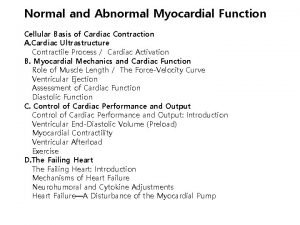
Heart Failure medication Types of Heart Failure Systolic

- Slides: 23
Heart Failure: medication
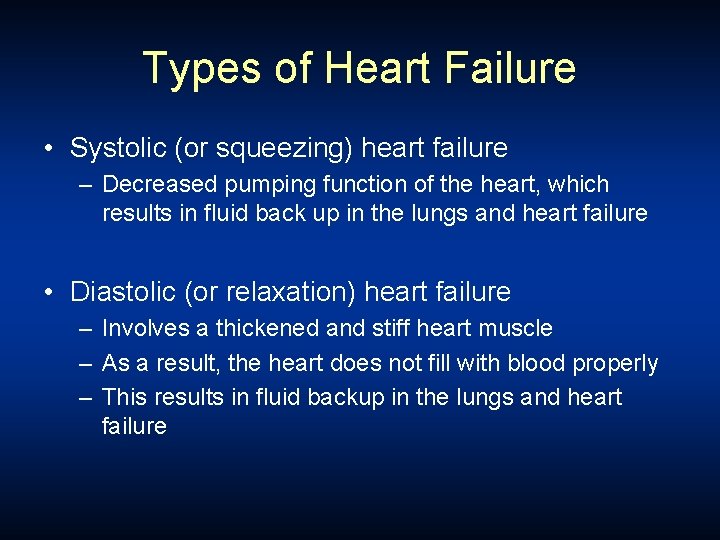
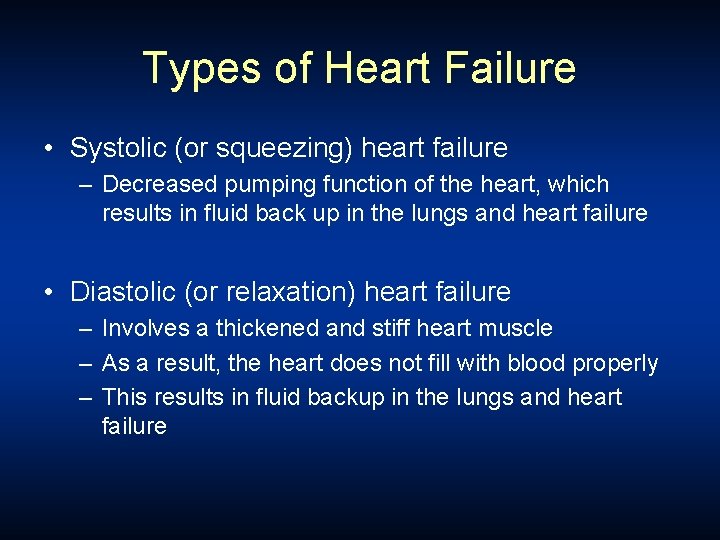
Types of Heart Failure • Systolic (or squeezing) heart failure – Decreased pumping function of the heart, which results in fluid back up in the lungs and heart failure • Diastolic (or relaxation) heart failure – Involves a thickened and stiff heart muscle – As a result, the heart does not fill with blood properly – This results in fluid backup in the lungs and heart failure
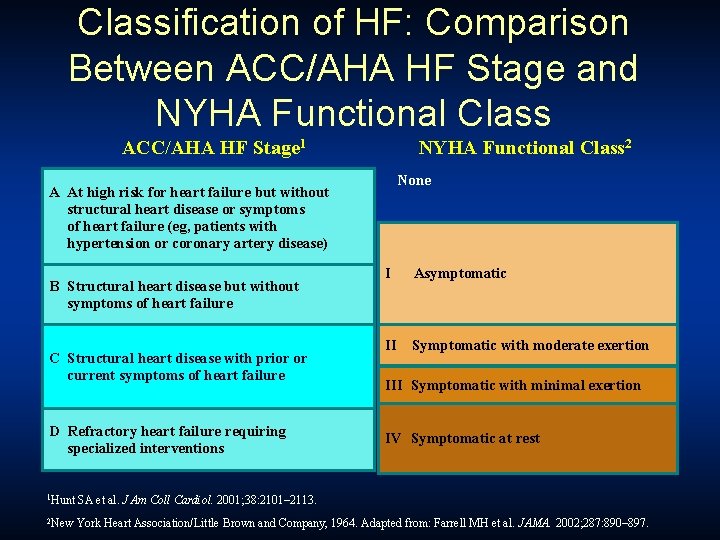
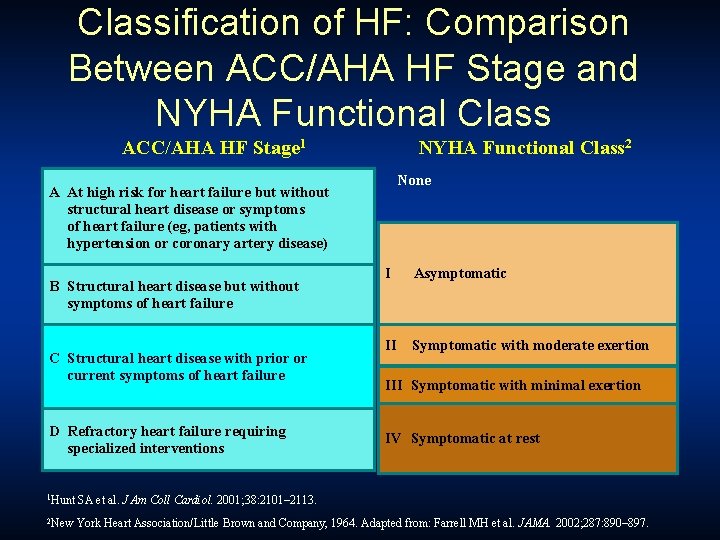
Classification of HF: Comparison Between ACC/AHA HF Stage and NYHA Functional Class ACC/AHA HF Stage 1 NYHA Functional Class 2 None A At high risk for heart failure but without structural heart disease or symptoms of heart failure (eg, patients with hypertension or coronary artery disease) B Structural heart disease but without symptoms of heart failure C Structural heart disease with prior or current symptoms of heart failure D Refractory heart failure requiring specialized interventions I Asymptomatic II Symptomatic with moderate exertion III Symptomatic with minimal exertion IV Symptomatic at rest 1 Hunt SA et al. J Am Coll Cardiol. 2001; 38: 2101– 2113. 2 New York Heart Association/Little Brown and Company, 1964. Adapted from: Farrell MH et al. JAMA. 2002; 287: 890– 897.
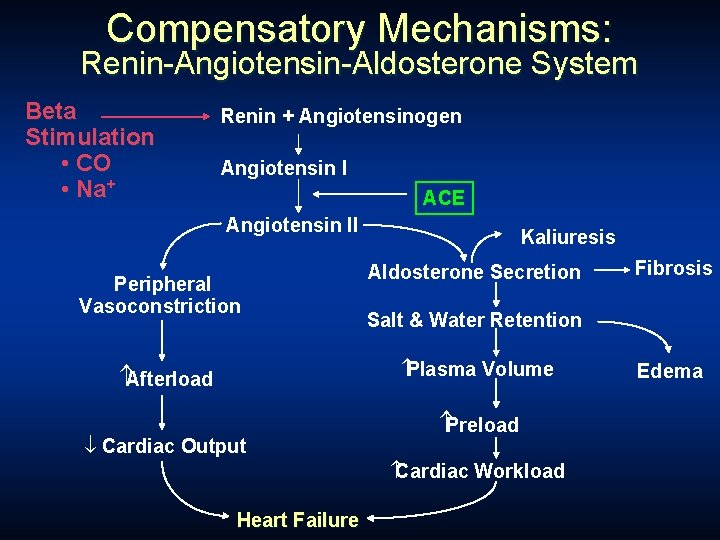
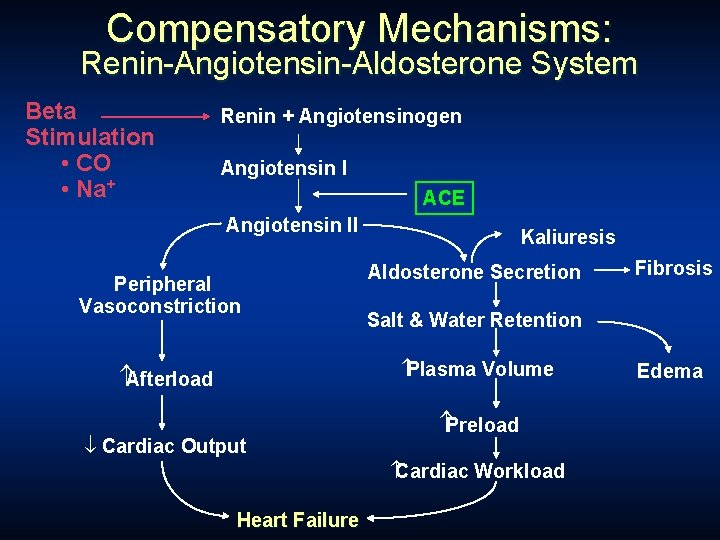
Compensatory Mechanisms: Renin-Angiotensin-Aldosterone System Beta Stimulation • CO • Na+ Renin + Angiotensinogen Angiotensin I ACE Angiotensin II Peripheral Vasoconstriction Kaliuresis Aldosterone Secretion Salt & Water Retention Plasma Volume Afterload ¯ Cardiac Output Preload Cardiac Workload Heart Failure Fibrosis Edema

