Dr Fiona Lisney Consultant in Palliative Medicine Fiona











- Slides: 34
Dr. Fiona Lisney Consultant in Palliative Medicine Fiona. Lisney@fhft. nhs. com 01753 634879


• 12 cases • All settings • Emerging themes
• Not recognizing that people are dying or responding to their needs • Poor symptom control • Poor communication • Inadequate out-of-hours services • Poor care planning • Delays in diagnosis and referrals for treatmen

• Not recognizing that people are dying or responding to their needs • Poor symptom control • Poor communication • Inadequate out-of-hours services • Poor care planning • Delays in diagnosis and referrals for treatmen

This is REALLY difficult work and increasingly so: Identification Communication Allocation of resources Specialty work Under resourced

• EOL strategy – 2008 – Last year of life • Neuberger enquiry - ‘More care, less pathway’ – Last hours to days • LACDP - ‘Five priorities of care’ – Last hours to days • One chance to get it right – Last hours to days • CQC – EOL inspections – Last year of life (NICE) including advance care planning and access to SPC (PEER review) – Care after death
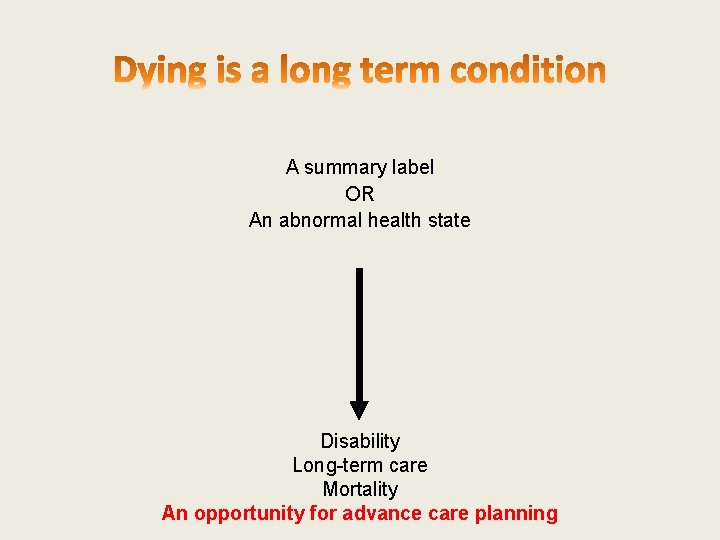
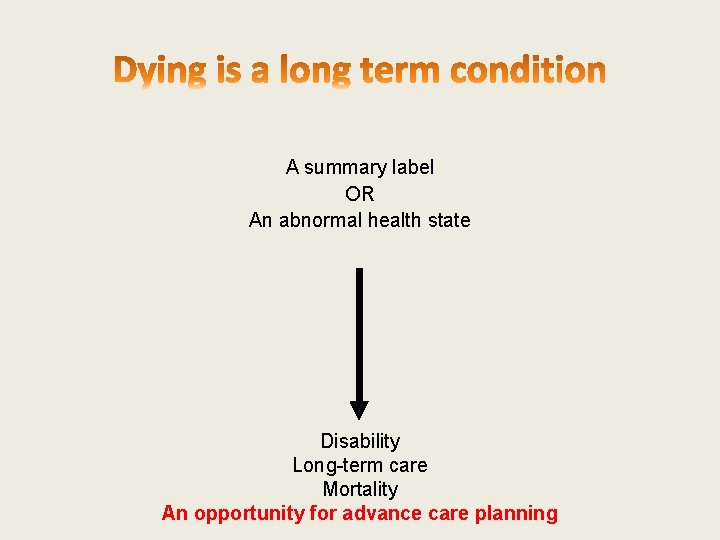
A summary label OR An abnormal health state Disability Long-term care Mortality An opportunity for advance care planning
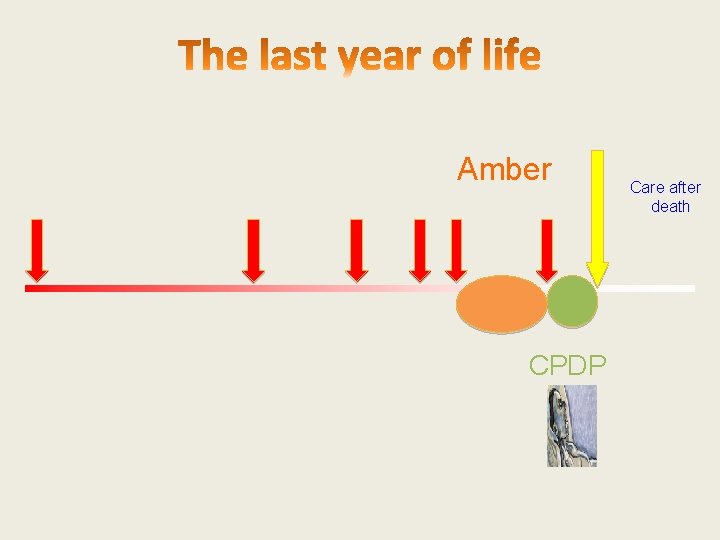
Amber CPDP Care after death
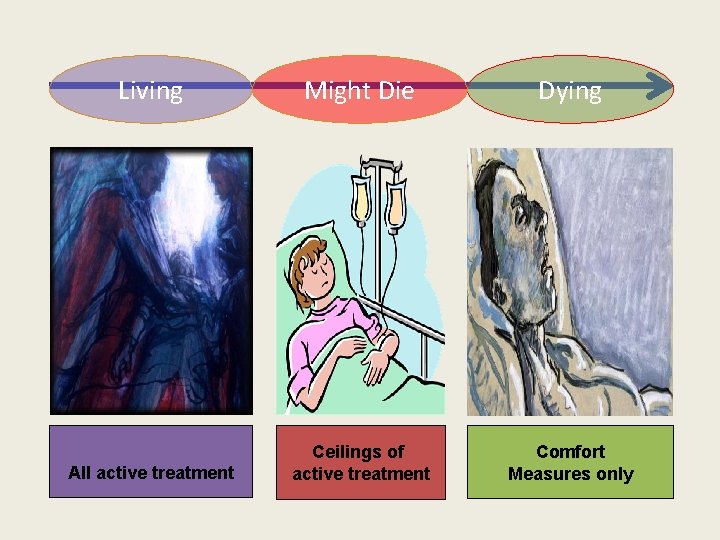
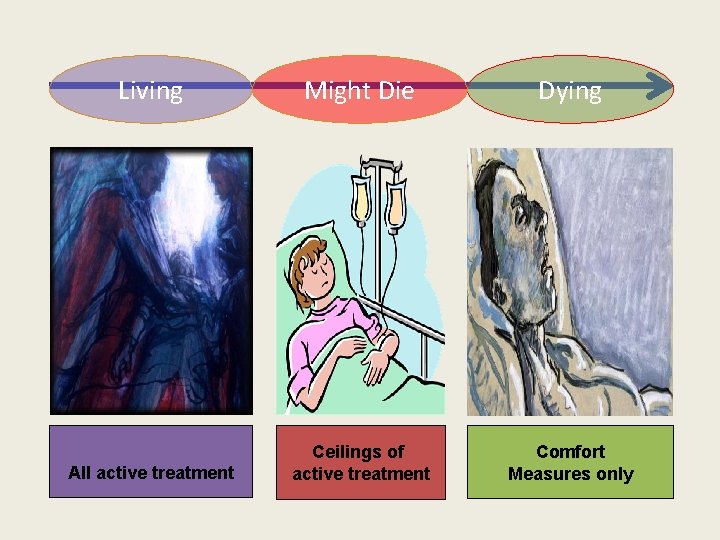
Living Might Die Dying All active treatment Ceilings of active treatment Comfort Measures only
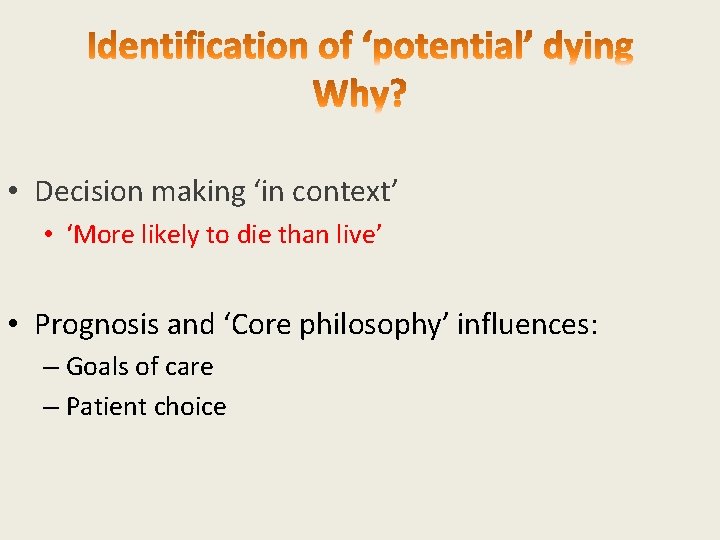
• Decision making ‘in context’ • ‘More likely to die than live’ • Prognosis and ‘Core philosophy’ influences: – Goals of care – Patient choice

Why is this so difficult? For doctors For patients
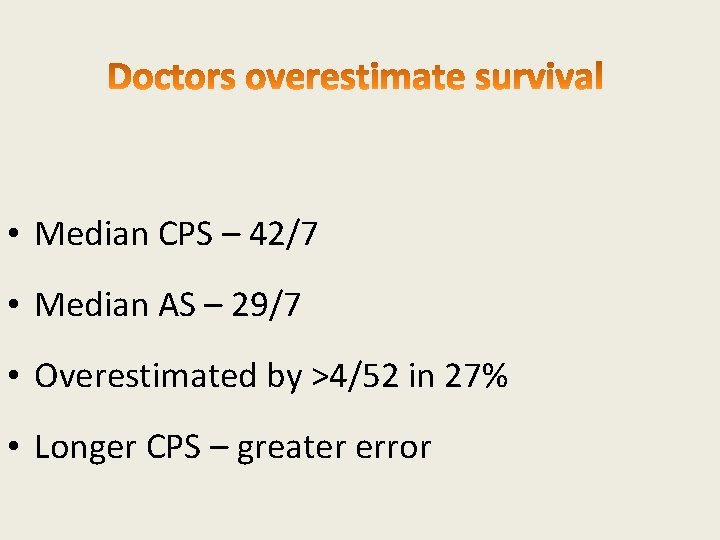
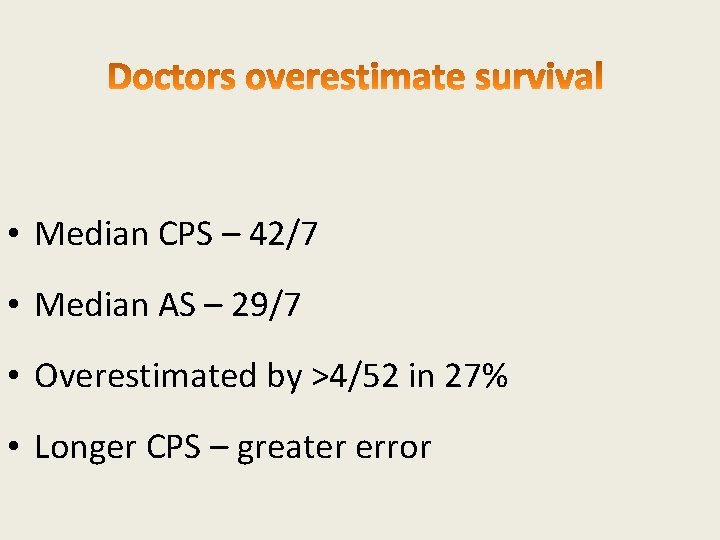
• Median CPS – 42/7 • Median AS – 29/7 • Overestimated by >4/52 in 27% • Longer CPS – greater error

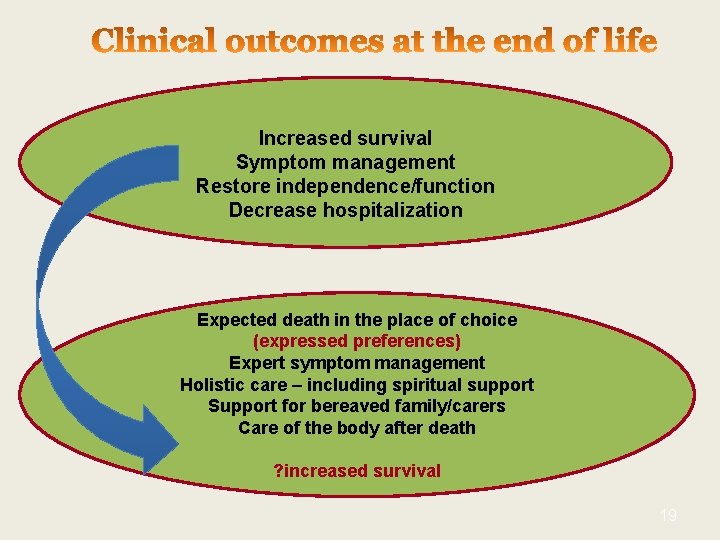
• Increased survival • Symptom management • Restore independence/function • Decrease hospitalization
