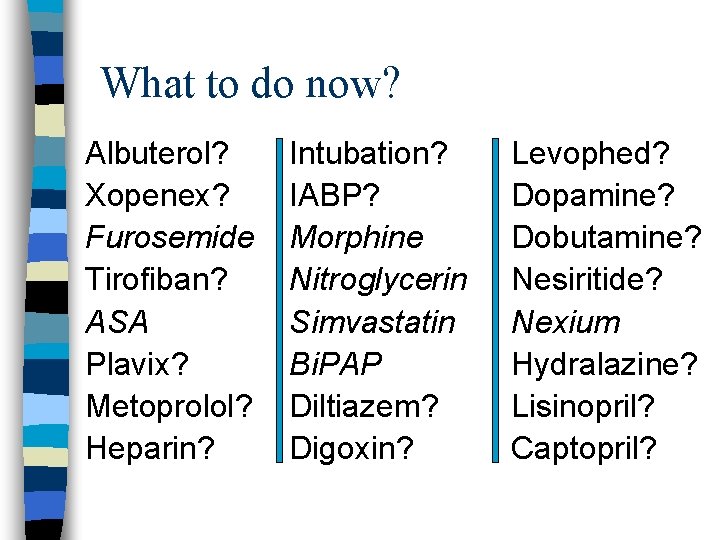
What to do now? Albuterol? Xopenex? Furosemide Tirofiban? ASA Plavix? Metoprolol? Heparin? Intubation? IABP? Morphine Nitroglycerin Simvastatin Bi. PAP Diltiazem? Digoxin? Levophed? Dopamine? Dobutamine? Nesiritide? Nexium Hydralazine? Lisinopril? Captopril?
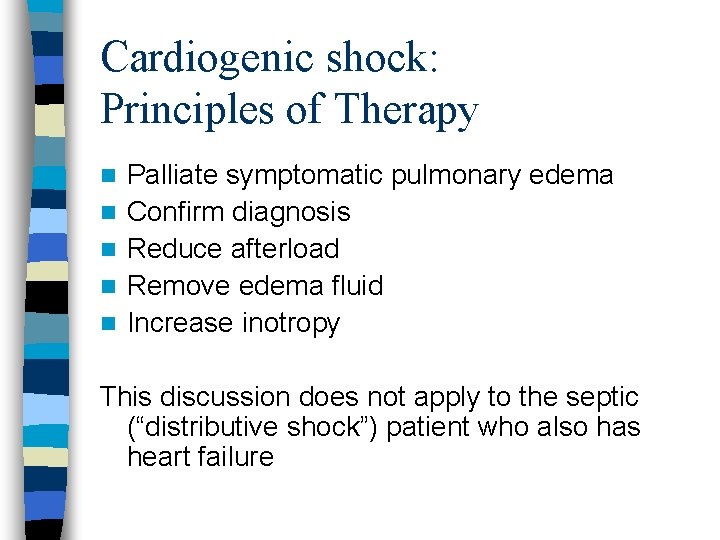
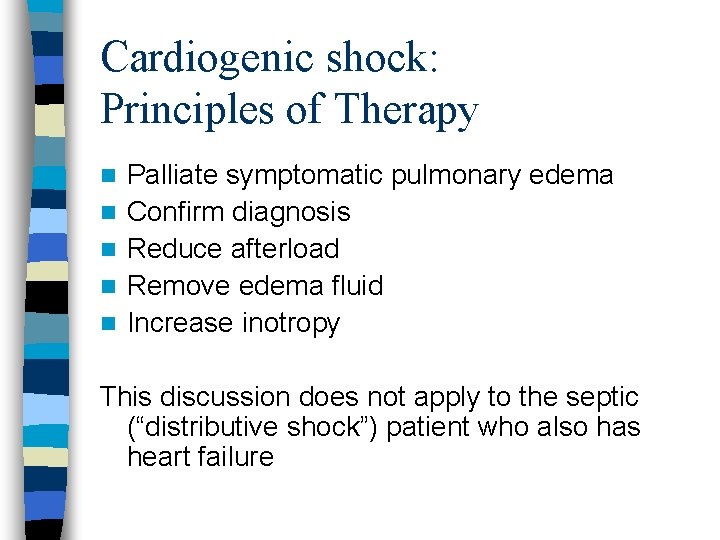
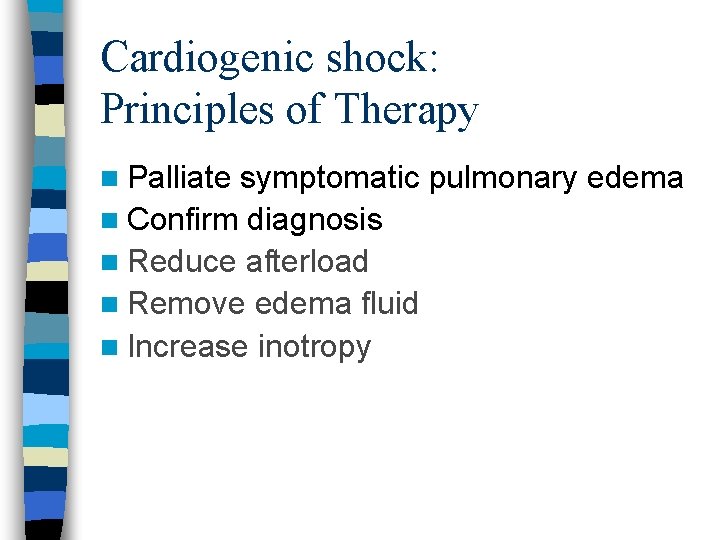
Cardiogenic shock: Principles of Therapy n n n Palliate symptomatic pulmonary edema Confirm diagnosis Reduce afterload Remove edema fluid Increase inotropy This discussion does not apply to the septic (“distributive shock”) patient who also has heart failure
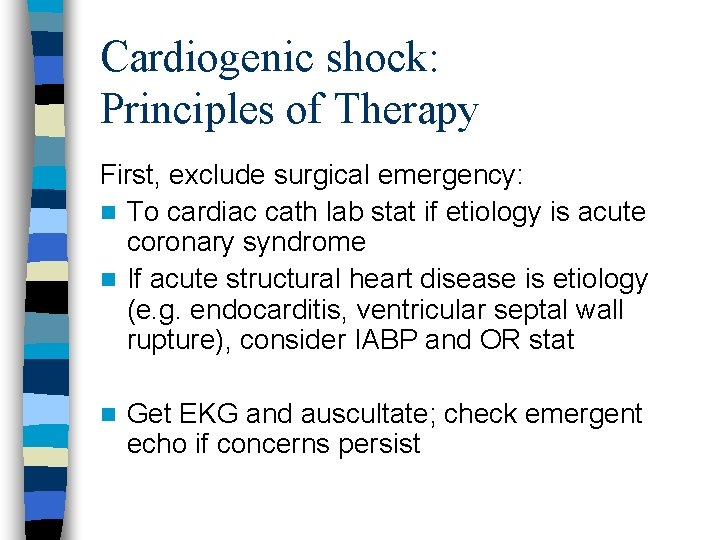
