HEART FAILURE Ron Leslie 19072017 AIMS Heart failure


- Slides: 21
HEART FAILURE. Ron Leslie 19/07/2017
AIMS. Heart failure definition and epidemiology Heart failure ‘types’ and treatment Case studies
DEFINITION. PHYSIOLOGICAL – inability of the heart to pump sufficient oxygenated blood to the metabolizing tissues despite an adequate filling pressure. CLINICAL – syndrome consisting of symptoms caused by cardiac dysfunction. Gardner et al (2007)
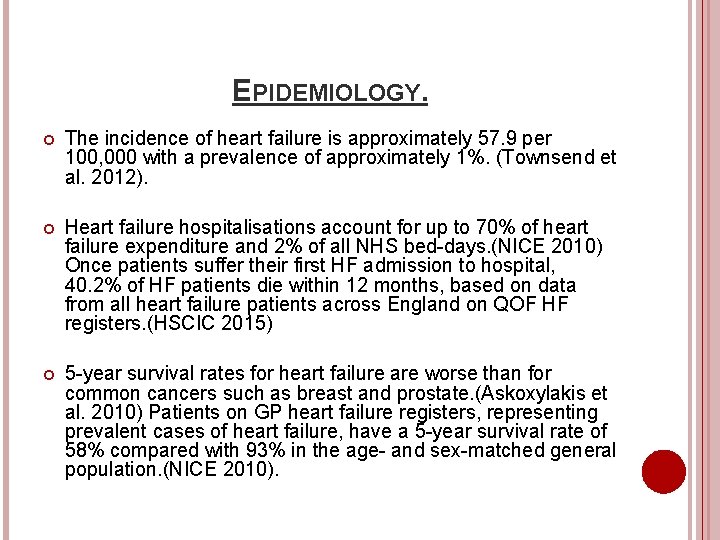
EPIDEMIOLOGY. The incidence of heart failure is approximately 57. 9 per 100, 000 with a prevalence of approximately 1%. (Townsend et al. 2012). Heart failure hospitalisations account for up to 70% of heart failure