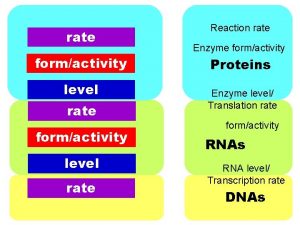
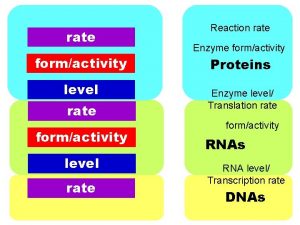
Enterovirus Myocarditis Nonenterovirus Myocarditis RATE STRAIN KAI STRAIN






































- Slides: 48






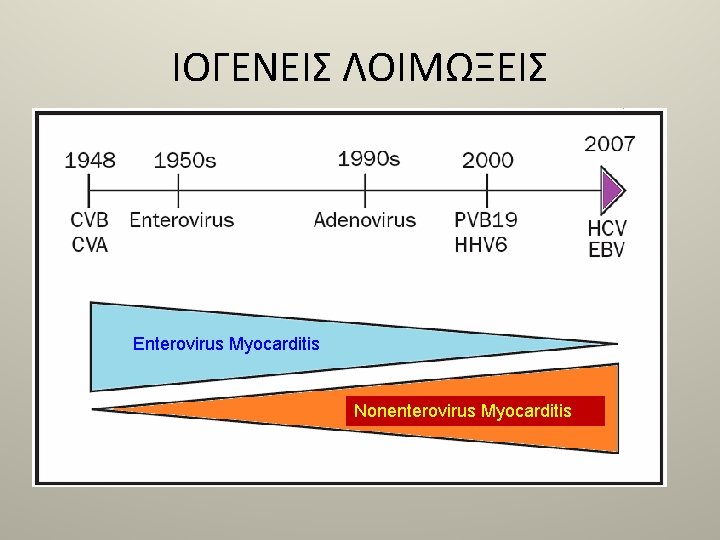
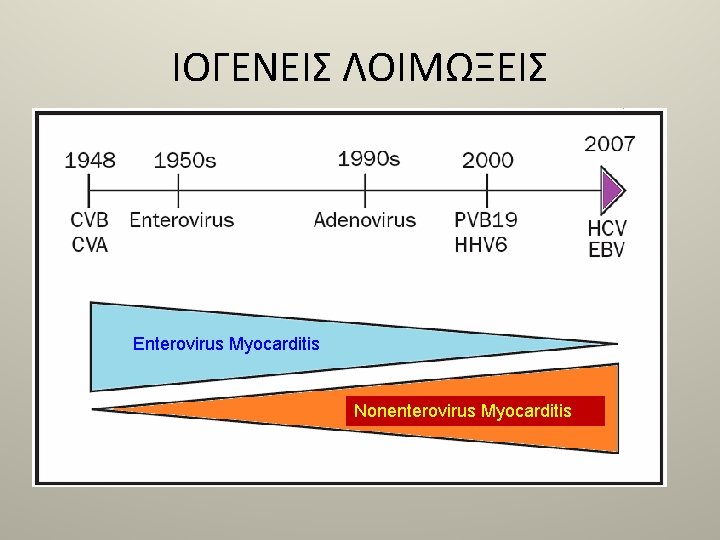
ΙΟΓΕΝΕΙΣ ΛΟΙΜΩΞΕΙΣ Enterovirus Myocarditis Nonenterovirus Myocarditis









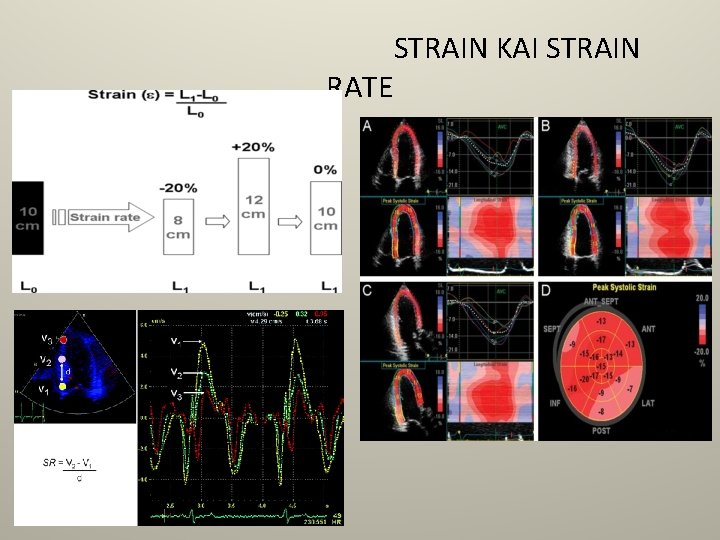
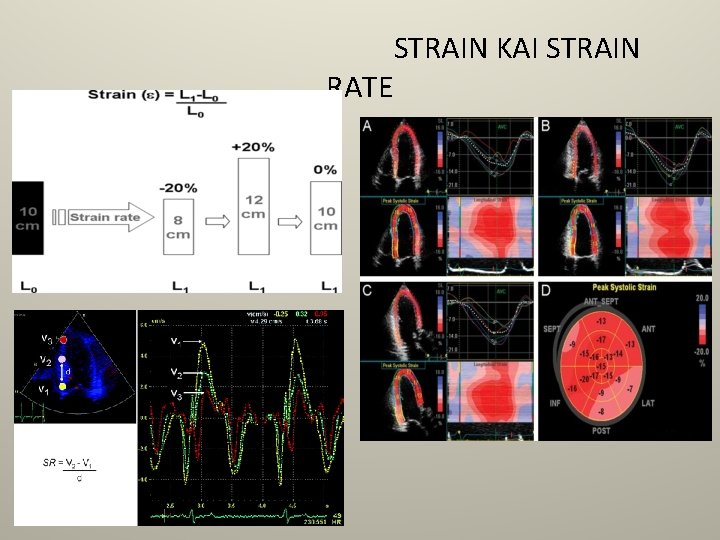
RATE STRAIN KAI STRAIN

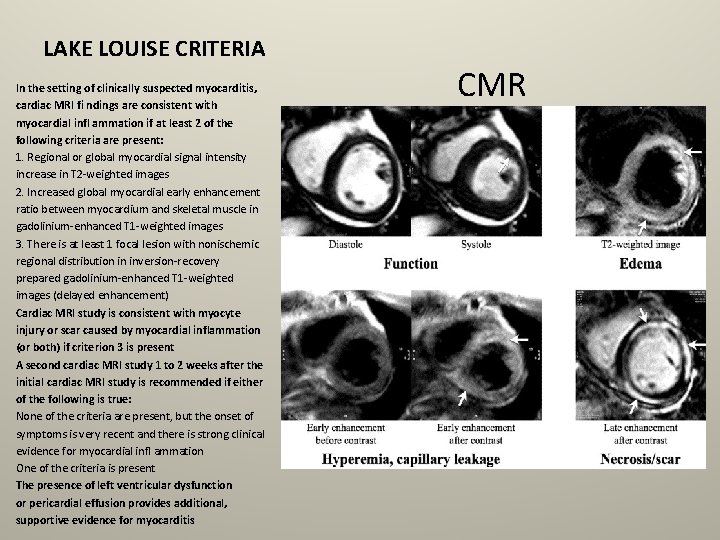
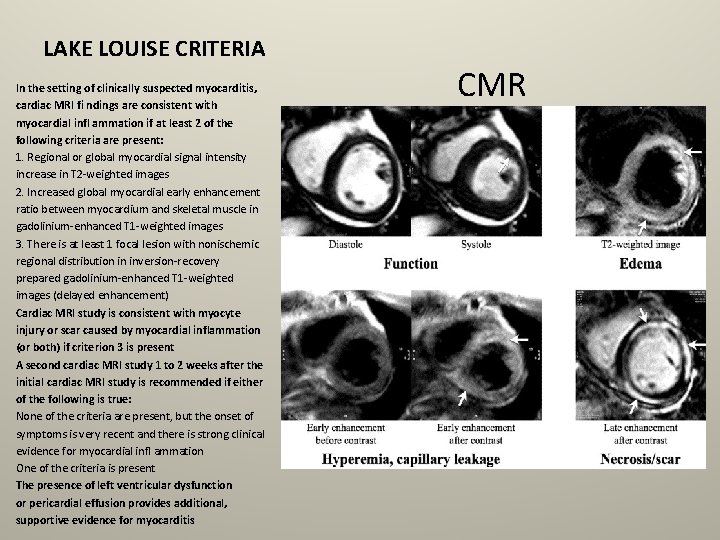
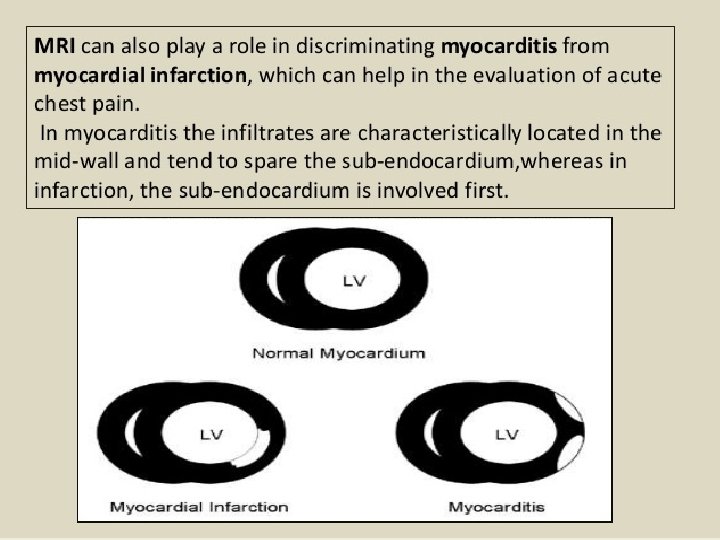
LAKE LOUISE CRITERIA In the setting of clinically suspected myocarditis, cardiac MRI fi ndings are consistent with myocardial infl ammation if at least 2 of the following criteria are present: 1. Regional or global myocardial signal intensity increase in T 2 -weighted images 2. Increased global myocardial early enhancement ratio between myocardium and skeletal