Cardiogenic shock: Principles of Therapy First, exclude surgical emergency: n To cardiac cath lab stat if etiology is acute coronary syndrome n If acute structural heart disease is etiology (e. g. endocarditis, ventricular septal wall rupture), consider IABP and OR stat n Get EKG and auscultate; check emergent echo if concerns persist
Cardiogenic shock: Principles of Therapy n Palliate symptomatic pulmonary edema n Confirm diagnosis n Reduce afterload n Remove edema fluid n Increase inotropy
Cardiogenic shock: Principles of Therapy n Palliate symptomatic pulmonary edema n Confirm diagnosis n Reduce afterload n Remove edema fluid n Increase inotropy
Afterload reduction options n Hydralazine n ACE/ARB n Dobutamine/Milrinone n Nesiritide n Diuresis/Ultrafiltration n Phlebotomy
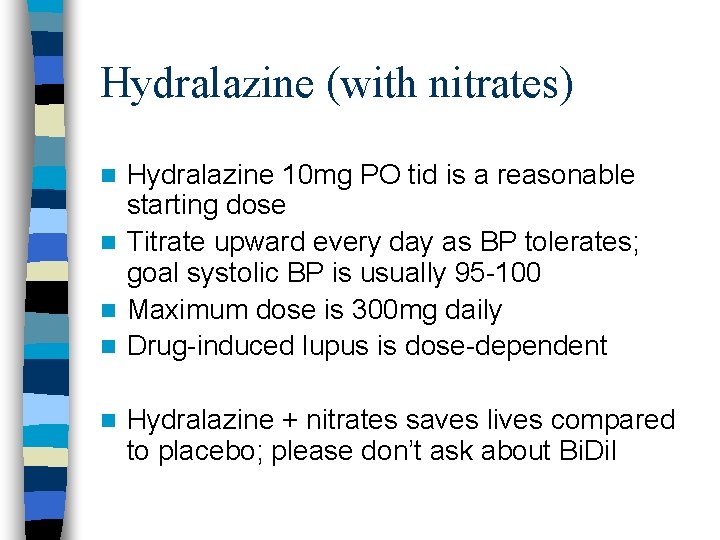