expenditure and 2% of all NHS bed-days. (NICE 2010) Once patients suffer their first HF admission to hospital, 40. 2% of HF patients die within 12 months, based on data from all heart failure patients across England on QOF HF registers. (HSCIC 2015) 5 -year survival rates for heart failure are worse than for common cancers such as breast and prostate. (Askoxylakis et al. 2010) Patients on GP heart failure registers, representing prevalent cases of heart failure, have a 5 -year survival rate of 58% compared with 93% in the age- and sex-matched general population. (NICE 2010).
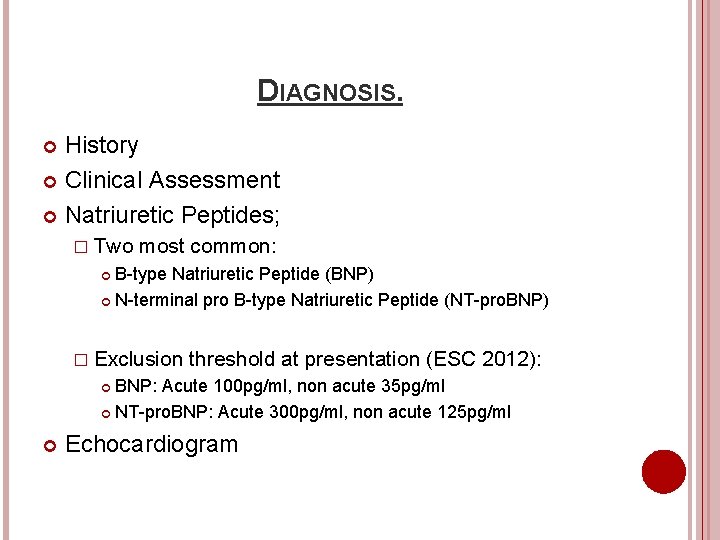
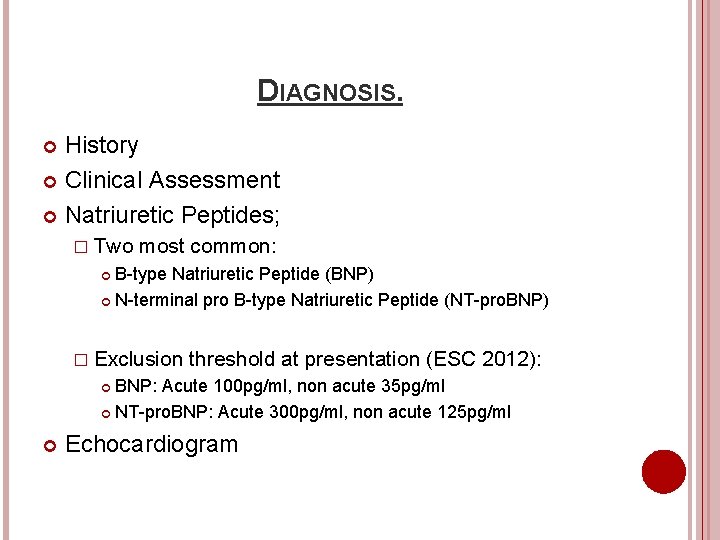
