Advances in Heart Failure June 2012 Heart Failure



- Slides: 33

Advances in Heart Failure June 2012
Heart Failure – a Definition “a complex clinical syndrome of symptoms and signs that suggest impairment of the heart as a pump supporting physiological circulation. It is caused by structural or functional abnormalities of the heart. The demonstration of objective evidence of these cardiac abnormalities is necessary for the diagnosis of heart failure to be made. The symptoms most commonly encountered are breathlessness (exertional dyspnoea, orthopnoea and paroxysmal nocturnal dyspnoea) fatigue and ankle swelling. ” NICE (2010)
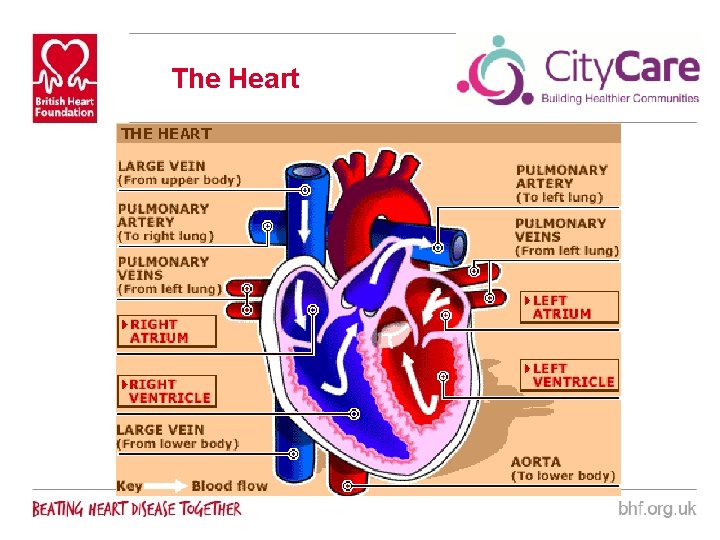
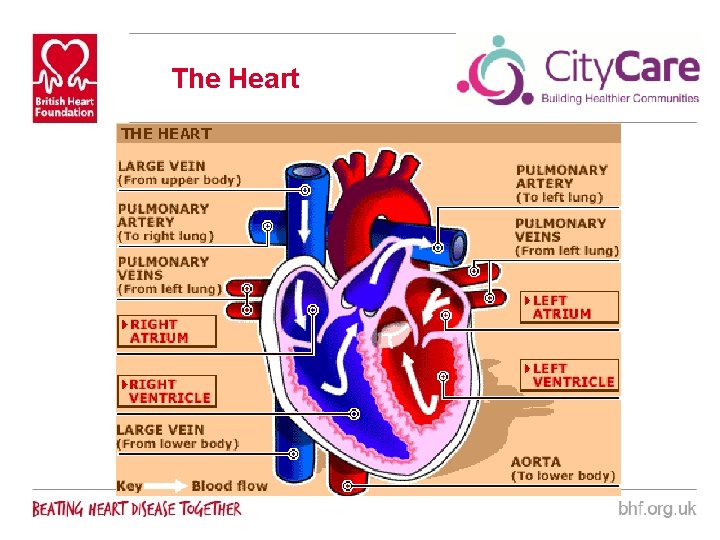
The Heart
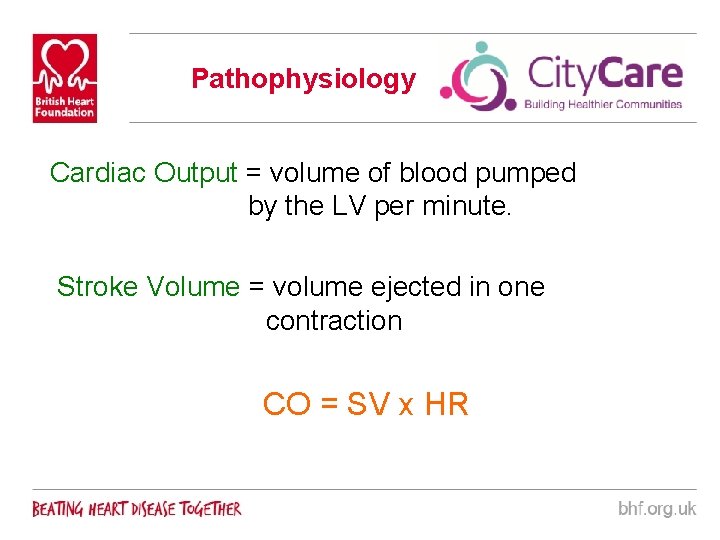
Pathophysiology Cardiac Output = volume of blood pumped by the LV per minute. Stroke Volume = volume ejected in one contraction CO = SV x HR
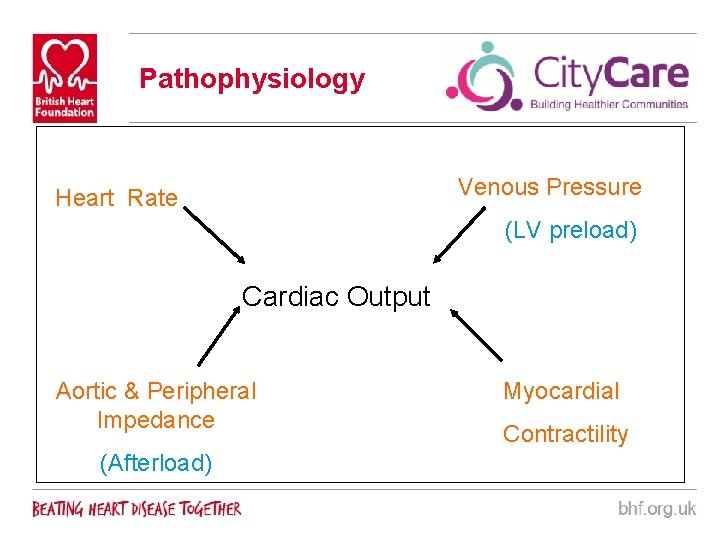
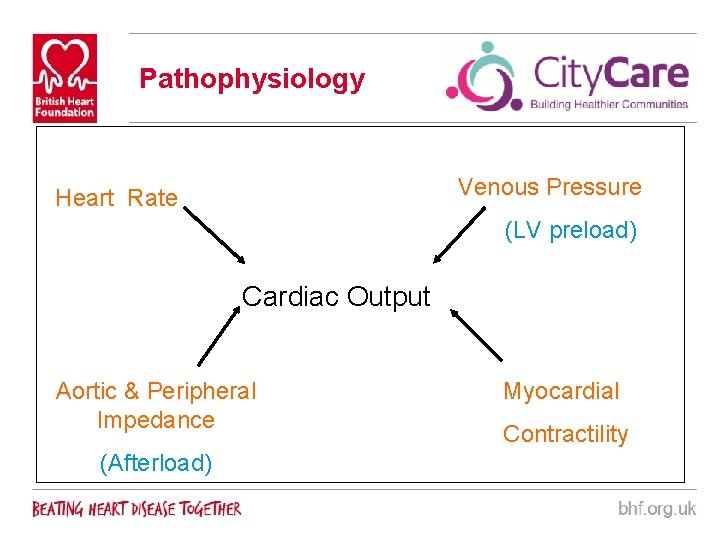
Pathophysiology Venous Pressure Heart Rate (LV preload) Cardiac Output Aortic & Peripheral Impedance (Afterload) Myocardial Contractility
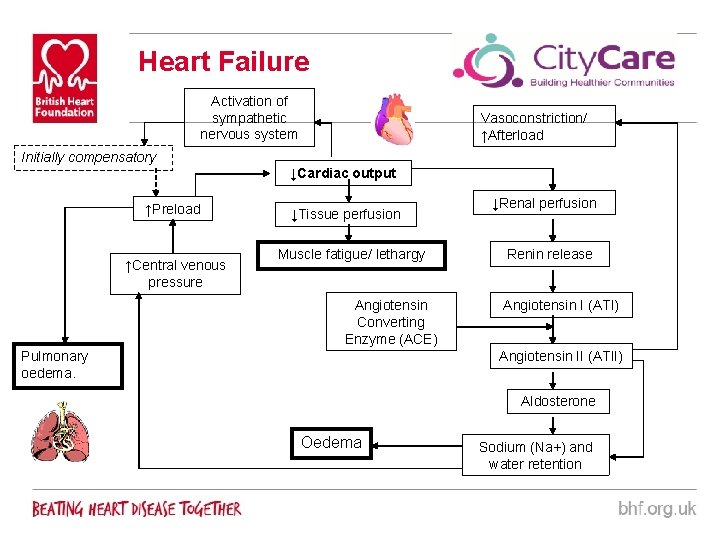
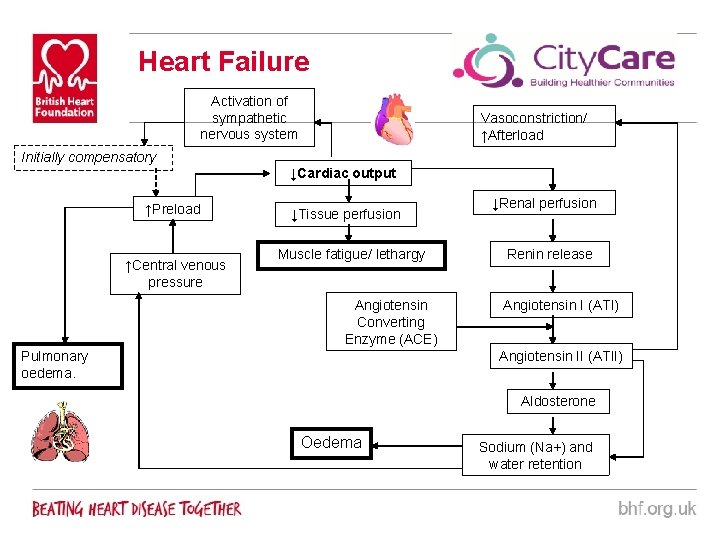