muscle in gadolinium-enhanced T 1 -weighted images 3. There is at least 1 focal lesion with nonischemic regional distribution in inversion-recovery prepared gadolinium-enhanced T 1 -weighted images (delayed enhancement) Cardiac MRI study is consistent with myocyte injury or scar caused by myocardial inflammation (or both) if criterion 3 is present A second cardiac MRI study 1 to 2 weeks after the initial cardiac MRI study is recommended if either of the following is true: None of the criteria are present, but the onset of symptoms is very recent and there is strong clinical evidence for myocardial infl ammation One of the criteria is present The presence of left ventricular dysfunction or pericardial effusion provides additional, supportive evidence for myocarditis CMR
ac


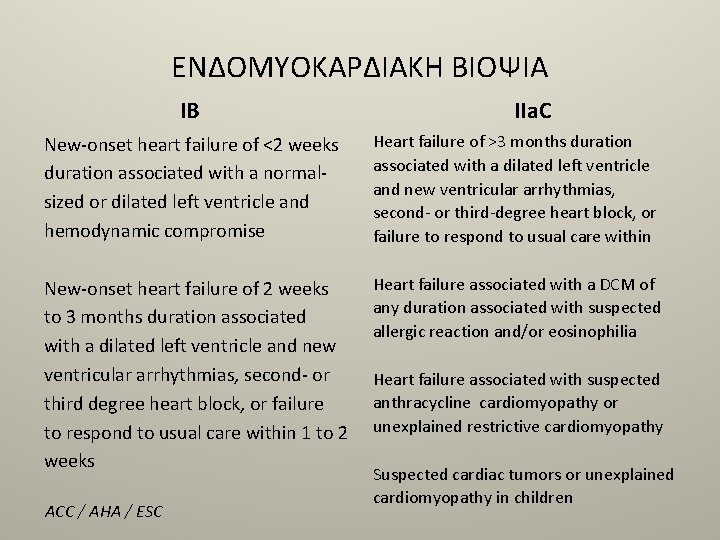
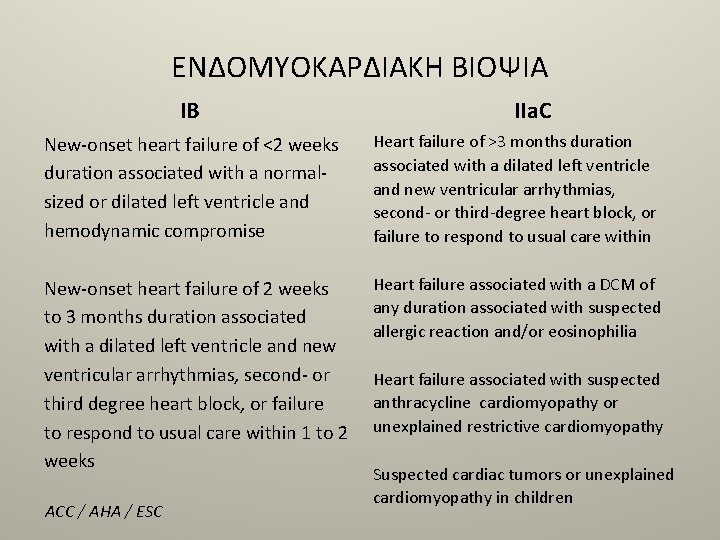
