Heart Failure Clinical Reasoning Case Study Keith Rischer
- Slides: 41
Heart Failure Clinical Reasoning Case Study Keith Rischer, RN, MA, CEN, CCRN
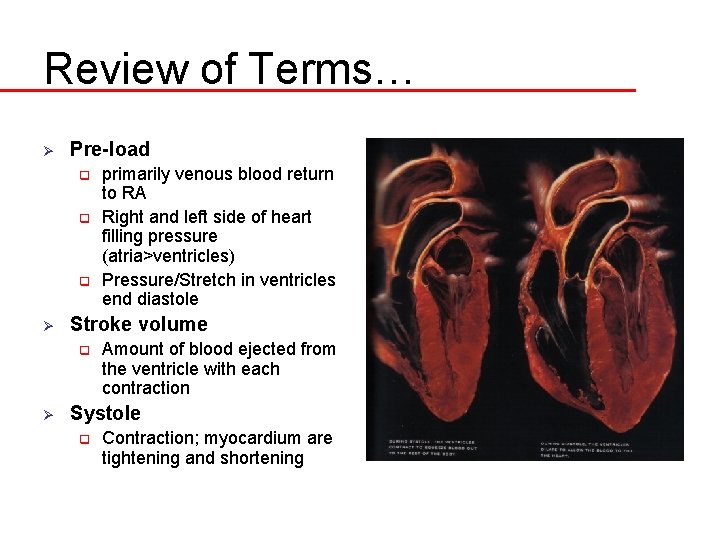
Review of Terms… Ø Pre-load q q q Ø Stroke volume q Ø primarily venous blood return to RA Right and left side of heart filling pressure (atria>ventricles) Pressure/Stretch in ventricles end diastole Amount of blood ejected from the ventricle with each contraction Systole q Contraction; myocardium are tightening and shortening
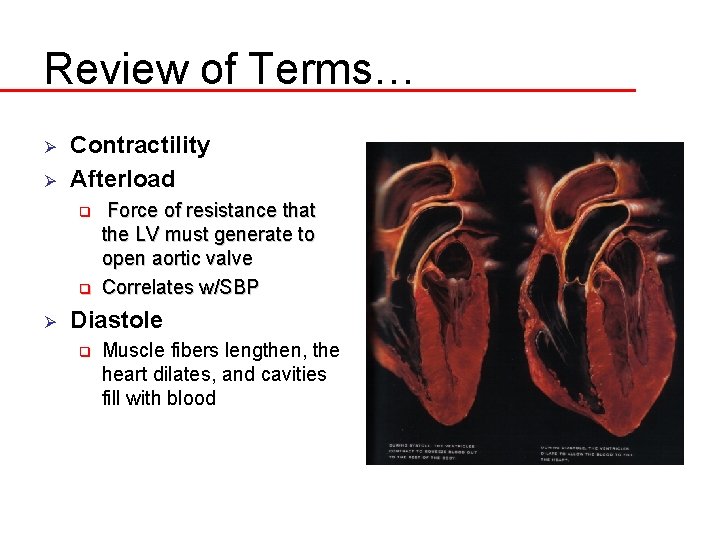
Review of Terms… Ø Ø Contractility Afterload q q Ø Force of resistance that the LV must generate to open aortic valve Correlates w/SBP Diastole q Muscle fibers lengthen, the heart dilates, and cavities fill with blood
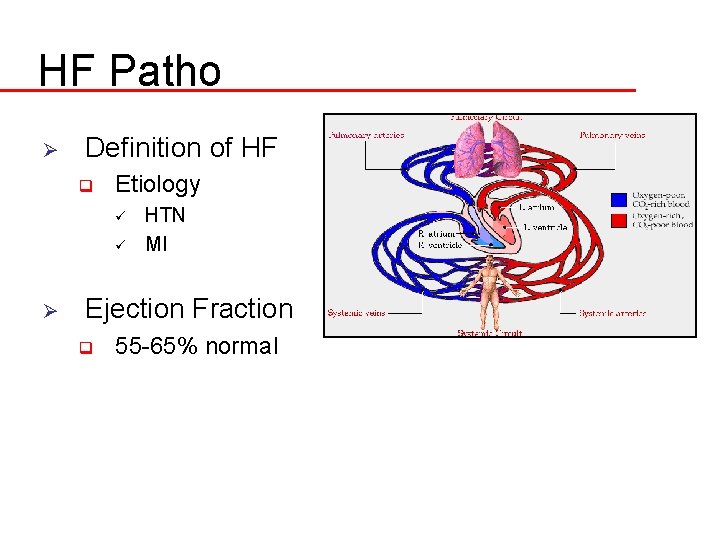
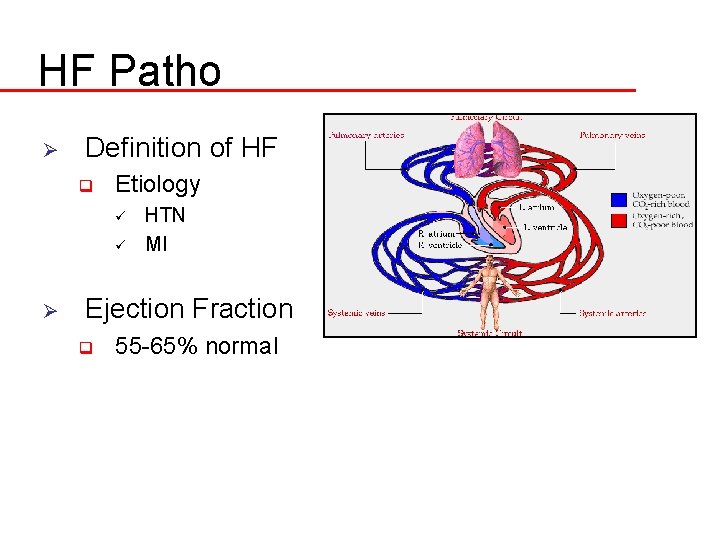
HF Patho Ø Definition of HF q Etiology ü ü Ø HTN MI Ejection Fraction q 55 -65% normal
Compensatory Mechanisms in CHF Ø Ø Increased Sympathetic Nervous System Stimulation Renin-angiotensin system activation Natriuretic peptides q BNP Ventricular hypertrophy
Types of HF Ø Systolic vs. Diastolic Systolic q Diastolic q Ø Left sided vs. Right sided q Lt sided ü ü q HTN & MI Cardiomyopathy Rt sided ü COPD
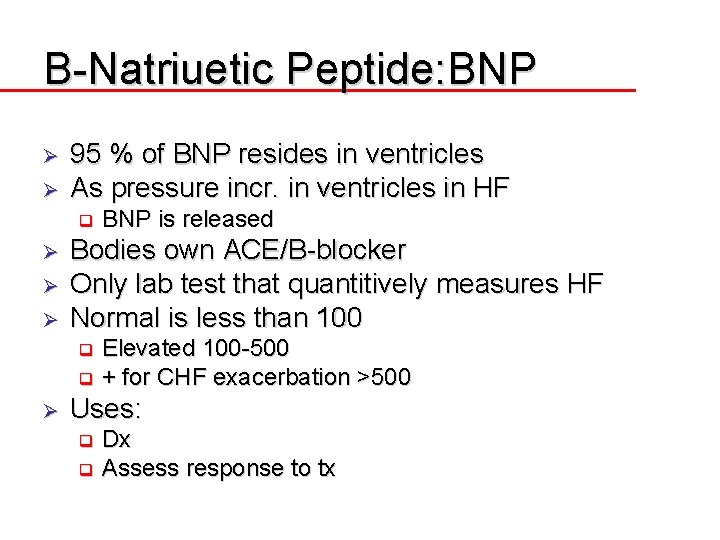
B-Natriuetic Peptide: BNP Ø Ø 95 % of BNP resides in ventricles As pressure incr. in ventricles in HF q Ø Ø Ø BNP is released Bodies own ACE/B-blocker Only lab test that quantitively measures HF Normal is less than 100 Elevated 100 -500 q + for CHF exacerbation >500 q Ø Uses: Dx q Assess response to tx q
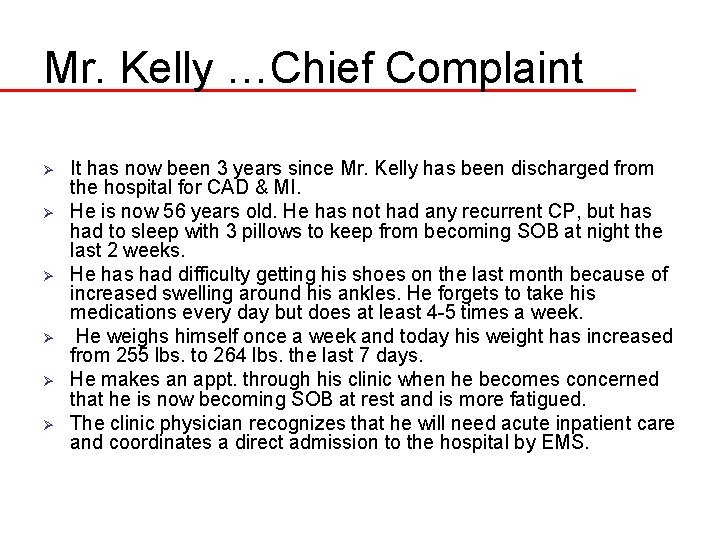
Mr. Kelly …Chief Complaint Ø Ø Ø It has now been 3 years since Mr. Kelly has been discharged from the hospital for CAD & MI. He is now 56 years old. He has not had any recurrent CP, but has had to sleep with 3 pillows to keep from becoming SOB at night the last 2 weeks. He has had difficulty getting his shoes on the last month because of increased swelling around his ankles. He forgets to take his medications every day but does at least 4 -5 times a week. He weighs himself once a week and today his weight has increased from 255 lbs. to 264 lbs. the last 7 days. He makes an appt. through his clinic when he becomes concerned that he is now becoming SOB at rest and is more fatigued. The clinic physician recognizes that he will need acute inpatient care and coordinates a direct admission to the hospital by EMS.