Heart Failure Activation of sympathetic nervous system Initially compensatory ↑Preload ↑Central venous pressure Vasoconstriction/ ↑Afterload ↓Cardiac output ↓Tissue perfusion Muscle fatigue/ lethargy Angiotensin Converting Enzyme (ACE) Pulmonary oedema. ↓Renal perfusion Renin release Angiotensin I (ATI) Angiotensin II (ATII) Aldosterone Oedema Sodium (Na+) and water retention
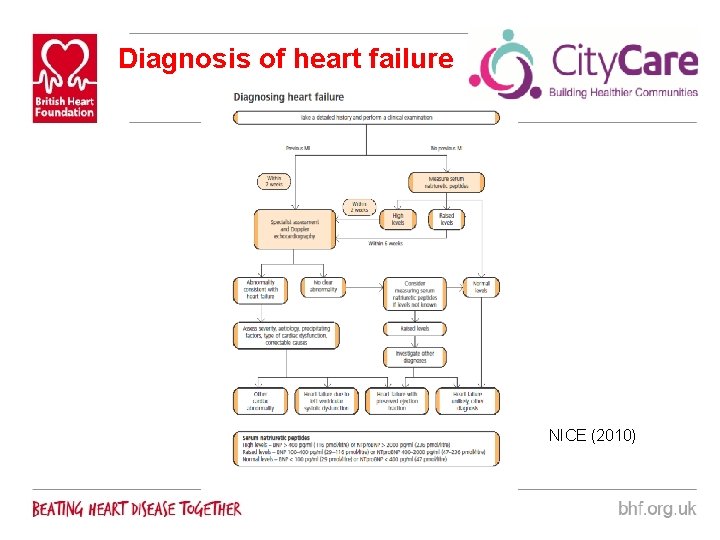
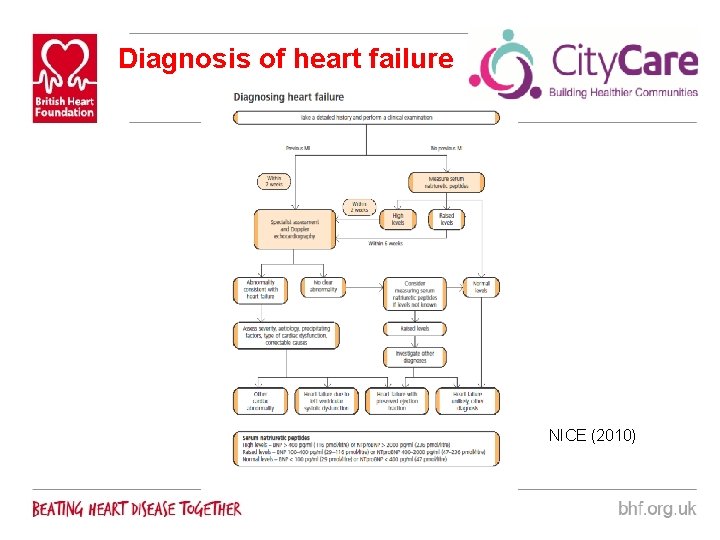
Diagnosis of heart failure NICE (2010)
Advances in Heart Failure ● ● Brain Natriuretic Peptides Heart Failure With Preserved Ejection Fraction New Pharmacological Therapies Community IV Diuretic Therapy
Brain Natriuretic Peptide (BNP) ● 32 Amino acid polypeptide ● Released by ventricles in response ventricular wall stretch and damage to myocytes ● Initially found in porcine brain cells. In humans is found in cardiac ventricles ● Measured by blood test ● Positive levels may indicate heart failure and should prompt further investigation ● Normal levels can rule out heart failure ● Does not confirm Left Ventricular Systolic Dysfunction – BNP also released in right sided heart failure and diastolic heart failure ● BNP measurement can be used to monitor effects of treatment ● About to be launched in Nottingham
Causes for Raised BNP Cardiac ● Heart Failure ● Acute Coronary Syndrome ● Valvular Disease ● Left Ventricular Hypertrophy ● Atrial Fibrillation