DIAGNOSIS. History Clinical Assessment Natriuretic Peptides; � Two most common: B-type Natriuretic Peptide (BNP) N-terminal pro B-type Natriuretic Peptide (NT-pro. BNP) � Exclusion threshold at presentation (ESC 2012): BNP: Acute 100 pg/ml, non acute 35 pg/ml NT-pro. BNP: Acute 300 pg/ml, non acute 125 pg/ml Echocardiogram
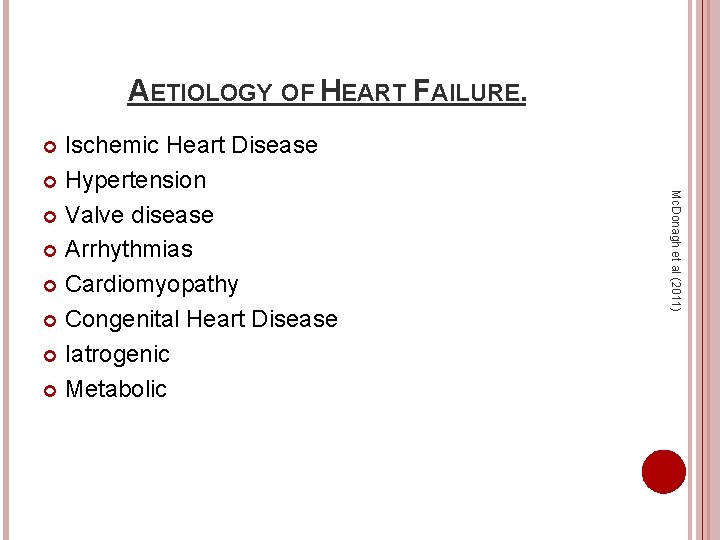
AETIOLOGY OF HEART FAILURE. Ischemic Heart Disease Hypertension Valve disease Arrhythmias Cardiomyopathy Congenital Heart Disease Iatrogenic Metabolic Mc. Donagh et al (2011)
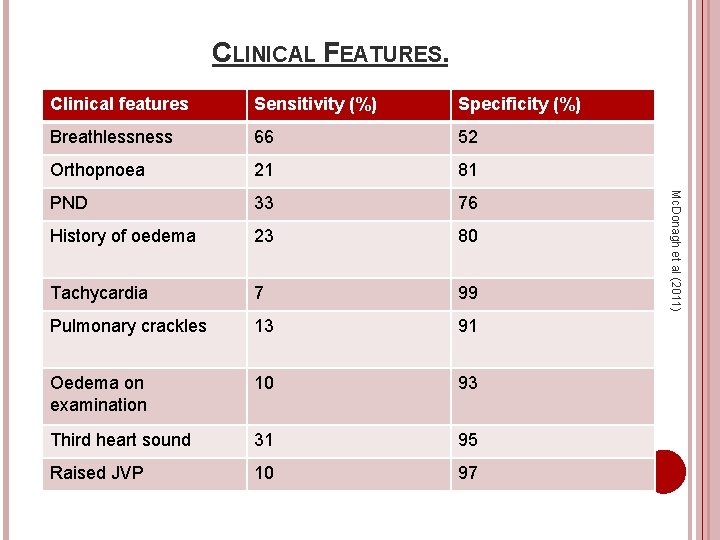
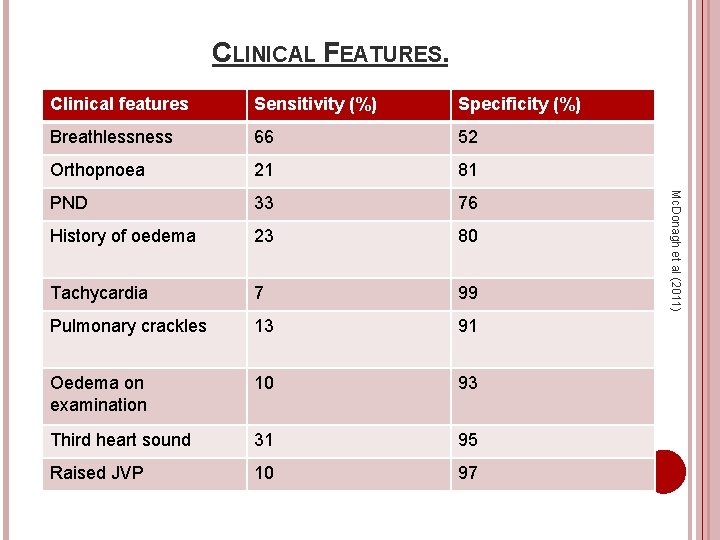
CLINICAL FEATURES. Sensitivity (%) Specificity (%) Breathlessness 66 52 Orthopnoea 21 81 PND 33 76 History of oedema 23 80 Tachycardia 7 