Drug Therapy
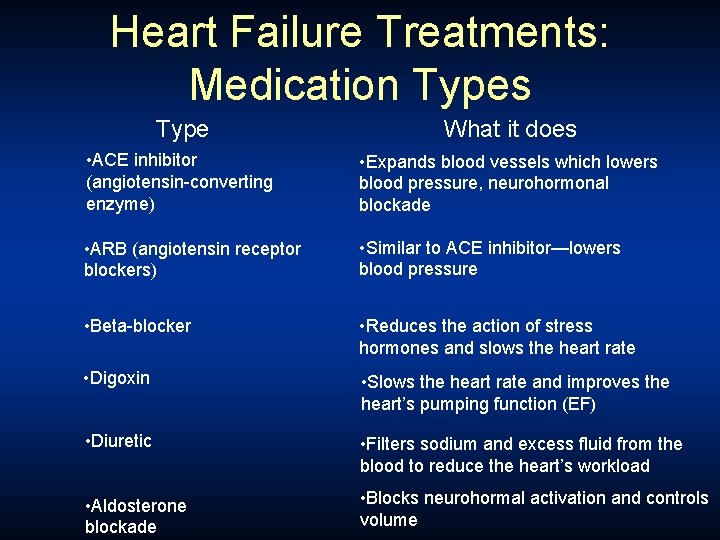
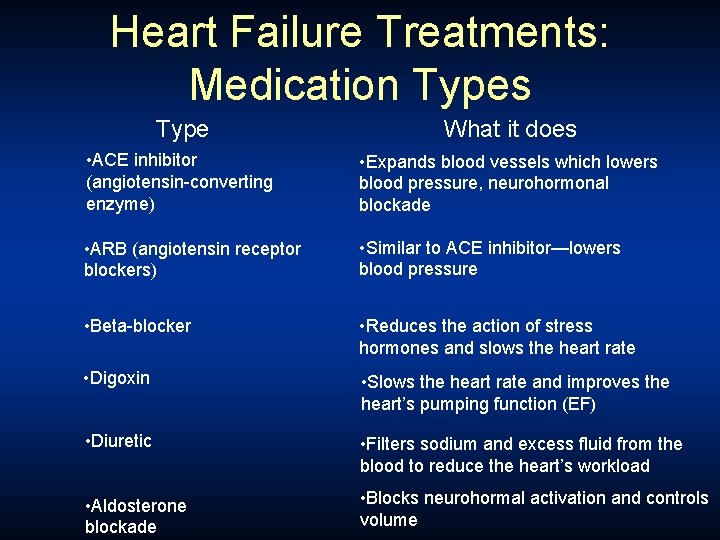
Heart Failure Treatments: Medication Types Type What it does • ACE inhibitor (angiotensin-converting enzyme) • Expands blood vessels which lowers blood pressure, neurohormonal blockade • ARB (angiotensin receptor blockers) • Similar to ACE inhibitor—lowers blood pressure • Beta-blocker • Reduces the action of stress hormones and slows the heart rate • Digoxin • Slows the heart rate and improves the heart’s pumping function (EF) • Diuretic • Filters sodium and excess fluid from the blood to reduce the heart’s workload • Aldosterone blockade • Blocks neurohormal activation and controls volume
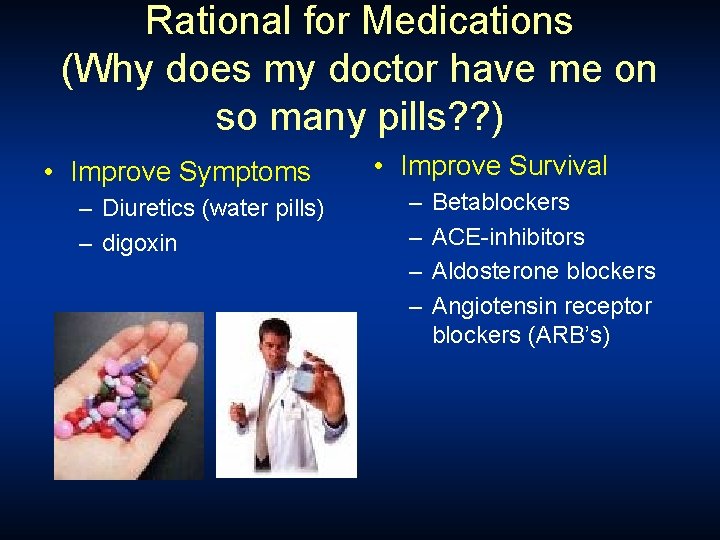
Rational for Medications (Why does my doctor have me on so many pills? ? ) • Improve Symptoms – Diuretics (water pills) – digoxin • Improve Survival – – Betablockers ACE-inhibitors Aldosterone blockers Angiotensin receptor blockers (ARB’s)