Causes for Raised BNP Non-Cardiac ● Renal failure ● Pulmonary Embolism ● Pulmonary Hypertension ● Sepsis ● Chronic Obstructive Pulmonary Disease (with corpulmonale or respiratory failure) ● Hyperthyroid disorder
Heart failure with preserved ejection fraction (diastolic heart failure) • Often presumed when symptoms and signs of heart failure occur in a patient with preserved left ventricular systolic function (normal ejection fraction/normal end-diastolic volume) at rest • Characterised by prolonged LV relaxation; slow LV filling and increased LV and arterial stiffness. • More common in the elderly, women and those with hypertension or diabetes • Diagnosis and management remain controversial • Echocardiography may help confirm the diagnosis • Normal LV ejection fraction with atrial enlargement / dilatation and/ or left ventricular hypertrophy (ESC, 2008; NICE, 2010)
Heart failure with preserved ejection fraction (diastolic heart failure) • Natriuretic peptides may be helpful in ruling out heart failure in those with preserved ejection fraction • Treatment: – ACE-Inhibitors • PEP-CHF Perindopril – No effect on Mortality or Hospital Admissions – Angiotensin Receptor Blockers • CHARM-Preserved Candesartan – No significant effect on cardiovascular death but there were fewer hospital admissions • I-Preserve Irbesartan – No effect on mortality or hospital admissions – Betablockers • OPTIMIZE-HF Registry – included both HFp. EF and LVSD. Patients discharged on betablockers. No effects on clinical outcomes in HFp. EF