Hydralazine (with nitrates) Hydralazine 10 mg PO tid is a reasonable starting dose n Titrate upward every day as BP tolerates; goal systolic BP is usually 95 -100 n Maximum dose is 300 mg daily n Drug-induced lupus is dose-dependent n n Hydralazine + nitrates saves lives compared to placebo; please don’t ask about Bi. Dil

ACE/ARB Compared to hydralazine and nitrates, ACE or ARB therapy extends life still more n This effect is not dose-dependent (low-dose ACE/ARB as life-extending as high dose) n In severely low output states, can cause renal hypoperfusion and injury (evidence poor) n No evidence that adding ACE to ARB or vice versa has any benefit n
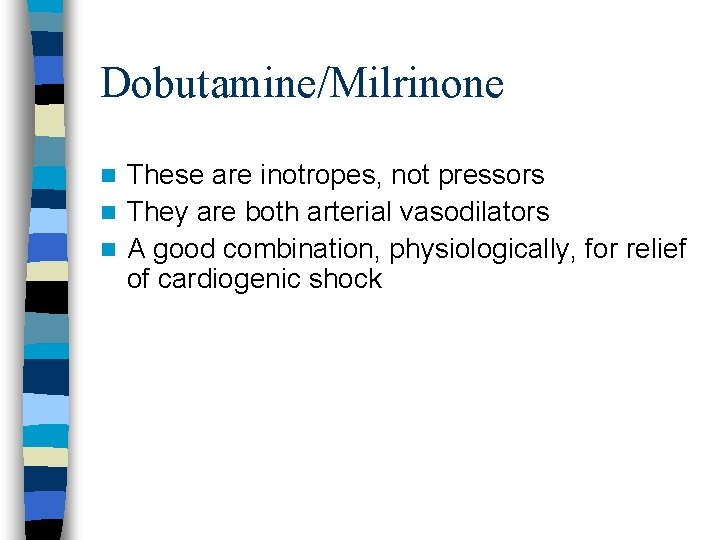
Dobutamine/Milrinone These are inotropes, not pressors n They are both arterial vasodilators n A good combination, physiologically, for relief of cardiogenic shock n