ΕΝΔΟΜΥΟΚΑΡΔΙΑΚΗ ΒΙΟΨΙΑ ΙB ΙΙa. C New-onset heart failure of <2 weeks duration associated with a normalsized or dilated left ventricle and hemodynamic compromise Heart failure of >3 months duration associated with a dilated left ventricle and new ventricular arrhythmias, second- or third-degree heart block, or failure to respond to usual care within New-onset heart failure of 2 weeks to 3 months duration associated with a dilated left ventricle and new ventricular arrhythmias, second- or third degree heart block, or failure to respond to usual care within 1 to 2 weeks Heart failure associated with a DCM of any duration associated with suspected allergic reaction and/or eosinophilia ACC / AHA / ESC Heart failure associated with suspected anthracycline cardiomyopathy or unexplained restrictive cardiomyopathy Suspected cardiac tumors or unexplained cardiomyopathy in children


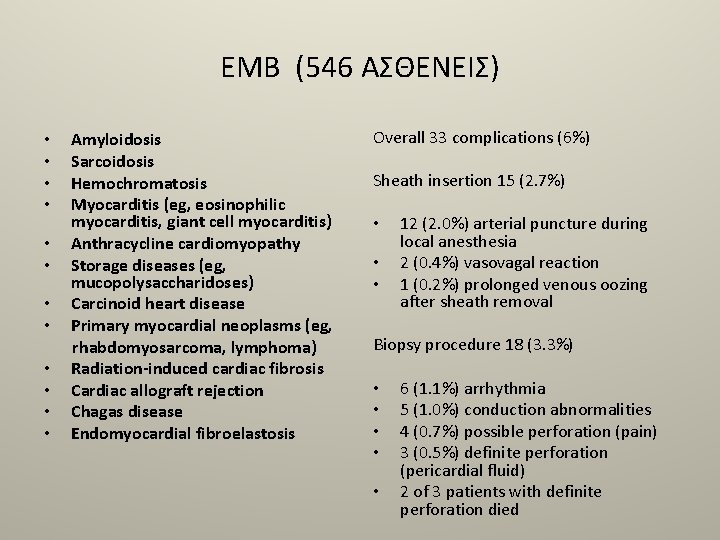
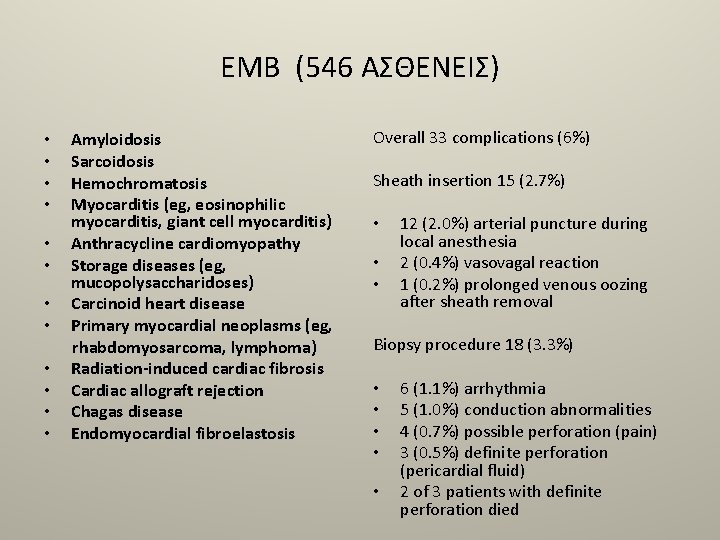