Heart failure with preserved ejection fraction (diastolic heart failure) • Ongoing Research: – Phosphodiesterase 5 Inhibitors • Reduce ventricular-vascular stiffening • Improve endothelial function • Reduce pulmonary vascular stiffness • Sildenafil currently being tested – Aldosterone Antagonists • Reduce vascular stiffness • Improve endothelial function • Spironolactone being tested
New Pharmacological Therapies • Eplerenone – Aldosterone Antagonist – Aldosterone contributes to vaso constriction and sodium and water retention – Previously used post myocardial infarction – reduced mortality if started within 30 days of MI in patients with LVEF <40% and clinical signs of heart failure (EPHESUS trial)
New Pharmacological Therapies • Now licensed in Chronic Heart Failure – Patients with LVEF <35% and NYHA 2. Eplerenone 2550 mg per day reduced cardiovascular mortality and hospital admissions (EMPHASIS trial) • Side effects: – As Spironolactone – Gynaecomastia less likely • Not on City. Care Formulary so needs to be prescribed by cardiologist
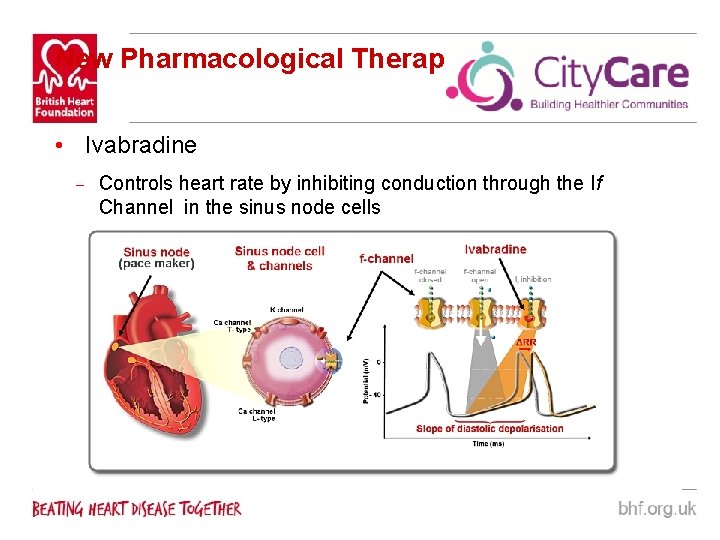
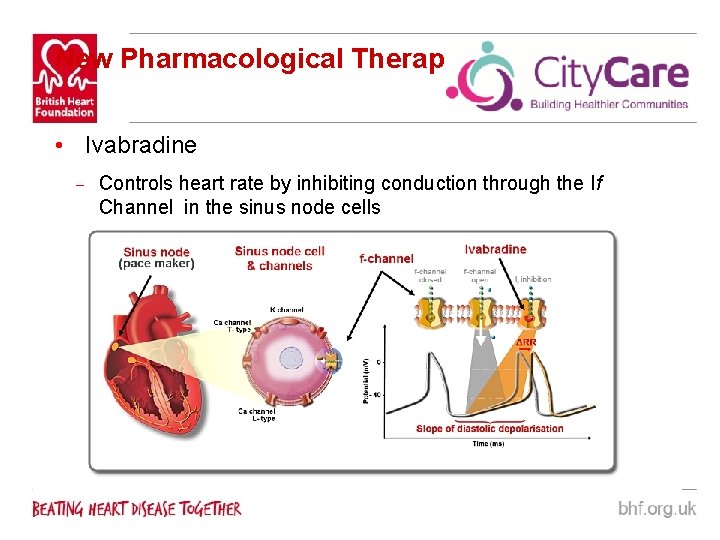
New Pharmacological Therapies • Ivabradine – Controls heart rate by inhibiting conduction through the If Channel in the sinus node cells
