DEMENTIA AND DELIRIUM Dr Fiona Mc Dowall Consultant

- Slides: 47
DEMENTIA AND DELIRIUM Dr Fiona Mc. Dowall. Consultant old age psychiatrist
DEMENTIAS • • What is dementia Demographics Clinical features Types of dementia Pathology Diagnosis Treatment
What is dementia • Dementia is a clinical term describing a symptom complex characterised by a decline from previously maintained intellectual function • It occurs in clear consciousness • Decline affects more than one higher cortical function • Affects memory, behaviour, personality, judgment, attention, spatial relations, language, abstract thought, other executive functions such as planning and social judgement
Demographics • >65 population has increased x 4 since start of century • 18% of the population now > 65 years old • Dementia affects 5% of those > 65 20% of those > 80 • Currently the leading cause of death in UK • Globally rise to 132 million by 2050
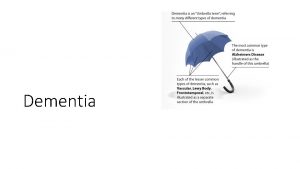
Types of dementia • Alzheimer’s Disease • Vascular dementia • Mixed dementia • Dementia with Lewy Bodies • Fronto-temporal Dementia
Clinical features of dementia 1. Loss of memory and higher brain functions such as planning, decision making, problem solving 2. Impairment of Activities of Daily Living (ADLs) Washing, dressing, cooking, telephone, TV, money, getting lost, driving, appliances. 3. Behavioural and Psychological Symptoms (BPSD)
Memory loss in dementia • Types of memory 1) Short-term - frontal lobes, tested by immediate recall of words or digit span • 2) Long-term memory - limbic system, t. neocortex • Episodic - personally experienced, temporal -specific • Semantic - general knowledge and factual • Information-procedural - learnt tasks
Memory loss in Alzheimer’s disease • Temporal gradient of forgetting • Shrinking repertoire of memories • Difficulty learning new information Short term memory loss >long term
Temporal lobe and dementia • • • Episodic memory - Limbic system -Semantic memory - Temporal neocortex -Dominant hemisphere - Verbal memory -Wernicke’s dysphasia - Language comprehension -Non-dominant hemisphere - Visual memory • • • -Activities of daily living -Forgetting appointments, medication/repetition -Living in the past - reminiscing -Confabulation -Non-recognition of familiar surroundings
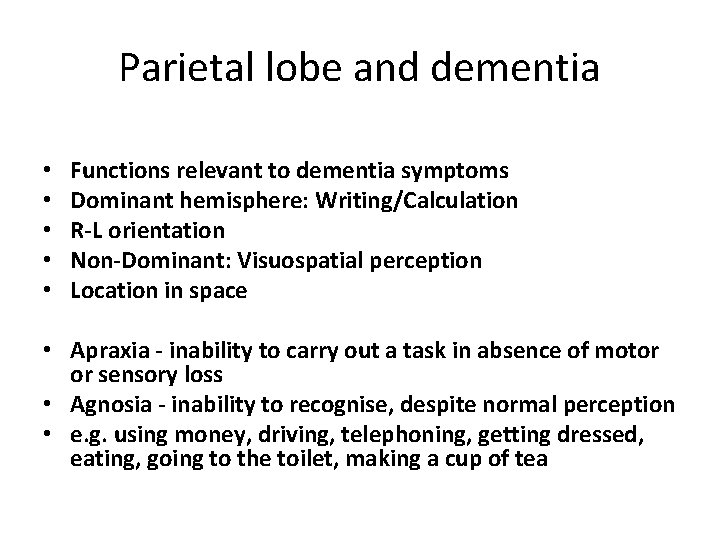
Parietal lobe and dementia • • • Functions relevant to dementia symptoms Dominant hemisphere: Writing/Calculation R-L orientation Non-Dominant: Visuospatial perception Location in space • Apraxia - inability to carry out a task in absence of motor or sensory loss • Agnosia - inability to recognise, despite normal perception • e. g. using money, driving, telephoning, getting dressed, eating, going to the toilet, making a cup of tea
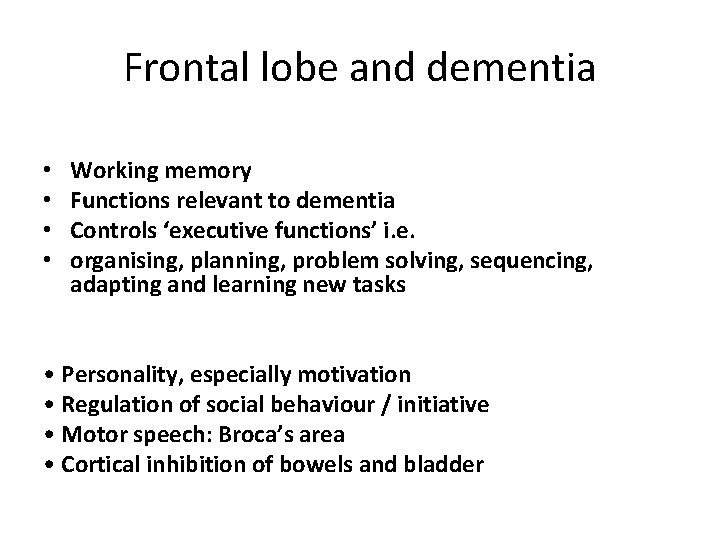
Frontal lobe and dementia • • Working memory Functions relevant to dementia Controls ‘executive functions’ i. e. organising, planning, problem solving, sequencing, adapting and learning new tasks • Personality, especially motivation • Regulation of social behaviour / initiative • Motor speech: Broca’s area • Cortical inhibition of bowels and bladder
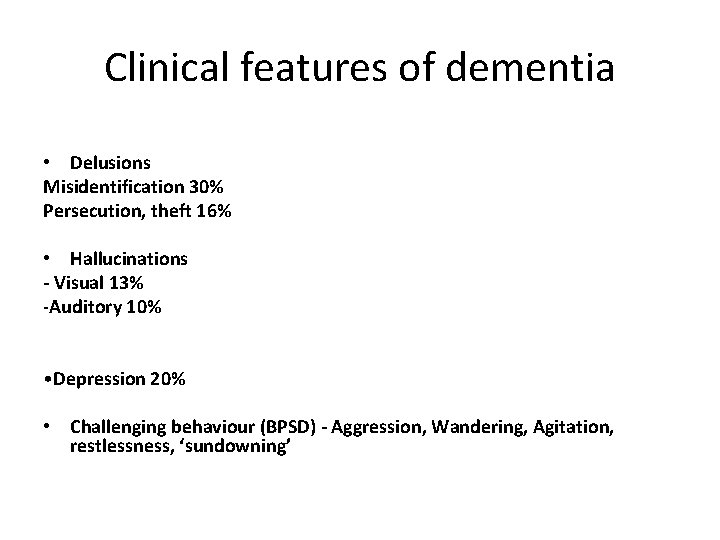
Clinical features of dementia • Delusions Misidentification 30% Persecution, theft 16% • Hallucinations - Visual 13% -Auditory 10% • Depression 20% • Challenging behaviour (BPSD) - Aggression, Wandering, Agitation, restlessness, ‘sundowning’
Risk assessment and dementia • • • Wandering Neglect Fire Financial exploitation Aggression Driving
Pathology and dementia • • • Global cortical atrophy Medial temporal atrophy(hippocampus) Vascular changes Infarcts Neurofibrillary tangles, amyloid plaques Neuronal loss and cholinergic deficits(acetyl cholinesterase inhibitors)
Risks and protective factors • Risks: Age, genetics, Down’s syndrome, life style, vascular risks, female, head injury. • Protective: company, IQ, cognitive stimulation, learning new things, life style and diet, decrease the vascular risks.