EMB (546 ΑΣΘΕΝΕΙΣ) • • • Amyloidosis Sarcoidosis Hemochromatosis Myocarditis (eg, eosinophilic myocarditis, giant cell myocarditis) Anthracycline cardiomyopathy Storage diseases (eg, mucopolysaccharidoses) Carcinoid heart disease Primary myocardial neoplasms (eg, rhabdomyosarcoma, lymphoma) Radiation-induced cardiac fibrosis Cardiac allograft rejection Chagas disease Endomyocardial fibroelastosis Overall 33 complications (6%) Sheath insertion 15 (2. 7%) • • • 12 (2. 0%) arterial puncture during local anesthesia 2 (0. 4%) vasovagal reaction 1 (0. 2%) prolonged venous oozing after sheath removal Biopsy procedure 18 (3. 3%) • • • 6 (1. 1%) arrhythmia 5 (1. 0%) conduction abnormalities 4 (0. 7%) possible perforation (pain) 3 (0. 5%) definite perforation (pericardial fluid) 2 of 3 patients with definite perforation died




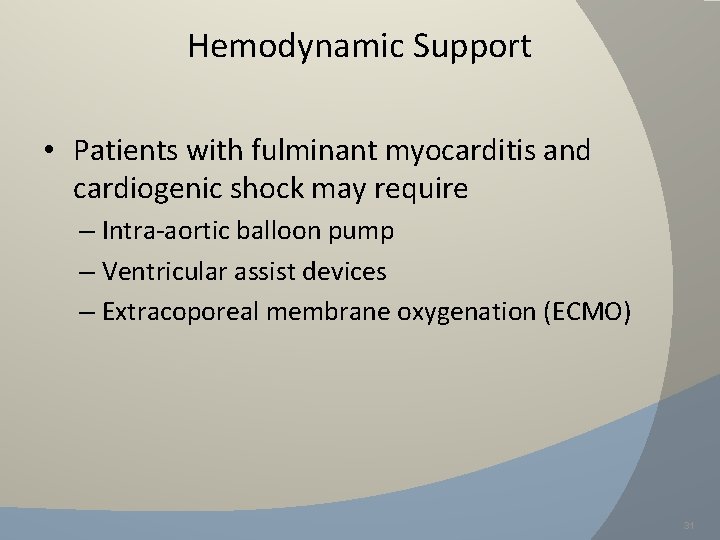
Hemodynamic Support • Patients with fulminant myocarditis and cardiogenic shock may require – Intra-aortic balloon pump – Ventricular assist devices – Extracoporeal membrane oxygenation (ECMO) 31