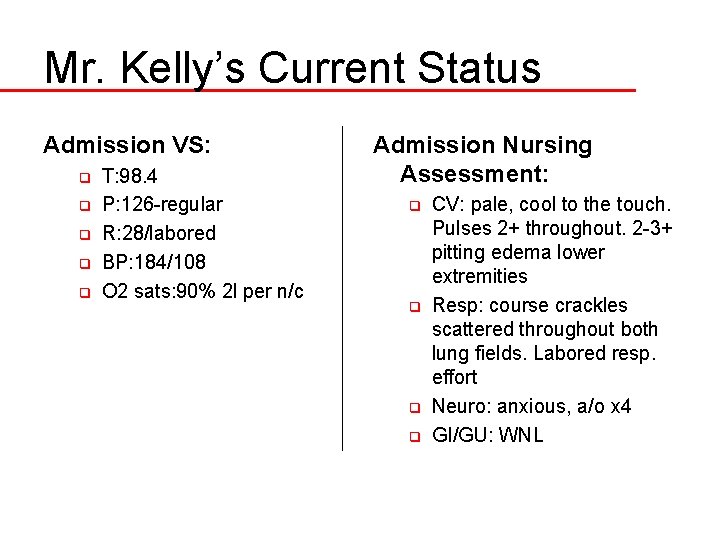
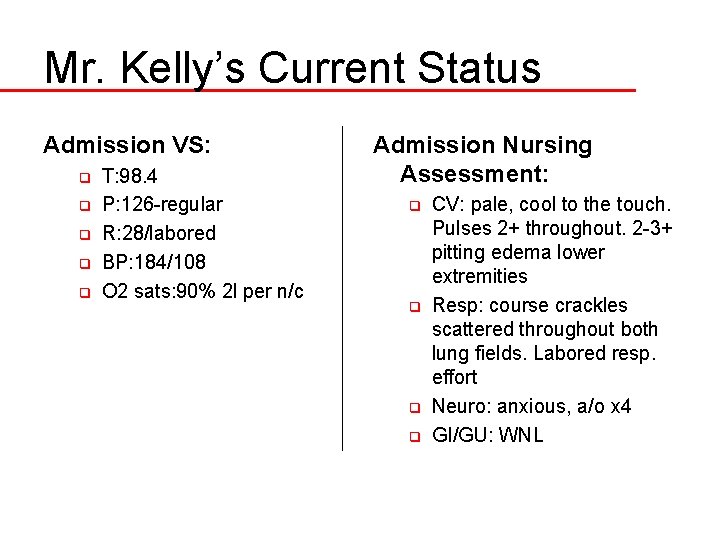
Mr. Kelly’s Current Status Admission VS: q q q T: 98. 4 P: 126 -regular R: 28/labored BP: 184/108 O 2 sats: 90% 2 l per n/c Admission Nursing Assessment: q q CV: pale, cool to the touch. Pulses 2+ throughout. 2 -3+ pitting edema lower extremities Resp: course crackles scattered throughout both lung fields. Labored resp. effort Neuro: anxious, a/o x 4 GI/GU: WNL
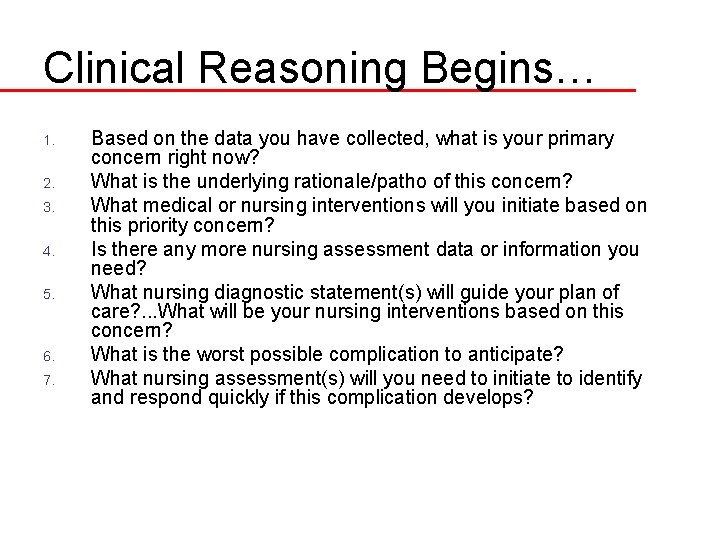
Clinical Reasoning Begins… 1. 2. 3. 4. 5. 6. 7. Based on the data you have collected, what is your primary concern right now? What is the underlying rationale/patho of this concern? What medical or nursing interventions will you initiate based on this priority concern? Is there any more nursing assessment data or information you need? What nursing diagnostic statement(s) will guide your plan of care? . . . What will be your nursing interventions based on this concern? What is the worst possible complication to anticipate? What nursing assessment(s) will you need to initiate to identify and respond quickly if this complication develops?