New Pharmacological Therapies • Raised resting heart rate is a known risk factor for mortality and cardiovascular outcomes • In coronary artery disease and LV dysfunction a heart rate >70 bpm increased risk of cardiovascular death by 34% and hospitalisation by 53% • Ivabradine can be used in addition to betablockade • No effect on Blood Pressure and safe in asthma so can be used as alternative to betablockade • Risk of cardiovascular death and hospital admission due to heart failure fell by 18% in heart failure patients treated with Ivabradine Vs Placebo – (SHIFT trial)
New Pharmacological Therapies • Does not work in AF • Start at 5 mg BD and titrate to 7. 5 mg BD • Side effects: – Visual disturbance (phosphenes) – Bradycardia • Previously used in angina. Now licensed in heart failure • Not on City. Care formulary so prescribed by cardiologist
Community IV Diuretics § Pilot project in Nottingham City. Care § BHF funded (18. 75 hours p/w band 6 nurse) § Supported by Cardiologist § 13 pilot sites in the UK § 2 years pilot with external evaluation § Nottingham City. Care and Nottingham West Consortia are “Case Study” sites
Evidence § Nurse led community heart failure follow up reduces hospital admissions (Blue et al, 2001) § IV diuretics in an outpatient setting in selected patients is safe, feasible, clinically effective and avoids hospital admissions (Ryder et al, 2008) § A nurse led IV antibiotic and IV iron service in Cheshire saved £ 1 m over three years (Lomas, 2009)