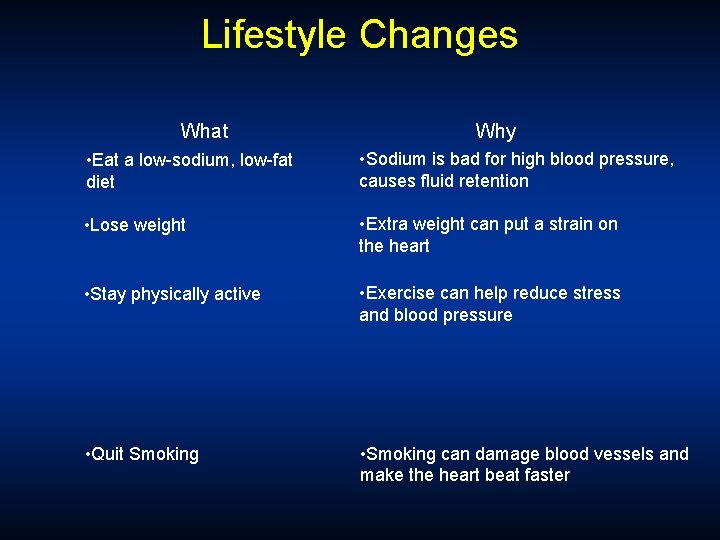
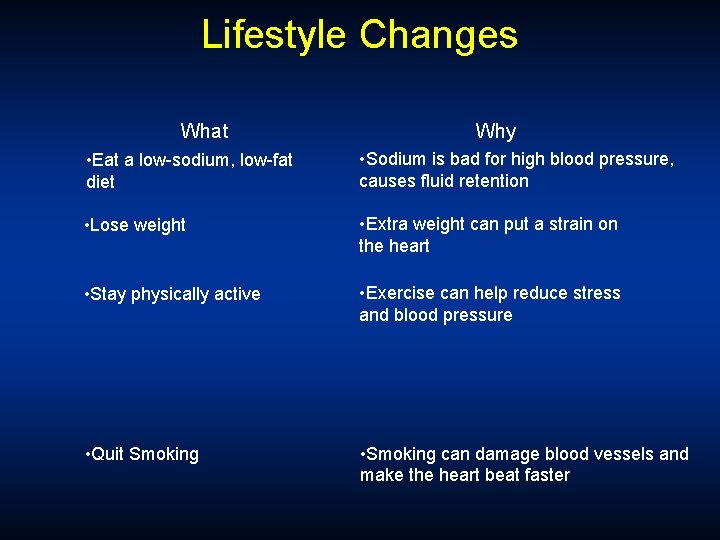
Lifestyle Changes What Why • Eat a low-sodium, low-fat diet • Sodium is bad for high blood pressure, causes fluid retention • Lose weight • Extra weight can put a strain on the heart • Stay physically active • Exercise can help reduce stress and blood pressure • Quit Smoking • Smoking can damage blood vessels and make the heart beat faster
1. АСЕ inhibitors
ACE inhibitors reduce pre- and afterload They are administered in lower doses alone or together with diuretics, cardiac glycoside, antiischemic agents, etc. in all stages of CHF, due to systolic dysfunction.
2. Thiazides and loop diuretics They increase salt and water loss, reduce blood volume and lower excessive venous filling pressure, reduce circulating blood volume and preload. The congestive features of oedema, in the lungs and periphery, are alleviated, cardiac output is also increased.