Making a diagnosis • History. COLLATERAL very important –which type of memory loss, examples –Speech / language difficulties –Orientation difficulties –Onset / course of deterioration –Personality change/ risk/challenging behaviour _ADLs • • FH Positive? PH educational level/ occupational attainment • Med Hx • SHx
Making a diagnosis • Mental state examination: • Depression, hallucinations, delusions. • Cognitive assessment: ACE-III, Mini-ACE • Cognitive decline in at least two domains(memory, language, orientation, visuospatial, fluency) for at least 6 months • AND decline with function (ADLS)
Investigations • Brain scans • Bloods: full confusion screen • FBC, ESR/CRP, Us and Es, LFTs, Ca, B 12, folate, TFTs, glucose.
Treatment • Medication: acetyl cholinesterase inhibitors, memantine, antidepressants, antipsychotics. • Psychological • Social • Supporting organisations: social care, Alzheimer’s society, carers, home care. • LPA, Advance care plans, driving, will.
Dementia and the general hospital • 1/4 patients in the acute hospital have a diagnosis of dementia • 1/3 in acute hospital have delirium • 1/3 patients on an acute take are in the last year of life • Diagnostic overshadowing • Dementia/delirium/depression overlap
Delirium • • Definition Diagnosis Investigations Treatment
Delirium definition • Delirium (acute confusional state) is a neuropsychiatric syndrome characterised by acute onset of fluctuating cognition and inattention linked to triggering factors. It usually develops over 1 -2 days. Delirium is a serious condition that may be associated with poor outcomes. However it can be prevented and symptoms treated if identified early
Delirium definition • The American Psychiatric Association’s Diagnostic and Statistical Manual, 4 th Edition (DSM-IV) defines delirium by the presence of 4 key clinical features: • Disturbance in consciousness with reduced ability to maintain or focus attention • A change in cognition or development of a perceptual disturbance which is not better explained by a preexisting dementia. • Acute onset and fluctuating course. • Evidence of a triggering medical condition or causative substance.
Delirium definition • Symptoms of delirium have a tendency to fluctuate throughout the course of a day, and as such is frequently under recognised. Delirium presents in one of three ways: • Hyperactive delirium: restless, agitated, delusions, hallucinations, risk of harm to patient or others. • Hypoactive delirium: lethargic, drowsy, reduced communication. • Mixed Delirium: demonstrates signs of both of the above. • Hypoactive and mixed delirium may be more difficult to recognise.
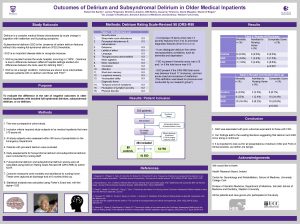
Delirium demographics • Delirium is common in hospital affecting: • 30% of older medical patients at some point during a hospital admission. • 10 -50% of patients post operatively. • 70 -80% of patients in an ITU setting • 20% of patients in post-acute care settings