99 Pulmonary crackles 13 91 Oedema on examination 10 93 Third heart sound 31 95 Raised JVP 10 97 Mc. Donagh et al (2011) Clinical features
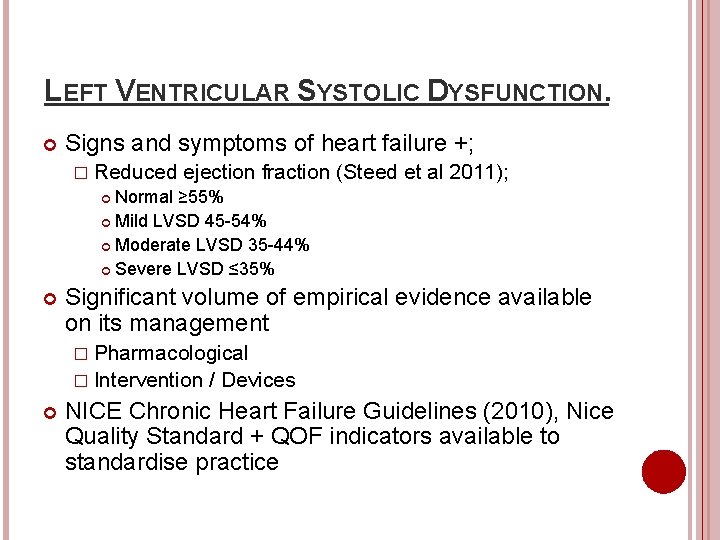
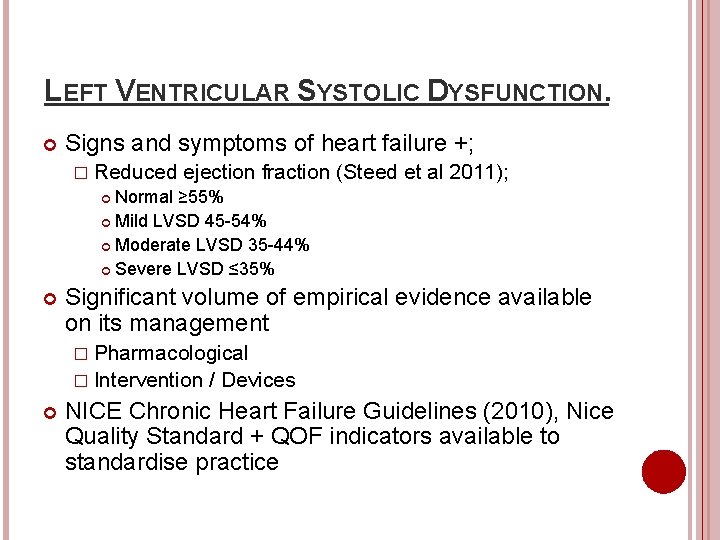
LEFT VENTRICULAR SYSTOLIC DYSFUNCTION. Signs and symptoms of heart failure +; � Reduced ejection fraction Normal ≥ 55% Mild LVSD 45 -54% Moderate LVSD 35 -44% Severe LVSD ≤ 35% (Steed et al 2011); Significant volume of empirical evidence available on its management � Pharmacological � Intervention / Devices NICE Chronic Heart Failure Guidelines (2010), Nice Quality Standard + QOF indicators available to standardise practice
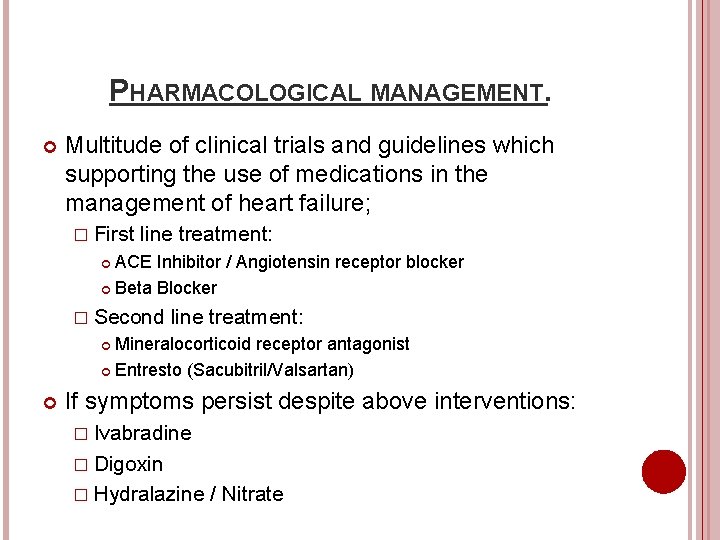