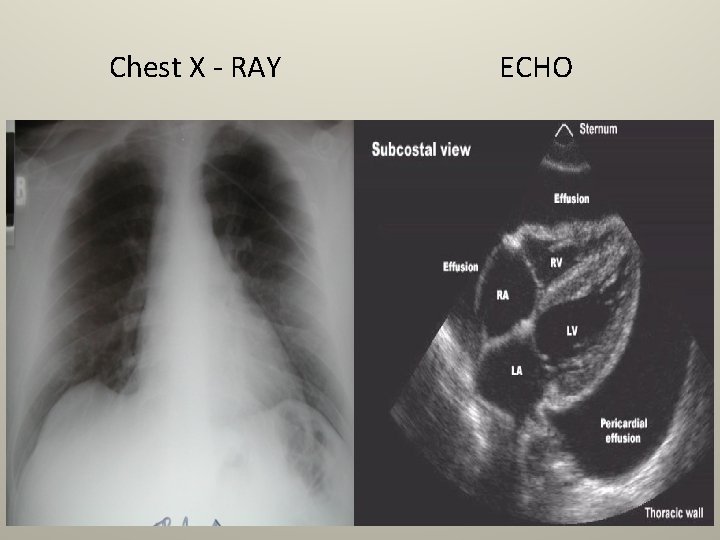
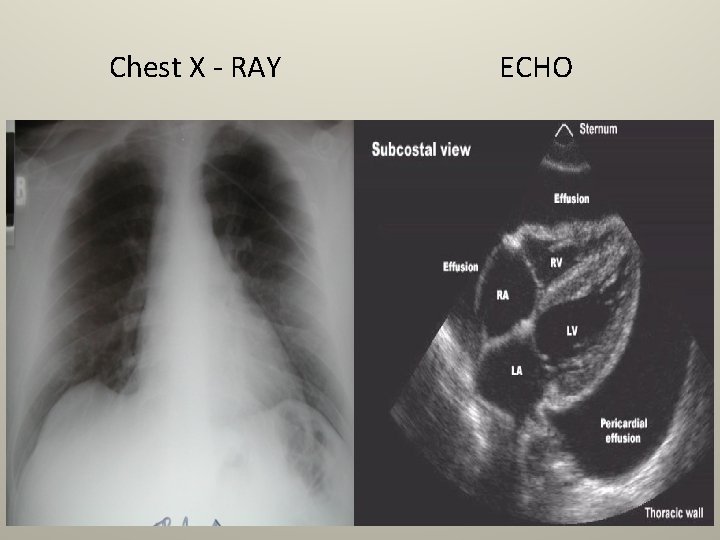
Chest X - RAY ECHO



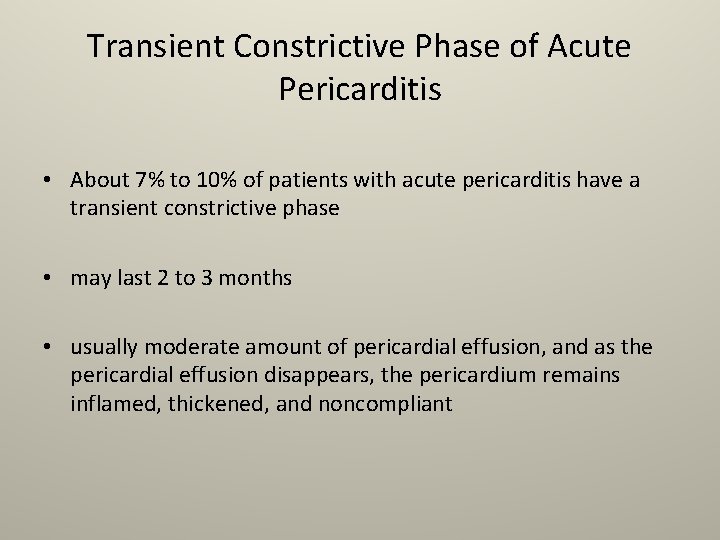
Transient Constrictive Phase of Acute Pericarditis • About 7% to 10% of patients with acute pericarditis have a transient constrictive phase • may last 2 to 3 months • usually moderate amount of pericardial effusion, and as the pericardial effusion disappears, the pericardium remains inflamed, thickened, and noncompliant
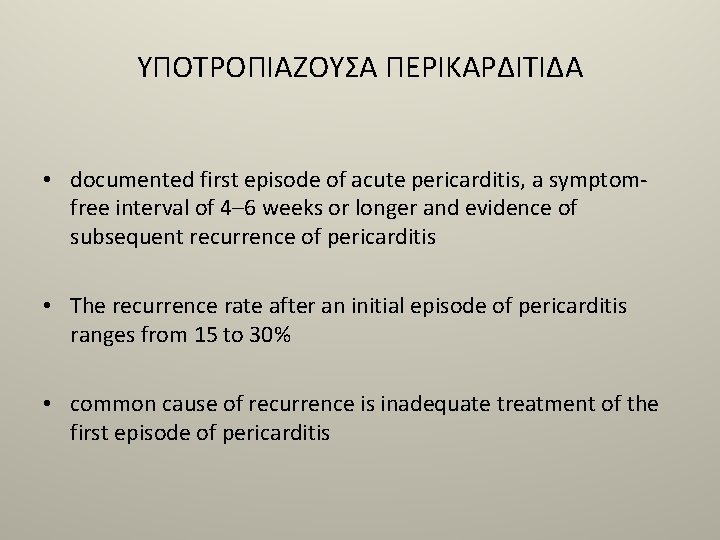
YΠΟΤΡΟΠΙΑΖΟΥΣΑ ΠΕΡΙΚΑΡΔΙΤΙΔΑ • documented first episode of acute pericarditis, a symptomfree interval of 4– 6 weeks or longer and evidence of subsequent recurrence of pericarditis • The recurrence rate after an initial episode of pericarditis ranges from 15 to 30% • common cause of recurrence is inadequate treatment of the first episode of pericarditis

 Egzantemli enterovirüs veziküler stomatiti
Egzantemli enterovirüs veziküler stomatiti Myocarditis