Delirium demographics • Despite its frequency delirium is under recognised in hospitals. Delirium should be considered a medical emergency and is associated with unfavourable outcomes including: • • Increased mortality in older people (35 -40% at 1 year) Increased length of stay. Increased rates of placement in care home. Increased risk of in-hospital complication such as pressure ulcers and falls. • In addition to the above up to 60% of older patients with delirium have persisting cognitive impairment and will go on to receive a diagnosis of dementia.
Delirium demographics • Delirium is preventable in up to 1/3 rd of cases and is treatable if identified and managed appropriately and urgently. As such it should be considered a medical emergency.
Delirium differential diagnosis • Diagnoses that may be difficult to distinguish from delirium are dementia, depression, psychotic illness, dysphasia, mania and non-convulsive epilepsy. • It can be difficult to distinguish between dementia and delirium because symptoms overlap and some patients may have both conditions. Dementia is associated with progressive decline and is irreversible. Delirium is associated with a fluctuating course and may be reversible. • If clinical uncertainty exists over diagnosis then initial management should be for delirium.
Delirium risk factors • • Age 65 years or older Current hip fracture Cognitive impairment or dementia Severe illness
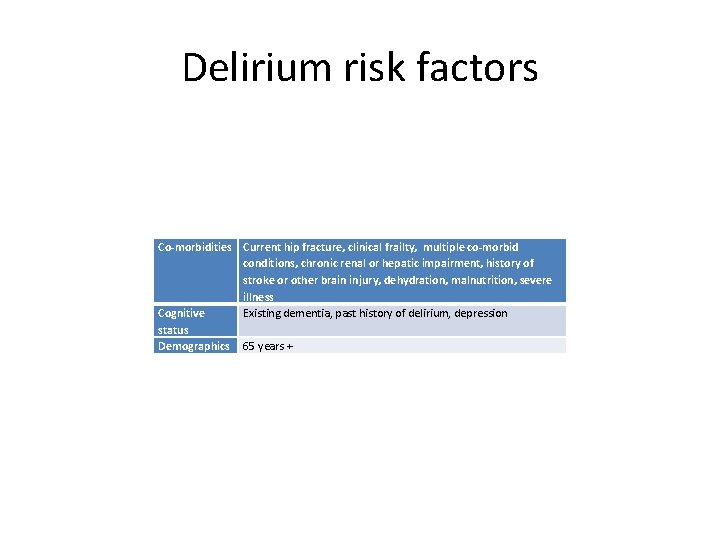
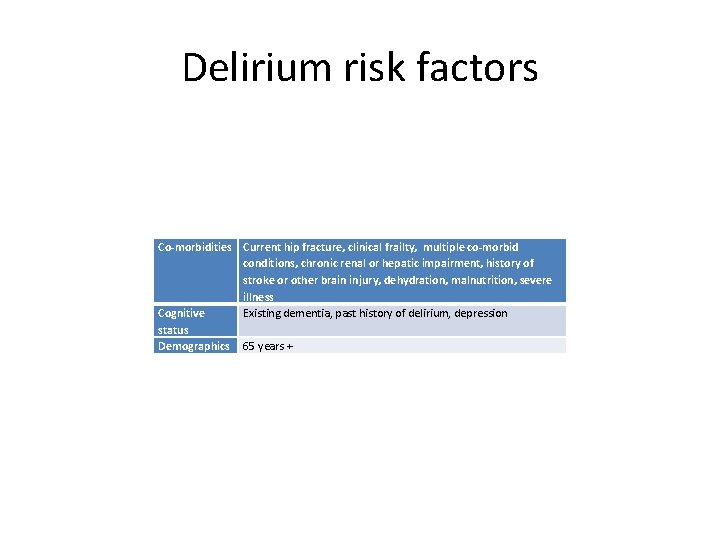
Delirium risk factors Co-morbidities Current hip fracture, clinical frailty, multiple co-morbid conditions, chronic renal or hepatic impairment, history of stroke or other brain injury, dehydration, malnutrition, severe illness Cognitive Existing dementia, past history of delirium, depression status Demographics 65 years +
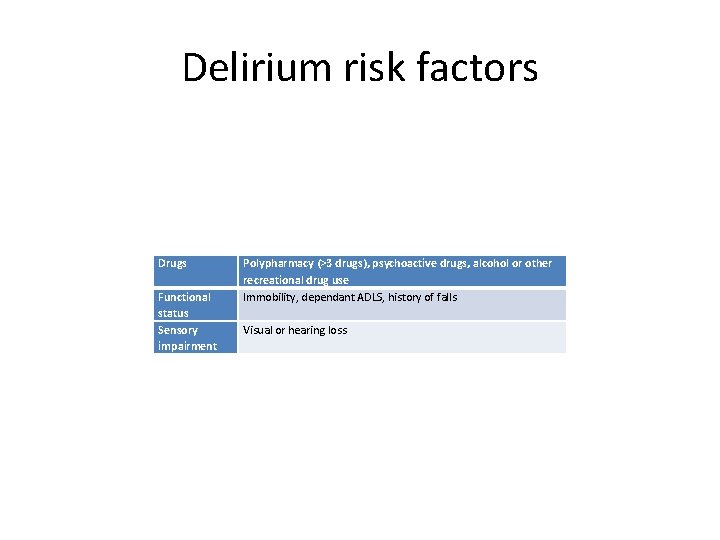
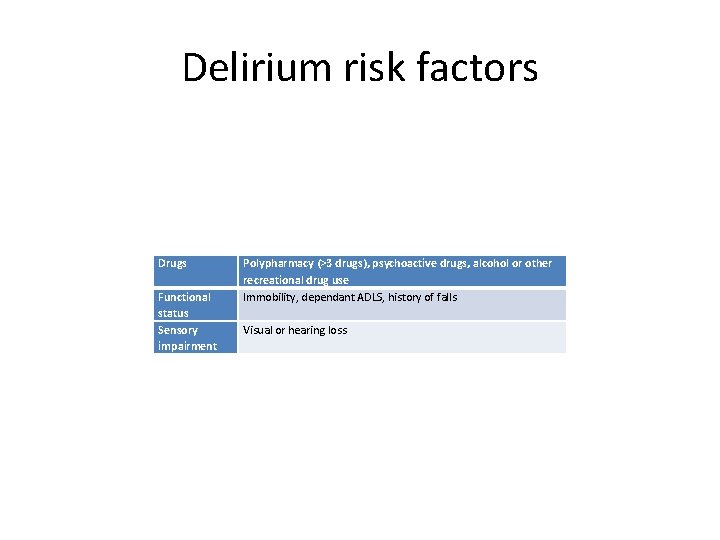
Delirium risk factors Drugs Functional status Sensory impairment Polypharmacy (>3 drugs), psychoactive drugs, alcohol or other recreational drug use Immobility, dependant ADLS, history of falls Visual or hearing loss
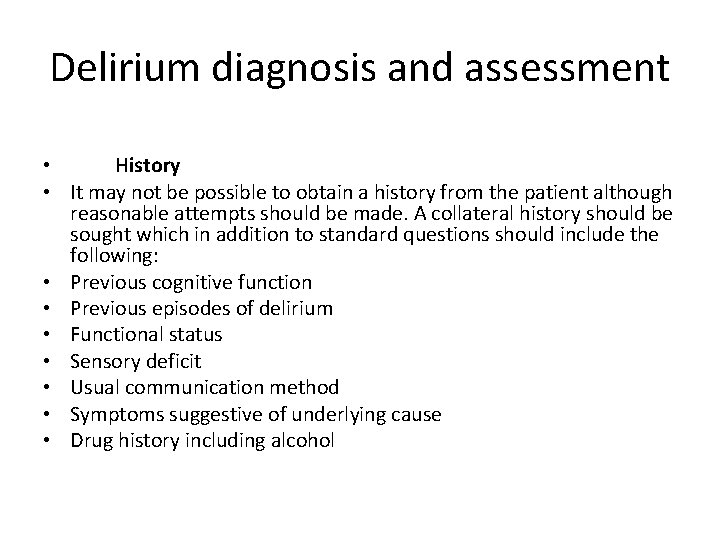
Delirium diagnosis and assessment • History • It may not be possible to obtain a history from the patient although reasonable attempts should be made. A collateral history should be sought which in addition to standard questions should include the following: • Previous cognitive function • Previous episodes of delirium • Functional status • Sensory deficit • Usual communication method • Symptoms suggestive of underlying cause • Drug history including alcohol
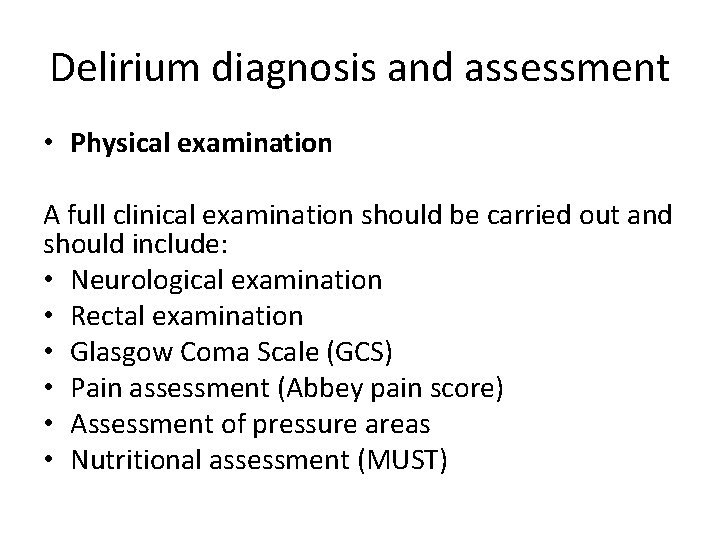
Delirium diagnosis and assessment • Physical examination A full clinical examination should be carried out and should include: • Neurological examination • Rectal examination • Glasgow Coma Scale (GCS) • Pain assessment (Abbey pain score) • Assessment of pressure areas • Nutritional assessment (MUST)
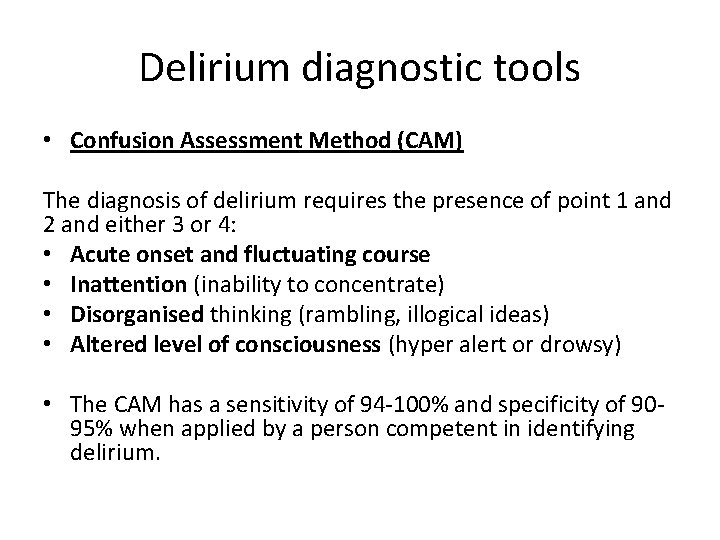
Delirium diagnostic tools • Confusion Assessment Method (CAM) The diagnosis of delirium requires the presence of point 1 and 2 and either 3 or 4: • Acute onset and fluctuating course • Inattention (inability to concentrate) • Disorganised thinking (rambling, illogical ideas) • Altered level of consciousness (hyper alert or drowsy) • The CAM has a sensitivity of 94 -100% and specificity of 9095% when applied by a person competent in identifying delirium.