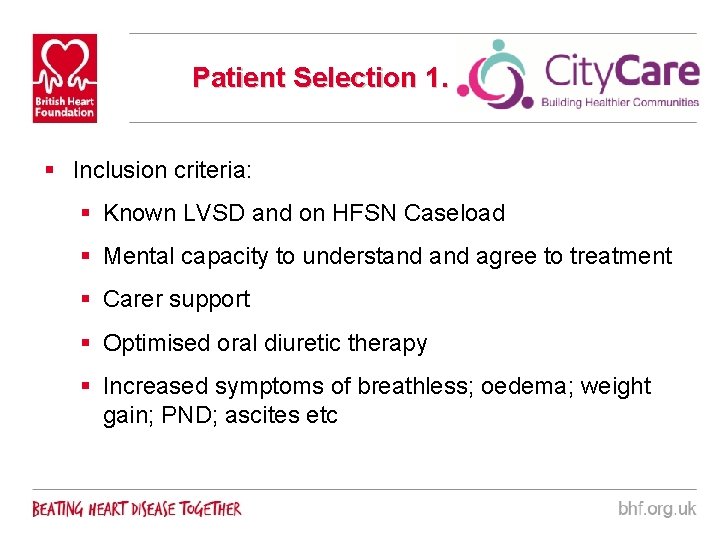
Patient Selection 1. § Inclusion criteria: § Known LVSD and on HFSN Caseload § Mental capacity to understand agree to treatment § Carer support § Optimised oral diuretic therapy § Increased symptoms of breathless; oedema; weight gain; PND; ascites etc
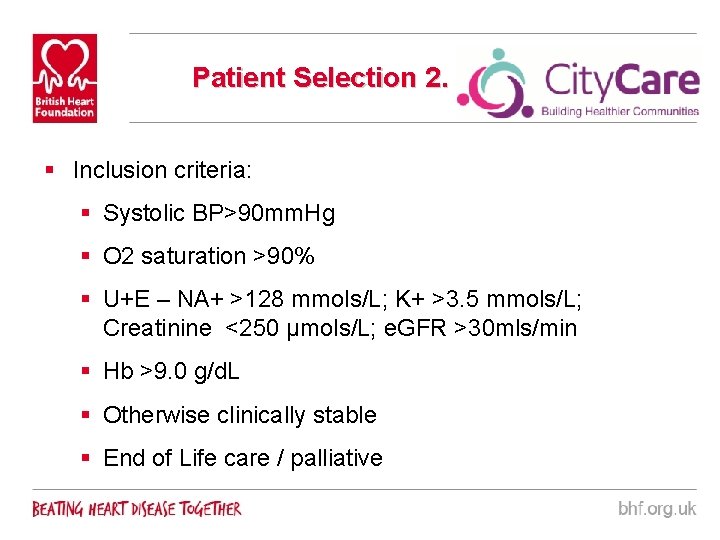
Patient Selection 2. § Inclusion criteria: § Systolic BP>90 mm. Hg § O 2 saturation >90% § U+E – NA+ >128 mmols/L; K+ >3. 5 mmols/L; Creatinine <250 µmols/L; e. GFR >30 mls/min § Hb >9. 0 g/d. L § Otherwise clinically stable § End of Life care / palliative
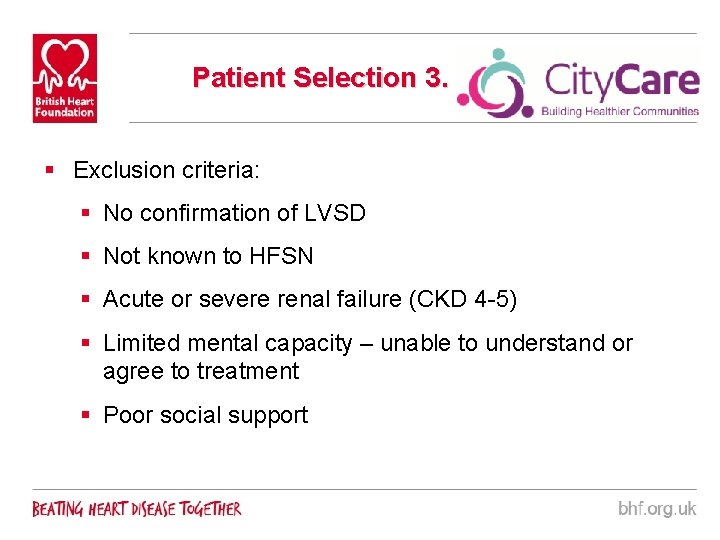
Patient Selection 3. § Exclusion criteria: § No confirmation of LVSD § Not known to HFSN § Acute or severe renal failure (CKD 4 -5) § Limited mental capacity – unable to understand or agree to treatment § Poor social support
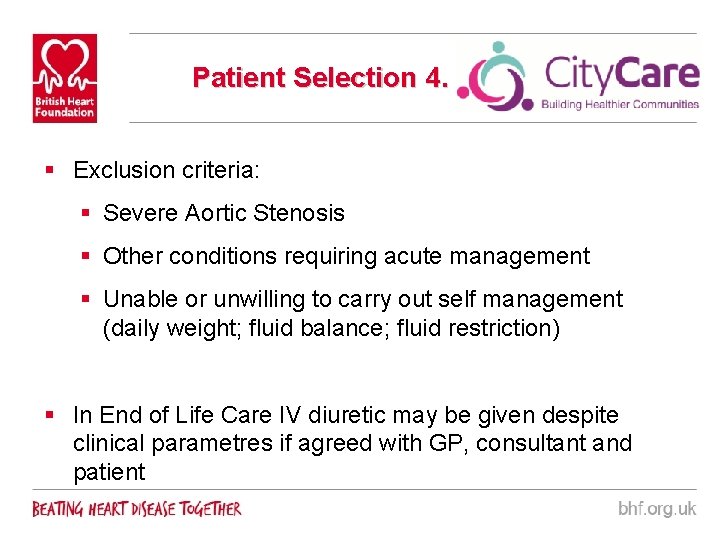
Patient Selection 4. § Exclusion criteria: § Severe Aortic Stenosis § Other conditions requiring acute management § Unable or unwilling to carry out self management (daily weight; fluid balance; fluid restriction) § In End of Life Care IV diuretic may be given despite clinical parametres if agreed with GP, consultant and patient