Myocarditis Pericarditis vs myocarditis
Pericarditis vs myocarditis Serous diffuse myocarditis
Serous diffuse myocarditis Pericarditis vs myocarditis
Pericarditis vs myocarditis Myocarditis
Myocarditis Pericarditis vs myocarditis ecg
Pericarditis vs myocarditis ecg Elastic strain and plastic strain
Elastic strain and plastic strain Compliance and stiffness
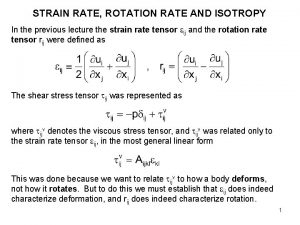
Compliance and stiffness Rotation rate tensor
Rotation rate tensor Mer kai
Mer kai Kiekgi rašyba
Kiekgi rašyba Chiang kai shek
Chiang kai shek Bayes net toolbox
Bayes net toolbox Kai wei chang
Kai wei chang Marcelijus martinaitis skaidres
Marcelijus martinaitis skaidres Kai bailey patty
Kai bailey patty Kai homs
Kai homs Chiang kai shek
Chiang kai shek Analisis chi square
Analisis chi square Marcelijus martinaitis kai sirpsta vyšnios suvalkijoj
Marcelijus martinaitis kai sirpsta vyšnios suvalkijoj Simtura
Simtura Pomrn
Pomrn Kai ruhsert