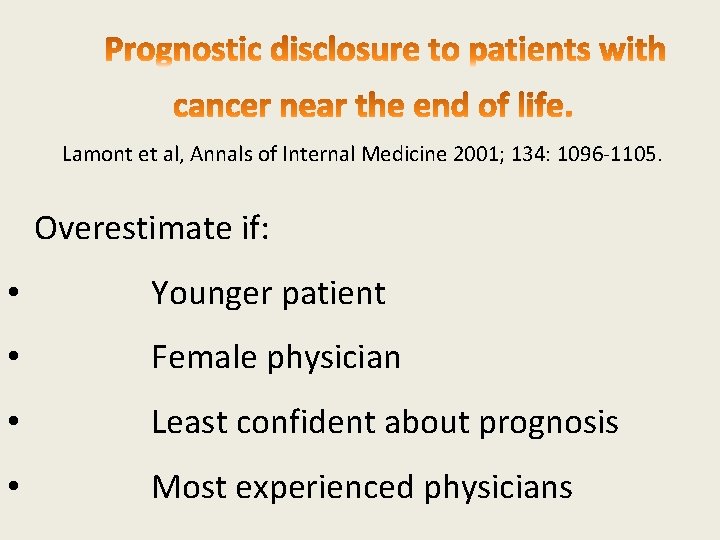
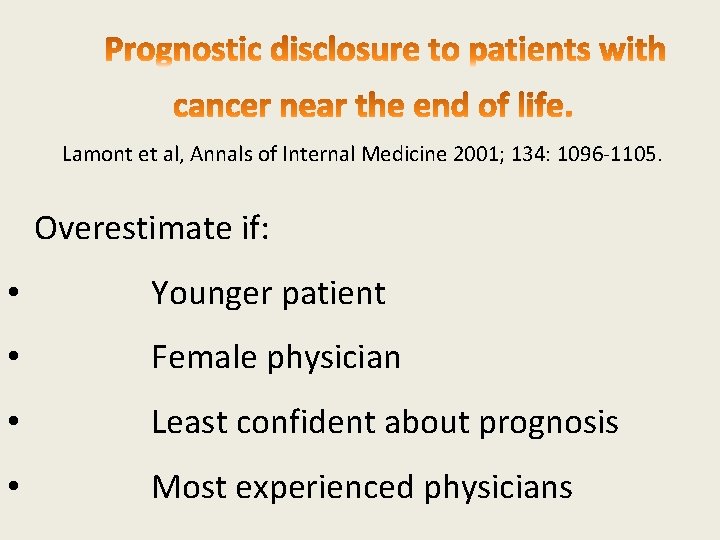
Lamont et al, Annals of Internal Medicine 2001; 134: 1096 -1105. Overestimate if: • Younger patient • Female physician • Least confident about prognosis • Most experienced physicians
Gwilliam B et al Ann Oncol. 2013 Feb; 24(2): 282 -8 • Nurses – No worse than doctors • MDT – Better than doctors or nurses alone • Patients – 61. 4% want to know, but nearly all are over optimistic
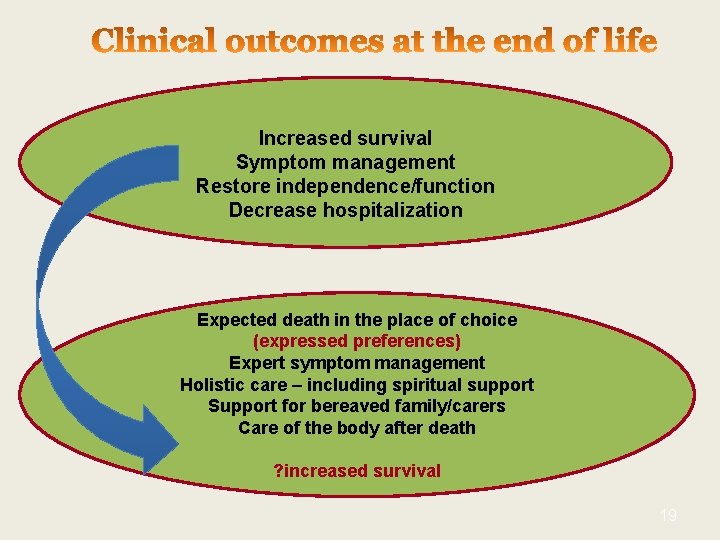
Increased survival Symptom management Restore independence/function Decrease hospitalization Expected death in the place of choice (expressed preferences) Expert symptom management Holistic care – including spiritual support Support for bereaved family/carers Care of the body after death ? increased survival 19
Patients Plan for death (‘will die’) but not serious illness (‘might die’) Caresse 2002 Some want to discuss eolc – best initiated after recurrence and topic introduced by someone skilled, over several meetings (Barnes 2007), and best not done in hospital in an acute episode Seamark 2012 Nearly all are over optimistic
