Coronary CT Angiography Evidence review Speaker Dr Suneesh


![Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography [14] Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography [14]](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-20.jpg)
![Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis [15] • Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis [15] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-21.jpg)
![ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [16] • 4, 609 ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [16] • 4, 609](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-26.jpg)

![Multi-Ethnic Study of Atherosclerosis [19] • Ethnicity affects the likelihood of having CAC • Multi-Ethnic Study of Atherosclerosis [19] • Ethnicity affects the likelihood of having CAC •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-29.jpg)
![Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography [20] • Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography [20] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-31.jpg)
![Non-invasive detection of coronary artery stenoses with multislice CT or MRI [30] • 129 Non-invasive detection of coronary artery stenoses with multislice CT or MRI [30] • 129](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-42.jpg)
![Prediction of coronary events with electron beam computed tomography [30] • Asymptomatic men and Prediction of coronary events with electron beam computed tomography [30] • Asymptomatic men and](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-46.jpg)
![Coronary artery calcium score and risk classification for coronary heart disease prediction [40] • Coronary artery calcium score and risk classification for coronary heart disease prediction [40] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-58.jpg)
![Quantification of coronary atherosclerosis and inflammation to predict coronary events and all-cause mortality [44] Quantification of coronary atherosclerosis and inflammation to predict coronary events and all-cause mortality [44]](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-62.jpg)
![Relationship between C-reactive protein and subclinical atherosclerosis: the Dallas Heart Study [45] • CRP Relationship between C-reactive protein and subclinical atherosclerosis: the Dallas Heart Study [45] • CRP](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-63.jpg)
![ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [48] • 4, 609 ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [48] • 4, 609](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-68.jpg)
![Possible effect of treatment in asymptomatic patients Observational studies [53] • Retrospective study of Possible effect of treatment in asymptomatic patients Observational studies [53] • Retrospective study of](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-74.jpg)
![Possible effect of treatment in asymptomatic patients- RCT St Francis Heart Study [55] • Possible effect of treatment in asymptomatic patients- RCT St Francis Heart Study [55] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-76.jpg)
![BELLES TRIAL-RCT [56] • 615 Hyperlipidemic postmenopausal women, most with no history of CAD BELLES TRIAL-RCT [56] • 615 Hyperlipidemic postmenopausal women, most with no history of CAD](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-77.jpg)

- Slides: 93
Coronary CT Angiography Evidence review Speaker: Dr. Suneesh. K Senior Resident, Dept. of Cardiology Govt. Medical College Kozhikode 04 th March 2016
Introduction • Stress testing is the traditional non-invasive approach to detecting obstructive CAD • Need for direct (anatomic) assessment of the coronary artery lumen with invasive coronary arteriography • However, catheter-based angiography is expensive and is associated with a small risk of serious complications • 50 % or more of patients referred for an elective CAG are found to not have significant CAD [1] • Non-invasive visualization of coronary arteries is rendered difficult • Thus, potential imaging modalities must possess high temporal and spatial resolution [1] Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med 2010; 362: 886.

MDCT
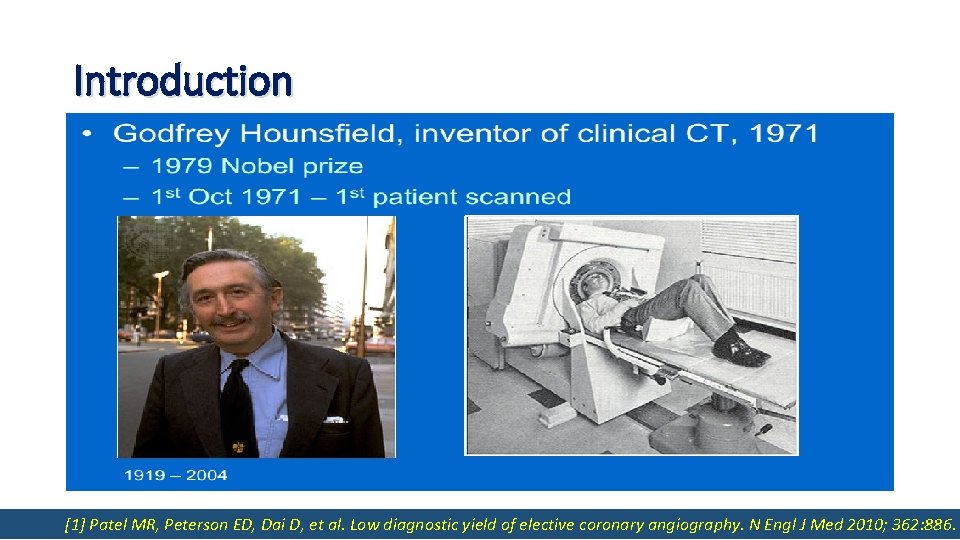
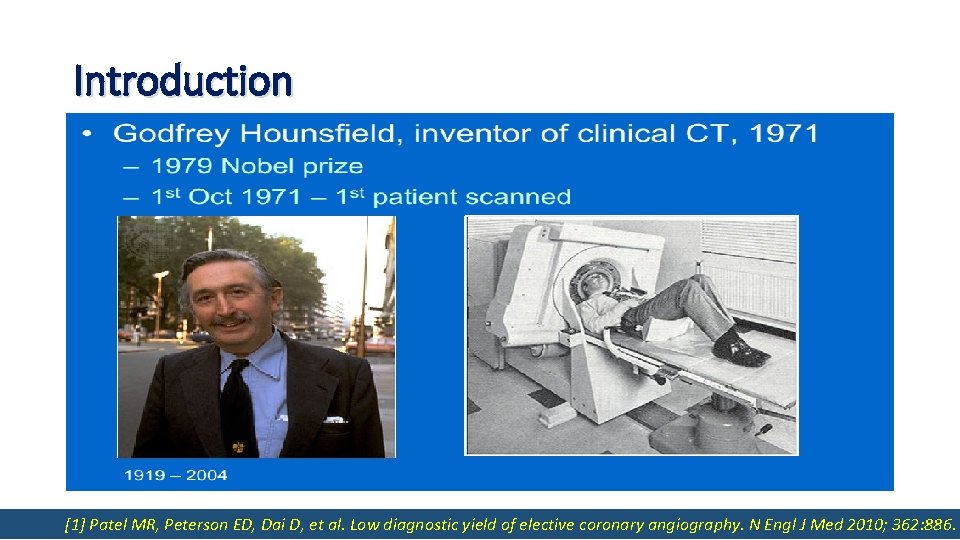
MDCT 4 ROW 16 ROW 64 ROW 320 ROW Temporal resolution (msec) 250 210 165 175 Spatial resolution (mm) 1. 25 1 0. 4 Volume coverage (cm) 0. 5 -0. 3 1 -2 2 -4 15 Breath-hold (S) 30 -40 20 10 2

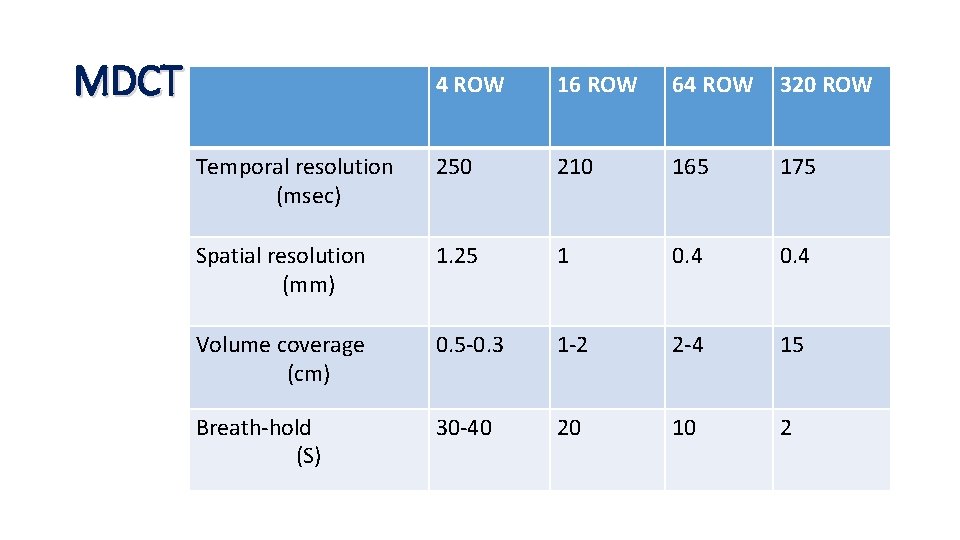
MDCT • Use mechanically rotating gantries • High temporal resolution • Acquisition of more than one image slice per gantry rotation • Temporal resolution of an MDCT scanner is defined by its gantry rotation time. • MDCT scanners used for CCTA should have a gantry rotation time of less than 420 msec corresponding to a temporal resolution of less than 210 msec [2] • Most MDCT scanners now in use acquire at least 64 slices simultaneously with a collimation of 0. 6 mm with a gantry rotation time of 333 msec (corresponding to a temporal resolution of approximately 167 msec) [3] [2]Leschka S, Alkadhi H, Plass A, et al. Accuracy of MSCT coronary angiography with 64 -slice technology: first experience. Eur Heart J 2005; 26: 1482. [3] Leber AW, Knez A, von Ziegler F, et al. Quantification of obstructive and nonobstructive coronary lesions by 64 -slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 2005; 46: 147.
Applications of Cardiac CT • Calcium scoring- Calcified plaque • Coronary CT angiography (CCTA) 1. Coronary artery anatomy 2. Stenosis 3. Stent viability 4. Graft anatomy and patency • Functional Imaging
The diagnostic and prognostic significance of Coronary calcium scanning coronary artery calcification. A report of 800 cases [5] • CAC - assessed in 800 by cardiac fluoroscopy and selective coronary cine-angiography • • Radiologic of fluoroscopy CAC in vivo - late 236 1950 [4]had > 75% stenosis Calcification detection was shown by in by 250 fluoroscopy subjects, of whom (94%) of 1 or more major coronary at CAG • Association between the arteries presence of CAC and the risk of cardiovascular events • was Among with significant CAD, 40% 1 st patients demonstrated by Margolis et(236/585) al [5] had calcification • Patients with calcification demonstrated poorer survival at all follow-up • EBCT in the early 1980 s permitted non-invasive and quantitative detection of CAC • 5 -year survival rate was 87% for patients without calcification, but 58% for those with st time for the 1 calcification • • Agatston The prognostic significance of coronary arteryand calcification appears to be independent of for score. The most widely used best-established measure of CAC information obtained by cardiac catheterization and angiocardiography assessment of the diagnostic and prognostic value of EBCT CAC scanning [4] BLANKENHORN DH, STERN D. Calcification of the coronary arteries. Am J Roentgenol Radium Ther Nucl Med 1959; 81: 772. [5] Margolis JR, Chen JT, et al. The diagnostic and prognostic significance of coronary artery calcification. A report of 800 cases. Radiology 1980; 137: 609. [6] Agatston AS, Janowitz WR, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827.