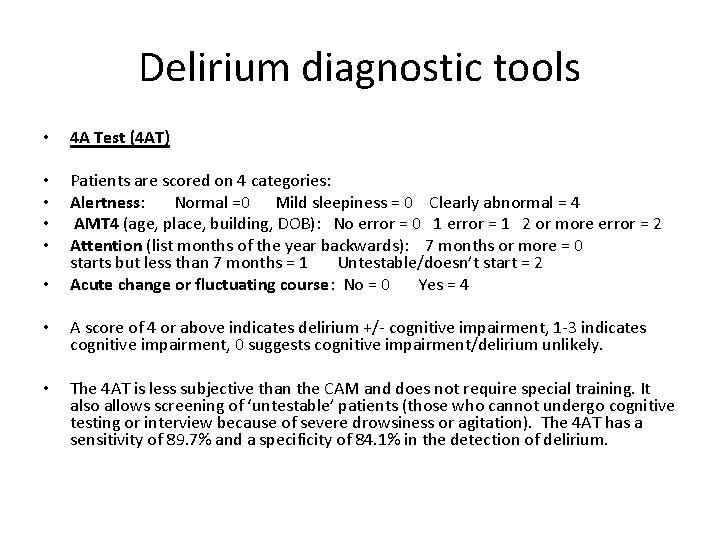
Delirium diagnostic tools • 4 A Test (4 AT) • • Patients are scored on 4 categories: Alertness: Normal =0 Mild sleepiness = 0 Clearly abnormal = 4 AMT 4 (age, place, building, DOB): No error = 0 1 error = 1 2 or more error = 2 Attention (list months of the year backwards): 7 months or more = 0 starts but less than 7 months = 1 Untestable/doesn’t start = 2 Acute change or fluctuating course: No = 0 Yes = 4 • • A score of 4 or above indicates delirium +/- cognitive impairment, 1 -3 indicates cognitive impairment, 0 suggests cognitive impairment/delirium unlikely. • The 4 AT is less subjective than the CAM and does not require special training. It also allows screening of ‘untestable’ patients (those who cannot undergo cognitive testing or interview because of severe drowsiness or agitation). The 4 AT has a sensitivity of 89. 7% and a specificity of 84. 1% in the detection of delirium.
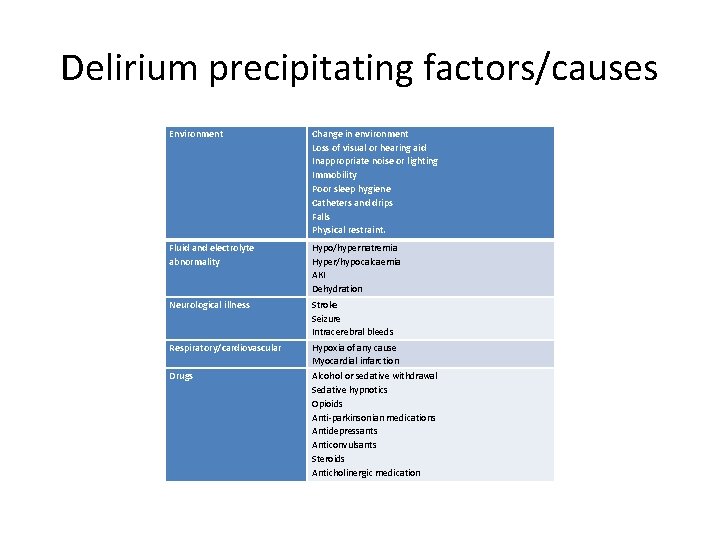
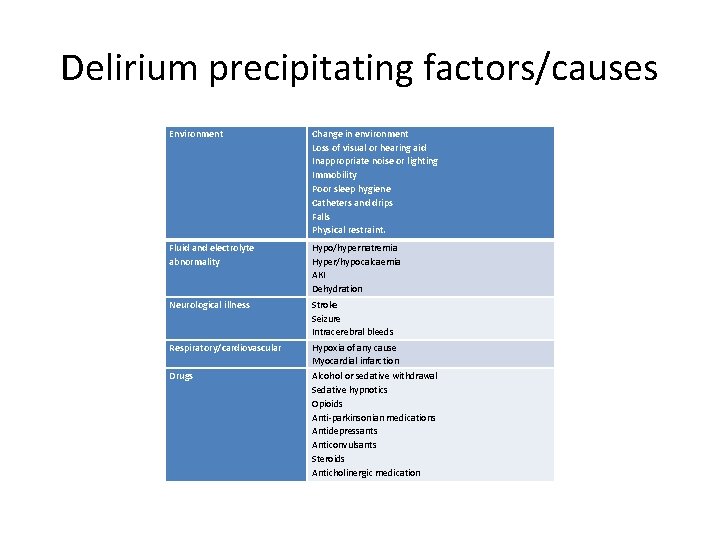