– Symptom management – Control and autonomy • place of death • QOL > survival – Avoid ‘burden’ to those we love – religious/spiritual needs met – A life lived • • Most desirable age to die is 81 -90 Only 6% of people >65 yrs want to live to >100 yrs


UK projections 1951 -2074 Government Actuary Department , 2004 • The population is ageing • The number who die each year will increase by 17 -20% by 2030 • Expensive • 15 -20% of health care resources are spent on those in the last year of life • If current trends continue hospitals will need >20% more beds
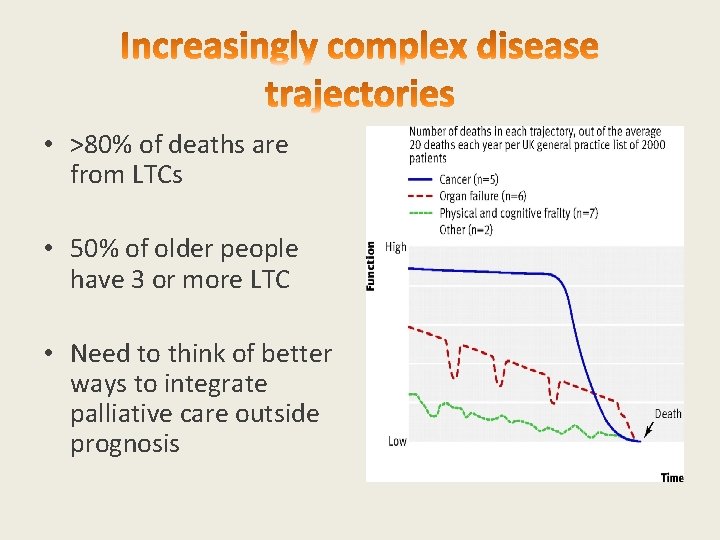
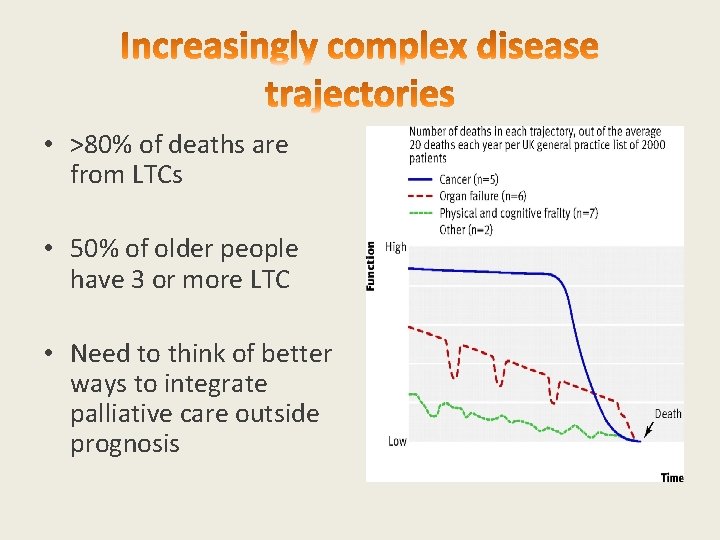
• >80% of deaths are from LTCs • 50% of older people have 3 or more LTC • Need to think of better ways to integrate palliative care outside prognosis
• Those in the last year have 3. 