3. Cardiac glycosides (CGs)
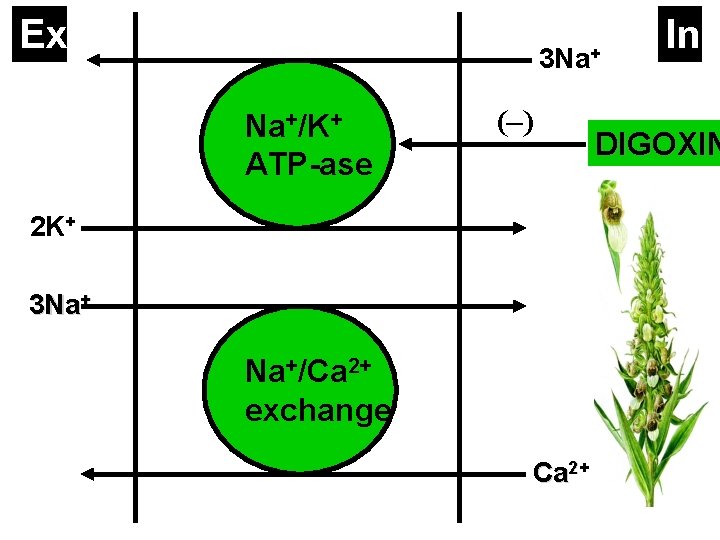
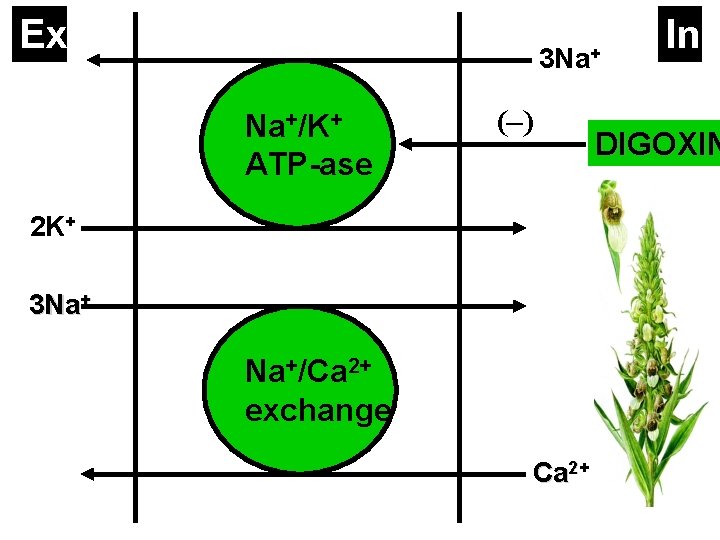
Ex 3 Na+ Na+/K+ ATP-ase (–) 2 K+ 3 Na+ Na+/Ca 2+ exchange Ca 2+ In DIGOXIN
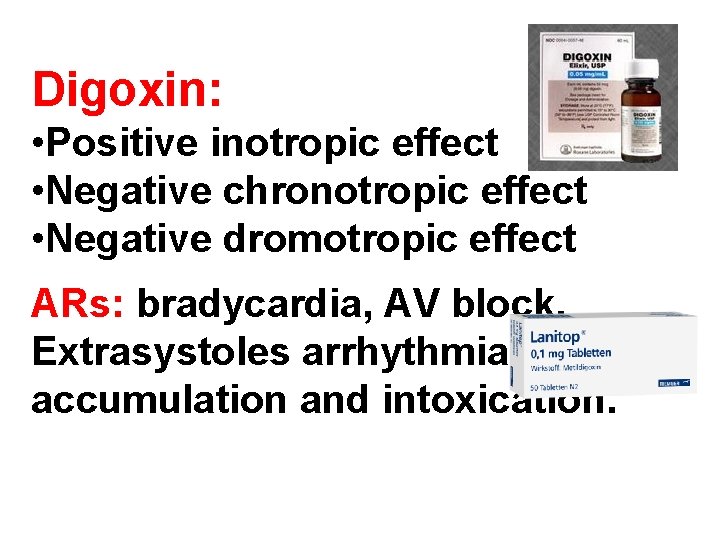
Digoxin: • Positive inotropic effect • Negative chronotropic effect • Negative dromotropic effect ARs: bradycardia, AV block, Extrasystoles arrhythmias, accumulation and intoxication.
Potassium and calcium have antagonistic a Hypokalemia and hypercalcemia potentiate the action of CGs.
CGs are effective in CHF, occuring wi normal or accelerated heart rhythm, especially in cases of atrial fibrillation Digoxin (t 1/2 40 h): p. o. or i. v.
4. Aldosterone antagonists In cases of severe heart failure low doses of Spironolactone are added to therapy while regularly checking creatinin and electrolyte levels. Spironolactone is a weak diuretic. It blocks aldosterone receptors in the distal renal tubules and reduces increased aldosterone levels in CHF.
In low doses (25 mg/24 h) Spironolactone potentiates the effects of ACE inhibitors. It also saves K+ and Mg 2+ and has antiarrhythmic activity. Spironolactone prevents myocardial fibrosis, caused by aldosterone, and in this way increases myocardial contractility. Similar to spironolactone is another aldosterone antagonist – Eplerenone.
5. Beta- and alpha-blocking agents Carvedilol is a blocker of β- and α- receptors. It also has antioxidant, vasodila and cardioprotective effects. It decreases cardiac output, peripheral vascular resista and afterload. Carvedilol lowers mortality with 25– 67%, but it is contraindicated in C occuring with cor pulmonale. The treatme begins with low doses (3. 125 mg/12 h).