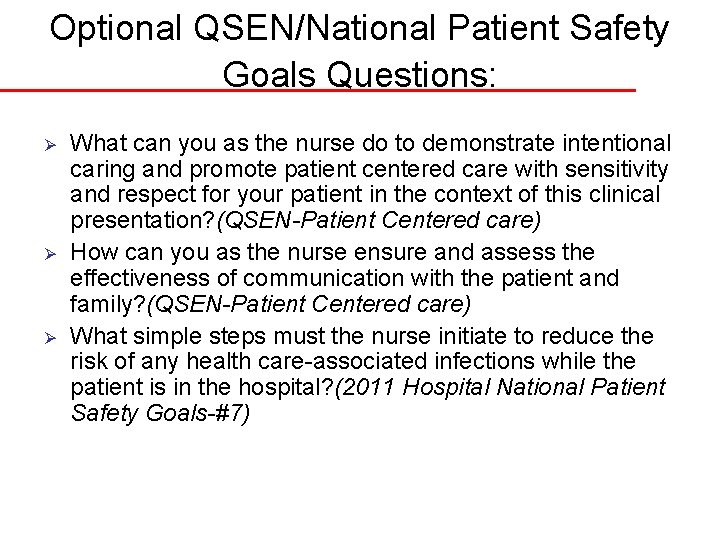
Optional QSEN/National Patient Safety Goals Questions: Ø Ø Ø What can you as the nurse do to demonstrate intentional caring and promote patient centered care with sensitivity and respect for your patient in the context of this clinical presentation? (QSEN-Patient Centered care) How can you as the nurse ensure and assess the effectiveness of communication with the patient and family? (QSEN-Patient Centered care) What simple steps must the nurse initiate to reduce the risk of any health care-associated infections while the patient is in the hospital? (2011 Hospital National Patient Safety Goals-#7)
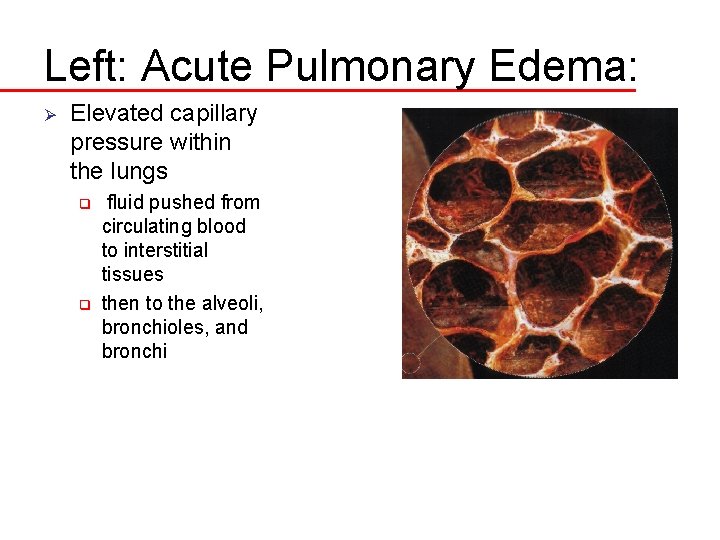
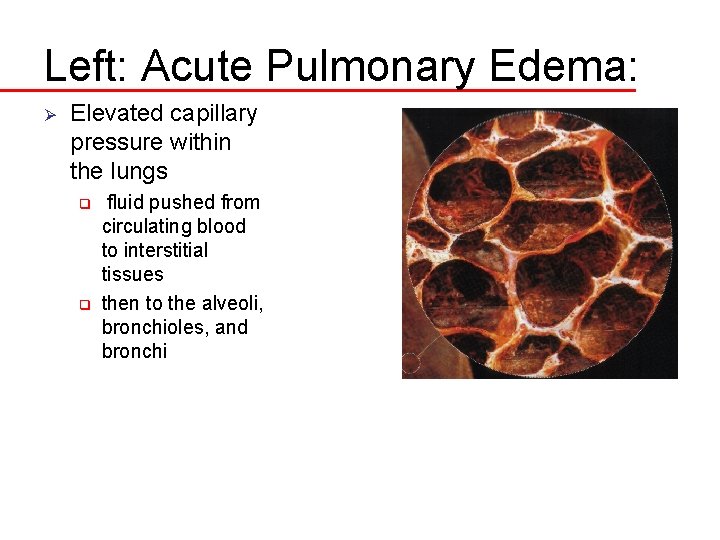
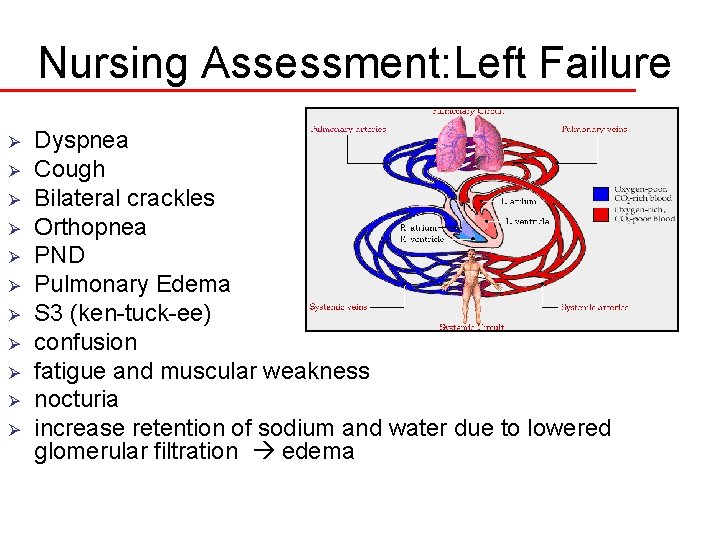
Left: Acute Pulmonary Edema: Ø Elevated capillary pressure within the lungs q q fluid pushed from circulating blood to interstitial tissues then to the alveoli, bronchioles, and bronchi
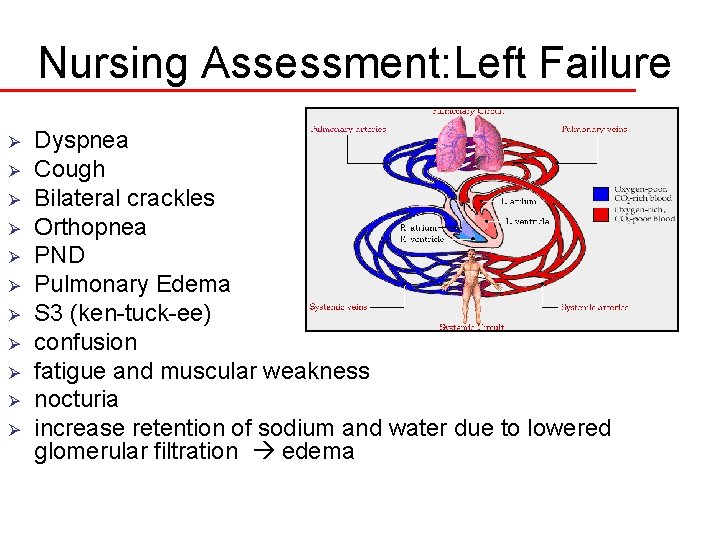
Nursing Assessment: Left Failure Ø Ø Ø Dyspnea Cough Bilateral crackles Orthopnea PND Pulmonary Edema S 3 (ken-tuck-ee) confusion fatigue and muscular weakness nocturia increase retention of sodium and water due to lowered glomerular filtration edema
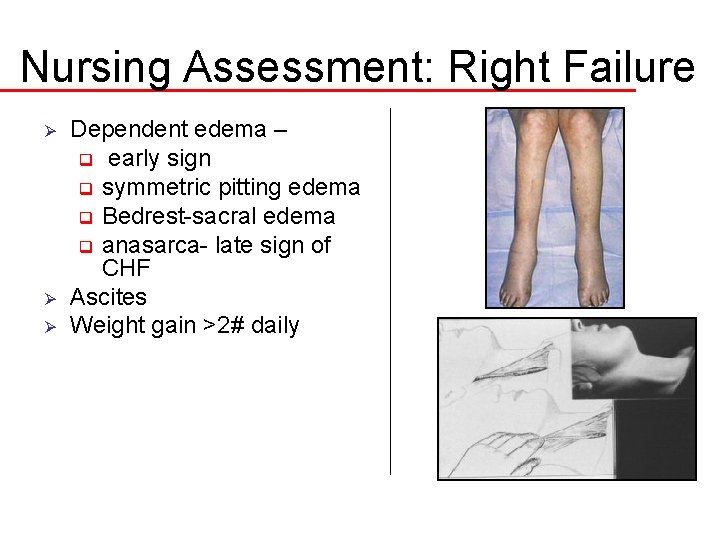
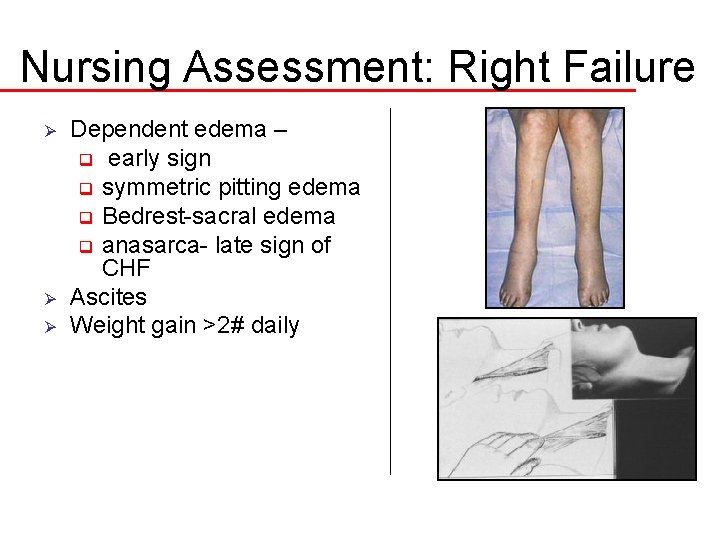
Nursing Assessment: Right Failure Ø Ø Ø Dependent edema – q early sign q symmetric pitting edema q Bedrest-sacral edema q anasarca- late sign of CHF Ascites Weight gain >2# daily
Name Mr. Kelly’s HF 10. What type of HF does Mr. Kelly likely have based on his previous documented history? 11. What clinical manifestations did Mr. Kelly present with that are consistent with biventricular HF? 12. What are other manifestations that also can be seen in HF?