5 Hospital admissions • Lyons and Verne 2011 • 1 in 3 DGH inpatients will die within a year • Clark et al, Palliative Medicine 2014/National audit office 2008 • Increases to 1 in 2 for the socio economically deprived extreme elderly (>85 yrs) admitted to medical wards via A&E • (Clark et al, Palliative Medicine 2014) • 1 in 10 adult inpatients in a DGH will die during the admission • • (Clark et al, Palliative Medicine 2014) 54% in hospital deaths follow an admission of ≥ 8 days. • 86% follow an emergency admission, the LOS is 27/7
• Hospital • Older • Ethnic minority groups – Chinese • Discordance between patient and family • Home • Married • Further education • Higher household income • Care home • Living alone

• Hospital – Higher levels of co-morbidity – Uncertain prognostication • Home – Longer disease trajectory • Care Home – Older – Dementia/cognitive impairment
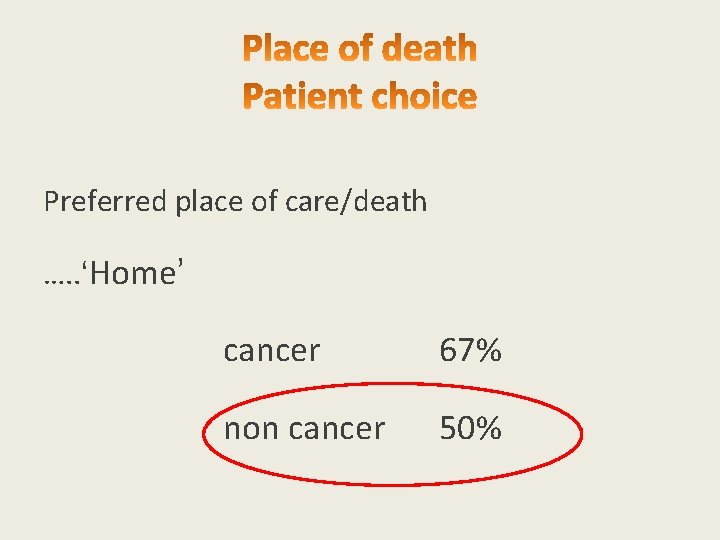
Preferred place of care/death …. . ‘Home’ cancer 67% non cancer 50%
1. Large volumes 2. Elderly 3. Most complex 1. Complex disease trajectory 2. Complex uncertain prognostication 3. Complex communication 4. Complex cultural/religious requirements 5. Complex social care needs