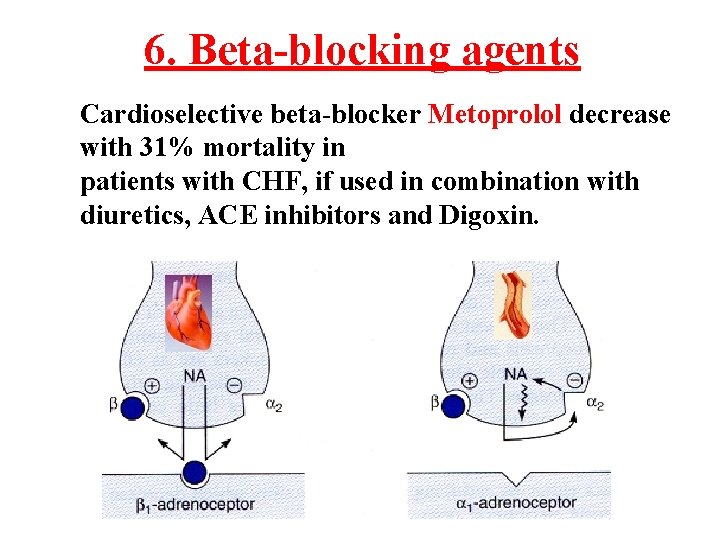
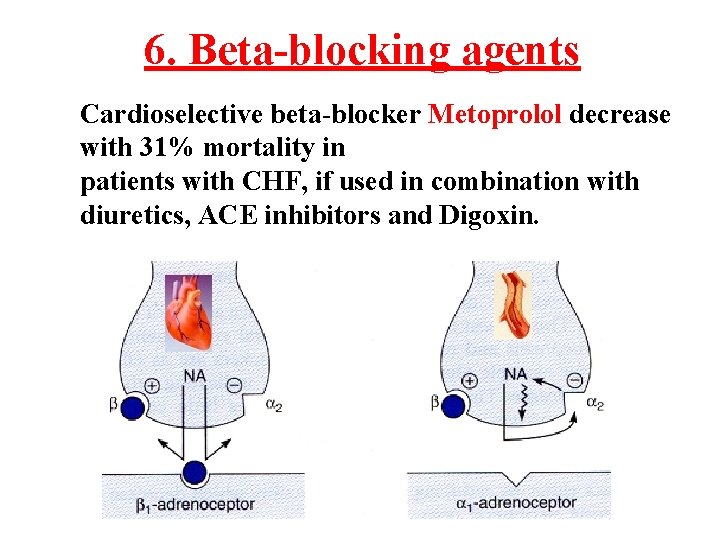
6. Beta-blocking agents Cardioselective beta-blocker Metoprolol decrease with 31% mortality in patients with CHF, if used in combination with diuretics, ACE inhibitors and Digoxin.
In congestive left-ventricular heart failure Isosorbide dinitrate and Isosorbide-5 -mononitrate are prescribed. To prevent tolerance development are necessary – 12 hours intervals without nitrates
Modern medicine often disproves this saying. “The heart never stops. When it stops, it stops forever”. Leonardo da Vinci
 Failure to capture vs failure to sense ecg
Failure to capture vs failure to sense ecg Supparerk vision center
Supparerk vision center Cup cone failure
Cup cone failure Systolic and diastolic pressure
Systolic and diastolic pressure End-diastolic volume vs end-systolic volume
End-diastolic volume vs end-systolic volume Stroke volume
Stroke volume Sam systolic anterior motion
Sam systolic anterior motion Ejection systolic murmur causes
Ejection systolic murmur causes Heart vowel sound
Heart vowel sound Pcwp
Pcwp Systolic over diastolic
Systolic over diastolic Systolic mm hg
Systolic mm hg Ps murmur
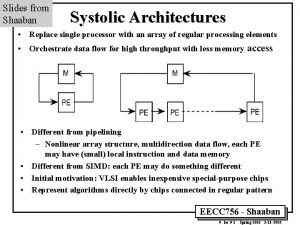
Ps murmur Systolic array vs simd
Systolic array vs simd Trunctus
Trunctus Systolic array
Systolic array Av shunt
Av shunt Isolated systolic hypertension
Isolated systolic hypertension What is systolic and diastolic pressure
What is systolic and diastolic pressure Why systolic architectures
Why systolic architectures Heart failure and frank starling law
Heart failure and frank starling law Classification of ejection fraction
Classification of ejection fraction Heart failure definition
Heart failure definition New york scale heart failure
New york scale heart failure