Delirium precipitating factors/causes Environment Change in environment Loss of visual or hearing aid Inappropriate noise or lighting Immobility Poor sleep hygiene Catheters and drips Falls Physical restraint. Fluid and electrolyte abnormality Hypo/hypernatremia Hyper/hypocalcaemia AKI Dehydration Neurological illness Stroke Seizure Intracerebral bleeds Respiratory/cardiovascular Hypoxia of any cause Myocardial infarction Alcohol or sedative withdrawal Sedative hypnotics Opioids Anti-parkinsonian medications Antidepressants Anticonvulsants Steroids Anticholinergic medication Drugs
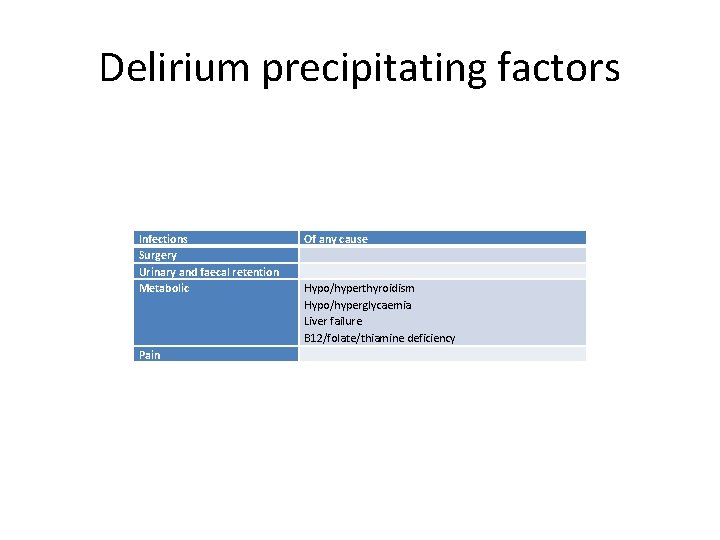
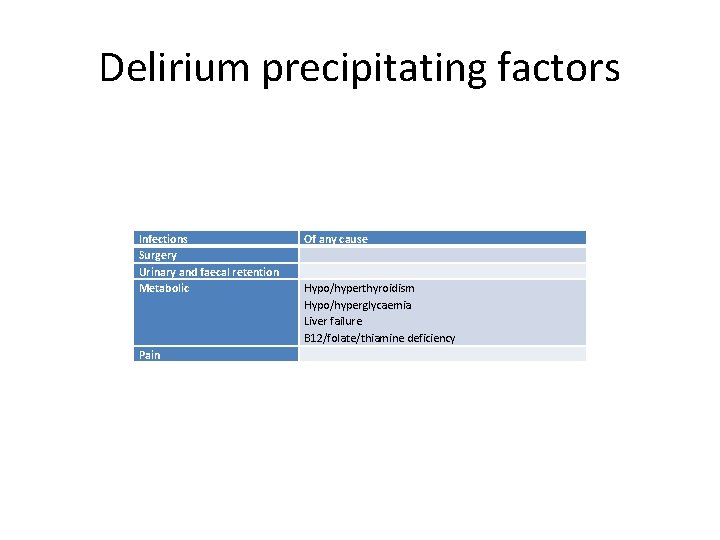
Delirium precipitating factors Infections Surgery Urinary and faecal retention Metabolic Pain Of any cause Hypo/hyperthyroidism Hypo/hyperglycaemia Liver failure B 12/folate/thiamine deficiency
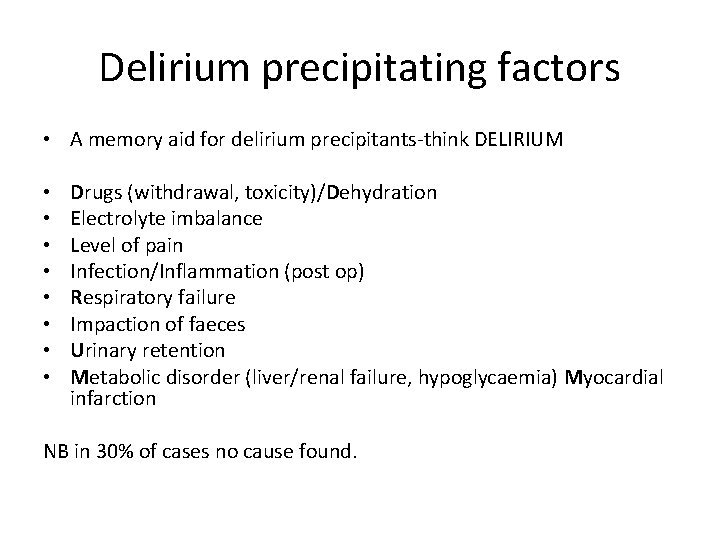
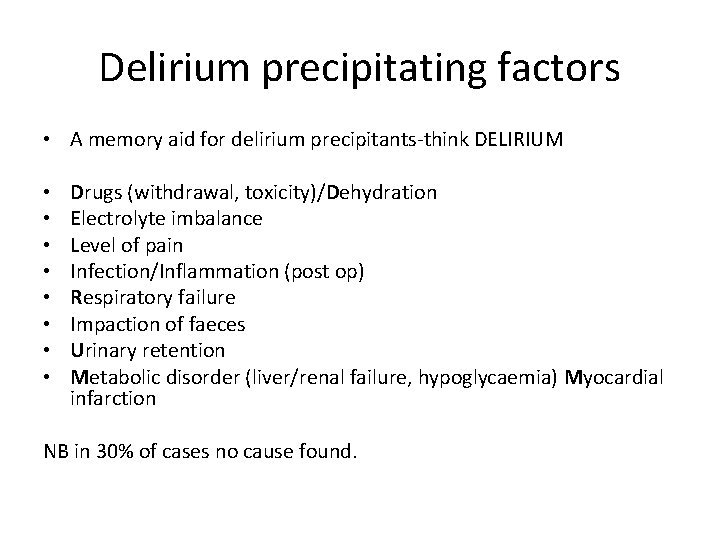
Delirium precipitating factors • A memory aid for delirium precipitants-think DELIRIUM • • Drugs (withdrawal, toxicity)/Dehydration Electrolyte imbalance Level of pain Infection/Inflammation (post op) Respiratory failure Impaction of faeces Urinary retention Metabolic disorder (liver/renal failure, hypoglycaemia) Myocardial infarction NB in 30% of cases no cause found.