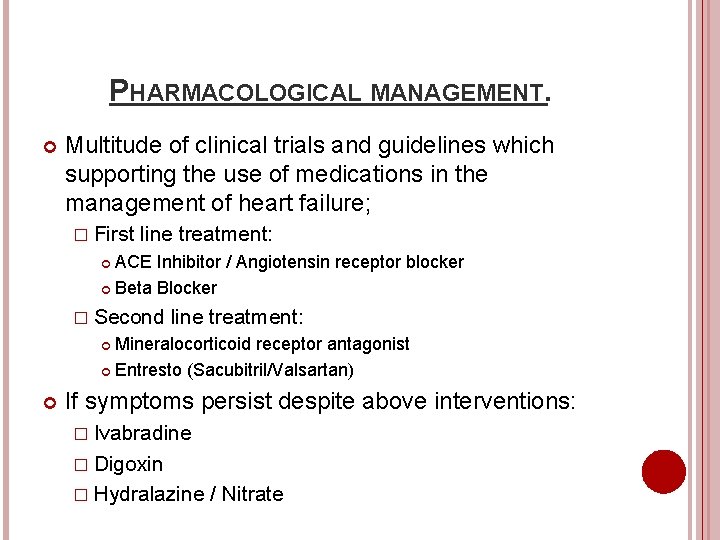
PHARMACOLOGICAL MANAGEMENT. Multitude of clinical trials and guidelines which supporting the use of medications in the management of heart failure; � First line treatment: ACE Inhibitor / Angiotensin receptor blocker Beta Blocker � Second line treatment: Mineralocorticoid receptor antagonist Entresto (Sacubitril/Valsartan) If symptoms persist despite above interventions: � Ivabradine � Digoxin � Hydralazine / Nitrate
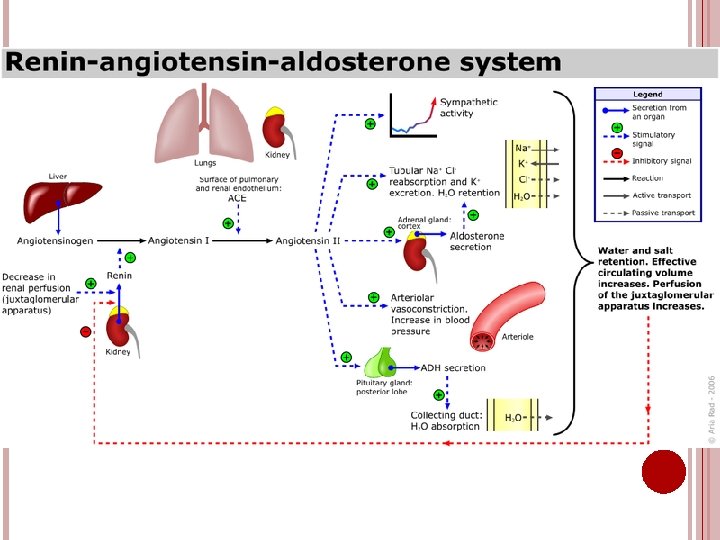
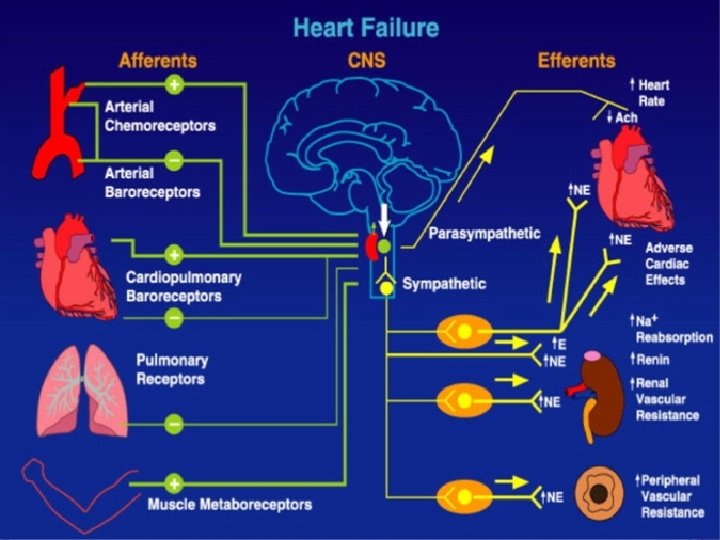
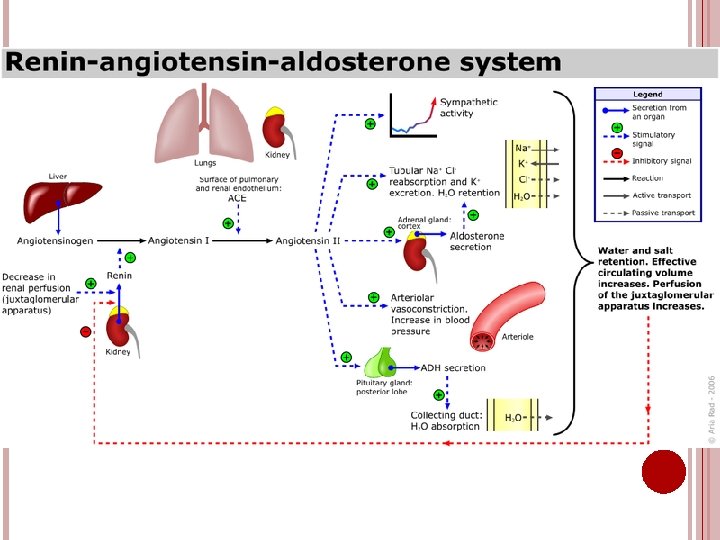
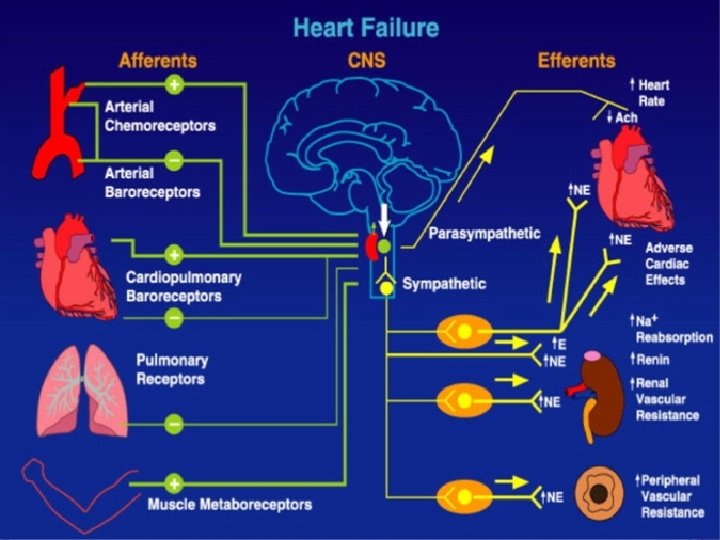
NEURO-HORMONAL ACTIVATION. Renin-Angiotensin-Aldosterone Sympathetic System. Nervous System Activation.