CAC Scanning (Contd. . ) Ultrafast CT was used to detect and quantify CAC levels in 584 subjects (mean age 48 +/- 10 years) 109 had clinical CAD and 475 had no clinical CAD 50 patients who 40 underwent and aultrafast CT were evaluated For age groups to 49 andfluoroscopy 50 to 59 years, total score of 50 also resulted in a sensitivity of 71% 20 contiguous 3 mm slices were obtained of the proximal coronary arteries and 74% andscores a specificity of 91% andbased 70%, on respectively Total calcium were calculated the number, areas and peak Hounsfield CT numbers of the calcific lesions detected For age group 60 to 69 years, a total score of 300 gave a sensitivity of 74% and a specificity of Ultrafast CT was more sensitive than fluoroscopy, detecting coronary calcium in 90% versus 52% of 81% patients • There were significant differences (p < 0. 0001) in mean total calcium scores for those with versus • those The NPV of a clinical 0 scorecoronary was 98%, artery 94% and 100%byfor age groups 40 to 49, 50 to 59 and 60 to 69 without disease decade: ü 5 years, versusrespectively 132, age 30 to 39 years ü 27 versus 291, age 40 to 49 years; • Ultrafast computed tomography is an excellent tool for detecting and quantifying coronary ü 83 versus 462, age 50 to 59 years artery calcium ü 187 versus 786, age 60 to 69 years • • • [6] Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15: 827.
Coronary artery calcium scanning (Contd. . ) • EBCT is now essentially obsolete • 64 -detector MDCT is considered state-of-the-art and most newer studies of CAC have been performed with this technology • One study demonstrated that CAC scores using both volume score and Agatston score were equivalent between EBT and 64 -detector MDCT
Comparison of coronary artery calcium scores between electron beam computed tomography and 64 -multidetector computed tomographic scanner [7] • Objective To Evaluate the interscan variation in CAC, Agatston score (AS), and volume score (VS) between EBT and 64 MDCT • Materials and methods 102 patients (mean age, 61. 1 years; 27 women) underwent dual CAC scanning with both EBT and 64 -MDCT. The AS and VS were measured with the Aquarius workstation (Tera. Recon, Inc, San Mateo, Calif). The correlation coefficient, Bland-Altman analysis, interscanner variation, and agreement in AS and VS scores between EBT and 64 -MDCT were computed. • Results Interscan agreement for presence of CAC was 99%. Median values were 286 and 268 mm for AS and 243 and 213 mm for VS with EBT and 64 -MDCT, respectively (P > 0. 05). There was significant linear relationship between scores from the 2 scanners (R = 0. 98 in AS and R = 0. 99 in VS; P < 0. 001). The interscanner variability between EBT and 64 -MDCT was 20. 9% and 17. 6% in AS and VS, respectively (P = NS) • Conclusion At CAC scanning, 64 -MDCT and EBT were comparable in AS and VS. The interscan variability between scanners is similar to interscan variability of 2 calcium scores done on the same equipment. [7] Mao SS, Pal RS, Mc. Kay CR, et al. Comparison of coronary artery calcium scores between electron beam computed tomography and 64 -multidetector computed tomographic scanner. J Comput Assist Tomogr 2009; 33: 175.
CAC and coronary artery stenosis • Presence and extent of CAC can predict the presence of coronary artery stenoses • But in general it is a better marker of the extent of coronary atherosclerosis than the severity of stenosis • Most of the clinical studies that examined the relationship between CAC and coronary artery stenoses have been performed in patients with chest pain who were referred for x-ray coronary angiography. Other studies evaluated coronary artery specimens obtained at autopsy.
CAC and coronary artery stenosis • Direct relationships have been established between CAC scores and histologic, intracoronary ultrasonic, and angiographic measures of coronary artery atherosclerosis and plaque burden on a vessel-by-vessel and segment-bysegment basis [ 8 -12 ] • MDCT performed without contrast enhancement has a low sensitivity for detecting plaques without appreciable calcification [ 9 ] and in one study, the cross-sectional plaque area found on histologic examination was approximately five times greater than the calcification area measured by EBCT [ 10 ]
Coronary Artery Calcium Area by Electron-Beam Computed Tomography and Coronary Atherosclerotic Plaque Area A Histopathologic Correlative Study [8] • 38 coronary arteries from 13 autopsy hearts were dissected, straightened, and scanned with EBCT in 3 -mm contiguous increments • Coronary calcium area was defined as 1 ≥ pixels with a density >130 HU (0. 18 mm 2/pixel) • Each artery was divided into corresponding 3 -mm segments, representative histological sections were stained, and atherosclerotic plaque area per segment (mm 2) was quantified. CAC and coronary artery plaque areas were correlated for the hearts as a whole, for individual coronary arteries, and for individual coronary artery segments. The sums of histological plaque areas versus the sums of calcium areas were highly correlated for each heart and for each coronary artery. However, coronary plaque area was on the order of five times greater than calcium area • This histopathologic study confirms an intimate relation between segmental coronary atherosclerotic plaque area and EBCT coronary calcium area [8] Rumberger JA, Simons DB, Fitzpatrick LA, et al. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation 1995; 92: 2157.
Comparison of electron beam computed tomography with intracoronary ultrasound and coronary angiography for detection of coronary atherosclerosis [9] • In 57 patients (54 +/- 9 years old), 267 coronary segments were analysed with EBCT, CAG and ICUS • The analysis was based on the number and extent of coronary calcifications on EBCT, coronary lumen reduction on CAG and plaque formation with and without ultrasound signs of calcifications on ICUS Results Conclusion • Compared with CAG, EBCT yielded a sensitivity of 66%, a specificity of 78%, a PPV of 39% and a NPV of 91% EBCT detects calcified plaques with high accuracy • Compared with ICUS, EBCT yielded an overall sensitivity of 66%, a specificity of 88% and an overall accuracy of 81% Plaques without ultrasound signs of calcifications can be detected by EBCT but with lower sensitivity • For plaques with and without ultrasound signs of calcifications, the sensitivity of EBCT was 97% and 47%, specificity 80% and 75% butandequivalent specificity overall accuracy 82% and 69%, respectively [9] Baumgart D, Schmermund A, Goerge G, et al. Comparison of electron beam computed tomography with intracoronary ultrasound and coronary angiography for detection of coronary atherosclerosis. J Am Coll Cardiol 1997; 30: 57.
Coronary calcium, as determined by electron beam computed tomography, and coronary disease on arteriogram. Effect of patient's sex on diagnosis [10] • 50 women and 89 men had EBCT scans done an average of 1 day after CAG • Maximum CAG % luminal diameter stenosis of any artery was paired with the total EBCT coronary calcium score for each subject • The women (age, 56 +/- 11 years [mean +/- SD]) were older than the men (age, 47 +/- 7 years), but the subjects were matched for indications for CAG and extent of disease as assessed by CAG • Sensitivity, specificity, and PPV and NPV for coronary calcium were nearly identical for men and women, regardless of the degree of arteriographic disease • EBCT was highly sensitive to the presence of arteriographic disease (range, 94% to 100%), but had only moderate specificity (57% to 66%) for significant disease (> or = 50% stenosis) and low specificity (35% to 38%) for any arteriographic disease (> 0% stenosis) • NPV in men and women ranged from 79% to 91% for any arteriographic disease and from 95% to 100% for significant disease, respectively [10] Rumberger JA, Sheedy PF 3 rd, Breen JF, Schwartz RS. Coronary calcium, as determined by electron beam computed tomography, and coronary disease on arteriogram. Effect of patient's sex on diagnosis. Circulation 1995; 91: 1363.
Ultrafast computed tomography as a diagnostic modality in the detection of coronary artery disease: a multicenter study [11] • 710 patients from 6 participating centres • Of the 710 patients enrolled, 427 patients had significant angiographic ds, and coronary calcification was detected in 404, yielding a sensitivity of 95% • Of the 23 patients without calcifications, 19 (83%) had SVD in CAG • Of the 283 patients without angiographically significant disease, 124 had negative ultrafast CT coronary studies, for a specificity of 44%. An increasing number of vessels with calcification present on ultrafast CT was found to increase specificity for the presence of obstructive CAD in at least one vessel (P <. 0001). As the log of the calcium score increases, the probability of multivessel obstructive disease increases (P <. 0001) Conclusion • The presence of calcifications in multiple vessels and in younger populations correlates with higher specificities for obstructive disease, making ultrafast CT coronary scanning a very useful diagnostic test [11] Budoff MJ, Georgiou D, Brody A, et al. Ultrafast computed tomography as a diagnostic modality in the detection of coronary artery disease: a multicenter study. Circulation 1996; 93: 898.
Coronary calcification and coronary atherosclerosis: site by site comparative morphologic study of electron beam computed tomography and coronary angiography [12] • 251 consecutive patients who underwent elective CAG for suspected CAD by EBCT and analyzed findings by site • Coronary calcifications were classified according to their length and width versus the diameter of the coronary artery in which the calcification was observed as: none, spotty, long, wide and diffuse • Coronary calcifications were found in 666 (27%) of 2, 470 segments • Morphologic evaluation of coronary calcifications using EBCT improved the prediction of coronary stenosis on a site by site basis and provided information related to angiographic morphology [12] Kajinami K, Seki H, Takekoshi N, Mabuchi H. Coronary calcification and coronary atherosclerosis: site by site comparative morphologic study of electron beam computed tomography and coronary angiography. J Am Coll Cardiol 1997; 29: 1549.
Correlation of coronary calcification and angiographically documented stenoses in patients with suspected coronary artery disease: results of 1, 764 patient [13] • A total of 1, 764 patients (1, 225 men and 539 women) with suspected CAD from a single center • EBCT (C 150 XP Imatron) and conventional coronary angiography • 56 % of men and 47% of women revealed significant coronary stenoses (> or =50 %) • Total exclusion of coronary calcium (14% of the study group) was associated with an extremely low probability of stenosis (<1 %). • With calcium scores > or =20 th, > or =100 th or > or =75 th percentile of age groups, the sensitivity to detect stenoses decreased to 97%, 93% and 81%, respectively, in men and to 98%, 82% and 76%, respectively, in women • Specificity increased up to 77% in men and women • There was a significant difference in coronary calcium between men and women in all age groups; however, ROC curves indicated that the test can be performed with equal accuracy in all of these subgroups • Calcium screening with EBCT is a highly sensitive and moderately specific test to predict stenotic disease [13] Haberl R, Becker A, Leber A, et al. Correlation of coronary calcification and angiographically documented stenoses in patients with suspected coronary artery disease: results of 1, 764 patients. J Am Coll Cardiol 2001; 37: 451.
![Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography 14 Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography [14]](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-20.jpg)
Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography [14] • 1851 patients with suspected CAD • EBCT in all patients • Total per-patient calcium scores and separate scores for the major coronary arteries were added • Overall sensitivity was 95%, and specificity was 66% for coronary calcium to predict obstructive disease on angiography • With calcium scores >20, >80, and >100, the sensitivity to predict stenosis decreased to 90%, 79%, and 76%, whereas the specificity increased to 58%, 72%, and 75%, respectively • EBCT calcium scanning provides incremental and independent power in predicting the severity and extent of angiographically significant CAD in symptomatic patients [14] Budoff MJ, Diamond GA, Raggi P, et al. Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation 2002; 105: 1791
![Electronbeam computed tomography in the diagnosis of coronary artery disease a metaanalysis 15 Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis [15] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-21.jpg)
Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis [15] • English-language studies from January 1, 1979, through February 29, 2000 • Study was included if it (1) used EBCT as a diagnostic test; (2) reported cases in absolute numbers of true-positive, false-positive, true-negative, and false-negative results; and (3) used CAG as the reference standard for diagnosing obstructive CAD (defined as > or = 50% diameter stenosis) • Results from 9 studies with 1662 subjects • Pooled sensitivity for EBCT was 92. 3% and pooled specificity was 51. 2% [15] Nallamothu BK, Saint S, Bielak LF, et al. Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis. Arch Intern Med 2001; 161: 833.
Single centre studies 64 -slice CT for diagnosis of coronary artery disease: a systematic review • Review of single center studies comparing 64 -slice MDCT and CAG • In 23 studies including results in 2045 patients, the per patient pooled sensitivity for significant (≥ 50%) stenosis was 98 % (range 88 to 100 %) and the pooled specificity was 88 % (range 59 to 100 %) • Data from 4 studies for detection of high-grade (≥ 70 %) stenosis yielded a pooled sensitivity of 91 % and a pooled specificity of 88 % Stein PD, Yaekoub AY, Matta F, Sostman HD. 64 -slice CT for diagnosis of coronary artery disease: a systematic review. Am J Med 2008; 121: 715.
Multicentre studies • ACCURACY trial - 230 (94 %) of 245 enrolled subjects completed the study protocol. Patient-based sensitivity PPV 64 % and specificity of CCTA were 95 % and 83 %, respectively NPV 95 -100 % Specificity fell to 53 % for patients with calcium scores >400 Agatston units • CORE 64 study - Multicenter, single vendor international, 291 (72 %) of 405 enrolled patients were eligible PPV 91 % NPV 95 -100 % Patient-based sensitivity and specificity of CCTA were 85 % and 90 %, respectively • Netherland multicentre multivendor study -360 (97 %) of 371 enrolled patients completed the protocol PPV 86 % NPV 95 -100 % Patient-based sensitivity and specificity of CCTA were 99 % and 64 %, respectively Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64 -multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY trial. J Am Coll Cardiol 2008; 52: 1724. Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64 -row CT. N Engl J Med 2008; 359: 2324. Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy of 64 -slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 2008; 52: 2135.
Combined testing with SPECT r. MPI • Limited ability to address the physiologic impact of any lesions • Persistently suboptimal specificity
Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions • First report of a combined CT (16 slice)/SPECT Scanner • Included 56 patients with known or suspected CAD who underwent pharmacologic / EST • All patients underwent CAG within 4 weeks of the procedure • Sensitivity increased from 84 to 96 % • Specificity increased from 74 to 95 % • PPV increased from 61 to 77 % and NPV increased from 90 to 99 % Further studies are anticipated, particularly those using higher resolution CT machines. But combined SPECT and CCTA exposes the patient to even greater doses of potentially harmful ionizing radiation. Rispler S, Keidar Z, Ghersin E, et al. Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions. J Am Coll Cardiol 2007; 49: 1059.
![ACCURACY Trial Progression of coronary artery calcium predicts allcause mortality 16 4 609 ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [16] • 4, 609](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-26.jpg)
ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [16] • 4, 609 consecutive asymptomatic individuals referred by primary physicians for CAC measurement with EBCT, who underwent repeat screening • Average interscan time was 3. 1 years, and there were 288 deaths • Progression of CAC was significantly associated with mortality regardless of the method used to assess progression (p < 0. 0001) • CAC progression added incremental value in predicting all-cause mortality over baseline score, time between scans, demographics, and cardiovascular risk factors. • ACCURACY trial confirmed the high sensitivity but low specificity of CAC for obstructive disease • Sensitivity/Specificity for CAC >0, >100, and >400 were 98 %/42 %, 88 %/71 %, and 60 %/88 %, respectively. [16] Budoff MJ, Hokanson JE, Nasir K, et al. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging 2010; 3: 1229.

CAC scoring • Highly sensitive for the presence of ≥ 50 percent angiographic stenosis • But only moderately specific, especially in individuals over 60 years of age • In a review of 16 studies, the sensitivity and specificity of EBCT were 91 and 49 %, respectively [ 18 ] • Absence of CAC is highly predictive of the absence of significant coronary artery stenosis [18] O'Rourke RA, Brundage BH, Froelicher VF, et al. ACC/AHA Expert Consensus document on electron-beam computed tomography for the diagnosis and prognosis of coronary artery disease. Circulation 2000; 102: 126.
CAC scoring • 0 — No identifiable disease • 1 to 99 — Mild disease • 100 to 399 — Moderate disease • ≥ 400 — Severe disease
![MultiEthnic Study of Atherosclerosis 19 Ethnicity affects the likelihood of having CAC Multi-Ethnic Study of Atherosclerosis [19] • Ethnicity affects the likelihood of having CAC •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-29.jpg)
Multi-Ethnic Study of Atherosclerosis [19] • Ethnicity affects the likelihood of having CAC • But the predictive value of CAC is similar among various ethnic groups • • 6814 As with of clinical coronary menthe andprevalence women (mean age 63 years) US disease, CAC scores were higher in men compared toinduvidual women and increased progressively with age • Asymptomatic • For men, CAC scores were highest in whites and Hispanics; the scores were lowest in • Among men, the prevalence of CAC was significantly higher in whites than in Chinese, Hispanics, blacks at (70 younger and Chinese at older ages and blacks versusages 59, 56, and 52 percent, respectively) • • AFor women, CAC scores were highest in whites and generally lowest in Hispanics, similar trend was noted in women, although CAC was less common (45 versus 42, 35, and 37 although Chinese women had the lowest scores in the oldest age group percent, respectively) [19] Bild DE, Detrano R, Peterson D, et al. Ethnic differences in coronary calcification: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2005; 111: 1313.
CAC and Myocardial Ischemia • CAC is present in most patients with myocardial ischemia, both symptomatic and asymptomatic • Silent (asymptomatic) myocardial ischemia is an important manifestation of coronary heart disease (CHD), accounting for more than 75 % of ischemic episodes during daily life • Most silent ischemic episodes occur during minimal or no physical exertion. The relationship between silent ischemia, detected by stress testing, and CAC has been evaluated in a number of studies
![Relationship between stressinduced myocardial ischemia and atherosclerosis measured by coronary calcium tomography 20 Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography [20] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-31.jpg)
Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography [20] • 1, 195 patients without known CAD, 51% asymptomatic, underwent stress MPS and CAC ischemia by MPS waswith compared to likelihood the magnitude CAC abnormality § • Frequency Ischemicof. MPS is associated a high of of subclinical atherosclerosis by • Among 76 patients with ischemic MPS, CAC scores >0 in 95%, >or=100 in 88%, and >or=400 in 68% CAC, but is rarely seen for CAC scores <100 • Of 1, 119 normal MPS, CAC scores were >0, >or=100, and >or=400 in 78%, 56%, and 31%, respectively § • The Normal MPSofpatients, frequently have. CAC extensive atherosclerosis by CAC criteria frequency ischemic MPS was <2% with scores <100 and increased progressively with CAC for trend <0. 0001). § >or=100 These (p findings imply a potential role for applying CAC screening after MPS among • Patients with symptoms with CAC scores >or=400 had increased likelihood of MPS ischemia versus patients manifesting those without symptoms (pnormal = 0. 025). MPS • Absolute rather than percentile CAC score was the most potent predictor of MPS ischemia by multivariable analysis. Importantly, 56% of patients with normal MPS had CAC scores >or=100. [20] Berman DS, Wong ND, Gransar H, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol 2004; 44: 923.
Severity of coronary artery calcification by electron beam computed tomography predicts silent myocardial ischemia [21] • 3895 asymptomatic subjects with EBCT • 411 of whom had SPECT within a close (median, 17 days) time period • SPECT and exercise treadmill results were compared with the CACS as assessed by EBCT • Although most subjects (78 %) with CAC on EBCT did not have inducible ischemia with exercise testing, the likelihood of ischemia increased with CAC score, regardless of age or sex • CACS <10 – normal SPECT • CAC 11 to 100 – 2. 6 % had abnormal SPECT • CAC 101 to 399 - 11. 3% had abnormal SPECT • CAC>/=400 - 46% had abnormal SPECT (P<0. 0001) • CACS predicted an abnormal SPECT regardless of subject age or sex • CACS identifies a high-risk group of asymptomatic subjects who have clinically important silent myocardial ischemia [21] He ZX, Hedrick TD, Pratt CM, et al. Severity of coronary artery calcification by electron beam computed tomography predicts silent myocardial ischemia. Circulation 2000; 101: 244.
Comparison of coronary calcium and stress MPI in apparently healthy siblings of individuals with premature coronary artery disease [22] • High-risk population • 260 asymptomatic middle-age siblings of hospitalized index patients <60 years of age with documented coronary artery disease • Maximal exercise testing with post-exercise and delayed attenuation-corrected thallium SPECT and MDCT for CAC • Inducible ischemia on r. MPI 26 % overall, in 51 % with a CAC score >100, and in 13 % with lower CAC scores. • 59 % of siblings with inducible ischemia had a CAC score ≤ 100 [22] Blumenthal RS, Becker DM, Yanek LR, et al. Comparison of coronary calcium and stress myocardial perfusion imaging in apparently healthy siblings of individuals with premature coronary artery disease. Am J Cardiol 2006; 97: 328.
Coronary artery calcification and myocardial perfusion in asymptomatic adults: the MESA (Multi-Ethnic Study of Atherosclerosis) [23] • Total of 222 men and women, ages 45 to 84 years old and free of CHD diagnosis • Myocardial blood flow (MBF) was measured using MRI during rest and adenosine-induced • These observations suggest that the presence of CAC can be associated with abnormal hyperemia endothelial (another potential predictor • Agatston physiology CAC score was determined from chest MDCT of future cardiac events) at an early stage of CHD when functionally significant, fixed coronary stenoses absent • Mean values of hyperemic MBF and perfusion reserve, but not resting MBF, are werestill monotonically lower across increasing CAC levels • Coronary vasodilatory response was associated inversely with the presence and severity of CAC in asymptomatic adults [23] Wang L, Jerosch-Herold M, Jacobs DR Jr, et al. Coronary artery calcification and myocardial perfusion in asymptomatic adults: the MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2006; 48: 1018.