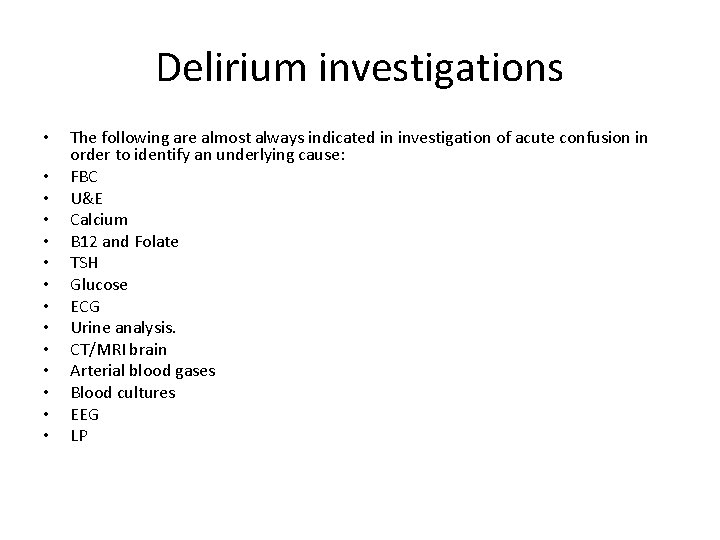
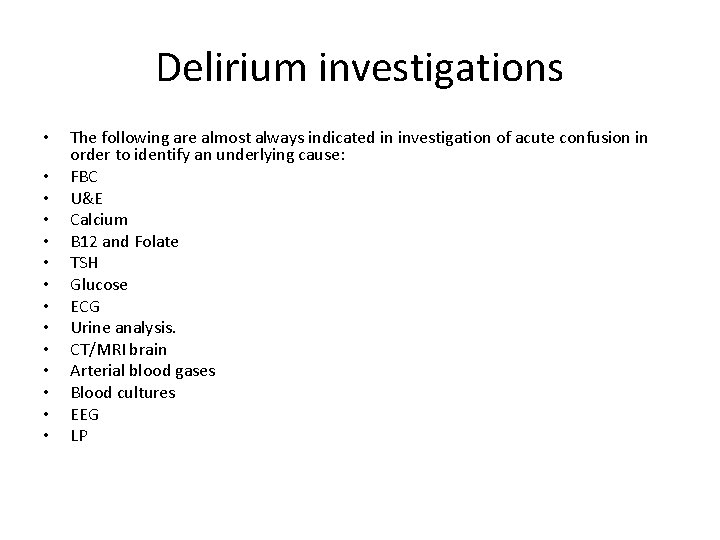
Delirium investigations • • • • The following are almost always indicated in investigation of acute confusion in order to identify an underlying cause: FBC U&E Calcium B 12 and Folate TSH Glucose ECG Urine analysis. CT/MRI brain Arterial blood gases Blood cultures EEG LP

Delirium non pharmacological treatment Do’s Don’ts Correct hypoxia Delay diagnosis Remain vigilant for infection Catheterise unnecessarily Correct dehydration Use IV lines unnecessarily Involve dieticians Order unnecessary tests Treat pain and use not verbal Disturb sleep for obs/medication scoring systems rounds Involve family in care Subject patient to unnecessary bay or Document well ward moves Involve mental health teams if Turn lights on unnecessarily at night psychotic symptoms present Use medication unless other Ensure patient is observed at interventions have failed. arms length and consider Use high doses of medications for extra staffing elderly patients. Engage patient in meaningful activities Repeated orientation Ensure patient has sensory aids Ensure good lighting levels in the day. Use non-confrontational and empathic de-escalation techniques
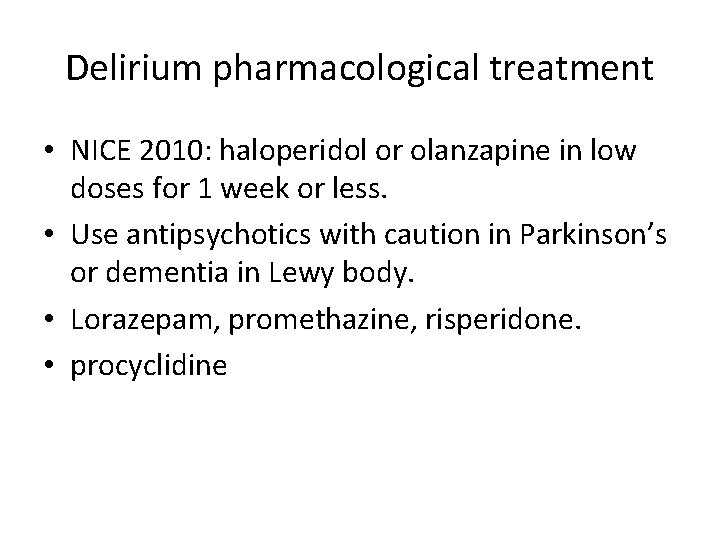
Delirium pharmacological treatment • NICE 2010: haloperidol or olanzapine in low doses for 1 week or less. • Use antipsychotics with caution in Parkinson’s or dementia in Lewy body. • Lorazepam, promethazine, risperidone. • procyclidine
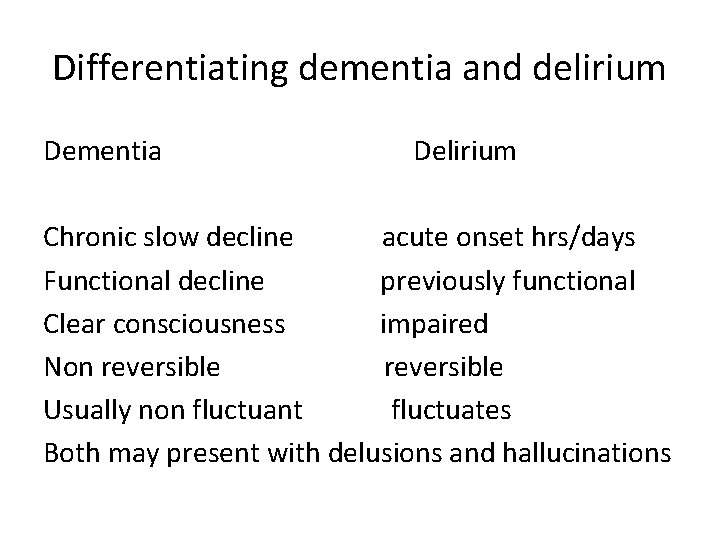
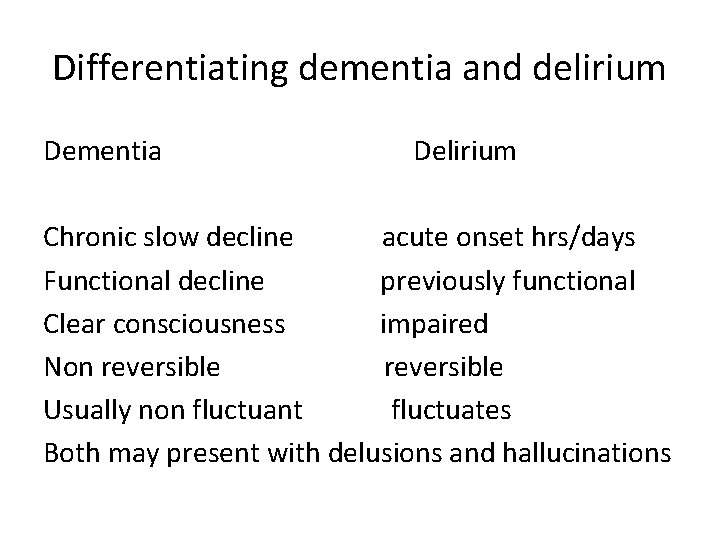