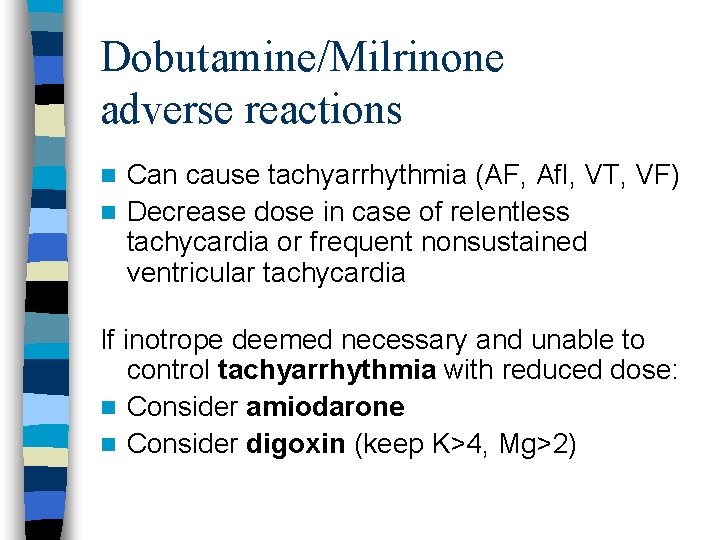
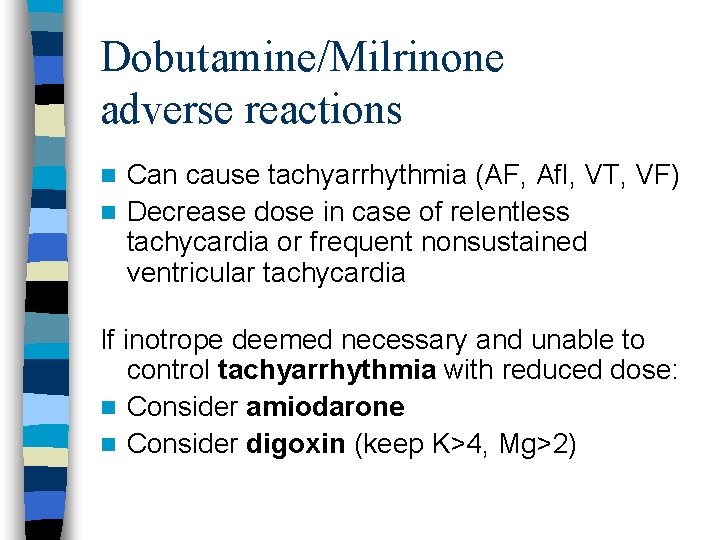
Dobutamine/Milrinone adverse reactions Can cause tachyarrhythmia (AF, Afl, VT, VF) n Decrease dose in case of relentless tachycardia or frequent nonsustained ventricular tachycardia n If inotrope deemed necessary and unable to control tachyarrhythmia with reduced dose: n Consider amiodarone n Consider digoxin (keep K>4, Mg>2)
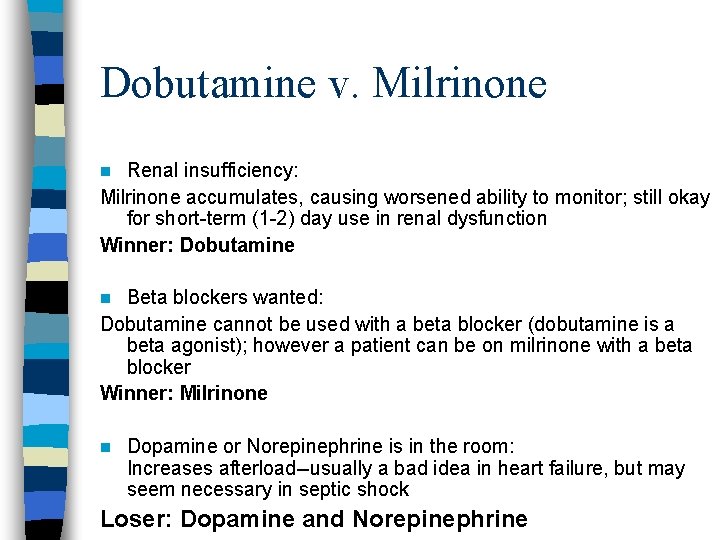
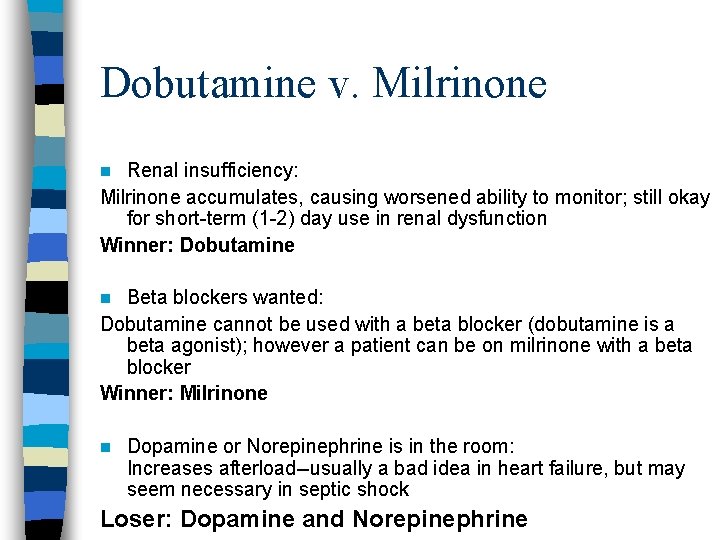
Dobutamine v. Milrinone Renal insufficiency: Milrinone accumulates, causing worsened ability to monitor; still okay for short-term (1 -2) day use in renal dysfunction Winner: Dobutamine n Beta blockers wanted: Dobutamine cannot be used with a beta blocker (dobutamine