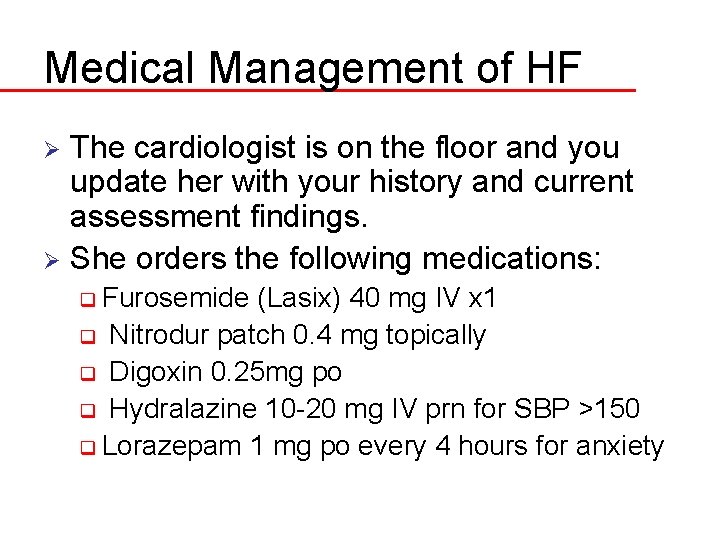
Medical Management of HF The cardiologist is on the floor and you update her with your history and current assessment findings. Ø She orders the following medications: Ø q Furosemide (Lasix) 40 mg IV x 1 q Nitrodur patch 0. 4 mg topically q Digoxin 0. 25 mg po q Hydralazine 10 -20 mg IV prn for SBP >150 q Lorazepam 1 mg po every 4 hours for anxiety
HF Medication Rationale 13. Describe the rationale for each of these interventions: q q q Furosemide Nitrodur Digoxin Hydralazine Lorazepam
HF Medication Management Furosemide Nitrodur Ø CATEGORY Ø ACTION Ø SE Ø NSG IMP Ø PT ED
HF Medication Management Digoxin Hydralazine Ø CATEGORY Ø ACTION Ø SE Ø NSG IMP Ø PT ED
HF Medication Management Lorazepam Ø CATEGORY Ø ACTION Ø SE Ø NSG IMP Ø PT ED
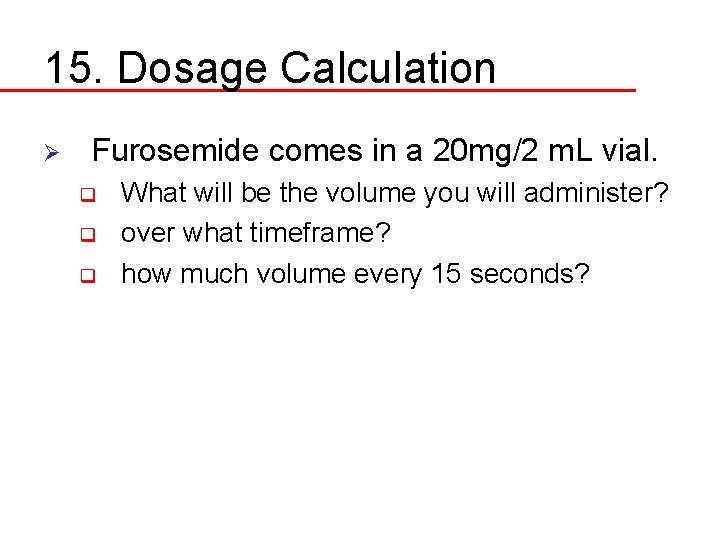
15. Dosage Calculation Ø Furosemide comes in a 20 mg/2 m. L vial. q q q What will be the volume you will administer? over what timeframe? how much volume every 15 seconds?
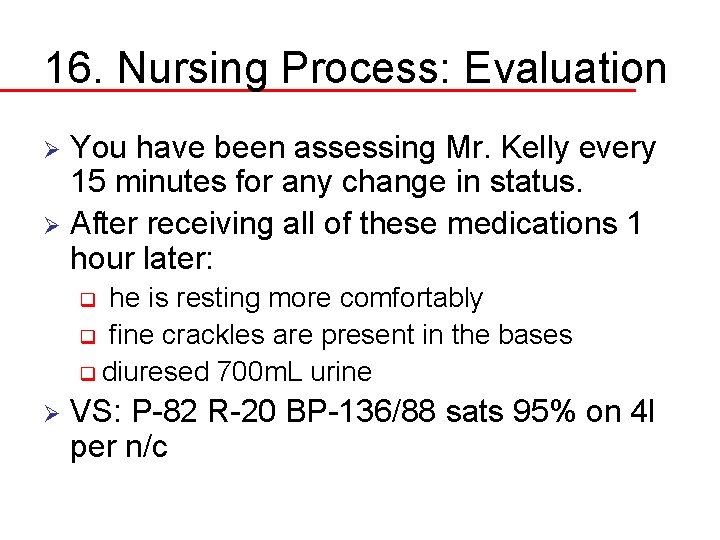
16. Nursing Process: Evaluation You have been assessing Mr. Kelly every 15 minutes for any change in status. Ø After receiving all of these medications 1 hour later: Ø he is resting more comfortably q fine crackles are present in the bases q diuresed 700 m. L urine q Ø VS: P-82 R-20 BP-136/88 sats 95% on 4 l per n/c