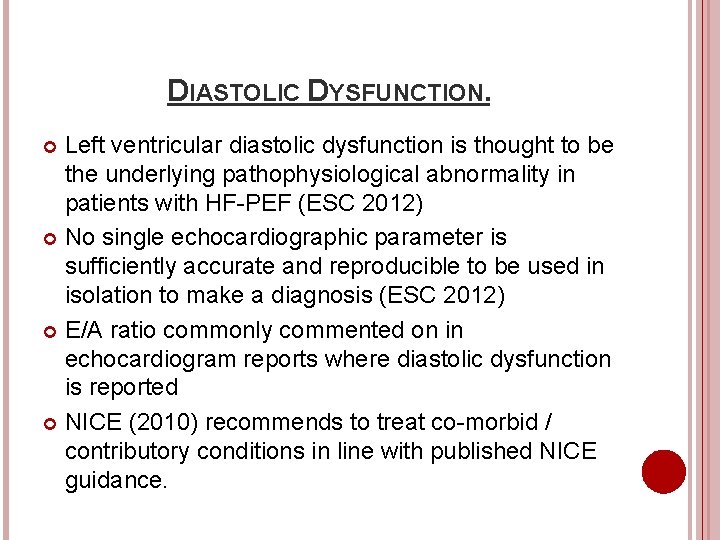
DIASTOLIC DYSFUNCTION. Left ventricular diastolic dysfunction is thought to be the underlying pathophysiological abnormality in patients with HF-PEF (ESC 2012) No single echocardiographic parameter is sufficiently accurate and reproducible to be used in isolation to make a diagnosis (ESC 2012) E/A ratio commonly commented on in echocardiogram reports where diastolic dysfunction is reported NICE (2010) recommends to treat co-morbid / contributory conditions in line with published NICE guidance.
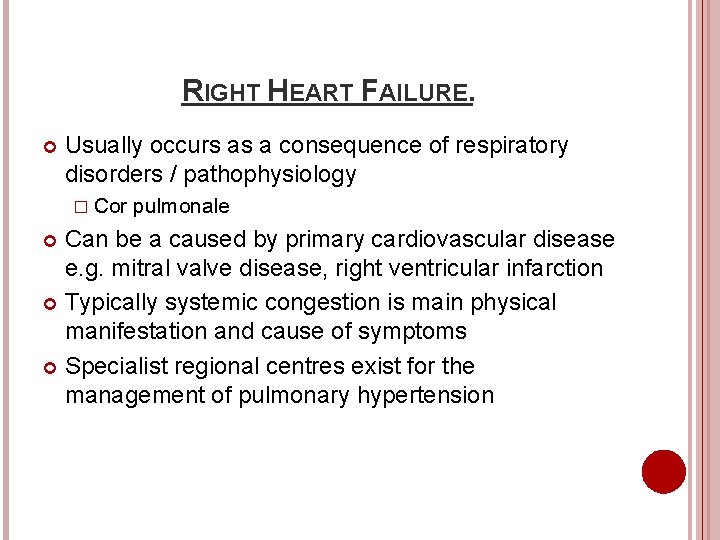
RIGHT HEART FAILURE. Usually occurs as a consequence of respiratory disorders / pathophysiology � Cor pulmonale Can be a caused by primary cardiovascular disease e. g. mitral valve disease, right ventricular infarction Typically systemic congestion is main physical manifestation and cause of symptoms Specialist regional centres exist for the management of pulmonary hypertension
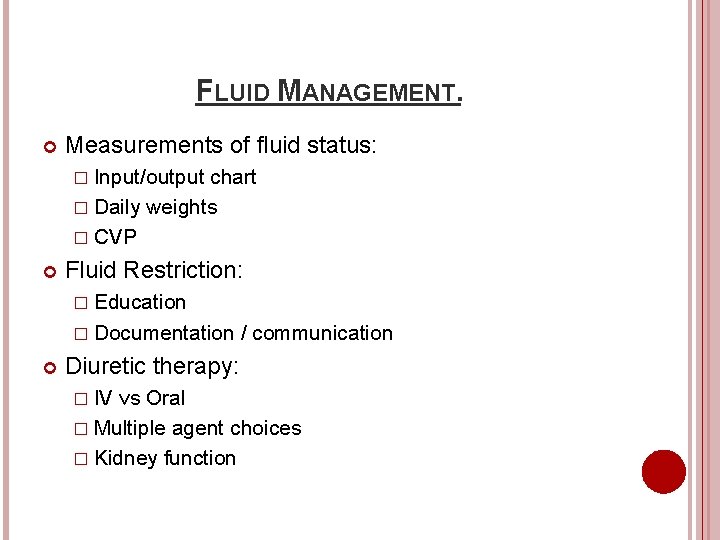
FLUID MANAGEMENT. Measurements of fluid status: � Input/output chart � Daily weights � CVP Fluid Restriction: � Education � Documentation / communication Diuretic therapy: � IV vs Oral � Multiple agent choices � Kidney function
HAEMODYNAMIC ALTERATIONS. Patients with cardiac conditions may experience: � High / low blood pressure � Fast / slow heart rates Questions to consider: � What are the patients normal parameters? � Are they compromised by abnormal findings? � What is their NEWS score, may this be adjusted for long term condition? Most importantly remember: � Documentation � Communication � Planning