is a beta agonist); however a patient can be on milrinone with a beta blocker Winner: Milrinone n n Dopamine or Norepinephrine is in the room: Increases afterload--usually a bad idea in heart failure, but may seem necessary in septic shock Loser: Dopamine and Norepinephrine
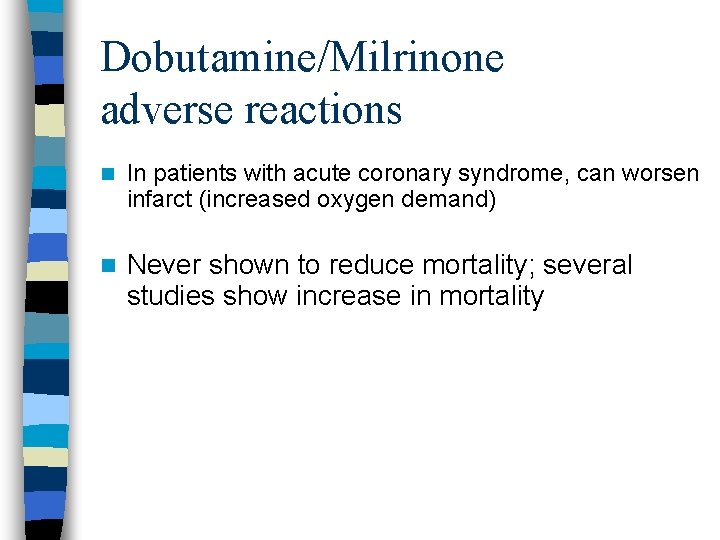
Dobutamine/Milrinone adverse reactions n In patients with acute coronary syndrome, can worsen infarct (increased oxygen demand) n Never shown to reduce mortality; several studies show increase in mortality
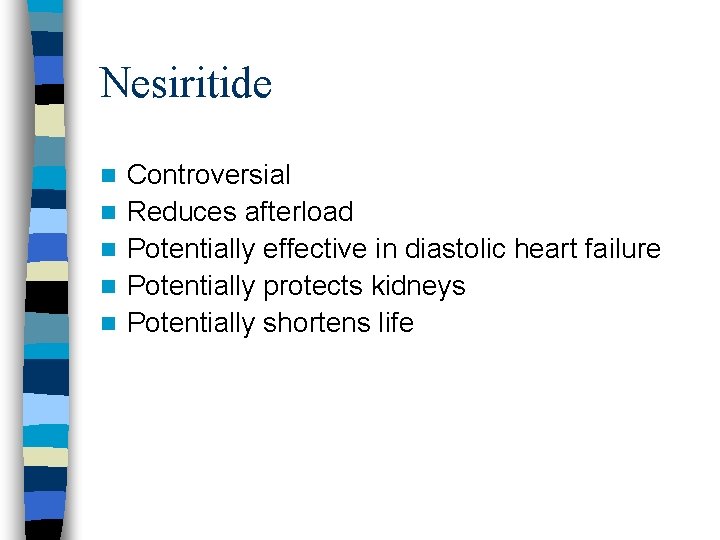
Nesiritide n n n Controversial Reduces afterload Potentially effective in diastolic heart failure Potentially protects kidneys Potentially shortens life
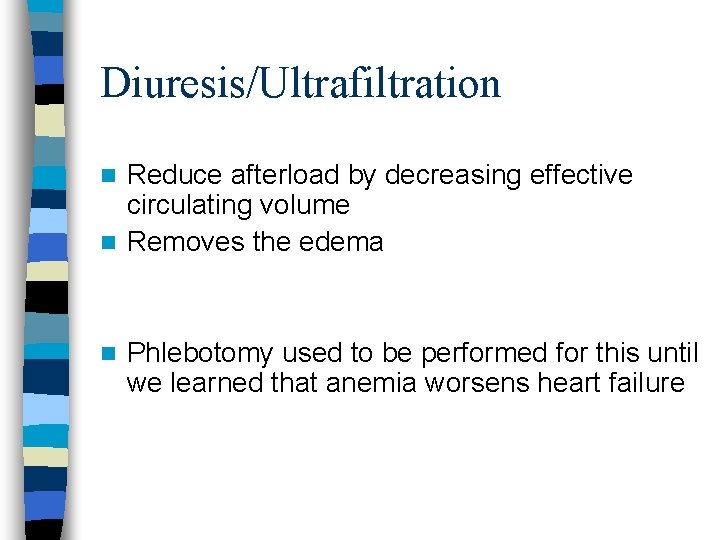