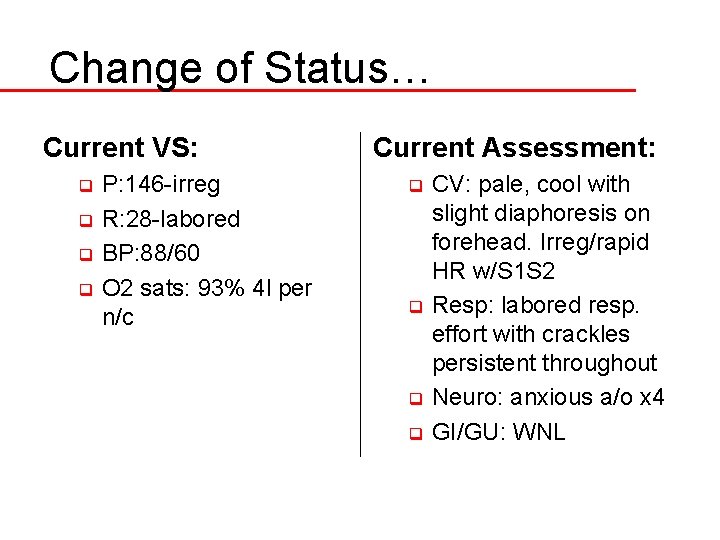
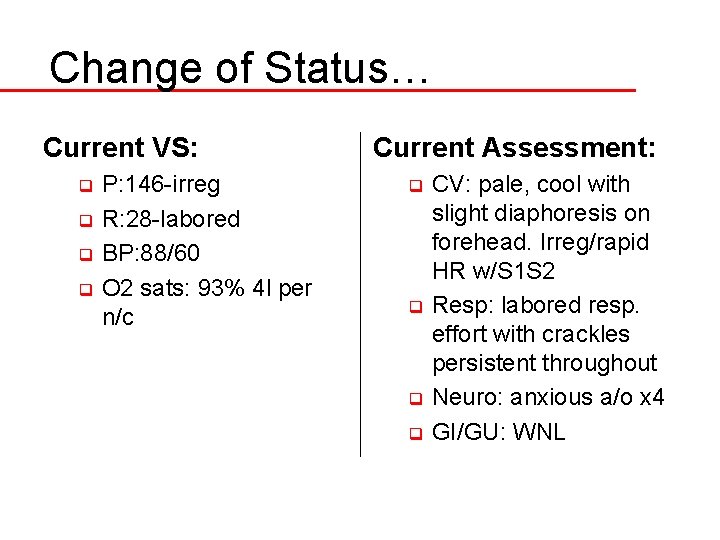
Change of Status… Current VS: P: 146 -irreg q R: 28 -labored q BP: 88/60 q O 2 sats: 93% 4 l per n/c q Current Assessment: CV: pale, cool with slight diaphoresis on forehead. Irreg/rapid HR w/S 1 S 2 q Resp: labored resp. effort with crackles persistent throughout q Neuro: anxious a/o x 4 q GI/GU: WNL q
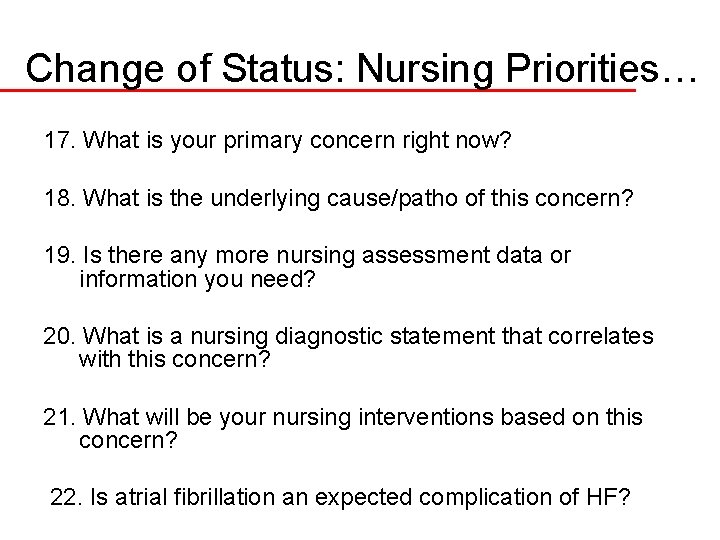
Change of Status: Nursing Priorities… 17. What is your primary concern right now? 18. What is the underlying cause/patho of this concern? 19. Is there any more nursing assessment data or information you need? 20. What is a nursing diagnostic statement that correlates with this concern? 21. What will be your nursing interventions based on this concern? 22. Is atrial fibrillation an expected complication of HF?
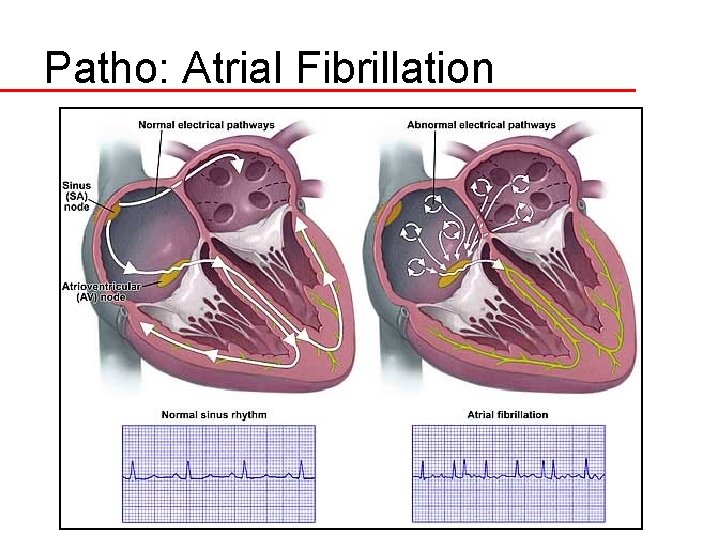
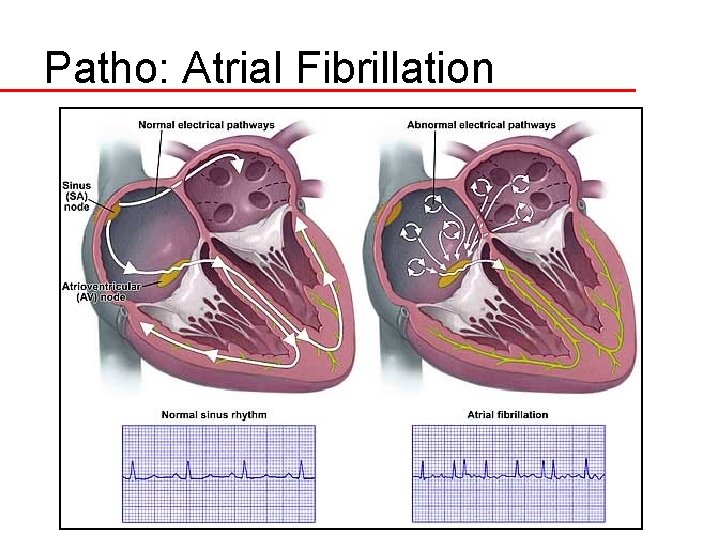
Patho: Atrial Fibrillation
23. Diltiazem (Cardizem) Ø CATEGORY Ø ACTION Ø SE Ø NSG IMP
Dosage Calculation 24. This medication comes in a vial of 25 mg/5 m. L. Ø What will be the dose in m. L you will administer? Ø How quickly can you administer this IV push? Ø How much volume every 15 seconds?