• Improves QOL and survival with no cost difference • (Higginson et al, Lancet Resp. Med Dec 2014; 2(12): 979987/Temel et al, NEJM 2010; 363: 733 -42) • Doubles the odds of dying at home • (Gomes et al, Cochrane database, 2013. June 6; 6: CDoo 7760) • Halves AE attendances for those in the last month of life • (Hensonet al, J Clin Onc 2015 Feb 1; 33(4): 370 -376)
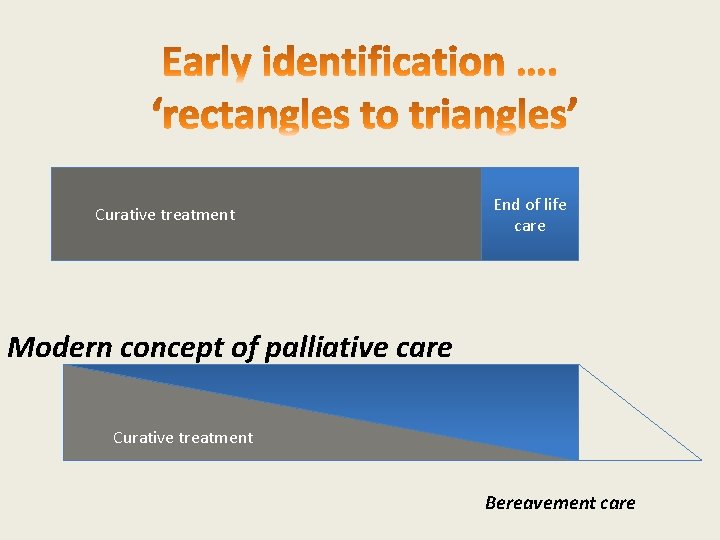
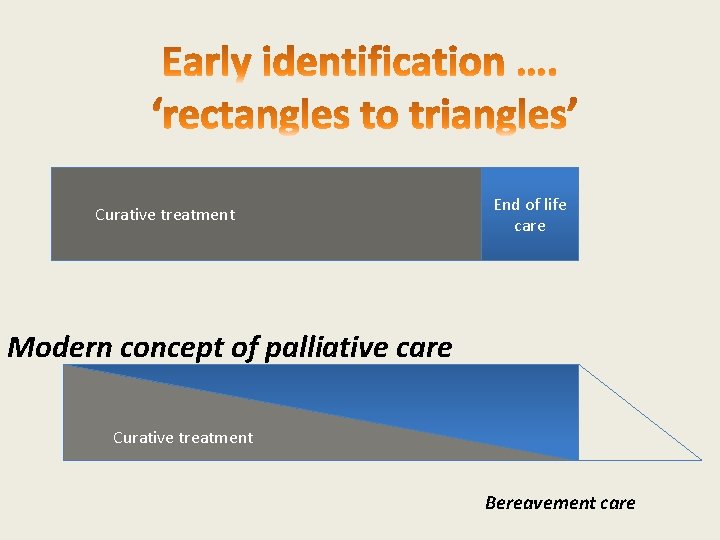
Curative treatment End of life care Modern concept of palliative care Curative treatment Bereavement care
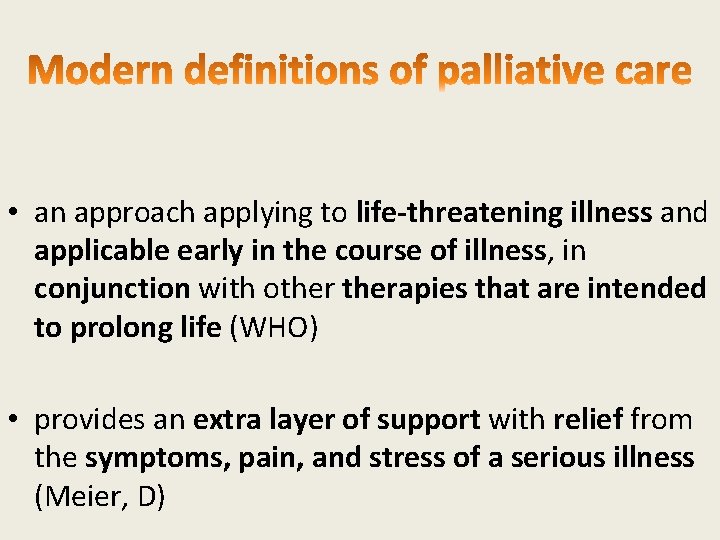
• an approach applying to life-threatening illness and applicable early in the course of illness, in conjunction with otherapies that are intended to prolong life (WHO) • provides an extra layer of support with relief from the symptoms, pain, and stress of a serious illness (Meier, D)
• Early identification desirable but is specialist work • Uncertainty will always remain • Communication is therefore complex – so hold on to Individualised care • Early integration with specialist palliative care improves outcomes for patients and families • Specialist palliative care is under resourced in Hospitals