Diuresis/Ultrafiltration Reduce afterload by decreasing effective circulating volume n Removes the edema n n Phlebotomy used to be performed for this until we learned that anemia worsens heart failure
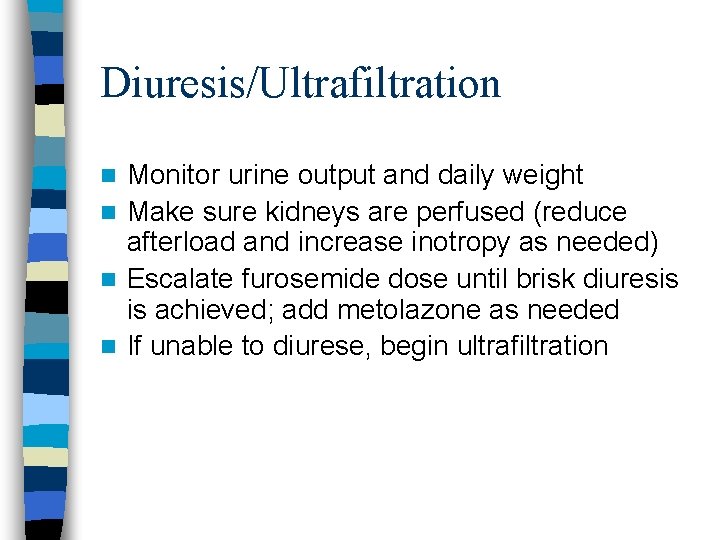
Diuresis/Ultrafiltration Monitor urine output and daily weight n Make sure kidneys are perfused (reduce afterload and increase inotropy as needed) n Escalate furosemide dose until brisk diuresis is achieved; add metolazone as needed n If unable to diurese, begin ultrafiltration n
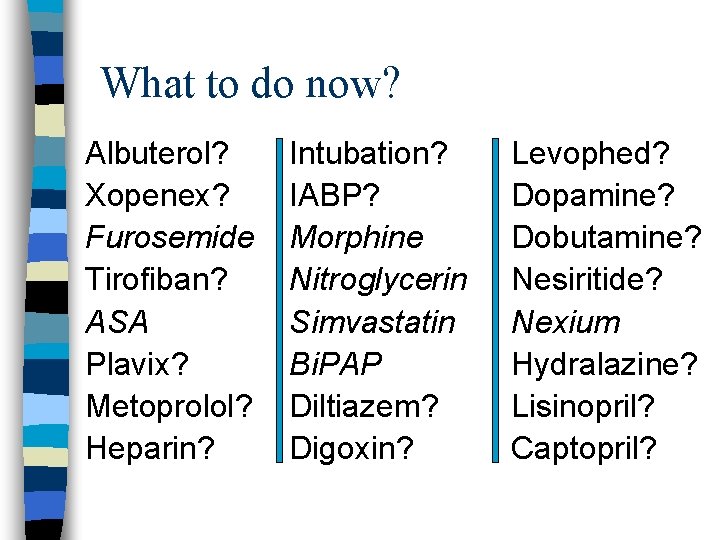
What to do now? Albuterol? Xopenex? Furosemide Tirofiban? ASA Plavix? Metoprolol? Heparin? Intubation? IABP? Morphine Nitroglycerin Simvastatin Bi. PAP Diltiazem? Digoxin? Levophed? Dopamine? Dobutamine? Nesiritide? Nexium Hydralazine? Lisinopril? Captopril?