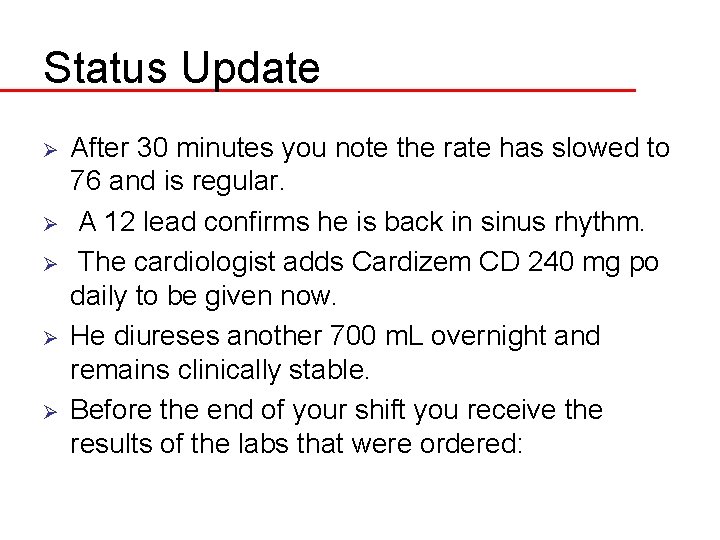
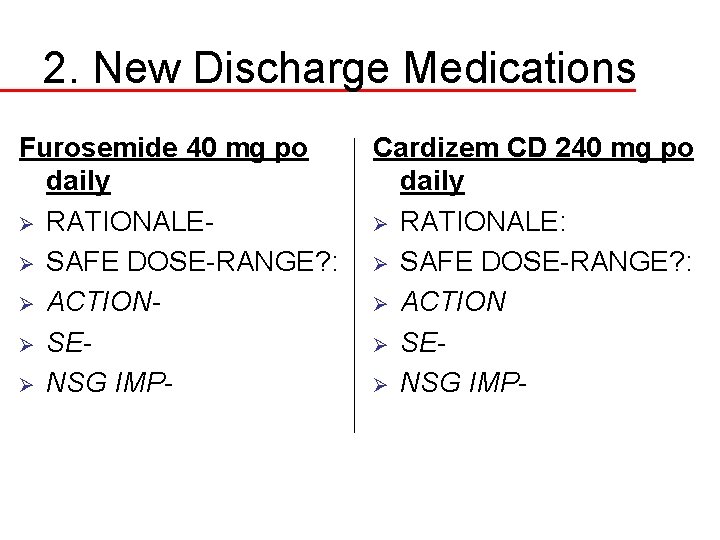
Status Update Ø Ø Ø After 30 minutes you note the rate has slowed to 76 and is regular. A 12 lead confirms he is back in sinus rhythm. The cardiologist adds Cardizem CD 240 mg po daily to be given now. He diureses another 700 m. L overnight and remains clinically stable. Before the end of your shift you receive the results of the labs that were ordered:
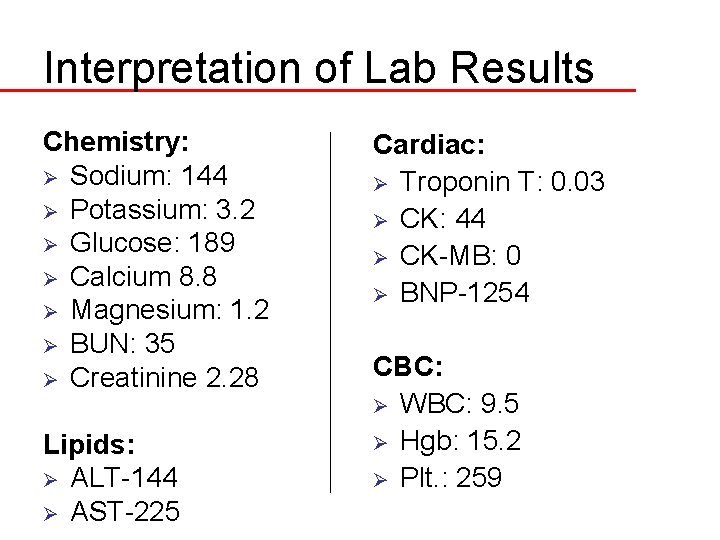
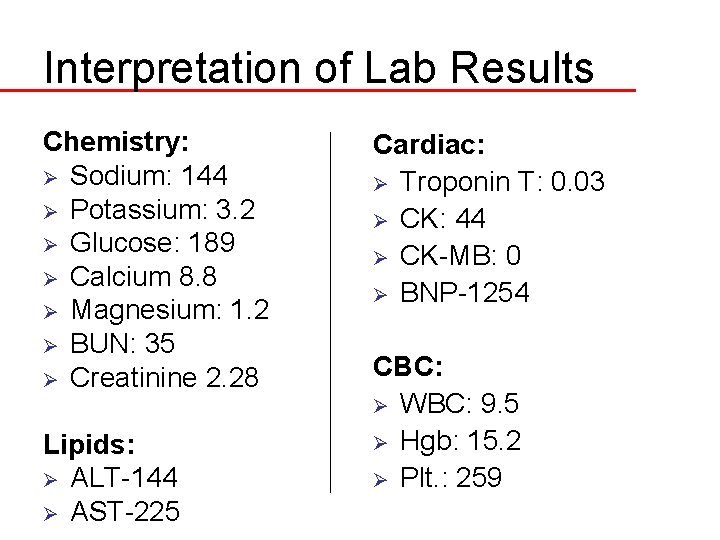
Interpretation of Lab Results Chemistry: Ø Sodium: 144 Ø Potassium: 3. 2 Ø Glucose: 189 Ø Calcium 8. 8 Ø Magnesium: 1. 2 Ø BUN: 35 Ø Creatinine 2. 28 Lipids: Ø ALT-144 Ø AST-225 Cardiac: Ø Troponin T: 0. 03 Ø CK: 44 Ø CK-MB: 0 Ø BNP-1254 CBC: Ø WBC: 9. 5 Ø Hgb: 15. 2 Ø Plt. : 259
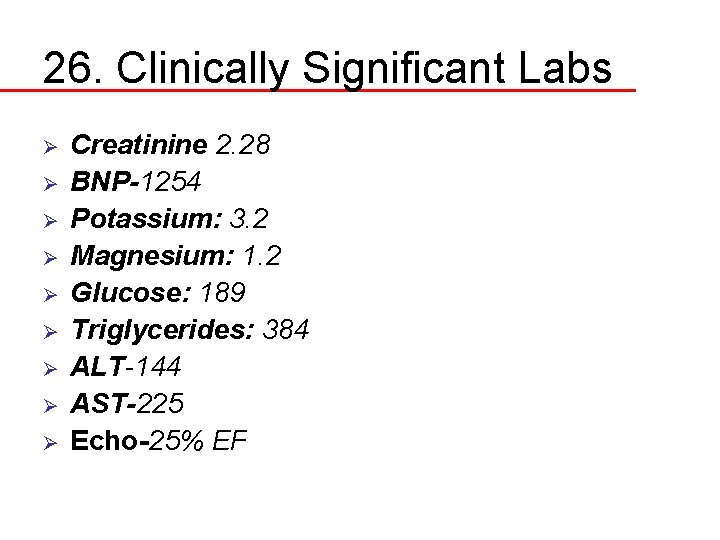
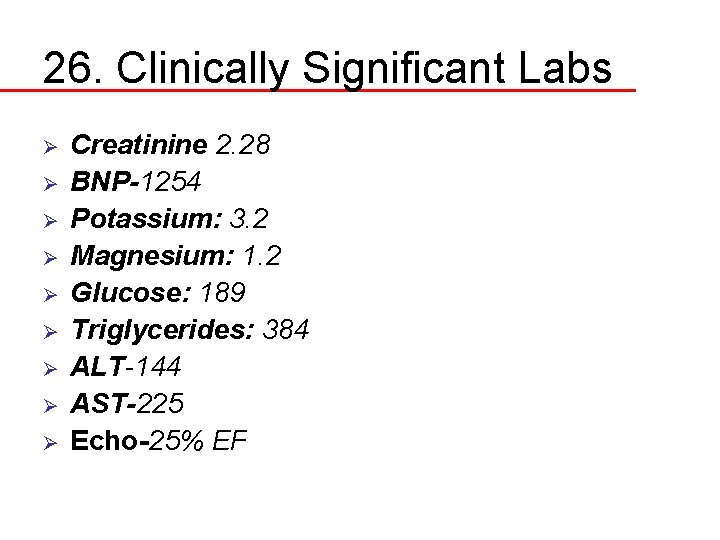
26. Clinically Significant Labs Ø Ø Ø Ø Ø Creatinine 2. 28 BNP-1254 Potassium: 3. 2 Magnesium: 1. 2 Glucose: 189 Triglycerides: 384 ALT-144 AST-225 Echo-25% EF
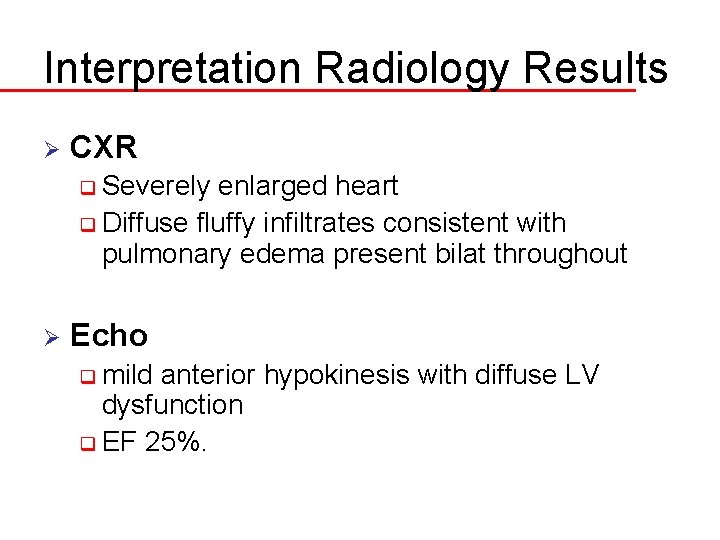
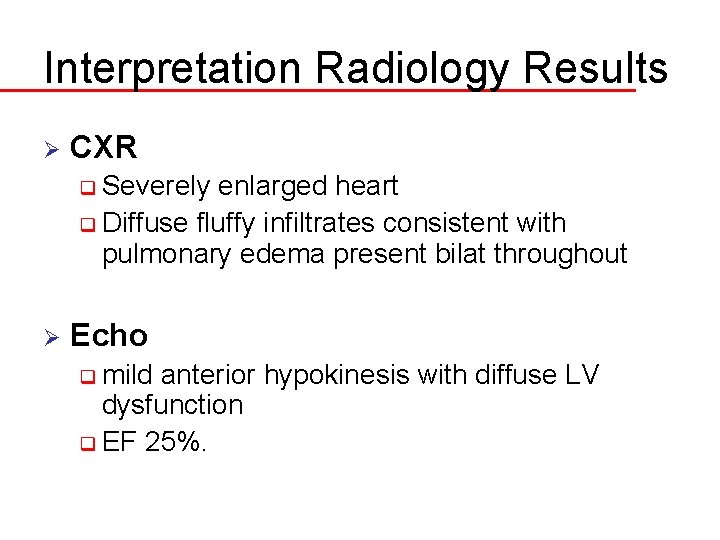
Interpretation Radiology Results Ø CXR q Severely enlarged heart q Diffuse fluffy infiltrates consistent with pulmonary edema present bilat throughout Ø Echo q mild anterior hypokinesis with diffuse LV dysfunction q EF 25%.