Fiona. lisney@fhft. nhs. uk 01753 634879 Thanks to: Jo Wilson, TVSCN and Prof Irene Higginson for their data and slides
 Peter lisney
Peter lisney Parallel planning palliative care
Parallel planning palliative care Palliative fase
Palliative fase Principles of palliative care
Principles of palliative care Palliative prognostic index
Palliative prognostic index Log80 ausl romagna
Log80 ausl romagna Oacc palliative care
Oacc palliative care Anorexia palliative care
Anorexia palliative care Criterios de terminalidad
Criterios de terminalidad Goc palliative care
Goc palliative care Amber care meaning
Amber care meaning Esas-r
Esas-r Adjuvant neoadjuvant palliative
Adjuvant neoadjuvant palliative Epec palliative care
Epec palliative care Bluegrass care navigators hazard ky
Bluegrass care navigators hazard ky Palliative care versus hospice care
Palliative care versus hospice care Palliative care quality collaborative
Palliative care quality collaborative Ethical issues in palliative care
Ethical issues in palliative care Npcrc
Npcrc Palliative care matters
Palliative care matters Palliative care assistant
Palliative care assistant Goscote palliative care centre
Goscote palliative care centre Akps palliative
Akps palliative Franciscan hospice and palliative care
Franciscan hospice and palliative care Textbook of palliative care communication
Textbook of palliative care communication Provocative/palliative
Provocative/palliative Palliative care in nepal
Palliative care in nepal Difference between metoclopramide and domperidone
Difference between metoclopramide and domperidone European certificate in essential palliative care
European certificate in essential palliative care Driver diagram palliative care
Driver diagram palliative care Dr hong-phuc tran
Dr hong-phuc tran Tarek mahdi md
Tarek mahdi md Barry laird
Barry laird Problem severity score
Problem severity score Integrated palliative care outcome scale
Integrated palliative care outcome scale