Before IV Diuretics § Patient selection – decompensated heart failure symptoms despite optimised oral therapy; fulfils inclusion criteria § Discussion with patient; carer; GP; Consultant § Preparation § Education § Informed consent § Cannulation § Equipment
Delivering IV Diuretics § Drug Administration § Mc. Kinley T 34 Syringe Driver § Furosemide for injection / infusion § 4 mg /min § Daily Monitoring § Fluid balance; weight; oedema; symptoms; VIP score § BP; HR; O 2 saturation; ? use of Telehealth § U+E (blood taken 4 hours post administration)
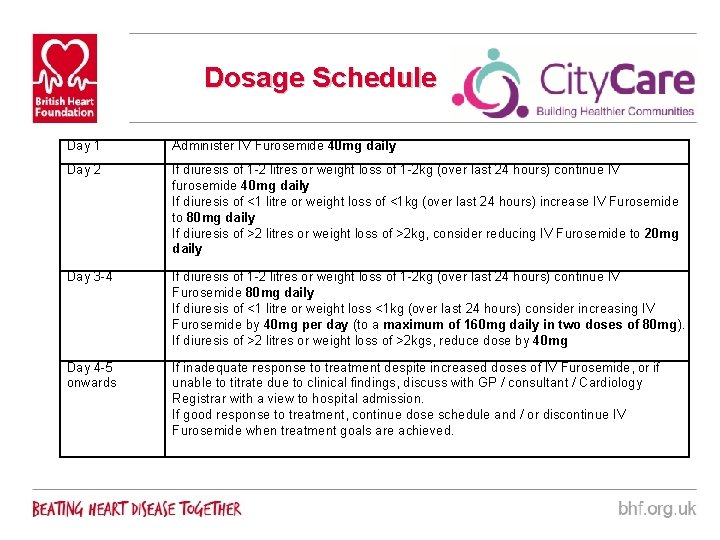
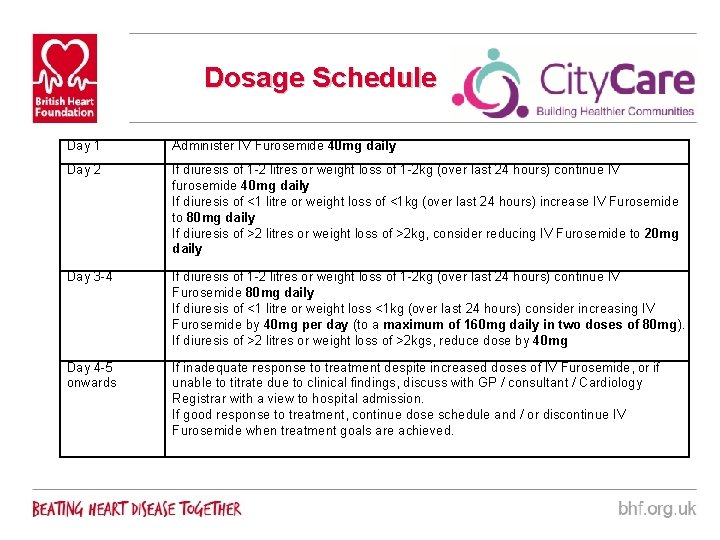
Dosage Schedule Day 1 Administer IV Furosemide 40 mg daily Day 2 If diuresis of 1 -2 litres or weight loss of 1 -2 kg (over last 24 hours) continue IV furosemide 40 mg daily If diuresis of <1 litre or weight loss of <1 kg (over last 24 hours) increase IV Furosemide to 80 mg daily If diuresis of >2 litres or weight loss of >2 kg, consider reducing IV Furosemide to 20 mg daily Day 3 -4 If diuresis of 1 -2 litres or weight loss of 1 -2 kg (over last 24 hours) continue IV Furosemide 80 mg daily If diuresis of <1 litre or weight loss <1 kg (over last 24 hours) consider increasing IV Furosemide by 40 mg per day (to a maximum of 160 mg daily in two doses of 80 mg). If diuresis of >2 litres or weight loss