Emergency department evaluation of chest pain • Among patients presenting to the ED with chest pain, those with no CAC have low cardiac event rates • Although coronary calcification does not occur in the absence of coronary atherosclerosis, the converse is not true • Functionally significant coronary stenosis due to non-calcified plaque can occur with minimal or totally absent coronary calcification
Screening patients with chest pain in the emergency department using electron beam tomography: a follow-up study [24] • Prospective observational study of 192 patients admitted to the ED of a tertiary care hospital for chest pain • EBCT for all patients • Average follow-up was 50 +/- 10 months • 58 patients had coronary events • Presence of CAC (score >0) and increasing score quartiles were strongly related to the occurrence of hard cardiac events including myocardial infarction and death (p < 0. 001) and all cardiovascular events (p < 0. 001) • CAC=0 might be useful in the emergency room setting as a tool to rule out myocardial ischemia in symptomatic patients [24] Georgiou D, Budoff MJ, Kaufer E, et al. Screening patients with chest pain in the emergency department using electron beam tomography: a follow-up study. J Am Coll Cardiol 2001; 38: 105.
Computed tomographic coronary artery calcium assessment for evaluating chest pain in the emergency department: long-term outcome of a prospective blind study [25] • Men aged 30 -62 years and Women aged 30 -65 years with chest pain and low-to-moderate probability of CAD • CT CAC assessment prospectively • Primary outcome- ACS, death, STEMI/NSTEMI, Secondary outcomes- CABG/PTCA • When a CAC cut-off score of 36 was used, as suggested by ROC analysis, • Follow-up at 30 days, 1 year, and 5 years sensitivity was 90%; specificity, 85%; PPV was 44%; and NPV was 99% • 263 study patients • • 133 During long-term follow-up, patients without CAC experienced no cardiac events (51%) had a CAC score of zero- correlated strongly with the LH of NCCP at 30133 days, 1 with year, • Among patients a CACand score 5 of years zero, only 1 (<1%) had cardiac chest pain • Of the 31 patients shown to have cardiac chest pain, 30 (97%) had CAC on CT [25] Laudon DA, Behrenbeck TR, Wood CM, et al. Computed tomographic coronary artery calcium assessment for evaluating chest pain in the emergency department: long-term outcome of a prospective blind study. Mayo Clin Proc 2010; 85: 314.
Non-invasive evaluation with multislice computed tomography in suspected ACS: plaque morphology on MDCT versus CAC score [26] • In 40 patients (age 57 ± 11 years, 26 men) suspected ACS • MSCT coronary angiography in combination with CCS was performed before conventional coronary angiography • MSCT angiograms were evaluated for the presence or absence of coronary atherosclerotic plaque and the presence or absence of obstructive (≥ 50% luminal narrowing) CAD • Plaque type was determined, and findings were related to the calcium score In with suspected noncalcified plaques are • 38 patients had CAD, presenting of whom 10 patients had nonobstructive and 28 patients ACS, had obstructive CAD (Confirmed by CAG) highly prevalent and the absence of coronary calcium does not reliably • In patients with CAD, plaques were distributed as follows: 39% noncalcified plaques, 47% mixed plaques, and 14% calcified plaques • CCS was detected in 27 patients, of whom 10 had a score >400 exclude thenopresence ofobserved, (significant) atherosclerosis • In 13 (33%) patients, coronary calcium was but in 11 (85%), atherosclerotic plaques were detected on MSCT angiography. [26] Henneman MM, Schuijf JD, Pundziute G, et al. Noninvasive evaluation with multislice computed tomography in suspected acute coronary syndrome: plaque morphology on multislice computed tomography versus coronary calcium score. J Am Coll Cardiol 2008; 52: 216.
Interrelation of coronary calcification, myocardial ischemia, and outcomes in patients with intermediate likelihood of coronary artery disease: a combined positron emission tomography/computed tomography study [27] • 695 consecutive intermediate-risk patients • Undergoing combined rest-stress rubidium 82 PET perfusion imaging and CAC scoring on a hybrid PET-CT scanner • Frequency of abnormal scans among patients with a CAC score > or = 400 was higher than that in patients with a CAC score of 1 to Although increasing CAC content is generally predictive of a higher likelihood of 399 (48. 5% versus 21. 7%, P<0. 001). • Frequency ofits ischemia among patients CAC was 16. 0%, and its absence only afforded a negative of predictive value of 84. 0% ischemia, absence doeswith notnocompletely eliminate the possibility flow-limiting • coronary Among patients with normal PET myocardial perfusion imaging, the annualized event rateoccurs in patientsin with no CAC wasof lower than artery disease. Importantly, a stepwise increase the risk in those with a CAC score > or = 1000 (2. 6% versus 12. 3%, respectively). Likewise, in patients with ischemia on PET myocardial adverse events increasing scores withpatients and without ischemia perfusion imaging, thewith annualized event rate in. CAC those with no CACin waspatients lower than among with a CAC score > or = 1000 (8. 2% versus 22. 1%) on PET myocardial perfusion imaging [27] Schenker MP, Dorbala S, Hong EC, et al. Interrelation of coronary calcification, myocardial ischemia, and outcomes in patients with intermediate likelihood of coronary artery disease: a combined positron emission tomography/computed tomography study. Circulation 2008; 117: 1693.
Comparison of CCTA and CMR Meta-analysis of comparative diagnostic performance of MRI and multislice CT for non-invasive coronary angiography [28] • Meta-analysis of 51 studies compared the diagnostic performance of multislice CCTA and CMRI for the detection of ≥ 50 % diameter stenosis • Multislice CCTA had significantly higher sensitivity (85 vs 72 % & specificity (95 vs 87 %) • Meta-analysis of the available studies with MRI and MSCT for non-invasive coronary angiography indicates that MSCT has currently a significantly higher accuracy to detect or exclude significant CAD [28] Schuijf JD, Bax JJ, Shaw LJ, et al. Meta-analysis of comparative diagnostic performance of magnetic resonance imaging and multislice computed tomography for noninvasive coronary angiography. Am Heart J 2006; 151: 404.
Head-to-head comparison of three-dimensional navigator-gated MRI and 16 -slice CT to detect coronary artery stenosis in patients [29] • 52 patients underwent CMR and 16 -slice MDCT before invasive CAG • MR and MDCT had similar sensitivity (75% vs. 82%, p = NS), specificity (77% vs. 79%, p = NS), and diagnostic accuracy (77%, vs. 80%, p = NS) for detection of >50 % stenosis [29] Kefer J, Coche E, Legros G, et al. Head-to-head comparison of three-dimensional navigator-gated magnetic resonance imaging and 16 -slice computed tomography to detect coronary artery stenosis in patients. J Am Coll Cardiol 2005; 46: 92.
![Noninvasive detection of coronary artery stenoses with multislice CT or MRI 30 129 Non-invasive detection of coronary artery stenoses with multislice CT or MRI [30] • 129](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-42.jpg)
Non-invasive detection of coronary artery stenoses with multislice CT or MRI [30] • 129 consecutive patients with suspected CAD • Single center study • Multislice CT and MRI were both performed within a median of 1 day before conventional CAG, which served as the reference standard • Per patient sensitivity was significantly better with CCTA (92 versus 74 %) and the specificities were similar • Sensitivity for detecting clinically significant stenoses was 82% for multislice CT and 54% for MRI (P < 0. 001) [30] Dewey M, Teige F, Schnapauff D, et al. Noninvasive detection of coronary artery stenoses with multislice computed tomography or magnetic resonance imaging. Ann Intern Med 2006; 145: 407.
CAC and prognosis in asymptomatic patients
Electron-beam tomography coronary artery calcium and cardiac events: a 37 month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults [28] • 8855 initially asymptomatic adults, Age 30 to 76 (26% women) • Follow-up 37+/-12 m • In men, events (n=192) were associated with the presence of CAC (RR=10. 5, P<0. 001), diabetes (RR=1. 98, P=0. 008), and smoking (RR=1. 4, P=0. 025) • In women, events (n=32) were linked to the presence of CAC (RR=2. 6, P=0. 037) and not risk factors • At 37 -month follow-up, presence of any CAC at baseline (score greater than 0) was associated with a Knowledge of the presence of EBT CAC provides incremental information in significantly higher event rate in men (6. 1 versus 0. 4 % for those without any CAC) and women (3. 3 versus 1. 0 %) addition to that defined by conventional CAD risk assessment [28] Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37 -month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation 2003; 107: 2571.
Predictive value of electron beam computed tomography of the coronary arteries. 19 -month follow-up of 1173 asymptomatic subjects [29] • 1173 asymptomatic subjects who underwent EBCT between September 1993 and March 1994 • Follow-up of 19 months • 18 subjects had 26 cardiovascular events • For CAC score thresholds of 100, 160, and 680, EBCT had sensitivities of 89%, and 50% and specificities of 77%, 82%, and 95%, respectively • Odds ratios ranged from 20. 0 to 35. 4 (P <. 0001 for all) • EBCT predicts future atherosclerotic cardiovascular disease events in asymptomatic subjects [29] Arad Y, Spadaro LA, Goodman K, et al. Predictive value of electron beam computed tomography of the coronary arteries. 19 month follow-up of 1173 asymptomatic subjects. Circulation 1996; 93: 1951.
![Prediction of coronary events with electron beam computed tomography 30 Asymptomatic men and Prediction of coronary events with electron beam computed tomography [30] • Asymptomatic men and](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-46.jpg)
Prediction of coronary events with electron beam computed tomography [30] • Asymptomatic men and women undergoing coronary EBCT • 1, 172 subjects (baseline age 53 +/- 11 years, 71% men) • Average follow-up of 3. 6 years • 39 subjects sustained coronary events • Mean CAC Score was 764 +/- 935 among subjects with events as compared with 135 +/- 432 among those without events (p < 0. 0001) • Odds ratios for all events remained high (14. 3 to 20. 2) • In asymptomatic adults, EBCT predicts coronary death and nonfatal MI and the need for revascularization [30] Arad Y, Spadaro LA, Goodman K, et al. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol 2000; 36: 1253.
Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study [31] • Prospective, population-based study, 4, 903 asymptomatic persons age 50 to 70 years underwent EBCT • 4. 3 years, follow-up • Subjects with ASCVD events had higher baseline CAC scores than those without events: 384 vs 10 (p < 0. 0001) • For CCA score threshold > or = 100 versus < 100, relative risk 9. 6 (95% CI 6. 7 to 13. 9) for all ASCVD events, 11. 1 (7. 3 to 16. 7) for all CAD events, and 9. 2 (4. 9 to 17. 3) for non-fatal myocardial infarction and death • Coronary calcium score predicted CAD events independently of standard risk factors and CRP (p = 0. 004), was superior to the Framingham risk index in the prediction of events [31] Arad Y, Goodman KJ, Roth M, et al. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol 2005; 46: 158.
Probabilistic model for prediction of angiographically defined obstructive coronary artery disease using electron beam computed tomography calcium score strata [32] • Clinical research patients (n=213) were examined with coronary angiography and EBCT (angiography group) • 765 research participants - only EBCT (nonangiography group) • Of the angiography group, 53% had obstructive CAD • After adjustment for verification bias, the estimated sensitivity and specificity for calcium score > or =1 were 97. 0% and 72. 4%, respectively • A calcium score > or =200 among those > or =50 years old and calcium score > or =100 among those <50 years old provided strong evidence that patients of either sex had obstructive CAD • A calcium score of 0 provided strong evidence that patients > or =50 years old did not have obstructive CAD [32] Probabilistic model for prediction of angiographically defined obstructive coronary artery disease using electron beam computed tomography calcium score strata. Circulation 2000; 102: 380.
Identifying high-risk individuals
Using the coronary artery calcium score to predict coronary heart disease events: a systematic review and meta-analysis [33] • Included studies that reported measuring CAC score by EBCT in asymptomatic subjects and subsequent follow-up for coronary events • Meta-analysis of the 4 studies meeting inclusion criteria • Adjusted RR of 2. 1 (95% CI 1. 6 -2. 9) for a CAC score of 1 to 100, compared to CAC score of 0 • RR estimates for higher calcium scores were higher, ranging from 3. 0 to 17. 0 • CAC score is an independent predictor of coronary heart disease events [33] Pletcher MJ, Tice JA, Pignone M, Browner WS. Using the coronary artery calcium score to predict coronary heart disease events:
Detection of high-risk young adults and women by coronary calcium and National Cholesterol Education Program Panel III guidelines [34] • • Purpose ofcalcium this study Absence of 35% was to investigate the classification of cardiovascular risk in • young CCS of 0 individuals to 99 (mild) and 44% women according to the NCEP guidelines across a of CAC Score • continuum 100 to 399 (moderate) 12% • 1, 611 > or =400 (severe) 9% individuals asymptomatic 59% of patients with CCS > or 73% with a CCSEBCT > or =75 th identified as • 67% men, mean age: 53=400 +/- and 10 yearssingle CACpercentile Scanningwere for not screening high risk and were not given pharmacotherapy on the basis of NCEP categories • Categorized into low-risk (n = 738, 46%), intermediate-risk (n = 583, 36%), NCEP guidelines seem to underestimate cardiovascular risk in young asymptomatic individuals moderately high-risk (n = 263, 16%), and high-risk (n = 27, 2%) according to the and women. For these individuals, assessment of plaque burden might provide incremental value NCEP ATP III to global risk assessment [34] Nasir K, Michos ED, Blumenthal RS, Raggi P. Detection of high-risk young adults and women by coronary calcium and National Cholesterol Education Program Panel III guidelines. J Am Coll Cardiol 2005; 46: 1931.
Dyslipidaemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium [35] • Multicenter cohort study of 6814 subjects (age 45 to 84) • Free of clinical cardiovascular disease at baseline • Among high-risk individuals, 19. 7% of those who did not qualify for lipid-lowering drug treatment had CAC >400 • Overall, 40 % of eligible persons with a CAC score >400 were not receiving lipid-lowering drugs [35] Goff DC Jr, Bertoni AG, Kramer H, et al. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): gender, ethnicity, and coronary artery calcium. Circulation 2006; 113: 647.
Effect on prognosis • CAC score adds independent prognostic information to that determined by the Framingham risk score across ethnic groups • The magnitude of this effect is best illustrated in the following five observational, population-based studies § § § Greenland et al……………… JAMA 2004 Shaw et al………………. Radiology 2003 Budoff et al…………………. J Am Coll Cardiol 2007 Erbel et al……………………. J Am Coll Cardiol 2010 Polonsky et al………………… JAMA 2010
Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals [36] • Prospective observational population-based study • 1461 asymptomatic adults • 8 year follow-up • Across categories of FRS, CACS was predictive of risk among patients with an FRS higher than 10% (P<. 001) but not with an FRS less than 10% • Increase in events was most pronounced at CAC scores above 300 [36] Greenland P, La. Bree L, Azen SP, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA 2004; 291: 210.
Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality [37] • 10, 377 asymptomatic individuals undergoing cardiac risk factor evaluation and coronary calcium screening with electron-beam CT • CAC score was a significant independent predictor of all-cause mortality after adjustment for family history, hyperlipidemia, hypertension, smoking, and diabetes • Using the NCEP/ATP III model 5 -year mortality varied according to the CAC score (from less than 10 to more than 1000) from 0. 9 to 3. 9 percent, 1. 1 to 9. 0 percent, and 2. 0 to 12. 2 percent in low, intermediate, and high-risk Framingham subsets • Coronary calcium was an independent predictor of mortality (P <. 001) [37] Shaw LJ, Raggi P, Schisterman E, et al. Prognostic value of cardiac risk factors and coronary artery calcium screening for allcause mortality. Radiology 2003; 228: 826.
Long-term prognosis associated with coronary calcification: observations from a registry of 25, 253 patients [38] • 25, 253 consecutive, asymptomatic individuals referred by their primary physician for CAC scanning to assess cardiovascular risk • Death rate was 2% after an average follow-up of 6. 8 years • After adjustment for age and traditional risk factors, 10 -year survival was 99. 4 %for a CAC score of 0 and 87. 8 % for a score >1000 • CAC score predicted all-cause mortality independent of and more accurately than standard coronary artery disease risk factors [38] Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25, 253 patients. J Am Coll Cardiol 2007; 49: 1860.
Coronary Risk Stratification, Discrimination, and Reclassification Improvement Based on Quantification of Subclinical Coronary Atherosclerosis: The Heinz Nixdorf Recall Study [39] • 4129 subjects without known CAD • Followed for 5 years after CAC • FRS was scored • In intermediate risk subjects by FRS, 21. 7 % were reclassified into the low-risk category and 30. 6 % were reclassified into the high-risk category • Adding CAC scores increased the area under the ROC from 0. 681 to 0. 749 compared to FRS and from 0. 653 to 0. 755 compared to NCEP/ATPIII [39] Erbel R, Möhlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 2010; 56: 1397.
![Coronary artery calcium score and risk classification for coronary heart disease prediction 40 Coronary artery calcium score and risk classification for coronary heart disease prediction [40] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-58.jpg)
Coronary artery calcium score and risk classification for coronary heart disease prediction [40] • Adding CAC to traditional risk factors in the MESA cohort including age, sex, tobacco use, systolic blood pressure, antihypertensive medication use, total and HDL cholesterol, race, and ethnicity resulted in a net reclassification index of 0. 25, implying that 25 % of patients were reclassified into a different risk group based on CAC [40] Polonsky TS, Mc. Clelland RL, Jorgensen NW, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 2010; 303: 1610.
Role in the elderly- Rotterdam Study • Followed 2028 asymptomatic elderly with a mean age of 69. 2 for a median of 9. 2 years • In the intermediate risk group (10 -year FRS 10 to 20 percent), CAC reclassified 52 percent of the population with scores >615 Agatston units reclassifying individuals as high risk and scores <50 reclassifying them as low risk [41] • A 3570 patients over the age of 70 • 40 percent of these patients could be reclassified, primarily by excluding risk (CAC <400) in those with multiple risk factors [42] [41] Elias-Smale SE, Proença RV, Koller MT, et al. Coronary calcium score improves classification of coronary heart disease risk in the elderly: the Rotterdam study. J Am Coll Cardiol 2010; 56: 1407. [42] Raggi P, Gongora MC, Gopal A, et al. Coronary artery calcium to predict all-cause mortality in elderly men and women. J Am Coll Cardiol 2008; 52: 17.
Comparison to hs. CRP and other biomarkers
Combined use of computed tomography coronary calcium scores and Creactive protein levels in predicting cardiovascular events in nondiabetic individuals [43] • 1461 patients without known CHD (1990 -1992) • Followed for 6. 4 years; 104 (7 %) had an MI, stroke, revascularization, or coronary death • Relative risk for those with the highest quartile hs. CRP and highest tertile CAC scores (>4. 05 and >142. 1) was 7. 5 -fold greater than the risk for those with lower hs. CRP (<4. 05) and the lowest quartile CAC (<3. 7) • Participants without diabetes and those at intermediate risk may benefit from risk stratification based on hs-CRP levels and CAC, because both factors contribute independently toward the incidence of cardiovascular events [43] Park R, Detrano R, Xiang M, et al. Combined use of computed tomography coronary calcium scores and C-reactive protein levels in predicting cardiovascular events in nondiabetic individuals. Circulation 2002; 106: 2073.
![Quantification of coronary atherosclerosis and inflammation to predict coronary events and allcause mortality 44 Quantification of coronary atherosclerosis and inflammation to predict coronary events and all-cause mortality [44]](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-62.jpg)
Quantification of coronary atherosclerosis and inflammation to predict coronary events and all-cause mortality [44] • 4129 individuals as CAC and hs. CRP • CAC and hs. CRP independently predicted coronary events and deaths • The net reclassification improvement was higher for CAC (23. 8 %) than for CRP (10. 5 %) [44] Möhlenkamp S, Lehmann N, Moebus S, et al. Quantification of coronary atherosclerosis and inflammation to predict coronary events and all-cause mortality. J Am Coll Cardiol 2011; 57: 1455.
![Relationship between Creactive protein and subclinical atherosclerosis the Dallas Heart Study 45 CRP Relationship between C-reactive protein and subclinical atherosclerosis: the Dallas Heart Study [45] • CRP](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-63.jpg)
Relationship between C-reactive protein and subclinical atherosclerosis: the Dallas Heart Study [45] • CRP in 3373 subjects 30 to 65 years of age • Multiethnic, population-based, probability sample • EBCT CAC in 2726 subjects, and • MRI was used to measure aortic plaque in 2393 • CRP levels were associated with most traditional cardiovascular risk factors • Subjects with CAC had higher median CRP levels than those without CAC • There was a modest trend toward increasing CRP levels with increased CAC levels in men (P for trend=0. 003) but not in women (P for trend=0. 08) • Male subjects with aortic plaque also had higher CRP levels than those without (median, 2. 3 versus 1. 8; P<0. 001) • In multivariate analysis adjusted for traditional cardiovascular risk factors, body mass index, and estrogen and statin medication use, the associations between CRP levels and CAC and CRP levels and aortic plaque were no longer statistically significant [45] Khera A, de Lemos JA, Peshock RM, et al. Relationship between C-reactive protein and subclinical atherosclerosis: the Dallas Heart Study. Circulation 2006; 113: 38.