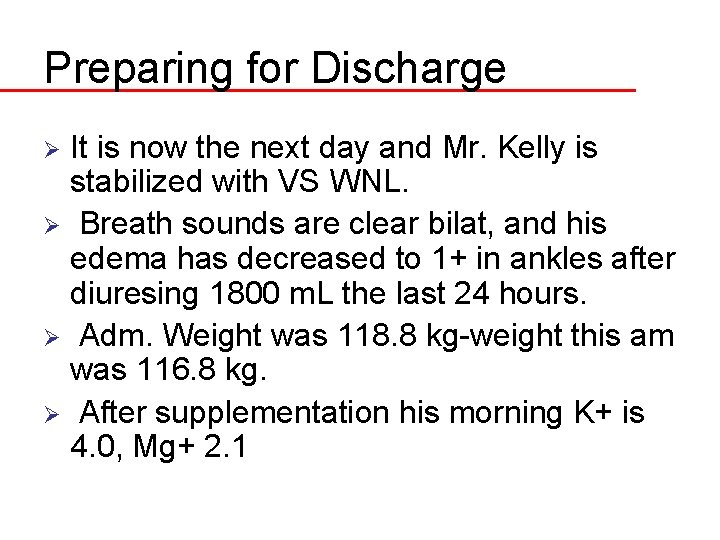
Preparing for Discharge It is now the next day and Mr. Kelly is stabilized with VS WNL. Ø Breath sounds are clear bilat, and his edema has decreased to 1+ in ankles after diuresing 1800 m. L the last 24 hours. Ø Adm. Weight was 118. 8 kg-weight this am was 116. 8 kg. Ø After supplementation his morning K+ is 4. 0, Mg+ 2. 1 Ø
Discharge Priorities 29. He is planned to be discharged to home tomorrow. What are your nursing diagnostic priorities today? 30. What will you emphasize with dietary restrictions and fluid restriction with HF management. 31. What will be the most important education priorities you will reinforce with his new diagnosis of worsening HF?
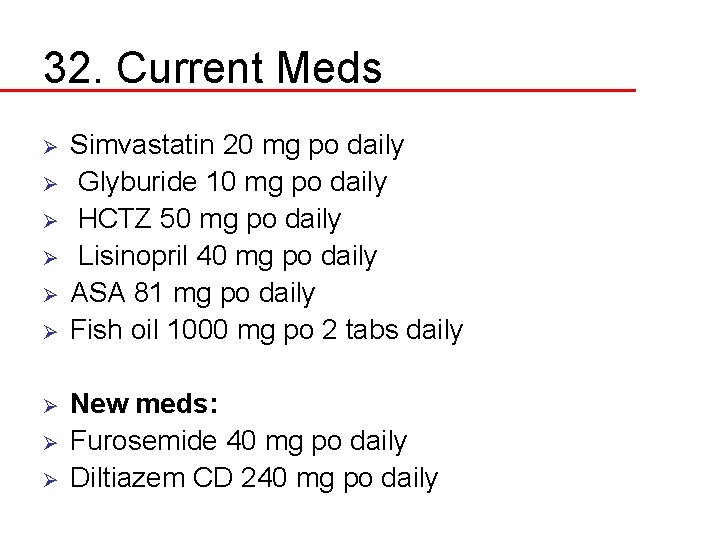
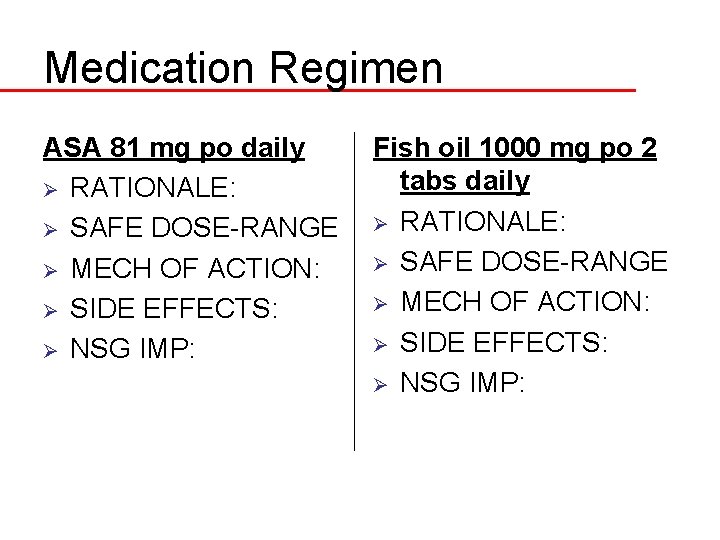
32. Current Meds Ø Ø Ø Ø Ø Simvastatin 20 mg po daily Glyburide 10 mg po daily HCTZ 50 mg po daily Lisinopril 40 mg po daily ASA 81 mg po daily Fish oil 1000 mg po 2 tabs daily New meds: Furosemide 40 mg po daily Diltiazem CD 240 mg po daily
Medication Regimen Simvastatin 20 mg po daily Ø RATIONALE: Ø SAFE DOSE-RANGE Ø MECH OF ACTION: Ø SIDE EFFECTS: Ø NSG IMP: Glyburide 10 mg po daily Ø RATIONALE: Ø SAFE DOSE-RANGE Ø MECH OF ACTION: Ø SIDE EFFECTS: Ø NSG IMP:
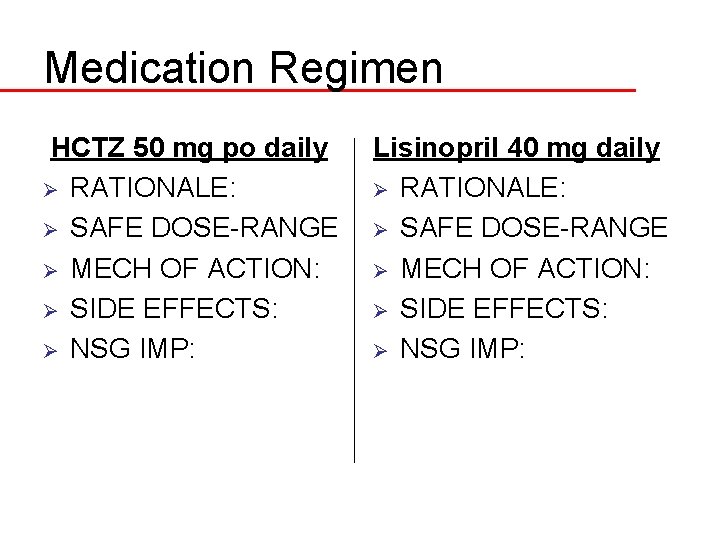
Medication Regimen HCTZ 50 mg po daily Ø RATIONALE: Ø SAFE DOSE-RANGE Ø MECH OF ACTION: Ø SIDE EFFECTS: Ø NSG IMP: Lisinopril 40 mg daily Ø RATIONALE: Ø SAFE DOSE-RANGE Ø MECH OF ACTION: Ø SIDE EFFECTS: Ø NSG IMP:
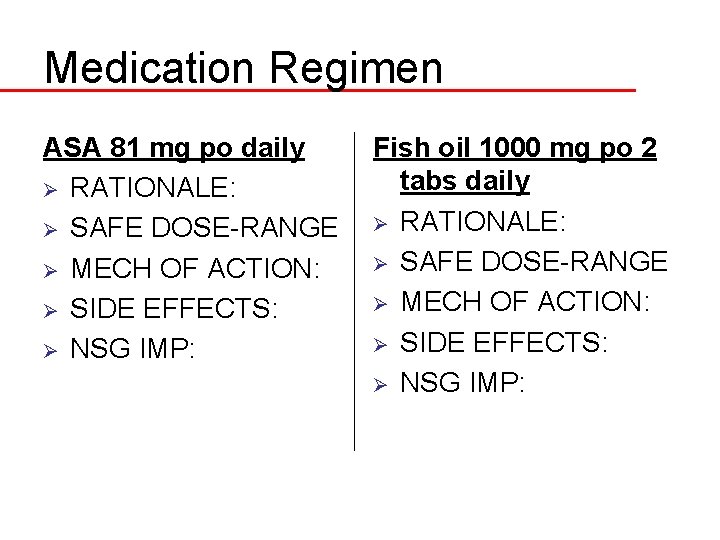
Medication Regimen ASA 81 mg po daily Ø RATIONALE: Ø SAFE DOSE-RANGE Ø MECH OF ACTION: Ø SIDE EFFECTS: Ø NSG IMP: Fish oil 1000 mg po 2 tabs daily Ø RATIONALE: Ø SAFE DOSE-RANGE Ø MECH OF ACTION: Ø SIDE EFFECTS: Ø NSG IMP:
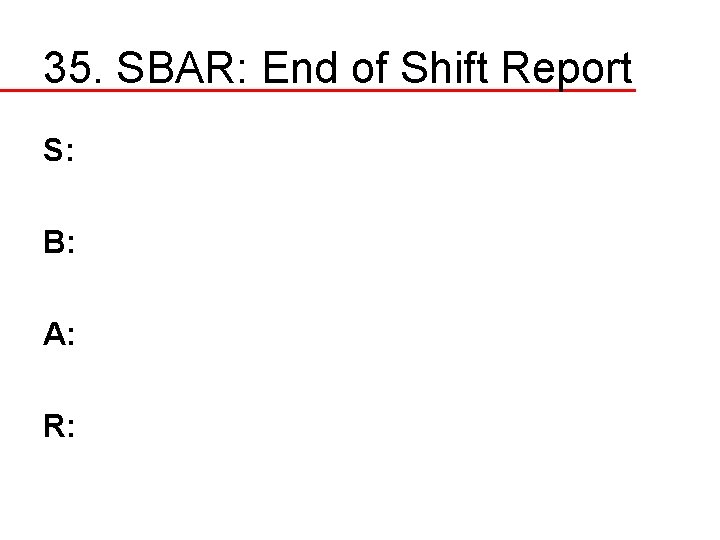
35. SBAR: End of Shift Report S: B: A: R:
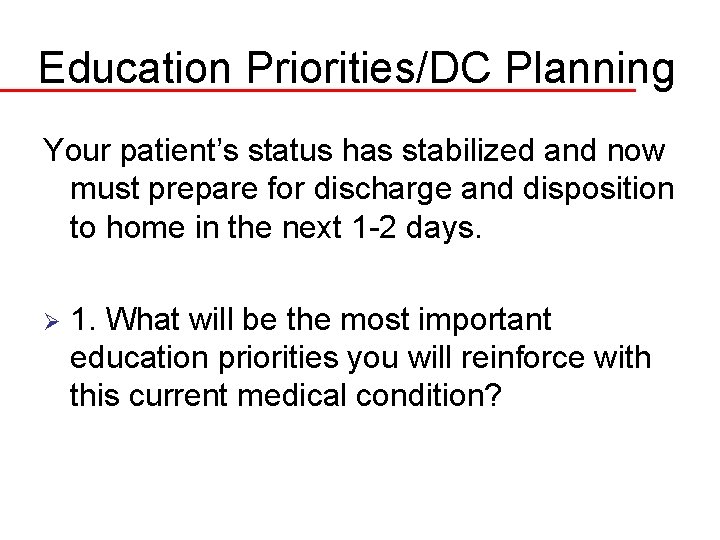
Education Priorities/DC Planning Your patient’s status has stabilized and now must prepare for discharge and disposition to home in the next 1 -2 days. Ø 1. What will be the most important education priorities you will reinforce with this current medical condition?
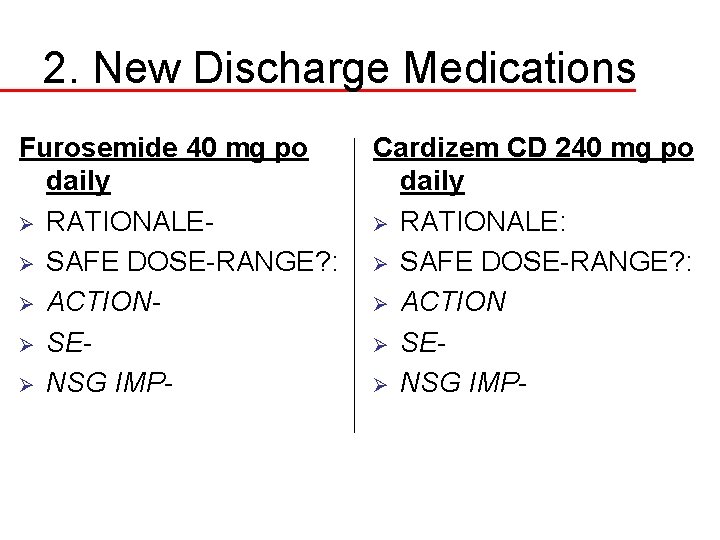
2. New Discharge Medications Furosemide 40 mg po daily Ø RATIONALEØ SAFE DOSE-RANGE? : Ø ACTIONØ SEØ NSG IMP- Cardizem CD 240 mg po daily Ø RATIONALE: Ø SAFE DOSE-RANGE? : Ø ACTION Ø SEØ NSG IMP-
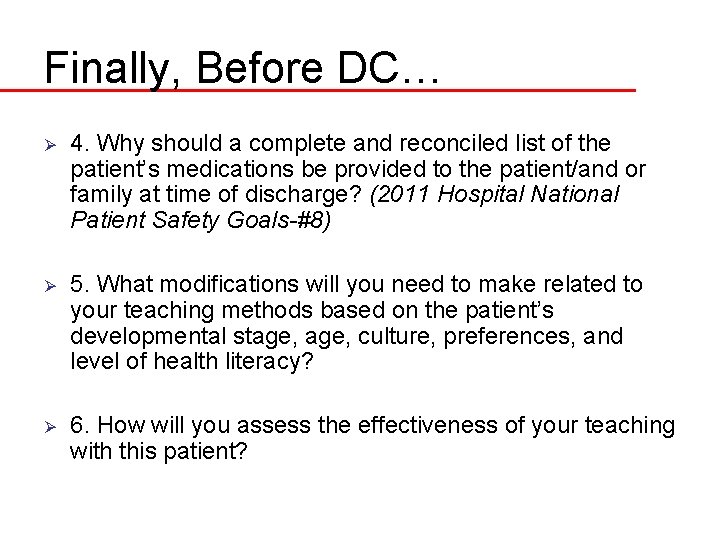
Finally, Before DC… Ø 4. Why should a complete and reconciled list of the patient’s medications be provided to the patient/and or family at time of discharge? (2011 Hospital National Patient Safety Goals-#8) Ø 5. What modifications will you need to make related to your teaching methods based on the patient’s developmental stage, culture, preferences, and level of health literacy? Ø 6. How will you assess the effectiveness of your teaching with this patient?