of >2 kgs, reduce dose by 40 mg Day 4 -5 onwards If inadequate response to treatment despite increased doses of IV Furosemide, or if unable to titrate due to clinical findings, discuss with GP / consultant / Cardiology Registrar with a view to hospital admission. If good response to treatment, continue dose schedule and / or discontinue IV Furosemide when treatment goals are achieved.
Withdrawal of IV Diuretics § Treatment has been effective § Treatment is not effective after 3 days (? hospital admission / cardiology review) § Patient chooses to withdraw § Adverse reactions occur § Clinical parametres indicate IV Diuretics should not be continued § If treatment effective, IV diuretics are stopped and normal oral dosing resumes
Evaluation of IV Diuretics at Home § Is it safe? § What doses are safe and effective? § Effect on hospital admissions? § Patient and carer experience. § Is it cost effective? § Is it sustainable § Impact on HF service? § Impact on other services (NEMS; DN; GP)?
What next? § Dissemination of IV Diuretics Procedure § Final sign off of all documentation § Development of IV Policy § Cannulation competence § Patient Recruitment § Ongoing training

Any Questions?

Contact information: Office: 0115 8834733 Fax: 0115 883 4799 firstname. surname@nottinghamcity. nhs. uk New Brook House 385 Alfreton Road Radford, NG 7 5 LR