Differentiating dementia and delirium Dementia Delirium Chronic slow decline acute onset hrs/days Functional decline previously functional Clear consciousness impaired Non reversible Usually non fluctuant fluctuates Both may present with delusions and hallucinations
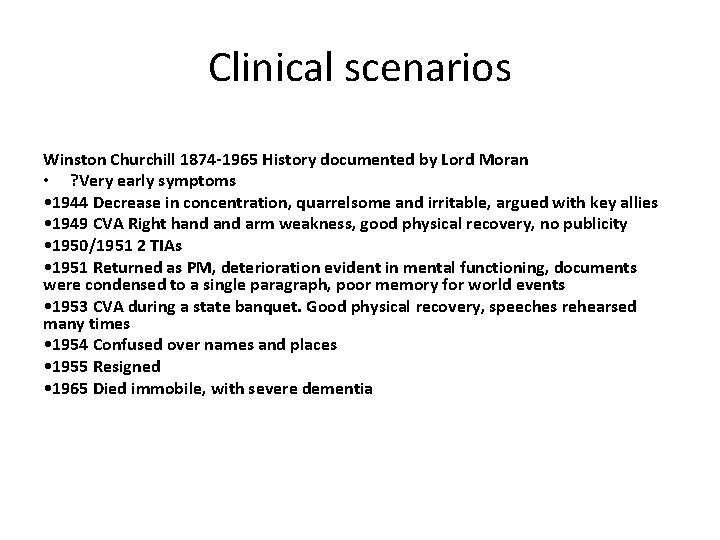
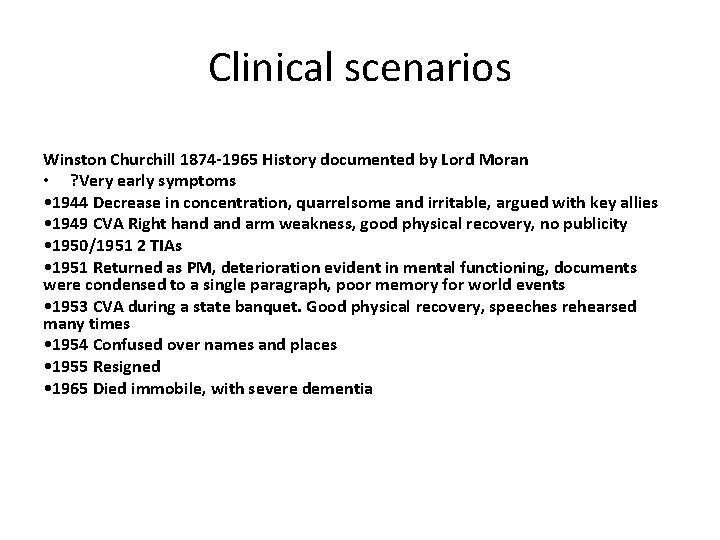
Clinical scenarios Winston Churchill 1874 -1965 History documented by Lord Moran • ? Very early symptoms • 1944 Decrease in concentration, quarrelsome and irritable, argued with key allies • 1949 CVA Right hand arm weakness, good physical recovery, no publicity • 1950/1951 2 TIAs • 1951 Returned as PM, deterioration evident in mental functioning, documents were condensed to a single paragraph, poor memory for world events • 1953 CVA during a state banquet. Good physical recovery, speeches rehearsed many times • 1954 Confused over names and places • 1955 Resigned • 1965 Died immobile, with severe dementia
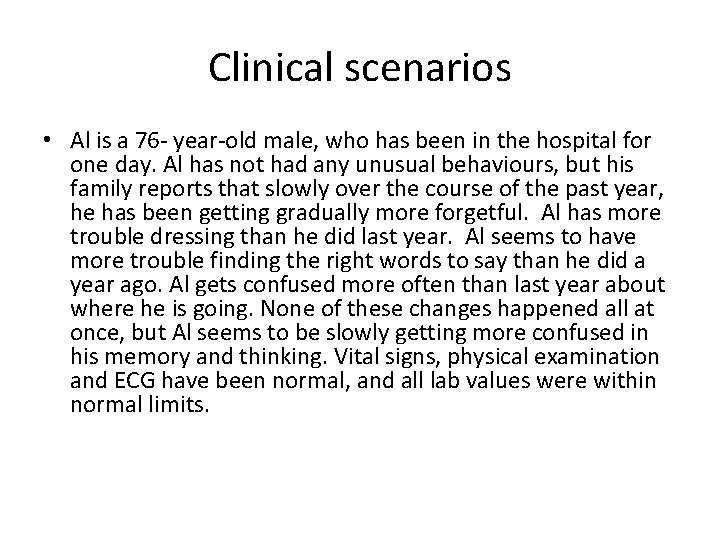
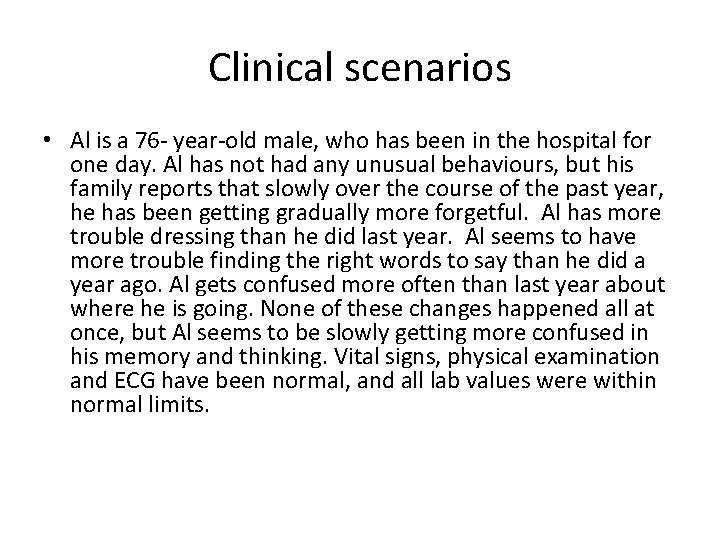
Clinical scenarios • Al is a 76 - year-old male, who has been in the hospital for one day. Al has not had any unusual behaviours, but his family reports that slowly over the course of the past year, he has been getting gradually more forgetful. Al has more trouble dressing than he did last year. Al seems to have more trouble finding the right words to say than he did a year ago. Al gets confused more often than last year about where he is going. None of these changes happened all at once, but Al seems to be slowly getting more confused in his memory and thinking. Vital signs, physical examination and ECG have been normal, and all lab values were within normal limits.