Added value in smokers Prognostic value of coronary artery calcium screening in asymptomatic smokers and non-smokers [46] • A referred patient registry of 10, 377 asymptomatic individuals • 40% were current smokers • 5 -year follow-up • Smokers had survival rates that varied directly with the CAC score, ranging from 99. 5 % in the 50 % of patients with a score of 0 to 10 to 81. 4 % in the 4. 4 % of patients with a score >1000 • This effect was seen in younger and older patients, with the RR being highest in older smokers • For smokers between the ages of 40 and 49, a CAC score >1000 was associated with a RR of mortality of 8. 9 [46] Shaw LJ, Raggi P, Callister TQ, Berman DS. Prognostic value of coronary artery calcium screening in asymptomatic smokers and non-smokers. Eur Heart J 2006; 27: 968.
CAC progression and risk
CAC progression and risk • Rapid angiographic progression of coronary atherosclerosis is associated with increased risk of cardiovascular events • Annualized progression of CAC measured by EBCT is approximately 25 % in the general population but as high as 50 % in asymptomatic patients with multiple conventional risk factors
Progression of Coronary Artery Calcium and Risk of First Myocardial Infarction in Patients Receiving Cholesterol-Lowering Therapy [47] • 495 asymptomatic subjects submitted to EBCT • Statins were started after the initial EBT scan • MI was recorded in 41 subjects (8. 3%) during a follow-up of 3. 2± 0. 7 years • Mean LDL level did not differ between groups • MI subjects demonstrated a CAC change of 42%± 23% yearly • Event-free subjects showed a 17%± 25% yearly change (P=0. 0001) • RR of having an MI in the presence of CAC progression was 17. 2 -fold (95% CI: 4. 1 to 71. 2) higher than without CAC progression (P<0. 0001) [47] Raggi P, Callister TQ, Shaw LJ. Progression of coronary artery calcium and risk of first myocardial infarction in patients receiving cholesterol-lowering therapy. Arterioscler Thromb Vasc Biol 2004; 24: 1272.
![ACCURACY Trial Progression of coronary artery calcium predicts allcause mortality 48 4 609 ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [48] • 4, 609](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-68.jpg)
ACCURACY Trial Progression of coronary artery calcium predicts all-cause mortality [48] • 4, 609 consecutive asymptomatic individuals referred by primary physicians for CAC measurement with EBCT, who underwent repeat screening • Average interscan time was 3. 1 years, and there were 288 deaths • Progression of CAC was significantly associated with mortality regardless of the method used to assess progression (p < 0. 0001) • CAC progression added incremental value in predicting all-cause mortality over baseline score, demographics, and cardiovascular risk factors • A >15 percent yearly increase had a hazard ratio of 2. 98 [48] Budoff MJ, Hokanson JE, Nasir K, et al. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging 2010; 3: 1229.
Metabolic syndrome, diabetes, and incidence and progression of coronary calcium: the Multi-ethnic Study of Atherosclerosis study [49] • Based on MESA study • Metabolic syndrome and DM were associated with a greater incidence of CAC as well as greater risk of progression than those without either • Progression of CAC in metabolic syndrome and diabetes was associated with CHD events with hazard ratios 4 -5 [49] Wong ND, Nelson JC, Granston T, et al. Metabolic syndrome, diabetes, and incidence and progression of coronary calcium: the Multiethnic Study of Atherosclerosis study. JACC Cardiovasc Imaging 2012; 5: 358.
CAC and prognosis in symptomatic patients
CAC and prognosis in symptomatic patients • CAC also has prognostic value in symptomatic patients • However, in symptomatic patients, a CAC score of 0 does not carry the same high NPV as it does in asymptomatic patients • In the CONFIRM registry of 10, 037 patients who underwent both CAC and CT angiography, 13 % of patients with a CAC of 0 had nonobstructive stenosis and 3. 5 % had a >50 percent stenosis [50] Villines TC, Hulten EA, Shaw LJ, et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry. J Am Coll Cardiol 2011; 58: 2533.
Prognostic value of coronary calcification and angiographic stenoses in patients undergoing coronary angiography [51 • 491 symptomatic patients underwent CAG and EBCT at 5 centers • Mean (+/- SE) area under the ROC curve was 0. 75 +/- 0. 02 for CCS, indicating discriminatory power for(CCS this score § moderate 1 patient in the 1 st quartile rangefor 0 predicting to 2. 1) angiographic findings § 2 in 2 nd quartile (CCS range 2. 1 to 75. 3) • 13 CAD death and 8 ACS occurred over 30 +/- 13 months § 8 in 3 rd quartile (CCS range 75. 3 to 397. 1) and 10 inwere 4 th sorted quartile (> 397. 1)order and divided into quartiles of equal size • § Scores in ascending • EBCT- CCS correlate moderately well with angiographic findings [51] Detrano R, Hsiai T, Wang S, et al. Prognostic value of coronary calcification and angiographic stenoses in patients undergoing coronary angiography. J Am Coll Cardiol 1996; 27: 285.
Long-term prognostic value of coronary calcification detected by electronbeam computed tomography in patients undergoing coronary angiography [52] • 88 patients who underwent CAG and EBCT were contacted after a mean of 6. 9 years • Median CAC score - 160 (Range 0 - 7633) • Only 1 of 87 patients with CAC score <20 experienced a hard event during follow-up • Event-free survival was significantly higher for patients with CAC scores <100 than for those with scores >/=100 (RR 3. 20; 95% CI 1. 17 to 8. 71) • Age and CAC- independent predictors of events (RR 1. 72 & 1. 88 respectively; P<0. 05) • In patients undergoing CAG, CAC extent on EBCT is highly predictive of future hard cardiac events and adds valuable prognostic information [52] Keelan PC, Bielak LF, Ashai K, et al. Long-term prognostic value of coronary calcification detected by electron-beam computed tomography in patients undergoing coronary angiography. Circulation 2001; 104: 412.
![Possible effect of treatment in asymptomatic patients Observational studies 53 Retrospective study of Possible effect of treatment in asymptomatic patients Observational studies [53] • Retrospective study of](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-74.jpg)
Possible effect of treatment in asymptomatic patients Observational studies [53] • Retrospective study of 149 patients with no history of CHD -EBCT screening • 65 were treated with a statin at the discretion of their physician • 12 - to 15 -month follow-up • Mean 7 % reduction in the CAC score was noted in the patients on statin therapy who attained a final serum LDL-cholesterol concentration below 120 mg/d. L • In contrast, the CAC score significantly increased by 25 % in the treated patients with higher LDL-cholesterol values and by 52 % in untreated patients who began with LDLcholesterol concentrations above 120 mg/d. L [53] Callister TQ, Raggi P, Cooil B, et al. Effect of HMG-Co. A reductase inhibitors on coronary artery disease as assessed by electron -beam computed tomography. N Engl J Med 1998; 339: 1972.
Influence of lipid-lowering therapy on the progression of coronary artery calcification: a prospective evaluation [54] • 66 patients with CAC on EBCT • Baseline, had a mean serum LDL- 130 mg/d. L and no statin therapy • Cerivastatin lowered serum LDL from 164 to 107 • EBCT was repeated at a mean of 14 months • In the 14 -month follow-up before cerivastatin was started, the median calcified volume • Rx withfrom cerivastatin increased 155 to 201 was then initiated • Median change a 27 % increaseafter in the 14 untreated • And arelative 3 rd EBCT scanwas performed monthsperiod of Rxand 3. 4 % reduction during the treatment period [54] Achenbach S, Ropers D, Pohle K, et al. Influence of lipid-lowering therapy on the progression of coronary artery calcification: a prospective evaluation. Circulation 2002; 106: 1077.
![Possible effect of treatment in asymptomatic patients RCT St Francis Heart Study 55 Possible effect of treatment in asymptomatic patients- RCT St Francis Heart Study [55] •](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-76.jpg)
Possible effect of treatment in asymptomatic patients- RCT St Francis Heart Study [55] • 1005 asymptomatic, apparently healthy men and women th percentile for age and gender • Age 50 to 70 years with CAC scores at or above the 80 • Treatment significantly reduced serum total cholesterol by 27 to 30 percent • All participants by were low dose aspirin andvalue randomly assigned • LDL-cholesterol 39 treated to 43 %with from a mean baseline of 146 mg/d. Ltoto a mean atorvastatin (20 mg/day), vitamin C (1 g/day), and vitamin E (1000 U/day) or matching value below 80 mg/d. L placebos • Treatment had no effect on progression of the CAC score • Primary endpoint was a composite of all atherosclerotic cardiovascular events • No significant difference between primary end point (6. 9 versus 9. 9 percent, p = 0. 08) • Mean follow-up of 4. 3 years • Event rates were directly related to the baseline CAC score [55] Arad Y, Spadaro LA, Roth M, et al. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol 2005; 46: 166.
![BELLES TRIALRCT 56 615 Hyperlipidemic postmenopausal women most with no history of CAD BELLES TRIAL-RCT [56] • 615 Hyperlipidemic postmenopausal women, most with no history of CAD](https://slidetodoc.com/presentation_image_h2/7a6d173158cec66bfd6c2f3adf15865e/image-77.jpg)
BELLES TRIAL-RCT [56] • 615 Hyperlipidemic postmenopausal women, most with no history of CAD • Randomly assigned to intensive (atorvastatin 80 mg/day) or moderate ( pravastatin 40 mg/day) lipid lowering Rx • EBCT CAC scanning at baseline and at a mean of 344 days • Degree of LDL lowering was greater in the atorvastatin group (47 versus 25 %) • There was no difference between the two groups in the degree of CAC progression (15. 1 versus 14. 3 percent) [56] Raggi P, Davidson M, Callister TQ, et al. Aggressive versus moderate lipid-lowering therapy in hypercholesterolemic postmenopausal women: Beyond Endorsed Lipid Lowering with EBT Scanning (BELLES). Circulation 2005; 112: 563.
Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: a multicenter, randomized, double-blind trial [57] • 471 patients (mean age 61 years) • No history of CHD, and no >50 % diameter Potential limitations of these trials include stenosis who had ≥ 2 cardiovascular risk factors, andofanfollow-up EBCT CAC score ≥ 30 (moderate atherosclerosis) 1. Short duration Patients atorvastatin at a dose of either 10 mg or 80 mg/day 2. • First trialwere usedassigned low dosetostatins High dose atorvastatin LDL-cholesterol 3. • Later two trials did notlowered assess clinical outcomefrom 106 to 87 mg/d. L • Lowthe dose atorvastatin had notrials, effectinstituting on LDL-cholesterol Given results of the above pharmacologic therapy to prevent • Atbased one year, CAC progression was similar the recommended two groups (27 versus 25%) CHD solely upon the presence of CAC in is not [57] Schmermund A, Achenbach S, Budde T, et al. Effect of intensive versus standard lipid-lowering treatment with atorvastatin on the progression of calcified coronary atherosclerosis over 12 months: a multicenter, randomized, double-blind trial.