CASE STUDY 1. 29 year old male MHX: Dilated cardiomyopathy (alcoholic), Chronic kidney disease, CRT-D. Echo: LVEF 20%, dilated left ventricle and atrium, trivial valve disease. Recent hospital admission, attending surgery for medication review: � SOB – NYHA III � Fatigue � Orthopnea � PND
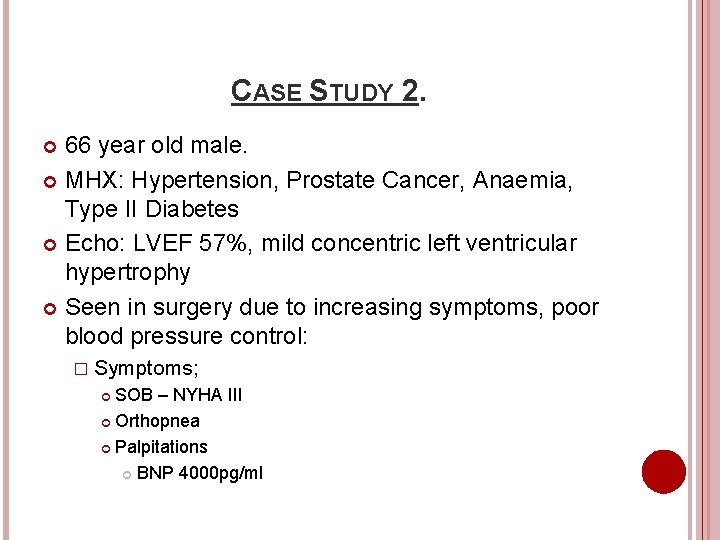
CASE STUDY 2. 66 year old male. MHX: Hypertension, Prostate Cancer, Anaemia, Type II Diabetes Echo: LVEF 57%, mild concentric left ventricular hypertrophy Seen in surgery due to increasing symptoms, poor blood pressure control: � Symptoms; SOB – NYHA III Orthopnea Palpitations BNP 4000 pg/ml
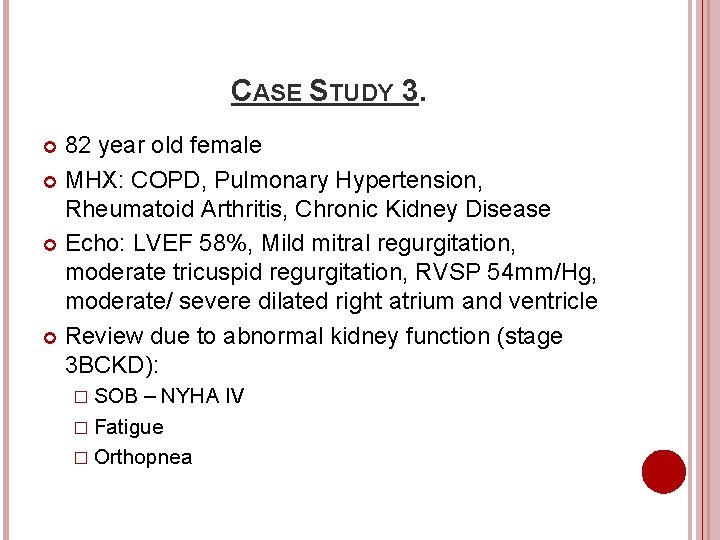
CASE STUDY 3. 82 year old female MHX: COPD, Pulmonary Hypertension, Rheumatoid Arthritis, Chronic Kidney Disease Echo: LVEF 58%, Mild mitral regurgitation, moderate tricuspid regurgitation, RVSP 54 mm/Hg, moderate/ severe dilated right atrium and ventricle Review due to abnormal kidney function (stage 3 BCKD): � SOB – NYHA IV � Fatigue � Orthopnea
ANY QUESTIONS?

REFERENCES / RESOURCES. Askoxylakis. Email V, Thieke C, Pleger S, Most P, Tanner J, Lindel K, Katus H, Debus J, Bischof M 2010 Long-term survival of cancer patients compared to heart failure and stroke: A systematic review 10: 105 BMC Cancer Gardner RS, Mc. Donagh TA, Walker NL 2007 Oxford Specialist Handbooks in Cardiology – Heart Failure Oxford: Oxford University Press Mc. Donagh TA, RS Gardner, AL Clark and H Dargie 2011 Oxford Textbook of Heart Failure Oxford: Oxford University Press Mc. Murray, JJ, S Adampoulos, SD Anker et al ESC Committee for Practice Guidelines 2012 ESC guidelines for the diagnosis and treatment of chronic heart failure European Heart Journal 33 (14) 1787 -1847 National