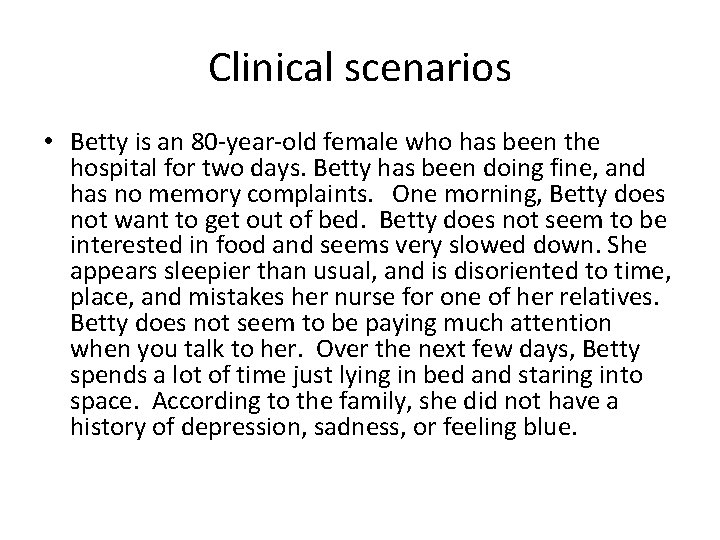
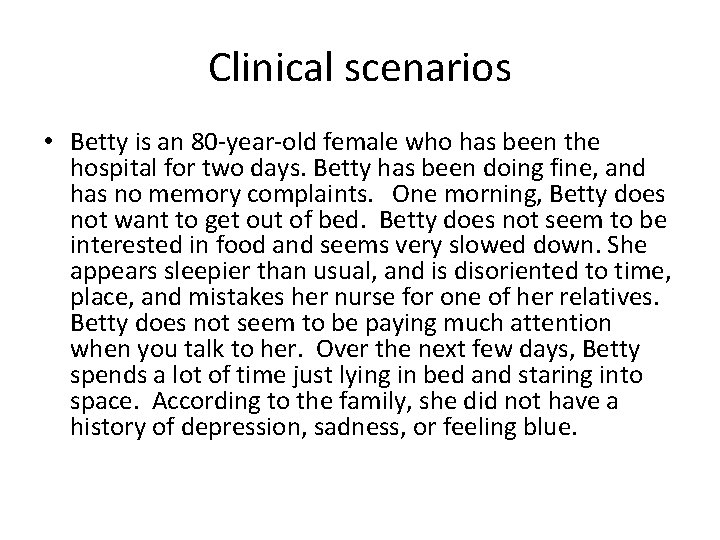
Clinical scenarios • Betty is an 80 -year-old female who has been the hospital for two days. Betty has been doing fine, and has no memory complaints. One morning, Betty does not want to get out of bed. Betty does not seem to be interested in food and seems very slowed down. She appears sleepier than usual, and is disoriented to time, place, and mistakes her nurse for one of her relatives. Betty does not seem to be paying much attention when you talk to her. Over the next few days, Betty spends a lot of time just lying in bed and staring into space. According to the family, she did not have a history of depression, sadness, or feeling blue.
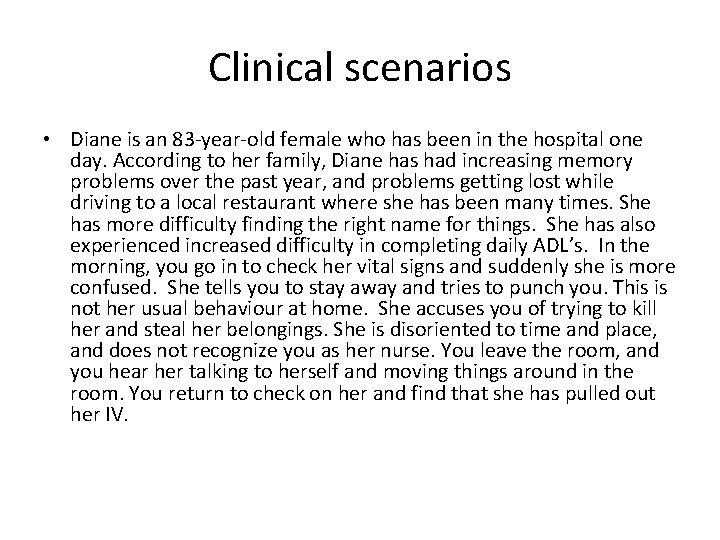
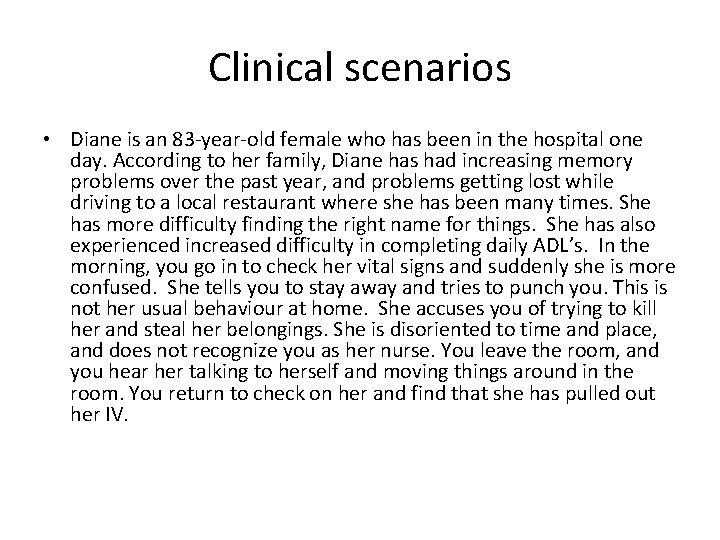
Clinical scenarios • Diane is an 83 -year-old female who has been in the hospital one day. According to her family, Diane has had increasing memory problems over the past year, and problems getting lost while driving to a local restaurant where she has been many times. She has more difficulty finding the right name for things. She has also experienced increased difficulty in completing daily ADL’s. In the morning, you go in to check her vital signs and suddenly she is more confused. She tells you to stay away and tries to punch you. This is not her usual behaviour at home. She accuses you of trying to kill her and steal her belongings. She is disoriented to time and place, and does not recognize you as her nurse. You leave the room, and you hear her talking to herself and moving things around in the room. You return to check on her and find that she has pulled out her IV.
Questions? ? fionamcdowall@nhs. net
 Difference between dementia and delirium
Difference between dementia and delirium Difference between delirium and dementia ppt
Difference between delirium and dementia ppt Types of amnesia
Types of amnesia Heidi dowall
Heidi dowall Pinch me delirium
Pinch me delirium Sindrom delirium akut
Sindrom delirium akut Nash delirium
Nash delirium Terminalt delirium
Terminalt delirium Escala cam delirium
Escala cam delirium Delirium care pathways
Delirium care pathways Acute confusion related to
Acute confusion related to Delirium definition
Delirium definition Excited delirium перевод
Excited delirium перевод Escala de cam
Escala de cam Delirium case presentation
Delirium case presentation Flocculation delirium
Flocculation delirium Gcs normal
Gcs normal Driver diagram palliative care
Driver diagram palliative care 3 zones of space and awareness dementia
3 zones of space and awareness dementia Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease If a resident with ad shows violent behavior the na should
If a resident with ad shows violent behavior the na should Moving and handling dementia patients
Moving and handling dementia patients Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Family history consultant training
Family history consultant training Bookcase analogy dementia
Bookcase analogy dementia Dementia pugilistica
Dementia pugilistica Enriched model of dementia care
Enriched model of dementia care Fast dementia scale
Fast dementia scale Dementia 2015
Dementia 2015 Tom kitwood enriched model of dementia care
Tom kitwood enriched model of dementia care Reversible dementia
Reversible dementia Epilepsy
Epilepsy Barbara's story dementia
Barbara's story dementia Fast scale for dementia
Fast scale for dementia Risk factor dementia
Risk factor dementia Hospice lcd dementia
Hospice lcd dementia Life story work dementia
Life story work dementia Dementia ddx
Dementia ddx Dementia friendly nevada
Dementia friendly nevada Promoting excellence in dementia care
Promoting excellence in dementia care Rarly signs of dementia
Rarly signs of dementia Dementia capable care
Dementia capable care Narritive text
Narritive text Pal assessment tool
Pal assessment tool Symptoms of dementia
Symptoms of dementia