CAC- Summary • CAC is highly sensitive for the presence of ≥ 50 % angiographic stenosis but only moderately specific especially in older patients • Both sensitivity and specificity vary with the degree of CAC; with higher CAC scores, sensitivity decreases but specificity increases • Individual CAC scores should be interpreted in relation to normative data based upon age, sex, and race • Absence of CAC particularly in an asymptomatic patient, is highly predictive of the absence of significant coronary artery stenosis and implies a favourable prognosis • CAC screening can enhance the prediction of risk in asymptomatic individuals and increase the predictive value of the Framingham Risk Score
CAC- Summary • Among asymptomatic patients with a low Framingham risk score (< = 5 %), only a small number § CAC for cardiovascular risk assessment is reasonable in selected asymptomatic adults at (less than 15 %) of those with CAC will have a cardiac event over the ensuing 5 years intermediate risk (10 to 20 % 10 -year risk) when the result is reasonably expected to lead • CAC screening is unlikely to benefit low-risk or high-risk patients, and is not recommended to change in management based upon reclassification to a lower or higher risk group • Instituting or intensifying pharmacologic risk factor modification in asymptomatic patients with CAC will not improve outcomes § CAC measurement is not reasonable in patients low (<6 dose %, (especially 10 -year risk) high (>20 %, • Potential harm associated with false-positive tests andatradiation with or repeated testing) is not known 10 -year) coronary heart disease risk
CABG Graft Stenosis • CABG can usually be imaged with good quality because of their relatively large calibre and the lack of motion of at least their proximal portions • Distal anastomosis can be difficult to assess with confidence because it moves with the coronary artery and its dimensions approximate those of a middle or distal coronary artery segment (i. e. , ≤ 2 mm)
Initial experience with 64 -slice cardiac CT: non-invasive visualization of coronary artery bypass grafts • 64 Slice CTA for 96 bypasses in 31 suspected patients • All bypass grafts and 94% of the distal bypass anastomoses could be visualized by CT • Non-evaluable distal arterial anastomoses were either due to clip material or calcification artefacts • 42 bypass graft occlusions and 3 significant stenoses were detected by CT and confirmed by CAG • Two venous grafts were missed and one arterial graft was not evaluable with CAG, but both were clearly depicted by multi-slice CT • Sensitivity 97. 8%, a specificity 89. 3%, PPV 90%, and NPV 97. 7% Pache G, Saueressig U, Frydrychowicz A, et al. Initial experience with 64 -slice cardiac CT: non-invasive visualization of coronary artery bypass grafts. Eur Heart J 2006; 27: 976.
Improved non-invasive assessment of coronary artery bypass grafts with 64 slice CTA in an unselected patient population • 64 -slice CT and invasive angiography were performed in 138 consecutive patients with a total of 418 bypass grafts • Relevant stenosis was defined as diameter reduction > or =50% • Assessment of stenosis or occlusion of bypass grafts resulted in a sensitivity of 97%, specificity of 97%, and PPV of 93% and NPV of 99%, respectively • Diagnostic accuracy for the detection of graft occlusion or stenosis did not differ between arterial and venous grafts Meyer TS, Martinoff S, Hadamitzky M, et al. Improved noninvasive assessment of coronary artery bypass grafts with 64 -slice computed tomographic angiography in an unselected patient population. J Am Coll Cardiol 2007; 49: 946.
Diagnostic accuracy of non-invasive CTA in patients after bypass surgery using 64 -slice spiral computed tomography with 330 -ms gantry rotation • All CABG grafts were evaluable and correctly classified as occluded or patent. The sensitivity and specificity for stenosis detection in CABG was 100 and 94 percent respectively • In 17 patients, at least one segment of the native coronary circulation was not evaluable and for the purpose of analysis, these patients were labelled as positive for stenosis • Sensitivity and specificity for stenosis detection in native coronary arteries and distal runoff vessels was 97 and 86 % respectively Ropers D, Pohle FK, Kuettner A, et al. Diagnostic accuracy of noninvasive coronary angiography in patients after bypass surgery using 64 -slice spiral computed tomography with 330 -ms gantry rotation. Circulation 2006; 114: 2334.
Coronary artery stents • Stents are difficult to visualize on CCTA because of image reconstruction artifacts in the presence of metal • Large calibre (>3 to 3. 5 mm) stents in the LM, proximal segments of other coronary arteries, or CABG have the highest likelihood of being imaged with diagnostic image quality
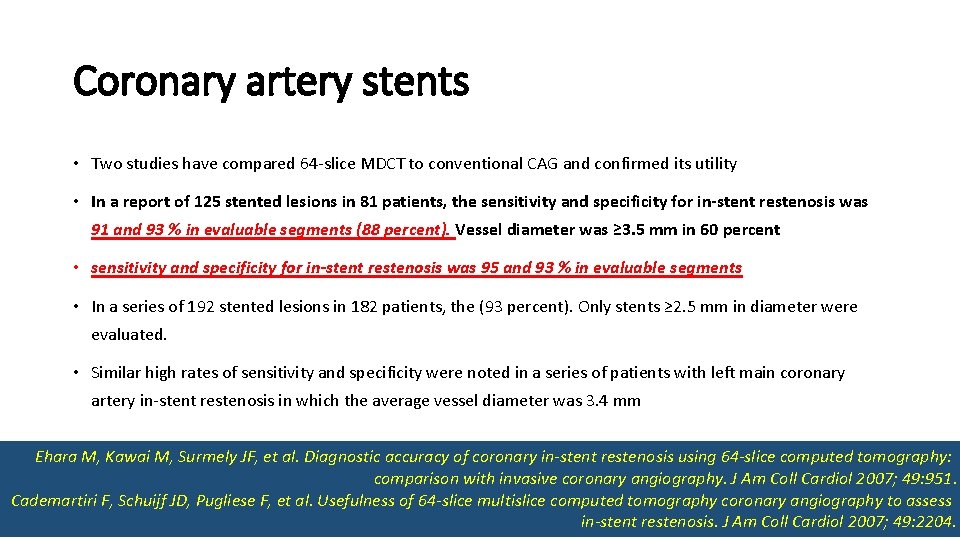
Coronary artery stents • Two studies have compared 64 -slice MDCT to conventional CAG and confirmed its utility • In a report of 125 stented lesions in 81 patients, the sensitivity and specificity for in-stent restenosis was 91 and 93 % in evaluable segments (88 percent). Vessel diameter was ≥ 3. 5 mm in 60 percent • sensitivity and specificity for in-stent restenosis was 95 and 93 % in evaluable segments • In a series of 192 stented lesions in 182 patients, the (93 percent). Only stents ≥ 2. 5 mm in diameter were evaluated. • Similar high rates of sensitivity and specificity were noted in a series of patients with left main coronary artery in-stent restenosis in which the average vessel diameter was 3. 4 mm Ehara M, Kawai M, Surmely JF, et al. Diagnostic accuracy of coronary in-stent restenosis using 64 -slice computed tomography: comparison with invasive coronary angiography. J Am Coll Cardiol 2007; 49: 951. Cademartiri F, Schuijf JD, Pugliese F, et al. Usefulness of 64 -slice multislice computed tomography coronary angiography to assess in-stent restenosis. J Am Coll Cardiol 2007; 49: 2204.
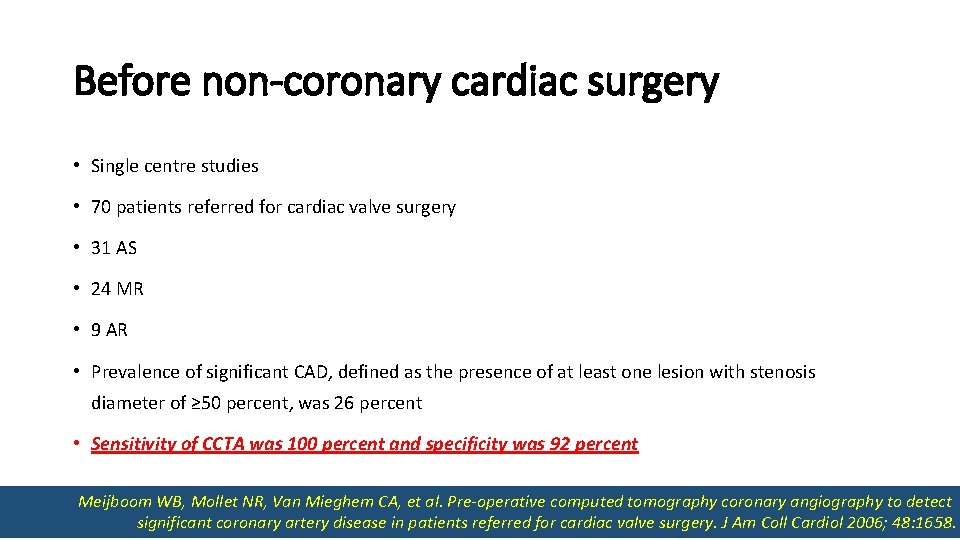
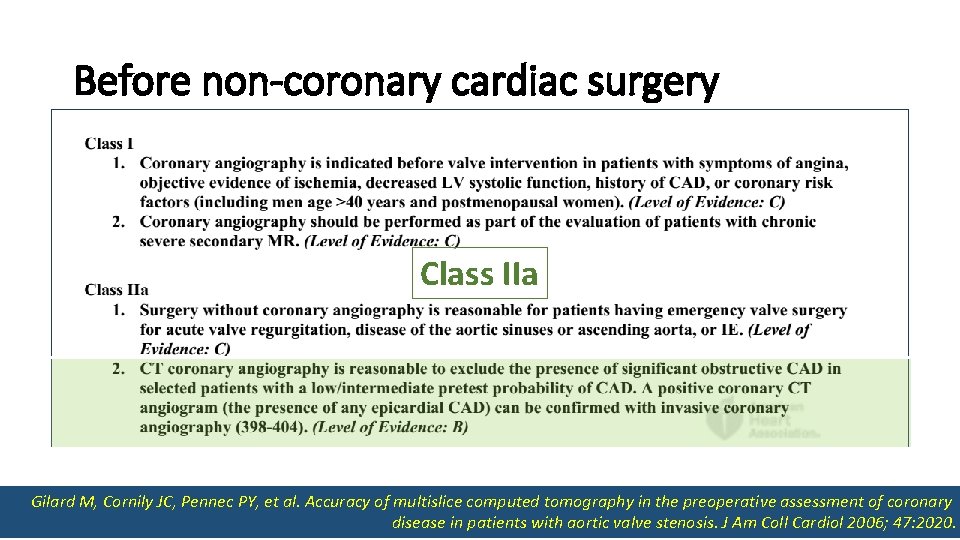
Before non-coronary cardiac surgery • Single centre studies • 70 patients referred for cardiac valve surgery • 31 AS • 24 MR • 9 AR • Prevalence of significant CAD, defined as the presence of at least one lesion with stenosis diameter of ≥ 50 percent, was 26 percent • Sensitivity of CCTA was 100 percent and specificity was 92 percent Meijboom WB, Mollet NR, Van Mieghem CA, et al. Pre-operative computed tomography coronary angiography to detect significant coronary artery disease in patients referred for cardiac valve surgery. J Am Coll Cardiol 2006; 48: 1658.