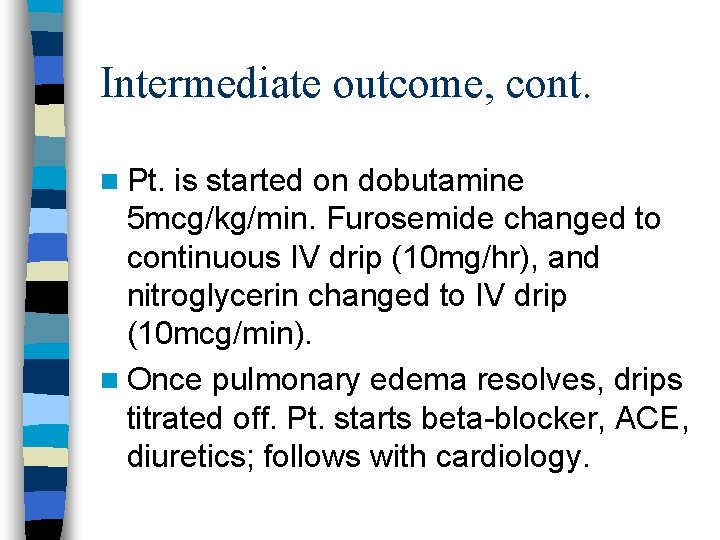
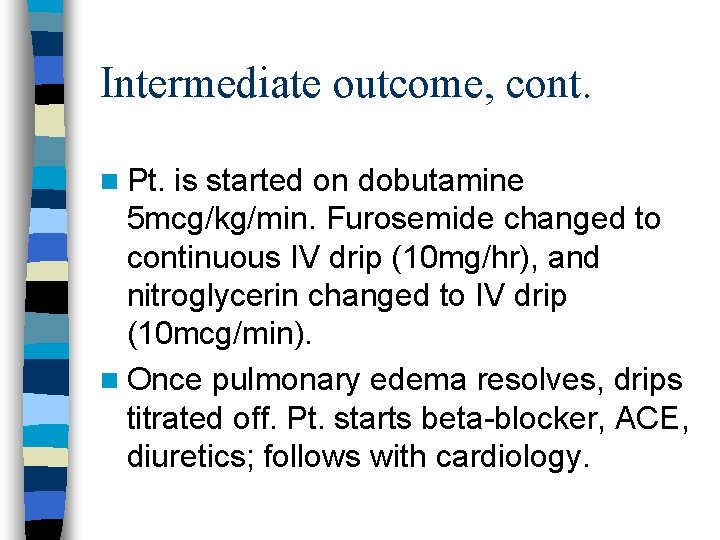
Intermediate outcome, cont. n Pt. is started on dobutamine 5 mcg/kg/min. Furosemide changed to continuous IV drip (10 mg/hr), and nitroglycerin changed to IV drip (10 mcg/min). n Once pulmonary edema resolves, drips titrated off. Pt. starts beta-blocker, ACE, diuretics; follows with cardiology.
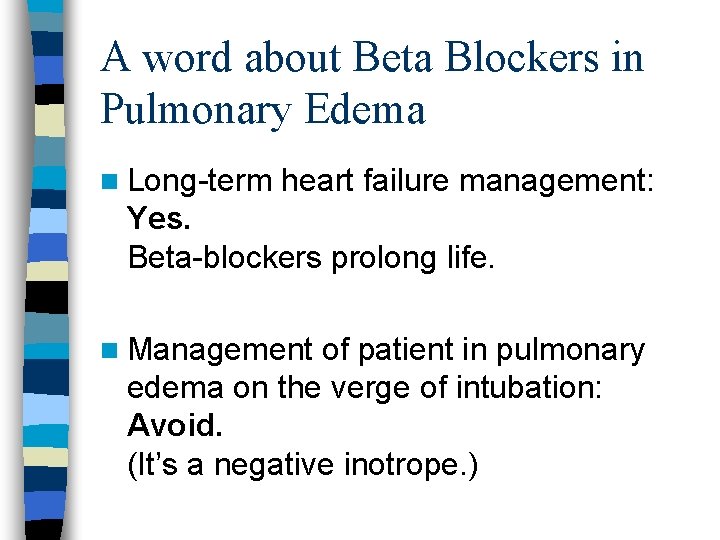
A word about Beta Blockers in Pulmonary Edema n Long-term heart failure management: Yes. Beta-blockers prolong life. n Management of patient in pulmonary edema on the verge of intubation: Avoid. (It’s a negative inotrope. )
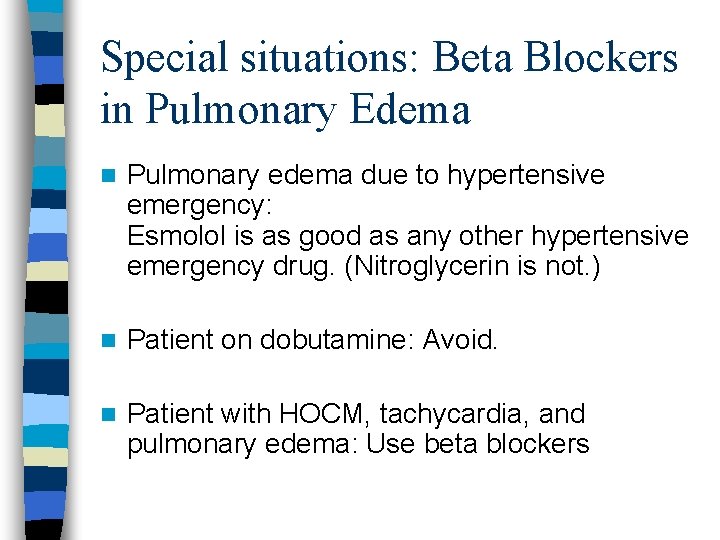
Special situations: Beta Blockers in Pulmonary Edema n Pulmonary edema due to hypertensive emergency: Esmolol is as good as any other hypertensive emergency drug. (Nitroglycerin is not. ) n Patient on dobutamine: Avoid. n Patient with HOCM, tachycardia, and pulmonary edema: Use beta blockers
Choose your own adventure. What would you like to discuss now? n Furosemide pharmacokinetics n DDx of elevated troponin n Heparin/LMWH in UA/NSTEMI n Why is this patient hyponatremic? n HOCM/ASH/IHSS/LVOT obstruction n Something completely different
 Acute vs chronic heart failure
Acute vs chronic heart failure Pulmonary edema
Pulmonary edema Cardiogenic vs noncardiogenic pulmonary edema
Cardiogenic vs noncardiogenic pulmonary edema Barrel chest with emphysema
Barrel chest with emphysema Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Acute liver failure
Acute liver failure Treatments for acute renal failure
Treatments for acute renal failure Acute brain failure
Acute brain failure Transaminitis definition
Transaminitis definition Cushings triad
Cushings triad Ductile break
Ductile break Failure to sense
Failure to sense Failure to fire pacemaker
Failure to fire pacemaker L
L Papillary muscles sheep heart
Papillary muscles sheep heart Congestive heart failure symtoms
Congestive heart failure symtoms Diabetes and heart failure
Diabetes and heart failure Heart failure complications
Heart failure complications Lmnop heart failure
Lmnop heart failure New york scale heart failure