Kai ruhsert Kai-min chung
Kai-min chung Kai mcgreevy
Kai mcgreevy Tee kai loon
Tee kai loon Nasyonalista sa silangan at timog silangang asya
Nasyonalista sa silangan at timog silangang asya Kai selander
Kai selander Kai bu
Kai bu Kai salta kates miega susirietusios kodel
Kai salta kates miega susirietusios kodel Chiang kai shek
Chiang kai shek Kai nexus
Kai nexus Dos moi pa sto kai tan gan kinaso
Dos moi pa sto kai tan gan kinaso Kai kuuspalu
Kai kuuspalu Kai schweda
Kai schweda Kokie hormonai išsiskiria kai žmogus sportuoja
Kokie hormonai išsiskiria kai žmogus sportuoja He honore karakia
He honore karakia Chiang kai-shek
Chiang kai-shek Kai pata
Kai pata Kai correa drills
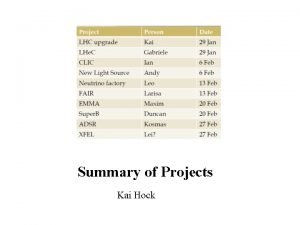
Kai correa drills Kai hock
Kai hock Kai hierarchy
Kai hierarchy En arche en ho logos
En arche en ho logos Kai übel
Kai übel Gymnasium asperg
Gymnasium asperg Kai metodu
Kai metodu Kai puolakanaho
Kai puolakanaho Kai cernat
Kai cernat