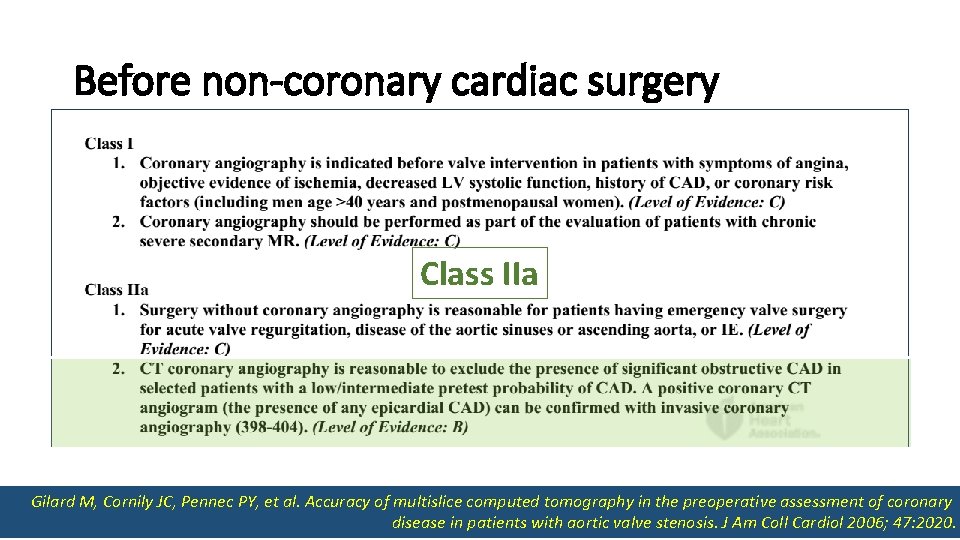
Before non-coronary cardiac surgery • 55 relatively young patients • Referred for valve replacement for AS Class IIa • Prevalence of significant coronary artery disease was 20 % • Sensitivity of CCTA was 100 % and its specificity was 80 % Gilard M, Cornily JC, Pennec PY, et al. Accuracy of multislice computed tomography in the preoperative assessment of coronary disease in patients with aortic valve stenosis. J Am Coll Cardiol 2006; 47: 2020.
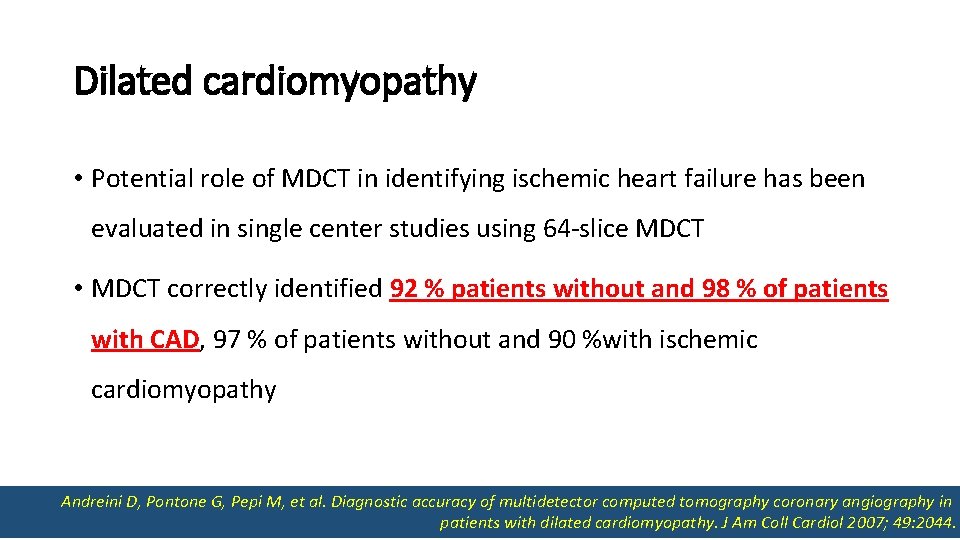
Dilated cardiomyopathy • Potential role of MDCT in identifying ischemic heart failure has been evaluated in single center studies using 64 -slice MDCT • MDCT correctly identified 92 % patients without and 98 % of patients with CAD, 97 % of patients without and 90 %with ischemic cardiomyopathy Andreini D, Pontone G, Pepi M, et al. Diagnostic accuracy of multidetector computed tomography coronary angiography in patients with dilated cardiomyopathy. J Am Coll Cardiol 2007; 49: 2044.
Coronary venography • Anatomy of the coronary venous system is of importance for certain electrophysiology procedures, such as left ventricular epicardial lead placement for CRT • CCTA can define coronary venous anatomy
Summary and Recommendations • CCTA should not be used to screen for CAD in patients who have no signs or symptoms suggestive of CAD • Non-invasive coronary angiography is reasonable for symptomatic patients who are at intermediate risk for CAD after initial risk stratification, including patients with equivocal stress test results. Diagnostic accuracy currently favours CCTA over CMRI for these patients • CCTA is NOT recommended in patients with either a very low pretest likelihood of coronary stenosis or a high pretest likelihood of coronary stenosis • Concerns about radiation exposure limit the use of CCTA in patients with very low likelihood of coronary disease. Patients with high likelihood of coronary artery disease are likely to require invasive coronary angiography and intervention.
Summary and Recommendations • In patients with CABG in whom it is not possible to selectively engage clinical important grafts during invasive angiography, CCTA is reasonable for graft patency • The usefulness of CCTA is reduced in patients with pronounced coronary calcification • CCTA is suggested to evaluate suspected or known congenital or acquired coronary anomalies, particularly to establish the proximal course relative to the great vessels of coronary arteries with abnormal origin

 Thebasian veins
Thebasian veins Equipment used in angiography
Equipment used in angiography Pixel shifting
Pixel shifting Coronary sulcus
Coronary sulcus Heart sounds location
Heart sounds location Coronary personality
Coronary personality Left lung
Left lung Ali sepahdari
Ali sepahdari Cardiac plexus
Cardiac plexus Coronary artery disease
Coronary artery disease Cpr routine
Cpr routine Posterior av groove
Posterior av groove Coronary steal syndrome
Coronary steal syndrome Annulus of vieussens
Annulus of vieussens Anterior cardiac veins of the right ventricle
Anterior cardiac veins of the right ventricle Global registry of acute coronary events
Global registry of acute coronary events Chronic coronary syndrome
Chronic coronary syndrome Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Worm like amphibian
Worm like amphibian Acute coronary syndrome
Acute coronary syndrome Intracapsular but extrasynovial
Intracapsular but extrasynovial Coronary blood flow
Coronary blood flow Coronary circulatory routes
Coronary circulatory routes Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Mesa coronary calcium score
Mesa coronary calcium score Ischemic heart disease
Ischemic heart disease Crash course cardiovascular system
Crash course cardiovascular system Cardiac output animation
Cardiac output animation Coronary circulation of heart
Coronary circulation of heart Function of coronary artery
Function of coronary artery Mesa coronary calcium score
Mesa coronary calcium score Coronary heart disease
Coronary heart disease Coronary calcium score guidelines
Coronary calcium score guidelines Qfr coronary
Qfr coronary Pulmonary semilunar valve
Pulmonary semilunar valve Pk papyrus covered coronary stent system
Pk papyrus covered coronary stent system Cantlie's line
Cantlie's line Coronary circulation
Coronary circulation What is primary sources
What is primary sources Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Why are fibers class evidence
Why are fibers class evidence Class vs individual evidence
Class vs individual evidence Explain how class evidence may be useful.
Explain how class evidence may be useful. Class evidence vs individual evidence
Class evidence vs individual evidence Genetic logical fallacy
Genetic logical fallacy Section 15-2 review evidence of evolution answer key
Section 15-2 review evidence of evolution answer key Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Ap gov review final exam review
Ap gov review final exam review Nader amin-salehi
Nader amin-salehi Example of inclusion and exclusion criteria
Example of inclusion and exclusion criteria Narrative review vs systematic review
Narrative review vs systematic review Debating speaker roles
Debating speaker roles Examples of inverted commas
Examples of inverted commas Rhetorical triangle subject
Rhetorical triangle subject Regretful tone
Regretful tone Welcome address for webinar sample
Welcome address for webinar sample Speaker in poems
Speaker in poems If by rudyard kipling tone
If by rudyard kipling tone Soapstone subject
Soapstone subject Occasion soapstone example
Occasion soapstone example Soapstone audience
Soapstone audience Soapstone rhetorical analysis example
Soapstone rhetorical analysis example Public speaking definitions
Public speaking definitions Dan baker speaker
Dan baker speaker Speaker in the poem
Speaker in the poem Speaker's point of view in poetry
Speaker's point of view in poetry What is the tone of let it go
What is the tone of let it go Speaker definition in poetry
Speaker definition in poetry Speaker listener plot clue
Speaker listener plot clue Html sucks
Html sucks Barbie doll poem theme
Barbie doll poem theme Rhetorical triangle
Rhetorical triangle Intraverbal examples
Intraverbal examples Name title date
Name title date Speaker literature
Speaker literature Situational audience analysis
Situational audience analysis The terrorist he watches
The terrorist he watches Bellshill speaker archives
Bellshill speaker archives Mug #12 answers
Mug #12 answers Speaker biodata
Speaker biodata Going beyond the native speaker in language teaching
Going beyond the native speaker in language teaching Elements of poetry speaker
Elements of poetry speaker James berry poet
James berry poet Asian parliamentary debate speaker roles
Asian parliamentary debate speaker roles Computer, computer basics, input and output devices
Computer, computer basics, input and output devices Guidelines for ethical speaking
Guidelines for ethical speaking Who is the assumed speaker of annabel lee
Who is the assumed speaker of annabel lee Define soapstone literature
Define soapstone literature Adau1701 arduino
Adau1701 arduino Atlas speaker calculator
Atlas speaker calculator Umur andira tiktok
Umur andira tiktok