Institute for Health and Clinical Excellence 2010 Chronic heart failure management: London Steed R, Wharton G, Allen J, Chambers J, Graham J, Jones R, Rana B, Masani N 2011 Echocardiography Guidelines for Chamber Quantification British Heart Foundation: London Townsend N, Wickramasinghe K, Bhatnagar P, Smolina K, Nichols M, Leal J, Luengo-Fernandez R, Rayner M 2012 Coronary heart disease statistics 2012 edition. British Heart Foundation: London.
 Ductile fracture vs brittle fracture
Ductile fracture vs brittle fracture Capture beat
Capture beat Failure to sense
Failure to sense British heart foundation aims and objectives
British heart foundation aims and objectives Heart failure
Heart failure Cardiomegay
Cardiomegay Acute vs chronic heart failure
Acute vs chronic heart failure Cor pulmonale
Cor pulmonale Right sided heart failure
Right sided heart failure Diabetes and heart failure
Diabetes and heart failure Congestive heart failure zones for management
Congestive heart failure zones for management Dr nienkemper
Dr nienkemper Heart failure defined
Heart failure defined Heart failure cells are seen in lungs
Heart failure cells are seen in lungs Heart failure complications
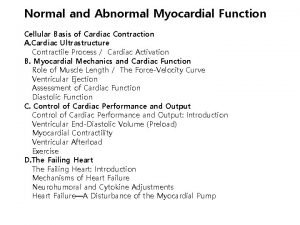
Heart failure complications Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Keith rn heart failure case study
Keith rn heart failure case study Lmnop heart failure
Lmnop heart failure New york scale heart failure
New york scale heart failure Heart failure forward vs backward
Heart failure forward vs backward Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Forrester classification heart failure
Forrester classification heart failure