New york scale heart failure Pvkov
Pvkov Compensatory mechanisms of heart failure
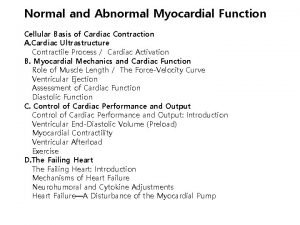
Compensatory mechanisms of heart failure Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Lvedp normal range
Lvedp normal range Keith rn heart failure case study
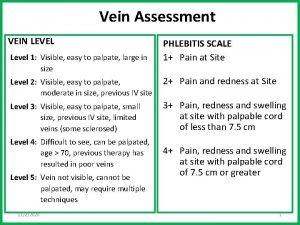
Keith rn heart failure case study Edema assessment
Edema assessment Right ventricular failure
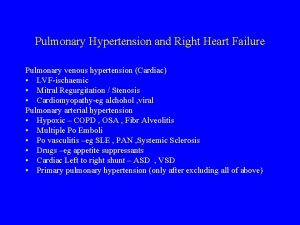
Right ventricular failure Heart failure
Heart failure Classification of ejection fraction
Classification of ejection fraction Donkey analogy heart failure
Donkey analogy heart failure Vetsulin dosage chart for dogs
Vetsulin dosage chart for dogs Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Right vs left-sided heart failure chart
Right vs left-sided heart failure chart Congestive heart failure zones for management
Congestive heart failure zones for management Heart failure definition
Heart failure definition Sam systolic anterior motion
Sam systolic anterior motion Systolic over diastolic
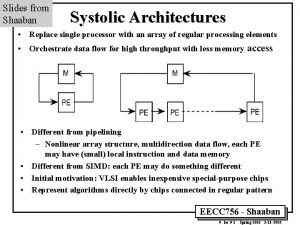
Systolic over diastolic Systolic array vs simd
Systolic array vs simd Auscultatory gap
Auscultatory gap Isolated systolic hypertension
Isolated systolic hypertension Heart sound
Heart sound 174/116 blood pressure
174/116 blood pressure Systolic and diastolic dysfunction
Systolic and diastolic dysfunction What decreases stroke volume
What decreases stroke volume What is systolic and diastolic pressure
What is systolic and diastolic pressure Systolic ejection murmur left sternal border
Systolic ejection murmur left sternal border Systolic array
Systolic array Murmur intensity grading
Murmur intensity grading Stroke volume ejection fraction
Stroke volume ejection fraction Why systolic architectures
Why systolic architectures Normal pulmonary artery pressure
Normal pulmonary artery pressure Av shunt
Av shunt Classificação do edema
Classificação do edema Teoria overflow edema
Teoria overflow edema Buergers angle
Buergers angle Perimalleolar edema
Perimalleolar edema Capillary refill
Capillary refill Edema polmonare
Edema polmonare Edema scale
Edema scale